its bio-topo-logic properties, its 5 Dimotions & s=T symmetri
CES2, ABCG2, TS and Topo-I Primary and Synchronous Metastasis Expression and Clinical Outcome in...
-
Upload
independent -
Category
Documents
-
view
1 -
download
0
Transcript of CES2, ABCG2, TS and Topo-I Primary and Synchronous Metastasis Expression and Clinical Outcome in...
PRELIMINARYCOMMUNICATION
Association of Computed TomographyMorphologic Criteria With Pathologic ResponseandSurvival inPatientsTreatedWithBevacizumabfor Colorectal Liver MetastasesYun Shin Chun, MDJean-Nicolas Vauthey, MDPiyaporn Boonsirikamchai, MDDipen M. Maru, MDScott Kopetz, MDMartin Palavecino, MDSteven A. Curley, MDEddie K. Abdalla, MDHarmeet Kaur, MDChusilp Charnsangavej, MDEvelyne M. Loyer, MD
THE ADDITION OF BEVACIZUMAB,a monoclonal antibody againstvascular endothelial growthfactor, to cytotoxic chemo-
therapy is associated with improvedsurvival in patients with stage IV colo-rectal cancer and higher pathologicresponse rates in patients undergoing re-section of colorectal liver metastases.1,2
Response to bevacizumab, which ex-erts an antiangiogenic mechanism of ac-tion, may be inadequately assessed bytraditional size-based radiologic crite-ria, the Response Evaluation Criteria inSolid Tumors (RECIST), which were de-signed for assessing tumor volume re-duction following cytotoxic chemo-therapy.3-5 In support of this, a recentphase 3 trial showed that the additionof bevacizumab to oxaliplatin-based che-motherapy for metastatic colorectal can-cer improved progression-free survivalwithout affecting RECIST-defined re-sponse rates.6
Recently, pathologic response to pre-operative chemotherapy has beenshown to correlate with improved sur-
Author Affiliations are listed at the end of thisarticle.Corresponding Authors: Jean-Nicolas Vauthey, MD, De-partment of Surgical Oncology, University of TexasM. D. Anderson Cancer Center, 1515 Holcombe Blvd,
Unit 444, Houston, TX 77030 ([email protected]), and Evelyne M. Loyer, MD, Department of Di-agnostic Radiology, University of Texas M. D. Ander-son Cancer Center, 1515 Holcombe Blvd, Unit 368,Houston, TX 77030 ([email protected]).
Context The standard criteria used to evaluate tumor response, the Response Evalu-ation Criteria in Solid Tumors (RECIST), were developed to assess tumor shrinkage af-ter cytotoxic chemotherapy and may be limited in assessing response to biologic agents,which have a cytostatic mechanism of action.
Objective To validate novel tumor response criteria based on morphologic changesobserved on computed tomography (CT) in patients with colorectal liver metastasestreated with bevacizumab-containing chemotherapy regimens.
Design, Setting, and Patients A total of 234 colorectal liver metastases were ana-lyzed from 50 patients who underwent hepatic resection after preoperative chemo-therapy that included bevacizumab at a comprehensive US cancer center from 2004to 2007; date of last follow-up was March 2008. All patients underwent routine contrast-enhanced CT at the start and end of preoperative therapy. Three blinded, indepen-dent radiologists evaluated images for morphologic response, based on metastaseschanging from heterogeneous masses with ill-defined margins into homogeneous hy-poattenuating lesions with sharp borders. These criteria were validated with a sepa-rate cohort of 82 patients with unresectable colorectal liver metastases treated withbevacizumab-containing chemotherapy.
Main Outcome Measures Response determined using morphologic criteria andRECIST was correlated with pathologic response in resected liver specimens and withpatient survival.
Results Interobserver agreement for scoring morphologic changes was good among3 radiologists (�, 0.68-0.78; 95% confidence interval [CI], 0.51-0.93). In resected tu-mor specimens, the median (interquartile range [IQR]) percentages of residual tumorcells for optimal morphologic response was 20% (10%-30%); for incomplete re-sponse, 50% (30%-60%); and no response, 70% (60%-70%; P� .001). With RECIST,the median (IQR) percentages of residual tumor cells were for partial response 30%(10%-60%); for stable disease, 50% (20%-70%); and for progressive disease, 70%(65%-70%; P=.04). Among patients who underwent hepatic resection, median over-all survival was not yet reached with optimal morphologic response and 25 months(95% CI, 20.2-29.8 months) with incomplete or no morphologic response (P=.03).In the validation cohort, patients with optimal morphologic response had median over-all survival of 31 months (95% CI, 26.8-35.2 months) compared with 19 months (95%CI, 14.6-23.4 months) with incomplete or no morphologic response (P=.009). RECISTdid not correlate with survival in either the surgical or validation cohort.
