A simplified model for mitral valve dynamics
-
Upload
independent -
Category
Documents
-
view
3 -
download
0
Transcript of A simplified model for mitral valve dynamics
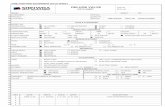
c o m p u t e r m e t h o d s a n d p r o g r a m s i n b i o m e d i c i n e 1 0 9 ( 2 0 1 3 ) 190–196
j o ur nal homep age : w ww.int l .e lsev ierhea l th .com/ journa ls /cmpb
A simplified model for mitral valve dynamics
K.T. Moorheada, S. Paemea,∗, J.G. Chaseb, P. Kolha, L. Pierarda, C.E. Hannc, P.C. Daubya,T. Desaivea
a Cardiovascular Research Center, University of Liège, 17 Allée du 6 Août, Liège 4000, Belgiumb Department of Mechanical Engineering, University of Canterbury, Private Bag 4800, Christchurch 8140, New Zealandc Department of Electrical and Electronic Engineering, University of Canterbury, Private Bag 4800, Christchurch 8140, New Zealand
a r t i c l e i n f o
Article history:
Received 3 May 2011
Received in revised form
27 October 2011
Accepted 27 October 2011
Keywords:
Cardiac cycle
Mitral valve
Non-linear rotational spring
Damping
Hysteresis
a b s t r a c t
Located between the left atrium and the left ventricle, the mitral valve controls flow between
these two cardiac chambers. Mitral valve dysfunction is a major cause of cardiac dysfunction
and its dynamics are little known.
A simple non-linear rotational spring model is developed and implemented to capture the
dynamics of the mitral valve. A measured pressure difference curve was used as the input
into the model, which represents an applied torque to the anatomical valve chords. A range
of mechanical model hysteresis states were investigated to find a model that best matches
reported animal data of chord movement during a heartbeat. The study is limited by the use
of one dataset found in the literature due to the highly invasive nature of getting this data.
However, results clearly highlight fundamental physiological issues, such as the damping
and chord stiffness changing within one cardiac cycle, that would be directly represented
in any mitral valve model and affect behaviour in dysfunction. Very good correlation was
achieved between modeled and experimental valve angle with 1–10% absolute error in the
best case, indicating good promise for future simulation of cardiac valvular dysfunction,
such as mitral regurgitation or stenosis. In particular, the model provides a pathway to
capturing these dysfunctions in terms of modeled stiffness or elastance that can be directly
related to anatomical, structural defects and dysfunction.
about 70–80% of the blood flow occurs during the early filling
1. Introduction
Valvular dysfunction is a relatively common and costly heartdisease, typically requiring mechanical valve replacement.It has two primary forms, stenosis and regurgitation. Mitralstenosis is the abnormal narrowing of the mitral valve, whichslows blood flow and is the only heart disease that is causedpredominately by rheumatic fever. Mitral stenosis accounts
for 10% of single native valve diseases [1]. Mitral regurgitationis more common in the elderly and is the leaking of bloodthrough the mitral valve from the left ventricle into the left∗ Corresponding author. Tel.: +32 4 3663356.E-mail address: [email protected] (S. Paeme).
0169-2607/$ – see front matter © 2011 Elsevier Ireland Ltd. All rights resdoi:10.1016/j.cmpb.2011.10.012
© 2011 Elsevier Ireland Ltd. All rights reserved.
atrium. Regurgitation occurs due to a dysfunction of the valveleaflets, papillary muscles or the chordae tendineae, and hasan occurrence of 2% [2].
The mitral valve separates the left atrium and ventricle.When functioning correctly, it allows blood to flow from theatrium to the ventricle during diastole, and prevents it flowingback during systole, thus maximizing flow out of the left ven-tricle into the systemic circulation. For a normal mitral valve,
phase of the left ventricle. After this phase, the left atrial con-traction contributes approximately 20% more to the volume inthe left ventricle prior to mitral valve closure and ventricular
erved.
i n b i o m e d i c i n e 1 0 9 ( 2 0 1 3 ) 190–196 191
st
cwetisda
dreli
imtcaotap
nehnanptgtivcol
2
2
TsscK
avssr
Fig. 1 – Force as a function of angle, representing three
fundamental behaviour of Fig. 1. The corresponding stiffness,K(�) from (3) is also shown in Fig. 2. Note that in Figs. 1 and 2,the stiffness in the first and last sections is assumed higher
c o m p u t e r m e t h o d s a n d p r o g r a m s
ystole. Similar behaviour is seen in the right ventricle withhe tricuspid valve.
