Walking performance, medical outcomes and patient training in FES of innervated muscles for...
Transcript of Walking performance, medical outcomes and patient training in FES of innervated muscles for...
1 of 13
1
WALKING PERFORMANCE, MEDICAL OUTCOMES AND PATIENT
TRAINING IN FES OF ENERVATED MUSCLES FOR AMBULATION BY
THORACIC-LEVEL COMPLETE PARAPLEGICS
Daniel Graupe*, Humberto Cerrel-Bazo**, Helmut Kern*** and Ugo Carraro****
* University of Illinois, 851 South Morgan St., Room 1117, Chicago, IL 60607-7053 , USA, EMAIL:
**Scuola di Specialità in Medicina Fisica e Riabilitazione, Università di Verona, Borgo Roma, Verona, Italy,
EMAIL : [email protected]
***Ludwig Boltzmann Institute of Electrostimulation and Physical Rehabilitation, Department of Physical
Medicine, Wilhelminenspital. A-1171 Vienna, Austria, EMAIL: [email protected]
**** Laboratory of Translational Myology of the Interdepartmental Research Institute of Myology & C.N.R.
Institute of Neuroscience, University of Padua Medical School, Padova, Italy, EMAIL:. [email protected]
ABSTRACT
Below is a discussion of an FDA-approved noninvasive Functional Electrical Neuromuscular Stimulation (FES)
System for ambulation by traumatic T1 to T12 paraplegics having no sensation and no motor function below their
SCI lesion. The system’s ambulation training, its ambulation performance evaluation and its medical evaluation
are summarized. Light microscopy muscle morphometry is included to explain ambulation performance based on
sound myology foundations of FES in enervated (upper motoneuron lesion) as compared with denervated (lower
motoneuron lesion) muscles.
KEY WORDS
FES (functional electrical stimulation), upper-motoneuron paraplegia, thoracic SCI, training, walking
performance, medical evaluation, myology, enervated muscle
2 of 13
2
1. INTRODUCTION:
The paper discusses ambulation training and
performance and medical outcomes via transcutaneous
FES using the PARASTEP FES system for ambulation
by thoracic-level paraplegics with traumatic complete
upper-motoneuron lesions of the spinal cord, namely
where stimulation is applied to peripheral nerves to
elicit motor function in enervated muscles. The FES
system considered is the Parastep system, presently the
only one approved by FDA1 , 1994 and approved by
US Medicare and Medicaid for reimbursement of
equipment cost and of training cost2, 2003. This FES
system (Graupe and Kohn3, 1994), which is shown to
trigger action potentials in the stimulated peripheral
nerves, allows paraplegics with traumatic complete
T1-T12 paraplegia (having no sensation or motor
function below the SCI lesion) and who are trained in
its used to walk short distances. Walking distances
vary with intensity of training protocol from an
average of 115 meters per walk after a 32-session 3
months training program (Klose et al.4, 1997) to 450
meters/walk average after a 4-months daily training
program (Cerrel-Bazoet al.5, 1997). The system allows
full patient independence in standing, walking, and in
donning/doffing the system.
Among the medical benefits beyond mobility, most
important is the improvement in blood flow at below
the lesion by 50%-60% average, to near normal pre-
injury levels.
The Parastep system is based on principles
stemming from Luigi Galvani’s work6 on exciting a
frog’s leg (1791). Noninvasive (transcutaneous)
functional electrical stimulation (FES, or FNS: functional
neuromuscular stimulation) of peripheral nerves for
eliciting function enervated muscles in humans was
reported in 1960 by Lieberson7 and was applied to
hemiplegic subject to correct heel-drop. Trascutaneous
FES stimulator of thoracic-level paraplegic patients was
first reported by Kralj et al8 (1980) to allow standing and
the taking a few steps. Graupe et al9, 10
have extended
Lieberson’s and Kralj’s earlier noninvasive FES systems
to a patient-borne patient-controlled FES system for
thoracic-level complete paraplegics (with upper
motoneuron paraplegia), aiming at maximizing patient’s
independence in ambulation and in the control of the
system (see Graupe, et al.9
1982 , Graupe and Kohn
10
1983) and designing the stimulation pulses and their
coordination and control accordingly. This design was
subsequently implemented in the (now commercially
available) Parastep system (Graupe and Kohn3 1994),
which is considered throughout this paper and is further
discussed in11
. Also, some modifications of this design
are considered.
Carraro12
, 2002 and Kern13
, 2005 have studied
extensively the myology of enervated and denervated
muscles and his results, which provide myological
understating of the long term performance of FES in
upper-motor-neuron paralysis and its applicability many
years post injury.
