A preliminary investigation of the brain injury family intervention: Impact on family members
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of A preliminary investigation of the brain injury family intervention: Impact on family members
Brain Injury, June 2009; 23(6): 535–547
A preliminary investigation of the brain injury family intervention:Impact on family members
JEFFREY S. KREUTZER1,2,3, TARYN M. STEJSKAL1, JESSICA M. KETCHUM4,JENNIFER H. MARWITZ1, LAURA A. TAYLOR5, & JENNIFER C. MENZEL6
1Department of Physical Medicine and Rehabilitation, 2Department of Neurological Surgery, 3Department of
Psychiatry, 4Department of Biostatistics, Virginia Commonwealth University, Richmond, VA, USA, 5Village Family
Psychiatry, Richmond, VA, USA, and 6Hunter Holmes McGuire Veterans Affairs Medical Center, Richmond,
VA, USA
(Received 23 September 2008; revised 25 February 2009; accepted 26 March 2009)
AbstractPrimary objective: To evaluate the benefits of the Brain Injury Family Intervention (BIFI) for families of persons withacquired brain injury and identify factors related to outcomes.Research design: Pre-test, post-test design with outcomes measured immediately after and 3 months following intervention.Methods and procedures: Family members and survivors participated in five 2-hour sessions over 10 weeks which includeddiscussions of typical effects of brain injury, coping with loss and change, managing stress and intense emotions, effectiveproblem-solving, setting reasonable goals and taking care of one’s self. Guided by principles of family systems theory (FST)and cognitive behaviour therapy (CBT), the manualized treatment included educational, skill building and psychologicalsupport components.Main outcomes and results: Analysis of data derived from family members indicated a greater number of met needs andperceptions of fewer obstacles to receiving services post-treatment and at 3 months follow-up. Before and after treatment,unmarried caregivers reported more unmet needs. Family members of persons with longer acute care lengths of stayreported more unmet needs and greater perceived obstacles to services. Post-treatment differences in family members’psychological distress, satisfaction with life and functioning were not identified.Conclusions: The investigation provided evidence that family members benefit from interventions designed to meet theirunique needs after brain injury. Uncertainties remain about the benefits of intervention to general family functioning andlife satisfaction.
Keywords: Family interventions, support systems, therapy
Introduction
A number of researchers have expressed concernthat rehabilitation lengths of stay are decreasing[1–3], especially with reduced reimbursement frommanaged care companies and Health MaintenanceOrganizations (HMOs). Shortened hospital staysnecessitate a greater in-hospital focus on physicaland functional goals and fewer opportunities forrehabilitation staff to address the full spectrum
of survivors’ and family members’ needs. Brieferrehabilitation stays also allow less time for neurobe-havioural recovery and discharge planning. Nine ofevery 10 patients are being discharged to home [2],leaving relatives to assume primary caregivingresponsibilities for years after the injury. Familymembers’ responsibilities typically include helpingsurvivors manage activities of daily living, appoint-ments, finances and medications. Family members
Correspondence: Jennifer H. Marwitz, Department of Physical Medicine and Rehabilitation, Virginia Commonwealth University, Richmond, VA, USA.Tel: 804-828-3704. Fax: 804-828-2378. E-mail: [email protected]
ISSN 0269–9052 print/ISSN 1362–301X online � 2009 Informa Healthcare Ltd.DOI: 10.1080/02699050902926291
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
also help arrange for socialization and recreationalactivities and often serve as survivors’ primary sourceof emotional support.
Despite rehabilitation staff members’ best effortsto educate and prepare families, many report feelingoverwhelmed and ill-equipped to provide for survi-vors’ complex and dynamic long-term needs [4–6].Recent research indicates a family’s ability to cope inthe face of stressors influences the quality of supportthey can provide to the person with the injury and,consequently, the extent of the survivor’s neurobe-havioural recovery [7, 8]. Earlier discharge alsoleaves family members with little time to personallyrecover from the emotional shock triggered by theinitial injury.
The impact of brain injury on families has beenwell documented. For example, a variety of research-ers have reported high rates of psychological distress,namely anxiety and depression among caregivers inthe acute and post-acute phases of injury [9–17].Many researchers have documented disruptions infamily functioning [18, 19] as manifested by lesseffective coping, problem-solving and communica-tion [20, 21]. An extensive body of literature onfamily needs indicates that family members rate theneeds for information and emotional support[22, 23], early intervention and advocacy [24] andcommunity reintegration [25] as very important.However, many important needs are identified asunmet [23, 26]. Investigators have reported detri-ments to life satisfaction when families hold percep-tions that services are unavailable, unaffordable andinaccessible [27].
In summary, research has indicated that TBI haslong-term adverse consequences for family mem-bers, especially primary caregivers. Many agree thatfamily members are adversely affected by braininjury and are likely to benefit from treatment[28, 29]. However, few investigators have developedevidence-based interventions for survivors and theirfamily members, leaving important unansweredquestions. A comparative review of family interven-tion studies (see Table I) indicates both differencesand similarities. In every case, intervention includedfamily members, but in most cases survivors werenot included. Treatment delivery methods variedgreatly, with some focused on groups of familymembers, others using individual counsellingsessions in-person or by telephone and some pro-viding informational websites. Many interventionsprovided combinations of education and psycholog-ical support while others focused on skills suchas behaviour management and problem-solving.Investigators’ findings were often equivocal, withsome providing evidence of reduced psychologicaldistress and improved problem-solving skills follow-ing intervention.
In summary, there is little doubt that brain injuryhas adverse long-term consequences for familymembers and survivors. Unfortunately, recentreviews of the literature conclude that there is adearth of scientifically rigorous empirical research onfamily interventions [30]. This manuscript has threemain purposes. First, a detailed description of theBrain Injury Family Intervention (BIFI), a manua-lized treatment for survivors and caregivers, isprovided. Secondly, information regarding care-givers’ well-being, needs, perceived obstacles toreceiving services and family functioning beforeand after treatment is described. Thirdly, limitationsof the present investigation, clinical implications anddirections for future research are discussed.
Methods
Participants
Of 79 families that initially enrolled in the BIFI,53 completed all sessions and assessments. Divorce,separation, moving out of state, severe illness andtransportation difficulties were the reasons mostcommonly cited by participants for discontinuation.Families that did not complete the programme werecompared to those that did on variables includingcaregiver relationship to patient, age, ethnicity,gender, education and patient’s length of hospitalstay and time post-injury. No differences werefound, with the one exception of caregiver age.Younger caregivers were less likely to complete theprogramme. The final sample included 53 personswith acquired brain injury (ABI) and their familymembers. The only two exclusion criteria wereactive psychosis or suicidal intent and no partici-pants were excluded.
