Diagnosing prion diseases: needs, challenges and hopes
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Diagnosing prion diseases: needs, challenges and hopes
R E V I E W S
DIAGNOSING PRION DISEASES:NEEDS, CHALLENGES AND HOPESClaudio Soto
Abstract | Prion diseases are among the most intriguing infectious diseases and are associatedwith unconventional proteinaceous infectious agents known as prions. Prions seem to lack nucleicacid and propagate by transmission of protein misfolding. The nature of prions and their uniquemode of transmission present challenges for early diagnosis of prion diseases. In this article, state-of-the-art prion diagnostic techniques, together with the new strategies that are being used to develop sensitive, early and non-invasive diagnoses for these diseases are reviewed.
Department of Neurology,University of Texas MedicalBranch, 301 UniversityBoulevard, Galveston,Texas 77555-0646, USA.e-mail: [email protected]:10.1038/nrmicro1003
NATURE REVIEWS | MICROBIOLOGY VOLUME 2 | OCTOBER 2004 | 809
Prion diseases, which are also called transmissiblespongiform encephalopathies (TSEs), comprise a groupof fatal infectious neurodegenerative diseases thatinclude Creutzfeldt–Jakob disease (CJD), kuru,Gerstmann–Sträussler–Sheinker syndrome (GSS) andfatal familial insomnia (FFI) in humans, and scrapie,bovine spongiform encephalopathy (BSE) and chronicwasting disease (CWD) in animals1. These diseasesare characterized by brain vacuolation, ASTROGLIOSIS,neuronal APOPTOSIS and accumulation of the misfoldedprion protein (PrPSc; see BOX 1 for nomenclature) inthe central nervous system2.
In animals, the most common prion disease isscrapie, but the most infamous and dangerous diseaseis the recently discovered BSE, which affects cattle andis known worldwide by the lay term ‘mad cow disease.’In humans, the most common TSE is CJD, whichoccurs worldwide with an incidence of 0.5–1.5 newcases per one million people each year3. Three differentforms of CJD have traditionally been recognized1:sporadic (sCJD; ~85% of cases), familial (fCJD; ~10%),and IATROGENIC (iCJD; ~5%). However, in 1996, a newvariant form of CJD (vCJD) emerged in the UnitedKingdom4, which has been associated with consump-tion of meat infected with BSE5–7. In contrast withtypical cases of sCJD, vCJD affects young patients (theaverage age of patients is 27 years), and is a relativelylong illness (14 months compared with 4.5 monthsfor sCJD). Owing to insufficient information aboutthe incubation time and the levels of exposure to con-taminated cattle food products, it is impossible to
make well-founded predictions about the potentialfuture incidence of vCJD8. In animals, there is no evi-dence for inherited forms of the disease and mostcases seem to be acquired by horizontal or verticaltransmission.
Although TSEs are neurodegenerative disorders,in some forms of the disease prions replicate andaccumulate in lymphoid tissues markedly earlier thanin the central nervous system9. It seems that the orallyingested infectious agent is absorbed through theintestine into the blood, which transports it to lymphoidorgans where the prions undergo a first round ofreplication and accumulation before being transportedto the brain by the peripheral nerves (FIG. 1). Thispathway has been proposed on the basis of infectivitystudies of different organs at various stages of theincubation period9,10. Recently, studies using brainperfusion and capillary depletion techniques in ani-mals injected with purified PrPSc have suggested thatprions can gain access to the brain directly through theblood–brain barrier11. Regardless of the route by whichthe infectious agent enters the brain, it seems clear thatprions can be associated with several peripheral tissuesand biological fluids.
Is PrPSc the infectious agent?The nature of the transmissible agent has been thesubject of much debate2,12–14. Initially, the agent wasthought to be a slow virus15. Further research, however,indicated that the transmissible agent is markedly dif-ferent from viruses and other conventional pathogens.
ASTROGLIOSIS
Proliferation and branching ofglial cells in response to varioustypes of brain damage.
APOPTOSIS
The process of programmed celldeath that is characterized bydistinctive morphologicalchanges in the nucleus andcytoplasm, chromatin cleavageat regularly spaced sites and theendonucleolytic cleavage ofgenomic DNA.
IATROGENIC
An abnormal condition that isunwittingly caused by a medicalintervention.
810 | OCTOBER 2004 | VOLUME 2 www.nature.com/reviews/micro
R E V I E W S
shown that PrPSc and infectivity co-purified and thatthe concentration of the protein was proportional tothe infectivity titre19. Moreover, infectivity was retainedin highly purified preparations of PrPSc. Owing to thepurification of PrP it was possible to obtain the aminoacid sequence and, ultimately, cDNA clones that con-tained the sequence that encodes PrP20. PrP mRNA isthe product of a single gene. It is synthesized in thebrains of uninfected animals and is also constitutivelyexpressed in many cell types20. It became clear that PrPhas two alternate forms — the normal cellular protein(PrPC) and the pathological ISOFORM (PrPSc). Chemicaldifferences between the PrPC and PrPSc isoforms havenot been detected21, and the conversion seems toinvolve a conformational change in which the α-helicalcontent of the normal protein is reduced whilst theamount of β-sheet increases22. The structural changesare accompanied by alterations in the biochemicalproperties: PrPC is soluble in non-denaturing deter-gents, whereas PrPSc is insoluble; PrPC is readilydigested by proteases, whereas PrPSc is mostly resistant,and digestion results in the formation of an amino-terminally truncated fragment known as PrP 27-30(REFS 2,23). The mechanism by which PrPC is convertedinto PrPSc is unknown, but two different models havebeen proposed23,24 (FIG. 2).
PrPSc has been shown to catalyse the conversion ofPrPC into a protease-resistant PrPSc-like form (PrPres; seeBOX 1 for nomenclature) in vitro. The original system,developed by Caughey and co-workers25, using puri-fied PrPC mixed with stoichiometric amounts ofpurified PrPSc, produced a low yield of PrPres undernon-physiological conditions. More recently, a newin vitro conversion system has been developed to con-vert large quantities of PrPC into PrPres using minuteamounts of PrPSc (REF. 26). This system, called proteinmisfolding cyclic amplification (PMCA), confirms acentral facet of the prion hypothesis, which is thatprion replication is a cyclical process and that newlyproduced PrPres can further propagate the proteinmisfolding27.
Despite the compelling evidence in favour of theprion hypothesis, it is widely accepted that its finalproof will be the generation of infectious prions in vitro. If the infectious agent is misfolded PrPSc, andits replication is promoted through its interaction withPrPC, then it should be possible to reproduce the wholeprocess entirely in vitro14. Recently, a recombinantmouse PrP fragment (residues 89–230) that wasassembled into AMYLOID fibrils was found to induce atransmissible spongiform encephalopathy with PrPres
formation when injected in TRANSGENIC mice over-expressing the same PrP sequence28. These findingscome close to be the long-awaited definitive proof ofthe prion hypothesis, but some experimental caveatsneed to be addressed in future research. The diseasewas originally transmitted to transgenic animalsoverexpressing the PrP gene rather than to wild-typeanimals, which is a matter of concern because it isknown that this type of animal develops a prion-likedisease spontaneously.
Accordingly, a new hypothesis regarding the nature ofthe transmissible agent has recently emerged and gainedwidespread acceptance. This hypothesis proposes thatthe material that is responsible for disease transmissionis a protein that has the surprising ability to replicateitself within the body2. This newly discovered pathogenis called a proteinaceous infectious particle or prion.An important breakthrough in understanding thenature of the novel infectious agent was the isolationof the prion protein from infectious material18. Usingbiochemical and immunochemical methods it was
Box 1 | Nomenclature for the different prion protein isoforms
PrPThis refers to all prion protein and does not distinguish between different isoforms.
PrPC
The normal cellular prion protein that is present in healthy people. This form is rich in α-helical conformation and is soluble and protease-sensitive.
PrPSc
The disease-associated misfolded prion protein that is present in individuals affectedby TSEs. It is infectious, largely in the β-sheet conformation, insoluble and mostlyprotease-resistant.
PrPres
This refers to a β-sheet-rich, protease-resistant prion protein, which may or may notbe identical to PrPSc. In particular, this term is used to refer to protease-resistantprotein that is produced in vitro and which has not been experimentally shown to beinfectious.
PrP 27-30This refers to the resistant protein core that remains after protease treatment of PrPSc orPrPres. It comprises the last two-thirds of the protein.
Appendix
Peyer's patches
Spleen
Brain
Lymphoid system
Tonsil
Blood
Peripheral nerves
Sites of prion replication
Sites of prion transport
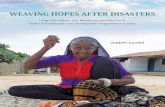
Figure 1 | Human tissues and body fluids involved in propagation and transport of theprion. Orally ingested prions are intestinally absorbed, mainly at the Peyer’s patches, andtransported to the blood and lymphoid fluids10. After a peripheral replication step in thespleen, appendix, tonsils or other lymphoid tissues, prions are transported to the brain mainlyby peripheral nerves9. Direct penetration into the brain across the blood–brain barrier is also possible11.
