A Novel Approach to Energy Ablative Therapy of Small Renal Tumours: Laparoscopic High-Intensity...
-
Upload
independent -
Category
Documents
-
view
4 -
download
0
Transcript of A Novel Approach to Energy Ablative Therapy of Small Renal Tumours: Laparoscopic High-Intensity...
123
4
5
6
7
8
9
101112
13
14
EURURO 2293 1–9
UN
CO
RR
EC
TED
PR
OO
FLaparoscopy
A Novel Approach to Energy Ablative Therapy of Small RenalTumours: Laparoscopic High-Intensity Focused Ultrasound
H. Christoph Klingler a,*, M. Susani b, R. Seip c, J. Mauermann a, N. Sanghvi c, M. Marberger a
aDepartment of Urology and Pathology, Medical University of Vienna, Vienna, AustriabDepartment of Pathology, Medical University of Vienna, Vienna, AustriacAustria, Focus Surgery Inc, Indianapolis, IN, USA
e u r o p e a n u r o l o g y x x x ( 2 0 0 7 ) x x x – x x x
avai lab le at www.sciencedi rect .com
journa l homepage: www.europeanurology.com
Article info
Article history:Accepted November 7, 2007Published online ahead ofprint on � � �
Keywords:Laparoscopic HIFURenal cell cancerLaparoscopyLaparoscopic partialnephrectomyEnergy ablative techniquesHigh-intensity focusedultrasoundHIFU
Abstract
Objective: High-intensity focused ultrasound (HIFU) permits targetedhomogeneous ablation of tissue. The objective of this phase 1 studywas to evaluate the feasibility of HIFU ablation of small renal tumoursunder laparoscopic control.Patients and methods: Ten kidneys with solitary renal tumours weretreated with a newly developed 4.0 MHz laparoscopic HIFU probe. Inthe first two patients with 9-cm tumours, a defined marker lesion wasplaced prior to laparoscopic radical nephrectomy. In eight patients witha mean tumour size of 22 mm (range, 11–40), the tumour was completelyablated as in curative intent, followed by laparoscopic partial nephrect-omy in seven tumours. One patient had post-HIFU biopsies and wasfollowed radiologically. Specimens were studied by detailed and whole-mount histology, including NADH stains.Results: Mean HIFU insonication time was 19 min (range, 8–42), with amean targeted volume of 10.2 cm3 (range, 9–23). At histological evalua-tion both marker lesions showed irreversible and homogeneous thermaldamage within the targeted site. Of the seven tumours treated andremoved after HIFU, four showed complete ablation of the entiretumour. Two had a 1- to 3-mm rim of viable tissue immediately adjacentto where the HIFU probe was approximated, and one tumour showed acentral area with about 20% vital tissue. There were no intra- or post-operative complications related to HIFU.Conclusion: The morbidity of laparoscopic partial nephrectomy mainlycomes from the need to incise highly vascularized parenchyma. Tar-geted laparoscopic HIFU ablation may render this unnecessary, butfurther studies to refine the technique are needed.
# 2007 Published by Elsevier B.V. on behalf of European Association of Urology.
* Corresponding author. Department of Urology, Medical University of Vienna,Waehringer Guertel 18-20, A-1090 Vienna, Austria. Tel. +43 1 404 00 2616; Fax: +43 1 408 99 66.E-mail address: [email protected] (H.C. Klingler).
0302-2838/$ – see back matter # 2007 Published by Elsevier B.V. on behalf of European Association of Urology. doi:10.1016/j.eururo.2007.11.020
Please cite this article in press as: Klingler HC, et al., A Novel Approach to Energy Ablative Therapy of Small Renal Tumours:
Laparoscopic High-Intensity Focused Ultrasound, Eur Urol (2007), doi:10.1016/j.eururo.2007.11.020
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
EURURO 2293 1–9
e u r o p e a n u r o l o g y x x x ( 2 0 0 7 ) x x x – x x x2
E
67
68
69
70
71
72
73
74
75
76
77
78
79
80
81
82
83
84
85
86
87
88
89
90
91
92
93
94
95
96
97
98
99
100
101
102
103
104
105
106
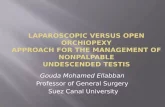
Fig. 1 – Intraoperative setup with laparoscopic high-
intensity focused ultrasound (HIFU) probe in place (center),
HIFU treatment unit (left), and laparoscopic ultrasound
probe (right).
UN
CO
RR
1. Introduction
Renal tumours with a diameter <4 cm are reliablycured by partial nephrectomy [1,2], but there is anassociated complication rate of up to �15%, whichmainly comes from the need to incise the highlyperfused renal parenchyma [3]. Less invasive energyablative techniques avoiding this therefore appearattractive, especially when performed through apercutaneous route. Percutaneous needle ablationusing radiofrequency has been utilized extensivelyfor this purpose, but recent meta-analyses reflectresidual tumour/early recurrences in up to 14–18% ofpatients [4,5]. Reports on needle cryoablation givesimilar failure rates [6,7]. The obvious problemcomes from the need for precise percutaneousneedle placement in a mobile organ and a fairlysmall target. Energy ablative techniques adminis-tered under laparoscopic control are more reliablebecause the needles can be placed under visual andlaparoscopic ultrasonography control. Radiofre-quency ablation has an inherent problem of skip-ping even in this situation [8], but cryoablationachieves reliable tumor ablation, with residual/recurrent tumour rates of 1.6% with follow-up over3 yr [9]. Nevertheless, the tumour still has to bepunctured, which may result in bleeding [10] andcarries an inherent risk of tumour cell spillage [11]. Atechnique ablating the tumour clearly appears moreattractive.
