Accumulation of aluminium in lamellar bone after implantation of titanium plates, Ti–6Al–4V...
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Accumulation of aluminium in lamellar bone after implantation of titanium plates, Ti–6Al–4V...
Biomaterials 25 (2004) 3837–3844
ARTICLE IN PRESS
*Correspondin
224-861.
E-mail addres
0142-9612/$ - see
doi:10.1016/j.bio
Accumulation of aluminium in lamellar bone after implantation oftitanium plates, Ti–6Al–4V screws, hydroxyapatite granules
Davide Zaffea,*, Carlo Bertoldib, Ugo Consolob
aDepartments of Anatomy and Histology, Section of Human Anatomy, University of Modena and Reggio Emilia, Via del Pozzo 71, Policlinico,
41100 Modena, MO, ItalybDepartment of Neurosciences, Head-Neck and Rehabilitation, Section of Dentistry, University of Modena and Reggio Emilia, Via del Pozzo 71,
Policlinico, 41100 Modena, MO, Italy
Received 18 June 2003; accepted 7 October 2003
Abstract
Titanium plates, Ti6Al4V screws and surrounding tissues, and biopsies of hydroxyapatite (Osprovits) grafts of maxillary sinus
lifting were investigated to evaluate the release and accumulation of ions. Optical microscopy, SEM and X-ray microanalysis were
carried out to evaluate the plates and screws removed from patients presenting inflammation and biopsies. Ions release from metallic
appliances or leaching from granules towards soft tissues was observed. An accumulation of aluminium but not titanium was found
in soft tissues. A peculiar accumulation of aluminium in the dense lamella of newly formed bone was recorded. The results seem to
indicate that biological perturbations may be related to aluminium release from the tested biomaterials. The aluminium content of
these biomaterials, its diffusion and accumulation are discussed. Further studies on ion release from biomaterials and aluminium
fate in skeletal tissues are suggested.
r 2003 Elsevier Ltd. All rights reserved.
Keywords: Titanium; Hydroxyapatite; EDS; Connective tissue; Bone
1. Introduction
Biomaterials currently in use are primary chosenbecause well tolerated by biological systems. Titanium isa widely used metal in appliances, and hydroxyapatite(natural or synthetic) is the most common ceramicapplied to promote bone defect healing. Sometimes,appliances made of these materials produce unexpectedclinical results or mild side effects. We retain that themolecular composition of the appliance might play arole in these outcomes.Some materials are known to produce inflammatory
responses (chromium, cobalt, copper, nickel, palladium,titanium and zinc alloys) in in vitro studies [1–3] andallergic reactions (chromium, cobalt, nickel, titaniumand Ni/Ti) in vivo [4–6]. Several studies highlight thatelements can diffuse from appliances and accumulate intissues [7–9]. Due to increased particle surface, metallicwear debris [10] may enhance the above mentionedeffects. Optical (OM) and scanning electron (SEM)
g author. Tel.: +39-0594-224-804; fax: +39-0594-
s: [email protected] (D. Zaffe).
front matter r 2003 Elsevier Ltd. All rights reserved.
materials.2003.10.020
microscopy [11] or ultrastructural analysis of tissues andanalysis of metal ions of the system [12–14] have beenperformed in many studies to analyse opaque particles(wear debris). Instead, few studies focus on the elementsreleased from biomaterials, without wear, and theirsubsequent fate in the surrounding tissues [8,15].In this study we analysed the skeletal tissues
surrounding two types of biomaterials without weardebris formation: titanium plates and screws andhydroxyapatite granules. The study was performed onmaterial retrieved from patients with untoward effectsfrom implants, such as swelling, inflammation or clinicaldeficiencies. Tissue morphology was studied using alight microscope and SEM, whereas elemental analysiswas performed by means of an Energy Dispersive X-raySpectroscopy (EDS). This work aims to contribute tobetter our knowledge on biomaterial ion diffusion inperiprosthetic tissues.
2. Materials and methods
The study was performed on (A) titanium appliancesand (B) hydroxyapatite granules used in human beings.