Abnormal dynamics in this filling phase in either ventri-le may suggest valve dysfunction, but could also suggest aider problem with the circulation, for example pulmonary
mbolism [3]. Pulmonary embolism is often characterised byricuspid regurgitation and causes the secondary effect ofncreased volume in the atrium and/or ventricle [3]. Thus,ignificant research concentrates on the understanding ofetailed flow dynamics and pressure around the valves andtria.
Methods for measuring flow include Doppler echocar-iography [4–6], cineangiography, and cinefluoroscopy withadiopaque marker implantation [7]. All of these methods areither invasive or complex and time-consuming. Hence, noneend themselves to regular use for ongoing patient monitoringn regular clinical care.
Another approach for characterising valvular dysfunctions through physical models [8,9], or, more commonly, fluid flow
odeling around the valves. Flow around the valves can beurbulent and represent a highly non-linear system that ishallenging to model. Current models of this type are usu-lly based on Navier–Stokes [10], or more simplified modelsf Bernoulli flow [11,12]. However, all of them require difficulto obtain, detailed geometric information to construct, andre very difficult to validate. Thus, they too are not useful foratient-specific regular clinical monitoring or diagnosis.
This research uses simple dynamic models of the stiff-ess of the valve leaflets to characterise the fundamentalffects on flow and pressure, rather than concentrating onighly detailed fluid flow models. The valve is treated as aon-linear rotational spring or a ‘hinge’ with the change inngle under pressure driven flow being related to the stiff-ess and damping of the valve. Thus, the essential flow andressure dynamics can potentially be used to back calculatehe strength of the different chord structures in the valve,iving a physiological measure of valve disease with respecto the overall non-linear stiffness defined. Perhaps moremportantly, this approach has the potential to directly relatealvular dysfunction to the anatomical, structural defects thatause it, via such simplified models. This model and the meth-ds developed are tested and compared with clinical data from
iterature for initial proof-of-concept validation.
. Methodology
.1. Generalised model
he model treats the valve’s fundamental response to pres-ure as a non-linear rotational spring or a hinge with atiffness force dependent on the angle. Fig. 1 shows this con-ept schematically as a piecewise linear function, where the
3 stiffness acts to limit valve opening at maximum angle.In the first section, 0 < � < �1, the force changes rapidly with
slope K1 = FK(�1)/�1, which corresponds to the stiffness of the
alve during this period. In the middle section, �1 < � < �2, thetiffness is much lower, and in the final section, �2 < � < �/2, thetiffness is high again. The FK(�) curve in Fig. 1 could also beepresented by many more piecewise linear sections, which, indifferent stiffness profiles.
the limit, would define a continuous curve, with the stiffnessas a continuous function of � defined:
K(�) = dFK(�)d�
(1)
The following continuous description of FK(�) is used, as it cancapture the fundamental dynamics illustrated in Fig. 1.
FK(�) = a1 + a2� + a3 e−b1� + a4 e−b2� (2)
yielding K(�):
K(�) = dFK(�)d�
= a2 − b1a3 e−b1� − b2a4 e−b2� (3)
For example, substituting a1 = −a3 − a4, a2 = 0.04, a3 = 0.002,a4 = −0.35, b1 = −3.7, b2 = 11 into (2), yields the force versus �
curve in Fig. 2. Note that in this case, the force dramaticallyincreases for 0 < � < 0.2, has a small slope for 0.2 < � < 1, andincreases more rapidly again for 1 < � < �/2. It thus captures the
Fig. 2 – Force as a function of angle (continuous curve) fora1 = −a3 − a4, a2 = 0.04, a3 = 0.002, a4 = −0.35, b1 = −3.7,b2 = 11, and corresponding stiffness profile.
s i n b i o m e d i c i n e 1 0 9 ( 2 0 1 3 ) 190–196
Fig. 3 – Animal data [13] showing LAP, LVP and theta, andthe calculated �P.