We note that parallel work on FES in upper-
motoneuron paralysis, based on implanted (invasive) FES
systems also began in the 1980’s, for the same purpose of
ambulation by thoracic-level paraplegics. The main
groups working on percutaneous (implanted) FES
systems were and still are those of Marsolais, et al.14
,
1983 and of Holle, et al.15
, 1984.
2. FES IN UPPER-MOTONEURON
PARALYSIS:
The FES Parastep system of Fig. 1, is limited
thoracic level paraplegics, to exclude patients with
lumbar-level lesions, namely, where the paralyzed
muscles are denervated. It also requires full upper-
extremity function to exclude patients with cervical-
level lesions. The system’s design is reported in detail
in Graupe and Kohn3 1994
and will therefore not be
repeated here. It employs 12 surface electrodes at 6 sites
(quadriceps, common peroneal nerve and paraspinals at
right and left side each). The stimulation signals to each
stimulation site are designed to maximize
standing/walking time, by proper selection of stimuli
generation, including coordination and synchronization of
signal amplitude variation over time and distribution
between stimulation sites, while using very short pulses
(individually adjustable, usually from 80 to 150
microseconds) and lowest possible pulse frequency and
amplitude. They are coordinated in time and amplitude
throughout stimulation by a microprocessor that resides
in the patient-borne system, in terms of 3 menus (stand,
right step, left step). These menus are selectable by a
single finger touch on a walker-mounted switch and the
full time-evolution of the stimuli throughout each menu
resides on the above microcomputer.
Walker-support, that usually carries only
approximately 5% of body weight, is required for
balance and for safe and independent stand-up and sit-
down. Furthermore, since the patients have no
sensation, the only information (but for visual) that
they have on their ground contact comes from
sensation of pressure through the walker on their arms.
Else they claim that they “feel like walking on air”.
3 of 13
3
Shoe-insert AFOs (ankle-foot orthoses) are useful for
providing ankle-foot stability. Since the system is noninvasive, patients may don
the system each morning and doff it in the evening.
Donning and doffing can be done by the patients
themselves without help and in short time (5-10 minutes
for donning, and 3-5 minutes for doffing).
2(a) Action Potential in the Stimulated Peripheral
Nerve
It is important to comment that FES
(transcutaneous or implanted) in upper-motoneuron
paralysis should only trigger action potential in the
stimulated peripheral nerve. This implies that the
stimulus should be of duration and level that suffice to
trigger an action potential (AP) that in turn, will travel
down the axon to the neuromuscular junction to
activate contraction in the neighboring enervated
muscle fibers. Fig. 1 shows the AP resulting from a
stimulation pulse measured at the quadriceps, as was
obtained from measuring the response-EMG at the
stimulation site with 3.75” x 1.75” surface electrodes.
We note that without FES there is no EMG at below
the SCI lesion and therefore any EMG at the
stimulated site is in response to FES. Furthermore,
with surface-FES all neurons that are being stimulated
respond simultaneously in a synchronized manner.
Hence, the APs at all the many hundreds of peripheral
neurons (that are affected by these quadriceps
electrodes) add-up to one strong signal, as in Fig. 1.
Note that the initial peak at the left-side of Fig. 1
(repeated after the flat section of the signal) is the
chopped artifact of the stimulus, while the far stronger
stimulus is gated off due its far higher (order of
hundreds) amplitude. Since with the progression of
muscle fatigue, many of the neurons that were
stimulated cease to fire, it was shown in Graupe and
Kohn3 that the level of the above response-EMG signal
goes down towards zero, the response-EMG has been
used in research versions of the Parastep to adjust
stimuli-level in order to recruit deeper neurons not
stimulated earlier in order to extend duration of
standing or of walking.
3. MYOLOGY OF THE ENERVATED MUSCLE
By means of needle biopsies of the vastus
lateralis muscle of long term enervated muscles of
thoracic-level complete paraplegics, we recently
showed that, after an initial period of rapid reduction
of muscle mass, the progression of atrophy is
extremely slow for many years (up to 20). After the
first few months in which muscle mass is well known
to decrease significantly; see: Scelsi et al. (1991)16
,
Lieber et al. (2004)17
, Kern et al. (2004)18
, the atrophy
reaches a steady state, that is likely maintained by the
residual spontaneous activity (spasms) of the lower
motor neuron that still innervates the myofibers. These
results are actually quite important for because they
suggest that, contrary to what described for lower
motor neuron lesion patients19
, 2004, severe atrophy
and degeneration of muscle tissue never occur in these
patients.