ARTICLE IN PRESSD. Zaffe et al. / Biomaterials 25 (2004) 3837–38443838
(A)
A total of 12 plates and 51 titanium screws(Gebr .uder Martin GmbH & Co. KG, Tuttlingen,D), 4 or more screws necessary to fix a plate, wereremoved 1–6 years after surgery from 6 trauma(facial bone fractured) patients (aged from 25 to 65years). Patients had previously undergone maxillo-facial surgery and fixing of bone segments bytitanium plates (internal rigid fixation). The metallicappliances and surrounding tissue were harvestedfrom selected patients who presented a markedlocal inflammation without dark pigmentation ofthe mucosa. This excluded exposed devices ordevices producing metallic particles that led tomucosal pigmentation. Plates and screws and thesoft and hard tissues surrounding them were fixedin 4% paraformaldehyde in 0.1m phosphate buffer,pH 7.2 for 4 h at room temperature, then dehy-drated through an ethanol series. Part of theconnective tissue adjacent to the appliance wasdetached and embedded in paraffin and in methyl-methacrylate (PMMA). Plates, screws and theadjacent soft tissue were desiccated in a criticalpoint dryer (CPD030, Bal-Tec, FL) at a tempera-ture of 40�C and pressure of 7.4MPa, using CO2 asthe intermediate agent. A small fragment of bone incontact with the plate was harvested with theappliances, fixed in paraformaldehyde, dehydratedand embedded in PMMA without decalcification.Titanium plates and screws and the surroundingconnective tissue used to study the titanium release[16] were used as controls.(B)
Biopsies were performed 3–6 months after surgeryin 6 additional patients (ranging in age from 42 to67 years) with atrophic maxillary bone. Patientshad previously undergone lifting of the sinus floorto achieve adequate bone volume for titaniumimplant (implant-based prosthetic rehabilitation).Sinus lift was performed using a 50/50 (v/v) mixtureof autologous bone/Osprovits (porous hydroxya-patite granule, Feldm .uhle A.G., Plochingen, D),externally covered by the vestibular periosteum.Osprovits is a trade hydroxyapatite materialcommonly used in oral and maxillo-facial treat-ments of bone defects. Biopsies were executed afterradiographies showed anomalous radiotransparentareas inside the graft. Biopsies were fixed in 4%paraformaldehyde in 0.1m phosphate buffer, pH7.2 for 1 h at room temperature and then at 4�C,dehydrated through an ethanol series and em-bedded in PMMA without decalcification.The PMMA blocks containing soft tissues or bonewere sectioned using a bone microtome (Autocut1150,Reichert-Jung GmbH, NuXloc, D) to obtain 5 micron-thick slices. The sections were stained with Hematox-ylin-Eosin, Toluidine Blue or histochemically treated
[17] to detect total alkaline phosphatase (TALP) andtartrate resistant acid phosphatase (TRAP). The re-maining part of the PMMA block containing bone wassectioned using a diamond saw microtome (1600, Leica,Wetzlar, D) to obtain a 1mm-thick slice. The surface ofeach section was polished with sandpaper and diamondcompound (3 mm). The polished sections and appliancessurrounded by fibrous tissue were carbon coated (CED020, Bal-Tec, FL), examined by SEM using a back-scattered electron detector (XL40, Philips, NL) andanalysed with an X-ray microprobe, EDS system(EDAX9900, Philips, Heindhoven, NL), at 25 kV, 0�
tilt, 31� take-off, 0.08 mm spot. Each specimen wassubmitted to 10–30 X-ray analyses at different sites.Semiquantitative analysis was subsequently performedafter the appropriate ZAF (Z, atomic number; A,absorption; F, secondary fluorescence) correction [18].X-ray maps (128� 100 pixel) were drawn up under thesame analysis conditions, but with 0.1 mm spot and 0.2 sdwell-time. Embedded bone, not mixed with Osprovits,and connective tissue from each patient were used ascontrols. The hydroxyapatite (produced by Fin-Cera-mica Faenza s.r.l., Faenza RA, Italy) and the surround-ing tissues of a previous study [19] were used as controls.
