MicroRNAs, Tristetraprolin Family Members and HuR - MDPI
-
Upload
khangminh22 -
Category
Documents
-
view
4 -
download
0
Transcript of MicroRNAs, Tristetraprolin Family Members and HuR - MDPI
Citation: Sobolewski, C.; Dubuquoy,
L.; Legrand, N. MicroRNAs,
Tristetraprolin Family Members and
HuR: A Complex Interplay
Controlling Cancer-Related Processes.
Cancers 2022, 14, 3516. https://
doi.org/10.3390/cancers14143516
Academic Editors: Stefan
Hüttelmaier and Tony Gutschner
Received: 29 June 2022
Accepted: 18 July 2022
Published: 20 July 2022
Publisher’s Note: MDPI stays neutral
with regard to jurisdictional claims in
published maps and institutional affil-
iations.
Copyright: © 2022 by the authors.
Licensee MDPI, Basel, Switzerland.
This article is an open access article
distributed under the terms and
conditions of the Creative Commons
Attribution (CC BY) license (https://
creativecommons.org/licenses/by/
4.0/).
cancers
Review
MicroRNAs, Tristetraprolin Family Members and HuR:A Complex Interplay Controlling Cancer-Related ProcessesCyril Sobolewski * , Laurent Dubuquoy and Noémie Legrand
Inserm, CHU Lille, U1286-INFINITE-Institute for Translational Research in Inflammation, Univ. Lille,F-59000 Lille, France; [email protected] (L.D.); [email protected] (N.L.)* Correspondence: [email protected]; Tel.: +33-673-148-952
Simple Summary: AU-rich Element Binding Proteins (AUBPs) represent important post-transcriptionalregulators of gene expression by regulating mRNA decay and/or translation. Importantly, AUBPscan interfere with microRNA-dependent regulation by (i) competing with the same binding sites onmRNA targets, (ii) sequestering miRNAs, thereby preventing their binding to their specific targets or (iii)promoting miRNA-dependent regulation. These data highlight a new paradigm where both miRNA andRNA binding proteins form a complex regulatory network involved in physiological and pathologicalprocesses. However, this interplay is still poorly considered, and our current models do not integratethis level of complexity, thus potentially giving misleading interpretations regarding the role of theseregulators in human cancers. This review summarizes the current knowledge regarding the crosstalksexisting between HuR, tristetraprolin family members and microRNA-dependent regulation.
Abstract: MicroRNAs represent the most characterized post-transcriptional regulators of gene ex-pression. Their altered expression importantly contributes to the development of a wide range ofmetabolic and inflammatory diseases but also cancers. Accordingly, a myriad of studies has sug-gested novel therapeutic approaches aiming at inhibiting or restoring the expression of miRNAsin human diseases. However, the influence of other trans-acting factors, such as long-noncodingRNAs or RNA-Binding-Proteins, which compete, interfere, or cooperate with miRNAs-dependentfunctions, indicate that this regulatory mechanism is much more complex than initially thought, thusquestioning the current models considering individuals regulators. In this review, we discuss theinterplay existing between miRNAs and the AU-Rich Element Binding Proteins (AUBPs), HuR andtristetraprolin family members (TTP, BRF1 and BRF2), which importantly control the fate of mRNAand whose alterations have also been associated with the development of a wide range of chronicdisorders and cancers. Deciphering the interplay between these proteins and miRNAs representsan important challenge to fully characterize the post-transcriptional regulation of pro-tumorigenicprocesses and design new and efficient therapeutic approaches.
Keywords: microRNAs; AUBP; HuR; TTP; cancers
1. Introduction
Trans-acting factors controlling the fate of mRNA importantly contribute to gene ex-pression regulation. Among them, intense efforts have been devoted to non-coding RNAs,mostly miRNAs, which mainly bind to the 3′Untranslated Region (3′-UTR) of target mR-NAs and promote either mRNA degradation and/or translation inhibition [1]. The impor-tance of miRNAs in physiological and pathological processes is now well-established. Formost human diseases, the altered miRnome has been identified through high-throughputapproaches and has suggested appealing therapeutic approaches to target deregulatedmiRNAs [2,3]. However, increasing studies indicate that the post-transcriptional regulationof gene expression is more complex than originally thought and requires other regulators,such as long-non-coding RNAs (lncRNA) or RNA-Binding Proteins (RBPs) [4–6]. AU-Rich
Cancers 2022, 14, 3516. https://doi.org/10.3390/cancers14143516 https://www.mdpi.com/journal/cancers
Cancers 2022, 14, 3516 2 of 30
Element Binding Proteins (AUBPs) are RBPs of particular importance due to their abilityto bind to AU-rich sequences in the 3′UTR of immediate response genes (e.g., TNF-α,cyclooxygenase-2) and promote either their decay or translation inhibition [7,8]. Similarly,for miRNAs, deregulated expression/activity of AUBPs strongly contributes to the de-velopment of a wide range of diseases due to their ability to control a whole set of genesassociated with pathological processes, including inflammation (e.g., Tumor Necrosis Fac-tor alpha, TNFα), fibrosis, metabolism, or carcinogenesis [9]. These proteins can interfere,compete, or synergize with miRNA-dependent regulation [10,11] and conversely, miRNAscan also regulate the expression of AUBPs. However, this complex interplay is poorlyconsidered in most studies (e.g., miR-21, [12]; let-7 [13], tristetraprolin [14]), and thus, ourcurrent comprehension of miRNA/RBPs biology in physiological and pathological pro-cesses is strongly limited, as evidenced by the increasing number of contradictory findingsin the literature regarding microRNA’s functions [15,16]. This can be explained by thedifficulty of fully recapitulating this degree of complexity in current preclinical models.In this review, our goal is to describe part of this complex regulatory network in humancancers, with an emphasis on the interplay between the most studied AUBPs (TTP familymembers and HuR) and miRNAs-dependent regulation.
2. MiRNAs: From Biogenesis to a Complex Regulatory Network
MicroRNAs are small endogenous ≈20 nucleotides non-coding sequences promot-ing mRNA decay or translation inhibition through their ability to bind to a specific seedsequence in the 3′UTR of target mRNAs [17–19]. In the canonical model, the perfectcomplementarity between the mRNA and the seed sequence of miRNAs leads to mRNAdecay, while imperfect complementarity is thought to mediate translation inhibition [19].However, this model is not completely understood. MiRNA biogenesis starts with thegeneration of a primary miRNA transcript (pri-miRNA) by RNA polymerase II/III [19].Then, the pri-miRNA is cleaved by the microprocessor complex comprised of the ribonu-clease III enzyme, Drosha and the RBP DGCR8 (DiGeorge Syndrome Critical Region 8),thereby producing a precursor miRNA (pre-miRNA), which is exported to the cytosol viathe Exportin5/RanGTP [19]. In the cytosol, pre-miRNAs are processed by the RNase IIIendonuclease Dicer, which removes the terminal loop, thereby producing a mature miRNAduplex comprised of a guide strand and a complementary passenger strand (miRNA*) [19].Although it was originally thought that only the guide strand is important for targetedgene silencing, it is now clear that depending on the cell type or the context (e.g., inflam-mation, deregulated metabolism), both strands can associate with argonaute proteins andincorporates into the RNA-Induced Silencing Complex (RISC), where it binds to its targetmRNAs [19]. MiRNAs can regulate hundreds of mRNAs, and conversely, one mRNA canbe regulated by multiple miRNAs. Moreover, depending on the cellular or physiologicalcontext (e.g., nutrients deprivation, hypoxia, treatment with anti-tumor agents), miRNAsmay exert different functions and regulate different targets. Finally, miRNAs are subjectedto sequence editing during processing (e.g., A-to-I), which strongly alters their bindingproperties and the choice of the strand incorporated into the RISC [20,21]. Considering thiscomplexity, the current models and approaches to study miRNA-dependent regulation ap-pear quite simplistic. Another layer of complexity comes from other trans-acting factors thatcontrol the fate of mRNAs and interfere with miRNA-dependent regulation or are regulatedby miRNAs. This includes lncRNAs but also RBPs, such as AUBPs, which can compete withthe same binding sites with miRNAs, cooperate with miRNAs or act as “sponges” to se-quester miRNAs, thereby preventing their binding to their target mRNA [22,23]. Whether amiRNA is active or not, therefore, depends on the availability of the seed sequence on targetmRNA and the bioavailability of miRNAs in each system. However, for most studies, onlymiRNAs with the most deregulated expression are considered in the pathophysiology ofhuman diseases. This choice is potentially wrong, given that the deregulated expression ofmRNAs does not always translate into a deregulated activity [24,25]. Finally, the complexityof such a regulatory network is further enhanced by the ability of several miRNAs to control
Cancers 2022, 14, 3516 3 of 30
the expression of AUBPs. Deciphering this complex regulatory network is therefore crucialfor identifying bioavailable and active miRNAs involved in physiological and pathologicalprocesses. Emerging databases (e.g., SIMIRA) can provide some help in predicting thecommon targets between RBPs and miRNAs (http://vsicb-simira.helmholtz-muenchen.de,accessed on 1 June 2022). Immunoprecipitation assays of RBPs coupled with RNAseq arealso highly relevant for identifying all non-coding RNAs bound to RBPs [26–28]. Thesedata are publicly available in specific databases (http://clipdb.ncrnalab.org, accessed on1 June 2022; http://rbpdb.ccbr.utoronto.ca/, accessed on 1 June 2022). Finally, the com-plexity of this regulatory network should be better represented in the in vitro and in vivomodels. Developing models that consider the interplay between miRNAs and these othertrans-acting factors represents a relevant approach to fully characterize the role of thesepost-transcriptional regulators and uncover novel and efficient therapeutic approaches.
3. AUBPs Interfering with miRNAs-Dependent Regulation
AUBPs represent a family of RBPs controlling gene expression at the post-transcriptionallevel [9,29]. These proteins have a high affinity for Adenine and Uridine-rich elements(ARE: e.g., AUUUA pentamer) within the 3′UTR of several immediate-early responsegenes (which represent about 5–8% of the human transcriptome) and mediate their decayand/or impair their translation through processes involving their recruitment into smallcytoplasmic compartments, namely, Stress Granules (SGs) or processing-bodies (P-bodies),respectively [9,29]. More than 20 different AUBPs have been identified and display vary-ing expression patterns depending on the tissue type or the physiological context (e.g.,inflammation, hypoxia, chemotherapy) [9]. While some AUBPs promote mRNA decay(e.g., tristetraprolin family members:), others are mostly stabilizing their target mRNAs(e.g., Human Antigen R, HuR) and/or blocking their translation (e.g., T-cell Intracellu-lar Antigen-1, TIA1) [9,29–32]. However, emerging studies showing opposite functionscurrently challenge this very strict and dogmatic view. The activity and subcellular local-ization of these proteins are regulated by various post-translational modifications (e.g.,phosphorylation, methylation), depending on the cellular context (e.g., mitosis, endoplas-mic reticulum, and oxidative stress) [33–35]. Alteration of AUBPs expression/activitycontributes to deregulated expression patterns of genes involved in inflammatory (e.g.,PTGS2, TNFA) [31,36,37], metabolic (e.g., FGF21, PTEN) [38,39] and carcinogenic processes(oncogenes/tumor suppressors, e.g., MYC, P53) [40,41] and thus contributes to the devel-opment of a wide range of chronic metabolic/inflammatory diseases and cancers [9,29].Importantly, these proteins can also compete with each other for the same mRNA targets(e.g., HuR and TTP for COX-2) [30], and increasing evidence indicates that these proteinscan regulate gene expression by interfering with miRNA-dependent regulation [42,43].Herein, we discuss these complex interactions and their role in cancer development, withan emphasis on HuR and TTP family members. The different connections between HuR,TTP family members and miRNA-dependent regulation of gene expression are discussedbelow and are summarized in Figures 1 and 2.
Cancers 2022, 14, 3516 4 of 30Cancers 2022, 14, x 4 of 31
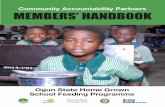
Figure 1. Antagonisms between HuR and microRNA-dependent regulation. HuR can interfere with miRNA-dependent regulation by different mechanisms: (i) HuR and miRNAs can compete for the binding to mRNAs due to overlapping binding sites; (ii) HuR, in concert with lncRNAs, can indi-rectly compete with miRNAs; (iii) HuR can directly sequester or inhibit miRNA expression; (iv) HuR can inhibit miRNA maturation (i.e., miR-199a); (v) HuR can promote lncRNA-dependent miRNA sponging. ONCO: Oncogenes; TS: Tumor Suppressor.
Figure 1. Antagonisms between HuR and microRNA-dependent regulation. HuR can interfere withmiRNA-dependent regulation by different mechanisms: (i) HuR and miRNAs can compete for thebinding to mRNAs due to overlapping binding sites; (ii) HuR, in concert with lncRNAs, can indirectlycompete with miRNAs; (iii) HuR can directly sequester or inhibit miRNA expression; (iv) HuRcan inhibit miRNA maturation (i.e., miR-199a); (v) HuR can promote lncRNA-dependent miRNAsponging. ONCO: Oncogenes; TS: Tumor Suppressor.
Cancers 2022, 14, 3516 5 of 30Cancers 2022, 14, x 5 of 31
Figure 2. Cooperation between HuR, TTP and microRNA-dependent regulation. (A) HuR can co-operate with miRNAs by directly interacting with miRNAs and favoring their binding to their target mRNAs. This effect can also require the binding of circRNA (e.g., circ_CCNB1). HuR promotes exo-some-dependent miR-1246 secretion. HuR can stabilize JUNB mRNAs, thereby favoring its overex-pression, which in turn promotes miR-494 expression. (B) Finally, TTP can promote let-7 expression, which, in turn, decreases its mRNA targets (e.g., CDC34).
3.1. HuR HuR (encoded by ELAVL1: Embryonic-Lethal Abnormal Vision in Drosophila) is ubiqui-
tously expressed AUBPs, which possess two tandems RNA-Recognition motif (RRM), and a hinge region followed by a third RRM [44,45]. The hinge region is subjected to various post-translational modifications (e.g., phosphorylations, methylation) and is mostly in-volved in the nucleo-cytoplasmic shuttling of HuR [46,47]. In the cytosol, HuR exerts its mRNA stabilizing function by targeting ARE and competing or displacing other destabi-lizing factors (e.g., miRNAs, TTP family members) with overlapping binding sites [48]. Finally, HuR can also sequester or potentiate miRNA functions [42]. HuR expression is frequently upregulated in human cancers and plays a compelling role in carcinogenic pro-cesses [44,45]. HuR has mostly been associated with tumor-promoting functions due to its ability to stabilize a whole set of oncogenic and pro-inflammatory transcripts (e.g., COX-2) [49]. However, increasing evidence indicates that HuR can interfere with miRNA-de-pendent regulation [42] and can exert tumor suppressive functions. Understanding the
Figure 2. Cooperation between HuR, TTP and microRNA-dependent regulation. (A) HuR cancooperate with miRNAs by directly interacting with miRNAs and favoring their binding to theirtarget mRNAs. This effect can also require the binding of circRNA (e.g., circ_CCNB1). HuR promotesexosome-dependent miR-1246 secretion. HuR can stabilize JUNB mRNAs, thereby favoring itsoverexpression, which in turn promotes miR-494 expression. (B) Finally, TTP can promote let-7expression, which, in turn, decreases its mRNA targets (e.g., CDC34).
3.1. HuR
HuR (encoded by ELAVL1: Embryonic-Lethal Abnormal Vision in Drosophila) is ubiq-uitously expressed AUBPs, which possess two tandems RNA-Recognition motif (RRM),and a hinge region followed by a third RRM [44,45]. The hinge region is subjected tovarious post-translational modifications (e.g., phosphorylations, methylation) and is mostlyinvolved in the nucleo-cytoplasmic shuttling of HuR [46,47]. In the cytosol, HuR exertsits mRNA stabilizing function by targeting ARE and competing or displacing other desta-bilizing factors (e.g., miRNAs, TTP family members) with overlapping binding sites [48].Finally, HuR can also sequester or potentiate miRNA functions [42]. HuR expression isfrequently upregulated in human cancers and plays a compelling role in carcinogenicprocesses [44,45]. HuR has mostly been associated with tumor-promoting functions dueto its ability to stabilize a whole set of oncogenic and pro-inflammatory transcripts (e.g.,COX-2) [49]. However, increasing evidence indicates that HuR can interfere with miRNA-
Cancers 2022, 14, 3516 6 of 30
dependent regulation [42] and can exert tumor suppressive functions. Understanding themolecular traits associated with HuR’s functions is, therefore, determinant prior to anytherapeutic intervention, as suggested by HuR inhibitors (e.g., MS-444, DHTS, KH-3) inseveral cancers [50–52].
3.1.1. Competitive Antagonism between HuR and miRNAs
HuR-miR-21: MiR-21 is a well-known miRNA frequently upregulated in human can-cers and associated with pro-tumorigenic functions and a poor clinical outcome in pa-tients [53–55]. Increasing evidence indicates that HuR can prevent the miR-21-dependentfunction. Indeed, the RBP, lupus antigen (La), together with HuR, binds to the 3′UTR ofPDCD4 (Programmed Cell Death Protein 4), a tumor suppressor, to prevent the binding ofmiR-21 [56]. Although HuR is mostly considered a tumor-promoting factor, these findingssuggest a tumor suppressive role of HuR. The tumor-promoting properties of miR-21 haveessentially been uncovered in vitro in transformed cancerous cell lines [53]. However,our previous study demonstrated for the first time that, in contrast to in vitro findings,miR-21 could also exert tumor suppressive properties [57]. Therefore, these data suggesta context-dependent function of HuR and miR-21. In agreement, the binding of HuR toPDCD4 mRNA is prevented in oxidative stress conditions (H2O2) due to the phosphory-lation of HuR by ERK8 (Extracellular Signal Regulated Kinase 8), as evidenced in Helacells [58]. Taken together, these data suggest cautions regarding the dogmatic statement ofmiR-21 functions in cancer cells, based on the miRNA expression only, without consideringits activity. A better characterization of this interplay is therefore required prior to thedevelopment of any therapeutic approaches aiming at targeting miR-21 or HuR in cancers.
HuR-miR-26a/b. In breast cancer, the resistance to tamoxifen treatment is associatedwith a competition between HuR and miR-26a/b, which regulates Erb-B2 receptor tyrosinekinase 2 (ERBB2) [59]. Indeed, in tamoxifen-resistant (TAMR) estrogen receptor-positive(ER+) breast cancer cells, HuR stabilizes ERBB2 mRNA, while miR-26a/b [59] inhibits itstranslation. Accordingly, overexpression of miR-26a/b or HuR silencing can restore thesensitivity of cancer cells to tamoxifen.
HuR-miR-34b-5p. In colon cancer cells (SW620, HT29, HCT116, LoVo and RKO cells),HuR binds and stabilizes the lncRNA OIP5-AS1 (OIP5 Antisense RNA 1) [60]. MiR-34b-5pcompetes with HuR for the binding to OIP5-AS1. Moreover, miR-34b-5p directly inhibitsthe expression of HuR. Accordingly, in CRC (colorectal cancer) patients, both OIP5-AS1and HuR expressions are elevated as compared to matched non-tumoral tissues. Thisinterplay importantly promotes carcinogenesis because of the ability of OIP5-AS to triggerthe PI3K/AKT pathway.