High-intensity focused ultrasound (HIFU) avoidsthe need to puncture because ultrasound waves arefocused to achieve high temperatures sufficient forimmediate thermal destruction of all tissues withinthe target zone. Ideally this procedure is done by anextracorporeal approach; however, because of theacoustic complexity of intervening structures andthe mobility of the kidney, attempts at this approachwere unsatisfactory [12]. Such problems are avoidedif the HIFU transducer is brought directly to thetarget (ie, with laparoscopic HIFU). This studyexamines the histological effects of laparoscopicHIFU ablation of small renal tumours to determinethe viability of the approach from the standpoint ofcomplete tumour ablation and potential technicallimitations.
2. Materials and methods
After being approved by the Institutional Ethics Review Board
(EK 536/2005), we conducted this clinical phase 1 study
between November 2006 and March 2007. The selection for
oncological treatment was based on standard surgical
principles (laparoscopic radical nephrectomy for large
tumours, laparoscopic partial nephrectomy in tumours
Please cite this article in press as: Klingler HC, et al., A Novel A
Laparoscopic High-Intensity Focused Ultrasound, Eur Urol (2007),
CTE
D P
RO
OF
<4 cm, and palliative renal tumour treatment in metastasized
renal cell carcinoma [RCC]). Ten patients with a solitary renal
mass suspicious for RCC on the basis of helical computed
tomography (CT) or magnetic resonance imaging (MRI) scans
were treated with laparoscopic HIFU. In two patients with
9-cm tumours, a defined marker lesion was generated with
HIFU at the external side of the tumour followed immediately
by laparoscopic radical nephrectomy to prove feasibility of the
technique. HIFU ablation of the entire tumour with a margin of
2–3 mm of surrounding parenchyma (‘‘curative intent’’) was
performed in the remaining eight patients with small tumors.
In seven patients, laparoscopic partial nephrectomy with
temporary clamping of the renal artery was conducted post-
HIFU as described elsewhere [8]. The plane of resection was
well outside of the treatment zone to be able to evaluate the
extent of ablation and to prove efficacy of HIFU ablation. In
patient 10 who had high comorbidity and proven lung
metastases, the tumour was not excised after HIFU, but the
same target zone was treated twice. Biopsies were performed
before and after HIFU. The patient was subsequently followed
with helical CT scans.
Laparoscopic surgical access, with the use of four 12-mm
access ports, was performed under general anesthesia as a
standard transperitoneal procedure with the patient in a 458lateral decubitus position. In all patients, the diseased kidney
was completely mobilized and cleared of fat. The hilar
structures were dissected, but the artery was not primarily
occluded. Intraoperative renal power Doppler ultrasonogra-
phy was performed with a 10-Hz laparoscopic ultrasound
probe (BK Medical, Denmark) to precisely locate the renal
lesion to be treated. Prior to HIFU treatment, two core tumour
biopsies were obtained from the tumour with an 18-G biopsy
needle (Boston Scientific, USA). One port was then changed to
an 18-mm port (Ethicon, USA) to allow access for the HIFU
probe.
The laparoscopic HIFU system (Sonatherm1, Misonix Inc,
Farmingdale, NY, USA) used consisted of the treatment
console, an articulated probe arm, a pump unit, and the
laparoscopic probe (Fig. 1). The latter is gas-sterilisable and
covered with a flexible bolus through which gas-free cold
pproach to Energy Ablative Therapy of Small Renal Tumours:
doi:10.1016/j.eururo.2007.11.020
CTE
D P
RO
OF
107
108
109
110
111
112
113
114
115
116
117
118
119
120
121
122
123
124
125
126
127
128
129
130
131
132
133
134
135
136
137
138
139
140
141
142
143
144
145
146
147
148
149
150
151
152
153
154
155
156
157
158
159
160
161
162
Fig. 2 – Intraoperative view of laparoscopic high-intensity
focused ultrasound of lower pole renal cell cancer; the
kidney is held in place with an endoretractor.
Fig. 3 – Marker lesion in large renal cell cancer (patient no. 2).
(a) Overview: The area within the dotted line shows
‘‘homogeneous severe thermal damage’’ (a), viable tissue
(v). (Hematoxylin-eosin stain; original magnification: T40.)
(b) Detail of 3a, showing ‘‘severe thermal damage’’defined
as diffuse pycnosis of nuclei, rupture of cell membranes,
erythrocytes with disrupted cell membranes.