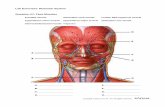
Figure 2.A, shows that in normal human
muscle the myofiber profiles are separated by minimal
interstitial tissue, fibers have a large diameter and
appear closely packed. In the long-term enervated
muscle (Fig. 2. B) the interstitial space between fibers
is slightly enlarged. Fiber size is more variable than in
normal muscle, with some fibers appearing unusually
large (asterisks) while a small percentage of them
present an extremely small diameter (pointed by
arrows). On the other hands, Fig. 2.C shows that the
muscle tissue is almost fully substituted by loose and
adipose connective tissue in the denervated
degenerated muscle of lower-motoneuron-lesioned
subjects. Indeed the long series of muscle biopsies of
the RISE trial allow to conclude that: (i) while human
skeletal muscles survive longer (years) than generally
accepted on the basis of experiments in rodents; see:
Kern et al. (2005)12
, Carraro20
2002, Midrio21
2005;
(ii) recovery to clinically significant muscle size and
function occurs in mid-term (3 to 5 years) lower motor
neuron SCI subjects (Carlson et al.19
2004, Carraro et
al.22
2005). However: (iii) starting FES within the first
year post-lesion results in a better recovery of muscle
function than when started many years after SCI
(Modlin et al.23
2005). Interestingly, the denervated
human muscle one-year after SCI appears much more
similar to that displayed in Fig. 2.B, than the expected
degenerated muscle of long term lower motoneuron
injured muscle (Figures 2.C and 2.F).
In conclusion, all together our morphometry findings
scientifically support the notion that also during the
late stage of upper motoneuron paraplegia there are no
upper-time limits to start successfully a training
program by Functional Electrical Stimulation of
enervated muscles.
In Figure 2, Myofiber profiles in normal
muscle (A) are separated by minimal interstitial tissue,
4 of 13
4
fibers have a large diameter and appear closely packed.
In the enervated muscle (B) the interstitial space
between fibers is slightly enlarged. Fiber size is more
variable with some fibers appearing unusually large
(asterisks) and a small percentage of them presenting
an extremely small diameters (pointed by arrows),
while in C the denervated muscle fibers are substituted
by adipocytes and loose connective tissue. Bars:
100µm. Tissue type morphometry: D, E, F. D, Normal
human muscle; E, Long-term enervated and F, Long-
term denervated paraplegics. The most significant
difference between normal (D), enervated (E) muscles
shows a slight increase (about 20%) in loose
connective tissue with a comparable loss of muscle
mass. On the other hand, the percentages of muscle
(15%) and connective tissue (85%, xx% of adipose
tissue included) are
reversed in the denervated muscle (F).
4. PATIENT TRAINING
Patient-training should start within a few years
after injury for best outcome. However, in one case, a
62-years old male T3/4 complete paraplegic, 40-years
post-injury, trained by one of the authors (DG), was
able to stand up (for approximately 2 minutes) within 6
minutes of start of training and to take his first 3 steps
3 days later24
. This outcome is not surprising in view
of the mycological discussion in Section 3 above.
The training preparatory to the use of the Parastep
system needs to contemplate the advent of derivative
factors resulting from the SCI, such as the consequent
rigidity, contracture, spasticity, metabolic fatigue (due
to lack of muscle force and endurance), energy
inefficiency, bad postural alignment, poor upper body
control and lack of motivation. All these factors may
be responsible, at least partly, from preventing SCI
subjects from the ability to properly stand and/or walk
under FES.
Generally speaking, traditional rehabilitation of
complete paraplegic subjects focuses on improving the
strength of the above-lesion muscles that are still under
voluntary control and on teaching living skills that will
lead to maximum self-sufficiency per level of injury.
Passive range of motion is given to the paralyzed
extremities with the objective of facilitating ADL
(activities of daily living) on a wheelchair but not with
the intent of achieving standing and/or walking. From
our experience with non-denervated or degenerated
paralyzed muscle, the time of acceptance to an FES
walking training program may be only limited by the
factors related to the non- inclusion criteria of the SCI
candidates (Chapter 6 in Graupe and Kohn3, Grraupe
and Kohn25
). It can be speculated that the earlier the
gait training is starthed (followowing the injury), the
better is the outcome of FES training. This rationale
may be supported in those cases in which spasticity,
rigidity and contractures can jeopardize the action of
achieving a proven ROM (range of motion) to achieve
standing. In any case, useful start of initiating a gait
training program preparatory for the use of the
Parastep walking system can be after medical
stabilization and up to 40 years post injury (see above
in this secction) if the SCI characteristics of these
subjects correspond to the inclusion criteria of the
Parastep program As an example in one case, a 62-
years old male (Chapter 6 in Graupe and Kohn3,
Graupe and Kohn25
).