NATURE REVIEWS | MICROBIOLOGY VOLUME 2 | OCTOBER 2004 | 811
R E V I E W S
This is combined with persistent painful sensorysymptoms and is followed by ataxia, myoclonus anddementia. vCJD is differentiated from sCJD by theduration of illness (usually longer than 6 months) andEEG analysis (vCJD does not show the atypical patternthat is observed in sCJD). A high bilateral pulvinarsignal noted during MRI is usually used to help diag-nose vCJD35. In addition, because many cases of vCJDhave been shown to test positive for PrPres staining inlymphoid tissue (such as tonsil and appendix), a tonsilbiopsy might help accurate vCJD diagnosis. However,owing to the invasive nature of this test, it should onlybe performed for patients who fulfil the clinical criteriaof vCJD, but lack the characteristic MRI pulvinarsignal36.
GSS is a dominant inherited illness that is character-ized by dementia, Parkinsonian symptoms and a rela-tively long duration (typically, 5–8 years)37,38. Clinically,GSS is similar to Alzheimer’s disease, except that it isoften accompanied by ataxia and seizures. Diagnosis isestablished by clinical examination and genetic screen-ing for PrP mutations38. FFI is also dominantly inheritedand linked to PrP mutations. However, the main clinicalobservation associated with FFI is insomnia, which isfollowed at the late stages of the disease by myoclonus,hallucinations, ataxia and dementia39.
Several neuronal, astrocytic and glial proteins thatare elevated in sCJD have been identified40. In theearly phase of sCJD, the concentrations of the proteinsS-100, neuron-specific isoenzyme and ubiquitin aremarkedly increased in the cerebrospinal fluid , anddecrease over the course of the illness40. A marker ofneuronal death, the 14-3-3 protein, is commonly usedto help the diagnosis of sCJD41, but it has not provenuseful for diagnosing vCJD42 and is less specific indiagnosing the genetic forms of CJD. As the 14-3-3protein might be elevated in the cerebrospinal fluid ofpatients with other neurological illnesses, the usefulnessof this test depends on the exclusion of other patholo-gies. More recently, the erythroid differentiation-relatedfactor has been reported to be markedly underex-pressed in TSE-infected blood43. However, the speci-ficity of this change and the relevance of this marker forTSE diagnosis is unknown44.
Post-mortem tests for BSEThe extent of the BSE epidemics motivated theEuropean Commission (see the online links box) toimplement a system to evaluate and validate biochemicaltests that aimed to rapidly detect infected animals45,46.Post-mortem analysis of sick cattle by histological assaysof the brain is an accurate method of identifyinginfected animals47. However, this procedure is time con-suming, labour intensive and cannot be carried out on alarge scale. New tests were developed to allow multiplesamples to be processed in just a few hours, so that saleof the animals could be delayed until the results wereavailable. Two campaigns were undertaken to evaluatenine different tests using blind samples from BSE-infected and normal cattle45,48,49. Using sensitivity (theproportion of infected reference animals that score
Current TSE diagnosisAt present, there is no accurate pre-mortem diagnosis forTSEs29–31. For human diseases, diagnosis is based mainlyon clinical examination and the disease is consideredpossible, or probable, depending on the extent to whichthe clinical symptoms fit the standard guidelines.Definitive diagnosis can only be made post-mortem bybrain histological analysis31,32 of spongiform changes,astrogliosis and amyloid plaques (although these plaquesare not consistently seen in all TSEs). Although brainbiopsy has been used to establish a definitive diagnosis, itis strongly discouraged because it is invasive and costly.Moreover, a brain biopsy sometimes produces a false-negative result, because the tissue sample has been takenfrom an unaffected area of the brain.
The clinical diagnosis of sCJD is based on a combi-nation of rapidly progressive multi-focal dementia withpyramidal and extrapyramidal signs, MYOCLONUS, andvisual or cerebellar signs, together with a characteristicperiodic electroencephalogram (EEG)30–33. An impor-tant feature for diagnosing sCJD, and distinguishing itfrom Alzheimer’s disease and other dementias, is therapid progression of clinical symptoms and the shortduration of the disease, which is often less than 2 years.Despite the increasing use of magnetic resonance imaging(MRI), it is generally accepted that imaging technologiesare used mainly to exclude other causes of pathology30.The clinical manifestation of fCJD is very similar, exceptthat the disease onset is slightly earlier than in sCJD.Family history of inherited CJD, or genetic screening formutations in the PrP gene, are used to establish fCJDdiagnosis, although lack of family history does notexclude an inherited origin32.
vCJD appears initially as a progressive neuropsy-chiatric disorder that is characterized by symptoms ofanxiety, depression, apathy, withdrawal and delusions34.
ISOFORM
One or more alternativeconformations of the sameprotein.
AMYLOID
A general term that is used for avariety of different proteinaggregates that accumulate asextracellular fibrils of 7–10 nmand have common structuralfeatures, including a β-pleatedsheet conformation and theability to bind dyes such asCongo red and thioflavine.
TRANSGENIC
Refers to animals that have beengenetically engineered to containextra copies of a particular gene,frequently from a differentspecies.
MYOCLONUS
A rapid twitch resulting from asudden muscular contraction.
PrPc PrPSc
PrPc
+
+ +
PrPScProtein X PrP*
a Nucleation–polymerization model
b Template-assisted model
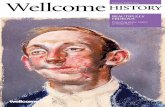
Figure 2 | Models for PrPC → PrPSc conversion. In the nucleation–polymerization model24,119
(a), the infectious PrPSc is a small oligomer that acts as a seed for recruiting, converting andstabilizing the misfolding of the normal PrPC. In the template-assisted conversion model23 (b), themain step is the formation of an intermediate state (PrP*) on binding to a molecular chaperone(protein X). This intermediate can interact with PrPSc (monomeric or oligomeric), which acts as atemplate for its conversion.
812 | OCTOBER 2004 | VOLUME 2 www.nature.com/reviews/micro
R E V I E W S
using a polyclonal primary antibody, a horseradishperoxidase-conjugated secondary antibody and anenhanced chemiluminescent reagent48,49. Brain samplesare directly loaded onto microplates immediately afterthe homogenization, extraction and protease digestionprocedure. During the European Commission evalua-tion the Enfer test correctly identified all positive andnegative samples48. After dilution, this test correctlydetected all samples diluted 10–1 and 10–1.5, but did notdetect any samples that were diluted 10–2. The mainadvantage of this assay is the rapidity and simplicity of themethod. In addition, the test makes a clear distinctionbetween positive and negative samples, thereby minimiz-ing problems with the interpretation of results. The maindisadvantage of this test is the potential for false-positivesowing to incomplete protease digestion of PrPC.
CEA/BioRad test. This test is a sandwich immunoassayfor PrP 27-30 that is carried out after denaturation andconcentration steps48,53. Two different monoclonalantibodies are used. The first antibody is immobilizedon the microplate before incubation with the solutioncontaining PrP 27-30, which is prepared by tissuehomogenization and digestion with proteinase K.Then the second antibody, which is coupled to anenzyme, is added to the plate and enzyme activity isdetected. In the original test evaluated by theEuropean Commission the enzyme was acetylcho-linesterase, but in recent commercial versions of thetest this enzyme was replaced by peroxidase, whichgives a lower background absorbance. During theevaluation, the CEA/BioRad test correctly identifiedall samples48. In the dilution assay, it correctly identi-fied all samples that were diluted 10–1, 10–1.5 and 10–2,and even identified 18 out of 20 samples that werediluted 10–2.5. The main advantage of this test is itssensitivity, which is comparable with the mouse infec-tivity bioassay54. For this reason, this test might be use-ful in pre-symptomatic diagnosis53. The main disad-vantages of the CEA/BioRad assay are that it is morelabour-intensive than the other methods and that ittakes longer to obtain results. The original version ofthis test took 24 hours to complete, but recentimprovements have reduced the time to approximately6 hours without significantly compromising the sensi-tivity of the test. However, this test has a higher rate offalse-positives owing to incomplete digestion of PrPC.
positive in the test) and specificity (the proportion ofhealthy reference animals that score negative in the test)as criteria, five tests were approved by the EuropeanCommission for BSE detection (for a detailed descrip-tion of these evaluations and their results, see REFS 49,50).All five tests are based on immunodetection of thepathological PrPSc isoform, and four use proteolysis todistinguish PrPC from misfolded PrP (TABLE 1).
