Nagib Yassin ESTATÍSTICA EXPERIMENTAL ESTATÍSTICA EXPERIMENTAL
Development and Experimental Evaluation of Oral ... - CiteSeerX
-
Upload
khangminh22 -
Category
Documents
-
view
0 -
download
0
Transcript of Development and Experimental Evaluation of Oral ... - CiteSeerX
Hiroyuki IshiiInstitute for Biomedical Engineering,Waseda University,Waseda Tsurumaki-cho 513, Shinjuku-ku,Tokyo 162-0041, Japan
Hiroki KogaYuichi ObokawaGraduate School of Science and Engineering,Waseda University, 3-4-1 Ookubo,Shinjuku-ku,Tokyo 162-0041, Japan
Jorge SolisFaculty of Science and Engineering,Waseda University, 3-4-1 Ookubo,Shinjuku-kuTokyo 169-8555, Japan
Atsuo TakanishiFaculty of Science and Engineering andHumanoid Research Institute,Waseda University,3-4-1 Ookubo, Shinjuku-ku,Tokyo 162-0041, Japan
Akitoshi KatsumataDepartment of Oral Radiography,Asahi University,1851-1 Hozumi,Mizuho-shi, Gifu 501-0296, Japan
Development andExperimental Evaluationof Oral RehabilitationRobot that ProvidesMaxillofacial Massage toPatients with OralDisorders
Abstract
We have developed an oral-rehabilitation robot WAO-1 (WasedaAsahi Oral-rehabilitation robot No. 1) for use in cases of oral disor-ders such as temperomandibular joint (TMJ) disorder and dry mouth.WAO-1 is the first robot designed to provide massage to the facial tis-sues of a patient with oral disorders. This robot provides massage tothe masseter and temporal muscles and to the parotid gland and duct
The International Journal of Robotics ResearchVol. 28, No. 9, September 2009, pp. 1228–1239DOI: 10.1177/0278364909104295c� The Author(s), 2009. Reprints and permissions:http://www.sagepub.co.uk/journalsPermissions.navFigures 1, 3–6, 10, 11, 13–15 appear in color online: http://ijr.sagepub.com
with simple operation. It consists of two six-degree-of-freedom armswith plungers, a body with headrest, a control box, a PC, and anautomatic massage trajectory generation system with virtual compli-ance control. Two evaluation experiments were performed to verifythe effectiveness of the oral massages of WAO-1 compared with themassages given by doctors. In the experiments, the massage to theparotid gland and duct by WAO-1 increased the amount of saliva inthe subjects, and the massage to the masseter muscle by WAO-1 in-creased facial skin temperature and width of the masseter muscle inthe subjects. We consider that these results indicate that massage byWAO-1 can be effective for patients with oral disorders.
KEY WORDS—medical robot� rehabilitation robot� temper-omandibular joint disorder� dry mouth� impedance control�maxillofacial massage.
1228
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
Ishii et al. / Development and Experimental Evaluation of Oral Rehabilitation Robot that Provides Maxillofacial Massage 1229
1. Introduction
In advanced countries, regional disparities in medical ser-vices, increased medical expense caused by aging societies,and shortages of doctors have become serious problems. Withthis in mind, several researchers have been developing medicalrobots as solutions to these problems. We consider that theserobots can be roughly classified into three groups according tothe development concept. The first group consists of robots foradvanced medical treatments that medical doctors are unableto perform using conventional medical tools. Da Vinci, Zeusand other surgical robots are classified into this group (Lan-genburg et al. 2003� Bann et al. 2004� Darzi and Munz 2004�Klein et al. 2007). The second group consists of robots thatperform simple but laborious medical tasks instead of medicaldoctors or other medical professionals. WTA and other manip-ulators used to hold medical implements are classified into thisgroup (Sadamitsu et al. 2006). The third group consists of ro-bots that support the motion of patients. HAL and other powerassist systems for rehabilitation are classified into this group(Lee and Sankai 2002� Hayashi et al. 2005� Krebs et al. 2007).We have developed a novel medical robot for oral disordersthat can be classified into the second group.
