Apparent Diffusion Coefficients for Differentiation of Cerebellar Tumors in Children
The evolution of the apparent diffusion coefficient in the pediatric brain at low and high diffusion...
Transcript of The evolution of the apparent diffusion coefficient in the pediatric brain at low and high diffusion...
Original Research
The Evolution of the Apparent Diffusion Coefficientin the Pediatric Brain at Low and High DiffusionWeightings
Richard A. Jones, PhD,1,2* Susan Palasis, MD,1,2 and J. Damien Grattan-Smith MD1,2
Purpose: To evaluate the evolution of the apparent diffu-sion coefficient (ADC) with age for different degrees of dif-fusion weighting using a clinically feasible approach.
Materials and Methods: Data was acquired using separatescans with b values in the range typically used for clinicalstudies (100–900 seconds/mm2) and higher b values(1800–3000 seconds/mm2). The ADC was calculated foreach of the data sets by fitting the data to a monoexponen-tial function.
Results: The results from 50 children aged three years andless showed some deviations from literature values derivedusing a full biexponential fit, with these differences reflect-ing the approximations inherent in this approach. The val-ues obtained with this technique appear to be reproduciblebut the resulting “institutional values” are comparable tothose from other centers only if identical measurementcriteria are used.
Conclusion: A significant decline in both components ofthe ADC during the first few months of life was observed; inaddition, the attenuated slow ADC values seen in adultwhite matter were only present at birth in early myelinatingregions. The subsequent development of the slow ADC inwhite matter suggests that it is associated with myelinationor processes associated with axonal development.
Key Words: MRI; diffusion; pediatric; brain development;myelinationJ. Magn. Reson. Imaging 2003;18:665–674.© 2003 Wiley-Liss, Inc.
MAGNETIC RESONANCE (MR) DIFFUSION imaginghas become a standard technique for the detection ofacute stroke in adults, and an increasing number ofapplications for quantitative diffusion imaging are be-
ing described in the literature (1–3). Recent researchsuggests that the use of very strong diffusion weight-ings may further enhance the utility of diffusion-weighted imaging (4,5). The apparent diffusion coeffi-cient (ADC) of cerebral tissue changes significantlyduring the initial year of life and exhibits significantregional variations in contrast to the homogeneousADC of the normal adult brain (6–8). This complicatesthe interpretation of both diffusion-weighted and ADCimages obtained from neonates and infants and mayaccount for some of the difficulty in interpreting thechanges in diffusion occurring subsequent to hypoxic-ischemic injury in the pediatric brain (9,10).
Studies performed to characterize the dependence ofthe ADC on the diffusion weighting (b value) haveshown that when the decay of the in vivo water signal issampled over an extended range of b values, the result-ing decay curve is well characterized by a two-compo-nent model with the two components having fast andslow diffusion coefficients, respectively (4,5,11–13). Thefast and slow apparent diffusion coefficients (ADCfast
and ADCslow) and the size of the components can beestimated using biexponential fitting; however, robustbiexponential fitting requires both a large number of bvalues and high signal-to-noise ratio (SNR), making itunsuitable for routine clinical use. The studies per-formed to date have either fitted the data from regions ofinterest (4,11,12), have used low spatial resolution andlimited spatial coverage to allow the collection of para-metric maps in a reasonable amount of time (13), orhave used exams with a very long duration (5). Analternative approach to examining the form of the ADCdecay curve is to use q-space imaging in which thediffusion related decay is subject to a Fourier analysis(14,15); however, this technique also requires a rela-tively large number of b values and is hence also timeconsuming. In addition, the q-space theory was devel-oped for very short gradient pulses and the validity ofthis approach to clinical systems where the duration ofthe gradient pulses has to be relatively long remains tobe proven. Recently, a more clinically feasible methodfor studying the fast and slow diffusion coefficients hasbeen suggested in which diffusion-weighted images areacquired using separate sets of low and high b values.ADC maps are then calculated by fitting each data set to
1Department of Radiology, Emory University School of Medicine, At-lanta, Georgia.2Department of Radiology, Children’s Healthcare of Atlanta, Atlanta,Georgia.Presented in part at the 10th Annual Meeting of ISMRM, Honolulu,2002.*Address reprint requests to: R.A.J., Department of Radiology, Chil-dren’s Healthcare of Atlanta, 1001 Johnson Ferry Road, Atlanta, GA30342. E-mail: [email protected] February 24, 2003; Accepted August 1, 2003.DOI 10.1002/jmri.10413Published online in Wiley InterScience (www.interscience.wiley.com).
