Project work Atta A J
-
Upload
independent -
Category
Documents
-
view
4 -
download
0
Transcript of Project work Atta A J
EFFECT OF THE NATIONAL HEALTH INSURANCE SCHEME (NHIS)ON THE FINANCIAL PERFORMANCE OF HEALTH INSTITUTIONS: ACASE STUDY OF BOAKYE DANKWA MEMORIAL HOSPITAL ASHANTI
REGION
A PROJECT WORK PRESENTED BY:
ATTA ADADE JUNIOR
(ACT05090266)
DECLARATION
I hereby declare that this submission is my own work towards theHigh National Diploma and that, to the best of my knowledge, it
i
contains neither material previously published by another personnor material which has been accepted for the award of any otherdegree, except where due acknowledgement has been made in thetext.
……………………………………………………………..
DATEATTA ADADE JUNIOR
(STUDENT)
I hereby declare that the preparation and presentation of thisproject work was supervised in accordance with the guidelines onsupervision of project work laid down by Kumasi Polytechnic.
……………………………………………………………..
DATEMR. BOADU AYEBOAFO
(SUPERVISOR)
I declare that a copy of the project has been submitted forinstitutional use.
…………………………….....………………………………
ii
DATEMR. ISHAQ KYEI-BROBBEY
(HEAD OF DEPARTMENT)
Table of ContentsDECLARATION.........................................................ii
CHAPTER ONE..........................................................1BACKGROUND OF THE STUDY..............................................1
1.1 INTRODUCTION.....................................................11.2 STATEMENT OF THE PROBLEM.........................................2
1.3 PURPOSE OF THE STUDY.............................................31.4 RESEARCH QUESTIONS...............................................4
1.5 SIGNIFICANCE OF THE STUDY........................................41.6 LIMITATION OF THE STUDY..........................................4
1.7 SCOPE OF THE STUDY...............................................51.8 ORGANISTION OF THE STUDY.........................................5
CHAPTER TWO..........................................................6LITERATURE REVIEW....................................................6
iii
2.1 INTRODUCTION.....................................................62.2 HISTORICAL BACKGROUND............................................6
2.3 INSURANCE-WHAT DOES IT MEAN?.....................................72.4 HEALTH-WHAT DOES IT MEAN?........................................8
2.5 HEALTH INSURANCE-WHAT IS IT?.....................................82.5.1 Types of Health Insurance......................................9
2.5.2 Objectives of Health Insurance.................................92.6 OVERVIEW OF THE NATIONAL HEALTH INSURANCE SCHEME................10
2.6.1 Objectives of the Scheme:.....................................102.6.2 Ownership and Administration of the Scheme....................11
2.6.3 Membership, Coverage and Benefit Package......................132.6.4 Financial Contribution........................................13
2.6.5 Fund Management...............................................14CHAPTER THREE.......................................................15
METHODOLOGY.........................................................153.1 INTRODUCTION....................................................15
3.2 RESEARCH DESIGN.................................................153.3 METHODS AND INSTRUMENTS.........................................15
3.4 ADMINISTRATION OF INSTRUMENT AND METHODS........................16CHAPTER FOUR........................................................18
DATA ANALYSIS.......................................................184.1 INTRODUCTION....................................................18
4.2 BACKGROUND OF THE HOSPITAL......................................184.2.1 The Vision of the NCHS........................................18
4.2.2 The Goal of the NCHS..........................................194.2.3 Catchment Area Basic Characteristics..........................19
4.3 NATIONAL HEALTH INSURANCE COVERAGE..............................194.3.1 Monitoring of Beneficiary Patients............................21
4.4 DISEASE INCIDENCE IN THE DISTRICT...............................21
iv
4.5 CONTRIBUTION OF THE SCHEME TO FINANCIAL PERFORMANCE.............224.5.1 Revenue Expenditure Trend of the Institution..................22
CHAPTER FIVE........................................................24SUMMARY OF FINDINGS, CONCLUSION AND RECOMMENDATIONS.................24
5.1 INTRODUCTION....................................................245.2 KEY FINDINGS OF THE STUDY.......................................24
5.3 CONCLUSION......................................................255.4 RECOMMENDATIONS.................................................25
References..........................................................26
List of Tables and Figures
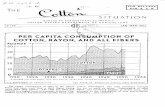
Figure 1: NHIS Status for 2011......................................20Table 2: Causes of OPD Morbidity from 2009 – 2011...................21
Table 3: IGF by Category for 2011...................................22Figure 2: Income and Expenditure Pattern from 2009 – 2011...........23
Appendix............................................................26
CHAPTER ONEBACKGROUND OF THE STUDY
1.1 INTRODUCTIONThe National Health Insurance Scheme (NHIS) was establish under
Act 650 of 2003 by the Government of Ghana to provide basic
healthcare services to persons resident in the country through
mutual and private health insurance schemes. The District Mutual,
Private Mutual and Private Commercial Schemes are regulated by
the National Health Insurance Council (NHIC). The object of the
v
NHIC is to secure the implementation of the national health
insurance policy that ensures access to basic healthcare services
to all residents of Ghana. The Council has the following
objectives:
Register, license and regulate health insurance schemes
Supervise the operation of health insurance schemes
Grant accreditation to healthcare providers
Perform other functions conferred upon it under Act 650 and
Regulations 1809
The NHIS derives its funds from;
The premiums paid by its subscribers.
