Concise Review: Skeletal Muscle Stem Cells and Cardiac Lineage: Potential for Heart Repair
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Concise Review: Skeletal Muscle Stem Cells and Cardiac Lineage: Potential for Heart Repair
Tissue-Specific Progenitor and Stem Cells
Concise Review: Skeletal Muscle Stem Cells andCardiac Lineage: Potential for Heart Repair
NARMEEN HASSAN,a,* JASON TCHAO,b,* KIMIMASA TOBITAa,b,c
Key Words. Adult stem cells x Cell transplantation x Tissue-specific stem cells xProgenitor cells x Cardiac
ABSTRACT
Valuable and ample resources have been spent over the last two decades in pursuit of interventionalstrategies to treat the unmet demand of heart failure patients to restore myocardial structure andfunction. At present, it is clear that full restoration of myocardial structure and function is outsideour reach from both clinical and basic research studies, but it may be achievable with a combinationof ongoing research, creativity, and perseverance. Since the 1990s, skeletal myoblasts have been ex-tensively investigated for cardiac cell therapy of congestive heart failure. Whereas the Myoblast Au-tologous Grafting in Ischemic Cardiomyopathy (MAGIC) trial revealed that transplanted skeletalmyoblasts did not integrate into the host myocardium and also did not transdifferentiate into cardi-omyocytes despite some beneficial effects on recipient myocardial function, recent studies suggestthat skeletal muscle-derived stem cells have the ability to adopt a cardiomyocyte phenotype in vitroand in vivo. This brief review endeavors to summarize the importance of skeletal muscle stem cellsand how they can play a key role to surpass current results in the future and enhance the efficaciousimplementationof regenerative cell therapy forheart failure. STEMCELLSTRANSLATIONALMEDICINE
2014;3:1–12
INTRODUCTION
In the United States, an estimated 15.4 millionpeople have coronary heart disease, of whom7.6 million are affected by myocardial infarctionand 2.1 million by congestive heart failure [1].In the last two decades, the classic concept ofthe heart as an organ with extremely limited re-generative capacity has been analyzed. The celltherapy approaches were limited at the turn ofthe newmillennium to the transfer of noncardiaccell types such as smoothmuscle cells, embryonicstem cells, mesenchymal bone marrow stromalcells, hematopoietic stem cells [2], and skeletalmyoblasts [3] into an injured heart. The idea ofthese engraftments was to stimulate repair andregeneration of the injured myocardium [4–6].The field of cardiac regenerative medicine wasbrought into greater focus with the recognitionof cardiac stem cells in 2001 [7] and the abilityto antigenically select cardiac progenitor cells ex-perimentally [8]. The capacity to generate cardio-myocytes in the adult human heart is 1% at theage of 25, and it decreases to 0.45% at the ageof 75 [9]. This rationale, together with publishedresearch reports and experimental studies [10],indicated that theheart is in fact capableof regen-eration, but therapeutic strategies are needed tostimulate this process in cardiac pathologies. Theuse of fetal cardiac cells poses ethical, logistical,and technical issues, and there still is no means
for effectively mobilizing a hypothetical poolof resident stem cells. Long-term functional im-provement requires stem cells with true cardio-myogenic properties and angiogenic potential.Presently, it is not clear whether such a perfectstem cell exists. However, a number of stem celltypes show promise for autologous cardiomyo-plasty, including multipotent stem cells isolatedfrom skeletal muscle, which we highlight in thisreview.
STEM CELLS ARE A PROMISING SOURCEFOR CARDIOMYOPLASTY
Unspecialized cells that are capable of continuousself-renewal, while maintaining the ability to dif-ferentiate into multiple different cell types, aredefined as stem cells. There are, broadly, threemajor categories of stem cells: embryonic stemcells, adult stem cells, and induced pluripotentstem (iPS) cells. Embryonic stem cells are undif-ferentiated cells, which are present during em-bryonic development and possess pluripotentdifferentiation capacity. Adult stem cells can beisolated from postnatal tissues and are multipo-tent. Sim et al. in 2002 [3] and Murry et al. in2004 [11] concluded that none of the adult stemcell sources convincingly demonstrated a poten-tial for significant long-term engraftment and dif-ferentiation into functional cardiomyocytes. The
aDepartment ofDevelopmental Biology,bDepartment ofBioengineering, andcMcGowan Institute ofRegenerative Medicine,University of Pittsburgh,Pittsburgh, Pennsylvania,USA
*Contributed equally as firstauthors.
Correspondence: KimimasaTobita, M.D., Rangos ResearchCenter, Room 8121, 4401 PennAvenue, Pittsburgh, Pennsylvania15224, USA. Telephone: 412-692-9902; E-Mail: [email protected]
Received July 5, 2013; acceptedfor publication September 13,2013.
©AlphaMed Press1066-5099/2013/$20.00/0
http://dx.doi.org/10.5966/sctm.2013-0122
STEM CELLS TRANSLATIONAL MEDICINE 2014;3:1–12 www.StemCellsTM.com ©AlphaMed Press 2014
TISSUE-SPECIFIC PROGENITOR AND STEM CELLS
technique developed by Takahashi and Yamanaka in 2006 [12]demonstrated that the introduction of a quartet of transcriptionfactors, Oct4, Sox2, Klf4, and c-Myc, into terminally differentiatedcells (e.g., skin fibroblasts) changed these cells into an embryonicstem cell-like state known as iPS cells. Human iPS cells are similarto human embryonic cells in morphology, proliferation, surfaceantigens, gene expression, telomerase activity, epigenetic statusof pluripotent cell-specific genes, and cardiac potential [13]. How-ever, the maturation of iPS cell-derived cardiomyocytes remainsnonuniform [14, 15]. Human implantation of embryonic and iPScell-derived cardiomyocytes is limited by significant safety andethical issues. Studies have revealed significant genetic and epi-genetic abnormalities in iPS cells, higher than embryonic stemcells or fibroblasts. The mutation rates are estimated to be 10times as high as those of fibroblasts [16]. Chromosome p12 hasbeen found to be over-represented in iPS cell cultures, a charac-teristic associated with testicular germ cell tumors [16]. Othermutations are also associatedwith cell cycle regulation and onco-genesis, which raises the risk of teratogenesis in vivo. High-throughput functional genomics approaches areneeded tobetterunderstand the nature and consequences of thesemutations. iPStechnology avoids the ethical dilemma of embryo destruction re-lated to embryonic stem cells, but other ethical issues, includinginformed consent and genetic anonymity of donors, must still becarefully considered. Although iPS technology holds great prom-ise for the regeneration of the heart and other organs, clinical useof iPS technology in ischemic heart disease remains untested.From this point of view, adult stem cells remain a more practicaloption at the present time.
Significant efforts in the field of cardiac cell therapy have fo-cused on bone marrow-derived cells, especially bone marrowmononuclear cells such as hematopoietic and mesenchymal stemcells.Mesenchymal stemcells havenumerousdesirable character-istics, including positive paracrine effects, angiogenic potential,and an immunoprivileged profile. Studies have shown thatmesen-chymal stem cells, but not hematopoietic stem cells, can differen-tiate into cardiomyocytes in vivo [17, 18], with slightly tosignificantlypositive results inclinical trials [19,20].However, bonemarrow mesenchymal stem cells do not differentiate into cardio-myocytes in significant numbers invitro, suggesting that their ther-apeutic benefit is predominantly paracrine rather than throughtransdifferentiation [21]. Challenges includeexpanding these stemcells in clinically relevant numbers and developing safe methodsfor cardiomyocyte differentiation. (5-Azacytidine used for in vitrodifferentiation of mesenchymal stem cells into cardiomyocytes istoxic [17].) More recent work has focused on cardiac stem cells,which are found in niches within the heart and can be isolatedby myocardial biopsies. Studies using immunosuppressed ratshave shown that human cardiac stem cells can give rise tomyocar-diumwith improved function [22]. In light of these results, clinicaltrials havebeen initiated [23, 24].Whereas initial results of the SCI-PIO trial are promising, the CADUCEUS trial showed no differencein ventricular function compared with control despite a reductionof infarct size. Isolationof cardiac stemcells is also invasiveandcar-ries higher risk comparedwith isolation fromother tissues. Furtherinvestigation isneededtosafelyandeffectively isolate,expand,dif-ferentiate, and deliver these stem cells.