JOURNAL OF MAGNETIC RESONANCE IMAGING 18:665–674 (2003)
© 2003 Wiley-Liss, Inc. 665
a monoexponential and the resulting values are as-sumed to approximately characterize the ADCfast andADCslow components, respectively (16).
The principle aim of this study was to use the tech-nique of acquiring separate low and high b-value datato evaluate the fast and slow components of the ADC ofchildren aged between zero and three years of age andto assess the limitations inherent in the use of thistechnique. The resulting data were used to assess if thefast and slow components of the ADC evolve in a similarmanner with age, if the changes with age correlatedwith myelination, and to determine normal ADC valuesfor both components in order to provide normative datafor future studies. Any differences observed betweenthe rates of evolution of the two components with age,or in the effect of myelination on these components,may provide information that could help clarify the or-igin of the two diffusion compartments.
MATERIALS AND METHODS
Selection of the Range of b Values
In order to make an appropriate choice of b values for apediatric population, a simulation was performed. Theglobal SNR of the brain was estimated using data fromfive neonates measured using our standard echo-pla-nar imaging (EPI) diffusion sequence with b � 0 sec-onds/mm2. The SNR was found to be approximately 65(this figure includes a correction for the Rician distri-bution of the background noise). The values for the fastand slow diffusion coefficients for both the internal cap-sule and cortex of the neonate and adult derived byMulkern et al (13) using biexponential fitting were fittedto a monoexponential function for various ranges of bvalues to estimate the values for ADCfast and ADCslow
that would be obtained using the methodology of Clarket al (16). The results are summarized in Table 1 andshow that significant errors in the estimate of the valueof the fast and slow components occur when using thisapproach. The fast component (ADCfast) was systemat-ically overestimated by between 16% and 45% for thetissues and ages in question. Changing the range ofvalues used for the calculation, while remaining in the
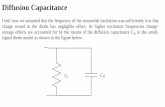
low b-value range (�1200 seconds/mm2) had relativelylittle effect on the calculated value (data not shown). Forthe slow component, the error in the simulation was, asexpected, reduced by using higher b values due to theincreased attenuation of the residual fast component.The curves shown in Figure 1 depict the decay curvesfor ADCfast and ADCslow that would be generated usingbiexponential fitting of the internal capsule, as well asthe composite biexponential curve. For b values of 3000seconds/mm2 and above, the SNR for the internal cor-tex neonatal brain can be seen to be very low. At lowSNR, the noise in the MR image data can significantlyincrease the mean signal intensity when using magni-tude reconstruction, and because the SNR depends on
Table 1Effect of the Choice of b Values on the ADC
b value range Category Region Mono-exp. ADC Bi-exp. ADC
100–900 Neonate (fast) Int. capsule 1032 1240100–900 Neonate (fast) Cortical GM 1215 1450100–900 Adult (fast) Int. capsule 690 1250100–900 Adult (fast) Cortical GM 1017 1690
1800–3000 Neonate (slow) Int. capsule 681 3401800–3000 Neonate (slow) Cortical GM 727 3801800–3000 Adult (slow) Int. capsule 280 1601800–3000 Adult (slow) Cortical GM 471 3703000–4200 Neonate (slow) Int. capsule 496 3403000–4200 Neonate (slow) Cortical GM 507 3803000–4200 Adult (slow) Int. capsule 196 1603000–4200 Adult (slow) Cortical GM 392 370
Results of fitting the data from Mulkern et al (13) using the separate fitting of low and high b values to monoexponential functions in orderto derive the fast and slow coefficients of the ADC. The calculated values are compared with actual values derived using biexponential fittingfor different regions and different ranges of b values. In all cases the ADC values are in �m2/sec.
Figure 1. Curves showing a biexponential fit and the fast andslow components that comprise the biexponential fit. Thecurves were based on the data presented for the internal cap-sule of the neonate in Mulkern et al (13). The relative signal atb � 0 seconds/mm2 was set to 65, which is typical of the SNRmeasured with our diffusion sequence at b � 0 seconds/mm2.
666 Jones et al.
the b value, the noise-related error increases at higherb values, causing the ADC to be overestimated (17). Inthe simulations shown in Figure 1 at b � 3000 sec-onds/mm2, the SNR has been reduced to around 5. Inanisotropic regions of the brain, such as the internalcapsule, the diffusion is orientation dependent, leadingto variations in the SNR that depend on the alignmentof the diffusion tensor of the tissue in question and thevector of the diffusion sensitizing gradients. When thesetwo are aligned, the SNR will be further reduced, lead-ing to a very low SNR.