(Hematoxylin-eosin stain; original magnification: T200.)
e u r o p e a n u r o l o g y x x x ( 2 0 0 7 ) x x x – x x x 3
EURURO 2293 1–9
UN
CO
RR
Ewater is circulated for cooling. The probe is inserted through
an 18-mm port to be brought into direct contact with the
tumour (Fig. 2). HIFU energy is delivered by a truncated
spherical shell 4-MHz transducer with a 30 � 13 mm aperture
and 35-mm focal length. Real-time imaging of the target area
in two planes is provided with an integrated single-element,
12-mm diameter imaging transducer aligned confocally with
the therapy transducer [13,14]. HIFU ablation was performed
in a ‘‘continuous ON’’ mode with the transducer moved under
computer control in a two-dimensional pattern within the
outlined treatment zone. HIFU delivery was interrupted every
30 s to obtain ultrasound images in two planes so that the
treatment process could be monitored. In addition to
continuous registration of areas covered by the focal zone,
energy deposition was also assessed qualitatively by examin-
ing hyperechoic changes in the treatment zone resulting from
boiling and cavitation events. The system was calibrated
according to results obtained in experimental studies in
porcine kidneys [14,15] to ablate tissue at an average rate of
0.6 cm3/min at typical power level between 30–38 W. The area
ablated by the probe has the shape of an ‘‘arctangle,’’ the
length and angular extent of which were defined by the
physician, so that the tumour was completely contained
within it. If, owing to tumour size, location, access port
placement, or probe geometry, the tumor area could not be
completely covered by a single treatment segment, a second
overlapping treatment segment was used to completely ablate
the entire tumour volume. The transducer’s focal length limits
the maximum HIFU penetration depth to approximately
35 mm. The maximum linear scanning extent of the transdu-
cer is 50 mm and the maximum angular scanning extent is 908.Specimens were sent for frozen section to check margin
status. Tumour specimens were thereafter evaluated by whole
mount, serial section hematoxylin-eosin staining, and exten-
sive histopathological evaluation. Before fixation in formal-
dehyde, one central slice of tumor tissue was snap-frozen in
liquid nitrogen for histochemical nicotinamide adenine
dinucleotide (NADH) staining, which was used as a marker
for irreversible heat damage [16]. ‘‘Severe thermal tissue
damage’’ was defined as homogeneous intravascular disrup-
Please cite this article in press as: Klingler HC, et al., A Novel A
Laparoscopic High-Intensity Focused Ultrasound, Eur Urol (2007),
tion of erythrocyte membranes, vacuolisation of tumour and
arterial smooth muscle cells, pycnosis and elongation of
tumour cell nuclei, rupture of tumour cell membranes, and
cell detachment throughout the area being investigated
(Fig. 3b). In our experience, severe thermal tissue damage
leads to irreversible and complete tissue necrosis if the time
between HIFU and removal of the specimen is longer [16]. In
addition, NADH staining of the entire region had to be negative
[17,18].
Patients were followed a mean 7.2 mo (range, 6–11) with
serum creatinin, renal ultrasonography, and helical contrast-
enhanced CT scan or MRI obtained at 1, 3, and 6 mo.
3. Results
Table 1 summarises patient characteristics prior totreatment, the treatment protocol used in individualpatients, and the final histological results.
pproach to Energy Ablative Therapy of Small Renal Tumours:
doi:10.1016/j.eururo.2007.11.020
ETE
D P
RO
OF
163
164
165
166
167
168
169
170
171
172
173
174
175
176
177
178
179
180
181
182
183
184
185
186
187
188
189
190
191
192
Table 1 – Pertinent patient characteristics and treatment details
Patno.
Age(yr)
Tumoursize
(mm)
Intentionto treat
Treatment details Targetedvolume
Final histologyof tumour
Severe thermaldamage ablation
within target
1 54 90 Marker 2 treatment zones 11 cm3 (33 W) Clear-cell RCC pT3a, G2 100%
Lap N 2.4 cm � 328: 13:58 min 9 cm3 (34 W)
2.0 cm � 428: 15:09 min
2 65 90 Marker 2 treatment zones 9 cm3 (35 W) Clear-cell RCC pT3b, G4 100%
Lap N 2.0 cm � 328: 17:09 min 5 cm3 (35 W)
and 1.4 cm � 248: 8:45 min
3 42 28 Curative 1 treatment zone 15 cm3 (30–32 W) Clear-cell RCC pT1a, G2 95%
Lap NSS 2.8 cm � 468: 31:39 min
4 77 25 Curative 1 treatment zone 7 cm3 (34–38 W) Clear-cell RCC pT1a, G2 96%
Lap NSS 2.3 cm � 268: 9:50 min
5 50 15 Curative 1 treatment zone 15 cm3 (32–33 W) Angiomyolipoma 100%
Lap NSS 2.6 cm � 508: 24:35 min
6 75 20 Curative 1 treatment zone 21 cm3 (33–36 W) Chronic inflammatory cyst 100%
Lap NSS 3.6 cm � 528: 30:16 min
7 79 10 Curative 1 treatment zone 5 cm3 (30 W) Clear-cell RCC pT1a, G2 80%
Lap NSS 1.6 cm � 268: 10:06 min skipping
8 33 48 Curative 1 treatment zone 23 cm3(30–34 W) Angiomyolipoma 100%
Lap NSS 3.4 cm � 588: 41:50 min
9 75 12 Curative 1 treatment zones 8 cm3 (35–37 W) Clear-cell RCC pT1a, G2 100%
Lap NSS 2.4 cm � 328: 13:58 min
10 55 23 Ablative 1 treatment zone treated twice 5 cm3 (35–37 W) Clear-cell RCC pT1a, G2 100%
Lap Bx 1.8 cm � 268: 7:46 min
Pat, patient; Lap N, laparoscopic nephrectomy; Lap NSS, laparoscopic nephron-sparing surgery; Lap Bx, laparoscopic biopsy; RCC, renal cell
carcinoma.
