WA Clinical Alert (MedAlert) Policy - Parliament of Western ...
-
Upload
khangminh22 -
Category
Documents
-
view
0 -
download
0
Transcript of WA Clinical Alert (MedAlert) Policy - Parliament of Western ...
Before referencing this mandatory policy please ensure you have the latest version from the Policy Frameworks website. MP 0053/17
Effective from 14 June 2017
WA Clinical Alert (MedAlert) Policy
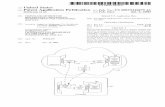
1. Purpose The WA Clinical Alert (MedAlert) Policy (the Policy) mandates the implementation of a standardised process of communicating clinical alerts across the WA health system using the PAS (Patient Administration System) for example TOPAS, webPAS, or HCare.
The objective of this policy is to reduce the risk of patients experiencing an adverse event related to a previously identified serious anaesthetic condition, specified medical condition, or serious unexpected drug reaction, by improving communication of these risks to clinicians when patients present to hospital before the medical record is retrieved.
This Policy outlines the minimum requirements for the approval and documentation of clinical alerts within patient health records and the PAS throughout the WA health system to ensure consistent, safe and immediately available clinical alert information to clinicians.
This Policy supersedes the WA Clinical Alert (MedAlert) Policy OD 0511/14.
This Policy forms part of the Clinical Governance, Safety and Quality Policy Framework.
2. Applicability
This Policy applies to Health Service Providers (HSPs) and contracted health entities that provide publicly-funded inpatient care.
3. Policy Requirements Each HSP must have its own local policy in place which includes governance arrangements, roles and responsibilities, and procedures to ensure the clinical alert process outlined below is followed and clinical alerts are entered into the PAS in a timely manner in all inpatient facilities. Clinical Alerts A Clinical Alert is a diagnosis which has the potential to be of critical importance to a patient’s management during the first 24 hours of their admission to hospital and assumes that the patient is not always capable of communicating such information. There are three classifications of clinical alerts; anaesthetic, medical and medication alerts.
Before referencing this mandatory policy please ensure you have the latest version from the Policy Frameworks website. MP 0053/17
Clinical Alert Process The clinical alert process involves:
Raising a clinical alert for a patient by completing MR ALERT 2 form (Appendix 1). This form is to be completed by a member of the treating medical team (for all alert categories) or pharmacist (for drug related clinical alerts only).
Assessing adverse drug reactions to determine whether they classify as a clinical alert – (Appendix 2).
Review and approval of the MR ALERT 2 form by the Clinical Alert Committee (CAC), or sole medical person/position at small facilities.
If approved, entering the alert into the PAS in a timely manner.
If a drug-related clinical alert occurs during hospitalisation a patient must be provided with the Adverse Drug Reaction Information Brochure for Consumers, or equivalent, that is completed by the treating medical team or pharmacist. (Appendix 5).
Standardised documentation requirements for adverse drug reactions, which may, or may not, be elevated to serious drug reactions that require a clinical alert (as outlined in Appendix 3).
Standardised documentation requirements for adverse drug reactions which occur during hospitalisation and require reporting to the Therapeutic Goods Administration (TGA) – Appendix 4).
All HSPs and contracted health entities with inpatient facilities are required to have a governance arrangements in place through their local policy, such as a Clinical Alert Committee (CAC):
Larger facilities are required to have a site-based CAC.
Smaller facilities may have a CAC managed at the regional/facility group level. In this situation there is a requirement to identify a sole medical person/position within each smaller facility responsible for reviewing and providing advice on clinical alerts. Clinical Alert Committee Membership To provide appropriate and comprehensive governance of each HSP local policy the CAC membership must at a minimum include a:
medical officer,
pharmacist,
health information manager, and
clinical coding representative.
Before referencing this mandatory policy please ensure you have the latest version from the Policy Frameworks website. MP 0053/17
Role and Responsibilities Each relevant CAC must be responsible for;
Reviewing appropriateness and approving all clinical alerts raised on MR ALERT 2 forms to be entered into the PAS.
Ensuring education is provided to all medical and pharmacy staff involved in raising clinical alerts ensuring a holistic understanding of what a clinical alert is, how to raise one for a patient and where to find the patient’s clinical alert information when the patient is admitted to hospital.
Managing the change requests for clinical alert categories and codes to be raised to the WA Clinical Alert Business User Group (Appendix 7).
Monitoring compliance at their facility/ies with this policy. The CAC must report regularly to the Clinical Governance Committee. Medication-related clinical alerts may also be tabled at the Drug and Therapeutics Committee/Medication Safety Committee as appropriate.
The PAS clinical alert system must not be used for:
Other PAS Alerts including Micro Alerts and patient and/or family member Behaviour (Risk) Alerts. These are outside the scope of, and are not defined within, this Policy.
MedicAlerts. The MedicAlert Foundation (who provides consumers with MedicAlert bracelets) has a registry to identify consumers with serious allergies or conditions and this is usually organised and authorised through the consumer’s general practitioner. This system is outside the scope of this policy.
4. Compliance, measurement and evaluation
HSPs are responsible for carrying out regular audits and evaluating compliance with the Policy. Each HSP Board must provide an annual statement of compliance assurance against all policy requirements to the [email protected] mailbox by 31 September for the preceding financial year. HSPs must make available the following indicators to the System Manager on request:
Percentage (%) (including numerator/denominator information) of alerts that were reviewed as appropriate to be entered onto PAS.
Percentage (%) (including numerator/denominator information) of medical, pharmacy and clerical staff who have received education on clinical alerts.