On the basis of the experience of one of the
authors (HCB), it is recommended that prior to
entering a gait training program, and in order to
maximize walking performance of the Parastep users,
the patients become involved in a basic conditioning
program. This may consist in passive and active
ROM, standing, progressive upper body weight lifting,
and upper body cycle ergometry26,,27 to condition the
cardiovascular and respiratory systems to perform at
75 % of the maximum heart rate for 20-30 minutes.
All training participants must be evaluated for the
degree of rigidity, spasticity and spasms and treated
accordingly to facilitate for hip and knee full ROM and
to reach at least 90° degree of the ankle joint necessary
to stand and walk. Muscle force and endurance of the
paralyzed muscles are obtained through an active
physical training program. This program takes into
account the use of the FES computer-controlled
systems. Muscle force training for the Quadriceps,
Hamstrings and Gluteus muscles is developed through
FES-based muscle contraction against a gradual and
progressive increase of load appropriately selected on
an isokinetic chair (for exercising leg
extension/flexion, hip abduction/adduction and muscle
force exercise). The FES weight lifting program starts
at 0 Kg and is gradually progressed, if no sign of
fatigue are encounter, to reach up to 10-15 Kilograms
for the quadriceps and hamstring muscles, and as much
as 5-10 Kg for the gluteus muscles. The training
protocol is set to train the above-mentioned muscles up
to 30 minutes at least three times per week. Once the
SCI subjects achieve the set weight lifting goals for
muscle reinforcement, the subjects are ready to switch
5 of 13
5
to the muscle endurance training program. An FES
cycle ergometry program is used and SCI subjects are
trained for 30 minutes five times per week. Load
resistance is increased gradually, starting at 0
kilopound reaching 3 kilopound four to eight weeks
later28. This protocol of training has demonstrated to
be superior to ameliorate gait performance on SCI
subjects willing to stand and walk with the Parastep
system. Following this initial conditioning program
the standing and walking program is initiated. To achieve FES-based standing and/or walking in
SCI subjects, it is necessary to understand the
kinematics of standing or walking. This may differ for
different SCI subjects and it may be related to the level
of injury, residual locomotor force and to the non-
linear components above mentioned. As in any
training activity, lack of motivation may play an
important role. Kinematic considerations imply that
we must emphasize that the Parastep users are allowed
to stand and walk against gravity, due to both active
and passive forces provided by the FES system. This
system is compound of two elements; the first element
is a computerized electrical stimulator that delivers to
the lower extremities (lower trunk and paralyzed
muscles extremities) FES synthesized and coordinated
trains of electrical impulses to produce the muscle
contraction for “locking-in” the hip and knee for
stability and to relax other such muscles when needed
in a coordinated manner. FES muscle contractions
anchor the lower trunk and hip through artificial FES
muscle activity, decreasing C shape lumbar curvature
and improving stability. Other coordinated stimuli
simulate the common peroneal nerve to produce a
coordinated hip-flexion reflex to facilitate the swing
phase of the gait movement.. The second component is
the AFO which, through a ground reaction sub-patellar
push, generates passive forces making the foot-ankle
joint stable and contributes to “lock-in” the knee for
stability. As a whole, this neuroprosthesis prevents the
body from falling and facilitates a stepping pattern
through the peroneal reflex (lower extremity
synergistic flexor activity) as above.
Standing and walking training implies several
acquired skills of motor control and the integration of
the FES neuroprosthesis to the residual components of
voluntary motor control at above the level of injury
and to the derivative factors resulting from the SCI.
When first learning a new motor skill (like
standing and walking), movements may be slow,
vacillating and poorly coordinated. Each trail is an
attempt to achieve a target or a goal. At this stage,
learning relies heavily on feedback to control each
action. The unskilled performer pauses between
movement as visual information, above-lesion posture
information and ground-contact information obtained
through the arms while holding and leaning (even if
with only 3% to 5% of body weight) on the walker, are
absorbed and evaluated. Subsequently, the movement
is attempted again with a revised plan.. Eventually, the
sequencing and timing of the movement becomes
automated, shifting from direct visual control to a
more internalized form of control 29
.
