Multilocus sequence typing of Mycobacterium xenopi
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Multilocus sequence typing of Mycobacterium xenopi
Multilocus Sequence Typing of Mycobacterium xenopi 1
David C. Alexander1,8, Theodore K. Marras2,3,4 Jennifer H. Ma1, Samia Mirza1,2, Daniel 2
Liu1, Julianne V. Kus1,2, Hafid Soualhine5, Vincent Escuyer6, David Warshauer7, Sarah 3
K. Brode3,4, David J. Farrell1, and Frances B. Jamieson1,2 * 4
5
1 Public Health Ontario Laboratories, Public Health Ontario, Toronto, ON, Canada 6
2 University of Toronto, Department of Laboratory Medicine and Pathobiology, Toronto, 7
ON, Canada 8
3 University of Toronto, Department of Medicine, Toronto, ON, Canada 9
4 University Health Network and Mount Sinai Hospital, Department of Medicine, 10
Toronto, ON, Canada 11
5 Laboratoire de Santé Publique du Québec, Institut National de Santé Publique du 12
Québec, Sainte–Anne–de–Bellevue, QC, Canada 13
6 Wadsworth Center, New York State Department of Health, Albany, NY, USA 14
7 Wisconsin State Laboratory of Hygiene, Madison, WI, USA 15
8 Saskatchewan Disease Control Laboratory, Saskatchewan Ministry of Health, Regina, 16
SK, Canada 17
18
19
20
21
* Corresponding author: [email protected] 22
23
24
JCM Accepts, published online ahead of print on 10 September 2014J. Clin. Microbiol. doi:10.1128/JCM.01601-14Copyright © 2014, American Society for Microbiology. All Rights Reserved.
Abstract 25
Mycobacterium xenopi (Mxe) is an opportunistic mycobacterial pathogen of increasing 26
clinical importance. Surveillance of Mxe is hampered by the absence of tools for 27
genotyping and molecular epidemiology. In this study, we describe the development and 28
evaluation of an effective multilocus sequence typing strategy for Mxe. 29
30
Introduction 31
Mycobacterium xenopi (Mxe) is an opportunistic mycobacterial pathogen of increasing 32
clinical importance. Mxe disease is most common among patients with underlying 33
medical conditions (e.g. chronic obstructive pulmonary disease, bronchiectasis, 34
immunodeficiencies) (1-4). Cases usually present as tuberculosis–like pulmonary disease, 35
but extrapulmonary (e.g. bone, joint, and muscle) infections have also been reported (5). 36
37
In North America, Mxe disease is not reportable, so the actual incidence of infection is 38
unknown. However, in a recent global survey of nontuberculous mycobacteria (NTM), 39
Mxe accounted for 8% of all NTM species isolated from pulmonary samples (6). 40
Although rarely seen in Asia, Australia, or South America, Mxe is common in North 41
America and Europe. Isolation frequency is highest in central Europe (e.g. Germany, 42
Italy, Switzerland, Hungary, Croatia, Poland and the Czech Republic), the English 43
Channel region (e.g. southeastern England, northern France, Belgium), and the Great 44
Lakes region of Canada and the United States (6, 7). In Hungary, Mxe is the dominant 45
NTM species and accounts for almost half of all NTM isolated from pulmonary samples 46
(6). In Ontario, Canada, Mxe prevalence is second only to that of the M. avium complex 47
(8). Moreover, population–based studies indicate that, in Ontario, the prevalence of Mxe 48
pulmonary disease has increased from 7.4 cases/100,000 persons during 1998–2002 to 49
9.5 cases/100,000 persons during 2006–2010 (9). 50
51
Surveillance of Mxe is hampered by the absence of effective tools for molecular 52
epidemiology. Restriction fragment length polymorphism (RFLP) methods have been 53
described but are not in routine use, and no public IS1081 or IS1395 RFLP databases 54