Ideally, one could try to compensate for the effect ofeach component on the other component; however, thisrequires an estimate of the size of the slow fraction.Clark et al (16) used geometric extrapolation of thesignal measured at high b values to estimate the frac-tional size of the slowly diffusing component. However,this approach suffers from the same inherent problemas the calculation of slow ADC; namely, it is influencedby the presence of a residual signal from the fast com-ponent and hence the range of b values chosen for thecalculation. Despite the inherent limitations of usingseparate, monoexponential fitting to derive ADCfast andADCslow, the available imaging time for this clinicalstudy (�10 minutes), the need for multiple slices, andthe ability to generate parametric maps of the fast andslow diffusivities, made this approach the only feasiblemethod for the study. Allowing for both the range ofADC values expected to be encountered (due to regionalvariations and the age-dependent variation in the ADC)and the SNR required for accurate fitting it was decidedto use three b values between 1800 and 3000 seconds/mm2 for the slow ADC study. As explained earlier, thisassures robust fitting of the ADC values but also resultsin a larger error from the residual fast ADC component.Higher b values could have been used if the SNR wereincreased by increasing the voxel size; however, consid-ering that at birth the neonatal brain is only a quarterthe size of the adult brain, this option was felt to berather unattractive.
Patient Selection
Because MRI studies generally require sedation foryoung children, ethical considerations prevented theuse of normal subjects. Instead, subjects in the agerange of zero to three years who had been referred forMR imaging and who fulfilled predefined criteria weregiven an additional set of diffusion studies at the end ofthe standard MR procedures. Suitable subjects wererequired to have been a normal term birth and have aclinical history that did not suggest any neurologicdamage. If the patient underwent a routine MR exam ofthe brain, then this exam had to show no abnormalitiesand be consistent with normal brain development. Inmany cases, the patient was referred for another exam(typically spine, orbits, or facial mass studies); in thesecases, scout and diffusion studies were performed afterthe completion of the clinical study. Out of a total of 73patients enrolled in the study, 17 did not meet theabove criteria and six studies were degraded by motionartifacts, leaving a total of 50 subjects. The addition ofthe diffusion studies to the standard imaging protocols
used in our institution was approved by the local insti-tutional review board.
Data Acquisition
A full characterization of anisotropic diffusion requiressix measurements; however, in this study, the mea-surement of an orientation-independent diffusion coef-ficient in the form of the trace of the diffusion tensorwas sufficient for our purposes. To approximate thetrace, the diffusion was measured along each of thethree principle gradient axes and the mean ADC wasdefined as being one-third of the trace. The diffusionimaging sequence was implemented on a Siemens sym-phony scanner equipped with gradients capable of de-livering up to 30 mT/m. For the fast diffusion tensor bvalues of 100, 500, and 900 seconds/mm2 were appliedalong each of the three principal gradient axes using anecho time of 125 msec. A total of 10 5-mm-thick sliceswere acquired using a single-shot EPI sequence with a256 � 192 mm field of view (FOV), a 128 � 96 matrix,and a bandwidth per pixel of 1.3 kHz. The relativelypoor spatial resolution combined with the poor pointspread function of single-shot EPI sequences meansthat partial volume effects from cerebrospinal fluid(CSF) are unavoidable in many anatomic locations. Tominimize this effect, a fluid-attenuated inversion recov-ery (FLAIR) preparation sequence was used to suppressthe signal from the CSF (TR � 6000 msec, TI � 2100msec). For the measurement of the slow diffusion ten-sor b values of 1800, 2400, and 3000 seconds/mm2
were used, which rendered the FLAIR preparation se-quence unnecessary because the CSF is effectively sup-pressed at these high diffusion weightings. The TR forthe slow diffusion study was 2000 msec, the echo timewas the same as for the short TE study (125 msec), and12 averages were used to improve the SNR; all otherimaging parameters were identical to those used for thefast diffusion study. The imaging times for the fast andslow component studies were 1:40 and 4:16 (minutes:seconds), respectively. To facilitate the location of ana-tomic features, rapid T1-weighted spin-echo (TR � 400msec, TE � 12 msec, flip angle � 90°) and T2-weightedTSE (TR � 2000 msec, TE � 110 msec) images wereobtained at the same slice locations but with 1-mmisotropic in-plane resolution. The acquisition time foreach of the two sequences was 40 seconds.