3. Results
3.1. Titanium appliances
No substantial differences were observed among thebiopsies despite the different implant time (1–6 years).Histology of the connective tissue showed a feeblelymphoplasmacytic reaction and polymorphonuclearinfiltrate with many mast cells. Scattered mastocyteswere found inside the fibrous tissue. SEM displayed anearly smooth surface of plates and screws, with noscratches or other alterations (Fig. 1).EDS confirmed the Ti/Al/V composition (90/6/
4wt%), i.e. Ti6Al4V alloy, of the screws and the puretitanium composition of all titanium plates (Fig. 2,graphs and ). EDS analysis on the fibrous tissueenveloping plates and screws revealed titanium inproximity of the metal parts. In the connective tissuelayer (100–150 mm thickness) adjacent to the titaniumappliance, titanium release followed a decreasing con-centration gradient, whereas no titanium was found at adistance greater than 300–500 mm. On the contrary,aluminium was found in connective tissue in proximityof the Ti6Al4V screws and adjacent to plates (Fig. 1),even though the aluminium content was low in thelatter. Instead, the aluminium content detected in thefibrous tissue near Ti6Al4V screws was very high (Fig. 2,graph ), and aluminium was also found at a distancegreater than 300–500 mm.
ARTICLE IN PRESS
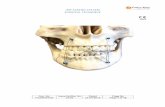
Fig. 1. Back-scattered SEM images showing the fibrous tissue
surrounding a titanium plate (A) and a Ti6Al4V screwhead (B). Note
the tissue density. The numbers indicate the sites that correspond to
the EDS analysis reported in Fig. 2. Field width: A ¼ 4:4mm;B ¼ 1:75mm.
Fig. 2. Graphs showing the EDS (full area at � 5000 SEM
magnification) of a Ti6Al4V screw ( ) and titanium plate ( ), plotted
on the same scale, and the fibrous tissue ( ) bounded to a Ti4Al6V
screw (see Fig. 1). Note in how fibrous tissue reveals the usual
elements such as carbon, oxygen, phosphorous and calcium, in
addition to titanium (small amounts) and aluminium (great amounts).
D. Zaffe et al. / Biomaterials 25 (2004) 3837–3844 3839
Titanium was not detected in lamellar bone surround-ing titanium plates. On the contrary, aluminium wasalmost always detected in lamellar bone (Fig. 3, bs).EDS analysis revealed aluminium in lamellar bone, bothnear the screw surfaces but also at a distance greater
than 1–2mm. The dense lamella, named also acellularlamella (Fig. 3), showed a very high aluminium contentwhereas only traces of aluminium were found in theloose lamella, also named cellular lamella (Fig. 3, ).No aluminium was detected in woven bone.Moreover, no aluminium was detected in the fibrous
control tissues.
3.2. Hydroxyapatite granules
Histology confirmed an adequate amount of newlyformed bone, residues of autologous bone and frag-mented Osprovits granules in 3-month biopsies (Fig. 4).Autologous bone presented a highly indented surface(Howship lacunae) due to osteoclast aggression. Newbone, woven but with lamellar structure in many parts,was more often located at a distance from granules,whereas fragmented bone was found in the proximity offragmented granules (Fig. 4). In 6-month biopsies, theamount of bone and granules were lower than pre-viously recorded. Hydroxyapatite granules were highlyfragmented and surrounded by large zones of fibroustissue.In 3-month biopsies, the TRAP reaction detected
several osteoclast-like cells eroding the Osprovits
porous granules (Fig. 5A). Few TRAP reactive cellswere found on the bone surrounding the granuleswhereas many TRAP reactive cells were located closeto the outer surface and on the surface of the internalcavities of granules (Fig. 5A, arrows). In 6-monthbiopsies, the number of granules was low and, accord-ingly, few TRAP reactive cells were found.The TALP reaction was strongly expressed only in
3-month biopsies, on autologous bone located far fromthe hydroxyapatite granules (Fig. 5B). No evidence ofTALP was found both around the granules and itssurrounding bone fragments. In the latter, the bonesurface was highly indented subsequent to osteoclastactivity. TALP was poorly expressed around bone in6-month biopsies.EDS revealed aluminium in skeletal tissue surround-
ing hydroxyapatite granules (Fig. 6). The amount ofaluminium was higher in the connective tissue contain-ing large amounts of phosphorous and calcium (Fig. 6,Al and P maps; Fig. 7, graph ). Nevertheless, aremarkable aluminium content was also found in siteswith fibrous tissue poor in phosphorous and calcium(Fig. 6, Al and P maps; Fig. 7, graph ).Semiquantitative X-ray analyses of unimplanted and
embedded Osprovits revealed an uneven aluminiumcontent in granules. The mean aluminium content ofeach unimplanted granule ranged between 0% and0.5%.EDS detected aluminium in bone adjacent to the
granules and also in newly formed bone located far fromthe granules. No aluminium was found in lamellar
ARTICLE IN PRESS
Fig. 3. Back-scattered SEM image (bs) and X-ray maps for aluminium (Al) and phosphorus (P) showing three dense lamellae (asterisks) and an
osteocyte lacunae (inside a large loose lamella) of lamellar bone formed at a distance from the titanium plate. The dense lamellae (darker in bs and P)
have a low phosphorus (P) but high aluminium content (lighter in Al). The opposite is seen in the loose lamella (lighter in bs and P). Field
width=32.5 mm.