Fig. 4 – Renal cell cancer treated with curative intent
showing a subcapsular rim of viable tissue adjacent to
entry of high-intensity focused ultrasound energy (v) with
otherwise homogenous severe thermal damage of entire
tumor (a) (patient no. 3). (Hematoxylin-eosin stain; original
magnification: T40.)
e u r o p e a n u r o l o g y x x x ( 2 0 0 7 ) x x x – x x x4
EURURO 2293 1–9
UN
CO
RR
Respiratory movement and/or kidney morbiditydid not impact delivery of HIFU energy. Comparisonof images taken at treatment planning with thoseduring insonication showed that target motion wasalways <5 mm.
The two marker lesions in patients 1 and 2 withextensive RCC showed homogenous severe thermaldamage that matched the site and volume targetedalmost precisely (Fig. 3a and b).
The mean diameter of the tumours treated in‘‘curative intent’’ in patients 3–10 was 22 mm(range, 11–48). Mean HIFU exposure time was19 min (range, 8–42), whereas the time needed forthe entire HIFU procedure (including port place-ment, probe insertion and positioning, treatmentplanning, and probe removal) was 39 min (range,27–59). Patients 3 and 4 showed a subcapsular rim of1–3 mm of vital tissue immediately adjacent towhere the HIFU probe was approximated to thekidney, with otherwise homogenous severe ther-mal damage of the entire tumour (Fig. 4). Assumingthat this outcome was caused by too aggressivecooling of the probe, we subsequently increased thetemperature of the coolant to 18 8C, and thisobservation was not experienced again. The tumour
Please cite this article in press as: Klingler HC, et al., A Novel A
Laparoscopic High-Intensity Focused Ultrasound, Eur Urol (2007),
Ctreated in patient 7 showed vital tissue in about 20%of the tumour, located centrally, with homogenoussevere thermal damage of the rest (Fig. 5). The otherfour tumours removed by partial nephrectomy afterHIFU were all found to have homogenous severe
pproach to Energy Ablative Therapy of Small Renal Tumours:
doi:10.1016/j.eururo.2007.11.020
CTE
D P
RO
OF
193
194
195
196
197
198
199
200
201
202
203
204
205
206
207
208
209
210
211
212
213
214
215
216
217
218
219
220
221
222
223
224
225
226
227
228
229
230
231
232
233
234
235
236
237
Fig. 5 – Renal cell cancer treated with curative intent with
homogeneous severe thermal damage within dotted line,
but viable tissue shown centrally (patient no. 7).
Fig. 6 – Renal cell cancer treated with curative intent
(patient no. 9). (a) Overview: The entire tumor shows
homogeneous severe thermal damage including margins
of normal parenchyma; viable tissue is only outside
treatment zone (v). (Hematoxylin-eosin stain; original
magnification: T40.) (b) Histochemical nicotinamide
adenine dinucleotide (NADH) stain from same patient.
Black arrows: positive NADH staining in a rim of normal
renal parenchyma (v); red arrows: homogeneous severe
thermal damage (a) with complete depletion of NADH.
e u r o p e a n u r o l o g y x x x ( 2 0 0 7 ) x x x – x x x 5
EURURO 2293 1–9
UN
CO
RR
Ethermal damage of the entire tumour withoutevidence of skip lesions (Fig. 6).
In patient 10 intraoperative power Doppler ultra-sonography showed no sign of residual perfusionafter HIFU ablation, and core biopsies taken imme-diately thereafter likewise demonstrated homoge-nous severe thermal damage. Follow-up helical CTscans after 3 and 6 mo showed no contrastenhancement and shrinking of the lesion.
Patient 1 had a tumour 9 cm in diameter in theupper half of the left kidney. At radical nephrectomythe tail of the pancreas was lacerated when the leftadrenal gland was removed. This complicationresulted in prolonged wound drainage, but requiredno further treatment. Otherwise no complicationswere observed in the entire group. Follow-up for allpatients now is a mean 7.2 mo (range, 6–11). Follow-up CT scans showed no evidence of hematoma,residual/recurrent tumour, or any other abnorm-ality.
