A usage-based analysis of alternating syntactic constructions
Microbial Growth Inhibition by Alternating Electric Fields
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Microbial Growth Inhibition by Alternating Electric Fields
ANTIMICROBIAL AGENTS AND CHEMOTHERAPY, Aug. 2010, p. 3212–3218 Vol. 54, No. 80066-4804/10/$12.00 doi:10.1128/AAC.01841-09Copyright © 2010, American Society for Microbiology. All Rights Reserved.
Microbial Growth Inhibition by Alternating Electric Fields in Micewith Pseudomonas aeruginosa Lung Infection�†
Moshe Giladi,1 Yaara Porat,1 Alexandra Blatt,1 Esther Shmueli,2 Yoram Wasserman,2Eilon D. Kirson,2 and Yoram Palti2,3*
NovoBiotic Limited, Matam Advanced Technology Centre, Haifa 31905, Israel1; NovoCure Limited, Matam Advanced Technology Centre,Haifa 31905, Israel2; and B. Rappaport Faculty of Medicine, Technion-Israel Institute of Technology,
Technion City, Haifa 32000, Israel3
Received 30 December 2009/Returned for modification 21 February 2010/Accepted 31 May 2010
High-frequency, low-intensity electric fields generated by insulated electrodes have previously been shown toinhibit bacterial growth in vitro. In the present study, we tested the effect of these antimicrobial fields(AMFields) on the development of lung infection caused by Pseudomonas aeruginosa in mice. We demonstratethat AMFields (10 MHz) significantly inhibit bacterial growth in vivo, both as a stand-alone treatment and incombination with ceftazidime. In addition, we show that peripheral (skin) heating of about 2°C can contributeto bacterial growth inhibition in the lungs of mice. We suggest that the combination of alternating electricfields, together with the heat produced during their application, may serve as a novel antibacterial treatmentmodality.
The 20th century was the golden era of the antibacterialagents, with millions of people owing their lives to the discov-ery of and treatment with the numerous antibiotic familiesused today. Surely, antibacterial agents will continue to play amajor role in the battle against pathogenic bacteria in the 21stcentury; however, the extensive use of antibiotics holds a threatof a far less optimistic future due to the rapid rise of multidrug-resistant bacteria. Recently, the potential use of physicalmeans as an aid to antibiotics in the battle against bacterialpathogens has been studied: photodynamic therapy (12, 21,35), ultrasound wave therapy (7, 23, 25), thermotherapy (26),and weak electric currents (4, 6, 24, 32, 33) are all being testedas treatment modalities against pathogenic microorganisms.The major drawback of the methods mentioned above is theirlow therapeutic index due to the high levels of heating pro-duced by ultrasonic waves, thermotherapy, and photodynamictherapy (36) and the activated oxygen generated by photody-namic therapy, both of which can damage the tissues in andaround the target area (22). In addition, the use of conductiveelectrodes for the generation of electric currents is associatedwith the release of metal ions and free radicals at the electrodesurface, all of which are toxic to living cells (18). Indeed, as oftoday, none of the above-mentioned means has matured intoan approved treatment modality against bacterial pathogens.
Recently, we demonstrated that low-intensity alternating elec-tric fields of high frequencies (antimicrobial fields [AMFields])have an in vitro inhibitory effect on the growth of pathogenicbacteria, including Staphylococcus aureus and Pseudomonasaeruginosa (8). AMFields were generated using electrically in-
sulated electrodes and therefore were not associated with theproduction of free radicals, toxic metal ions, or electrolysis atthe electrode surface. Fields of the relatively high frequency atwhich the AMFields effects were observed (with an optimumat 10 MHz) have no known effect on human cells (13, 14).Indeed, we found that AMFields have no effect on the growthof cell cultures in vitro (unpublished results). Furthermore, thehigh frequencies of the AMFields allow for the application ofrelatively high intensities without nerve and muscle stimula-tion, and their nonattenuated spread in tissues makes deeptreatment realistic.
In view of the above-described factors, the objective of thepresent study was to test the feasibility of using AMFieldsgenerated by insulated electrodes for the inhibition of P.aeruginosa proliferation in the infected lungs of mice.
MATERIALS AND METHODS
Reagents. Unless stated otherwise, all reagents were purchased from Sigma(Israel). Dehydrated culture medium was purchased from Difco (Difco Labora-tories, Detroit, MI).
