Role of the translocation partner in protection against AID-dependent chromosomal translocations
Transcript of Role of the translocation partner in protection against AID-dependent chromosomal translocations
Role of the translocation partner in protection againstAID-dependent chromosomal translocationsMila Jankovica, Davide F. Robbiania, Yair Dorsetta, Thomas Eisenreicha,b, Yang Xuc, Alexander Tarakhovskyd,Andre Nussenzweige, and Michel C. Nussenzweiga,b,1
aLaboratory of Molecular Immunology and bHoward Hughes Medical Institute, The Rockefeller University, New York, NY 10065; cDivision of BiologicalSciences, University of California, San Diego, CA 92093; dLaboratory of Lymphocyte Signaling, The Rockefeller University, New York, NY 10065; andeExperimental Immunology Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD 20892
Edited by Jeffrey Ravetch, The Rockefeller University, New York, NY, and approved November 5, 2009 (received for review August 7, 2009)
Chromosome translocations between Ig (Ig) and non-Ig genes arefrequently associated with B-cell lymphomas in humans and mice.The best characterized of these is c-myc/IgH translocation, which isassociated with Burkitt’s lymphoma. These translocations arecaused by activation-induced cytidine deaminase (AID), which pro-duces double-strand DNA breaks in both genes. c-myc/IgH translo-cations are rare events, in part because ATM, p53, and p19 activelysuppress them. To further define the mechanism of protectionagainst the accumulation of cells that bear c-myc/IgH translocation,we assayed B cells from mice that carry mutations in cell-cycle andapoptosis regulator proteins that act downstream of p53. We findthatPUMA,Bim, andPKCδare required forprotectionagainst c-myc/IgH translocation, whereas Bcl-XL and BAFF enhance c-myc/IgHtranslocation. Whether these effects are general or specific to c-myc/IgH translocation and whether AID produces dsDNA breaks ingenes other than c-myc and Ig is not known. To examine thesequestions, we developed an assay for translocation between IgHand Igβ, both of which are somatically mutated by AID. Igβ/IgH, likec-myc/IgH translocations, areAID-dependent, andAID is responsiblefor lesions on IgH and the non-IgH translocationpartners. However,ATM, p53, and p19 do not protect against Igβ/IgH translocations.Instead, B cells are protected against Igβ/IgH translocations by aBAFF- and PKCδ-dependent pathway. We conclude that AID-induceddouble-strandbreaks in non-Iggenesother than c-myc leadto their translocation, and that at least two nonoverlapping path-ways protect against translocations in primary B cells.
B lymphocyte | c-myc | cancer | immunoglobulin
Mature B-cell lymphomas are frequently associated withchromosomal translocations between Ig loci and non-Ig
genes. The latter include c-myc in Burkitt’s lymphoma, bcl-2 infollicular lymphoma, bcl-6 in diffuse large-cell lymphoma, andFGFR in multiple myeloma (1–3). These translocations are be-lieved to be important for malignant transformation becausethey can deregulate the transcription of oncogenes by placingthem under the control of the Ig transcriptional elements.Translocations are thought to be particularly prevalent in B-cell
lymphomas because B cells undergo a series of DNA remodelingreactions that involve obligate double-strand breaks (DSBs) in Igloci. V(D)J recombination is the first of these reactions, and ismediated by the RAG1/2 endonuclease (4, 5). This enzyme pro-duces paired hairpin and blunt DNA ends when it cuts recombi-nation signal sequences during antigen receptor gene assembly indeveloping B-cell precursors (6, 7). Class switch recombination(CSR) and somatic hypermutation (SHM) remodel Ig genes inmature B cells activated during immune responses. CSR is a DNArecombination reaction that alters the effector function of theantibody by replacing one constant region with another withoutaltering the antigen-binding variable region. In contrast to V(D)Jrecombination, CSR is not sequence-specific but instead region-specific, resulting in recombination between repetitive DNA ele-ments found 5′ of Ig constant region genes (8). SHM changes theaffinity of the antibody by introducing nontemplated nucleotide
changes in the variable region of the antibody gene.AlthoughCSRand SHMaremechanistically distinct, both processes are initiatedby activation-induced cytidine deaminase (AID) (9–11). AID de-aminates cytosine residues in ssDNA that are exposed duringtranscription, thereby producing U:G mismatches in target DNA(12–16). The resulting lesion is processed by base excision repairand/or mismatch repair enzymes to create mutations or DSBs (8,17, 18).Unlike RAG1/2, which targets well-defined recombination sig-
nal sequences embedded in Ig variable, diversity, and joining genesegments, AID has a preference for the RGYW motif but canmutate nearly any cytosine residue (18, 19). This lack of specificityis essential to AID’s function because it allows the enzyme to in-troduce mutations in multiple locations in large families of Igheavy-chain, κ, and λ variable genes, thereby maximizing theprobability of mutations that enhance antibody affinity. However,this lack of strong nucleotide specificity also makes AID a dan-gerous enzyme, because of its potential to damage DNAthroughout the genome.AID targets Igs preferentially; however, it produces low levels
of mutations in multiple non-Ig loci including several importantB-cell cancer-associated genes such as Pim1, Pax5, Rhoh, Bcl-6,and fas (20–24). Indeed, a recent survey suggested that up to25% of the genes expressed in B cells may be mutated by AID,but the mutational load in these genes is 20- to 100-fold lowerthan those seen in Igs (25).In addition to somatic mutations, AID also produces double-
strand breaks in IgH and at c-myc (26). As a result, AID createssubstrates for c-myc/IgH translocations (27–29). These trans-locations are infrequent events under physiologic circumstancesbecause genomic caretakers and checkpoint regulators such asATM, p19, and p53 actively suppress the emergence of cellscarrying deregulated c-myc (28, 30). Whether AID is responsiblefor dsDNA breaks that lead to translocation by genes other thanc-myc, and how these other translocations might be suppressed,has not been determined.Here we show that AID mediates the formation of lesions that
result in translocations between IgH and Igβ. These noveltranslocations are not suppressed by ATM, p53, or p19, but in-stead by a PKCδ-dependent pathway that can be activated byBAFF. The PKCδ-dependent pathway also suppresses c-myc/IgH translocation.
