Primary breast lymphoma
-
Upload
independent -
Category
Documents
-
view
1 -
download
0
Transcript of Primary breast lymphoma
Cancer Treatment Reviews xxx (2014) xxx–xxx
Contents lists available at ScienceDirect
Cancer Treatment Reviews
journal homepage: www.elsevierheal th.com/ journals /c t rv
Tumor Review
Primary breast lymphoma
http://dx.doi.org/10.1016/j.ctrv.2014.05.0100305-7372/� 2014 Elsevier Ltd. All rights reserved.
⇑ Corresponding author at: Peter MacCallum Cancer Centre, Locked Bag 1,A’Beckett St, East Melbourne, Victoria 8006, Australia. Tel.: +61 3 9656 1076; fax:+61 3 9656 1408.
E-mail addresses: [email protected] (C.Y. Cheah), [email protected] (B.A. Campbell), [email protected] (J.F. Seymour).
1 Tel.: +61 3 9656 1915; fax: +61 3 8678 0636.2 Tel.: +61 3 9656 1111; fax: +61 3 9656 1408.
Please cite this article in press as: Cheah CY et al. Primary breast lymphoma. Cancer Treat Rev (2014), http://dx.doi.org/10.1016/j.ctrv.2014.05.01
Chan Y. Cheah a,b,1, Belinda A. Campbell b,c,2, John F. Seymour a,b,⇑a Department of Haematology, Peter MacCallum Cancer Centre, East Melbourne, Melbourne, Victoria, Australiab University of Melbourne, Parkville, Melbourne, Victoria, Australiac Division of Radiation Oncology, Peter MacCallum Cancer Centre, East Melbourne, Melbourne, Victoria, Australia
a r t i c l e i n f o a b s t r a c t
Article history:Received 17 March 2014Received in revised form 22 May 2014Accepted 26 May 2014Available online xxxx
Keywords:Primary breast lymphomaBreast neoplasmsNon-Hodgkin lymphomaReview articleExtranodal lymphoma
Primary breast lymphoma is a rare form of extranodal lymphoma, defined by the presence of a primarylesion within the breast with or without regional nodal involvement but no other extra-mammary sites ofinvolvement. It comprises diverse histologic subtypes, but diffuse large B-cell lymphoma is the mostcommon. In this review, we describe in detail the clinical features, diagnosis and staging, pathogenesis,risk factors and therapy of primary breast diffuse large B-cell lymphoma. We consider choice and numberof cycles of chemotherapy, the indications for radiotherapy and discuss the need for central nervous sys-tem prophylaxis. We also provide a brief overview of the less commonly encountered histologic subtypesincluding marginal zone, follicular, Burkitt and breast implant associated anaplastic large cell lymphoma.We conclude with a suggested treatment approach and potential areas of future research.
� 2014 Elsevier Ltd. All rights reserved.
Introduction
Primary breast lymphoma (PBL) is a rare but distinct extranodallymphoma subtype, comprising 0.5% of breast malignancies,around 1% of all non-Hodgkin lymphoma (NHL) and <3% of extran-odal lymphomas [1–6]. Over 98% of cases occur in women [2–10];the most common histology is diffuse large B-cell lymphoma(DLBCL). The case definition proposed by Wiseman and Liao, mod-ified by Hugh et al. requires the presence breast tissue in closeproximity with lymphoma, no antecedent diagnosis of lymphomaand no extramammary disease other than ipsilateral axillary nodes[11,12]. A strong case can be made to also include patients withinvolvement of regional (supraclavicular and internal mammary)nodes, and we use this slightly broader definition throughout thisreview. Patients with bilateral breast involvement without evi-dence of distant disease beyond regional nodal involvement shouldalso be included. Secondary breast lymphoma is defined by thepresence of systemic lymphoma with concurrent or subsequentinvolvement of the breast. In practice it is often difficult to distin-guish between primary breast involvement with secondarydissemination and primary involvement at another site with
secondary breast involvement. Although this review will mainlyfocus on primary breast DLBCL (PB-DLBCL), an overview of rarerhistologies will be presented.
Clinical features
The median age at diagnosis in Western countries 62–64 years,however the age range is broad [2–4,9]. In East Asian countries themedian age is lower (45–53 years) [8,10,13–15], a finding which(as with breast carcinoma) likely reflects differences in demographicsrather than biology [16]. PBL almost exclusively affects women – ahandful of male cases have been reported; although data are limited,outcomes appear similar [4,17–21]. Clinically, PBL is difficult to dis-tinguish from breast carcinoma as both typically present with a pain-less breast mass [2,9,22]. The right breast is involved slightly morefrequently for reasons that are unknown [2,4,8,22,23]. Constitutionalsymptoms are uncommon, reported in 4% of patients and usuallyindicative of disseminated disease [2,4,8–10,22]. Cutaneous manifes-tations, nipple retraction and discharge are rare [6,24]. The mediantumor diameter is 4 cm, although masses of up to 20 cm have beenreported [4].
Diagnosis and staging
Although up to 20% of patients are diagnosed following detec-tion of a mass by screening mammography [22,25]. Sabaté et al.noted differences between the mammographic appearance of PBL
0
2 C.Y. Cheah et al. / Cancer Treatment Reviews xxx (2014) xxx–xxx
compared with breast carcinoma, proposing size (4–5 cm in lym-phoma, 2–3 cm carcinoma) and the absence of spiculation, calcifi-cation and architectural distortion in the surrounding tissue asdistinguishing characteristics [24]. The same study found patientswith PB-DLBCL had diffuse opacity, whilst those with low-gradehistology a nodular pattern [24]. However, no radiologic featuresare truly diagnostic and biopsy remains mandatory. The sono-graphic and magnetic resonance imaging (MRI) features are alsonon-specific and have been reviewed in detail elsewhere [6]. Giventhe superficial anatomic location of most lesions, when possiblewithout extensive surgery or patient morbidity, excisional biopsyshould be performed to facilitate correct diagnosis. When this isnot feasible, core biopsy under imaging guidance is an acceptablealternative. Although fine needle aspiration may differentiate car-cinoma from lymphoma, it lacks architectural detail necessary toaccurately classify subtypes of NHL and thus is insufficient as adiagnostic procedure.
Recommended staging procedures for PB-DLBCL are as for nodalDLBCL and include whole body positron emission tomographywith computed tomography (PET-CT) and bone marrow biopsy.Although the contralateral breast should be examined for bilateralinvolvement, PET-CT should detect contralateral lymphomatousinvolvement. Ultrasound can be reserved for guiding biopsy of sus-picious lesions. Given that the risk of central nervous system (CNS)involvement in PB-DLBCL appears to be higher than nodal DLBCL,we also recommend lumbar puncture for cerebrospinal fluid(CSF) analysis by cytology and flow cytometry (which has greatersensitivity for occult CNS involvement) [26]. MRI of the brainshould be performed if neurologic manifestations are present. Atdiagnosis 70% of patients are stage IE, whilst 30% have regionalnodes involved (stage IIE) [2,4,8]. Bilateral breast involvement ispresent in 4–13% at diagnosis although the cumulative incidenceapproaches 30% [2,4,8,27,28]. The staging of bilateral breastinvolvement is controversial, with expert opinion divided betweenallocation to stages IE, IIE and IV. In contrast to primary testicularlymphoma (where patients with bilateral involvement are consid-ered stage IE/IIE due to their similar prognosis [29], bilateralinvolvement of the breasts appears to be a feature of aggressivedisease with poor prognosis [4,28]. We consider bilateral diseasestage IIE, as the adverse prognosis can be conveyed using thestage-modified International Prognostic Index (IPI), which substi-tutes one point for stage II in place of stage III/IV [30].
Risk factors and etiology
Data concerning the specific risk factors for PBL are scarce. Anumber of investigators have observed concurrent lesions withthe morphologic features of both marginal zone lymphoma (MZL)and DLBCL in the same biopsy specimen, suggesting histologictransformation from low-grade lymphoma is responsible for atleast some cases of PBL [4,31]. Niitsu et al. found cytogenetic evi-dence of 18q21/BCL2 translocations in three patients with germinalcenter B-cell phenotype, suggesting that some cases of PB-DLBCLprobably arise from follicular lymphoma [32].
