A Sardinian map for multiple sclerosis
Transcript of A Sardinian map for multiple sclerosis
10.2217/FMB.12.135 © 2013 Future Medicine Ltd ISSN 1746-0913Future Microbiol. (2013) 8(2), 223–232
Futu
re M
icro
bio
log
y
part of
223
Multiple sclerosis etiologyMultiple sclerosis (MS) is one of the most prevalent autoimmune and neurodegenerative disorder of the CNS, affecting 0.1% of the population living in high-prevalence areas [1]. The hallmark of this disease is the loss of the protective myelin sheath surrounding the axons of neurons, resulting in neurological damage [2]. Inflammatory demyelination is mainly due to the infiltration of myelin-specific CD4+ T cells, which penetrate the blood–brain barrier (BBB) and thus attack the myelin sheath [3].
MS is a complex disease, the etiology of which remains elusive, but according to current data, MS is considered, in many aspects, to be the result of an interaction between genetic and environmental factors. Genetic susceptibility is strongly correlated with the HLA class II locus; in particular, the alleles DR and DQ account for 10–60% of MS genetic risk [4]. More recently, genome-wide association studies have identified approximately 50 potential genes associated with MS; nonetheless, taken individually, each gene has only a weak effect. These include immune-related genes associated with Type 1 diabetes (T1D), such as IL-2RA and IL-7RA alleles [5]. Thus, it is clear that genetics exert a role in conferring MS susceptibility, and in any case, there is a growing body of epidemiological evidence supporting an equally important role for the environment as an inducing stimulus [6].
A number of observations suggest that the environment also plays a role in the pathogenesis of MS [7]. There are multiple theories regarding how infections may induce autoimmunity, and different pathogens (mainly viruses) have been reported to be linked to MS over the past four
decades [8]. However, confirmation of the vast majority of these findings is lacking. Among the viruses, EBV is the best candidate, and it has been thoroughly described elsewhere [9]. Concerning bacteria, several data support the involvement of both Helicobacter pylori and Chlamydia pneumoniae in MS [10,11].
Recent findings propose that Mycobacterium avium subsp. paratuberculosis (MAP) infection could act as a risk factor favoring MS progression in the Sardinian population [12–14]. The total number of individuals suffering from MS in the world is approximately 2.5 million, 400,000 of whom are in Europe and 57,000 in Italy [1]. Sardinia represents an unusual exception to the MS distribution, as there is a notable difference in MS frequency compared with other Mediterranean populations. Sardinians have a genetically isolated background characterized by a uniquely high rate of incidence of several autoimmune disorders, among which MS presents one of the highest incidence rates worldwide [15]. A recent study looking at the prevalence of 12 autoimmune diseases in Sardinia showed that 5% of the general population is affected by one or more autoimmune diseases. The most common disease is Hashimoto’s thyroiditis, whereas T1D and MS are respectively the fourth and the fifth most prevalent diseases. The results reported showed that individuals affected by one autoimmune disease are most likely to develop a second autoimmune disorder, suggesting that there might be a common pathogenic mechanism behind them [16].
Sardinians are probably prone to developing MS due to their particular genetic structure.
A Sardinian map for multiple sclerosis
Davide Cossu1, Speranza Masala1 & Leonardo A Sechi*1
1Department of Biomedical Sciences, Division of Experimental & Clinical Microbiology, University of Sassari, Sassari, Italy *Author for correspondence: Tel.: +39 079 228462 n Fax: +39 079 212345 n [email protected]
Multiple sclerosis (MS) is a complex autoimmune disease of the CNS. At present, MS etiology remains unknown, but it is believed to be caused by environmental factors acting on a genetic predisposition. Several studies suggest that different microorganisms could play a role in tr iggering autoimmunity, through immunological cross-reactivity or molecular mimicry. An overview of the knowledge regarding the bacteria involved in MS is given, placing emphasis on the newest candidate proposed: Mycobacterium avium subsp. paratuberculosis. This review will focus on discussing several arguments that might support a causal role for Mycobacterium avium subsp. paratuberculosis as an etiologic agent in MS. Additionally, a possible mechanism is postulated attempting to explain how the bacteria could initiate autoimmunity.
Keywords
n bacteria n environmental n etiology n molecular mimicry n multiple sclerosis n Mycobacterium avium subsp. paratuberculosis
Revie
w
Author Pro
of
Future Microbiol. (2013) 8(2) future science group224
Several factors, such as malaria, have led to the fixing of a unique distribution of alleles [17]. It is also plausible that environmental factors, such as bacteria, play a major role in shaping such a unique distribution. It has been hypothesized that autoreactive T cells activated against MAP antigens might cross-react with human myelin epitopes sharing similar amino acid sequences.
Given that some genetic variants associated with MS can influence the immunological response of the host towards environmental agents, the relationship between environmental factors and predisposing genes in the context of the Sardinian population has been investigated [12–14,18]. MAP was previously associated with other inflammatory and autoimmune diseases, such as Crohn’s disease (CD) [19], T1D [20] and Hashimoto’s thyroiditis [21].
Concerning MS, MAP DNA was first detected in the peripheral blood of MS patients, and its possible involvement was further supported by the discovery of two MAP proteins (MAP2694 and MAPFprB) sharing sequence homology with two human proteins [12,13].
Even if these MAP antigens were not homologs of CNS myelin proteins, they share sequence homology with myelin protein P0, T-cell receptor (TCR)-g chain C region, complement activation product C1q and the ionotropic NMDA glutamate receptors.
It was then hypothesized that MAP may trigger autoimmunity through a mechanism of molecular mimicry, leading to the activation of the relevant autoreactive T-cell clones [12,13].
