Tissue microarray - a high-throughput molecular analysis in head and neck cancer
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Tissue microarray - a high-throughput molecular analysis in head and neck cancer
REVIEW ARTICLE
Tissue microarray – a high-throughput molecular analysis inhead and neck cancer
Raghu Radhakrishnan1, Monica Solomon
1, Kapaettu Satyamoorthy
2, Leslie E. Martin
3, Mark W. Lingen
3
1Department of Oral Pathology, MCODS, MAHE, Manipal, India; 2Department of Molecular and Cellular Biology, MAHE LifeSciences Center, Manipal, India; 3Department of Pathology, University of Chicago, Chicago, IL, USA
With the identification of a number of novel markers
having diagnostic, prognostic, and therapeutic signifi-
cance, the application of tissue microarray (TMA) has
become a valuable tool for validating candidate markers
in cancer research. The TMA is a high-throughput tech-
nique, which allows large-scale analyses of hundreds of
archival clinical tissue samples using the ‘array’ approach.
This paper highlights briefly its robust technology, tech-
nical aspects of its construction, and the validity of the
TMA results for oral pathology diagnostics by reviewing
data from recent literature particularly with reference to
head and neck cancer.
J Oral Pathol Med (2008) 37: 166–176
Keywords: head and neck cancer; oral cancer; tissue microarray
Introduction
Identification and characterization of novel molecularmarkers using robust approaches provide a powerfulmeans of discovering disease-related targets. With thecompletion of human genome sequences, informationon majority of genes and their validation at once havebecome possible using functional techniques, such ascDNA arrays (1), Serial Analysis of Gene Expression(2), and proteomics approaches. Besides determininggenes which are truly significant in terms of diagnosis,prognosis, and therapy, the development of these high-throughput screening accelerates pace of research forbasic pathologists. Correlation of genes and proteins,involved in many signaling pathways resulting in theuncontrolled proliferation of cells and their expressioncould be analyzed in situ at the molecular level by
assessing tissues in tandem utilizing tissue microarrayanalysis (TMA; 3).
Traditionally, pathologists study hundreds and thou-sands of tissue sections slide by slide, which is unfortu-nately laborious and time-consuming. Nevertheless, thistype of approach is necessary for diagnostics and⁄ordetection of specific features from the whole section.Although the primary goal of pathologist was to providea diagnostic consultation, it only answers the clinician’simmediate query of what the disease is, but not why orhow the disease has occurred. The fundamental issues ofbasic research are unanswered by these methods becauseof shortage of tissue sections in terms of both the numberand amount. The classic phrase in conclusion eventuallywould be that further studies are deemed necessary usingother markers and using larger sample size. The difficultyof working with human tissue is further compounded byincreasingly stringent guidelines particularly regardingobtaining informed patient consent for its use.
Tissue microarrays come to the fore
In 1986, Hector Battifora (4) first introduced theso-called ‘sausage’ or Multi Tumor Tissue Block, whereup to 100 separate tissues were processed together in onesingle paraffin wax block. In this method, 1-mm-thickrods of tissue specimen were carefully wrapped in sheetsof small intestine and this sausage of tissue wereembedded in a paraffin wax block. Although thistechnique conferred a significant advantage of simulta-neously examining multiple tissue specimens underidentical condition, the inability to satisfactorily identifyindividual tissue rods undid the cause.
In 1997, Juhan Kononen (3) at the National HumanResearch Institute, promulgated the idea of translatingthe convenience of DNA microarrays to tissues andevaluate the molecular targets in parallel. This approachthat allows simultaneous screening of large collectives oftumor specimens for any molecular alteration by relo-cating tissues from conventional histologic paraffinblocks, such that tissues from multiple patients or
Correspondence: Raghu Radhakrishnan, Department of OralPathology and Microbiology, Manipal College of Dental Sciences,Manipal – 576 104, India. Tel: +91 820 257 1201 (ext 22204), Fax:+91 820 257 1966, E-mail: [email protected] for publication June 29, 2007
J Oral Pathol Med (2008) 37: 166–176
ª 2007 The Authors. Journal compilation ª Blackwell Munksgaard 2007 Æ All rights reserved
www.blackwellmunksgaard.com/jopm
doi: 10.1111/j.1600-0714.2007.00606.x
blocks could be seen on the same slide came to bepopularly called the TMA. In contrast to DNA micro-arrays, spots in TMAs are slightly larger and contain ahistologic section from unique tissue or tumors. TMAsrepresent a significant advancement in molecular pathol-ogy over traditional methods, as they provide the abilityto rapidly identify and characterize molecular targets inhundreds or thousands of tissue samples.
This approach was primarily designed for the optimalmanagement of tissue and yet maximizes its value.Because of its miniaturization an experiment usingTMAs can be used to provide information on molecularand protein characteristics such as the incidence ofmolecular variation, cellular localization, or detectionand development of new prognostic and predictiveindicators in tumor cells. TMAs are not constrainedby application, as slides can be probed using any assayprotocol developed for whole tissue sections in a non-destructive manner, for histology, immunochemistry(IHC), and fluorescent in situ hybridization (FISH).Tissue microarrays are emerging as a breakthrough inour ability to rapidly analyze the expression of existingand new biomarkers using archival pathology specimens(5). Understanding the working principle and construc-tion of TMA and to explore the scope of TMA in headand neck cancer is of paramount importance.
Working principle and construction of tissuemicroarray
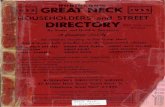
The technology of TMA involves harvesting smalldisks of tissue from individual donor paraffin-embed-ded tissue blocks and placing them in a recipient blockwith defined array coordinates. These miniaturizedcollections of tissue spots result in a dramatic increasein throughput for in situ examination of gene statusand gene expression from archival specimens. A singleTMA block may yield information on the molecularcharacterization of up to 1000 samples at a time(Fig. 1).
Most TMA studies have been undertaken usingarchival formalin-fixed paraffin-embedded (FFPE) tis-sues. Arrays are typically constructed by the removal of0.6–2 mm diameter core of tissues from the donorsamples and transferal of these to a recipient block in agrid-like fashion, thus retaining a link to the originalblock and its pathology. A morphologically representa-tive area of interest with the donor block is identifiedunder the microscope using a stained hematoxylin andeosin (H&E) section on a glass slide as a guide. Using aprecise spacing pattern, 0.6 mm cylinders allow as manyas 1000 specimens arrayed into a new recipient block ofapproximately 45 · 20 mm. Up to 200 consecutivesections can be cut from each TMA block and sectionscut from the array could be used for simultaneousdetection of DNA by FISH, RNA by mRNA ISH, orprotein by IHC. For optimal preparation areas ofappropriate morphology or antigenicity are selectedfrom the original donor blocks and cores taken fromthese areas thus ensuring inclusion of relevant andrepresentative tissue (5–7).