192 c o m p u t e r m e t h o d s a n d p r o g r a m
than the middle section. This assumption was initially madefrom a thought experiment based on clinical data showingvalve motion [13] that the chords would stretch more at thebeginning and end of the opening, similar to the elastic prop-erties of blowing up a balloon. However, this dynamic will beshown not to be the case.
In general, the FK(�) curve of (2) and stiffness of (1) and(3) could be used to describe the physiological and mechan-ical behaviour of the valve as a function of the angle. Thisbehaviour can then be physiologically related to the anatom-ical chord structures and how they are utilised during aheartbeat.
However, to have a complete model or simulate thisbehaviour, the input driving force that opens and closes thevalve must be included. For the mitral valve, this input forcearises from the difference in pressure �P(t) between the leftventricle and the left atrium.
Thus, for a simplified and minimal model, a rotationalspring mass damper model may be defined by:
I�̈ + c�̇ + FK(�) = ̨ �P(t) (4)
�P(t) = LAP(t) − LVP(t) (5)
where I is the inertia due to the mass and size of the leaflets,c is the damping coefficient due to the blood surrounding theleaflets, FK(�) is the non-linear restoring force, LAP(t) is the leftatrial pressure, LVP(t) is the left ventricular pressure, and ̨ isthe torque constant converting differential pressure into aninput torque on the valve.
Applying Hooke’s Law to each section in Fig. 1 yields:
FK(�) = K1�, 0 < � < �1 (6)
FK(�) = K1�1 + K2(� − �1), �1 < � < �2 (7)
FK(�) = K1�1 + K2(�2 − �1) + K3(� − �2), �2 < � <�
2(8)
In the limit, where (6)–(8) are replaced by an infinite number ofpiecewise approximations, and, as the leaflets mass is reallylow, inertia is set to zero as a first approximation, (I = 0), (4)becomes:
c�̇ +∫ �
0
K(�) d� = ̨ �P(t) (9)
Note that if K were constant, the integral in (9) would reduceto the standard K(�). The stiffness based restoring force in(9) can be thought of as the rotational spring force or torquethat opposes the input torque ̨ �P(t) based on the varyinganatomical stiffness of the chords of the mitral valve. Moreimportantly, damage to the valve can be modeled by alteringK(�) in (9). This approach illustrates how K(�) can be used toquantify mechanical dysfunction with respect to the physio-logical damage or dysfunction of chords and resulting chord
stiffness.The damping coefficient, c, in (9) causes the delay betweenincreased pressure difference between the left atrium andventricle, and the mitral valve opening.
The overall goal of the model of (9) is to capture the mea-sured motion of the valve in terms of an estimated angle, �,using a measured pressure profile �P(t).
2.2. Modeling input pressure difference and mitralvalve response
The input pressure difference profile, �P(t), shown in Fig. 3was taken from measured animal data [13]. This pressure dif-ference was inferred from LAP and LVP profiles, measuredinvasively with catheters. This animal data also consisted ofdistance measurements of the amount the chords moved dur-ing the ventricular filling period of a heartbeat, as measured bycamera in a catheter or endoscope. Heart rate is 97.5 ± 19 bpm,giving a cardiac cycle duration of 0.62 s while the ventricularfilling period which corresponds to the opened period of themitral lasts 0.3 s. During this period, it was assumed the move-ment of the chords would reasonably correlate to the changein angle, �(t), of (9). Thus, the chord distance graph [13] wasscaled to a peak of �/2, as shown in Fig. 3.