Before referencing this mandatory policy please ensure you have the latest version from the Policy Frameworks website. MP 0053/17
Evaluations to review the quality and appropriateness of information entered onto the PAS clinical alert system will be undertaken by the Clinical Alert Business User Group (within the Department of Health) on behalf of the System Manager. Feedback will be provided to the HSPs to review and rectify as required to ensure compliance. Non-mandatory suggested qualitative indicators for HSPs to monitor their compliance with this policy include:
Average time for alerts to be uploaded onto PAS, i.e. number of days from date of generating MR ALERT 2 form (filled out to date entered onto PAS).
Percentage (%) of patient medical records with MR ALERT 2 form that have been entered onto PAS from a 50 percentage sample.
Percentage (%) of patients with a clinical alert that has not been notified (e.g. patient has had an anaphylactic reaction to medication which has been documented in medical record (admission notes or medication chart) but has not be raised as a clinical alert on an MR ALERT 2 form).
5. Related documents The following documents are required to give affect to this policy (i.e. the documents included are mandatory):
Appendix 1 – MRALERT 2 Form for raising clinical alerts for PAS entry Appendix 2 - Serious Adverse Drug Reactions for Inclusion on the PAS Appendix 3 - Documentation of Adverse Drug Reactions (ADRs) Appendix 4 - Adverse Drug Reactions occurring during hospital admission
6. Supporting information
The following documents inform this policy (i.e. documents that are not mandatory to the implementation of this policy but may support the implementation of the policy):
Appendix 5 – Consumer Adverse Drug Reaction Brochure
Appendix 6 – Dietary Allergy / Food Allergy Appendix 7 - Raising a New Clinical Alert Appendix 8 - Patient Alert Form Appendix 9 - Recommended Process for Medical Condition (M) and Drug-
Related (D) Clinical Alerts Appendix 10 - Advance Health Directives
Before referencing this mandatory policy please ensure you have the latest version from the Policy Frameworks website. MP 0053/17
7. Definitions
Adverse Drug Reaction
A harmful or undesirable effect associated with the exposure to a medication/drug at therapeutic or sub-therapeutic doses.
Clinical handover Refers to any situation in which responsibility and accountability for some or all aspects of a patients care is passed from one clinician, or group of clinicians, to another.
Clinical Alert A diagnosis which has the potential to be of critical importance to patients’ management during the first 24 hours of their admission to hospital and assumes that the patient is not always capable of communicating such information. There are three classifications of clinical alerts; anaesthetic, medical and drug alerts. By raising a Clinical Alert (also known as MedAlert) for approval to be entered onto the PAS (patient administration system –e.g. TOPAS/webPAS/HCare), critical clinical information can be immediately flagged from the PAS for notification to clinicians before the medical record is retrieved.
Clinician Clinicians include doctors, nurses, pharmacists and allied health professionals.
PAS Patient Administration System (i.e. TOPAS – The Open Patient Administration System, webPAS, The Web based Patient Administration System, HCare – Health Care and Related Systems).
Patient medical record
The complete electronic or paper file associated with each patient.
Protocol Refers to a site-specific operating guidance document based on this document
Serious Drug Reaction
A serious adverse drug reaction is defined reaction that may lead to a life-threatening event and has an absolute or relative contraindication to repeat administration of the drug.
8. Policy owner
Assistant Director General, Clinical Services and Research Refer queries to the Secretariat of Clinical Alert Business User Group by email.
Clinical Alert Business User Group Division: Patient Safety and Clinical Quality Enquiries relating to this mandatory policy may be directed to: [email protected].
Before referencing this mandatory policy please ensure you have the latest version from the Policy Frameworks website. MP 0053/17
9. Review
This mandatory policy will be reviewed and evaluated as required to ensure it is relevant and recent. At a minimum it will be reviewed within 3 years after first issue and at least every 3 years thereafter.
Version Effective from Effective to Amendment(s) MP 0053/17 14 June 2017 1 June 2021 Original version
The review table indicates previous versions of the mandatory document and any significant changes.
10. Approval
This mandatory policy has been approved and issued by the Director General of the Department of Health.
Approval by Dr David Russell-Weisz, Director General, Department of Health
Approval date 23 May 2017
Published date 14 June 2017
RMR# F-AA-15932
Valid at the time of print
APPENDIX 1 – Clinical Alert (MedAlert) FORM _ MR ALERT 2 FORM Front Page
Example only
Valid at the time of print
APPENDIX 1 (continued) –Clinical Alert (MedAlert) Form /MR ALERT 2 Form Current clinical alert codes are printed on the back of the Clinical Alert (MedAlert) Form (MR Alert 2). They are broken down in the anaethetic alerts, drug/dietary reaction alerts and medical condition alerts. These alerts are reviewed periodically for relevance and use. Please refer to Safety and Quality website for most current version of this form. http://ww2.health.wa.gov.au/Health-for/Health-professionals/Safety-and-quality - Managing Clinical Risk.
Valid at the time of print
APPENDIX 2 - Serious Adverse Drug Reactions for Inclusion on the PAS Only serious life threatening reactions are to be documented on the PAS. Both the drug implicated and the reaction which occurred MUST be specified. A serious adverse drug reaction is defined as an absolute or relative contraindication to repeat administration of the drug. There is a need to differentiate between serious and severe reactions -“severe” is often used to describe the intensity of a medical event. Other cases require further clarification. Medications /drugs of concern are those likely to be given without verbal consultation with the patient (i.e. when the patient is too unwell). Examples include antibiotics, anaesthetics, and analgesics. Allergic reactions for inclusion: (Drug and Non Drug Allergies e.g. Latex, Intravenous Contrasts, Chlorhexidine):
Rash – if thought to be serious or severe, or accompanied by swelling of the whole body (not localised).