With a mean age of 40.73 (SD¼ 16.52), personswith ABI were primarily male (58%), Caucasian(83%) and married (57%). With regard to cause ofinjury, the majority had sustained a traumatic braininjury (87%). Among persons with TBI, the per-centage with mild (admission GCS 13–15), moder-ate (GCS 9–12) and severe (GCS 3–8) injury was47%, 13% and 40%, respectively. Motor vehicleaccidents were the primary cause of injury (52%),with a smaller number injured by motorcycle orbicycle accidents (10%), falls (14%) and bluntobjects (11%). The remaining participants (13%)included individuals with aneurysm, brain abscess,stroke, encephalitis, epilepsy or hypoxia. Additionalinformation regarding injury characteristics is pro-vided in Table II. Data was collected on ancillaryservices received at the time of intervention and amajority of patients were receiving none.Psychological, psychiatric and vocational services
536 J. S. Kreutzer et al.
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
were most often reported, with fewer than 20%receiving such services.
Family members included persons described bysurvivors as a family relation, a partner, a significantother or friend. When more than one family mem-ber was available, data was obtained from the oneperson identified by the patient as providing the
majority of care. Ranging in age from 22–72, with amean of 50.22 years (SD¼ 12.52), the majority ofparticipating family members were spouses andfemale. Other participants included siblings andadult children. Table III provides detailed informa-tion regarding educational level, employment statusand marital status.
Table I. Comparative review of family intervention research studies.
Reference n
Intervention deliverymethod Recipient Intervention purpose
Caregiver interventionbenefits
[68] 19 group; in-person; three 5-hour sessions over 3weekends; manualized
family members psychological support,education
No significant changes incoping ability, self-esteem, or life-satisfaction.
[64] 91 group; in-person, on site vstelephone; ten 1.5–2.0 hour sessions over 10weeks; not manualized
family members psychological support Improvements in psycho-logical distress for bothtreatment groups but noimprovements in familyfunctioning or burdenfor either.
[65] 33 individual; off site; twofollow-up telephonecalls over 5 weeks; notmanualized
family members psychological support,education via informa-tion booklet
No improvements in psy-chological distress.
[63] 56 individual; on site in personand off site, post-dis-charge by telephone;sessions varied in lengthfor a period up to 16months; not manualized
family members psychological support,education
Intervention reducedburden levels, improvedsatisfaction with care-giving and increasedperceptions of caregivingcompetency.
[66] 27 individual; in-person, homeand community setting;2 hour education ses-sions provided weeklyover 4 weeks to all par-ticipants; behaviouralintervention group com-pleted additional 2 hoursessions weekly for 8weeks; not manualized
family members,survivors
behavioural management,problem-solving skillstraining
No significant changes inperceived stress orpsychological distress.
[67] 41 survivor and familymember groups, in-person; eight, 2.5-hoursessions over 8 weeks;not manualized
family members,survivors
education No significant changes inpsychological distress,coping or self-esteem.
Rivera (2008) [61] 67 individual; 12 monthly ses-sions over 1 year, fourin-home, eight by tele-phone; not manualized
family members problem-solving skillstraining
Positive treatment impacton psychological dis-tress/depression, health,dysfunctional problem-solving styles. No impacton caregiver life satis-faction, burden or con-structive problem-solving styles.
Present study 53 individual; on-site; five 1.5–2 hour sessions deliveredover 10 weeks;manualized
family members,survivors
psychological support,education, skills training
Increases in met familyneeds and perceivedaccess to services. Noimpact on psychologicaldistress, family func-tioning, satisfaction withlife.
Family intervention after brain injury 537
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
Intervention structure and content
The Brain Injury Family Intervention (BIFI) is astructured treatment designed to meet the needsmost commonly identified by family members andsurvivors. The intervention was conceived toimprove survivors’ and family members’ psycholog-ical well-being, life satisfaction, access to servicesand enhance family functioning [31]. The BIFI isimplemented over the course of five 90–120 minutesessions. During each session, two or three topics areaddressed, as delineated in Table IV. The 11 topicsare covered in the same sequence with each family.The BIFI was constructed such that sessions werelogically organized to achieve the greatest therapeu-tic impact. Earlier sessions focus on the needs andconcerns most frequently identified during inter-views conducted with family members and withinthe literature. Later sessions reinforce and buildupon the foundation of knowledge and skills learnedin earlier sessions. Each session begins with anoverview of topics and concludes with a summaryand homework assignments.
Clinicians depend on the BIFI manual [32] todeliver the intervention systematically and effi-ciently. For each topic covered in each session, themanual delineates goals, materials needed and, ifnecessary, accommodations for disability. Using astep-by-step approach, the manual provides theclinician with detailed scripts for each module,instructions, therapeutic activities and homework.Bibliotherapy also serves as a helpful complement.Fact sheets, guides and supplementary readings fromthe book Getting Better and Better after Brain Injury:A Guide for Family, Friends, and Caregivers [33] wereprovided and reviewed by participants during treat-ment sessions and for homework.
The BIFI incorporates principles of family systemstheory (FST [34, 35]) and utilizes family therapytechniques. A primary postulate of FST is thatfamilies are interconnected systems. The actions,communications and feelings of each family membertypically influence those of other family members
and the family as a whole. The impact of brain injuryon patients has been well documented. Researchershave also identified a profound impact on familymembers, especially primary caregivers [36, 37]. Assuch, the BIFI is delivered jointly to family membersand survivors. To strengthen family systems, theBIFI relies heavily on family therapy techniquesincluding empathic reflections, validation, reframingand normalization of common concerns.
Cognitive Behavioural Theory (CBT [38]) ispredicated on the idea that a person’s cognitionsinfluence his or her emotions and behavior [39].Change in one area is thought to produce relatedchanges in the other areas of functioning. Recentresearch studies have substantiated the benefits ofCBT after brain injury [40–43]. As such, CBTtechniques have been adapted and incorporated inthe BIFI to improve cognitive, emotional andbehavioural functioning. Educational techniquesare used to inform participants about commoninjury sequelae and recovery. Psychological supporttechniques are used to help participants recognizetheir feelings and improve their emotional well-being. Skills training techniques are used to improveproblem-solving, communication and emotionalcontrol.
The BIFI also makes significant use of thetechnique, collaborative self-examination, developedby Kreutzer and Taylor [32]. Injury typically causesrapid and dramatic changes in the lives of survivorsand family members. Family members are oftenuncertain about their feelings, capabilities, concernsand plans for the future. Survivors often harboursimilar uncertainties which are compounded byimpaired self-awareness. Using collaborative self-examination, each family member shares theirperspectives about events, one another’s behaviour
Table III. Caregiver information at intake.
n¼53 Percentage
Relation to survivorSpouse 29 55%Parent 15 28%Sibling 3 5%Adult child 2 4%Boyfriend/girlfriend 2 4%Other relative 2 4%
Female gender 35 66%Married 44 83%Education level
Less than high school 3 6%High school graduate/some college 28 52%College degree or greater 22 42%
Employment statusCompetitively employed 35 66%Not competitively employed 18 34%
Table II. Injury characteristics (n¼ 53).