However, the recent preparation of frozen TMAs hasextended its application to areas where antigenicity isnot compromised through formalin fixative (8). Thepreparation of frozen analysis is similar to that ofparaffin arrays except that to avoid ice crystal artifact,all coring and preparation must be performed at subzerotemperature. Although greater preservation of antigencan be achieved using frozen sections, an inherentproblem in standard method is that morphology isinferior to that of equivalent FFPE preparation.
The construction of FFPE – TMA entails firstly, theselection of tissue and preparation of the donor block.The routine H&E-stained tissue section on a standardglass slide may be used for the selection of tissue area.The area which usually represents a specific pathologicdiagnosis is circled using a xylene-free pen and isdesignated with a unique label for case identification.The marked glass slide is overlaid on the paraffin blockto determine its corresponding region. Donor blocksplaced under a low wattage bulb will warm up slightlymaking them a little softer. In the mean time therecipient blocks are prepared using a wax softer than thestandard paraffin wax. After melting the wax at 56–59�C, the wax is poured into a deep mold and tissuecassette placed atop. After cooling the cassette isseparated from the mold. The face of the recipientblock is trimmed using a dedicated rotary microtomeprior to use. This ensures that the block is smooth andarrays that are made will be in identical plane therebyminimizing block realignment and wastage of sectionsfor the same.
Ideally, an instrument built to create holes in therecipient block and for acquiring tissue core from thedonor block is set up. The instrument consists of a thinwall stainless steel tube with an inner diameter of about0.6 mm and held in an X–Y Precision guide. A solidstainless steel wire closely fit in the tube acts as a stylet totransfer the tissue cores into the recipient block. Theprecision guide allows the needle to move only parallelto its own axis. This guide is mounted vertically on ahorizontal XY stage and moved with digital micrometersto successive locations in the growing array. Theadjustable depth stop maintains the length of therecipient holes and the transferred cores. As many as
Figure 1 Principle of tissue microarray construction.
Tissue microarray
Radhakrishnan et al.
167
J Oral Pathol Med
1000 such tissue cylinders could be placed in one45 · 20 mm recipient paraffin block.After the block construction is completed, 5 lm
sections of the resulting tumor TMA block are cut witha microtome. An adhesive-coated tape system fromInstrumedics (Hackensack, NJ, USA) is a usefulmethod for sectioning the tumor array blocks. Themicrotome cuts underneath a piece of tape that is placedover the block surface. The thin tissue sections adheredto the tape is then rolled on an adhesive-coatedmicroscopic slide to transfer the section onto the slide(Fig. 2).
Equipment set up for TMA construction
There are four sizes of punch available: 0.6, 1.0, 1.5, and2.0 mm. For majority of TMAs, the 0.6 mm is used, aslarger cores may damage the donor and recipient block.Generally, not more than 600 cores are placed into asingle TMA block. It is also important to have conve-nient spacing between cores and spaces from 0.1 mmonwards has been used successfully.Each block and slide pair should be arranged in the
order that they would be used following the map design.The base plate with recipient block is placed on thearrayer and a pair of punches is positioned. The largerone is used for extracting tissue from the donor blockand the smaller one is for making a hole in the recipientblock where the donor tissue will be positioned. Thealignment of the punches has to be ensured by making amark in the paraffin and the needles moved into theposition of the first punch with X- and Y-micrometeradjustment knobs. At this point it may be necessary toadjust the depth stop, which dictates how deep thepunch will be in the recipient block. Tightening orloosening the nut at the top left of the turret does this.The nut stops the downward movement of the turret toachieve the desired depth. A squeezing motion is used topush the tissue core into the paraffin. Rotating of thearm both ways while maintaining pressure on the turrettop helps free the core from the recipient block. Byreleasing the pressure on the turret, the springs raise toits resting position. Paraffin core is ejected and its lengthexamined by pressing down on the stylus guiding thecore into the hole while expelling the tissue from thepunch.By moving the X-axis micrometer knob to 0.8 mm the
procedure is repeated and continued till the last core inthe X-axis has been placed. After this the X-axismicrometer knob positioned to 0 and the Y-axis knobto 0.8 mm and repeated until the block is complete. Thearray block should be wiped, brushed, or dusted afterthe placement of every punch. After doing severalpunches the stylus⁄punch complex may retain someparaffin. It is removed by moving the stylus up anddown and cleaned with KimWipes. To put more than600 cores into a single TMA block, it is necessary toremove the block from the base plate and rotate theblock 180�. This is due to the limitation in travel alongthe X-axis. If the block is removed it is difficult to realignthe rows and columns.
On completion of the array block, it is removed fromthe base plate and placed in an oven at 37�C for 15 min,face down on a clean glass slide. This facilitates theadherence of the cores to the walls of the punches in therecipient block. Gently the slide from the block is
(f) A preserved tissue array organization(f) A preserved tissue array organization
(e) UV Curing and peel off the tape(e) UV Curing and peel off the tape
(d) Microtomy using a tape system(d) Microtomy using a tape system
(c) Cores bundled into array blocks(c) Cores bundled into array blocks
(a) Sample the core in pre-defined zone(a) Sample the core in pre-defined zoneDONOR BLOCKDONOR BLOCK
RECIPIENT BLOCK(b) Transfer cores into pre-made holes(b) Transfer cores into pre-made holes
RECIPIENT BLOCK
Figure 2 Construction of formalin-fixed paraffin-embedded tissuemicroarray.
Tissue microarray
Radhakrishnan et al.
168
J Oral Pathol Med
separated and any irregularity in the block is removedby applying gentle and even pressure. Subsequently, theTMA block is sited onto a block of ice and cooledcompletely. Setting the temperature of the water bath to37�C, sections of 4–5 lm are taken and positioned onthe slide in the same orientation. After complete drying,the slides are placed front to back, wrapped tightly withparafilm label and then stored at )20�C.
Image acquisition and statistical analysis
The array is usually laid out in an electronic spread sheetand all the pertinent information that identifies a sampleshould be included in the map design. Suitable controlsalong with matched normal and tumor samples arearrayed in the same row. It is preferable to havereplicate cores of each sample. Building in an orienta-tion marker with plus sign indicating where the arrayshould begin is advisable.