The trace measurement used in this study assumesthat the cross-terms from the imaging gradients have anegligible effect on the calculated b values. To verify theaccuracy of this assumption, a water phantom wasimaged using low b values (100, 500, and 900 seconds/mm2) without the CSF suppression preparation se-quence. The temperature of the phantom during theimaging sequence was 22°C � 1°C. To assess the extentof any distortion induced by eddy currents at high bvalues, data from the initial studies were unwarpedusing a previously described registration technique(18). The artifacts induced by the eddy currents werefound to be small (typically �1 pixel) so this procedurewas not applied to the rest of the studies.
ADC in Pediatric Brain 667
Data Processing
Firstly the brain was segmented using in-house soft-ware written in IDL 5.5 (RSI, CO), the images were thenqualitatively assessed for motion by using cine loopsand comparing brain contours. Studies showing signif-icant motion (�1 pixel) were discarded. For the remain-ing studies, isotropic diffusion-weighted (IDW) imageswere derived for each b value by taking the cubed root ofthe product of the three images obtained at each bvalue. This approach is both computationally less in-tensive and generates higher signal-to-noise data thencalculating a separate ADC for each direction and thencalculating the tensor from the mean of these values.An IDL implementation of a MINPACK-1 nonlinear leastsquares curve fitting routine (19) was used to fit thedata from each range of b values (low or high) to a singleexponential on a pixel-by-pixel basis.
It has been suggested that taking the histogram of awhole slice, or the whole brain, is an appropriatemethod for assessing diffusion changes in the adultbrain in a general, operator independent manner(20,21). To assess if this approach is suitable for char-acterizing the pediatric brain at both high and low bvalues, histograms were generated using data sets froma neonate and an infant. The histograms and the fittedGaussian distributions are shown in Figure 2, and thefitted parameters are shown in Table 2. The curves andthe fitted parameters clearly show how the distribu-tions change with age, with the curves shifting to theleft and becoming narrower with increasing age. Theeffectiveness of the CSF suppression at low b values isevident from the absence of a tail to the distribution athigher ADC values. In general, all of the data exceptthat obtained from the infant using high b values werewell characterized by a Gaussian distribution; however,in the case of the infant ADCslow the higher ADC valuesin white matter regions resulted in a noticeably poorerfit. In this case, two separate populations would betterdescribe the distribution; however, as this would not beappropriate for the other cases, it was decided to useregion of interest measurements, rather than histo-grams, to analyze the data. The ADC was measured asthe mean value in regions of interest located in theinternal capsule, forceps minor, forceps major, cen-trum semi-ovale, thalamus, cortical gray matter (visualcortex), spleenum of the corpus callosum, and the cer-ebellum on ADC maps. These regions were identifiedusing either the IDW images or the rapid T1- and T2-weighted images obtained using the same slice thick-ness and slice orientation.
RESULTS
The phantom measurements yielded an ADC value of2180 � 99 �m2/second for water at 22°C � 1°C, whichis in good agreement with the theoretical value of 2134�m2/second. Figure 3 shows representative fast andslow IDW images, fast and slow ADC maps, and T2- andT1-weighted images for a slice through the internalcapsule of a 2.5-year-old infant. For the high b IDWimages hyperintensity is seen in several white matterregions and corresponding regions of hypointensity are
seen in the slow ADC map. The fast IDW image and thefast ADC map both exhibit very little contrast, which isconsistent with the histograms shown in Figure 2. InFigure 4, the low and high b IDW images and the cor-responding ADC maps for children ages 1, 16, 35, 75,and 130 weeks are shown. Considering the slow ADCimage of the one-week-old neonate, hypointensity isobserved only in the internal capsule; at 16 weeks thecorpus callosum also shows strong hypointensity,which then progresses to other white matter areas asthe age increases. For the fast ADC images, hyperin-tense signal is seen in the forceps major and minor ofthe younger children, but this disappears with increas-ing maturity and by 130 weeks, both the fast ADC mapand the low b IDW images show very little inherentcontrast.
To characterize the evolution with age of the fast andslow ADC values in different regions, the ADC valuesmeasured in regions of interest plotted against ageand then fitted to a model. A model of the form: a � b*exp(–c*x), where x is the age in weeks, was chosenbecause the ADC in adulthood is known to be constantand the rapid decay in the ADC during the first year oflife is consistent with an exponential model. More com-plicated models have been suggested (7), but in theabsence of a physiologic justification for such models,we preferred to retain a simpler model. Fitting was per-formed using a Levenberg-Marquardt fitting routineand acceptable fits, as assessed using the adjustedcoefficient of multiple determination, were obtained inall regions except for the slow ADC in the visual cortex.For the latter region a linear model produced a better fit.The results of the fitting for five regions of interest anda plot of the ratio ADCfast/ADCslow are shown in Figure 5and the best fit parameters are summarized in Table 3.