Mean Median SD Range
Acute care lengthof stay (days)
14.4 7 18.28 0–80
Rehabilitation lengthof stay (days)
27.8 18 26.23 0–121
Months post-injury 38.6 12.8 50.79 1.6–185Length of unconsciousness
(days)*3.5 0.0 9.51 0–47
Admission GlasgowComa Scale*
10.4 12 4.72 3–15
*For participants with TBI.
538 J. S. Kreutzer et al.
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
and their interactions with one another, encouragingperspective taking, self-monitoring and enhancedawareness. Collaborative self-examination chal-lenges family members’ perceptions of themselvesand provides an opportunity for each person tounderstand how others perceive them. When imple-menting the technique, family members are asked toanswer standardized questions to illuminate infor-mation about their perspective. Then, family mem-bers are asked to communicate their perspectivewhile others listen. All family members are remindedthat they do not have to agree. The discussion ismeant to facilitate understanding, encourage discus-sion, improve family members’ communication skillsand enhance support for one another. Through theuse of collaborative self-examination, family mem-bers are encouraged to recognize and stop usingapproaches that do not work or make things worse.
Family members are also assisted in recognizingand making greater use of approaches that work welland make their lives better.
All clinicians conducting the BIFI treatment weredoctoral level psychologists who received trainingfrom the first author. Initially, clinicians carefullystudied the treatment manual and observed thefirst author providing a course of sessions. Next,therapists were observed and given feedback.Clinicians met weekly for supervision with the firstauthor. At the end of each session, participantscompleted feedback forms indicating their percep-tion of the extent to which session goals wereachieved and their overall satisfaction with the ses-sion and the material presented. Completedforms indicated a high level of satisfaction andthat the goals delineated in the manual wereconsistently achieved.
Table IV. Overview of BIFI sessions and topics.
Session Topic Objective(s)
I. Effects of brain injury on thesurvivor and family
What is normal after brain injury? Recognize, understand and appreciatecommon injury consequences; recognizeeach family member’s point of view aboutthe injury’s effects
Brain injury happens to the whole family Improve communication and recognitionthat each family members’ responsibil-ities, life plans and feelings about thefuture have been significantly changed
II. Understanding recovery Emotional and physical recovery are twodifferent things
Appreciate expectations for improvementand clearly understand the differencesbetween emotional and physiologicalrecovery
Mastering the art of patience Appreciate the benefits of patience andmaster the skill of overcoming impatience
Coping with loss and change Identify and implement strategies to bettercope with loss and change
III. Solving problems and settinggoals
Setting reasonable goals Understand the characteristics and dangersof unrealistic goals and take steps to setmore reasonable and achievable goals
Solving problems effectively Identify obstacles to solving problems effec-tively; learn and apply a framework ofstrategies for efficient problem-solving
IV. Managing stress and intenseemotions
Managing stress effectively Identify current stress levels and recognizepersonal ‘red flags’ which signal stress;employ strategies for managing stresseffectively
Managing intense emotions Recognize communication obstacles and theimportance of communication; employstrategies to effectively manage frustra-tion, anger and other intense emotions
V. Strategies for optimal recovery Taking care of yourself Recognize the adequacy and importanceof self-care; take steps to better care forone’s self
Focusing on gains and accomplishments Realize the strong relationship betweenthoughts and feelings; better recognizestrengths and progress
Most important lessons learned and where togo from here
Recognize and communicate the mostimportant things learned during thecourse of intervention
Family intervention after brain injury 539
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
Measures
. Family Needs Questionnaire (FNQ): The FNQ isa widely used 40-item self-report questionnairedeveloped to measure family members’ perceivedneeds after a family member sustains a braininjury [44–48]. The items were designed toaddress diverse psychosocial and educationalneeds apparent in the acute and post-acutephases after injury. Family members rate theextent to which needs are perceived as importanton a scale ranging from 1¼not important to4¼ very important. Respondents also rate thedegree to which they perceive that each need hasbeen met (not met, partly met or met). Contentand construct validity as well as internal consis-tency has been established (Spearman-Brownsplit-half reliability of 0.75) [22]. A later factoranalytic investigation [49] revealed six indepen-dent factors comprising six scales: HealthInformation, Emotional Support, InstrumentalSupport, Professional Support, CommunitySupport Network and Involvement with Care.Internal consistency for individual factors wasindicated by Chronbach’s alpha’s ranging from0.78–0.89. The proportion of needs described asmet (converted to a 10-point scale) was theprimary family outcome measure for the presentstudy.
. Service Obstacles Scale (SOS): The SOS [50] wasdeveloped to evaluate individuals’ and caregivers’perceptions of brain injury services in the com-munity with regard to quality and accessibility.The six-item scale solicits information regardingobstacles to receiving brain injury services, knowl-edge of and availability of resources and satisfac-tion with the quality of care. Items are rated ona seven-point Likert-type scale ranging from1¼ strongly disagree through 7¼ strongly agree.Lower scores denote greater access and satisfac-tion with services. The SOS has three maincomponents: (1) satisfaction with treatmentresources; (2) finances as an obstacle to receivingservices; and (3) transportation as an obstacle toreceiving services. A recent regional needs assess-ment study provided evidence of the SOS’svalidity [51]. The total score for items relatingto satisfaction with treatment resources served asa primary outcome measure in the presentinvestigation.
. Family Assessment Device (FAD): The FAD is a60-item questionnaire designed to assess diverseaspects of family functioning [52, 53]. A numberof investigators have used the measure to charac-terize families after brain injury. For example,a number of researchers have also utilized theFAD to assess family functioning after brain
injury [7, 54–56]. The present investigation onlyutilized items from the 12-item GeneralFunctioning Scale, developed to characterizeoverall family functioning. Items are rated on ascale ranging from 1–4, indicating ‘strongly agree’to ‘strongly disagree’. Some items are reverse-coded, with lower scores indicative of moreoptimal functioning.
. Brief Symptom Inventory-18 (BSI-18): The BSI-18[57] is an 18 item self-report instrument designedto quantify psychological distress in the generalpopulation. Increasingly, the measure has beenused to quantify family members’ distress afterbrain injury [58, 59]. The instrument is apsychometrically sound [60], abbreviated versionof the SCL-90-R [57]. Frequency ratings foritems in three primary symptom dimensions areadded to yield scores for Somatization,Depression and Anxiety. The Global SeverityIndex (GSI) reflects the sum of scores for thethree primary symptom dimensions. T-scores foreach dimension and the GSI are calculated basedon community norms.
. Satisfaction With Life Scale (SWLS): The SWLS[43] is a measure of global life satisfactioncomprised of five statements scored on a Likertscale such that 1¼Strongly disagree and7¼Strongly agree. The measure has been usedby a number of researchers to characterizecaregivers post-injury [58, 61]. Lower scoresindicate lower levels of life satisfaction.Normative data are available and the scale showsgood convergent validity with other scalesand with other types of assessments of subjectivewell-being [62]. The SWLS has shown sufficientsensitivity to detect changes as a result of clini-cal interventions and has good discriminantvalidity [62].