Role of estrogen
The nearly exclusive incidence in females suggests a role for sexhormones in the pathogenesis of PBL. Epidemiological data regard-ing estrogen as a risk factor for lymphoma are mixed [33–35] but arecent large study found a 29% increase in risk of developing NHL(but not specifically PBL) for women treated with unopposed estro-gen hormone replacement therapy compared with women neverexposed [36]. The role of estrogens on carcinogenesis is complex,but the cellular effects of estrogen depend on the balance of the
Please cite this article in press as: Cheah CY et al. Primary breast lymphoma. C
two isoforms of estrogen receptor (ERa and ERb) present in the tar-get organ or tissue [37]. ERa predominates in breast, uterus andprostate, and receptor signaling results in cellular proliferation[38]. In contrast ERb is predominant in ovary, lung, CNS and leuko-cytes, and stimulation has an anti-proliferative effect [39]. Ofrelevance to PBL, ERb is found on lymphoma cell lines [40] andERb-selective agonists have demonstrated potent in vitro andin vivo activity against ERb expressing lymphomas [41]. Activationof ERb has been shown to inhibit angiogenesis and lymphangio-genesis in vivo [42]. ERa expression by PBL was demonstrated byimmunohistochemistry 4/40 (10%) in three older case series[12,43,44]. Furthermore, ERb expression has been demonstratedon primary human MCL cells [42]. The empiric use of the selectiveestrogen receptor modulator tamoxifen (an agonist of ERa but notERb) as a therapeutic strategy, with one success and one failure[12,45]. Analysis of ERb expression in a larger cohort of patientswith PBL appears warranted, given the promising preclinical activ-ity of selective ERb agonists.
Autoimmune disease
A number of case series have reported high prevalence of ante-cedent autoimmune diseases such as Hashimoto’s thyroiditis (19–30%) [46,47]. Although robust data directly addressing the risk ofPBL in such patients are lacking, the increased risk of NHL in con-nective tissue and autoimmune is well described [48,49], suggest-ing a potential role in lymphomagenesis for patients with PBL.
Pathology
The commonest histologies are DLBCL (56–84% of PBL)[4,5,8,9,28,50], MZL (9–28%) [2,5,25,28,51], follicular (10–19%)[2,9,51], and Burkitt lymphoma (<6%) [50,52,53]. Rarer histologiesinclude anaplastic large cell lymphoma [54], peripheral T-cell lym-phoma [55,56], small lymphocytic lymphoma [2,25], lymphoplas-macytic lymphoma [2], mantle cell lymphoma [57–59] andHodgkin lymphoma (each < 1%) [5].
Here we present an overview of the more important rare sub-types, followed by more detailed evaluation of the pathology andclinical aspects of PB-DLBCL.
Marginal zone lymphoma (MZL)
Primary breast MZL (PB-MZL) affects slightly older women, withmedian age at diagnosis 68 years [51]. No pathophysiologic role forchronic infection has been identified, in contrast to other extranod-al sites (e.g. Helicobacter pylori in stomach or Chlamydophila psittaciin ocular adnexal tissue). PB-MZL appears indolent – in the largestretrospective study (from the IELSG, n = 24) the 5-year progression-free survival (PFS) and overall survival (OS) were 56% and 92%,respectively [51]. The excellent OS suggests that although relapsesfrequently occur, second responses and subsequent disease controlare possible. In the companion IELSG paper on PB-DLBCL, 5% ofpatients had concomitant histologic evidence of MZL, though thisappeared not to have prognostic impact [4,51]. To our knowledgeno prospective studies have been conducted; thus no standardtreatment has been defined. Surgery, radiotherapy and chemother-apy have all been used, however surgical resection results in infe-rior local and distant control to radiotherapy, with no patientsrelapsing within the irradiated field [51]. The IELSG series did notinclude rituximab treated patients; also, due to the low numberof patients treated with chemotherapy, no conclusion could bereached regarding its impact. Given these findings, extensive sur-gery should be avoided. Patients with limited-stage disease shouldreceive radiotherapy, with chemo-immunotherapy reserved for
ancer Treat Rev (2014), http://dx.doi.org/10.1016/j.ctrv.2014.05.010
C.Y. Cheah et al. / Cancer Treatment Reviews xxx (2014) xxx–xxx 3
patients experiencing symptomatic distant relapse. In this scenarioprotocols for systemic MZL such as rituximab in combination witheither bendamustine (BR) [60], cyclophosphamide, vincristine andprednisolone (R-CVP) [61] or chlorambucil [62] are all reasonablechoices, although no prospective studies specifically in patientswith PB-MZL exist.
Follicular lymphoma (FL)
Similar to PB-MZL, primary breast follicular lymphoma (PB-FL)represents a rare entity described in small case series[2,9,25,31,51,63]. The IELSG study of indolent PBL is the largest,including 36 patients with PB-FL in whom median age was 62 years[51]. Treatment included surgery, radiotherapy and chemotherapyeither alone or in combination, which in aggregate yielded a 5-yearPFS and OS of 49% and 64% respectively – less favorable than PB-MZL[51]. As in PB-MZL, mastectomy was inferior to radiotherapy. Nopatients receiving breast irradiation relapsed within field – mostoccurred at distant sites. Eastern Cooperative Oncology Group(ECOG) Performance Status >1 predicted inferior OS but this analy-sis was limited by sample size. Therefore, we consider that in PB-FL(as in limited stage nodal FL) [64] local radiotherapy should beincorporated into first-line therapy, with no role for extensive sur-gery. The addition of chemotherapy appeared to reduce relapse risk,though not in a statistically significant manner, possibly due to lownumbers [51]. It is tempting given the more aggressive course toincorporate chemo-immunotherapy upfront, although the benefitremains unproven. Patient who experience multifocal distantrelapse may be offered a choice of regimens appropriate for nodalFL such as BR, R-CVP or rituximab, cyclophosphamide, doxorubicin,vincristine and prednisolone (R-CHOP). Re-treatment with radio-therapy could be considered if the site(s) of relapse can be safelyencompassed within a radiotherapy field without undue risks oftoxicity.
Mantle cell lymphoma (MCL)
Although MCL frequently involves extranodal sites, involve-ment of the breast is uncommon. Rare cases have been reported,however evidence of extramammary disease was typically present[57–59,65,66]. This is unsurprising given the majority of patientshave gut and marrow involvement at baseline if sensitive tech-niques are used [67–69]. Furthermore, the limited data regardingoutcome in patients with limited stage MCL suggest that their out-comes are similar to patients with advanced stage, with the caveatthat radiotherapy may improve PFS [70,71]. Thus patients withapparent primary breast MCL should undergo careful staging eval-uation if the planned treatment of advanced stage disease differsfrom limited stage disease. We treat patients with apparent pri-mary breast MCL identically to systemic MCL using chemo-immu-notherapy protocols, with consideration for the addition ofradiotherapy to the breast (after autologous stem cell transplantif included), if that is a predominant site of disease.
Burkitt lymphoma
Primary Burkitt lymphoma of the breasts is a rare but highlyaggressive entity of younger women with poor prognosis oftenassociated with lactation or pregnancy (in which it represents47% of cases of NHL) [72]. This suggests a possible role for sex hor-mones in pathogenesis. A recent review examined 28 cases; themedian age was 30 years, most were bilateral, occurred duringpregnancy or lactation and outcomes were particularly poor withcrude survival rates of 14.3% and 30.8% in lactating and pregnantpatients respectively [52]. Although no prospective studies exist,we recommend management as systemic Burkitt lymphoma with
Please cite this article in press as: Cheah CY et al. Primary breast lymphoma. C
chemotherapy protocols containing central nervous system (CNS)prophylaxis such as cyclophosphamide, vincristine, doxorubicin,methotrexate, ifosfamide, etoposide and cytarabine (CODOXM-IVAC) [73]. The role of radiotherapy is uncertain given that relapsestend to be systemic and involve distant nodal and extranodal sitessuch as the CNS.