Prionics-Check Western test. This test is designed to detectthe protease-resistant fragment of PrPres (PrP 27-30)51,52.Briefly, a piece of brain stem (usually the obex region)is homogenized, digested with proteinase K and resolvedby SDS–PAGE analysis. PrP 27-30 is detected by WEST-
ERN BLOT analysis using the monoclonal antibody 6H4(recognition sequence DYEDRYYRE)51. The testrequires at least 6–8 hours, and ~100 tests (and dupli-cates) can be performed each day by one person. Of the300 positive samples and 1,000 negative samples testedas part of the European Commission evaluation, allwere correctly detected using this test48. After the sam-ples were diluted 10–1, of 20 positive samples that weretested, 15 were correctly identified as positive, two asdoubtful and three as negative48. At the 10–1.5 dilution,three of the 20 positive samples were scored as doubtfuland the remainder were identified as negative. Belowthis dilution, the method cannot detect positive sam-ples48. The main advantage of the Prionics-CheckWestern test is the high level of reproducibility andthe reduced rate of false-positives that result fromincomplete protease digestion as compared with theenzyme-linked immunosorbent assay (ELISA) tests.This is because Western blotting distinguishesbetween incompletely digested PrPC and PrP 27-30because the molecular mass of PrP 27-30 is less thanthat of the full-length protein. Another possible advan-tage of the Prionics-Check Western test is that it mightaid the identification of new strains of prions throughanalysis of Western blot profiles. The main disadvan-tages of this method are the low sensitivity, lowthroughput and the laborious and time-consumingprocedure compared with ELISA tests.
Enfer test. This test is a high-throughput CHEMILUMINES-
CENT ELISA that can be completed in less than 4 hours.The assay comprises a unique, rapid sample-extractionprocedure that is coupled to a simple ELISA technique
WESTERN BLOT
A method of identifying proteinsand peptides that have beenelectrophoretically separatedand transferred ontonitrocellulose or nylonmembranes. Also calledimmunoblotting.
CHEMILUMINESCENCE
Light that is produced bytransformation of chemicalenergy.
Table 1 | Summary of the tests currently approved for post-mortem detection of altered PrP isoforms in cattle brain
Technique Principle Detection limit Advantages Disadvantages
Prionics-Check Gel electrophoresis and 5.0–20 pmol Good reproducibility, low Low throughput, low sensitivityWestern test Western blot rate of false-positives
Enfer test Simple ELISA 1.0–10 pmol Rapid and simple Potential for false-positives
CEA/Biorad test Sandwich ELISA using two 0.5–2.0 pmol High sensitivity Longer and more laborious; different antibodies potential for false-positives
Prionics-Check LIA Sandwich ELISA using two 1.0–5.0 pmol Rapid, automated and Variability depending on sample test different antibodies simple preparation; potential for false-positives
Conformational- Differential antibody binding 0.5–5.0 pmol Independent of protease Complicated and involves more stepsdependent immunoassay to native and denatured PrP digestion, high sensitivity than other tests
Detection limits were calculated based on estimates reported in previous publications29,31.
NATURE REVIEWS | MICROBIOLOGY VOLUME 2 | OCTOBER 2004 | 813
R E V I E W S
The need for a pre-symptomatic diagnosisAlthough TSEs are rare diseases in humans, theemergence of vCJD and the compelling experimentalevidence linking it to BSE5–7 have raised concerns abouta possible large epidemic in the human population5,58.Over the past few years, it has become clear that BSE is aserious problem and, despite the imposition of stringentprecautionary measures, the disease continues to spreadin some European countries and has recently beenreported in the United States, Canada and Japan, whereit has caused serious economic damage to the beefindustry59–61. Part of the problem is that many countrieshave not yet adopted routine inspection of animalsusing the BSE post-mortem rapid tests. In addition, onthe basis of the estimated detection limits (TABLE 1) it isunlikely that these tests can detect cattle that are incu-bating the disease at the pre-symptomatic stage59. So, itis possible that infected animals that do not show theclinical signs of BSE and that give a negative result usingthe available biochemical tests are still entering the foodchain and presenting a serious risk to human health.
Pre-symptomatic detection of CJD in living patientsis not currently possible29,31,59. If large numbers of peopleare incubating vCJD, the lack of a pre-symptomatic testraises concerns about the iatrogenic propagation of thedisease5,62. Iatrogenic spread of sCJD has already causedfatal disease in several hundred people owing to trans-mission of prions by medical or surgical interventionswith accidentally contaminated materials63. Iatrogenictransmission of sCJD has occurred in cases thatinvolved corneal transplants, implantation of electrodesin the brain, DURA MATER grafts, contaminated surgicalinstruments and treatment with human growth hor-mone derived from cadaveric pituitaries63. Although thisproves that sCJD can be horizontally transmitted, thelow incidence of iCJD indicates that the disease is notcontagious in the traditional sense. Family memberswho live with, or medical professionals that treat, sCJDpatients are not at a greater risk of contracting the dis-ease than the general population. However, in the caseof vCJD, the concern is increased because the concen-tration of disease-associated prion protein in peripherallymphoreticular tissues is much higher than in sCJD62,indicating that a different pattern of peripheral patho-genesis is involved. Indeed, although there is no evidencefor sCJD transmission by blood transfusion, a recentstudy reported the first possible case of vCJD contractedthrough blood transfusion64. A 69-year-old patientdeveloped vCJD symptoms 6.5 years after receiving atransfusion of red cells donated by an individual whodeveloped symptoms of vCJD 3.5 years after donatingthe blood. If the possibility of transmission of vCJD byblood transfusion is supported by the discovery ofsimilar cases, it could have serious implications for apotential vCJD epidemic, because it would indicate thatblood can harbour infectivity several years before theonset of clinical symptoms. Owing to this possibility, thedevelopment of a sensitive and pre-symptomatic bloodtest for CJD is a priority. Additional evidence for bloodtransfusion as a possible route of TSE transmissioncomes from elegant experiments by Houston and
Prionics-Check LIA test. This assay is a sandwich ELISAthat uses two different monoclonal antibodies to detectproteinase K-resistant PrP (REF. 55). Samples are firstincubated with one of the specific antibodies and themixture is transferred to another microtitre plate that iscoated with a second monoclonal antibody specific forPrP. The complexes are bound to this capture antibodyand become accessible for detection by a chemilumines-cence-producing reaction. The system is designed for a96-well format and can be fully automated from homog-enization to detection and analysis. Processing time is<4 hours. Sensitivity was 97.9% and specificity was100% in the European Commission evaluation50. In thedilution study, this test correctly identified the samplesthat had been diluted 10–1 or 10–2 depending on theexperimental conditions used for protease digestion andtissue homogenization. The advantages of this assay areits simplicity, automation and speed in obtaining theresults. Its disadvantages are the variable sensitivitydepending on the experimental conditions and thepotential for false-positives owing to undigested PrPC.
Conformational-dependent immunoassay (CDI) test.This test consists of a sandwich immunoassay withtime-resolved fluorescence detection using high-affinityrecombinant antibody fragments for the detection andcapture of PrP (REFS 56,57). The CDI test simultaneouslymeasures binding of specific antibody to denaturedand native forms of PrP. The detection antibody recog-nizes a conformation-dependent epitope, which,although always exposed in PrPC, only becomesexposed in PrPSc after denaturation56. Unlike otherassays that are used for the rapid detection of prions,the CDI test does not rely on the protease-resistantproperties of PrPSc. This allows the CDI test to measureboth the protease-sensitive and protease-resistantforms of misfolded PrP. The procedure consists ofhomogenization, enrichment of PrPSc and splitting ofthe sample into two aliquots, one of which is treatedwith a chaotropic agent (denaturated sample) while theother one is not (native sample). The samples are addedto microtitre plates that are coated with the Fab frag-ment of a recombinant capture antibody. After incuba-tion, a labelled detection antibody fragment is added.In its current state of development, this test takes lessthan 8 hours to complete. The results of the Europeanevaluation of this test showed 100% sensitivity andspecificity50. In the dilution series study, out of the fourpositive samples that were diluted 10–1.5, two wereclearly identified as positive and two were borderlinepositive. For positive samples diluted 10–2, one wasidentified as positive and two as borderline positive.The main advantage of this method is the distinctionbetween PrPC and PrPSc, making it independent of pro-tease digestion and thereby capable of detecting pro-tease-sensitive forms of misfolded PrP. In addition, ithas the potential to identify novel strains of prions thatare thought to arise from slightly different PrPSc confor-mations56. The main disadvantage of this technology isthat it is rather complicated and requires more stepsthan other rapid tests.
DURA MATER
The tough fibrous membranecovering the brain and spinalcord and lining the inner surfaceof the brain.
814 | OCTOBER 2004 | VOLUME 2 www.nature.com/reviews/micro
R E V I E W S
Difficulties of early diagnosisInfectious diseases are relatively easy to diagnose bio-chemically, either by the immune reaction that is pro-duced in response to the infectious agent or by theamplification of a nucleic acid that is specific to the agentusing PCR. However, in TSEs there is no immune reac-tion, because the infectious agent is a protein that hasthe same sequence as a protein that occurs naturally inthe body, and PCR is not useful because prions do notseem to contain nucleic acids that could potentially beamplified.