HuR-OIP5-AS1 and miR-424. As described previously in colon cancer, HuR stabilizesthe lncRNA OIP5-AS1 in human cervical cancer cells (Hela cell line). Moreover, OIP5-AS1 acts as a decoy to prevent the binding of HuR on mRNA targets, thereby reducingcancer cell proliferation. In contrast, miR-424 competes with HuR and downregulatesOIP5-AS1 expression [61].
HuR-miR-16. In breast cancer cells, the regulation of cyclin E1 mRNA (CCNE1) de-pends on the interplay between HuR and miR-16 [62]. Indeed, in a luciferase-reporterconstruct, HuR blocks the binding of miR-16 on the 3′UTR of CCNE1 in MCF-7 cells. Whilethis effect was not observed with the endogenous CCNE1 transcript, miR-16 was able toprevent the HuR-dependent CCNE1 stabilization. Together, these findings highlight theimportance of this interplay during cell cycle progression.
HuR-miR-194/miR-206. Nucleolin (NCL) is overexpressed in several malignancies andpromotes cancer cell proliferation [63]. This overexpression of NCL is mediated by theelevated expression of HuR and the downregulation of miR-194 and miR-206, whichcompetitively bind to NCL 3′UTR, as evidenced in MCF-7 and MDA-231 cells (breastcancer cells) [64].
HuR-OSER1-AS1-miR-17-5p. OSER1-AS1 is a lncRNA with tumor suppressive proper-ties in Non-Small Cell Lung Cancer (NSCLC). In agreement, the loss of its expression in
Cancers 2022, 14, 3516 7 of 30
tumor from patients correlates with a poor clinical outcome. In the H1299 cell line, OSER1-AS1 binds to HuR and acts as a decoy to prevent HuR from stabilizing its mRNA target. Onthe other hand, miR-17-5p competes with HuR to bind and downregulate OSER1-AS1 [65].
HuR-miR-548c-3p. Topoisomerase II alpha (TOP2A) is a key enzyme involved incell proliferation, which is frequently overexpressed in cancers of different origins andinfluences the efficiency of the chemotherapeutic agent (e.g., doxorubicin) [66–68]. Recently,it has been suggested that the expression of TOP2A is regulated by HuR and miR-548c-3p,which competes for the binding to TOP2A 3′UTR [69]. Indeed, in Hela cells, HuR bindsdirectly to mRNA (TOP2A) and increases its translation [69], while miR-548c-3p reducesTOP2A protein expression.
HuR-miR-195. Stromal interaction molecule 1 (STIM1) is a key regulator of store oper-ated Ca2+ entry (SOCE), a process involved in cancer cell migration/invasion [70]. HuRpromotes STIM1 mRNA stabilization [71]. In contrast, miR-195 competes with HuR anddecreases its expression, as evidenced in IEC-6 cells (normal rat intestinal crypt cells) [71].
HuR-miR-133b. In gastric cancer (GC) tissue and cell lines (BGC-823, MKN-45, MGC-803, SGC-7901, and AGS), HuR expression is high and promotes cancer cell proliferationand migration in vitro and in vivo [72]. This effect is mediated by the ability of HuR todecrease miR-133b expression, which exerts a tumor suppressive function in GC cells.Furthermore, HuR stabilizes CDC5L (cell division cycle 5-like protein) mRNA, while miR-133b inhibits its expression. Therefore, the overexpression of CDC5L, which promotes cellcycle progression, results from the overexpression of HuR and the loss of miR-133b inGC cells [72].
HuR-miR-4319. Semaphorin 4D (SEMA4D) is overexpressed in esophageal squamouscell carcinoma (ESCC) cells and contributes to cancer progression [73]. A competitionbetween HuR and miR-4319 for the binding to SEMA4D mRNA has been demonstratedin ESCC cells (KYSE-150, TE-10 and TE-1). While HuR stabilizes SEMA4D mRNA andcontributes to cell proliferation and migration in ESCC, miR-4319 overexpression destabi-lizes SEMA4D mRNA and prevents ESCC progression [73]. Interestingly, the expression ofmiR-4319 is low in ESCC cells [74], while HuR is overexpressed [75], thus indicating thatSEMA4D overexpression in ESCC is mediated by this double hit.
HuR-miR-300. In gastric cancer, the expression of UBE2C (Ubiquitin ConjugatingEnzyme E2 C), a potent tumor promoter [76], is under the regulation of HuR, whichstabilizes its mRNA by preventing the binding of miR-300 [77].
HuR-miR-494. Nucleolin (NCL), an RBP promoting cancer cell proliferation, is regu-lated at the post-transcriptional level by HuR and miR-494 [78]. Indeed, in Hela cells, HuRinteracts with NCL and promotes its translation. In contrast, miR-494 competes with HuRand represses NCL expression [78].
HuR-miR-4458. MiR-4458 is downregulated in melanoma, thus contributing to theoverexpression of the pro-tumorigenic factor PBX3 (Pre-B-Cell Leukemia TranscriptionFactor 3) [79]. In contrast, HuR, which is overexpressed in melanoma, stabilizes PBX3mRNA by competing with miR-4458 [80].
HuR-miR-4312. In pancreatic ductal adenocarcinoma (PDAC), the overexpression ofBcl-2 associated athanogene 3 (BAG3) promotes IL-8 mRNA stability by promoting HuRbinding to the 3′UTR [81]. The binding of HuR prevents the binding of miR-4312 and thusthe downstream inhibition of IL-8 translation [81].
HuR-miR-184. In chronic myelogenous leukemia (CML), HuR and miR-184 com-pete for the binding to MDR1 (Multidrug Resistance Protein 1) 3′UTR and thus playa major role in chemosensitivity [82]. In Adriamycin-resistant CML cells (K562), theinduction of the lncRNA FENDRR (FOXF1 Adjacent Non-Coding Developmental Reg-ulatory RNA) promotes miR-184 sponging, thereby favoring HuR-dependent MDR1mRNA stabilization [82].
HuR-miR-675-5p. HuR importantly contributes to cancer cell survival and aggressive-ness during hypoxia by stabilizing HIF1A (Hypoxia Inducible Factor 1 Subunit Alpha)mRNA, as evidenced in glioma cells (U51). In contrast, miR-675-5p competes with HuR
Cancers 2022, 14, 3516 8 of 30
for the binding to HIF1A expression and promotes its downregulation [83]. These findingshighlight an important mechanism involved in glioma progression.
HuR-miR-320a. This interplay importantly regulates the DNA damage response bycontrolling the expression of NONO, a RBP involved in the S phase checkpoint of the cellcycle [84]. In Hela cells, ultra-violet (UV) irradiation increases miR-320 expression in ap53-dependent manner [84] but fails to downregulate NONO expression due to the induc-tion of HuR, which stabilizes NONO mRNA by competing with miR-320a. Accordingly,HuR inhibition destabilizes NONO mRNA, and the concomitant silencing of miR-320arestores NONO expression. These findings suggest that HuR represent an important bar-rier against the DNA damage response in cancer cells, which may represent an appealingtherapeutic target.
HuR-miR-124-3p. In ovarian cancer, HuR overexpression contributes to increasedstability of NEAT1 (Nuclear Enriched Abundant Transcript 1), a lncRNA promoting cancercell proliferation and invasion [85]. In contrast, NEAT1 expression is suppressed by miR-124-3p [85]. However, it is unclear in this study whether HuR and miR-124-3p compete forthe same binding sites. Nevertheless, it is likely that the overexpression of NEAT1 in cancercells is a consequence of both HuR overexpression and miR-124-3p silencing.
HuR-miR-125b. HuR binds to adjacent binding sites of miR-125b in the 3′UTR of P53mRNA in MCF7 human breast carcinoma cells [86]. Upon ultraviolet C (UVC) exposure,HuR translocates from the nucleus to the cytosol, where it binds to P53 mRNA, thuspreventing miR-125b-mediated translation inhibition of P53. This interplay is, therefore,important for the DNA damage response [86].
HuR-miR-200b. In bone marrow-derived macrophages (BMDMs) derived from myeloid-specific HuR KO mice, miR-200b expression is increased, and a computational analysishas revealed that miR-200b binding sites overlap with HuR binding sites on several tran-scripts [87]. Among them, HuR stabilizes VEGFA (Vascular Endothelial Growth Factor A)mRNA by preventing miR-200b binding. These findings demonstrate the importance ofthis competition in angiogenesis.
HuR-Ptn-dt-miR-96. Ptn-dt is an oncofetal lncRNA promoting hepatic carcinogenesis [88].HuR, which is overexpressed in HCC, interacts and stabilizes Ptn-dt. Moreover, HuR directlyinteracts with miR-96, thereby preventing its negative effect on Ptn-dt expression [88].
HuR-miR-331-3p. In prostate cancer cells (LNCaP), HuR binds directly to the 3′UTR ofERBB2 and stabilizes it [89], while miR-331-3p exerts an opposite function. Interestingly,HuR reduces the activity of miR-331-3p without preventing the binding of miR-331-3p onits specific site [89].
HuR-other miRNAs. A miRNA-binding site mapping in wild-type and HuR knockoutmacrophages indicate that HuR binding sites overlap with other miRNAs (i.e., miR-27) [90].Moreover, a transcriptome-wide analysis has allowed identifying 788 HuR bound 3′UTRamong the 2653 AGO2 bound 3′UTR [91]. Finally, other mechanisms have been describedin chronic disorders fostering carcinogenesis, such as the competition between HuR andmiR-30e for the regulation of sphingosine 1-phosphate receptor 3 (S1PR3) during liverfibrosis [92]. A potential interplay between HuR, miR-873 and miR-125a-3p has also beensuggested for the regulation of cancer stemness through the regulation of CDK3 (Cyclin De-pendent Kinase 3) expression in lung cancer [93]. However, the nature of this interplay wasnot fully depicted in this study. Finally, HuR may also affect the activity of other miRNAsthrough its ability to inhibit AGO2. Indeed, the circular RNA (circAGO2) generated fromthe AGO2 gene can bind to HuR protein and facilitate its translocation to the cytoplasm,thereby promoting its binding to the 3′UTR of several transcripts (i.e., EIF4EBP3, HNF4A,MAP4K1, NOTCH4, SLC2A4, and SLC44A4) and reducing AGO2/miRNA-dependent regu-lation (miR-224-5p, miR-143-3p, miR-181a-5p, miR-503-5p, or miR-125a-3p) [94]. CircAGO2is overexpressed in various cancers, where it correlates with a poor prognosis and promotestumorigenesis and aggressiveness [95]. Therefore, the circAGO2/HuR interplay representsa major oncogenic axis that should be considered in other malignancies.
Cancers 2022, 14, 3516 9 of 30
3.1.2. Other Antagonisms between HuR and miRNAs
HuR-miR-21: In addition to the competition between HuR and miR-21 for PDCD4binding, HuR directly binds and sequesters miR-21, as evidenced in MCF7 cells, therebypreventing the downregulation of miR-21 targets (i.e., PDCD4) [55].
HuR-miR-7. ALKBH5 (AlkB Homolog 5, RNA Demethylase) expression is increasedin ovarian cancer tissues and cells (A2780, SKOV3 cell lines), where it contributes to cancercell proliferation, migration, and autophagy [96]. Mechanistically, ALKBH5 increases HuRexpression, which in turn downregulates miR-7 expression. MiR-7 directly targets theexpression of EGFR (Epidermal Growth Factor Receptor) in SKOV3 cells [96]. Accordingly,ALKBH5 promotes EGFR expression by promoting HuR-dependent inhibition of miR-7.
HuR-miR-16. In colorectal cancer, cyclooxygenase 2 (COX-2), a major enzyme of in-flammation, is frequently overexpressed and promotes various cancerous hallmarks [97].This overexpression is due to the ability of HuR to directly bind and stabilize its mRNAtranscript. In addition, HuR binds directly and sequesters miR-16, which directly inhibitsCOX-2, expression [98].
HuR-miR-107: In non-small cell lung cancer cells (NSCLC, A549, H1299, Calu6 andH520) ALKBH5 (AlkB homolog 5), inhibits Hippo/YAP signaling and reduces cancer cellproliferation, migration, and invasion [99]. This effect is partially promoted by an increasedexpression of HuR, which in turn prevents miR-107-dependent downregulation of LATS2(Large Tumor Suppressor Kinase 2) [99,100]. In this study, HuR binds directly to miR-107and acts as a miRNA sponge. These findings suggest a tumor suppressive function of HuR.
HuR-UFC1-miR-34a. UFC1 is a lincRNA overexpressed in HCC [101] and acts as atumor promoter by favoring cancer cell proliferation, inhibiting apoptosis in vitro andin vivo. This effect is partially attributed to its ability to increase β-catenin expressionby interacting with HuR. In contrast, miR-34a is a negative regulator of UFC1 and thusprevents the induction of β-catenin in cancer cells [101].
HuR-BBOX1-AS1- miR-361-3p. The lncRNA BBOX1-AS1 (BBOX1 antisense RNA 1) isoverexpressed in cervical cancer, where it promotes cancer progression and metastasisformation by increasing HOXC6 (homeobox C6) expression [102]. This effect has beenassociated with the capacity of BBOX-AS1 to sponge miR-361-3p, a direct negative regulatorof HOXC6 expression [102]. In addition, HuR binds and stabilizes BBOX-AS1, therebypromoting the downstream inhibition of miR-361-3p. In addition, HuR binds directly andstabilizes HOXC6. Together, these findings indicate that the regulation of HOXC6 is HuRand miR-361-3p-dependent, but this interplay is indirect through BBOX1-AS1 [102].
HuR-LINC00336-miR6852. LINC00336 is upregulated in lung cancer and promotescancer-related processes by acting as a competing endogenous RNA (ceRNA) on miR-6852 [103]. This miRNA is an important regulator of cystathionine-β-synthase (CBS)expression, an inhibitor of ferroptosis [103]. HuR, which is overexpressed in lung cancer,binds to LINC00336 and stabilizes it, thus inhibiting miR-6852 and favoring CBS expression.Accordingly, miR-6852 overexpression reduces cancer cell proliferation (A549 cells) andsurvival by inducing ferroptosis.
HuR-LncRNA-HGBC-miR-502-3p. In gallbladder carcinoma, the long-non-coding RNAHGBC is upregulated and is associated with poor survival in patients [104]. This lncRNAimportantly promotes tumorigenic processes (e.g., cancer cell proliferation, migration) [104].HuR binds and stabilizes HGBC RNA and thus contributes to its overexpression. Mecha-nistically, HGBC is a miRNA sponge that directly binds to miR-503-3p, thereby preventingthe downregulation of its target mRNAs, including SET (SET Nuclear Proto-Oncogene), anupstream regulator of AKT (Protein Kinase B) signaling [104].
HuR-circ-CCND1-miR-646. In laryngeal squamous carcinoma, circ-CCND1 importantlypromotes cancer-related processes by sponging miR-646, which inhibits CCND1 (cyclinD1) expression [105]. In parallel, circ-CCND1 interacts with HuR to stabilize CCND1mRNA [105]. However, these two mechanisms seem to act independently of each other,and thus the overexpression of CCND1 is more a consequence of a coordinated effect ofHuR and miR-646 rather than an interplay between them.
Cancers 2022, 14, 3516 10 of 30
HuR-CircPVT1-miR-30d/e. In lung squamous cell carcinoma (LUSC), circPVT1 is upreg-ulated and correlates with a poor clinical outcome. As demonstrated in LUSC cells (A549,H520, H226, SKMES-1, and H1270), circPVT1 acts as a ceRNA, which inhibits miR-30d,thereby promoting the expression of cyclin F, a direct target of miR-30d and miR-30e. HuRstabilizes circPVT1 and thus indirectly contributes to the inhibition of these miRNAs [106].
HuR-circ-FAT3-miR-136-5p. In lung cancer cells, HuR promotes the cyclization andgeneration of a circular RNA, circ-FAT3 [107], involved in various cancer-related pro-cesses. Circ-FAT3 act as a ceRNA (competing endogenous RNA) to sponge miR-136-5p,thereby increasing the expression of its mRNA targets, including HuR [107], thus forming aregulatory loop.
HuR-miR-199a. HuR is an important regulator of miR-199a maturation [108] in hepato-cellular carcinoma in hypoxic conditions. Hypoxia induces HuR expression and promotesits binding to the primary miR-199a (pri-miR-199a), thereby inhibiting its maturation. Dueto the ability of miR-199a to regulate hexokinase-2 (HK2) and pyruvate kinase-M2 (PKM2),this interplay strongly contributes to the metabolic switch of HCC cells toward glycolysisduring hypoxia [108].
HuR-TTN-AS-1 and miR-133b. The lncRNA TTN-AS1 promotes cell proliferation andinhibits apoptosis in esophageal squamous cell carcinoma (KYSE410 cell line) [109]. Mecha-nistically, this effect is associated with its ability to sponge miR-133b, thereby preventingthe downregulation of the mRNA targets of this miRNA (e.g., FSCN1, SNAIL, N-cadherin,Vimentin). Moreover, TTN-AS1 recruits HuR, which, in turn, stabilizes FSCN1 (FascinActin-Bundling Protein 1) and promotes epithelial–mesenchymal transition. Finally, HuRdirectly reduces miR-133b expression through a poorly characterized mechanism [109].
HuR-circ_0036412-miR-579-3p. In hepatocellular carcinoma, the circular RNA circ_0036412increases GLI2 (GLI Family Zinc Finger 2) expression, which promotes the Hedgehog pathwayand cancer cell proliferation [110]. Mechanistically, circ_0036412 sponges miR-579-3p toprevent GLI2 downregulation and recruits HuR to stabilize GLI2 transcript, as evidenced inHCC cells (Huh-7 and Hep3B cell lines) [110].
HuR-HOTAIR and miR-7. In Neck Squamous Cell Carcinoma, the lncRNA Homeobox(HOX) transcript antisense RNA (HOTAIR) is overexpressed, and this effect is partiallymediated by HuR, which directly binds and stabilizes HOTAIR [111]. HOTAIR acts asa miRNA sponge on miR-7 to promote cancer cell (CC25 and FaDu cells) proliferation,migration, and invasion.
HuR-H19 and miR-675. HuR interacts directly with the lncRNA H19 in the placentaand prevents its processing for the biogenesis of miR-675 [112]. This inhibitory effect occursduring the processing by drosha [112]. However, it is unclear whether this link exists inhuman cancers. Moreover, depending on the cancer type, miR-675 expression is reduced oroverexpressed and displays both oncogenic (e.g., Non-Small Cell lung cancer, [113] andtumor-suppressive properties (e.g., prostate cancer, [114]). In contrast, H19 is upregulatedand promotes cancer progression. Therefore, the induction of HuR, frequently observed inhuman cancer, may inhibit miR-675 expression in cancer cells. However, this link remainsto be determined.