The Vicenza gait-training procedure with the
Parastep system starts at the first achievement of the
upright position by neuro-modulating the FES currents
to useful lower-extremities muscle contraction and by
cuing the subjects for good postural alignment. This
postural behavior can also be helped through by using
mirror-feedback training. Gait training follows and
walking is allowed at first on a flat surface. In the
beginning, fuzzy behavior (slow, vacillating, and
poorly coordinated movements) is evidenced. Each
trail is an attempt to achieve a target or a goal of good
performance, until the learned movement becomes
smooth and coordinated, and requires little attention.
Learning this new behavior relies also in repetition
and, as such, treadmill training has allowed the SCI
subjects to repeat movement hundreds of times more
than on ground surface, thus improving performance
(see Tables 1 and 2).
5. RESULTS
Ambulation performance, concerning average
walking distances (meters-per-walk) were reported by
Klose et al.4 and by Cerrel-Bazo et al.
5 and are given in
Table 3 below. These relate to two different training
methods, one, at Vicenza, Italy of 4 months of daily
training5, including considerable muscle-strengthening
routines using treadmill exercises (see Fig. 3), the
second24
, at the University of Miami school of
Medicine, being of 11 weeks of training (3 one-hour
sessions per week). Medical and psychological evaluation results were
published in References 3, 11, 29, 30, 31, 32, 33 and are
summarized in Table 4 below. A 15 minute movie (T9
and T10 complete traumatic SCI paraplegics) is
accessible in Graupe34
.
6 of 13
6
6. STOCHASTIC MODULATION OF FES
PULSES TO REDUCE RATE OF FATIGUE
When considering future improvements in FES,
we briefly discuss one possible approach that should
be examined, as follows:
A study by Graupe et al.35
reports very
preliminary results (one patient only) of a 36.6%
reduction (+/- 10.2% at 95% confidence level ) in the
rate of muscle fatigue when the FES stimulation signal
undergoes a 12% stochastic modulation of the time of
arrival (frequency) of the stimuli at the quadriceps, as
shown in Table 5. Whereas many more tests are
needed before definite conclusions can be reached,
these results point to a possible and simple way to
reduce the rate of muscle fatigue and increase of
walking range in upper motoneuron paraplegia, thus
making FES more efficient. This may be worth
testing also when FES is employed in denervated
muscles.
The motivation for these tests is that it can be
observed36
that the natural rate of action potentials in
healthy individuals varies in what appears (to the
outside observer who has no access to the regulation
carried out in the CNS), to be random at about 10%-
20% around some average rate. Also, in the
mathematical analysis of nonlinear systems it is known
that stochastic modulation improves stability37
and it is
possible that the neuromuscular loops (which are
certainly highly nonlinear) “take advantage” of this
feature.
The results above were carried out by stimulating
the quadriceps of a complete T7 (traumatic) paraplegic
patient, while seated at a fixed (marked) position
repeatedly, over 25 test sessions, at an average inter-
pulse interval of 42 milliseconds (average 24 Hz) and
with stochastic modulation of 0, +/-5, +/-10 , +/-20
milliseconds. Time to fatigue was measured from start
of stimulation (Leg lifting) to when the heel touched
the floor. Stimulation level and all other parameter
were held constant and patient had no knowledge
which (if any) modulation was applied. There was a 5
minutes rest between each stimulation test and sessions
were held at same time each day, with approximately
10 stimulation runs, each of a different (randomly
selected) modulation unknown to the patient.
7. CONCLUSIONS
In this paper we described a non-invasive
FDA-approved readily available FES system for
ambulation by persons with complete thoracic-level
upper motoneuron SCI, together with a description of
the Vicenza procedure for patient- training when using
that system, with ambulation results and medical
outcomes and with the mycological foundations for its
performance even when training is started many years
after injury. We note that the very rigorous Vicenza
training procedure, results in average ambulation
distances of several hundreds of meters (aver 400 m.)
per walk, since it first monitors and treats the
derivative factors discussed in Sect. 4. It continues to
monitor address these factors throughout actual
training of standing/walking rather than concentrating
on muscle contraction force. The mycological tissue
slides that are shown (Section 3) serve to explain how
training can be initiated many years (40 years in one
case that is reported) post injury. The results indicate
that the Parastep FES system, which is presently also
approved for reimbursement of both equipment cost
and training cost by Medicare and Medicaid in the
USA, is not a futuristic or experimental system, but a
valid system to allow SCI patients with complete
lesions between T1 an T12 (no sensation and no motor
function below the lesion) for independent walking of
reasonable distances at reasonable though low speeds
(ave. 14.5 m/sec). Furthermore, cardiovascular
parameters are improved such that blood flow to the
lower extremities (which drops significantly after SCI
– by about 30% to 49%) is essentially restored to near
post-injury levels (ave. 56% increase).