2.5% of the National Health Insurance Levy.
2.5% of the Social Security and National Insurance Trust
(SSNIT) deducted from the formal sector.
Funds from the Government of Ghana (GoG) to be allocated by
Parliament and returns from investment.
One can register with the NHIS through an agent of the NHIS in
the community District NHIS office. Children less than 18 years
of age whose parents or guardians are contributors are not
required to pay premiums. Children in this category have to
register to obtain coverage. Full time students over 18 years of
age are required to pay the minimum premium of GHC 7.20 to enjoy
benefits. Those who are neither in Tertiary institutions nor are
contributions to Social Security are registered in the informal
sector.
vi
The elderly is covered under the NHIS. Residents 70 years and
over are exempted from payment of contribution. People in this
category should register to enjoy NHIS benefits. The Very Poor
(Indigent) is covered under the NHIS. A person is classified as
Indigent and exempted from payment of premium if she/he meets the
following;
Does not have any visible sources of income.
Does not have a fixed place of residence.
Does not live with a person who is employed.
A pensioner under SSNIT Scheme is not required to pay any
contribution to NHIS. If the spouse is not a SSNIT pensioner, 70
years of age or over 70 years, nor current SSNIT contributor,
she/he must pay a premium set for the informal sector.
The informal sector worker (self-employed) pays the informal
sector rates (at least GHC 7.20, max GHC48) to register to
receive healthcare coverage by NHIS.
One might ask of the advantages of the NHIS to its members. The
advantages include:
Members do not pay cash at the point of care.
The problem of converting assets to cash especially in case
of catastrophic illnesses can be avoided.
Furthermore, portability allows a NHIS member to access
services outside his/her district scheme.
vii
There are exclusions in the NHIS. These exclusions are mostly
specialist cases such as cancers except cervical and breast
cancers and dialysis for chronic renal failure. HIV/AIDS is not
covered but associated opportunistic illnesses like diarrhea,
tuberculosis, etc. are covered. In a situation where prescribed
drugs are out of stock, it is a member responsibility to visit
additional NHIS accredited pharmacies until the prescription can
be filled.
1.2 STATEMENT OF THE PROBLEMIt is presumed that the National Health Insurance Scheme (NHIS)
is having a negative effect on the financial performance of
Health Institutions. The primary objective of the NHIS is to
provide quality basic healthcare to all residents at the least
cost. As with any Non profit making organization (NPO), Health
Institutions will use a combination of financial and non-
financial objectives in order to achieve the aim of the NHIS.
Besides the introduction of the NHIS, health institutions were
using the cash and carry system. This is where patients were made
to make payments before services were rendered to them. With the
introduction of the NHIS, the health institution provides
services to patients before payment is made to the health
institution by the scheme. This usually causes delay in the
payment of monies by the scheme to the health institution. This
is because, documents to prove payment have to pass through a
bureaucratic process.
viii
The delay by the scheme to the institution makes it difficult to
mobilize enough funds to administer its internal operations,
which makes patients to directly buy drugs at the pharmacies.
Also as a result of the delay in payment, the health institutions
purchase drugs outside on credit basis from suppliers which
increase their gearing ratio (Debt component). At times as a
result, suppliers feel reluctant in supplying drugs and other
services.
In addition, staffs are not well financially motivated because
the institutions do not have sufficient funds to boost their
moral. The cash and carry system was a major source of the
finance to the health institutions and had a positive impact on
its financial performance. Therefore its critical examination is
crucial to determine the possible effects the NHIS on the
financial performance of health services. There is therefore the
need to know why there is a delay in the payment of monies to the
health services.
1. Are these actions deliberate?
2. What factors account for this inability to refund on time?
3. Are the lapses on the part of the health institutions or on
NHIS?