Test strains and growth conditions. Pseudomonas aeruginosa strain PAO1 wasa generous gift from Shiri Navon-Venezia (Division of Infectious Diseases,Sourasky Medical Center, Tel Aviv, Israel). Bacteria were grown in LB medium(1.0% Bacto tryptone, 0.5% yeast extract, 1.0% NaCl [Frutarom, Haifa, Israel]).Broth cultures of freshly plated bacteria were grown in 250 ml of liquid mediumat 37°C in an orbital shaker at 220 rpm (New Brunswick Scientific, NJ) up tologarithmic phase, centrifuged, and resuspended in saline containing 15% glyc-erol. Stocks were divided into aliquots of 50 �l each containing 2.17 � 107
CFU/ml and kept at �70°C until use.Experimental animals. All experiments were conducted on 7- to 8-week-old
(body weight, 26 to 35 g) ICR female mice obtained from Harlan Laboratories(Israel). Mice were housed under standard conditions of light and temperatureand were fed standard laboratory chow and water ad libitum. The experimentswere approved by the NovoCure Internal Animal Care and Use Committee inaccordance with the Technion-Israel Institute of Technology guidelines for thecare of laboratory animals.
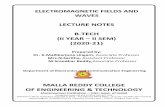
AMFields generation system. AMFields were generated by 2 pairs of parallel,insulated electrodes, 15 mm long and 3 mm high (Fig. 1A) (8). Each electrodecontained a thermistor placed within the epoxy directly on top of the ceramic inorder to allow for constant monitoring of the electrode’s temperature (Fig. 1A).
* Corresponding author. Mailing address: Faculty of Medicine,Technion-Israel Institute of Technology, Technion City, Haifa 32000,Israel. Phone: 972-4-8500232. Fax: 972-4-8501207. E-mail: [email protected].
� Published ahead of print on 14 June 2010.† The authors have paid a fee to allow immediate free access to this
article.
3212
on August 20, 2016 by guest
http://aac.asm.org/
Dow
nloaded from
In order to allow for AMFields generation in mice while maintaining the strictisolation required when working with animals infected with pathogens, the micewere held in an individually ventilated cage system (IVC) (TouchSLIM; Tech-niplast, Italy) that was modified as follows: each cage (GR900; Techniplast, Italy)was split by a polycarbonate partition into two units, each housing one mouse(Fig. 1B). Each mouse was treated with a separate AMFields generator consist-ing of a radiofrequency (RF) amplifier (75A250; AR Worldwide, Souderton, PA)activated by a sine wave generator (model 662; OR-X, Israel) (Fig. 1C). Sixhermetically sealed, shielded electric connection sockets (SM3416 BNC; S.M.electronics, TX) were positioned at the front panel of the cage. Each socketallowed for the connection (by means of coaxial cables) of a connection boxplaced inside the cage to an exterior device—an RF amplifier or a temperaturemeasuring system. The connection box served for transferring the electric cur-rents to the mouse electrodes and the mouse temperature readout to the com-puter.
The entire IVC system, together with the AMFields generating system, wasplaced inside a Faraday cage in order to meet the guidelines for limiting per-sonnel exposure to time-varying electric, magnetic, and electromagnetic fields(International Non-Ionizing Radiation Committee [INIRC]). To avoid field in-terference with temperature measurements, temperatures were measured peri-odically while the field was briefly turned off.
As AMFields are associated with heat production, the electrode surface tem-perature was kept constant at the desired level by computer feedback control ofthe field amplitude. The current source output was switched, every 300 ms,between the two electrode pairs. This interval was found previously to be effec-tive against P. aeruginosa while preventing the formation of temperature gradi-ents that could affect the bacterial growth rate (8). The lung temperature wasmeasured periodically by inserting a thermocouple connected to a temperaturedata logger (TC08 USB; Pico Technology, Cambridgeshire, United Kingdom)into the mouse trachea.
Two control groups were set in each experiment: a sham heat control and anuntreated control (referred to as “control”). Control electrodes identical in sizeand shape to the AMFields electrodes were placed on mice of the two controlgroups. The sham heat electrodes produced temperature changes equal to thoseproduced by the field electrodes by means of a heating resistor incorporatedwithin them. Except for the differences in the electrodes, the control mice andthe sham heat-treated mice were held in conditions identical to those of theAMFields-treated mice (Fig. 1C). The skin temperature of both control groupswas constantly monitored as described above for the AMFields electrodes.
The electric field intensity was measured using a shielded coaxial cable andprobe having two exposed tips positioned at a distance of 1 cm from each other.The probe was connected to a floating input oscilloscope (190B; Fluke, Nether-lands). Field intensities within lungs were measured by making a 5-mm-longincision in the thoracic skin of an anesthetized mouse and inserting the mea-surement probe at an intercostal space to a depth of 5 mm into the thorax. Theprobe was oriented such that the line connecting the two measuring points wasparallel to the lines of the electric field. Field intensities are expressed as peak-to-peak volts per centimeter of distance (V/cm).