The system can be donned by the patient without
assistance in 5 to 19 minutes and doffed without
assistance. in 3 to 5 minutes.
Concerning future possible improvements, we
discussed (Set. 2.a) the possibility of using response
EMG for automatic feedback to adjust stimulation
level with the progression of muscle fatigue, We also
outlined (Sect. 5) the possibility that stochastically
modulated stimulation signals may significantly
enhance performance. Whereas this possibility is
presently only confirmed in one patient (36.6%
improvement in time to fatigue) requires more study, it
is based on theoretical foundations and on parallelity to
rate of action potential in intact animal data . It should
also be noted that whereas our experiments employ
only stochastic rate modulation, stochastic amplitude
modulation and even stochastic pulse rate modulation
should also be investigated for the same purpose. If
confirmed, such stochastic modulation may have
benefit in other electrical stimulation applications, say,
7 of 13
7
to denervated muscles (with or without stem cell
implantation) and beyond.
A minor improvement that was recently designed
by one of the present authors (DG) involves wireless
(RF) links between walker and the body of the FES
unit, to avoid wiring between these components, to
further enhance patient independence.
REFERENCES
1. FDA approval P900038,
http://www.fda.gov/cdrh/pma94.html , April 20, 1994.
2. Centers for Medicare and Medicaid Centers (CMS), Code
K0600 (Parastep-I equipment acquisition), and Code 97116
(physical training services with Parastep-I),
http://www.cms.hhs.gov/coverage 2003.
3. Graupe D, Kohn KH, Functional Electrical Stimulation
for Ambulation by Paraplegics, Krieger Publishing Co.,
Malabar, FL, 1994.
4. Klose KJ, Jacobs PL, Broton J, Guest S, Needham-
Shopshire BM, Lebwohl N, Nash MS , Green BA, Arch.
Phys. Med. Rehab., 78:789-793, 1997
5. Cerrel-Bazo HA, Rizetto A, Pauletto D, Lucca L,
Caldana L, Session 91, Paper 66, Proc. Eighth World
Congress of the International Rehabilitation Medicine
Association, Kyoto, Japan, 1997.
[6. Galvani L, Commentary on the effects of Electricity on
Muscular Motion, Proc. Bologna Acad. And Inst. of
Sciences and Arts, 1791.
7. Lieberson WT, Holmquest HJ, Scott D, Arch. Phys.
Med. And Rehab., 42:101,1961.
8. Kralj, A, Bajd T, Turk R, Med. Prog. Technol., 7: 3,
1980.
9. Graupe D, Kralj A, Kohn K., Proc IFAC Symp.
Prosthet. Control, Columbus, OH, 1982.
10. Graupe D, Kohn, KH, Basseas S, Naccarato E., Proc.
IEEE Frontiers of Eng. & Comp. in Health Care, Columbus,
OH, 1983.
11. Graupe D, Transcutaneous FES for ambulation: The
Parastep system, Chapter 31 in: Biomedical Engineering
Foundations - The Biomedical Engineering Handbook,
Third Edition , Editor: J D Bronzino, CRC Press, Boca
Raton, FL, 2006
12. Kern H, Rossini K, Boncompagni S,Protasi F, Hofer C,
Modlin M, Long lasting muscle trophism in complete upper
motor neuron lesion paraplegia, Basic Appl. Myology, 191-
201, 2005.
13. Marsolais E, Kobetic R, Clin. Orthop., 175:30-36, 1983.
14. Holle J, Frey M, Gruber H, Stohr H, Thoma H,
Orthopedics, 84:145-160, 1984.
15. Lotta S, Scelsi R, Alfonsi E, Saitta A, Nicolotti D,
Epifani P, Carraro U. Morphometric and neurophysiological
analysis of skeletal muscle in paraplegic patients with
traumatic cord lesion, Paraplegia; 29(4):247-252, 1991.
16. Scelsi R. Skeletal muscle pathology after spinal cord
injury. Our 20-year experience and results on skeletal
muscle changes in paraplegics, related to functional
rehabilitation. Basic Appl Myol.; 11 (2): 75-86, 2001.
17. Lieber RL, Steinman S, Barash IA, Chambers H.
Structural and functional changes in spastic skeletal muscle.