exist (10-12). Moreover, RFLP is time consuming, labor–intensive and, like other gel 55
electrophoresis–based typing methods, suffers from poor inter–lab reproducibility and 56
portability. In contrast, multilocus sequence typing (MLST) is readily portable and 57
reproducible. MLST is a DNA sequencing–based method that exploits nucleotide 58
variations present in predefined sets of genetic loci (13, 14). The traditional approach 59
involves Sanger sequencing of PCR amplicons, but MLST is compatible with whole 60
genome sequencing technologies, and thus, is future–proof. MLST schemes have been 61
developed for dozens of bacterial species and some pathogenic fungi. Although not 62
widely used for Mycobacterium species, a MLST scheme for the M. abscessus complex 63
has recently been described (15, 16). In this study, we describe the development and 64
evaluation of an effective MLST strategy for Mxe. 65
66
Materials and Methods 67
Bacterial Strains. A collection of 106 Mxe isolates was assembled for this study. 68
Clinical isolates (n=104) were provided by the Public Health Ontario Laboratories 69
(PHOL; n = 37), the Laboratoire National de Santé Publique du Québec (LSPQ; n = 22), 70
the Wisconsin State Laboratory of Hygiene (WSLH; n = 27), and the Wadsworth Center, 71
New York State Department of Health (WCNY; n = 18). The clinical strains include 72
respiratory isolates cultured from specimens submitted to the source laboratories for 73
routine mycobacterial testing as well as referral isolates sent to the laboratories for 74
identification. Two independent aliquots of the Mxe type strain ATCC 19250T, provided 75
by the LSPQ and WSLH were also examined. All Mxe isolates were submitted to the 76
PHOL for analysis. 77
78
DNA Extraction. Mxe isolates obtained from the PHOL, LSPQ, WSLH and WCNY 79
were subcultured on Lowenstein Jensen slants (Bio–media Unlimited Ltd., Toronto, ON, 80
Canada) and incubated at 40ºC until sufficient growth was observed (4 to 6 weeks). DNA 81
was extracted using a modified boiling lysis method (17). Briefly, a loopful of culture 82
was resuspended in 200 µL buffer (10 mM Tris, 1 mM EDTA, pH 8), vortexed to 83
disperse any clumps, and then heated at 95ºC for 20 minutes. Samples were centrifuged 84
to pellet cellular debris and the DNA–containing supernatant was transferred to a fresh 85
tube and stored at –20ºC until required for downstream applications. 86
87
PCR. Six genes (atpD, fusA1, glnA1, pheT, secA1, and topA) plus the 16S–23S rRNA 88
internal transcribed spacer (ITS) region were used for MLST of Mxe. Primer pairs for 89
each MLST target are listed in Table 1. PCR was performed with the HotStarTaq Plus 90
Master Mix Kit (Qiagen, Louisville, KY, USA). Each 20 µL amplification reaction 91
contained 10 μL of 2× HotStartMM master mix, 2 μL of Q solution, 2 μL of 10× CL 92
buffer, 3 μL of nuclease free water, 1 µL (10 nmol) of each primer, plus 1 μL of crude 93
DNA lysate. PCR was performed for 35 cycles using the following conditions: 94
denaturation (94°C for 45 sec), annealing (57°C for 45 sec), and extension (72°C for 1 95
minute), with a final extension cycle at 72°C for 10 minutes. Agarose gel electrophoresis 96
was used to confirm amplification of each MLST target and estimate amplicon 97
concentration. 98
99
DNA Sequencing. The BigDye Terminator v3.1 Cycle Sequencing Kit (Life 100
Technologies Inc., Burlington, ON, Canada) was used for DNA sequencing of amplicons 101
for MLST. Labelling reactions were performed following the manufacturer’s instructions 102