Today, many people suffer from oral disorders such as tem-poromandibular joint (TMJ) disorders and dry mouth. TMJdisorders are a group of conditions that cause pain and dys-function in the jaw joint and the muscles that control jawmovement. Some estimates suggest that over 10 million Amer-icans are affected by TMJ disorder (Westesson 1993�Haskin etal. 1995� NIH 2006a). Dry mouth is also one of the oral disor-ders that induce people to feel a shortage of saliva in the mouth(NIH 2006b). All people might occasionally experience suchshortages of saliva when they are nervous, upset, under stress,or taking certain medications. People with dry mouth conditionfeel this shortage of saliva all of the time. Some estimates sug-gest that 10% of the population have dry mouth, and one sug-gests that 25% of all elderly people have dry mouth (Billingset al. 1996� Nederfors 2000� Field et al. 2001� NIH 2006b).Elderly people with dry mouth sometimes have the conditioncomplicated by deglutition disorder and gustatory anesthesia.
Patients with these oral disorders are treated in depart-ments of oral and maxillofacial surgery and dental clinics,where therapeutic drugs and physiotherapy are provided (NIH2006a,b). Some studies have reported the effectiveness of oralmassage for TMJ disorders and dry mouth (DeBar et al. 2003�Riley et al. 2007). However, oral massage has not become pop-ular, and only a limited number of patients receive it. One rea-son for its lack of popularity is the fact that no treatment proto-col has been established. The other is that providing massageto patients represents heavy work for doctors. Thus, we con-sider that a machine capable of providing facial massages forpatients suffering with oral disorders would be welcomed.
Several companies, such as Panasonic and Human Touch,sell massage chairs that provide massage to the human body.
Fig. 1. WAO-1 (Waseda Asahi Oral-rehabilitation RobotNo.1). This robot massages the face of a patient whose headis positioned on a rest mounted on the robot’s body.
However, these chairs provide massage only below the neck,making them, of course, ineffective for oral disorders. On theother hand, some companies sell facial massage machines.However, these are developed to act on the skin, rather thanthe facial tissues associated with oral disorders, meaning thatthey are ineffective for oral disorders.
Takanobu et al. (2003) and Okino et al. (2004) developedopening jaw robots WY-5 and WY-6 and reported their effec-tiveness for people unable to open their mouths by themselvesbecause of severe TMJ disorders. However, these robots arenot effective for people in the first stages of TMJ disordersand dry mouth.
Consequently, we developed an oral-rehabilitation robotWAO-1 (Waseda Asahi Oral-rehabilitation robot No. 1� seeFigure 1) that provides massages to the facial tissues to treatTMJ disorders and dry mouth. WAO-1 is the first robot de-veloped for this aim. WAO-1 consists of two six-degree-of-freedom (DOF) arms and a body with a headrest. Like humandoctors, this robot provides massages to a patient’s facial tis-sues via these two arms, which are automatically computer-controlled. In this paper we describe WAO-1 in detail. We alsodescribe an evaluation test with a head mannequin and a pre-clinical test with healthy people.
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
1230 THE INTERNATIONAL JOURNAL OF ROBOTICS RESEARCH / September 2009
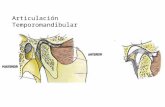
Fig. 2. Maxillofacial tissues associated with TMJ disorder (NIH 2006a).
2. Maxillofacial Anatomies Associated with TMJDisorders and Dry Mouth
2.1. TMJ Disorders
TMJ disorders are a group of conditions that cause painand dysfunction in the jaw joint and the muscles that con-trol jaw movement (Figure 2). In the NIH report, three ma-jor symptoms are described. The first is “myofacial pain, themost common temporomandibular disorder, involving discom-fort or pain in the muscles that control the jaw function”.The second is “internal derangement of the joint, involvinga displaced disc, dislocated jaw, or injury to the condyle”.The third is “arthritis, which refers to a group of degenera-tive/inflammatory joint disorders that can affect the temporo-mandibular joint”. This report also describes how a person mayhave one or more of these conditions at the same time.
In clinical treatment, a stabilization splint (also called anoral appliance or bite guard), which is a plastic guard that fitsover the upper or lower teeth, is the most widely used formof treatment for TMJ disorders, and several studies have re-ported, although not conclusively, its effectiveness in provid-ing pain relief. Patients with severe TMJ disorders are some-times treated surgically, although the NIH report states thatsurgical treatments should be avoided whenever possible.
Some studies have reported the effectiveness of oral mas-sages for TMJ disorders. In these studies, pain relief is reportedas a major goal of oral massage. However, the means by whichoral massages provide pain relief has not been clarified. The
massages applied to the oral muscles probably induce relax-ation and increased blood flow, hence providing pain relief topatients with TMJ disorders.