�P in Fig. 3 contains two peaks, one during early diastoleand one during atrial contraction. The first period of blood flowfrom the left atrium to the left ventricle is passive, and largelypressure driven. This period is commonly referred to as theE wave or the early filling phase. The second period of flow,called the A wave, occurs as the left atrium contracts causinga rise in LAP (and thus �P) [14]. The left ventricle contractssoon after, increasing the pressure in the left ventricle, andreducing �P. Therefore, the A wave is largely driven by theflow from the atrial contraction. Hence, each period of mitralvalve opening during one cardiac cycle is governed by differentdynamics in each period, and suggests that each peak shouldbe considered separately.
Fig. 3 shows that the pressure difference becomes nega-tive as the mitral valve closes after both peaks. The first valveopening is longer than the second opening and significantlylags the peak in �P. In contrast, the second valve opening
corresponds almost precisely with the second peak in �P.c o m p u t e r m e t h o d s a n d p r o g r a m s i n b i
2
DmrsaseUsFtoci
3
Wmmr
wi
tapFni
c
profile of Fig. 7b is physiologically reasonable and matches
Fig. 4 – Solution process.
.3. Model solution process
ue to the different dynamics governing each peak, eachitral valve opening (E and A waves) are considered sepa-
ately. Eq. (9) is then solved numerically using a standard ODEolver in MATLAB, to find the optimal parameters of FK(�), c,nd ˛, using linear least-squares. Firstly, the measured pres-ure difference time profile is generated using (5) from thexperimental data [13] and used as the input to the model.sing combinations of FK(�), c, and ̨ determined using a gridearch, �(t) is computed using (9). For each combination of
K(�), c, and ˛, the sum-squared error is calculated betweenhe resulting �(t) and the experimental �(t), to determine theptimal parameters. Finally, the selected piecewise FK(�) isonverted into a continuous function using (2), and the result-ng �(t) recalculated. This process is summarised in Fig. 4.
. Results and discussion
e will now investigate a range of mechanical model to find aodel that best matches reported animal data of chord move-ent during a heartbeat. Table 1 shows the sum-squared error
esults for various FK(�) and c profiles.When a single FK(�) profile is assumed across both peaks,
ith an individual damping coefficient, c, for each peak, Fig. 5s obtained for �(t).
The corresponding FK(�) profile is shown in Fig. 5b. Simula-ions have revealed that changing the FK(�) profile in Fig. 5b has
smaller effect on the first peak than the second. For exam-le, even a constant stiffness or equivalently a linear line inig. 5b gives a similar match to the first peak in Fig. 5a (resultsot shown). Thus, F (�) is largely governed by the second peak
Kn this modeling framework.Fig. 5a also shows the damping coefficient, c, scaled for
larity. It is observed that the damping coefficient identified
o m e d i c i n e 1 0 9 ( 2 0 1 3 ) 190–196 193
is much higher for the first peak, as expected based on thegreater lag from the peak of �P seen in Fig. 3. Physiologi-cally, the first opening corresponds to a rapid filling and highblood flow velocity during the E wave. The second peak has alower flow and blood flow velocity [14]. Thus it follows that thedamping coefficient would decrease in the second opening.The Saito study [13] did not report flow velocity data. There-fore, it was not possible to model this effect which may be alimitation to this study.
To improve the match on the second peak, a hystere-sis effect was considered, whereby a different FK(�) profile isallowed when � is increasing versus when � is decreasing. Hys-teresis is considered relevant to the second opening due to thedifferent governing dynamics. When the valve opens the sec-ond time, it is not opening from a completely closed position,and the opening is driven by flow rather than by pressure.It is possible there is a hysteresis effect in the first opening.However, the insensitivity of � to changes in FK(�) means itis very difficult to prove this effect with the given data, andhighlights the need for animal studies with more completemeasurements to fully validate this, or any, type of model.Thus, to keep the model as simple as possible, it is assumedthe valve closes the same way for both openings. Fig. 6a showsthe corresponding �(t).
When considering a hysteresis effect, the FK(�) profile ofthe decreasing first peak must intersect with the FK(�) pro-file of the increasing second peak at the � value at whichone profile ends and the next begins. If the valve closed com-pletely between openings, this outcome would simply meanthat the two FK(�) profiles must start at the coordinate [0,0].However, it is observed that the valve does not close com-pletely between each opening. Instead, the valve closes toan angle of approximately 0.245 radians. Therefore, the two� profiles must intersect at � = 0.245, as seen in Fig. 6a.