Fig. 4. Back-scattered SEM image showing a 3-month Osprovits
biopsy. Note on the right how granules appear highly fragmented and
surrounded by bone fragments. The arrows point to autologous bone
residues (light gray), the result of osteoclast erosion, on which the
osteoblasts have formed the new bone (NFB). Field width=1200mm.
Fig. 5. Optical microscope images showing the result of TRAP (A)
and TALP (B) histochemical reactions performed on a 3-month
Osprovits biopsy. The black arrows in A point to osteoclast-like cells
(red in slide) which erode the granule (O). An osteoclast in the fibrous
tissue is identified by a white arrow; no osteoclasts are eroding the
bone (b). In B note the osteoblast lamina, identified by the positive
reaction for alkaline phosphatase (blue in slide). Osteoblasts form new
bone in apposition on autologous bone (b), confirmed microradio-
D. Zaffe et al. / Biomaterials 25 (2004) 3837–38443840
autologous bone (evaluated on microradiographs andwith the back-scattered SEM probe) and in newlyformed woven bone at a distance from hydroxyapatite.On the contrary, newly formed lamellar bone (Fig. 8)was peculiarly rich in aluminium: loose lamella con-tained little aluminium whereas dense lamella containedgreater amounts of aluminium (Fig. 9).No aluminium was detected in control bone and
connective tissues. Moreover, no aluminium was de-tected in hydroxyapatite (produced by Fin-Ceramica)and in the surrounding newly formed hard and softtissue inside a hydroxyapatite chamber implanted inrabbit [19].
graphically, at a distance from the Osprovits granules. Field width:
A ¼ B ¼ 350mm.
4. Discussion
Titanium and hydroxyapatite are considered goodbiomaterials. They normally give excellent results [19,20]
and are widely used in implantology due to theirhigh biocompatibility. The observed interference ofthese materials with oral tissue is probably due to
ARTICLE IN PRESS
Fig. 6. Back-scattered SEM image (bs) and X-ray maps for oxygen (O), aluminium (Al) and phosphorus (P) showing the topographic composition of
a 3-month Osprovits biopsy. The greater the element content, the lighter the pixel. The numbers indicate the sites that correspond to the EDS
analysis reported in Fig. 7. Field width=250mm.
D. Zaffe et al. / Biomaterials 25 (2004) 3837–3844 3841
different reasons for the metallic and ceramic materialtested.EDS reveals titanium release from the surfaces of the
tested metallic appliances. In a recent work [16] weshowed that titanium produces small amounts of ionswhich are rapidly drained through skeletal tissues.Ti6Al4V releases titanium but also aluminium andvanadium. We were not able to follow the fate ofvanadium ions because in the EDS method appliedvanadium Ka emission (4.95 keV) is covered by titaniumKb emission (4.93 keV). On the contrary we can easilystudy the aluminium, whose release from Ti6Al4Vscrews can probably be ascribed to the activity ofcells and biological fluids. Operation processes andfretting between plate and screw might be an additionalcause of ion release. We did not find metallic debris atthe plate removal. A debris dissolution probablyoccurred over the extended period from positioning toremoval.