2.2. Dry Mouth
Dry mouth (also called Xerostomia) is one of the oral disordersthat induce people to feel a shortage of saliva in the mouth.Such a condition can be provoked for several reasons, such asdiabetes mellitus, kidney diseases, stress, drugs, etc. The mainsymptoms include dehydration, pain in the oral cavity, and ab-normalities in the sensation of tasting. Since saliva helps the di-gestion of foods, protects teeth from decay, and prevents infec-tion by controlling bacteria, severe dry mouth induces seriouscomplications, such as difficulty in tasting, chewing, swallow-ing, and speaking. Dry mouth also increases the risk of dentaldecay and other infections in the mouth.
Nowadays, pharmacotherapy and physiotherapy are themain treatment procedures administered to patients to stimu-late saliva production. In addition, some studies have reportedthe effectiveness of oral massages for dry mouth. Saliva isproduced mainly from three sorts of glands: sublingual, sub-mandibular, and parotid (Figure 3). The oral massages fordry mouth are administered to the parotid gland, because ofits significant contribution to saliva production. The therapeu-tic treatment consists of administering massage to the parotidgland and its excretory ducts to stimulate salivary flow. Themassage includes both petrissage and effleurage manipulation
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
Ishii et al. / Development and Experimental Evaluation of Oral Rehabilitation Robot that Provides Maxillofacial Massage 1231
Fig. 3. Maxillofacial tissues associated with dry mouth.
Table 1. Range of massage force.
Maximum (N) 20
Appropriate (N) 5–15
techniques. Petrissage manipulation is useful in directly stimu-lating the specific target organ, while effleurage manipulationprovides indirect stimulation by rubbing the skin surface.
3. Required Specifications of theOral-rehabilitation Robot
3.1. Massage Ability
The oral-rehabilitation robot massages the oral muscles, suchas the masseter and temporal muscles, and the facial tissuesassociated with saliva production, such as the parotid glandand duct. Therefore, using as a reference the “average Japanesemale’s head” provided by the Advanced Industrial Science andTechnology in Japan, we fixed the target area on the face wherethe robot gives its massage (Figure 4).
To decide on the specifications of the oral-rehabilitation ro-bot, we visited three hospitals and interviewed seven medicaldoctors. Based on the results of these interviews, we fixed therange of massage force as shown in Table 1.
3.2. Safety
For medical robots, safety is the key issue. The medical robotmust not endanger patients under any circumstances. There-fore, we had to consider the safety of the oral rehabilitation ro-bot before we designed it. Accidents that result in injury to the
Fig. 4. Massage target area based on “average Japanese male’shead” (units are in millimeters).
patient or the operator can possibly occur during the massage.The facial tissues and necks of patients are especially sensi-tive, and applying too much massage force can cause seriousproblems. The oral rehabilitation robot must not cause theseaccidents even if the following unexpected events or problemsoccur.
(a) The patient moves their head.
(b) The PC that controls the robot experiences problemssuch as unexpected shut down, freeze-up, and runaway.
(c) The power supply unit experiences fluctuation in volt-age.
3.3. Usability
The oral-rehabilitation robot is developed for use by doctorsor other medical professionals in hospitals and dental clinics,meaning it should be easy to operate. Therefore, the oral re-habilitation robot should be capable of being operated by anoperator who is given instructions via a graphical user inter-face.
4. Design and Control of WAO-1
4.1. Overview
WAO-1 is illustrated in Figure 5, and its specifications areshown in Table 2. WAO-1 consists of two six-DOF arms witha plunger, a body with a headrest, a control box, and a com-puter. WAO-1 massages the patient’s face by pressing or rub-bing with a plunger. The motion of the plunger is automaticallycomputer-controlled. A demonstration video of the maxillofa-cial massage by WAO-1 can be found online (see Extension 1).
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
1232 THE INTERNATIONAL JOURNAL OF ROBOTICS RESEARCH / September 2009
Fig. 5. Photographs of WAO-1.
Table 2. Specifications of WAO-1.
Height (mm) 782
Width and length (mm) 600� 482
Weight (kg) 120
DOF configuration 12
Supply voltage (V) 100 (AC)
Power consumption (W) 500 (Max)
Control PC CPU 3.4 GHz (Pentium VI)
OS Windows XP
4.2. Six-DOF Arm
WAO-1 has two six-DOF arms with a plunger. By moving theplungers on the human face, WAO-1 applies physical stimula-tion in the form of pressing or rubbing the facial tissues. Eacharm consists of a two-DOF linear actuator and a four-DOF se-rial manipulator on it, as shown in Figure 6. A two-DOF linearactuator consists of two active orthogonally crossed linear ac-tuators, while a four-DOF serial manipulator consists of fouractive rotational joints. Each joint consists of a DC servomotorand a harmonic drive gear. Several positional limit sensors arealso implemented in each arm. These limit sensors send a stopsignal to the control circuit once an active joint moves beyondits safety range.