Development of P. aeruginosa pulmonary infection in ICR mice. The pulmo-nary infection model of Takeda et al. (31) was used with minor modifications:mice were rendered neutropenic (neutrophil counts, �100/mm3), as described inAndes and Craig (2), by two intraperitoneal injections of cyclophosphamide, onefour days before infection (150 mg/kg of body weight) and an additional injectionone day before infection (100 mg/kg of body weight). On the day of infection,immediately before use, frozen bacterial cultures were thawed and diluted insaline to the desired concentration. Anesthetized ICR mice were challengedintranasally with 20 �l of saline containing various concentrations (1 � 104 to 1 �107 CFU/ml) of P. aeruginosa strain PAO1. Mice were sacrificed at 0, 3, 6, 9, 24,and 48 h after infection in order to determine the CFU counts in their lungs.After skin disinfection with 70% alcohol, lungs from sacrificed mice were re-
FIG. 1. Schematic design of an insulated AMFields electrode (A), AMFields mouse treatment chamber (B), AMFields generation system withwires shown for one mouse (C), and electrodes placed on a mouse for the treatment of lung infection (D). Following depilation, four insulatedelectrodes were attached to the mouse’s skin using a layer of adhesive hydrogel. The electrodes were fixed by wrapping them with medical tape(Leukoplast), and the electrode wires were connected to the AMFields generating system or to the sham heat control system. The four electrodeswere functionally divided into two pairs, identified by red or blue wires. The electrode pairs were positioned so as to create two perpendicular fielddirections at the center of the animal’s body. Sham heat and control electrodes were placed in the same configuration.
VOL. 54, 2010 MICROBIAL GROWTH INHIBITION BY AMFields IN MICE 3213
on August 20, 2016 by guest
http://aac.asm.org/
Dow
nloaded from
moved aseptically, photographed, and weighed, and their CFU contents weredetermined.
Application of AMFields to mice with P. aeruginosa pulmonary infection. Theapplication of AMFields to the mouse torso was carried out as follows. Four daysbefore infection, the torso of the anesthetized mouse was shaved with electricalclippers and depilated using cold wax. On the day of infection, four insulatedelectrodes were placed around the mouse torso (Fig. 1D) so as to generate fieldsof two perpendicular directions through the lungs. Mice were placed inside theIVC cages, and the electrodes were connected to the connection box. Theelectrode wires were encapsulated within silicon cable protector and tied tothe cage top in order to protect the wires from being damaged by the mice.Treatment with AMFields began 3 h after infection and was maintained for48 h with 2 brief stops daily for monitoring the physical condition of the mice.After 48 h of treatment, the mice were sacrificed and the lungs were removedaseptically.
Combined treatment of P. aeruginosa pulmonary infection by AMFields andceftazidime. The combined effect of AMFields and antibiotics was tested usingceftazidime, an agent recommended by the Infectious Diseases Society of Amer-ica for the treatment of hospital-acquired pneumonia.
A preliminary experiment was conducted with the aim of determining thebacterial titer of the inoculum and the ceftazidime concentration that allow themaintenance of a persistent infection without fully eradicating it, thus allowingthe combined effect of AMFields and the antibiotic to be measured.
Experiments were conducted as described above for AMFields treatment of P.aeruginosa pulmonary infection, with the following modifications. Mice werechallenged intranasally with a predetermined bacterial titer. Ceftazidime (5mg/kg of body weight) was administered intraperitoneally twice daily for 48 hstarting 3 h after infection. Antibiotic administration was stopped at least 12 hbefore the termination of the experiment.
Bacterial counts and statistical analysis. Cold sterile saline was added to eachlung sample tube, with the saline-to-tissue weight ratio maintained at 10:1. Tubeswere placed in an ice bath, and the suspensions were homogenized using anOmni tissue homogenizer (Omni, GA) with Omni disaggregation tips. Appro-priate suspension dilutions were plated on LB agar plates and kept at 37°C for24 h. Bacterial counts were expressed as the number of P. aeruginosa CFU perlung.
Bacterial growth in the lungs of each mouse was expressed using the formulalog(CFUT48/CFUT0), where CFUT48 is the CFU count in the mouse lungs at theend of treatment and CFUT0 is the initial number of bacteria used for inocula-tion in the specific experiment.
The results for all mice that received the same treatment were pooled, and theaverage bacterial growth was calculated for each group. A two-tailed t test forequal variance was used to compare the mean values.
Histological evaluation. Lungs were fixed and embedded in paraffin wax.Histological sections, 5 �m thick, were stained with hematoxylin-eosin (HE) andexamined by an independent expert. A semiquantitative grading scheme wasused to evaluate the extent of the lesions in the sections as follows: minimal(grade 1) lesions involving less than 10% of the lung section; mild (grade 2),involving 11% to 40%; moderate (grade 3), involving 41% to 80%; and marked(grade 4), involving 81% to 100%.
RESULTS
Measurement of temperature and AMFields intensity inlungs of treated mice. In a preliminary set of experiments, fieldintensities and temperature measurements were done duringAMFields treatment and sham heat application. The averageAMFields intensity in the lungs was 12 � 4 V/cm (mean �
standard deviation). Under these conditions, lung temperaturewas identical to or up to 1°C lower than the electrode surfacetemperatures, which were set to 37°C for both the AMFieldsand the sham heat control. The skin temperature of the controlmice was in the range of 33 to 35°C.