(Life Technologies). For each MLST target, bidirectional sequencing was performed. 103
Unincorporated dyes were removed by ethanol/EDTA precipitation and the labeled 104
amplicons were resuspended in 10 µL of nuclease–free water. DNA sequencing was 105
performed via capillary electrophoresis with an Applied Biosystems 3730xl DNA 106
Analyzer. Editing, analysis, and alignment of DNA sequences were performed with 107
MEGA 5.2 (18). 108
109
Results 110
MLST. DNA sequencing results for the MLST targets are summarized in Table 2 and 111
Supplementary Table 1. Individual genes were found to have two (atpD), three (fusA1, 112
topA), four (glnA1, pheT) or five (secA1) allelic variants. All single nucleotide 113
polymorphisms (SNPs) associated with the atpD, fusA1, glnA1 and topA1 alleles were 114
synonymous. However, the pheT ST–2 , pheT ST–3, secA1 ST–3 and secA1 ST–5 115
variants contained non–synonymous SNPs. The six locus MLST strategy (MLST–6) 116
divided the 106 Mxe isolates into 15 distinct sequence types (ST). The MLST profile 117
shared by the two aliquots of ATCC19250T was designated ST–1. Most STs were only 118
observed once or twice, but three STs were prevalent among the clinical isolates: ST–2 119
(n= 48; 46.1%), ST–5 (n=23; 22.1%) and ST–9 (n=20; 19.2%). 120
Previous studies have documented the existence of three distinct Mxe 16S–23S rRNA 121
ITS alleles (i.e. Mxe–A, Mxe–B, Mxe–C) (19). As such, the ITS region was selected as a 122
seventh MLST target. However, for some isolates, sequencing of this target was 123
confounded by the presence of multiple, non–identical ITS sequences. Whereas genomes 124
from the majority of ‘slow growing’ mycobacterial species feature a single rRNA operon, 125
the Mxe genome contains two. Because the ITS PCR did not use operon–specific primers, 126
both ITS loci were amplified and sequenced together. Thus, homozygous strains (e.g. ITS 127
A/A) generated ‘clean’ sequences but heterozygous strains (e.g. ITS A/B) generated 128
‘mixed’ electropherograms. By comparing the mixed electropherograms to published ITS 129
sequences, it was possible to identify characteristic mixed base patterns for heterozygous 130
allele combinations (e.g. ITS A/B, ITS A/C, ITS B/C) and assign ITS profiles to all but 131
nine isolates. The seven loci MLST strategy (MLST–7; MLST–6 plus ITS) divided the 132
remaining 97 Mxe isolates into 21 STs (Table 2). In most cases, strains that clustered by 133
six loci MLST also clustered by ITS. For example, all isolates in the ST–9 group shared 134
the same ITS A/A profile. In contrast, ST–2 was subdivided into four ITS clusters (A/A = 135
3, A/B = 26, B/B = 4, B/C = 9), ST–5 was subdivided into three clusters (B/B = 1, B/C = 136
16, C/C = 4), and the ST–13 pair included one A/B and one B/B isolate. 137
138
MLST of Consecutive Isolates from Individual Patients. Table 3 includes MLST–6 139
results for a subset of PHOL strains: 17 consecutive isolates recovered from 7 patients. 140
For five patients, only Mxe isolates of identical ST were recovered. However, the isolates 141
from Patient F were distinct (ST–11 in 2011 and ST–5 in 2012) and the four isolates 142
recovered from Patient G included one of ST–2 and three of ST–9. 143
144
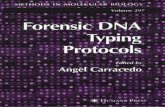
Geographic Distribution of STs. The geographic distribution of MLST–6 defined STs is 145
summarized in Figure 1 and Supplementary Figure 1. Most STs were only observed once 146
or, in the case of the ST–3 and ST–13 pairs, were isolated by a single source laboratory. 147