Cellular cardiomyoplasty of autologous skeletal muscle cellsinto the myocardium to reinforce its structure and function canbe used as an alternative to heart transplantation [25]. Transdif-ferentiation directly converts a specialized cell type to another
specialized cell type, bypassing a pluripotent state. In the 1980s,itwas shown that fibroblasts can be converted into skeletalmusclecells with the use of the MyoD transcription factor [26]. In recentyears, direct reprogramming of cardiac fibroblasts into functionalcardiomyocytes by transcription factors GATA4, Tbx5, and Mef2cboth in vitro and in vivo has been reported [15, 27]. However,the low reprogramming efficiency of this approach and the useof viral vectors are undesirable characteristics. It is interesting tospeculate that direct reprogramming to cardiomyocytes mightbe more effective in skeletal muscle stem cells, which are pre-endowed with myogenic potential. Lymphocytes were convertedinto macrophages by using a transcription factor called C/EBPa[28]. But once they are in one committed lineage, it is a challengetomake themconvert to another unrelated cell type, and transdif-ferentiation efficiency is often low. Szabo et al. [29] also provedthat blood cells can be generated from fibroblasts, making it likelythat transcription factors can induce large jumpsbetweendistantlyrelated cell types. This opened up the prospect that any desiredspecialized cell could be generated from essentially any other celltype. Because skeletal and cardiac muscle both arise from myo-genic, mesodermal lineages and share some characteristics, trans-differentiation from skeletal muscle progenitors to cardiac musclewould require less comprehensive alteration compared with dis-tantly relatedcell types,at least intheory.Cellsareconsidered idealif they are derived from relatively easy to obtain tissue, readilygrown in large numbers, available off the shelf for acute indica-tions, nonimmunogenic, nonarrhythmogenic, and able to regener-ate healthy myocardium [30]. Although the skeletal muscle stemcell isolation procedure is invasive comparedwith isolation of cellsfrombloodorurine, skeletalmuscle comprises the largest percent-age of total bodymass [31]. These desirable characteristics andde-velopmental similarity to cardiac muscle, described below, makeskeletal muscle-derived cells a strong candidate to repopulatedamaged myocardium.
SKELETAL MUSCLE AND CARDIAC MUSCLE: DIFFERENCE AND
SIMILARITY DURING DEVELOPMENT
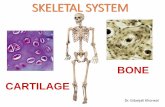
It is awidely acceptednotion that terminally differentiatedmaturecardiac muscle does not express proteins that are specific to skel-etalmuscle. However, developing skeletalmuscle hasbeenprovento be similar to cardiac muscle by various studies, suggesting thatthey have a similar cell lineage. Different isoforms ofmyosin heavychain (MHC) are present in different muscle fiber types to meettheir functional needs. There are four major MHC isoforms in ratskeletal muscle. I/b is a slow type, and IIa, IIx/IId, and IIb are fasttypes. These are equivalent to skeletal muscle-specific fast MHC(sk-fMHC) [32–34]. In the adult myocardium, a-MHC and b-MHCare present, with the latter being identical to I/b-MHC found inskeletal muscle. Noncardiac MHCs play a major role during theearly myofibrillogenesis of nascent cardiomyocytes in assemblingsarcomere structure [35]. Recently, it was found that sk-fMHCwasexpressed in developing rat myocardium, and its expression wasattenuated in postnatal life [36].
The thin filament system in skeletal and cardiacmuscle is reg-ulated by a family of proteins known as troponins, which formpart of the troponin complex. Troponin I is encoded by three dif-ferent genes. Cardiac troponin I was previously shown to be ex-clusively expressed in the myocardium in adults [37], butrecently, it was revealed that it is also expressed in developing
2 Muscle Stem Cells for Heart Repair
©AlphaMed Press 2014 STEM CELLS TRANSLATIONAL MEDICINE
skeletal muscle [36]. It is distinct from the fast and slow forms inskeletalmuscle [37]. Cardiac troponin T is a component of the tro-ponin complex. It is encoded by the gene TNNT2 and allows acto-myosin interaction and contraction to occur in response to Ca2+.TNNT2 is a common mutation in familial hypertrophic cardiomy-opathy, but surprisingly, it has been found that distinct TNNT2mutations also lead to dilated cardiomyopathy [38]. It is alsoexpressed in skeletal muscle during injury. Apart from this, skel-etal muscle-specific troponins are transiently present in the im-mature heart [39]. In the early phases of myogenesis in skeletalmuscle, cardiac-like excitation-contraction coupling mechanismsdominate, whereas skeletal muscle-like excitation-contractioncoupling dominates in more mature muscle [40, 41]. Thus, be-tween cardiac and skeletal muscle, there is a strong overlap inthe genes encoding key proteins responsible for contractility,which is a hallmark of striated muscle.
Cardiac andskeletalmusclesalsosharecommonmetabolic reg-ulatoryproteins.Fattyacid-bindingprotein3 isamemberofa familyof binding proteins and is mainly expressed in cardiac and skeletalmuscle cells, and it has been linked to fatty acid metabolism, traf-ficking, and signaling [42]. UDP-N-acetylglucosamine 2 epimerase/N-acetylmannosamime kinase (GNE) is involved in the early devel-opment of both cardiac and smoothmuscle. GNE-deficient cardiaccells degraded very soon, and their beating capacity decayed rap-idly. Skeletal muscle-committed cells were identified in the GNE-deficient embryonic stem cell cultures by the expression of Pax7,MyoD, andMHCmarkers. GNE is strongly involved in cardiac tissueand skeletal muscle early survival and organization, as shown bythese results [43].
A common finding in certain types of muscular dystrophy, in-cluding Emery-Dreifuss, Duchenne, and Becker type dystrophies,is chronic cardiac diseases [44]. Some types are caused by muta-tions in the b-sarcoglycan-associated proteins [45], which areexpressed both in cardiac and skeletal muscle. Limb-girdle mus-cular dystrophy type 2E is caused by mutations in Sgcb gene,and Sgcb-deficient mice develop severe cardiomyopathy and se-vere muscular dystrophy, suggesting that cardiac and skeletalmuscle pathologies arise from a common origin [46]. All of thesestudies indicate how closely cardiac and skeletalmuscle are inter-linked, especially in their immature phase. Recently, our groupfound that skeletal and cardiac muscle share similar transcriptionfactors and structural proteins during development [36]. How-ever, the molecular mechanisms that regulate the fate determi-nation between these two lineages of striated muscle remainpoorly understood.
SKELETAL MYOBLASTS: AN EARLY CANDIDATE FOR
CELLULAR CARDIOMYOPLASTY
Given their phenotypic similarity to cardiac muscle, ease ofisolation/expansion, and relative resilience to hypoxia, skeletalmyoblasts were considered an appealing cell source for cellularcardiomyoplasty [47–54]. Skeletal myoblasts have shown prom-ise for ischemic heart regeneration, making them potentialcandidates for early cardiomyoplasty studies [55]. Skeletal myo-blasts were the first cell type to enter the clinical arena of heartregeneration. Lavine and Upcott in 1937 [56] performed the firstof its kind surgery in which his team treated myocardial ischemiaby using a skeletal muscle graft to the heart. The patient was typ-ically acromegalic. Before the procedure, he could not walk 5
yards without any rest, but after the surgery, he was able to walk140 yards without any shortness of breath. Early animal studiesconducted in porcine animal models showed that myoblast-derived muscle grafts remained functionally isolated from thesurrounding myocardium. The outcome did not reveal an in-creased frequency in ventricular tachycardia or fibrillation [57].Menasche et al. [49] in 2001 transplanted autologous skeletalmyoblasts into the postinfarction scar during coronary artery by-pass grafting of remotemyocardial areas. However, in thedistinctcase of skeletal myoblasts, the results of several preclinical andclinical studies have shown improved functional outcomes fol-lowing transplantation of these myogenic progenitors into post-infarction scar.
Table 1 summarizes the potential advantages and disadvan-tages of using various stem cells types for cardiac repair. Arrhyth-mogenic complications have raised concern over the safety ofadoptive transfer of skeletal muscle cell therapy [3, 11, 46–48,58]. There is a risk of ventricular arrhythmias [49, 59–62]. The factremains that myoblast transplantation has its limitations, asimplanted cells have limited survival and do not spread uniformlyat the siteof injury [48]. Skeletalmyoblastsdonotdifferentiate intocardiomyocytes but rather into multinucleated myotubes after in-jection into the heart. These myotubes form islands of conductionblock in the heart and lack gap junctions. This results in electricalinhomogeneities that slow conduction velocity and predisposepatients to re-entrant ventricular arrhythmias [63]. Whereas skel-etal myoblasts (and other skeletal muscle-derived cells) showpromise of improved myocardial contractile function, risk of ar-rhythmia is an issue that needs to be addressed to advance thistherapy.