Development of animal models. Pulmonary infection wasinduced by intranasal administration of different amounts of P.aeruginosa strain PAO1 to neutropenic ICR mice. Bacterialinocula of around 3.6 log CFU/mouse were found to induce asevere pulmonary infection which persisted for at least 48 h.Larger inocula resulted in a high mortality rate, while smallerones resulted in spontaneous recovery.
Effect of AMFields on pulmonary infection caused by P.aeruginosa. AMFields treatment for 48 h of mice suffering frompulmonary infection resulted in a 3.4-log reduction in the CFUcontent of the lungs in treated mice compared to the CFUcount in untreated control mice (Table 1). The sham heatcontrol treatment led to a 2.5-log reduction compared to theCFU count in the control mice (Table 1). The average bacte-rial growth [log(CFUT48/CFUT0)] in both AMFields-treatedmice and sham heat-treated mice was significantly lower thanin control mice (Fig. 2A). The CFU content of the AMFields-treated mice did not reach a significant level of decrease com-pared to the CFU count in the sham heat-treated mice, al-though a clear trend was seen (P � 0.09). A significantreduction was observed in the weight of the lungs of AMFields-treated mice compared to the lung weights of both sham heat-treated control mice (P � 0.02) and untreated control mice(P � 0.001) (Fig. 2B). Representative photos of lungs fromuninfected, AMFields-treated, and control group mice areshown in Fig. 2C, D, and E, respectively. Histopathologicalexamination of the lung samples from AMFields-treated micegraded them as normal to grade 1 with focal acute inflamma-tion. Lungs from both control mice and sham heat-treatedmice were graded as grade 2 to 3, associated with acute necro-tizing pneumonia and the presence of numerous bacterial col-onies (Fig. 2F, G, and H).
Combined treatment with AMFields and ceftazidime of pul-monary infection caused by P. aeruginosa. The inoculum andceftazidime concentration were determined experimentally soas to establish a persistent infection throughout the experimentwithout leading to a complete recovery or a significant deathrate in the presence of the antibiotic. The inoculum that wasfound to induce a persistent pulmonary infection in the pres-ence of ceftazidime (5 mg/kg of body weight twice daily) alonewas approximately 4.6 log CFU/mouse. The results presentedin Table 1 demonstrate that combined treatment with bothAMFields and ceftazidime for 48 h resulted in a 1.5-log reduc-
TABLE 1. The logs of the numbers of bacteria in the inoculums and in the lungs of mice after treatment
Treatment
Without ceftazidime With ceftazidime
Loginoculum � SD
LogCFUT48 � SD P valuea No. of
miceLog
inoculum � SDLog
CFUT48 � SD P valuea No. ofmice
AMFields 3.6 � 0.2 4.1 � 1.5 �0.001 17 4.6 � 0.2 5.0 � 1.7 0.005 36Sham heat 3.6 � 0.2 5.0 � 2.5 0.009 20 4.6 � 0.2 6.0 � 2.3 0.398 27Control 3.6 � 0.2 7.5 � 2.7 24 4.6 � 0.2 6.5 � 2.5 40
a P values are in comparison to the results for the control.
3214 GILADI ET AL. ANTIMICROB. AGENTS CHEMOTHER.
on August 20, 2016 by guest
http://aac.asm.org/
Dow
nloaded from
tion in the lung CFU content compared to the CFU count in theantibiotic-treated control. The combined treatment of sham heatand ceftazidime did not result in a significant CFU count reduc-tion compared to the CFU count in the control (Table 1). Thebacterial growth [log(CFUT48/CFUT0)] in the lungs of micetreated with both AMFields and ceftazidime was significantlylower than that in the control mice (P � 0.004) (Fig. 3A). Theaverage lung weight was significantly lower in both the ceftazi-
dime/AMFields combination treatment group (P � 0.001) andthe ceftazidime/sham heat combination treatment group (P �0.047) than in the control group (Fig. 3B). The CFU content ofthe ceftazidime/AMFields-treated mice nearly reached a signifi-cant decrease compared to that of the ceftazidime/sham heat-treated mice (P � 0.06). The lung weights of the ceftazidime/AMFields-treated mice were significantly lower than thoseobserved for the ceftazidime/sham heat-treated mice (P � 0.05).
FIG. 2. Effect of AMFields on mice with P. aeruginosa lung infection. (A) Relative bacterial growth compared to the inoculum size after 48 hof treatment. (B) Lung weight at the end of treatment. STDEV, standard deviation. P values versus results for control: **, P � 0.01; ***, P �0.001. (C to E) Representative photos of a healthy lung from an uninfected mouse (C), a lung from an AMFields-treated mouse (D), and a lungfrom a control mouse (E). (F to H) Microscope slides, stained with HE, prepared from a lung of an uninfected mouse (F), a lung of anAMFields-treated mouse (G), and a lung of a control mouse (H). Scale bars, 100 �m.