The negative effects are in most health institutions in Ghana, of
which has caused the researcher to find out the causes and how
the problems can be minimized if not eliminated.
ix
1.3 PURPOSE OF THE STUDYThere is an assumption that the NHIS is having a negative effect
on the financial performance of health institutions. The purpose
of the study is to find out whether this assumption is true, the
factors responsible for this canker by looking at the financial
performance of health institutions and come out with suggestions
and recommendations to guide the management of health
institutions to improve on its financial performance. This
objective forms the basis for the research questions that provide
support for the main point of the study.
1.4 RESEARCH QUESTIONSAn analysis of the above stated purpose and review of the
literature, the following research questions were appropriate to
form the focus of the study:
1. What can management do to reduce or eliminate the negative
effect of NHIS on the financial performance on the health
institutions?
2. What can the registrar of the NHIS do to reduce this
problem?
3. What factor accounts for the delay in payments of monies by
the NHIS to the health institutions?
x
1.5 SIGNIFICANCE OF THE STUDYThe purpose of the research is that, the information provided
would help the management and the beneficiaries of NHIS as well
as the general public aware of how the system operates and how
the problem associated with the negative effects on the financial
of health institutions would be reduced if not eliminated.
It is hoped that, this study will bring to light the extent of
the negative effects the NHIS has on the financial performance of
the health institutions, the result on its general operations and
long term survival. The study is also expected to contribute to
academic knowledge and possibly lead to another research on the
problem.
1.6 LIMITATION OF THE STUDYCertain weakness of the study could influence the results or its
purpose but which the research had little or no control. The
extent to which data collected could give a reliable picture
about the study would depend on a large extent on the validity of
the questionnaires and objectives of the respondents. It is
inappropriate to use one health institutions to form an opinion
since every health institution has its own internal policies and
even different methods of financial operations. The results and
recommendation may not be applicable to all health institutions.
1.7 SCOPE OF THE STUDYThere cannot be a research without a problem. The researcher
encountered some problem in terms of access to information sincexi
some respondent were reluctant to give out information for fear
of divulging, especially workers of health institutions who were
approached, movement from one institutions to another in search
of information was difficult. The researcher therefore could not
get all necessary information for the study. The research was
therefore limited to the Boakye Dankwa Memorial Hospital Ashanti
Region. The main focus is on the effect of NHIS on the financial
performance of health institutions.
1.8 ORGANISTION OF THE STUDYThe research study has been grouped into five (5).
Chapter one deals with the background of the study, statement of
the problem, purpose of the study, significance of the study and
research questions. Other aspects of the chapter are organization
and limitation of the study. Chapter two deals with the
literature review. Chapter three is on methodology which
describes the research design, the population and sample
procedures, instrumentation and data collection procedures of the
study. In chapter four, result and discussion of the findings are
presented. Finally in chapter five, summary of findings
conclusions and recommendations to end the study.
xii
CHAPTER TWOLITERATURE REVIEW
2.1 INTRODUCTIONThis chapter covers the review of literature on the National
Health Insurance scheme in Ghana. It begins with the general
background of health insurance pursues to review the Ghana
government perception of the schemes operation, and ends with the
current literature relevant to this study.
2.2 HISTORICAL BACKGROUNDLike Africa economies in general, African’s health care sector
has undergone dramatic changes in the post independence years.
Many countries began independence with welfare states that
provided health care on a free or at least heavily subsidized
basis to user of public health services, but these services were
rarely available to people outside urban areas and mining
enclaves. However, real public sector per capital expenditure in
the health sector has been declining in many African countries
since the late 1970’s. One of the main impacts of the economies
crisis of the 1970’s and 1980’s on the social and welfare sectors
such as health was the reduction of state subside to these areas
in an effort to cut deficit levels.
xiii
Another aspect of the policy to reduce budget deficit was the
introduction of the user fee at public health care institutions
to recover some of the cost of running such institutions. The
circumstance that made implementing such cost recovery system
favorable include, rundown public services, the complaints of
health care providers, competitions from private sources of
service provision and increasing cost of assets to care of
acceptable quality as well as external pressure on conditionally
(Crease and Kutzon 1995), cited by Chris Atim. The mutual health
organizations began to spread in response to the health care
sector crisis and more specifically because of, the following
four factors:
a) The introduction of user fee at existing publicly provided
health facilities.
b) The introduction of such fees in the context of generally
unacceptable quality of public services which reinforce
people willingness to pay for better quality health care.
c) The rise of alternative private sources of health care
provision, frequently associated with good quality.
d) Finally, the general democratization and development of
civil society in the last decade. (Chris Atim 1998)
By 1980’s, ninety (90) developing countries were studied. Forty
(40) were using one or more forms of insurance to provide medical
services. (Zschook D. K. 1982 cited in Arhin D. C. 1995).
xiv
ILO also in a 1990 survey of 28 African countries found that
whiles countries like Ghana had virtually no social security or
social partnership scheme in the health care sector, others like
Gabon, Kenya, Tunisia, Cape Verde and Egypt had public health
services combined with classical social insurance. (ILO 1993
cited byYao-Dablu K.K.).