Conclusion Among patients with colorectal liver metastases treated with bevacizumab-containing chemotherapy, CT-based morphologic criteria had a statistically signifi-cant association with pathologic response and overall survival.JAMA. 2009;302(21):2338-2344 www.jama.com
2338 JAMA, December 2, 2009—Vol 302, No. 21 (Reprinted) ©2009 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a BIBLIOSAN remote cilea clas User on 09/28/2014
vival and has been proposed as a newoutcome end point after resection of co-lorectal liver metastases.7-9 To date, anoninvasive method of predictingpathologic response to chemotherapyin colorectal liver metastases, particu-larly biologic agents, is lacking. Weobserved that after bevacizumab-containing therapy, colorectal liver me-tastases tend not only to decrease in sizebut also to undergo unique morpho-logic changes on computed tomogra-phy (CT). Metastases that have hetero-geneous attenuation, variable degree ofenhancement, and ill-defined bordersbefore treatment transform into homo-geneous, hypoattenuating lesions withwell-defined borders.
We hypothesized that these changeson CT reflect the pathologic response inpatients treated with bevacizumab-containing chemotherapy before hepaticresection of colorectal liver metastases.To test this hypothesis, we correlated tu-mor response based on these morpho-logic criteria and tumor response basedonRECISTwithpathologic response.Wethen tested the morphologic criteria inpatientswithunresectable colorectal livermetastases treated with bevacizumab.The morphologic criteria and RECISTwere correlated with survival in pa-tients who underwent resection andthose who did not.
METHODSInitial Patient Cohort
From a prospective hepatobiliary da-tabase at the University of Texas M. D.Anderson Cancer Center, we identi-fied 234 colorectal liver metastases in50 consecutive patients who receivedfirst-line chemotherapy with bevaci-zumab before undergoing hepatic re-section between March 2004 and March2007. All patients underwent contrast-enhanced CT scans of the abdomen atthe start and end of preoperativetherapy as part of their standard evalu-ation. Patients who had undergoneprior liver resection were excluded.
Postoperatively, patients were fol-lowed up with history and physical ex-amination, CT scans, and serum car-cinoembryonic antigen levels at 3- to
6-month intervals for the first 2 to 3years after resection and at more ex-tended intervals thereafter. The me-dian follow-up time was 18 months(range, 3-42 months). Date of last fol-low-up was March 2008. This study in-volved retrospective review of medi-cal information and was conductedunder the approval of the institutionalreview board, which waived the re-quirement for informed consent.
Validation Patient Cohort
From a prospective gastrointestinalmedical oncology database at the Uni-versity of Texas M. D. Anderson Can-cer Center, we identified 82 patientswith unresectable colorectal liver me-tastases treated with bevacizumab com-bined with cytotoxic chemotherapy be-tween March 2004 and April 2007.Patients were considered unresectableif 2 contiguous hepatic segments couldnot be preserved, vascular inflow andoutflow or biliary drainage was inad-equate, or the volume of the future liverremnant was 20% or less of the total es-timated liver volume.10 All patients un-derwent contrast-enhanced CT scans ofthe abdomen before starting chemo-therapy and at 2- to 3-month intervalsthereafter. Median follow-up was 25months (range, 6-57 months). Date oflast follow-up was April 2009.
Imaging Analysis
Computed tomographic scans were per-formed with 4- or 16-slice CT (Light-Speed, GE Healthcare, Piscataway, NewJersey) using a collimation of 5 mm andreconstruction at 2.5 mm. Images wereacquired with 1 of 2 methods: a tripha-sic liver protocol following a noncon-trast evaluation of the liver or a single-phase technique. For the triphasic liver
protocol, images were obtained 30, 50,and 70 seconds after the start of intra-venous injection of ioversol at a rate of5 mL/s. For the single-phase tech-nique, images were obtained 60 to 70seconds after the start of ioversol in-jection at a rate of 2 to 3 mL/s. Be-cause of the routine concomitant ac-quisition of chest CT scans and delayedimages through the kidneys, single-phase scans also permitted partial evalu-ation of the liver during the early anddelayed phases of enhancement.