CARDIOMYOCYTE DIFFERENTIATION POTENTIAL FROM SKELETALMUSCLE-DERIVED CELLS
Since skeletal myoblasts do not differentiate into functioning car-diomyocytes in vivo, efforts have been made to isolate cells fromskeletal muscle that can differentiate into cardiomyocytes in vitroor in vivo.Theskeletalmuscle-derived stemcell (MDSC) is a somaticstem cell that is different from skeletal myoblasts (satellite cell)in its multipotent properties [64–66]. Table 2 summarizes the dif-ferences between skeletal myoblasts and MDSCs. MDSCs areobtained fromskeletalmuscle via apreplatemethodor fluorescentactivated cell sorting of surface markers and are easily expandedunder in vitro culture environment as an autologous cell source[54, 65, 66]. MDSCs differentiate into skeletal muscle, bone, ten-don, nerve, endothelial, hematopoietic, and smooth muscle cells[54, 64–67]. They have long-term proliferation capacity and en-hanced resistance to hypoxia. Several studies have shown thatMDSCs can differentiate into functioning cardiomyocytes usingvarious strategies. Clause et al. [68] demonstrated that rat MDSCscoulddifferentiate intocardiomyocyte-likecellsexpressingcardiac-specific genes and proteins by combining cell aggregation with 3Dculture in a collagen bioreactor.Winitsky et al. [69] isolated nonad-herent cells, skeletal-based precursors of cardiomyocytes (SPOC)cells (skeletal-based precursors of cardiomyocytes), from adultmurine skeletal muscle that become beating floating cells. TheyareCD342/CD452/c-kit2. Themuscle-derivedsidepopulationcellsexpress the surface marker Sca-1 (65%), and the beating cellsdevelop out of the Sca-12 pool, which makes up 20%–40% ofthe total isolated cells. Cells expressing the cardiac-specific
Hassan, Tchao, Tobita 3
www.StemCellsTM.com ©AlphaMed Press 2014
marker Nkx2.5 and spontaneously contracting in culture weredetected in reverse transcription-polymerase chain reactionanalysis. The presence of specificmRNA codingmarkers for skel-etal (myogenin, Myf5) and cardiac muscle (GATA4) and smoothmuscle actin was seen in differentiated cells. Interestingly, allthe above-mentionedmarkerswere alsodetected in floating pro-liferating progenitor cells. This supports the idea that stem cellscan express markers of multiple lineages in their differentiatingstate [70]. Skeletal muscle interstitium-derivedmultipotent stemcells (Sk-34 and Sk-DN cells) differentiated into cardiomyocytes ina cardiac environment [50, 71]. After 4 weeks, the transplantedcells became cardiomyocytes with desmosomes and intercalateddiscs associated with gap junctions [50]. Myotube formation was
not observed. Sk-34 and Sk-DN cell differentiation is based ona cardiac environment. Table 3 lists the studies done over theyears showing cardiomyocyte differentiation and cardiac repairpotential from skeletal muscle-derived stem/progenitor cells.Taken together, these studies emphasize the importance of iso-lation techniques and culture conditions in obtaining the desiredtarget cell. For example, Parker et al. [72] showed that activationof Notch signaling during ex vivo expansion of muscle-derivedcells can significantly improve their engraftment.
There are a number of problems faced during isolation ofthese cells. Cell surface markers define muscle-derived stemand progenitor cell populations. Some of these markers are re-stricted to these populations, whereas other markers are shared
Table 1. Advantages and disadvantages of various stem cell sources
Cell type Advantages Disadvantages
Skeletal myoblast (satellite cell) Contractile phenotypeProduction of proangiogenic factorsCan be rapidly harvested and easily expandedin vitro prior to autologous transplantation.
Relatively resistant to hypoxic conditionsImproved functional outcomes followingtransplantation
Arrythmogenic complicationsLow long-term survival rateNonuniform spreading at the site of injury with
conventional delivery methodsHigh rate of rejectionLack of differentiation into cardiomyocytes in vivoLimited expansion compared with pluripotent
stem cellsInvasive isolation procedure
Bone marrow mesenchymalstem cells
Has been tested in clinical settings with positiveoutcomes
Immunoprivileged profilePotent paracrine and proangiogenic effectsleading to improved cardiac function
Differentiate into cardiomyocytes and endothelialcells in vivo
No widely used protocols for in vitro cardiomyocytedifferentiation with nontoxic agents
Lack of well-defined markers for cell isolationLimited expansion ability in vitroInvasive isolation procedure
Adipose stem cells Phenotype similar to that of bone marrowmesenchymal stem cells
Can differentiate into cardiomyocytes in vitroEasy to obtain large numbers of multipotent stemcells by liposuction
Augment cardiac function similar to bone marrowmesenchymal stem cells
Therapeutic benefit mainly from paracrine effectsand angiogenesis rather than differentiationinto cardiomyocytes
No widely used protocols for in vitro cardiomyocytedifferentiation with nontoxic agents or withoutcoculture with cardiomyocytes
Somewhat invasive isolation procedureLimited expansion ability in vitro
Induced pluripotent stem cells Can theoretically be expanded indefinitely in vitro,providing an unlimited source of stem cells
Similar in morphology, proliferation, surfaceantigens, gene expression, telomerase activity,epigenetic status of pluripotent cell specificgenes, and cardiac potential to humanembryonic cells
AutologousPluripotent
Risk of teratogenesisMaturation stages are not uniformChromatin modificationRisk of unwanted cellular transdifferentiationEpigenetic reprogrammingPotential immunogenicitySomatic cell isolation can be invasive from some
tissuesUntested in clinical setting
Table 2. Comparison of MDSCs and skeletal myoblasts
Characteristic MDSCs Satellite cells
Differentiation potential Osteogenic, chondrogenic, neural, endothelial,hematopoietic, cardiac, myogenic [31]
Myogenic [108]
Marker profile Sca-1+/2, Flk-1+, Pax72, M-cadherin2 [31] Sca-12, Flk-12, Pax7+, M-cadherin+ [31]
Regeneration potential Better [81] Good [81]
Engraftment Over 3 months [54] Several weeks [54]
Ischemia tolerance Better [54] Good [54]
Clinical outcomes Preclinical; MDSC sheets can improve heartfunction and prevent arrhythmias in animalmodels [90]
Studies suggest improved ventricularfunction but variable incidence of arrhythmias[62, 109]
Abbreviation: MDSC, muscle-derived stem cell.
4 Muscle Stem Cells for Heart Repair
©AlphaMed Press 2014 STEM CELLS TRANSLATIONAL MEDICINE
Table3.
Studiesofcardiacdifferentiation/rep
airfrom
skeletalmusclestem
cells
Study
Species
Isolationmethod
Culture
conditions
Timein
culture
Cardiomyocyte
induction/
differentiation
Key
findings
Winitskyet
al.[69
],20
05Mouse
Platingandpassaging
nonadheren
tSca-12
/+cells
50:50DMEM
/F12
,5%FBS,
EGF,bFG
F,insulin,
transferrin,selen
ium,
ethanolamine
Upto
4weeks
Spontaneo
uslybeating
phen
otype
Theinjected
cells
inamouse
modelofacute
infarctionarestillvisibleafter3monthsas
striated
heartmusclerestricted
tothe
regionofthecardiacinfarct.
Roelletal.[98
],20
07Transgen
icmice
Cardiac
andskeletal
musclecells
expressing
EGFP
under
controlofthe
human
a-actinpromoter
wereharvested
from
transgen
icmice
Invivo
transplantation
Upto
2weeks
Transplantedinto
syngeneic
wild-typemice
Skeletalmyoblastsgenetically
engineered
toexpressCx43
conferredaprotection
similar
tothatofem
bryoniccardiomyocytesagainst
indu
cedventriculartachycardia.
Invernicietal.[110],200
8Human
Isolatedfrom
the
brachioradialis
and
paravertebralm
uscleand
culturedinflasks
coated
withtype
Icollagen
TypeIcollagen/SCM,
20–50
mg/lplatelet-derived
growth
factorBB,102
7
to10
29M9cis-RA
Upto
10days
Retinoicacidtreatm
ent
Expression
ofcardiomyogeniclineage-specific
antibo
dies
withimmun
ostaining;CD133,
CD105,desm
in,and
vimentin.
Spon
taneou
scontraction.
Cardiac-like
respon
setoincreasedextracellular
calcium.
Retinoicacid-treated
skeletalmusclestem
cells
expressedconnexin43
whencocultured
with
mou
secardiomyocytes.
Cells
weredetectableeven
5weeks
after
injectionwhentransplanted
into
ischem
icheart.
Tamakietal.[50
],20
08Mouse
CD34
+/CD45
2(Sk-34
)stem
cells
wereen
zymatically
isolatedfrom
green
fluorescentprotein
transgen
icmice
DMEM
,5%–10
%FCS;IM
DM/
10%FCS;20
%FCS/IM
DM
6days
Invitroclonalculture
and
coculture
withem
bryonic
cardiomyocytes,invivo
transplantation
into
anude
ratmyocardialinfarction
model
Highexpression
ofGATA
-4,N
kx2-5,Isl-1,M
ef2,
andHand2
was
seen
oncoculturetogether
withform
ationof
gap-junction
sand
synchronou
scontractionfollowing
sphere-like
colony
form
ation.
Donor
cells
exhibitedtypicalcardiom
yocyte
structurewith
form
ationof
gap-junctio
ns,as
wellasintercalated
discsanddesm
osom
esbetweendonorandrecipientand/or
donor
anddonorcells
at4weeks
after
transplantationoffreshlyisolated
Sk-34cells.
Arsicet
al.[70],2008
Mouse
Serialpreplatingtechnique;
nonadheren
tcell
population
isolated
50:50DMEM
/F12
Upto
2months
Plated
onCCL14
6fibroblast
MDSC
exhibitedSca-1(65%
),Bcrp-1(80%
),MyoD(15%
),Neuronalb
IIItubulin(25%
),GFAP(30%
),andNkx2.5(1%).
Tamakietal.[71
],20
10Mouse
CD34
2/452
(Sk-DN)stemcells
wereen
zymaticallyisolated
from
greenfluorescent
proteintransgen
icmice
DMEM
,5%–10
%FCS;IM
DM/
10%FCS,10
ng/mlbFG
F,20
ng/mlEGF
Upto
2weeks
Singlecell-derived
single-sphereim
plantation
into
myocardium
Donorcells
exhibited
typicalcardiomyocyte
structure
withtheform
ationof
gap-junctions
betweendonorandrecipient
cells
after4weeks
ofimplantation.