4. Discussion
As an ultrasound wave propagates through biolo-gical tissues, it is progressively absorbed and itsmechanical energy converted to heat. If brought toa tight focus at a selected depth within tissues(HIFU), the high energy density produced in thisregion rapidly results in temperatures exceedingthe threshold of irreversible protein degradationand subsequently coagulative necrosis [19]. Theenergy decreases sharply outside the focal zone, sothat surrounding tissues remain unharmed. This
Please cite this article in press as: Klingler HC, et al., A Novel A
Laparoscopic High-Intensity Focused Ultrasound, Eur Urol (2007),
permits targeted ablation within organs withoutthe need of directly accessing the target site. Asheat generation is extremely rapid, potential heatsinks such as large blood vessels impact lesioningto a lesser degree than with other, slowertechniques of thermal ablation [19]. Obviouslyfor the same reason, HIFU of malignant tumourshas not been shown to cause tumour cell dis-semination or an increased rate of metastases[20,21].
Unfortunately these principles of HIFU ablationalso require fairly homogeneous tissue structureswithout significant acoustic interphases along thepath of ultrasound delivery and a stationary target
pproach to Energy Ablative Therapy of Small Renal Tumours:
doi:10.1016/j.eururo.2007.11.020
E
238
239
240
241
242
243
244
245
246
247
248
249
250
251
252
253
254
255
256
257
258
259
260
261
262
263
264
265
266
267
268
269
270
271
272
273
274
275
276
277
278
279
280
281
282
283
284
285
286
287
288
289
290
291
292
293
294
295
296
297
298
299
300
301
302
303
304
305
306
307
308
309
310
311
312
313
314
315
316
317
318
319
320
321
322
323
324
325
326
327
328
329
330
331
332
333
334
335
336
337
338
339
340
341
342
343
344
345
e u r o p e a n u r o l o g y x x x ( 2 0 0 7 ) x x x – x x x6
EURURO 2293 1–9
UN
CO
RR
for precise energy deposition. Clinically this can beachieved trans-scrotally to the testis [22], transrec-tally to the prostate [19,23], and even to the kidneywhen the organ is surgically exposed [16]. HIFU ofrenal tumors by an extracorporeal approach hasproven unreliable both in animal experiments andclinical pilot studies [24–26]. The acoustical com-plexity of the abdominal wall and perirenal struc-tures, and the mobility of the kidney are eliminatedif the transducer is brought directly to the kidney.With the laparoscopic HIFU transducer with anoverall diameter of 18 mm used in this study, thisapproach becomes feasible with standard laparo-scopy techniques and equipment. Albeit moreinvasive than an extracorporeal HIFU approach,the time needed compares well with laparoscopiccryoablation. The morbidity of nephron-sparingexcision of renal tumours mainly arises from theneed to incise the renal parenchyma, with orwithout clamping the renal artery [3]. This compli-cation is avoided by laparoscopic HIFU ablation. NoHIFU-specific complications were observed in thestudy.
Homogeneous and severe thermal damage of theentire targeted zone was documented histologicallyin six of nine masses. Not all lesions treated wereconfirmed to be RCC. In a similar study of radio-frequency ablation, angiomyolipomas and septated,cystic tumours showed most pronounced skipping[8]. In contrast all nonmalignant tumours treatedherein, including the vascularised angiomyolipomaand the complex cyst, showed homogeneous severethermal damage of the entire lesion and 2–3 mm ofsurrounding parenchyma. The superficial zone ofvital tissue observed in two of the first patients withrenal cancer treated with curative intent wasassumed to result from overzealous cooling of theHIFU probe. It was not observed again when thecooling was limited to 18 8C. It may also haveresulted from insufficient energy coupling fromthe probe bolus to the kidney at HIFU insonication,which was routinely performed by securing thekidney in place with a fan retractor and by generousapplication of sterile ultrasonography gel. The geltends to dissipate rapidly during insonication, andonly with growing experience was the problemmastered satisfactory. The one tumour documentedto have a central area of vital tissue remains a reasonfor concern. It had a homogeneous structure andwas correctly insonicated according to the intrao-perative ultrasonography documentation. Unno-ticed problems at energy coupling are also themost likely explanation because we found small airbubbles at the HIFU probe at the end of theprocedure. The air bubbles may have interfered
Please cite this article in press as: Klingler HC, et al., A Novel A
Laparoscopic High-Intensity Focused Ultrasound, Eur Urol (2007),
CTE
D P
RO
OF
with energy deposition, even if the amount of airwas small.
The objective of this phase 1 study was toestablish clinical proof of principle and to docu-ment safety. These goals were achieved andunderline the results in porcine kidneys [15].Laparoscopic HIFU of small peripheral renaltumours is clinically feasible and resulted in noHIFU-specific complications. Nevertheless, it isimportant to note the limitations of the studyand the technique applied. Because of the probe’sfocal distance, only tumours (or target lesions) lessthan 3.5 cm diameter and in a peripheral exophyticposition were treated. With larger or more centrallylocated tumours, the entire lesion cannot beinsonicated and incomplete ablation has to beassumed. It appears fair to point out that centraland very large tumours are poorly suited for energyablative therapy in general and have a high failurerate regardless of the technique used [8,26,27].Although all lesions were assumed to be solidtumours at preoperative imaging, one was actuallya complicated cyst and three were benign tumours.This reflects the clinical experience when treatingthese tumors [28]. The ablation technique, espe-cially concerning energy coupling and definingtarget volume, was modified during the study inincremental steps with growing experience, but theoptimum technique may still not have beenreached. Finally the completeness of ablationwas concluded from homogeneity of histologicalsigns of severe acute thermal damage. Althoughthe criteria defined have been shown to correlatewith irreversible cell damage and, with more timebetween thermal insult and histological evalua-tion, the extent of coagulative necrosis [16,19,22],they cannot automatically be equated. Repairprocesses, but also additional posttraumatic mal-perfusion injury also impact the extent of ablationultimately achieved. Defining the clinical efficacyof laparoscopic HIFU ablation of renal tumoursrequires long-term follow-up studies [29], withserial cross-sectional imaging and percutaneousbiopsy of any residual contrast-enhancing lesion,and ultimately long-term data on recurrence-freesurvival.