The FK(�) profile of Fig. 6b is very similar to Fig. 5b with theexception that the valve is “easier” to open, or, specifically,it has a lower stiffness for the second opening. This result isphysiologically reasonable, since the valve is not opening froma completely closed position, and thus retains some “memory”of the previous opening. In addition, the impact of the chordsin resisting flow may be different once a valve is even partlyopen.
It had originally been envisaged that the FK(�) profile wouldlook similar to Fig. 1, with increased stiffness when the valveopens and closes, and decreased stiffness in between. Theresulting �(t) and FK(�) profiles are shown in Fig. 7a and b.
It is clear that even though a profile of this type has animproved match with first peak, it is not possible to match the�(t) profile of the second peak. The initial dip in the �(t) profilefor the second peak cannot be avoided unless the initial slopeof Fig. 7b is much lower, further validating the results in Fig. 6b.In addition, to maintain the shape of Fig. 7b, the final slope isrequired to be so large that �(t) becomes negative towards theend of the second peak.
The issues with the second peak of Fig. 7a highlight somelimitations of this study and the data used. Specifically, the
the observed anatomy of the valve chordae. In particular, theplateau between peaks is not fully closed, but given the onedataset it is also not necessarily the only possible value and
194 c o m p u t e r m e t h o d s a n d p r o g r a m s i n b i o m e d i c i n e 1 0 9 ( 2 0 1 3 ) 190–196
Table 1 – Sum-squared error for FK(�) and c profiles.
FK(�) c (incr. �) c (decr. �) Sum-squared error
1st 2nd 1st 2nd 1st 2nd
Fig. 5 0.085 0.009 0.085 0.009 1.219 1.739Fig. 6 0.083 0.006 0.083 0.006 1.253 1.104Fig. 7 0.110 0.0078 0.110 0.0078 0.699 3.180Fig. 8 0.100 0.0028 0.088 0.0105 1.129 0.342
Fig. 5 – (a) Comparison of modeled theta with animal data, assuming a single FK(�) across both peaks, and a separatedamping coefficient, c, for each peak. (b) Corresponding stiffness force FK(�).
Fig. 6 – (a) Comparison of modeled theta with animal data. Different FK(�) for increasing � in the second peak. (b) Thecorresponding stiffness force FK(�).
Fig. 7 – (a) Comparison of modeled theta with animal data usingFK(�).
FK(�) profile type of Fig. 1. (b) Corresponding stiffness force
c o m p u t e r m e t h o d s a n d p r o g r a m s i n b i o m e d i c i n e 1 0 9 ( 2 0 1 3 ) 190–196 195
Fig. 8 – (a) Comparison of modeled theta with animal data for unique FK(�) and c profiles. (b) Corresponding stiffness forceF
tmo
aoddlpnroTwti
nrminooFi
tptretptKbtt
ic
K(�).
here is, equally, no assurance that a lower value would notitigate the issues in Fig. 7a and thus provide a better match
verall.Hence, the limited data used is a limitation of this study
nd trying to match this only data set may increase the riskf over modeling. Due to the highly specialised nature of theata and highly invasive means required to obtain it, this oneata set is the only one the authors know of available in the
iterature. However, the results clearly show the fundamentalhysiological issues, such as the damping and chord stiff-ess changing within one cardiac cycle, that would be directlyepresented in any mitral valve dynamic model and be partf the effect and behaviour in cases of valvular dysfunction.hus, the data, while limited, does provide proof of concept,hich is the goal of this study and thus justifies the acquisi-
ion of further data sets in (planned) animal trials to clarify thisssue.
In addition, the profile of Fig. 7b, while physiological, doesot account for any hysteresis. Such an effect might improveesults, and could arise from several either chord or valve
aterial properties under stress or from un-modeled dynam-cs. In particular, this model does not directly account foronlinearities arising from the changing size of the valvepening during the cardiac cycle [13], which exerts forcesn the valve chordae and thus affect this type of model.urther efforts and improved datasets should clarify thisssue.