Numerous ‘semiquantitative’ grading systems havebeen devised by pathologists for analysis and validation.However, with the advent of computers and digitaliza-tion, quantitative analysis has become realistic. Tissuemicroarray affords a quantitative analysis when viewedunder conventional microscope using a spread sheetcorresponding to the xy-coordinates system and inter-pretations thus recorded are directly fed into a com-puter. One problem with this approach is that one mayloose the path of xy-coordinates of a given spot.
Methods to acquire and archive digital images of aTMA spot have been developed for evaluation on acomputer monitor and the image of each spot routed toits clinicopathologic details. An automated protocolprovides evidence not only of the region of interest, butof every other disk in a comparable manner. Analysisbased on algorithms and objective scoring technologyhas revealed numerous associations not previouslydiscernible by traditional two observers’ analysis. BLISSimage system (BacusTM laboratories, Lobard, IL, USA)is the one used in many laboratories used to acquiredigital image of TMA spots (Fig. 3).
Several studies have been carried out to determinethe validity of immunostained TMAs with wholesection for clinicopathologic correlation (9, 10). Froma theoretical point of view, a single TMA spot per casemay be adequate for a homogenous marker. However,four cores each from area any tumor and matchednormal controls may maximize the usefulness of TMApresuming any new biomarker may be tested in thefuture.
In a typical TMA study, every core is associatedwith data elements such as the core image and patientdemographics. Analysis of TMA data are ratherchallenging as the covariates are highly skewed,semicontinuous, and highly correlated. There arereadily available data analysis tools that uses well-established statistical techniques to interpret the resultsof TMA. Novel statistical methods also could be
AA
BB
CC
DD
1 2 3 4 5 6 7 8 1 2 3 4 5 6 7 8
Figure 3 Image acquisition and analysis for tissue microarray analysis.
Tissue microarray
Radhakrishnan et al.
169
J Oral Pathol Med
employed to extradite signals obtained (11). As clini-cians and pathologists prefer threshold tumor markerexpression, it is natural to use statistical methods thatare based on threshold covariates including regressiontrees, survival trees, and forest prediction. Whendealing with multiple markers one may use a survivaltree and detect possible interaction between them. Thetree method may be too acquisitive to detect signi-ficant interactions, which is why bump hunting is usedwith survival data.The dichotomized marker expression is often fitted in
a Cox (or alternative) regression model. This multivar-iate analytical tool is used to study the impact ofbiomarkers on the clinical outcome and thereby helpingin identifying important prognostic markers. For findingtumor markers to predicting clinical outcomes on thebasis of TMA data, hierarchical clustering is used, wherepatients are grouped into relatively homogeneous sub-groups based on a set of variables. It identifiesprognostically significant clusters of the patients basedon biomarkers⁄clinicopathologic variables. The survivalinformation of patients within each cluster is used todetermine whether the clusters formed are significantlydifferent from each other. The survival analysis helps inidentifying biomarkers that are prognostically signifi-cant and in categorizing patients into high- and low-riskgroups. Kaplan–Meier survival analysis is one such toolwhich is used for comparative analysis of survival ratesacross cohorts. Tissue microarrays coupled with statis-tical techniques such as Kaplan–Meier survival analysishelp in accurate identification of clinicopathologicparameters and important biomarkers that influencethe outcome.
Benefits, potential issues, and remedy con-cerning TMA
Tissue microarray allows high-throughput molecularprofiling of cancer by simultaneous analysis of hundredsof tissue specimens. This technology provides maximaluse of limited tissue resources and renders the advantageof generating gene expression profiles of cells as theyoccur in actual neoplastic tissues in vivo. All availablemethods for examination of histologic sections, includ-ing IHC, ISH, DNA ploidy analysis, nuclear morphom-etry, and FISH can be performed on sections fromTMA blocks. By TMA, because the cores are small,previous archival specimens could be preserved and beused for many research experiments because of hun-dreds of slides are reduced to one. Other advantages thistechnology offers include, providing uniform reactionsconditions and thereby reducing variability by includingmultiple positives and negative controls. As TMAallows one to economize the use of reagents, thisadvantage raises the possibility of TMAs in screeningprocedures, a protocol that is impossible using conven-tional sections.As TMA allows entire cohort to be analyzed in one
batch on a single slide, the reagent concentrations areidentical for each case as are incubation times, temper-ature, wash conditions, and antigen retrieval. Labor-
intensive microtome sectioning of numerous blocks canbe cut down by TMA. Finally, on occasion when theblock has to returned to the patient or donatinginstitution, block may be cored without destroying andused for array-based studies without causing anyhindrance for diagnosis.
The tissue array technology facilitates procurement,distribution, and application of human tumor tissues forresearch purposes. Automation of the procedure forsampling and arraying would allow creation of dozensof replicas of tumor arrays, each providing up to 200sections for molecular analysis. In principle, entirearchives of tens of thousands of existing formalin-fixedtissues from pathology laboratories could be placed in afew high-density TMAs to survey a variety of tumortypes as well as different stages of tumor progression.
Although TMA holds promise, the major limitationof this technique is the tissue volume. The punches of0.6 mm diameter from tumor are perceived as too smalland potentially not representative of the entire area.This may be especially true of tumors which may behighly heterogeneous. To guarantee the high quality andrepresentivity of distinct tumor arrays, the introductionof a new array designed to investigate perhaps new sofar unknown factors in carcinogenesis, should include atleast some experiments, reproducing data described inthe literature, as was carried out in the originaldescription of TMA (3). However, it must be notedthat there is an essential difference with respect to theapplications of TMAs and their low-density counter-parts. While large tissue sections are used for thepurpose of clinical diagnosis, the strength of TMA liesnot in its usage for diagnostics, but as a research toolwith the ability to provide statistically significant,population level data faster and more economicallythan other methodologies (Table 1).
Other alternatives to circumvent these problems havebeen proposed, such as the use of larger punch needles ofup to 2 mm in diameter. Large punch arrays may bepreferable for distinct area of cancer researchwhen tissuesrequire simultaneous investigation of various regions inan organ as in liver. Thus, punches of 2 m diameter fromliver tissue are sufficient to define the staining pattern in allthe relevant anatomical region. Larger needles may alsobe advisable for the investigation of small benign ormalignant tumor in a complex tissue.
Nevertheless, the use of larger punch needles may notoffer any significant advantage as this increase is hardlymore representative than 0.6 mm in diameter. On thecontrary, instead of several hundreds of tumor on a
Table 1 Benefits and issues concerning tissue microarray
Advantages Disadvantages
Preserve precious archives Tissue volume too lessExperimental uniformity Tissues may not be representativeUseful screening procedure Defective coringImproves statistical significance Observational slip-upSignificant reduction in labor Not suitable for diagnosticsConsumables are economized Setting up array time-consuming
Tissue microarray
Radhakrishnan et al.
