Advances in Attenuation Correction Techniques in PET - HUG
-
Upload
khangminh22 -
Category
Documents
-
view
2 -
download
0
Transcript of Advances in Attenuation Correction Techniques in PET - HUG
Author's personal copy
Advances in Attenuation CorrectionTechniques in PETHabib Zaidi, PhD, PDa,*, Marie-Louise Montandon, PhDa,Abass Alavi, MDb
In positron emission tomography (PET), theimaging system records two antiparallel 511 keVphotons that are emitted after electron–positronannihilation. In this case, the annihilation photonstraverse a total tissue thickness that is equal to thebody thickness intersected by the line between thetwo detectors, also called the line of response(LoR). Since its inception, photon attenuation inbiological tissues has been identified as the mostimportant physical degrading factor affecting PETimage quality and quantitative accuracy [1]. Photonattenuation usually refers to the combination of
photoelectric absorption and Compton scattering.That is, both are components of the general processof photon attenuation [2].
A particularity of PET (in contrast to single-photon emission computed tomography - SPECT) isthat the attenuation factor for a given LoR dependson the total distance traveled by both annihilationphotons within the attenuating medium, and it isindependent of the emission (EM) point alongthis LoR. This makes attenuation correction (AC)easier, owing to the fact that it only requires a simplepremultiplication of the EM data by the resultant
P O S I T R O NE M I S S I O N
T O M O G R A P H Y
PET Clin 2 (2007) 191–217
This work was supported by Grant Number SNSF 3100A0-116547 from the Swiss National Foundation.a Division of Nuclear Medicine, Geneva University Hospital, CH-1211 Geneva 4, Switzerlandb Division of Nuclear Medicine, Department of Radiology, Hospital of the University of Pennsylvania, 3400Spruce Street, Philadelphia, PA 19104, USA* Corresponding author.E-mail address: [email protected] (H. Zaidi).
- What is photon attenuation?- Practical and clinical consequences of
photon attenuation- Methods for determination of the
attenuation mapRadionuclide-based transmission scanningX-ray CT-based transmission scanningMRI-guided derivation of the attenuation
mapComparison of methods
- Attenuation correction strategies inpositron emission tomography
- Attenuation correction in small animalpositron emission tomography
- Pitfalls of CT-based attenuation correctionin positron emission tomography andpotential solutions
Artifacts resulting from polychromaticityof x-ray photons and beam hardening
Artifacts resulting from misregistrationbetween emission and transmissiondata
Artifacts arising from the use ofcontrast-enhanced CT
Truncation artifactsArtifacts arising from metallic objectsArtifacts arising from x-ray scatter in CT
images- Summary- References
191
1556-8598/07/$ – see front matter ª 2007 Elsevier Inc. All rights reserved. doi:10.1016/j.cpet.2007.12.002pet.theclinics.com
Author's personal copy
attenuation correction factors (ACFs). Yet, the ACFsin PET are huge, and quantitation is virtually impos-sible without compensating for the nonlinear atten-uation effect. The magnitude of the ACFs required inPET often might exceed 100 for some LoRs throughthe body [3]. Various strategies have been devisedto determine an accurate attenuation map to enablecorrection for photon attenuation in whole-bodyPET studies. Accurate attenuation compensation re-lies on robust determination of the attenuationmap, which usually is derived through an externaltransmission (TX) scanning apparatus (eg, x-rayCT) integrated into the PET system design. The in-troduction of combined PET/CT scanners in theclinic has facilitated the AC process and allowedTX scanning time to decrease substantially com-pared with radionuclide TX scanning.
Thorough reviews of attenuation map derivationand AC techniques were published previously fornuclear medicine imaging in general [1,3], particu-larly for PET/CT [4], and more recently for cerebralPET imaging [5]. This article addresses this issuefrom a different perspective in the sense that itfocuses on most recent developments in the fieldin general and the most promising approaches inparticular. Given the widespread interest both indual-modality PET/CT imaging and preclinicalinstrumentation, the pitfalls associated with CT-based attenuation correction and potential solu-tions and the unique problems of attenuationcorrection in small animal PET also are addressed.The physical and methodological bases of photonattenuation are addressed briefly, and state-of-the-art developments in algorithms used to derive theattenuation map aiming at accurate AC of PETdata are summarized. Future prospects, researchtrends, and challenges are identified, and directionsfor future research are discussed.
What is photon attenuation?
The physical basis of photon attenuation lies in thenatural property that annihilation photons emittedby the positron-emitting radiotracers (followingpositron–electron interaction) interact with humantissue and other materials as they travel through thebody. The emitted annihilation photons have anenergy of 511 keV and thus can undergo photoelec-tric interactions where the incident photon isabsorbed completely, or more likely, can be scat-tered following interaction with loosely bound elec-trons in biological tissues. Scattering results ina change in the original direction of the incomingphoton with (in the case of incoherent or Comptonscattering) or without (in the case of coherent orRayleigh scattering) energy loss. It should be empha-sized that for soft tissue (the major constituent of the
body), a moderately low atomic number (Z) mate-rial, two distinct regions of single interaction domi-nance can be differentiated: photoelectric below andCompton above 20 keV. In addition, the percentageof scattered events that undergo Compton interac-tions in the object is over 99.5% at 511 keV for softtissues, which renders the number of interactionsby photoelectric absorption or coherent scatteringnegligible.
In mathematical terms, the magnitude of photonattenuation can be expressed by the exponentialequation:
I 5 Io exp
24� Z
S
m ðsÞ ds
35 ð1Þ
where Io and I are the incident and transmitted pho-ton fluences, respectively, (in units of photons perunit area), and ds is a differential of the thicknessof tissue encountered as the photon beam passesthrough the body along path S. The linear attenua-tion coefficient (m) represents the probability thatthe photon will undergo an interaction while pass-ing through a unit thickness of biological tissue. Inother terms, the linear attenuation coefficient isa measure of the fraction of primary photons that in-teract while traversing an absorber, and the linear at-tenuation coefficient is expressed in units of inversecentimeters (cm�1).
Fig. 1 illustrates typical reconstruction artifacts(depression of activity concentration in the center)resulting from the lack of AC for a uniform distribu-tion of activity in a cylindric phantom. The figureshows a PET image reconstructed without AC, theCT-based attenuation map, the same slice obtainedafter applying AC but without scatter correction,and the same slice after applying attenuation andscatter corrections. Corresponding horizontal pro-files drawn through the center of the slices alsoare shown (bottom row). Note the overestimationof activity distribution at the center of the cylinderbefore scatter correction and the recovery of a uni-form activity distribution after attenuation and scat-ter compensations.
Practical and clinical consequencesof photon attenuation
It is well established that PET images reconstructedwithout AC can introduce severe artifacts, henceobscuring subjective qualitative interpretation per-formed by nuclear medicine physicians and causingthoughtful inaccuracies when quantitative assess-ment of PET images is performed [6]. It is thereforeimperative to be aware of the physical processesthat underlie nonlinear photon attenuation, itsclinical impact on reconstructed PET images, and
Zaidi et al192
Author's personal copy
the performance of various methods that can be usedto correct PET images for this physical degrading fac-tor. AC in PET is widely accepted by the nuclear med-icine community as a crucial part of data correctionprocedures that need to be applied for the productionof artifact-free, quantitative PET data. It is should benoted that while the value of advanced techniquesimplemented on commercial clinical systems is nolonger the subject of debate in cardiovascular imag-ing [7–10] and oncology imaging [11,12], there arestill some controversies regarding their relevance inroutine clinical brain studies where simple calculatedtechniques are available [5,13].
In realistic clinical situations, the magnitude of theerror introduced by photon attenuation can vary re-gionally in reconstructed PET images, because thethickness of tissue varies for different regions of thepatient’s anatomy. Consequently, a lesion locateddeep within the body will produce a signal that ismuch highly attenuated compared with that for a su-perficial lesion. Likewise, a region containing a uni-form activity distribution that lies beneath tissuehaving a variable thickness will produce an imagewith variable count density. This might happen invarious situations such as myocardial perfusion/metabolism imaging where soft tissue attenuationcaused by the diaphragm or breast tissue can pro-duce false-positive defects [1]. Reconstruction of to-mographic images without attenuation can causeerroneously high-count densities and reduced imagecontrast in low-attenuation regions such as the lung.
The literature reporting systematic comparativestudies of the effect of different AC strategies inwhole-body PET is impressive [1,4,5,14]. A limitednumber of studies, however, addressed the clinicalimpact of attenuation-corrected images versus no
correction [15–24]. Nuyts and colleagues [25]modified the maximum-likelihood expectationmaximization (ML-EM) reconstruction algorithmby allowing negative intensity values to compensatethe loss of image detail in conventional ML-EMreconstructions, thus improving the visual qualityof uncorrected whole-body PET images.
It is well accepted that AC increases statisticalnoise. In general, however, AC recovers the contrastlost and improves the quantitative accuracy anddeep lesion detectability compared with the casewhere no correction is applied. The extent to whichit can be shown mathematically that the lack of AChas a disabling effect upon the goal for which theimage is to be used is a much more delicate issueto discuss and to corroborate. Fig. 2 shows a clinicalwhole-body PET study reconstructed without ACand images of the same study corrected for attenu-ation using measured TX scanning. The uncorrectedimage shows typical reconstruction artifacts (de-pression of activity concentration at the center)resulting from the lack of AC. More importantly,the mass (volume approximately 65cc; averagestandardized uptake value (SUV) approximately2.1) apparent on the TX scan is clearly visible onthe PET images reconstructed with AC but is notseen in the images without AC [12]. This is a clearargument supporting the need for AC in daily clin-ical PET examinations and against the claim thatit has no impact on lesion detectability.
Methods for determination of theattenuation map
Various methods have been developed to compen-sate for photon attenuation in whole-body PET
Fig. 1. Illustration of reconstruction artifacts resulting from the lack of attenuation correction for a uniform distri-bution of activity in a cylindric phantom (top row) and corresponding horizontal profiles drawn at the center of thecylinder (bottom row). From left to right: reconstructed image without attenuation correction, the CT-based atten-uation map, the same slice after applying attenuation correction but without scatter correction, and finally thesame slice after applying attenuation and scatter corrections. Note the loss of activity at the center of the cylinderon the noncorrected image, the overestimation of activity distribution at the center of the cylinder before scattercorrection, and the recovery of a uniform activity distribution after attenuation and scatter corrections.
Advances in PET Attenuation Correction Techniques 193
Author's personal copy
imaging. In a clinical setting, the balance betweenalgorithmic complexity and the validity of resultsobtained is an important criterion when selectingan AC technique. Even though the methods thatmake a large number of assumptions frequentlycan be undemanding, it is not necessarily truethat complex algorithms always will perform better.The extra complexity must be used judiciously andjustified for the particular application at hand. Inmany cases, extra complexity can result just as easilyin unreliability as in improved results. In a clinicalsetting, it has become standard practice to use sim-plified techniques compared with the often com-plex methods developed for research where thereis greater emphasis on quantitative accuracy.
Methods that do not require a TX scan, oftenreferred to as calculated methods, belong to thehistory of nuclear medicine, as they are consideredto be obsolete with the introduction of dual-modal-ity imaging systems. They still might be relevant (andlikely will remain the method of choice) in brainPET imaging on research prototypes dedicated forbrain research that are not equipped with TX scan-ning devices [26], or when radiation dose reduction(by elimination of the additional radiation dosecontributed by the TX scan) is sought. These tech-niques are reviewed in Zaidi and colleagues [5].
In clinical and research settings, one needs toaccommodate situations of nonuniform attenua-tion for which the spatial distribution of attenua-tion coefficients is not known a priori. Measuredtransmission-based AC is the most commonlyused procedure in clinical and research settings,because it is expected to yield the best attenuationmap as a result of matched energy and spatial reso-lution. Motion-induced misalignment between TXand EM scans, however, can result in erroneous
estimation of regional tissue activity concentrationsin cerebral [27,28], myocardial [29–34], and onco-logic whole-body [35–42] imaging.
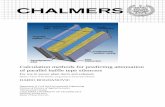
Fig. 3 shows a sketchy representation of differentTX scanning sources and geometries and theexpected quality of obtained attenuation maps. TheTX sources include rotating positron-emitting(68Ga/68Ge) rods measuring TX in coincidencemode, single-photon point sources (137Cs) produc-ing coincidence events between the known sourceposition and photons detected on the opposingside of the detector ring, and x-ray CT units combin-ing a x-ray tube and detector on the opposite side typ-ically used on modern combined PET/CT scanners.Note that x-ray CT produces the best possible diag-nostic quality anatomic images, thus allowing an al-most noise-free attenuation map to be derived. Thehigh cost of dual-modality PET/CT units and the po-tential introduction of artifacts when using CT-basedattenuation correction (CT-AC), which might disturbthe visual interpretation of PET images and biasquantitative PET estimates, are major limitations ofthis approach, however. The previously mentionedtechniques vary in complexity, accuracy, and compu-tation time andwill be described more in detail below.
Radionuclide-based transmission scanning
Before the advent of PET/CT, the most accuratemeans of determining a patient-specific attenuationmap were based on measured radionuclide-basedTX sources that could be acquired before (preinjec-tion), during (simultaneous), or after (postinjec-tion) the PET scan [3]. The first-generation PETscanners used TX ring sources of 68Ga/68Ge (T1/2 568 minutes and 270.8 days, respectively), whichcoexist in secular equilibrium, whereas the second-generation scanners used on average one or more
Fig. 2. Coronal sections of whole-body images of a patient with hamartoma (arrow), which is clearly visible asdense object in transmission image (A) and shows uptake of 18F-FDG in attenuation-corrected emission image(B). In same image, plane of emission image reconstructed without attenuation correction (C); however, hamar-toma is not detectable. (Reprinted from Bai C, Kinahan PE, Brasse D, et al. An analytic study of the effects of at-tenuation on tumor detection in whole-body PET oncology imaging. J Nucl Med 2003;44:1855–61; withpermission.)
Zaidi et al194
Author's personal copy
rod sources of the same radionuclide (approxi-mately 400 MBq) [1]. The sources rotated aroundthe edge of the field of view (FoV), recording coinci-dences between detectors on the near and far sides ofthe subject. A separate scan using the same sources isperformed without the patient in the FoV. The coin-cidences recorded during the blank (without the ob-ject in the FoV) scan are divided by those acquiredduring the TX scan (with the object in the FoV) togive the ACFs for each LoR:
ACF 5blank
transmission5
I0
I0exp
�
RLðs;qÞ
mðxÞdx
!
5 exp
0B@ Z
Lðs;qÞ
mðxÞdx
1CA ð3Þ
where I0 is the blank count rate recorded at the cur-rent LoR; m(x) is the linear attenuation coefficient atposition x in the body, and L(s,q) is the integrationpath along the LoR.