ST–9 strains were isolated at both the PHOL and LSPQ, and ST–5 strains were isolated 148
at three facilities, but only ST–2 strains were isolated by all four source laboratories. 149
150
Discussion 151
Despite increasing recognition of Mxe as an important human pathogen, little is known 152
about the genetic diversity of this species. MLST is a sequencing–based method that has 153
been used for genotyping of many bacterial species. Traditionally, MLST strategies target 154
‘housekeeping’ or ‘core’ genes, loci that are conserved within the species of interest. For 155
typing to be effective, these targets must also be heterogeneous, such that distinct isolates 156
exhibit distinct sequence polymorphisms. To develop an MLST strategy for Mxe, we 157
initially targeted 19 housekeeping genes: alaS, atpD, dnaK ffh, ftsK, fum, fusA1, gap, 158
gcvB, glnA1, gyrB, hsp65, infB, leuS, pheT, tpi, rpoB, secA1, and topA. Preliminary 159
sequencing results, derived from a panel of 21 Mxe isolates, revealed that 13 of these loci 160
were invariant, and thus, unsuitable for MLST (20). 161
The MLST–6 approach used in this study targets six polymorphic Mxe loci: atpD, fusA1, 162
glnA1, pheT, secA1, and topA. The MLST–7 strategy includes one additional target, the 163
Mxe ITS region. The two approaches were used to genotype a collection of 106 Mxe 164
isolates provided by four mycobacteriology laboratories (Table 2, Figure 1, 165
Supplementary Figure 1). The MLST–6 strategy divided the collection into 15 STs. The 166
MLST–7 strategy provided greater resolution (21 STs) even though genotyping could not 167
be completed for nine isolates. Despite the potential utility of the MLST–7 strategy, 168
technical challenges, especially the requirement for interpretation of ‘mixed’ ITS 169
electropherograms, make the current MLST–7 approach less suitable for routine use than 170
MLST–6. However, if the Sanger sequencing method used here was replaced by a next 171
generation approach, it would be possible to resolve distinct ITS loci and type additional 172
targets. Tools to facilitate such analysis, sometimes called core genome multilocus 173
sequence typing (cgMLST), have recently been described for M. tuberculosis (21). 174
175
For patients with multiple positive cultures or multiple episodes of disease, MLST can be 176
used to distinguish cases of relapse from those of reinfection. MLST–6 analysis of 17 177
consecutive isolates obtained from 7 patients is summarized in Table 3. In six of the 178
seven cases, multiple isolates of identical ST were obtained. These STs persisted over a 179
period of months (Patients C, D, G) to two (Patient A) and three (Patients B, E) years. 180
The two isolates from Patient F were of different STs and isolated in different years, 181
which is consistent with a case of reinfection. However, in the case of Patient G, isolates 182
of ST–2 and ST–9 were obtained within a few months of one another. Since subsequent 183
isolates were also of ST–2, the situation may be indicative of strain replacement. Or, it 184
may represent a polyclonal infection, a phenomenon that is common among patients with 185
infections due to other nontuberculous mycobacteria, such as M. avium (22, 23). 186
187
MLST analysis demonstrates that Mxe isolates are genotypically heterogeneous. Nine of 188
the MLST–6 defined STs, and twelve of the MLST–7 defined STs, were only observed 189
once (Table 2, Figure 1). Because Mxe is an ‘environmental’ mycobacterial species, it is 190