The evolution of the ADC with age in all white matterregions showed a similar form for both ADCfast andADCslow. There was a noticeable decline during the firstsix months of life; subsequently, the rate of declineslowed progressively and by the third year of life wasevolving at a very slow rate. The evolution of the slowADC in gray matter can be seen to be markedly lesspronounced than that of the white matter. In general,with increasing age, the fast ADC in white matter con-verges towards the gray matter value, while for the slowADC, the values diverge. Thus, the fast ADC maps showa reduction in contrast with increasing age, while forthe slow ADC maps, the contrast increases with age asthe white matter signal diverges from the gray mattersignal. The one exception is the internal capsule, whichalready exhibits a hypointensity in neonates (see Figs. 3and 4). As shown in Figure 5, the ratio ADCfast/ADCslow
shows a similar form for all white matter regions, withan increase in the ratio from approx. 1.5 to 2.5 duringthe first year of life. The ratio then remains approxi-mately constant for the next two years. For gray matterregions, the ratio remains approximately constant overthe age range studied.
DISCUSSION
Using separate sets of diffusion-weighted images tomeasure low and high diffusion-weighted images and
668 Jones et al.
then separately fitting the data for each set to a mono-exponential in order to estimate ADCfast and ADCslow isprobably the only feasible method for clinical studiesthat require whole brain coverage in a reasonableamount of time. However, the limitations inherent in
the method mean that the values obtained are not thesame as would be obtained from biexponential fitting ofdata obtained using a large number of b values. Usingthe data from Table 3 to derive ADCfast and ADCslow
values for the internal capsule of a one-week-old infant
Figure 2. Histograms showing the distribution of the fast (A,C) and slow (B,D) ADC values in slice through the internal capsulein a neonate (A,B) and a 2.5-year-old infant (C,D). The histograms were fitted to a Gaussian distribution using a SIMPLEX fittingroutine, and the dashed lines show the resulting fits The difference between the fast and slow components and the evolution ofthese components with age is clearly illustrated by the changes in the distributions of the ADC values. The distribution of thefast and slow ADC values in the neonate and the fast ADC in the infant are all well characterized by a normal distribution. Thehistogram of the slow ADC of the infant (D) shows a prominent shoulder at low b values corresponding to the slower white matterdiffusion seen in older children and adults.
ADC in Pediatric Brain 669
yields values of 1017 and 542 �m2/second. These arelower and higher, respectively, than those obtained us-ing biexponential fitting by Mulkern et al (13) for thesame region and age (1240 and 340 �m2/second). How-ever, as shown in Table 1, if we apply the methodologyused in this article to the data presented by Mulkern etal (13), we obtain values of 1032 and 681 �m2/secondfor the fast and slow components, respectively, whichare in better agreement with our results. If we assumethat the constant term in the fit to the evolution of theADC with age represents the adult value, then the val-ues obtained in this study for the fast ADC of the inter-nal capsule (749 �m2/second) are lower than those
reported by Mulkern et al (1250 �m2/second) and Yo-shiura et al (5) (1180 �m2/second). Similarly, the slowADC (265 �m2/second) is higher than the values of 160and 220 mm2/second reported by the same authors(5,13). Applying the dual fit methodology to the adultdata presented by Mulkern et al (13) and Yoshiura et al(5) yields values of 690 and 944 �m2/second for ADCfast
and 280 and 289 �m2/second for ADCslow, which are inbetter agreement with our results.
Considering the results for neonatal cortical graymatter, we obtained a fast ADC of 1055 �m2/second,whereas Mulkern et al (13) obtained 1450 �m2/sec-ond; applying the dual fit methodology to their datayields a value of 1215 �m2/second. Our extrapolatedadult value for ADCfast is 792 �m2/second, and thecorresponding values obtained by Mulkern et al (13)were 1690 �m2/second for a biexponential fit and1017 �m2/second for the dual fit methodology. Thevalues obtained applying the dual fit methodology tothe data of Mulkern et al (13) are closer, but some-what higher, than our values. The fact that, even aftercorrecting for the methodology, their values for corticalgray matter are higher than ours may be due, in part, tothe fact the Mulkern et al (13) did not employ fluid sup-pression to remove the effects of partial volumes of CSF.Given the low spatial resolution employed in their study,some degree of CSF was almost inevitable.
Table 2Categorisation of ADC Values Using Histograms
Category � �
Neonate. low b values 1165 120Neonate. high b values 878 146Infant. low b values 843 104Infant. high b values 574 117
The ADCfast and ADCslow values of all pixels in a single slice at thelevel of the internal capsule were calculated, using low and high bvalues respectively, for a neonate and an infant. The distributions ofthe ADC values were plotted and then fitted to a Gaussian distribu-tion, the table shows the mean (�) and variance (�) of the fitteddistributions for each of the four categories.