Finally, the best match can obtained by allowing FK(�) and co vary, as seen in Fig. 8a and b, which thus enables the modelrofile used to match the observed data. However, it is difficulto justify such a situation physiologically without more accu-ate data including velocity profiles, to better understand theffect of flow velocity on damping. It is noted that the slope ofhe raw �(t) profile is greater for the increasing side of the firsteak, and the decreasing side of the second peak, suggestinghat c could also be a function of �̇, similar to the definition that
is a function of �. The decreasing side of the first peak can beetter matched with increased damping; however, this causeshe valve to remain open at an angle of 0.5 radians, rather than
he 0.245 radians seen experimentally.It is observed in Fig. 8a that the model-fit is greatlymproved, particularly for the second, flow-driven peak. Theorresponding FK(�) profiles are shown in Fig. 8b.
As expected, the sum-squared error (Table 1) reduces asmodel complexity increases, particularly in the second, flow-driven peak. Although the model of Fig. 7a achieves the bestmatch for the first peak using the originally conceived FK(�)profile of Fig. 1, it cannot capture the effect of the valve notclosing completely between subsequent openings. Thus, thisballoon-type model appears not to apply over a full heartbeatin its present form.
4. Limitations
The current hinge model does not account for either the trans-lation or narrowing of the valve aperture during mitral valvemotion. Such an addition could alter the boundary param-eters of the FK(�) profiles in both peaks, possibly allowinga much more physiologically explainable stiffness profile tobe obtained, while retaining a good match to the reportedanimal data. Future work will quantify the effect of transla-tion and narrowing of the valve aperture during mitral valvemotion and its impact on this simplified model structure andapproach.
The effect of inertia has not been modeled and will also bepart of future improvements. It will also help to better under-stand the effect of flow velocity on damping and to adapt themodel as required to capture the dynamics of vascular dys-function.
This study is based on a single set of parameter com-ing from [13]. Their pressure data set was acquired with5Fr micronanometer-tipped catheter (MPC-500, Millar instru-ments, Houston, TX, USA) which guarantees that data isaccurate enough for the use of this study. However, as noted,this study, written as a proof of concept, will need moreaccurate and broader (more subjects) data, including velocityprofiles, to improve the proposed model, while avoiding therisk of over modeling to match this only dataset. Such datawould more fully validate the modeling approach. However,the results presented do justify such (planned) animal trials.
The piecewise stiffness profile used in this study is very
simple and should be improved to better describe the valvedynamics and ensure the uniqueness of identified parameters.In particular, more parsimonious models, including hystereticeffects that separate loading (systole) and unloading (diastole)s i n
r
196 c o m p u t e r m e t h o d s a n d p r o g r a m
are available in other fields such as structural dynamics thatmight better suit the dynamics observed. The use of such mod-els, based on this proof of concept should enable results thatbetter capture the observed dynamics in a physiologically andclinically relevant manner.
5. Conclusions
This research presents on the initial model structure, methodsand approach to assessing and capturing valvular dysfunctionin simplified, clinically applicable models.
A simple non-linear rotational spring model has beenimplemented to model the mitral valve. A measured pres-sure difference curve was used as the input into the model,which represents an applied torque to the valve leaflets. Vari-ous damping and hysteresis states were investigated to finda model that best matches reported animal data of chordmovement during a heartbeat and results were compared toa realistic �(t) profile obtained from the literature.
Once more completely validated and enhanced, this modelstructure can be incorporated into a closed-loop cardio-vascular system model to investigate the hemodynamicrepercussions of several pathological conditions, such asmitral regurgitation or stenosis. Correlating the stiffness anddamping profiles of the hinge model with specific anatomicalpart of the valve, will lead to a better knowledge of valvu-lar pathophysiology. More importantly, such a modified modelwould provide a useful tool to the clinicians to monitor, diag-nose and control valvular dysfunctions.
Acknowledgements
Katherine MOORHEAD: University of Liege Post-Doctoral Fel-lowship Grant.
Sabine PAEME: FRIA-FNRS (Fonds National de la RechercheScientifique) PhD Grant.