possible that this genotypic diversity is related to geographic distribution. Although ST–2 191
strains were isolated by all four source laboratories, the distribution of other STs was 192
restricted. For example, ST–9 strains were only isolated by the Canadian laboratories, 193
while both ST–3 isolates were collected by WSLH. Most of the PHOL isolates were 194
obtained from patients living in the Greater Toronto Area (GTA) of southern Ontario, but 195
the genotypically distinct ST–15 strain was isolated from a patient in central Ontario. 196
Analysis of the PHOL isolates suggests a geographic trend, with distribution of the ST–5, 197
ST–9 and ST–2 strains restricted to the east/central, north/central, and west regions of the 198
GTA, respectively. Additional isolates and environmental sampling are required to 199
confirm this observation, but Mxe is typically associated with aquatic ecosystems of both 200
natural and anthropogenic origin (24, 25). The geographic distribution of STs in the GTA 201
may overlap with patient exposure to specific engineered (e.g. domestic water reservoirs, 202
distribution systems, hot tubs) or natural (e.g. lakes, rivers, aquifers) water sources. 203
204
The ST–1 profile assigned to Mxe type strain ATCC 19250T was not shared by any of the 205
clinical isolates. Most likely, this is due to the fact that the type strain is from a different 206
place and time (i.e. England, c1958) (26). However, Mxe ATCC 19250T was isolated 207
from the skin of an amphibian (Xenopus laevis), not the respiratory tract of a mammal. 208
As such, the ST differences may be indicative of differences in the pathogenic potential 209
and host preferences of genotypically distinct Mxe populations. Among other 210
mycobacterial species, including the M. tuberculosis complex and M. avium complex, 211
lineage–specific differences in pathogenicity and host range are well documented(27-29). 212
213
Despite its prevalence and increasing clinical importance, little is known about the 214
genetic diversity and molecular epidemiology of Mxe. Gel electrophoresis–based 215
methods are widely considered the ‘gold standard’ for mycobacterial typing and RFLP 216
can been used to differentiate Mxe isolates. Unfortunately, for many laboratories, RFLP 217
is not a practical option for routine typing. In contrast, in an era where labor is expensive 218
but sequencing is cheap, MLST may be a faster and more affordable alternative. With the 219
development of an effective MLST scheme, it becomes possible to routinely examine the 220
distribution, evolution, and population structure of Mxe. Future studies may provide 221
insight into the geographic preferences of specific STs, or uncover associations between 222
Mxe genotype and disease phenotype, antibiotic susceptibility, and pathogenic potential. 223
224
Acknowledgements 225 226 The authors would like to acknowledge the skill and dedication of the laboratory staff 227 from PHOL, LSPQ, WLSH, and WCNY responsible for the initial isolation and 228 cultivation of the M. xenopi isolates used in the study. 229 230
231
References 232 233 1. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, 234
Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ, 235 Jr., Winthrop K, Subcommittee ATSMD, American Thoracic S, Infectious Disease Society of A. 236 2007. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous 237 mycobacterial diseases. Am. J. Resp. Crit. Care Med. 175:367-416. 238