Procedure
Participants were recruited from a variety of sourcesand included persons with neurobehavioural pro-blems referred by rehabilitation providers, advocacyorganizations and agencies. Screening, assessmentand intervention were centralized in an outpatientrehabilitation clinic attached to a major medicalcentre. During the initial intake session, project staffprovided information about the research pro-gramme, confirmed eligibility and interest in parti-cipation, identified the primary family member andobtained informed consent from all participantsin each family.
On giving informed consent, the individual withTBI and primary family member were given baselineassessment materials to complete. One therapistworked with each family through completion of the
540 J. S. Kreutzer et al.
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
intervention. The five 90–120 minute sessions werescheduled over a 10-week period. Participants wereasked to review and discuss materials and completeworksheets between sessions. Post-treatment datawas collected following completion of the fifthsession. Three month follow-up data was collected10–14 weeks following the last session.
Data analysis
Descriptive statistics including means, standarddeviations and proportions were computed forvariables relating to injury and caregiver character-istics. Means and standard errors were calculated forthe five outcome measures. Repeated measuresmixed models were used to model the means ofeach outcome measure over time. For all models, anautoregressive variance–covariance structure waschosen to model the correlations in observationsover time within subjects. Models for measures withmultiple scales (e.g. BSI, FNQ) also utilized anunstructured variance–covariance structure toaccount for the correlation between scales.
The initial models for each outcome measure wereexamined to determine if there were changes inscores over time without adjusting for covariates.When there was evidence of at least a marginalamount of change in scores (p-value< 0.20), anadjusted model was fit to more accurately model themeans. The variables considered for adjustmentincluded caregiver characteristics such as relationto survivor (spouse, parent, other), age, gender,ethnicity (minority, non-minority) and marital status(married/cohabitating, not married) and survivorcharacteristics including age and acute care lengthof stay. The adjusted models were initially fit in aforward stepwise fashion, entering covariates with
p< 0.2. Interactions between evaluation interval,scales and each covariate were considered to deter-mine if the changes over time varied in relation todemographic and injury characteristics. Insignificantcovariates and interaction effects were subsequentlyremoved if p� 0.05. To control the type I error rate,Bonferroni adjustments for multiple comparisonswere utilized.
An alternative to MANOVA, mixed-effectsmodels have the advantage of accounting forcorrelated data by assuming specific variance–covar-iance structures. The mixed-effects model also hasthe advantage of simultaneously modelling, withineach subject, correlations in measures across time aswell as across scales. Participants with missing datacan be examined and need not be excluded fromanalysis. Furthermore, modelling more data togetherincreases statistical power and decreases standarderrors of estimates.
Results
Family needs
Means and standard errors for the six FNQ scalesare detailed in Table V. A single repeated measuresmixed model was used to model the six FNQ scalesover time, assuming an autoregressive structureacross the visits and an unstructured structureacross the domains. Changes in the FNQ over timewere not significantly different across the six scales(p¼ 0.4913). Regardless of scale, scores changedsignificantly over time (F(2, 81)¼ 8.97, p¼ 0.0003).Using a Bonferroni correction (�¼ 0.0083) for post-hoc comparisons, significant increases in met needsover time were evident for Health Information
Table V. Means and standard errors for outcome measures before and after treatment.
MeasurePre-treatment
Mean (SE)Post-treatment
Mean (SE)3 Month follow-up
Mean (SE)
Family Needs Questionnaire*Health Information 5.25 (0.43) 7.09 (0.44) 7.63 (0.50)Emotional Support 3.72 (0.47) 5.31 (0.47) 5.32 (0.54)Instrumental Support 3.40 (0.51) 4.75 (0.51) 4.90 (0.59)Professional Support 3.55 (0.51) 5.72 (0.52) 6.25 (0.59)Community Support 3.75 (0.49) 4.80 (0.49) 5.81 (0.56)Care Involvement 5.09 (0.58) 6.58 (0.58) 7.64 (0.67)
Family Assessment Device 23.71 (0.85) 23.83 (0.87) 23.59 (0.95)Service Obstacles Scale 14.60 (0.73) 12.26 (0.77) 10.30 (0.87)Brief Symptom Inventory-18
Somatic 51.82 (1.40) 51.71 (1.44) 51.69 (1.62)Depression 54.19 (1.35) 51.10 (1.38) 53.40 (1.56)Anxiety 54.61 (1.32) 52.15 (1.35) 53.24 (1.52)Global Severity Index 54.65 (1.37) 52.14 (1.41) 53.48 (1.59)
Satisfaction with Life Scale 21.45 (1.06) 22.29 (1.06) 21.45 (1.13)
*FNQ scale score values were transformed to a 10-point scale.
Family intervention after brain injury 541
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
(p¼0.0002), Professional Support (p¼ 0.0002) andCare Involvement (p¼ 0.0083) needs, but not forEmotional Support (p¼ 0.0104), InstrumentalSupport (p¼ 0.0506) or Community Support(p¼0.0147).
Subsequently, an adjusted model was fit thatincluded main effects for time (F(2, 78)¼ 9.05,p¼ 0.0003), FNQ scale (F(5, 240)¼ 12.71,p< 0.0001), caregiver marital status (F(1, 46)¼12.11, p¼ 0.0011) and acute LOS (F(1, 46¼ 7.52,p¼ 0.0087), as well as an interaction effect for timeby domain (F(10, 379)¼ 1.06, p¼ 0.3941). Afteradjusting for caregiver marital status and acute LOS,the FNQ changes over time were not significantlydifferent among the six scales. All six FNQ scalesshowed significant changes over time.
Using a Bonferroni correction (�¼0.0083) forpost-hoc comparisons, changes over time weresignificant for the Health Information (p¼ 0.0002),Emotional Support (p¼0.0069), ProfessionalSupport (p¼ 0.0002) and Care Involvement(p¼0.0083) scales. Significant changes were notobserved for the Instrumental Support (p¼ 0.1336)or Community Support (p¼ 0.0171) scales.
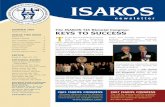
For the Health Information, Emotional Support,Professional Support and Care Involvement scales,changes over time were further examined using aBonferroni correction (�¼ 0.0167). As indicated inTable VI, significant pre- to post-treatment increaseswere identified for Health Information, EmotionalSupport and Professional Support needs, but not forCare Involvement. Comparisons between pre-treat-ment and 3 month follow-up data revealed signifi-cant increases for the four scales. The data presentedin Figure 1 provides evidence that treatment benefitsmay continue to accrue for several months beyondcompletion of formal intervention. However,
analysis did not provide evidence of differencesbetween post-treatment and 3 month follow-upscores.