Anaphylaxis or Anaphylactoid reactions. Serum Sickness. Angioedema - swelling of face, throat, neck, tongue. Bronchospasm, asthma, other breathing difficulties.
Other serious or life threatening reactions for inclusion: Agranulocytosis (e.g. clozapine). Extrapyramidal side effects (severe dystonia / laryngospasm) to antipsychotics. Stevens Johnson Syndrome. Toxic epidermal necrolysis. Malignant hyperthermia. Scoline apnea or cholinesterase problem. Neuroleptic Malignant Syndrome. Hepatitis or Nephritis. Other – must be deemed serious and life-threatening/causing significant harm.
Adverse drug reactions that are NOT deemed Clinical Alerts/Med Alerts: Non-dose Related Reactions – Unpredictable and uncommon side-effects not related to
pharmacological action, with a low mortality rate (e.g. Timolol causing depression, Lithium induced neutropenia).
Time-related Reactions – Uncommon reactions which are usually dose-related, and occur sometime after the use of the drug (e.g. Tardive dyskinesia secondary to antipsychotic drugs).
Dose Related Reactions – Predictable side-effects related to pharmacological action of drugs (e.g. moderate extrapyramidal side-effects to antipsychotic drugs, excessive nausea and vomiting with opioids, vancomycin causing Red Man Syndrome).
Mild to moderate side-effects or unknown reactions are not to be recorded as a clinical alert but should be documented in the medical record. Examples of these include: - mild diarrhoea, nausea and mild vomiting, itch, hayfever / blocked nose, local swelling
or pain. - Non-serious adverse reactions to non-drug allergens (e.g. bee stings, grasses).
Valid at the time of print
Appendix 3 - Documentation of Adverse Drug Reactions (ADRs)
Before new medications/drugs are prescribed, dispensed or administered for a patient it is important that the patient’s ADR documentation is reviewed to prevent patient re exposure to a drug which may lead to an adverse event. On first hospital encounter with the patient (i.e. admission to hospital or outpatient clinic) the patient should be interviewed to determine whether the patient has experienced any previous adverse drug reaction or allergic responses when taking medications /drugs in the past. The treating clinician is responsible for determining whether an ADR is clinically important. For each adverse drug reaction identified the following information must be documented in the medical record, on all National Inpatient Medication Charts (NIMCs), and in the patient’s discharge summary:
The generic name of the medication/drug implicated. The reaction which occurred. The date of the reaction (if known). The person documenting the ADR must sign and date the record.
In the case of ADRs involving hypersensitivity reactions or clinically important side effects the following actions are required:
If the ADR occurs during the current admission, follow the actions below and refer to Appendix 5.
Document details on MR ALERT 1 – Patient Alert Form. An “ALERT” sticker should be placed next to the text and on the front cover.
Document details on every National Inpatient Medication Chart (NIMC) in the red Adverse Drug Reaction box. Attach an “ADVERSE DRUG REACTION” sticker on the red “Attach ADR Sticker” box and on the back page.
ADR details must be transferred to all new medication charts that are commenced. Patients with a known allergy, or suspected clinically important ADR or other
known risk should be issued with a RED patient identification band. No other coloured patient identification band is to be used.
If an allergy is identified subsequent to admission the standard white identification band will be replaced by a RED identification band by nursing/midwifery staff caring for the patient.
Valid at the time of print
Whether or not a reaction is deemed a drug-related clinical alert requires clarification by either a medical officer or senior pharmacist. If the ADR meets the criteria as a clinical alert outlined in Appendix 2, initiate the clinical alert process. (Recommended process outlined in Appendix 9. Information in this section is provided as a recommended example of how the process may function within a hospital site. Sites may vary process to meet individual circumstances). Rechallenge of Drug If a drug has been prescribed and there is documentation to state a previous adverse drug reaction has occurred (e.g. NIMC, medical record, triage records), the nurse/midwife must check with the prescriber that the medication is safe to administer. If a previous adverse drug reaction has been identified and documented appropriately, and there is a clinical need to rechallenge the patient due to no other therapeutic option being available and/or lack of clarification of the reaction, the adverse drug reaction must be acknowledged by the medical officer and reasons for rechallenge must be documented in the medical record. If the reaction is a serious adverse drug reaction (e.g. anaphylaxis, angioedema, bronchospasm, rash etc. refer to Appendix 2) the team consultant must review the order and document in the medical record if the drug is required to be administered.
Valid at the time of print
Appendix 4 - Adverse Drug Reactions occurring during hospital admission A new adverse drug reaction (ADR) occurring during a hospital episode requires: Documentation of the adverse drug reaction details (culprit drug [generic name],
reaction observed and date of reaction) in the medical notes, on the medication chart, on the PAS if appropriate, and in the discharge summary.
Supply patient with red patient identification band. The patient is to be given an Adverse Drug Reaction Information Brochure if an
adverse drug reaction has occurred during hospitalisation. (Refer to Appendix 2) Information detailing a new ADR must be communicated to the general practitioner or
receiving hospital in the discharge summary. An Advisory Committee on the Safety of Medicines (ACSOM) form may need to be
completed and forwarded to the Pharmacy Department and the Therapeutic Goods Administration (TGA) http://www.tga.gov.au/safety/medicines-statistics-2010.htm#report.
Alternatively online reporting can be done through the TGA website. Reports of suspected adverse drug reactions can be made: Online at 'Report a Problem' (http://www.tga.gov.au/safety/medicines-statistics-
2010.htm#report.) Using a 'Blue Card' available from the TGA's Office of Product Review (1800 044 114
or [email protected] ) or downloaded from the TGA website at 'Blue Card' adverse reaction reporting form, or MIMS Online. ( https://www.mimsonline.com.au)
Adverse drug reactions meeting status of serious adverse drug reaction in this policy should be reported to the TGA - Advisory Committee of the Safety of Medicines (ACSOM).