Breast implant associated anaplastic large cell lymphoma (BIA-ALCL)
Whilst >90% of PBL in the absence of breast implants are of B-cellorigin [2,5,8,9,28], in the women with implants T-cell phenotypepredominates, due to BIA-ALCL [74]. For an excellent recent reviewof this topic, see Thompson and Prince [75]. This rare but likelyunder-reported entity can occur following implants for both recon-structive and cosmetic purposes, with many cases arising aroundtextured implants, a recent modification in design that results ingreater silicone shedding and possibly increased chronic antigenicstimulation. Cell lines established from primary tumors showeddependence on IL-2 for survival and proliferation, supportingchronic inflammation as a potential pathophysiologic mechanism[76]. By immunohistochemistry, CD30 is strongly positive; ALK1negative and T-cell lineage and cytotoxic markers are variably pres-ent [74]. There are two distinct clinical presentations with disparateclinical behavior: (1) the more common and indolent seroma-typein which fluid containing malignant lymphocytes accumulatesbetween the implant and the surrounding fibrous capsule, (2) theless frequent but more aggressive mass lesion which is usuallyaccompanied by seroma [77]. Miranda et al. recently reported thelargest experience of BIA-ALCL, comprising 60 women (42 ser-oma-type, 18 mass-type), with median age 52 years [54]. The med-ian time from implant insertion to diagnosis of BIA-ALCL was 9(range 1–32) years and 93% had localized disease (83% stage I, 10%stage II). Capsulectomy was performed in 93% of cases; chemother-apy (mostly CHOP) and radiotherapy were given to 71% and 55% ofpatients, respectively. Outcomes were favorable, with actuarial 3-year OS 100% and 82% in seroma and mass types, respectively(P = 0.03). No other prognostic factors were identified. Importantly,16 patients who did not receive chemotherapy (14 seroma-type and2 mass-type; R. Miranda, personal communication) were alive in CRat last follow up, with one developing local relapse successfullytreated with radiotherapy. From the limited available evidence,patients with seroma-type BIA-ALCL may be managed with localtreatment, including capsulectomy ± radiotherapy. In contrast,those with a mass lesion, likely benefit from the addition of chemo-therapy ± radiotherapy. In the absence of prospective data, we rec-ommend 4–6 cycles of CHOP and radiotherapy to the breast.
Diffuse large B-cell lymphoma (DLBCL)
Activated B-cell (ABC) type comprises 62–77% of PB-DLBCL instudies reporting cell of origin [5,13,78–80]. Immunohistochemis-try findings are consistent with this: one study reported germinalcenter B-cell marker CD10 positive in 30% whilst ABC-markersBCL6 and MUM1 were positive in 92% and 84% of cases respectively[22]. Cytogenetic data in PB-DLBCL are limited. Kupper-Hommelet al. performed both conventional cytogenetic analysis and fluo-rescence in situ hybridisation (FISH) in 15 patients with PBL (a mix-ture of MALT, de novo PB-DLBCL and composite MALT/DLBCL) [81].Interestingly, they found cases with numeric gains of chromosomes3 and 18 common to all three histologic presentations. Molecularcytogenetic evidence of t(14;18)(q32q21) involving IGH/MALT1was present in both DLBCL/MALT and de novo DLBCL. Niitsu et al.using found an abnormal karyotype in 13/18 cases of PB-DLBCLby conventional cytogenetic analysis: three had 18q21/BCL2 trans-locations with t(14;18)(q32q21) in two and t(12;18)(p13q21) inone patient. Of eight patients with 3q27/BCL6 translocation,
ancer Treat Rev (2014), http://dx.doi.org/10.1016/j.ctrv.2014.05.010
4 C.Y. Cheah et al. / Cancer Treatment Reviews xxx (2014) xxx–xxx
t(3;4)(q27q32) was present in three patients and der(3)(q27) infive. Two patients had evidence of 17p deletions [32]. No attemptwas made to correlate cytogenetic lesions with outcome in eitherstudy, presumably due to small numbers. Recently, of relevancein nodal ABC-type DLBCL, significant advances in understandingof events upstream of the NF-jB pathway have been made. Ofpotential relevance to PB-DLBCL (which is more commonly ABC-type) the presence of chronic B-cell receptor signaling (throughactivating mutations in CD79A/B or CARD11) or through constitutiveactivating mutations in MYD88 might be expected, however in PB-DLBCL no such data have been reported to our knowledge.
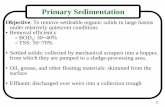
Fig. 1. Stage-modified International Prognostic Index predicts overall survival inpatients with primary breast DLBCL treated largely with R-CHOP. Reproduced withpermission from Hosein et al. [22].
Prognostic factors
DLBCL
Identification of robust prognostic factors in rare diseases such asPBL is problematic, as those reported are generally derived fromsmall retrospective series of heterogeneous composition and treat-ment, subject to bias and inconsistency. In spite of these limitations,some insights can be gleaned (Table 1). The IPI in several studiesremains predictive of outcome in PB-DLBCL [4,5,32]. Hosein et al.found stage-modified IPI to predict OS in a patients treated primarilywith R-CHOP (Fig. 1). Other investigators have found stage IIE diseaseto be independently associated with inferior outcome [3,19,23,82].Other adverse prognostic markers identified include poor perfor-mance status [9,25], erythrocyte sedimentation rate > 30 mm/hr[9], tumor size > 4–5 cm [3,27,32], soluble serum IL2 > 1000U/ml[32] and high tumor microvascular density [82]. Some series havesuggested bilateral involvement with DLBCL to be a particularlyaggressive entity. The 3-yr PFS and OS of 11 such cases in theIELSG-15 series were 36% and 46% respectively – although numeri-cally inferior, the hazard ratios for progression or death comparedwith unilateral involvement were 1.6 (P = 0.22) and 1.9 (P = 0.15),respectively [4]. Guo et al. reported bilateral involvement in 3/42(7%) patients and found it to be a significant adverse predictor of bothPFS and OS, largely because all three patients developed CNS relapse[28].
Patterns of relapse
PB-DLBCL, like primary testicular lymphoma, displays extran-odal tropism at relapse [83]. In particular, relapse involved the ipsi-lateral or contralateral breast in 12–44% of cases [3,4,9,10]. In theIELSG-15 series, ipsilateral breast relapse occurred in within3 years of treatment, whilst contralateral relapse occurred up to
Table 1Adverse prognostic factors identified in retrospective series of patients with primarybreast lymphoma. Abbreviations: IPI – International Prognostic Index; ECOG – EasternCooperative Oncology Group; ESR – erythrocyte sedimentation rate.
Progression free survival Overall survival
IPI (per unit increase [4] or >2[10,28])
IPI (per unit increase [4] or >2 [5,28])
Omission of anthracycline [4] orchemoradiation [2,5]
Omission of anthracycline, [4] radiation[4] or chemoradiation [2,4]
Stage IIE (vs. stage IE) [2,3] Stage IIE (vs. stage IE) [3,19]<4 Cycles of chemotherapy [10] Received mastectomy [3]Bilateral involvement of the
breasts [28]Tumor size > 4–5 cm [3,27]
Tumor size > 5 cm [27] <4 Cycles of chemotherapy [10]ESR > 30 mm/hr [9]ECOG performance status [9,25]Bilateral involvement of the breasts [28]High microvascular density [81]Soluble serum IL-2 > 1000 IU/ml [32]
Please cite this article in press as: Cheah CY et al. Primary breast lymphoma. C
13.3 years later [4]. The pathophysiologic mechanism for this tro-pism is unclear but could include chemokine-mediated migrationof lymphoma cells to breast tissue [84]. Other extranodal sitesincluding the bone marrow, lung or pleura, skin, gastrointestinaltract and CNS have all been reported with greater frequency thanone would expect for nodal DLBCL [3,9,10,15,19].
CNS relapse
The frequency of CNS involvement in PB-DLBCL is difficult toestimate due to the limited size, retrospective nature and hetero-geneous treatment of patients in most series. However, in largerseries with data, CNS relapse occurred in 5–16% of patients(Table 2). Yhim et al. found higher rates of CNS relapse (3-yearcumulative incidence 23.6% vs. 1.4%, P < 0.001) in a matched-pairanalysis of PB-DLBCL (n = 25) with limited stage nodal DLBCL uni-formly treated with R-CHOP [79]. Similar to CNS relapse in nodalDLBCL, most CNS relapses occurred <2 years following completionof therapy [22]. We conclude CNS relapse risk is increased, butwhether this justifies CNS-directed prophylaxis is controversial.
Risk factors for CNS relapse
Given wide confidence intervals of published estimates, theidentification of predictive factors to refine risk and target prophy-laxis would be useful. Unfortunately rarity makes this difficult.Potential risk factors suggested by smaller series include bilateralbreast involvement [28] and tumor size >5 cm [27]. However, inthese studies no formal statistical analysis to show associationwas performed, and others have failed to replicate these findings.Hosein et al. reported 6/27 (22%) stage IIE patients developedCNS relapse, in comparison with 6/49 (12%) with stage IE; 5/22(22%) patients with stage-modified IPI 2–4 experience CNS relapsecompared with 7/54 (13%) with stage-modified IPI 0–1. These dif-ferences were reported not to be significant, but even a CNS relapserisk of 12% warrants consideration of CNS prophylaxis given thedismal outcome. Because of the relatively high event rate even inpatients with stage IE or low stage-modified IPI, we recommendin all patients with PB-DLBCL, consideration be given to CNS-direc-ted prophylaxis. This recommendation is stronger if potentialhigh-risk features for CNS involvement are present (stage IIE,
ancer Treat Rev (2014), http://dx.doi.org/10.1016/j.ctrv.2014.05.010
Table 2CNS relapse in primary breast DLBCL, summarising larger retrospective reporting on CNS relapse.