Response to treatmentwasassessed in-dependently by 3 radiologists with 2, 15,and 20 years of experience in abdomi-nal oncologic imaging. Radiologists wereblinded to pathologic results, patienttreatment, and outcomes. Discrepan-cies between radiologists were resolvedby consensus review. Response wasevaluated using new morphologic crite-ria, assigning each metastasis to 1 of 3groups (TABLE 1). A group-3 metasta-sis was characterized by heterogeneousattenuation and a thick, poorly definedtumor-liver interface (FIGURE 1A and C).A group-1 metastasis was character-ized by homogeneous low attenuationwith a thin, sharply defined tumor-liver interface (Figure 1B). A group-2metastasis had morphology that couldnot be rated as 3 or 1 (Figure 1D).When present, a peripheral rim of hy-perattenuating contrast enhancementwas designated a group-3 characteris-tic, and resolution of this enhance-ment was classified group 1.
Morphologic response criteria weredefined as optimal if the metastasischanged from a group 3 or 2 to a 1, in-complete if the group changed from 3 to2, and none if the group had not changedor increased. In patients with multipletumors, morphologic response criteria
Table 1. Computed Tomographic Morphologic Groups
MorphologyGroup
Computed Tomographic Tumor Characteristics
Overall AttenuationTumor-Liver
Interface Peripheral Rim of Enhancement
3 Heterogeneous Ill defined May be present
2 Mixed Variable If initially present, partially resolved
1 Homogeneous andhypoattenuating
Sharp If initially present, completely resolved
CT MORPHOLOGIC CRITERIA, BEVACIZUMAB, AND SURVIVAL
©2009 American Medical Association. All rights reserved. (Reprinted) JAMA, December 2, 2009—Vol 302, No. 21 2339
Downloaded From: http://jama.jamanetwork.com/ by a BIBLIOSAN remote cilea clas User on 09/28/2014
were assigned based on the response seenin the majority of tumors. Response byRECIST was defined as previously de-scribed: complete response, disappear-ance of all tumors; partial response, morethan a 30% decrease in sum of the long-est diameter of target tumor; progres-sive disease, more than a 20% increasein the sum of the longest diameter of tar-get tumor; and stable disease, none of thecomplete response, partial response, orprogressive disease criteria met.11 The ap-pearance of new metastases was de-fined as progression by RECIST and mor-phology assessment.
Assessment of PathologicResponse to Chemotherapy
Hematoxylin and eosin−stained speci-mens sectioned into 5-mm-thick sliceswere evaluated by a gastrointestinal pa-thologist who was blinded to treatmentregimen, radiologic results, and patient
outcomes. The extent of residual carci-nomawasassessedsemiquantitativelyasapercentagerelativetothetotaltumorsur-facearea,aspreviouslydescribed.2,8Patho-logicresponsewasscoredasminorif50%or more of residual tumor cells werepresent, major with 1% to 49% residualtumor cells, and complete if no residualtumor cells were detected.
Statistical Analysis
Continuous variables were comparedusing the Kruskal-Wallis or Mann-Whitney test; discrete variables, ex-pressed as number and percentage, werecompared using the �2 test or Fisher ex-act test, when appropriate. A post hocpower analysis showed that based on theactual number of patients enrolled in thecurrent study, therewasgreater than95%statistical power to detect a difference ina pathologic response rate of 32% be-tween patients with optimal vs incom-
plete or no morphologic response at aconventional P value of .05. � Statisticswere used to determine interobserveragreement of the proposed morpho-logic criteria among 3 radiologists.
Survival was determined from time ofhepatic resection until the time of deathor last follow-up. If more than 3 monthshad lapsed since the date of last follow-up, then survival was calculated accord-ing to whether patients were alive at thetime the study was closed, as recordedin tumor registry data or medical rec-ords. Five patients with residual diseasein the liver, lung, or an intact primarytumor at the time of hepatectomy wereexcluded from the survival analysis.Among patients with unresectabletumors, survival was calculated from thestart of bevacizumab-containing chemo-therapy. Survival curves were gener-atedusingtheKaplan-Meiermethod,anddifferences were evaluated with the log-rank test. Analyses were performed withSPSS software (version 12.0, SPSS Inc,Chicago, Illinois).All statistical testswere2-sided, and significance was set atP� .05.
RESULTSInitial Surgical Cohort
Two hundred thirty-four lesions in 50patients were evaluated; their demo-graphic and clinicopathologic charac-teristics are presented in TABLE 2. Of the130 CT scans reviewed, 53 were per-formed with triphasic liver protocol and77 with the single-phase technique.Among the 33 patients with multiple tu-mors, the morphologic responses of themetastases within the same patient wereconcordant in all but 2 patients.