Hydroxyapatite does not contain aluminium, butsmall amounts of aluminium were detected in Ospro-vits granules. We cannot ascribe the aluminium contentof the tested granules to impurities in the originalmaterial or to the manufacturing processes. Granulesrelease large amount of aluminium which is not drainedoff like titanium [16] but stored locally. This highaluminium concentration may produce biological per-turbations: not only is bone erosion enhanced, butosteoclast-like cells erode the granules reducing them tosmall fragments. Moreover, granule erosion increasesthe surface-bulk rate and perpetuates aluminium release.This boosted erosion is probably not the first eventwhich occurs after grafting. Erosion of autologous boneis normal after a sinus lift, but new bone is soon formedin apposition to the residues of autologous bone. At thesame time, new bone is formed in proximity of thegranule before hydroxyapatite dissolution. The lastevent blocked bone deposition near the granules and
ARTICLE IN PRESS
Fig. 9. Graphs (all plotted on the same scale) showing the EDS (full
area at � 10,000 SEM magnification) of a dense ( ) and loose ( )
lamella of bone, formed at a distance from the Osprovits granules.
Note how the aluminium peak (1.49 keV) is hardly plotted in the loose
lamella whereas a strong peak can be observed in the dense lamella.Fig. 7. Graphs (all plotted on the same scale) showing the EDS (full
area at � 5000 SEM magnification) of Osprovits granule ( ), and of
sites rich ( ) and poor ( ) in P and Ca of fibrous tissue (see Fig. 6).
Note how the aluminium peak (1.49 keV) is the highest on both sites of
fibrous tissue.
Fig. 8. Back-scattered SEM image showing the bone, formed at a
distance from Osprovits granules, in a 3-month biopsy. The new bone
was formed in apposition to a residue of autologous bone (AB—lighter
in the image), presenting an indented surface due to osteoclast erosion.
The numbers indicate the sites that correspond to the EDS analysis
reported in Fig. 9. Field width=205 mm.
D. Zaffe et al. / Biomaterials 25 (2004) 3837–38443842
produced initial bone erosion, transforming bonetrabeculae into small fragments, after which erosionactivity focused on the granule surfaces. This is thetypical situation found 3 months after implant; 6months after implant, bone mass was reduced. Hydro-xyapatite is used to avoid this event, which normallyoccurs after bone grafting (subsidence). We believe thatthe hydroxyapatite tested not only obviates subsidencebut prompts severe osteoclasia.Despite different biomaterials, skeletal tissues show
the same behaviour towards aluminium. In line withShahgaldi et al. [21], our results indicate that aluminiumis locally accumulated in soft tissue. A long period ofaluminium draining follows, and aluminium accumula-
tion in soft tissues will eventually cease if new releasedoes not occur. This draining and diffusion of alumi-nium towards the surrounding soft tissues may explainthe peculiar accumulation of aluminium in bone in sitesdistant from the biomaterials. In fact, newly formedlamellar bone had marked aluminium accumulation,and a large amount of aluminium was found inside thedense lamella.Lamellar bone is not a variety of parallel-fibred bone
[22,23] but, instead, is made up of alternating collagen-rich (dense lamellae) and collagen-poor (loose lamellae)layers, all having an interwoven arrangement of fibres[22–24]. The loose lamella is also named cellular lamellabecause it contains osteocyte lacunae, whereas the denselamella is also named acellular lamella due to theabsence of lacunae. The lamellae have a relativelyconstant size in osteons [23,24]: the dense lamella isthinner (about 1.5–2 mm) and the loose lamella isbroader (about 3–6 and up mm). It has been hypothe-sized that the alternation of dense and loose lamellaedepends on osteocyte recruitment from osteogeniclaminae in successive layers [23]. The loose lamellacontains fewer fibres but more bone matrix, the denselamella contains more fibres but less bone matrix. Dueto the high affinity for calcium salt of the bone matrix,the loose lamella is more mineralized whereas the denselamella has the same apatitic structure (Ca/P=2.15w/w) but is less mineralized (about 2–4% in Ca content)[25].We can make two speculations: (A) collagen has a
higher affinity for aluminium than bone matrix, so thatthe dense lamella is richer in this element; (B) if collagenproduction by the osteoblast remains constant over thetime required to form two adjacent lamellae, thedifference between the loose and dense lamella maydepend on matrix production but not on the time offormation. Osteocyte recruitment constitutes a signalfor osteogenic lamina: osteoblasts and preosteocytes
ARTICLE IN PRESSD. Zaffe et al. / Biomaterials 25 (2004) 3837–3844 3843
become active in abundant matrix production, and soloose lamella is formed. If the aluminium concentrationof soft tissue surrounding the osteogenic lamina remainssubstantially constant, the dense and loose lamellashould contain an equal amount of aluminium. How-ever, the lower the lamella thickness, the higher thealuminium density. Both events may occur at the sametime. Further studies are needed to confirm ourhypothesis.Aluminium is an element involved in severe neurolo-
gical, e.g. Alzheimer’s disease [26], and metabolic bonediseases, e.g. osteomalacia [27]. Aluminium accumula-tion in bone is only a temporal soft tissue deprivation.Bone remodeling will produce further aluminiumrelease, even after the appliances no longer leach outaluminium, perpetrating the dangerous side effects ofthis element [26,27].