M. avium subsp. paratuberculosis MAP is a Ziehl–Neelsen-positive rod-shaped bacterium and it is a member of the M. avium complex, which comprises four subspecies: M. avium subsp. avium, M. avium subsp. silvaticum, MAP and M. avium subsp. hominissuiss. These subspecies represent phenotypically diverse organisms, ranging from environmental bacteria that cause opportunistic infections of swine and immunocompromised people to successful pathogens of birds and ruminants [22]. It belongs to the family of Mycobacteriaceae, which are defined by their acid-fast properties, having a cell wall containing mycolic acids, and a high (61–71%) genomic C + G content. In vitro doubling times vary between subspecies from 12 to over 20 h, with MAP being one of the slowest growers (over 48 h). A MAP primary culture from veterinary/clinical or food specimens can take 3–4 months or longer. MAP is an obligate pathogenic parasite
of animals and protozoa; the only place it can multiply in nature is within a susceptible host, inside their macrophages. When MAP leaves an animal (e.g., in feces or milk), it can survive for extended periods in soil and water, but it is unable to multiply outside the host. MAP can also be found in milk in humans; therefore, one of the primary sources of MAP infection could be vertical, from an infected mother to newborns [23]. MAP can survive pasteurization, as demonstrated in different studies [24], and cheese, meat and vegetables can be contaminated [25]. Moreover, MAP has been found in powdered milk for infants [26]. There is evidence that MAP can exist in vegetative, cell wall-deficient, dormant forms, and it has been shown to form spores [27]. MAP is the established causative agent of debilitating chronic granulomatous enteritis in cattle and other domestic and wild ruminants, called Johne’s disease (JD) or paratuberculosis [28]. MAP has been associated with CD in humans, a chronic inflammatory bowel disease of the GI tract, which is characterized by general malaise, chronic weight loss, abdominal pain and diarrhea [28]. CD presents strikingly similar symptoms to JD, and both diseases are characterized by granuloma formation. While it is simple to picture the role played by MAP in JD/CD disease, it is difficult to investigate the presence of intestinal granulomas in autoimmune diseases characterized by a strong autoantibody response.
Regarding MAP and T1D, it has been shown that MAP can play a role in triggering autoimmunity towards pancreatic b-cells [29], and MAP has been isolated from the peripheral blood of T1D patients [30].
A link between MAP and Hashimoto’s thyroiditis has been postulated, as the presence of viable MAP was ascertained by reverse transcription-PCR in a few Italian family members suffering from the aforementioned pathology [21].
MAP is present worldwide, but epidemio-logical studies are lacking regarding its true distribution [31]. In northern Italy, it has been reported that approximately 70% of bovine herds are infected with MAP [32] and approximately 60% of Sardinian sheep flocks are infected by this pathogen [29]. In fact, the introduction of paratuberculosis, along with a distribution of MS over the years, has been documented in Iceland. Notably, this geographically isolated island was paratuberculosis free until 1938. The introduction of MAP is probably due to
Review Cossu, Masala & Sechi
Author Pro
of
www.futuremedicine.com 225future science group
the importing of 20 sheep from Germany, among which there were hidden carriers of paratuberculosis [33]. If we look at the increase of new MS cases reported in Iceland, there is a sharp increase from 1950 [34]. Taking into account that these 20 silent carriers could have spread the bacteria for years without manifesting the disease, it is noteworthy to consider the fact that the sharp increase in new MS cases might occur many years after the introduction of an environmental factor, such as a peculiar slow-growing pathogen bacterium. The introduction of MAP and its spread within farms might be one of the environmental agents involved in favoring MS. MS epidemiology in the Faroe Islands supports the hypothesis of an infectious cause [35], although it is not certain when paratuberculosis was introduced to the islands.
GeneticsThis section aims to highlight the associations between MS and polymorphisms with genes involved in resistance to intracellular microorganisms; for those interested who are in a complete overview, we suggest Sawcer et al. [36].
The particular genetic makeup of Sardinians and the spreading of MAP in this island could act synergistically in predisposing the population to develop MS.
The SLC11A1 gene (formerly known as NRAMP1) is exclusively expressed in monocytes/macrophages and peripheral blood mononuclear cells. It encodes for an antiport protein within the phagosomes that transports Fe2+ to acidic late endosomes and lysosomes, where toxic radicals are generated via Fenton and/or Haber–Weiss reactions [37]. Associations between SLC11A1 polymorphisms and TB susceptibility have been reported several times [38–40]. A consistent association between SLC11A1 polymorphisms and TB in different populations, which supports the hypothesis that SLC11A1 might play an important role in the host defense against the development of TB, was recently reported [41]. Concerning paratuberculosis, an SLC11A1 polymorphism (P356A) that could alter SLC11A1 protein function was reported in cattle [42]. This association study supports the involvement of the SLC11A1 gene in susceptibility to MAP infection in cattle. Regarding human autoimmune diseases, the presence of SLC11A1 gene polymorphisms in MS [14,18], T1D [43,44] and CD patients [45] led to the concl usion
that MAP might be implicated in MS auto-immune process, in the same function as for T1D and CD.
SLC11A1 exerts influence on the function of macrophages, which are not only essential in the protection against mycobacterial infec-tions, but are also important in the initia-tion and development of several autoimmune diseases [37].