5. Conclusion
The morbidity of laparoscopic partial nephrect-omy mainly comes from the need to incisehighly vascularized parenchyma. Targeted laparo-scopic HIFU ablation may render this unnecessary,but further studies to refine the technique areneeded.
pproach to Energy Ablative Therapy of Small Renal Tumours:
doi:10.1016/j.eururo.2007.11.020
C
Q1
346
347
348
349
350
351
352
353
354
355
356
357
358
359
360
361
362
363
364
365
366
367
368
369
370
371
372
373
374
375
376
377
378
379
380
381
382
383
384
385
386
387
388
389
390
391
392
393
394
395
396
397
398457457
458
398
399
400
401
402
403
404
405
406
407
408
409
410
411
412
413
414
415
416
417
418
419
420
421
422
423
424
425
426
427
428
429
430
431
432
433
434
435
436
437
438
439
440
441
442
443
444
445
446
447
448
449
450
451
452
453
454
455
456456
e u r o p e a n u r o l o g y x x x ( 2 0 0 7 ) x x x – x x x 7
EURURO 2293 1–9
UN
CO
RR
E
Conflicts of interest
The HIFU equipment and the 18-mm disposableports were provided free of charge for this study byFocus Surgery Inc (Indianapolis, IN, USA) andMisonix Inc (Farmingdale, NY, USA).
R. Seip and N. Sanghvi are employees of FocusSurgery Inc. The other authors have no financialconnection with Focus Surgery Inc or other conflictsof interest.
References
[1] Fergany AF, Saad IR, Woo L, Novick AC. Open partial
nephrectomy for tumor in a solitary kidney: experience
with 400 cases. J Urol 2006;175:1630–3.
[2] Lane BR, Gill IS. 5-year outcomes of laparoscopic partial
nephrectomy. J Urol 2007;177:70–4.
[3] Gill IS, Matin SF, Desai MM, et al. Comparative analysis of
laparoscopic versus open partial nephrectomy for renal
tumors in 200 patients. J Urol 2003;170:64–8.
[4] Klingler HC. Energy ablative therapy of renal tumours.
Urologe A 2007;46:485–95.
[5] Park S, Cadeddu JA, Shingleton WB. Oncologic outcomes
for ablative therapy of kidney cancer. Curr Urol Rep
2007;8:31–7.
[6] Miki K, Shimomura T, Yamada H, et al. Percutaneous
cryoablation of renal cell carcinoma guided by horizontal
open magnetic resonance imaging. Int J Urol 2006;13:
880–4.
[7] Permpongkosol S, Link RE, Kavoussi LR, Solomon SB.
Percutaneous computerized tomography guided cryoa-
blation for localized renal cell carcinoma: factors influen-
cing success. J Urol 2006;176:1907–8.
[8] Klingler HC, Marberger M, Mauermann J, Remzi M, Susani
M. Skipping is still a problem with radiofrequency abla-
tion of small renal tumours. BJU 2007;99:998–1001.
[9] Aron M, Gill IS. Minimally invasive nephron-sparing sur-
gery (MINSS) for renal tumours. Part II: probe ablative
therapy. Eur Urol 2007;51:348–57.
[10] Wyler SF, Sulser T, Ruszat R, et al. Intermediate-term
results of retroperitoneoscopy-assisted cryotherapy for
small renal tumours using multiple ultrathin cryoprobes.
Eur Urol 2007;51:971–9.
[11] Krambeck AE, Farrell MA, Charboneau JW, Frank I,
Zincke H. Intraperitoneal drop metastasis after radiofre-
quency ablation of pararenal tumor recurrences. Urology
2005;65:797.
[12] Marberger M. Ablation of renal tumours with extracor-
poreal high-intensity focused ultrasound. BJU Int
2007;99:1273–6.
[13] Tavakkoli J, Mehta A, Miller C, et al. A laparoscopic HIFU
probe with integrated phased array ultrasound imagi-
ngIn: Proceedings of the International Symposium on
Therapeutic Ultrasound. 2003;417–22.
Please cite this article in press as: Klingler HC, et al., A Novel A
Laparoscopic High-Intensity Focused Ultrasound, Eur Urol (2007),
TED
PR
OO
F
[14] Paterson RF, Barret E, Siqueira TM, et al. Laparoscopic
partial kidney ablation with high intensity focused ultra-
sound. J Urol 2003;169:347–51.
[15] Orvieto M, Lyon M, Mikhail A, et al. High intensity focused
ultrasound renal tissue ablation in a laparoscopic porcine
model. J Urol 2006;175:338.