It might seem at first glance that the AC process isstraightforward and can be performed simply bymultiplying the EM projection data by the mea-sured ACFs on a LoR-by-LoR basis. The noisy natureof TX data, however, will lead to a substantialdecrease of signal-to-noise ratio (SNR) in the cor-rected PET data [43]. This takes place owing to thefact that the denominator in Equation 3 might bevery small, either in the presence of high-densitytissue, or large attenuation path length throughwhich annihilation photons pass and because TXdata obey Poisson statistics (as do all radiation EMand detection processes). One efficient way to get
around this hurdle consists in low-pass filtering ofTX and blank scans before computing the ACFs [5].
The rod windowing technique was developedmainly to allow postinjection TX scanning [44].The principle is based on continuous encoding ofthe source location and discrimination betweenprojection elements indicating collinear (or nearlycollinear) detector pairs and those that are not.Coincidences recorded in a narrow window cen-tered on each rod source (primarily TX events) arestored independently from those recorded outsidethe window (mostly EM events). Appropriate tech-niques were proposed to correct for EM contamina-tion of TX measurements recorded within thewindow in postinjection TX scanning [45–47].
The previously described rod windowing tech-nique was extended later on to allow simultaneousEM and TX scanning [48,49], which has the advan-tage to reduce substantially the acquisition time.Despite its promising features, very few centers adop-ted the approach for use in routine clinical whole-body PETstudies [50,51]. A more elaborate approachalso was proposed to reduce contamination of theEM data by the TX photons in simultaneous scan-ning through the use of a fast, dedicated, lutetiumoxyorthosilicate (LSO)-based reference detectorplaced close to the collimated coincidence pointsource used to produce the TX data [52].
The most important drawback of positron-emit-ting TX sources is the high photon flux in the detec-tors closest to the source, which usually leads tolonger scan times because of dead time. To improvecounting statistics without increasing acquisitiontime, some investigators proposed to use single-photon emitting sources such as 137Cs (662 keV,T1/2 5 30.04 years), where LoRs are formed between
Fig. 3. Sketchy illustration of different configurations of transmission scanning geometries for positron emissiontomography (PET) is shown. (A) rotating positron-emitting rods measuring transmission in coincidence mode. (B)Single-photon source producing coincidence events between the known source position and photons detectedon the opposing side of the detector ring. (C) X-ray CT scanning using a x-ray tube and detector on the oppositeside typically mounted on modern combined PET/CT scanners.
Advances in PET Attenuation Correction Techniques 195
Author's personal copy
the known location of the point source as it rotatesaround the patient and the detector on the oppositeside that absorbs the transmitted photons [53,54].This is a more efficient approach compared withcoincidence detection using positron-emitting ra-dionuclide sources, which necessitates detection ofboth annihilation photons by the PET detectors.The direct consequence is a much improved SNRin ACFs generated using single-photon sourcescompared with those generated using positron-emitting sources [3]. An additional advantage isthat single-photon sources can use isotopes thatemit photons at an energy different from the 511keV of annihilation photons (eg, 137Cs), thus allow-ing efficient implementation of postinjection TXscanning with reduced contamination of TX imagesby PET data. The technique has a major drawback,however, given that the TX data need to be normal-ized on a daily basis (90 minutes on the ECAT ARTscanner (CTI/Siemens Medical Solutions, Knoxville,Tennessee) [55]) to a slab phantom scan to correctacquired data for scatter and cross section variationusing a log–linear transformation of the attenuationfactors [56]. Various strategies also have been sug-gested to reduce contamination of EM data by TXphotons for simultaneous scanning and to reducespillover of EM data into the TX energy window[47–51]. For example, it has been demonstrated,using data from the High Resolution ResearchTomograph (HRRT - Siemens Medical Solutions,Knoxville, Tennessee) brain dedicated PET scanner,that EM contamination can lead to gross underesti-mation of attenuation coefficients [57]. It also wasreported that the most accurate way to compensatefor this is to combine nonuniform EM contamina-tion subtraction with TX image segmentation.
Segmented AC was proposed to reduce noisepropagation from the short TX to the EM scansduring the multiplicative AC process. This can beachieved through tissue classification schemes,which consist of delineating anatomic regionshaving different attenuation properties followedby assignment of known tissue-dependent attenua-tion coefficients using weighted averaging. Thesegmented attenuation maps then are forward pro-jected to generate ACFs with reduced noise that canbe used for AC of the PET data.
Clinically relevant segmentation algorithms weredesigned by balancing image quality and requiredalgorithmic complexity and resulting computa-tional time [58]. Most TX image segmentation algo-rithms fall into one of the following two classes:classical histogram-based adaptive thresholdingtechniques [59–61] and fuzzy clustering-basedapproached [55,62]. Adaptive thresholding-basedtechniques use the gray-level histogram counts todistinguish between regions. Because only intensity
information is used for the segmentation, this oftenresults in noisy segmentations, and the techniquemost likely fails in regions where the total numberof counts is small (eg, the skull), given that theclassification is based solely on the characteristicsof the histogram. Therefore, the performance of suchtechniques strongly depends on the choice of thethresholds. On the contrary, fuzzy clustering-basedsegmentation techniques have proved to be morerobust as automated, unsupervised algorithms forsegmenting noisy images for different applications[58]. These are iterative approaches that minimizean objective function requiring the number ofclusters as input parameter to assign a membershipdegree to all voxels with respect to a cluster center.
Other attractive approaches to segment noisy TXdata include the use of active contour models [63],neural networks [64], three-dimensional edge detec-tion techniques [65], morphologic segmentation[66], and hidden Markov modeling [67]. Alterna-tives to segmentation of TX images with the goal ofreducing noise in PET TX measurements includeBayesian image reconstruction [68–70] and nonlin-ear Gaussian [71] and non-Gaussian [72] smooth-ing or anisotropic diffusion filtering [73].
X-ray CT-based transmission scanning
Conventional AC procedures developed for stand-alone PET units traditionally have been performedusing external radionuclide TX sources. The proce-dure is conceptually analogous to the principle ofx-ray CT imaging, where the radiation emanatingfrom a rotating x-ray tube is transmitted throughthe patient’s body and recorded by an array of detec-tor elements on the opposite side. A tomographic re-construction algorithm then is used to calculate thespatial distribution of attenuation coefficients. Oncommercial CT scanners, the reconstructed intensi-ties usually are represented in terms of normalized(to water) CT numbers or Hounsfield units (HU),named after Godfrey Hounsfield, an established pi-oneer and recipient of Nobel prize in medicine(1979) for significant contributions to the develop-ment of CT [74]. Yet, the pixel values are related di-rectly to the linear attenuation coefficient (m) at thesame point in the patient, calculated for the effectiveenergy of the polyenergetic photon beam used tocreate the CT image:
CT number 5m� mH2O
mH2O
� 1000 ð4Þ
Note that with this definition, air and water havea CT number of -1000 HU and 0 HU, respectively.
As a result, the use of low-noise x-ray CT images tocreate patient-specific attenuation map for correct-ing the PET data for photon attenuation is relativelystraightforward. The technique first was explored in
Zaidi et al196
Author's personal copy
the context of SPECT imaging using realigned CTdata [75] and pioneered by the University of Califor-nia San Francisco (UCSF) group for combinedSPECT/CT imaging [76]. The same approach was in-vestigated later by the University of Pittsburgh Med-ical Center group (Pittsburgh, Pennsylvania), whichdeveloped the basis of CT-based AC using sequentialscanning of the patient separately on standalone PETand CT scanners followed by off-line image registra-tion [77]. Interest in CT-AC was revived with thecommercial introduction and popularity of com-bined PET/CT and SPECT/CT units [78]. Neverthe-less, numerous pitfalls arise from the use of CT togenerate attenuation maps for correction of thePET data that must be considered to avoid typicalartifacts that are unique to PET/CT imaging. Theseare discussed further in the Pitfalls of CT-AC section.
As mentioned previously, x-ray CT inherentlyprovides a patient-specific measurement of the elec-tron density and thus the linear attenuation coeffi-cient at each pixel in the CT image. Usually thehigh-resolution anatomic images are first down-sampled, followed by Gaussian filtering to matchthe resolution of the PET data. The energy depen-dence of the attenuation coefficient is taken intoaccount by calculating scaling factors to convertthe linear attenuation coefficient at the x-ray effec-tive energy to the 511 keV energy of annihilationphotons. The most widely used calibration methodis based on techniques developed for bone mineraldensity studies with quantitative CT. The calibra-tion procedure begins by acquiring CT scans froma phantom containing tissue-equivalent calibrationmaterials having known chemical compositions(Fig. 4). CT scans of the calibration phantom are ac-quired. Regions of interest then are defined for each
compartment containing a calibration material, al-lowing the user to determine the mean CT numberproduced for each specific material. A calibrationcurve then is generated in which the measured CTnumber is plotted against the known attenuationcoefficient at the photon energy of the radionuclideused in the EM study. The resulting calibrationcurve is piece-wise linear and covers the range oflinear attenuation coefficients commonly encoun-tered in the body. CT values below that of soft tissue(ie, water) have a slope corresponding to mixturesof soft tissue and air (eg, including those encoun-tered in lung), while those having attenuation coef-ficients above water have a slope corresponding tomixtures of soft tissue and bone. The resulting cali-bration curve can be used to convert CT values ob-tained from patient scans to their equivalent linearattenuation coefficients for the desired radionuclidephoton energy. Fig. 4 shows typical piece-wise cali-bration curve required for practical implementationof CT-AC. It should be noted that attenuationcaused by Compton scatter is related to object density,whereas photoelectric absorption is related to bothdensity and atomic number. This results in a cleardistinction between soft tissue and cortical bone;the latter has more calcium and phosphorus (havinghigher atomic numbers). Bone has a higher photo-electric absorption cross section because of presenceof calcium. Note also that at the PET energy(511 keV) almost all interactions are Compton scatter.
MRI-guided derivation of theattenuation map
The use of MRI guided attenuation correction innuclear medicine imaging dates back to the 1990s,when the approach was investigated independently
Fig. 4. Representative bilinear calibration curve determined experimentally at 120 kVp for conversion of CTnumbers (HU) into linear attenuation coefficients at 511 keV. A typical polyethylene cylindric phantom contain-ing eight cylindric holes allowing one to calibrate the CT scanner using various samples with known density andcomposition is shown in the upper left corner.
Advances in PET Attenuation Correction Techniques 197
Author's personal copy
in the context of thoracic SPECT [79] and brain PETimaging [80]. These techniques relied on software-based image registration algorithms to realign func-tional and anatomic images. The recent interest andsuccessful implementation of simultaneous PET/MRI units that can operate simultaneously (ratherthan sequentially as compared with PET/CT) fur-ther stimulated the development of these tech-niques [81].
The major difficulty facing MRI guided AC lies inthe fact that the magnetic resonance signal or tissueintensity level is related directly to proton densityand not to electronic density, which renders conver-sion of magnetic resonance images to attenuationmaps less obvious compared with CT. The limitedspace available on PET/MRI units makes placementof external radionuclide sources difficult or evenimpossible. The basic problem of attenuation mapdetermination from MRI is to locate and map themajor attenuating structures in the body. Theoreti-cally, this can be achieved in two steps: segmenta-tion into regions of tissues/organs having differentattenuating properties and assignment of corre-sponding linear attenuation coefficients at 511 keVto the segmented tissues/organs.
Attempts were pursued to construct a nonuniformattenuation map from MRI for brain SPECT imaging[82]. In this approach, the MRI is segmented intobone and soft tissue classes to yield a nonuniformattenuation map by modifying the uniform attenua-tion map to model bone of the skull by the waterthickness that would result in the same attenuation(eg, m equals 0.153 cm�1 at 140 keV). A nonuniformwater envelope then is added to the surface of thebrain to account for nonuniform bone compart-ment. The method, however, ignores the hollowspace of sinus and air cavities that are inevitably
present within the head. A more sophisticated ap-proach for brain PET imaging based on coregisteredT1 weighted three-dimensional magnetic resonanceimages has been proposed recently [83]. The mag-netic resonance images are first realigned (after brainextraction) to preliminary reconstructions of PETdata obtained using calculated AC and then seg-mented using a fuzzy clustering technique by identi-fying tissues of significantly different density andcomposition. The voxels belonging to different re-gions are classified into bone, brain tissue, andsinus cavities. These voxels then are assigned theo-retic tissue-dependent attenuation coefficients asreported in the International Commission on Ra-diological Units and Measurements 44 report [84]and the resulting image smoothed using a Gaussiankernel. The technique was refined further by auto-mating the segmentation of the skull procedure ofT1 weighted MRI using a sequence of mathematicalmorphologic operations [5]. Before the segmenta-tion of skull, the algorithm segments the scalp andthe brain from the magnetic resonance image. Thescalp mask allows one to quickly eliminate back-ground voxels with intensities similar to those ofthe skull, while the brain mask ensures that the braindoes not intersect the skull segmentation [85]. Theinner and the outer skull boundaries can be com-puted using thresholding and morphologic closingand opening operations. The results then aremasked with the scalp and brain volumes to guaran-tee closed and nonintersecting skull boundaries.Fig. 5 illustrates the performance of MRI-guided der-ivation of the attenuation map as compared with theCT-based approach for clinical brain PET imaging[5]. The figure shows the transaxial CT cross section,the corresponding coregistered MRI cross section,and the segmented MRI required to generate
Fig. 5. Illustration of the performance of MRI-guided derivation of the attenuation map as compared withCT-based approach for clinical brain positron emission tomography (PET) imaging. From left to right: transaxialCT cross section and its corresponding coregistered MRI cross section and the segmented MRI required togenerate a three-tissue compartment head model corresponding to brain, skull, and scalp. White voxels arelabeled as skull; dark gray voxels are labeled as scalp, and intracranial black voxels are labeled as brain tissue.(Reprinted from Zaidi H, Montandon M-L, Meikle S. Strategies for attenuation compensation in neurologicalPET studies. Neuroimage 2007;34:518–41; with permission.)
Zaidi et al198
Author's personal copy
a three-tissue compartment head model correspond-ing to brain, skull, and scalp using the algorithmmentioned previously [85]. Compensation for atten-uation in the bed and head holder can be accom-plished as discussed in Zaidi and colleagues [5] forcalculated AC methods. The techniques describedpreviously were developed originally for use on ded-icated high-resolution brain PET cameras not equip-ped with TX scanning devices and where MRI isreadily available for brain research studies [26]. Themethod is also useful for the simultaneous PET/MRI scanning system dedicated for brain researchbeing developed by one scanner manufacturer [86].