FIG. 3. Combined treatment with AMFields and ceftazidime of mice with P. aeruginosa lung infection. (A) Relative bacterial growth comparedto the inoculum size after 48 h of treatment. (B) Lung weight at the end of treatment. STDEV, standard deviation. P values versus results forcontrol: *, P � 0.05; **, P � 0.01; ***, P � 0.001.
VOL. 54, 2010 MICROBIAL GROWTH INHIBITION BY AMFields IN MICE 3215
on August 20, 2016 by guest
http://aac.asm.org/
Dow
nloaded from
DISCUSSION
In the present study, we show that AMFields, previouslyshown to be an effective in vitro tool for inhibiting bacterialpathogen proliferation (8), are also effective in vivo. Specifi-cally, it is demonstrated that AMFields, applied using nonin-vasive, insulated electrodes, have a significant inhibitory effecton the growth of a pulmonary bacterial infection in mice.The inhibitory effect was observed when AMFields wereapplied either as a monotherapy or as an adjuvant to anti-biotic therapy.
One striking outcome of the AMFields application was thefact that the number of bacteria in the lungs of AMFields-treated mice increased by only a fraction of an order of mag-nitude compared to the number in the inoculums used forinfection, while at the same time the number of bacteria in thelungs of the control group increased by 3.8 orders of magni-tude. This observation could be the consequence of either abacteriostatic or a bactericidal effect of AMFields. Histopatho-logical analysis demonstrated that in AMFields-treated mice,the lung morphology was normal and without any evidence ofprior acute infection. Thus, it is reasonable to assume that theAMFields treatment led to cell proliferation arrest rather thanto the elimination of the bacteria after they had proliferated inthe lungs. Supportive evidence for this conclusion can be foundin the results of the experiment in which the combinedAMFields/ceftazidime treatment was tested. Ceftazidime is anexpanded-spectrum cephalosporin antibiotic with a broad bac-tericidal activity against Gram-positive and Gram-negativebacteria. Like other beta-lactam antibiotics, ceftazidime ismost effective against dividing bacteria. Indeed, ceftazidimetreatment (5 mg/kg of body weight twice daily) alone resultedin a growth reduction of close to 2 logs compared to the growthin untreated lungs (1.9 versus 3.8 CFU, respectively) (Fig. 2Aand 3A). Yet, the combined treatment of AMFields and cef-tazidime did not lead to a reduction in bacterial growth com-pared to the growth with the AMFields treatment alone (0.4versus 0.5, respectively) (Fig. 2A and 3A), nor did it signifi-cantly reduce CFU counts in the lungs compared to the inocu-lums (Table 1) suggesting that bacterial growth was arrested.
Previously, we demonstrated that the application of AMFieldsin vitro led to a 20% reduction in the number of treated bac-teria compared to the number of control bacteria—consider-ably less than the level of inhibition seen in the present study.One possible explanation for the higher efficacy in the in vivoexperiments could be the fact that the AMFields inhibitoryeffect is field intensity dependent (8). While the AMFieldsintensity in the in vitro experiments was limited to 4 V/cm inorder to avoid overheating of the culture, the AMFieldsintensity in vivo was significantly higher (�12 V/cm). Theapplication of AMFields of higher intensities was a conse-quence of active heat removal from the electrodes by themice’s circulation.
Another possible explanation for the higher efficacy ofAMFields treatment in vivo may be related to the inhibitoryeffect on bacterial growth seen with heat treatment alone.Though the sham heat control effect was smaller than theAMFields effect, it was still significant. Bacterial growth inhi-bition due to elevated temperatures may result from either adirect effect of the heat on bacterial growth or from local and
systemic host responses to heating. The former hypothesis wastested in vitro by comparing the growth rate of P. aeruginosa atvarious temperatures within the range of normal-to-febriletemperatures. As shown previously (20), we found that thegrowth rate of P. aeruginosa is positively correlated with in-creasing temperature in the range of 34 to 38°C. Thus, we canrule out the possibility that heating was directly responsible forthe observed reduction in bacterial growth. The second possi-bility, i.e., that local and systemic host reactions to elevatedtemperatures decrease bacterial growth, is not new. In fact,historically, heat and fever were used as a tool against micro-bial pathogens for over a century (3, 10). There are numerousreports regarding the effects of elevated host temperatures onthe growth of bacterial pathogens. For example, the inductionof fever after inoculation with malaria can serve as a treatmentagainst Treponema pallidum (34). It has also been shown thatfebrile core temperature is essential for optimal host defenseagainst Klebsiella pneumoniae peritonitis in mice (11) and thatfever in elderly patients with community-acquired pneumoniais positively correlated with high survival rates (1). Finally,maintaining a normal core body temperature (36.6 � 0.5°C)after anesthesia has been shown to decrease the incidence ofinfectious complications in patients undergoing colorectal re-section (16). Among the mechanisms suggested in the antibac-terial effect of heating, augmentation of the innate immunefunction is probably the most intensively studied (9, 10, 17, 19,27). Though our results demonstrate that the application ofAMFields and sham heat did not cause an increase in lungtemperatures, these treatments did raise the temperature ofthe peripheral organs of the treated mice by at least 2 degrees(the normal skin temperature of mice is 34 to 35°C, while in thepresent study, the electrode temperature was set to 37°C).Hanson (9) demonstrated that the response of mature primaryT cells is strongly regulated by temperature changes in therange of 29 to 37°C, which corresponds to the peripheral tissuetemperature elevation during febrile episodes. This findingprovides a possible explanation for the inhibitory effect of thesham heat-treatment reported in the present study. Since theapplication of AMFields is always associated with heat produc-tion, it is reasonable to assume that the enhanced efficacy ofthe fields reported in the present study compared to the find-ings in our previous report (8) is due, at least in part, to theelevated temperatures of peripheral tissues.