5. Conclusions
Our results highlight that biocompatible materialsmay lead to problems due to impurities contained inbiomaterial (as in the examined hydroxyapatite) or toaluminium alloys (Ti4Al6V). Our results show thataluminium is able to perturb the biological systemcausing the local inflammation. We do not know if thesmall amount of aluminium released from the testedappliances can have a systemic impact or promote severeneurological and metabolic bone diseases. This aspectwill need additional quantitative studies, as also under-lined by Chang et al. [28], in terms of elements known tobe dangerous but also for titanium which we advancemight be active in bone processes [16].Our results document a slow drainage of aluminium
by fibrous tissue and a peculiar accumulation in lamellarbone. We do not know the fate and meaning of theseeffects, what happens when bone is remodeled, and ifaluminium is accumulated in the same way in allsituations. Since our work was performed in man, wedo not know the relationship between aluminium–boneaccumulation and the amount of aluminium releasefrom biomaterial, in particular if all the skeletalsegments are concerned. Another question may concernthe aluminium introduced ‘‘per os’’: is aluminiumaccumulated in bone in the same way? Only furthermore in depth qualitative and quantitative studies withexperimental animals and different types of biomaterialscontaining aluminium or diet treatments will be able toanswer these questions.
Acknowledgements
The authors wish to thank Dr. John Pradelli, M.D.for assistance in manuscript revision and the ‘‘Centro
Interdipartimentale Grandi Strumenti’’ (CIGS) of theUniversity of Modena and Reggio Emilia for software,SEM and EDS availability and assistance. The ResearchFund of the Department of Anatomy and Histology,University of Modena and Reggio Emilia supported thisinvestigation.
References
[1] Rogers SD, Howie DW, Graves SE, Pearcy MJ, Haynes DR. In
vitro human monocyte response to wear particles of titanium
alloy containing vanadium or niobium. J Bone Joint Surg 1997;
79B:311–5.
[2] Horowitz SM, Luchetti WT, Gonzales JB, Ritchie CK. The
effects of cobalt chromium upon macrophages. J Biomed Mater
Res 1998;41:468–73.
[3] Schmalz G, Schuster U, Schweikl H. Influence of metals on IL-6
release in vitro. Biomaterials 1998;19:1689–94.
[4] Burden DJ, Eedy DJ. Orthodontic headgear related to allergic
contact dermatitis: a case report. Br Dent J 1991;170:447–8.
[5] Veien NK, Borchorst E, Hattel T, Laurberg G. Stomatitis or
systemically induced contact dermatitis from metal wire in
orthodontic materials. Contact Dermatitis 1994;30:210–3.
[6] Tamai K, Mitsumori M, Fujishiro S, Kokubo M, Ooya N,
Nagata Y, Sasai K, Hiraoka M, Inamoto T. A case of allergic
reaction to surgical metal clips inserted for postoperative boost
irradiation in a patient undergoing breast-conserving therapy.
Breast Cancer 2001;8:90–2.
[7] Moberg IE, Norderam A, Kjellman O. Metal release from plates
used in jaw fracture treatment. J Oral Maxillofac Surg 1989;18:
311–4.
[8] Torgersen S, Gjerdet NR, Erichsen ES, Bang G. Metal particles
and tissue changes adjacent to miniplates. A retrieval study. Acta
Odontol Scand 1995;53:65–71.
[9] Alpert B, Seligson D. Removal of asymptomatic bone plates used
for orthognathic surgery and facial fractures. J Oral Maxillofac
Surg 1996;54:618–21.