Some of the problematic tissues in whole-bodyimaging are bone and brain skull, the lungs, andother unpredictable benign or malignant anatomicabnormalities with varying densities. Bone is intrin-sically not detectable by MRI, as it provides a black orvoid signal, making it difficult to distinguish air frombone. In the head, however, the skull bone is coveredby subcutaneous fat and encloses the brain. Incorpo-ration of a priori anatomic knowledge allows forsufficient information to be collected to preciselysegment magnetic resonance scans and thus to pro-vide an accurate attenuation map. More sophisti-cated bone segmentation techniques using activeshape models might help to circumvent the limita-tions discussed previously [87]. Ignoring bone wasreported to be acceptable in the abdomen and hips[88] but certainly not in the thorax [89].
Another appealing approach for segmentation ofthe skull and bony structures is to use multispectralmagnetic resonance data acquisition with varyingcontrast characteristics to provide additional infor-mation for distinguishing between different tissues.For example, T1 weighted images show better softtissue contrast, whereas T2 weighted images showbony structures more clearly. The development ofmore refined magnetic resonance sequences to labelthe bone structure more precisely will play a signifi-cant role in novel methodological developmentsaiming at deriving attenuation maps from magneticresonance images [90,91]. Careful optimization ofthe magnetic resonance sequences is a prerequisitefor successful implementation of the techniqueand needs to be investigated further. Long acquisi-tion times, however, make acquisition of morethan one magnetic resonance sequence (as neededfor some segmentation algorithms) almost impossi-ble in practice. Another possibility would be toexploit the potential of rapid dual-tracer PET[92,93], where combination of fluoride (18F)-PETfor bone scanning with the tracer of interest (eg,11C-methionine) should allow scanning bothtracers in a single acquisition. The preliminaryresults obtained using dynamic dual-tracer imagingwith staggered injections appear to allow recovering
overlapping signals through the use of informationfrom kinetics and radioactive decay. Provided theadditional absorbed dose is reasonable, the bonescan should allow—through segmentation—themapping of bony structures in the body.
Segmentation of lung regions in thoracic MRI isanother challenging issue that has received littleattention owing to its limited clinical value untilthis modality became feasible as a result of newdevelopments in enhanced pulse sequences, reducedscanning time, and introduction of new contrastmedia (eg, hyperpolarized gas) [94–97]. This hasbeen performed, for example, through merging ofmultiple active contours [94], region-based segmen-tation [98], and edge-based and model-based tech-niques [99], successfully partitioning the imagevolumes into major anatomic structures, includinglungs, heart, cardiac ventricles, and thorax outlines.Despite successful segmentation,however, anotewor-thy difficulty is that some tissue regions have contin-uously varying densities that may not be representedcorrectly by a discrete set of a priori established tissuemodels. With respect to MRI-guided AC, the lung isone of the most challenging organs, given that ithas been shown that the density of lung tissue: Is con-siderably different from subject to subject, dependson breathing patterns, and varies with age and in theevent of respiratorydiseases by as much as 30% [100].
Another approach is to use representative ana-tomic atlas registration, where the MRI atlas is reg-istered to the patient’s MRI, and prior knowledge ofthe atlas’ attenuation properties (for examplethrough coregistration to CT or TX atlas) is usedto yield a patient-specific attenuation map [101].The critical and crucial part of the algorithm is theregistration procedure, which might fail in somecases with large deformations. The second funda-mental question that remains to be addressed is:does the global anatomy depicted by an atlas reallypredict individual attenuation map? The use of sup-port vector machines to predict the attenuation co-efficients directly from the local image informationby training a machine learning algorithm usingsmall image patches has been reported recently[102]. Combination of this approach with the atlasregistration described previously might be an ap-pealing technique. Despite the remarkable resultspresented so far, which seem promising, more re-search remains needed to fully automate the proce-dure and to render it applicable to whole-bodyimaging [81]. Moreover, the clinical applicabilityof this approach remains to be demonstrated.
Comparison of methods
Within the context of whole-body imaging, theproblems associated with the use of CT-AC on onehand and the complexity inherent to advanced
Advances in PET Attenuation Correction Techniques 199
Author's personal copy
computational methods for transmissionless AC[70,103,104] spurred the further development ofTX-based AC methodologies, which remain anactive research area. Some scanner manufacturers de-cided to preserve radionuclide TX scanning deviceson new-generation hybrid PET/CT units such asthose implemented on the SceptreP3 (Hitachi Med-ical Systems America, Inc., Twinsburg, Ohio), Gem-ini (Philips Medical Systems, Best, The Netherlands),and also the first units of the Discovery LS PET/CT se-ries (GE Health care Technologies, Waukesha, Wis-consin). This allows the combination of both CTand radionuclide scanning-based AC to effectivelyimage patients with metal implants and prosthetics.A limited number of studies reported in the literaturedetailed comparative assessment studies betweenCT-AC and radionuclide scanning-based AC, includ-ing 68Ga versus CT-AC [31,105–114] and 137Cs versusCT-AC [115,116]. Clinical and scientific data are re-quired to impartially establish whether the advan-tages and clinical benefits of TX scanning-based ACare sufficient to offset its additional running costs,or whether CT-AC should be the only option on hy-brid PET/CT units [14].
It is undisputable that CT-AC has several virtuesand should be targeted for further research. Itshould be recognized, however, that its clinical ben-efits have not been demonstrated unequivocally,and these benefits should be documented carefullyby investigators for wider acceptance. The key pointis that many PET procedures do not require a diag-nostic quality CT, and radionuclide-based TX scan-ning would be a better option than low-dose CTprotocols. It is still too early to claim that TX scan-ning devices are obsolete for PET/CT, and that CT-AC should be the gold standard on these systems.The authors’ opinion is that TX scanning still hasa genuine role and remains an appealing alternativeuntil all the problems associated with CT-AC areresolved through research [14].
Attenuation correction strategiesin positron emission tomography
The fundamental equation that links the imagedobject f(x,y) and corresponding attenuation mapm(x,y) to its measured projections p(s,q) is calledthe attenuated Radon transform and is given inthe case of PET by:
p ðs; qÞ 5
ZLðs;qÞ
f ðx; yÞ dr
� exp
264� Z
Lðs;qÞ
m ðx; yÞ dl
375 dr ð5Þ
where L(s,q) is the integration path along the LoR,and q is the angle between the rotating detectorplane and the stationary reconstruction plane.
The ideal solution would have been to use an exactformula for the inverse problem to solve the Radontransform and reconstruct the spatial distributionof the tracer f(x,y). Owing to the complexity of theequation in the case of nonuniform attenuation,however, an exact solution is not possible in general.The seminal contribution by Novikov [117,118],who recently gave an explicit inversion formula forthe attenuated Radon transform for a particular im-portant family of weights, was a major breakthroughin the field. Moreover, Novikov’s formula was provenfor a somewhat larger class of weight functions usinga completely different and more straightforwardmethod [119,120]. In spite of recent progress in thefield, various approximate methods have beenproposed and still are used to solve the problem ofreconstructing an object from its measured projec-tions in the presence of photon attenuation.
Measured TX scanning for AC purposes was usedduring the early developments of PET, which startedmainly as a research tool with greater emphasis onaccurate quantitative analysis. Two additional fac-tors contributed to this logical advancement. First,AC in PET is relatively straightforward, Since inprinciple it requires a simple premultiplication ofthe measured EM data by the corresponding ACFs,and second, the ACFs in PET are large, and withoutAC, quantification cannot be realized.
As mentioned earlier, photon attenuation in PETis independent of the EM point along measuredLoRs. In contrast, modeling the attenuation processin SPECT involves taking into account the fact thatattenuation factors are dependent on the EM point,because the emitted photon crosses only part of thepatient’s anatomy before reaching the detector. Thedirect consequence is that nonuniform AC forSPECT generally requires iterative reconstruction [1].
Because AC in PET is relatively straightforward,and its accuracy is limited only by the noise (limitedstatistics) present in the acquired TX scans, only twotechniques have materialized, and both require thecomputation of the ACFs through forward projec-tion of the attenuation map at appropriate angles.To reduce processing time and data storage require-ments for the three-dimensional PET data collectionmode, it is often convenient to work with precor-rected data. This is the basis of the first approach,where data correction is performed in projectionspace through multiplication of the ACFs by themeasured EM data using the following expression:
pACðs; qÞ 5 ACF � pðs; qÞ 5
ZLðs;qÞ
f ðx; yÞ dr ð6Þ
Zaidi et al200
Author's personal copy
The attenuation-corrected projections pACðs; qÞthen are used to reconstruct the images using eitheranalytic or iterative reconstruction techniques. Anattractive option is to produce a smaller set ofsinograms by precorrecting the data and applyingFourier rebinning (FORE). The data, however, areno longer Poisson-distributed. It has been shownthat iterative algorithms (eg, ordered subsets –expectation maximisation or OSEM) yield subopti-mal images from such data [121]. Alternatively,when OSEM is used, the ACFs can be applied to pro-vide proper statistical weighting to the data as isdone in attenuation-weighted OSEM (AW-OSEM)[121]. This latter technique has better noise proper-ties and now is incorporated in commercial soft-ware used routinely in many clinical PET facilities.For instance, it has been shown that the FORE1AW-OSEM algorithm results in the best overalldetection and localization performance for 1 cmdiameter lesions compared with FORE1OSEMand FORE1FBP algorithms in PET imaging [122].
Attenuation correction in small animalpositron emission tomography
The demand for functional, metabolic, and molec-ular imaging of small animals, including mice, rats,small primates, and other mammalian species, hasstimulated the development of dedicated small-bore high-resolution PET systems that contributeunique information that is becoming relevant forbiomedical research [123]. Similar to scatter model-ing and correction [2], little has been published onAC in small animal PET scanners owing to the lowmagnitude of attenuation factors (compared withclinical imaging) when imaging rodents. The mag-nitude of the correction factors ranges from approx-imately 45 for a 40 cm diameter human subject anddecreases down to 1.6 for a 5 cm diameter rat) tonearly 1.3 for a 3 cm diameter mouse [124]. Thiselucidates why the problem of photon attenuationis small animal imaging has been overlooked evenin the third generation of preclinical PET scanners[125]. PET scanner calibration factors usually aredetermined with and without AC, given that AC stillis not well established in small animal imaging.
Fahey and colleagues [126] have shown that theuse of TX-based AC improved the quantitative accu-racy but also reduced the precision as indicated inthe variability of the attenuation corrected data.As stated previously, this can be compensated bynoise reduction schemes such as segmentation ofthe TX data. Another study compared several mea-sured TX-based techniques for deriving the attenua-tion map on the micro-PET Focus 220 animalscanner (Siemens Preclinical Solutions, Knoxville,Tennessee) [127]. This includes coincidence mode
with and without rod windowing, singles modewith two different TX sources (68Ge and 57Co),and postinjection TX scanning. Moreover, the effi-ciency of TX image segmentation and the propaga-tion of TX bias and noise into the emission imageswere examined. It was concluded that 57Co-basedAC provides the most accurate attenuation maphaving the highest SNR. Single-photon TX scanningusing 68Ge sources suffered from degradationsresulting from object Compton scatter. MonteCarlo simulation studies also demonstrated thatbackground contamination in the 68Ge singles-mode data caused by intrinsic 176Lu radioactivitypresent in the detector crystals can be compensatedfor by using a simple technique [128]. Compensat-ing for scatter improved the accuracy for a cylindricphantom approximately 10 cm diameter) but over-corrected for attenuation for a mouse phantom.Low-energy 57Co-based AC also resulted in lowbias and noise in postinjection TX scanning foractivities in the FoV up to 20 MBq. Attenuationmap segmentation was most successful using 57Cosingle-photon sources; however, the modest im-provement in quantitative accuracy and SNR maynot rationalize its use, particularly for small ani-mals. More sophisticated techniques using multiplesources for TX scanning where each point source issurrounded by a plastic scintillator coupled toa miniature photomultiplier tube to allow collec-tion of the energy the positron must lose beforeannihilation also were developed. [129,130] alsowere developed. The LoR joining the current sourceposition and detector position are identifiedthrough the pulse provided by the energy lost inthe plastic scintillator, whereas scanner’s conven-tional detectors provide the second pulse.
The potential use of small-animal CT for AC is es-tablished and considered to be one of the potentialapplications of low-dose micro-CT imaging thatcan drive the further development of dual-modalitysmall animal PET/CT [131]. Similar to SPECT/CT[132,133], the accuracy of CT-AC in preclinicalimaging was demonstrated using phantom andanimal studies, where the low-dose CT was suitablefor both PET data correction and PET tracer locali-zation [124]. Noise analysis in phantom studieswith the TX-based method showed that noise inthe TX data increases the noise in the correctedPET emission data, whereas the CT-based methodwas accurate and resulted in less noisy images. Forsmall animal imaging, hardware image registrationapproaches that rely on the use of custom madeimaging chambers that can be mounted rigidlyand reproducibly on separate PET and CT preclini-cal scanners [134] is a reasonable alternative tocombined PET/CT designs [135–137]. CalculatedAC was reported to provide similar correction
Advances in PET Attenuation Correction Techniques 201
Author's personal copy
compared with CT-AC for a cylindric phantom anda mouse for which the attenuation medium volumematches the PET emission source distribution[138]. It undercorrects for attenuation, however,when the EM image outline underestimates theattenuation medium volume (unmatched sourcedistribution and attenuation medium).
Pitfalls of CT-based attenuation correctionin positron emission tomographyand potential solutions
The progress in CT-AC methodology has beenimmense in the last few years, the main opportuni-ties arising from the development of both optimizedscanning protocols and innovative and faster imageprocessing algorithms. This has permitted the imple-mentation of much more ambitious algorithms thattackle the challenges of whole-body imaging usingPET. Some solutions recently were proposed andused successfully in clinical and research settings.These include optimized contrast-enhanced CT pro-tocols [139,140], respiratory motion compensation[39,141–143], metal artifacts reduction [144–165],truncation artifacts correction [166–170], beamhardening correction [171,172], and x-ray scattercompensation in CT [173–176]. These hot topicsare discussed in the following section, and in theauthors’ opinion undoubtedly still require furtherresearch and development efforts.
Artifacts resulting from polychromaticityof x-ray photons and beam hardening
The x-ray beam used in CT is polyenergetic, ratherthan monoenergetic, as is the case for photons emit-ted by radionuclide TX sources. The linear attenua-tion coefficient measured with CT is calculated atthe effective energy of the x-ray beam rather thanat the energy of the annihilation photons emitted bythe positron-emitting radiopharmaceutical duringthe emission study. A precise conversion of CT num-bers derived from low-energy polychromatic x-rayspectra to linear attenuation coefficients at 511 keVis thus essential. Several strategies have been devisedfor calibrating the CT image for AC of the PET data,including scaling [177], segmentation [4], hybridsegmentation/scaling [77], piece-wise linear scaling[109,178], and dual-energy decomposition methods[179,180]. The dual-energy x-ray method requiresacquisition of two CT scans from the same regionsat different x-ray energies, which are combined togenerate accurate attenuation coefficients at anydesired photon energy. The technique seems promis-ing, particularly with the development of dual-source x-ray CT scanners [181] and the introductionof dose-reduction CT scanning protocols [182,183].It should be noted that most commercial PET/CT
scanners use the bilinear calibration curve method,which generally is calculated at a preset tube voltage(eg, 120 to 140 kVp) and tube current. The effect oftube current [105,184] and tube voltage [185] onthe accuracy of CT-AC has been found to be relativelysmall. The last reference demonstrated that the use ofa single calibration curve acquired under standardimaging conditions does not affect to a visible ormeasurable extent neurologic PET images recon-structed using CT-AC when CT images are acquiredin different tube voltages [185]. The situation is dif-ferent for whole-body scanning, where calibrationfactors must be calculated separately for each kVp-setting at which the CT scanner is operated [186].