3.1.3. Cooperation between HuR and miRNAs
HuR-let-7. HuR can potentiate the effect of some miRNAs, as exemplified by let-7,which binds to the 3′UTR of c-Myc more efficiently when HuR binds to a proximal AREsite [115,116]. This interplay promotes a translational repression of c-Myc due to the abilityof HuR to promote the interaction between AGO2/let-7b/c with c-Myc mRNA. Giventhe oncogenic potential of c-Myc [117], this study questions the dogmatic view of HuRas a strict oncogenic/tumor-promoting factor. Interestingly, both the expression of HuRand c-Myc are enhanced in most cancers, while the expression of let-7b and c is frequentlydecreased [118–121]. These findings suggest a decoupling between HuR and Let-7 in cancercells, thereby preventing the ability of HuR to inhibit the translation of oncogenic transcripts(e.g., c-Myc). Re-expressing let-7 expression may, therefore, represent a potent therapeutic
Cancers 2022, 14, 3516 11 of 30
approach by restoring the capacity of HuR to inhibit the translation of several transcripts.The cooperation between HuR and let-7b/RISC, favoring tumor progression, has also beendescribed in HeLa cells. HuR recruits let-7b and both binds to and downregulates lincRNAp21. LincRNA p21 directly binds and prevents the translation of β-catenin and JUNB [122].Therefore, the HuR-let-7b axis favors β-catenin and JUNB protein expression in cancer cells.
HuR-miR-9. In Hodgkin lymphoma, miR-9 directly represses several cytokines, in-cluding IL-6 (interleukin-6), TNFα (tumor necrosis factor-alpha), and CCL-5 (C-C MotifChemokine Ligand 5). Interestingly, the regulation of IL-5 (interleukin-5) and TNFα isHuR-dependent. Indeed, the knockdown of HuR in HEK293T cells increases the expressionof these cytokines, and this effect is prevented by the inhibition of miR-9. Although theunderlying mechanism has not been fully depicted, these data suggest that HuR and miR-9cooperate for the regulation of these cytokines [123].
HuR-miR-19a and b. MiRNAs bind to their targets through a specific base pairingbetween their seed sequence and the target mRNAs [17–19]. However, increasing evidenceindicates a non-canonical mechanism of miRNAs binding, which is mediated by HuR.More precisely, in breast cancer cells, ABCB1 (P-glycoprotein), a multidrug resistanceprotein, is regulated by miR-19b despite the absence of miR-19b binding sites within the3′UTR of ABCB1 mRNA [124]. The binding of miR-19 is mediated by HuR [124], thussuggesting that this cooperation importantly controls the chemosensitivity of cancer cells.Interestingly, HuR is also important for miR-19-dependent regulation of Ras homolog B(RhoB) in keratinocytes upon UV exposure [125]. Finally, in papillary thyroid cancer cells(BCAP) and HEK-293T cells, HuR overexpression promotes miR-19a synthesis, while itssilencing reduces miR-19a levels [126]. This effect is mediated by the binding of HuR to pre-miR-19a, thereby increasing its stability and favoring its maturation. These findings furtherindicate that HuR is not only an mRNA stabilizing factor. Interestingly, this study suggeststhat the HuR-miR-19a/b axis promotes cancer cell proliferation. However, miR-19a targetsRas-related RAP-IB (RAP1B), a GTPase member of the Ras-associated protein family (RAS),which is overexpressed in BCAP and promotes cancer cell proliferation, migration, andinvasion [127]. Further investigations are, therefore, required to fully characterize theimportance of the HuR/miR-19a axis in carcinogenesis.
HuR-miR-1246. In gastric cancer cells (AGS cells), HuR binds to an ARE present onmiR-1246 and promotes its secretion in the exosome [128]. Although the underlyingmechanism is still unclear, exsosomal miR-1246 is frequently observed in the serum ofpatients with GC and may contribute to various cancerous processes [129–131].
HuR-miR-200a. MiR-200a and HuR cooperate to stabilize c-Jun mRNA, as evidencedin HEK293T cells [132]. This study challenges again the dogmatic view of miRNAs asstrict gene expression repressors and indicates that this mechanism can contribute to theoverexpression of important oncogenes.
HuR-miR-200c. In ovarian cancer, the role of miR200c depends on the localization ofHuR. Indeed, when HuR is in the nucleus, miR200c acts as a tumor suppressor by inhibitingthe expression of TUBB3 (class III β-tubulin) mRNA. In contrast, when HuR localizes inthe cytoplasm, miR200c binds to HuR and acts in concert to stabilize TUBB3 mRNA, thuspromoting carcinogenesis [133]. Together, these data further indicate that HuR exerts adual function depending on the context, which influences HuR localization.
HuR-miR-494. In muscle invasive bladder cancer (MIBC) cells (T24T), the anti-cancerouscompound ChlA-F, a novel C8 fluoride derivative of cheliensisin A, increases JUNB mRNAstability in a HuR-dependent manner [134]. Then, Jun-B promotes miR-494 expression,which, in turn, directly binds and decreases c-Myc mRNA [134].
HuR-circular RNAs. Increasing evidence indicates an interplay between HuR andlncRNAs, which is not limited to their ability to sponge miRNAs. The circZNF609 RNAinteracts with HuR to stabilize CKAP5 (Cytoskeleton Associated Protein 5) mRNA [135],a cytoskeleton/mitosis-associated factor, in RD cells (embryonal rhabdomyosarcoma cellline). Similarly, HuR and AGAP2-AS interact and stabilize CPT1A (Carnitine Palmitoyltrans-ferase 1A) in mesenchymal stem cells, thereby promoting trastuzumab resistance in breast
Cancers 2022, 14, 3516 12 of 30
cancer [136]. CCAT2 (Colon Cancer Associated Transcript 2), a lncRNA, interacts withHuR in the nucleus to promote HCC progression, potentially by regulating the expressionof autophagy-related genes [137]. Finally, HuR interacts with circCCNB1 and miR-516b-5p and cooperates to stabilize cyclin-D1 (CCND1) mRNA in glioma, thereby favoringcancer progression [138].
HuR-RPSAP52-miR-15a, miR-15b, and miR-16. This interplay between HuR, the lncRNARPSAP52 (Ribosomal Protein SA Pseudogene 52) and miRNA-dependent regulation hasbeen associated with the regulation of the cell cycle inhibitor, p21, in colorectal cancer cells(HT-29) [139]. In this study, RPSAP52 directly binds to HuR protein, thereby preventingits ability to stabilize CDKN1A (Cyclin Dependent Kinase Inhibitor 1A) transcript. Inaddition, RPSAP52 shifts the localization of miR-15a, miR-15b and miR-16 from HMGA(High Mobility Group AT-Hook 1) to CDKN1A mRNA. One potential explanation discussedin this study is the change in mRNA conformation, thus allowing better access of miRNAto CDKNA1.
HuR-other miRNAs. Although HuR has mainly been associated with a stabilizingfunction, this dogmatic view is further challenged by other studies showing cooperationbetween HuR and miRNAs in other diseases. For instance, HuR and miR-26 act synergisti-cally to regulate the expression of the negative regulator of G-protein signaling 4 (Rgs4) inneurons [140]. Whether this cooperation exists in human cancers remains to be determined,but these findings suggest that this destabilizing function of HuR is underestimated incancers and may be tissue dependent.
3.2. TTP Family Members (TTP, TIS11, GOS24, NUP475)
TTP is one of the most studied AUBPs, which belongs to the family of Cys-Cys-Cys-His zinc finger proteins [141–143]. This family contains three members, TTP (tristetraprolin,ZFP36), BRF1 (Butyrate response factor 1, ZFP36L1) and BRF2 (Butyrate response factor 2,ZFP36L2) [143]. TTP is rapidly induced by various stimuli, including TGF-β (transforminggrowth factor-beta) [144,145], LPS (lipopolysaccharide) [146], TNFα, or insulin [147,148]and is, therefore, considered as an immediate–early response gene [9]. TTP is one of the best-characterized AUBPs involved in ARE-mediated mRNA decay through a process involvingthe nucleation of small cytoplasmic granules called (P-bodies), where the target mRNAs arebound by various enzymes promoting deadenylation, decapping and degradation [9,149].The importance of TTP in physiological/pathological processes is illustrated by Zfp36knockout mice, which develop a severe inflammatory syndrome and growth retardationdue to the overexpression of pro-inflammatory factors (e.g., TNF-α) [9,150,151]. TTP ismostly considered a tumor suppressor whose expression is lost in tumors. This effect is dueto its ability to control a whole network of oncogenic and pro-inflammatory transcripts [9].However, this concept has recently been challenged in HCC, where TTP plays a potentpro-tumorigenic function in vivo, as evidenced in liver specific TTP KO mice treated with ahepatic carcinogen (i.e., diethylnitrosamine) [152]. The interplay between TTP and miRNA-dependent regulation is poorly known and even less understood in the context of cancer.TTP can cooperate with some miRNAs, such as miR-16, as evidenced in drosophila S2cells [153]. MiR-16 sequence (UAAAUAUU) is complementary to the canonical AREsequence. This cooperation requires the binding of TTP to AGO/EIF2C family members toassist miR-16 binding to ARE on its target [153] mRNAs. Moreover, TTP can also promotethe expression of some miRNAs, as evidenced by let-7, whose expression is increased byectopic overexpression of TTP in various cancer cells (PA1, HCT-116) [154]. This effect leadsto the downregulation of let-7 target genes, such as CDC34 (Cell Division Cycle 34), andreduces cancer cell proliferation [154]. Interestingly, this effect seems to be P53-dependent,as DNA-damaging agents such as doxorubicin trigger P53 activation and induce bothTTP and let-7 expression [155]. These data also indicate that the expression of TTP istightly dependent on the mutational landscape in cancer cells. However, it is currentlyunclear whether the expression of TTP is similarly affected by other mutations. Whether aspecific mutation is associated with a specific post-transcriptional signature remains to be
Cancers 2022, 14, 3516 13 of 30
determined. Both TTP and let-7 are frequently downregulated in human cancers. RestoringTTP expression may, therefore, represent a potential approach to restoring let-7 expressionin cancer cells. Several approaches aiming at restoring TTP expression in cancer cellshave been proposed, such as DNA demethylating agents in hepatocellular carcinoma orhistone deacetylase inhibitors (HDAC) in colorectal cancer and HCC [152,156]. In ovariancancer cells (CaOV-3, SKOV-3, HEYA-8 cell lines), p70S6K (70 S6 kinase) phosphorylatesand inhibits the interaction of TTP with Dicer, thereby reducing the expression of miR-145 [157]. Other studies have also demonstrated that TTP can reduce the expression ofmiRNAs, such as miR-155 in cystic fibrosis [158]. This effect is mediated by the inductionof miR-1, which reduces miR-155 biogenesis in lung epithelial cells. Collectively, thesefindings indicate that TTP can indirectly control the expression of a myriad of transcriptsby controlling the expression of miRNAs. This interplay is currently poorly known forthe other TTP family members, BRF1 and BRF2. In lung cancer, the lncRNA MNX1-AS1promotes cancer progression by interacting with miR-527, thereby preventing miR-527-induced BRF2 downregulation. In this study, BRF2 importantly promotes cancer cellproliferation, migration, and invasion [159].
4. MiRNAs-Regulating HuR and TTP Family Members
Several miRNAs targeting AUBPs have been documented in different cancers. Tar-geting these miRNAs may, therefore, represent a potential therapeutic approach aimingat restoring the “beneficial” AUBPs. In this section, we discuss the miRNAs regulat-ing the expression of the most studied AUBPs, TTP family members and HuR (Table 1and Figure 3).
4.1. HuR
Several miRNAs regulating HuR expression have been identified in human cancers.Although HuR expression is increased in most neoplasms [160], this knowledge is limitedto certain types of cancers and has essentially been demonstrated in vitro using cancercell lines.
Gastric Cancer (GC): HuR expression is increased in GC as compared to normal tissueand contributes to tumor growth and metastasis [161]. This induction of HuR can beattributed to the loss of expression/activity of several miRNAs, including miR-145 [161],miR-519 [162] or miR-582-3p [163]. Interestingly, the activity of miR-582-3p is inhibitedby a circular RNA, circSHKBP1, which is upregulated in GC. These data illustrate wellthe complex regulatory network regulating HuR expression, with various miRNAs andncRNA acting in concert to increase HuR expression. Finally, not only the expression butalso the cytoplasmic localization of HuR is under miRNAs influence in GC. Indeed, GAS5(Growth Arrest Specific 5) directly binds to HuR and promotes its cytoplasmic translocation,thereby stabilizing the FAM83B (Family With Sequence Similarity 83 Member B) transcriptand promoting cancer cell proliferation, migration, and invasion. MiR-140-3p, which isdownregulated in GC patients, directly binds and inhibits the expression of GAS5, and thus,promotes HuR nuclear localization and the downregulation of FAM83B expression [164].
Hepatocellular Carcinoma (HCC). MiR-16 is a potent regulator of cyclooxygenase-2 ex-pression in human hepatoma/HCC cells (Hep3B, WRL68) [165]. This effect is mediatedby two different mechanisms with (i) a direct regulation of COX-2 mRNA by miR-16 and(ii) the ability of miR-16 to downregulate HuR expression, which stabilizes COX-2 mRNA.MiR-16 exerts tumor suppressive properties in vitro and in vivo (xenograft model), and itsexpression inversely correlates with COX-2 level in HCC tissue [165].
Cancers 2022, 14, 3516 14 of 30Cancers 2022, 14, x 14 of 31
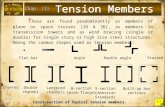
Figure 3. MicroRNAs regulating HuR and TTP family members. (A) miRNAs regulating HuR ex-pression and frequently downregulated in cancers. (B) Predicted and validated miRNAs regulating HuR (miRWalk database: http://mirwalk.umm.uni-heidelberg.de/, accessed on 13 June 2022). (C) miRNAs regulating TTP family members (TTP, BRF1 and BRF2) expression and frequently upreg-ulated in cancers. (D) Predicted and validated miRNAs regulating TTP expression in cancers (miR-Walk database: http://mirwalk.umm.uni-heidelberg.de/, accessed on 13 June 2022).
4.1. HuR Several miRNAs regulating HuR expression have been identified in human cancers.
Although HuR expression is increased in most neoplasms [160], this knowledge is limited to certain types of cancers and has essentially been demonstrated in vitro using cancer cell lines.
Gastric Cancer (GC): HuR expression is increased in GC as compared to normal tissue and contributes to tumor growth and metastasis [161]. This induction of HuR can be at-tributed to the loss of expression/activity of several miRNAs, including miR-145 [161], miR-519 [162] or miR-582-3p [163]. Interestingly, the activity of miR-582-3p is inhibited by a circular RNA, circSHKBP1, which is upregulated in GC. These data illustrate well the complex regulatory network regulating HuR expression, with various miRNAs and ncRNA acting in concert to increase HuR expression. Finally, not only the expression but also the cytoplasmic localization of HuR is under miRNAs influence in GC. Indeed, GAS5 (Growth Arrest Specific 5) directly binds to HuR and promotes its cytoplasmic transloca-tion, thereby stabilizing the FAM83B (Family With Sequence Similarity 83 Member B) transcript and promoting cancer cell proliferation, migration, and invasion. MiR-140-3p, which is downregulated in GC patients, directly binds and inhibits the expression of
Figure 3. MicroRNAs regulating HuR and TTP family members. (A) miRNAs regulating HuRexpression and frequently downregulated in cancers. (B) Predicted and validated miRNAs regulatingHuR (miRWalk database: http://mirwalk.umm.uni-heidelberg.de/, accessed on 13 June 2022).(C) miRNAs regulating TTP family members (TTP, BRF1 and BRF2) expression and frequentlyupregulated in cancers. (D) Predicted and validated miRNAs regulating TTP expression in cancers(miRWalk database: http://mirwalk.umm.uni-heidelberg.de/, accessed on 13 June 2022).
Ovarian cancer. The upregulation of HuR in ovarian cancer is also associated withthe downregulation of miRNAs, such as miR-139-3p, whose loss promotes tumor growthand metastasis of ovarian cancer cells [166]. Moreover, similarly to GC, miR-519 is alsodownregulated in ovary, lung, and kidney cancer, and miR-519 overexpression reducestumor growth by reducing HuR expression [167,168].
Papillary thyroid carcinoma. In this cancer, only miR-31 downregulation has been asso-ciated with HuR overexpression [169]. In thyroid carcinoma, HuR is an important tumorpromoting factor due to its ability to stabilize oncogenic transcripts [170], and thus, a betterunderstanding of the post-transcriptional regulation of HuR is required to envisage noveltherapeutic options.
Non-Small Cell Lung Carcinoma (NSCLC). NSCLC is a leading cause of cancer mortal-ity [171]. As described for ovarian cancer, miR-139-3P downregulation contributes to HuRoverexpression in lung cancer cells [172]. In addition, other miRNAs, including miR-146A-5p [173], miR-31 [174], miR-136-5p [107], or miR-519 [167], have been recognized as directregulators of HuR, which are downregulated/inhibited in tumors.
Colorectal cancer. HuR is upregulated in CRC and this effect has been associated withthe downregulation of various miRNAs, including miR-22 [175], miR-324-5P [176], miR-519 [168,177], miR-155-5p [178] or miR-34b-5p [60]. In addition, HuR overexpression has
Cancers 2022, 14, 3516 15 of 30
been associated with TNFRSF10A-AS1; a lncRNA overexpressed in CRC, which binds andinhibits miR-3121-3p, a direct regulator of HuR [179]. Together, these studies illustratethat HuR upregulation depends on a concerted effect of all these miRNAs, whose activitydepends on lncRNAs.
Cervical cancer. Similarl to CRC, miR-324-5P and miR-519 are potent regulators of HuRexpression in cervical cancer, which are downregulated in tumors and associated withradiotherapy resistance to cancer cells [168,180,181].
Rhabdomyosarcoma (RMS). In RMS cells (Rh30 cells), miR-29 interacts directly withHuR and acts as a decoy to prevent HuR binding to A20 mRNA (TNF Alpha InducedProtein 3), an upstream repressor of NFkB (Nuclear factor kappa B) [182]. In these cells,HuR overexpression leads to A20 downregulation. In RMS and osteosarcoma cells, as wellas in tumor samples from patients (e.g., liposarcoma, RMS, osteosarcoma), the expressionof A20 and miR-29 is low, while HuR is strongly upregulated. The decoy activity of miR-29may reside in the precursor sequence of the miR, which contains putative binding sitesfor HuR. Together, these results provide further evidence that HuR can also function as anRNA-destabilizing factor.
Glioblastoma multiforme: miR-3127-5P is a direct regulator of HuR in glioma [183].Interestingly, this miRNA is sponged by LncRNA gastric cancer-associated transcript 3(GACAT3), which is upregulated in glioma tissues from patients and thus promotes HuRoverexpression [183]. In glioma stem cells (GSCs), [184], miR-146b-5p is also a directregulator of HuR, and its downregulation in glioma promotes HuR expression, which, inturn, negatively regulates the expression of LincRNA-p21, a long intergenic non-coding RNAinvolved in the inhibition of β-catenin expression and nuclear translocation in GSC [184].
Breast cancer: Knockdown of miR-16 in MDA-MB-231 human breast carcinoma in-creases HuR expression [185]. MiR-16 directly interacts with the 3′UTR of HuR [185].Other miRNAs regulating HuR have been identified in breast carcinoma, including miR-125A [186] but also miR-519 [187]. Interestingly, miR-29a can also regulate HuR indirectlythrough its ability to downregulate TTP. Indeed, HuR mRNA contains ARE in its 3′UTR,which are recognized by TTP. Therefore, miR-29a inhibition restores TTP expression, which,in turn, downregulates HuR [188].