Author contributions: M.J., D.F.R., Y.D., A.N., and M.C.N. designed research; M.J. and T.E.performed research; M.J., D.F.R., Y.D., Y.X., A.T., and A.N. contributed new reagents/analytic tools; A.N. and M.C.N. analyzed data; and M.J. and M.C.N. wrote the paper.
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
Freely available online through the PNAS open access option.1To whom correspondence should be addressed. E-mail: [email protected].
This article contains supporting information online at www.pnas.org/cgi/content/full/0908946107/DCSupplemental.
www.pnas.org/cgi/doi/10.1073/pnas.0908946107 PNAS | January 5, 2010 | vol. 107 | no. 1 | 187–192
IMMUNOLO
GY
ResultsProtection Against c-myc/IgH Translocations. c-myc/IgH trans-location is an infrequent event in activated B cells that is increasedin the absence of ATM or p53 (28). ATM can phosphorylate p53directly or through activation of Chk2 (31–36). To evaluate therole of Chk2 in protecting cells from c-myc/IgH translocations, weanalyzed the frequency of these events in lipopolysacharide (LPS)-and IL4-stimulated Chk2−/− B cells (36). Chk2-deficient B cellswere indistinguishable from controls in terms of cell division asmeasured by CFSE [5- (and 6-) carboxyfluorescein diacetate suc-cinyl ester] dye dilution and switching to IgG1 (Fig. 1A). However,loss of Chk2 increased the frequency of c-myc/IgH translocations6-fold compared to wild type (P = 0.0237), which is ?30% of thelevel found in p53−/− B cells (Fig. 1B). We conclude that Chk2 isrequired for optimal protection of B cells from c-myc/IgH trans-locations and, like p53, it has no significant effect on classswitch recombination.ATM and Chk2 stabilize p53 by serine phosphorylation (37).
Phosphorylation of p53S18 is required for maximum activationof p53 and plays a role in activating DNA damage-inducedapoptosis (38–40), whereas phosphorylation of p53S23 is be-lieved to be required for p53 function in only certain cell types(41). Finally, combined phosphorylation of p53S18/S23 is es-sential for p53-dependent IR-induced apoptosis and tumorsuppression (38). To determine whether these p53 phosphor-ylation sites are required for protection against the accumulationof cells that bear c-myc/IgH translocations, we analyzed B cells
from mutant mice in which serines 18 and 23 have been replacedby alanines (p53S18A/23A) (38). These mutations did not alterB-cell division as measured by CFSE dye dilution, but p53S18A/23A B cells showed a small decrease in CSR and increased c-myc/IgH translocation to a level that was comparable to loss ofChk2 (P = 0.0068) (Fig. 1B). Thus, phosphorylation of p53residues S18 and/or S23 is required for protection against theaccumulation of cells that bear newly arising c-myc/IgH trans-locations in stimulated B cells in vitro, but phosphorylation ofthese residues does not account for the full effect of p53.Activation of p53 induces apoptosis through PUMA, and pro-
duces cell-cycle arrest by activating the cell-cycle inhibitor p21(42–44). To determine whether the protective effects of p53 on c-myc/IgH translocations are achieved through apoptosis or cell-cycle arrest or both, we analyzed CSR and c-myc/IgH translocationin LPS- and IL4-activated PUMA- and p21-deficient B cells.PUMA−/− and p21−/− B cells were similar in that neither alteredCSR or cell division significantly (Fig. 2A). However, loss of PU-MA increased the frequency of translocation whereas loss of p21did not (Fig. 1B).We conclude that PUMA is required for optimalprotection against c-myc/IgH translocation in activated B cells.PUMA is a Bcl-2 family member that induces apoptosis by
binding to and inhibiting prosurvival Bcl-2 family members (45).To determine whether persistent activation of Bcl-2 or Bcl-XL issufficient to protect against c-myc/IgH translocation, we analyzedactivated B cells from Bcl-2 and Bcl-XL transgenic mice (46, 47).Consistent with their prosurvival function, deregulated ex-pression of Bcl-2 or Bcl-XL increased the number of live cellsthat failed to divide or underwent a small number of cell divi-sions in response to LPS + IL4 (Fig. 2A). In addition, we found adecrease in switching to IgG1 in Bcl-2 but not Bcl-XL transgenicB cells. However, only Bcl-XL increased the frequency of c-myc/IgH translocations (Fig. 2B). We conclude that deregulated ex-pression of Bcl-XL can counteract the normal protective effects
FL4-H
p53S18/23 p21-/- Puma-/-Chk2-/-
% o
f iso
type
sw
itchi
ng
0
0.20.4
0.60.8
1
1.21.4
1.61.8
2
c-m
yc/Ig
H t
ran
slo
cati
on
s
WT Chk2-/-
100 101 102 103 104
# o
f cells
p21-/-
100 101 102 103 104100 101 102 103 104
Puma-/-
100 101 102 103 104
8.09 8.66 6.466.551
GgI
CFSE
p53S18/23 p21-/- Puma-/- Chk2-/-WT p53-/-
p=0.0068
p=0.0237
p=0.1595
p=0.0127
p<0.0001
A
B
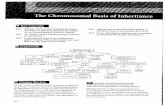
Fig. 1. CSR and c-myc/IgH translocation in mutant B cells. (A) Flow cyto-metric analysis of CSR to IgG1 and cell division by dilution of CFSE inp53S18A/23A mutant, Chk−/−, Puma−/−, and p21−/− B cells activated with LPSand IL4 for 72 h. Graphs show percentage of switching relative to matchedwild-type controls and/or relative to B cells stimulated with RP105 to inducecell division but not CSR. Each bar represents the mean value of two or moreindependent experiments. (B) Graph shows the number of Southern blot-confirmed c-myc/IgH translocations per 106 cells. Each value was obtainedfrom independent samples from at least two mice in which a total of 10–20million cells were assayed.