On the other hand, the polychromatic nature ofCT and the energy-dependent attenuation of mostmaterials make CT subject to beam hardening arti-facts caused by the preferential absorption of lower-energy photons as they pass through the patient’sbody [187,188]. Therefore, the mean energy ofthe x-ray beam is higher in thick patient regionsthan in thin patient regions. Correspondingly, thelinear attenuation coefficient calculated for thickbody regions is lower than in thin regions. The con-sequence is that Beer’s law is no longer valid, andtherefore errors will propagate in the measuredline integrals of the attenuation map. This can causecupping artifacts induced by nonlinearities in theprojection data that generally are corrected inthe calibration software implemented as part ofthe standard CT reconstruction software of com-mercial scanners. More sophisticated beam harden-ing correction strategies with varying degrees ofsuccess have been proposed in the literature[159,171,172,188–190]. The field remains openfor further developments.
Artifacts resulting from misregistrationbetween emission and transmission data
The advantages and drawbacks of hardware integra-tion versus software registration in dual-modalityimaging still are being debated even one decadefollowing the introduction of combined PET/CT inclinical routine [191–195]. Notwithstanding thesuccess and widespread clinical adoption of PET/CT, there are several challenges that still are facingthe use of dual-modality imaging, and that representinherent limitations in this technique. One of themost significant challenges of PET/CT is the diffi-culty to achieve accurate registration of both imag-ing modalities in the presence of motion [196]. Ithas been advocated that software-based registrationmight play a complementary role when using hybridPET/CT to offset inherent patient motion [197].
Despite much worthwhile research performedduring the last few years, artifacts induced by respi-ratory and cardiac motion remain among the most
Zaidi et al202
Author's personal copy
difficult problems to solve [196,198]. This probabletrouble arises when the patient moves either volun-tarily or involuntarily between or during the CT andPET data acquisitions. This might take place, for in-stance, if the patient changes his position while ly-ing on the patient bed. Patient motion also mightoccur due to respiration, cardiac motion, peristalsis,and bladder filling, all of which can lead to motionblurring or misregistration errors between PET andCT data [199,200].
Diagnostic-quality CT data usually are acquiredusing a breath-hold protocol, whereas PET dataare acquired over several minutes with the patientbreathing softly. Differences between PET and CTbreathing protocols might lead to misalignmentartifacts owing to anatomic dislocations of thediaphragm and chest wall during a PET/CT scan.A slight displacement of the diaphragm’s positionon the CT scan can cause a substantial bias in theestimation of the tracer concentration in the recon-structed PET data when the former is used for AC[39,201]. The outcome of an inconsistency indiaphragmatic location between PET and CT isfrequently the appearance of the so-called coldartifact at the lung base, which is illustrated inFig. 6 for data acquired on the Biograph Sensation16 PET/CT scanner (Siemens Medical Solutions,Erlangen, Germany). Many studies reported signifi-cant misalignment between the CT and the PETdata. For example, in a study of 300 clinical PET/CT studies with proven liver lesions; approximately2% appeared to have the lesion localized in thelung [202], whereas the misalignment betweenPET and CT data was greater than 2 cm in 34 of100 patient studies because of respiratory motion[39].
The impact of respiratory motion has been inves-tigated extensively in the context of oncologic PETimaging [35,37–42,141,202–209]. It has beenreported that motion-induced artifacts also mightaffect the appearance of upper abdomen lesions,thus resulting in false-negative interpretation ofliver dome lesions [115,210]. Caution therefore isrecommended when reading PET/CT scans ofpatients suffering from disease in the periphery ofthe lung, where noticeable tracer uptake can bethe result of respiratory motion rather than disease.Modern PET/CT scanners are equipped with helicalCT technology, allowing one to acquire high-resolu-tion anatomic images within a few seconds follow-ing patient positioning and definition of the axialFoV on the topogram. It is therefore obvious thatPET is the limiting factor when it comes to scanningspeed on combined PET/CT. Whenever faster scan-ning times are sought, PET is the imaging modalityrequiring improvement through the developmentof novel detector technologies, faster scintillation
crystals and electronic boards, new geometriesoffering higher sensitivity, and many other meansthat are being explored. One possibility would beto substitute conventional PET detector blockswith LSO panel detectors [211] covering a largeraxial FoV with the aim of achieving faster scan timesthan are achievable with current systems. In anycase, faster scan times improve patient comfortand reduce the time during which patient motioncan occur. Likewise, faster scan times can increasepatient throughput and thereby boost system useand improve cost-effectiveness.
As an alternative, many potential solutions havebeen suggested to accommodate differences betweenbreathing patterns, including retrospective AC usingfree-breathing CT [212], the use of optimal CTacqui-sition protocols [213,214], respiratory averaged CT[34,39,41,42], phased CT acquisitions [141], cineCT acquisition [215], respiratory correlated acquisi-tions [38,216,217], deep-inspiration breath-holdacquisition [209,218], and the use of respiratory-gated PET/CT acquisitions [196,198,204–208,219–221]. Fig. 7 shows the principle of respiratory-averaged CT (ACT), which consists of averaging 10phases of the four-dimensional CT data sets or aver-aging the images from a breathing cycle to match thetemporal resolutions of the CTand the PET data. Thetechnique offers significant advantages comparedwith helical CT (HCT) and enhances significantlythe observed tracer uptake in pulmonary lesions.Fig. 8 illustrates an example of registration errorcaused by an undercorrection of attenuation byHCT [41]. The HCT and ACT images are shown in(A) and (B), respectively. The region of mismatchwas derived from the difference image (E) betweenthe PET data corrected with ACT (D) and the PETdata corrected with HCT (C). The region of differ-ence in quantification corresponds to the differencein the lateral walls between the HCT and the ACTdata. This example emphasizes the importance ofregistration between the PET and the CT data toensure an accurate quantification of the myocardiumdata in PET/CT imaging [41]. Cardiac motion alsocan be a source of misregistration between the CTand PET images and has been described extensivelyin the literature [29–34,112,214,215,222,223]. Simi-lar findings have been reported using combinedSPECT/CT units [224–227].
Artifacts arising from the useof contrast-enhanced CT
Owing to its low sensitivity, perfusion is the only invivo functional information provided by CT incontrast-enhanced studies. On the basis of pub-lished literature, the authors understand that theuse of contrast-enhanced CT in connection withPET/CT imaging remains subject to controversy
Advances in PET Attenuation Correction Techniques 203
Author's personal copy
[228–237]. Diagnostic-quality CT, however, gener-ally dictates the administration of either intrave-nous or oral contrast, or both as in the case oflymphoma studies, and the use of high current, toprovide high-quality diagnostic CT studies. Recentstudies seem to suggest that contrast-enhanced CTmight not be needed in many indications includingHodgkin’s disease and non-Hodgkin’s lymphoma[238,239], whereas it is advised strongly in stagingand therapy planning in nonsmall cell lung cancer[236].
The concern of whether the use of contrast me-dium in dual-modality PET/CT imaging producesmedically significant artifacts remains controversial,
with some studies corroborating [176,228,240,241]and others contradicting [231–233,242,243] thefact that the presence of contrast medium can bea source of errors and artifact when the CT dataare used for attenuation correction of PET imagesdepending on the route of administration andphase protocol of CT imaging [140]. The optimalquantity and route of administration of contrastmedium and potential correction schemes remainopen questions that require further research anddevelopment efforts [139]. Other strategies includethe acquisition of precontrast and postcontrast CTscans that can be used to minimize possible artifactscontributed by the presence of contrast media when
Fig. 6. Illustration of a respiratory motion related artifact on positron emission tomography (PET) images recon-structed with CT-based attenuation correction. (A) Coronal CT, (B) coronal attenuation corrected 18F-FDG PET, (C)coronal fused PET/CT image, (D) coronal nonattenuation corrected 18F-FDG PET, (E) sagittal CT, (F) sagittal atten-uation corrected 18F-FDG PET, (G) sagittal fused PET/CT image, (H) sagittal nonattenuation corrected 18F-FDG PET.A region of decreased metabolic activity is demonstrated in the diaphragmatic region (vertical arrow), repre-senting a cold artifact. Note that this artifact is not apparent on the noncorrected image.
Zaidi et al204
Author's personal copy
the CT scan is to be used as an attenuation map forcorrection of the PET data. As a rule of thumb, exam-ination of the uncorrected images is recommendedto distinguish technical artifacts from physiologic/pathologic hypermetabolism.
Various techniques were suggested to correct forthe presence of oral [242,244–246] and intrave-nous [176,247,248] contrast agents in whole-body PET/CT, including cardiac PET/CT [249].The segmented contrast correction (SCC) methodoriginally proposed by Nehmeh and colleagues[242] consists of identifying through manualsegmentation the regions that contain contrast me-dium and then substitute the CT numbers of pixelsbelonging to these regions with their equivalent ef-fective bone CT numbers, because the commonlyused bilinear calibration curve is derived based onthe assumption that positive CT numbers are con-tributed by a mixture of tissue and bone. The tech-nique later was extended to be applicable tointravenous contrast agents [176]. The techniquewas evaluated using phantom and clinical studiesand proved to accurately recover lesion size anduptake. One of the drawbacks of this technique is
the limited scope of possible applications giventhat the enhanced regions reflecting the spatialdistribution of contrast medium are limited to sim-ple geometric shapes. This limitation renders the al-gorithm of limited value in clinical settings wherethe shapes encountered are rather irregular. Theproblem arises from the difficulty in appropriatelysegmenting and classifying bone and contrast-en-hanced fluids (CEF) in patient’s CT images. Morerecently, an automated algorithm for segmentationand classification of irregular shapes of regionscontaining contrast medium usually found inclinical CT images was proposed for wider applica-bility of the SCC algorithm for correction of oralcontrast artifacts [246]. Fig. 9 shows a clinicalPET/CT study deemed to be problematic to demon-strate the applicability of the previously referencedautomated segmentation technique in a clinicalenvironment. The patient previously had oralbarium administration for esophageal, gastric, andduodenal transit assessment, which was known toremain in the abdomen during the PET/CT scan.It can be seen that the correction of oral contrastartifacts improves the readability and interpretation
Fig. 7. (A) Axial helical CT (HCT) and positron emission tomography (PET) data (corrected by HCT) for a clinicalPET/CT study. (B) Corresponding axial respiration-averaged CT (ACT) and PET data (corrected by ACT). Toenhance interpretation, both HCT and ACT images are shown with CT level of -700 and window width of1000. SUV for HCT PET and ACT PET were 4.3 and 7.4, respectively. SUV increased 70.1% from HCT PET to ACTPET. (C) Coronal HCT, HCT PET, and maximum-intensity projection (MIP) of HCT PET data. (D) Coronal ACT,ACT PET, and MIP of ACT PET data. With ACT, there was a significant reduction in breathing artifacts causedby different breathing states during HCT and PET. Note that ACT did not cover whole lung and was still ableto correct for breathing artifacts. On each image, crosshair or arrow indicates tumor location. (Reprintedfrom Pan T, Mawlawi O, Nehmeh SA, et al. Attenuation correction of PET images with respiration-averagedCT images in PET/CT. J Nucl Med 2005;46:1481–7; with permission.)
Advances in PET Attenuation Correction Techniques 205
Author's personal copy
of the PET scan and shows substantial decrease ofthe SUV (104.3%) in the region containing contrastmedium after correction [246].
Truncation artifacts
Truncation artifacts occur when there is a discrep-ancy between PET and CT fields of view in a com-bined PET/CT scanner. In most commercialdesigns, the FoV of the CT component usually istruncated to 50 cm, whereas the PET FoV may extendup to 70 cm. Truncation artifacts potentially occurwhen scanning extends beyond the CT FoV, whichmight happen frequently when scanning obese pa-tients. It is also very common to extend the CT FoVto 70 cm through analytic extrapolation of the pro-jection. This might increase the bias introduced
into the PET data through the CT-AC procedure,however. Few studies focused on the assessment ofthe impact of artifacts resulting from truncation ofCT images, particularly on tracer activity concentra-tions in clinical oncology resulting in the proposalof various strategies for truncation correction[166–170]. In most of the cases, an extended FoValgorithm is used to estimate complete unmeasuredprojections outside the CT FoV from nonlinearextrapolation of the truncated projections. Perfor-mance assessment of algorithms usually is per-formed by comparing PET tracer distribution anduptake obtained through reconstructions using CTimages reconstructed from truncated and extendedprojections, respectively. It has been shown thattruncation artifacts in whole-body PET/CT lead to
Fig. 8. Illustration of the difference in quantification of the positron emission tomography (PET) data in (E)between the PET data in (C), corrected with the axial helical CT HCT data in (A), and the PET data in (D) correctedwith the ACT data in (B). A segmented region in (E) also is duplicated in the HCT data in (A) and the ACT data in(B). This example demonstrates the cause of misregistration when a part of the lateral walls of myocardium inthe PET data are attenuation corrected with the lower attenuation of the lungs when they should have beencorrected with the higher attenuation of the heart tissues. (Reprinted from Pan T, Mawlawi O, Luo D, et al.Attenuation correction of PET cardiac data with low-dose average CT in PET/CT. Med Phys 2006;33:3931–8;with permission.)
Zaidi et al206
Author's personal copy
visual and quantitative distortions of the CT andattenuation-corrected PET images in the area oftruncation [166–168]. Truncation correction algo-rithms allow one not only to achieve artifact-freeimages in the FoV but also to extend the imagesbeyond the FoV, and these algorithms should beapplied when available.
Artifacts arising from metallic objects
The presence of metallic objects is a major problemin CT, as they tend to generate strong artifacts inreconstructed CT images owing to the presence ofstrongly attenuating objects in the FoV. The pres-ence of metallic dental implants [250,251] or elec-troencephalogram (EEG) electrodes [165] typicallyused for monitoring epilepsy patients can introducevisible artifacts into brain images when CT is used todetermine the attenuation map in PET/CT. Similarobservations have been made for metallic hipprosthetic material [252,253] and pacemakers[160,254,255]. The most important causes of metalartifacts are noise, beam hardening, the non-linearpartial volume effect, and scatter.