The animal bioassay of infectivity remains the onlymethod available to directly measure the presence of theinfectious agent and is, by far, the most sensitive methodavailable for the detection of prions31,71.Animal bioassayshave been extensively used in TSE research and diag-nostic testing. Although ruminants such as sheep andgoats were used in the first infectivity assays, the bio-assays have improved markedly with the introductionof rodent-adapted scrapie strains and by intracranialinoculation72.A further breakthrough in the detection ofprions by bioassay was achieved by the genetic engineer-ing of PrP transgenic mice. In particular, mice expressinghigh levels of human or bovine PrPC in a PrP-null back-ground have shown great potential as diagnostictools57,72–74. However, widespread use of bioassays arelimited by the length of time that it takes to obtain results(several months to years) and the species barrier effect.
PrPSc is not only the main component of the infec-tious agent and the most likely cause of TSE, it is also theonly validated surrogate marker for the disease2,31.Detection of PrPres in tissues and cells correlates widelywith presence of the disease and with the presence ofTSE infectivity75. Therefore, identification of PrPSc inhuman or animal tissues is considered important forTSE diagnosis. The main problem with a diagnosis thatis based on the detection of PrPSc is that the pathologicalform of PrP is abundant only at late stages of the diseasein the primary target organ — the brain. However,infectivity studies have shown that prions are also pre-sent in minute amounts in peripheral tissues, such aslymphoid organs and blood, at early stages of the dis-ease during the pre-symptomatic period29,76,77. At pre-sent, efforts are focused on increasing the sensitivity ofthe detection methods and/or designing procedures thatconcentrate or amplify the PrPSc marker in the sample(FIG. 4). The aim should be not only to detect prions inthe brain in early pre-symptomatic cases, but also togenerate a test for diagnosing the disease in living ani-mals and humans. For this purpose, a tissue other thanbrain is required, and to develop an easy, non-invasivetesting method, body fluids (such as urine or blood) arethe best candidates.
New approaches for early pre-mortem diagnosisAlthough no systematic studies have been under-taken, on the basis of the estimated sensitivities of thecurrent tests (TABLE 1), it is unlikely that they could beused to detect individuals at early stages of the infec-tious period59. It is also unlikely that they could detectPrPres in tissues other than the brain. This is essential
Hunter, in which transmission of BSE was shown tooccur by blood transfusion in sheep65,66. Interestingly, inthese experiments the blood that was used for transfu-sion was obtained from sheep that were midwaythrough the incubation period. Infectivity has alsobeen shown in blood during the incubation periodand symptomatic phase in a rodent model of vCJD67.These findings have important implications, not onlyfor TSE diagnosis, but also for several other applications,such as blood-bank safety and the plasma-productsindustry (FIG. 3).
Pre-symptomatic diagnosis is extremely importantfor the effective treatment of patients, as it wouldenable therapeutic intervention to start at an earlystage of the disease before the appearance of clinicalsigns and permanent brain damage. It is known thatby the time people exhibit clinical symptoms the brainalterations are extensive and most likely irreversible.The importance of early treatment is evident from thedata available from animal models, which shows thatseveral compounds can delay the onset of the disease,but that none, so far, has shown a significant effectwhen treatment has started at the symptomaticstage68–70.
Food industry
Blood banks andplasma products
Clinical trials
Organ transplant
Drugs from human origin
Brain surgery
Disease diagnosis
TSE diagnosis
Figure 3 | Diagrammatic representation of the need for a TSE biochemical diagnosis andthe many areas that might benefit. Increasing the safety of blood banks, plasma products anddrugs produced from human tissues would be possible with a sensitive test for prions. In addition,surgical manipulations of nervous tissue (for example, brain surgery and the use of cerebralelectrodes) and organ transplants could be made safer by a TSE diagnosis test. Finally, a sensitiveand quantitative test would enable early diagnosis with the consequent benefit of improving drugtreatment both by allowing the treatment to begin early and by improving the quality of clinicaltrials to evaluate new drugs.
NATURE REVIEWS | MICROBIOLOGY VOLUME 2 | OCTOBER 2004 | 815
R E V I E W S
by TSE has been reported84. However, a recent studyhas questioned the interpretation of these results,suggesting that the PrPres-like reactivity that wasdetected in urine was due to contamination with bac-terial proteins85. Nevertheless, neither urine nor anyof the other external tissues or peripheral fluids (withthe exception of blood) has ever been shown to beinfectious in humans or experimental animals29.Hence, blood seems the best option for a routinelynon-invasive diagnosis of TSE (BOX 2). Several strate-gies are being used to develop more sensitive tests andare described below.
Conformational antibodies. One objective that haslong been pursued is the production of PrPSc-specificconformational antibodies. Such antibodies might beuseful for the detection of small quantities of PrPSc influids and would eliminate the need for proteasedigestion, which decreases the amount of PrPSc anddetects only a subset of PrPSc species86. Consideringthe significant structural differences between PrPC
and PrPSc, it was originally thought that the produc-tion of conformational antibodies would be possible.However, attempts by many different research groupsusing several strategies have failed over severalyears86–88. In 1997, Korth and colleagues89 produced anantibody, called 15B3, that specifically immuno-precipitates bovine, murine or human PrPSc but notPrPC, indicating that it recognizes an epitope that iscommon to prions from different species89,90.However, the practical use of this antibody for priondiagnosis has not been pursued, most likely owingto its relatively low affinity for the protein. Attemptsto produce conformational antibodies have beenmore successful in recent years, leading to the identifi-cation of three putative PrPSc-specific antibodies. Oneof the new strategies that has been used to generateconformational antibodies is based on experimentsshowing that the creation of β-sheet structures inrecombinant PrP is associated with increased solventaccessibility of tyrosine residues91. As tyrosine is often
for the development of non-invasive tests that can beused in living individuals. An important milestonewas the discovery of PrPres in the tonsillar tissue ofvCJD patients36,78. Interestingly, there have been reportsof individual cases of detection of PrPres at preclinicalstages of the disease in sheep tonsil79 as well as in humanappendix80, indicating that a lymphoid tissue biopsymight be useful for diagnosing pre-symptomaticindividuals. Moreover, a recent screening of samplesfrom tonsil and appendix that were collected fromhospital histopathology departments across the UnitedKingdom showed three appendicectomy samples withlymphoreticular accumulation of PrPres, giving anestimated prevalence of 3 cases per 12,674 people or237 per million81. Although PrPres-positive lymphoidtissue was considered to be specific for vCJD36,62,recent studies have identified PrPres in as many as one-third of skeletal muscle and spleen samples82 andin the olfactory epithelium83 of patients sufferingfrom sCJD.
Routine laboratory diagnosis of any disease in pre-symptomatic individuals is limited to the examinationof external tissues or fluids such as hair, skin, saliva,sputum, urine, faeces or blood. Detection of a PrPres-likemolecule in the urine of humans and animals affected
BUFFY COAT
The component (1%) of wholeblood that contains leukocytesand platelets. Aftercentrifugation, the red bloodcells collect at the the bottom ofthe tube and the white bloodcells cover the red blood celllayer in a thin layer — the buffycoat — whilst the liquid plasmarises to the top.
a Sample with low concentration of PrPres
b Increase sensitivity
c Concentrate PrPres marker
d Amplify PrPres
marker
Figure 4 | Strategies to increase the sensitivity of TSE detection. At least three differentapproaches can be used to develop a highly sensitive diagnosis of TSE that can detect PrPSc
in samples containing a very low amount of the marker (a). b | Increase the sensitivity ofcurrent detection methods. c | Concentrate or enrich the amount of PrPres in the sample. d | Amplify the amount of PrPres to produce a solution containing a large concentration of the marker.
Box 2 | How close is a TSE blood test?
To evaluate the feasibility of a blood diagnosis for TSE, it is important to know the PrPSc concentration that isexpected to be present in the blood. From infectivity studies in rodent models of TSE, it seems that the maximumconcentration of infectivity in circulating blood resides in the BUFFY COAT, where it can be present at a level of 5–10infectious units (IU) ml–1 during the incubation period and then rise to around 100 IU ml–1 at the onset ofsymptomatic disease29,120–122. One picogram of PrPSc is estimated to contain 100 IU (REF. 29); therefore, theconcentration of PrPSc in the buffy coat is expected to be 1 pg ml–1 (~3 × 10–14 M) and 0.1 pg ml–1 (~3 × 10–15 M)during the symptomatic and pre-symptomatic phases, respectively. The concentrations of PrPSc in plasma and redblood cells are estimated to be at least 5–10-fold lower than in the buffy coat121. Therefore, for a test to succesfullydetect PrPSc in blood samples during the pre-symptomatic phase of the disease, it would have to detect the proteinin the femtomolar concentration range. In other words, such a test would have to detect as few as 60,000 moleculesof PrPSc, which is the amount that is estimated to be present in 100 µl of rodent blood. However, on the basis of thecomparison with the infectivity in brain, it is likely that in human and cattle blood samples, PrPSc concentrationsare even lower. According to these estimations and the sensitivity thresholds that have been reported for the testsunder development, detection levels of current tests are still approximately 2–4 orders of magnitude away fromreaching the sensitivities required for blood detection. It seems that a concentration or amplification step coupledwith some of the most sensitive assays might provide the required sensitivity. If these estimations are correct, ablood test for TSE is feasible.