Study n(DLBCL)
Chemotherapy Rituximab(%)
Use of CNSprophylaxis
Effect of CNSprophylaxis
Localization of CNSrelapse
Rate of CNS relapse (%)
Ryan [4] 204 70% Anthracycline 0 None NA Not reported 5-Year cumulative 5Hosein [22] 76 72% CHOP 69 12%; mostly IT MTX No impact Leptomeningeal 4/12
(33%)Crude incidence 16
Parenchymal 6/12 (50%)Both 2/12 (16%)
Jeanerette-Sozzi[3]
57* Any 70%; mostly CHOP-like
0 Not reported NA Not reported Crude incidence 12
Yhim [10] 49 97% Anthracycline based 62 5/49 (10%) IT chemo No relapses in IT group Not reported 5-Year cumulative 12.3Aviles [87] 96 CHOP-21 0 None NA Not reported Crude incidence 11.4
* Only histologic grade reported, this figure includes high and intermediate grade lymphoma. Abbreviations: DLBCL – diffuse large B-cell lymphoma; CNS – central nervoussystem; NA – not applicable; CHOP – cyclophosphamide, doxorubicin, vincristine, prednisolone.
C.Y. Cheah et al. / Cancer Treatment Reviews xxx (2014) xxx–xxx 5
stage-modified IPI score > 2, bilateral breast involvement orbulk > 5 cm).
Efficacy of CNS prophylaxis
In most series IT chemotherapy was minimally used, making itdifficult to assess impact on CNS relapse. In three series, the hand-ful (<10%) of patients receiving IT chemotherapy did not experi-ence CNS relapse [4,10,27] whilst other studies did not find ITprophylaxis to impact CNS relapse rate [9,22]. However, thesestudies were neither designed nor adequately powered to answerthe question. Where localization of CNS relapse has been reported,most involve brain parenchyma [22,27], suggesting that that as innodal DLBCL, the addition of high-dose intravenous (IV) metho-trexate or cytarabine may be a more effective prophylactic strategy[85]. We administer IT methotrexate with each cycle of R-CHOPand incorporate two cycles of IV methotrexate (3 g/m [2] adjustedfor renal function and age), two weeks apart after the completionof chemo-immunotherapy as this reduces CNS relapse in high-riskpatients with nodal DLBCL [86].
Fig. 2. Combined modality therapy with anthracycline containing chemotherapyand radiotherapy was associated with superior overall survival in the IELSG-15retrospective series of 204 patients with primary breast DLBCL. Abbreviations: RT –radiotherapy; SC – systemic chemotherapy; S – surgery. Reproduced with permis-sion from Ryan et al. [4].
Treatment
The role of surgery
There are robust data that surgical resection results in inferiorlocal control [18], with multiple series demonstrating treatmentincluding mastectomy associated with higher all-cause and dis-ease-specific mortality [3,4,50]. In a large series managed with sur-gery alone, the 5-year OS for stage IE and IIE were 40.5% and 20.5%respectively [8]. Therefore, surgical intervention beyond excisionalbiopsy should be avoided. Patients who undergo surgical excisionbecause of an initial misdiagnosis of PB-DLBCL as breast carcinomashould undergo chemo-immunotherapy followed by radiotherapyas soon as practical after wound healing.
Chemotherapy
Chemotherapy is a key component of therapy, with early seriesshowing improvements in local and distant control for patients inwhom chemotherapy was included [2,8]. Published experiencewith chemotherapy focusing on PB-DLBCL is derived mostly fromretrospective series with two completed prospective studies[87,88]. An ongoing Korean multicenter study is attempting toevaluate R-CHOP Q21 plus IT methotrexate as reference therapyfor PB-DLBCL (ClinicalTrials.gov identifier: NCT01448096). In nodalDLBCL, R-CHOP is widely accepted standard of care [89], and hasbecome routine for PB-DLBCL also. The IELSG-15 study highlightedthe importance of including an anthracycline with hazard ratios for
Please cite this article in press as: Cheah CY et al. Primary breast lymphoma. C
PFS 0.4 (95%CI 0.3–0.7) and OS 0.5 (0.3–0.9) (Fig. 2). A summary ofthe larger series is presented in Table 3. Series using predomi-nantly CHOP ± R and radiotherapy have reported 5-year PFS andOS ranging from 50% to 70% [2,4,22,87]. There are data suggestingreducing the number of cycles of chemotherapy compromises out-come. In the pre-rituximab era IELSG-15 study patients receiving>3 cycles (compared with 63) of chemotherapy had improvedcause-specific survival (hazard ratio 0.5 (95%CI 0.2–0.9)) [4]. In amore recent study in which 62% of patients received rituximab,Yhim et al. found patients treated with >4 cycles to have superior5-year PFS (58 v 28%, P < 0.0001) and OS (66 v 19%, P < 0.001) [10].
Aviles et al. attempted to improve on CHOP by increasing alky-lator dose and adding rituximab in a phase-II study of R-CEOPQ14 (cyclophosphamide 1500 mg/m [2], epirubicin 100 mg/m2,vincristine 1.2 mg/m2, rituximab 375 mg/m2 D1 prednisolone100 mg/m2 PO D1-5) with all patients receiving radiation [87].The patient cohort was young (median age 45 years) but otherwisetypical of PB-DLBCL, being mostly stage IE and favorable perfor-mance status. The treatment was tolerable but did not improve out-come in a historic comparison with CHOP for 5-year DFS 64% v 60%,P = 0.66) or OS (53% v 52% P = 0.50) [80,88] Other studies examiningthe impact of rituximab are mixed, with several studies showing anon-significant trend toward improvement in PFS and OS [2,10] andothers no benefit [22,32]. Only the study by Zhao et al. showed mar-ginal improvement in 5-year PFS for patients treated with R-CHOP vCHOP (82 v 67%, P = 0.038) [82]. It should be noted that these stud-ies were neither designed nor powered to measure the impact of
ancer Treat Rev (2014), http://dx.doi.org/10.1016/j.ctrv.2014.05.010
Table 3Treatment and outcome summary of larger recent series of primary breast DLBCL.
Study Year Type n DLBCL (% of series) Chemotherapy Rituximab(%)
RT (%) PFS (%) OS (%)
Ryan [4] 2008 Retrospective 204 (100) 70% Anthracycline based 0% 64 5-Year PFS 54 5-Year OS 63Hosein
[22]2014 Retrospective 76 (100) CHOP 72% 62% 63 5-Year PFS 66 5-Year OS 75
Yhim [10] 2010 Retrospective 49 (100) 97% Anthracycline based 62% 31 5-Year PFS 54 5-Year OS 60Caon [2] 2012 Retrospective 28 (87*) CHOP 73%* 43%* 50* 5-Year ‘distant control’
70*
5-Year OS 54*
Validire [9] 2008 Retrospective 38 (84) 80% ‘‘anthracyclinebased’’
10% 71 5-Year PFS 54** 5-Year OS 61**
Zhao [81] 2011 Retrospective 28 (90) CHOP 74% % not stated 65 5-Year PFS 57** 5-Year OS 71**
Guo [28] 2008 Retrospective 37 (82) CHOP-like 79% 14% 49 5-Year PFS 35** 5-Year OS 50**
Aviles [87] 2005 Prospective 96 RT v CHOP v combined 10-Year PFS 50, 56, 83 10-Year OS 50, 50, 76Aviles [86] 2007 Prospective 32 R-CEOP Q14 100% 100 3-Year PFS 75 3-Year OS 63
Abbreviations: DLBCL – diffuse large B-cell lymphoma; PFS – progression free survival; OS – overall survival; DFS – disease-free survival; CHOP – cyclophosphamide,doxorubicin, vincristine, prednisolone; CEOP – cyclophosphamide, epirubicin, doxorubicin, vincristine, prednisolone; RT – radiotherapy.* Data includes all aggressive histologies.** Data includes non-DLBCL histologies.
6 C.Y. Cheah et al. / Cancer Treatment Reviews xxx (2014) xxx–xxx
rituximab. However, a randomized study in PB-DLBCL is unlikely;given R-CHOP is standard of care in nodal DLBCL there is little con-troversy recommending its use in PB-DLBCL.