% o
f is
oty
pe
swit
chin
g
100 101 102 103 104100 101 102 103 104 100 101 102 103 100
Bcl2TgWT BclXLTG
Bcl2TG BclXL Bim-/-0
0.2
0.4
0.6
0.8
1
1.2
c-m
yc/Ig
H t
ran
slo
cati
on
s# o
f cells
CFSE
Bcl2TG BclXL Bim-/-
p=0.0013
p=0.0023
A
B
Fig. 2. Class switch recombination and c-myc/IgH translocations in Bcl-2family mutant B cells. (A) Flow cytometric analysis of cell division by CFSE dyedilution and CSR in LPS and IL4 stimulated B cells from wild-type, Bcl-2 trans-genic, Bcl-XL transgenic, and Bim−/− mice. Graphs show percentage of CSRrelative to matched controls. (B) Graph represents the number of c-myc/IgHtranslocations per 106 cells. Each value was obtained from three independentsamples with a total of 10–20 million cells assayed.
188 | www.pnas.org/cgi/doi/10.1073/pnas.0908946107 Jankovic et al.
of p53 and enhance the survival of B cells that undergo c-myc/IgH translocation.Like PUMA, Bim is a proapoptotic Bcl-2 family member
whose deletion accelerates lymphomagenesis in Eμ-myc trans-genic mice (48). To determine whether loss of Bim also enhancesc-myc/IgH translocation, we assayed LPS- and IL4-activatedBim−/− B cells. Loss of Bim produced a decrease in CSR to IgG1and increased the frequency of c-myc/IgH translocations to thesimilar degree as loss of PUMA or transgenic expression of Bcl-XL (P = 0.0023) (Fig. 2B). Our results suggest that c-myc/IgHtranslocation activates p53-induced apoptosis through PUMAand Bim possibly by inhibition of Bcl-XL and Bcl-6 (49).BAFF is an important B-cell cytokine that promotes B-cell sur-
vival and whose deregulated expression is associated with auto-immunity and increased incidence of lymphoma (50–52). Todetermine whether BAFF enhances translocation, we added thiscytokine to cultures of LPS- and IL4-stimulated B cells. BAFF didnot alter cell division or switching to IgG1, but like transgenic Bcl-2and Bcl-XL enhanced survival of cells that had undergone fewerdivisions (Fig. 3A). BAFF increased the frequency of c-myc/IgHtranslocation 10-fold (P = 0.0007). Similar to BAFF, addition ofcaspase inhibitor II resulted ina7-fold increase in translocation (P=0.0127) (Fig. 3A). We conclude that BAFF enhances the survival ofB cells that carry c-myc/IgH translocation.BAFF promotes B-cell survival by activating antiapoptotic
responses throughNF-κBand by preventing nuclear localization ofprotein kinase Cδ (PKCδ) (53). Because nuclear accumulation ofPKCδ is essential for induction of apoptosis, we analyzed CSR andc-myc/IgH translocations in PKCδ−/− B cells. Although CSR wasnot affected by the absence of PKCδ, the frequency of c-myc/IgHtranslocation was dramatically increased (Fig. 3B). We concludethat apoptotic signals that depend on PKCδ play an important rolein elimination of B cells with c-myc/IgH translocations.
Igβ/IgH Translocations. Up to 25% of the 118 genes expressed ingerminal center B cells are mutated by AID, but at levels that are20- to 100-fold lower than Ig (25). For example, mutations in Igβ,an essential signaling component of the B-cell receptor, arefound at a rate of 1 × 10−4 whereas mutations in Ig JH4 werepresent at 1.6 × 10−2 in the same experiments (22, 25).To determine whether AID produces DSBs in Igβ that might
lead to chromosomal translocations, we designed a PCR assayfor detecting translocations between Igβ and IgH (Fig. 4A).Amplified products were confirmed as authentic Igβ/IgH trans-locations by sequencing. Translocation breakpoints showed smallamounts of microhomology (1–4 bp) and a few nucleotide ad-ditions (Table S1). Igβ/IgH translocations appeared at a fre-quency of 0.4 × 10−6 in wild-type B cells stimulated with LPS andIL4 but were not detected in the absence of AID (Fig. 5A). Thus,in addition to c-myc/IgH translocations, activated B cells alsosuffer AID-dependent translocations between Igβ and IgH.To determine whether AID is the source of dsDNA breaks in
Igβ that lead to Igβ/IgH translocations, we made use of mice thatcarry an I-SceI site in IgH (IgHI/I) (26). I-SceI is an endonucleasethat recognizes an 18-bp site that is not normally present in themouse genome (54). Expression of I-SceI in IgHI/I B cells pro-duces DSBs 5′ of Sμ irrespective of AID expression (26). Similarto c-myc/IgH translocation, I-SceI expression in IgHI/I B cellsresulted in high levels of Igβ/IgH translocations (3 × 10−6 Igβ/IgHversus 4.5 × 10−6 c-myc/IgH) (Fig. 4C). In contrast, AID-defi-cient IgHI/I B cells (IgHI/IAID−/−) assayed under the sameconditions were devoid of both c-myc/IgH and Igβ/IgH trans-locations (Fig. 4C). Thus, AID is required for the DSBs in theIgβ gene that lead to Igβ/IgH translocations in activated B cells.