Prostate cancer. MiR-133b is a potent regulator of HuR, which is downregulated inprostate cancer cells (PC3, DU-145 cell lines) [189]. Accordingly, overexpression of miR-133b decreases HuR expression through a direct binding to HuR 3′UTR. This negativeimpact on HuR expression induced docetaxel cytotoxicity in prostate cancer cells [190]by reducing the expression of ABCG2 (ATP Binding Cassette Subfamily G Member 2), atransporter involved in chemoresistance. HuR expression is also negatively regulated bymiR-34a in paclitaxel-resistant PC3 cells (PC3PR). The downregulation of HuR by miR-34aleads to a decrease in SIRT1 (Silent mating type information regulation 2 homolog 1) andBcl-2, thereby sensitizing cancer cells to paclitaxel [191].
Nasopharyngeal Carcinoma (NPC). MiR-514-5p is a direct regulator of HuR expressionin NPC cells (CNE1, CNE2, C666–1 and HNE1 cell lines) [192]. Interestingly, the activityof this miRNA is negatively regulated by the lncRNA SNHG7, which is upregulated inNPC cells [192].
Oropharyngeal Squamous Cell Carcinoma (OPSCC). MiR-133a-3p is downregulated inOPSCC smokers, Human Papilloma Virus (HPV) positive cells and in E6/E7 overexpressingHPV negative cells treated with cigarette smoke extract [193]. MiR-133a-3p knockdownleads to an upregulation of HuR [193].
Laryngeal squamous cell carcinoma. MiR-519a is a potent tumor suppressor in laryn-geal squamous cells [194]. This effect is partially mediated by its ability to directly in-hibit HuR expression, as evidenced in laryngeal squamous cell carcinoma human epithe-lial type 2 cells [194]. Interestingly, HuR is also directly regulated by miR-519b-3p inlarynx squamous Hep-2 cells, and the expression of this miRNA is reduced in tumorsfrom patients [195].
Cancers 2022, 14, 3516 16 of 30
Esophageal Squamous Cell Carcinoma (ESCC). In ESCC cells (KYSE410), miR-133b in-hibits HuR expression and prevents FSCN1 (Fascin Actin-Bundling Protein 1) expres-sion and epithelia-mesenchymal transition [109]. In patients, miR-133b loss correlateswith a poor prognosis and contributes to HuR overexpression, which promotes cancercell proliferation.
Hematologic malignancies. MiR-519 regulates HuR expression in HL60 cells (acutemyeloid leukemia, AML) [196]. Overexpression of miR-519 in AML cells reduces can-cer cell proliferation by reducing HuR expression, thus indicating that HuR is not only apro-tumorigenic factor. Other miRNAs have been involved in HuR regulation in AML,including miR-199a-3p [197] and miR-25. However, this latest is an indirect regulatorinvolving the regulation of the NOX4 (NADPH Oxidase 4)/JNK (JUN N-Terminal Kinase)axis involved in HuR phosphorylation and cytoplasmic translocation [198]. In multiplemyeloma cells, miR-16 downregulation correlates with the overexpression of HuR [199].These results have been demonstrated by using a statistical approach (LIMMA method). InT-Large Granular Lymphocyte Leukemia (T-LGLL), miR-146b is a regulator of HuR expres-sion, which is downregulated in a STAT3 (Signal Transducer and Activator of Transcription3)-dependent manner [200]. Finally, in a model of Hodgkin lymphoma (L428, L540 andKM-H2 cell lines), miR-9 directly targets HuR and inhibits its expression [123]. Accord-ingly, the use of miR-9 antagomiR promotes HuR upregulation [123]. In B lymphomacells (RAMOS, Daudi), miR-17-19b binds and reduces MYC expression [201]. This effect isindirectly mediated by the downregulation of checkpoint 2 expression (CHK2), an upstreamregulator of HuR phosphorylation. The decreased HuR phosphorylation promotes HuRbinding to MYC, which reduces its translation [201].
Other potential miRNAs regulating HuR? The number of miRNAs regulating HuR ex-pression is probably underestimated given that several miRNAs have been predictedin several databases (e.g., miRwalk: http://mirwalk.umm.uni-heidelberg.de/: accessedon 13 June 2022) but have not been validated yet (Figure 3B,D). Therefore, it is likelythat the overexpression of HuR in cancers may also result from a concerted effect of allthese miRNAs.
4.2. TTP Family Members4.2.1. Tristetraprolin (ZFP36)
TTP is mostly associated with tumor suppressive properties in human cancers, andaccordingly, its expression is frequently reduced in tumors [143]. Although various mecha-nisms have been described (e.g., promoter methylation, constitutive protein degradation,HDAC-dependent silencing of transcription factors) [156,202], several miRNAs have beeninvolved in its loss. Among them, miR-29a is a direct regulator of TTP, which is upregulatedin breast cancer [188,203]. MiR-29a is also upregulated in pancreatic cancer [204] and pro-motes cancer cell proliferation and migration by directly targeting TTP, thereby increasingthe expression of epithelial-mesenchymal transition (EMT) and inflammatory markers.Whether this link between miR-29a and TTP exists in other cancers remains unclear, but theexpression of this miRNA is frequently increased in human cancers [205], while TTP expres-sion is lost. MiR-182 is another well-known miRNA able to downregulate the expression ofTTP in cancers, which is frequently overexpressed in tumors [206]. Interestingly, this miR-182/ZFP36 axis is also regulated by the circular RNA_00054 (circRNA_00054), which acts asa miRNA sponge against miR-182 [206]. Accordingly, overexpression of circRNA_00054 inbreast cancer cells reduces miR-182 bioavailability, restores TTP expression and promotescancer cell growth, invasion, and migration in vitro and in vivo. MiR-128a, which is upreg-ulated in Acute Myeloid Leukemia (AML), is also a potential regulator of TTP expression,as demonstrated in AML cells (OCI-AML3 and APL/AML cells), where its knockdownstrongly triggers TTP expression [207]. However, it is unclear in this study whether thiseffect is direct or not. In hepatocellular carcinoma, miR-9-5p is a direct inhibitor of TTPexpression [208]. Interestingly, the transfer of exosomal SENP3-EIF4A1 inhibits tumorgrowth in vivo by sequestering miR-9-5p, thereby increasing TTP expression [208]. Finally,
Cancers 2022, 14, 3516 17 of 30
miR-200c was also identified as a direct regulator of TTP expression in mouse breast cancercells (4TO7) [209].
Together, these findings strongly suggest that TTP loss is promoted by the concertedimpact of several miRNAs on TTP mRNA. Like for HuR, the number of miRNAs regulatingTTP expression is probably underestimated given that many other miRNAs are predictedto target ZFP36 mRNA but have not been validated yet (Figure 3B, D).
4.2.2. Butyrate Response Factor 1 (ZFP36L1)
In contrast to HuR and TTP, very few miRNAs involved in ZFP36L1 regulation havebeen identified. Among them, miR-93-3P is strongly increased during wound healingin mice and contributes to keratinocyte proliferation by targeting ZFP36L1 mRNA. [210].In glioblastoma multiforme (GBM) cells, overexpression of miR-129-5p reduces ZFP36L1expression and impairs cancer cell proliferation, migration, and invasion [211]. High ex-pression of ZFP36L1 in GBM patients correlates with a poor clinical outcome and correlateswith the downregulation of miR-129-5p. Finally, miR-181b was suggested as a potentialregulator of ZFP36L1 in Chronic Lymphocytic Leukemia (CLL). However, no validationexperiments were provided in this study, and thus, the link between this miRNA and BRF1remains to be firmly demonstrated [212].
4.2.3. Butyrate Response Factor 2 (ZFP36L2)
The post-transcriptional regulation of BRF2 is almost unknown, but emerging evidenceindicates that some miRNAs are also involved, such as miR-375 in pancreatic ductaladenocarcinoma [213]. In this study, the authors demonstrated that the expression of miR-375 is strongly reduced in PDAC from patients. Furthermore, overexpression of miR-375 inPDAC cells (i.e., PANC-1 and SW1990) strongly refrains cancer cell proliferation, migration,and invasion. This effect is partially attributed to the decrease in ZFP36L2, which is a directtarget of miR-375. Finally, in patients, high expression of ZFP36L2 is associated with apoor clinical outcome. In NSCLC, miR-373, which is a direct regulator of BRF2 [214], isdownregulated. The loss of miR-373 and the overexpression of BRF2 correlates with a poorprognosis in patients. Accordingly, miR-373 overexpression or BRF2 knockdown in cancercells (A549 cells) impairs proliferation, migration, and invasion [214]. Similar findings wereobtained in lung adenocarcinoma with let-7b-3p, which is also downregulated and is adirect regulator of BRF2 expression [215].
Table 1. MiRNAs regulating HuR and TTP family members and involved in cancers. n.a: not available.
miRNA Targets(AUBPs) Models Used Expression/Activity in
Patients Reference
Gastric cancer
miR-145
ELAVL1
SK-OV-3, A2780 and OVCAR-3 Down [161]
miR-519 n.a Down [162]
miR-582-3p HGC27, BGC823 cells Down [163]
Ovarian cancer
miR-139-3pELAVL1
SK-OV-3, A2780 and OVCAR-3 Down [166]
miR-519 Hela, A21780 and HOSE-B cells Down [167]
Papillary thyroid carcinoma
miR-31 ELAVL1 Ovarian carcinoma cells Down [169]
Cancers 2022, 14, 3516 18 of 30
Table 1. Cont.
miRNA Targets(AUBPs) Models Used Expression/Activity in
Patients Reference
Non-small cell lung carcinoma
miR-139-3p
ELAVL1
Normal bronchial epithelial cells (BEAS-2B)and NSCLC cells (H1299, H1975, HCC827,
H1650 A549)Down [172]
miR-146a-5p A549 cells Down [173]
miR-31 n.a Down [174]
miR-519 Hela, A21780 and HOSE-B cells Down [167]
miR-373 ZFP36L2 A549 cells Down [214]
Lung adenocarcinoma
Let-7b-3p ZFP36L2 H1299, A549 cells Down [215]
Hepatocellular carcinoma
miR-16 ELAVL1 Hep3B, WRL68 Down [165]
miR-9-5p ZFP36 HuH7, Hep3B Down [208]
Colorectal cancer
miR-22
ELAVL1
NCM460, SW480, HT29, HCT15, HCT116,SW620, Caco2, LOVO Down [175]
miR-324-5p SW620, SW480, NCM-460 cells Down [176]
miR-519 S1, S1M1 80 (mitoxantrone-resistant),Caco-2, HT-29, SW620 Down [168,177]
miR-155-5p HT-29 Up [178,216]
miR-34b-5p NCM460, SW620, HT-29, HCT116, LoVo,RKO Down [60]
miR-3121-3p DLD-1, HCT116, HT29, SW480 Down [179].
Prostate cancer
miR-133bELAVL1
PC3, DU-145 cell lines Down [189,217,218]
miR-34a PC3 Down [191,219]
Cervical cancer
miR-324-5pELAVL1
33A, ME-180, Hela and Caski Down [168,180]
miR-519 Hela cells Down [168,180]
Pancreatic cancer
miR-29a ZFP36 Panc-1, HPDE6c7, BXPC-3 Up [204]
miR-375 ZFP36L2 Pancreatic ductal adenocarcinoma PANC-1and SW1990 Down [213]
Glioblastoma
miR-3127-5pELAVL1
Down [183]
miR-146b-5p Glioma stem cells Down [184]
miR-129-5p ZFP36L1 LN229, A172, U87, T98G, U251, H4, LN118and normal astrocytes Down [211]
Breast cancer
miR-16ELAVL1
MDA-MB-231 Down [185]
miR-125a MCF-7 Down [186,220]
Cancers 2022, 14, 3516 19 of 30
Table 1. Cont.
miRNA Targets(AUBPs) Models Used Expression/Activity in
Patients Reference
miR-29a ELAVL1(indirectly)
MDA-MB-231, MCF-7, MCF12A, MCF10Acells Up [188]
miR-519 ELAVL1 MCF-7 cells Down [187]
miR-29a ZFP36MDA-MB-231 and MCF-7, MCF12A and
MCF10A (normal-like breast cell line), andHEK293 kidney cells
Up [188,203]
miR-182 ZFP36 MDA-MB-231, SUM-159, MCF-7, SK-BR-3,MDA-MB-157 Up [206]
miR-200c ZFP36 4TO7 cells Up [209,221]
Nasopharyngeal carcinoma
miR-514-5p ELAVL1 CNE1, CNE2, C666–1 and HNE1 cells Down [192]
Oropharyngeal squamous cell carcinoma
miR-133a-3p ELAVL1 UMSCC47 and UMSCC11A cells Down [193]
Laryngeal squamous cell carcinoma
miR-519a ELAVL1 laryngeal squamous cell carcinoma humanepithelial type 2 cells Down [194]
Hematologic malignancies
miR-519 ELAVL1 HL-60 cells (AML) Up [196]
miR-25 ELAVL1(indirectly) U937 (AML) Down [198,222]
miR-199a-3p ELAVL1 Bone marrow cells n.a. [197]
miR-25 ELAVL1(indirect) Bone marrow cells Down [197,222]
miR-146b ELAVL1 T-large granular lymphocyte leukemia(T-LGLL), Down [200]
miR-128a ZFP36 AML cells (OCI-AML3 and APL/AML) Up [207]
miR-181b ZFP36L1 (notvalidated) CLL cells Down [212]
miR-9 ELAVL1 Hodgkin lymphomaL428 cells Up [123,223]
5. Conclusions
In this review, we discussed several mechanisms associated with HuR and TTP familymembers, which indicate that these proteins form a complex regulatory network withnon-coding RNAs, that can exert both oncogenic and tumor-suppressive functions. Thislevel of complexity between these post-transcriptional regulators is poorly considered inhuman diseases but also in physiological processes (e.g., development), and thus, ourcurrent interpretation of their role in cancers is mostly incomplete and probably misleading.Moreover, emerging evidence indicates that these crosstalks also occur in preneoplasticstages, including chronic inflammatory and metabolic disorders, and thus may contributeto the onset of cancers [224,225]. These findings challenge the dogmatic function of someAUBP (e.g., HuR) and miRNAs (e.g., miR-21) in cancers and clearly indicate that miRNAactivity is not reflected by their deregulated expression only but also their bioavailability.Taken together, these findings suggest cautions regarding the therapeutic approaches aimedat targeting miRNAs or AUBPs (e.g., HuR-specific inhibitors suggested for the treatmentof cancers) [51,226]. Therefore, a better understanding of this regulatory network and
Cancers 2022, 14, 3516 20 of 30
of the impact of these therapeutic approaches on miRNA-dependent regulation of geneexpression is needed prior to any clinical application. In this regard, one of the major issuesis the current models available to study human diseases, which do not fully recapitulate thecomplexity of these interactions occurring in patients. Therefore, intense efforts are requiredto integrate these networks in more physiological models (in vivo) rather than assessing therole of individual regulators in vitro. In this review, we discussed the crosstalks betweenthe AUBPs, HuR, TTP family members, and miRNAs, but it is likely that a higher level ofcomplexity is occurring with other RBPs, lncRNA, ceRNA, and RNA editing. Althoughmodeling this entire network is currently challenging, new bioinformatics tools (databaserepository, deep learning, artificial intelligence) [227] will represent an asset in the futureto achieve this goal and to identify new players of carcinogenesis, which may representnovel therapeutic targets. Finally, identifying the miRNAs/lncRNA regulating AUBPs andthus important oncogenes and tumor suppressors is also of major importance for designingnovel therapeutic approaches. The current findings indicate that this regulation depends onseveral miRNAs regulating HuR and TTP family members in concert. Targeting the mostconsistent mechanisms (e.g., miR-519 for HuR) may also represent an appealing approachfor different cancers.
Author Contributions: Conceptualization, N.L. and C.S.; writing—review and editing, N.L., C.S. andL.D.; supervision, C.S.; funding acquisition, C.S. All authors have read and agreed to the publishedversion of the manuscript.
Funding: This research was funded by the “Métropole Européenne de Lille” (MEL) and the StaRsprogram (Hauts-de-France). The APC was funded by the “Métropole Européenne de Lille” (MEL).
Conflicts of Interest: The authors declare no conflict of interest.