A six-axis force and torque sensor (IFS-50M31A25-I25,Nitta Ltd) is fixed at the end-effecter of each arm, and aplunger is mounted on the sensor. The six-axis force/torquesensor measures the reaction force exerted by the facial tissues
Fig. 6. DOF arrangement of the six-DOF arm.
on the plunger. Data from the sensors are used in the virtualcompliance control system, as described in Section 4.5. Theplunger is mounted on the sensor via a simple lock–releasemechanism� hence, operators can easily change it by handwithout any implements.
A force limit mechanism (TG16, Tsubakimoto Cain Co.) isimplemented in each arm to guarantee patient safety. It stopstransmitting force when the reaction force exerted by the facialtissues on the plunger is over 40 N. This safety mechanismworks independently, requiring neither sensors nor actuators,meaning it works even when the PC or power supply is op-erating under unstable conditions. Therefore, this mechanismguarantees that the plunger does not apply more than 40 N tothe facial tissues. Owing to this mechanism, WAO-1 satisfiesthe requirements for safety described in Section 3.2.
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
Ishii et al. / Development and Experimental Evaluation of Oral Rehabilitation Robot that Provides Maxillofacial Massage 1233
Table 3. List of plungers (hardness was measured using an ASKER Durometer Type C).
No. Name Passive joint Material Hardness*
1 Plastic hemisphere No Plastic silicon 80
2 Plastic ball roller Rotational � 1 Plastic silicon 80
3 Soft ball roller Rotational � 1 Ultra soft urethane 15
4 Plastic roller Rotational � 1 Plastic silicon 80
5 Soft roller Rotational � 1 Ultra soft urethane 15
6 Ball joint Omni-directional � 1 Ceramics Over 100
Fig. 7. System configuration of WAO-1.
4.3. Plunger
Five different kinds of plungers have been prepared for usewith WAO-1 (Table 3). The operator can choose the bestplunger for a patient according to their disorder.
4.4. System Configuration and Process
The WAO-1 system configuration is shown in Figure 7. Be-fore starting the massage, the medical doctor chooses the mas-sage type and then decides the massage starting point. Beforeinputting the massage starting point, the doctor should knowwhich tissues are related to the patient’s disorder. Having de-termined the location of these tissues by palpation or diagnos-tic imaging, the doctor then decides the massage starting point.In addition, the doctor chooses the massage force and time pe-riod. After the doctor gives these parameters to the robot viathe graphical user interface on the PC monitor, the massagetrajectory generator and the unit automatically generate a mas-sage trajectory. The doctor then pushes the start button on theinterface to start the massage. During the massage WAO-1 iscontrolled as described in Section 4.5. When the massage pe-riod is over, WAO-1 automatically stops the massage. A sys-tem monitor timer monitors the program operation. It keeps
sending a monitor signal to the control circuit and stops send-ing only when the operating system program stops working asa result of problems with the PC such as freeze-up or runaway.When it fails to receive the monitor signal, the control circuitshuts off the energy supply to the motors, which then stop.Owing to this monitoring system, WAO-1 immediately stopsits operation whenever it might lose control as the result of PCproblems. This monitoring system also contributes to patientsafety.
Furthermore, both the operator and the patient have imme-diate access to stop buttons. Whenever either pushes the but-ton, a stop signal is sent to the control circuit. When it receivesa stop signal, the control circuit shuts off the energy supply tothe motors. This stop-button also contributes to the safety ofthe patient.
4.5. WAO-1 Control System
The control system of WAO-1 includes an automatic massagetrajectory generation module based on a reference magneticresonance imaging (MRI) image (Figure 8) and the virtualcompliance control module (Figure 9). The automatic mas-sage trajectory generation module was originally developed
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
1234 THE INTERNATIONAL JOURNAL OF ROBOTICS RESEARCH / September 2009
Fig. 8. Automatic massage trajectory generation based on aMRI image. (a) MRI image of an adult male, on which thetarget massage trajectory xtg is calculated. (b) Block diagramof automatic massage trajectory generator.
for WAO-1. This is the first time that virtual compliance con-trol has been used for facial massage. With this control system,WAO-1 provides six massage procedures: pressing massetermuscle, rubbing masseter muscle, pressing temporal muscle,rubbing temporal muscle, pressing parotid gland, and rubbingparotid duct. The massage trajectory of each arm is calculated,respectively, as described in the following.