In Vogel (1990 b), he defined health insurance, ‘as the formal
pool of funds held by third party or by the provider in the case
of health maintenance organizations’.
It can also be defined as a health plan to provide health care
service for people in an area in exchange for payment of a
premium.
In Ghana, the National Health Insurance Scheme was established
under Act 650 of 2003 by the Government of Ghana to provide basic
health care service to persons resident in the country through
mutual and private health insurance schemes.
2.3 INSURANCE-WHAT DOES IT MEAN?Insurance may be defined as, ‘a formal social device for reducing
risk by transferring the risk of several individual entities to
an insurer’. The insurer agrees for a consideration, to assume to
a specific extent, the losses suffered by the insured (Handbook
on National Health Insurance). It can also be defined as a system
xv
of cover for risk or uncertain event by prior sharing of the
expected cost among many individuals.
The International Labour Organization (ILO) also defines
insurance as being the reduction or elimination of the uncertain
risk of loss for the individual or household by combining a large
number of similar exposed individual or household who are
included in a common fund that make good the loss cost to anyone
member. (ILO 1996). The main purpose of insurance is to
compensate the insured if he incurs a loss in relation to what
has been insured. Insurance is operated by collecting regular
contributions called the premium from person’s who take up
insurance policies with an insurance company. Any insured person
who incurs a loss is then indemnified by the insurance company.
Insurance is thus based on the principle of pooling of risk.
Several people contribute to a common fund out of which those who
incur losses are compensated. Insurance in this way lightens the
burden of risk that would have fallen on one person.
2.4 HEALTH-WHAT DOES IT MEAN?According to the World Health Organization’s (WHO) definition,
‘health is a complete state of physical, mental and social well-
being, and not only the absence of illness or infirmity’. This
means, the entire human system must be free from any form of
short comings not necessarily illness or infirmity but also
mentally and socially sound. It is therefore very important for
xvi
care to be taken against anything that could pose a problem to
the human health, because human life without health is valueless.
2.5 HEALTH INSURANCE-WHAT IS IT?According to the handbook on the National Health Insurance
Scheme, Health Insurance is an insurance method which provides
members of a defined group of community with protection against
cost of medical treatment resulting from sickness bodily injury.
The insured, under a health insurance scheme, exchange for
premium payment, passes on the cost of his/her medical expenses
incurred within the agreed health benefit package to the
insurance scheme for payment. Health Insurance can be organized
in many different ways with different implications. For the
organization and delivery of health service at a minimum, it is a
means of paying for health care and of ensuring access to service
by providing a mechanism for sharing a risk of incurring medical
expenditure among different individuals. This definition implies
that:
a) There must be a financial cost ties to the use of health
service and
b) People are able and willing to use the insured health
services when they perceive themselves to be sick.
The latter point reflects the importance of physical access to
services of acceptable qualities. To be effectively insured,
xvii
therefore implies both financial protection and access to
desirable health services. (Joseph Kutzin 1996).
2.5.1 Types of Health InsuranceThere are two main core types of health insurance; these are
social and private actuarial health insurance schemes. There are
variations of these two types. Social health insurance schemes
include community based schemes and employee based scheme. Other
forms of the private actuarial health insurance arrangements are
Health Maintenance Organizations (HMO’s) and Preferred Provider
Organization (PPO’s). Both are types of private health insurance
scheme which came into preeminence in the United States during
the 80’s. (Donaldson and Gerard, 1993) cited by Yao-Dablu K.K.
i. Social Health Insurance
Social health insurance systems pay for health services through a
health fund. The most common system for contribution is the
payroll system, with contributions from both employer and
employees. Contributions are based on ability to pay and access
to service depends on reed. The health fund is usually
independent government, but works within a tight frame-work of
regulations. It is normal under social health insurance for
entitlement to services to be listed in details, and for
contribution rate to be set at level intended to ensure that
these entitlements can be met.
xviii
2.5.2 Objectives of Health InsuranceHealth insurance schemes are a mechanism for mobilizing community
resources to share in the financing of both local health
services. In addition to serving as a financing mechanism, health
insurances schemes aim to achieve the following objectives:
a) Improving access; schemes seek to increase access to health
care for those who have some capacity to pay but who may not
be able to pay user fee for each visit by a family member.
b) Improve quality; health insurance scheme can contribute to
quality health care which makes people ready to pay for the
health care. Health insurance schemes could make a
significant impact on the quality of health care through
their contractual relations with health care providers.