Figure 3. Images of a 2.5-year-old infant. The first column shows an IDW image obtained with b � 900 seconds/mm2 (top) andthe fast ADC map (bottom), the second column shows an IDW image obtained with b � 3000 seconds/mm2 (top), and the slowADC map (bottom). The third column shows rapid T2-weighted (top) and T1-weighted (bottom) anatomic images for comparison.
670 Jones et al.
The results from this study are more easily comparedwith those of Clark et al (16) who introduced the meth-odology used in this article. In general, there was rea-sonable agreement between the two studies. TheirADCfast values were, on average, 12% lower than ourswhile their ADCslow values were 10% lower. The princi-pal reasons for these differences are probably that weextrapolated, rather than measured, the adult valuesand the fact that different ranges and numbers of bvalues were used for the two studies. In particular, theyused higher b values for the calculation of ADCslow and,as shown in Table 1, this will improve the accuracy oftheir estimate of ADCslow assuming that the images re-tain adequate SNR. Because the rate of diffusion in theadult brain is lower than that of the neonatal or infantbrain, higher b values can generally be used while re-taining adequate SNR. The range of b values used forthe ADCfast measurements was also different from thatused in our study; the effect of this will be less pro-
nounced than that of using a different range of high bvalues but will tend to reduce the value obtained forADCfast.
The results presented in this article are relativelyconsistent with the existing literature data providingthat one takes into account the methodology used inthis study; however, the values derived in this studycan only be directly compared with values obtainedusing the same methodology. Even if the same method-ology is used, the range of b values employed will affectthe values derived for ADCfast and ADCslow. These re-strictions obviously limit the usefulness of the ap-proach used in this article; however, if useful clinicalapplications are found for parametric maps of the slowcomponent of the ADC, then this may be the best way toobtain such data, despite the limitations of the meth-odology. It should be noted that some of these stricturesalso apply when comparing conventional ADC mapsfrom different centers because the use of a different
Figure 4. The changes in the IDW images and the fast and slow ADC maps is illustrated with images of children aged 1, 16, 35,75, and 130 weeks (columns from left to right). The first row shows IDW images obtained with b � 900 seconds/mm2 and thesecond row shows the fast ADC maps calculated using images with b values of 100, 500, and 900 seconds/mm2. The third rowshows IDW images obtained using b � 3000 seconds/mm2 and the fourth row shows the slow ADC maps calculated using bvalues of 1800, 2400, and 3000 seconds/mm2.
ADC in Pediatric Brain 671
range (or number) of b values can also affect the ADCvalues derived with conventional diffusion-weightedimaging sequences (22).
A second question is how much of the form of theevolution of the slow ADC with age is due to the residualcontribution from the fast ADC (and vice versa) for the
Figure 5. A–E: The evolution of the fast and slow ADCs with age in five anatomic regions. For each region, the best fit is shownby either a solid line (ADCfast) or a dashed line (ADCslow). The dashed lines on either side of the best fits represent the 95%confidence intervals for the ADC values. F: The evolution of the ratio ADCfast/ADCslow in seven different regions.
672 Jones et al.
number and amplitude of the b values used in thisstudy. Considering the mean values from the forcepsmajor at one week of age, the fast ADC will be approx-imately 1500 �m2/second; hence, for a b value of 1800seconds/mm2, the signal from the fast ADC will beapproximately 7% of that observed with b � 0 seconds/mm2. By one year of age, ADCfast will have declined toapproximately 1000 �m2/second and the residual sig-nal from the fast component will be 17% of the initialvalue. Because ADCslow declines over the same period oftime, a residual ADCfast component cannot explain all ofthe age-dependent variations seen in this region. Giventhat the true fast ADC is probably higher than thevalues obtained in this study then the actual contribu-tions may be somewhat lower but the same trend re-mains. The form of the evolution with age of the fast andslow ADC curves were noticeably different in severalregions, including the visual cortex, cerebellum, andthe centrum semi-ovale, which implies that a residualfast ADC component cannot explain all of the age-de-pendent changes seen in the slow ADC (and vice versa).