Morphologic response was signifi-cantly associated with the percentage ofresidual tumor cells: median (interquar-tile range [IQR]) values were 70% (60%-70%) for patients with no response, 50%(30%-60%) for patients with incom-plete response, and 20% (10%-30%) forpatients with optimal response (P�.001,FIGURE 2A). RECIST was also signifi-cantly associated with the percentageof residual tumor cells: median (IQR)values were 70% (65%-70%) for pa-tients with progressive disease, 50%
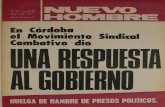
Figure1.Representative Pretreatment and Posttreatment Computed Tomographic Scans Evaluatedby Response Evaluation Criteria in Solid Tumors (RECIST) and Morphologic Criteria
A B
PosttreatmentPretreatment
PosttreatmentPretreatment
RECIST-stable disease and morphologic incomplete response
RECIST-stable disease and morphologic optimal response
C D
Arrowheads indicate the tumor-liver interface. Morphologic optimal response is characterized by decreasedattenuation and sharp tumor-liver interface (B); morphologic incomplete response is characterized by de-creased attenuation but persistent ill-defined tumor-liver interface remaining after treatment (D).
CT MORPHOLOGIC CRITERIA, BEVACIZUMAB, AND SURVIVAL
2340 JAMA, December 2, 2009—Vol 302, No. 21 (Reprinted) ©2009 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a BIBLIOSAN remote cilea clas User on 09/28/2014
(20%-70%) for patients with stable dis-ease, and 30% (10%-60%) for patientswith partial response (P=.04, Figure 2).
Whenpathologic responsewas strati-fied as minor, major, or complete usingpreviously determined cutoff values forthe percentage of residual tumor cells,8
2 patients had a complete response, 27had a major response, and 21 had a mi-nor response. Metastases with majorpathologic response were characterizedby replacement of tumor cells by fibro-sis.Necrosiswasobservedinlessthan5%oftumors.Completeormajorpathologicresponse corresponded to morphologicoptimal response in 22 of 29 patients(76%),whileminorpathologic responsewasassociatedwithmorphologicpartialornoresponsein17of21patients(81%).When correlated with RECIST, com-plete or major pathologic response cor-respondedtoRECISTpartial response in23 of 29 patients (79%), while minorpathologic responsewasassociatedwithRECIST stable or progressive disease in10 of 21 patients (48%). None of the pa-tients had RECIST complete response.Therefore, incompleteornoresponsebymorphology was more specific for pre-dicting minor pathologic response thanRECISTstableorprogressivedisease(17of 21, morphology vs 10 of 21, RECIST,P=.02). Morphologic optimal responseand RECIST partial response had simi-lar sensitivities for predicting completeor major pathologic response (22 of 29,morphologyvs23of29,RECIST,P=.75).
Patients Who Underwent Resection
Thirtypatients (60%)haddisease recur-rence during the study period, and 9(18%)diedofdisease.Fivepatients(10%)with residual disease in the liver, lung,or an intact primary tumor at the time ofhepatectomywereexcludedfromthesur-vival analysis. Patients with optimal re-sponse by morphology were classifiedas responders while the remaining pa-tients were classified as nonresponders.When morphologic criteria were usedin tumor response evaluation, medianoverall survival was not yet reached forresponders and 25 months for nonre-sponders (95%confidence interval [CI],20.2-29.8 months; P=.03, FIGURE 3).
When RECIST were used, median over-all survival was not yet reached in pa-tientswhoachievedpartial responseand
34monthswithstableorprogressivedis-ease (95%CI,20.0-48.0months;P=.25,Figure 3). On univariate analysis of tra-
Table 2. Baseline Characteristics
No. (%) of Patients
InitialSurgical Cohort
(n = 50)
Patients WithUnresectable Tumor
(n = 82)Age, median (range), y 57 (34-84) 57 (26-69)Sex
Female 21 (42) 37 (45)Male 29 (58) 45 (55)
Primary tumorColon 36 (72) 63 (77)Rectum 14 (28) 19 (23)
Sites of metastasesLiver only 48 (95) 45 (55)Liver and extrahepatic 2 (4) 37 (45)
Liver metastasesSolitary 17 (34) 4 (5)Multiple 33 (66) 78 (95)Tumor size, median (range), cma 2.3 (0.4-13) 4.9 (1.5-18.0)
ChemotherapyFOLFIRI with bevacizumab 7 (14) 47 (57)FOLFOX with bevacizumab 43 (86) 35 (43)
HepatectomyMinor 24 (48) NAMajor 26 (52) NARadiofrequency ablation at time of hepatectomy 8 (16) NANo. of chemotherapy cycles before
hepatectomy, median (range)6 (3-12) NA
Interval between last CT and surgery,median (range), d
18 (2-56) NA
Overall survivalbMedian, mo Not reached 253 years, % 51 24
Abbreviations: CT, computed tomography; FOLFIRI, infusional fluorouracil (FU) and leucovorin with irinotecan; FOLFOX,infusional FU and leucovorin with oxaliplatin; NA, not applicable.
aBased on the largest diameter of the resected tumor specimen in surgical patients and largest diameter on prechemo-therapy computed tomography in unresectable patients.
bFrom time of hepatectomy in surgical cohort and from start of bevacizumab-containing chemotherapy in unresectablecohort.