In event of an adverse drug reaction where agent is not clearly identified, clarification from Immunology (where available) and documentation of all drugs the patient is prescribed must be reported to the TGA - Advisory Committee of the Safety of Medicines (ACSOM).
Valid at the time of print
APPENDIX 5 - Adverse Drug Reaction Information Brochure for Consumers
A print ready version can be found on the Safety and Quality website - Managing Clinical Risk http://ww2.health.wa.gov.au/Health-for/Health-professionals/Safety-and-quality
Valid at the time of print
Appendix 6 – Dietary Allergy / Food Allergy Dietary (Food) allergy is deemed a clinical alert (which must be differentiated from a food intolerance which is not a clinical alert). A food allergy is an abnormal immune mediated reaction to ingested food, resulting in clinical symptoms. Reactions can occur after eating a small amount of food. Food allergy affects 10% of infants <1 year, 4-8% of children <5 years and up to 2% of the adult population in Australia. It is the responsibility of the treating medical team to ensure a clinical alert is recorded for patients with a food allergy. A food intolerance does not involve the immune system and does not cause severe life-threatening allergic reactions (known as anaphylaxis) and should not be listed as a clinical alert (see clinical alert definition). Food intolerance reactions are dose related and are often delayed. Symptoms may include headaches or gastrointestinal symptoms after eating. Food Allergies to be reported as a clinical alert include: Anaphylaxis or anaphylactoid reaction Swelling of face, lips, eyes, tongue or throat Flushing or hives/welts on the skin Tingling mouth Severe abdominal pain, severe vomiting, severe diarrhoea Difficult /noisy breathing Difficulty talking and / or hoarse voice Wheeze or persistent cough Persistent dizziness and/or collapse Pale and floppy (in young children) Acute onset of hypotension, severe breathing difficulty, bronchospasm or upper
airway obstruction where anaphylaxis is considered possible.
There are nine common allergens in Australia specified by the Australasian Society of Clinical Immunology and Allergy (ASCIA). These are wheat, egg, soy, cow’s milk (diary), peanuts, tree nuts, fish, shell fish (Crustacean), and sesame. These foods cause around 90% of food allergic reactions in Australia. Food labels are required by law to declare if the food or beverage contains any of these common nine allergens. (Note: The legislation identifies gluten, not wheat). Outside of the nine common food allergens, any other food can cause an allergic reaction. A food allergy clinical alert (DOther10), must include in the comments field the words either ‘unconfirmed’ or ‘confirmed’ depending on what follow up has been completed in determining the association between the allergy symptoms and the suspected food allergen. A ‘confirmed’ food allergy must been diagnosed by an immunology or allergy specialist. When a food allergy challenge has been completed, the hospital (or HSP for smaller sites) must have a system in place to document de-labelling of a food allergy including removal of a food allergy clinical alert.
Valid at the time of print
Appendix 7 – Changes or additions to Clinical Alert categories, codes or definitions
The WA Clinical Alert Business User Group is established through the Patient Safety and
Clinical Quality Directorate, Clinical Services and Research Division, Department of
Health.
Responsibilities of this group include:
assessment of existing Clinical Alert code definitions to be used on the PAS;
assessment of any proposed changes made on TOPAS/WebPAS; and
provision of guidance on standardisation of documentation of adverse drug
reactions (and serious non drug allergies e.g. Latex, Intravenous Contrasts,
Chlorhexidine) which may, or may not, be elevated to serious drug reactions that
require a clinical alert.
Proposed changes to clinical alerts categories, codes or definitions must be requested
through the WA Clinical Alert Business User Group via the hospital’s local committee
(CAC) or representative.
CA representatives or equivalent may refer queries and proposals for such changes to the WA Clinical Alert BUG Secretariat via [email protected]
Valid at the time of print
Appendix 9 - Recommended Process for Medical Condition (M) and Drug-Related (D) Clinical Alerts Information in this section is provided as a recommended example of how the process may function within a hospital site. Sites may vary process to meet individual circumstances. It is up to the individual health service provider to assign authorisation to the appropriate position/s to enter the alerts onto the PAS. Positions responsible for entering alerts must have undertaken training on clinical alerts and use of the PAS.
1. Identification of alert and completion of Clinical Alert / Med Alert Notification (MR ALERT 2) form
During the patient’s admission it is the responsibility of the medical officer to report clinical alerts in accordance with specified medical, anaesthetic or drug-related alerts and specific detailing as per Clinical Alert / Med Alert Notification (MR ALERT 2) form. This form must be forwarded to clinical coding to enter onto the PAS. The form is then to be filed at the front of the medical record.
During the patient’s admission it is the responsibility of the clinical pharmacist to report adverse drug reactions in accordance with specified clinical guidelines and specific detailing as per Clinical Alert / Med Alert Notification (MR ALERT 2) form. This form must be forwarded to clinical coding to enter onto the PAS. The form is then to be filed at the front of the medical record.
Clinical coding staff are to identify records with new *Med Alert/Clinical Alert Notification (MR ALERT 2) form/s for medical, anaesthetic or drug alerts. Initiate Patient Alert Form (MR ALERT 1) if alert identified during coding.
2. Authorisation process The designated Clinical Alert Committee (CAC) / dedicated position (depending on
size of institution - ideally a medical officer or clinical pharmacist (if drug related)) responsible for governance of clinical alerts for each site will review all medical alerts and drug alert queries in a timely manner, with the exclusion of anaesthetic and specified alerts.