Abbreviations
ABCB1: P-glycoprotein; ABCG2: ATP Binding Cassette Subfamily G Member 2; AGAP2-AS1:AGAP2 Antisense RNA 1; AGO2: Argonaute RISC Catalytic Component 2; ALKBH5: AlkB Homolog5 RNA Demethylase; AML: Acute Myeloid Leukemia; ARE: Adenine and Uridine-Rich Elements;AUBP: Adenylate-Uridylate-Rich Elements Binding Protein; BAG3: Bcl-2 Associated Athanogene 3;BBOX1-AS1: BBOX1 antisense RNA 1; BMDMs: Bone Marrow-Derived Macrophages; BRF1: ButyrateResponse Factor 1; BRF2: Butyrate Response Factor 1; CBS: Cystathionine-β-Synthase; CCAT2: ColonCancer Associated Transcript 2; CCL-5: C-C Motif Chemokine Ligand 5; CCND1: Cyclin D1; CCNE1cylclin E1; CDC34: Cell Division Cycle 34; CDC5L: Cell Division Cycle 5-Like Protein; CDK3: CyclinDependent Kinase 3; CDKN1A: Cyclin Dependent Kinase Inhibitor 1A; ceRNA: Competing Endoge-nous RNA; CHK2: Checkpoint 2; ChlA-F: Cheliensisin A Fluoride; circCCNB1: Circular Cyclin B1;circRNA: Circular RNA; CKAP5: Cytoskeleton Associated Protein 5; CLL: Chronic LymphocyticLeukemia; CML: Chronic Myelogenous Leukemia; c-Myc: Myelocytomatosis; COX-2: Cyclooxy-genase 2; CPT1A: Carnitine Palmitoyltransferase 1A; CRC: Colorectal Cancer; DGCR8: DiGeorgeSyndrome Critical Region 8; DHTS: Dihydrotanshinone-I; EGFR: Epidermal Growth Factor Receptor;EIF4EBP3: Eukaryotic Translation Initiation Factor 4E Binding Protein 3; ELAV: Embryonic-LethalAbnormal Vision in Drosophila; EMT: Epithelial-Mesenchymal Transition; ERBB2: Erb-B2 ReceptorTyrosine Kinase 2; ERK8: Extracellular Signal Regulated Kinase 8; ESCC: Esophageal Squamous CellCarcinoma; FAM83B: Family With Sequence Similarity 83 Member B; FAT3: FAT ATipycal cadherin 3;FENDRR: FOXF1 Adjacent Non-Coding Developmental Regulatory RNA; FGF21: Fibroblast GrowthFactor 21; FSCN1: Fascin Actin-Bundling Protein 1; GACAT3: Gastric Cancer-Associated Transcript 3;GAS5: Growth Arrest Specific 5; GC: Gastric Cancer; GLI2: GLI Family Zinc Finger 2; GSC: GliomaStem Cells; HCC: Hepatocellular Carcinoma; HDAC: Histone Deacetylase Inhibitors; LncHGBC:Long Non Coding RNA Highly Expressed In Gallblader Cancer; HIF1A: Hypoxia Inducible Factor 1Subunit Alpha; HK2: Hexokinase-2; HMGA: High Mobility Group AT-Hook 1; HNF4A: HepatocytesNuclear Factor 4 Alpha; HOTAIR: Homeobox Transcript Antisense RNA; HOX: Homeobox; HOXC6:Homeobox C6; HPV: Human Papilloma Virus; HuR: Human Antigen R; IL: Interleukin; JNK: JUN N-Terminal Kinase; LATS2: Large Tumor Suppressor Kinase 2; Linc: Long Intergenic Non Coding RNA;lncRNA: Long-Non-Coding RNA; LPS: lipopolysacharide; LUSC: Lung Squamous Cell Carcinoma;
Cancers 2022, 14, 3516 21 of 30
MAP4K1: Mitogen-Activated Protein Kinase Kinase Kinase Kinase 1; MDR1: Multidrug ResistanceProtein 1; MIBC: Muscle Invasive Bladder Cancer; miRNA: micro RNA; MNX1-AS1: MNX1 AntisenseRNA 1; mRNA: messenger RNA; NCL: Nucleolin; NcRNA: Non-Coding RNA; NEAT1: Nuclear En-riched Abundant Transcript 1; NFkB: Nuclear Factor Kappa B; NONO: Non-Pou Domain-ContainingOctamer Binding Protein; NOTCH4: Neurogenic Locus Notch Homolog 4; NOX4: NADPH Oxidase4; NSCLC: Non-Small Cell Lung Cancer; p70S6K: 70kDa Ribosomal Protein S6 Kinase; P-bodies:Processing Bodies; PBX3: Pre-B-Cell Leukemia Transcription Factor 3; PDAC: Pancreatic DuctalAdenocarcinoma; PDCD4: Programmed Cell Death Protein 4; PI3K /AKT: Phosphoinositide 3 Kinase/ Protein Kinase B; PKM2: Pyruvate Kinase-M2; Pre-miRNA: Precursor miRNA; Pri-miRNA: PrimarymiRNA; PTEN: Phosphatase and TENsin homolog; PTGS2: Prostaglandin Endoperoxide Synthase2; Ptn-dt: Pleiotrophin; PVT1: Plasmacytoma Variant Translocation 1; RanGTP: Ras related nuclearProtein GTP (guanosine triphosphate); RBP: RNA-Binding Protein; Rgs4: Regulator of G-protein sig-naling 4; RhoB: Ras homolog B; RISC: RNA-Induced Silencing Complex; RMS: Rhabdomyosarcoma;RNP: Ribonucleoprotein; RPSAP52: Ribosomal Protein SA Pseudogene 52; RRM: RNA-Recognitionmotif; S1PR3: Sphingosine 1-Phosphate Receptor 3; SEMA4D: Semaphorin 4D; SG: Stress Granules;SIRT1: Silent Mating Type Information Regulation 2 Homolog 1; SLC2A4: Solute Carrier Family2 Member 4; SLC44A4: Solute Carrier Family 44 Member 4; SOCE: Store Operated Ca2+ Entry;STAT3: Signal Transducer and Activator Of Transcription 3; STIM1: Stromal Interaction Molecule 1;TAMR: Tamoxifen-Resistant; TGF-β: Transforming Growth Factor-Beta; T-LGLL: T-Large GranularLymphocyte Leukemia; TNFα: Tumor Necrosis Factor-Alpha; TOP2A: Topoisomerase II Alpha;TTN-AS1: Titin mRNA-Antisense RNA 1; TTP: Tristetraprolin; TUBB3: class III β-tubulin; UBE2C:Ubiquitin Conjugating Enzyme E2 C; UFC1: Ubiquitin Fold Modifier Conjugating Enzyme 1; UTR:Untranslated Region; UV: Ultra-Violet; UVC: Ultra-Violet C; VEGFA: Vascular Endothelial GrowthFactor A; YAP: Yes-Associated Protein; ZFP36: Zinc Finger Protein 36 Homolog; ZFP36L1: ZincFinger Protein 36 Homolog Like 1; ZFP36L2: Zinc Finger Protein 36 Homolog Like 2; ZNF609: ZincFinger Protein 609.
References1. Hill, M.; Tran, N. miRNA interplay: Mechanisms and consequences in cancer. Dis. Model. Mech. 2021, 14. [CrossRef] [PubMed]2. Monaci, R.; Meoni, S.; Rondine, P.; Leone, G.; Ciuffoletti, L.; Cecchin, A.; Morandini, M. Echotomography in abdominal
emergencies. Apropos of 16 controlled clinical cases. (A description of some of them). Minerva Med. 1989, 80, 117–121. [PubMed]3. Bernardo, B.C.; Ooi, J.Y.Y.; Lin, R.C.Y.; McMullen, J.R. miRNA therapeutics: A new class of drugs with potential therapeutic
applications in the heart. Future Med. Chem. 2015, 7, 1771–1792. [CrossRef]4. Yin, X.; Lin, H.; Lin, L.; Miao, L.; He, J.; Zhuo, Z. LncRNAs and CircRNAs in cancer. MedComm 2022, 3, e141. [CrossRef] [PubMed]5. Winkler, L.; Dimitrova, N. A mechanistic view of long noncoding RNAs in cancer. Wiley Interdiscip. Rev. RNA 2022, 13, e1699.
[CrossRef] [PubMed]6. Pereira, B.; Billaud, M.; Almeida, R. RNA-Binding Proteins in Cancer: Old Players and New Actors. Trends Cancer 2017, 3, 506–528.
[CrossRef] [PubMed]7. Barreau, C.; Paillard, L.; Osborne, H.B. AU-rich elements and associated factors: Are there unifying principles? Nucleic Acids Res.
2005, 33, 7138–7150. [CrossRef] [PubMed]8. Lamarre, J.; Gingerich, T.J.; Feige, J.-J. AU-rich elements and the control of gene expression through regulated mRNA stability.
Anim. Health Res. Rev. 2004, 5, 49–63. [CrossRef]9. Dolicka, D.; Sobolewski, C.; De Sousa, M.C.; Gjorgjieva, M.; Foti, M. mRNA Post-Transcriptional Regulation by AU-Rich
Element-Binding Proteins in Liver Inflammation and Cancer. Int. J. Mol. Sci. 2020, 21, 6648. [CrossRef]10. Moore, A.E.; Young, L.E.; Dixon, D.A. MicroRNA and AU-rich element regulation of prostaglandin synthesis. Cancer Metastasis
Rev. 2011, 30, 419–435. [CrossRef]11. Kedde, M.; Agami, R. Interplay between microRNAs and RNA-binding proteins determines developmental processes. Cell Cycle
2008, 7, 899–903. [CrossRef] [PubMed]12. Zhang, H.; Huang, Z.; Zhong, S.; Fei, K.; Cao, Y. miR21 inhibits autophagy and promotes malignant development in the bladder
cancer T24 cell line. Int. J. Oncol. 2020, 56, 986–998. [CrossRef] [PubMed]13. Ma, X.; Li, C.; Sun, L.; Huang, D.; Li, T.; He, X.; Wu, G.; Yang, Z.; Zhong, X.; Song, L.; et al. Lin28/let-7 axis regulates aerobic
glycolysis and cancer progression via PDK1. Nat. Commun. 2014, 5, 5212. [CrossRef] [PubMed]14. Zhang, Z.; Guo, M.; Li, Y.; Shen, M.; Kong, D.; Shao, J.; Ding, H.; Tan, S.; Chen, A.; Zhang, F.; et al. RNA-binding protein
ZFP36/TTP protects against ferroptosis by regulating autophagy signaling pathway in hepatic stellate cells. Autophagy 2020, 16,1482–1505. [CrossRef]
Cancers 2022, 14, 3516 22 of 30
15. Gjorgjieva, M.; Sobolewski, C.; Ay, A.-S.; Abegg, D.; De Sousa, M.C.; Portius, D.; Berthou, F.; Fournier, M.; Maeder, C.; Rantakari,P.; et al. Genetic Ablation of MiR-22 Fosters Diet-Induced Obesity and NAFLD Development. J. Pers. Med. 2020, 10, 170.[CrossRef] [PubMed]
16. Yang, Z.; Qin, W.; Huo, J.; Zhuo, Q.; Wang, J.; Wang, L. MiR-22 modulates the expression of lipogenesis-related genes andpromotes hepatic steatosis in vitro. FEBS Open Bio 2021, 11, 322–332. [CrossRef]
17. Mohr, A.M.; Mott, J.L. Overview of MicroRNA Biology. Semin. Liver Dis. 2015, 35, 3–11. [CrossRef]18. Szczepanek, J.; Skorupa, M.; Tretyn, A. MicroRNA as a Potential Therapeutic Molecule in Cancer. Cells 2022, 11, 1008. [CrossRef]19. Winter, J.; Jung, S.; Keller, S.; Gregory, R.I.; Diederichs, S. Many roads to maturity: MicroRNA biogenesis pathways and their
regulation. Nat. Cell Biol. 2009, 11, 228–234. [CrossRef]20. de Sousa, M.C.; Gjorgjieva, M.; Dolicka, D.; Sobolewski, C.; Foti, M. Deciphering miRNAs’ Action through miRNA Editing. Int. J.
Mol. Sci. 2019, 20, 6249. [CrossRef]21. Kim, M.; Hur, B.; Kim, S. RDDpred: A condition-specific RNA-editing prediction model from RNA-seq data. BMC Genom. 2016,
17 (Suppl. S1), 85–95. [CrossRef] [PubMed]22. Karagkouni, D.; Karavangeli, A.; Paraskevopoulou, M.D.; Hatzigeorgiou, A.G. Characterizing miRNA–lncRNA Interplay. Methods
Mol. Biol. 2021, 2372, 243–262. [CrossRef] [PubMed]23. Sharma, S.; Verma, S.; Vasudevan, M.; Samanta, S.; Thakur, J.K.; Kulshreshtha, R. The interplay of HuR and miR-3134 in regulation
of AU rich transcriptome. RNA Biol. 2013, 10, 1283–1290. [CrossRef] [PubMed]24. Baccarini, A.; Brown, B.D. Monitoring MicroRNA Activity and Validating MicroRNA Targets by Reporter-Based Approaches.
Methods Mol. Biol. 2010, 667, 215–233. [CrossRef]25. Clément, S.; Sobolewski, C.; Gomes, D.; Rojas, A.; Goossens, N.; Conzelmann, S.; Calo, N.; Negro, F.; Foti, M. Activation of the
oncogenic miR-21-5p promotes HCV replication and steatosis induced by the viral core 3a protein. Liver Int. 2019, 39, 1226–1236.[CrossRef]
26. Li, J.-H.; Liu, S.; Zhou, H.; Qu, L.-H.; Yang, J.-H. starBase v2.0: Decoding miRNA-ceRNA, miRNA-ncRNA and protein–RNAinteraction networks from large-scale CLIP-Seq data. Nucleic Acids Res. 2014, 42, D92–D97. [CrossRef]
27. Nicholson, C.O.; Friedersdorf, M.B.; Keene, J.D. Quantifying RNA binding sites transcriptome-wide using DO-RIP-seq. RNA2017, 23, 32–46. [CrossRef]
28. Lebedeva, S.; Jens, M.; Theil, K.; Schwanhäusser, B.; Selbach, M.; Landthaler, M.; Rajewsky, N. Transcriptome-wide Analysis ofRegulatory Interactions of the RNA-Binding Protein HuR. Mol. Cell 2011, 43, 340–352. [CrossRef]
29. Legrand, N.; A Dixon, D.; Sobolewski, C. AU-rich element-binding proteins in colorectal cancer. World J. Gastrointest. Oncol. 2019,11, 71–90. [CrossRef]
30. Young, L.E.; Sanduja, S.; Bemis–Standoli, K.; Pena, E.A.; Price, R.L.; Dixon, D.A. The mRNA Binding Proteins HuR andTristetraprolin Regulate Cyclooxygenase 2 Expression During Colon Carcinogenesis. Gastroenterology 2009, 136, 1669–1679.[CrossRef]
31. Dixon, D.A.; Tolley, N.D.; King, P.H.; Nabors, L.B.; McIntyre, T.M.; Zimmerman, G.A.; Prescott, S.M. Altered expression of themRNA stability factor HuR promotes cyclooxygenase-2 expression in colon cancer cells. J. Clin. Investig. 2001, 108, 1657–1665.[CrossRef] [PubMed]
32. Dixon, D.A.; Balch, G.; Kedersha, N.; Anderson, P.; Zimmerman, G.A.; Beauchamp, R.D.; Prescott, S.M. Regulation ofCyclooxygenase-2 Expression by the Translational Silencer TIA-1. J. Exp. Med. 2003, 198, 475–481. [CrossRef] [PubMed]
33. Kim, H.H.; Abdelmohsen, K.; Lal, A.; Pullmann, R.; Yang, X.; Galban, S.; Srikantan, S.; Martindale, J.L.; Blethrow, J.; Shokat, K.M.;et al. Nuclear HuR accumulation through phosphorylation by Cdk1. Genes Dev. 2008, 22, 1804–1815. [CrossRef]
34. Tiedje, C.; Ronkina, N.; Tehrani, M.; Dhamija, S.; Laass, K.; Holtmann, H.; Kotlyarov, A.; Gaestel, M. The p38/MK2-DrivenExchange between Tristetraprolin and HuR Regulates AU–Rich Element–Dependent Translation. PLoS Genet. 2012, 8, e1002977.[CrossRef] [PubMed]
35. Sandler, H.; Stoecklin, G. Control of mRNA decay by phosphorylation of tristetraprolin. Biochem. Soc. Trans. 2008, 36, 491–496.[CrossRef]
36. Sengupta, S.; Jang, B.-C.; Wu, M.-T.; Paik, J.-H.; Furneaux, H.; Hla, T. The RNA-binding Protein HuR Regulates the Expression ofCyclooxygenase-2. J. Biol. Chem. 2003, 278, 25227–25233. [CrossRef] [PubMed]
37. Dean, J.L.E.; Wait, R.; Mahtani, K.R.; Sully, G.; Clark, A.R.; Saklatvala, J. The 3′ Untranslated Region of Tumor Necrosis FactorAlpha mRNA Is a Target of the mRNA-Stabilizing Factor HuR. Mol. Cell. Biol. 2001, 21, 721–730. [CrossRef]
38. Sawicki, K.T.; Chang, H.-C.; Shapiro, J.S.; Bayeva, M.; De Jesus, A.; Finck, B.N.; Wertheim, J.A.; Blackshear, P.J.; Ardehali, H.Hepatic tristetraprolin promotes insulin resistance through RNA destabilization of FGF21. JCI Insight 2018, 3. [CrossRef]
39. Zhang, Z.; Zong, C.; Jiang, M.; Hu, H.; Cheng, X.; Ni, J.; Yi, X.; Jiang, B.; Tian, F.; Chang, M.-W.; et al. Hepatic HuR modulateslipid homeostasis in response to high-fat diet. Nat. Commun. 2020, 11, 3067. [CrossRef]
40. Rounbehler, R.J.; Fallahi, M.; Yang, C.; Steeves, M.A.; Li, W.; Doherty, J.R.; Schaub, F.X.; Sanduja, S.; Dixon, D.A.; Blackshear, P.J.;et al. Tristetraprolin Impairs Myc-Induced Lymphoma and Abolishes the Malignant State. Cell 2012, 150, 563–574. [CrossRef]
41. Cao, Y.; Huang, W.; Wu, F.; Shang, J.; Ping, F.; Wang, W.; Li, Y.; Zhao, X.; Zhang, X. ZFP36 protects lungs from intestinalI/R-induced injury and fibrosis through the CREBBP/p53/p21/Bax pathway. Cell Death Dis. 2021, 12, 685. [CrossRef] [PubMed]
42. Srikantan, S.; Tominaga, K.; Gorospe, M. Functional Interplay between RNA-Binding Protein HuR and microRNAs. Curr. ProteinPept. Sci. 2012, 13, 372–379. [CrossRef] [PubMed]
Cancers 2022, 14, 3516 23 of 30
43. Mukherjee, N.; Corcoran, D.L.; Nusbaum, J.D.; Reid, D.W.; Georgiev, S.; Hafner, M.; Ascano, M.; Tuschl, T.; Ohler, U.; Keene,J.D. Integrative Regulatory Mapping Indicates that the RNA-Binding Protein HuR Couples Pre-mRNA Processing and mRNAStability. Mol. Cell 2011, 43, 327–339. [CrossRef] [PubMed]
44. Brennan, C.M.; Steitz, J.A. HuR and mRNA stability. Cell Mol. Life Sci. 2001, 58, 266–277. [CrossRef]45. Brody, J.R.; Dixon, D.A. Complex HuR function in pancreatic cancer cells. Wiley Interdiscip. Rev. RNA 2018, 9, e1469. [CrossRef]
[PubMed]46. Grammatikakis, I.; Abdelmohsen, K.; Gorospe, M. Posttranslational control of HuR function. Wiley Interdiscip. Rev. RNA 2017, 8.
[CrossRef] [PubMed]47. Doller, A.; Pfeilschifter, J.; Eberhardt, W. Signalling pathways regulating nucleo-cytoplasmic shuttling of the mRNA-binding
protein HuR. Cell. Signal. 2008, 20, 2165–2173. [CrossRef]48. Dixon, D.A.; Blanco, F.F.; Bruno, A.; Patrignani, P. Mechanistic aspects of COX-2 expression in colorectal neoplasia. Recent Results
Cancer Res. 2013, 191, 7–37. [CrossRef]49. A Dixon, D. Regulation of COX-2 Expression in Human Cancers. Prog. Exp. Tumor. Res. 2003, 37, 52–71. [CrossRef]50. Wu, X.; Gardashova, G.; Lan, L.; Han, S.; Zhong, C.; Marquez, R.T.; Wei, L.; Wood, S.; Roy, S.; Gowthaman, R.; et al. Targeting the
interaction between RNA-binding protein HuR and FOXQ1 suppresses breast cancer invasion and metastasis. Commun. Biol.2020, 3, 193. [CrossRef]
51. Blanco, F.F.; Preet, R.; Aguado, A.; Vishwakarma, V.; Stevens, L.E.; Vyas, A.; Padhye, S.; Xu, L.; Weir, S.J.; Anant, S.; et al. Impact ofHuR inhibition by the small molecule MS-444 on colorectal cancer cell tumorigenesis. Oncotarget 2016, 7, 74043–74058. [CrossRef][PubMed]
52. Lal, P.; Cerofolini, L.; D’Agostino, V.G.; Zucal, C.; Fuccio, C.; Bonomo, I.; Dassi, E.; Giuntini, S.; Di Maio, D.; Vishwakarma, V.; et al.Regulation of HuR structure and function by dihydrotanshinone-I. Nucleic Acids Res. 2017, 45, 9514–9527. [CrossRef] [PubMed]
53. Pfeffer, S.R.; Yang, C.H.; Pfeffer, L. The Role of miR-21 in Cancer. Drug Dev. Res. 2015, 76, 270–277. [CrossRef]54. Arghiani, N.; Matin, M.M. miR-21: A Key Small Molecule with Great Effects in Combination Cancer Therapy. Nucleic Acid Ther.