Figure 2. Correlation Between Morphologic Response or Response Evaluation Criteria inSolid Tumors (RECIST) and Percentage of Residual Tumor Cells
80
40
60
20
0 P <.001
None Incomplete Optimal
Response
Res
idua
l Tum
or, %
Morphologic response criteriaA
80
40
60
20
0
ProgressiveDisease
StableDisease
PartialResponse
Response
Res
idua
l Tum
or, %
RECISTB
P = .04
Lines inside boxes represent the median; end points of whiskers represent minimum and maximum values.Lower and upper edges of boxes represent 25th and 75th percentiles. P values were derived from the Kruskal-Wallis test comparing the percentage of residual tumor cells among patients with optimal, incomplete, or nomorphologic response; and RECIST partial response, stable disease, or progressive disease.
CT MORPHOLOGIC CRITERIA, BEVACIZUMAB, AND SURVIVAL
©2009 American Medical Association. All rights reserved. (Reprinted) JAMA, December 2, 2009—Vol 302, No. 21 2341
Downloaded From: http://jama.jamanetwork.com/ by a BIBLIOSAN remote cilea clas User on 09/28/2014
ditional predictors of survival and po-tential radiologicpredictorsofoutcome,onlymorphologiccriteriademonstratedasignificantcorrelationwithoverall sur-vival (TABLE 3).
Validation in PatientsWith Unresected Tumors
To validate the CT response criteria inassessing clinically significant tumor re-sponse of liver metastases, a separate co-hort of 82 patients with unresectable co-lorectal liver metastases treated with
bevacizumab-containing chemo-therapy was analyzed. Their clinico-pathologic features are presented inTable 2. Among the 78 patients withmultiple liver metastases, the morpho-logic responses of the metastases withinthe same patient were concordant in allbut 10 patients; in these patients, themorphology score was assigned based onthe dominant pattern observed.
Among the 82 patients with stage IVcolorectal cancer treated with chemo-therapyonly,thosewithoptimalresponse
bymorphologiccriteriahadsignificantlybetter overall survival than patientswithincompleteornoresponse,withme-dian overall survival of 31 months (95%CI, 26.8-35.2 months) and 19 months(95%CI,14.6-23.4months),respectively(P=.009,Figure3). Incontrast, responsebyRECISTwasnotassociatedwithanim-provementinsurvival.Medianoverallsur-vival was 28 months (95% CI, 22.5-33.5months) inpatientswithpartial responseand 22 months (95% CI, 15.3-28.7months) in those with stable or progres-sivedisease(P=.45,Figure3).Thefollow-ing variables did not significantly affectoverallsurvival:sex,age,sizeormultiplic-ity of hepatic metastases, rectal primarytumor, and the presence of extrahepaticmetastases.
Interobserver Agreementfor Morphologic Criteria
The interobserveragreementbetween the3 radiologists for scoring morphologicchanges was good: �,0.78 (95% CI, 0.63-0.93) between readers 1 and 2; �, 0.72(95% CI, 0.56-0.88) between readers 1and 3; and �, 0.68 (95% CI, 0.51-0.85)between readers 2 and 3. Among the ra-diologists, there were discrepancies inscoring morphologic criteria in 13 of the50 surgical patients, which were re-solved by consensus review.
COMMENTWe present novel qualitative morpho-logic CT criteria for predicting re-sponse to bevacizumab-containing che-motherapy in patients with colorectalliver metastases. These criteria were re-producible, as shown by the good in-terobserver agreement in scoring mor-phologic changes among 3 independentradiologists with varied experience in ab-dominal oncologic imaging. Morpho-logic criteria correlated strongly with thepercentage of residual tumor cells andalso with pathologic response stratifiedas complete, major, or minor using 50%residual tumor cells as the cutoff valuebetween major and minor pathologic re-sponse. Optimal morphologic responseto preoperative therapy translated intoa survival benefit after hepatic resec-tion. In a separate validation cohort of
Figure 3. Overall Survival in Responders and Nonresponders by Morphologic Criteria andResponse Evaluation Criteria in Solid Tumors (RECIST) in the Initial Surgical Cohort and inPatients With Unresectable Tumor (Validation Cohort)
1.0
0.8
0.6
0.4
Log-rank P = .03 Log-rank P = .25
0.2
0.0
No. at riskResponderNonresponder
0 10 20 30 40 50
20 12 4 218 9 3 0
2223
Months
Pro
port
ion
Sur
vivi
ng
1.0
0.8
0.6
0.4
0.2
0.00 10 20 30 40 50
26 14 3 212 7 4 0
3114
Months
Pro
port
ion
Sur
vivi
ng
Optimal responseIncomplete or no response
Partial responseStable disease or progressive disease
1.0
0.8
0.6
0.4
Log-rank P = .009 Log-rank P = .45
0.2
0.0
No. at riskResponderNonresponder
0 10 20 30 5040 60
3049
2625
1614
21
64
3052
Months
Pro
port
ion
Sur
vivi
ng
1.0
0.8
0.6
0.4
0.2
0.00 10 20 30 5040
34 25 14 0345 26 16 37
60
3547
Months
Pro
port
ion
Sur
vivi
ng
Morphologic response criteria
Patients with unresectable tumor
RECIST
Morphologic response criteria
Surgical cohort
RECIST
Survival was evaluated in 45 surgical patients who underwent complete resection.