Muscle Nerve; 29: 615-627, 2004.
18. Kern H, Boncompagni S, Rossini K, Mayr W, Fanò G,.
Zanin ME, Podhorska-Okolow M, Protasi F, Carraro U.
Long-term denervation in humans causes degeneration of
both contractile and excitation-contraction coupling
apparatus that can be reversed by functional electrical
stimulation (FES). A role for myofiber regeneration? J.
Neuropath. Exp. Neurol.; 63:919-931, 2004.
19. Carlson MC, Borisov AB, Dedkov EI, Dow D,
Kostrominov TY. The biology and restorative capacity of
long-term denervated skeletal muscle. Basic Appl Myol.; 12:
47-254, 2002.
20. Carraro U. Modulation of trophism and fiber type
expression of denervated muscle by different patterns of
electrical stimulation. Basic Appl Myol.; 12: 263-273, 2002.
21. Midrio M: The denervated muscle: facts and d
hypotheses. A historical review. Eur. J. Appl. Physiol.;
98:1-21, 2006.
22. Carraro U, Rossini K, Mayr W, Kern H. Muscle fiber
regeneration in human permanent lower motoneuron
denervation: relevance to safety and effectiveness of FES-
training, which induces muscle recovery in SCI subjects.
Artif Organs; 29:187-191, 2005.
23. Modlin M, Forstner C, Hofer C, Mayr W, Richter W,
Carraro U et al. Electrical Stimulation of Denervated
Muscles: First Results of a Clinical Study Artificial Organs;
29:203–206, 2005.
24. Lotersztain H, La Nacion (daily), page 3, Dec. 24,
Buenos Aires, 1997.
25. Graupe D, Kohn KH, Neurol. Res., 19: pp. 323-333.
1997.
26. Ragnarsson, KT, Physiological effects of functional
electrical stimulation-induced exercises in spinal cord
injures individuals. Clinical Orthopeadics,1998; 233: 53-63
, 1998.
27. Faghri PD, Glaser RM, Figoni SF. Functional Electrical
Stimulation Leg Cycle Ergometer Exercise: Training Effects
on Cardiorespiratory Responses of Spinal Cord Injured
Subjects at Rest and During Submaximal Exercise. Arch
Phys Med Rehabil, 1992; 73: 1085-93, 1992.
28. Cerrel Bazo H., Petrofsky JS, Brown SW. Recent
Advances in the Applications of Computer Controlled
Exercise. Ambulation and Functional Electrical Stimulation
in the Rehabilitation of Spinal Cord Injury Patients. Proc.
Fifth Congress of SOMIPAR [Società Medica Italiana di
Paraplegia], Perugia, Italy, Oct. 1992.
29. Schmidt RA. Motor control and learning: a behavioral
emphasis, second edition, Champaign, Illinois: Humans
Kinetics, 1998.
30. Nash MS, Jacobs PL, Montalvo PM, Klose KJ, Guest
8 of 13
8
RS, Needham-Shropshire BM, Arch. Phys. Med. Rehab.,
78:808-814, 1997.
31. Jacobs PL, Nash MS, Klose KJ, Guest RS, Needham-
Shrpshire BM, Green BA, Arch. Phys. Med. Rehab., 78:794-
798, 1997.
32. Needham-Shropshire BM, Broton GJ, Klose KJ ,
Lebwohl N, Guest RS, Jacobs PL, Arch. Phys. Med.
Rehab., 78:799-803, 1997
33. Guest RL, Klose KJ, Needham-Shropshire BM, Jacobs
PL, Arch. Phys. Med and Rehab., 78:804-807, 1997.
34. Graupe D, www.ece.uic.edu/~graupe, 1994
35. Graupe D, Suliga P, Prudian C and Kohn KH,
Stochastically modulated stimulation to slow down muscle
fatigue at stimulated sites in paraplegics using FES for leg
extension, Neurol. Res., 22, 703-704, Oct. 2000
36. Stalberg E, Trontelj I V, Single Fiber
Electromyography, Mirvale Press, Old Woking, UK, 1979.
37. Chung, H.S.-H. Hui, S.Y.R. Tang, S.C. Wu, A. On
the use of current control scheme for switched-capacitor
DC/DC converters, IEEE Trans. Industrial Electronics, 47,
2, 238-244, Apr. 2000.