In the case of rubbing, WAO-1 moves the plungers alongto the muscles or the duct. Before massage is started, the au-tomatic massage trajectory generator automatically calculatesa target massage trajectory xtg according to the parameters in-putted by the medical doctor as shown in Figure 8(b). A fa-cial shape model around the masseter muscle, temporal mus-cle, and parotid gland obtained from a reference MRI image ofan adult male is recorded in this generator. Depending on thetarget organ, this model generates a surface line xs of the targetorgan. In addition, according to the target massage force Ftg,the elastic compensator calculates the amount of pressing xec
based on a facial elastic model of the adult male that representsthe elastic modulus that previously has been experimentallyobtained of each facial tissue such as fat (“A” in Figure 8(a)),muscle (“B” in Figure 8(a)), and gland (“C” in Figure 8(a)).The target massage trajectory xtg is then calculated as the sumof xs and xec.
In the case of pressing, WAO-1 circularly moves theplungers on the muscle or the gland. Depending on the tar-get organ, the facial surface model generates a circle line xs
on the target organ. According to the target massage force Ftg,the elastic compensator calculates the amount of pressing xec
based on the facial elastic model. The target massage trajectoryxtg is then calculated as the sum of xs and xec.
The automatic massage trajectory generator generates themassage trajectories based on the facial shape model of anadult male. Obviously, the shapes of individual faces are differ-ent. Therefore, virtual compliance control is then implementedso that these massage trajectories can be applied to other peo-ple.
During massage, the virtual compliance calculator calcu-lates compliance displacement xcc based on the reaction forcefrom the face measured by the six-axis force/torque sensor inreal time, as shown in Figure 9. The basic idea of virtual com-pliance control is expressed in Equation (1) (Sugahara et al.2005):
Fre�t� � K � xcc�t�� C � �xcc�t� (1)
where Fre(t) is force and torque vector measured by the six-axis force/torque sensor at time t, xcc(t) is compliance displace-ment vector at time t, �xcc�t� is compliance velocity vector attime t, K and C donate the stiffness and dumping matrices, re-spectively. The compliance position of the plunger at t ��t iscalculated by the approximation of Equation (1) as expressedin the following equation:
xcc�t ��t� ��
K � C
�t
��1
��
Fre�t�� Cxcc�t�
�t
�(2)
where �t depends on the specification of the control PC andcontrol cycle. In WAO-1, �t is 5 ms.
The values of xcc(t) and xtg(t) of each arm are calculated,and the massage trajectory of each arm xre f (t) is calculatedas the sum of xcc(t) and xtg(t) of each arm. Each arm is thencontrolled to move the plunger according to the obtained tra-jectory.
5. Evaluation Test with a Head Mannequin
5.1. A Head Mannequin
To verify the massage ability of WAO-1, we developed a headmannequin (Figure 10) (Katsumata et al. 2008). This man-nequin consists of a skull made from hard resin, dummy skinmade from soft silicone, and a six-axis force/torque sensor.The sensor embedded in the mannequin measures forces Fx ,Fy , Fz , and torques Mx , My , Mz exerted on the mannequin.Thus, this mannequin is useful for comparing the massageforce provided by WAO-1 with that provided by a doctor.
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
Ishii et al. / Development and Experimental Evaluation of Oral Rehabilitation Robot that Provides Maxillofacial Massage 1235
Fig. 9. Control diagram of virtual compliance control module.
Fig. 10. Head mannequin with six-axis force/torque sensor.The sensor measures the force exerted on the facial surfaceof the mannequin.
5.2. Comparison Between Doctor’s Massage and WAO-1’sMassage
Figure 11 shows the massage forces exerted by WAO-1 and bya doctor who is an expert in oral massage during rubbing andpressing massages. In the case of pressing the masseter musclewith a circular massage trajectory, the average massage forcesexerted by WAO-1 and the doctor are at the same level. Inaddition, the massage forces exerted by WAO-1 and the doc-tor change periodically. The results of fast Fourier transform(FFT) show that the frequency of the doctor’s waveform isaround 2.5 Hz while that of WAO-1 is around 1.9 Hz. Thus,the pressing massage by WAO-1 is expected to be as effec-tive as that provided by the doctor. In the case of rubbing theparotid duct, the average massage forces of the doctor andWAO-1 are at the same level, while the waveform of the doc-tor changes more smoothly than that of WAO-1. However, therubbing massage of both WAO-1 and the doctor are expectedto be effective.