Still, AMFields-treated mice demonstrated reproducible re-ductions in total CFU content, bacterial growth in the lungs,and lung weights compared to these parameters in sham heat-treated mice. This reduction was statistically significant forlung weights and reached nearly significant values for the otherparameters, indicating that the effect could not be attributedsolely to the heat generated.
Previous experiments that utilized electric currents as an invivo treatment against microbial infections applied weak DCcurrents generated using conductive electrodes (5, 6, 28, 32).Such use of DC currents for the treatment of infections has thefollowing three main limitations. (i) DC currents may stimulatenerves and muscles, causing pain and muscular contractions.(ii) DC currents can only be generated by using conductiveelectrodes and are therefore always associated with electroly-sis, the release of metal ions, and the generation of free radi-cals. (iii) When relatively small electrodes are used, electric
3216 GILADI ET AL. ANTIMICROB. AGENTS CHEMOTHER.
on August 20, 2016 by guest
http://aac.asm.org/
Dow
nloaded from
fields and DC currents spread in the body volume such thattheir density decreases with distance from the electrodes.Thus, current density of sufficient intensity can only be appliedto superficial lesions unless implanted electrodes are used toreach deeper lesions. The DC current densities used in theabove-mentioned reports were too low to induce nerve stimu-lation. However, it is reasonable to assume that treatment ofdeeper tissues, such as lung infections, would require muchhigher currents, thus subjecting the patient to the risk of nervestimulation, electrolysis, and the formation of toxic derivatives.Note also that in some studies, the currents were generated bysilver electrodes and the inhibitory effect was observed onlywhen the silver electrode served as the anode, implying theinvolvement of silver ions that may potentially be toxic. Unlikethe fields in the above-mentioned reports, AMFields are notassociated with electrolysis, the production of free radicals,toxic metal ions, etc. due to their unique properties. Indeed,during the AMFields treatment described above, no side ef-fects were detected in the treated mice.
The mechanisms responsible for the inhibitory effect ofAMFields can be deduced from the experiments conducted byKirson et al. (13, 14) with tumor-treating fields (TTFields).TTFields are used to inhibit the growth of cancerous cells andare similar to AMFields in all aspects, with the exception offrequency (100 to 200 kHz for TTFields versus 5 to 30 MHz forAMFields). Kirson et al. demonstrated that the inhibitory ef-fect of TTFields is related to the formation of inhomogeneouselectric fields near the bridge separating the daughter cellsduring cytokinesis. Such inhomogeneous fields, of any fre-quency in the relevant ranges, exert unidirectional dielectro-phoresis forces on charged and polar particles and moleculesand, thus, may result in their movement toward the furrow. Wehypothesized that the AMFields inhibitory effect is the resultof a similar mechanism. Modeling of the AMFields distribu-tion and the associated electric forces inside dividing bacteriaduring cytokinesis, using finite element mesh simulations, hasshown that the magnitude of these forces in a bacterial cell issufficient to induce particle and macromolecule distortion andmovement (8). This mechanism is very different from the onessuggested to be involved with DC current (18, 29, 30).
The results presented herein serve as a proof of concept forthe use of low-intensity alternating electric fields as a treat-ment against pulmonary infections caused by P. aeruginosa.Such a treatment would involve the placement of insulatedelectrodes on the skin surrounding the infected organs (e.g., onthe chest) and the generation of the electric fields using anAMFields generator, similar to the treatment of patients suf-fering from brain glioblastoma and lung cancer using aTTField generator (13–15). In the near future, we intend totest the inhibitory effect of AMFields on additional bacterialspecies and other in vivo models of infection in order to test thegenerality of the observations reported above.
REFERENCES
1. Ahkee, S., L. Srinath, and J. Ramirez. 1997. Community-acquired pneumo-nia in the elderly: association of mortality with lack of fever and leukocytosis.South Med. J. 90:296–298.