[10] Kohilas K, Lyons M, Lofthouse R, Frondoza CG, Jinnah R,
Hungerford DS. Effect of prosthetic titanium wear debris on
mitogen-induced monocyte and lymphoid activation. J Biomed
Mater Res 1999;47:95–103.
[11] Breen DJ, Stoker DJ, Acero J, Calderon J, Salmeron JI,
Verdaguer JJ, Concejo C, Somacarrera ML. The behaviour of
titanium as biomaterial: microscopy study of plates and
surrounding tissues in facial osteosynthesis. J Craniomaxillofac
Surg 1999;27:117–23.
[12] Woodman JL, Jacobs JJ, Galante JO, Urban RM. Metal ion
release from titanium-based prosthetic segmental replacement of
long bones in baboons. A long-term study. J Orthop Res 1984;
1:421–30.
[13] Onodera K, Ooya K, Kawamura H. Titanium lymph node
pigmentation in the reconstruction plate system of a mandibular
bone defect. Oral Surg Oral Med Oral Pathol 1993;75:495–7.
[14] Schliephake H, Lehmann H, Kunz U, Schmelzeisen R. Ultra-
structural findings in soft tissues adjacent to titanium plates used
in jaw fracture treatment. Int J Oral Maxillofac Surg 1993;22:
20–5.
[15] Jorgenson DS, Mayer MH, Ellenbogen RG, Centeno JA,
Johnson FB, Mullick FG, Manson PN. Detection of titanium
in human tissues after craniofacial surgery. Plast Reconstr Surg
1997;99:976–9.
[16] Zaffe D, Bertoldi C, Consolo U. Element release from titanium
devices used in oral and maxillofacial surgery. Biomaterials
2003;24:1093–9.
ARTICLE IN PRESSD. Zaffe et al. / Biomaterials 25 (2004) 3837–38443844
[17] Zaffe D, Bertoldi C, Palumbo C, Consolo U. Morphofunctional
and clinical study on mandibular alveolar distraction osteogen-
esis. Clin Oral Implant Res 2002;13:550–7.
[18] Sanchez-Quevedo MC, Crespo PV, Garcia JM, Campos A. X-ray
microanalytical histochemistry of human circumpulpar and
mantle dentine. Bone Miner 1989;6:323–9.
[19] Zaffe D, Adani R, Ravaglioli A, Kraiewski A, Mazzocchi M. An
HA-chamber for biomaterial evaluations: first results. In:
Ravaglioli A, Krajewski A, editors. Proceedings of the Seventh
CCT—Seminar and Meeting on Biomimetic Engineering, ISTEC-
CNR, Faenza, Italy, 2002. p. 266–72.
[20] Soncini M, Rodriguez-y-Baena R, Pietrabissa R, Quaglini V,
Rizzo S, Zaffe D. Experimental procedure for the evaluation of
the mechanical properties of the bone surrounding dental
implants. Biomaterials 2002;23:9–17.
[21] Shahgaldi BF, Heatley FW, Dewar A, Corrin B. In vivo corrosion
of cobalt-chromium and titanium wear particles. J Bone Joint
Surg Br 1995;77:962–6.
[22] Marotti G. A new theory of bone lamellation. Calcif Tissue Int
1993;53(Suppl. 1):S47.
[23] Marotti G. The structure of bone tissues and the cellular control
of their deposition. Ital J Anat Embryol 1996;101:25–79.
[24] Ardizzoni A. Osteocyte lacunar size–lamellar thickness relation-
ships in human secondary osteons. Bone 2001;28:215–9.
[25] Marotti G, Muglia MA, Palumbo C, Zaffe D. The microscopic
determinants of bone mechanical properties. Ital J Miner
Electrolyte Metab 1994;8:167–75.
[26] Mjoberg B, Hellquist E, Mallmin H, Lindh U. Aluminum,
Alzheimer’s disease and bone fragility. Acta Orthop Scand
1997;68:511–4.
[27] Boyce BF, Byars J, McWilliams S, Mocan MZ, Elder HY, Boyle
IT, Junor BJ. Histological and electron microprobe studies of
mineralisation in aluminium-related osteomalacia. J Clin Pathol
1992;45:502–50.
[28] Chang TJ, Werd MB, Hovelsen C. Metallic implants used in foot
surgery. Clin Podiatr Med Surg 1995;12:457–74.