170
J Oral Pathol Med
single slide, far fewer than 100 samples could only beinvestigated. In addition, these large punches may alsocause considerable damage to the donor and acceptorblock. Differences in original tissue thickness or inaccu-rate core sampling and placement may lead to some ofthe tissue cores being of different length and upontransfer may result in the absence of tissue material. Toovercome this problem, the tissue arrayers should beaccurately placed to the same depth when taking eachcore of tissue and as far as possible the original tissueblock should be of the same depth. An additional checkis to ensure that when sectioning the microarray, every25th slide is retained for an H&E section to check all thecores are present at the same depth.
As thousands of tissue cores are arrayed on a singlemicroscopic slide, there could be observational slip-upwhile viewing TMA. To outweigh these problems,marker tissue cores of distinctive type could be placedamong test cores in a pattern that allows easy identifi-cation. However, some special problems related to TMAare overcome using automated reader and using dedi-cated software.
Finally, making tissue arrays is time-consuming andshould be regarded as a project in itself. Preparatory stepsthat include marking of the representative tissue area israther more complex than the array construction. Assetting up an array construction takes considerableamount of time making multiple replicates of arrayconstructs may seem more practical. Currently, there areat least three ways to get TMAs for research. It could bemade using commercially available manual and auto-mated arrayers or one canorder custommicroarrays fromacademic institutions or buy pre-made arrays includingarrays of mouse tissues, human tissue representingvarious disease states, and normal tissue controls.
Other expected problems related to TMA pertain topossible alterations in antigenicity or nucleic acid struc-ture following fixation and paraffin embedding. As aresult a frozen tumor TMA has been described wherecores are taken from optimum cutting temperature(OCT)-embedded tissue samples and are arrayed into arecipientOCTblock. Although frozen TMAsmaywell beexcellent in preserving antigenicity, distortion of tissuemorphology may be evident. Also, it has been noted thatfewer samples can be embedded in the array media.Additionally, coring needles can sometimes break due tothe low temperature required to keep the array frozen (8).
Preserving the arrays after tissue sectioning is onefinal issue as problems related to antigenic loss maypresumably occur because of oxidation when largebatches of microarray sections are produced. Use ofZenkers’ formalin may help overcome instead of usingneutral-buffered formalin as it is known to causeoxidation of sections. Loss of antigenicity may beobserved if sections are stored for about a week priorto immunostaining. This loss to some extent can beprevented by sectioning without water using tapetransfer system. Removal of degreasing agent after taperelease by short incubation in xylene and finally reco-ating the slides within paraffin prior to staining in anitrogen safe cabinet may improve the shelf life.
Applications of TMA
Although the TMA technique was initially described forcharacterization of biomarkers in cancer research as theconventional methods were far too elaborate, theutilization of this technique is promptly expanding(Fig. 4). Simultaneous assessment of molecular markersof clinical relevance in hundreds of tissue specimens hassignificantly made many advances in cancer research.Theoretically, anything that one can do with regulartissue section could be extrapolated using TMA. Thehigh-throughput approach for analysis of intact tissuesallows validation of relative frequencies of moleculartargets by IHC, FISH, mRNA, and ISH. The validity ofTMA analysis has been shown to correspond well forwhole-section analysis as seen in breast (9), prostate(12), and brain (13). TMA analysis facilitates analysisand validation of novel targets obtained from genomicsurveys by cDNA microarrays. This is best illustrated ina study by Barlund et al. (14), who found overexpressionof ribosomal s6 kinase in a breast cancer cell line bycDNA microarrays and then showed, using TMAs, how9–15% of breast cancers amplify this gene, may be aprognostic significance in breast cancer.
Nocito et al. (15) have proposed three useful designsfor TMA construction to enable their use in research.The ‘multitumor tissue microarrays’ are constructedfrom different tumors from different sites in the bodythat may allow comparison of molecular markers acrossthe spectrum of neoplastic disease. Samples frompotentially heterogeneous tumors could provide mean-ingful information about distribution and frequency ofgene amplification in different tumor types. Tissuemicroarray technology with the potential to greatlyfacilitate analysis of alterations in multiple tumor typesallowed rapid screening for molecular alteration in asmany as 17 different tumors in a single paraffin blockarraying 397 individual tumors (16). Gene amplificationof CCND at 11q13, ERBB2 at 17q21, and CMYC at8q24, which are overexpressed in neoplastic states whenanalyzed by FISH experiments from sections cut withTMA block revealed increased expression in breast,lung, head and neck, bladder cancer, and melanoma aswell. These results from arrays were comparable toexisting data, suggesting that multitumor arrays are a
Figure 4 Scope and applications of tissue microarray.
Tissue microarray
Radhakrishnan et al.
171
J Oral Pathol Med
powerful tool to rapidly screen different tumor types.The rapid screening of multiple genes and multipletumor types by TMA approach leads to an unbiasedanalysis of gene amplifications in various cancer types.The ‘tumor progression arrays’ include a range of
tissue from normal to pre-malignant to malignant.Molecular alterations with specific stage of tumorprogression could be identified by this construct aswas observed in case of prostate cancer progressionwhere amplification of Androgen Receptor (AR) gene(17), overexpression of IGFBP2 (18; insulin-like growthfactor binding protein 1) were found to be very commonin hormone refractory end-stage prostate cancer butinfrequent in untreated primary tumors. A broad surveyusing high-density TMA technology in a prostate tumorTMA construct showed a transient downregulation of Ecadherin expression in localized prostate cancer and astrong expression in metastatic cancer (19).The ‘patient outcome tissue microarrays’ are con-
structed from patient samples for whom follow-up dataare available such as survival rate, metastatic spread,treatment response, etc. Any change in protein expres-sion identified from these array constructs.Even though immunohistochemistry (IHC) is an
established and widely used technique, quality controlis one of the major issue in IHC. This is mainly becauseof the variation in antigen retrieval, staining protocols,and the interpretations of the results used. The use ofTMAs offers an alternative method of quality control
for research purposes. The potential for TMAs inquality assessment for routine IHC has been demon-strated in a few laboratories (20–22).