Expression
ofspecificmRN
Asfor
cardiomyocytes,such
ascardiacactin
and
GATA-4,N
kx2-5,Isl-1,M
ef2,andHand2.
Cellfusion-independentdifferentiation.
Hassan, Tchao, Tobita 5
www.StemCellsTM.com ©AlphaMed Press 2014
Table3.
(Con
t’d)
Study
Species
Isolationmethod
Culture
conditions
Timein
culture
Cardiomyocyte
induction/
differentiation
Key
findings
Clauseet
al.[68],2010
Rat
Modifiedpreplating
technique
DMEM
,10%
FBS,10
%horse
serum,collagentype
I/Matrigeltissueconstruct,
DMEM
,5%FBSfor
differentiation
Upto
9days
Three-dim
ensionalgel
bioreactor
MDSCsexpressed
cardiacgenes/proteins
afteraggregateform
ationand3D
bioreactorculture.
MDSC-CMsexpressed
Cx43gapjunctionsand
generated
cardiac-likecalcium
transien
ts.
MDSC-CMsgenerated
strain-dep
enden
tactive
contractileforce.
Neefet
al.[111],2012
Neo
natalmice
Prep
latingtechnique
40%Ham
’sF10med
ium,20%
FBS,2.5ng/mlbFG
F,40
%DMEM
,2%horseserum,
pen
icillin/strep
tomycin
(1:100),fungizone(1:1,000)
Upto
14days
Collagenconstructs
Coup
lingofcells
from
pre-engineeredtissue
constructsto
cellsinem
bryonicheartslices
showed
slower
conductionvelocities
than
myocardialcellswiththeem
bryonicheart
slices,lower
maxim
um
stim
ulation
freq
uen
cies,higher
sensitivities
tothegap
junctioninhibitor,skeletalmyoblast-based
transplantablegraftsthat
electrically
coupledto
myocardium.
PerumalSrinivasan
etal.[11
2],201
2Neo
natalmice
Prep
latingtechnique
40%Ham
’sF10med
ium,20%
FBS,2.5ng/mlbFG
F,40
%DMEM
,2%horseserum,
pen
icillin/strep
tomycin
(1:100),fungizone(1:1,000)
Upto
14days
Collagenconstructs,serum
starvation
Skeletalmyoblastswithintissueconstructs
dem
onstratedlong-term
survival,o
rdered
alignmen
t,preserved
ability
todifferentiateinto
contractilemyotubes.
Theexpressionofgapjunctionandcell
adheren
ceproteinswas
maintained
or
increasedthroughoutd
ifferentiationwhen
thetissueconstructsweresubjected
topassive
longitudinaltensilestress.
Oshim
aet
al.[54],2005
Mouse
Modifiedpreplating
technique
DMEM
,10%
FBS,10
%horse
serum,1%pen
icillin/
streptomycin,0.5%chick
embryoextract
12weeks
Invivo
transplantation
(C57
BL/6mice)
Compared
withmyoblasts,MDSCs
dem
onstratedmore
persisten
ten
graftm
ent,expressionofconnexin43,
increasedangiogenesis,b
ettertolerance
foroxidativestress,greater
functional
improvemen
t,andadoptionofacardiac
phen
otypeat
lowfreq
uen
cy.
Okadaet
al.[75],20
08Human
Fluorescen
ceactivatedcell
sortingbyCD34,C
D56,and
CD14
4
DMEM
,10%
FBS,10
%horse
serum,1%pen
icillin/
streptomycin,1%chick
embryoextract
6weeks
Invivo
transplantation
(NOD/SCID
mice)
Human
myogenic-endothelialcells(CD34
2/
CD45
+/CD14
4+)aresimilarto
murine
MDSCsintheircapacityforheartrepair.
They
improved
cardiacfunctio
n,reduced
scarring,stimulated
neovascularization
,and
demon
stratedlong-term
engraftm
ent
better
than
myoblastsor
endo
thelialcells.
Xianget
al.[113],201
1Mouse,h
uman
Modifiedpreplating
technique
DMEM
,10%
FBS,10
%horse
serum,1%pen
icillin/
streptomycin,0.5%chick
embryoextract
3weeks
Invivo
transplantation
(NOD/SCID
mice)
Wnt11-transducedMDSCsshow
edgreater
engraftm
entandcardiomyogenic
differentiationcomparedwith
controlM
DSCs.
SomeWnt11-transducedMDSCsbeat
spontaneouslyinvitro.
6 Muscle Stem Cells for Heart Repair
©AlphaMed Press 2014 STEM CELLS TRANSLATIONAL MEDICINE
with other cell populations. The marker profile-based isolationmethods exclusively depend on the expression of cell surfacemarkers that are variable and may change under in vitro cell cul-ture conditions. Thus, thesemethods have their limitations. Pres-ently, the most prevalent method for isolating MDSCs is themodified preplate technique. It is a marker profile-independenttechnique that is based on variable adherence of freshly dissoci-atedmuscle cells to collagen-coated flasks. However, the isolatedpopulations are heterogeneous [73]. Multiple nonsatellite stemcell fractions reside in skeletalmuscle, although it remainsunclearhow these different populations are related. Okada et al. [74]demonstrated that slowly adhering cells showed greater regener-ative potential and oxidative/inflammatory stress tolerance com-pared with rapidly adhering cells. Myogenic-endothelial cells,cells that express both myogenic and endothelial markers (CD56,CD34, and CD144), can be isolated from skeletal muscle and havebeen shown to have superior regenerative properties and stresstolerance compared with myoblasts [75, 76]. The blood vesselsof skeletal muscle also contain stem cells, perivascular stem cells,whichdemonstratemyogenic andmultipotent potential [77]. Theyare isolated on the basis of CD146 expression and lack of CD34,CD45, CD144, and CD56 expression.
In vitro generated MDSC-derived cardiomyocytes are moresimilar functionally and biochemically to fetal cardiomyocytes[78]. However, the rate of cardiomyocyte differentiation alone islikely not sufficient to explain the functional improvements gainedfromMDSC transplantation. Another possiblemechanismbywhichMDSCs exert therapeutic benefit is by acting as a reservoir to se-crete paracrine factors that promote angiogenesis and cell survivalwithin the injured microenvironment [54]. Transplanted undiffer-entiated human skeletal myoblasts (CD56+) in an immunodeficientnude ratmodel demonstrated expression of human-specificmatrixmetalloproteinase 2 (MMP-2) TNNI3, CNN3, proangiogenic factors(PGF), TNNT2, PAX7, transforming growth factor-b (TGF-b), andinsulin-like growth factor-1 (IGF-1) 1 month after transplant. Geneexpression showed upregulation of PGF, antiapoptotics (BAG-1,BCL-2), heart development (TNNT2, TNNC1), and extracellular ma-trix remodeling (MMP-2, MMP-7) in skeletal myoblasts. The datasuggested that myoblast-secreted factors may contribute to thebeneficial effects ofmyogenic cell transplantation in infarctedmyo-cardium [79].
The paracrineeffectexertedbyMDSCsandother stemcells hasa positive effect within the injured myocardium. Bioactive mole-cules such as basic fibroblast factor (bFGF), vascular endothelialgrowth factor (VEGF), platelet-derived growth factor, SDF-1, hepa-tocyte growth factor (HGF), and IGF-1 confer cardioprotectiveeffects. Inaddition, secretionofmolecules suchasVEGF, angiopoie-tin, and bFGF increase blood vessel formation in the ischemicregion, improving perfusion and function. HGF and IGF-1 also acti-vate resident stem cells and promote endogenous repair mecha-nisms. Additional factors such as TGF-b, MMPs, and tissueinhibitorofmetalloproteinasereduce fibroblastproliferation, fibro-sis, and left ventricular dilation [80, 81]. Okada et al. [82] showedthat a subpopulation of slowly adhering MDSCs showed enhancedparacrine factor secretion, increased stress tolerance, engraftment,and angiogenesis compared with rapidly adhering MDSCs. Theyalso found increased cardiomyocyte proliferationwithin the infarctregion, suggesting the enhancement of endogeneous repairmech-anisms. The selective enrichment of certain types of MDSCs mayimprove their regenerative effects through enhancement of para-crineeffects. StudiesofMDSCtransplantationhaveshownthatonlyTa
ble3.
(Con
t’d)
Study
Species
Isolationmethod
Culture
conditions
Timein
culture
Cardiomyocyte
induction/
differentiation
Key
findings
Sekiya
etal.[90],2013
Mouse
Modifiedpreplating
technique
DMEM
,10%
FBS,10
%horse
serum,1%pen
icillin/
streptomycin,0.5%chick
embryoextract
12weeks
Invivo
transplantation
(NOD/SCID
mice)
MDSCstransplantedas
cellsheetsshowed
areductionofleftventriculardilationand
sustained
contraction.
MDSC
sheetsform
edaligned
myotubes
with
increasedcapillaryden
sity
compared
with
directinjectionofMDSCs.