Regarding caregiver marital status, FNQ scoreswere significantly higher for married caregivers thannon-married caregivers by 2.253 units (95%CI¼ 0.950, 3.556), irrespective of scale or evalua-tion interval (i.e. pre-treatment, immediate post-treatment, 3 months follow-up). Additionally, a10-day increase in acute LOS was associated witha 0.38 unit decrease (95% CI¼ 0.10, 0.66) in FNQscore, irrespective of scale or evaluation interval.There was no evidence of interaction effects forFNQ scale, evaluation interval and the covariates(e.g. marital status, acute care LOS).
Family functioning
A single repeated measures mixed effects model wasused to model the FAD scores over time, assumingan autoregressive structure across the visits. Scoresdid not change significantly over time (F(2, 80)¼0.05, p¼ 0.9486). Means and standard errors arepresented in Table V. Since there was not evidenceof changes in family functioning over time(p¼ 0.9486> 0.20), an adjusted model was not fit.
Service obstacles
A single repeated measures mixed effects model wasused to model the total SOS scores over time,assuming an autoregressive structure across thevisits. Scores changed significantly over time (F(2,78)¼ 8.58, p¼ 0.0004). Mean values and standarderrors are presented in Table V. Using a Bonferronicorrection (�¼0.0167) for post-hoc comparisons,significant pre- to post-treatment (p¼0.0062) andpre-treatment to 3 month follow-up (p¼0.0001)
Table VI. Adjusted FNQ score increases: mean, standard error, 95% confidence intervals and associated p-values.
Mean increase SE 95% CI p-value
Health informationPre–post-treatment 1.743 0.490 (0.842, 2.878) 0.0004Post–3 month follow-up 0.523 0.535 (�0.568, 1.698) 0.3286Pre–3 month follow-up 2.267 0.596 (1.184, 3.665) 0.0002
Emotional supportPre–post-treatment 1.611 0.543 (0.585, 2.612) 0.0032Post–3 month follow-up 0.063 0.592 (�1.078, 1.175) 0.9156Pre–3 month follow-up 1.674 0.660 (0.414, 2.881) 0.0116
Professional supportPre–post-treatment 2.106 0.591 (1.006, 3.327) 0.0004Post–3 month follow-up 0.562 0.645 (�0.769, 1.816) 0.3844Pre–3 month follow-up 2.668 0.717 (1.279, 4.101) 0.0002
Care involvementPre–post-treatment 1.431 0.675 (0.157, 2.842) 0.0346Post–3 month follow-up 1.087 0.736 (�0.436, 2.550) 0.1403Pre–3 month follow-up 2.519 0.823 (0.918, 4.195) 0.0024
542 J. S. Kreutzer et al.
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
decreases were identified. The post-treatment to3 month follow-up (p¼ 0.0428) decrease wasnominal.
With evidence of significant SOS changes overtime, an adjusted model was built to account forcaregiver and survivor characteristics. The modelincluded main effects for time (F(2, 74)¼ 10.26,p¼ 0.0001), acute LOS (F(1, 74)¼1.87,p¼ 0.1779) and the interaction effect (F(2,74)¼3.55, p¼ 0.0338). Table VII provides infor-mation regarding the interaction between evaluationinterval and acute LOS. Comparisons are made atfirst (i.e. 1 day) and third (i.e. 19 days) quartileLOS values. In comparison to family members ofparticipants with longer lengths of stay, familymembers of participants with shorter stays showedgreater improvements pre- to post-intervention andpre-intervention to 3 month follow-up.
Family members’ distress and life satisfaction
Means and standard errors for BSI-18 scales areprovided in Table V. A single repeated measures
mixed model was used to model the four BSI-18scales over time, assuming an autoregressive struc-ture across evaluation intervals and an unstructuredstructure across the scales. Analysis indicatedthat BSI-18 scale scores did not change significantlyover time, (F(2, 81)¼ 1.49, p¼0.2318) and therewere no significant differences between scales(F(6, 243)¼ 1.25, p¼ 0.2792). Since there was notevidence that the BSI changed significantly over time(p¼ 0.2318> 0.20), an adjusted model was not fit.
A single repeated measures mixed model was usedto model the caregiver SWLS scores over time,assuming an autoregressive structure across thevisits. Caregiver SWLS scores did not changesignificantly over time (F(2, 82)¼ 1.33,p¼ 0.2694). Means and standard errors are providedin Table V.
Discussion
Family intervention researchers have examined dif-ferent types of outcomes, yet most studies have notyielded evidence of treatment benefits. Investigationsof benefits to psychological distress, problem-solvingand burden have generated equivocal findings[61, 63–67]. No investigators have identified signif-icant improvements in post-intervention familyfunctioning, life satisfaction, coping or self-esteem[61, 64, 67, 68]. On a positive note, familyparticipants in the present investigation showed agreater number of met family needs and perceivedfewer obstacles to obtaining services following theBIFI. Post-hoc analyses suggested that treatmentbenefits continued to accrue for at least 3 monthsbeyond the cessation of treatment. These findingsare unique in that other researchers have notexamined how intervention affects family needs orperceptions of access to services.
The present investigation was also unique in usingcovariance analyses to identify factors that influ-enced treatment. There was no indication thatcaregivers’ relationship to survivor, gender, age orethnicity related to treatment. Nor was there evi-dence that survivors’ age influenced treatment out-come. On the other hand, caregivers’ marital statusand survivors’ length of hospitalization were identi-fied as significant covariates. With regard to maritalstatus, married caregivers reported more met needsthan unmarried caregivers. The higher rate of metneeds was evident before and after treatment.With regard to length of stay, caregivers of survivorswith longer hospitalizations reported fewer metneeds. Researchers have only begun to examine theimpact of brain injury on marriages and factors thatinfluence marital stability. Findings from thepresent investigation suggest that marriage providesimportant supports for caregivers. With regard to
Table VII. Adjusted SOS score decreases by acute care length ofstay: mean, standard error, 95% confidence intervals andassociated p-values.
Meandecrease SE 95% CI p-value**
1 day acute care*Pre–post-treatment 4.02 1.04 (1.95, 6.09) 0.0002Post–3 month follow-up 1.36 1.16 (�0.96, 3.68) 0.2455Pre–3 month follow-up 5.38 1.32 (2.76, 8.03) 0.0001
19 days acute care*Pre–post-treatment 1.87 0.86 (0.16, 3.59) 0.0325Post–3 month follow-up 1.91 0.95 (0.01, 3.81) 0.0487Pre–3 month follow-up 3.78 1.08 (1.63, 5.93) 0.0008
*1 and 19 day length of stay values correspond to 1st and 3rdquartiles.**post hoc comparisons are made in reference to a Bonferronicorrection (�¼ 0.0083).
0
0.5
1
1.5
2
2.5
3
HealthInformation
EmotionalSupport
InstrumentalSupport
ProfessionalSupport
CommunitySupport
CareInvolvement
Pre-Post Post-3 Months
Mea
n In
crea
se
Figure 1. Mean post-treatment changes in met needs.