Since MAP persists within macrophages and is recognized and presented by dendritic cells and macrophages, mutant forms of SLC11A1 impairing divalent cation transport through the membrane may alter the processing or presentation of MAP antigen homologs to MS autoantigens, leading to autoimmunity [41]. Going into detail, a recent pilot study based on PCR-restriction fragment length polymorphism typing of eight SLC11A1 single nucleotide polymorphisms (SNPs) reported a novel association between MS and the rs2276631 SNP within the SLC11A1 gene [14]. The polymorphism rs2276631 is a nucleotide substitution that occurs in exon 3 (codon 66 for Phe). It consists of a C/T substitution at residue 274, which could impair iron transport through the channel. This, in turn, could cause avoidance of phagosome acidification and enable mycobacterial survival inside the macrophage. This rs2276631 SNP was also associated with T1D [43], suggesting that the same polymorphism may be common to the major autoimmune diseases that are widespread in Sardinia. These results also suggest that the rs2276631 SNP might contribute to increased susceptibility to MS, although further studies are needed in order to assess the robustness of this association. In fact, the study described above lacks an analysis of the 5´(GT)n repeat polymorphism (rs34448891), which has been previously associated with MS [18].
Moreover, given that the SLC11A1 gene has not been found to be associated with MS in large genome-wide screens, it is now absolutely necessary to replicate these results in larger datasets.
So far, the available data seem to suggest that intracellular pathogens, such as MAP, could play a role in initiating MS in genetically susceptible individuals.
Detection of MAP DNAMAP was detected in 42% of MS patients, but only in 6.3% of healthy controls (HCs) [12]. This first cohort of MS patients was chosen among patients that had been entirely drug free
A Sardinian map for multiple sclerosis Review
Author Pro
of
Future Microbiol. (2013) 8(2)226 future science group
for at least 6 months before recruitment and with the following clinical courses: 42 relaps-ing–remitting, six secondary progressive and two primary progressive. MAP DNA was detected in peripheral blood mononuclear cells by PCR amplification of the IS900 sequences. The IS900 element is highly specific for the MAP organism, and PCR targeting of this ele-ment is accepted to be the reference standard to discriminate MAP from other mycobacteria [23]. This finding shaped the basis of the sub-sequent search for evidence linking MAP to MS. In a larger sample size study (this time including patients under immunomodulating drugs), 27.5% of MS patients and 6.3% of HCs were IS900 PCR positive, and the association was proven to be very statistically significant [13]. MS patients were diagnosed according to the 2010 Revised McDonald criteria [46], while HCs were chosen to all be ethnically Sardinian for at least three generations with no personal or familial history of autoimmune diseases. In order to both fulfill Koch’s postulates and to adduce tangible evidence of MAP presence, a compulsory next step would be to isolate and culture the bacteria from the blood of the posi-tive MS patients, as has previously been done for T1D patients [30].
Molecular mimicry: the role of MAP2694, MAPFprB & mycobacterial heat shock proteins
The association of MAP with MS is based on the concept of molecular mimicry, a mechanism by which MAP can induce autoimmunity. Structural similarity between MAP and self-components might be implicated in the mechanism of antibody (Ab) production. Table 1 reports the mycobacterial proteins, along with the respective human homolog proteins, linked to MS. Molecular mimicry occurs when an infectious agent, such as a bacterium, displays antigenic elements similar to host components. Due to this resemblance, the pathogen structure elicits an immune response capable of breaking the immune tolerance to the host component. For example, TCRs specific for epitopes derived from MAP might be activated during the infection and cross-react with self-antigens, inducing autoimmune disease. Either linear amino acid sequences of the molecules or their conformational epitopes may be shared, even though their origins are separate (in the case of humoral response) [41]. Two MAP-specific proteins were identified by comparisons between the MAP proteome and
the repertoire of human proteins: MAP2694 and MAPFprB [12 ,13] . An immunoassay (indirect ELISA) was designed for the detection of anti-MAP Abs against these two proteins in MS patients. Receiver operator characteristic curves were used to score the performance of each single ELISA in discriminating MS patients from HCs. On account of the reported high prevalence of MAP infection in Sardinian MS patients, Sechi et al. postulated that both MAP2694 and MAPFprB proteins are the targets of Ab responses capable of cross-reacting with homologous human sequences [12,13]. Abs against MAP2694 antigen were detected in 32% of MS patients and in 2% of HCs [12]. MAP2694 is located in the MAP cell wall; it displays sequence homology to the TCR-g chain C region and to C1q. Analyses of the entire MAP2694 sequence using the DNASTAR® program shows that this amino acid region (MAP2694
301–309) is likely to be
an important epitope, on account of it having a very high antigenic index, together with a predicted high probability to be exposed on the surface of the membrane. gd T cells, with the potential to influence all levels of inflammation, are known to play a pathogenic role in CNS inflammation and autoimmunity [47]. Several studies have documented the deposition of C1q in MS lesions [48].
What is more, MAP2694 has homology with the ionotropic NMDA glutamate receptors [Cossu D, Masala S, Sechi LA, Unpublished Data]. These receptors are known to be implicated in MS pathology [49,50]. There is evidence that corroborates that the high level of extracellular glutamate can alter BBB permeability [51]. This is interesting, as gd T cells are commonly known for their response to mycobacteria and for lodging at mucosal sites [52]. gd T cells are the main producer of IL-17, a pro-inflammatory autoimmune-associated cytokine [53].
The MAPFprB gene encodes for a putative ferredoxin reductase protein. This protein gave strong ELISA titer values in 27% in the sera of MS patients and only 4% in HCs [13]. MAPFprB protein is homologous to human myelin P0, which is the main protein of the peripheral nervous system in mammals and is expressed in the CNS of both fish and amphibians. Some case reports linked mutations in the P0 gene with MS in subjects affected with hereditary neuropathies [54], but the meaning of this association is still under scrutiny. Interestingly, P0 is a homolog to MOG, a CNS-specific autoantigen. Experiments based on animal
Review Cossu, Masala & Sechi
Author Pro
of
www.futuremedicine.com 227future science group
models showed that MOG is a target of demyelinating Abs [55].