Figure 1: Response-EMG as measured at quadriceps of complete thoracic-level paraplegic
9 of 13
9
Figure 2: Morphological appearance and distribution of tissue types of human normal and paraplegic muscle: H-E Stained: (A) Normal adult human muscle; (B) Upper motor neuron lesion (enervated) muscle; (C), lower motor neuron
lesion (denervated) paraplegic muscles; (D) Normal human muscle; (E) Long-term enervated; (F) Long-term
denervated paraplegics.
FIGURE 3: Parastep Users, trained at Vicenza’s Villa Margherita Neurorehabilitation and Research Center
(under the direction of Dr. H. Cerrel-Bazo) - shown at the finish of 1.5 kilometer walk in Carpi, Italy, part of
the city's "Marathon Run" celebration.
Research
Subjects
SEX A
GE
Height
meters
Weight
kg
TYPE
Of SCI
SCI - LEVEL
(Thoracic)
MF 1 M 20 1,75 70 Motor Car Accid. 8
SM 2 M 23 1,75 65 MCA 10
TC 3 M 22 1,80 67 MCA 5
RB 4 M 25 1,83 75 Gun Shot 10
LL 5 F 25 1,60 53 FALL-horse 8
MG 6 M 32 1,77 62 MCA 7
MEAN 24,5 1,75 65,3 8
SD 4,14 0,08 7,5011 1,8973
TABLE 1: Demographics characteristics of some SCI gait train in Vicenza, Italy.
Research
Subjects
Months
after SCI
METERs
Continuous walk
M/MIN
speed
Minutes of
Continuous walk
10 of 13
10
MF 1 28 600 20 30
SM 2 57 600 15 40
TC 3 10 675 15 45
RB 4 72 675 15 45
LL 5 20 650 13 50
MG 6 22 900 15 60
MEAN 34,83 683,33 15,5 45
SD 24,175 111,43 2,345 10
TABLE 2: SCI walking Performance (Parastep gait training in Vicenza, Italy)
Ave. Distance m/walk Ave speed m/sec
Approx 85 sessions daily over 4 months Vicenza (Cerrel-Bazo et al. [5]):
14 patients 444.3 14.5
32 sessions 3/week, 12 weeks Univ. of Miami (Klose et al. [4] ):
16 patients (13 male, 3 female) 115 5.0
TABLE 3: Ambulation Performance Results (Parastep Users) COMMENT: For most USA patients, 4 -months training program that first concentrates on the SCI derivative factors
(see Sect. 4) programs as in Vicenza are impractical. On completing a 32 session program, performance may
reach that of a 4-month program in 6-12 months if patients continue ambulating at least 30 Min./day for some patients
Pre-FES-Training
(Ave)
Post-FES-Training
(Ave)
Lower-extremity Blood Flow 417 mL/min 650 mL/min (improv.) (Nash et al. [29] )12 patient data/ U. of Miami
Heart Rate 70.1 63.2 (improv.) (Nash et al. [29]) 12 patients/Miami
Time to fatigue (at peak arm ergometry test) 15.3min 19.2min (impr.) (Jacobs et al. [30]) 15 patients/Miami
Peak Workload Heart Rate (pk arm ergom. test) 188.5 183.1 (impr.) (Jacobs et al. [30] 15 patients/Miami
Oxyg. Uptake (pk Arm ergom. test) 20mL/Kg/min 23mL/Kg/min (improv.) (Jacobs et al. [30) 15 patients/Miami
Spasticity usually improvement especially
for very spastic pre-training
(Graupe, Kohn [3], [9], [31])
Michael Reese Hospital, Chicago
Bone Density No follow-up data except for 11 weeks after start of
training, where no significant change was reported (Needham-Shropshire et al.[32)
Physical Self Concept (TSCS scores) 43.2 TSCS 52 TSCS (improv.) (Guest et al. [33]) 15 patients/Miami
Depression Scores (BDI scores) 8.8 BDI 5.4 BDI (impr.) (Guest et al. [33]) 15 patient data
TABLE 4: Medical and Psychological Evaluation Outcomes (Parastep Users) Notation: TSCS: Tennessee Self Concept Scale; BDI: Beck Depression Inventory score
11 of 13
11
___________________________________________________________________
Pulse interval )m.sec) 42+/- 0 42+/-5 42+/-10 42+/- 20_
Ave. extension time (m.sec) 82.22 112.33 97.42 94.78
% improvement 0 +36.62 +18.5 +15.3
Stand. Dev. (m.sec) 11.43 18.06 16.8 13.2
95% conf. range (t-test) (m.sec) +/-8.8 +/-11.45 +/-10.7 +/-10.2___
Table 5: Leg extension times with stochastically modulated stimulation inter-pulse intervals: