Reduced oxygen tension results in reduced human T cell proliferation and increased intracellular...
Transcript of Reduced oxygen tension results in reduced human T cell proliferation and increased intracellular...
Free Radical Biology & Medicine 48 (2010) 26–34
Contents lists available at ScienceDirect
Free Radical Biology & Medicine
j ourna l homepage: www.e lsev ie r.com/ locate / f reeradb iomed
Original Contribution
Reduced oxygen tension results in reduced human T cell proliferation and increasedintracellular oxidative damage and susceptibility to apoptosis upon activation
Anis Larbi a,⁎, Filipe Cabreiro b, Henning Zelba a, Shiva Marthandan c, Emilie Combet d, Bertrand Friguet b,Isabelle Petropoulos b, Yvonne Barnett c, Graham Pawelec a
a Center for Medical Research, Tübingen Aging and Tumor Immunology Group, University of Tübingen, 72072 Tübingen, Germanyb Laboratoire de Biologie et Biochimie Cellulaire du Vieillissement, EA 3106, Université Paris 7–Denis Diderot, 75251 Paris Cedex 05, Francec Nottingham Trent University, Clifton Campus, Nottingham NG11 8NS, Englandd Medical Sciences, Faculty of Medicine, University of Glasgow, Glasgow G11 6NT, Scotland
Abbreviations: 7-AAD, 7-amino-actinomycin D; Alkescein succinimidyl ester; CT-L, chymotrypsin-like activFCS, fetal calf serum; Fpg, formamidopyrimidine glycantioxidant power; GSH, reduced glutathione; GSSG,hypoxia-inducible factor-1α; IL-2, interleukin-2; Msr, mPBMC, peripheral blood mononuclear cells; PGPH, peptiactivity; ROS, reactive oxygen species; TCR, T cell recep⁎ Corresponding author. Fax: +49 7071 294677.
E-mail address: [email protected]
0891-5849/$ – see front matter © 2009 Elsevier Inc. Adoi:10.1016/j.freeradbiomed.2009.09.025
a b s t r a c t
a r t i c l e i n f oArticle history:Received 19 November 2008Revised 21 September 2009Accepted 23 September 2009Available online 28 September 2009
Keywords:Oxygen tensionT cellsOxidative damageProteasomeMethionine sulfoxide reductaseApoptosisFree radicals
Cell culture and in vitro models are the basis for much biological research, especially in human immunology.Ex vivo studies of T cell physiology employ conditions attempting to mimic the in vivo situation as closely aspossible. Despite improvements in controlling the cellular milieu in vitro, most of what is known about T cellbehavior in vitro is derived from experiments on T cells exposed to much higher oxygen levels than arenormal in vivo. In this study, we report a reduced proliferative response and increased apoptosissusceptibility after T cell activation at 2% oxygen compared to in air. To explain this observation, we testedthe hypothesis of an impaired efficacy of intracellular protective mechanisms including antioxidant levels,oxidized protein repair (methionine sulfoxide reductases), and degradation (proteasome) activities. Indeed,after activation, there was a significant accumulation of intracellular oxidized proteins at more physiologicaloxygen levels concomitant with a reduced GSH:GSSG ratio. Proteasome and methionine sulfoxide reductaseactivities were also reduced. These data may explain the increased apoptotic rate observed at morephysiological oxygen levels. Altogether, this study highlights the importance of controlling oxygen levels inculture when investigating oxygen-dependent phenomena such as oxidative stress.
© 2009 Elsevier Inc. All rights reserved.
Cell culture and in vitro models have become one of the mainstaysof immunological research, especially in human immunology. Thelarge amount of data on T cell physiology thus acquired has greatlycontributed to our understanding of T cell behavior in physiologicaland pathological circumstances. T cell physiology studied ex vivoemploys conditions attempting to mimic the in vivo situation asclosely as possible. Recent advances in cell culture techniques includethe use of improved media, for example, avoiding the addition ofanimal-derived serum, which might cause artifacts [1]. Despite theseand several other improvements in controlling the cellular milieu invitro [2], one critical parameter, with a few exceptions neglected overthe decades (only 0.6% of T cell studies, according to a PubMedsearch), is the level of oxygen to which the cells are exposed. Cells inex vivo experiments are almost always cultured in air supplemented
, alkaline; CFSE, carboxyfluor-ity; Endo III, endonuclease III;osylase; FRAP, ferric reducingoxidized glutathione; HIF-1α,ethionine sulfoxide reductase;dylglutamyl peptide hydrolasetor; T-L, trypsin-like activity.
(A. Larbi).
ll rights reserved.
with 5% CO2, which is severalfold higher than encountered by T cellsin vivo [3]. Probably, the good T cell response in air (even enhanced insevere hyperoxia, i.e., 30–40% oxygen) is responsible for the lack ofinterest in more conditions [4]; therefore, most of what is knownabout T cell behavior in vitro is derived from experiments on T cellsexposed tomuch higher oxygen levels than are normal in vivo [3]. Theoxygen level in the peripheral blood is lower than in air, and thesmaller the arteries, the lower the oxygen level. Although somediscrepancies exist, there is a consensus that the mean oxygen levelexperienced by T cells varies from 1 to 10% [5,6] according to theirlocalization [7], whereas under certain pathological conditions, e.g.,tumor-infiltrating lymphocytes (TIL), it is certainly much lower; TILmust cope with an almost entire absence of oxygen in the commonlyhypoxic tumor environment [8].
There are a small number of studies on human T cell behaviorunder different oxygen levels, but results have been controversial [9–11]. Recently, lower oxygen level was reported to cause a loss of T cellproliferative function [6,12]. These studies suggested that a change inthe cell redox status was in part responsible for reduced proliferationat a more physiological oxygen level (5% oxygen in that study). Thiswas substantiated by a greater production of intracellular reactiveoxygen species (ROS1) and NO after stimulation in 5% oxygencompared to atmospheric oxygen (20%). The machinery responsible
27A. Larbi et al. / Free Radical Biology & Medicine 48 (2010) 26–34
for the maintenance of the redox status and oxidized proteinhomeostasis is complex. Among other factors, it involves (i)glutathione (GSH and GSSG), (ii) methionine sulfoxide reductase(Msr), and (iii) the proteasome system. Reduced glutathione, theprincipal intracellular low-molecular-weight thiol, plays a critical rolein cellular defense against oxidative and nitrosative stress inmammalian cells [13]. GSH detoxifies peroxides generated fromoxygen radical attack and reduces oxidized sites on DNA, proteins, andother molecules when the oxidation is reversible. MsrA and MsrBcatalyze the reversion of methionine S-sulfoxide and methionine R-sulfoxide, respectively, to the reduced form of methionine withinproteins. Methionine can be easily oxidized intomethionine sulfoxide,and its reduction by MsrA [14] and MsrB2 [15] could represent anefficient antioxidant system, because in proteins, the surface-exposedmethionine residues can act as scavengers of a variety of oxidants[16]. The proteasome system has been implicated in the degradationof oxidatively modified proteins [17]. The proteasome is also involvedin regulating protein contents and degrading misfolded proteins. Inmammals, the β1, β2, and β5 subunits are catalytic; although theyshare a common mechanism, they have three distinct substratespecificities referred to as peptidyl-glutamyl peptide-hydrolyzing,trypsin-like, and chymotrypsin-like activities [18].
Here we have investigated the redox status of the extracellular andintracellular milieu in human T cells cultured at a lower than usualoxygen level. The exact dynamics of oxygen diffusion in culture mediausing various culture plate sizes has only been reported in experi-ments using 2% oxygen; thus, we used this as the basis for our study[19]. Our aim was to test the hypothesis that impaired efficacy ofintracellular protective mechanisms, including antioxidant levels,oxidized protein repair (methionine sulfoxide reductases), anddegradation (proteasome) activities, is responsible for impaired Tcell proliferative responses in lower oxygen.
Materials and methods
Cells
Blood samples obtained from healthy middle-aged individuals atthe University Hospital Blood Bank, Tübingen (courtesy of Professor D.Wernet) were processed using FicoLite-H (Linaris, Wertheim-Bettin-gen, Germany) to separate PBMCs. Cells were resuspended (1 to5×106 cells/ml) in serum-free culture medium X-Vivo 15 and leftuntreated or stimulated with anti-CD3 and anti-CD28-coated beads(Dynabeads, Dynal, Karlsruhe, Germany). Samples were prepared induplicate, half being placed in the Hypoxia Workstation (Ruskinn,Pencoed, Bridgend, UK) in 2% oxygen and 5% CO2 balanced withnitrogen and the other half in a regular incubator in which cells growin air supplemented with 5% CO2.
Cell proliferation
Cell proliferation was determined using carboxyfluorescein succi-nimidyl ester (CFSE), which diffuses inside and is retained by the cellin the cytoplasm. During each round of cell division, relativefluorescence intensity of the dye is decreased by half and this canbe determined by flow cytometry. Cells (1×106 cells/ml) wereresuspended in labeling buffer (phosphate-buffered saline, 0.1% BSA).Frozen CFSE (1 mM) (Invitrogen, Karlsruhe, Germany) in extradryDMSO (Invitrogen) was thawed and a 2.5 μM staining solution wasused to stain the cells in the dark for 10 min at room temperature on ashaker. FCS (2%) was then added to stop the labeling reaction. Thecells were washed twice to remove residual CFSE and FCS beforestimulation. At the end of the stimulation time, the CFSE-stained cellswere harvested, washed, and stained for surface markers (CD3, CD4,and CD8). Samples were analyzed on an LSR-II cytometer (BDBiosciences) equipped with three lasers. For each experiment,
mouse or hamster/rat κ-chain Comp Beads (BD) were stained withcorresponding fluorochrome-labeled antibodies and incubated for20 min at room temperature in the dark. Negative Comp Beads wereused as an unstained negative control (BD Biosciences). After beingwashed, the beadswere used for automatic compensationwith the BDFACSDiva acquisition software. Data were processed and analyzedusing FACSDiva and Flowjo 7.2.2 (Treestar, Ashland, OR, USA)following recently updated guidelines [20].
Apoptosis
PBMCs were harvested, washed once with labeling buffer, andstained for surface marker expression described above in addition toannexin V–PE and 7-amino-actinomycin D (7-AAD) following themanufacturer's recommendations. Cells were washed and resuspendedin labeling buffer and analyzed within 30 min. CD4+ and CD8+ T cellswere gated before plotting for annexin V and 7-AAD fluorescence. AllAnnexin V-positive cells were considered apoptotic.
Western blots
PBMCs were centrifuged and lysed with CelLytic lysis reagent(Sigma, Munich, Germany) containing 0.01% leupeptin, 0.01% pep-statin, 0.02% phenylmethylsulfonyl fluoride, and 0.02% NaVO4.Proteins (30 μg, assessed by the Bradford assay) were loaded forSDS–PAGE experiments. Proteins were transferred to a nitrocellulosemembrane. Incubations with anti-HIF-1α at a 1/250 dilution, anti-MsrA at a 1/10,000 dilution, anti-MsrB2 [15] at a 1/2500 dilution, andanti-β1, anti-β2, and anti-β5 proteasome subunits (Biomol Interna-tional, Exeter, UK) at a 1/1500 dilution were performed after themembrane was blocked in 5% skimmedmilk. Loading controls, anti-β-actin and anti-Akt, were included. After several washing steps thesecondary antibody diluted at 1/2000 was added for an additionalhour before luminescence visualization.
OxyBlot analysis
Detection of carbonyl groups was performed with the OxyBlotoxidized protein detection kit (Chemicon International, Hampshire,UK) according to the manufacturer's protocol. Total protein extracts(2.5 μg) were incubated for 15 min at room temperature with 2,4-dinitrophenylhydrazine to form the carbonyl derivative dinitrophe-nylhydrazone before SDS–PAGE separation. After transfer ontonitrocellulose, modified proteins were revealed by anti-dinitrophenolantibodies. Blots were developed with chemiluminescence using theSuperSignal West Femto chemiluminescence substrate (PerbioSciences). Films were scanned and the amount of signal wasquantified by densitometric analysis using ImageMaster 1D software(GE Healthcare, Chalfont St Giles, UK).
Determination of Msr activities
Total Msr enzymatic activity was measured in cellular homo-genates using N-acetyl-[3H]methionine R,S-sulfoxide substrate (GEHealthcare) as previously described [15]. Twenty micrograms ofproteins was used to measure Msr activities.