Radiotherapy
The primary role of radiotherapy is to consolidate the responsesachieved by systemic therapy. In particular, irradiation of the ipsilat-eral breast (the most common site of first relapse) appears to reducethis risk [4]. The published literature is limited to a small number ofretrospective analyses that suggest that improved disease control inthe breast translates into an improvement in survival [4,88]. Thelargest retrospective series supporting consolidation radiotherapywas the IELSG-15 study, in which the combination of anthracy-cline-containing chemotherapy and radiotherapy was associatedwith improved OS compared to chemotherapy or radiotherapy alone(P = 0.001) [4]. Aviles et al. reported the combination of six cycles ofCHOP chemotherapy plus radiotherapy to the ipsilateral breast andregional nodes was also associated with significantly improved out-comes compared to chemotherapy or radiotherapy alone: 10-yearevent-free survival rates were 83%, 56% and 50%, (P < 0.01); 10-yearOS rates were 76%, 50% and 50%, (P < 0.01) [88]. Thus chemo-immu-notherapy and consolidation radiotherapy is standard of care for PB-DLBCL.
The optimal volume for consolidation radiotherapy in PB-DLBCLis controversial. Earlier published series of PB-DLBCL described theuse of radiotherapy techniques that encompassed the ipsilateralbreast at a minimum, and have acknowledged the uncertain bene-fits of additional irradiation of regional nodes +/� contralateralbreast [4,18,90]. This uncertainty is heightened by the evolutionof modern functional imaging, improved radiotherapy planningtechniques and the addition of molecular-based therapies to thetreatment. Extrapolating from nodal DLBCL [91,92], the currentapproach for consolidation radiotherapy is involved site radiother-apy (ISRT) [91–93]. This concept was first developed for Hodgkinlymphoma, and has now been applied to DLBCL [94]. The primarydifference between ISRT and involved field radiotherapy (IFRT) vol-umes is that the latter also includes prophylactic radiotherapy toadjacent uninvolved nodes. The principle of ISRT is to restrict theradiotherapy volume to encompass the pre-chemotherapy site(s)of disease, with adequate margins to allow for subclinical disease,physiological movement and set-up variation, whilst also consider-ing post-chemotherapy anatomical changes [94]. Therefore, ISRTrelies on the sensitivity of the pre-chemotherapy imaging studies.In PB-DLBCL, we hypothesize the entire ipsilateral breast maypotentially harbor subclinical disease, thus we propose that theISRT volume should include the whole ipsilateral breast plus any
Please cite this article in press as: Cheah CY et al. Primary breast lymphoma. C
additional sites of known pre-chemotherapy disease in the regio-nal nodes or contralateral breast. Elective nodal irradiation of thecontralateral breast, axillae or supraclavicular fossae is not rou-tinely included within the ISRT field. However, in the unusual sit-uation that the patient has not been adequately staged withfunctional and structural imaging prior to the initiation of systemictherapy, then the traditional IFRT is a safer treatment choice forconsolidation radiotherapy.
Technically, ISRT volumes tend to be smaller than the tradi-tional IFRT. It is hypothesized that with effective systemic therapyfor DLBCL, these smaller radiotherapy volumes will translate intolower risks of radiation-induced side effects, without compromis-ing disease control. A population-based cohort study from BritishColumbia of 288 patients with limited-stage DLBCL (includingPB-DLBCL, but excluding primary DLBCL of the testis or central ner-vous system) demonstrated the safety of reducing the radiotherapyfield size from IFRT, noting a reassuringly low rate of marginalrelapse and no detrimental impact on survival [91]. Reducing theradiotherapy field size spares adjacent uninvolved tissues, andextrapolating from radiotherapy planning studies performed inHodgkin lymphoma, will likely be associated with lower risks ofsecond malignancy and other late effects [95,96]. With respect toPB-DLBCL in the era of ISRT, the radiotherapy volume includesthe ipsilateral breast [93], and only includes regional nodal irradi-ation or contralateral breast irradiation if these sites were knownto be previously involved with DLBCL. In this setting, the smallerfield size with ISRT (vs. IFRT) reduces the radiation exposure tothe contralateral breast, lung, and thyroid gland, and thus the risksof late radiation-induced toxicities and second malignancies inthese organs. Modern technological advances in radiotherapydelivery may further reduce the risk of late toxicities; for example,inverse-planning techniques to reduce higher-dose radiation expo-sure to organs at risk, and breath-holding techniques or respira-tory-gating to reduce the cardiac exposure in patients receivingradiotherapy to the left breast.
Treatment recommendation
A suggested approach to treatment for PB-DLBCL is displayed inFig. 3. Patients with stage-modified IPI 0–1 and no risk factorsshould receive 4–6 cycles of anthracycline containing chemother-apy with rituximab. Patients with high-risk disease (defined bystage-modified IPI 2–4, bilateral disease or bulk > 5 cm) shouldhave 6 cycles of anthracycline containing chemotherapy with rit-uximab. All patients should be considered for CNS-directed pro-phylaxis; all should receive consolidative ISRT to the ipsilateralbreast. Patients with bilateral breast involvement may represent
ancer Treat Rev (2014), http://dx.doi.org/10.1016/j.ctrv.2014.05.010
Fig. 3. Proposed treatment algorithm for patients with primary breast DLBCL. Abbreviations: DLBCL –diffuse large B-cell lymphoma; IPI – International Prognostic Index; R-CHOP Q21 – rituximab, cyclophosphamide, doxorubicin, vincristine, prednisolone every 21 days; IT – intrathecal; HD IV MTX – high dose intravenous methotrexate; ISRT –involved site radiotherapy.
C.Y. Cheah et al. / Cancer Treatment Reviews xxx (2014) xxx–xxx 7
a particularly high risk group, and it would be useful to evaluatethe tolerability and efficacy of more intensive chemotherapy regi-mens such as R-Hyper CVAD (rituximab, hyper-fractionated cyclo-phosphamide, doxorubicin, vincristine and dexamethasone)/R-MA(rituximab, high dose IV methotrexate, cytarabine) in youngerpatients without significant comorbidities.
Relapsed disease
The scarce data available regarding outcomes of patients withPB-DLBCL after relapse suggests prognosis is poor. In the IELSG-15series the median survival after relapse was 1.0 (95%CI 0.7–2.1)years and 5-year OS 20% [4]. These data are supported by the sim-ilarity between PFS and OS curves in most series, implying limitedability to successfully salvage patients. As in other forms of aggres-sive lymphoma, CNS relapse carries a particularly poor prognosis.The median OS of patients with CNS relapse was 5.0 months inthe series from British Columbia [2]. Despite a 54% response rateusing high dose IV methotrexate as salvage for CNS relapse, Avileset al. found all patients subsequently died of progressive lymphoma[88].
Future directions
The decreasing cost and increasing availability of high through-put technologies such as ‘‘next generation’’ sequencing has resultedin exponential growth in the understanding of genetic alterations innodal DLBCL. Of particular relevance to PB-DLBCL (which is mostlyof ABC-subtype), the recent discovery of oncogenic mutations ingenes such as CARD11, CD79B and MYD88 driving constitutive NF-jB activity [97] will likely translate into clinical development ofnew small molecule inhibitors of pathways such as STAT3 [98].Inhibition of NF-jB using bortezomib may sensitize ABC-typeDLBCL cells to chemotherapy, as R-CHOP with bortezomib hadmarkedly superior ORR and OS in recurrent ABC (compared withGCB) -subtype DLBCL [99]. A prospective study of this combinationin PB-DLBCL has appeal. Other potential chemotherapy partnerstargeting the NF-jB pathway include lenalidomide [100], ibrutinib[101], enzastaurin [102] (an inhibitor of PKCb) and fostamatinib[103] (a SYK inhibitor) which all display promising activity inABC-type nodal DLBCL. Some of these are being investigated inphase II/III studies in combination with R-CHOP, which will likelyhave applicability to PB-DLBCL (ClinicalTrials.gov identifiers:RCHOP ± ibrutinib, NCT01855750; R-CHOP + lenalidomide mainte-nance NCT01122472, R-CHOP ± enzastaurin NCT00451178). Giventhe preclinical promise, exploration of ERb agonists in PB-DLBCLappears warranted.
Please cite this article in press as: Cheah CY et al. Primary breast lymphoma. C
Conclusion
The breast is a rare extranodal site of involvement for lym-phoma with particular biological and clinical characteristics. Ingeneral, surgery has no role beyond obtaining a histologic diagno-sis to guide definitive therapy. For PB-DLBCL, the commonest sub-type, anthracycline-containing chemotherapy followed byconsolidative ipsilateral breast irradiation is standard of care. Fur-ther studies into oncogenic mutations will hopefully assist in thedevelopment of more effective agents for the significant minorityof patients failing existing treatments.