2021, 31, 271–283. [CrossRef] [PubMed]55. Poria, D.K.; Guha, A.; Nandi, I.; Ray, P.S. RNA-binding protein HuR sequesters microRNA-21 to prevent translation repression of
proinflammatory tumor suppressor gene programmed cell death 4. Oncogene 2016, 35, 1703–1715. [CrossRef] [PubMed]56. Kumar, R.; Poria, D.K.; Ray, P.S. RNA-binding proteins La and HuR cooperatively modulate translation repression of PDCD4
mRNA. J. Biol. Chem. 2021, 296, 100154. [CrossRef] [PubMed]57. de Sousa, M.C.; Calo, N.; Sobolewski, C.; Gjorgjieva, M.; Clément, S.; Maeder, C.; Dolicka, D.; Fournier, M.; Vinet, L.; Montet, X.;
et al. Mir-21 Suppression Promotes Mouse Hepatocarcinogenesis. Cancers 2021, 13, 4983. [CrossRef]58. Liwak-Muir, U.; Dobson, C.C.; Naing, T.; Wylie, Q.; Chehade, L.; Baird, S.D.; Chakraborty, P.K.; Holcik, M. ERK8 is a novel
HuR kinase that regulates tumour suppressor PDCD4 through a miR-21 dependent mechanism. Oncotarget 2016, 7, 1439–1450.[CrossRef]
59. Tan, S.; Ding, K.; Chong, Q.-Y.; Zhao, J.; Liu, Y.; Shao, Y.; Zhang, Y.; Yu, Q.; Xiong, Z.; Zhang, W.; et al. Post-transcriptionalregulation of ERBB2 by miR26a/b and HuR confers resistance to tamoxifen in estrogen receptor-positive breast cancer cells. J.Biol. Chem. 2017, 292, 13551–13564. [CrossRef]
60. Wang, Y.; Lin, C.; Liu, Y. Molecular mechanism of miR-34b-5p and RNA binding protein HuR binding to lncRNA OIP5-AS1 incolon cancer cells. Cancer Gene Ther. 2022, 29, 612–624. [CrossRef]
61. Kim, J.; Abdelmohsen, K.; Yang, X.; De, S.; Grammatikakis, I.; Noh, J.H.; Gorospe, M. LncRNA OIP5-AS1/cyrano spongesRNA-binding protein HuR. Nucleic Acids Res. 2016, 44, 2378–2392. [CrossRef] [PubMed]
62. Guo, X.; Connick, M.C.; Vanderhoof, J.; Ishak, M.-A.; Hartley, R.S. MicroRNA-16 Modulates HuR Regulation of Cyclin E1 inBreast Cancer Cells. Int. J. Mol. Sci. 2015, 16, 7112–7132. [CrossRef] [PubMed]
63. Carvalho, L.S.; Gonçalves, N.; Fonseca, N.A.; Moreira, J.N. Cancer Stem Cells and Nucleolin as Drivers of Carcinogenesis.Pharmaceuticals 2021, 14, 60. [CrossRef] [PubMed]
64. Bose, S.; Tholanikunnel, T.E.; Reuben, A.; Tholanikunnel, B.G.; Spicer, E.K. Regulation of nucleolin expression by miR-194,miR-206, and HuR. Mol. Cell. Biochem. 2016, 417, 141–153. [CrossRef] [PubMed]
65. Xie, W.; Wang, Y.; Zhang, Y.; Xiang, Y.; Wu, N.; Wu, L.; Li, C.; Cai, T.; Ma, X.; Yu, Z.; et al. Single-nucleotide polymorphismrs4142441 and MYC co-modulated long non-coding RNA OSER1-AS1 suppresses non-small cell lung cancer by sequesteringELAVL1. Cancer Sci. 2021, 112, 2272–2286. [CrossRef]
66. Pei, Y.-F.; Yin, X.-M.; Liu, X.-Q. TOP2A induces malignant character of pancreatic cancer through activating β-catenin signalingpathway. Biochim. Biophys. Acta Mol. Basis Dis. 2018, 1864, 197–207. [CrossRef]
67. Bouchalova, K.; Cizkova, M.; Cwiertka, K.; Trojanec, R.; Hajduch, M. Triple negative breast cancer-current status and prospectivetargeted treatment based on HER1 (EGFR), TOP2A and C-MYC gene assessment. Biomed. Pap. Med. Fac. Univ. Palacky OlomoucCzech. Repub. 2009, 153, 13–17. [CrossRef]
68. Zhang, R.; Xu, J.; Zhao, J.; Bai, J.H. Proliferation and invasion of colon cancer cells are suppressed by knockdown of TOP2A. J.Cell. Biochem. 2018, 119, 7256–7263. [CrossRef]
69. Srikantan, S.; Abdelmohsen, K.; Lee, E.K.; Tominaga, K.; Subaran, S.S.; Kuwano, Y.; Kulshrestha, R.; Panchakshari, R.; Kim, H.H.;Yang, X.; et al. Translational Control of TOP2A Influences Doxorubicin Efficacy. Mol. Cell. Biol. 2011, 31, 3790–3801. [CrossRef]
Cancers 2022, 14, 3516 24 of 30
70. Wang, Y.; Wang, H.; Pan, T.; Li, L.; Li, J.; Yang, H. STIM1 silencing inhibits the migration and invasion of A549 cells. Mol. Med.Rep. 2017, 16, 3283–3289. [CrossRef]
71. Zhuang, R.; Rao, J.N.; Zou, T.; Liu, L.; Xiao, L.; Cao, S.; Hansraj, N.Z.; Gorospe, M.; Wang, J.-Y. miR-195 competes with HuR tomodulate stim1 mRNA stability and regulate cell migration. Nucleic Acids Res. 2013, 41, 7905–7919. [CrossRef] [PubMed]
72. Cui, J.; Cao, N.; Wang, G.; Wang, F.; Yang, B.; Wang, J.; Lv, Y.; Chen, Y.; Li, F. HuR Promotes the Progression of Gastric Cancerthrough Mediating CDC5L Expression. Dis. Markers 2022, 2022, 5141927. [CrossRef] [PubMed]
73. Wang, Y.; Zhao, H.; Zhi, W. SEMA4D under the posttranscriptional regulation of HuR and miR-4319 boosts cancer progression inesophageal squamous cell carcinoma. Cancer Biol. Ther. 2020, 21, 122–129. [CrossRef] [PubMed]
74. Hu, X.; Wang, M.; Cao, L.; Cong, L.; Gao, Y.; Lu, J.; Feng, J.; Shen, B.; Liu, D. miR-4319 Suppresses the Growth of EsophagealSquamous Cell Carcinoma Via Targeting NLRC5. Curr. Mol. Pharmacol. 2020, 13, 144–149. [CrossRef]
75. Xu, X.; Song, C.; Chen, Z.; Yu, C.; Wang, Y.; Tang, Y.; Luo, J. Downregulation of HuR Inhibits the Progression of EsophagealCancer through Interleukin-18. Cancer Res. Treat. 2018, 50, 71–87. [CrossRef]
76. Hao, Z.; Zhang, H.; Cowell, J. Ubiquitin-conjugating enzyme UBE2C: Molecular biology, role in tumorigenesis, and potential as abiomarker. Tumor Biol. 2012, 33, 723–730. [CrossRef]
77. Wang, Y.; Huang, F.; Liu, M.; Zhao, Q. UBE2C mRNA expression controlled by miR-300 and HuR determines its oncogenic role ingastric cancer. Biochem. Biophys. Res. Commun. 2021, 534, 597–603. [CrossRef]
78. Tominaga, K.; Srikantan, S.; Lee, E.K.; Subaran, S.S.; Martindale, J.L.; Abdelmohsen, K.; Gorospe, M. Competitive Regulation ofNucleolin Expression by HuR and miR-494. Mol. Cell. Biol. 2011, 31, 4219–4231. [CrossRef]
79. Morgan, R.; Pandha, H.S. PBX3 in Cancer. Cancers 2020, 12, 431. [CrossRef]80. Zhou, H.; Rao, Y.; Sun, Q.; Liu, Y.; Zhou, X.; Chen, Y.; Chen, J. MiR-4458/human antigen R (HuR) modulates PBX3 mRNA stability
in melanoma tumorigenesis. Arch. Dermatol. Res. 2020, 312, 665–673. [CrossRef]81. Li, C.; Jiang, J.-Y.; Wang, J.-M.; Sun, J.; An, M.-X.; Li, S.; Yan, J.; Wang, H.-Q. BAG3 regulates stability of IL-8 mRNA via interplay
between HuR and miR-4312 in PDACs. Cell Death Dis. 2018, 9, 863. [CrossRef] [PubMed]82. Zhang, F.; Ni, H.; Li, X.; Liu, H.; Xi, T.; Zheng, L. LncRNA FENDRR attenuates adriamycin resistance via suppressing MDR1
expression through sponging HuR and miR-184 in chronic myelogenous leukaemia cells. FEBS Lett. 2019, 593, 1993–2007.[CrossRef] [PubMed]
83. Dico, A.L.; Costa, V.; Martelli, C.; Diceglie, C.; Rajata, F.; Rizzo, A.; Mancone, C.; Tripodi, M.; Ottobrini, L.; Alessandro, R.;et al. MiR675-5p Acts on HIF-1α to Sustain Hypoxic Responses: A New Therapeutic Strategy for Glioma. Theranostics 2016, 6,1105–1118. [CrossRef] [PubMed]
84. Alfano, L.; Costa, C.; Caporaso, A.; Antonini, D.; Giordano, A.; Pentimalli, F. HUR protects NONO from degradation by mir320,which is induced by p53 upon UV irradiation. Oncotarget 2016, 7, 78127–78139. [CrossRef] [PubMed]
85. Chai, Y.; Liu, J.; Zhang, Z.; Liu, L. HuR-regulated lncRNA NEAT1 stability in tumorigenesis and progression of ovarian cancer.Cancer Med. 2016, 5, 1588–1598. [CrossRef]
86. Ahuja, D.; Goyal, A.; Ray, P.S. Interplay between RNA-binding protein HuR and microRNA-125b regulates p53 mRNA translationin response to genotoxic stress. RNA Biol. 2016, 13, 1152–1165. [CrossRef]
87. Chang, S.-H.; Lu, Y.-C.; Li, X.; Hsieh, W.-Y.; Xiong, Y.; Ghosh, M.; Evans, T.; Elemento, O.; Hla, T. Antagonistic Function of theRNA-binding Protein HuR and miR-200b in Post-transcriptional Regulation of Vascular Endothelial Growth Factor-A Expressionand Angiogenesis. J. Biol. Chem. 2013, 288, 4908–4921. [CrossRef]
88. Huang, J.-F.; Jiang, H.; Cai, H.; Liu, Y.; Zhu, Y.-Q.; Lin, S.-S.; Hu, T.-T.; Wang, T.-T.; Yang, W.-J.; Xiao, B.; et al. Genome-widescreening identifies oncofetal lncRNA Ptn-dt promoting the proliferation of hepatocellular carcinoma cells by regulating the Ptnreceptor. Oncogene 2019, 38, 3428–3445. [CrossRef]
89. Epis, M.R.; Barker, A.; Giles, K.M.; Beveridge, D.J.; Leedman, P.J. The RNA-binding Protein HuR Opposes the Repression ofERBB-2 Gene Expression by MicroRNA miR-331-3p in Prostate Cancer Cells. J. Biol. Chem. 2011, 286, 41442–41454. [CrossRef]
90. Lu, Y.-C.; Chang, S.-H.; Hafner, M.; Li, X.; Tuschl, T.; Elemento, O.; Hla, T. ELAVL1 Modulates Transcriptome-wide miRNABinding in Murine Macrophages. Cell Rep. 2014, 9, 2330–2343. [CrossRef]
91. Li, Y.; Estep, J.A.; Karginov, F.V. Transcriptome-wide Identification and Validation of Interactions between the miRNA Machineryand HuR on mRNA Targets. J. Mol. Biol. 2018, 430, 285–296. [CrossRef] [PubMed]
92. Chang, N.; Ge, J.; Xiu, L.; Zhao, Z.; Duan, X.; Tian, L.; Xie, J.; Yang, L.; Li, L. HuR mediates motility of human bone marrow-derivedmesenchymal stem cells triggered by sphingosine 1-phosphate in liver fibrosis. J. Mol. Med. 2017, 95, 69–82. [CrossRef] [PubMed]
93. Zhang, Y.; Yang, L.; Ling, C.; Heng, W. HuR facilitates cancer stemness of lung cancer cells via regulating miR-873/CDK3 andmiR-125a-3p/CDK3 axis. Biotechnol. Lett. 2018, 40, 623–631. [CrossRef]
94. Chen, Y.; Yang, F.; Fang, E.; Xiao, W.; Mei, H.; Li, H.; Li, D.; Song, H.; Wang, J.; Hong, M.; et al. Circular RNA circAGO2drives cancer progression through facilitating HuR-repressed functions of AGO2-miRNA complexes. Cell Death Differ. 2019, 26,1346–1364. [CrossRef] [PubMed]
95. Pellecchia, S.; Quintavalle, C.; Pallante, P. The control of tumor progression by circular RNAs: Novel prognostic and therapeuticinsights resulting from the analysis of the circAGO2/human antigen R complex. Transl. Cancer Res. 2019, 8, S211–S215. [CrossRef]
96. Zhu, H.; Gan, X.; Jiang, X.; Diao, S.; Wu, H.; Hu, J. ALKBH5 inhibited autophagy of epithelial ovarian cancer through miR-7 andBCL-2. J. Exp. Clin. Cancer Res. 2019, 38, 163. [CrossRef]
Cancers 2022, 14, 3516 25 of 30
97. Sheng, J.; Sun, H.; Yu, F.-B.; Li, B.; Zhang, Y.; Zhu, Y.-T. The Role of Cyclooxygenase-2 in Colorectal Cancer. Int. J. Med Sci. 2020,17, 1095–1101. [CrossRef]
98. Young, L.E.; Moore, A.E.; Sokol, L.; Meisner-Kober, N.; Dixon, D.A. The mRNA Stability Factor HuR Inhibits MicroRNA-16Targeting of COX-2. Mol. Cancer Res. 2012, 10, 167–180. [CrossRef]
99. Jin, D.; Guo, J.; Wu, Y.; Yang, L.; Wang, X.; Du, J.; Dai, J.; Chen, W.; Gong, K.; Miao, S.; et al. m6A demethylase ALKBH5 inhibitstumor growth and metastasis by reducing YTHDFs-mediated YAP expression and inhibiting miR-107/LATS2–mediated YAPactivity in NSCLC. Mol. Cancer 2020, 19, 40. [CrossRef]
100. Panneerdoss, S.; Eedunuri, V.K.; Yadav, P.; Timilsina, S.; Rajamanickam, S.; Viswanadhapalli, S.; Abdelfattah, N.; Onyeagucha,B.C.; Cui, X.; Lai, Z.; et al. Cross-talk among writers, readers, and erasers of m 6 A regulates cancer growth and progression. Sci.Adv. 2018, 4, eaar8263. [CrossRef]
101. Cao, C.; Sun, J.; Zhang, D.; Guo, X.; Xie, L.; Li, X.; Wu, D.; Liu, L. The Long Intergenic Noncoding RNA UFC1, a Target ofMicroRNA 34a, Interacts With the mRNA Stabilizing Protein HuR to Increase Levels of β-Catenin in HCC Cells. Gastroenterology2015, 148, 415–426. [CrossRef] [PubMed]
102. Xu, J.; Yang, B.; Wang, L.; Zhu, Y.; Zhu, X.; Xia, Z.; Zhao, Z.; Xu, L. LncRNA BBOX1-AS1 upregulates HOXC6 expression throughmiR-361-3p and HuR to drive cervical cancer progression. Cell Prolif. 2020, 53, e12823. [CrossRef] [PubMed]
103. Wang, M.; Mao, C.; Ouyang, L.; Liu, Y.; Lai, W.; Liu, N.; Shi, Y.; Chen, L.; Xiao, D.; Yu, F.; et al. Correction to: Long noncodingRNA LINC00336 inhibits ferroptosis in lung cancer by functioning as a competing endogenous RNA. Cell Death Differ. 2020, 27,1447. [CrossRef] [PubMed]
104. Hu, Y.-P.; Jin, Y.-P.; Wu, X.-S.; Yang, Y.; Li, Y.-S.; Li, H.-F.; Xiang, S.-S.; Song, X.-L.; Jiang, L.; Zhang, Y.-J.; et al. Correction to:LncRNA-HGBC stabilized by HuR promotes gallbladder cancer progression by regulating miR-502-3p/SET/AKT axis. Mol.Cancer 2021, 20, 110. [CrossRef]
105. Zang, Y.; Li, J.; Wan, B.; Tai, Y. circRNA circ-CCND1 promotes the proliferation of laryngeal squamous cell carcinoma throughelevating CCND1 expression via interacting with HuR and miR-646. J. Cell. Mol. Med. 2020, 24, 2423–2433. [CrossRef]
106. Shi, J.; Lv, X.; Zeng, L.; Li, W.; Zhong, Y.; Yuan, J.; Deng, S.; Liu, B.; Yuan, B.; Chen, Y.; et al. CircPVT1 promotes proliferation oflung squamous cell carcinoma by binding to miR-30d/e. J. Exp. Clin. Cancer Res. 2021, 40, 193. [CrossRef]
107. Jiang, H.; Tian, Y.; Zhao, X.; Zhang, L.; Wu, Z. A circular RNA derived from FAT atypical cadherin 3 promotes lung cancerprogression via forming a regulatory loop with oncogenic ELAV like RNA binding protein 1. J. Biochem. 2022, 171, 519–528.[CrossRef]
108. Zhang, L.; Lou, J.; Lu, M.; Gao, C.; Zhao, S.; Li, B.; Liang, S.; Li, Y.; Li, D.; Liu, M. Suppression of miR-199a maturation by HuR iscrucial for hypoxia-induced glycolytic switch in hepatocellular carcinoma. EMBO J. 2015, 34, 2671–2685. [CrossRef]
109. Lin, C.; Zhang, S.; Wang, Y.; Wang, Y.; Nice, E.; Guo, C.; Zhang, E.; Yu, L.; Li, M.; Liu, C.; et al. Functional Role of a Novel LongNoncoding RNA TTN-AS1 in Esophageal Squamous Cell Carcinoma Progression and Metastasis. Clin. Cancer Res. 2018, 24,486–498. [CrossRef]
110. Wang, L.; Bin Li, B.; Yi, X.; Xiao, X.; Zheng, Q.; Ma, L. Circ_0036412 affects the proliferation and cell cycle of hepatocellularcarcinoma via hedgehog signaling pathway. J. Transl. Med. 2022, 20, 154. [CrossRef]
111. Xu, C.Z.; Jiang, C.; Wu, Q.; Liu, L.; Yan, X.; Shi, R. A Feed-Forward Regulatory Loop between HuR and the Long NoncodingRNA HOTAIR Promotes Head and Neck Squamous Cell Carcinoma Progression and Metastasis. Cell Physiol Biochem 2016, 40,1039–1051. [CrossRef] [PubMed]
112. Keniry, A.; Oxley, D.; Monnier, P.; Kyba, M.; Dandolo, L.; Smits, G.; Reik, W. The H19 lincRNA is a developmental reservoir ofmiR-675 that suppresses growth and Igf1r. Nat. Cell Biol. 2012, 14, 659–665. [CrossRef] [PubMed]