816 | OCTOBER 2004 | VOLUME 2 www.nature.com/reviews/micro
R E V I E W S
spectra of many control and prion-infected samplesand, after derivatization and transformation, thespectra are used as an input for the artificial neuralnetwork analysis96,97. The software finds patterns inthe spectra that distinguish samples from healthy andsick animals. After the training and validation phases,the software can analyse unknown samples and classifythem as ‘normal’ or ‘infected’. This test was 97% sensi-tive and 100% specific for the identification of healthyand diseased cases using blood samples96. The tech-nology has also been used to detect infected animalsin the pre-symptomatic phase of the disease98. Theseintriguing findings are promising for the developmentof a blood test for the identification of TSEs. Themain disadvantage of this assay is that it is unclearwhat is being detected, as the analysis merely identifiesdifferences in the FTIR spectra of samples frominfected and uninfected individuals. In addition, themethod requires a high level of skill to measure andinterpret the results, so its widespread application forblood diagnosis would be difficult to implement.
Schmerr and colleagues at the US Department ofAgriculture have reported the development of amethod that is based on a combination of capillaryelectrophoresis and antigen/antibody competition99–101.In this assay, a fluorescein-labelled synthetic peptidewith a short PrP sequence is incubated with an anti-PrP antibody, and the concentrations are carefullyadjusted to produce binding to 50% of the peptide.This material is mixed with a sample that is treatedwith proteinase K and, if PrPres is present, it will dis-place the peptide from the antibody, thereby changingthe amounts of free and bound peptide101. Thischange can be measured by laser-induced fluores-cence during capillary zone electrophoresis. Using thismethod, PrPres has been detected in blood fromscrapie-infected sheep and elks with chronic wastingdisease100. The main disadvantages of this technologyare that it seems difficult to standardize and it doesnot directly measure PrPSc but instead depends on thecomparison of signal ratios among different samples.In addition, these results have not been reproduced inother laboratories and studies designed to measure PrPSc
in blood from CJD patients by capillary electrophoresishave consistently failed102.
PrPres concentration and specific ligands. An alternativestrategy to increase the sensitivity of PrPSc detection isto increase the concentration of the marker in thesample before detection (FIG. 4c). It has been reportedthat sodium phosphotungstic acid selectively precipi-tates PrPSc from different sources56,62. This procedure,coupled with an enhanced chemiluminescence detec-tion system, has been used to develop a highly sensi-tive test for identifying PrPSc in diverse samples. Usingthis assay, Wadsworth et al. have detected PrPSc in dif-ferent tissues from vCJD patients, including spinalcord, thymus, lymph nodes, tonsil, spleen, adrenalgland, rectum, retina and optic nerve62. However,detection of PrPSc in blood samples is not possibleusing this test.
found in the tyrosine–tyrosine–arginine repeat motif,animals were immunized with synthetic peptidescontaining this sequence. Several of the antibodiesthat were produced recognized PrPSc (but not PrPC)as shown by immunoprecipitation, plate-captureimmunoassays and flow cytometry91. Another reportedPrPSc-specific monoclonal antibody, called V5B2, wasgenerated against a carboxy-terminal PrP syntheticpeptide92. This antibody recognized PrPSc (but notPrPC) from humans affected by CJD, as shown by dotblot, ELISA, immunoprecipitation and immunohisto-chemistry analyses. Finally, it was recently reportedthat an anti-DNA antibody, called OCD4, capturedPrP from brains affected by prion diseases in bothhumans and animals but not from unaffectedcontrols93. OCD4 seems to immunoreact with DNA (ora DNA-associated molecule) that forms a conforma-tion-dependent complex with PrPSc in prion diseases.Although PrP that is immunocaptured by OCD4 islargely protease-resistant, some remains protease-sen-sitive. Further studies are needed to analyse the speci-ficity and usefulness of these three conformationalantibodies for TSE diagnosis.
Spectroscopic techniques. Several spectrophotometrictechniques are being developed with the aim of prod-ucing a sensitive test for PrPSc. Among these tech-niques are multispectral ultraviolet fluoroscopy(MUFS), confocal dual-colour fluorescence correla-tion spectroscopy (FCS), fourier-transformed infraredspectroscopy (FTIR) and fluorescence detectionafter capillary electrophoresis.
MUFS detects a specific fluorescent emission patternafter excitation in the ultraviolet range94. This techniquecan discriminate between PrPC and PrPSc and differentforms of PrPSc from different strains. The main strengthof this method is that it does not rely on antibodies orprotease digestion for detection of PrPSc, thereby pro-viding an alternative to the other tests. However, thesensitivity of this assay is still lower than ELISA orWestern blot tests.
In FCS, a laser beam excites single fluorescentmolecules in solution, which are detected by a confo-cal microscope equipped with a single photoncounter95. In this method, the sample is mixed withanti-PrP antibodies labelled with two different fluo-rescent dyes. PrPSc aggregates provide multiple sitesfor antibody binding, producing intensely fluorescentmolecules that can be scanned and separated frommonomeric PrPC. This technique seems to be moresensitive than Western blots and ELISA assays and wasshown to detect PrPSc in the cerebrospinal fluid of asubset of sCJD patients but not in healthy controls95.However, the widespread use of this technique for TSEdiagnosis does not seem feasible as the expensive andsophisticated equipment that is required is not readilyavailable.
Analysis of FTIR spectra of samples that containPrPSc by artificial neural networks has resulted in anassay that is sensitive enough to diagnose TSEs usingblood samples96. The assay measures the infrared
PROTEIN MISFOLDING
DISORDERS
A recently recognized group ofdiseases, which involve themisfolding, aggregation andtissue deposition of a protein.
NATURE REVIEWS | MICROBIOLOGY VOLUME 2 | OCTOBER 2004 | 817
R E V I E W S
ther study. In particular, the use of this technology inhuman diagnosis might be compromised by therequirement for normal brain homogenate as a sub-strate for the conversion process. This problem couldbe circumvented by the use of cellular extracts or byidentification of the factors that catalyse the amplifi-cation process.
Another strategy that is used to amplify PrPres is thecell infectivity assay115. This assay uses mouse neuro-blastoma N2a cell sublines that are highly susceptibleto mouse prions, as shown by the accumulation ofPrPres and infectivity116,117. In this assay, susceptibleN2a cells are exposed to prion-containing samplesand grown for several generations. The proportion ofcells that contain PrPres is determined with automatedcounting equipment. The dose-response to infectionis linear over two logs of prion concentrations.Furthermore, it has been claimed that the cell assay isas sensitive as the mouse bioassay, ten times faster, twoorders of magnitude less expensive and suitable forrobotization115. Prion replication has also been shownto occur in cells that are not of neural origin118.However, a potential problem with this assay is that,so far, no cellular systems have been available forpropagating prions from the most relevant cattle andhuman origins.
Conclusions and perspectivesTSEs are a major human and animal health problemand, owing to their infectious origin, the develop-ment of a method for early and sensitive diagnosis isessential to reduce further spread of disease. Thenature of the prion infectious material and the un-answered questions regarding the mechanism oftransmission have made the development of diagnos-tic procedures challenging. However, great progresshas been made in the past five years and several of thenew strategies are promising for the development of early, non-invasive detection of infected, but stillclinically unaffected, individuals. Some of theapproaches under development for TSE diagnosismight lead to applications in other areas, such as theearly detection of other neurodegenerative diseasesthat are associated with protein misfolding andaggregation (BOX 3). The goal for the future of prionresearch will be not only to reduce the risk of TSE prop-agation, but also to attempt to eradicate all infectiousforms of TSEs.
Several groups are attempting to identify ligandmolecules that are able to bind specifically to PrPSc.These molecules would be useful to precipitateminute quantities of the marker. They might also beused instead of conformational antibodies in ELISAor dot-blot assays. It has been reported that plas-minogen from human and mouse blood can specifi-cally interact with PrPSc, but not with PrPC or dena-tured PrPSc (REF. 103). Furthermore, plasminogenseems to bind PrPSc from multiple species104. Thesefindings represent the first naturally occurringendogenous PrP ligand that is able to bind differentlyto both PrP isoforms. However, it has been reportedby other groups that plasminogen also has a remark-able affinity for PrPC (REFS 105–107), which might com-promise its application for diagnosis. Another strat-egy that has been analysed takes advantage of theknown capacity of PrPSc to bind nucleic acids, in par-ticular RNA108–111. Artificial ligands (aptamers) havebeen identified by in vitro selection from a large ran-domized library of 2′-fluoro-modified RNA112. Oneof these ligands (aptamer SAF-93) was found to havemore than 10-fold higher affinity for PrPSc than forrecombinant PrPC and inhibited the accumulation ofPrPres in a cell-free conversion assay113,114. The suit-ability of this and other RNA aptamers for priondiagnosis remains to be evaluated.