In addition to intact tissues, cell culture materials andcell lines may be used (23). Frozen TMAs have beendeveloped by at least two groups (8, 24) and a variationof TMA using primary cultures have been used byincorporating cell cultures into a recipient block. Celllines may be preserved in this way after isolating them,fixing them in formalin, embedding in agarose, and thensubmitting them for routine processing into paraffin.The advantage of using cell lines in solid support is thatthey could be used as excellent controls especially whenworking up a new antibody (25).
Tissue microarray analysis in head and necksquamous cell carcinomas
The squamous cell carcinomas of head and neck(HNSCC) are heterogeneous in terms of its distributionwith each of these subentities having varied biologic andclinical characteristics. As majority of these lesionsoccur because of stepwise accumulation of geneticdefects, determination of various factors resulting intumorigenesis becomes important for understanding thedisease process and advocating suitable therapeuticinterventions. TMA by its high-throughput technologyhas demonstrated its power in revealing cellular alter-ations in large series of specimens in HNSCC, thereby
Table 2 List of molecular markers studied by tissue microarray analysis in head and neck cancer research
Tissue type Size Molecular markers Method End point References
HNSCCs 609 CCND1, EGFR, MYC,ZNF, and ERBB
FISH Prevalence of amplification Freier et al. 2003 (26)
Primary head andneck squamous cellcarcinoma (HNSCC)
547 Cyclin D1, c-myc,erbb1, and erbb2
IHC Prevalence of amplificationand variable expression withclincopathologic data
Freier et al. 2003 (27)
Carcinoma oral cavity,lungs, esophagusPrecursor lesions
11834
Furin IHC Frequency, tumor progression,multitumor analysis, andcomparison with whole section
Lopez de Cicco et al. 2002 (28)
Oral or oropharynxsquamous cellcarcinoma
102 CD68 to identify tissuemacrophages
IHC Correlation with clinicopathologicdata and survival
Marcus et al. 2004 (29)
Oropharyngealsquamous cellcarcinoma
123 p16 IHC Independent prognostic factor forlocal recurrence, disease-freesurvival, and overall survival
Weinberger et al. 2004 (30)
HNSCC 280 CCNL1, SNO,PIK3CA, TP73L
FISH Prevalence of copy number gains Sticht et al. 2005 (33)
Primary OSCC 178 FGFR1 FISH, IHC Prevalence of expression andamplification
Freier et al. 2007 (34)
Oral carcinomas 85 Catenins IHC Prognostic marker Fillies et al. 2005 (35)Oral cancer 308 Ck 5⁄6, Ck 8⁄18, Ck 1,
CK 10, Ck 14, Ck 19,and vimentin
IHC Correlations between clinicalfeatures and the expressionof intermediary filaments
Fillies et al. 2006 (36)
OSCC 109 EGFR1 IHC Prognostic marker Laimer et al. 2007 (37)HNSCC 113 Rho C GTPase IHC Prognostic marker Kleer et al. 2006 (38)OSCC 79 Akt In situ Prognostic marker Yu et al. 2007 (39)HNSCC 81 NBS1 IHC Prognostic marker Yang et al. 2007 (40)HNSCC 664 P16INK4A
p53IHC Tumor Progression and
prevalence of expressionKarsai et al. 2007 (41)
OSCC 296 SurvivinBIRC5
FISH, IHC Prevalence of copy number gains,tumor progression, andmultitumor analysis
Freier et al. 2007 (42)
HNSCC, squamous cell carcinomas of head and neck; OSCC, oral squamous cell carcinoma.
Tissue microarray
Radhakrishnan et al.
172
J Oral Pathol Med
determining its clinical outcome and prognostic poten-tial (Table 2).
To determine the role of oncogene amplification,Freir et al. (26) generated a tissue array of clinically well-defined HNSCC. Fluorescence in situ hybridization wasapplied on a collection of 609 SCCs of the head andneck (HNSCCs), including 511 primary carcinomas ofdifferent clinical stages and anatomical localization and98 recurrent carcinomas, second primary carcinomas,and regional metastases on a TMA. The overall pre-valence of amplifications of five oncogenes CCND 1,EGFR, MYC, ZNF217, and ERBB2 were analyzed.Significantly, CCND1 amplifications were associatedwith the pharyngeal site in primary carcinomas, whereasamplifications of ZNF217 were less frequent in pharyn-geal carcinomas when compared with primary oral andlaryngeal carcinomas. The amplification pattern of theseoncogenes suggested that different molecular pathwayswere involved in HNSCCs of different localizations.
Similarly, a TMA containing 547 primary HNSCCwas used for the analysis of cyclin D1, c-myc, erbb1, anderbb2 expression by IHC (27). Cyclin D1 and c-mycwere overexpressed at higher frequencies in primarypharyngeal and laryngeal carcinomas compared withprimary oral carcinomas, while erbb1 and erbb2 over-expression was associated with oral site. Furthermore,cyclin D1 overexpression correlated with stage IVprimary carcinoma suggesting that HNSCC as a heter-ogeneous group of tumors, depending on anatomic sitesand clinical stage, showed variable expressions of theoncoproteins described.
Furin, a proprotein convertase that activates manycancer development-related substrates such as growthfactors, growth factor receptors, adhesion molecules,and matrix-degrading enzyme was studied in sectionsfrom TMA in a collection of SCCs (28). Furin expres-sion was notably higher in most precursor lesions thanin normal epithelia. High levels of furin expression wereobserved approximately in 50% SCCs of three differentsites as well as in precursor lesions of the oral andbronchial mucosa. The normal epithelia showed lowlevels of expression and basal cells were always negative.These results show that furin was upregulated in SCCsfrom three different organs and its use as a tumormarker in both invasive and pre-invasive neoplasia wasvalidated.
To test the hypothesis if tumor-associated macro-phages contribute to HNSCC aggressiveness, mRNAexpression analysis, and a large cohort of clinicalspecimens were used (29). Oligonucleotide microarrayanalysis was performed on a prospective cohort of20 patients with previously untreated oral cavity ororopharynx SCC and on normal oropharyngeal mucosafrom four patients. A high-density TMA of 102 patientswith previously untreated oral cavity or oropharynxSCC was stained immunohistochemically for CD68to identify tissue macrophages, and the results werecorrelated with clinicopathologic data and survival.Monocyte chemoattractant protein 1 was upregulatedsignificantly in tumors compared with normal mucosa.Tissue microarray data revealed that macrophage con-
tent of the primary tumor was associated strongly withlymph node metastasis, extracapsular lymph nodespread, and advanced clinical disease stage. When itwas evaluated along with other clinicopathologic data,the macrophage content was found to be an independentpredictor of lymph node metastasis thus proving theirhypothesis that primary tumor macrophage content is astrong predictor of tumor aggressiveness in HNSCC.