It is still premature to conclude whether cross-recognition between MAP proteins/homologous human proteins involves an epitope mimicry phenomenon starting or precipitating MS. To achieve this objective, the human homolog proteins/peptides should be synthesized and tested by indirect ELISA with the same human sera. If the results are the same, this would mean that cross-recognition is highly likely to occur. Moreover, in a T-cell-mediated autoimmune disease such as MS, it is mandatory to explore potentially cross-reactive T-cell responses. Of further note, to definitely prove that MAP infection plays a causal role in MS, animal model studies should be performed.
It has been ascertained that during MAP infection, both MAP and the host express heat shock proteins (HSPs). This group of proteins is highly conserved and shares some epitopes that might be cross-recognized, leading to autoimmunity [56]. HSP65 has been recently suggested by Dow to be the missing piece of the intricate puzzle that leads to autoimmunity in MAP-infected and genetically predisposed individuals [57]. Even if HSP65 genes are highly conserved among the species, the issues of cross-recognition can be avoided simply by genotyping the 3´ end of this gene [57].
Generally, HSP expression can be cons-titutive or inducible depending on cell conditions. Under physiological conditions, HSPs are constitutively expressed and exert housekeeping function, acting as molecular chaperones. Molecular chaperones assist in the correct folding of proteins, synthesized de novo, preventing misfolding and aggregation of folding intermediates. On the other hand, stress conditions such as heat shock, infection and oxidative and toxic stress are able to induce HSP expression, which exerts cell survival functions and maintains cellular homeostasis [58]. HSP70 exists not only as an intracellular protein, but also as an extracellular one. In particular, HSP70 exerts different functions in accordance with its location. Intracellular HSP70 exerts cytoprotective functions as a chaperone protein, while extracellular HSP70 has immunoregulatory activity, being able to trigger both proinflammatory and immunoregulatory responses. Anti-HSP autoantibodies are found in numerous autoimmune diseases and inflammatory disorders, including MS. Yokota et al. reported that anti-HSP70 autoantibodies
in the cerebrospinal fluid of MS patients may play a pathophysiological role in enhancing inflammation [59]. Moreover, HSP70 has also been associated with MS [58], but it is difficult to elucidate whether it plays a beneficial or harmful role in the disease.
Interestingly, the presence of T lymphocytes capable of recognizing sequences of HSP65 and HSP70 shared by humans and mycobacteria has been documented [60], but it was not possible to clarify whether this cross-recognition was a sporadic or common event. Given that HSPs function as immune targets, and their expression is upregulated during infection, there is a high chance of cross-reactive responses to epitopes shared by the host and the mycobacteria. In silico analyses have led to the identification of a number of Mycobacterium tuberculosis and human cross-reactive specific T-cell epitopes that may be molecular triggers of autoimmunity [61]. With regard to what has been reported, it would be intriguing to decipher whether MAP/human HSPs display considerably similar sequence homology, and if so, to discover the epitopes capable of initiating MS.
Proposed course of actionNatural infections with MAP primarily occur via the fecal–oral route. Assuming that MAP has a role in the pathogenesis of MS, then the infection has to be food- or water-borne. The strongest candidates as vehicles of transmission of MAP from cattle to humans are milk, beef
Table 1. Mycobacterium avium subsp. paratuberculosis and Mycobacterium tuberculosis antigens and their respective human homolog proteins potentially involved in multiple sclerosis through a molecular mimicry mechanism.
Antigen Protein length
Function Homologous human proteins
Mycobacterium paratuberculosis
MAP-2694 351 aa Hypothetical protein
Ionotropic glutamate receptorNMDA-associated protein 1Complement component 1T-cell receptor g chain C region
MAPFprB 566 aa Ferredoxin NADP reductase
Myelin protein P0
Mycobacterium tuberculosis
HSP60 559 aa Molecular chaperone
HSP60cDNA FLJ5491260-kDa chaperonin (fragment; (HSPD1)
A Sardinian map for multiple sclerosis Review
Author Pro
of
Future Microbiol. (2013) 8(2)228 future science group
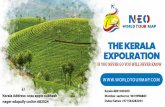
and water. MAP is often acquired during childhood and its colonization site is the GI tract. MAP resides and colonizes the mucosa-associated lymphoid tissue of the small intestine. It passes the intestinal epithelium through the M cells of Peyer’s patches, after which it may be phagocytosed by intraepithelial macrophages and/or dendritic cells [62]. The GI tract and CNS are strictly bidirectionally connected through immune mechanisms [63]. Antigen-presenting cells process and expose MAP epitopes on MHC class I and II activating T cells in the gut that may successively migrate to the periphery and the CNS. MAP persistence in the gut might cause the spreading of inflammatory mediators that, in turn, are responsible for initiating inflammation in the brain. These soluble mediators orchestrate the immune response, attracting CD4+ effector T cells, accounting for inflammation, and driving the polarization of the immune response towards