Determination of proteasome activities
Peptidase activities of the proteasome were assayed using thefluorogenic peptide succinyl-Leu-Leu-Val-Tyr-amidomethylcoumarin(LLVY-AMC) (Sigma–Aldrich) for the chymotrypsin-like (CT-L)activity, N-t-butyloxycarbonyl-Leu-Ser-Thr-Arg-amidomethylcou-marin (LSTR-AMC) (Sigma–Aldrich) for the trypsin-like (T-L) activity,and N-benzyloxycarbonyl-Leu-Leu-Glu-β-naphthylamide (LLE-NA)(Sigma–Aldrich) for the peptidylglutamyl peptide hydrolase (PGPH)
28 A. Larbi et al. / Free Radical Biology & Medicine 48 (2010) 26–34
activity. The mixture, containing 20 μg of crude protein cellularextracts for the T-L and PGPH activity and 50 μg for the CT-L activity inproteasome buffer (25 mM Tris–HCl, pH 7.5), was incubated at 37 °Cwith the appropriate peptide substrate (LLVY-AMC at 25 μM, LLE-NAat 150 μM, or LSTR-AMC at 40 μM) in a final volume of 200 μl.Enzymatic kinetics were conducted in a temperature-controlledmicroplate fluorimetric reader (Fluostar Galaxy, Stuttgart, Germany).Excitation/emission wavelengths were 350/440 and 340/410 nm foraminomethylcoumarin and β-naphthylamine, respectively. Protea-some activity was determined as the difference between the totalactivity and the remaining activity of the crude extract in the presenceof 20 μM proteasome inhibitor N-Cbz-Leu-Leu-leucinal (MG132).
GSH:GSSG quantification
The reduced and oxidized forms of glutathione were assessedusing a GSH:GSSG kit (Calbiochem, San Diego, CA, USA) incorporatinga thiol-scavenging reagent, 1-methyl-2-vinylpyridinium trifluoro-methane-sulfonate-1 (M2VP), at a level that rapidly scavenges GSHbut does not interfere with the glutathione reductase in recyclingGSSG into GSH. Cells (2×106 cells/ml for GSH and 5×106 cells/ml forGSSG) were harvested and whole-cell extract was prepared accordingto the manufacturer's instructions. The GSH and GSSG concentrations(in μM) of human PBMCs (resting and activated), cultured at either 20or 2% oxygen, were photometrically measured at 412 nm inmicromolar concentrations, and the GSH:GSSG ratio was calculated.The lower limit of detection for GSSG according to the manufacturer'sprotocol was 0.54 μM.
Assessment of oxidative DNA damage levels
The levels of oxidative damage to the DNA of human PBMCs,cultured at either 20 or 2% oxygen, were determined using themodified alkaline comet assay, previously described by Collins et al.[21]. In the modified alkaline comet assay, cells are pretreated withformamidopyrimidine glycosylase (Fpg) or endonuclease III (EndoIII), which recognize oxidatively modified purines or oxidativelymodified pyrimidines, respectively [21]. These enzymes nick DNA atthe sites of oxidatively damaged nucleotides, creating single-strandbreaks that can be detected with the comet assay. Comet analysis wasperformed on the enzyme-pretreated cells using computer imageanalysis software (Komet 5.5; Andor Technology, UK), counting 50cells per slide. The observed percentage of DNA in the comet tail wasused to measure levels of DNA damage in the cell samples.
Antioxidant capacity assay
Cells were cultured for 3 days in X-Vivo 15 only or X-Vivo 15supplemented with 0, 5, 10, 25, 50, or 100 μM resveratrol (Sigma)under either 2 or 20% oxygen. The ferric reducing antioxidant power(FRAP) of the cell supernatant wasmeasured according to the methodof Benzie and Strain [22]. The FRAP reagent was prepared by mixing10 mM 2,4,6-tripyridyl-s-triazine (10 ml) into 20 mM ferric chloridesolution (10 ml) and 0.3 M acetate buffer, pH 3.6 (100 ml). Samples(50 μl) diluted in distilled water (150 μl) were mixed with 1.5 ml ofthe freshly prepared FRAP reagent. Samples were incubated for 4 min,and their absorbencies determined spectrophotometrically at593 mM. Quantification was achieved using a 0 to 1 mM ferroussulfate calibration curve, and the antioxidant power of the sample wasexpressed as micromoles of Fe2+ per liter of supernatant.
Statistical analysis
GraphPad Prism 4.0 was used to display and analyze the data.Sampleswere tested for significance using paired two-sample Studentt-test assuming equal variances; p values are presented as appropriate.
Results
Culture in low oxygen maintains the antioxidant capacity ofculture media
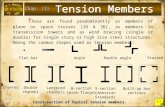
Cell adaptation to a low oxygen level is reflected in the up-regulation of the hypoxia-inducible factor-1α. We therefore firstestablished whether HIF-1α expression was induced in PBMCscultured in low oxygen (2%). HIF-1α expression, determined byWestern blotting, is shown in Fig. 1A, together with Akt as a control.In these PBMC cultures, containing approximately 90% lymphocytesas assessed by flow cytometry, HIF-1α up-regulation was observedafter 24 h of culture in 2% oxygen, whereas it was not present incells cultured in 20% oxygen. HIF-1α expression was maintained aslong as cultures remained in low oxygen, but was rapidly down-regulated (within 10 min) when the cultures were removed to air(data not shown). Optical densitometry analysis is shown in Fig. 1B.Because one might expect that lower oxygen tension should result inreduced oxidation levels, we tested whether culturing cells at 2%oxygen increased the antioxidant capacity remaining in the culturemedium. PBMCs were cultured at 2 or 20% oxygen and thesupernatant was tested for its overall antioxidant capacity bymeasuring the ferric reducing antioxidant power. A 3-day cultureunder 20% oxygen caused a fourfold greater decrease in the ferricreducing antioxidant power of the supernatant compared to cultureunder 2% oxygen (Fig. 1C, pb0.0001). We tested the same parameterwhen an antioxidant, in this case resveratrol (ranging from 5 to100 μM), was added to the cultures. Resveratrol supplementationsignificantly increased the basal antioxidant capacity from 51.6±2.0to 100.7±14.3 μM Fe2+ equivalent under low oxygen tension,whereas similar supplementation achieved lesser results under 20%oxygen, bringing the antioxidant capacity of the cell supernatant to amaximum of 45.6±7.4 μM Fe2+ equivalent (Fig. 1D). These resultssuggest that low exogenous oxygen levels preserve the antioxidantcapacity in the culture medium.
T cell response under low oxygen
Next we investigated T cell proliferative responses and suscepti-bility to apoptosis at low oxygen levels. T cells were activated with α-CD3/α-CD28-coated microbeads and tested for proliferation usingthe CFSE dilution assay. T cell proliferationwas observed at both lowerand higher oxygen levels, but the number of cell divisions undergonein a given time was less in the former (Fig. 2A, bottom and top,respectively). The overall percentage of dividing CD3+ T cells wasreduced in low oxygen and the maximum of cell divisions achievedunder high oxygenwas higher in the same period of 5 days. Moreover,only 12.0±2.4% of T cells divided seven times at low oxygen, whereas21.6±4.3% divided at least this number of times under high oxygen.The absolute cell number at the end of the culture period was greaterin high oxygen. To explain the lower T cell number at the end ofstimulation in 2% oxygen we analyzed T cell susceptibility toapoptosis. We found that although spontaneous resting (unstimu-lated) cell death was not significantly different after culture in low orhigh oxygen (Fig. 2B, 5.7±3.2 and 4.2±1.6%, respectively), apoptosiswas higher among activated cells (Fig. 2C) cultured in low (27.5±7.3%) compared to high oxygen (12.3±3.9%). These data suggest thatT cells do not respond equally well when the oxygen level is reducedand that the improved antioxidant properties of the surroundingmedium do not correlate with better cell function.
Lower oxygen tension increases protein oxidative damage in PBMCs
Because low oxygen level was found to preserve the antioxidantcapacity of the culture medium, we next investigated whether thiswould also be true for the intracellular redox status. To this end, we
Fig. 1. Effect of low oxygen and HIF-1α expression on antioxidant capacity of the cultures. (A) PBMCs were cultured for 3 days under 20 or 2% oxygen (n=5). The expression of theoxygen sensor HIF-1α was investigated as a reflection of the hypoxic status of the cells. HIF-1α was monitored in cellular extracts, prepared as described under Materials andmethods, byWestern blotting. The expression of Akt was used as a loading control. (B) Densitometric analysis of HIF-1α expression using Akt as control (n=6). (C) The supernatantof cultures tested in (A) was collected and its antioxidant capacity measured by FRAP assay as described under Materials and methods. Significant change in the antioxidant index isindicated (⁎pb0.01). (D) Similar results were obtained when the cultures were supplemented with increasing concentrations, 0–100 μM, of resveratrol, with known antioxidantcapacities.
29A. Larbi et al. / Free Radical Biology & Medicine 48 (2010) 26–34
tested whether the increased antioxidant capacity of the surroundingmedium under low oxygen was paralleled by increased intracellularantioxidant capacity as well, and whether this translated into pro-tection against protein oxidative damage. Glutathione is the major
Fig. 2. Altered T cell proliferation and apoptosis under low oxygen. Resting and α-CD3/α-CDof divisions achieved by these cells is indicated by CFSE fluorescence in the histograms. CFSEof cell division. This allows precise information concerning the proliferative index of the celapoptosis of resting cells was tested by flow cytometry using annexin V and 7-AAD as descriSimilar experiments were performed for activated cultures under 2 (bottom) and 20% oxyg
intracellular low-molecular-weight thiol that plays a critical role incellular defense against oxidative stress in tissues and cells. Wetherefore measured the ratio of intracellular reduced glutathione tooxidized glutathione in PBMCs from three individuals. Fig. 3A shows
28-activated PBMCs were cultured for 5 days under 20 and 2% oxygen. (A) The numberfluorescence is at its maximum in undivided cells and is divided by half after each roundls to be obtained. One representative experiment is shown (n=8). (B) Susceptibility tobed under Materials and methods. One representative experiment is shown (n=8). (C)en (top). One representative experiment is shown (n=8).
Fig. 3. Glutathione redox and protein carbonylation status under low oxygen tension. (A) PBMCs were cultured for 2 (D2) and 4 (D4) days under 20 and 2% oxygen. The intracellular(i) GSH:GSSG ratio was assessed as described under Materials and methods and showed a significant decrease in the reduced form in unstimulated cultures under 2% (⁎pb0.05). (B)A similar phenomenon occurred in activated cells (⁎pb0.05). (C) Resting and activated PBMCs were lysed and processed for OxyBlot analysis following the manufacturer'sinstructions. A representative experiment is shown. (D) Mean levels of carbonyl products analyzed using Scion Corp. Imaging Software (http://www.scioncorp.com/index.htm) aredisplayed (n=5) and significant differences between 2 and 20% oxygen are indicated (⁎pb0.05). AU, arbitrary units.
Fig. 4. Methionine sulfoxide reductase and proteasome activities. (A) Resting and activated PBMCs (n=3) cultured for 3 days under 20 and 2% oxygen were harvested andmethionine sulfoxide reductase (Msr) activity wasmeasured. Significant differences inMsr activity are indicated (⁎⁎⁎pb0.001). (B–D) In the same set of samples we investigated theproteasome activity by measuring the chymotrypsin-like, trypsin-like, and peptidylglutamyl peptide hydrolase activities (CT-L, T-L, and PGPH, respectively) using fluorogenicpeptides as described under Materials and methods. Significant differences in specific proteasome activity are indicated (⁎pb0.05).
30 A. Larbi et al. / Free Radical Biology & Medicine 48 (2010) 26–34
31A. Larbi et al. / Free Radical Biology & Medicine 48 (2010) 26–34
the GSH:GSSG ratios in resting (unstimulated) cells were maintainedat 20 and 2% oxygen for up to 4 days. The GSH:GSSG ratio of cellsmaintained under 2% oxygen was significantly lower at the end of day4 compared to day 2, whereas there was no significant difference inthe GSH:GSSG ratio of cells maintained at 20% oxygen with time. Fig.3B shows the GSH:GSSG ratio in activated cells maintained at 20 and2% oxygen for up to 4 days. Again, the GSH:GSSG ratio of cellsmaintained at 20% oxygen was significantly higher than that for thecells maintained at 2% oxygen at the end of 2 or 4 days. Next, weinvestigated whether these reduced levels of intracellular antiox-idants were accompanied by increased levels of protein damage. Wemonitored carbonyl group formation on intracellular proteins, whichis a good index of global protein oxidation, using the OxyBlottechnique (Fig. 3C). Densitometric quantification analysis of carbonyllevels showed that protein oxidation under low oxygen was 124±15and 181±43% of that under high oxygen in resting and α-CD3/α-CD28-activated cells, respectively (Fig. 3D). A detailed analysis of theOxyBlot membranes revealed that the intensity of protein oxidationwas not increased because of the oxidation of a particular set ofproteins (data not shown).
Msr and proteasome activities in PBMCs are enhanced by stimulationwith α-CD3/α-CD28 beads but decreased by low oxygen tension
Protein carbonyl accumulation results from decreases in thesystems involved in the efficient repair and degradation of oxidizedproteins. The Msr system is one of the few known protein repair
Fig. 5.Methionine sulfoxide reductase A and B2 and catalytic β-subunit expression. (A) RestCell lysates were used forWestern blotting of MsrA andMsrB as well as the catalytic β1-, β2-donors are shown. (B) The densitometry analysis of MsrB2 andMsrA expression was performexpression using β-actin as reference. Significant differences are indicated (⁎pb0.05, ⁎⁎pb0
systems. Msr activity was therefore measured with N-acetyl-[3H]MetR,S-(O), a radioactive substrate, allowing the determination of theMsrA and MsrB activities in cellular extracts prepared from activatedand resting PBMCs after culture at various oxygen tensions. Fig. 4Ashows that Msr activity was slightly but not significantly reducedwithlow oxygen tension in resting cells. In contrast, in theα-CD3/α-CD28-activated cells, culture in 2% oxygen greatly reduced Msr activity tohalf of the activity present at 20%. In addition, the level of Msr activitywas two- and fourfold higher in activated PBMCs compared to restingPBMCs at 2 and 20% oxygen, respectively.
Because the proteasome has been implicated in oxidized proteindegradation, we measured the three catalytic activities of theproteasome (Figs. 4B, 4C, and 4D). Chymotrypsin-like, trypsin-like,and peptidylglutamyl peptide hydrolase peptidase activity of theproteasome was measured using fluorogenic peptides as substrates.As for theMsr activity, the same trend was observed in all proteasomeactivities and was shown to be significantly lower in activated cellscultured in 2% oxygen compared with 20%. Levels of proteasomeactivity were always higher in activated than in resting cells,independent of the level of oxygen in which they had been cultured.
To determine whether the modulation of both Msr and protea-some activities was due to modifications in the expression of MsrA/MsrB2 or proteasome subunits, Western blotting experiments wereconducted on PBMC protein extracts (Fig. 5A). The densitometryanalysis of the protein expression compared to β-actin revealed nosignificant difference in MsrA expression in resting cells but adecrease in the expression of the protein in activated cells cultured
ing and α-CD3/α-CD28-activated PBMCs were cultured for 3 days at 20 and 2% oxygen., and β5-subunit expression. β-Actin was used as loading control. The results from threeed using β-actin as reference. (C) The same was performed for β1-, β2-, and β5-subunit.01, and ⁎⁎⁎pb0.001).
32 A. Larbi et al. / Free Radical Biology & Medicine 48 (2010) 26–34
in 2% compared to 20% oxygen (Fig. 5B, ⁎pb0.05). In contrast, for theMsrB2 protein there was a significant decrease in the amount ofprotein expressed in 2% oxygen compared to 20% in resting cells(⁎⁎pb0.01). More importantly, stimulation of PBMCs by α-CD3/α-CD28 beads strongly increased the expression of MsrB2 protein(⁎⁎⁎pb0.001). Taken together, these results explain, at least in part,the observed effects on total Msr activity due to stimulation andoxygen treatment conditions. Low oxygen tension (2%) greatlydecreased the expression of the β1 and β2 subunits (⁎pb0.05)carrying the catalytic activities of the proteasome (Fig. 5C). Inaddition, stimulation by α-CD3/α-CD28 beads contributed to theoverexpression of all catalytic subunits in 20% oxygen (⁎pb0.05) and2% oxygen (⁎⁎⁎pb0.001). The differences in β-subunit expression inresting cells are responsible for the differences in protein expressionenhancement after activation; whereas the overall β-subunit expres-
Fig. 6. Time-dependent analysis of DNA damage under low oxygen tension. DNA damagedetects genotoxicity by visualizing DNA migration caused by strand breaks, alkaline labile sEndo III (middle) were tested and are shown as the mean values during the course of culture48, 72, and 96 h incubation. All incubation times at 2% oxygen show significantly increased fr(pb0.01) compared to 20% oxygen.
sion in cells in 20% increased by 2-fold, in cells in 2% it increased by 10-fold after activation. These results could account for the observeddifferences in the three catalytic activities of the proteasome due toboth stimulatory and oxygen tension effects.
Oxidative DNA damage levels in human PBMCs
Finally, we sought to determine whether the increased cellularprotein oxidative damage counterintuitively produced in low oxygenand partly explained by the observed reduced expression ofproteasome subunits was limited to cytosolic proteins or whethercell nuclei were also affected. The levels of oxidative damage to theDNA were determined using the comet assay measuring alkaline(Alk), Endo III, and Fpg. Endo III and Fpg allow assessment ofoxidatively modified purines or pyrimidines, respectively. The mean
was assessed using the alkaline comet assay. This single-cell gel electrophoresis assayites, and transient repair sites (Alk, top). The enzyme-sensitive sites Fpg (bottom) and. Resting and activated PBMCs (white and gray bars, respectively) were tested after 24,equency of DNA in the comet tail for the Alk (pb0.05), Endo III (pb0.01), and Fpg assay
33A. Larbi et al. / Free Radical Biology & Medicine 48 (2010) 26–34
observed percentages of Alk, Endo III, and Fpg DNA in the comet tailwere used to measure levels of DNA damage in the cell samples. Thelevel of oxidative damage to DNAwas investigated in either resting oractivated PBMCs maintained at 20 or 2% during the course of theculture (24 to 96 h). Human PBMCs maintained at 2% oxygen hadhigher levels of oxidative damage to DNA (the percentage of DNA incomet tail) compared to those at 20% in the case of resting as well asactivated cells (Fig. 6). This was significant for the DNA strand breaksand alkali labile sites (Alk; pb0.05), for the damaged pyrimidine bases(Endo III; pb0.01), and the damaged purine bases (Fpg; pb0.01) andfor all incubation periods.
Discussion
Cell culture ex vivo is traditionally performed at ambient oxygenconcentrations with very little attention to the level of oxygenexperienced by the cells. Under changing oxygen levels the HIF-1αpathway has dramatically different effects on the posttranslationalmodification of proteins and can influence a broad range of cellularpathways by acting at the transcriptional level [23]. It would seemappropriate that at least certain applications, such as the study ofoxidative stress, need to take oxygen levels into account [24]. Theexact intracellular oxygen level in vivo is unknown and only recentdevelopments have allowed its measurement ex vivo [25]. Thus, itwas shown that following K+ exposure of PC12 neuronal cells, theaverage intracellular O2 level was reduced from 85–90% air saturationto 55–65%, which correlated with an increase in cellular ATP. Thissuggested that even in a stable O2 environment the intracellular O2
level fluctuates depending on cell status. However, it was shown thatthe extracellular environment of cells rapidly equilibrated to theambient oxygen level [19]. Cell culture media in air contain 2% oxygenas rapidly as 24 h after being transferred from air to a 2% oxygenincubator [19].
With this in mind, we first determined that, as expected, theculture medium under low oxygen tension (2%) maintained a highantioxidant capacity. However, we found that this did not positivelyinfluence T cell functions, as suggested by others [10,12]. Oxygentension at either 2 or 20% had a significant impact on the antioxidantcapacity of the cell supernatant, indicating either a sparing ofantioxidant resources at reduced oxygen tension or a heightenedantioxidant consumption at 20% oxygen. It is also possible that therespiratory chain or the molecular exchanges between cells and theenvironment are different in low vs high oxygen levels. It was shownthat NCX-4016, a NO-releasing derivative of aspirin, caused atransient hypoxic status in PBMC that inhibited cell proliferation aswell as cytokine secretion. Adding substrates of complexes II, III, andIV of the mitochondrial respiratory chain reversed the inhibitoryactivities of NCX-4016 [26]. In our study the intracellular GSH:GSSGratio was decreased and correlated with increased levels of carbony-lated proteins for activated PBMC cultured under low oxygen. This isin accordance with previous reports showing that hypoxia unexpect-edly induced higher intracellular damage [27]. This finding might alsobe explained by the reduced Msr and proteasome activities. At theprotein level, only a slight up-regulation of Msr and proteasomesubunit expression was observed after activation under low oxygentension. The loss of cellular functions including those involved inproteinmaintenance and turnover were also shown to happen in vitroand are thought at least in part to explain cellular senescence [28]. Theincreased carbonylation of proteins was corroborated by theincreased amount of DNA damage under low oxygen, suggestingthat an overall increased oxidation in low oxygen takes place, whichmay be due to a lack of efficiency in intracellular protective and repairmechanisms.
The role of ROS in cell physiology and inflammation is complex.Although ROS are damaging when in excess there is no doubt thatthey are essential for many important processes. Animal models
showed that lower than normal levels of ROS were associated withincreased autoimmunity and arthritis severity. This highlights theimportance of adequate ROS production in maintenance of tolerance[29]. ROS not only are important players in innate immunity but alsoregulate signaling [30]. T cell receptor signaling is redox-dependentand also relies on the production of ROS [31]. T cell hyporesponsive-ness under low oxygen is therefore likely to be due to changes in theredox equilibrium of the cells. Mucosal T cells, which experiencedifferent oxygen levels compared to the peripheral T cells we studiedhere, were shown to have a higher threshold of activation. The reasonfor this may be a shift between the balance of kinases and proteintyrosine phosphatases [32]. Elevated glutathione can more readilydetoxify TCR-induced reactive oxygen species, partly explaining thereduced apoptosis seen in our experiments [32]. Nevertheless, T cellsmust cope with such harsh environments to perform their role ofimmune surveillance. It is known that hypoxia hinders immuneresponses to tumors by reducing IL-2 and interferon-γ production byT cells and interfering with the proliferation/survival equilibrium.Lymphoma-specific T cells genetically engineered to up-regulate theIL-2 promoter at low oxygen (HRE-IL2) displayed an increasedsurvival and proliferation at oxygen concentrations as low as 1%.HRE-IL-2 T cells mediated enhanced tumor regression compared tonormal cells [33].
The data presented here show that under low oxygen, cell culturemedia better maintain antioxidant capacity, but this was not the casefor the cells themselves. This suggested a problem in moleculeexchange between T cells and the extracellular milieu. It is possiblethat antioxidants present in the milieu are not available any longer toT cells at low oxygen because of a still unknown mechanism: thiscould conceivably be a change in membrane potential, fluidity, orintegrity. During hypoxia, the cholesterol/phospholipid ratio isincreased, along with extensive remodeling of lipids at the sn-1position, causing a decrease in membrane fluidity [34]. This wasassociated with changes in CD73 expression, another molecule up-regulated during hypoxia and involved in some important cAMP-dependent signaling processes [35]. However, there are somediscrepancies regarding the effects of hypoxia on cell membranefluidity [36] that are certainly cell-type-dependent. Thus, thereremains a clear requirement for a better understanding of low-molecular-weight antioxidant exchanges under anoxic, hypoxic,normoxic, and hyperoxic conditions.
The counterintuitively increased intracellular protein and DNAdamage observed under decreased oxygen may be explained by thedisturbance in free radical production, use, and fate during therespiratory chain and signaling processes. Evidence suggests anincreased free radical cytotoxicity to Jurkat cells under lower oxygenlevels [37]. Increased lipid peroxidation, release of cytochrome c, andapoptosis under low oxygen were ascribed to oxygen consumption byalkyl radicals [37]. Activated cells may experience even moredisturbance as suggested by the increased apoptotic rate comparedto resting cells. Data suggest the mitochondria as major regulators ofhypoxia-induced apoptosis [38], whereas others imply p66Shc in theup-regulation of HIF-1α and the related cell death [39]. T cells arenormally exposed to b20% oxygen in vivo and although they doproliferate better at 20% oxygen this might not reflect their realphysiology. The paradox that reduced oxygen level is associated withincreased intracellular damage comes along with the paradox thatreduced oxygen level is associated with poor T cell response [40].Moreover, intracellular oxygen levels oscillate highly, thus participatein the complexity of free radical turnover.
In humans, HIF-1α is expressed in T cells in vivo [41] as well asunder normoxic conditions after activation [41–43]. Similar observa-tions were made in murine models [44]. This suggests HIF-1αinduction to be a stress signal to the cells to adapt to a new envi-ronment (oxygen level) but also an integrated pathway essential toinduce the expression of certain genes (e.g., after activation) necessary
34 A. Larbi et al. / Free Radical Biology & Medicine 48 (2010) 26–34
for “physiological” processes such as proliferation or cytokineproduction. One limit of the data presented here comes from the factthat the experiments were performed toward the lower end (2%) ofphysiological oxygen tension (1–10%) and for this reason representonly a snapshot of what could happen in vivo. Moreover, it is difficultto state with the current knowledge where the limit between hypoxiaand normoxia is. One reason for this is the differential susceptibility tooxygen among different cell types. Another reason is the variousoxygen levels T cells may experience over short time periods, whereasresident T cells (in lymphoid organs or other tissues) may experiencerelatively constant low oxygen levels. Further investigations shouldaim at defining T cell functions in an oxygen concentration-dependentmanner to understandhowT cells adapt to these changes andwhat thebiological significance of such data is.
Acknowledgments
This work was supported by the Deutsche Forschungsge-meinschaft (DFG PA 361/11-1) and the European Commission (EU-LSHG-CT-2007-036894 “LifeSpan” and EU-LSHM-CT-2006-51830“Proteomage”).We thank Professor H. Eltzschig (Department ofAnesthesiology, University of Tübingen) for providing the hypoxiachamber. We thank Lilly Wedel and Florian Heubach for theirtechnical help. We are grateful to Professor D. Wernet (Blood Bank,University of Tübingen) for providing blood samples.
References
[1] Ostler, T.; Ehl, S. A cautionary note on experimental artefacts induced by fetal calfserum in a viral model of pulmonary eosinophilia. J. Immunol. Methods 268:211–218; 2002.
[2] Coolen, N. A.; Verkerk,M.; Reijnen, L.; Vlig,M.; van denBogaerdt, A. J.; Breetveld,M.;Gibbs, S.; Middelkoop, E.; Ulrich, M. M. Culture of keratinocytes for transplantationwithout the need of feeder layer cells. Cell Transplant 16:649–661; 2007.
[3] de Souza, N. Too much of a good thing. Nat. Methods 4:386; 2007.[4] Bodeker, B. G.; Lehmann, J.; Muhlradt, P. F. Lymphokine (interleukin-2)
production by mitogen-stimulated human lymphocytes in small reactors. Dev.Biol. Stand. 50:193–200; 1981.
[5] Caldwell, C. C.; Kojima, H.; Lukashev, D.; Armstrong, J.; Farber, M.; Apasov, S. G.;Sitkovsky, M. V. Differential effects of physiologically relevant hypoxic conditionson T lymphocyte development and effector functions. J. Immunol. 167:6140–6149; 2001.
[6] Atkuri, K. R.; Herzenberg, L. A.; Niemi, A. K.; Cowan, T.; Herzenberg, L. A.Importance of culturing primary lymphocytes at physiological oxygen levels. Proc.Natl. Acad. Sci. USA 104:4547–4552; 2007.
[7] Westermann, J.; Bode, U. Distribution of activated T cells migrating through thebody: a matter of life and death. Immunol. Today 20:302–306; 1999.
[8] Vaupel, P.; Kallinowski, F.; Okunieff, P. Blood flow, oxygen consumption and tissueoxygenation of human tumors. Adv. Exp. Med. Biol. 277:895–905; 1990.
[9] MacDonald, H. R.; Koch, C. J. Energy metabolism and T-cell-mediated cytolysis. I.Synergism between inhibitors of respiration and glycolysis. J. Exp. Med. 146:698–709; 1977.
[10] Zuckerberg, A. L.; Goldberg, L. I.; Lederman, H. M. Effects of hypoxia oninterleukin-2 mRNA expression by T lymphocytes. Crit. Care Med. 22:197–203;1994.
[11] Naldini, A.; Carraro, F.; Silvestri, S.; Bocci, V. Hypoxia affects cytokine productionand proliferative responses by human peripheral mononuclear cells. J. Cell.Physiol. 173:335–342; 1997.
[12] Atkuri, K. R.; Herzenberg, L. A.; Herzenberg, L. A. Culturing at atmospheric oxygenlevels impacts lymphocyte function. Proc. Natl. Acad. Sci. USA 102:3756–3759;2005.
[13] Griffith, O. W. Biologic and pharmacologic regulation of mammalian glutathionesynthesis. Free Radic. Biol. Med. 27:922–935; 1999.
[14] Yermolaieva, O.; Xu, R.; Schinstock, C.; Brot, N.; Weissbach, H.; Heinemann, S. H.;Hoshi, T. Methionine sulfoxide reductase A protects neuronal cells against briefhypoxia/reoxygenation. Proc. Natl. Acad. Sci. USA 101:1159–1164; 2004.
[15] Cabreiro, F.; Picot, C. R.; Perichon, M.; Castel, J.; Friguet, B.; Petropoulos, I.Overexpression of mitochondrial methionine sulfoxide reductase B2 protectsleukemia cells from oxidative stress-induced cell death and protein damage.J. Biol. Chem. 283:16673–16681; 2008.
[16] Levine, R. L.; Mosoni, L.; Berlett, B. S.; Stadtman, E. R. Methionine residues asendogenous antioxidants in proteins. Proc. Natl. Acad. Sci. USA 93:15036–15040;1996.
[17] Poppek, D.; Grune, T. Proteasomal defense of oxidative protein modifications.Antioxid. Redox Signaling 8:173–184; 2006.
[18] Orlowski, M.; Wilk, S. Catalytic activities of the 20 S proteasome, a multicatalyticproteinase complex. Arch. Biochem. Biophys. 383:1–16; 2000.
[19] Newby, D.; Marks, L.; Lyall, F. Dissolved oxygen concentration in culture medium:assumptions and pitfalls. Placenta 26:353–357; 2005.
[20] Herzenberg, L. A.; Tung, J.; Moore, W. A.; Herzenberg, L. A.; Parks, D. R.Interpreting flow cytometry data: a guide for the perplexed. Nat. Immunol. 7:681–685; 2006.
[21] Collins, A. R.; Duthie, S. J.; Dobson, V. L. Direct enzymic detection of endogenousoxidative base damage in human lymphocyte DNA. Carcinogenesis 14:1733–1735;1993.
[22] Benzie, I. F.; Strain, J. J. The ferric reducing ability of plasma (FRAP) as a measure of“antioxidant power”: the FRAP assay. Anal. Biochem. 239:70–76; 1996.
[23] Lukashev, D.; Klebanov, B.; Kojima, H.; Grinberg, A.; Ohta, A.; Berenfeld, L.;Wenger, R. H.; Ohta, A.; Sitkovsky, M. Cutting edge: hypoxia-inducible factor1alpha and its activation-inducible short isoform I.1 negatively regulate functionsof CD4+ and CD8+ T lymphocytes. J. Immunol. 177:4962–4965; 2006.
[24] Esteban, M. A.; Maxwell, P. H. Manipulation of oxygen tensions for in vitro cellculture using a hypoxic workstation. Expert Rev. Proteomics 2:307–314; 2005.
[25] Zhdanov, A. V.; Ward, M. W.; Prehn, J. H.; Papkovsky, D. B. Dynamics ofintracellular oxygen in PC12 cells upon stimulation of neurotransmission. J. Biol.Chem. 283:5650–5661; 2008.
[26] Fiorucci, S.; Mencarelli, A.; Distrutti, E.; Baldoni, M.; del Soldato, P.; Morelli, A.Nitric oxide regulates immune cell bioenergetic: a mechanism to understandimmunomodulatory functions of nitric oxide-releasing anti-inflammatory drugs.J. Immunol. 173:874–882; 2004.
[27] Magalhaes, J.; Ascensao, A.; Soares, J. M.; Ferreira, R.; Neuparth, M. J.; Marques, F.;Duarte, J. A. Acute and severe hypobaric hypoxia increases oxidative stress andimpairs mitochondrial function in mouse skeletal muscle. J. Appl. Physiol. 99:1247–1253; 2005.
[28] Petropoulos, I.; Friguet, B. Protein maintenance in aging and replicativesenescence: a role for the peptide methionine sulfoxide reductases. Biochim.Biophys. Acta 1703:261–266; 2005.
[29] Hultqvist, M.; Backlund, J.; Bauer, K.; Gelderman, K. A.; Holmdahl, R. Lack ofreactive oxygen species breaks T cell tolerance to collagen type II and allowsdevelopment of arthritis in mice. J. Immunol. 179:1431–1437; 2007.
[30] D'Autreaux, B.; Toledano, M. B. ROS as signalling molecules: mechanisms thatgenerate specificity in ROS homeostasis. Nat. Rev. Mol. Cell Biol. 8:813–824; 2007.
[31] Williams, M. S.; Kwon, J. T cell receptor stimulation, reactive oxygen species, andcell signaling. Free Radic. Biol. Med. 37:1144–1151; 2004.
[32] Reyes, B. M.; Danese, S.; Sans, M.; Fiocchi, C.; Levine, A. D. Redox equilibrium inmucosal T cells tunes the intestinal TCR signaling threshold. J. Immunol. 175:2158–2166; 2005.
[33] Kim, H.; Peng, G.; Hicks, J. M.; Weiss, H. L.; Van Meir, E. G.; Brenner, M. K.; Yotnda,P. Engineering human tumor-specific cytotoxic T cells to function in a hypoxicenvironment. Mol. Ther. 16:599–606; 2008.
[34] Botto, L.; Beretta, E.; Daffara, R.; Miserocchi, G.; Palestini, P. Biochemical andmorphological changes in endothelial cells in response to hypoxic interstitialedema. Respir. Res. 7:7; 2006.
[35] Bhatnagar, A. Surviving hypoxia: the importance of rafts, anchors, and fluidity.Circ. Res. 92:821–823; 2003.
[36] Block, E. R.; Patel, J. M.; Edwards, D. Mechanism of hypoxic injury to pulmonaryartery endothelial cell plasma membranes. Am. J. Physiol. 257:C223–C231; 1989.
[37] Chen, Z. H.; Saito, Y.; Yoshida, Y.; Niki, E. Effect of oxygen concentration on freeradical-induced cytotoxicity. Biosci. Biotechnol. Biochem. 72:1491–1497; 2008.
[38] Weinmann, M.; Jendrossek, V.; Handrick, R.; Guner, D.; Goecke, B.; Belka, C.Molecular ordering of hypoxia-induced apoptosis: critical involvement of themitochondrial death pathway in a FADD/caspase-8 independent manner. Onco-gene 23:3757–3769; 2004.
[39] Carraro, F.; Pucci, A.; Pellegrini, M.; Pelicci, P. G.; Baldari, C. T.; Naldini, A. p66Shc isinvolved in promoting HIF-1alpha accumulation and cell death in hypoxic T cells.J. Cell. Physiol. 211:439–447; 2007.
[40] Chandel, N. S.; Budinger, G. R. The cellular basis for diverse responses to oxygen.Free Radic. Biol. Med. 42:165–174; 2007.
[41] Lukashev, D.; Sitkovsky, M. Preferential expression of the novel alternativeisoform I.3 of hypoxia-inducible factor 1alpha in activated human T lymphocytes.Hum. Immunol. 69:421–425; 2008.
[42] Haddad, J. J.; Land, S. C. A non-hypoxic, ROS-sensitive pathway mediates TNF-alpha-dependent regulation of HIF-1alpha. FEBS Lett. 505:269–274; 2001.
[43] Scharte, M.; Jurk, K.; Kehrel, B.; Zarbock, A.; Aken, H.; Singbaertl, K. IL-4 enhanceshypoxia induced HIF-1α protein levels in human transformed intestinal cells.FEBS Lett. 27:6399–6404; 2006.
[44] Lukashev, D.; Caldwell, C.; Ohta, A.; Chen, P.; Sitkovsky, M. Differential regulationof two alternatively spliced isoforms of hypoxia-inducible factor-1 alpha inactivated T lymphocytes. J. Biol. Chem. 276:48754–48763; 2001.