Conflicts of interest
We declare no conflicts of interest in relation to this article.
References
[1] Aviv A, Tadmor T, Polliack A. Primary diffuse large B-cell lymphoma of thebreast: looking at pathogenesis, clinical issues and therapeutic options. AnnOncol 2013;24:2236–44.
[2] Caon J, Wai ES, Hart J, Alexander C, Truong PT, Sehn LH, et al. Treatment andoutcomes of primary breast lymphoma. Clin Breast Cancer 2012;12:412–9.
[3] Jeanneret-Sozzi W, Taghian A, Epelbaum R, Poortmans P, Zwahlen D, AmslerB, et al. Primary breast lymphoma: patient profile, outcome and prognosticfactors. A multicentre Rare Cancer Network study. BMC Cancer2008;8:1471–2407.
[4] Ryan G, Martinelli G, Kuper-Hommel M, Tsang R, Pruneri G, Yuen K, et al.Primary diffuse large B-cell lymphoma of the breast: prognostic factors andoutcomes of a study by the International Extranodal Lymphoma Study Group.Ann Oncol 2008;19:233–41.
[5] Talwalkar SS, Miranda RN, Valbuena JR, Routbort MJ, Martin AW, Medeiros LJ.Lymphomas involving the breast: a study of 106 cases comparing localizedand disseminated neoplasms. Am J Surg Pathol 2008;32:1299–309.
[6] Surov A, Holzhausen HJ, Wienke A, Schmidt J, Thomssen C, Arnold D, et al.Primary and secondary breast lymphoma: prevalence, clinical signs andradiological features. Br J Radiol 2012;85:e195–205.
[7] Arber DA, Simpson JF, Weiss LM, Rappaport H. Non-Hodgkin’s lymphomainvolving the breast. Am J Surg Pathol 1994;18:288–95.
[8] Uesato M, Miyazawa Y, Gunji Y, Ochiai T. Primary non-Hodgkin’s lymphomaof the breast: report of a case with special reference to 380 cases in theJapanese literature. Breast Cancer 2005;12:154–8.
[9] Validire P, Capovilla M, Asselain B, Kirova Y, Goudefroye R, Plancher C, et al.Primary breast non-Hodgkin’s lymphoma: a large single center study of initialcharacteristics, natural history, and prognostic factors. Am J Hematol2009;84:133–9.
[10] Yhim HY, Kang HJ, Choi YH, Kim SJ, Kim WS, Chae YS, et al. Clinical outcomesand prognostic factors in patients with breast diffuse large B cell lymphoma;Consortium for Improving Survival of Lymphoma (CISL) study. BMC Cancer2010;10:321.
[11] Wiseman C, Liao KT. Primary lymphoma of the breast. Cancer1972;29:1705–12.
[12] Hugh JC, Jackson FI, Hanson J, Poppema S. Primary breast lymphoma. Animmunohistologic study of 20 new cases. Cancer 1990;66:2602–11.
ancer Treat Rev (2014), http://dx.doi.org/10.1016/j.ctrv.2014.05.010
8 C.Y. Cheah et al. / Cancer Treatment Reviews xxx (2014) xxx–xxx
[13] Li D, Deng J, He H, Bu Y, Peng F, Tang X, et al. Primary breast diffuse large B-cell lymphoma shows an activated B-cell-like phenotype. Ann Diagn Pathol2012;16:335–43.
[14] Jung SP, Kim M, Han KM, Kim JH, Kim JS, Nam SJ, et al. Primary breastlymphoma: a single institution’s experience. J Korean Surg Soc2013;84:267–72.
[15] Au WY, Chan AC, Chow LW, Liang R. Lymphoma of the breast in Hong KongChinese. Hematol Oncol 1997;15:33–8.
[16] Desantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer JClin 2013.
[17] Rathod J, Taori K, Disawal A, Gour P, Dhakate S, Mone R, et al. A rare case ofmale primary breast lymphoma. J Breast Cancer 2011;14:333–6.
[18] Radkani P, Joshi D, Paramo JC, Mesko TW. Primary breast lymphoma: 30 yearsof experience with diagnosis and treatment at a single medical center. JAMASurg 2013.
[19] Wong WW, Schild SE, Halyard MY, Schomberg PJ. Primary non-Hodgkinlymphoma of the breast: the Mayo Clinic experience. J Surg Oncol2002;80:19–25 [discussion 6].
[20] Mpallas G, Simatos G, Tasidou A, Patra E, Galateros G, Lakiotis G, et al. Primarybreast lymphoma in a male patient. The Breast 2004;13:436–8.
[21] Murata T, Kuroda H, Nakahama T, Goshima H, Shiraishi T, Yatani R. Primarynon-Hodgkin malignant lymphoma of the male breast. Jpn J Clin Oncol1996;26:243–7.
[22] Hosein PJ, Maragulia JC, Salzberg MP, Press OW, Habermann TM, Vose JM,et al. A multicentre study of primary breast diffuse large B-cell lymphoma inthe rituximab era. Br J Haematol 2014;165:358–63.
[23] Brustein S, Filippa DA, Kimmel M, Lieberman PH, Rosen PP. Malignantlymphoma of the breast. A study of 53 patients. Ann Surg 1987;205:144–50.
[24] Sabaté JM, Gómez A, Torrubia S, Camins A, Roson N, De Las Heras P, et al.Lymphoma of the breast: clinical and radiologic features with pathologiccorrelation in 28 patients. Breast J 2002;8:294–304.
[25] Ganjoo K, Advani R, Mariappan MR, McMillan A, Horning S. Non-Hodgkinlymphoma of the breast. Cancer 2007;110:25–30.
[26] Benevolo G, Stacchini A, Spina M, Ferreri AJ, Arras M, Bellio L, et al. Finalresults of a multicenter trial addressing role of CSF flow cytometric analysis inNHL patients at high risk for CNS dissemination. Blood 2012;120:3222–8.
[27] Fukuhara S, Watanabe T, Munakata W, Mori M, Maruyama D, Kim SW, et al.Bulky disease has an impact on outcomes in primary diffuse large B-celllymphoma of the breast: a retrospective analysis at a single institution. Eur JHaematol 2011;87:434–40.
[28] Guo H-Y, Zhao X-M, Li J, Hu X-C. Primary non-Hodgkin’s lymphoma of thebreast: eight-year follow-up experience. Int J Hematol 2008;87:491–7.
[29] Go RS, Gundrum JD. Uncertainty and discordance in the staging and prognosisof diffuse large B-cell lymphoma with isolated bilateral testicularinvolvement. Am J Hematol 2009;84:762–3.
[30] Miller TP, Dahlberg S, Cassady JR, Adelstein DJ, Spier CM, Grogan TM, et al.Chemotherapy alone compared with chemotherapy plus radiotherapy forlocalized intermediate- and high-grade non-Hodgkin’s lymphoma. N Engl JMed 1998;339:21–6.
[31] Fruchart C, Denoux Y, Chasle J, Peny AM, Boute V, Ollivier JM, et al. High gradeprimary breast lymphoma: is it a different clinical entity? Breast Cancer ResTreat 2005;93:191–8.
[32] Niitsu N, Okamoto M, Nakamine H, Hirano M. Clinicopathologic features andtreatment outcome of primary breast diffuse large B-cell lymphoma. Leuk Res2008;32:1837–41.
[33] Norgaard M, Poulsen AH, Pedersen L, Gregersen H, Friis S, Ewertz M, et al. Useof postmenopausal hormone replacement therapy and risk of non-Hodgkin’slymphoma: a Danish population-based cohort study. Br J Cancer2006;94:1339–41.
[34] Mildon KH, Ansell P, Roman E, Kane EV. Reproductive factors, menopausalhormone therapy, and risk of non-Hodgkin, diffuse large B-cell and follicularlymphomas: a UK case-control study. Cancer Causes Control2010;21:2079–83.
[35] Fernandez E, Gallus S, Bosetti C, Franceschi S, Negri E, La Vecchia C. Hormonereplacement therapy and cancer risk: a systematic analysis from a network ofcase-control studies. Int J Cancer 2003;105:408–12.
[36] Teras LR, Patel AV, Hildebrand JS, Gapstur SM. Postmenopausal unopposedestrogen and estrogen plus progestin use and risk of non-Hodgkin lymphomain the American Cancer Society Cancer Prevention Study-II Cohort. LeukLymphoma 2013;54:720–5.