(Stephen Musau 1999).
c) Schemes seek to increase the efficiency in the allocation
and use of available resource through improved accounting,
financial management and utilization management tools. This
enables more accurate identification of inflows and uses of
funds, which in turn helps prevent fraud and abuse of the
system.
d) Equity; schemes attempt to make health service more
equitable. Health insurance can narrow the disparity in
health services available to those who have health care and
those who do not by scheduling premiums or membership
payment to coincide with the seasonal availability of
people’s income, often related to harvest.
xix
2.6 OVERVIEW OF THE NATIONAL HEALTH INSURANCE SCHEMEFollowing the introduction of the fee for service (cash and
carry) system into Ghana’s health sector in the 1980’s, many
patients began to have difficulty with paying for their health
care especially admission cost. As a result, many did not go to
the hospital until it was too late or their illness had advanced
to a more complicated phase. Others who were admitted and treated
subsequently absconded without paying for their treatment. Many
individuals quite simply could not afford to pay for their care.
The population therefore had reduced access to hospital services
and in turn, this had a negative impact on the financial
performance of hospitals(Chris Atim, March 2000).
2.6.1 Objectives of the Scheme:The main objective of the scheme as in its initial project
document was to reduce the cost per individual hospital
admission, thus making service accessible to all within the
country. In the scheme’s report of 1998, these same objectives
were restated.
1. To encourage the people to pall their financial resources
together to cater for their hospitalization bills.
2. To improve the country’s population economic accessibility
to curative care by making health delivery more accessible
and affordable
xx
Although not explicitly stated as an objective, it is clear that
improving the scheme would also lead to more reliable revenue for
the hospital by at least reducing bad debt and attracting more
clients. (Chris Atim, March 2000)
2.6.2 Ownership and Administration of the SchemeIn terms of the typology of mutual health schemes emerging in
Ghana, the country has no direct role in its management and
policy making. The scheme has in effect run as it was another
department of the hospital with its staff and management
subordinate to the hospital management. As a result, the scheme
enjoys no separate legal status as a corporate body and therefore
has no need for a separate constitution. There are however rules
and regulations governing membership and access to its services
(which are described as scheme policies). These are revised
annually before the registration exercise and circulated within
the community.
The rules (those relating to 1998/1999) state that, membership is
by entire family unless it is in the case of an individual living
alone. Children born after the annual registration can be
registered within forty (40) days after delivery and membership
is not transferable. The organization chart of the scheme
reinforce the point that the scheme is not separate from the
hospital and it is not controlled by the country, though some key
persons in the country are present at the top level of the
structure . (Chris Atim, March 2000).xxi
The scheme is administered through five (5) main hierarchical
units. These are Field workers, Zonal coordinators, District
coordinator, Insurance Management Team (IMT) and Insurance
Advisory Board (IAB).
i. Field Workers
In each zone, there are people who carry out the registration and
education of the people on the scheme. They are selected by the
management of the scheme. They are to possess at least a JHS or
Middle School Living Certificate. They should be able to write
and interpret records. Their remuneration is on commission basis;
that is depending on the premium collected.
ii. Zonal Coordinator
For the purpose of effective management of the scheme, districts
have been developed into zones. Each zone had coordinators with
one of them as their leader. Their selection is similar to that
of the field workers but they are expected to have experience in
leadership and be people of high moral character and proven
integrity. They coordinate the activities at the zonal level and
act as liaison officer between the district coordinators, field
workers and the country.
iii. District Coordinator
He is the link between the insurance management team, zonal
coordinators and field workers. He is to conduct educational
xxii
fora, coordinate all scheme activities on the field and to
supervise zonal coordinators and audit record sheet and accounts
of the field workers. He also seeks to the welfare of the
insured, conducting checks to prevent impersonation and
investigate all cases reported to him. He reports to the manager
of the scheme. He should possess at least a higher secondary
school certificate and has undergone in-service training in
management and administration.
iv. Insurance Management Team
The IMT is the decision making body of the scheme. It is composed
of the manager, the district coordinator and his assistant,
district director of medical service, the district health service
administrator and medical nursing administrators.