The maximum voxel intensity in reconstructedCT images is 3071 HU on virtually all clinical CTscanners except when an extended CT scale isused [256]. The consequence is that metallic objectswill be assigned this maximum value, which
obviously underestimates their true HU. Evenwhen the extended CT scale is used, however, cur-rently available conversion methods likely willundercorrect for attenuation of metallic objects.When the obtained CT data are used for AC of thecorresponding PET emission data, LoRs passingthrough metallic objects will be assigned wrongACFs [165].
The general hypothesis lying behind the develop-ment of metal artifact reduction algorithms is thatthe artifacts are caused by deviations of the acquisi-tion model assumed by the reconstruction from thetrue acquisition process. Consequently, improvingthe acquisition model should reduce artifacts.Various metal artifact reduction (MAR) algorithmshave been suggested in the literature [110,144–165,184,254,255,257–259]. For example, theMAR algorithm proposed in by Lemmens and col-leagues [161,165] starts with an initial reconstruc-tion performed using an iterative ML algorithmfor transmission tomography (MLTR) [158]. Thisinitial image estimate is used to produce a label im-age on which multimodal priors are defined [70]. Amaximum-a-posteriori (MAP) reconstruction thenis performed using these priors to obtain an arti-fact-free starting image [260]. This starting imageserves as the basis for an image-based projectioncompletion procedure, where the measured metal
Fig. 9. Transaxial slices of generated CT-based attenuation maps before (A) and after (B) correction of oralcontrast-related artifacts using an automated segmentation algorithm and corresponding positron emissiontomography (PET) images (C and D) reconstructed using the attenuation maps shown in (A) and (B), respectively.Note the contrast-related artifacts (arrows).
Advances in PET Attenuation Correction Techniques 207
Author's personal copy
projections are substituted by artificially computedprojections. The final step of the algorithm consistsin performing the final reconstruction through theuse of the corrected dataset and MLTR.
Artifacts arising from x-ray scatterin CT images
A limited number of studies have investigatedthe magnitude and spatial distribution of the scattercomponent in radionuclide TX scanning [261,262].Historically, the scatter component was assessedextensively in the context of quantitative CT imag-ing [189,263–265]. Interest in scatter characteriza-tion and correction in CT images was revivedfollowing the introduction of PET/CT and thesuccessful implementation of CT-AC procedures.The scatter component in CT data was assessedboth in fan beam [189,263–265] and cone beam[173,175,266–269], including flat-panel [174–176,270–274] geometries. This is discussed in detail inthe article by Zaidi and Montanden in this specialissue [2].
Summary
High-resolution cutting-edge PET and PET/CT tech-nology is poised to advance the understanding ofhuman disease complexity and improve the clinicalmanagement of patients through translationalresearch. The hope is to be able to provide predic-tive, preventative, and personalized medicine thatis expected to radically transform the practice ofmedicine and shift in health care. This only canbe achieved using quantitative molecular imaging,which provides accurate measures of biological pro-cesses in vivo using the most advanced PET datacorrection and reconstruction algorithms availabletoday. AC is one of the most pertinent correctionsthat needs to be performed to get reliable results.The ability to accurately carry out AC with validatedhardware/software solutions, combined with theuse of rigorous quality control measures, enhancesthe interpretive confidence and accuracy of molecu-lar PET imaging. Consequently, there has beengrowing clinical acceptance of the need to systemat-ically perform AC in clinical setting following itssuccessful implementation in research environ-ments. Postinjection TX scanning remains themost widely used method on standalone PET units,although this is changing rapidly with the introduc-tion of dual-modality PET/CT systems, where CT-AC was imposed as the new gold standard despitethe many problems discussed in this article [14].The development of suitable AC strategies on noveldual-modality imaging technologies such as PET/MR remains challenging and will attract the interest
of active researchers in the field in the foreseeablefuture [81].
Despite the remarkable progress in AC achievedduring the last decade, there is still scope for furtherresearch to address the challenges of novel tech-niques and stringent demands of diagnostic molec-ular imaging. There is every reason to believe thefield will move forward more rapidly in the nearfuture with the advent of better computing powerand the unlimited imagination of researchers inthe field. There is no shortage of challenges and op-portunities, as the field is very open to future novelideas (hardware, and especially software) aimed atimproving the quantitative capabilities of molecu-lar imaging techniques.
References
[1] Zaidi H, Hasegawa BH. Determination of the at-tenuation map in emission tomography. J NuclMed 2003;44:291–315.
[2] Zaidi H, Montandon M. Scatter compensationtechniques in PET. PET Clinics, in press.
[3] Bailey DL. Transmission scanning in emissiontomography. Eur J Nucl Med 1998;25:774–87.
[4] Kinahan PE, Hasegawa BH, Beyer T. x-ray-basedattenuation correction for positron emissiontomography/computed tomography scanners.Semin Nucl Med 2003;33:166–79.
[5] Zaidi H, Montandon M-L, Meikle S. Strategiesfor attenuation compensation in neurologicalPET studies. Neuroimage 2007;34:518–41.
[6] Huang SC, Hoffman EJ, Phelps ME, et al. Quan-titation in positron emission computed tomog-raphy: 2. Effects of inaccurate attenuationcorrection. J Comput Assist Tomogr 1979;3:804–14.
[7] Ficaro EP. Should SPET attenuation correctionbe more widely employed in routine clinicalpractice? For. Eur J Nucl Med 2002;29:409–12.
[8] Wackers FJT. Should SPECT attenuation correc-tion be more widely employed in routine clini-cal practice? Against. Eur J Nucl Med 2002;29:412–5.
[9] Heller GV, Links J, Bateman TM, et al. AmericanSociety of Nuclear Cardiology and Society ofNuclear Medicine joint position statement:attenuation correction of myocardial perfusionSPECT scintigraphy. J Nucl Cardiol 2004;11:229–30.
[10] Garcia EV. SPECT attenuation correction: an es-sential tool to realize nuclear cardiology’s man-ifest destiny. J Nucl Cardiol 2007;14:16–24.
[11] Wahl RL. To AC or not to AC: that is the ques-tion. J Nucl Med 1999;40:2025–8.
[12] Bai C, Kinahan PE, Brasse D, et al. An analyticstudy of the effects of attenuation on tumordetection in whole-body PET oncology imag-ing. J Nucl Med 2003;44:1855–61.
[13] Zaidi H, Sossi V. Correction for image degrad-ing factors is essential for accurate
Zaidi et al208
Author's personal copy
quantification of brain function using PET. MedPhys 2004;31:423–6.
[14] Zaidi H. Is radionuclide transmission scanningobsolete for dual-modality PET/CT systems?Eur J Nucl Med Mol Imaging 2007;34:815–8.
[15] Bengel FM, Ziegler SI, Avril N, et al. Whole-body positron emission tomography in clinicaloncology: comparison between attenuation-corrected and uncorrected images. Eur J NuclMed 1997;24:1091–8.
[16] Bedigian MP, Benard F, Smith RJ, et al. Whole-body positron emission tomography for oncol-ogy imaging using singles transmission scanningwith segmentation and ordered subsets–expec-tation maximization (OS-EM) reconstruction.Eur J Nucl Med 1998;25:659–61.
[17] Bleckmann C, Dose J, Bohuslavizki KH, et al.Effect of attenuation correction on lesion detect-ability in FDG PET of breast cancer. J Nucl Med1999;40:2021–4.
[18] Farquhar TH, Llacer J, Hoh CK, et al. ROCand localization ROC analyses of lesion detec-tion in whole-body FDG PET: effects of acqui-sition mode, attenuation correction, andreconstruction algorithm. J Nucl Med 1999;40:2043–52.
[19] Lonneux M, Borbath I, Bol A, et al. Attenuationcorrection in whole-body FDG oncologicalstudies: the role of statistical reconstruction.Eur J Nucl Med 1999;26:591–8.
[20] Weber WA, Neverve J, Sklarek J, et al. Imaging oflung cancer with fluorine-18 fluorodeoxyglu-cose: comparison of a dual-head gammacamera in coincidence mode with a full-ringpositron emission tomography system. EurJ Nucl Med 1999;26:388–95.
[21] Hustinx R, Dolin RJ, Benard F, et al. Impact ofattenuation correction on the accuracy ofFDG-PET in patients with abdominal tumors:a free-response ROC analysis. Eur J Nucl Med2000;27:1365–71.
[22] Delbeke D, Martin WH, Patton JA, et al. Valueof iterative reconstruction, attenuation correc-tion, and image fusion in the interpretation ofFDG PET images with an integrated dual-headcoincidence camera and x-ray-based attenua-tion maps. Radiology 2001;218:163–71.
[23] Maintas D, Houzard C, Ksyar R, et al. Is nonat-tenuation-corrected PET inferior to body atten-uation-corrected PET or PET/CT in lung cancer?Nucl Instr Meth A 2006;569:167–70.
[24] Reinhardt MJ, Wiethoelter N, Matthies A, et al.PET recognition of pulmonary metastases onPET/CT imaging: impact of attenuation-correctedand nonattenuation-corrected PET images. EurJ Nucl Med Mol Imaging 2006;33:134–9.
[25] Nuyts J, Stroobants S, Dupont P, et al. Reducingloss of image quality because of the attenuationartifact in uncorrected PET whole-body images.J Nucl Med 2002;43:1054–62.
[26] Braem A, Chamizo Llatas M, Chesi E, et al.Feasibility of a novel design of high-resolution
parallax-free Compton-enhanced PET scannerdedicated to brain research. Phys Med Biol2004;49:2547–62.
[27] van den Heuvel OA, Boellaard R, Veltman DJ,et al. Attenuation correction of PET activationstudies in the presence of task-related motion.Neuroimage 2003;19:1501–9.
[28] Zaidi H, Montandon M-L, Slosman DO. Atten-uation compensation in cerebral 3D PET: effectof the attenuation map on absolute and relativequantitation. Eur J Nucl Med Mol Imaging2004;31:52–63.
[29] Bacharach SL, Buvat I. Attenuation correction incardiac positron emission tomography andsingle-photon emission computed tomography.J Nucl Cardiol 1995;2:246–55.
[30] Loghin C, Sdringola S, Gould KL. Commonartifacts in PET myocardial perfusion imagesdue to attenuation–emission misregistration:clinical significance, causes, and solutions.J Nucl Med 2004;45:1029–39.
[31] Souvatzoglou M, Bengel F, Busch R, et al. Atten-uation correction in cardiac PET/CT with threedifferent CT protocols: a comparison with con-ventional PET. Eur J Nucl Med Mol Imaging2007;34:1991–2000.
[32] Lautamaki R, Brown TL, Merrill J, et al. CT-basedattenuation correction in (82)Rb-myocardialperfusion PET-CT: incidence of misalignmentand effect on regional tracer distribution. EurJ Nucl Med Mol Imaging, 2008; in press.
[33] Gould KL, Pan T, Loghin C, et al. Frequent diag-nostic errors in cardiac PET/CT due to misregis-tration of CT attenuation and emission PETimages: a definitive analysis of causes, conse-quences, and corrections. J Nucl Med 2007;48:1112–21.
[34] Cook RAH, Carnes G, Lee T-Y, et al. Respira-tion-averaged CT for attenuation correction incanine cardiac PET/CT. J Nucl Med 2007;48:811–8.
[35] Osman MM, Cohade C, Nakamoto Y, et al.Clinically significant inaccurate localization oflesions with PET/CT: frequency in 300 patients.J Nucl Med 2003;44:240–3.
[36] Goerres GW, Kamel E, Seifert B, et al. Accuracyof image coregistration of pulmonary lesions inpatients with nonsmall cell lung cancer usingan integrated PET/CT system. J Nucl Med2002;43:1469–75.
[37] Goerres GW, Burger C, Kamel E, et al. Respira-tion-induced attenuation artifact at PET/CT:technical considerations. Radiology 2003;226:906–10.
[38] Erdi YE, Nehmeh SA, Pan T, et al. The CTmotion quantitation of lung lesions and its im-pact on PET-measured SUVs. J Nucl Med 2004;45:1287–92.
[39] Pan T, Mawlawi O, Nehmeh SA, et al. Attenua-tion correction of PET images with respiration-averaged CT images in PET/CT. J Nucl Med2005;46:1481–7.
Advances in PET Attenuation Correction Techniques 209
Author's personal copy
[40] Beyer T, Rosenbaum S, Veit P, et al. Respirationartifacts in whole-body (18)F-FDG PET/CTstudies with combined PET/CT tomographsemploying spiral CT technology with 1 to 16detector rows. Eur J Nucl Med Mol Imaging2005;32:1429–39.
[41] Pan T, Mawlawi O, Luo D, et al. Attenuationcorrection of PET cardiac data with low-doseaverage CT in PET/CT. Med Phys 2006;33:3931–8.
[42] Chi P-CM, Mawlawi O, Nehmeh SA, et al.Design of respiration averaged CT for attenua-tion correction of the PET data from PET/CT.Med Phys 2007;34:2039–47.
[43] Dahlbom M, Hoffman E. Problems in signal-to-noise ratio for attenuation correction in high-resolution PET. IEEE Trans Nucl Sci 1987;34:288–93.
[44] Jones WF, Digby WM, Luk WK, et al. Optimiz-ing rod window width in positron emissiontomography. IEEE Trans Med Imaging 1995;14:266–70.
[45] Carson RE, Daube-Witherspoon ME, Green MV.A method for postinjection PET transmissionmeasurements with a rotating source. J NuclMed 1988;29:1558–67.
[46] Daube-Witherspoon M, Carson RE, Green MV.Postinjection transmission attenuation mea-surements for PET. IEEE Trans Nucl Sci 1988;35:757–61.
[47] Hooper PK, Meikle SR, Eberl S, et al. Validationof postinjection transmission measurements forattenuation correction in neurological FDG-PET studies. J Nucl Med 1996;37:128–36.
[48] Thompson CJ, Ranger N, Evans AC, et al. Vali-dation of simultaneous PET emission and trans-mission scans. J Nucl Med 1991;32:154–60.
[49] Meikle SR, Eberl S, Hooper PK, et al. Simulta-neous emission and transmission (SET) scan-ning in neurological PET studies. J ComputAssist Tomogr 1997;21:487–97.
[50] Meikle SR, Bailey DL, Hooper PK, et al. Simulta-neous emission and transmission measurementsfor attenuation correction in whole-body PET.J Nucl Med 1995;36:1680–8.
[51] Lodge MA, Badawi RD, Marsden PK. A clinicalevaluation of the quantitative accuracy of simul-taneous emission/transmission scanning inwhole-body positron emission tomography.Eur J Nucl Med 1998;25:417–23.
[52] Watson CC, Eriksson L, Casey ME, et al. Designand performance of collimated coincidencepoint sources for simultaneous transmissionmeasurements in 3-D PET. IEEE Trans NuclSci 2001;48:673–9.
[53] deKemp RA, Nahmias C. Attenuation correc-tion in PET using single-photon transmissionmeasurement. Med Phys 1994;21:771–8.