CT MORPHOLOGIC CRITERIA, BEVACIZUMAB, AND SURVIVAL
2342 JAMA, December 2, 2009—Vol 302, No. 21 (Reprinted) ©2009 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a BIBLIOSAN remote cilea clas User on 09/28/2014
patientswithunresectable colorectal livermetastases, response by morphologic cri-teria was also associated with improvedoverall survival. RECIST was also sen-sitive for predicting complete or majorpathologic response but with a signifi-cantly lower specificity for predicting mi-nor pathologic response. RECIST wasassociated with neither the stratifiedpathologic response nor survival.
Optimalmorphologicresponsewasde-fined as a change in metastases from le-sionswithheterogeneousattenuationandthick,irregularbordersintobland,homo-geneouslyhypodensemasseswithasharpinterfacebetweenthetumorandadjacentnormal liverparenchyma,whichinsomecases could mimic a cyst. This homoge-neousattenuationofmetastasesrespond-ingtotreatmentlikelyreflectsthereplace-mentof treatedtumorbyfibroconnectivetissue rather than tumornecrosis,whichwaspresent in less than5%ofpatients inthis study. Rubbia-Brandt et al7 also ob-served that histological tumor responseis characterized by fibrous replacementoftumorratherthantumornecrosisinco-lorectal livermetastases. Inpatientswithmultiplelivermetastases,themorphologicresponses of the metastases within thesame patient were uniform in 99 of 111patients(89%).Thisresultconfirmsapre-viousstudydemonstratingthatinpatientswithmultiplecolorectal livermetastases,the histological tumor responses withinthe same patient were similar.7
The effect of pathologic response topreoperative therapy on survival inpatients with solid tumors is well-established.12,13 In patients with colorec-tal liver metastases, histological tumorregression, graded by the extent of fibro-sis and presence of residual tumor cells,has been shown to correlate with sur-vival.7 In this study, we scored patho-logic response semiquantitatively as thepercentage of residual tumor cells rela-tive tothetotal tumorsurfacearea.Patho-logicresponsewasscoredasminor if50%or more of residual tumor cells were pre-sent, major with 1% to 49% residualtumorcells,andcompletewith0%.Usingthis 50% cutoff to define major vs minorpathologic response,werecently showedthat in patients with colorectal liver
metastases,majorpathologic response topreoperative chemotherapy indepen-dently predicted improved patient sur-vival.8 In the present study, overall sur-vival was correlated with morphologicresponse but not RECIST-based prog-nostic factors, such as tumor size andnumber. Although the sample size in thesurgical cohort is small, these resultshighlight the importance of responserather than baseline clinical factors indetermining patient outcome after liverresection.8,14
The limitations of this study includeits retrospective nature and potentiallythepredominantuseof a single-phaseCTtechnique. Although triphasic liver pro-tocol CT is not required to apply the mor-phologic criteria and is probably not
needed routinely in nonsurgical pa-tients with colorectal liver metastases, itmight improve sensitivity by allowingevaluation of early and delayed phasesof tumor enhancement. Recent studieson evaluating response to antiangio-genic agents with CT or magnetic reso-nance imaging have focused on tumorperfusion.15-18 Although tumoral en-hancement was a component of our mor-phology response criteria, the degree ofenhancement could not be consistentlyassessed because of variations in scan-ning techniques. While colorectal livermetastases are considered hypovascu-lar tumors, enhancement does occur andis characterized by an ill-defined rim ofperipheral enhancement that is maxi-mal during the arterial phase and fades
Table 3. Univariate Analysis of Predictors of Overall Survival Among 45 Surgical Patients
VariableNo. of
PatientsActuarial 2-YearSurvival Rate, % P Value
SexMale 26 79
.71Female 19 74
Age, y�60 17 71
.83�60 28 89
Primary siteColon 33 78
.24Rectum 12 76
Primary tumorNode negative 16 83
.90Node positive 29 74
Prehepatectomy serum CEA, ng/mL�200 45 77
NA�200 0
Resection marginNegative 43 79
.11Positive 2 50
Disease-free interval, mo�12 15 69
.55�12 30 81
No. of tumors1 16 75
.79�1 29 78
Tumor size, cma
�5 40 79.11
�5 5 50
Morphologic responseOptimal 22 90
.03Incomplete or none 23 42
RECISTPartial response 31 80
.25Stable or progressive disease 14 64
Abbreviations: CEA, carcinoembryonic antigen; NA, not applicable; RECIST, Response Evaluation Criteria in Solid Tumors.aBased on the largest diameter of the resected tumor specimen.