Functional inactivation of p16 as an early andfrequent event in head and neck squamous cell cancerswas determined by IHC in a TMA (30). p16 over-expression was associated with more advanced Tumor-Node-Metastasis stage with decreased 5-year localrecurrence rates and increased 5-year disease-free sur-vival. In patients with oropharyngeal SCC, it wasconcluded that overexpression of p16 was associatedwith significantly improved prognosis and lower localrecurrence rates.
Large-scale expression analysis of Smads in HNSCCby IHC on TMA showed loss of TGF-b⁄Smad signalingapproximately in 15–20% of cases suggesting thatdisruption in TGG-b signaling and alteration in Smadwere associated with greater tendency for metastaticspread and regional recurrences (31).
Protein expression studies for evaluation of variouscyclin-dependent kinases using TMA has significantlycontributed to understanding the cell cycle alterations inthe development of HNSCC and thereby predictingprognosis and response to chemotherapy. Cyclin A hasbeen identified as an independent marker of tumorprogression and their absence in tissues correlated withpoor treatment response to chemotherapy (32).
Overrepresentation of chromosomal bands 3q25–q29has been associated with shortened disease-specificsurvival in head and neck squamous cell carcinoma(HNSCC). To assess the prevalence of copy numbergains (>4 signals per cell) and high-level amplifications(>8 signals per cell) from putative oncogenes in thechromosomal region for CCNL1, SNO, PIK3CA,TP73L, and TMA analysis was applied on 280 HNSCCsby FISH (33). In general, gains were more frequentlydetected in stage IV compared to stages I–III tumors. Asignificant association of CCNL1 gains and the presenceof lymph node metastases was found, which wasindependent of anatomical site and T-stage of theprimary tumor. Site-specific subgroup analysis furthershowed that copy number gains of CCNL1 and SNOoccurred more frequently in oral carcinomas inadvanced clinical stages when compared to N0 orallesions. Kaplan–Meier survival analysis also revealedthat high-level amplifications of CCNL1 correlated withshorter overall survival of the patients. Their resultsindicated that CCNL1 played a critical role in the loco-regional progression of HNSCC thus serving as anindicator for occult advanced tumor stages.
Detailed FISH analysis on OSCC TMA sectionsrevealed amplification prevalence for FGFR1 of 17.4%.Furthermore, FGFR1 protein analysis by IHC on aTMA containing 178 OSCC found a high FGFR1expression in tumors of early t-stadium and UICC stage.Their results indicated that an increase in FGFR1
Tissue microarray
Radhakrishnan et al.
173
J Oral Pathol Med
expression contributes to oral carcinogenesis at an earlystage of development (34).Catenin expression in oral carcinomas was evaluated
in relation to clinicopathologic features to determine itsvalue as a prognostic marker as reduction of theexpression of catenin is a crucial step in the pathogen-esis, progression, and prognosis of many epithelialcancers. A TMA consisting of multiple representativetissue cores of histologically proven T1⁄2 SCC of theoral floor that underwent surgical treatment wereincluded in the study group. The expression levels ofalpha-, beta-, and gamma-catenins were determinedimmunohistologically. Loss of alpha-catenin expressionin carcinoma of the floor of the mouth correlatedsignificantly with poor prognosis. Conversely, signifi-cantly reduced rates of lymph node metastases wereobserved in alpha- and beta-catenin-positive T1 and T2SCCs. Loss of gamma-catenin expression indicated areduced survival rate in nodal-negative tumors. Cateninexpression in carcinomas of the floor of the mouthseemed to be a predictive parameter in the prognosis ofT1 and T2 SSCs (35).Immunohistochemical expression of a variety of
intermediary filaments including high- and low-mole-cular weight cytokeratins (Cks), such as Ck 5⁄6, Ck 8⁄18,Ck 1, CK 10, Ck 14, Ck 19, and vimentin, using theTMA technique were studied in histologically provenand surgically treated SCCs of oral cavity. The expres-sion of Ck 8⁄18 and Ck 19 were overall significantlycorrelated with a poor clinical prognosis and thesefindings could also be reproduced for Ck 8⁄18 in primarynodal-negative SCCs and held true in multivariateanalysis. The expression of Ck 8⁄18 in SCCs of the oralcavity served as an independent prognostic marker andindicates a decreased overall and progression-free sur-vival. These results reaffirmed the fact that intermediaryfilaments are involved in cell motility and cancerprogression (36).A retrospective study by Laimer et al. (37), designed
TMA to investigate the prognostic significance ofEGFR overexpression in human oral SCC on a long-term follow up from 109 patients who underwentsurgical treatment. High EGFR expression was foundin 73.42% of the tumor samples. Kaplan–Meier curvesshowed that EGFR overexpression was significantlyrelated to decreased overall survival and these resultsconfirmed that EGFR overexpression as an independentprognostic marker in patients with SCC of the oralcavity and oropharynx.Kleer et al. (38) evaluated the expression of RhoC in
head and neck carcinoma and investigated the prognosticuse of this marker on a large cohort of previouslyuntreated patients withHNSCC.The in vivo expression ofRhoC in metastatic and non-metastatic SCCHN wasinvestigated using immunohistochemical analysis on aTMA composed of 113 independent tumor samples. Thein vivo expression of RhoC correlated with advancedclinical stage and lymph node metastases for the entirepatient cohort as well as in small primary tumors T (1)and T (2). It was concluded from this observation thatRhoC is a specific marker of lymph node metastases and
seems to identify a subset of patients with early tumorstage, primary tumors, and high metastatic potential thatmight benefit from more aggressive therapy. Throughcontinued investigation, blockade of RhoC activity maybe a potential target in the development of novelstrategies for treatingmetastases of head and neck cancer.
Recently, the protein expression levels of phosphor-ylated Akt (p-Akt) and PTEN examined in oropha-ryngeal squamous cell carcinoma (OSCC) cohort ofpatients on a TMA showed an inverse relationshipbetween the two. Akt activation in OSCC was associ-ated with adverse patient outcome and loss of phos-phatase PTEN was one of the proposed mechanisms ofAkt activation (39). In addition to this NBS1 over-expression identified in 45% of advanced HNSCCpatients was identified as an independent marker ofpoor prognosis and the underlying mechanism wasassumed to be due to the activation of the PI3 K⁄Aktpathway (40).