[54] Karp JS, Muehllehner G, Qu H, et al. Singlestransmission in volume-imaging PET witha 137Cs source. Phys Med Biol 1995;40:929–44.
[55] Zaidi H, Diaz-Gomez M, Boudraa AE, et al.Fuzzy clustering-based segmented attenuationcorrection in whole-body PET imaging. PhysMed Biol 2002;47:1143–60.
[56] Watson CC, Schaefer A, Luk WK, et al. Clinicalevaluation of single-photon attenuation correc-tion for 3D whole-body PET. IEEE Trans NuclSci 1999;46:1024–31.
[57] de Jong HWAM, Boellaard R, Lenox M, et al.Correction for emission contamination intransmission scans for the high-resolution re-search tomograph. IEEE Trans Nucl Sci 2004;51:673–6.
[58] Boudraa A, Zaidi H. Image segmentation tech-niques in nuclear medicine imaging. In:Zaidi H, editor. Quantitative analysis of nuclearmedicine images. New York: Springer; 2006.p. 308–57.
[59] Meikle SR, Dahlbom M, Cherry SR. Attenuationcorrection using count-limited transmissiondata in positron emission tomography. J NuclMed 1993;34:143–50.
[60] Xu M, Cutler P, Luk W. Adaptive, segmentedattenuation correction for whole-body PETimaging. IEEE Trans Nucl Sci 1996;43:331–6.
[61] Bilger K, Kupferschlager J, Muller-Schauenburg W,et al. Threshold calculation for segmented attenu-ation correction in PET with histogram fitting.IEEE Trans Nucl Sci 2001;48:43–50.
[62] Bettinardi V, Pagani E, Gilardi M, et al. An auto-matic classification technique for attenuationcorrection in positron emission tomography.Eur J Nucl Med 1999;26:447–58.
[63] Tai Y-C, Lin K-P, Dahlbom M, et al. A hybridattenuation correction technique to compen-sate for lung density in 3-D total body PET.IEEE Trans Nucl Sci 1996;43:323–30.
[64] Yu SK, Nahmias C. Segmented attenuation correc-tion using artificial neural networks in positrontomography. Phys Med Biol 1996;41:2189–206.
[65] Reutte B, Klein GJ, Huesman RH. Automated3-D segmentation of respiratory-gated PETtransmission images. IEEE Trans Nucl Sci1997;44:2473–6.
[66] Riddell C, Brigger P, Carson RE, et al. The water-shed algorithm: a method to segment noisy PETtransmission images. IEEE Trans Nucl Sci 1999;46:713–9.
[67] Anderson JMM, Srinivasan R, Mair BA, et al.Hidden Markov model-based attenuation cor-rection for positron emission tomography.IEEE Trans Nucl Sci 2002;49:2103–11.
[68] Fessler JA, Ficaro EP, Clinthorne NH, et al.Grouped-coordinate ascent algorithms forpenalized-likelihood transmission image recon-struction. IEEE Trans Med Imaging 1997;16:166–75.
[69] Alenius S, Ruotsalainen U, Astola J. Attenuationcorrection for PET using count-limited trans-mission images reconstructed with medianroot prior. IEEE Trans Nucl Sci 1999;46:646–51.
Zaidi et al210
Author's personal copy
[70] Nuyts J, Dupont P, Stroobants S, et al. Simulta-neous maximum a posteriori reconstruction ofattenuation and activity distributions fromemission sinograms. IEEE Trans Med Imaging1999;18:393–403.
[71] Kitamura K, Iida H, Shidahara M, et al. Noisereduction in PET attenuation correction usingnonlinear Gaussian filters. IEEE Trans Nucl Sci2000;47:994–9.
[72] Pawitan Y, Bettinardi V, Teras M. Non-Gaussiansmoothing of low-count transmission scans forPET whole-body studies. IEEE Trans Med Imag-ing 2005;24:122–9.
[73] Demirkaya O. Anisotropic diffusion filtering ofPET attenuation data to improve emissionimages. Phys Med Biol 2002;47:N271–8.
[74] Hounsfield GN. Computerized transverse axialscanning (tomography). 1. Description of system.Br J Radiol 1973;46:1016–22.
[75] Nickoloff EL, Perman WH, Esser PD, et al. Leftventricular volume: physical basis for attenua-tion corrections in radionuclide determina-tions. Radiology 1984;152:511–5.
[76] Blankespoor SC, Xu X, Kaiki K, et al. Attenua-tion correction of SPECT using x-ray CT on anemission–transmission CT system: myocardialperfusion assessment. IEEE Trans Nucl Sci1996;43:2263–74.
[77] Kinahan PE, Townsend DW, Beyer T, et al.Attenuation correction for a combined 3DPET/CT scanner. Med Phys 1998;25:2046–53.
[78] TownsendDW, Carney JPJ, Yap JT, et al.PET/CT to-day and tomorrow. J Nucl Med 2004;45:4S–14S.
[79] Rowell NP, Glaholm J, Flower MA, et al. Ana-tomically derived attenuation coefficients foruse in quantitative single photon emissiontomography studies of the thorax. Eur J NuclMed 1992;19:36–40.
[80] Le Goff-Rougetet R, Frouin V, Mangin J-F, et-al.Use of segmented MR images for brain attenu-ation correction in PET. In: Loew MH, editor.Proc. SPIE, Newport Beach, CA, 1994. vol.2167. p. 725–36.
[81] Zaidi H. Is MRI-guided attenuation correctiona viable option for dual-modality PET/MRimaging? Radiology 2007;244:639–42.
[82] El Fakhri G, Kijewski MF, Moore SC. Absoluteactivity quantitation from projections using ananalytical approach: comparison with iterativemethods in Tc-99m and I-123 brain SPECT.IEEE Trans Nucl Sci 2001;48:768–73.
[83] Zaidi H, Montandon M-L, Slosman DO. Mag-netic resonance imaging-guided attenuationand scatter corrections in three-dimensionalbrain positron emission tomography. MedPhys 2003;30:937–48.
[84] ICRU. Tissue substitutes in radiation dosimetryand measurement. Report No. 44. Bethesda(MD): International Commission on Radiolog-ical Units and Measurements; 1989.
[85] Dogdas B, Shattuck DW, Leahy RM. Segmenta-tion of skull and scalp in 3-D human MRI using
mathematical morphology. Hum Brain Mapp2005;26:273–85.
[86] Burbar Z, Grazioso RF, Corbeil J, et al. PET per-formance of MR/PET brain insert tomograph[abstract]. In: Philips B, editor. Proc. of theIEEE Nuclear Science Symposium and MedicalImaging Conference. San Diego, October 29-November 4, 2006. San Diego, CA, 2006.
[87] Fripp J, Crozier S, Warfield SK, et al. Automaticsegmentation of the bone and extraction of thebone & cartilage interface from magnetic reso-nance images of the knee. Phys Med Biol2007;52:1617–31.
[88] Martinez-Moller A, Souvatzoglou M, Botnar R,et al. An approach for MR-based attenuation cor-rection for combined MR/PET: effects of ignor-ing bones [abstract]. J Nucl Med 2007;48:156.
[89] Steinberg J, Zhang J, Sammet S, et al. Attenua-tion maps for PET reconstruction using MRI-based segmentation [abstract]. J Nucl Med2007;48:412P.
[90] Robson MD, Gatehouse PD, Bydder M, et al.Magnetic resonance: an introduction to ultra-short TE (UTE) imaging. J Comput AssistTomogr 2003;27:825–46.
[91] Robson MD, Bydder GM. Clinical ultrashortecho time imaging of bone and other connec-tive tissues. NMR Biomed 2006;19:765–80.
[92] Kadrmas DJ, Rust TC. Feasibility of rapid multi-tracer PET tumor imaging. IEEE Trans Nucl Sci2005;52:1341–7.
[93] Rust TC, Kadrmas DJ. Rapid dual-tracerPTSM+ATSM PET imaging of tumour bloodflow and hypoxia: a simulation study. PhysMed Biol 2006;51:61–75.
[94] Ray N, Acton ST, Altes T, et al. Merging paramet-ric active contours within homogeneous imageregions for MRI-based lung segmentation. IEEETrans Med Imaging 2003;22:189–99.
[95] Heverhagen JT, Hahn HK, Wegmann M, et al.Volumetric analysis of mice lungs in a clinicalmagnetic resonance imaging scanner. MAGMA2004;17:80–5.
[96] Plathow C, Schoebinger M, Fink C, et al. Evalu-ation of lung volumetry using dynamic three-dimensional magnetic resonance imaging.Invest Radiol 2005;40:173–9.
[97] Bottger T, Grunewald K, Schobinger M, et al.Implementation and evaluation of a new work-flow for registration and segmentation of pul-monary MRI data for regional lung perfusionassessment. Phys Med Biol 2007;52:1261–75.
[98] Sensakovic WF, Armato SG III, Starkey A, et al.Automated lung segmentation of diseased andartifact-corrupted magnetic resonance sections.Med Phys 2006;33:3085–93.
[99] Lelieveldt BP, van der Geest RJ, Rezaee MR, et al.Anatomical model matching with fuzzy implicitsurfaces for segmentation of thoracic volumescans. IEEE Trans Med Imaging 1999;18:218–30.
[100] Robinson PJ, Kreel L. Pulmonary tissue attenu-ation with computed tomography: comparison
Advances in PET Attenuation Correction Techniques 211
Author's personal copy
of inspiration and expiration scans. J ComputAssist Tomogr 1979;3:740–8.
[101] Montandon M-L, Zaidi H. Atlas-guided nonuni-form attenuation correction in cerebral 3D PETimaging. Neuroimage 2005;25:278–86.
[102] Hofmann M, Steinke F, Scheel V, et al. MR-basedPET attenuation correction—method and vali-dation. Proc. IEEE Nuclear Science Symposiumand Medical Imaging Conference, 30 Oct. - 03Nov. 2007; Honolulu, Hawaii, USA.
[103] Bronnikov AV. Reconstruction of attenuationmap using discrete consistency conditions.IEEE Trans Med Imaging 2000;19:451–62.
[104] Panin VY, Kehren F, Hamill J, et al. Applicationof discrete data consistency conditions forselecting regularization parameters in PETattenuation map reconstruction. Phys MedBiol 2004;49:2425–36.
[105] Kamel E, Hany TF, Burger C, et al. CT vs 68Geattenuation correction in a combined PET/CTsystem: evaluation of the effect of loweringthe CT tube current. Eur J Nucl Med Mol Imag-ing 2002;29:346–50.
[106] Chin BB, Patel PV, Nakamoto Y, et al. Quantita-tive evaluation of 2-deoxy-2-[18F] fluoro-D-glucose uptake in hepatic metastases withcombined PET-CT: iterative reconstruction withCT attenuation correction versus filtered backprojection with 68Germanium attenuationcorrection. Mol Imaging Biol 2002;4:399–409.
[107] Goerres GW, Schmid DT, Eyrich GK. Do hard-ware artifacts influence the performance ofhead and neck PET scans in patients with oralcavity squamous cell cancer? DentomaxillofacRadiol 2003;32:365–71.
[108] Nakamoto Y, Osman M, Cohade C, et al. PET/CT: comparison of quantitative tracer uptakebetween germanium and CT transmissionattenuation-corrected images. J Nucl Med2002;43:1137–43.
[109] Burger C, Goerres G, Schoenes S, et al. PETattenuation coefficients from CT images: exper-imental evaluation of the transformation of CTinto PET 511-keV attenuation coefficients. EurJ Nucl Med Mol Imaging 2002;29:922–7.
[110] Visvikis D, Costa DC, Croasdale I, et al. CT-based attenuation correction in the calculationof semiquantitative indices of [18F]-FDG uptakein PET. Eur J Nucl Med 2003;30:344–53.
[111] Koepfli P, Hany TF, Wyss CA, et al. CT attenua-tion correction for myocardial perfusion quanti-fication using a PET/CT hybrid scanner. J NuclMed 2004;45:537–42.
[112] Fitzpatrick GM, Wells RG. Simulation study ofrespiratory-induced errors in cardiac positronemission tomography/computed tomography.Med Phys 2006;33:2888–95.
[113] Souvatzoglou M, Ziegler SI, Martinez MJ, et al.Standardised uptake values from PET/CTimages: comparison with conventional attenua-tion-corrected PET. Eur J Nucl Med Mol Imag-ing 2007;34:405–12.
[114] van Dalen JA, Visser EP, Vogel WV, et al. Impactof Ge-68/Ga-68-based versus CT-based attenua-tion correction on PET. Med Phys 2007;34:889–97.
[115] Papathanassiou D, Becker S, Amir R, et al.Respiratory motion artifact in the liver domeon FDG PET/CT: comparison of attenuationcorrection with CT and a caesium externalsource. Eur J Nucl Med Mol Imaging 2005;32:1422–8.
[116] Mirzaei S, Guerchaft M, Bonnier C, et al. Use ofsegmented CT transmission map to avoid metalartifacts in PET images by a PET-CT device. BMCNucl Med 2005;5:3.
[117] Novikov RG. An inversion formula for theattenuated x-ray transformation. Ark Mat2002;40:145–67.
[118] Novikov RG. On the range characterization forthe two-dimensional attenuated x-ray transfor-mation. Inverse Probl 2002;18:677–700.
[119] Natterer F. Inversion of the attenuated radontransform. Inverse Problems 2001;17:113–9.
[120] Boman J, Stromberg J-O. Novikov’s inversionformula for the attenuated radon transform—a new approach. J Geom Anal 2004;14:185–98.
[121] Michel C, Sibomana M, Boi A, et al. PreservingPoisson characteristics of PET data withweighted OSEM reconstruction. Conf. Rec. ofIEEE Nuclear Science Symposium and MedicalImaging Conference, Toronto, ON, 8-14November, 1998;2:1323–9.
[122] Lartizien C, Kinahan PE, Swensson R, et al.Evaluating image reconstruction methods fortumor detection in 3-dimensional whole-bodyPET oncology imaging. J Nucl Med 2003;44:276–90.
[123] Levin C, Zaidi H. Current trends in preclinicalPET system design. PET Clinics, in press.
[124] Chow PL, Rannou FR, Chatziioannou AF.Attenuation correction for small animal PETtomographs. Phys Med Biol 2005;50:1837–50.
[125] Tai YC, Ruangma A, Rowland D, et al. Perfor-mance evaluation of the micro-PET focus:a third-generation micro-PET scanner dedicatedto animal imaging. J Nucl Med 2005;46:455–63.
[126] Fahey FH, Gage HD, Buchheimer N, et al. Eval-uation of the quantitative capability of a high-resolution positron emission tomographyscanner for small animal imaging. J ComputAssist Tomogr 2004;28:842–8.