ATM, p53, and p19 Do Not Protect Against Igβ/IgH Translocations.ATM, p53, and p19 protect B cells against c-myc/IgH translocation.
FL4-H
FL4-HFL4-H
100 101 102 103 104 100 101 102 103 104 100 101 102 103 104
+BAFF +caspase inh.
8.04 8 7.24
LPS + IL4
0
0.2
0.4
0.6
0.8
1
1.2
1.4
c-m
yc/Ig
H t
ran
slo
cati
on
s
LPS+IL4 LPS+IL4+caspase inh.
LPS+IL4+BAFF
p=0.0007
p=0.0127
% o
f iso
type
sw
itchi
ng
LPS+IL4+caspase inh.
LPS+IL4+BAFF
# o
f cells
1G
gI
CFSE
0
0.5
1
1.5
2
2.5
3
3.5
WT PKC -/- p53-/-
WT PKC -/-
14.412.5
# o
f cells
1G
gI
CFSE
WT PKC -/-
% o
f iso
type
sw
itchi
ngc-
myc
/IgH
tra
nsl
oca
tio
ns
p<0.001
A B
Fig. 3. CSR and c-myc/IgH translocations from BAFF-stimulated wild-type B cells or PKCδ−/− B cells. (A) Flow cytometric analysis of CSR to IgG1, and celldivision and c-myc/IgH translocation in wild-type B-cell cultures supplemented with BAFF or caspase inhibitor II (50 μM; Calbiochem). (B) CSR to IgG1 andc-myc/IgH translocations in LPS- and IL4-stimulated PKCδ−/− B cells. Each value was obtained from four independent samples (10 million cells were assayed).
Jankovic et al. PNAS | January 5, 2010 | vol. 107 | no. 1 | 189
IMMUNOLO
GY
These factors canbeactivateddirectlybyany event that is associatedwithDNAdamagebefore translocation or by c-mycoverexpression,which induces the oncogenic stress response after aberrant chro-mosome joining (55, 56). In contrast, Igβ/IgH translocation shouldnot activate the oncogenic stress pathway. To determine whetherATM,p53, andp19 suppress Igβ/IgH translocations,wecompared c-myc/IgH and Igβ/IgH translocations in activated ATM−/−, p53−/−,and p19−/− B cells. Whereas the frequency of c-myc/IgH trans-location was increased in the absence of ATM or p53 or p19, wefound no increase in the rate of Igβ/IgH translocations in the samesamples (Fig. 5A). We conclude that dsDNA breaks that are obli-gate intermediates in Igβ/IgH translocations fail to activate ATM-p53-p19-dependent cellular responses. The difference between thetwo types of translocations suggests that activation of ATM, p53,
and p19 ismediated by overexpression of c-myc and that the degreeof DNA damage incurred during CSR is not sufficient to inducep53-mediated cell death.
Protection Against Translocation by PKCδ. BAFF promotes B-cellsurvival by PKCδ- and NF-κB-dependent pathways that are notknown to intersect with ATM or the oncogenic stress response(52). To determine the role of this pathway in Igβ/IgH trans-locations, we analyzed PKCδ−/− or BAFF-treated wild-type Bcells. Similar to c-myc/IgH, the frequency of Igβ/IgH translocationwas increased by addition of BAFF or in the absence of PKCδ(Fig. 5B). We conclude that PKCδ protects against and thatBAFF enhances the survival of B cells that carry either c-myc/IgH or Igβ/IgH translocations.
DiscussionB-cell transformation is the endproduct of amultistep process thatfrequently includes chromosomal translocations that activateoncogenes (56). An additional common lesion is inactivation oftumor suppressors such as p53, either directly by mutation orthrough alterations in its regulators like ATM or Bcl-6 (1). Theexperiments presented here provide additional insights into mo-lecular requirements for translocation reactions in B lymphocytesand the cellular pathways that protect against these events.Chromosomal translocations between c-myc and IgH are sig-
nature features of Burkitt’s lymphoma (57–64). These trans-locations, like all others, require formation of double-strandbreaks on both partner chromosomes. In the case of c-myc/IgHtranslocation, AID creates the DSBs on both partners, but theDSBs on c-myc are rare and limit the frequency of translocation(26, 65). This is consistent with the rather low rate of AID-mediated mutation in c-myc and this gene’s propensity for high-fidelity repair (24, 25). But c-myc is only one of many non-Iggenes that are translocated in lymphoma or mutated by AID (1–3, 25). Our experiments show that in addition to c-myc, AID alsoproduces lesions in Igβ that can serve as substrates for trans-location to IgH. Thus, AID-induced DSBs are not limited to c-myc or IgH. We speculate that in addition to Igβ, such lesionsmay occur at many of the other known AID target genes andaccount for a substantial fraction of the DSBs that lead to lym-phoma-associated translocations in Ig and non-Ig genes.B cells are normally protected against developing AID-induced
c-myc/IgH translocations by ATM, p53, and p19, or genes such as
Ig /IgH c-myc/IgH
I-SceI I-SceI* I-SceI I-SceI*
IgHI/I
IgHI/IAID-/-
FL4-H
14.1
FL4-H
0.076
IgHI/I IgHI/IAID-/-
G1
gI
GFP
00.51
1.52
2.53
3.54
4.55
Jh4 Em Im Sm repeats Cm
Ig
IgHI/I
c-myc/IgH Ig /IgH
I-SceI
I-SceI*
I-SceI
I-SceI*
sn
oitaco ls
nart
A
C
B
6 exon12345
Fig. 4. Igβ/IgH translocations. (A) Schematic representation of Igβ and IgH locus showing the position of the primers used to detect Igβ/IgH translocations. (B)Flow cytometric analysis of CSR to IgG1 from IgHI/I and IgHI/I AID−/− B cells stimulated with LPS and IL4 and infected with a retrovirus carrying I-SceI or I-SceI*and GFP as a marker (26). GFP+ cells were sorted and analyzed for translocations. (C) Translocations by retroviral I-SceI or I-SceI*, which is an inactive mutantform of the enzyme. Ethidium bromide-stained agarose gels with PCR products corresponding to Igβ/IgH and c-myc/IgH translocations as verified by se-quencing. Graph represents the comparison of translocation frequencies from two independent experiments in which a total of 10 million cells were assayed.