The officer in charge of the scheme is responsible for the day-
to-day management of the scheme. The IMT ensures good
communication and working relationship between the scheme, the
hospital and the other partners. In taking decisions, the IMT
consultation with the Insurance Advisory Board (IAB), the
Hospital Management Team (HMT) and Diocesan Health Officer (DHO)
sit together. The DHO receives report from IMT through Advisory
board.
v. Insurance Advisory Board
It is made up of the key players in a country and opinion leaders
of recognized groups in a country. There is representation on the
xxiii
board for the traditional council, the District Chief Executive
and religious groups, educational heads and other equally
recognized groups or leaders in the country. They are
constitutionally obliged to meet ones every month and to advise
on issues concerning the scheme as and when necessary.
2.6.3 Membership, Coverage and Benefit PackageMembership of the scheme is voluntary. It is open to all citizens
of Ghana who are willing to contribute a premium. During a
stipulated period each into fund finance the impatient care of
those members who will fall sick within the year (the insurance
year is from February to January). It is insisted that a whole
family would have to register. This is aimed at reducing the
problem of adverse selection, premium calculation is uniform and
per individual, registration of newly born babies are permissible
at any time during the year but should be done between first
forty(40) days after delivery, membership rates are not so high.
The highest coverage since the inception of the scheme was 33.2%
of the estimated total population in 1993. The scheme provides
financial coverage for the total impatient bill of the registered
members at any hospital that has registered with the scheme; such
bills are considered as inpatient expenses (out-patient
department [OPD] or emergency unit on day of admission)
Exemptions from the scheme include the following;
i. Out-patient treatment.
xxiv
ii. Detention at out-patient department for less than twenty
four (24) hours.
iii. Normal deliveries.
iv. Admission with complications resulting from self-induced
abortions.
v. Treatment cost at other health institution (not registered
with the scheme) when referral was at patients request.
vi. Admission for treatment as a result of alcoholism. (Daablu-
Yaw K.K.2000)
2.6.4 Financial ContributionThe scheme charges an annual flat or premium per head
irrespective of age or sex. These premium must be paid during
single registration period lasting two months from September to
October every year, (except in the case of newborn babies who can
be registered any time after birth for up to forty [40] days).
Currently, the premium of newly registered members is Twelve
Ghana Cedis (12.00) while existing members pay Nine Ghana Cedis
(9.00). Other sources of finance are donor support and returns of
investment. The premium over the years depending on the hospital
cost, inflation and utilization levels expected.
2.6.5 Fund ManagementIn order to ensure that funds that are collected once a year are
able to cover the financial commitments of the scheme for the
whole year. The funds collected are invested in government bonds
xxv
and fixed deposits at banks, revenue from these investments help
to cover the health insurance scheme. For instance, revenue from
1997, 1998 financial year formed 8% of the total income that
accrued to the scheme.
i. Provider Payment Mechanism
The scheme pays the provider (Boakye Dankwa Memorial Hospital) on
a fee for service bases. The attending physician or nurse knows
the services performed on the in-patient admission card. If the
inpatient is insured, that insured person would hand over his/her
insurance card to the person in charge of the ward arrival, who
writes the number of insurance card on the hospital admission
card. An account clerk makes regular runs to record (from the
admission card). The details of services performed on the
admitted patients, the number of their insurance card as well.
This information is used by the department to prepare cost
corresponding to the admitted person. A monthly bill summarizing
the cost of care provided to insure in-patient is prepared by the
accounts department and submitted to the insurance manager for
payment.
This bill detail month numbers of in- patients and cost incurred
broken down into the following categories; Laboratory, Drugs, X-
ray, Material and Others.
xxvi
CHAPTER THREE
METHODOLOGY3.1 INTRODUCTION The chapter mainly covers the procedures and the justification
for their adoption. To ensure the collection of reliable and
accurate data for the research work; certain procedures and
methods were adopted. The various methods for data collection can
be described under the following sub-topics
1. Research Design
2. Population and Sampling
3. Methods and Instruments
4. Administration of Instruments
3.2 RESEARCH DESIGNThe research which is a case study of National Health Insurance
Scheme in Boakye Dankwa Memorial Hospital was viewed as something
that needs to be researched into. The researcher decided to
collect and collate data about the insurance scheme. The data
collected would provide a better insight into the operation of
the health insurance scheme from which conclusion could be drawn.xxvii
The data was both quantitative and qualitative in nature.
Quantitative in a sense that numerous instruments such as;
questionnaires and interviews, among others were used to get all
needed information for analysis. Again on the question of
qualitative nature of the data, all possible procedures were
adopted to collect the accurate and reliable source of
information to make generalization of the work possible.
3.3 METHODS AND INSTRUMENTSThis sub-topic presents a description of the methods and
instruments employed in this research study to obtain
information. The data and information of this work were obtained
through these methods and instruments;
Interview
Library search
Questionnaire
The methods and instruments listed above had different purposes
to the research work.
The interview approach was aimed at finding out the
responsibilities of managers of the scheme to hospital
administrators of Boakye Dankwa Memorial Hospital in Kumasi on
the performance of the scheme and the possible measure of
improvement.
Library Search also aimed at knowing the option of other writers
as far as the National Health Insurance Scheme is concerned.
xxviii
Finally, the questionnaires are designed to collect primary and
secondary information from the trustees; who are the scheme
administrators (management), the insured; who are the
beneficiaries and the hospital administrators who are the service
providers. This purposed at knowing the different views they hold
on the Health Insurance Scheme as a means of financing health
care.
3.4 ADMINISTRATION OF INSTRUMENT AND METHODS
This sub-topic explains in detail how the below methods and
instruments were administered.
i. Interview
ii. Library search
iii. Questionnaire
i. Interview
The interview was conducted on the individual bases and was
granted by the hospital administrators and beneficiaries. The
length of the interview lasted from 30 to 45 minutes and hand
writing notes were made during the interview. It took almost
three weeks.
xxix
ii. Library Search
Under library search variety of authority book tracks, handbills
and others were consulted. Books related to health and insurance
were used, to know the meaning of health and insurance and then
blending them together.
iii. Questionnaire
On the administration of the questionnaire, questions were
designed for the management of the hospital to obtain the primary
and secondary information as well data.
The questions were aimed at finding their views on the effect of
the scheme (The National Health Insurance Scheme) on the
financial performance of the health institution.
Well structured questions were designed for the hospital
administration. This was to deduce how the introduction of the
National Health Insurance Scheme is making health care accessible
to the population within the catchments area. It was to find out
if there is a future for the health institutions with the
introduction of Health Insurance Scheme. The questionnaire for
the hospital administrator comprised open-ended questions, and
pre-coded questions. Refer to appendix xx. The questionnaires
were left for the administrators to answer at their own
convenient time.
xxx
CHAPTER FOUR
DATA ANALYSIS
4.1 INTRODUCTION
This chapter presents data that were collected from the Boakye
Dankwa Memorial Hospital. The main areas of the chapter include
the background of the hospital, the coverage of NHIS, the disease
incidence in the hospital as well as the financial performance of
the hospital in sequential with the NHIS.
4.2 BACKGROUND OF THE HOSPITAL
Boakye Dankwa Memorial Hospital was established in May 1992 by Dr
Boakye Dankwa. He has been responsible for the infrastructural
development and provision of resources while he employed others
to take care of the managerial and administrative work for the
last twenty (20) years that the hospital has been in existence.
It is located in Kumasi, Dichemso to be precise in the Ashanti
Region.
xxxi
4.2.1 The Mission and Vision of the hospital
“To provide quality and affordable healthcare for all that, leads
to the general well being of all individuals in the Ashanti and
beyond”. This “mission and vision” adheres to the mission
statement of the national health insurance scheme.
4.2.3 Monitoring of Beneficiary Patients
Since there is reimbursement of funds spent on the insured
clients, the management has put in measures to tract patients
that have been provided with the services. The study found that
the main tracking systems are the use of in-patient register and
electronic database of patients attendance.
4.4 DISEASE INCIDENCE IN THE HOSPITAL
In the hospital, the main diseases that are common for three
successive years are malaria, Respiratory tract infections and
Typhoid fever. These three diseases alone account for over 50% of
all OPD cases. This implies that these are the cases mostly
treated by the NHIS. Table 2 shows three top diseases that are
treated mostly under NHIS.
xxxii
Table 1: Causes of OPD Morbidity from 2009 – 20112009 2010 2011
No.Conditi
on
% Conditio
n
% Conditio
n
%
1 Malaria 36.5 Malaria 38.0 Malaria 39.3
2
Respira
tory
tract
infecti
on
8.5
Respirat
ory
tract
infectio
n
9.0
Respirat
ory
tract
infectio
n
9.1
3Typhoid
fever4.5
Typhoid
fever4.9
Typhoid
fever5.3
4 Others 50.5 Others 48.1 Others 46.3
Source: Annual Report, 2011
As indicated in Table 1, malaria continues to increase in both
proportion and absolute figures while all other diseases continue
to increase at a decreasing rate. Malaria increased from 36.5% in
2009 to 39.3% in 2011.
xxxiii
4.5 CONTRIBUTION OF THE SCHEME TO FINANCIAL PERFORMANCE OF THE
HOSPITAL
The introduction of the NHIS has an influence over the financial
performance of the hospital. According to the study, the
existence of the NHIS has improved the financial performance of
the health institution. Table 3 shows the main categories of IGF
for the institution. From Table 3, out of the total IGF, the NHIS
contributes 98.5% while the remaining 1.5% comes for direct
payment for health services.