Family intervention after brain injury 543
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
perceived obstacles to receiving services, survivors’acute care length of stay was the only significantcovariate. Families of survivors with longer hospital-ization lengths reported more obstacles to receivingservices. The findings for marital status and serviceaccessibility are not surprising and they fit with thenotion that adjustment is more difficult for unmar-ried persons and caregivers of survivors with moresevere injury. Clearly these findings should beviewed as preliminary and more research is neededto delineate factors influencing treatment success.
The present investigation also examined post-treatment changes in psychological distress, familyfunctioning and life satisfaction. Among the sevenprevious family intervention studies reviewed, onlyBrown et al. [64] examined impact on familyfunctioning. As in the present investigation, Brownet al. utilized the Family Assessment Device andsignificant treatment effects were not observed.Acorn [68] used the Life Satisfaction Index [69]and Rivera [61] used the Satisfaction with Life Scale(SWLS [43]) to measure caregivers’ satisfaction withlife. As in Rivera’s investigation, the present inves-tigation also utilized the SWLS. Non-significantfindings were reported in all three investigations.
A majority of family intervention studies haveincluded a psychological support component andfindings have been equivocal. Brown et al. [64] andRivera et al. [61] identified treatment-related psy-chological distress reductions. Brown et al. reliedupon the Profile of Mood States [70] and Riveraet al.’s participants completed the CES-D [71].As reported by Morris [65], Carnevale et al. [66] andSinnakaruppan et al. [67], the present investigationdid not identify treatment-related reductions indistress. Morris and Sinnakaruppan et al. bothutilized the HADS to measure distress. Differentialfindings regarding psychological distress seem unre-lated to intervention delivery method, recipient orpurpose. Instead, differential findings may be attrib-utable to the differential sensitivity of outcomemeasures. Equivocal findings may also indicate thatsmaller samples did not provide sufficient statisticalpower. The samples used by Brown et al. (n¼91)and Rivera et al. (n¼ 67) were larger than those in allthe other investigations.
In fact, sample size may be one of the salientfactors distinguishing studies that have showntreatment-related benefits from those that have not.The four studies [65–68] with the smallest samplesizes showed no treatment benefit. Sample sizesranged from 19–41. Including the present investiga-tion, the four studies with greater than 50 partici-pants provided evidence of treatment-relatedbenefits [61, 63, 64].
Unfortunately, comparing the benefits of differentinterventions has been difficult because
methodologies vary widely. Some have providedtreatment to groups while others have providedindividual treatment. In some cases treatment hasbeen delivered by telephone and in other cases inperson. Standardization of treatment has beendifficult, with most providers not relying on atreatment manual. Treatment has been provided inhospitals, homes, clinics and other community-basedsettings. Some interventions have included survivors,though most have not. There has been great vari-ability in the frequency and duration of treatment,with some investigators delivering treatment for lessthan 1 month and others for over 1 year. Finally,interventions have been developed for varyingpurposes. Most investigators have included a psy-chological support component and an educationalcomponent. A relatively small number have focusedon skill building. The present investigation is the firstto incorporate all three components, education,psychological support and skill building.
Investigations have also utilized widely varyingoutcome measures, even when measuring the sameconstruct. Variation in measures utilized to quantifypsychological distress and coping are most impress-ive. For example, two investigators examined care-givers’ coping [67, 68] and each relied on a differentmeasure. The Satisfaction With Life Scale, FamilyAssessment Device, HADS and the Rosenberg Self-Esteem Scale were each used in two research studies.Unfortunately, no measures have been used in morethan two studies.
The findings of the present investigation must beinterpreted within the context of several method-ological limitations. First, a control group was notutilized, leaving questions about factors underlyingtreatment benefits. Self-report measures were uti-lized and outcome data was not derived fromstandardized observational methods or interviews.Some might suggest that a combination of observa-tional and self-report measures is optimal. Thesample was relatively small, raising questions aboutstatistical power and representativeness. Data wascollected at a single centre, perhaps adding toquestions about generalization from findings.Treatment spanned five sessions over a 10-weekperiod, leaving uncertainties about optimal treat-ment intensity, duration and frequency. The dataprovided support for the durability of treatmenteffects, but there are questions about durabilitybeyond 3 month follow-up.
Without a doubt additional research is needed.Ideally, future studies should include a combinationof well-validated measures, especially toolsdeveloped for brain injury populations and shownto be treatment sensitive. Inclusion of a control groupwill enable researchers to draw firmer conclusionsabout factors underlying treatment benefits. Wait-list
544 J. S. Kreutzer et al.
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
controls may be preferred to no-treatment controlsbecause of ethical concerns about withholding treat-ment entirely. Multi-centre studies with larger sam-ples will increase statistical sensitivity and reduce thelikelihood of Type II error. Comparing treatmentswith varying frequency and duration and includinglonger-term follow-up will help ascertain the idealtreatment regimen and the longevity of treatmentbenefits. Finally, the present investigation focused ondata derived from caregivers. More research isneeded to identify the benefits of the BIFI andother treatments for survivors.
In conclusion, analysis of data derived from thepresent investigation provides evidence that a man-ualized intervention which includes education,skill building and psychological support componentshas benefits for family members in a post-acutesetting. Caregivers of persons with more severeinjuries, as measured by hospital length of stay,reported more unmet needs and perceived moreobstacles to receiving services before and after injury.However, analysis indicated similar interventionbenefits for families regardless of injury severity.The quantitative data was complemented by quali-tative data, indicating that the intervention helpedfamily members learn about the nature of injury,improve communication and enhance problem-sol-ving skills. Many family members also reported thatthe BIFI helped them recognize how the injury hadaffected them personally and the family as a whole. Infact, 100% of family members reported that theywould recommend the programme to others.The literature clearly provides evidence that familymembers have a critical role in survivors’ rehabilita-tion, yet they are adversely impacted as well.The present investigation provides evidence that theBIFI effectively addresses family members’ needs,alleviates obstacles to receiving services and has apositive impact on family members’ lives.
Acknowledgement
Supported by grants H133A070036 andH133P040006 from the National Institute onDisability and Rehabilitation Research, UnitedStates Department of Education.
Declaration of interest: The authors reportno conflicts of interest. The authors alone areresponsible for the content and writing of the paper.
References
1. Kreutzer JS, Kolakowsky-Hayner SA, Ripley D, Cifu DX,Rosenthal M, Bushnik T, Zafonte R, Englander J, High W.Charges and lengths of stay for acute and inpatient rehabili-tation treatment of traumatic brain injury 1990–1996. BrainInjury 2001;15:763–774.
2. Harrison-Felix C, Newton CN, Hall KM, Kreutzer JS.Descriptive findings from the Traumatic Brain Injury ModelSystems National Database. Journal of Head TraumaRehabilitation 1996;11:1–14.