Some clinical alerts can be entered by clinical coding staff without co-authorisation (including, but is not exclusive to organ transplant, heart valve replacements, pacemaker or other implanted devices when inserted during the admission being coded, asplenia and Advance Health Directive). Alerts that meet this criterion should be decided by the governing body within the hospital.
3. Data entry and file form in medical record Once the clinical alert has been approved by the CAC/dedicated position, the alert
must be entered into the PAS clinical alert system. This must be undertaken by persons authorised to enter patient data onto the PAS clinical alert system. This role may be allocated to a clinician (doctor) or pharmacist (for drug-related alerts) if trained
Valid at the time of print
sufficiently to do so. If no authorised person is available in the clinical area the MR ALERT 2 form should be forwarded with the medical record (if requested) to medical records/ clinical coding to be entered onto the system.
4. If the proposed clinical alert is not approved for entry onto PAS If the alert is not deemed to be a clinical alert (i.e. serious/life threatening issue) but is
still required to be captured in the patient’s medical record (such as mild to moderate side-effects to a drug), the position responsible for approval of alerts should ensure the alert (medical, anaesthetic or drug alert information) is documented on inside cover of the health record, the Patient Alert Form (MR ALERT1) or in the digital medical record if not already documented.
Cross the Clinical Alert/ Med Alert Notification forms through with two diagonal lines and state the reason why not approved. The MR ALERT 2 form should still be filed as a record of proposed Clinical Alert with reason why it was not approved.
5. Removal of alerts from PAS If an alert is entered in error it needs to be removed from the PAS to reduce the risk to
the patient. If an alert is no longer active, or is no longer relevant, the alert should be inactivated
so they do not automatically be displayed. When the alert codes are being reviewed and need to be updated (new ones added or
obsolete ones removed) then a change request is raised by the committee to update the PAS, and the relevant communications sent to stakeholders regarding the change.
6. Recommended process for alert queries within hospitals The designated local committee / dedicated person (depending on size of institution)
responsible for governance of clinical alerts for each site will review all medical alerts and drug alert queries, with the exclusion of anaesthetic and specified alerts.
Chair, Clinical Alert Committee will: Review medical records / Clinical Alert / Med Alert Notification (MR ALERT 2) form/s
flagged as containing new alerts. Approve/not approve Clinical Alert/Med Alert Notification forms and adjust wording as
needed.
If Clinical Alert is approved: Document the clinical alert information as per section 6.4. Record your name, designation and date of entry. Place alert labels on the outside of the health record. Forward Clinical Alert/Med Alert Notification form (MR ALERT 2) and health record to
Clinical Coding for addition onto the PAS.
Valid at the time of print
If Clinical Alert Not Approved: Cross the Clinical Alert/Med Alert Notification form (MR ALERT 2) through with two
diagonal lines and state the reason why not approved. Ensure relevant alert information is documented on inside cover of the health record and the Patient Alert Form (MR ALERT1).
Return records/Clinical Alert/MedAlert Notification (MR ALERT 2) form to medical records.
Where a clinical alert for a patient does not fit within one of the specified categories the Medical Other (M.Other.4) or Drug Other (Drug.Other.3) category may be used. The M.Other 4 /Drug.Other.3 alerts must only be used for clinical alerts that are potentially life-threatening conditions that are crucial for treating physicians to be alerted to immediately on patient presentation to hospital. D.Other3 alerts must have the specific drug and the reaction documented before being submitted for input to the PAS. The use of these codes will be reviewed periodically by the Clinical Alert Business User Group to determine if new codes are required.
Valid at the time of print
Appendix 10 - Advance Health Directives If a patient has an Advance Health Directive (ADH) a clinical alert should be raised for the patient. An Advanced Health Directive (AHD) is a document that contains the patient’s decisions about future treatment. Treatment includes medical, surgical and dental treatment and other health care. An AHD can either provide consent, or refuse consent, to future treatment. An AHD comes into effect only if the patient is unable to make reasonable judgments about a treatment decision at the time that the treatment is required. In these circumstances, the AHD acts as your ‘voice’. When a patient presents to hospital (whether as an emergency presentation or a direct admission) it is important to identify if the patient has an AHD and ensure the presence of the patient’s AHD is recorded as a clinical alert and filed within the patient’s medical record. Completing a clinical alert and filing a copy of the patient’s AHD within their medical record will raise awareness of advance care planning (ACP) and also improve access to an AHD at point of care. The presence of an AHD alert (M11.02) on the PAS provides a flag that identifies that an AHD exists for the patient. The details of the AHD are not stored on the PAS. On identifying an AHD alert the doctor must discuss the AHD with the patient or the family/carer to determine the content and currency of the AHD. It is important that the treating team be familiar with the patient’s AHD and their treatment wishes. As soon as possible an ACP discussion should be held with the patient to clarify if they remain comfortable with their choice of preferred treatment decision(s). Please refer to the Advance Care Planning website for further information. www.health.wa.gov.au/advancecareplanning
Valid at the time of print
This document can be made available in alternative formats on request for a person with a disability. © Department of Health 2017 Copyright to this material is vested in the State of Western Australia unless otherwise indicated. Apart from any fair dealing for the purposes of private study, research, criticism or review, as permitted under the provisions of the Copyright Act 1968, no part may be reproduced or re-used for any purposes whatsoever without written permission of the State of Western Australia”.
Date of Last Review: November 2017 Page 1 of 4 Date Next Review: November 2020
Effective: 5 December 2017
Anaphylaxis During Anaesthesia - Endorsed for use in Clinical Practice Policy
1. Background
The WA Country Health Service (WACHS) seeks to provide direction and guidance to all staff through the availability of appropriate evidence based guidelines and procedures. It is envisaged that this information will assist in the efficiency and effectiveness of the organisation in meeting current legislation and the key principles of quality improvement.