2. Marusic A, Katalinic-Jankovic V, Popovic-Grle S, Jankovic M, Mazuranic I, Puljic I, Sertic Milic 239 H. 2009. Mycobacterium xenopi pulmonary disease - epidemiology and clinical features in non-240 immunocompromised patients. J. Infect. 58:108-112. 241
3. van Ingen J, Boeree MJ, de Lange WC, Hoefsloot W, Bendien SA, Magis-Escurra C, Dekhuijzen 242 R, van Soolingen D. 2008. Mycobacterium xenopi clinical relevance and determinants, the Netherlands. 243 Emerg. Infect. Dis. 14:385-389. 244
4. Varadi RG, Marras TK. 2009. Pulmonary Mycobacterium xenopi infection in non-HIV-infected 245 patients: a systematic review. Int. J. Tuberc. Lung Dis. 13:1210-1218. 246
5. Meybeck A, Fortin C, Abgrall S, Adle-Biassette H, Hayem G, Ruimy R, Yeni P. 2005. Spondylitis 247 due to Mycobacterium xenopi in a human immunodeficiency virus type 1-infected patient: case report 248 and review of the literature. J. Clin. Microbiol. 43:1465-1466. 249
6. Hoefsloot W, van Ingen J, Andrejak C, Angeby K, Bauriaud R, Bemer P, Beylis N, Boeree MJ, 250 Cacho J, Chihota V, Chimara E, Churchyard G, Cias R, Daza R, Daley CL, Dekhuijzen PN, 251 Domingo D, Drobniewski F, Esteban J, Fauville-Dufaux M, Folkvardsen DB, Gibbons N, Gomez-252 Mampaso E, Gonzalez R, Hoffmann H, Hsueh PR, Indra A, Jagielski T, Jamieson F, Jankovic M, 253 Jong E, Keane J, Koh WJ, Lange B, Leao S, Macedo R, Mannsaker T, Marras TK, Maugein J, 254 Milburn HJ, Mlinko T, Morcillo N, Morimoto K, Papaventsis D, Palenque E, Paez-Pena M, 255 Piersimoni C, Polanova M, Rastogi N, Richter E, Ruiz-Serrano MJ, Silva A, da Silva MP, Simsek 256 H, van Soolingen D, Szabo N, Thomson R, Tortola Fernandez T, Tortoli E, Totten SE, Tyrrell G, 257 Vasankari T, Villar M, Walkiewicz R, Winthrop KL, Wagner D, Nontuberculous Mycobacteria 258 Network European Trials G. 2013. The geographic diversity of nontuberculous mycobacteria isolated 259 from pulmonary samples: an NTM-NET collaborative study. Eur. Resp. J. 42:1604-1613. 260
7. Martin-Casabona N, Bahrmand AR, Bennedsen J, Thomsen VO, Curcio M, Fauville-Dufaux M, 261 Feldman K, Havelkova M, Katila ML, Koksalan K, Pereira MF, Rodrigues F, Pfyffer GE, Portaels 262 F, Urgell JR, Rusch-Gerdes S, Tortoli E, Vincent V, Watt B, Spanish Group for Non-Tuberculosis 263 M. 2004. Non-tuberculous mycobacteria: patterns of isolation. A multi-country retrospective survey. Int. 264 J. Tuberc. Lung Dis. 8:1186-1193. 265
8. Marras TK, Chedore P, Ying AM, Jamieson F. 2007. Isolation prevalence of pulmonary non-266 tuberculous mycobacteria in Ontario, 1997-2003. Thorax 62:661-666. 267
9. Marras TK, Mendelson D, Marchand-Austin A, May K, Jamieson FB. 2013. Pulmonary 268 nontuberculous mycobacterial disease, Ontario, Canada, 1998-2010. Emerg. Infect. Dis. 19:1889-1891. 269
10.Collins DM. 1994. DNA Fingerprinting of Mycobacterium xenopi. Lett. Appl. Microbiol. 18:234-235. 270 11.Lenart K, Sajduda A, Augustynowicz-Kopec E, Dziadek J. 2011. Profiling Mycobacterium xenopi 271
with restriction fragment length polymorphism of insertion element IS1395. Int. J. Infect. Dis. 15:e321-272 325. 273
12.Picardeau M, Varnerot A, Rauzier J, Gicquel B, Vincent V. 1996. Mycobacterium xenopi IS1395, a 274 novel insertion sequence expanding the IS256 family. Microbiology 142:2453-2461. 275
13.Maiden MC. 2006. Multilocus sequence typing of bacteria. Ann. Rev. Microbiol. 60:561-588. 276 14.Perez-Losada M, Cabezas P, Castro-Nallar E, Crandall KA. 2013. Pathogen typing in the genomics 277
era: MLST and the future of molecular epidemiology. Infect. Genet. Evol. 16:38-53. 278 15.Kim SY, Kang YA, Bae IK, Yim JJ, Park MS, Kim YS, Kim SK, Chang J, Jeong SH. 2013. 279