This work was financially supported in part by the Univer-sity of Liège, the University of Canterbury, the French Commu-nity of Belgium (Actions de Recherches Concertées–AcadémieWallonie-Europe).
e f e r e n c e s
[1] E. Iung, G. Baron, E.G. Butchart, A prospective survey ofpatients with valvular heart disease in Europe: the EuroHeart Survey on valvular heart disease, Eur. Heart J. 24 (2003)1231–1243.
b i o m e d i c i n e 1 0 9 ( 2 0 1 3 ) 190–196
[2] E.C. Jones, R.B. Devereux, M.J. Roman, J.E. Liu, D. Fishman,E.T. Lee, T.K. Welty, R.R. Fabsitz, B.V. Howard, Prevalence andcorrelates of mitral regurgitation in a population-basedsample (the Strong Heart study), Am. J. Cardiol. 87 (2001)298–304.
[3] B. Ristow, S. Ali, X. Ren, M.A. Whooley, N.B. Schiller, Elevatedpulmonary artery pressure by Doppler echocardiographypredicts hospitalization for heart failure and mortality inambulatory stable coronary artery disease, Am. Coll. Cardiol.49 (1) (2007).
[4] G.T. Wilkins, L.D. Gillam, G.L. Kritzer, R.A. Levine, I.F.Palacios, A.E. Weyman, Validation of continuous-waveDoppler echocardiographic measurements of mitral andtricuspid prosthetic valve gradients: a simultaneousDoppler-catheter study, Circulation 74 (1986) 786–795.
[5] M.S. Firstenberg, P.M. Vabdervoort, N.L. Greenberg, N.G.Smedira, P.M. McCarthy, M.J. Garcia, J.D. Thomas,Non-invasive estimation of transmitral pressure drop acrossthe normal mitral valve in humans: importance ofconvective and inertial forces during left ventricle filling,Cardiac Physiol. 36 (2000) 6.
[6] S. Laniado, E. Yellin, M. Kotler, L. Levy, J. Stadler, R.Terdiman, A study of the dynamic relations between themitral valve echogram and phasic mitral flow, Circulation 51(1975) 104–113.
[7] G.M. Pohost, R.E. Dinsmore, J.J. Rubenstein, D.D. O’Keefe, R.N.Grantham, H.E. Scully, E.A. Beirholm, J.W. Frederiksen, M.L.Weisfeldt, W.M. Dagget, The echocardiogram of the anteriorleaflet of the mitral valve. Correlation with hemodynamicand cineroentgenographic studies in dogs, Circulation 51(1975) 88–97.
[8] G. Wright, Mechanical simulation of cardiac function bymeans of pulsatile blood pumps, J. Cardiothorac. Vasc.Anesth. 11 (May (3)) (1997) 299–309.
[9] D.A. Nordsletten, S.A. Niederer, M.P. Nash, P.J. Hunter, N.P.Smith, Coupling multi-physics models to cardiacmechanics, Prog. Biophys. Mol. Biol. (2009).
[10] B. Baccani, F. Domenichini, G. Pedrizzetti, Model andinfluence of mitral valve opening during the left ventricularfilling, J. Biomech. 36 (2003) 355–361.
[11] C. Clark, The fluid mechanics of aortic stenosis. I. Theoryand steady flow experiments, J. Biomech. 9 (1976)521–528.
[12] B.J. Bellhouse, Fluid mechanics of a model mitral valve andleft ventricle, Cardiovasc. Res. 6 (1972) 199–210.
[13] S. Saito, A. Yoshimori, A. Usui, T. Akita, H. Oshima, J. Yokote,Y. Ueda, Mitral valve motion assessed by high-speed videocamera in isolated swine heart, Eur. J. Cardiothorac. Surg. 30(2006) 584–591.
[14] L. Schmitz, H. Koch, G. Bein, K. Brockmeier, Left ventriculardiastolic function in infants children, and adolescents.
Reference values and analysis of morphologic andphysiologic determinants of echocardiographic Doppler flowsignals during growth and maturation, J. Am. Coll. Cardiol.32 (1998) 1441–1448.