2. Policy Statement Whole of WA Health policy documents are the overarching policy documents that must be complied with by all WA Health staff. To complement these documents, the WACHS has endorsed specific policies, guidelines and procedures covering a range of issues related to clinical practice. WA Health and WACHS policy documents are available via the HealthPoint Policies intranet site.
The WACHS endorses the Anaphylaxis Management Guidelines developed by the Australian and New Zealand Anaesthetic Allergy Group (ANZAAG) in conjunction with ANZCA, through the Anaesthetic Allergy Subcommittee of the Quality and Safety Committee as evidence based recommended practice for use by medical, nursing and midwifery staff. ANZAAG have developed an anaphylaxis box to aid with management of patients where perioperative anaphylaxis occurs. The box should be stored in an agreed location in operating theatres well known to staff.
The ANZAAG has a policy of continuous resource monitoring and quality improvement. Feedback from ANZCA Fellows is welcome. Changes to resources will occur in accordance with current best evidence. Please check the ANZAAG website to ensure your department is using the most up-to-date version of resources.
External sources that are endorsed for use in WACHS clinical practice provide a standard for clinical governance and service delivery, and provide a range of information and evidence-based practice to support best practice by all staff for country health patients and clients.
When applied, the information contained in these guidelines must take account of the context and scope of practice, level of service delivery and facility capacity.
These guidelines do not indicate an exclusive course of action or serve as a definitive mode of patient care. Variations that take into account individual circumstances, clinical judgment, scope of professional practice and patient choice, may be appropriate dependent on the health care setting. While every reasonable effort is made to ensure the accuracy of the information contained in these guidelines, no guarantee can be given that the information is free from error or omission. Users are strongly recommended to confirm by way of independent sources, that the information contained within these guidelines and procedures is correct, especially drug doses that may change from time of publication. Please note the web-based electronic copy is the master copy for all guidelines, policies and procedures.
05/12/2017 2:59 pmDocument valid at:
WACHS Anaphylaxis During Anaesthesia - Endorsed for use in Clinical Practice Policy
Date of Last Review: November 2017 Page 2 of 4 Date Next Review: November 2020
3. Procedure on suspecting anaphylaxis.
Call for immediate assistance.
Follow Management Cards (printed in colour and stored within the box) Hyperlinks available here for ready access online.
Anaphylaxis Box Contents Checklist
Perioperative Anaphylaxis Management Guidelines: Introduction
Anaphylaxis during Anaesthesia – Adult Immediate Management
Anaphylaxis during Anaesthesia – Paediatric Immediate Management
Anaphylaxis during Anaesthesia – Adult Refractory Management
Anaphylaxis during Anaesthesia –Paediatric Refractory Management
Anaphylaxis during Anaesthesia – Differential Diagnosis
Anaphylaxis during Anaesthesia - Post Crisis Management
Form Letter for Patient
ANZAAG Referral Form
Patient Information Brochure Drug Infusions Follow the Australian Injectable Drugs Handbook for infusions.
4. Definitions
Anaphylaxis is the most severe form of allergic reaction and is potentially life threatening. It must be treated as a medical emergency, requiring immediate treatment. Anaphylaxis is a generalised allergic reaction that often involves more than one body system. It can occur within seconds or minutes of exposure to something you are allergic to.
5. Suggested Roles and Responsibilities
5.1 Coordinator – Team Leader 5.2 Anaesthetist and anaesthetic nurse or Anaesthetic Technician – Airway 5.3 Circulating Nurse – Anaphylaxis Box 5.4 First responder – Scribe 5.5 Second responder – Runner
05/12/2017 2:59 pmDocument valid at:
WACHS Anaphylaxis During Anaesthesia - Endorsed for use in Clinical Practice Policy
Date of Last Review: November 2017 Page 3 of 4 Date Next Review: November 2020
5.6 Doctor Form Letter for Patient. This letter provides the patient with a record to
identify all drugs given prior to the reaction. Allergic Reaction in the Operating Room: Patient Information – this brochure
can be given to the patient to explain the reaction they experienced and what needs to be done to guide their management for future anaesthetics.
Testing Referral Form – allows recording of details of reaction and appropriate referral.
5.7 WACHS Executive Directors of Medical and Nursing and Midwifery
Services, and the Chief Operating Officers are responsible for: acting as the principal endorsement authority for external organisations’
clinical policy documents.
5.8 WACHS Area and Regional Medical, Nurse, Mental Health, Aged Care and Population Health Directors are responsible for: participating in the review for appropriateness of external organisations’
clinical policy and guideline documents for use by clinicians within the WACHS.
5.9 All WACHS clinicians are accountable for their own practice and are to provide
care: within their registration status in accordance with the codes and guidelines approved by their relevant
National Board supported by AHPRA within their scope of practice and competence within their prescribed responsibilities and duties as defined in their Job
Description Form (JDF) and within the context of practice that they are operating.
6. Policy Reviewers
This policy was reviewed by the following WACHS subject matter experts: Dr Pat Coleman Consultant and Clinical Lead (Anaesthetics) WACHS Geraldton Hospital Anaesthetic Clinical Governance / WACHS Anaesthetists Dr James Lloyd Consultant Anaesthetist Geraldton Hospital Anne Annear CNM Theatre / CSSD Geraldton Midwest WACHS peri-operative leaders All WACHS sites' Clinical Practice Improvement Coordinators, anaesthetists,
Regional Medical Directors, theatre key stakeholders. 7. Evaluation
The number of reportable clinical incidents or near misses relating to inappropriate care provided by clinicians.