MDSC
sheetsallowed
betterfunctional
recovery
witharrhythmias.
Abbreviations:3D
,three-dim
ensional;bFG
F,basicfibroblastgrowth
factor;CM,cardiomyocyte;D
MEM
,Dulbecco’smodifiedEagle’smed
ium;EGF,ep
idermalgrowth
factor;EG
FP,enhancedgreenfluorescent
protein;FBS,fetalbovineserum;FCS,fetalcalfserum;IMDM,Iscove’smodifiedDulbecco’smed
ium;M
DSC,m
uscle-derived
stem
cell;RA,retinoicacid;SCM,stem
cellmed
ium.
Hassan, Tchao, Tobita 7
www.StemCellsTM.com ©AlphaMed Press 2014
a small fraction of donor cells demonstrates long-term engraft-ment, and themajority of cells within the regenerating tissue comefrom the host via the chemoattraction of postnatal stem cells fromthe vasculature [83]. Thus, the paracrine or bystander effect ofMDSCs may be as important as, if not more important than, myo-genic differentiation in contributing to cardiac repair.
TISSUE-ENGINEERING APPROACHES TO CARDIAC REPAIR
Transvascular methods of cell delivery are commonly used to treatrecently infarcted myocardium. Intracoronary artery infusion candeliver a high concentration of cells homogeneously to the siteof injury. Direct needle injection into the ventricular wall is pre-ferred for patients late in the disease process when occlusion ofthe coronary artery prevents transvascular delivery [84]. However,it often results inpoor engraftment, poor survival, and further dam-age by needle injury. Tissue-engineering approaches may providea more effective means of cell transplantation. Two main engi-neered tissue transplantation approaches for cardiac tissue arethree-dimensional scaffolds and cell sheets. One of the most chal-lenging issues in tissueengineering is the reconstructionofmyocar-dium in three dimensions. Three-dimensional (3D) scaffolds arenow available [85, 86]. Cell sheets are used for treating advancedheart failure. Myocardial cell sheets decrease fibrosis and increasevascularization in the injured heart [87–90]. In 2006, Zimmermanet al. [91] produced convincing evidence that a heart tissue canbe produced with enough contractile force to support a failingheart.Neonatal ratheart cellswereseededwith liquidcollagentypeI and Matrigel (BD Biosciences, San Diego, CA, http://www.bdbiosciences.com) in molds. The rings were grafted onto the in-farcted ratheart andafter1monthshowedpositive results. Furtherdilation of the heart was prevented, and systolic wall thicknessincreased. In 2011, Fujimoto et al. also proved that engineeredcardiac tissue from immature cardiomyocytes can functionally inte-grate intodamagedmyocardium. In this study,engineered fetal car-diac tissue proved to be more successful than neonatal tissue.Engineered fetal cardiac tissue implantation increased left ventriclecontraction and showed higher cardiomyocyte proliferation thanengineered neonatal cardiac tissue [92].
The major issues concerning the therapeutic application ofstem cells remain unresolved because of three primary factors:poor survival, marginal proliferation, and limited functionalengraftment/commitment within the host tissue. Furthermore,the cells should be prepared to combat against apoptotic, ne-crotic, and hypoxic conditions prevalent within the damaged tis-sue. Finally, if cellsmanage to proliferate, they can be functionallyincapable of appropriate lineage commitment and can end in anoncogenic transformation [93].
The in vivo studies with MDSCs show promising results formeeting some of these challenges. Repair of the infarcted heartwith MDSCs is more effective than conventional myoblasts [54].MDSCs injected into the myocardium of infarcted heart showedoutstanding survival and engraftment, promoted angiogenesis,and increased left ventricular function in amore effectivemannerin comparisonwith the transplantation of skeletalmyoblasts [94].In a postinfarctedmyocardium, transplantedMDSCs sustained itscontractile function, preventing left ventricular chamber remod-eling. Some transplanted donor MDSCs differentiated into bothsk-fMHC- and/or cardiac troponin I-positive muscle cells [54,75]. Clause et al. [68] demonstrated that MDSCs cultured withina three-dimensional engineered tissue construct differentiated
into an immature functioning cardiomyocyte phenotype. Trans-plantation of tissue-engineered cell sheets has negated someof the limitations by eliminating use of trypsin, direct needle in-jury to the heart, and by covering larger infarcted area [95, 96].Reduction in left ventricle (LV) dilation and sustained LV contrac-tion were displayed with the implanted MDSC sheet. It yieldedbetter functional recovery of chronic infarctedmyocardium com-paredwith directMDSC injectionwithout any significant arrhyth-mic events, indicating that this cell sheet delivery system couldmarkedly improve the myocardial regenerative potential of theMDSCs [90]. These studies suggest that tissue-engineering ap-proachesmay provide ameans to further improve upon the func-tional benefits derived from MDSC transplantation.
Tissue-engineering approaches help to address one of themajor limitations of current delivery modalities—the immediateandmassive attrition of naked cells that occurs after cell delivery,which leads to low retention of implanted cells even 24 hoursafter the procedure. However, current tissue-engineering ap-proaches focus on building complex 3D structures, which pre-cludes catheter-based delivery and necessitates surgery. Usingthe cell patch approach, transplanted cells are initially localizedto the epicardial region. A recent development, which improvescell retention, is the delivery of hydrogel-cell liquid suspensionsvia catheter [97]. The hydrogel polymerizes en route and trapscells in the target tissue. If successful, this method can combinethe demonstrated safety of catheter-based delivery with the abil-ity of a tissue-engineered scaffold to improve engraftment.
FUTURE CHALLENGES AND OPPORTUNITIES
Although skeletal muscle stem/progenitor cells have benefits,a large number of injected cells undergo early death. The first pro-spective randomized placebo-controlled phase II skeletal myoblasttrial (MAGIC trial) exhibited lack of efficacy and was discontinuedprematurely [48]. The trial’s disappointing results were due to sev-eral reasons: a low rate of initial cell retention, a high rate of sub-sequent cell death, and the inability of engrafted myoblasts toestablish functional electromechanical connections with the hostcardiomyocytes [3]. In addition, a trend toward excess arrhythmiaswas observed in myoblast-treated patients despite the use of theprophylactic antiarrhythmic drug amiodarone. This raised safetyconcerns that had already been raised by earlier phase 1 trials. Incontrast, SEISMIC trial [63] argued that injectionof autologous skel-etal myoblasts in heart failure patients is safe and may providesymptomatic relief, as a trend toward increased exercise tolerancewasobserved in the cell-treated group.Nevertheless, no significanteffect on global left ventricular ejection fraction was detected. Allthis taken together indicates that more work needs to be doneto bridge the gap between preclinical animal models and clinicaltrials.
In light of the mixed results from clinical trials, further workhas gone into eliminating the heterogeneity of transplanted cellsand improving electromechanical coupling between transplantedand host myocytes. Transplantation of myogenic-endothelialcells that express CD56, CD146, and Ulex, purified from humanskeletal muscle into the ischemic heart, drastically improved leftventricular function, reduced scar tissue, and promoted angio-genesis [54]. Connexin-43 is the predominant gap junction ofthe ventricular myocardium. Skeletal myoblasts lack connexin-43 after fusion into elongated contractile myotubes. In cellularmonolayers, conduction velocity was slowed and re-entry-induced
8 Muscle Stem Cells for Heart Repair
©AlphaMed Press 2014 STEM CELLS TRANSLATIONAL MEDICINE
arrhythmias were promoted when skeletal myoblasts werecocultured with neonatal cardiomyocytes in vitro and studiedwith high-resolution optical mapping. The proarrhythmic effectwas reducedwhen engineered cells overexpressed connexin-43[98]. The findings were later tested in an animal model [11].Methods to improve electromechanical compatibility betweenengrafted muscle and host myocardium are currently underinvestigation.
Issues related to electromechanical compatibility betweencardiac and skeletal muscle tissue could be ameliorated by gen-erating cells from MDSCs that have a cardiomyocyte-like pheno-type. The heart also contains resident stem cells. Oh et al. [99]identified in 2003 an independent population of Sca-1+ cardiacstem cells as a subgroup of cells (constituting ∼14%) isolated inthe noncardiomyocyte cell fraction of the adult mouse heart ina whole heart digestion. Sca-1+ cells coexpressed CD31 andCD38 and lacked c-Kit, CD34, and CD45 when freshly isolated.Ninety-three percent of the side population was Sca-1+. Freshlyisolated Sca-1+ cells did express the early cardiac-specific tran-scription factors GATA4, Mef2C, and Tef-1 but not Nkx2.5 orgenes encoding cardiac sarcomeric proteins. Sca-1+ cells en-graftedat amuchhigher rate than Sca-12 cells in amousemodelof ischemia-reperfusion after 2weeks and could be found form-ing new cardiomyocytes. Cardiac stem cells in bulk cultureupregulated GATA-4 expression resulting in enhanced cardio-myocyte differentiation, suggesting that the GATA-4 high c-kit+
cardiac stem cells have potent cardiac regenerative potential.The study also demonstrated spontaneous differentiation intoskeletalmyocytes [100].Hasanet al. [101] establishedcardiacplu-ripotent stem cell-like cells from the left atriumof adult rat heartsthat could differentiate into beating cardiomyocytes in the
methylcellulose-based medium containing interleukin-3 andstem cell factor, which contributed to the differentiation into car-diac troponin I-positive cells. Distinctly small populations of plu-ripotent stem cell-like cells from the left atrium coexpressedGATA4 and myogenin, which are markers specific to cardiomyo-cytes and skeletal myocytes, respectively. These could differenti-ate intoboth cardiac and skeletalmyocytes. These studies suggestthe possibility that cardiac and skeletal muscle can arise froma common myogenic progenitor, and stem cells purified fromskeletal muscle may have similar differentiation potential, asdemonstrated by studies of cardiomyocyte differentiation fromMDSCs.However, thepathways thatdeterminewhether a cell dif-ferentiates into a cardiomyocyte or skeletal muscle cell are onlybeginning to be unraveled.