2. Andes, D., and W. A. Craig. 1998. In vivo activities of amoxicillin andamoxicillin-clavulanate against Streptococcus pneumoniae: application tobreakpoint determinations. Antimicrob. Agents Chemother. 42:2375–2379.
3. Atkins, E. 1982. Fever: its history, cause, and function. Yale J. Biol. Med.55:283–289.
4. Caubet, R., F. Pedarros-Caubet, M. Chu, E. Freye, M. de Belem Rodrigues,J. M. Moreau, and W. J. Ellison. 2004. A radio frequency electric currentenhances antibiotic efficacy against bacterial biofilms. Antimicrob. AgentsChemother. 48:4662–4664.
5. Chu, C. S., A. T. McManus, B. A. Pruitt, Jr., and A. D. Mason, Jr. 1988.Therapeutic effects of silver nylon dressings with weak direct current onPseudomonas aeruginosa-infected burn wounds. J. Trauma 28:1488–1492.
6. Del Pozo, J. L., M. S. Rouse, G. Euba, C. I. Kang, J. N. Mandrekar, J. M.Steckelberg, and R. Patel. 2009. The electricidal effect is active in an exper-imental model of Staphylococcus epidermidis chronic foreign body osteomy-elitis. Antimicrob. Agents Chemother. 53:4064–4068.
7. Ensing, G. T., B. L. Roeder, J. L. Nelson, J. R. van Horn, H. C. van der Mei,H. J. Busscher, and W. G. Pitt. 2005. Effect of pulsed ultrasound in combi-nation with gentamicin on bacterial viability in biofilms on bone cements invivo. J. Appl. Microbiol. 99:443–448.
8. Giladi, M., Y. Porat, A. Blatt, Y. Wasserman, E. D. Kirson, E. Dekel, and Y.Palti. 2008. Microbial growth inhibition by alternating electric fields. Anti-microb. Agents Chemother. 52:3517–3522.
9. Hanson, D. F. 1993. Fever and the immune response. The effects of physi-ological temperatures on primary murine splenic T-cell responses in vitro.J. Immunol. 151:436–448.
10. Hasday, J. D., K. D. Fairchild, and C. Shanholtz. 2000. The role of fever inthe infected host. Microbes Infect. 2:1891–1904.
11. Jiang, Q., A. S. Cross, I. S. Singh, T. T. Chen, R. M. Viscardi, and J. D.Hasday. 2000. Febrile core temperature is essential for optimal host defensein bacterial peritonitis. Infect. Immun. 68:1265–1270.
12. Jori, G., C. Fabris, M. Soncin, S. Ferro, O. Coppellotti, D. Dei, L. Fantetti,G. Chiti, and G. Roncucci. 2006. Photodynamic therapy in the treatment ofmicrobial infections: basic principles and perspective applications. LasersSurg. Med. 38:468–481.
13. Kirson, E. D., V. Dbaly, F. Tovarys, J. Vymazal, J. F. Soustiel, A. Itzhaki, D.Mordechovich, S. Steinberg-Shapira, Z. Gurvich, R. Schneiderman, Y. Was-serman, M. Salzberg, B. Ryffel, D. Goldsher, E. Dekel, and Y. Palti. 2007.Alternating electric fields arrest cell proliferation in animal tumor modelsand human brain tumors. Proc. Natl. Acad. Sci. U. S. A. 104:10152–10157.
14. Kirson, E. D., Z. Gurvich, R. Schneiderman, E. Dekel, A. Itzhaki, Y. Was-serman, R. Schatzberger, and Y. Palti. 2004. Disruption of cancer cell rep-lication by alternating electric fields. Cancer Res. 64:3288–3295.
15. Kirson, E. D., R. S. Schneiderman, V. Dbaly, F. Tovarys, J. Vymazal, A.Itzhaki, D. Mordechovich, Z. Gurvich, E. Shmueli, D. Goldsher, Y. Wasser-man, and Y. Palti. 2009. Chemotherapeutic treatment efficacy and sensitivityare increased by adjuvant alternating electric fields (TTFields). BMC Med.Phys. 9:1.
16. Kurz, A., D. I. Sessler, and R. Lenhardt. 1996. Perioperative normothermiato reduce the incidence of surgical-wound infection and shorten hospitaliza-tion. Study of Wound Infection and Temperature Group. N. Engl. J. Med.334:1209–1215.
17. Lederman, H. M., C. R. Brill, and P. A. Murphy. 1987. Interleukin 1-drivensecretion of interleukin 2 is highly temperature-dependent. J. Immunol.138:3808–3811.
18. Liu, W. K., M. R. Brown, and T. S. Elliott. 1997. Mechanisms of the bacte-ricidal activity of low amperage electric current (DC). J. Antimicrob. Che-mother. 39:687–695.