Completion and reporting of Datix CIMS. Patients to be reviewed at the Anaesthetic Clinical Governance meeting.
05/12/2017 2:59 pmDocument valid at:
WACHS Anaphylaxis During Anaesthesia - Endorsed for use in Clinical Practice Policy
Date of Last Review: November 2017 Page 4 of 4 Date Next Review: November 2020
8. Standards
National Safety and Quality Health Care Standards 1.5.2 Actions are taken to minimise risks to patient safety and quality of care. 1.6.2 Actions are taken to maximise patient quality of care. 9.3 Implementing mechanisms for recording physiological observations that
incorporate triggers to escalate care when deterioration occurs. 9.4 Developing and implementing mechanisms to escalate care and call for
emergency assistance where there are concerns that a patient’s condition is deteriorating.
9.4.1 Mechanisms are in place to escalate care and call for emergency assistance. 9.4.3 Action is taken to maximise the appropriate use of escalation processes.
9. References
See references listed in Anaphylaxis Management Guidelines
10. Compliance Failure to comply with this policy may constitute a breach of the WA Health Code of Conduct (Code). The Code is part of the Employment Policy Framework issued pursuant to section 26 of the Health Services Act 2016 (HSA) and is binding on all WACHS staff which for this purpose includes trainees, students, volunteers, researchers, contractors for service (including all visiting health professionals and agency staff) and persons delivering training or education within WACHS. WACHS staff are reminded that compliance with all policies is mandatory.
11. Policy Framework Clinical Governance, Safety and Quality Policy Framework
This document can be made available in alternative formats on request for a person with a disability
Contact: Surgical Services Coordinator Midwest (S. Hogan) Directorate: Nursing and Midwifery Services TRIM Record # ED-CO-15-23219
Version: 2.00 Date Published: 5 December 2017 Copyright to this material is vested in the State of Western Australia unless otherwise indicated. Apart from any fair dealing for the purposes of private study, research, criticism or review, as permitted under the provisions of the Copyright Act 1968, no part may be reproduced or re-used for any purposes whatsoever without written permission of the State of Western Australia.
05/12/2017 2:59 pmDocument valid at:
MEDICATION ADMINISTRATION POLICY
FOR NURSES, MIDWIVES AND UNREGULATED HEALTH WORKERS
The Medicines and Poisons Act 2014 and Medicines and Poisons Regulations 2016 came into effect on 30 January 2017. The transitional provisions of this legislation ensure the continuity of arrangements outlined in this policy.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Effective: 25 January 2018
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 1 of 50
TITLE: MEDICATION ADMINISTRATION POLICY FOR NURSES, MIDWIVES AND UNREGULATED HEALTH WORKERS
TABLE OF CONTENTS 1. BACKGROUND .......................................................................................................... 3 2. LEGISLATIVE REQUIREMENTS ............................................................................... 4 3. DEFINITIONS .............................................................................................................. 4 4. ROLES AND RESPONSIBILITIES ............................................................................. 5
4.1 Registered Nurse and Midwife ............................................................................ 5 4.2 Direct Entry Midwife (who is not a registered nurse) ........................................... 6 4.3 Enrolled Nurse .................................................................................................... 7 4.4 Enrolled Nursing or Registered Nursing or Midwifery Students .......................... 8 4.5 Unregulated Health Worker ................................................................................. 8
5. PRINCIPLES OF MEDICATION ADMINISTRATION ................................................. 9 5.1 Administration Standards .................................................................................... 9 5.2 National Inpatient Medication Charts ................................................................ 10 5.3 Medication History and Management Plan ........................................................ 10 5.4 Patient’s Self Medication ................................................................................... 11 5.5 Withholding Medication ..................................................................................... 12 5.6 Correct Documentation ..................................................................................... 12 5.7 Discharge, Transfer, or Non-admitted Patient Medication Planning .................. 13 5.8 Fees and Charges for Medication ..................................................................... 13 5.9 Patient Education ............................................................................................. 13
6. MEDICATION ERRORS ........................................................................................... 14 7 MEDICATION PRESCRIBERS ................................................................................. 15
7.2 Labelling of medications other than starter packs ............................................. 15 7.3 Registered Nurse’s Legal Responsibility ........................................................... 16
8. VERBAL ORDERS ................................................................................................... 16 9. DESIGNATED REMOTE AREA NURSING POST ................................................... 17 10. APPROVED STARTER PACKS ............................................................................... 17
10.1 Approved Starter Pack Supply .......................................................................... 17 10.2 Before Giving an Approved Starter Pack .......................................................... 18 10.3 Provision of a Psychiatric Starter Pack ............................................................. 18
11 NURSE INITIATED NON PRESCRIPTION MEDICATIONS ..................................... 18 12. NURSE INITIATED STI TREATMENT CODE .......................................................... 19 13. GUIDELINES FOR USE OF OXYGEN ..................................................................... 19 14. VACCINATIONS/IMMUNISATIONS ......................................................................... 19 15. COMPLEMENTARY MEDICINES............................................................................. 20 16. PRESCRIBING NUTRITIONAL SUPPLEMENTS..................................................... 20 17. HIGH RISK MEDICATIONS ...................................................................................... 20
17.1 Anti infective agents. ......................................................................................... 20 17.2 Guidelines for Midazolam for Adult or Paediatric Sedation .............................. 19 17.3 Potassium Chloride ........................................................................................... 22
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 2 of 50
17.4 Insulin ................................................................................................................ 22 17.5 Narcotics (opioids) ............................................................................................ 22 17.6 Chemotherapy................................................................................................... 22 17.7 Heparin and other anticoagulants ..................................................................... 22 17.8 Systems ............................................................................................................ 23