[37] Heldring N, Pike A, Andersson S, Matthews J, Cheng G, Hartman J, et al.Estrogen receptors: how do they signal and what are their targets. PhysiolRev 2007;87:905–31.
[38] Kuiper GG, Carlsson B, Grandien K, Enmark E, Haggblad J, Nilsson S, et al.Comparison of the ligand binding specificity and transcript tissue distributionof estrogen receptors alpha and beta. Endocrinology 1997;138:863–70.
[39] Shim GJ, Gherman D, Kim HJ, Omoto Y, Iwase H, Bouton D, et al. Differentialexpression of oestrogen receptors in human secondary lymphoid tissues. JPathol 2006;208:408–14.
[40] Yakimchuk K, Jondal M, Okret S. Estrogen receptor a and b in the normalimmune system and in lymphoid malignancies. Mol Cell Endocrinol 2013.
[41] Yakimchuk K, Iravani M, Hasni M, Rhönnstad P, Nilsson S, Jondal M, et al.Effect of ligand-activated estrogen receptor b on lymphoma growth in vitroand in vivo. Leukemia 2011;25:1103–10.
Please cite this article in press as: Cheah CY et al. Primary breast lymphoma. C
[42] Yakimchuk K, Hasni MS, Guan J, Chao MP, Sander B, Okret S. Inhibition oflymphoma vascularization and dissemination by estrogen receptor betaagonists. Blood 2014;123:2054–61.
[43] Ariad S, Lewis D, Cohen R, Bezwoda WR. Breast lymphoma. A clinical andpathological review and 10-year treatment results. S Afr Med J 1995;85:85–9.
[44] Bobrow LG, Richards MA, Happerfield LC, Diss TC, Isaacson PG, Lammie GA,et al. Breast lymphomas: a clinicopathologic review. Hum Pathol1993;24:274–8.
[45] Millis RR, Bobrow LG, Rubens RD, Isaacson PG. Histiocytic lymphoma ofbreast responds to tamoxifen. Br J Cancer 1988;58:808–9.
[46] Avenia N, Sanguinetti A, Cirocchi R, Bistoni G, Trastulli S, D’Ajello F, et al.Primary breast lymphomas: a multicentric experience. World J Surg Oncol2010;8:53.
[47] Domchek SM, Hecht JL, Fleming MD, Pinkus GS, Canellos GP. Lymphomas ofthe breast: primary and secondary involvement. Cancer 2002;94:6–13.
[48] Bagg A, Dunphy CH. Immunosuppressive and immunomodulatory therapy-associated lymphoproliferative disorders. Semin Diagn Pathol2013;30:102–12.
[49] Jonsson MV, Theander E, Jonsson R. Predictors for the development of non-Hodgkin lymphoma in primary Sjogren’s syndrome. Presse Med2012;41:e511–6.
[50] Jennings WC, Baker RS, Murray SS, Howard CA, Parker DE, Peabody LF, et al.Primary breast lymphoma: the role of mastectomy and the importance oflymph node status. Ann Surg 2007;245:784–9.
[51] Martinelli G, Ryan G, Seymour JF, Nassi L, Steffanoni S, Alietti A, et al. Primaryfollicular and marginal-zone lymphoma of the breast: clinical features,prognostic factors and outcome: a study by the International ExtranodalLymphoma Study Group. Ann Oncol 2009;20:1993–9.
[52] Negahban S, Ahmadi N, Oryan A, Khojasteh HN, Aledavood A, SoleimanpourH, et al. Primary bilateral Burkitt lymphoma of the lactating breast: a casereport and review of the literature. Mol Diagn Ther 2010;14:243–50.
[53] Savvari P, Matsouka C, Barbaroussi D, Christoulas D, Nikitas N, DimopoulosMA, et al. Burkitt’s lymphoma in pregnancy with bilateral breastinvolvement: case report with review of the literature. Onkologie2010;33:461–4.
[54] Miranda RN, Aladily TN, Prince HM, Kanagal-Shamanna R, de Jong D, FayadLE, et al. Breast implant-associated anaplastic large-cell lymphoma: long-term follow-up of 60 patients. J Clin Oncol 2014;32:114–20.
[55] Gualco G, Chioato L, Harrington Jr WJ, Weiss LM, Bacchi CE. Primary andsecondary T-cell lymphomas of the breast: clinico-pathologic features of 11cases. Appl Immunohistochem Mol Morphol 2009;17:301.
[56] Ozkan K, Sehsuvar G, Erdem C, Mustafa C, Ibrahim S, Fatih O. A rareoccurrence of primary T-cell lymphoma of the breast in pregnancy. ActaOncol 2011;50:1262–3.
[57] Boullanger N, Renou P, Dugay J, Boyer J, de Yberlucea LR, Combe M. Et al.[Palpable mantel cell lymphoma in the breast]. Presse Med 2001;30:163–5.
[58] Hill P, Seale M. Mantle cell lymphoma with bilateral palpable breast masses.Breast J 2008;14:303–5.
[59] Windrum P, Morris TC, Catherwood MA, Alexander HD, McManus DT, MarkeyGM. Mantle cell lymphoma presenting as a breast mass. J Clin Pathol2001;54:883–6.
[60] Rummel MJ, Niederle N, Maschmeyer G, Banat GA, von Grünhagen U, LosemC, et al. Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: anopen-label, multicentre, randomised, phase 3 non-inferiority trial. The Lancet2013.
[61] Kang HJ, Kim WS, Kim SJ, Lee J-J, Yang D-H, Kim JS, et al. Phase II trial ofrituximab plus CVP combination chemotherapy for advanced stage marginalzone lymphoma as a first-line therapy: Consortium for Improving Survival ofLymphoma (CISL) study. Ann Hematol 2012;91:543–51.
[62] Zucca E, Conconi A, Laszlo D, Lopez-Guillermo A, Bouabdallah R, Coiffier B,et al. Addition of rituximab to chlorambucil produces superior event-freesurvival in the treatment of patients with extranodal marginal-zone B-celllymphoma: 5-year analysis of the IELSG-19 Randomized Study. J Clin Oncol2013;31:565–72.
[63] Patron R, Miles EF. Stage IAE follicular lymphoma of the breast: case reportand review of the literature. Case Rep Oncol Med 2013;2013:597527.
[64] Mac Manus MP, Hoppe RT. Is radiotherapy curative for stage I and II low-grade follicular lymphoma? Results of a long-term follow-up study ofpatients treated at Stanford University. J Clin Oncol 1996;14:1282–90.
[65] Fadare O, Shukla P. Another case of mantle cell lymphoma presenting asbreast masses. J Clin Pathol 2002;55:640.
[66] Dane F, Seker M, Fulden Yumuk P, Gunduz F, Peker O, Basaran G, et al.Primary breast mantle cell lymphoma with atypical relapse patterns. J BUON2011;16:181–2.
[67] Ferrer A, Salaverria I, Bosch F, Villamor N, Rozman M, Bea S, et al. Leukemicinvolvement is a common feature in mantle cell lymphoma. Cancer2007;109:2473–80.
[68] Pott C, Schrader C, Gesk S, Harder L, Tiemann M, Raff T, et al. Quantitativeassessment of molecular remission after high-dose therapy with autologousstem cell transplantation predicts long-term remission in mantle celllymphoma. Blood 2006;107:2271–8.
[69] Romaguera JE, Medeiros LJ, Hagemeister FB, Fayad LE, Rodriguez MA, Pro B,et al. Frequency of gastrointestinal involvement and its clinical significance inmantle cell lymphoma. Cancer 2003;97:586–91.
ancer Treat Rev (2014), http://dx.doi.org/10.1016/j.ctrv.2014.05.010
C.Y. Cheah et al. / Cancer Treatment Reviews xxx (2014) xxx–xxx 9
[70] Bernard M, Tsang RW, Le LW, Hodgson DC, Sun A, Wells W, et al. Limited-stage mantle cell lymphoma: treatment outcomes at the Princess MargaretHospital. Leuk Lymphoma 2013;54:261–7.
[71] Leitch HA, Gascoyne RD, Chhanabhai M, Voss NJ, Klasa R, Connors JM.Limited-stage mantle-cell lymphoma. Ann Oncol 2003;14:1555–61.
[72] Horowitz NA, Benyamini N, Wohlfart K, Brenner B, Avivi I. Reproductiveorgan involvement in non-Hodgkin lymphoma during pregnancy: asystematic review. Lancet Oncol 2013;14:e275–82.