6. Experimental Evaluation of WAO-1
6.1. Experimental Verification of Virtual ComplianceControl
In our system, the massage trajectories are calculated based ona facial shape model of an adult male, and then virtual compli-
ance control is implemented so that these massage trajectoriescan be applied to many people. Thus, the effectiveness of ourvirtual compliance control should be verified before WAO-1 isapplied to real patients with oral disorders. In this verificationexperiment, WAO-1 provided rubbing massages with the softurethane ball roller plunger to the parotid duct of a subject,different from the adult male who provided the facial shapemodel. The massage trajectory with/without the virtual com-pliance control is shown in Figure 12. The reaction forces ex-erted on the facial tissues by the right arm and the left arm dur-ing massage are shown in Figure 13(a) with the virtual com-pliance control and in Figure 13(b) without the virtual compli-ance control.
In Figure 12, the trajectories generated with the virtualcompliance control are more rounded and seem to fit well witha facial shape while those generated without the virtual com-pliance control are less rounded and seem to not fit well witha facial shape. Comparing Figure 13(a) with (b), the massageforces exerted by the right arm and the left arm seem very sim-ilar with virtual compliance control while they do not seemthat similar without virtual compliance control. In addition, theappropriate massage force (5–15 N) was applied to the facialtissues for the entire time that the plungers were rubbing theface with virtual compliance control. However, the appropri-ate massage force was applied to the facial tissues for only alimited time without virtual compliance control.
Consequently, when virtual compliance control is applied,the massage trajectories made from the facial shape modelof an adult male can be applied to many people withoutmodification of the model.
6.2. Pre-clinical Test of WAO-1 with Healthy Subjects
6.2.1. Verification Test of Massage to Parotid Gland and Duct
In this experiment, six healthy subjects (without oral disorders)received massage to the parotid gland and duct by a doctor andby WAO-1. The doctor massaged each subject for 2 minutes bypressing the parotid gland and rubbing the parotid duct. WAO-1 gave a similar massage to each patient for 1–2 minutes. Toevaluate the effectiveness of the massages, the amount of saliva
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
1236 THE INTERNATIONAL JOURNAL OF ROBOTICS RESEARCH / September 2009
Fig. 11. Massage forces exerted to the head mannequin. (a) Pressing force provided by the doctor. (b) Pressing force provided byWAO-1. (c) Rubbing force provided by the doctor. (d) Rubbing force provided by WAO-1.
Fig. 12. Comparison of massage trajectory with/without vir-tual compliance control (VC).
was measured by the Saxon test, which is a standard method toconfirm the effectiveness of a massage for dry mouth. In thistest, gauze is put into subject’s mouth for 2 minutes, and theweight of saliva is then measured.
Figure 14 shows the experimental results, based on the av-erage amount of subject saliva. The average saliva amount in-creased significantly during the massage by the doctor, and theincrease of saliva was confirmed 5 minutes after the massage(paired t-test). The average saliva amount also increased sig-nificantly during the massage by WAO-1, and the increase of
Fig. 13. Comparison of reaction forces exerted on the facialtissues during massage. (a) With virtual compliance control.(b) Without virtual compliance control.
saliva also was confirmed 5 minutes after the massage. Conse-quently, we consider that the massage to masseter muscle by
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
Ishii et al. / Development and Experimental Evaluation of Oral Rehabilitation Robot that Provides Maxillofacial Massage 1237
Fig. 14. Experimental results of massage to parotid gland and duct by (a) medical doctor and (b) by WAO-1 (*p � 0.05, pairedt-test).
WAO-1 increases the amount of saliva as well as the massageby a medical doctor. Therefore, this result indicates the effec-tiveness of the oral massage by WAO-1 for dry mouth.
6.2.2. Verification Test of Massage to the Masseter Muscle
In this experiment, 11 healthy subjects (without oral disorders)received massages to their masseter muscles by a doctor, andanother 7 healthy subjects received massages to their massetermuscles by WAO-1. Whether being massaged by the doctoror by WAO-1, each subject received a massage consisting ofpressing and rubbing for 2 minutes. To evaluate the effective-ness of the massages, the temperature of the facial skin wasmeasured by a thermal camera (TVS-500, Nippon AvionicsCo., Ltd), and the width of the masseter muscle was measuredby an ultrasonic imaging scanner (SonoSite 180II, SonoSiteInc.).