CT MORPHOLOGIC CRITERIA, BEVACIZUMAB, AND SURVIVAL
©2009 American Medical Association. All rights reserved. (Reprinted) JAMA, December 2, 2009—Vol 302, No. 21 2343
Downloaded From: http://jama.jamanetwork.com/ by a BIBLIOSAN remote cilea clas User on 09/28/2014
away during the portal phase.19,20 We re-viewed many CTs that were single-phase studies, lacking an arterial phase.Nevertheless, in cases for which an earlyhyperattenuating rim of enhancementwas present before treatment, it disap-peared in all patients with an optimalmorphologic response. In addition, theapplicability of these criteria in assess-ing response to other biologic agents ap-proved for colorectal liver metastases re-quires investigation.
In conclusion, we present novel quali-tative radiologic criteria that predict thepathologic response to preoperativebevacizumab-containing chemo-therapy in patients undergoing resec-tion of colorectal liver metastases. Mor-phologic response correlated withpathologic response stratified as com-
plete, major, or minor, as well as over-all survival, whereas RECIST did not.This correlation between survival andmorphologic response, but not RECIST,was confirmed in a nonsurgical cohort.Thus, our results indicate that morpho-logic response may be a useful, nonin-vasive surrogate marker of pathologic re-sponse and improved survival in patientswith colorectal liver metastases receiv-ing a bevacizumab-containing regi-men. It provides complementary infor-mation to traditional size-based criteriain assessing CT response to bevaci-zumab in colorectal liver metastases
Author Affiliations: Departments of Surgical Oncology(Drs Chun, Vauthey, Palavecino, Curley, and Abdalla),DiagnosticRadiology(DrsBoonsirikamchai,Kaur,Charn-sangavej, and Loyer), Pathology (Dr Maru), and Gas-trointestinal Medical Oncology (Dr Kopetz), Universityof Texas M. D. Anderson Cancer Center, Houston.
Author Contributions: Dr Vauthey had full access toall of the data in the study and takes responsibility forthe integrity of the data and the accuracy of the dataanalysis. Drs Vauthey and Loyer contributed equallyas senior authors of this article.Study concept and design: Vauthey, Loyer.Acquisition of data: Boonsirikamchai, Maru, Kopetz,Palavecino, Kaur, Loyer.Analysis and interpretation of data: Chun, Vauthey,Kopetz, Curley, Abdalla, Charnsangavej, Loyer.Drafting of the manuscript: Chun, Vauthey, Kopetz,Loyer.Critical revision of the manuscript for important in-tellectual content: Vauthey, Boonsirikamchai, Maru,Palavecino, Curley, Abdalla, Kaur, Charnsangavej,Loyer.Statistical analysis: Chun, Vauthey.Administrative, technical, or material support:Vauthey, Loyer.Study supervision: Vauthey, Loyer.Financial Disclosures: Dr Kopetz reports receivingresearch grants and honoraria from AstraZenecaand honoraria from Genentech, Roche, and Sanofi-Aventis. Dr Abdalla reports receiving honorariafrom Sanofi-Aventis. Dr Vauthey reports receivinggrants and honoraria from Sanofi-Aventis, Genen-tech, and Roche. No other authors reported disclo-sures.