[127] Lehnert W, Meikle SR, Siegel S, et al. Evaluationof transmission methodology and attenuationcorrection for the micro-PET Focus 220 animalscanner. Phys Med Biol 2006;51:4003–16.
[128] Vandervoort E, Camborde M-L, Jan S, et al.Monte Carlo modeling of singles-mode trans-mission data for small animal PET scanners.Phys Med Biol 2007;52:3169–84.
[129] Thompson CJ, Lecomte R, Cadorette J. Feasibil-ity of using beta-gamma coincidence for 3DPET attenuation correction. IEEE Trans NuclSci 2000;47:1176–81.
Zaidi et al212
Author's personal copy
[130] Camborde M-L, Thompson CJ, Togane D, et al.A positron decay-triggered transmission sourcefor positron emission tomography. IEEE TransNucl Sci 2004;51:53–7.
[131] Ritman EL. Molecular imaging in smallanimals—roles for micro-CT. J Cell BiochemSuppl 2002;39:116–24.
[132] Hwang A, Hasegawa B. Attenuation correctionfor small animal SPECT imaging using x-rayCT data. Med Phys 2005;32:2799–804.
[133] Hwang AB, Taylor CC, Vanbrocklin HF, et al.Attenuation correction of small animal SPECTimages acquired with 125I-Iodorotenone.IEEE Trans Nucl Sci 2006;53:1213–20.
[134] Chow PL, Stout DB, Komisopoulou E, et al.A method of image registration for small ani-mal, multimodality imaging. Phys Med Biol2006;51:379–90.
[135] Goertzen AL, Meadors AK, Silverman RW, et al.Simultaneous molecular and anatomical imag-ing of the mouse in vivo. Phys Med Biol 2002;21:4315–28.
[136] Fontaine R, Belanger F, Cadorette J, et al. Archi-tecture of a dual-modality, high-resolution,fully digital positron emission tomography/computed tomography (PET/CT) scanner forsmall animal imaging. IEEE Trans Nucl Sci2005;52:691–6.
[137] Liang H, Yang Y, Yang K, et al. A micro-PET/CTsystem for in vivo small animal imaging. PhysMed Biol 2007;52:3881–94.
[138] Yao R, Seidel J, Liow J-S, et al. Attenuationcorrection for the NIH ATLAS small animalPET scanner. IEEE Trans Nucl Sci 2005;52:664–8.
[139] Beyer T, Antoch G, Bockisch A, et al. Optimizedintravenous contrast administration for diag-nostic whole-body 18F-FDG PET/CT. J NuclMed 2005;46:429–35.
[140] Brechtel K, Klein M, Vogel M, et al. Optimizedcontrast-enhanced CT protocols for diagnosticwhole-body 18F-FDG PET/CT: technical aspectsof single-phase versus multiphase CT imaging.J Nucl Med 2006;47:470–6.
[141] Nagel CCA, Bosmans G, Dekker ALAJ, et al.Phased attenuation correction in respirationcorrelated computed tomography/positronemitted tomography. Med Phys 2006;33:1840–7.
[142] Li T, Thorndyke B, Schreibmann E, et al.Model-based image reconstruction for four-dimensional PET. Med Phys 2006;33:1288–98.
[143] Lamare F, Cresson T, Savean J, et al. Respiratorymotion correction for PET oncology applica-tions using affine transformation of list modedata. Phys Med Biol 2007;52:121–40.
[144] Lewitt RM, Bates RHT. Image reconstructionfrom projections: III projection completionmethods (theory). Optik 1978;50:189–204.
[145] Kalender WA, Hebel R, Ebersberger J. Reductionof CT artifacts caused by metallic implants.Radiology 1987;164:576–7.
[146] Tuy HK. A postprocessing algorithm to reducemetallic clip artifacts in CT images. Eur Radiol1993;V3:129–34.
[147] Glover GH, Pelc NJ. An algorithm for the reduc-tion of metal clip artifacts in CT reconstruc-tions. Med Phys 1981;8:799–807.
[148] Klotz E, Kalender WA, Sokiransky R, et al. Algo-rithms for the reduction of CT artifacts causedby metallic implants. In: Dwyer SJ, Jost RG,editors. Medical imaging IV: PACS systems de-sign and evaluation 1990;1234:642–50.
[149] Wang G, Snyder DL, O’Sullivan JA, et al. Itera-tive deblurring for CT metal artifact reduction.IEEE Trans Med Imaging 1996;15:657–64.
[150] Williamson JF, Whiting BR, Benac J, et al. Pros-pects for quantitative computed tomographyimaging in the presence of foreign metal bodiesusing statistical image reconstruction. MedPhys 2002;29:2404–18.
[151] Soltanian-Zadeh H, Windham JP, Soltanian-Zadeh J. CT artifact correction: an image-process-ing approach. In: Loew MH, Hanson KM,editors. Medical Imaging 1996:2710:477–85.
[152] Wei J, Chen L, Sandison GA, et al. X-ray CThigh-density artifact suppression in the pres-ence of bones. Phys Med Biol 2004;49:5407–18.
[153] Mahnken AH, Raupach R, Wildberger JE, et al.A new algorithm for metal artifact reductionin computed tomography: in vitro and in vivoevaluation after total hip replacement. InvestRadiol 2003;38:769–75.
[154] Robertson DD, Yuan J, Wang G, et al. Total hipprosthesis metal artifact suppression usingiterative deblurring reconstruction. J ComputAssist Tomogr 1997;21:293–8.
[155] Wang G, Frei T, Vannier MW. Fast iterative algo-rithm for metal artifact reduction in x-ray CT.Acad Radiol 2000;7:607–14.
[156] Zhao S, Robertson DD, Wang G, et al. X-ray CTmetal artifact reduction using wavelets: anapplication for imaging total hip prostheses.IEEE Trans Med Imaging 2000;19:1238–47.
[157] De Man B, Nuyts J, Dupont P, et al. Metal streakartifacts in x-ray computed tomography: a simu-lation study. IEEE Trans Nucl Sci 1999;46:691–6.
[158] De Man B, Nuyts J, Dupont P, et al. Reductionof metal streak artifacts in x-ray computedtomography using a transmission maximuma posteriori algorithm. IEEE Trans Nucl Sci2000;47:977–81.
[159] De Man B, Nuyts J, Dupont P, et al. An iterativemaximum-likelihood polychromatic algorithmfor CT. IEEE Trans Med Imaging 2001;20:999–1008.
[160] Hamill JJ, Brunken RC, Bybel B, et al. A knowl-edge-based method for reducing attenuationartifacts caused by cardiac appliances in myo-cardial PET/CT. Phys Med Biol 2006;51:2901–18.
[161] Lemmens C, Faul D, Hamill J, et al. Suppres-sion of metal streak artifacts in CT using
Advances in PET Attenuation Correction Techniques 213
Author's personal copy
a MAP reconstruction procedure. IEEE NuclearScience Symposium Conference Record 2006;6:3431–7.
[162] Bal M, Spies L. Metal artifact reduction in CTusing tissue class modeling and adaptive prefil-tering. Med Phys 2006;33:2852–9.
[163] Kalvin AD. System and method for reducing re-construction artifacts in computed tomographyimages. United States Patent 5933471, 1999.Available at: http://www.freepatentsonline.com/5933471.html.
[164] Watzke O, Kalender WA. A pragmatic approachto metal artifact reduction in CT: merging ofmetal artifact reduced images. Eur Radiol2004;14:849–56.
[165] Lemmens C, Montandon M-L, Nuyts J, et al.Impact of metal artifacts due to EEG electrodesin brain PET imaging. Proc. IEEE NuclearScience Symposium and Medical ImagingConference, 30 Oct. - 03 Nov. 2007; Honolulu,Hawaii, USA, in press.
[166] Michel C, Noo F, Sibomana M, et al. An itera-tive method for creating attenuation mapsfrom highly truncated CT data. Conf. Proc. ofthe VIIth International Meeting on FullyThree-dimensional Image Reconstruction inRadiology and Nuclear Medicine, Utah, USA,2005:88–91.
[167] Beyer T, Bockisch A, Kuhl H, et al. Whole-body18F-FDG PET/CT in the presence of truncationartifacts. J Nucl Med 2006;47:91–9.
[168] Mawlawi O, Erasmus JJ, Pan T, et al. Truncationartifact on PET/CT: impact on measurements ofactivity concentration and assessment of a cor-rection algorithm. AJR Am J Roentgenol 2006;186:1458–67.
[169] Sourbelle K, Kachelriess M, Kalender WA.Reconstruction from truncated projections inCT using adaptive detruncation. Eur Radiol2005;15:1008–14.
[170] Zamyatin AA, Nakanishi S. Extension of thereconstruction field of view and truncationcorrection using sinogram decomposition.Med Phys 2007;34:1593–604.
[171] Hsieh J, Molthen RC, Dawson CA, et al. An iter-ative approach to the beam hardening correc-tion in cone beam CT. Med Phys 2000;27:23–9.
[172] Kachelriess M, Sourbelle K, Kalender WA.Empirical cupping correction: a first-order rawdata precorrection for cone beam computedtomography. Med Phys 2006;33:1269–74.
[173] Malusek A, Seger MM, Sandborg M, et al. Effectof scatter on reconstructed image quality incone beam computed tomography: evaluationof a scatter reduction optimisation function.Radiat Prot Dosimetry 2005;114:337–40.
[174] Siewerdsen JH, Daly MJ, Bakhtiar B, et al. Asimple, direct method for x-ray scatter estima-tion and correction in digital radiography andcone beam CT. Med Phys 2006;33:187–97.
[175] Zbijewski W, Beekman FJ. Efficient MonteCarlo based scatter artifact reduction in cone
beam micro-CT. IEEE Trans Med Imaging2006;25:817–27.
[176] Ay M, Zaidi H. Assessment of errors caused byx-ray scatter and use of contrast medium whenusing CT-based attenuation correction in PET.Eur J Nucl Med Mol Imaging 2006;33:1301–13.
[177] Beyer T, Kinahan PE, Townsend DW, et al. Theuse of X-ray CT for attenuation correction ofPET data. Proc. IEEE Nuclear Science Symposiumand Medical Imaging Conference, 30 Oct.-5Nov., Norfolk, VA, USA, 4:1573–7.
[178] Bai C, Shao L, Da Silva AJ, et al. A generalizedmodel for the conversion from CT numbersto linear attenuation coefficients. IEEE TransNucl Sci 2003;50:1510–5.
[179] Guy MJ, Castellano-Smith IA, Flower MA, et al.DETECT dual-energy transmission estimationCT for improved attenuation correction in SPECTand PET. IEEE Trans Nucl Sci 1998;45:1261–7.
[180] Kinahan PE, Alessio AM, Fessler JA. Dual-energy CT attenuation correction methods forquantitative assessment of response to cancertherapy with PET/CT imaging. Technol CancerRes Treat 2006;5:319–27.
[181] Flohr TG, McCollough CH, Bruder H, et al. Firstperformance evaluation of a dual-source CT(DSCT) system. Eur Radiol 2006;16:256–68.
[182] Greess H, Lutze J, Nomayr A, et al. Dose reduc-tion in subsecond multislice spiral CT examina-tion of children by online tube currentmodulation. Eur Radiol 2004;14:995–9.
[183] Wang J, Li T, Lu H, et al. Noise reduction forlow-dose single-slice helical CT sinograms.IEEE Trans Nucl Sci 2006;53:1230–7.
[184] Ay M, Zaidi H. Impact of x-ray tube settings andmetallic leads on neurological PET imagingwhen using CT-based attenuation correction.Nucl Instrum Methods Phys Res A 2007;571:411–4.
[185] Ay M, Zaidi H. Computed tomography-basedattenuation correction in neurological positronemission tomography: evaluation of the effectof x-ray tube voltage on quantitative analysis.Nucl Med Commun 2006;27:339–46.
[186] Carney JP, Townsend DW, Rappoport V, et al.Method for transforming CT images for attenu-ation correction in PET/CT imaging. Med Phys2006;33:976–83.
[187] Shikhaliev PM. Beam hardening artifacts incomputed tomography with photon counting,charge integrating and energy weighting detec-tors: a simulation study. Phys Med Biol 2005;50:5813–27.
[188] Alles J, Mudde RF. Beam hardening: analyticalconsiderations of the effective attenuation coef-ficient of x-ray tomography. Med Phys 2007;34:2882–9.
[189] Kanamori H, Nakamori N, Inoue K, et al. Effectof scattered x-ray on CT images. Phys Med Biol1985;30:239–49.
[190] Kachelriess M, Kalender WA. Improving PET/CTattenuation correction with iterative CT beam
Zaidi et al214
Author's personal copy
hardening correction. IEEE Nuclear ScienceSymposium Conference Record San Juan, PuertoRico, October 23–29, 2005;4:5.
[191] Krishnasetty V, Fischman AJ, Halpern EL, et al.Comparison of alignment of computer-registereddata sets: combined PET/CT versus independentPET and CT of the thorax. Radiology 2005;237:635–9.
[192] Xing L, Wessels B. The value of PET/CT is beingoversold as a clinical tool in radiation oncol-ogy. Med Phys 2005;32:1457–9.
[193] Beyer T, Townsend D. Putting clear into nuclearmedicine: a decade of PET/CT development[editorial]. Eur J Nucl Med Mol Imaging2006;33:857–61.
[194] Zaidi H. The quest for the ideal anato–molecu-lar imaging fusion tool. Biomed Imaging IntervJ 2006;2:e47.
[195] Alavi A, Mavi A, Basu S, et al. Is PET-CT the onlyoption? Eur J Nucl Med Mol Imaging 2007;34:819–21.
[196] Rahmim A, Rousset OG, Zaidi H. Strategies formotion tracking and correction in PET. PETClinics, in press.
[197] Pietrzyk U. Does PET/CT render software fusionobsolete? Nuklearmedizin 2005;44:S13–7.
[198] Visvikis D, Lamare F, Bruyant P, et al. Respi-ratory motion in positron emission tomogra-phy for oncology applications: problems andsolutions. Nucl Instr Meth A 2006;569:453–7.
[199] Cohade C, Osman M, Marshall LN, et al. PET-CT: accuracy of PET and CT spatial registrationof lung lesions. Eur J Nucl Med Mol Imaging2003;30:721–6.
[200] Nakamoto Y, Chin BB, Cohade C, et al. PET/CT: artifacts caused by bowel motion. NuclMed Commun 2004;25:221–5.
[201] Cohade C, Wahl RL. Applications of positronemission tomography/computed tomographyimage fusion in clinical positron emission tomog-raphy - clinical use, interpretation, methods, diag-nostic improvements. Semin Nucl Med 2003;33:228–37.
[202] Osman MM, Cohade C, Nakamoto Y, et al.Respiratory motion artifacts on PET emissionimages obtained using CT attenuation correc-tion on PET-CT. Eur J Nucl Med Mol Imaging2003;30:603–6.