a Th1/Th17 phenotype. These cells may reach the CNS via the bloodstream, penetrating the BBB in order to infect the CNS and create a milieu of Th1/Th17-type cytokines involved in the pathogenesis and apoptosis of neuronal cells in MS [64]. Figure 1 illustrates the proposed hypothetical mechanism. Notably, the existence of silent MS, an autoimmune process that operates in the predisease stage, has been proven [65]. It has been shown that during this latent phase, an abnormal immunological mechanism occurs, which in turn favors the phenomenon of epitope spreading, which is often related to environmental and genetic factors in a time-dependent mechanism. MAP could be one environmental factor that is responsible for the activation of this apoptotic process during the early youth of genetically predisposed subjects. Therefore, MAP persistence in the gut, together with its ability to induce the production of several inflammatory mediators, appears to
CNS
Bloodstream
Mesenteric lymph nodeIL-12
IL-1, IL-6
IL-18, IL-23
IL-1,IL-18, IL-23IL-1, IL-6,
IL-12, IL-18, IL-23
TLRrecognition
IL-17IL-21
BBBdisruptedTh1
Th1
Th0
Th0T-cellactivation
APCPeyer’spatches
Lamina propria
Epithelium
Intestinal lumenMAP
Th17
Th17
γδT
γδT
Future Microbiol. © Future Science Group (2013)
Figure 1. Mycobacterium avium subsp. paratuberculosis proposed course of action. MAP colonizes the intestinal lumen and passes the epithelium through M cells of Peyer’s patches. Dendritic cells patrolling Peyer’s patches sample MAP bacilli and, acting like APC process and expose MAP epitopes (highly homologous with self antigens) to naive T cells. Naive T cells (Th0) migrate to mesenteric lymph nodes, where Th0 cells differentiate into Th1-type and Th17-type cells, driven by both dendritic cells and gd T-cell-secreted cytokines. Differentiated autoreactive T cells exit the mesenteric lymph nodes and migrate through the blood. Once they have penetrated the BBB, they reach the CNS and attack myelin and host homologous antigens. APC: Antigen presenting cell; BBB: Blood–brain barrier; MAP: Mycobacterium avium subsp. paratuberculosis; TLR: Toll-like receptor.
Review Cossu, Masala & Sechi
Author Pro
of
www.futuremedicine.com 229future science group
Executive summary
Multiple sclerosis etiology�n Multiple sclerosis (MS) is a complex disease, the etiology of which remains elusive, but a number of observations highlight that it stems
from an interaction between genetic and environmental factors. �n Among the environmental factors called into question, EBV has been linked to MS over the past four decades, and concerning bacteria,
the data support an involvement of both Helicobacter pylori and Chlamydia pneumoniae. �n Recent findings propose that Mycobacterium avium subsp. paratuberculosis (MAP) infection could be a risk factor favoring MS
progression in the Sardinian population. MAP DNA was detected in the peripheral blood of MS patients and two MAP proteins sharing sequence homology with two human proteins were identified.
Mycobacterium avium subsp. paratuberculosis �n MAP is a member of the M. avium complex. MAP is the etiological agent of paratuberculosis, a chronic enteritis disease that affects
dairy herds. Not only has MAP transmission to humans long been associated with Crohn’s disease, but MAP infection has also been proposed to be a potential environmental trigger of Type 1 diabetes in humans.
�n MAP is distributed worldwide. In northern Italy, it infects 70% of bovine herds and approximately 60% of Sardinian sheep flocks are MAP positive.
Genetics�n Sardinia is one of the regions with the highest incidence of MS worldwide. Sardinians might be prone to develop MS due to their
particular genetic makeup entrenched by centuries of isolation and endogamy.�n The SLC11A1 gene plays an important role in the immune response against intracellular bacteria, such as MAP.�n Associations between SLC11A1 polymorphisms and MAP infection have been reported.
Molecular mimicry: the role of MAP2694, MAPFprB & mycobacterial heat shock proteins�n Molecular mimicry theory explains how cross-reactive immune responses towards common human and pathogen epitopes can initiate
autoimmunity.�n Based on sequence homology between two MAP proteins and some human proteins, it is suggested that MAP may trigger
autoimmunity in Sardinian MS patients. Sardinian MS patients have preferential humoral responses to both MAP2694 and MAPFprB proteins.
�n During MAP infection, both MAP and the host express heat shock proteins. This group of proteins is highly conserved and share some epitopes that might be cross-recognized, leading to autoimmunity.
Proposed course of action �n MAP may trigger autoimmunity in MS through molecular mimicry and activation of the relevant autoreactive T-cell clones in the gut
towards a pathogenic proinflammatory Th1 and Th17 response.
Conclusion �n MAP is one of the candidates that best suits the role of an environmental trigger in MS pathology.�n MS patients in Sardinia mount a consistent humoral response towards both MAP2694 and MAPFprB proteins. MAP-specific DNA
(IS900) can be detected in a significantly higher proportion of MS patients than controls.�n Definitive evidence proving a causal relationship between MAP and MS is still to be found, but the presence of an association is
undeniable.
be a common denominator influencing the pathophysiology of autoimmune diseases such as MS, T1D and CD.
Conclusion MS is a complex autoimmune disease consid-ered to be the consequence of an environmental pressure in genetically susceptible individuals. MS causative agents remain to be determined, despite the fact that a number of studies have been set up in order to discover a putative etio-logical agent. To date, MAP is one of the candi-dates that best suits the role of the environmental trigger. The foremost evidence supporting a link between MAP and MS comes from both the higher detection rates of MAP by IS900-specific PCR in samples from MS patients compared
with age- and gender-matched HCs and from the demonstration of a serological response toward two specific MAP antigens. Definitive evidence proving a causal relationship between MAP and MS is not available at present – per-haps it may never be. However, there is evidence that suggests some kind of association between MAP and at least some cases of MS.