113. Zheng, Z.; Wu, D.; Fan, S.; Zhang, Z.; Chen, G.; Lu, J. Upregulation of miR-675-5p induced by lncRNA H19 was associated withtumor progression and development by targeting tumor suppressor p53 in non–small cell lung cancer. J. Cell. Biochem. 2019, 120,18724–18735. [CrossRef] [PubMed]
114. Zhu, M.; Chen, Q.; Liu, X.; Sun, Q.; Zhao, X.; Deng, R.; Wang, Y.; Huang, J.; Xu, M.; Yan, J.; et al. lncRNA H19/miR-675 axisrepresses prostate cancer metastasis by targeting TGFBI. FEBS J. 2014, 281, 3766–3775. [CrossRef] [PubMed]
115. Gunzburg, M.J.; Sivakumaran, A.; Pendini, N.R.; Yoon, J.-H.; Gorospe, M.; Wilce, M.C.; A Wilce, J. Cooperative interplay of let-7mimic and HuR with MYC RNA. Cell Cycle 2015, 14, 2729–2733. [CrossRef] [PubMed]
116. Kim, H.H.; Kuwano, Y.; Srikantan, S.; Lee, E.K.; Martindale, J.L.; Gorospe, M. HuR recruits let-7/RISC to repress c-Myc expression.Genes Dev. 2009, 23, 1743–1748. [CrossRef]
117. Dhanasekaran, R.; Deutzmann, A.; Mahauad-Fernandez, W.D.; Hansen, A.S.; Gouw, A.M.; Felsher, D.W. The MYC oncogene—the grand orchestrator of cancer growth and immune evasion. Nat. Rev. Clin. Oncol. 2022, 19, 23–36. [CrossRef]
118. Wang, Y.; Mo, Y.; Wang, L.; Su, P.; Xie, Y. Let-7b contributes to hepatocellular cancer progression through Wnt/β-catenin signaling.Saudi J. Biol. Sci. 2018, 25, 953–958. [CrossRef]
119. Han, X.; Zhang, J.-J.; Han, Z.-Q.; Zhang, H.-B.; Wang, Z.-A. Correction: Let-7b attenuates cisplatin resistance and tumor growth ingastric cancer by targeting AURKB. Cancer Gene Ther. 2019, 26, 256. [CrossRef]
120. Chen, F.; Chen, C.; Yang, S.; Gong, W.; Wang, Y.; Cianflone, K.; Tang, J.; Wang, D.W. Let-7b Inhibits Human Cancer Phenotype byTargeting Cytochrome P450 Epoxygenase 2J2. PLoS ONE 2012, 7, e39197. [CrossRef]
121. Han, X.; Chen, Y.; Yao, N.; Liu, H.; Wang, Z. MicroRNA let-7b suppresses human gastric cancer malignancy by targeting ING1.Cancer Gene Ther. 2015, 22, 122–129. [CrossRef] [PubMed]
Cancers 2022, 14, 3516 26 of 30
122. Yoon, J.-H.; Abdelmohsen, K.; Srikantan, S.; Yang, X.; Martindale, J.L.; De, S.; Huarte, M.; Zhan, M.; Becker, K.G.; Gorospe, M.LincRNA-p21 Suppresses Target mRNA Translation. Mol. Cell 2012, 47, 648–655. [CrossRef] [PubMed]
123. Leucci, E.; Zriwil, A.; Gregersen, L.H.; Jensen, K.T.; Obad, S.; Bellan, C.; Leoncini, L.; Kauppinen, S.; Lund, A.H. Inhibition ofmiR-9 de-represses HuR and DICER1 and impairs Hodgkin lymphoma tumour outgrowth in vivo. Oncogene 2012, 31, 5081–5089.[CrossRef] [PubMed]
124. Thorne, J.L.; Battaglia, S.; Baxter, D.E.; Hayes, J.L.; Hutchinson, S.A.; Jana, S.; Millican-Slater, R.A.; Smith, L.; Teske, M.C.; Wastall,L.M.; et al. MiR-19b non-canonical binding is directed by HuR and confers chemosensitivity through regulation of P-glycoproteinin breast cancer. Biochim. Biophys. Acta Gene Regul. Mech. 2018, 1861, 996–1006. [CrossRef] [PubMed]
125. Glorian, V.; Maillot, G.; Polès, S.; Iacovoni, J.S.; Favre, G.; Vagner, S. HuR-dependent loading of miRNA RISC to the mRNAencoding the Ras-related small GTPase RhoB controls its translation during UV-induced apoptosis. Cell Death Differ. 2011, 18,1692–1701. [CrossRef] [PubMed]
126. da Silva, G.H.G.; dos Santos, M.G.P.; Nagasse, H.Y.; Coltri, P.P. Human Antigen R (HuR) Facilitates miR-19 Synthesis and AffectsCellular Kinetics in Papillary Thyroid Cancer. Cell. Physiol. Biochem. 2022, 56, 105–119. [CrossRef]
127. Zhou, B.; Xu, J.; Chen, Y.; Gao, S.; Feng, X.; Lu, X. miR-200b/c-RAP1B axis represses tumorigenesis and malignant progression ofpapillary thyroid carcinoma through inhibiting the NF-κB/Twist1 pathway. Exp. Cell Res. 2020, 387, 111785. [CrossRef]
128. Shi, Y.; Wang, Z.; Zhu, X.; Chen, L.; Ma, Y.; Wang, J.; Yang, X.; Liu, Z. Exosomal miR-1246 in serum as a potential biomarker forearly diagnosis of gastric cancer. Int. J. Clin. Oncol. 2020, 25, 89–99. [CrossRef]
129. Peng, W.; Li, J.; Chen, R.; Gu, Q.; Yang, P.; Qian, W.; Ji, D.; Wang, Q.; Zhang, Z.; Tang, J.; et al. Upregulated METTL3 promotesmetastasis of colorectal Cancer via miR-1246/SPRED2/MAPK signaling pathway. J. Exp. Clin. Cancer Res. 2019, 38, 393.[CrossRef]
130. Guo, S.; Chen, J.; Chen, F.; Zeng, Q.; Liu, W.-L.; Zhang, G. Exosomes derived from Fusobacterium nucleatum-infected colorectalcancer cells facilitate tumour metastasis by selectively carrying miR-1246/92b-3p/27a-3p and CXCL16. Gut 2020, 70, 1507–1519.[CrossRef]
131. Si, G.; Li, S.; Zheng, Q.; Zhu, S.; Zhou, C. miR-1246 shuttling from fibroblasts promotes colorectal cancer cell migration. Neoplasma2021, 68, 317–324. [CrossRef] [PubMed]
132. Del Vecchio, G.; De Vito, F.; Saunders, S.J.; Risi, A.; Mannironi, C.; Bozzoni, I.; Presutti, C. RNA-binding protein HuR andthe members of the miR-200 family play an unconventional role in the regulation of c-Jun mRNA. RNA 2016, 22, 1510–1521.[CrossRef] [PubMed]
133. Prislei, S.; Martinelli, E.; Mariani, M.; Raspaglio, G.; Sieber, S.; Ferrandina, G.; Shahabi, S.; Scambia, G.; Ferlini, C. MiR-200c andHuR in ovarian cancer. BMC Cancer 2013, 13, 72. [CrossRef] [PubMed]
134. Tian, Z.; Luo, Y.; Zhu, J.; Hua, X.; Xu, J.; Huang, C.; Jin, H.; Huang, H.; Huang, C. Transcriptionally elevation of miR-494 by newChlA-F compound via a HuR/JunB axis inhibits human bladder cancer cell invasion. Biochim. Biophys. Acta Gene Regul. Mech.2019, 1862, 822–833. [CrossRef]
135. Rossi, F.; Beltran, M.; Damizia, M.; Grelloni, C.; Colantoni, A.; Setti, A.; Di Timoteo, G.; Dattilo, D.; Centrón-Broco, A.; Nicoletti,C.; et al. Circular RNA ZNF609/CKAP5 mRNA interaction regulates microtubule dynamics and tumorigenicity. Mol. Cell 2022,82, 75–89.e9. [CrossRef] [PubMed]
136. Han, J.; Qu, H.; Han, M.; Ding, Y.; Xie, M.; Hu, J.; Chen, Y.; Dong, H. MSC-induced lncRNA AGAP2-AS1 promotes stemness andtrastuzumab resistance through regulating CPT1 expression and fatty acid oxidation in breast cancer. Oncogene 2021, 40, 833–847.[CrossRef]
137. Shi, J.; Guo, C.; Ma, J. CCAT2 enhances autophagy-related invasion and metastasis via regulating miR-4496 and ELAVL1 inhepatocellular carcinoma. J. Cell. Mol. Med. 2021, 25, 8985–8996. [CrossRef]
138. Li, X.; Wang, C.; Chen, G.; Zou, W.; Deng, Y.; Zhou, F. EIF4A3-induced circCCNB1 (hsa_circ_0001495) promotes glioma progressionby elevating CCND1 through interacting miR-516b-5p and HuR. Metab. Brain Dis. 2022, 37, 819–833. [CrossRef]
139. D’Angelo, D.; Arra, C.; Fusco, A. RPSAP52 lncRNA Inhibits p21Waf1/CIP Expression by Interacting With the RNA BindingProtein HuR. Oncol. Res. Featur. Preclin. Clin. Cancer Ther. 2020, 28, 191–201. [CrossRef]
140. Ehses, J.; Fernández-Moya, S.M.; Schröger, L.; Kiebler, M.A. Synergistic regulation of Rgs4 mRNA by HuR and miR-26/RISC inneurons. RNA Biol. 2021, 18, 988–998. [CrossRef]
141. Taylor, G.A.; Lai, W.S.; Oakey, R.J.; Seldin, M.F.; Shows, T.B.; Eddy, R.L.; Blackshear, P.J. The human TTP protein: Sequence,alignment with related proteins, and chromosomal localization of the mouse and human genes. Nucleic Acids Res. 1991, 19, 3454.[CrossRef] [PubMed]
142. Varnum, B.C.; Ma, Q.F.; Chi, T.H.; Fletcher, B.; Herschman, H.R. The TIS11 primary response gene is a member of a gene familythat encodes proteins with a highly conserved sequence containing an unusual Cys-His repeat. Mol. Cell. Biol. 1991, 11, 1754–1758.[CrossRef] [PubMed]
143. Saini, Y.; Chen, J.; Patial, S. The Tristetraprolin Family of RNA-Binding Proteins in Cancer: Progress and Future Prospects. Cancers2020, 12, 1539. [CrossRef]
144. Ogawa, K.; Chen, F.; Kim, Y.-J.; Chen, Y. Transcriptional Regulation of Tristetraprolin by Transforming Growth Factor-β in HumanT Cells. J. Biol. Chem. 2003, 278, 30373–30381. [CrossRef] [PubMed]
145. Blanco, F.F.; Sanduja, S.; Deane, N.G.; Blackshear, P.; Dixon, D.A. Transforming Growth Factor β Regulates P-Body Formationthrough Induction of the mRNA Decay Factor Tristetraprolin. Mol. Cell. Biol. 2014, 34, 180–195. [CrossRef]
Cancers 2022, 14, 3516 27 of 30
146. Chen, Y.-L.; Jiang, Y.-W.; Su, Y.-L.; Lee, S.-C.; Chang, M.-S.; Chang, C.-J. Transcriptional regulation of tristetraprolin by NF-κBsignaling in LPS-stimulated macrophages. Mol. Biol. Rep. 2013, 40, 2867–2877. [CrossRef]
147. Lai, W.S.; Stumpo, D.J.; Blackshear, P.J. Rapid insulin-stimulated accumulation of an mRNA encoding a proline-rich protein. J.Biol. Chem. 1990, 265, 16556–16563. [CrossRef]
148. Cao, H.; Urban, J.F.; Anderson, R.A. Insulin Increases Tristetraprolin and Decreases VEGF Gene Expression in Mouse 3T3-L1Adipocytes. Obesity 2008, 16, 1208–1218. [CrossRef]
149. Carballo, E.; Blackshear, P. Roles of tumor necrosis factor-α receptor subtypes in the pathogenesis of the tristetraprolin-deficiencysyndrome. Blood 2001, 98, 2389–2395. [CrossRef]
150. Sanduja, S.; Blanco, F.F.; Young, L.E.; Kaza, V.; Dixon, D.A. The role of tristetraprolin in cancer and inflammation. Front. Biosci.2012, 17, 174–188. [CrossRef]
151. A Taylor, G.; Carballo, E.; Lee, D.M.; Lai, W.S.; Thompson, M.J.; Patel, D.D.; I Schenkman, D.; Gilkeson, G.S.; E Broxmeyer, H.;Haynes, B.F.; et al. A Pathogenetic Role for TNFα in the Syndrome of Cachexia, Arthritis, and Autoimmunity Resulting fromTristetraprolin (TTP) Deficiency. Immunity 1996, 4, 445–454. [CrossRef]
152. Dolicka, D.; Sobolewski, C.; Gjorgjieva, M.; de Sousa, M.C.; Berthou, F.; De Vito, C.; Colin, D.J.; Bejuy, O.; Fournier, M.; Maeder, C.;et al. Tristetraprolin Promotes Hepatic Inflammation and Tumor Initiation but Restrains Cancer Progression to Malignancy. Cell.Mol. Gastroenterol. Hepatol. 2021, 11, 597–621. [CrossRef] [PubMed]
153. Jing, Q.; Huang, S.; Guth, S.; Zarubin, T.; Motoyama, A.; Chen, J.; Di Padova, F.; Lin, S.-C.; Gram, H.; Han, J. Involvement ofMicroRNA in AU-Rich Element-Mediated mRNA Instability. Cell 2005, 120, 623–634. [CrossRef] [PubMed]
154. Kim, C.W.; Vo, M.-T.; Kim, H.K.; Lee, H.H.; Yoon, N.A.; Lee, B.J.; Min, Y.J.; Joo, W.D.; Cha, H.J.; Park, J.W.; et al. Ectopicover-expression of tristetraprolin in human cancer cells promotes biogenesis of let-7 by down-regulation of Lin28. Nucleic AcidsRes. 2012, 40, 3856–3869. [CrossRef] [PubMed]
155. Lee, J.Y.; Kim, H.J.; Yoon, N.A.; Lee, W.H.; Min, Y.J.; Ko, B.K.; Lee, B.J.; Lee, A.; Cha, H.J.; Cho, W.J.; et al. Tumor suppressorp53 plays a key role in induction of both tristetraprolin and let-7 in human cancer cells. Nucleic Acids Res. 2013, 41, 5614–5625.[CrossRef] [PubMed]
156. Sobolewski, C.; Sanduja, S.; Blanco, F.F.; Hu, L.; Dixon, D.A. Histone Deacetylase Inhibitors Activate Tristetraprolin Expressionthrough Induction of Early Growth Response Protein 1 (EGR1) in Colorectal Cancer Cells. Biomolecules 2015, 5, 2035–2055.[CrossRef] [PubMed]
157. Lam, S.S.N.; Ip, C.K.M.; Mak, A.S.C.; Wong, A.S.T. A novel p70 S6 kinase-microRNA biogenesis axis mediates multicellularspheroid formation in ovarian cancer progression. Oncotarget 2016, 7, 38064–38077. [CrossRef]
158. Bhattacharyya, S.; Kumar, P.; Tsuchiya, M.; Bhattacharyya, A.; Biswas, R. Regulation of miR-155 biogenesis in cystic fibrosis lungepithelial cells: Antagonistic role of two mRNA-destabilizing proteins, KSRP and TTP. Biochem. Biophys. Res. Commun. 2013, 433,484–488. [CrossRef]
159. Liu, H.; Han, L.; Liu, Z.; Gao, N. Long noncoding RNA MNX1-AS1 contributes to lung cancer progression through the miR-527/BRF2 pathway. J. Cell. Physiol. 2019, 234, 13843–13850. [CrossRef]
160. Goutas, D.; Pergaris, A.; Giaginis, C.; Theocharis, S. HuR as Therapeutic Target in Cancer: What the Future Holds. Curr. Med.Chem. 2022, 29, 56–65. [CrossRef]
161. Li, Q.; Tong, D.; Guo, C.; Wu, F.; Li, F.; Wang, X.; Jiang, Q.; Wei, Y.; Liu, L.; Ni, L.; et al. MicroRNA-145 suppresses gastric cancerprogression by targeting Hu-antigen R. Am. J. Physiol. Cell Physiol. 2020, 318, C605–C614. [CrossRef] [PubMed]
162. Zhou, N.; Zhou, Y.; Tang, Y.; Yu, W. [MiR-519 inhibits gastric cancer cell activity through regulation of HuR expression]. ZhongNan Da Xue Xue Bao Yi Xue Ban 2016, 41, 19–23. [CrossRef] [PubMed]
163. Xie, M.; Yu, T.; Jing, X.; Ma, L.; Fan, Y.; Yang, F.; Ma, P.; Jiang, H.; Wu, X.; Shu, Y.; et al. Exosomal circSHKBP1 promotes gastriccancer progression via regulating the miR-582-3p/HUR/VEGF axis and suppressing HSP90 degradation. Mol. Cancer 2020, 19,112. [CrossRef] [PubMed]
164. Wang, Z.; Chen, K.; Li, D.; Chen, M.; Li, A.; Wang, J. miR-140-3p is involved in the occurrence and metastasis of gastric cancer byregulating the stability of FAM83B. Cancer Cell Int. 2021, 21, 537. [CrossRef] [PubMed]
165. Andrieu, N.A.; Motiño, O.; Mayoral, R.; Izquierdo, C.L.; Fernández-Alvarez, A.; Boscá, L.; Casado, M.; Martín-Sanz, P.Cyclooxygenase-2 Is a Target of MicroRNA-16 in Human Hepatoma Cells. PLoS ONE 2012, 7, e50935. [CrossRef]
166. Xue, F.; Li, Q.R.; Xu, Y.H.; Bin Zhou, H. MicroRNA-139-3p Inhibits The Growth And Metastasis Of Ovarian Cancer By InhibitingELAVL1. Onco. Targets Ther. 2019, 12, 8935–8945. [CrossRef]
167. Abdelmohsen, K.; Kim, M.M.; Srikantan, S.; Mercken, E.M.; Brennan, S.E.; Wilson, G.; de Cabo, R.; Gorospe, M. miR-519suppresses tumor growth by reducing HuR levels. Cell Cycle 2010, 9, 1354–1359. [CrossRef]
168. Abdelmohsen, K.; Srikantan, S.; Kuwano, Y.; Gorospe, M. miR-519 reduces cell proliferation by lowering RNA-binding proteinHuR levels. Proc. Natl. Acad. Sci. USA 2008, 105, 20297–20302. [CrossRef]
169. Wu, D.; Wang, B.; Shang, J.; Song, J.; Zhang, H. miR-31 Reduces Cell Growth of Papillary Thyroid Carcinoma by RNA-BindingProtein HuR. Clin. Lab. 2015, 61, 1625–1634. [CrossRef]
170. Schultz, C.W.; Preet, R.; Dhir, T.; Dixon, D.A.; Brody, J.R. Understanding and targeting the disease-related RNA binding proteinhuman antigen R (HuR). Wiley Interdiscip. Rev. RNA 2020, 11, e1581. [CrossRef]
171. Garinet, S.; Wang, P.; Mansuet-Lupo, A.; Fournel, L.; Wislez, M.; Blons, H. Updated Prognostic Factors in Localized NSCLC.Cancers 2022, 14, 1400. [CrossRef] [PubMed]
Cancers 2022, 14, 3516 28 of 30