PrPres amplification. An interesting alternative toincreasing the sensitivity of PrPSc detection is toincrease the amount of the marker that is present in asample (FIG. 4d). PMCA is an in vitro technique thatmimics the replication of prions in vivo 26. Samples aresubjected to cycles of incubation and sonication in thepresence of a large amount of normal PrPC. The num-ber of incubation–sonication cycles can be repeated asmany times as necessary to produce an exponentialincrease in the amount of PrPres. The procedure specifi-cally amplifies prions because, in the absence of theabnormal protein, PrPC is not converted26. Originally,PMCA was able to increase the sensitivity of detectionby 30–50 fold26, but in the current optimized and auto-mated procedure, the sensitivity is much greater, mak-ing it possible to detect PrPres at the concentrations atwhich it is predicted to be found in blood (C.S. andcolleagues, unpublished observations) (BOX 2). Theapplication of PMCA for TSE diagnosis and its sensi-tivity and specificity in relevant samples requires fur-
Box 3 | Applications of prion diagnostic assays to other protein misfolding disorders
In addition to TSEs, there are several other diseases that involve changes in the conformation of a natural protein toform an altered structure with toxic properties that is capable of inducing tissue damage and organdysfunction123,124. This group of diseases, called PROTEIN MISFOLDING DISORDERS, includes some of the most commonneurodegenerative diseases such as Alzheimer’s, Parkinson’s and Huntington’s disease as well as a group of morethan 15 distinct systemic disorders involving deposition of protein aggregates in diverse organs. The proteinconformational changes that are associated with the pathogenesis of these diseases also result in the formation ofabnormal proteins that are rich in β-sheet structure, partially resistant to proteolysis and highly likely toaggregate123. Some of the strategies under development for TSE diagnosis, such as the spectroscopic techniques andthe PMCA amplification procedure, might be applied to detect misfolded oligomeric markers of these diseases,leading to early and sensitive biochemical diagnosis of other protein misfolding disorders.
818 | OCTOBER 2004 | VOLUME 2 www.nature.com/reviews/micro
R E V I E W S
1. Collinge, J. Prion diseases of humans and animals: theircauses and molecular basis. Annu. Rev. Neurosci. 24,519–550 (2001).
2. Prusiner, S. B. Prions. Proc. Natl Acad. Sci. USA 95,13363–13383 (1998).
3. Johnson, R. T. & Gibbs,C. J. Jr. Creutzfeldt–Jakob diseaseand related transmissible spongiform encephalopathies. N. Eng. J. Med. 339, 1994–2004 (1998).
4. Will, R. G. et al. A new variant of Creutzfeldt–Jakob diseasein the UK. Lancet 347, 921–925 (1996).First report of variant CJD.
5. Collinge, J. Variant Creutzfeldt–Jakob disease. Lancet 354,317–323 (1999).
6. Bruce, M. E. ‘New variant’ Creutzfeldt–Jakob disease andbovine spongiform encephalopathy. Nature Med. 6,258–259 (2000).
7. Scott, M. R. et al. Compelling transgenetic evidence fortransmission of bovine spongiform encephalopathy prionsto humans. Proc. Natl Acad. Sci. USA 96, 15137–15142(1999).
8. Balter, M. Infectious diseases. Uncertainties plagueprojections of vCJD toll. Science 294, 770–771 (2001).
9. Aguzzi, A. Prions and the immune system: a journey throughgut, spleen, and nerves. Adv. Immunol. 81, 123–171 (2003).
10. Kimberlin, R. H. & Walker, C. A. Pathogenesis of scrapie inmice after intragastric infection. Virus Res. 12, 213–220(1989).
11. Banks, W. A., Niehoff, M. L., Adessi, C. & Soto, C. Passageof murine scrapie prion protein across the mouse vascularblood-brain barrier. Biochem. Biophys. Res. Commun. 318,125–130 (2004).
12. Mestel, R. Putting prions to the test. Science 273, 184–189(1996).
13. Chesebro, B. BSE and prions: uncertainties about theagent. Science 279, 42–43 (1998).
14. Soto, C. & Castilla, J. The controversial protein-only hypothesisof prion propagation. Nature Med. 10, S63–S67 (2004).
15. Cho, H. J. Is the scrapie agent a virus? Nature 262,411–412 (1976).
16. Alper, T., Haig, D. A. & Clarke, M. C. The exceptionally smallsize of the scrapie agent. Biochem. Biophys. Res. Commun.22, 278–284 (1966).
17. Alper, T. Scrapie agent unlike viruses in size andsusceptibility to inactivation by ionizing or ultravioletradiation. Nature 317, 750 (1985).
18. Bolton, D. C., McKinley, M. P. & Prusiner, S. B. Identificationof a protein that purifies with the scrapie prion. Science 218,1309–1311 (1982).Reports the identification of the prion protein as animportant constituent of the scrapie infectious agent,opening the door for the ‘protein-only’ hypothesis ofprion propagation.
19. Gabizon, R., McKinley, M. P., Groth, D. & Prusiner, S. B.Immunoaffinity purification and neutralization of scrapie prioninfectivity. Proc. Natl Acad. Sci. USA 85, 6617–6621 (1988).
20. Basler, K. et al. Scrapie and cellular PrP isoforms are encodedby the same chromosomal gene. Cell 46, 417–428 (1986).
21. Stahl, N. et al. Structural studies of the scrapie prion proteinusing mass spectrometry and amino acid sequencing.Biochemistry 32, 1991–2002 (1993).
22. Pan, K. M. et al. Conversion of α-helices into β-sheetsfeatures in the formation of scrapie prion poteins. Proc. NatlAcad. Sci. USA 90, 10962–10966 (1993).
23. Cohen, F. E. & Prusiner, S. B. Pathologic conformations ofprion proteins. Annu. Rev. Biochem. 67, 793–819 (1998).
24. Caughey, B. et al. Interactions and conversions of prionprotein isoforms. Adv. Protein Chem. 57, 139–169 (2001).
25. Kocisko, D. A. et al. Cell-free formation of protease-resistantprion protein. Nature 370, 471–474 (1994).
26. Saborio, G. P., Permanne, B., & Soto, C. Sensitive detectionof pathological prion protein by cyclic amplification of proteinmisfolding. Nature 411, 810–813 (2001).Reports the efficient conversion of PrPC into PrPSc
in vitro, which has many applications forunderstanding prion biology and for the developmentof high-sensitivity diagnostic assays.
27. Soto, C., Saborio, G. P. & Anderes, L. Cyclic amplification ofprotein misfolding: application to prion-related disorders andbeyond. Trends Neurosci. 25, 390–394 (2002).
28. Legname, G. et al. Synthetic mammalian prions. Science305, 673–676 (2004).Describes, for the first time, the generation ofinfectious prion protein in vitro. Although severalexperimental concerns have to be addressed, itrepresents an important step towards confirming theprion hypothesis.
29. Brown, P., Cervenakova, L. & Diringer, H. Blood infectivityand the prospects for a diagnostic screening test inCreutzfeldt–Jakob disease. J. Lab. Clin. Med. 137, 5–13(2001).
30. Collins, S. et al. Recent advances in the pre-mortemdiagnosis of Creutzfeldt–Jakob disease. J. Clin. Neurosci. 7,195–202 (2000).
31. Ingrosso, L., Vetrugno, V., Cardone, F. & Pocchiari, M.Molecular diagnostics of transmissible spongiformencephalopathies. Trends Mol. Med. 8, 273–280 (2002).
32. Kordek, R. The diagnosis of human prion diseases. FoliaNeuropathol. 38, 151–160 (2000).
33. Weber, T., Otto, M., Bodemer, M. & Zerr, I. Diagnosis ofCreutzfeld–Jakob disease and related human spongiformencephalopathies. Biomed. Pharmacother. 51, 381–387(1997).
34. Henry, C. & Knight, R. Clinical features of variantCreutzfeldt–Jakob disease. Rev. Med. Virol. 12, 143–150(2002).
35. Coulthard, A. et al. Quantitative analysis of MRI signalintensity in new variant Creutzfeldt–Jakob disease. Br. J. Radiol. 72, 742–748 (1999).
36. Hill, A. F. et al. Investigation of variant Creutzfeldt–Jakobdisease and other human prion diseases with tonsil biopsysamples. Lancet 353, 183–189 (1999).
37. Boellaard, J. W., Brown, P. & Tateishi, J.Gerstmann–Straussler–Scheinker disease — the dilemma ofmolecular and clinical correlations. Clin. Neuropathol. 18,271–285 (1999).
38. Ghetti, B. et al. Gerstmann–Straussler–Scheinker diseaseand the Indiana kindred. Brain Pathol. 5, 61–75 (1995).
39. Cortelli, P., Gambetti, P., Montagna, P. & Lugaresi, E. Fatalfamilial insomnia: clinical features and molecular genetics. J. Sleep Res. 8, S23–S29 (1999).
40. Jimi, T. et al. High levels of nervous system specific protein inthe cerebrospinal fluid in patients with early stageCreutzfeldt–Jakob disease. Clin. Chim. Acta 211, 37 (1992).