Future perspectiveAll of the drugs actually in use for MS work by suppressing or altering the activity of the body’s immune system. Thus, these therapies are based on the theory that MS is a result of an abnormal response of the body’s immune system that causes it to attack myelin sheaths. It can be reasonably assumed that during the
A Sardinian map for multiple sclerosis Review
Author Pro
of
Future Microbiol. (2013) 8(2)230 future science group
next 5–10 years, immunodominant peptides of MAP will be determined, helping in turn to discover the specific regions targeted by the immune system. In the future, new vaccines based on these regions may be used to protect susceptible individuals. This approach is an advance to ‘personalized medicine’. This alternative method of treatment is an extension of traditional approaches and better takes into account the specific needs of each patient. This is of fundamental importance given the unique background of the Sardinian population.
It is therefore necessary to obtain extra data supporting a direct involvement of MAP in triggering the disease, and the association must be confirmed outside Sardinia. A step forward in supporting the proposed mechanism
could be the setting up of an animal model to document whether MAP infection, MAP2694 or MAPFprB immunization or MAP-reactive T cells induce disease.
Financial & competing interests disclosureThis work was funded by the Sardinian Region L.R.7 2009 and 2010 Progetti di Ricerca di Base, PRIN MIUR Programmi di Ricerca Scientifica di Rilevante Interesse Nazionale Bando PRIN 2009 protocollo: 2009ZYECWZ. The authors have no other relevant affiliations or financial involvement with any organi-zation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
ReferencesPapers of special note have been highlighted as:n of interestnn of considerable interest
1. Gourraud PA, Harbo HF, Hauser SL, Baranzini SE. The genetics of multiple sclerosis: an up-to-date review. Immunol. Rev. 248(1), 87–103 (2012).
2. Pirko I, Johnson AJ, Lohrey AK, Chen Y, Ying J. Deep gray matter T2 hypointensity correlates with disability in a murine model of MS. J. Neurol. Sci. 282(1–2), 34–38 (2009).
3. Kawakami N, Bartholomäus I, Pesic M, Mues M. An autoimmunity odyssey: how autoreactive T cells infiltrate into the CNS. Immunol. Rev. 248(1), 140–155 (2012).
4. Hafler DA, Compston A, Sawcer S et al. Risk alleles for multiple sclerosis identified by a genomewide study. N. Engl. J. Med. 357(9), 851–862 (2007).
5. Oksenberg JR, Baranzini SE. Multiple sclerosis genetics – is the glass half full, or half empty? Nat. Rev. Neurol. 6(8), 429–437 (2010).
6. Ascherio A, Munger K. Epidemiology of multiple sclerosis: from risk factors to prevention. Semin. Neurol. 28(1), 17–28 (2008).
7. Kakalacheva K, Lunemann JD. Environmental triggers of multiple sclerosis. FEBS Lett. 585(23), 3724–3729 (2011).
8. Javierre BM, Hernando H, Ballestar E. Environmental triggers and epigenetic deregulation in autoimmune disease. Discov. Med. 12(67), 535–545 (2011).
9. Carter CJ. Epstein–Barr and other viral mimicry of autoantigens, myelin and vitamin D-related proteins and of EIF2B, the cause of vanishing white matter disease: massive mimicry of multiple sclerosis relevant
proteins by the Synechococcus phage. Immunopharmacol. Immunotoxicol. 34(1), 21–35 (2012).
10. Gavalas E, Kountouras J, Deretzi G et al. Helicobacter pylori and multiple sclerosis. J. Neuroimmunol. 188(1–2), 187–189; author reply 190 (2007).
11. Contini C, Seraceni S, Cultrera R et al. Chlamydophila pneumoniae infection and its role in neurological disorders. Interdiscip. Perspect. Infect. Dis. 2010, 273573 (2010).
12. Cossu D, Cocco E, Paccagnini D et al. Association of Mycobacterium avium subsp. paratuberculosis with multiple sclerosis in Sardinian patients. PLoS One 6(4), e18482 (2011).
nn� First report of the association between Mycobacterium avium subsp. paratuberculosis (MAP) and multiple sclerosis in the context of the Sardinian population.
13. Cossu D, Masala S, Cocco E et al. Are Mycobacterium avium subsp. paratuberculosis and Epstein–Barr virus triggers of multiple sclerosis in Sardinia? Mult. Scler. 18(8), 1181–1184 (2012).
nn� Identified a new immunogenic MAP protein potentially involved in autoimmunity.
14. Cossu D, Masala S, Cocco E et al. Association of Mycobacterium avium subsp. paratuberculosis infection and SLC11A1 polymorphisms in Sardinian multiple sclerosis patients. J. Infect.Dev. Count. (2012) (In press).
n� Linking of a novel polymorphism in the SLC11A1 gene to multiple sclerosis and MAP infection in a Sardinian cohort.
15. Cocco E, Sardu C, Massa R et al. Epidemiology of multiple sclerosis in south-
western Sardinia. Mult. Scler. 17(11), 1282–1289 (2011).
16. Sardu C, Cocco E, Mereu A et al. Population based study of 12 autoimmune diseases in Sardinia, Italy: prevalence and comorbidity. PLoS One 7(3), e32487 (2012).
17. Sotgiu S, Angius A, Embry A, Rosati G, Musumeci S. Hygiene hypothesis: innate immunity, malaria and multiple sclerosis. Med. Hypotheses 70(4), 819–825 (2008).
18. Gazouli M, Sechi L, Paccagnini D et al. NRAMP1 polymorphism and viral factors in Sardinian multiple sclerosis patients. Can. J. Neurol. Sci. 35(4), 491–494 (2008).