Ig /IgH
WT AID-/- ATM-/- p53-/- p19-/-0
0.2
0.4
0.6
0.8
1
1.2
1.4
01X
ST
fo
ycne
uqerf
6-
c-myc/IgH
WT AID-/- ATM-/- p53-/-
01X
ST
fo
ycne
uqerf
-6
0
0.2
0.4
0.6
0.8
1
1.2
1.4
0
0.2
0.4
0.6
1
1.2
1.4
1.6
1.8
LPS/IL4 BAFF
0.8
P=0.179
P=0.3
P<0.0001
PKC -/-
p19-/-
P=0.443
P<0.0001
A
B
Fig. 5. Frequency of Igβ/IgH translocations in mutant B cells. (A) Graphsrepresent number of translocations per 106 cells from wild-type, AID−/−,ATM−/−, p53−/−, and p19−/− B cells. c-myc/IgH (left) and Igβ/IgH (right)translocation frequency obtained from the same DNA samples. (B) Igβ/IgHtranslocations in wild-type B cells supplemented with BAFF or PKCδ−/− B cells.Graph represents the comparison of translocation frequencies from threeindependent samples in which a total of 10 million cells were assayed.
190 | www.pnas.org/cgi/doi/10.1073/pnas.0908946107 Jankovic et al.
Bcl-6 that interfere with p53 induction (28, 30, 49, 66) (Fig. 2C). Itis therefore not surprising that the expression of these genes isfrequently altered in translocation-bearing lymphomas (67). Thep53 pathway might be triggered directly by the DSBs created byAID, or alternatively indirectly by deregulated expression oftranslocated genes such as c-myc (56). DNA damage-dependentactivation of p53 would be expected to suppress any translocationirrespective of the site of the DNA break. In contrast, the onco-genic stress response would only be engaged by the subset oftranslocations that involve oncogene deregulation. Our experi-ments show that loss of ATM, or p53 or p19, is not sufficient toalter the frequency of Igβ/IgH translocations, and therefore AID-induced DNA damage alone is insufficient to activate the p53pathway. In contrast to p53 and p19, ATM is activated duringCSRand is required for efficient completion of the reaction (68, 69).Therefore, despite ATM’s activation during CSR, AID-inducedDSBs alone fail to prevent accumulation of Igβ/IgH translocations.This disconnect between the ATM-mediated DNA damage re-sponse and p53-induced cell death is likely to be necessary forsuccessful CSR; otherwise, all cells that activate ATM while at-tempting CSR would be eliminated. We conclude that B cells areprotected from c-myc/IgH translocations primarily by the p53-mediated oncogenic stress response.The idea that p53-induced apoptosis is an important mecha-
nism for elimination of B cells that overexpress c-myc as a resultof translocation is supported by the observation that deregulatedexpression of antiapoptotic factors like Bcl-2 or Bcl-XL accel-erates lymphoma development in c-myc transgenic mice (70–72).Our experiments demonstrate that cells that develop AID-mediated c-myc/IgH translocations are eliminated by a pathwaythat requires PUMA, Bim, and caspase activation and can bereversed by overexpression of Bcl-XL but not Bcl-2. The sur-prising difference between Bcl-XL and Bcl-2 might in part beattributed to a reciprocal expression pattern of these two factorsin developing and activated B cells. Whereas Bcl-XL is expressedin pre-B cells, Bcl-2 is expressed in and is crucial for the survivalof immature and mature naïve B cells (47, 73), and only Bcl-XLis significantly up-regulated in activated B cells (47). Thus, en-forced transgenic expression of Bcl-2 under the control of Igregulatory elements in the Bcl-2 transgene may account in partfor its interference with CSR and inability to protect againstaccumulation of cells with c-myc/IgH translocation. The p53pathway is only one of many molecular pathways that regulatesurvival by inducing apoptosis (30). One of the other key survivalpathways in mature B cells is mediated by the tumor necrosisfactor (TNF) family of cytokines, which includes BAFF (52).Like loss of p53, deregulated expression of BAFF is associatedwith lymphomas that carry chromosomal translocations in hu-mans and mice (50, 74, 75). This effect is likely due to the en-hanced survival of translocation-bearing B cells when they are
stimulated with BAFF (Fig. 3A). More intriguing is the ob-servation that PKCδ, a key mediator of the BAFF signalingpathway, is essential to prevent the survival of B cells that carryboth c-myc/IgH and Igβ/IgH translocations. Therefore, in contrastto the p53-mediated pathway, the apoptosis pathway triggered byPKCδ does not require oncogene activation.Finally, deregulated expression of BAFF is associated with
autoimmune diseases such as Sjogren’s syndrome, rheumatoidarthritis, and systemic lupus erythematosus that also show an in-crease in the incidence of lymphoma (50, 76). BAFF is believed topromote autoimmunity by promoting the survival of autoreactiveB cells. We speculate that BAFF-dependent increase in survivalof B cells with chromosome translocation may in part account forthe link between autoimmunity and lymphoma.