172. Ni, Z.-Z.; He, J.-K.; Tang, X.; Tao, Z.; Zhang, Y.; Xie, B. Identification of ELAVL1 gene and miRNA-139-3p involved in theaggressiveness of NSCLC. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 9453–9464. [CrossRef] [PubMed]
173. Iacona, J.R.; Monteleone, N.J.; Lemenze, A.D.; Cornett, A.L.; Lutz, C.S. Transcriptomic studies provide insights into the tumorsuppressive role of miR-146a-5p in non-small cell lung cancer (NSCLC) cells. RNA Biol. 2019, 16, 1721–1732. [CrossRef]
174. Xu, H.; Ma, J.; Zheng, J.; Wu, J.; Qu, C.; Sun, F.; Xu, S. MiR-31 Functions as a Tumor Suppressor in Lung Adenocarcinoma Mainlyby Targeting HuR. Clin. Lab. 2016, 62, 711–718. [CrossRef]
175. Liu, Y.; Chen, X.; Cheng, R.; Yang, F.; Yu, M.; Wang, C.; Cui, S.; Hong, Y.; Liang, H.; Liu, M.; et al. The Jun/miR-22/HuR regulatoryaxis contributes to tumourigenesis in colorectal cancer. Mol. Cancer 2018, 17, 11. [CrossRef] [PubMed]
176. Gu, C.; Zhang, M.; Sun, W.; Dong, C. Upregulation of miR-324-5p Inhibits Proliferation and Invasion of Colorectal Cancer Cellsby Targeting ELAVL1. Oncol. Res. Featur. Preclin. Clin. Cancer Ther. 2019, 27, 515–524. [CrossRef] [PubMed]
177. To, K.K.; Leung, W.; Ng, S.S. Exploiting a novel miR-519c–HuR–ABCG2 regulatory pathway to overcome chemoresistance incolorectal cancer. Exp. Cell Res. 2015, 338, 222–231. [CrossRef] [PubMed]
178. Al-Haidari, A.; Algaber, A.; Madhi, R.; Syk, I.; Thorlacius, H. MiR-155-5p controls colon cancer cell migration via post-transcriptional regulation of Human Antigen R (HuR). Cancer Lett. 2018, 421, 145–151. [CrossRef]
179. Wang, D.-D.; Sun, D.-L.; Yang, S.-P.; Song, J.; Wu, M.-Y.; Niu, W.-W.; Song, M.; Zhang, X.-L. Long noncoding RNA TNFRSF10A-AS1promotes colorectal cancer through upregulation of HuR. World J. Gastroenterol. 2022, 28, 2184–2200. [CrossRef]
180. Fan, M.; He, P.; Lin, X.; Yang, C.; Li, C.; Xing, L. MicroRNA -324-5p affects the radiotherapy response of cervical cancer viatargeting ELAV-like RNA binding protein 1. Kaohsiung J. Med Sci. 2020, 36, 965–972. [CrossRef]
181. Marasa, B.S.; Srikantan, S.; Martindale, J.L.; Kim, M.M.; Lee, E.K.; Gorospe, M.; Abdelmohsen, K. MicroRNA profiling in humandiploid fibroblasts uncovers miR-519 role in replicative senescence. Aging 2010, 2, 333–343. [CrossRef] [PubMed]
182. Balkhi, M.Y.; Iwenofu, O.H.; Bakkar, N.; Ladner, K.J.; Chandler, D.S.; Houghton, P.J.; London, C.A.; Kraybill, W.; Perrotti, D.;Croce, C.M.; et al. miR-29 Acts as a Decoy in Sarcomas to Protect the Tumor Suppressor A20 mRNA from Degradation by HuR.Sci. Signal. 2013, 6, ra63. [CrossRef] [PubMed]
183. Pan, B.; Zhao, M.; Xu, L. Long noncoding RNA gastric cancer-associated transcript 3 plays oncogenic roles in glioma throughsponging miR-3127-5p. J. Cell. Physiol. 2019, 234, 8825–8833. [CrossRef]
184. Yang, W.; Yu, H.; Shen, Y.; Liu, Y.; Yang, Z.; Sun, T. MiR-146b-5p overexpression attenuates stemness and radioresistance of gliomastem cells by targeting HuR/lincRNA-p21/β-catenin pathway. Oncotarget 2016, 7, 41505–41526. [CrossRef] [PubMed]
185. Xu, F.; Zhang, X.; Lei, Y.; Liu, X.; Liu, Z.; Tong, T.; Wang, W. Loss of Repression of HuR Translation by miR-16 May Be Responsiblefor the Elevation of HuR in Human Breast Carcinoma. J. Cell. Biochem. 2010, 111, 727–734. [CrossRef] [PubMed]
186. Guo, X.; Wu, Y.; Hartley, R. MicroRNA-125a represses cell growth by targeting HuR in breast cancer. RNA Biol. 2009, 6, 575–583.[CrossRef]
187. Ren, L.; Li, Y.; Zhao, Q.; Fan, L.; Tan, B.; Zang, A.; Yang, H. miR-519 regulates the proliferation of breast cancer cells via targetinghuman antigen R. Oncol. Lett. 2020, 19, 1567–1576. [CrossRef]
188. Al-Ahmadi, W.; Al-Ghamdi, M.; Al-Souhibani, N.; Khabar, K.S. miR -29a inhibition normalizes HuR over-expression and aberrantAU -rich mRNA stability in invasive cancer. J. Pathol. 2013, 230, 28–38. [CrossRef]
189. Sun, J.; Xu, Y.; Zhou, H.; Zhang, A.; Qi, H. Levels, occurrence and human exposure to novel brominated flame retardants (NBFRs)and Dechlorane Plus (DP) in dust from different indoor environments in Hangzhou, China. Sci. Total Environ. 2018, 631-632,1212–1220. [CrossRef]
190. Liu, H.; Song, X.; Hou, J.; Zhao, Z.; Chang, J. Posttranscriptional Regulation of Human Antigen R by miR-133b EnhancesDocetaxel Cytotoxicity Through the Inhibition of ATP-Binding Cassette Subfamily G Member 2 in Prostate Cancer Cells. DNACell Biol. 2018, 37, 210–219. [CrossRef]
191. Kojima, K.; Fujita, Y.; Nozawa, Y.; Deguchi, T.; Ito, M. MiR-34a attenuates paclitaxel-resistance of hormone-refractory prostatecancer PC3 cells through direct and indirect mechanisms. Prostate 2010, 70, 1501–1512. [CrossRef]
192. Hu, W.; Li, H.; Wang, S. LncRNA SNHG7 promotes the proliferation of nasopharyngeal carcinoma by miR-514a-5p/ELAVL1 axis.BMC Cancer 2020, 20, 376. [CrossRef] [PubMed]
193. House, R.; Majumder, M.; Janakiraman, H.; Ogretmen, B.; Kato, M.; Erkul, E.; Hill, E.; Atkinson, C.; Barth, J.; Day, T.A.; et al.Smoking-induced control of miR-133a-3p alters the expression of EGFR and HuR in HPV-infected oropharyngeal cancer. PLoSONE 2018, 13, e0205077. [CrossRef]
194. Shen, Z.; Zhan, G.; Deng, H.; Ren, Y.; Ye, D.; Xiao, B.; Guo, J. MicroRNA-519a demonstrates significant tumour suppressiveactivity in laryngeal squamous cells by targeting anti-carcinoma HuR gene. J. Laryngol. Otol. 2013, 127, 1194–1202. [CrossRef]
195. Shen, Z.; Zhan, G.; Deng, H.; Kang, C.; Guo, J. Growth inhibitory effect of microRNA-519b-3p on larynx squamous Hep-2 cells.Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi = CN. J. Otorhinolaryngol. Head Neck Surg. 2014, 49, 151–156.
196. Huang, K.; Dong, B.; Wang, Y.; Tian, T.; Zhang, B. MicroRNA-519 enhances HL60 human acute myeloid leukemia cell lineproliferation by reducing the expression level of RNA-binding protein human antigen R. Mol. Med. Rep. 2015, 12, 7830–7836.[CrossRef] [PubMed]
197. Alemdehy, M.F.; Haanstra, J.R.; de Looper, H.W.J.; van Strien, P.M.H.; Verhagen-Oldenampsen, J.; Caljouw, Y.; Sanders, M.A.;Hoogenboezem, R.; de Ru, A.H.; Janssen, G.M.C.; et al. ICL-induced miR139-3p and miR199a-3p have opposite roles inhematopoietic cell expansion and leukemic transformation. Blood 2015, 125, 3937–3948. [CrossRef] [PubMed]
Cancers 2022, 14, 3516 29 of 30
198. Wang, L.-J.; Chiou, J.-T.; Lee, Y.-C.; Chang, L.-S. Docetaxel-triggered SIDT2/NOX4/JNK/HuR signaling axis is associated withTNF-α-mediated apoptosis of cancer cells. Biochem. Pharmacol. 2022, 195, 114865. [CrossRef] [PubMed]
199. Peng, Y.; Song, X.; Lan, J.; Wang, X.; Wang, M. Bone marrow stromal cells derived exosomal miR-10a and miR-16 may be involvedin progression of patients with multiple myeloma by regulating EPHA8 or IGF1R/CCND1. Medicine 2021, 100, e23447. [CrossRef]
200. Mariotti, B.; Calabretto, G.; Rossato, M.; Teramo, A.; Castellucci, M.; Barilà, G.; Leoncin, M.; Vicenzetto, C.; Facco, M.; Semenzato,G.; et al. Identification of a miR-146b-Fas ligand axis in the development of neutropenia in T large granular lymphocyte leukemia.Haematologica 2020, 105, 1351–1360. [CrossRef]
201. Mihailovich, M.; Bremang, M.; Spadotto, V.; Musiani, D.; Vitale, E.; Varano, G.; Zambelli, F.; Mancuso, F.; Cairns, D.A.; Pavesi, G.;et al. miR-17-92 fine-tunes MYC expression and function to ensure optimal B cell lymphoma growth. Nat. Commun. 2015, 6, 8725.[CrossRef]
202. Sohn, B.H.; Park, I.Y.; Lee, J.J.; Yang, S.; Jang, Y.J.; Park, K.C.; Kim, D.J.; Lee, D.C.; Sohn, H.A.; Kim, T.W.; et al. FunctionalSwitching of TGF-β1 Signaling in Liver Cancer via Epigenetic Modulation of a Single CpG Site in TTP Promoter. Gastroenterology2010, 138, 1898–1908.e12. [CrossRef] [PubMed]
203. Al-Souhibani, N.; Al-Ghamdi, M.; Al-Ahmadi, W.; Khabar, K.S. Posttranscriptional control of the chemokine receptor CXCR4expression in cancer cells. Carcinogenesis 2014, 35, 1983–1992. [CrossRef]
204. Sun, X.-J.; Liu, B.-Y.; Yan, S.; Jiang, T.-H.; Cheng, H.-Q.; Jiang, H.-S.; Cao, Y.; Mao, A.-W. MicroRNA-29a Promotes PancreaticCancer Growth by Inhibiting Tristetraprolin. Cell. Physiol. Biochem. 2015, 37, 707–718. [CrossRef]
205. Wang, J.-Y.; Zhang, Q.; Wang, D.-D.; Yan, W.; Sha, H.-H.; Zhao, J.-H.; Yang, S.-J.; Zhang, H.-D.; Hou, J.-C.; Xu, H.-Z.; et al. MiR-29a:A potential therapeutic target and promising biomarker in tumors. Biosci. Rep. 2018, 38. [CrossRef]
206. Mao, Y.; Lv, M.; Cao, W.; Liu, X.; Cui, J.; Wang, Y.; Wang, Y.; Nie, G.; Liu, X.; Wang, H. Circular RNA 000554 represses epithelial-mesenchymal transition in breast cancer by regulating microRNA-182/ZFP36 axis. FASEB J. 2020, 34, 11405–11420. [CrossRef][PubMed]
207. De Luca, L.; Trino, S.; Laurenzana, I.; Tagliaferri, D.; Falco, G.; Grieco, V.; Bianchino, G.; Nozza, F.; Campia, V.; D’Alessio, F.; et al.Knockdown of miR-128a induces Lin28a expression and reverts myeloid differentiation blockage in acute myeloid leukemia. CellDeath Dis. 2017, 8, e2849. [CrossRef] [PubMed]
208. Wang, J.; Pu, J.; Zhang, Y.; Yao, T.; Luo, Z.; Li, W.; Xu, G.; Liu, J.; Wei, W.; Deng, Y. Exosome-transmitted long non-coding RNASENP3-EIF4A1 suppresses the progression of hepatocellular carcinoma. Aging 2020, 12, 11550–11567. [CrossRef]
209. Perdigão-Henriques, R.; Petrocca, F.; Altschuler, G.; Thomas, M.P.; LE, T.N.M.; Tan, S.M.; Hide, W.; A Lieberman, J. miR-200promotes the mesenchymal to epithelial transition by suppressing multiple members of the Zeb2 and Snail1 transcriptionalrepressor complexes. Oncogene 2016, 35, 158–172. [CrossRef]
210. Feng, X.; Zhou, S.; Cai, W.; Guo, J. The miR-93-3p/ZFP36L1/ZFX axis regulates keratinocyte proliferation and migration duringskin wound healing. Mol. Ther. Nucleic Acids 2021, 23, 450–463. [CrossRef]
211. Guo, X.; Piao, H.; Zhang, Y.; Sun, P.; Yao, B. Overexpression of microRNA-129-5p in glioblastoma inhibits cell proliferation,migration, and colony-forming ability by targeting ZFP36L1. Bosn. J. Basic Med Sci. 2020, 20, 459–470. [CrossRef] [PubMed]
212. Kou, Z.; Liu, H.; Wang, Y.-C.; Huang, Q.; Wang, Z.-S.; Gu, Z.-L.N.E.; Lang, T.; Nie, Y.-L.; An, L.; Li A, Z.-G.; et al. Expression Leveland Target Gene Prediction of miR-181b in Patients with Chronic Lymphocytic Leukemia. Zhongguo Shi Yan Xue Ye Xue Za Zhi2020, 28, 808–814. [CrossRef] [PubMed]
213. Yonemori, K.; Seki, N.; Kurahara, H.; Osako, Y.; Idichi, T.; Arai, T.; Koshizuka, K.; Kita, Y.; Maemura, K.; Natsugoe, S. ZFP36L2promotes cancer cell aggressiveness and is regulated by antitumor microRNA-375 in pancreatic ductal adenocarcinoma. CancerSci. 2017, 108, 124–135. [CrossRef] [PubMed]
214. Wang, L.; Qu, J.; Zhou, L.; Liao, F.; Wang, J. MicroRNA-373 Inhibits Cell Proliferation and Invasion via Targeting BRF2 in HumanNon-small Cell Lung Cancer A549 Cell Line. Cancer Res. Treat. 2018, 50, 936–949. [CrossRef]
215. Li, Y.; Dong, R.; Lu, M.; Cheng, C.; Feng, Z.; Zhao, R.; Liang, J.; Han, J.; Jiang, J.; Xu-Welliver, M.; et al. Let-7b-3p inhibits tumorgrowth and metastasis by targeting the BRF2-mediated MAPK/ERK pathway in human lung adenocarcinoma. Transl. LungCancer Res. 2021, 10, 1841–1856. [CrossRef]
216. Qu, Y.-L.; Wang, H.-F.; Sun, Z.-Q.; Tang, Y.; Han, X.-N.; Yu, X.-B.; Liu, K. Up-regulated miR-155-5p promotes cell proliferation,invasion and metastasis in colorectal carcinoma. Int. J. Clin. Exp. Pathol. 2015, 8, 6988–6994.
217. Cheng, G.; Song, Z.; Liu, Y.; Xiao, H.; Ruan, H.; Cao, Q.; Wang, K.; Xiao, W.; Xiong, Z.; Liu, D.; et al. Long noncoding RNASNHG12 indicates the prognosis of prostate cancer and accelerates tumorigenesis via sponging miR-133b. J. Cell. Physiol. 2020,235, 1235–1246. [CrossRef]
218. Huang, S.; Wa, Q.; Pan, J.; Peng, X.; Ren, D.; Li, Q.; Dai, Y.; Yang, Q.; Huang, Y.; Zhang, X.; et al. Transcriptional downregulationof miR-133b by REST promotes prostate cancer metastasis to bone via activating TGF-β signaling. Cell Death Dis. 2018, 9, 779.[CrossRef]
219. Duan, K.; Ge, Y.-C.; Zhang, X.-P.; Wu, S.-Y.; Feng, J.-S.; Chen, S.-L.; Zhang, L.; Yuan, Z.-H.; Fu, C.-H. miR-34a inhibits cellproliferation in prostate cancer by downregulation of SIRT1 expression. Oncol. Lett. 2015, 10, 3223–3227. [CrossRef]
220. Russo, A.; Potenza, N. Antiproliferative Activity of microRNA-125a and its Molecular Targets. MicroRNA 2019, 8, 173–179.[CrossRef]
221. Fontana, A.; Barbano, R.; Dama, E.; Pasculli, B.; Rendina, M.; Morritti, M.G.; Melocchi, V.; Castelvetere, M.; Valori, V.M.; Ravaioli,S.; et al. Combined analysis of miR-200 family and its significance for breast cancer. Sci. Rep. 2021, 11, 2980. [CrossRef] [PubMed]
Cancers 2022, 14, 3516 30 of 30
222. Niu, M.; Feng, Y.; Zhang, N.; Shao, T.; Zhang, H.; Wang, R.; Yao, Y.; Yao, R.; Wu, Q.; Cao, J.; et al. High expression of miR-25predicts favorable chemotherapy outcome in patients with acute myeloid leukemia. Cancer Cell Int. 2019, 19, 122. [CrossRef][PubMed]
223. Paczkowska, J.; Giefing, M. MicroRNA signature in classical Hodgkin lymphoma. J. Appl. Genet. 2021, 62, 281–288. [CrossRef]224. Li, X.; Zeng, L.; Cao, C.; Lu, C.; Lian, W.; Han, J.; Zhang, X.; Zhang, J.; Tang, T.; Li, M. Long noncoding RNA MALAT1 regulates
renal tubular epithelial pyroptosis by modulated miR-23c targeting of ELAVL1 in diabetic nephropathy. Exp. Cell Res. 2017, 350,327–335. [CrossRef] [PubMed]
225. Shwetha, S.; Sharma, G.; Raheja, H.; Goel, A.; Aggarwal, R.; Das, S. Interaction of miR-125b-5p with Human antigen R mRNA:Mechanism of controlling HCV replication. Virus Res. 2018, 258, 1–8. [CrossRef]
226. Wang, J.; Hjelmeland, A.B.; Nabors, L.B.; King, P.H. Anti-cancer effects of the HuR inhibitor, MS-444, in malignant glioma cells.Cancer Biol. Ther. 2019, 20, 979–988. [CrossRef]
227. HafezQorani, S.; Lafzi, A.; De Bruin, R.G.; Van Zonneveld, A.J.; Van Der Veer, E.P.; Son, Y.A.; Kazan, H. Modeling the combinedeffect of RNA-binding proteins and microRNAs in post-transcriptional regulation. Nucleic Acids Res. 2016, 44, e83. [CrossRef]