Standardization of multilocus sequence typing scheme for Mycobacterium abscessus and Mycobacterium 280 massiliense. Diag. Microbiol. Infect. Dis. 77:143-149. 281
16.Macheras E, Konjek J, Roux AL, Thiberge JM, Bastian S, Leao SC, Palaci M, Sivadon-Tardy V, 282 Gutierrez C, Richter E, Rusch-Gerdes S, Pfyffer GE, Bodmer T, Jarlier V, Cambau E, Brisse S, 283 Caro V, Rastogi N, Gaillard JL, Heym B. 2014. Multilocus sequence typing scheme for the 284 Mycobacterium abscessus complex. Res. Microbiol. 165:82-90. 285
17.Turenne CY, Tschetter L, Wolfe J, Kabani A. 2001. Necessity of Quality-Controlled 16S rRNA 286 Gene Sequence Databases: Identifying Nontuberculous Mycobacterium Species. J. Clin. Microbiol. 287 39:3637-3648. 288
18.Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. 2011. MEGA5: molecular 289 evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum 290 parsimony methods. Mol. Biol. Evol. 28:2731-2739. 291
19.Roth A, Fischer M, Hamid ME, Michalke S, Ludwig W, Mauch H. 1998. Differentiation of 292 phylogenetically related slowly growing mycobacteria based on 16S-23S rRNA gene internal transcribed 293 spacer sequences. J. Clin. Microbiol. 36:139-147. 294
20.Mirza S, Farrell DJ, Marras TK, Ma JH, Liu D, Alexander DC, Kus JV, Jamieson FB. 2013. 295 Sequence-based typing of clinical isolates of Mycobacterium xenopi isolated from Ontario, Canada. J. 296 Undergrad. Life Sci. 7:41-45. 297
21.Kohl TA, Diel R, Harmsen D, Rothganger J, Walter KM, Merker M, Weniger T, Niemann S. 298 2014. Whole-Genome-Based Mycobacterium tuberculosis Surveillance: a Standardized, Portable, and 299 Expandable Approach. J. Clin. Microbiol. 52:2479-2486. 300
22.Fujita K, Ito Y, Hirai T, Kubo T, Maekawa K, Togashi K, Ichiyama S, Mishima M. 2014. 301 Association between polyclonal and mixed mycobacterial Mycobacterium avium complex infection and 302 environmental exposure. Ann. Am. Thorac. Soc. 11:45-53. 303
23.Wallace RJ, Jr., Zhang Y, Brown BA, Dawson D, Murphy DT, Wilson R, Griffith DE. 1998. 304 Polyclonal Mycobacterium avium complex infections in patients with nodular bronchiectasis. Am. J. 305 Resp. Crit. Care Med. 158:1235-1244. 306
24.Sebakova H, Kozisek F, Mudra R, Kaustova J, Fiedorova M, Hanslikova D, Nachtmannova H, 307 Kubina J, Vraspir P, Sasek J. 2008. Incidence of nontuberculous mycobacteria in four hot water 308 systems using various types of disinfection. Can. J. Microbiol. 54:891-898. 309
25.Vaerewijck MJ, Huys G, Palomino JC, Swings J, Portaels F. 2005. Mycobacteria in drinking water 310 distribution systems: ecology and significance for human health. FEMS Microbiol. Rev. 29:911-934. 311
26.Schwabacher H. 1959. A strain of Mycobacterium isolated from skin lesions of a cold-blooded animal, 312 Xenopus laevis, and its relation to atypical acid-fast bacilli occurring in man. J. Hyg. 57:57-67. 313
27.Manabe YC. 2002. Naturally Attenuated, Orally Administered Mycobacterium microti as a 314 Tuberculosis Vaccine Is Better than Subcutaneous Mycobacterium bovis BCG. Infect. Immun. 70:1566-315 1570. 316
28.Perez-Lago L, Navarro Y, Garcia-de-Viedma D. 2013. Current knowledge and pending challenges in 317 zoonosis caused by Mycobacterium bovis: A review. Res. Vet. Sci. DOI: 10.1016/j.rvsc.2013.11.008 318
29.Turenne CY, Alexander DC. 2010. Mycobacterium avium Complex, p. 60-71. In Behr MA, Collins 319 DM (ed.), Paratuberculosis: Organism, Disease, Control. CAB International. 320
321
0
10
20
30
40
50
2 3 4 5 6 7 8 9 10 11 12 13 14 15
Sequence Type (MLST-6)
# I
sola
tes
Figure 1. Geographic Distribution of Mycobacterium xenopi MLST-6 Sequence Types.