3. Chesnut RM, Carney N, Maynard H, Mann NC. Summaryreport: evidence for the effectiveness of rehabilitation forpersons with traumatic brain injury. Journal of Head TraumaRehabilitation 1999;14:176–188.
4. Gillen R, Tennen H, Affleck G, Steinpreis R. Distress,depressive symptoms, and depressive disorder among care-givers of patients with brain injury. Journal of Head TraumaRehabilitation 1998;13:31.
5. Hall KM, Karzmark P, Stevens M, Englander J, O’Hare P,Wright J. Family stressors in traumatic brain injury: a two-year follow-up. Archives of Physical Medicine andRehabilitation 1994;75:876–884.
6. Jacobs HE. The Los Angeles Head Injury Survey: proceduresand initial findings. Archives of Physical Medicine andRehabilitation 1988;69:425–431.
7. Testa JA, Malec JF, Moessner AM, Brown AW.Predicting family functioning after TBI: impact of neurobe-havioral factors. Journal of Head Trauma Rehabilitation2006;21:236.
8. Oddy M, Herbert C. Intervention with families followingbrain injury: evidence-based practice. NeuropsychologyRehabilitation 2003;13:259–273.
9. Brooks DN. The head-injured family. Journal of Clinical andExperimental Neuropsychology 1991;13:155–188.
10. Carnes SL, Quinn WH. Family adaptation to brain injury:coping and psychological distress. Family Systems andHealth 2005;23:186–203.
11. Livingston MG, Brooks DN, Bond MR. Patient outcome inthe year following severe head injury and relatives’ psychiatricand social functioning. Journal of Neurology, Neurosurgeryand Psychiatry 1985;48:876–881.
12. Livingston MG, Brooks DN, Bond MR. Three months aftersevere head injury: psychiatric and social impact on relatives.Journal of Neurology, Neurosurgery and Psychiatry 1985;48:870–875.
13. Marsh NV, Kersel DA, Havill JH, Sleigh JW. Caregiverburden at 6 months following severe traumatic brain injury.Brain Injury 1998;12:225.
14. Marsh NV, Kersel DA, Havill JH, Sleigh JW. Caregiverburden at 1 year following severe traumatic brain injury.Brain Injury 1998;12:1045–1059.
15. Mauss-Clum N, Ryan M. Brain injury and the family. Journalof Neurosurgery Nursing 1981;13:165–169.
16. Perlesz A, Kinsella G, Crowe S. Psychological distress andfamily satisfaction following traumatic brain injury:injured individuals and their primary, secondary, and tertiarycarers. Journal of Head Trauma Rehabilitation 2000;15:909–929.
17. Riley GA. Stress and depression in family carersfollowing traumatic brain injury: the influence of beliefsabout difficult behaviours. Clinical Rehabilitation 2007;21:82–88.
18. Kreutzer JS, Gervasio AH, Camplair PS. Patient correlates ofcaregivers’ distress and family functioning after traumaticbrain injury. Brain Injury 1994;8:211–230.
19. Groom KN, Shaw TG, O’Connor ME, Howard NI,Pickens A. Neurobehavioral symptoms and family function-ing in traumatically brain-injured adults. Archives of ClinicalNeuropsychology 1998;13:695–711.
20. Anderson MI, Parmenter TR, Mok M. The relationshipbetween neurobehavioural problems of severe traumaticbrain injury (TBI), family functioning and the psychologicalwell being of the spouse/caregiver: path model analysis. BrainInjury 2002;16:743.
Family intervention after brain injury 545
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
21. Curtiss G, Klemz S, Vanderploeg RD. Acute impact of severetraumatic brain injury on family structure and copingresponses. Journal of Head Trauma Rehabilitation 2000;15:1113.
22. Kreutzer JS, Serio C, Bergquist S. Family needs followingbrain injury: a quantitative analysis. Journal of Head TraumaRehabilitation 1994;9:104–115.
23. Sinnakaruppan I, Williams DM. Family carers and the adulthead-injured: a critical review of carers’ needs. Brain Injury2001;15:653–672.
24. Leith KH, Phillips L, Sample PL. Exploring the service needsand experiences of persons with TBI and their families: theSouth Carolina experience. Brain Injury 2004;18:1191–1208.
25. Rotondi AJ, Sinkule J, Balzer K, Harris J, Moldovan R. Aqualitative needs assessment of persons who have experi-enced traumatic brain injury and their primary familycaregivers. Journal of Head Trauma Rehabilitation 2007;22:14–25.
26. Kolakowsky-Hayner SA, Miner KD, Kreutzer JS. Long-termlife quality and family needs after traumatic brain injury.Journal of Head Trauma Rehabilitation 2001;16:374–385.
27. Pickelsimer EE, Selassie AW, Sample PL, A WH, Gu JK,Veldheer LC. Unmet service needs of persons with traumaticbrain injury. Journal of Head Trauma Rehabilitation2007;22:1–13.
28. Gordon WA, Zafonte R, Cicerone K, Cantor J, Brown M,Lombard L, Goldsmith R, Chandna T. Traumatic braininjury rehabilitation: state of the science. American Journal ofPhysical Medicine and Rehabilitation 2006;85:343–382.
29. Ragnarsson KT. Traumatic brain injury research since the1998 NIH Consensus Conference: accomplishments andunmet goals. Journal of Head Trauma Rehabilitation2006;21:379–387.
30. Boschen K, Gargaro J, Gan C, Gerber G, Brandys C. Familyinterventions after acquired brain injury and other chronicconditions: a critical appraisal of the quality of the evidence.NeuroRehabilitation 2007;22:19–41.
31. Kreutzer JS, Kolakowsky-Hayner SA, Demm SR,Meade MA. A structured approach to family interventionafter brain injury. Journal of Head Trauma Rehabilitation2002;17:349–367.
32. Kreutzer JS, Taylor LA. Brain injury family interventionmanual. Richmond, VA: National Resource Center forTraumatic Brain Injury; 2004.
33. Kreutzer JS, Kolakowsky-Hayner SA. Getting better (andbetter) after brain injury: a guide for family, friends, andcaregivers. Richmond, VA: The National Resource Centerfor Traumatic Brain Injury; 1999.
34. Bertalanffy LV. General system theory: Foundationsdevelopment, applications. New York: George Braziller;1968.
35. Nichols MP, Schwartz RC. 6th ed. Family therapy conceptsand methods. 6th ed. Boston, MA: Pearson Education: Inc.;2004.
36. Gan C, Campbell KA, Gemeinhardt M, McFadden GT.Predictors of family system functioning after brain injury.Brain Injury 2006;20:587–600.
37. Cavallo MM, Kay T. The family system. In: Silver JM,McAllister TW, Yudofsky SC, editors. Textbook of traumaticbrain injury. Washington, DC: American PsychiatricPublishing, Inc; 2005. pp 533–558.