[16] Susani M, Madersbacher S, Kratzik C, Hennige LV, Mar-
berger M. Morphology of tissue destruction induced by
focused ultrasound. Eur Urol 1993;23(Suppl):34–43.
[17] Nikfarjam M, Malcontenti-Wilson C, Christophi C. Focal
hyperthermia produces progressive tumor necrosis inde-
pendent of the initial thermal effects. J Gastroent Surg
2005;9:410–7.
[18] Stern JM, Anderson JK, Lotan Y, Park S, Cadeddu JA.
Nicotinamide adenine dinucleotide staining following
radio frequency ablation of renal tumours—is a positive
stain synonymous with ablative failure? J Urol
2007;176:1969–72.
[19] Madersbacher S, Pedevilla M, Vinger L, Susani M, Marber-
ger M. Effect of high-intensity focused ultrasound of
human prostate cancer in vivo. Cancer Res
1995;55:3346–51.
[20] Murat FJ, Poissonnier L, Pasticier G, Gelet A. High-inten-
sity focused ultrasound (hifu) for prostate cancer. Cancer
Control 2007;14:244–9.
[21] Oosterhof GO, Cornel EB, Smits GA, Debruyne FM,
Schalken JA. Influence of high-intensity focused ultra-
sound on the development of metastases. Eur Urol
1997;32:91–5.
[22] Kratzik C, Schatzl G, Lackner J, Marberger M. Transcuta-
neous high-intensity focused ultrasonography can cure
testicular cancer in solitary testis. Urology 2006;76:1269–
973.
[23] Poissonnier L, Chapelon JY, Rouviere O, et al. Control of
prostate cancer by transrectal HIFU in 227 patients. Eur
Urol 2007;51:381–7.
[24] Kohrmann KU, Michel MS, Gaa J, Marlinghaus E, Alken P.
High intensity focused ultrasound as non invasive ther-
apy for multifocal renal cell carcinoma: case study and
review of the literature. J Urol 2002;167:2397–403.
[25] Marberger M, Schatzl G, Cranston D, Kennedy JE. Extra-
corporeal ablation of renal tumours with high-intensity
focused ultrasound. BJU Int 2005;95(Suppl. 2):52–5.
[26] Illing RO, Kennedy JE, Wu F, et al. The safety and feasi-
bility of extracorporeal high-intensity focused ultrasound
(HIFU) for the treatment of liver and kidney tumours in a
Western population. Br J Cancer 2005;93:890–5.
[27] Hacker A, Michel MS, Marlinghaus E, Kohrmann KU,
Alken P. Extracorporeally induced ablation of renal tissue
by high-intensity focused ultrasound. BJU Int 2006;97:779–
85.
[28] Remzi M, Ozsoy M, Klingler HC, et al. Are small renal
tumors harmless? Analysis of histopathological features
according to tumors 4 cm or less in diameter. J Urol
2006;176:896–8.
[29] Patard JJ. With increasing minimally invasive options for
small renal tumours, it is time to develop patient-specific
treatment strategies. Eur Urol 2007;51:876–8.
pproach to Energy Ablative Therapy of Small Renal Tumours:
doi:10.1016/j.eururo.2007.11.020
UN
CO
RR
EC
TED
PR
OO
F
Editorial Comment on: A Novel Approach toEnergy Ablative Therapy of Small RenalTumours: Laparoscopic High-Intensity FocusedUltrasoundAmnon ZismanUrology Department, [email protected]
Assaf Harofeh M.C. ZerifinAffiliated to Sackler Faculty of Medicine,Tel-Aviv University, Tel Aviv, Israel
Technological advances as well as cultural andeconomic vectors have caused a dramatic shift fromtraditional ‘‘Robsonian’’ open, radical nephrectomyto nephron-sparing surgery (NSS) using laparoscopyand minimally invasive techniques. Three locomo-tives are driving the process: (1) NSS provideslifelong advantage (ie, freedom from dialysis) [1].(2) NSS for T1 masses provides a curative outcomethat is as good as nephrectomy [2]. (3) Laparoscopy islessmorbid than the supracostal open approach. Fora long period, high-intensity focused ultrasound(HIFU) has promised to deliver the ultimate non-invasive extracorporeal tumor ablation. Onlyrecently has HIFU, in conjunction with improvedimaging capabilities, materialized into a clinicaloption additional to laparoscopic partial nephrect-omy, radiofrequency ablation, and cryoablation.Within this framework, the authors report on aphase 1 study in a small group of patients withlimited follow-up using laparoscopic-guided intra-corporeal HIFU ablation of small renal tumors[3].Turning to laparoscopic guidance as opposedto an extracorporeal approach suggests that for thetime being, extracorporeal HIFU ablation is facinggreat technical difficulties. This is intensified by thedisturbing rate of residual viable tumor reported by
the authors. Two patients had a 1–3-mm rim ofviable tissue immediately adjacent to where theHIFU probe was approximated to the tumor. Onepatient had a central area of vital tissue of about 20%of its volume. Having that said, this is the newestablative technique introduced and still in theprocess of development. By no means will HIFUbe judged in the future by its ability to turn into aneffective extracorporeal procedure in a competitiveenvironment. On one hand the indication for NSS isalready being extended but, on the other hand,elderly patients or those with poor surgical risk arebeing followed expectantly within the frame of fewexperimental studies. Although controversial, abla-tive measures may perhaps have a role in thecytoreduction of primary tumors in patients withmetastatic disease in the present era of moreeffective targeted therapies.