A hypothesis is presented in Figure 1 showing how skeletalmuscle stem/progenitor cells can be induced to become cardiacmuscle with post-transcriptional modification. Microribonucleicacids (micro-RNAs, miRs) are post-transcriptional regulators ofcardiac and skeletal myogenesis, including miR206, which specif-ically promotes skeletal myogenesis [102–104] as part of anintrinsic cell-regulatory program. Crippa et al. [105] isolated car-diac progenitors from neonatal sarcoglycan-null mouse heartsaffected by dilated cardiomyopathy, and they spontaneously dif-ferentiated into skeletal muscle fibers both in vitro and whentransplanted into regenerating muscles or infarcted hearts. Theabsence of expression of miR669q and with downregulation ofmiR669a was associated with differentiation potential. Skeletalmyogenesis was prevented by miR669a and miR669q acting up-stream of myogenic regulatory factors by directly targeting theMyoD untranslated region. Successful conversion of cardiac cellsinto skeletal muscle fibers opened a huge area of discussion if the
Figure 1. MicroRNAs post-transcriptionally regulatemyogenesis. miR-206 specifically promotes skeletal muscle differentiation, whereasmiR-669 promotes cardiac differentiation by inhibiting MyoD, a skeletal muscle transcription factor. By modulating expression of these and othermuscle-specific microRNAs, stem cells can be induced to differentiate into cardiac or skeletal muscle. The local microenvironment and solublefactors also play important roles in stem cell differentiation. Abbreviations: CM, cardiomyocyte; ECM, extracellular matrix; MHC, myosin heavychain; MIR, microRNA.
Hassan, Tchao, Tobita 9
www.StemCellsTM.com ©AlphaMed Press 2014
reverse is possible. MDSCs have genes similar to those of cardiacand skeletal muscle, and cardiac and skeletal muscles are inter-changeable because of miR669. The physical environment mayalso present important environmental cues [106]. Three-dimensional cultures and cardiac-specific extracellular matrixhave been shown to promote cardiomyocyte induction [36, 68,107].
CONCLUSION
In any endeavor as complex and perplexing as stem cell research,controversies and disagreements are to be expected. Whereasearly clinical trials of skeletal myoblast transplantation yieldedmixed results and did not meet initial expectations, more recentworks have shown that improved isolationmethods, novel tissue-engineering approaches, and differentiation strategies may im-prove the efficacy of myogenic stem cell transplantation. Skeletalmuscle-derived stem cells remain the only stem cell that can
differentiate into a muscle phenotype and can be isolated easilyin abundant numbers. Cardiovascular regenerative medicine isstill in its early stages, but recent studies show renewed promise.The field of regenerative medicine has been quite progressive, asa search on PubMed for the keywords “cardiac, stem cell, heart,”yields more than 9,000 references as of today with almost 2,000review articles to summarize all current understanding. This fieldwas nonexistent a little over a decade ago.
AUTHOR CONTRIBUTIONS
N.H. and J.T.: conception and design, manuscript writing; K.T.:conception and design, manuscript writing, final approval ofmanuscript.
DISCLOSURE OF POTENTIAL CONFLICTS OF INTEREST
The authors indicate no potential conflicts of interest.
REFERENCES1 Go AS,Mozaffarian D, Roger VL et al. Execu-
tive summary: Heart disease and stroke statistics—2013update: A report from theAmericanHeartAssociation. Circulation 2013;127:143–152.2 MacLellan RW. Mending broken hearts
one cell at a time. J Mol Cell Cardiol 2002;34:87–89.3 SimEK, JiangS, Ye L et al. Skeletalmyoblast
transplant in heart failure. J Card Surg 2003;18:319–327.4 Dai W, Hale SL, Martin BJ et al. Allogeneic
mesenchymal stem cell transplantation in post-infarcted ratmyocardium: Short- and long-termeffects. Circulation 2005;112:214–223.5 Olivares EL, RibeiroVP,WerneckdeCastro
JP et al. Bonemarrow stromal cells improve car-diac performance in healed infarcted rat hearts.Am J Physiol Heart Circ Physiol 2004;287:H464–H470.6 XuM,WaniM, Dai YS et al. Differentiation
of bone marrow stromal cells into the cardiacphenotype requires intercellular communica-tion with myocytes. Circulation 2004;110:2658–2665.7 Orlic D, Kajstura J, Chimenti S et al. Bone
marrow cells regenerate infarcted myocar-dium. Nature 2001;410:701–705.8 Beltrami AP, Barlucchi L, Torella D et al.
Adult cardiac stem cells are multipotent andsupport myocardial regeneration. Cell 2003;114:763–776.9 BergmannO,BhardwajRD,BernardSet al.
Evidence for cardiomyocyte renewal inhumans. Science 2009;324:98–102.10 Kajstura J, Urbanek K, Perl S et al. Cardi-
omyogenesis in the adult human heart. Circ Res2010;107:305–315.11 Murry CE, SoonpaaMH, Reinecke H et al.
Haematopoietic stemcells donot transdifferen-tiate into cardiac myocytes in myocardialinfarcts. Nature 2004;428:664–668.12 Takahashi K, Yamanaka S. Induction of
pluripotent stem cells from mouse embryonicand adult fibroblast cultures by defined factors.Cell 2006;126:663–676.13 Shiba Y, Hauch KD, Laflamme MA. Car-
diac applications for human pluripotent stemcells. Curr Pharm Des 2009;15:2791–2806.
14 Wu SM, Hochedlinger K. Harnessing thepotential of induced pluripotent stem cells forregenerative medicine. Nat Cell Biol 2011;13:497–505.15 IedaM, Fu JD, Delgado-Olguin P et al. Di-
rect reprogramming of fibroblasts into func-tional cardiomyocytes by defined factors. Cell2010;142:375–386.16 Pera MF. Stem cells: The dark side of in-
duced pluripotency. Nature 2011;471:46–47.17 Fukuda K, Yuasa S. Stem cells as a source
of regenerative cardiomyocytes. Circ Res 2006;98:1002–1013.18 Nygren JM, Jovinge S, Breitbach M et al.
Bone marrow-derived hematopoietic cells gen-erate cardiomyocytes at a low frequencythrough cell fusion, but not transdifferentia-tion. Nat Med 2004;10:494–501.19 Assmus B, Schachinger V, Teupe C et al.
Transplantation of progenitor cells and regen-eration enhancement in acute myocardial in-farction (TOPCARE-AMI). Circulation 2002;106:3009–3017.20 Strauer BE, BrehmM, Zeus T et al. Repair
of infarcted myocardium by autologous intra-coronary mononuclear bonemarrow cell trans-plantation in humans. Circulation 2002;106:1913–1918.21 Martin-Rendon E, Sweeney D, Lu F et al.
5-Azacytidine-treated human mesenchymalstem/progenitor cells derived from umbilicalcord, cord blood and bone marrow do not gen-erate cardiomyocytes in vitro at high frequen-cies. Vox Sang 2008;95:137–148.22 Bearzi C, Rota M, Hosoda T et al. Human
cardiac stem cells. Proc Natl Acad Sci USA 2007;104:14068–14073.23 Bolli R, ChughAR,D’AmarioDetal. Cardiac
stemcells in patientswith ischaemic cardiomyop-athy (SCIPIO): Initial results of a randomisedphase 1 trial. Lancet 2011;378:1847–1857.24 MakkarRR, SmithRR, ChengKet al. Intra-
coronary cardiosphere-derived cells for heartregeneration after myocardial infarction (CA-DUCEUS): A prospective, randomised phase 1trial. Lancet 2012;379:895–904.25 Rajnoch C, Chachques JC, Berrebi A
et al. Cellular therapy reverses myocardialdysfunction. J Thorac Cardiovasc Surg 2001;121:871–878.
26 Choi J, Costa ML, Mermelstein CS et al.MyoD converts primary dermal fibroblasts,chondroblasts, smooth muscle, and retinalpigmented epithelial cells into striated mono-nucleated myoblasts and multinucleatedmyotubes. Proc Natl Acad Sci USA 1990;87:7988–7992.27 Qian L, Huang Y, Spencer CI et al. In vivo
reprogramming of murine cardiac fibroblastsinto induced cardiomyocytes. Nature 2012;485:593–598.28 Laiosa CV, Stadtfeld M, Xie H et al.