19. Sabatino A, Paccagnini D, Vidali F et al. Detection of Mycobacterium avium subsp. paratuberculosis (MAP)-specific IS900 DNA and antibodies against MAP peptides and lysate in the blood of Crohn’s disease patients. Inflamm. Bowel Dis. 17(5), 1254–1255 (2011).
20. Sechi LA, Paccagnini D, Salza S, Pacifico A, Ahmed N, Zanetti S. Mycobacterium avium subspecies paratuberculosis bacteremia in Type 1 diabetes mellitus: an infectious trigger? Clin. Infect. Dis. 46(1), 148–149 (2008).
21. Sisto M, Cucci L, D’Amore M, Dow TC, Mitolo V, Lisi S. Proposing a relationship between Mycobacterium avium subspecies paratuberculosis infection and Hashimoto’s thyroiditis. Scand. J. Infect. Dis. 42(10), 787–790 (2010).
22. Turenne CY, Collins DM, Alexander DC, Behr MA. Mycobacterium avium subsp. paratuberculosis and M. avium subsp. avium are independently evolved pathogenic clones of a much broader group of M. avium organisms. J. Bacteriol. 190(7), 2479–2487 (2008).
Review Cossu, Masala & Sechi
Author Pro
of
www.futuremedicine.com 231future science group
23. Turenne CY, Wallace R Jr, Behr MA. Mycobacterium avium in the postgenomic era. Clin. Microbiol. Rev. 20(2), 205–229 (2007).
n� Overview of the main characteristics of the M. avium complex.
24. Botsaris G, Slana I, Liapi M et al. Rapid detection methods for viable Mycobacterium avium subspecies paratuberculosis in milk and cheese. Int. J. Food Microbiol. 141(Suppl. 1), S87–S90 (2010).
25. Klanicova B, Slana I, Vondruskova H, Kaevska M, Pavlik I. Real-time quantitative PCR detection of Mycobacterium avium subspecies in meat products. J. Food Prot. 74(4), 636–640 (2011).
26. Klanicova B, Slana I, Roubal P, Pavlik I, Kralik P. Mycobacterium avium subsp. paratuberculosis survival during fermentation of soured milk products detected by culture and quantitative real time PCR methods. Int. J. Food Microbiol. 157(2), 150–155 (2012).
27. Lamont EA, Bannantine JP, Armien A, Ariyakumar DS, Sreevatsan S. Identification and characterization of a spore-like morphotype in chronically starved Mycobacterium avium subsp. paratuberculosis cultures. PLoS One 7(1), e30648 (2012).
28. Chiodini RJ, Chamberlin WM, Sarosiek J, McCallum RW. Crohn’s disease and the mycobacterioses: a quarter century later. Causation or simple association? Crit. Rev. Microbiol. 38(1), 52–93 (2012).
29. Masala S, Paccagnini D, Cossu D et al. Antibodies recognizing Mycobacterium avium paratuberculosis epitopes cross-react with the beta-cell antigen ZnT8 in Sardinian Type 1 diabetic patients. PLoS One 6(10), e26931 (2011).
30. Rosu V, Ahmed N, Paccagnini D et al. Specific immunoassays confirm association of Mycobacterium avium subsp. paratuberculosis with Type-1 but not Type-2 diabetes mellitus. PLoS One 4(2), e4386 (2009).
31. Nielsen SS, Toft N. A review of prevalences of paratuberculosis in farmed animals in Europe. Prev. Vet. Med. 88(1), 1–14 (2009).
32. Pozzato N, Capello K, Comin A et al. Prevalence of paratuberculosis infection in dairy cattle in northern Italy. Prev. Vet. Med. 102(1), 83–86 (2011).
33. Fridriksdottir V, Gunnarsson E, Sigurdarson S, Gudmundsdottir KB. Paratuberculosis in Iceland: epidemiology and control measures, past and present. Vet. Microbiol. 77(3–4), 263–267 (2000).
34. Benedikz J, Stefansson M, Guomundsson J et al. The natural history of untreated multiple sclerosis in Iceland. A total population-based 50 year prospective study.
Clin. Neurol. Neurosurg. 104(3), 208–210 (2002).
35. Kurtzke JF. Multiple sclerosis in time and space – geographic clues to cause. J. Neurovirol. 6(Suppl. 2), S134–S140 (2000).
36. Sawcer S, Hellenthal G, Pirinen M et al. Genetic risk and a primary role for cell-mediated immune mechanisms in multiple sclerosis. Nature 476(7359), 214–219 (2011).
37. Purdie AC, Plain KM, Begg DJ, de Silva K, Whittington RJ. Candidate gene and genome-wide association studies of Mycobacterium avium subsp. paratuberculosis infection in cattle and sheep: a review. Comp. Immunol. Microbiol. Infect. Dis. 34(3), 197–208 (2011).
38. Meilang Q, Zhang Y, Zhang J et al. Polymorphisms in the SLC11A1 gene and tuberculosis risk: a meta-analysis update. Int. J. Tuberc. Lung Dis. 16(4), 437–446 (2012).
39. Nugraha J, Anggraini R. NRAMP1 polymorphism and susceptibility to lung tuberculosis in Surabaya, Indonesia. Southeast Asian J. Trop. Med. Public Health 42(2), 338–341 (2011).
40. Singh A, Gaughan JP, Kashyap VK. SLC11A1 and VDR gene variants and susceptibility to tuberculosis and disease progression in east India. Int. J. Tuberc. Lung Dis. 15(11), 1468–1474, i (2011).