References
[1] Huang WC, Levey AS, Serio AM, et al. Chronic kidney
disease after nephrectomy in patients with renal cortical
tumours: a retrospective cohort study. Lancet Oncol
2006;7:735.
[2] Dash A, Vickers AJ, Schachter LR, Bach AM, Snyder ME,
Russo P. Comparison of outcomes in elective partial vs
radical nephrectomy for clear cell carcinoma 4–7 cm.
BJU Int 2006;97:939.
[3] Klingler C, Martin S, Ralf S, Mauermann M, Naren S,
Marberger MJ. A novel approach to energy ablative ther-
apy of small renal tumours: laparoscopic high-intensity
focused ultrasound. Eur Urol. In press. doi:10.1016/j.eur-
uro.2007.11.020.
DOI: 10.1016/j.eururo.2007.11.021
DOI of original article: 10.1016/j.eururo.2007.11.020
Editorial Comment on: A Novel Approach toEnergy Ablative Therapy of Small RenalTumours: Laparoscopic High-Intensity FocusedUltrasoundQuoc-Dien TrinhDepartment of Urology, University of Montreal HealthCenter, Montreal, QC, [email protected]
The widespread use of abdominal computedtomography and ultrasonography complicates the
management of small incidentally detected renalmasses. Their slow growth and the difficulty indifferentiating benign from malignant lesionspreoperatively make the clinical significance ofsuch lesions unclear. Although partial nephrect-omy is currently considered the standard of carefor these lesions, minimally invasive probe abla-tion techniques are now emerging as potentialalternative approaches [1,2]. Although laparo-scopic cryoablation represents the most widelyused of these novel techniques, high-intensity
e u r o p e a n u r o l o g y x x x ( 2 0 0 7 ) x x x – x x x8
EURURO 2293.2 1–9
Please cite this article in press as: Klingler HC, et al., A Novel Approach to Energy Ablative Therapy of Small Renal Tumours:
Laparoscopic High-Intensity Focused Ultrasound, Eur Urol (2007), doi:10.1016/j.eururo.2007.11.022
UN
CO
RR
EC
TED
PR
OO
F
focused ultrasound (HIFU) ablation has shownpromise in the treatment of solid tumors [3,4].
In this original study [5], Klingler et al report ontheir initial phase 1 experience with laparoscopicintracorporeal HIFU ablation of small renal tumors.Ten patients with radiographic suspicion of renalcell carcinoma (RCC) underwent laparoscopic HIFUablation, followed by, in nine of these patients,laparoscopic nephrectomy to pathologically vali-date the HIFU ablation.
The objective of this phase 1 study was todemonstrate proof of principle and to documentsafety and should only be considered as such. Asfar as a new ablative measure, it has to be furtherrefined because the rate of residual viable tumor isworrisome. Their experience is limited due to thesmall number of patients (n = 10) and the quiteshort reported median follow-up of 7.2 mo.
In conclusion, these results show that laparo-scopic HIFU ablation is not a suitable option for thetreatment of RCC, but further studies mightultimately demonstrate otherwise. Moreover, onehas to wonder if this study signals that theattempts for extracorporeal HIFU ablation of renalmasses are concluded, for the time being, due totechnical limitations.
References
[1] Patard JJ. With increasing minimally invasive options
for small renal tumours, it is time to develop patient-
specific treatment strategies. Eur Urol 2007;51:
876–8.
[2] Aron M, Gill IS. Minimally invasive nephron-sparing
surgery (MINSS) for renal tumours. Part II: probe ablative
therapy. Eur Urol 2007;51:348–57.
[3] Aus G. Current status of HIFU and cryotherapy in pros-
tate cancer—a review. Eur Urol 2006;50:927–34, discus-
sion 934.
[4] Hacker A, Michel MS, Marlinghaus E, Kohrmann KU,
Alken P. Extracorporeally induced ablation of renal tis-
sue by high-intensity focused ultrasound. BJU Int
2006;97:779–85.
[5] Klingler HC, Susani M, Seip R, Mauermann J, Sanghvi N,
Marberger MJ. A novel approach to energy ablative ther-
apy of small renal tumours: laparoscopic high-intensity
focused ultrasound. Eur Urol. In press. doi:10.1016/j.
eururo.2007.11.020.
DOI: 10.1016/j.eururo.2007.11.022
DOI of original article: 10.1016/j.eururo.2007.11.020
e u r o p e a n u r o l o g y x x x ( 2 0 0 7 ) x x x – x x x 9
EURURO 2293.2 1–9
Please cite this article in press as: Klingler HC, et al., A Novel Approach to Energy Ablative Therapy of Small Renal Tumours:
Laparoscopic High-Intensity Focused Ultrasound, Eur Urol (2007), doi:10.1016/j.eururo.2007.11.022