19. Mackowiak, P. A., and M. Marling-Cason. 1983. Hyperthermic enhance-ment of serum antimicrobial activity: mechanism by which fever might exerta beneficial effect on the outcome of gram-negative sepsis. Infect. Immun.39:38–42.
20. Magnusson, V., T. Jonsdottir, H. Gudmundsdottir, H. Erlendsdottir, and S.Gudmundsson. 1995. The in-vitro effect of temperature on MICs, bacteri-cidal rates and postantibiotic effects in Staphylococcus aureus, Klebsiellapneumoniae and Pseudomonas aeruginosa. J. Antimicrob. Chemother. 35:339–343.
21. Maisch, T. 2007. Anti-microbial photodynamic therapy: useful in the future?Lasers Med. Sci. 22:83–91.
22. Oleinick, N. L., and H. H. Evans. 1998. The photobiology of photodynamictherapy: cellular targets and mechanisms. Radiat Res. 150:S146–S156.
23. Pitt, W. G., M. O. McBride, J. K. Lunceford, R. J. Roper, and R. D. Sagers.1994. Ultrasonic enhancement of antibiotic action on gram-negative bacte-ria. Antimicrob. Agents Chemother. 38:2577–2582.
24. Rabinovitch, C., and P. S. Stewart. 2006. Removal and inactivation of Staph-ylococcus epidermidis biofilms by electrolysis. Appl. Environ. Microbiol. 72:6364–6366.
25. Rediske, A. M., N. Rapoport, and W. G. Pitt. 1999. Reducing bacterialresistance to antibiotics with ultrasound. Lett. Appl. Microbiol. 28:81–84.
26. Reithinger, R., M. Mohsen, M. Wahid, M. Bismullah, R. J. Quinnell, C. R.Davies, J. Kolaczinski, and J. R. David. 2005. Efficacy of thermotherapy totreat cutaneous leishmaniasis caused by Leishmania tropica in Kabul, Af-ghanistan: a randomized, controlled trial. Clin. Infect. Dis. 40:1148–1155.
27. Rosenspire, A. J., A. L. Kindzelskii, and H. R. Petty. 2002. Cutting edge:fever-associated temperatures enhance neutrophil responses to lipopolysac-charide: a potential mechanism involving cell metabolism. J. Immunol. 169:5396–5400.
VOL. 54, 2010 MICROBIAL GROWTH INHIBITION BY AMFields IN MICE 3217
on August 20, 2016 by guest
http://aac.asm.org/
Dow
nloaded from
28. Spadaro, J. A., T. J. Berger, S. D. Barranco, S. E. Chapin, and R. O. Becker.1974. Antibacterial effects of silver electrodes with weak direct current.Antimicrob. Agents Chemother. 6:637–642.
29. Stewart, P. S., W. Wattanakaroon, L. Goodrum, S. M. Fortun, and B. R.McLeod. 1999. Electrolytic generation of oxygen partially explains electricalenhancement of tobramycin efficacy against Pseudomonas aeruginosa biofilm.Antimicrob. Agents Chemother. 43:292–296.
30. Stoodley, P., D. deBeer, and H. M. Lappin-Scott. 1997. Influence of electricfields and pH on biofilm structure as related to the bioelectric effect. Anti-microb. Agents Chemother. 41:1876–1879.
31. Takeda, S., T. Nakai, Y. Wakai, F. Ikeda, and K. Hatano. 2007. In vitro andin vivo activities of a new cephalosporin, FR264205, against Pseudomonasaeruginosa. Antimicrob. Agents Chemother. 51:826–830.
32. van der Borden, A. J., P. G. Maathuis, E. Engels, G. Rakhorst, H. C. van derMei, H. J. Busscher, and P. K. Sharma. 2007. Prevention of pin tract
infection in external stainless steel fixator frames using electric current in agoat model. Biomaterials 28:2122–2126.
33. van der Borden, A. J., H. van der Werf, H. C. van der Mei, and H. J.Busscher. 2004. Electric current-induced detachment of Staphylococcus epi-dermidis biofilms from surgical stainless steel. Appl. Environ. Microbiol.70:6871–6874.
34. Wagner-Jauregg, J. 1965. The treatment of dementia paralytica by malariainoculation, p. 159–172. In Nobel Lectures, Physiology or Medicine 1922–1941. Elsevier Publishing Company, Amsterdam, Netherlands.
35. Wainwright, M. 1998. Photodynamic antimicrobial chemotherapy (PACT).J. Antimicrob. Chemother. 42:13–28.
36. Zolfaghari, P. S., S. Packer, M. Singer, S. P. Nair, J. Bennett, C. Street, andM. Wilson. 2009. In vivo killing of Staphylococcus aureus using a light-activated antimicrobial agent. BMC Microbiol. 9:27.
3218 GILADI ET AL. ANTIMICROB. AGENTS CHEMOTHER.
on August 20, 2016 by guest
http://aac.asm.org/
Dow
nloaded from