Under the assumptions that separate sampling of thefast and slow ADCs is valid, and that three b values aresufficient to characterize each of these components,then these preliminary results are consistent with theidea that the evolution with age of both components ofthe ADC reflects the maturation of cerebral white mat-ter. At any given age during the first six months of life,the early maturing areas show lower ADC values thanlate maturing areas for both fast and slow ADC values.In gray matter, both components show only a modestchange with age and the ratio ADCfast/ADCslow remainsapproximately constant. The small changes seen inADCs of areas such as the thalamus, which are nomi-nally gray matter, may be due to the presence of a smallamount of white matter, in the form of microfibers, inthese regions. The origin of the changes in the ADC isundoubtedly multifactorial and includes the reductionin the size of the extracellular space, the physical re-striction of water diffusion by myelin, an increase in theconcentration of macromolecules in and around theaxons, and the development of functional ionic chan-nels before myelination. However, the reduction of theADC in white matter regions parallels the progression ofmyelination, and regions that are myelinated at birth,such as the internal capsule, exhibited a slow ADC
value that changed little with age and had a much lowerinitial value than white matter regions that are unmy-elinated at birth. Studies in animals suggests thatchanges in the diffusion anisotropy actually occur dur-ing premyelination rather than during myelination it-self (23,24) and are hence related to the development ofionic fluxes formed by the development of action poten-tials with the axons (24) rather than to myelination perse. The data acquired here cannot determine if thechanges are associated with premyelination or myeli-nation, but in either case, the data presented here areconsistent with the development of the axons as a dis-tinct compartment with the cell is a major factor in thedifference in the slow ADC values between white andgray matter.
The increased contrast in the slow ADC maps can beboth advantageous and disadvantageous. For the pur-pose of evaluating stroke lesions, the white matter hy-perintensity at high b values may make the delineationof the extent of lesions more problematic. DeLano et al(25) showed that gray and white matter are isointensefor b values between 1000 and 2000 seconds/mm2 andthis is probably the optimum range for observing acutestroke because an isointense background will facilitateaccurate definition of the ischemic lesion (25). Both thefast and slow ADCs measured in this study changedmarkedly during brain development and it may be pos-sible to use them as markers for myelination; however,how quantitative these results are remains to be as-sessed, as does whether other measures, such as T2(26), are equally sensitive markers of brain develop-ment. The high b IDW images and the slow ADC mapsmay provide an easily interpretable visualization ofbrain development, albeit with limited spatial resolu-tion; however, further study is required to fully evaluatethis suggestion.
REFERENCES
1. Warach S, Gaa J, Siewart B, Wielopolski P, Edelman RE. Acutehuman stroke studied by whole brain echo-planar diffusionweighted magnetic resonance imaging. Ann Neurol 1995;37:231–241.
2. Sorensen AG, Buonanno FS, Gonzalez RG, et al. Hyperacute stroke:evaluation with combined multi-slice diffusion weighted and hae-modynamically weighted echo planar MR imaging. Radiology 1996;199:391–401.
Table 3The Evolution of the Fast and Slow ADCs With Age
RegionFast ADC Slow ADC
A B C aR2 A B C aR2
Forceps major 586 � 50 0.045 � 0.007 929 � 22 0.78 601 � 29 0.052 � 0.005 361 � 12 0.91Forceps minor 604 � 43 0.050 � 0.007 925 � 17 0.84 609 � 31 0.035 � 0.004 337 � 17 0.89Centrum SO 476 � 29 0.036 � 0.005 830 � 16 0.86 662 � 29 0.053 � 0.005 332 � 28 0.93Internal capsule 283 � 24 0.053 � 0.008 749 � 9 0.78 296 � 21 0.066 � 0.011 265 � 10 0.75Corpus callosum 389 � 35 0.032 � 0.007 763 � 22 0.73 333 � 41 0.034 � 0.010 241 � 24 0.60Visual cortex 276 � 31 0.048 � 0.010 792 � 12 0.67Thalamus 296 � 33 0.100 � 0.018 821 � 8 0.69 201 � 15 0.035 � 0.006 516 � 9 0.79Cerebellum 361 � 34 0.105 � 0.016 710 � 8 0.76 105 � 15 0.076 � 0.018 415 � 4 0.57
The evolution was characterized by fitting the data from 50 children to a function of the form A*EXP(B*age) � C where the age wasmeasured in weeks (a normal term birth being 0 weeks). The values obtained and the adjusted coefficient of multiple determination (aR2)of the fit are shown for all regions with the exception of the slow ADC of the visual cortex which could not be fitted.
ADC in Pediatric Brain 673
3. Horsfield MA, Jones DK. Applications of diffusion weighted anddiffusion tensor MRI to white matter diseases: a review. NMRBiomed 2002;15:570–577
4. Clark CA, Le Bihan D. Water diffusion compartmentation and an-isotropy at high b values in the human brain. Magn Reson Med2000;44:852–859.