Table 3: IGF by Category for 2011Revenue NHIS % Paying Total %
Medicines
217,319.
37
97.7 5,012.
68
2.3
222,332.05
100
Non
Medicine
1,071,07
3.71
98.7 14,317
.91
1.3 1,085,391.
62
100
Total
1,288,39
3.08
98.5 19,330
.59
1.5 1,307,723.
67
100
Source: Annual Report, 2011
The continuous reimbursement of quarterly claims is the major
source of internally generated fund for the institution. The
study established that with improved financial performance, the
institution is able to improve its service delivery. This is
because there is ready fund to run the institutions.
xxxiv
Prior to the establishment of the NHIS, some clients who default
payment for services rendered increased the debt ratio of the
hospitals. However, the current system has reduced and in fact
eliminated defaulters in the system. Though the quarterly claims
sometimes come very late, it has relatively improved the
financial performance of the district.
4.5.1 Revenue Expenditure Trend of the Institution
The financial performance of an institution and for that matter,
health institution is better understood when the expenditure
pattern is compared with the revenue. The institution is not only
doing well in terms of raising funds from the NHIS but equally
performing well in the revenue-expenditure pattern. Figure 2
shows the expenditure and revenue pattern of the district.
xxxv
Figure 2: Income and Expenditure Pattern from 2009 – 2011
0.00
200,000.00
400,000.00
600,000.00
800,000.00
1,000,000.00
1,200,000.00
2009 2010 2011
Amou
nt (G
H¢)
Incom eExpenditure
Source: Annual Report, 2011
As indicated in the figure, from 2009 to 2011 the revenue pattern
has continuously exceeded the expenditure pattern.
xxxvi
CHAPTER FIVE
SUMMARY OF FINDINGS, CONCLUSION AND RECOMMENDATIONS
5.1 INTRODUCTION
This chapter presents the key research findings, the conclusion
and recommendations. The findings are presented in line with the
key components of the research.
5.2 KEY FINDINGS OF THE STUDY
The institution depends much on its internal generated
funds. There was an appreciable increase in revenue
generation from 2010 to 2011. This saw an increase of 24.4%
over 2010 revenue. The revenue trend of the institution has
over the three years exceeded the expenditure level. This
testifies that the NHIS has had a positive effect on the
financial performance of the institution.
There is wide acceptance of the National Health Insurance
Scheme. This is evident by the fact that 99.5% of the
district population has registered with the scheme.
Discussing with the institution revealed that renewal of the
xxxvii
premium has been regular. This has contributed to the
internal generated funds of the institution.
The high proportion of registered members has influenced the
category of clients at the hospital. At the hospital level,
a greater proportion of the clients (97.6%) at the OPD are
registered members of the NHIS.
Though the scheme is doing well in terms of financial
performance, a major challenge is the delay in reimbursement
of quarterly funds. This according to management can be
traced to the national level.
The major disease in the district is malaria. This has been
the leading cause of OPD attendance for the past three
years. Besides being the top cause of OPD attendance, the
incidence is increasing at a high rate.
5.3 CONCLUSION
The introduction of the National Health Insurance Scheme improved
the financial performance of the institution. Sustainability of
good financial performance is contingent on the level of
patronage of the both the NHIS and the hospital. Where there is
poor service delivery at the hospital level, there will be the
tendency to change institution. The NHIS is better than the cash
and carry system in the sense that with the NHIS, the level of
xxxviii
payment defaulters has reduced. Therefore there is some level of
certainty that once services have been rendered to insured
clients will to be reimbursed.
5.4 RECOMMENDATIONS
Based on the findings of the study, the following recommendations
are made to sustain and perhaps improve the financial performance
of the institution.
The institution need to improve the services rendered to
clients. This is to motivate the patronage of the
institution anytime the need arises. According to management
of the institution, furnishing of the waiting rooms at the
hospital, adequate beds and provision of quality drugs are
some of the services that can be improved.
There is the need for the national level to timely release
the quarterly reimbursement to the institutions. This will
ensure timely availability of funds at the institution level
to effectively carry out its services.
xxxix