Isolates from PHOL (black), LSPQ (grey), WSLH (hatched), and WCNY (white) are shown.
Table 1. Oligonucleotide Primers for MLST Analysis of Mycobacterium xenopi
Target Primer 1 Primer 2 Size (bp) Function atpD 5'-CGGTGTTCTCCAAGGGCATC-3' 5'-TTGTCGGTGTTGTCGGCCTG-3' 499 ATP synthase (subunit β) fusA1 5'-GCATCATGGCGCACATCGAC-3' 5'-TTCATCTCGACCAGGTCGACGACG-3' 505 Elongation factor G glnA1 5'-ATTCTGCACCATGCGCCTTC-3' 5'-ACACGTCGAAGTACAGCGCG-3' 511 Glutamine synthetase pheT 5'-TACAGCTGGCTGCGCGAAGT-3' 5'-ATGGCCAGGTGGAACACCACGT-3' 494 Phenylalanyl-tRNA synthetase (subunit β) secA1 5'-CGAGCACCTCTACGAGATGG-3' 5'-TTAGCGCTTCTTGGCCGATT-3' 502 Preprotein translocase topA 5'- AAAACCCGCTCGCCCCAAAC-3' 5'- GTGCCTTGCGGGTCGTCTTCTT-3' 515 DNA topoisomerase I ITS 5’-TTGTACACACCGCCCGTCA-3’ 5’-TCTCGATGCCAAGGCATCCACC-3’ 445 16S-23S rRNA Internal Transcribed Spacer
Table 2. MLST Analysis of Mycobacterium xenopi
MLST-6 atpD fusA1 glnA1 pheT secA1 topA ITS # Isolates†
ST-1 1 1 1 1 1 1 AA 2
ST-2 1 1 1 1 2 1 variable1 48
ST-3 1 1 1 1 3 1 AB 2
ST-4 1 1 1 1 1 2 CC 1
ST-5 1 1 1 1 2 2 variable2 23
ST-6 1 1 2 1 2 1 BC 1
ST-7 1 1 3 1 2 2 CC 1
ST-8 1 1 3 1 2 3 CC 1
ST-9 1 1 2 2 2 1 AA3 20
ST-10 1 1 4 3 4 1 AC 1
ST-11 1 1 2 2 2 2 AA 1
ST-12 1 1 4 4 5 3 CC 1
ST-13 1 2 1 1 2 2 variable4 2
ST-14 1 3 1 1 2 1 AB 1
ST-15 2 1 2 2 2 1 AA 1
† Duplicate isolates (i.e. genotypically identical isolates from individual patients; see Table 3) were only counted once.
1 ST-2 isolates were associated with multiple ITS patterns: AA (n=3), AB (n=26), BB (n=4), BC (n=9), non-typable (n=6)
2 ST-5 isolates were associated with multiple ITS patterns: BB (n=1), BC (n=16), CC (n=4), non-typable (n=2)
3 The ITS of one ST-9 isolate was non-typable
4 ST-13 isolates were associated with two ITS patterns: AB (n=1) and BB (n=1)
Table 3: MLST-6 Analysis of Consecutive Isolates from Individual Patients
Patient Isolate Date MLST-6
A 1 10/2010 ST-5 2 11/2011 ST-5
B 1 08/2010 ST-15 2 08/2012 ST-15
C 1 09/2010 ST-5 2 10/2010 ST-5
D 1 09/2012 ST-2 2 11/2012 ST-2
E 1 2009 ST-5 2 10/2010 ST-5 3 01/2011 ST-5
F 1 10/2010 ST-11 2 01/2012 ST-5
G
1 02/2012 ST-2 2 04/2010 ST-9 3 08/2012 ST-9 4 10/2012 ST-9