MethodsMice. IgHI/I (26); Chk2−/− (36); p53S18A/23A (38); p21−/− (42); PUMA−/− (44);Bcl-XL (47); Bcl-2 (46); PKCδ−/− (77) p19−/− (78); ATM−/− (79) (obtained fromthe Mouse Models of Human Cancer Consortium); and p53−/− (purchasedfrom Taconic Laboratories) were previously described. All experiments withmice were performed according to protocols approved by the RockefellerUniversity Animal Care and Use Committee.
B-Cell Cultures and Retroviral Transduction. B lymphocytes were cultured andtransduced with retroviruses as described (28). The I-SceI and mutant controlI-SceI* retroviruses were as described (26). BAFF (R&D Systems) was used at aconcentration of 50 ng/mL caspase inhibitor II (Calbiochem) was used at aconcentration of 50 μM. Cells were analyzed after 3 days of culture unlessotherwise indicated.
Flow Cytometry and Cell Sorting. For flow cytometric analysis, cell suspensionswere stained with fluorochrome-conjugated anti-IgG1 (Pharmingen). Datawere acquired on a FACSCalibur (Becton Dickinson) and analyzedwith FlowJosoftware (Treestar). CFSE labeling for cell division was at 37°C for 10 min in 5μM carboxyfluorescein succinimidyl ester (CFSE; Molecular Probes). Lym-phoid populations were sorted to >95% purity with a FACSVantage SE withDiVa option or FACSAria instruments (Becton Dickinson).
PCR Assay for Translocations. PCR reactions for c-myc/IgH translocations wereperformed as described (28). For Igβ/IgH translocations, nested PCR was doneusing the following primers. For the Igβ side, the following primers (Igβ exon4) were used for nested PCR: 5′-AAGTAGCAGGAAGATGGGCAC AATG-3′; 5′-TGAAGAGGATGATGAGGAGGGTCTG-3′. For the IgH side, the following pri-mers upstream of Sm were used for nested PCR: 5′-TGAGGACCAGAGAGGGAT AAAAGAGAA-3′ and 5′-GGGGAGGGGGTGTCAAATAATAAGA-3′; Igβ/IgH translocations were confirmed by direct cloning and sequencing.
ACKNOWLEDGMENTS. We thank Klara Velinzon for FACSorting and DavidBosque for help in managing the mouse colonies. The work was supported inpart by an NIH grant to M.C.N. (AI037526). A.N. was supported by theIntramural Research Program of the NIH, National Cancer Institute and theCenter for Cancer Research. M.C.N. is an HHMI Investigator.
1. Küppers R, Dalla-Favera R (2001) Mechanisms of chromosomal translocations in B cell
lymphomas. Oncogene 20:5580–5594.2. Leder P, et al. (1983) Translocations among antibody genes in human cancer. Science
222:765–771.3. Rabbitts TH (1994) Chromosomal translocations in human cancer. Nature 372:
143–149.4. Schatz DG, Oettinger MA, Baltimore D (1989) The V(D)J recombination activating
gene, RAG-1. Cell 59:1035–1048.5. Oettinger MA, Schatz DG, Gorka C, Baltimore D (1990) RAG-1 and RAG-2, adjacent
genes that synergistically activate V(D)J recombination. Science 248:1517–1523.6. Bassing CH, Swat W, Alt FW (2002) The mechanism and regulation of chromosomal V
(D)J recombination. Cell 109 (Suppl):S45–S55.7. Sleckman BP (2005) Lymphocyte antigen receptor gene assembly: Multiple layers of
regulation. Immunol Res 32:253–258.8. Stavnezer J, Guikema JE, Schrader CE (2008) Mechanism and regulation of class switch
recombination. Annu Rev Immunol 26:261–292.9. Muramatsu M, et al. (2000) Class switch recombination and hypermutation require
activation-induced cytidine deaminase (AID), a potential RNA editing enzyme. Cell
102:553–563.
10. MuramatsuM, et al. (1999) Specific expression of activation-induced cytidine deaminase
(AID), a novel member of the RNA-editing deaminase family in germinal center B cells.
J Biol Chem 274:18470–18476.11. Revy P, et al. (2000) Activation-induced cytidine deaminase (AID) deficiency causes the
autosomal recessive form of the Hyper-IgM syndrome (HIGM2). Cell 102:565–575.12. Chaudhuri J, et al. (2003) Transcription-targeted DNA deamination by the AID
antibody diversification enzyme. Nature 422:726–730.13. Dickerson SK, Market E, Besmer E, Papavasiliou FN (2003) AID mediates hypermutation
by deaminating single stranded DNA. J Exp Med 197:1291–1296.14. Petersen-Mahrt SK, Harris RS, Neuberger MS (2002) AID mutates E. coli suggesting a
DNA deamination mechanism for antibody diversification. Nature 418:99–103.15. Ramiro AR, Stavropoulos P, Jankovic M, Nussenzweig MC (2003) Transcription
enhances AID-mediated cytidine deamination by exposing single-stranded DNA on the
nontemplate strand. Nat Immunol 4:452–456.16. Pham P, Bransteitter R, Petruska J, Goodman MF (2003) Processive AID-catalysed
cytosine deamination on single-stranded DNA simulates somatic hypermutation.
Nature 424:103–107.17. Rada C, et al. (2002) Immunoglobulin isotype switching is inhibited and somatic
hypermutation perturbed in UNG-deficient mice. Curr Biol 12:1748–1755.