41. Hsich, G., Kenney, K., Gibbs, C. J. Jr, Lee, K. H. &Harrington, M. G. The 14-3-3 brain protein in cerebrospinalfluid as a marker for transmissible spongiformencephalopathies. N. Eng. J. Med. 335, 924 (1996).
42. Will, R. G. et al. Diagnosis of new variant Creutzfeldt–Jakobdisease. Ann. Neurol. 47, 575–582 (2000).
43. Miele, G., Manson, J. & Clinton, M. A novel erythroid-specific marker of transmissible spongiformencephalopathies. Nature Med. 7, 361–364 (2001).
44. Glock, B. et al. Transcript level of erythroid differentiation-related factor, a candidate surrogate marker fortransmissible spongiform encephalopathy diseases inblood, shows a broad range of variation in healthyindividuals. Transfusion 43, 1706–1710 (2003).
45. Bird, S. M. European Union’s rapid TSE testing in adult cattleand sheep: implementation and results in 2001 and 2002.Stat. Methods Med. Res. 12, 261–278 (2003).
46. Butler, D. Brussels seeks BSE diagnostic test to screenEuropean cattle. Nature 395, 205–206 (1998).
47. Heim, D. & Wilesmith, J. W. Surveillance of BSE. Arch. Virol.Suppl. 127–133 (2000).
48. Moynagh, J. & Schimmel, H. Tests for BSE evaluated.Bovine spongiform encephalopathy. Nature 400, 105(1999).
49. Moynagh, J. & Schimmel, H. The evaluation of tests for thediagnosis of transmissible spongiform encephalopathy inbovines. July 8, 1999. Report from the EuropeanCommission. [online],<http://europa.eu.int/comm/food/fs/bse/bse12_en.pdf>(1999).
50. Schimmel, H. et al. The evaluation of five rapid tests for thediagnosis of transmissible spongiform encephalopathy inbovines (2nd study). March 27, 2002. Report from theEuropean Commission. [online],<http://europa.eu.int/comm/food/fs/bse/bse42_en.pdf>(2002).References 48–50 report the results from theEuropean Commission evaluations of the rapid testsfor post-mortem BSE detection.
51. Schaller, O. et al. Validation of a western immunoblottingprocedure for bovine PrPSc detection and its use as a rapidsurveillance method for the diagnosis of bovine spongiformencephalopathy (BSE). Acta Neuropathol. (Berl.) 98,437–443 (1999).
52. Oesch,B. et al. Application of prionics Western blottingprocedure to screen for BSE in cattle regularly slaughteredat Swiss abattoirs. Arch. Virol. Suppl. 189–195 (2000).
53. Grassi, J. et al. Rapid test for the preclinical postmortemdiagnosis of BSE in central nervous system tissue. Vet. Rec.149, 577–582 (2001).
54. Deslys, J. P. et al. Screening slaughtered cattle for BSE.Nature 409, 476–478 (2001).
55. Biffiger, K. et al. Validation of a luminescence immunoassayfor the detection of PrPSc in brain homogenate. J. Virol.Methods 101, 79–84 (2002).
56. Safar, J. et al. Eight prion strains have PrPSc molecules withdifferent conformations. Nature Med. 4, 1157–1165 (1998).
57. Safar, J. G. et al. Measuring prions causing bovinespongiform encephalopathy or chronic wasting disease byimmunoassays and transgenic mice. Nature Biotechnol. 20,1147–1150 (2002).
58. Cousens, S. N., Vynnycky, E., Zeidler, M., Will, R. G. &Smith, P. G. Predicting the CJD epidemic in humans. Nature385, 197–198 (1997).
59. Schiermeier, Q. Testing times for BSE. Nature 409, 658–659(2001).
60. Donnelly, C. A., Ferguson, N. M., Ghani, A. C. & Anderson,R. M. Extending backcalculation to analyse BSE data. Stat.Methods Med. Res. 12, 177–190 (2003).
61. Nolen, R. S. Washington state dairy cow nation’s first caseof BSE. J. Am. Vet. Med. Assoc. 224, 345–346 (2004).
62. Wadsworth, J. D. et al. Tissue distribution of proteaseresistant prion protein in variant Creutzfeldt–Jakob diseaseusing a highly sensitive immunoblotting assay. Lancet 358,171–180 (2001).Describes the distribution of PrPres in diverse tissuesof patients affected by vCJD.
63. Brown,P. et al. Iatrogenic Creutzfeldt–Jakob disease at themillennium. Neurology 55, 1075–1081 (2000).
64. Llewelyn,C. A. et al. Possible transmission of variantCreutzfeldt–Jakob disease by blood transfusion. Lancet363, 417–421 (2004).Reports a case of vCJD that might have arisen after ablood transfusion from an individual incubating thedisease.
65. Houston, F., Foster, J. D., Chong, A., Hunter, N. & Bostock,C. J. Transmission of BSE by blood transfusion in sheep.Lancet 356, 999–1000 (2000).
66. Hunter, N. et al. Transmission of prion diseases by bloodtransfusion. J. Gen. Virol. 83, 2897–2905 (2002).
67. Brown, P. et al. Further studies of blood infectivity in anexperimental model of transmissible spongiformencephalopathy, with an explanation of why bloodcomponents do not transmit Creutzfeldt–Jakob disease inhumans. Transfusion 39, 1169–1178 (1999).
68. Aguzzi, A., Glatzel, M., Montrasio, F., Prinz, M. & Heppner, F. L.Interventional strategies against prion diseases. Nature Rev.Neurosci. 2, 745–749 (2001).
69. Dormont, D. Approaches to prophylaxis and therapy. Br. Med. Bull. 66, 281–292 (2003).
70. Rossi, G., Salmona, M., Forloni, G., Bugiani, O. & Tagliavini, F.Therapeutic approaches to prion diseases. Clin. Lab. Med.23, 187–208 (2003).
71. Field, E. J. & Shenton, B. K. Rapid diagnosis of scrapie inthe mouse. Nature 240, 104–106 (1972).
72. Baron, T. Mouse models of prion disease transmission.Trends Mol. Med. 8, 495–500 (2002).
73. Castilla, J. et al. Early detection of PrPres in BSE-infectedbovine PrP transgenic mice. Arch. Virol. 148, 677–691(2003).
74. Buschmann, A., Pfaff, E., Reifenberg, K., Muller, H. M. &Groschup, M. H. Detection of cattle-derived BSE prionsusing transgenic mice overexpressing bovine PrPC. Arch.Virol. Suppl. 75–86 (2000).
75. De Armond, S. J. et al. PrPSc in scrapie-infected hamsterbrain is spatially and temporally related to histopathologyand infectivity titer. Prog. Clin. Biol. Res. 317, 601–618(1989).
76. Aguzzi, A. Prion diseases, blood and the immune system:concerns and reality. Haematologica 85, 3–10 (2000).
77. Brown, P. The risk of blood-borne Creutzfeldt–Jakobdisease. Dev. Biol. Stand. 102, 53–59 (2000).
78. Hill, A. F., Zeidler, M., Ironside, J. & Collinge, J. Diagnosis ofnew variant Creutzfeldt–Jakob disease by tonsil biopsy.Lancet 349, 99–100 (1997).A short report describing for the first time the detectionof PrPres in human tonsil in a patient affected by vCJD.
79. Schreuder, B. E., van Keulen, L. J., Vromans, M. E.,Langeveld, J. P. & Smits, M. A. Preclinical test for priondiseases. Nature 381, 563 (1996).
80. Hilton, D. A., Fathers, E., Edwards, P., Ironside, J. W. &Zajicek, J. Prion immunoreactivity in appendix before clinicalonset of variant Creutzfeldt–Jakob disease. Lancet 352,703–704 (1998).
81. Hilton, D. A. et al. Prevalence of lymphoreticular prionprotein accumulation in UK tissue samples. J. Pathol. 203,733–739 (2004).Reports the results of the screening of 16,703samples of appendix or tonsil for PrPres. The findingsof this study allow an experimental estimation of thesize of the vCJD epidemic in the United Kingdom.
82. Glatzel, M., Abela, E., Maissen, M. & Aguzzi, A. Extraneuralpathologic prion protein in sporadic Creutzfeldt–Jakobdisease. N. Engl. J. Med. 349, 1812–1820 (2003).
83. Zanusso, G. et al. Detection of pathologic prion protein inthe olfactory epithelium in sporadic Creutzfeldt–Jakobdisease. N. Engl. J. Med. 348, 711–719 (2003).
NATURE REVIEWS | MICROBIOLOGY VOLUME 2 | OCTOBER 2004 | 819
R E V I E W S
84. Shaked, G. M. et al. A protease-resistant prion protein isoformis present in urine of animals and humans affected with priondiseases. J. Biol. Chem. 276, 31479–31482 (2001).
85. Furukawa, H. et al. A pitfall in diagnosis of human priondiseases using detection of protease-resistant prion proteinin urine: contamination with bacterial outer membraneproteins. J. Biol. Chem. 279, 23661–23667 (2004).