Figure 15 shows the experimental results, based on the av-erage facial skin temperature of the subjects. As shown in Fig-ure 15(a), the facial skin temperature increased significantlyimmediately after the massage by the doctor, and the increaseof temperature was confirmed 10 minutes after the massage(paired t-test). In addition, as shown in Figure 15(c), the widthof the masseter muscle increased significantly after the mas-sage by the doctor. On the other hand, as shown in Fig-ure 15(b), facial skin temperature did not increase significantlyimmediately after the massage by WAO-1, but significant in-crease was confirmed 10 minutes after and 20 minutes afterthe massage by WAO-1. Also, as shown in Figure 15(d), thewidth of the masseter muscle also increased significantly af-ter the massage by WAO-1. Consequently, the massage to themasseter muscle by WAO-1 increases the facial skin tempera-ture and the width of the masseter muscle as well as the mas-sage by the doctor. We conclude that the massage increased
the blood flow to the masseter muscle, which increased bothfacial skin temperature and width of the masseter muscle. Thisresult indicates the effectiveness of WAO-1’s oral massage forTMJ disorders.
7. Summary and Future Work
We have developed an oral-rehabilitation robot WAO-1(Waseda Asahi Oral-rehabilitation robot No. 1) for use in casesof oral disorders such as TMJ disorder and dry mouth that issimple to operate. This robot is designed to provide massageto a patient’s face, specifically to the masseter and temporalmuscles and to the parotid gland and duct. It consists of twosix-DOF arms with plungers, a body with headrest, a controlbox, and a PC. It also includes an automatic massage trajectorygeneration system with virtual compliance control.
Two evaluation experiments were performed to verify theeffectiveness of the oral massages of WAO-1 compared withthe massages given by doctors. In the experiments, the mas-sage to the parotid gland and duct by WAO-1 increased theamount of saliva in the subjects, and the massage to the mas-seter muscle by WAO-1 increase both facial skin temperatureand width of the masseter muscle in the subjects. We considerthat these results indicate massage by WAO-1 can be effectivefor patient with oral disorders. Currently, patients with oral dis-orders can receive massage therapy in only a limited number ofhospitals or dental clinics because of shortage of doctors whoprovide such massage. WAO-1 can be a solution for this short-age. Using WAO-1, the doctor only has to input several para-meters� they do not have to give the actual massage. Therefore,WAO-1 has the potential to make massage therapy popular.
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
1238 THE INTERNATIONAL JOURNAL OF ROBOTICS RESEARCH / September 2009
Fig. 15. Experimental results of massage to masseter muscle (*p � 0.05, paired t-test). (a) Temperature following massage bymedical doctor. (b) Temperature following massage by WAO-1. (c) Width of masseter muscle following massage by medicaldoctor. (d) Width of masseter muscle following massage by WAO-1.
The experiments described in this paper are not enough toconclusively establish the effectiveness of WAO-1. A statis-tical study has to be performed on the effect of the massagetherapy provided by WAO-1. In fact, we have started clinicaltests of WAO-1 in two university hospitals to gather data aboutWAO-1’s effectiveness. In addition, the safety measures of thesystem should be further improved. A multiple safety-measuresystem already has been implemented in WAO-1, but furtherimprovement and verification of it are required to obtain theapproval of national government agencies such as MHLW ofJapan and FDA of the United States.
Acknowledgments
This study was supported in part by the special coordinationfund for promoting science and technology from the MEXT,
Japan, the “Humanoid Research Institute (HRI)” Waseda Uni-versity, “the innovative research on symbiosis technologies forhuman and robots in the elderly dominated society”, 21st cen-tury Center of Excellence (COE) program, Japan Society forthe Promotion of Science. The authors would like to acknowl-edge the financial support of “the GIFU and OGAKI Robot-ics Advanced Medical Cluster”. The authors also would liketo acknowledge the support of SolidWorks Japan K.K. andNitta Corporation. Finally, the authors would like to thank Pro-fessor Kaoru Kobayashi, Professor Eiichiro Ariji, ProfessorMasami Fujishita, Dr Masahiro Izumi, Dr Chinami Igarashi,Dr Yoshiko Ariji, and Dr Takashi Osano. This study was per-formed under the guideline of experiments with humans inWaseda University.