Jankovic et al. PNAS | January 5, 2010 | vol. 107 | no. 1 | 191
IMMUNOLO
GY
18. Di Noia JM, Neuberger MS (2007) Molecular mechanisms of antibody somatichypermutation. Annu Rev Biochem 76:1–22.
19. Rogozin IB, Pavlov YI, Bebenek K, Matsuda T, Kunkel TA (2001) Somatic mutationhotspots correlate with DNA polymerase η error spectrum. Nat Immunol 2:530–536.
20. Shen HM, Peters A, Baron B, Zhu X, Storb U (1998) Mutation of BCL-6 gene in normalB cells by the process of somatic hypermutation of Ig genes. Science 280:1750–1752.
21. Pasqualucci L, et al. (1998) BCL-6 mutations in normal germinal center B cells:Evidence of somatic hypermutation acting outside Ig loci. Proc Natl Acad Sci USA 95:11816–11821.
22. Gordon MS, Kanegai CM, Doerr JR, Wall R (2003) Somatic hypermutation of the B cellreceptor genes B29 (Igβ, CD79b) and mb1 (Igα, CD79a). Proc Natl Acad Sci USA 100:4126–4131.
23. Müschen M, et al. (2000) Somatic mutation of the CD95 gene in human B cells as aside-effect of the germinal center reaction. J Exp Med 192:1833–1840.
24. Pasqualucci L, et al. (2001) Hypermutation of multiple proto-oncogenes in B-celldiffuse large-cell lymphomas. Nature 412:341–346.
25. Liu M, et al. (2008) Two levels of protection for the B cell genome during somatichypermutation. Nature 451:841–845.
26. Robbiani DF, et al. (2008) AID is required for the chromosomal breaks in c-myc thatlead to c-myc/IgH translocations. Cell 135:1028–1038.
27. Kovalchuk AL, et al. (2007) AID-deficient Bcl-xL transgenic mice develop delayedatypical plasma cell tumors with unusual Ig/Myc chromosomal rearrangements. J ExpMed 204:2989–3001.
28. Ramiro AR, et al. (2006) Role of genomic instability and p53 in AID-induced c-myc-Ightranslocations. Nature 440:105–109.
29. Ramiro AR, et al. (2004) AID is required for c-myc/IgH chromosome translocations invivo. Cell 118:431–438.
30. Hoffman B, Liebermann DA (2008) Apoptotic signaling by c-MYC. Oncogene 27:6462–6472.
31. Canman CE, et al. (1998) Activation of the ATM kinase by ionizing radiation andphosphorylation of p53. Science 281:1677–1679.
32. Banin S, et al. (1998) Enhanced phosphorylation of p53 by ATM in response to DNAdamage. Science 281:1674–1677.
33. Nakagawa K, Taya Y, Tamai K, Yamaizumi M (1999) Requirement of ATM inphosphorylation of the human p53 protein at serine 15 following DNA double-strandbreaks. Mol Cell Biol 19:2828–2834.
34. Ahn J, Urist M, Prives C (2004) The Chk2 protein kinase. DNA Repair (Amst) 3:1039–1047.
35. Hirao A, et al. (2002) Chk2 is a tumor suppressor that regulates apoptosis in both anataxia telangiectasia mutated (ATM)-dependent and an ATM-independent manner.Mol Cell Biol 22:6521–6532.
36. Takai H, et al. (2002) Chk2-deficient mice exhibit radioresistance and defective p53-mediated transcription. EMBO J 21:5195–5205.
37. Xu Y (2003) Regulation of p53 responses by post-translational modifications. CellDeath Differ 10:400–403.
38. Chao C, Herr D, Chun J, Xu Y (2006) Ser18 and 23 phosphorylation is required for p53-dependent apoptosis and tumor suppression. EMBO J 25:2615–2622.
39. Borges HL, Chao C, Xu Y, Linden R, Wang JY (2004) Radiation-induced apoptosis indeveloping mouse retina exhibits dose-dependent requirement for ATM phosphorylationof p53. Cell Death Differ 11:494–502.
40. Sluss HK, Armata H, Gallant J, Jones SN (2004) Phosphorylation of serine 18 regulatesdistinct p53 functions in mice. Mol Cell Biol 24:976–984.
41. Wu Z, et al. (2002) Mutation of mouse p53 Ser23 and the response to DNA damage.Mol Cell Biol 22:2441–2449.
42. Deng C, Zhang P, Harper JW, Elledge SJ, Leder P (1995) Mice lacking p21CIP1/WAF1undergo normal development, but are defective in G1 checkpoint control. Cell 82:675–684.
43. Yu J, Zhang L (2005) The transcriptional targets of p53 in apoptosis control. BiochemBiophys Res Commun 331:851–858.
44. Villunger A, et al. (2003) p53- and drug-induced apoptotic responses mediated byBH3-only proteins Puma and Noxa. Science 302:1036–1038.
45. Adams JM, Cory S (2007) Bcl-2-regulated apoptosis: Mechanism and therapeuticpotential. Curr Opin Immunol 19:488–496.
46. McDonnell TJ, et al. (1989) bcl-2-immunoglobulin transgenic mice demonstrateextended B cell survival and follicular lymphoproliferation. Cell 57:79–88.
47. Grillot DA, et al. (1996) bcl-x exhibits regulated expression during B cell developmentand activation and modulates lymphocyte survival in transgenic mice. J Exp Med 183:381–391.
48. Egle A, Harris AW, Bouillet P, Cory S (2004) Bim is a suppressor of Myc-induced mouseB cell leukemia. Proc Natl Acad Sci USA 101:6164–6169.