86. Groschup, M. H., Harmeyer, S. & Pfaff, E. Antigenic featuresof prion proteins of sheep and of other mammalian species.J. Immunol. Methods 207, 89–101 (1997).
87. Demart, S. et al. New insight into abnormal prion proteinusing monoclonal antibodies. Biochem. Biophys. Res.Commun. 265, 652–657 (1999).
88. Kascsak, R. J., Fersko, R., Pulgiano, D., Rubenstein, R. &Carp, R. I. Immunodiagnosis of prion disease. Immunol.Invest. 26, 259–268 (1997).
89. Korth, C. et al. Prion (PrPSc)-specific epitope defined by amonoclonal antibody. Nature 390, 74–77 (1997).
90. Korth, C., Streit, P. & Oesch, B. Monoclonal antibodiesspecific for the native, disease-associated isoform of theprion protein. Methods Enzymol. 309, 106–122 (1999).
91. Paramithiotis, E. et al. A prion protein epitope selective forthe pathologically misfolded conformation. Nature Med. 9,893–899 (2003).
92. Curin,S. et al. Monoclonal antibody against a peptide ofhuman prion protein discriminates betweenCreutzfeldt–Jacob’s disease-affected and normal braintissue. J. Biol. Chem. 279, 3694–3698 (2004).
93. Zou, W. Q., Zheng, J., Gray, D. M., Gambetti, P., & Chen, S. G.Antibody to DNA detects scrapie but not normal prionprotein. Proc. Natl Acad. Sci. USA 101, 1380–1385 (2004).References 91–93 describe the production ofantibodies that are specific for the pathologicalconformation of PrPSc.
94. Rubenstein, R., Gray, P. C., Wehlburg, C. M., Wagner, J. S.& Tisone, G. C. Detection and discrimination of PrPSc bymulti-spectral ultraviolet fluorescence. Biochem. Biophys.Res. Commun. 246, 100–106 (1998).
95. Bieschke, J. et al. Ultrasensitive detection of pathologicalprion protein aggregates by dual-color scanning forintensely fluorescent targets. Proc. Natl Acad. Sci. USA 97,5468–5473 (2000).
96. Lasch, P. et al. Ante-mortem identification of bovinespongiform encephalopathy from serum using infraredspectroscopy. Anal. Chem. 75, 6673–6678 (2003).
97. Kneipp, J., Lasch, P., Baldauf, E., Beekes, M. & Naumann, D.Detection of pathological molecular alterations in scrapie-infected hamster brain by Fourier transform infrared (FT-IR)spectroscopy. Biochim. Biophys. Acta 1501, 189–199 (2000).
98. Kneipp, J., Beekes, M., Lasch, P. & Naumann, D. Molecularchanges of preclinical scrapie can be detected by infraredspectroscopy. J. Neurosci. 22, 2989–2997 (2002).
99. Schmerr, M. J. & Jenny, A. A diagnostic test for scrapie-infected sheep using a capillary electrophoresisimmunoassay with fluorescent-labeled peptides.Electrophoresis 19, 409–414 (1998).
100. Schmerr, M. J. et al. Use of capillary electrophoresis andfluorescent labeled peptides to detect the abnormal prion
protein in the blood of animals that are infected with atransmissible spongiform encephalopathy. J. Chromatogr. A853, 207–214 (1999).
101. Jackman, R. & Schmerr, M. J. Analysis of theperformance of antibody capture methods usingfluorescent peptides with capillary zone electrophoresiswith laser-induced fluorescence. Electrophoresis 24,892–896 (2003).
102. Cervenakova, L. et al. Failure of immunocompetitive capillaryelectrophoresis assay to detect disease-specific prionprotein in buffy coat from humans and chimpanzees withCreutzfeldt–Jakob disease. Electrophoresis 24, 853–859(2003).
103. Fischer, M. B., Roeckl, C., Parizek, P., Schwarz, H. P. &Aguzzi, A. Binding of disease-associated prion protein toplasminogen. Nature 408, 479–483 (2000).
104. Maissen, M., Roeckl, C., Glatzel, M., Goldmann, W. &Aguzzi, A. Plasminogen binds to disease-associated prionprotein of multiple species. Lancet 357, 2026–2028(2001).
105. Kornblatt, J. A. et al. The fate of the prion protein in theprion/plasminogen complex. Biochem. Biophys. Res.Commun. 305, 518–522 (2003).
106. Shaked, Y., Engelstein, R. & Gabizon, R. The binding ofprion proteins to serum components is affected bydetergent extraction conditions. J. Neurochem. 82, 1–5(2002).
107. Praus, M. et al. Stimulation of plasminogen activation byrecombinant cellular prion protein is conserved in the NH2-terminal fragment PrP 23-110. Thromb. Haemost. 89,812–819 (2003).
108. Akowitz, A., Sklaviadis, T. & Manuelidis, L. Endogenous viralcomplexes with long RNA cosediment with the agent ofCreutzfeldt–Jakob disease. Nucleic Acids Res. 22,1101–1107 (1994).
109. Deleault, N. R., Lucassen, R. W. & Supattapone, S. RNA molecules stimulate prion protein conversion. Nature 425, 717–720 (2003).
110. Gabus, C. et al. The prion protein has RNA binding andchaperoning properties characteristic of nucleocapsid proteinNCP7 of HIV-1. J. Biol. Chem. 276, 19301–19309 (2001).
111. Weiss, S. et al. RNA aptamers specifically interact with theprion protein PrP. J. Virol. 71, 8790–8797 (1997).
112. Rhie, A. et al. Characterization of 2′-fluoro-RNA aptamersthat bind preferentially to disease-associated conformationsof prion protein and inhibit conversion. J. Biol. Chem. 278,39697–39705 (2003).
113. Proske, D. et al. Prion-protein-specific aptamer reducesPrPSc formation. Chembiochem 3, 717–725 (2002).
114. Sayer, N. M. et al. Structural determinants ofconformationally selective, prion-binding aptamers. J. Biol.Chem. (2004).
115. Klohn, P. C., Stoltze, L., Flechsig, E., Enari, M. &Weissmann, C. A quantitative, highly sensitive cell-basedinfectivity assay for mouse scrapie prions. Proc. Natl Acad.Sci. USA 100, 11666–11671 (2003).Describes the application of cell infectivity assays forthe detection of PrPSc.
116. Enari, M., Flechsig, E. & Weissmann, C. Scrapie prionprotein accumulation by scrapie-infected neuroblastomacells abrogated by exposure to a prion protein antibody.Proc. Natl Acad. Sci. USA 98, 9295–9299 (2001).
117. Bosque, P. J. & Prusiner, S. B. Cultured cell sublines highlysusceptible to prion infection. J. Virol. 74, 4377–4386(2000).
118. Vorberg, I., Raines, A., Story, B. & Priola, S. A.Susceptibility of common fibroblast cell lines totransmissible spongiform encephalopathy agents. J. Infect. Dis. 189, 431–439 (2004).
119. Jarrett, J. T. & Lansbury, P. T. Jr. Seeding ‘one-dimensionalcrystallization’ of amyloid: a pathogenic mechanism inAlzheimer’s disease and scrapie? Cell 73, 1055–1058(1993).
120. Brown, P. Creutzfeldt–Jakob disease: blood infectivity andscreening tests. Semin. Hematol. 38, 2–6 (2001).
121. Brown, P. et al. The distribution of infectivity in bloodcomponents and plasma derivatives in experimental modelsof transmissible spongiform encephalopathy. Transfusion38, 810–816 (1998).
122. Holada, K. et al. Scrapie infectivity in hamster blood isnot associated with platelets. J. Virol. 76, 4649–4650(2002).
123. Soto, C. Protein misfolding and disease; protein refoldingand therapy. FEBS Lett. 498, 204–207 (2001).
124. Carrell, R. W. & Lomas, D. A. Conformational disease.Lancet 350, 134–138 (1997).
AcknowledgementsThe author would like to thank J. Castilla, P. Saa, K. Abib and C.Hetz for critical reading of the manuscript. This work was sup-ported in part by the National Institutes for Health. Dr Soto is amember of the European Commission project TSELAB.
Competing interests statementThe author declares no competing financial interests.
Online links
DATABASESThe following terms in this article are linked online to:Entrez: http://www.ncbi.nlm.nih.gov/Entrez/prion proteinInfectious Disease Information:http://www.cdc.gov/ncidod/diseases/index.htmbovine spongiform encephalopathyOMIM: http://www.ncbi.nlm.nih.gov/Omim/Creutzfeldt–Jakob disease | fatal familial insomnia |Gerstmann–Sträussler–Sheinker syndrome | kuru
FURTHER INFORMATIONEuropean Commission prion research network:http://europa.eu.int/comm/research/press/2004/pr2805en.cfmWHO CJD factsheet:http://www.who.int/mediacentre/factsheets/fs180/en/Access to this links box is available online.