In one of the largest cohorts studied, IHC wasperformed on TMA of 664 tumors to study the loss ofp16INK4A protein expression and p53 alteration (41).Both loss of p16(INK4a) expression and p53 alterationsdiffered significantly across both tumor sites and stages,being more prevalent in the hypopharynx than in theother tumor sites and in advanced tumor stages. Anincreased DNA methyltransferase 1 protein levelsoccurred preferentially in tumors with aberrant p53and negative p16INK4A expression. These changes wererelated and perceived to be important particularly inearly carcinogenesis of HNSCC.
Tumor TMA analysis was performed applying FISHand IHC to 296 OSCC specimens to check whethersurviving and BIRC5, which is a surviving encodingprotein could serve as a progressive marker (42).Increased gene copy numbers of BIRC5 correlated withhigh UICC stage and presence of lymph node metasta-sis, but not with unfavorable patient outcome. Similarly,high surviving expression was found to predict 5- to 10-year survival of patients in a multivariate model. Thiswas also found to be true in patients who receivedradiation therapy, where high survivin expression wasfound to be the only predictor of favorable survival in amultivariate Cox regressive analysis. These findings mayprove to be important in identifying OSCC patients,who would benefit from radiotherapy.
Our group carried out a study to analyze theimmunohistochemical expression of bcl2 in OSCC.FFPE tissue blocks of OSCC and their correspondingH&E slides retrieved from the departmental archiveswere used for this study. The tissue array blocks wereconstructed manually (Beechers Instruments, Inc., SunPrairie, WI, USA) with cores of 1.5 mm with a spacingof 2.5 mm apart. Two core biopsies from each donorblock were taken and assembled on the recipient block.Apart from the tumor tissue, two cores from a normaltonsil as control were included in the tissue array.Following the construction of TMA blocks, two 5 lmthin sections were obtained from the block and immu-nostained with bcl2 monoclonal antibodies. Our resultsrevealed positivity in 62.5% of cases. The percentage of
Tissue microarray
Radhakrishnan et al.
174
J Oral Pathol Med
positive cells determined using the automated imagesystem chroma vision workstation ranging from 11% to86%. Overexpression of bcl2 reflected suppression ofprogrammed cell death and extension of tumor cell lifespan. A combined approach of IHC and TMA revealedcellular alterations in OSCC which is of diagnostic andprognostic importance. Further studies using multiplemarkers will be undertaken and this technique shall beused to screen pre-malignant oral lesions using tumorprogression TMA models.
The future perspectives of tissue microarraysand conclusion
To fully exploit TMAs and to maximize the chances of asuccessful study outcome, proper consideration must begiven to the array source. Some researchers constructtheir own slides, which require a high level of technicalexpertise and resources. It is of note that somecommercial organizations are now offering TMAs froma range of normal and malignant human tissues in theirproduct range. TMA helps in preservation of precioustissue, save storage space and explore any new molec-ular markers as and when they are discovered. With thedevelopment of patient database and their relevantindicator marker information using arrays, it may befeasible to plan appropriate treatment modality. Anarray of arrays in miniature form may change the waythe research is conducted in future and laboratory on ablock is not too far away.
Tissue microarray technology has the potential tosignificantly accelerate molecular studies and hasbecome one of the most promising tools in head andneck cancer research. Presently, TMAs are mostcommonly used for cancer studies and for basicresearch and it is only a matter of time before TMAsfind their role for educational purposes. As TMAsreduce tedious, labor-intensive pathologic exercise toone test and on a single slide, arrays’ inherent multi-plexing can cut 2500 slides down to five. As costsassociated with bringing new therapeutic agents in-crease and focus of rational drug design and develop-ment come to the fore, TMAs may well become astandard investigational tool.
References
1. DeRisi J, Penland L, Brown PO, et al. Use of cDNAmicroarray to analyse gene expression patterns in humancancer. Nat Genet 1996; 14: 457–60.
2. Velculescu VE, Zhang L, Vogelstein B, Kinzler KW. Serialanalysis of gene expression. Science 1995; 270: 484–7.
3. Kononen J, Bubendorf L, Kallioniemi A, et al. Tissuemicroarrays for high throughput molecular profiling oftumor specimens. Nat Med 1998; 4: 844–7.
4. Battifora H. The multitumor (sausage) tissue block: Novelmethod for immunohistochemical antibody testing. LabInvest 1986; 55: 244–8.
5. Kallioniemi OP, Wagner U, Kononen J, Sauter G. Tissuemicroarray technology for high-throughput molecularprofiling of cancer. Hum Mol Genet 2001; 10: 657–62.
6. Packeisen J, Korsching E, Herbst H, Boecker W, BuergerH. Demystified… tissue micrarray technology. Mol Pathol2003; 56: 198–204.
7. Simon R, Nocito A, Hubscher T, et al. Patterns of her)2⁄neu amplification and overexpression in primary andmetastatic breast cancer. J Natl Cancer Inst 2001; 93:1141–6.
8. Schoenberg Fejzo M, Slamon DJ. Frozen tumor tissuemicroarray technology for analysis of tumor RNA, DNAand Protiens. Am J Pathol 2001; 159: 645–50.
9. Camp RL, Charette LA, Rimm DL. Validation of tissuemicroarray technology in breast carcinoma. Lab Invest2000; 80: 1943–9.
10. Rubin MA, Dunn R, Strawderman M, Pienta KJ. Tissuemicroarray sampling strategy for prostate cancer biomar-ker analysis. Am J Surg Pathol 2002; 2: 312–9.
11. Liu X, Minin V, Huang Y, Seligson DB, Horvath S.Statistical methods for analyzing tissue microarray data.J Biopharm Stat 2004; 14: 671–85.
12. Mucci NR, Akdas G, Manley S, Rubin MA. Neuroen-docrine expression in metastatic prostate cancer: evalua-tion of high throughput tissue microarrays to detectheterogeneous protein expression. Hum Pathol 2000; 31:406–14.
13. Sallinen SL, Sallinen PK, Haapasalo HK, et al. Identifi-cation of differentially expressed genes in human gliomasby DNA microarray and tissue chip techniques. CancerRes 2000; 60: 6617–22.
14. Barlund M, Forozan F, Kononen J, et al. Detectingactivation of ribosomal protein s6 kinase by complemen-tary DNA and tissue microarray analysis. J Natl CancerInst 2000; 92: 1252–9.
15. Nocito A, Kononen J, Kallioniemi OP, Sauter G. Tissuemicroarrays for high-throughput molecular pathologyresearch. Int J Cancer 2001; 94: 1–5.
16. Schraml P, Kononen J, Bubendorf L, et al. Tissuemicroarrays for gene amplification surveys in manydifferent tumor types. Clin Cancer Res 1999; 5: 1966–75.