Reprogramming of committed T cell progeni-tors to macrophages and dendritic cells byC/EBP alpha and PU.1 transcription factors. Im-munity 2006;25:731–744.29 Szabo E, Rampalli S, Risue~no RMet al. Di-
rect conversion of human fibroblasts to multili-neage blood progenitors. Nature 2010;468:521–526.30 Antman EM, Anbe DT, Armstrong PW
et al. ACC/AHA guidelines for the managementof patients with ST-elevationmyocardial infarc-tion—executive summary: A report of theAmerican College of Cardiology/AmericanHeart Association Task Force on Practice Guide-lines (Writing Committee to Revise the 1999Guidelines for the Management of Patientswith Acute Myocardial Infarction). Circulation2004;110:588–636.31 �Usas A, Maciulaitis J, Maciulaitis R et al.
Skeletalmuscle-derived stemcells: Implicationsfor cell-mediated therapies. Medicina 2011;47:469–479.32 Schiaffino S, Gorza L, Sartore S et al.
Three myosin heavy chain isoforms in type 2skeletal muscle fibres. J Muscle Res Cell Motil1989;10:197–205.33 Pette D, Staron RS. Cellular and molecu-
lar diversities of mammalian skeletal musclefibers. Rev Physiol Biochem Pharmacol 1990;116:1–76.34 Bortolotto SK, Cellini M, Stephenson DG
et al. MHC isoform composition and Ca(2+)- orSr(2+)-activation properties of rat skeletal mus-cle fibers. Am J Physiol Cell Physiol 2000;279:C1564–C1577.35 Du A, Sanger JM, Sanger JW. Cardiac
myofibrillogenesis inside intact embryonichearts. Dev Biol 2008;318:236–246.
10 Muscle Stem Cells for Heart Repair
©AlphaMed Press 2014 STEM CELLS TRANSLATIONAL MEDICINE
36 Clause KC, Tchao J, Powell MC et al. Devel-oping cardiac and skeletal muscle share fast-skeletal myosin heavy chain and cardiactroponin-I expression. PLoS One 2012;7:e40725.37 Apple FS. Tissue specificity of cardiac tro-
ponin I, cardiac troponin T and creatine kinase-MB. Clin Chim Acta 1999;284:151–159.38 Sehnert AJ, Huq A, Weinstein BM et al.
Cardiac troponin T is essential in sarcomere as-sembly and cardiac contractility. Nat Genet2002;31:106–110.39 Saggin L, Gorza L, Ausoni S et al. Troponin
I switching in the developing heart. J Biol Chem1989;264:16299–16302.40 Cognard C, Rivet-Bastide M, Constantin B
et al. Progressive predominance of ‘skeletal’ ver-sus ‘cardiac’ types of excitation-contraction cou-plingduring invitro skeletalmyogenesis. PflugersArch 1992;422:207–209.41 Haufe V, Camacho JA, Dumaine R et al.
Expression pattern of neuronal and skeletalmuscle voltage-gated Na+ channels in the de-veloping mouse heart. J Physiol 2005;564:683–696.42 Zhu C, Hu DL, Liu YQ et al. Fabp3 inhibits
proliferation andpromotes apoptosis of embry-onic myocardial cells. Cell Biochem Biophys2011;60:259–266.43 Milman Krentsis I, Sela I, Eiges R et al.
GNE is involved in the early development ofskeletal and cardiac muscle. PLoS One 2011;6:e21389.44 Muntoni F. Cardiomyopathy in muscular
dystrophies. Curr Opin Neurol 2003;16:577–583.45 Barresi R, Di Blasi C, Negri T et al. Disrup-
tion of heart sarcoglycan complex and severecardiomyopathy caused by beta sarcoglycanmutations. J Med Genet 2000;37:102–107.46 DurbeejM, Cohn RD, Hrstka RF et al. Dis-
ruption of the beta-sarcoglycan gene revealspathogenetic complexity of limb-girdle muscu-lar dystrophy type2E.Mol Cell 2000;5:141–151.47 Hunt SA, Abraham WT, Chin MH et al.
2009 focused update incorporated into theACC/AHA 2005 Guidelines for the Diagnosisand Management of Heart Failure in Adults: Areport of the American College of CardiologyFoundation/American Heart Association TaskForce on Practice Guidelines: Developed in col-laboration with the International Society forHeart and Lung Transplantation. Circulation2009;119:e391–e479.48 Menasche P, Alfieri O, Janssens S et al. The
MyoblastAutologousGrafting in IschemicCardio-myopathy (MAGIC) trial: First randomizedplacebo-controlled study of myoblast transplan-tation. Circulation 2008;117:1189–1200.49 Menasche P, Hagege AA, Scorsin M et al.
Myoblast transplantation for heart failure. Lan-cet 2001;357:279–280.50 Tamaki T, AkatsukaA,Okada Y et al. Cardi-
omyocyte formation by skeletal muscle-derivedmulti-myogenic stem cells after transplantationinto infarcted myocardium. PLoS One 2008;3:e1789.51 Kessler PD, Byrne BJ. Myoblast cell graft-
ing into heart muscle: Cellular biology and po-tential applications. Annu Rev Physiol 1999;61:219–242.52 Hansson EM, Lindsay ME, Chien KR. Re-
generation next: Toward heart stem cell thera-peutics. Cell Stem Cell 2009;5:364–377.53 Segers VF, Lee RT. Stem-cell therapy for
cardiac disease. Nature 2008;451:937–942.
54 OshimaH, PayneTR,Urish KL et al. Differ-ential myocardial infarct repair with musclestem cells compared to myoblasts. Mol Ther2005;12:1130–1141.55 Johnston PV, Sasano T, Mills K et al. En-
graftment, differentiation, and functional ben-efits of autologous cardiosphere-derived cellsin porcine ischemic cardiomyopathy. Circula-tion 2009;120:1075–1083.56 Lavine L, Upcott H.Myocardial ischaemia
treated by graft of skeletal muscle to the heart.Proc R Soc Med 1937;30:772.57 AbrahamMR, Henrikson CA, Tung L et al.
Antiarrhythmic engineering of skeletal myo-blasts for cardiac transplantation. Circ Res2005;97:159–167.58 Marban E, Cingolani E. Heart to heart:
Cardiospheres for myocardial regeneration.Heart Rhythm 2012;9:1727–1731.59 Hagege AA,Marolleau JP, Vilquin JT et al.
Skeletal myoblast transplantation in ischemicheart failure: Long-term follow-up of the firstphase I cohort of patients. Circulation 2006;114:I108–I113.60 Gavira JJ, Perez-Ilzarbe M, Abizanda G
et al. A comparison between percutaneousand surgical transplantation of autologous skel-etalmyoblasts in a swinemodel of chronicmyo-cardial infarction. Cardiovasc Res 2006;71:744–753.61 Gavira JJ, Herreros J, Perez A et al. Autol-
ogous skeletal myoblast transplantation inpatients with nonacute myocardial infarction:1-year follow-up. J Thorac Cardiovasc Surg2006;131:799–804.62 Menasche P, Hagege AA, Vilquin JT et al.
Autologous skeletal myoblast transplantationfor severe postinfarction left ventricular dys-function. J Am Coll Cardiol 2003;41:1078–1083.63 Duckers HJ, Houtgraaf J, Hehrlein C et al.
Final results of a phase IIa, randomised, open-label trial toevaluatethepercutaneous intramyo-cardial transplantation of autologous skeletalmyoblasts in congestive heart failure patients:The SEISMIC trial. EuroIntervention 2011;6:805–812.64 Sato K, Li Y, FosterW et al. Improvement
of muscle healing through enhancement ofmuscle regeneration and prevention of fibrosis.Muscle Nerve 2003;28:365–372.65 Peng H, Huard J. Muscle-derived stem
cells for musculoskeletal tissue regenerationand repair. Transpl Immunol 2004;12:311–319.66 Jankowski RJ, Deasy BM, Cao B et al. The
role of CD34 expression and cellular fusion inthe regeneration capacity of myogenic progen-itor cells. J Cell Sci 2002;115:4361–4374.67 Peng H, Usas A, Gearhart B et al. Con-
verse relationship between in vitro osteogenicdifferentiation and in vivo bone healing elicitedby different populations ofmuscle-derived cellsgenetically engineered to express BMP4. J BoneMiner Res 2004;19:630–641.68 Clause KC, Tinney JP, Liu LJ et al. A three-
dimensional gel bioreactor for assessment ofcardiomyocyte induction in skeletal muscle-derived stem cells. Tissue Eng Part C Methods2010;16:375–385.69 Winitsky SO, Gopal TV, Hassanzadeh S
et al. Adult murine skeletal muscle containscells that can differentiate into beating cardio-myocytes in vitro. PLoS Biol 2005;3:e87.70 Arsic N, Mamaeva D, Lamb NJ et al.