[203] Goerres GW, Kamel E, Heidelberg TN, et al.PET-CT image coregistration in the thorax:influence of respiration. Eur J Nucl Med MolImaging 2002;29:351–60.
[204] Pevsner A, Nehmeh SA, Humm JL, et al. Ef-fect of motion on tracer activity determina-tion in CT attenuation corrected PET images:a lung phantom study. Med Phys 2005;32:2358–62.
[205] Nehmeh SA, Erdi YE, Ling CC, et al. Effect ofrespiratory gating on reducing lung motionartifacts in PET imaging of lung cancer. MedPhys 2002;29:366–71.
[206] Nehmeh SA, Erdi YE, Ling CC, et al. Effect ofrespiratory gating on quantifying PET imagesof lung cancer. J Nucl Med 2002;43:876–81.
[207] Nehmeh SA, Erdi YE, Pan T, et al. Four-dimen-sional (4D) PET/CT imaging of the thorax. MedPhys 2004;31:3179–86.
[208] Nehmeh SA, Erdi YE, Pan T, et al. Quantitationof respiratory motion during 4D-PET/CT acqui-sition. Med Phys 2004;31:1333–8.
[209] Nehmeh SA, Erdi YE, Meirelles GS, et al. Deepinspiration breath-hold PET/CT of the thorax.J Nucl Med 2007;48:22–6.
[210] Sarikaya I, Yeung HW, Erdi Y, et al. Respiratoryartifact causing malpositioning of liver domelesion in right lower lung. Clin Nucl Med2003;28:943–4.
[211] Conti M, Bendriem B, Casey M. Performance ofa high sensitivity PET scanner-based on LSOpanel detectors. IEEE Trans Nucl Sci 2006;53:1136–42.
[212] Fitton I, Steenbakkers RJHM, Zijp L, et al. Retro-spective attenuation correction of PET data forradiotherapy planning using a free-breathingCT. Radiother Oncol 2007;83:42–8.
[213] Gilman MD, Fischman AJ, Krishnasetty V, et al.Optimal CT breathing protocol for combinedthoracic PET/CT. AJR Am J Roentgenol 2006;187:1357–60.
[214] Nye JA, Esteves F, Votaw JR. Minimizing artifactsresulting from respiratory and cardiac motionby optimization of the transmission scan incardiac PET/CT. Med Phys 2007;34:1901–6.
[215] Alessio AM, Kohlmyer S, Branch K, et al. CineCT for attenuation correction in cardiac PET/CT. J Nucl Med 2007;48:794–801.
[216] Nehmeh SA, Erdi YE, Rosenzweig KE, et al.Reduction of respiratory motion artifacts inPET imaging of lung cancer by respiratory corre-lated dynamic PET: methodology and compari-son with respiratory gated PET. J Nucl Med2003;44:1644–8.
[217] Mageras GS, Pevsner A, Yorke ED, et al. Mea-surement of lung tumor motion using respira-tion-correlated CT. Int J Radiat Oncol BiolPhys 2004;60:933–41.
[218] Meirelles GSP, Erdi YE, Nehmeh SA, et al. Deepinspiration breath-hold PET/CT: clinical find-ings with a new technique for detection andcharacterization of thoracic lesions. J NuclMed 2007;48:712–9.
[219] Boucher L, Rodrigue S, Lecomte R, et al. Respi-ratory gating for 3-dimensional PET of the tho-rax: feasibility and initial results. J Nucl Med2004;45:214–9.
[220] Martinez-Moller A, Zikic D, Botnar R, et al.Dual cardiac respiratory gated PET: implemen-tation and results from a feasibility study. EurJ Nuc Med Mol Imaging 2007;34:1447–54.
[221] Klein GJ, Reutter BW, Ho MH, et al. Real-time sys-tem for respiratory–cardiac gating in positrontomography. IEEE Trans Nucl Sci 1998;45:2139–43.
Advances in PET Attenuation Correction Techniques 215
Author's personal copy
[222] Le Meunier L, Maass-Moreno R, Carrasquillo JA,et al. PET/CT imaging: effect of respiratorymotion on apparent myocardial uptake. J NuclCardiol 2006;13:821–30.
[223] Martinez-Moller A, Souvatzoglou M, Navab N,et al. Artifacts from misaligned CT in cardiac per-fusion PET/CT studies: frequency, effects,and potential solutions. J Nucl Med 2007;48:188–93.
[224] Takahashi Y, Murase K, Higashino H, et al.Attenuation correction of myocardial SPECTimages with x-ray CT: effects of registrationerrors between x-ray CT and SPECT. Ann NuclMed 2002;16:431–5.
[225] Goetze S, Pannu HK, Wahl RL. Clinically signif-icant abnormal findings on the nondiagnosticCT portion of low-amperage CT attenuation-corrected myocardial perfusion SPECT/CT stud-ies. J Nucl Med 2006;47:1312–8.
[226] Goetze S, Brown TL, Lavely WC, et al. Attenua-tion correction in myocardial perfusion SPECT/CT: effects of misregistration and value of rere-gistration. J Nucl Med 2007;48:1090–5.
[227] Graf S, Khorsand A, Stix G, et al. Attenuationcorrection for myocardial perfusion imaging.A comparison between SPECT and PET imagingby polar map analysis. Nuklearmedizin 2006;45:171–6.
[228] Antoch G, Freudenberg LS, Beyer T, et al. Toenhance or not to enhance? 18F-FDG and CTcontrast agents in dual-modality 18F-FDG PET/CT. J Nucl Med 2004;(45 Suppl 1):56S–65S.
[229] Schaefer NG, Hany TF, Taverna C, et al. Non-Hodgkin lymphoma and Hodgkin disease:coregistered FDG PET and CT at staging andrestaging—do we need contrast-enhanced CT?Radiology 2004;232:823–9.
[230] Strobel K, Thuerl C, Hany T. How much intra-venous contrast is needed in FDG-PET/CT?Nuklearmedizin 2005;44:S32–7.
[231] Yau Y-Y, Chan W-S, Tam Y-M, et al. Applicationof intravenous contrast in PET/CT: does it reallyintroduce significant attenuation correctionerror? J Nucl Med 2005;46:283–91.
[232] Berthelsen AK, Holm S, Loft A, et al. PET/CTwith intravenous contrast can be used for PETattenuation correction in cancer patients. EurJ Nucl Med Mol Imaging 2005;32:1167–75.
[233] Groves AM, Kayani I, Dickson JC, et al. Oralcontrast medium in PET/CT: should you orshouldn’t you? Eur J Nucl Med Mol Imaging2005;32:1160–6.
[234] von Schulthess GK, Veit-Haibach P. Quid desproduits de contraste en TEP/TDM? MedecineNucleaire 2007;31:202–5.
[235] Gollub MJ, Hong R, Sarasohn DM, et al. Limi-tations of CT during PET/CT. J Nucl Med 2007;48:1583–91.
[236] Pfannenberg AC, Aschoff P, Brechtel K, et al.Low-dose nonenhanced CT versus standarddose contrast-enhanced CT in combined PET/CT protocols for staging and therapy planning
in nonsmall cell lung cancer. Eur J Nuc MedMol Imaging 2007;V34:36–44.
[237] Tateishi U, Maeda T, Morimoto T, et al. Nonen-hanced CT versus contrast-enhanced CT in inte-grated PET/CT studies for nodal staging ofrectal cancer. Eur J Nuc Med Mol Imaging2007;34:1627–34.
[238] Rodriguez-Vigil B, Gomez-Leon N, Pinilla I,et al. PET/CT in lymphoma: prospective studyof enhanced full-dose PET/CT versus unen-hanced low-dose PET/CT. J Nucl Med 2006;47:1643–8.
[239] Rodriguez-Vigil B, Gomez-Leon N, Pinilla I,et al. Positron emission tomography/computedtomography in the management of Hodgkin’sdisease and non-Hodgkin’s lymphoma. CurrProbl Diagn Radiol 2006;35:151–63.
[240] Antoch G, Kuehl H, Kanja J, et al. Dual-modal-ity PET/CT scanning with negative oral contrastagent to avoid artifacts: introduction and evalu-ation. Radiology 2004;230:879–85.
[241] Dizendorf E, Hany TF, Buck A, et al. Cause andmagnitude of the error induced by oral CTcontrast agent in CT-based attenuation correc-tion of PET emission studies. J Nucl Med 2003;44:732–8.
[242] Nehmeh SA, Erdi YE, Kalaigian H, et al. Correc-tion for oral contrast artifacts in CT attenuation-corrected PET images obtained by combinedPET/CT. J Nucl Med 2003;44:1940–4.
[243] Nakamoto Y, Chin BB, Kraitchman DL, et al.Effects of nonionic intravenous contrast agentsat PET/CT imaging: phantom and caninestudies. Radiology 2003;227:817–24.
[244] Carney J, Beyer T, Brasse D, et al. CT-basedattenuation correction for PET/CT scanners inthe presence of contrast agent. IEEE NuclearScience Symposium Conference Record 2002;3:1443–6.
[245] Otsuka H, Graham MM, Kubo A, et al.The effect of oral contrast on large bowel activ-ity in FDG-PET/CT. Ann Nucl Med 2005;19:101–8.
[246] Bidgoli J, Ay M, Sarkar S, et al. Correction oforal contrast artifacts in CT-based attenuationcorrection of PET images using an automatedsegmentation algorithm. IEEE Nuclear ScienceSymposium Conference Record, 30 Oct. - 03Nov. 2007; Honolulu, Hawaii, USA, in press.
[247] Tang HR, Brown JK, Da Silva AJ, et al. Imple-mentation of a combined x-ray CT-scintillationcamera imaging system for localizing and mea-suring radionuclide uptake: experiments inphantoms and patients. IEEE Trans Nucl Sci1999;46:551–7.
[248] Lonn AHR. Evaluation of method to minimizethe effect of x-ray contrast in PET-CT attenua-tion correction. Nuclear Science SymposiumConference Record, 2003 IEEE, Portland, USA,2003;3:2220–1.
[249] Buther F, Stegger L, Dawood M, et al. Effectivemethods to correct contrast agent-induced
Zaidi et al216
Author's personal copy
errors in PET quantification in cardiac PET/CT.J Nucl Med 2007;48:1060–8.
[250] Goerres GW, Hany TF, Kamel E, et al. Head andneck imaging with PET and PET/CT: artifactsfrom dental metallic implants. Eur J NuclMed Mol Imaging 2002;29:367–70.
[251] Kamel EM, Burger C, Buck A, et al. Impact ofmetallic dental implants on CT-based attenua-tion correction in a combined PET/CT scanner.Eur Radiol 2003;13:724–8.
[252] Heiba SI, Luo J, Sadek S, et al. Attenuation-cor-rection induced artifact in F-18 FDG PET imag-ing following total knee replacement. ClinPositron Imaging 2000;3:237–9.
[253] Goerres GW, Ziegler SI, Burger C, et al. Artifactsat PET and PET/CT caused by metallic hip pros-thetic material. Radiology 2003;226:577–84.
[254] Halpern BS, Dahlbom M, Waldherr C, et al.Cardiac pacemakers and central venous linescan induce focal artifacts on CT-corrected PETimages. J Nucl Med 2004;45:290–3.
[255] DiFilippo FP, Brunken RC. Do implanted pace-maker leads and ICD leads cause metal-relatedartifact in cardiac PET/CT? J Nucl Med 2005;46:436–43.
[256] Coolens C, Childs PJ. Calibration of CT Houns-field units for radiotherapy treatment planningof patients with metallic hip prostheses: the useof the extended CT-scale. Phys Med Biol 2003;48:1591–603.
[257] Robertson DD, Weiss PJ, Fishman EK, et al.Evaluation of CT techniques for reducing arti-facts in the presence of metallic orthopedicimplants. J Comput Assist Tomogr 1988;12:236–41.
[258] Yu H, Zeng K, Bharkhada DK, et al. A segmen-tation-based method for metal artifact reduc-tion. Acad Radiol 2007;14:495–504.
[259] Olive C, Klaus M, Pekar V, et al. Segmentationaided adaptive filtering for metal artifact reduc-tion in radio-therapeutic CT images. Proc SocPhoto Opt Instrum Eng 2004;5370:1991–2002.
[260] Reader A, Zaidi H. Advances in PET imagereconstruction. PET Clinics, in press.
[261] Thompson CJ, Dagher A, Lunney DN, et al.A technique to reject scattered radiation inPET transmission scans. International work-shop on physics and engineering of com-puterized multidimensional imaging and
processing. Proc Soc Photo Opt Instrum Eng1986;671:244–53.
[262] Wegmann K, Adam L-E, Livieratos L, et al. In-vestigation of the scatter contribution in singlephoton transmission measurements by meansof Monte Carlo simulations. IEEE Trans NuclSci 1999;46:1184–90.
[263] Joseph PM, Spital RD. The effects of scatter inx-ray computed tomography. Med Phys 1982;9:464–72.
[264] Merritt RB, Chenery SG. Quantitative CT mea-surements: the effect of scatter acceptance andfilter characteristics on the EMI 7070. PhysMed Biol 1986;31:55–63.
[265] Ohnesorge B, Flohr T, Klingenbeck-Regn K.Efficient object scatter correction algorithm forthird- and fourth-generation CT scanners. EurRadiol 1999;9:563–9.
[266] Endo M, Tsunoo T, Nakamori N, et al. Effect ofscatter radiation on image noise in cone beamCT. Med Phys 2001;28:469–74.
[267] Rinkel J, Gerfault L, Esteve F, et al. A newmethod for x-ray scatter correction: first assess-ment on a cone-beam CT experimental setup.Phys Med Biol 2007;52:4633–52.
[268] Endo M, Mori S, Tsunoo T, et al. Magnitudeand effects of x-ray scatter in a 256-slice CTscanner. Med Phys 2006;33:3359–68.
[269] Wiegert J, Bertram M, Rose G, et al. Model-based scatter correction for cone beam com-puted tomography. Proc Soc Photo Opt InstrumEng 2005;5745:271–82.
[270] Siewerdsen JH, Jaffray DA. Cone beam com-puted tomography with flat-panel imager: mag-nitude and effects of x-ray scatter. Med Phys2001;28:220–31.
[271] Ning R, Tang X. X-ray scatter correction algo-rithm for cone beam CT imaging. Med Phys2004;31:1195–202.
[272] Kyriakou Y, Kalender WA. X-ray scatter data forflat-panel detector CT. Phys Med 2007;23:3–15.
[273] Zhu L, Bennett NR, Fahrig R. Scatter correctionmethod for x-ray CT using primary modula-tion: theory and preliminary results. IEEE TransMed Imaging 2006;25:1573–87.
[274] Bertram M, Wiegert J, Rose G. Potential of soft-ware-based scatter corrections in cone beamvolume CT. Proc Soc Photo Opt Instrum Eng2005;5745:259–70.
Advances in PET Attenuation Correction Techniques 217