[73] Evens AM, Carson KR, Kolesar J, Nabhan C, Helenowski I, Islam N, et al. Amulticenter phase II study incorporating high-dose rituximab and liposomaldoxorubicin into the CODOX-M/IVAC regimen for untreated Burkitt’slymphoma. Ann Oncol 2013;24:3076–81.
[74] Taylor CR, Siddiqi IN, Brody GS. Anaplastic large cell lymphoma occurring inassociation with breast implants: review of pathologic andimmunohistochemical features in 103 cases. Appl Immunohistochem MolMorphol 2013;21:13–20.
[75] Thompson PA, Prince HM. Breast implant-associated anaplastic large celllymphoma: a systematic review of the literature and mini-meta analysis.Curr Hematol Malig Rep 2013;8:196–210.
[76] Lechner MG, Lade S, Liebertz DJ, Prince HM, Brody GS, Webster HR, et al.Breast implant-associated, ALK-negative, T-cell, anaplastic, large-celllymphoma: establishment and characterization of a model cell line (TLBR-1) for this newly emerging clinical entity. Cancer 2011;117:1478–89.
[77] Thompson PA, Lade S, Webster H, Ryan G, Prince HM. Effusion-associatedanaplastic large cell lymphoma of the breast: time for it to be defined as adistinct clinico-pathological entity. Haematologica 2010;95:1977–9.
[78] Yoshida S, Nakamura N, Sasaki Y, Yoshida S, Yasuda M, Sagara H, et al.Primary breast diffuse large B-cell lymphoma shows a non-germinal centerB-cell phenotype. Mod Pathol 2005;18:398–405.
[79] Yhim HY, Kim JS, Kang HJ, Kim SJ, Kim WS, Choi CW, et al. Matched-pairanalysis comparing the outcomes of primary breast and nodal diffuse large B-cell lymphoma in patients treated with rituximab plus chemotherapy. Int JCancer 2012;131:235–43.
[80] Aviles A, Neri N, Nambo MJ. The role of genotype in 104 cases of diffuse largeB-cell lymphoma primary of breast. Am J Clin Oncol 2012;35:126–9.
[81] Kuper-Hommel MJ, Schreuder MI, Gemmink AH, van Krieken JH.T(14;18)(q32;q21) involving MALT1 and IGH genes occurs in extranodaldiffuse large B-cell lymphomas of the breast and testis. Mod Pathol2013;26:421–7.
[82] Zhao S, Zhang QY, Ma WJ, Zhang MH, Sun WZ, Li HB, et al. Analysis of 31 casesof primary breast lymphoma: the effect of nodal involvement andmicrovascular density. Clin Lymphoma Myeloma Leuk 2011;11:33–7.
[83] Cheah CY, Wirth A, Seymour JF. Primary testicular lymphoma. Blood2014;123:486–93.
[84] Hopken UE, Rehm A. Homeostatic chemokines guide lymphoma cells totumor growth-promoting niches within secondary lymphoid organs. J MolMed (Berl) 2012;90:1237–45.
[85] Holte H, Leppä S, Björkholm M, Fluge Ø, Jyrkkiö S, Delabie J, et al. Dose-densified chemoimmunotherapy followed by systemic central nervoussystem prophylaxis for younger high-risk diffuse large B-cell/folliculargrade 3 lymphoma patients: results of a phase II Nordic Lymphoma Groupstudy. Ann Oncol 2013;24:1385–92.
[86] Cheah CY, Herbert K, O’Rourke K, Kennedy G, George A, Fedele P, et al.Incorporating high-dose IV methotrexate into initial therapy results in lowerrates of central nervous system (CNS) relapse in patients with high-riskdiffuse large b-cell lymphoma (DLBCL). Blood 2013;122:4353.
[87] Aviles A, Castaneda C, Neri N, Cleto S, Nambo MJ. Rituximab and dose densechemotherapy in primary breast lymphoma. Haematologica 2007;92:1147–8.
Please cite this article in press as: Cheah CY et al. Primary breast lymphoma. C
[88] Aviles A, Delgado S, Nambo MJ, Neri N, Murillo E, Cleto S. Primary breastlymphoma: results of a controlled clinical trial. Oncology 2005;69:256–60.
[89] Martelli M, Ferreri AJ, Agostinelli C, Di Rocco A, Pfreundschuh M, Pileri SA.Diffuse large B-cell lymphoma. Crit Rev Oncol Hematol 2013;87:146–71.
[90] Ryan GF, Roos DR, Seymour JF. Primary non-Hodgkin’s lymphoma of thebreast: retrospective analysis of prognosis and patterns of failure in twoAustralian centers. Clin Lymphoma Myeloma 2006;6:337–41.
[91] Campbell BA, Connors JM, Gascoyne RD, Morris WJ, Pickles T, Sehn LH.Limited-stage diffuse large B-cell lymphoma treated with abbreviatedsystemic therapy and consolidation radiotherapy: involved-field versusinvolved-node radiotherapy. Cancer 2012;2012:26687.
[92] Campbell BA. The role of radiation therapy in the treatment of stage I-IIdiffuse large B-cell lymphoma. Curr Hematol Malig Rep 2013;8:236–42.
[93] Non-Hodgkin’s Lymphomas, version 1.2014. NCCN Clinical PracticeGuidelines in Oncology (NCCN Guidelines): National Comprehensive CancerNetwork; 2014.
[94] Specht L, Yahalom J, Illidge T, Berthelsen AK, Constine LS, Eich HT, et al.Modern radiation therapy for Hodgkin lymphoma: field and dose guidelinesfrom the International Lymphoma Radiation Oncology Group (ILROG). Int JRadiat Oncol Biol Phys 2013.
[95] Campbell BA, Hornby C, Cunninghame J, Burns M, Mac Manus M, Ryan G,et al. Minimising critical organ irradiation in limited stage Hodgkinlymphoma: a dosimetric study of the benefit of involved noderadiotherapy. Ann Oncol 2011;2011:29.
[96] Filippi AR, Ciammella P, Namsyl-Kaletka A, Botticella A, Todisco L, Fiandra C,et al. Single institution preliminary experience on dose reduction to organs atrisk in thoracic radiotherapy for patients enrolled in EORTC-GELA-IIL H10study protocol on early stage Hodgkin’s lymphoma. Eur J Cancer Suppl2009;7:158.
[97] Morin RD, Gascoyne RD. Newly identified mechanisms in B-cell non-Hodgkinlymphomas uncovered by next-generation sequencing. Semin Hematol2013;50:303–13.
[98] Ashizawa T, Miyata H, Ishii H, Oshita C, Matsuno K, Masuda Y, et al. Antitumoractivity of a novel small molecule STAT3 inhibitor against a humanlymphoma cell line with high STAT3 activation. Int J Oncol 2011;38:1245–52.
[99] Dunleavy K, Pittaluga S, Czuczman MS, Dave SS, Wright G, Grant N, et al.Differential efficacy of bortezomib plus chemotherapy within molecularsubtypes of diffuse large B-cell lymphoma. Blood 2009;113:6069–76.
[100] Chiappella A, Tucci A, Castellino A, Pavone V, Baldi I, Carella AM, et al.Lenalidomide plus cyclophosphamide, doxorubicin, vincristine, prednisoneand rituximab is safe and effective in untreated elderly diffuse large B-celllymphoma patients: phase I study by the Fondazione Italiana Linfomi.Haematologica 2013.
[101] Wilson WH, Gerecitano JF, Goy A, de Vos S, Kenkre VP, Barr PM, et al. TheBruton’s tyrosine kinase (BTK) inhibitor, ibrutinib (PCI-32765), haspreferential activity in the ABC subtype of relapsed/refractory de novodiffuse large B-cell lymphoma (DLBCL): interim results of a multicenter,open-label, phase 2 study. ASH Annual Meeting Abstracts 2012;120:686.
[102] Robertson MJ, Kahl BS, Vose JM, de Vos S, Laughlin M, Flynn PJ, et al. Phase IIstudy of enzastaurin, a protein kinase C beta inhibitor, in patients withrelapsed or refractory diffuse large B-cell lymphoma. J Clin Oncol2007;25:1741–6.
[103] Friedberg JW, Sharman J, Sweetenham J, Johnston PB, Vose JM, Lacasce A,et al. Inhibition of Syk with fostamatinib disodium has significant clinicalactivity in non-Hodgkin lymphoma and chronic lymphocytic leukemia. Blood2010;115:2578–85.
ancer Treat Rev (2014), http://dx.doi.org/10.1016/j.ctrv.2014.05.010