REFERENCES
1. Hurwitz H, Fehrenbacher L, Novotny W, et al. Be-vacizumab plus irinotecan, fluorouracil, and leucovo-rin for metastatic colorectal cancer. N Engl J Med. 2004;350(23):2335-2342.2. Ribero D, Wang H, Donadon M, et al. Bevaci-zumab improves pathologic response and protectsagainst hepatic injury in patients treated with oxalipla-tin-based chemotherapy for colorectal liver metastases.Cancer. 2007;110(12):2761-2767.3. Sathornsumetee S, Cao Y, Marcello JE, et al. Tu-mor angiogenic and hypoxic profiles predict radio-graphic response and survival in malignant astrocy-toma patients treated with bevacizumab and irinotecan.J Clin Oncol. 2008;26(2):271-278.4. Grothey A, Hedrick EE, Mass RD, et al. Response-independent survival benefit in metastatic colorectalcancer: a comparative analysis of N9741 and AVF2107.J Clin Oncol. 2008;26(2):183-189.5. Choi H, Charnsangavej C, Faria SC, et al. Corre-lation of computed tomography and positron emis-sion tomography in patients with metastatic gastro-intestinal stromal tumor treated at a single institutionwith imatinib mesylate: proposal of new computed to-mography response criteria. J Clin Oncol. 2007;25(13):1753-1759.6. Saltz LB, Clarke S, Diaz-Rubio E, et al. Bevaci-zumab in combination with oxaliplatin-based chemo-therapy as first-line therapy in metastatic colorectalcancer: a randomized phase III study. J Clin Oncol.2008;26(12):2013-2019.7. Rubbia-Brandt L, Giostra E, Brezault C, et al. Im-
portance of histological tumor response assessmentin predicting the outcome in patients with colorectalliver metastases treated with neo-adjuvant chemo-therapy followed by liver surgery. Ann Oncol. 2007;18(2):299-304.8. Blazer DG III, Kishi Y, Maru DM, et al. Pathologicresponse to preoperative chemotherapy: a new out-come end point after resection of hepatic colorectalmetastases. J Clin Oncol. 2008;26(33):5344-5351.9. Adam R, Wicherts DA, de Haas RJ, et al. Com-plete pathologic response after preoperative chemo-therapy for colorectal liver metastases: myth or reality?J Clin Oncol. 2008;26(10):1635-1641.10. Charnsangavej C, Clary B, Fong Y, Grothey A,Pawlik TM, Choti MA. Selection of patients for resec-tion of hepatic colorectal metastases: expert consen-sus statement. Ann Surg Oncol. 2006;13(10):1261-1268.11. Therasse P, Arbuck SG, Eisenhauer EA, et al; Eu-ropean Organization for Research and Treatmentof Cancer, National Cancer Institute of the UnitedStates, National Cancer Institute of Canada. Newguidelines to evaluate the response to treatment insolid tumors. J Natl Cancer Inst. 2000;92(3):205-216.12. Swisher SG, Hofstetter W, Wu TT, et al. Pro-posed revision of the esophageal cancer staging sys-tem to accommodate pathologic response (pP) fol-lowing preoperative chemoradiation (CRT). Ann Surg.2005;241(5):810-817.13. Ajani JA, Mansfield PF, Crane CH, et al. Paclitaxel-
based chemoradiotherapy in localized gastric carci-noma: degree of pathologic response and not clinicalparameters dictated patient outcome. J Clin Oncol.2005;23(6):1237-1244.14. Adam R, Pascal G, Castaing D, et al. Tumor pro-gression while on chemotherapy: a contraindicationto liver resection for multiple colorectal metastases?Ann Surg. 2004;240(6):1052-1061.15. Provenzale JM. Imaging of angiogenesis: clinicaltechniques and novel imaging methods. AJR Am JRoentgenol. 2007;188(1):11-23.16. Sabir A, Schor-Bardach R, Wilcox CJ, et al. Per-fusion MDCT enables early detection of therapeuticresponse to antiangiogenic therapy. AJR Am JRoentgenol. 2008;191(1):133-139.17. Kan Z, Phongkitkarun S, Kobayashi S, et al. Func-tional CT for quantifying tumor perfusion in antian-giogenic therapy in a rat model. Radiology. 2005;237(1):151-158.18. Miles KA, Leggett DA, Kelley BB, Hayball MP,Sinnatamby R, Bunce I. In vivo assessment of neo-vascularization of liver metastases using perfusion CT.Br J Radiol. 1998;71(843):276-281.19. Outwater E, Tomaszewski JE, Daly JM, KresselHY. Hepatic colorectal metastases: correlation of MRimaging and pathologic appearance. Radiology. 1991;180(2):327-332.20. Muramatsu Y, Takayasu K, Moriyama N, et al. Pe-ripheral low-density area of hepatic tumors: CT-pathologic correlation. Radiology. 1986;160(1):49-52.
CT MORPHOLOGIC CRITERIA, BEVACIZUMAB, AND SURVIVAL
2344 JAMA, December 2, 2009—Vol 302, No. 21 (Reprinted) ©2009 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a BIBLIOSAN remote cilea clas User on 09/28/2014