Muscle-derived stem cells isolated as non-
adherent population give rise to cardiac, skele-tal muscle and neural lineages. Exp Cell Res2008;314:1266–1280.71 Tamaki T,UchiyamaY,OkadaYetal. Clonal
differentiation of skeletal muscle-derived CD34(-)/45(-) stem cells into cardiomyocytes in vivo.Stem Cells Dev 2010;19:503–512.72 Parker MH, Loretz C, Tyler AE et al. Acti-
vation of Notch signaling during ex vivo expan-sion maintains donor muscle cell engraftment.STEM CELLS 2012;30:2212–2220.73 Gharaibeh B, Lu A, Tebbets J et al. Isola-
tion of a slowly adhering cell fraction containingstem cells from murine skeletal muscle by thepreplate technique. Nat Protoc 2008;3:1501–1509.74 Okada M, Payne TR, Drowley L et al. Hu-
man skeletal muscle cells with a slow adhesionrate after isolation and an enhanced stress re-sistance improve function of ischemic hearts.Mol Ther 2012;20:138–145.75 Okada M, Payne TR, Zheng B et al. Myo-
genic endothelial cells purified from humanskeletal muscle improve cardiac function aftertransplantation into infarcted myocardium. JAm Coll Cardiol 2008;52:1869–1880.76 Zheng B, Cao B, Crisan M et al. Prospec-
tive identification of myogenic endothelial cellsin human skeletalmuscle. Nat Biotechnol 2007;25:1025–1034.77 Crisan M, Yap S, Casteilla L et al. A peri-
vascular origin for mesenchymal stem cells inmultiple human organs. Cell Stem Cell 2008;3:301–313.78 Jacot JG,Kita-MatsuoH,WeiKAetal. Car-
diac myocyte force development during differ-entiation and maturation. Ann N Y Acad Sci2010;1188:121–127.79 Perez-Ilzarbe M, Agbulut O, Pelacho B
et al. Characterization of the paracrine effectsof human skeletalmyoblasts transplanted in in-farcted myocardium. Eur J Heart Fail 2008;10:1065–1072.80 BaraniakPR,McDevitt TC. Stemcell para-
crine actions and tissue regeneration. RegenMed 2010;5:121–143.81 Usas A, Huard J. Muscle-derived stem
cells for tissue engineering and regenerativetherapy. Biomaterials 2007;28:5401–5406.82 Okada M, Payne TR, Drowley L et al. Hu-
man skeletal muscle cells with a slow adhesionrate after isolation and an enhanced stress re-sistance improve function of ischemic hearts.Mol Ther 2012;20:138–145.83 Gharaibeh B, Lavasani M, Cummins JH
et al. Terminal differentiation is not a major de-terminant for the success of stem cell therapy:Cross-talk between muscle-derived stem cellsand host cells. Stem Cell Res Ther 2011;2:31.84 Wollert KC, Drexler H. Clinical applica-
tions of stem cells for the heart. Circ Res2005;96:151–163.85 Rane AA, Christman KL. Biomaterials for
the treatmentofmyocardial infarction:A5-yearupdate. J Am Coll Cardiol 2011;58:2615–2629.86 ChristmanKL, LeeRJ. Biomaterials for the
treatment of myocardial infarction. J Am CollCardiol 2006;48:907–913.87 Shudo Y, Miyagawa S, Nakatani S et al.
Myocardial layer-specific effect of myoblastcell-sheet implantation evaluated by tissuestrain imaging. Circ J 2013;77:1063–1072.88 Saito S, Miyagawa S, Sakaguchi T et al.
Myoblast sheet can prevent the impairment
Hassan, Tchao, Tobita 11
www.StemCellsTM.com ©AlphaMed Press 2014
of cardiac diastolic function and late remodel-ing after left ventricular restoration in ische-mic cardiomyopathy. Transplantation 2012;93:1108–1115.89 MasumotoH,Matsuo T, Yamamizu K et al.
Pluripotent stem cell-engineered cell sheets reas-sembledwith defined cardiovascular populationsameliorate reduction in infarct heart functionthrough cardiomyocyte-mediated neovasculari-zation. STEM CELLS 2012;30:1196–1205.90 Sekiya N, Tobita K, Beckman S et al.
Muscle-derived stem cell sheets support pumpfunction and prevent cardiac arrhythmias ina model of chronic myocardial infarction. MolTher 2013;21:662–669.91 Zimmermann WH, Melnychenko I,
Wasmeier G et al. Engineeredheart tissuegraftsimprove systolic and diastolic function in in-farcted rat hearts. Nat Med 2006;12:452–458.92 Fujimoto KL, Clause KC, Liu LJ et al. Engi-
neered fetal cardiac graft preserves its cardio-myocyte proliferation within postinfarctedmyocardium and sustains cardiac function. Tis-sue Eng Part A 2011;17:585–596.93 Mohsin S, Siddiqi S, Collins B et al.
Empowering adult stem cells for myocardial re-generation. Circ Res 2011;109:1415–1428.94 Payne TR, Oshima H, Sakai T et al. Regen-
eration of dystrophin-expressing myocytes inthe mdx heart by skeletal muscle stem cells.Gene Ther 2005;12:1264–1274.95 Memon IA, Sawa Y, Fukushima N et al.
Repair of impairedmyocardiumbymeansof im-plantation of engineered autologous myoblastsheets. J Thorac Cardiovasc Surg 2005;130:1333–1341.96 Kondoh H, Sawa Y, Miyagawa S et al.
Longer preservation of cardiac performanceby sheet-shapedmyoblast implantation indilated
cardiomyopathic hamsters. Cardiovasc Res 2006;69:466–475.97 Vunjak-Novakovic G, Tandon N, Godier A
et al. Challenges in cardiac tissue engineering.Tissue Eng Part B Rev 2010;16:169–187.98 RoellW, Lewalter T, SassePet al. Engraft-
ment of connexin 43-expressing cells preventspost-infarct arrhythmia. Nature 2007;450:819–824.99 Oh H, Bradfute SB, Gallardo TD et al. Car-
diac progenitor cells from adult myocardium:Homing, differentiation, and fusion after infarc-tion. Proc Natl Acad Sci USA 2003;100:12313–12318.100 Miyamoto S, Kawaguchi N, Ellison GM
et al. Characterization of long-term cultured c-kit+ cardiac stem cells derived from adult rathearts. Stem Cells Dev 2010;19:105–116.101 KamrulHasanM,KomoikeY, Tsunesumi
S et al. Myogenic differentiation in atrium-derived adult cardiac pluripotent cells and thetranscriptional regulationofGATA4andmyoge-nin on ANP promoter. Genes Cells 2010;15:439–454.102 McCarthy JJ. MicroRNA-206: The skele-
tal muscle-specific myomiR. Biochim BiophysActa 2008;1779:682–691.103 Yuasa K, Hagiwara Y, Ando M et al.
MicroRNA-206 is highly expressed in newlyformed muscle fibers: Implications regardingpotential for muscle regeneration and matura-tion in muscular dystrophy. Cell Struct Funct2008;33:163–169.104 Williams AH, Valdez G, Moresi V et al.
MicroRNA-206 delays ALS progression and pro-motes regenerationof neuromuscular synapsesin mice. Science 2009;326:1549–1554.105 Crippa S, Cassano M, Messina G et al.
miR669a and miR669q prevent skeletal muscle
differentiation in postnatal cardiac progenitors.J Cell Biol 2011;193:1197–1212.106 Clause KC, Barker TH. Extracellular ma-
trix signaling in morphogenesis and repair. CurrOpin Biotechnol 2013;24:830–833.107 Duan Y, Liu Z, O’Neill J et al. Hybrid gel
composed of native heart matrix and collageninduces cardiac differentiation of human em-bryonic stem cells without supplementalgrowth factors. J Cardiovasc Transl Res 2011;4:605–615.108 Dıez Villanueva P, Sanz-Ruiz R, Nu~nez
Garcia A et al. Functional multipotency of stemcells:What dowe need from them in the heart?Stem Cells Int 2012;2012:817364.109 Siminiak T, Kalawski R, Fiszer D et al.
Autologous skeletal myoblast transplanta-tion for the treatment of postinfarction myo-cardial injury: Phase I clinical study with 12months of follow-up. Am Heart J 2004;148:531–537.110 Invernici G, Cristini S, Madeddu P et al.
Human adult skeletal muscle stem cells differ-entiate into cardiomyocyte phenotype in vitro.Exp Cell Res 2008;314:366–376.111 Neef K, Choi YH, Perumal Srinivasan S
et al. Mechanical preconditioning enables elec-trophysiologic coupling of skeletal myoblastcells to myocardium. J Thorac Cardiovasc Surg2012;144:1176–1184.112 Perumal Srinivasan S, Neef K, Treskes P
et al. Enhanced gap junction expression inmyoblast-containing engineered tissue. Bio-chemBiophysResCommun2012;422:462–468.113 Xiang G, Yang Q, Wang B et al.
Lentivirus-mediated Wnt11 gene transferenhances cardiomyogenic differentiation ofskeletal muscle-derived stem cells. Mol Ther2011;19:790–796.
12 Muscle Stem Cells for Heart Repair
©AlphaMed Press 2014 STEM CELLS TRANSLATIONAL MEDICINE
























![A Concise History of Ancient Kurdistan [in Kurdish]](https://static.fdokumen.com/doc/165x107/63335467b6829c19b80c5cc1/a-concise-history-of-ancient-kurdistan-in-kurdish.jpg)