49. Pasqualucci L, et al. (2008) AID is required for germinal center-derived lymphomagenesis.Nat Genet 40:108–112.
50. Batten M, et al. (2004) TNF deficiency fails to protect BAFF transgenic mice againstautoimmunity and reveals a predisposition to B cell lymphoma. J Immunol 172:812–822.
51. Chiu A, et al. (2007) Hodgkin lymphoma cells express TACI and BCMA receptors andgenerate survival and proliferation signals in response to BAFF and APRIL. Blood 109:729–739.
52. Mackay F, Schneider P (2009) Cracking the BAFF code. Nat Rev Immunol 9:491–502.53. Mecklenbräuker I, Kalled SL, Leitges M, Mackay F, Tarakhovsky A (2004) Regulation of
B-cell survival by BAFF-dependent PKCδ-mediated nuclear signalling. Nature 431:456–461.
54. Stoddard BL (2005) Homing endonuclease structure and function. Q Rev Biophys 38:49–95.
55. Cleveland JL, Sherr CJ (2004) Antagonism of Myc functions by Arf. Cancer Cell 6:309–311.
56. Lowe SW, Cepero E, Evan G (2004) Intrinsic tumour suppression. Nature 432:307–315.57. Adams JM, Gerondakis S, Webb E, Corcoran LM, Cory S (1983) Cellular myc oncogene
is altered by chromosome translocation to an immunoglobulin locus in murineplasmacytomas and is rearranged similarly in human Burkitt lymphomas. Proc NatlAcad Sci USA 80:1982–1986.
58. Adams JM, et al. (1982) Transcriptionally active DNA region that rearrangesfrequently in murine lymphoid tumors. Proc Natl Acad Sci USA 79:6966–6970.
59. Crews S, Barth R, Hood L, Prehn J, Calame K (1982) Mouse c-myc oncogene is locatedon chromosome 15 and translocated to chromosome 12 in plasmacytomas. Science218:1319–1321.
60. Dalla-Favera R, Martinotti S, Gallo RC, Erikson J, Croce CM (1983) Translocation andrearrangements of the c-myc oncogene locus in human undifferentiated B-celllymphomas. Science 219:963–967.
61. Erikson J, Ar-Rushdi A, Drwinga HL, Nowell PC, Croce CM (1983) Transcriptionalactivation of the translocated c-myc oncogene in Burkitt lymphoma. Proc Natl AcadSci USA 80:820–824.
62. Hamlyn PH, Rabbitts TH (1983) Translocation joins c-myc and immunoglobulin γ 1genes in a Burkitt lymphoma revealing a third exon in the c-myc oncogene. Nature304:135–139.
63. Marcu KB, et al. (1983) Transcriptionally active c-myc oncogene is contained withinNIARD, a DNA sequence associated with chromosome translocations in B-cellneoplasia. Proc Natl Acad Sci USA 80:519–523.
64. Taub R, et al. (1982) Translocation of the c-myc gene into the immunoglobulin heavychain locus in human Burkitt lymphoma and murine plasmacytoma cells. Proc NatlAcad Sci USA 79:7837–7841.
65. Wang JH, et al. (2009) Mechanisms promoting translocations in editing and switchingperipheral B cells. Nature 460:231–236.
66. Saito M, et al. (2009) BCL6 suppression of BCL2 via Miz1 and its disruption in diffuselarge B cell lymphoma. Proc Natl Acad Sci USA 106:11294–11299.
67. Eischen CM, Weber JD, Roussel MF, Sherr CJ, Cleveland JL (1999) Disruption of theARF-Mdm2-p53 tumor suppressor pathway in Myc-induced lymphomagenesis. GenesDev 13:2658–2669.
68. Lumsden JM, et al. (2004) Immunoglobulin class switch recombination is impaired inAtm-deficient mice. J Exp Med 200:1111–1121.
69. Reina-San-Martin B, Chen HT, Nussenzweig A, Nussenzweig MC (2004) ATM isrequired for efficient recombination between immunoglobulin switch regions. J ExpMed 200:1103–1110.
70. Beverly LJ, Varmus HE (2009) MYC-induced myeloid leukemogenesis is accelerated byall six members of the antiapoptotic BCL family. Oncogene 28:1274–1279.
71. Strasser A, Harris AW, Bath ML, Cory S (1990) Novel primitive lymphoid tumoursinduced in transgenic mice by cooperation between myc and bcl-2. Nature 348:331–333.
72. Vaux DL, Cory S, Adams JM (1988) Bcl-2 gene promotes haemopoietic cell survival andcooperates with c-myc to immortalize pre-B cells. Nature 335:440–442.
73. Chao DT, Korsmeyer SJ (1998) BCL-2 family: Regulators of cell death. Annu RevImmunol 16:395–419.
74. Moreaux J, et al. (2004) BAFF and APRIL protect myeloma cells from apoptosisinduced by interleukin 6 deprivation and dexamethasone. Blood 103:3148–3157.
75. He B, et al. (2004) Lymphoma B cells evade apoptosis through the TNF familymembers BAFF/BLyS and APRIL. J Immunol 172:3268–3279.
76. Mackay F, Schneider P, Rennert P, Browning J (2003) BAFF AND APRIL: A tutorial on Bcell survival. Annu Rev Immunol 21:231–264.
77. Leitges M, et al. (2001) Exacerbated vein graft arteriosclerosis in protein kinase Cδ-null mice. J Clin Invest 108:1505–1512.
78. Kamijo T, et al. (1997) Tumor suppression at the mouse INK4a locus mediated by thealternative reading frame product p19ARF. Cell 91:649–659.
79. Barlow C, et al. (1996) Atm-deficient mice: A paradigm of ataxia telangiectasia. Cell86:159–171.
192 | www.pnas.org/cgi/doi/10.1073/pnas.0908946107 Jankovic et al.