17. Bubendorf L, Kononen J, Koivisto P, et al. Survey of geneamplifications during prostate cancer progression by highthroughput fluorescence in situ hybridization on tissuemicroarrays. Cancer Res 1999; 59: 803–6.
18. Bubendorf L, Kolmer M, Kononen J, et al. Hormonetherapy failure in human prostate cancer: analysis bycomplementary DNA and tissue microarrays. J NatlCancer Inst 1999; 91: 1758–64.
19. Rubin MA, Mucci NR, Figurski J, Fecko A, Pienta KJ,Day ML. E cadherin expression in postate cancer: a broadsurvey using high density tissue microarray technology.Hum Pathol 2001; 32: 690–7.
20. Parker RL, Huntsman DG, Lesack DW, et al. Assess-ment of inter laboratory variation in the immunohisto-chemical determination of estrogen receptor status usinga breast cancer tissue microarray. Am J Clin Pathol 2002;117: 723.
21. Hsu FD, Nielsen TO, Alkushi A, et al. Tissue microarraysare an effective quality assurance tool for diagnosticimmunohistochemisty. Mod Pathol 2002; 15: 1374–80.
22. Mengel M, Von Wasielewski R, Wiese B, et al. Interlaboratory and inter observer reproducibility of immuno-histochemical assessment of the Ki – 67 labelling index in alarge multi centre trial. J Pathol 2002; 198: 613–5.
23. Hoos A, Cordon-Cardo C. Tissue microarray profiling ofcancer specimens and cell lines: opportunities and limita-tions. Lab Invest 2001; 81: 1331–8.
Tissue microarray
Radhakrishnan et al.
175
J Oral Pathol Med
24. Struckmann K, Schraml P, Simon R, et al. Impairedexpression of the cell cycle regulator BTG2 is common inclear cell renal cell carcinoma.Cancer Res 2004; 64: 1632–8.
25. Moskaluk CA, Stoler MH. Agarose mold embedding ofcultured cells from tissue microarays. Diagn Mol Pathol2002; 11: 234–8.
26. Freier K, Joos S, Flechtenmacher C, et al. Tissuemicroarray analysis reveals site-specific prevalence ofoncogene amplifications in head and neck squamous cellcarcinoma. Cancer Res 2003; 63: 1179–82.
27. Freier K, Bosch FX, Flechtenmacher C, et al. Distinct site-specific oncoprotein overexpression in head and necksquamous cell carcinoma: a tissue microarray analysis.Anticancer Res 2003; 23: 3971–7.
28. Lopez de Cicco R, Bassi DE, Page R, Klein-Szanto AJ.Furin expression in squamous cell carcinomas of the oralcavity and other sites evaluated by tissue microarraytechnology. Acta Odontol Latinoam 2002; 15: 29–37.
29. Marcus B, Arenberg D, Lee J, et al. Prognostic factors inoral cavity and oropharyngeal squamous cell carcinoma.Cancer 2004; 101: 2–779.
30. Weinberger PM, Yu Z, Haffty BG, et al. Prognosticsignificance of p16 protein levels in oropharyngeal squa-mous cell cancer. Clin Cancer Res 2004; 10: 5684–91.
31. Xie W, Bharathy S, Kim D, Haffty BG, Rimm DL, ReissM. Frequent alterations of Smad signaling in human headand neck squamous cell carcinomas: a tissue microarrayanalysis. Oncol Res 2003; 14: 61–73.
32. Rodriguez-Pinilla M, Rodriguez-Peralto JL, Hitt R, et al.Cyclin A as a predictive factor for chemotherapy responsein advanced head and neck cancer. Clin Cancer Res 2004;10: 8486–92.
33. Sticht C, Hofele C, Flechtenmacher C, et al. Amplificationof Cyclin L1 is associated with lymph node metastases inhead and neck squamous cell carcinoma (HNSCC). Br JCancer 2005; 92: 770–4.
34. Freier K, Schwaenen C, Sticht C, et al. Recurrent FGFR1amplification and high FGFR1 protein expression in oralsquamous cell carcinoma (OSCC). Oral Oncol 2007; 43:60–6.
35. Fillies T, Buerger H, Gaertner C, et al. Catenin expressionin T1⁄2 carcinomas of the floor of the mouth. Int J OralMaxillofac Surg 2005; 34: 907–11.
36. Fillies T, Werkmeister R, Packeisen J, et al. Cytokeratin8⁄18 expression indicates a poor prognosis in squamouscell carcinomas of the oral cavity. BMC Cancer 2006; 13:6–10 (PMID: 16412231; doi: 10.1186/1471-2407-6-10).
37. Laimer K, Spizzo G, Gastl G, et al. High EGFRexpression predicts poor prognosis in patients with squa-mous cell carcinoma of the oral cavity and oropharynx: aTMA-based immunohistochemical analysis. Oral Oncol2007; 43: 193–8.
38. Kleer CG, Teknos TN, Islam M, et al. RhoC GTPaseexpression as a potential marker of lymph node metastasisin squamous cell carcinomas of the head and neck. ClinCancer Res 2006; 12: 4485–90.
39. Yu Z, Weinberger PM, Sasaki C, et al. Phosphorylation ofAkt (Ser473) predicts poor clinical outcome in oropha-ryngeal squamous cell cancer. Cancer Epidemiol Biomar-kers Prev 2007; 16: 553–8.
40. Yang MH, Chiang WC, Chou TY, et al. Increased NBS1expression is a marker of aggressive head and neck cancerand overexpression of NBS1 contributes to transforma-tion. Clin Cancer Res 2006; 12: 507–15.
41. Karsai S, Abel U, Roesch-Ely M, et al. Comparison ofp16(INK4a) expression with p53 alterations in head andneck cancer by tissue microarray analysis. J Pathol 2007;21: 314–22.
42. Freier K, Pungs S, Sticht C, et al. High survivin expressionis associated with favorable outcome in advanced primaryoral squamous cell carcinoma after radiation therapy. IntJ Cancer 2007; 120: 942–6.
Acknowledgments
The authors acknowledge the financial support offered by the International
Union Against Cancer. Dr Monica Charlotte Solomon was awarded a
UICC ICRETT fellowship (ICR⁄05⁄23) for the project ‘Immunohistochem-
ical analysis of tumor markers during the development and progression of
head and neck cancers using tissue microarrays: a systematic approach’,
which was carried out at the Department of Pathology, University of
Chicago, IL, USA, August–September 2005
Tissue microarray
Radhakrishnan et al.
176
J Oral Pathol Med