38. Ellis A. A new guide to rational living. Englewood Cliffs:Prentice Hall; 1975.
39. Epstein NB, Baucom DH. Enhanced cognitive-behaviortherapy for couples. Washington, DC: AmericanPsychological Association; 2002.
40. Mateer CA, Sira CS, O’Connell ME. Putting HumptyDumpty together again: the importance of integrating cogni-tive and emotional interventions. Journal of Head TraumaRehabilitation 2005;20:62–75.
41. Mateer CA, Sira CS. Cognitive and emotional consequencesof TBI: intervention strategies for vocational rehabilitation.NeuroRehabilitation 2006;21:315–326.
42. Hodgson J, McDonald S, Tate R, Gertler P. A randomizedcontrolled trial of a cognitive-behavioural therapy programfor managing social anxiety after acquired brain injury. BrainImpairment 2005;6:169–180.
43. Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfactionwith life scale. Journal of Personal Assessment 1985;49:71.
44. Murray HM, Maslany GW, Jeffery B. Assessment of familyneeds following acquired brain injury in Saskatchewan. BrainInjury 2006;20:575–585.
45. Kim JW, Moon SS. Needs of family caregivers caring forstroke patients: based on the rehabilitation treatment phaseand the treatment setting. Social Work and Health Care2007;45:81–97.
46. Hauber RP, Jones ML. Telerehabilitation support for familiesat home caring for individuals in prolonged states of reducedconsciousness. Journal of Head Trauma Rehabilitation2002;17:535–541.
47. Moules S, Chandler BJ. A study of the health and socialneeds of carers of traumatically brain injured individualsserved by one community rehabilitation team. Brain Injury1999;13:983.
48. Kreutzer JS. Family Needs Questionnaire. Richmond, VA:Rehabilitation Research and Training Center onSevere Traumatic Brain Injury, Medical College of Virginia;1998.
49. Serio CD, Kreutzer JS, Witol AD. Family needs aftertraumatic brain injury: a factor analytic study of the FamilyNeeds Questionnaire. Brain Injury 1997;11:1–9.
50. Marwitz JH, Kreutzer JS. The Service Obstacles Scale (SOS).Richmond, VA: Medical College of Virginia, VirginiaCommonwealth University; 1996.
51. Kolakowsky-Hayner SA, Kreutzer JS, Miner KD.Validation of the Service Obstacles Scale for the traumaticbrain injury population. NeuroRehabilitation 2000;14:151–158.
52. Kabacoff R, Miller I, Bishop D, Epstein N, Keitner G. Apsychometric study of the McMaster family assessmentdevice in psychiatric, medical, and nonclinical samples.Journal of Family Psychology 1990;3:431–439.
53. Miller I, Epstein N, Bishop D, Keitner G. The McMasterFamily Assessment Device: reliability and validity. Journal ofMarital and Family Therapy 1985;11:345–356.
54. Malec JF, Testa JA, Rush BK, Brown AW, Moessner AM.Self-assessment of impairment, impaired self-awareness, anddepression after traumatic brain injury. Journal of HeadTrauma Rehabilitation 2007;22:156–166.
55. Ponsford J, Olver J, Ponsford M, Nelms R. Long-termadjustment of families following traumatic brain injury wherecomprehensive rehabilitation has been provided. Brain Injury2003;17:453–568.
56. Sherer M, Evans CC, Leverenz J, Stouter J, Irby JW,Lee JE, Yablon SA. Therapeutic alliance in post-acutebrain injury rehabilitation: predictors of strength of allianceand impact of alliance on outcome. Brain Injury 2007;21:663–672.
57. Derogatis LR. BSI 18. Brief Symptom Inventory 18.Minneapolis, MN: NCS Pearson; 2000.
58. Hart T, O’Neil-Pirozzi TM, Williams KD, Rapport LJ,Hammond F, Kreutzer J. Racial differences incaregiving patterns, caregiver emotional function, and
546 J. S. Kreutzer et al.
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.
sources of emotional support following traumatic braininjury. Journal of Head Trauma Rehabilitation 2007;22:122–131.
59. Kreutzer JS, Gervasio AH, Camplair PS. Primary caregivers’psychological status and family functioning after traumaticbrain injury. Brain Injury 1994;8:197–210.
60. Meachen SJ, Hanks RA, Millis SR, Rapport LJ. Thereliability and validity of the brief symptom inventory-18in persons with traumatic brain injury. Archives ofPhysical Medicine and Rehabilitation 2008;89:958–965.
61. Rivera PA, Elliott TR, Berry JW, Grant JS. Problem-solvingtraining for family caregivers of persons with traumaticbrain injuries: a randomized controlled trial. Archivesof Physical Medicine and Rehabilitation 2008;89:931–941.
62. Pavot W, Diener E, Colvin CR, Sandvik E. Further valida-tion of the Satisfaction with Life Scale: evidence for the cross-method convergence of well-being measures. Journal ofPersonal Assessment 1991;57:149–161.
63. Albert SM, Im A, Brenner L, Smith M, Waxman R. Effect ofa social work liaison program on family caregivers to peoplewith brain injury. Journal of Head Trauma Rehabilitation2002;17:175–189.
64. Brown R, Pain K, Berwald C, Hirschi P, Delhanty R,Miller H. Distant education and caregiver support groups:comparison of traditional and telephone groups. Journal ofHead Trauma Rehabilitation 1999;14:257–268.
65. Morris KC. Psychological distress in carers of head injuredindividuals: the provision of written information. Brain Injury2001;15:239.
66. Carnevale GJ, Anselmi V, Busichio K, Millis SR. Changes inratings of caregiver burden following a community-basedbehavior management program for persons with traumaticbrain injury. Journal of Head Trauma Rehabilitation2002;17:83.
67. Sinnakaruppan I, Downey B, Morrison S. Head injury andfamily carers: a pilot study to investigate an innovativecommunity-based educational programme for family carersand patients. Brain Injury 2005;19:283.
68. Acorn S. Assisting families of head-injured survivors througha family support programme. Journal of Advanced Nursing1995;21:872–877.
69. Wood V, Wylie ML, Sheafor B. An analysis of ashort self-report measure of life satisfaction: correlationwith rater judgments. Journal of Gerontology 1969;24:465–469.
70. McNair DM, Lorr M, Droppleman LF. Profile ofmood states. San Diego, CA: Educational and IndustrialTesting Service; 1971.
71. Weissman MM, Sholomskas D, Pottenger M, Prusoff BA,Locke BZ. Assessing depressive symptoms in five psychiatricpopulations: a validation study. American Journal ofEpidemiology 1977;106:203–214.
Family intervention after brain injury 547
Bra
in I
nj D
ownl
oade
d fr
om in
form
ahea
lthca
re.c
om b
y V
irgi
nia
Com
mon
wea
lth U
nive
rsity
on
03/0
8/15
For
pers
onal
use
onl
y.