41. Li X, Yang Y, Zhou F et al. SLC11A1 (NRAMP1) polymorphisms and tuberculosis susceptibility: updated systematic review and meta-analysis. PLoS One 6(1), e15831 (2011).
42. Ruiz-Larranaga O, Garrido JM, Manzano C et al. Identification of single nucleotide polymorphisms in the bovine solute carrier family 11 member 1 (SLC11A1) gene and their association with infection by Mycobacterium avium subspecies paratuberculosis. J. Dairy Sci. 93(4), 1713–1721 (2010).
43. Paccagnini D, Sieswerda L, Rosu V et al. Linking chronic infection and autoimmune diseases: Mycobacterium avium subspecies paratuberculosis, SLC11A1 polymorphisms and Type-1 diabetes mellitus. PLoS One 4(9), e7109 (2009).
n� Association of a relevant SCL11A1 polymorphism with Type 1 diabetes and detection of MAP DNA in the blood of Type 1 diabetes subjects.
44. Yang JH, Downes K, Howson JM et al. Evidence of association with Type 1 diabetes in the SLC11A1 gene region. BMC Med. Genet. 12, 59 (2011).
45. Sechi LA, Gazouli M, Sieswerda LE et al. Relationship between Crohn’s disease, infection with Mycobacterium avium
subspecies paratuberculosis and SLC11A1 gene polymorphisms in Sardinian patients. World J. Gastroenterol. 12(44), 7161–7164 (2006).
46. Polman CH, Reingold SC, Banwell B et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 69(2), 292–302 (2011).
47. Chastain EM, Miller SD. Molecular mimicry as an inducing trigger for CNS autoimmune demyelinating disease. Immunol. Rev. 245(1), 227–238 (2012).
48. Gandhi R, Laroni A, Weiner HL. Role of the innate immune system in the pathogenesis of multiple sclerosis. J. Neuroimmunol. 221(1–2), 7–14 (2010).
49. Brink BP, Veerhuis R, Breij EC, van der Valk P, Dijkstra CD, Bo L. The pathology of multiple sclerosis is location-dependent: no significant complement activation is detected in purely cortical lesions. J. Neuropathol. Exp. Neurol. 64(2), 147–155 (2005).
50. Rossi S, Studer V, Motta C et al. Inflammation inhibits GABA transmission in multiple sclerosis. Mult. Scler. 18(11), 1633–1635 (2012).
51. Newcombe J, Uddin A, Dove R et al. Glutamate receptor expression in multiple sclerosis lesions. Brain Pathol. 18(1), 52–61 (2008).
52. Bolton C, Paul C. Glutamate receptors in neuroinflammatory demyelinating disease.Mediators Inflamm. (2), 93684 (2006).
53. Hayes SM, Laird RM. Genetic requirements for the development and differentiation of interleukin-17-producing gd T cells. Crit. Rev. Immunol. 32(1), 81–95 (2012).
54. Kilfoyle DH, Dyck PJ, Wu Y et al. Myelin protein zero mutation His39Pro: hereditary motor and sensory neuropathy with variable onset, hearing loss, restless legs and multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 77(8), 963–966 (2006).
55. Mayer MC, Meinl E. Glycoproteins as targets of autoantibodies in CNS inflammation: MOG and more. Ther. Adv. Neurol. Disord. 5(3), 147–159 (2012).
56. Rajaiah R, Moudgil KD. Heat-shock proteins can promote as well as regulate autoimmunity. Autoimmun. Rev. 8(5), 388–393 (2009).
57. Dow CT. M. paratuberculosis heat shock protein 65 and human diseases: bridging infection and autoimmunity. Autoimmune Dis. 2012, 150824 (2012)
58. Mansilla MJ, Montalban X, Espejo C. Heat shock protein 70: roles in multiple sclerosis. Mol. Med. 18, 1018–1028 (2012).
A Sardinian map for multiple sclerosis Review
Author Pro
of
Future Microbiol. (2013) 8(2)232 future science group
59. Yokota S, Chiba S, Furuyama H, Fujii N. Cerebrospinal fluids containing anti-HSP70 autoantibodies from multiple sclerosis patients augment HSP70-induced proinflammatory cytokine production in monocytic cells. J. Neuroimmunol. 218(1–2), 129–133 (2010).
60. Rees A, Scoging A, Mehlert A, Young DB, Ivanyi J. Specificity of proliferative response of human CD8 clones to mycobacterial antigens. Eur. J. Immunol. 18(12), 1881–1887 (1988).
61. Babu Chodisetti S, Rai PK, Gowthaman U et al. Potential T cell epitopes of
Mycobacterium tuberculosis that can instigate molecular mimicry against host: implications in autoimmune pathogenesis. BMC Immunol. 13, 13 (2012).
62. Khare S, Lawhon SD, Drake KL et al. Systems biology analysis of gene expression during in vivo Mycobacterium avium paratuberculosis enteric colonization reveals role for immune tolerance. PLoS One 7(8), e42127 (2012).
63. Aszalos Z. [Neurological and psychiatric aspects of some gastrointestinal diseases.] Orv. Hetil. 149(44), 2079–2086 (2008).
n� Describes the bidirectional connection between the CNS and the GI tract.
64. Berer K, Mues M, Koutrolos M et al. Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination. Nature 479(7374), 538–541 (2011).
65. Achiron A, Grotto I, Balicer R, Magalashvili D, Feldman A, Gurevich M. Microarray analysis identifies altered regulation of nuclear receptor family members in the predisease state of multiple sclerosis. Neurobiol. Dis. 38(2), 201–209 (2010).
Review Cossu, Masala & Sechi
Author Pro
of