5. Yoshiura T, Wu O, Zaheer A, Reese TG, Sorensen AG. Highly diffu-sion sensitised MRI of brain: dissociation of gray and white matter.Magn Reson Med 2001;45:734–740.
6. Neil JJ, Shiran SI, McKinstry RC et al. Normal brain in humannewborns: apparent diffusion coefficient and diffusion anisotropymeasured by using diffusion tensor MR imaging. Radiology 1998;209:57–66.
7. Mukherjee P, Miller JH, Shimony JS, et al. Normal brain matu-ration during childhood: developmental trends characterizedwith diffusion-tensor MR imaging. Radiology 2001;221:349–358.
8. Forbes KPN, Pipe JG, Bird CR. Changes in brain water diffusionduring the first year of life. Radiology 2002;222:405–409.
9. Robertson RL, Ben-Sira L, Barnes Pd, et al. MR line scan diffusionweighted imaging of term neonates with perinatal ischaemia. Am JNeuroradiol 1999;20:1658–1670.
10. Forbes KPN, Pipe JG, Bird R. Neonatal hypoxic-ischaemic enceph-alopathy: detection with diffusion weighted MR imaging. Am JNeuroradiol 2000;21:1490–1496.
11. Niendorf T, Dijkhuizen RM, Norris DG, Van Lookeren Campagne M,Nicolay K. Biexponential diffusion attenuation in various states ofbrain tissue: implications for diffusion-weighted imaging. MagnReson Med 1996;36:847–857.
12. Mulkern RV, Gudbjartsson H, Westin C-F, et al. Multi-componentapparent diffusion coefficients in human brain. NMR Biomed 1999;12:51–62.
13. Mulkern RV, Vajapeya S, Robertson RL, Caruso PA, Rivkin MJ,Maier SE. Bi-exponential apparent diffusion coefficient parametri-sation in adult vs newborn brain. Magn Reson Imag 2001;19:659–668.
14. Callaghan PT. Principles of nuclear magnetic resonance micros-copy. Oxford: Oxford Science Publications; 1991.
15. Assaf Y, Ben-Bashat D, Chapman J, et al. High b value q spaceanalyzed diffusion weighted MRI: application to multiple sclerosis.Magn Reson Med 2002;47:115–126.
16. Clark CA, Hedhus M, Moseley ME. In vivo mapping of the fast andslow diffusion tensors in human brain. Magn Reson Med 2002;47:623–628.
17. Dietrich O, Heiland S, Sartor K. Noise correction for the exactdetermination of apparent diffusion coefficients at low SNR. MagnReson Med 2001;45:448–453.
18. Haselgrove JC, Moore JR. Correction for distortion of echo planarimages used to calculate the apparent diffusion coefficient. MagnReson Med 1996;36:960–964.
19. Markwardt CB. IDL curve fitting and function optimization. http://cow.physics.wisc.edu/~craigm/idl
20. Cercignani M, Inglese M, Pagani E, Comi G, Fillipi M. Mean diffu-sivity and fractional anisotropy histograms of patients with multi-ple sclerosis. Am J Neuroradiol 2001;22:952–958.
21. Nusbaum AO, Tang CY, Wei T, Buchsbaum MS, Atlas SW. Whole-brain diffusion MR histograms differ between MS subtypes. Neu-rology 2000;54:1421–1427.
22. Melham ER, Itoh R, Jones L, Barker PB. Diffusion tensor imaging ofthe brain: effect of diffusion weighting on trace and anisotropymeasurements. AJNR Am J Neuroradiol 2000;21:1813–1820.
23. Wimberger D, Roberts TPL, Barkovich AJ, Prayer D, Moseley ME,Kucharczyk J. Identification of pre-myelination by diffusionweighted MRI. J Comput Assist Tomogr 1995;19:28–33.
24. Prayer D, Barkovich AJ, Kirschner DA, et al. Visualisation of non-structural changes in early white matter development on diffusionweighted MR images: evidence supporting premyelination anisot-ropy. Am J Neuroradiol 2001;22:1572–1576.
25. DeLano MC, Cooper TG, Siebert JE, Potchen MJ, Kuppusamy K.High b value diffusion weighted imaging of the adult brain: imagecontrast and apparent diffusion map features. AJNR Am J Neuro-radiol 2000;21:1830–1836.
26. Baratti C, Barnett AS, Pierpaoli C. Comparative MR imaging studyof brain maturation in kittens with T1, T2 and the trace of thediffusion tensor. Radiology 1999;210:133–142.
674 Jones et al.