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from
Ishii et al. / Development and Experimental Evaluation of Oral Rehabilitation Robot that Provides Maxillofacial Massage 1239
Appendix: Index to Multimedia Extensions
The multimedia extension page is found at http://www.ijrr.org
Extension Type Description
1 Video The video of massage to masseter andtemporal muscle with the virtual com-pliance control.
References
Bann, S., et al. (2004). Robotics in surgery. Journal of theAmerican College of Surgeons, 196(5): 784–795.
Billings, R. J., Proskin, H. M., and Moss, M. E. (1996). Xeros-tomia and associated factors in a community-dwelling adultpopulation. Community Dentistry and Oral Epidemiology,24(5): 312–316.
Darzi, S. A. and Munz, Y. (2004). The impact of minimallyinvasive surgical techniques. Annual Review of Medicine,55: 223–237.
DeBar, L. L., Vuckovic, N., Schneider, J., and Ritenbaugh, C.(2003). Use of complementary and alternative medicine fortemporomandibular disorders. Journal of Orofacial Pain,17(3): 224–236.
Field, E. A., et al. (2001). Age and medication are significantrisk factors for xerostomia in an English population, attend-ing general dental practice. Gerodontology, 18(1): 21–24.
Haskin, C. L., Milam, S. B., and Cameron, I. L. (1995). Patho-genesis of degenerative joint disease in the human tem-poromandibular joint. Critical Reviews in Oral Biology andMedicine, 6(3): 248–277.
Hayashi, T., Kawamoto, H., and Sankai, Y. (2005). Controlmethod of robot suit HAL working as operator’s muscleusing biological and dynamical information. Proceedingsof Intelligent Robots and Systems, pp. 3063–3068.
Katsumata, A., et al. (2008). Development of a force measure-ment system for massage of face using 3D modeling tech-nique. Proceedings of Computer Assisted Radiology andSurgery 2008.
Klein, M. D., et al. (2007). Pediatric robotic surgery: lessonsfrom a clinical experience. Journal of Laparoendoscopicand Advanced Surgical Techniques. Part A, 17(2): 265–271.
Krebs, H. I., et al. (2007). Robot-aided neurorehabilitation: arobot for wrist rehabilitation. IEEE Transactions on NeuralSystem and Rehabilitation Engineering, 15(3): 327–335.
Langenburg, S. E., Knight, C. G., and Klein M. D. (2003).Robotic surgery: an update. Journal of Long-term Effectsof Medical Implants, 13(5): 429–436.
Lee, S. and Sankai, Y. (2002). Power assist control for leg withHAL-3 based on virtual torque and impedance adjustment.Proceedings of the IEEE International Conference on Sys-tems, Man and Cybernetics.
Nederfors, T., (2000). Xerostomia and hyposalivation. Ad-vances in Dental Research, 14: 48–56.
NIH (2006a). Dry mouth. NIH Publication No. 06-3174, U.S.Department of Health and Human Services.
NIH (2006b) TMJ disorders. NIH Publication No. 06-3487,U.S. Department of Health and Human Services.
Okino, A., et al. (2004). Development of a clinical jaw move-ment training robot for intermaxillary traction therapy. Pro-ceedings of the 2004 IEEE International Conference on Ro-botics and Automation, pp. 2492–2497.
Riley, J.L., et al. (2007). Self-care behaviors associated withmyofascial temporomandibular disorder pain. Journal ofOrofacial Pain, 21(3): 194–202.
Sadamitsu, Y., et al. (2006). Development of a robotic carotidblood flow measurement system—a compact ultrasonicprobe manipulator consisting of a parallel mechanism. Pro-ceedings of 2006 IEEE International Conference on CISand RAM, P0415.
Sugahara, Y., et al. (2005). Walking control method of bipedlocomotors on inclined plane. Proceedings of the 2005IEEE International Conference on Robotics and Automa-tion, pp. 1989–1994.
Takanobu, H., et al. (2003). Jaw training robot and its clinicalresults. Proceedings of the IEEE/ASME International Con-ference on Advanced Intelligent Mechatronics, 932–937.
Westesson P. L. (1993). Reliability and validity of imaging di-agnosis of temporomandibular joint disorder. Advances inDental Research, 7(2): 137–151.
at PENNSYLVANIA STATE UNIV on March 5, 2016ijr.sagepub.comDownloaded from