17.8.1 Intrathecal Medication .......................................................................... 23 17.8.2 Epidural Therapy .................................................................................. 23 17.8.3 Medication Restrictions to Nurse Administered IV Bolus Treatment .... 23 17.8.4 Infusion Pumps..................................................................................... 23
18. RECORDABLE DRUGS INCLUDING CONTROLLED DRUGS/ DRUGS OF ADDICTION .............................................................................................................. 24 18.1 Schedule 4 Restricted Medications ................................................................... 24 18.2 Schedule 8 Medications .................................................................................... 24 18.3 Administering Schedule 4 Restricted or Schedule 8 medications from dose
administration aids in hostel and aged care facilities. ....................................... 25 18.4 Patient Discharge and Schedule 8 Medication .................................................. 26 18.5 Storage, transfer or disposal of medication refer to section 20 .......................... 26
19. INTRAVENOUS (IV) ADMINISTRATION .................................................................. 26 19.1 Intravenous therapy and infusion and bolus medication administration ............ 26 19.2 I V Flushes ........................................................................................................ 28 19.3 Intravenous Additives and Bolus Dose .............................................................. 28 19.4 Infusion Pump Safety Information ..................................................................... 29 19.5 Labeling, Changing Infusions and Intravenous Lines ........................................ 30
20. STORAGE OF MEDICATIONS ................................................................................. 30 20.1 Bedside Storage ................................................................................................ 30 20.2 Storage of Patient’s Own Medication ................................................................ 31 20.3 Storage of controlled drugs ............................................................................... 31 20.4 Keys and Access to Controlled Drug Keys ........................................................ 32 20.5 Transfer of controlled drug keys ........................................................................ 32 20.6 Transfer of recordable medication including Controlled Drugs. ......................... 33 20.7 Disposal of Drugs of Addiction and Poisons Included in
Schedule 4 Restricted and Schedule 8 ............................................................. 33 20.8 Reporting Of Schedule 4 Restricted and 8 Medication Stock Discrepancies 34 20.9 Medication Fridge .............................................................................................. 34
21. EVALUATION ........................................................................................................... 35 21.1 Compliance ....................................................................................................... 35 21.2 Mitigation strategies .......................................................................................... 35
REFERENCES ................................................................................................................. 36 APPENDIX 1 Starter Pack Approval Site List ................................................................. 39 APPENDIX 2 “Approved Starter Packs” as at 18 September 2013 ................................ 42 APPENDIX 3a Nurse Initiated Medications Non-Prescribed Schedule 2 and 3
Medications for Adult Patients .................................................................. 44 APPENDIX 3b Nurse Initiated Non-Prescribed Schedule 2 and 3 Medications for
Paediatric Patients .................................................................................... 45 APPENDIX 4 Designated Remote Area Nursing Posts .................................................. 46 APPENDIX 5 Supply by Registered Nurses at Remote Area Nursing Posts .................. 47 APPENDIX 6 Drug and IV flow calculations ................................................................... 48 APPENDIX 7 Anaphylaxis Flowchart .............................................................................. 49 APPENDIX 8 Policy Review Contributors ....................................................................... 50
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 3 of 50
1. BACKGROUND
The Medication Administration Policy – Nursing Practice Standard is for application across WA Country Health Service sites (adult and paediatric), including hospital in the home, community health and public health settings, sub-acute care, mental health and aged care facilities, and remote area nursing posts. Contributors to this policy review are listed in Appendix 8. Nurses and midwives are accountable for their own practice and must only undertake medication management activities which are within their scope of practice and for which they are legally entitled to perform; educationally prepared for and competent to undertake. The scope is outlined in the: Australian Nursing and Midwifery Council: A national framework for the
development of decision-making tools for nursing and midwifery practice 2007 WA Health Operational Directive OP 1988/05 Scope of Enrolled Nursing
Practice and Enrolled Nurse Competencies The nurse or midwife must consult appropriate resources and references when unsure of details of the prescription, preparation or administration of medications. These include but are not limited to: Australian Medicines Handbook Australian Injectable Drug Handbook Australian Medicines Handbook - Children's Dosing Companion eMIMs eTG (Electronic Therapeutic Guidelines) Royal Flying Doctor Service (RFDS) product information WACHS Regional Pharmacist.
WA Health Operational Directives and Operational Circulars hyperlinked in this policy are to be read, understood and adhered to by WACHS nurses and midwives and health workers at all times. Reference to some guidelines via the HealthPoint website may also be necessary for approved WACHS protocols including some South Metropolitan Health Service (SMHS) Nursing Practice Standards, the Princess Margaret Hospital (PMH) Nursing Practice Manual or King Edward Memorial Hospital (KEMH) clinical guidelines also endorsed for use in WACHS. This Medication Administration Policy – Nursing Practice Standard is to be read in conjunction with the National Standards in Quality Health Service Standard 4 (NSQHSS) National Inpatient Medication Chart (NIMC) Standardised Charts and Guidelines (2008) endorsed for use in WACHS (Medical Record series 170s) (e.g. adults, paediatric, neonatal, residential care and adult anticoagulant).
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 4 of 50
2. LEGISLATIVE REQUIREMENTS The WA Country Health Service (WACHS) provides safe medication administration in accordance with the national and state legislative requirements as per the: Health Practitioner Regulation National Law (WA) Act 2010 Australian Health Practitioner Regulation Agency (AHPRA) Code of Ethics and
Professional Code of Conduct for Nurses August 2008 Carers Recognition Act (WA) 2004 Poisons Act (WA) 1964, Poisons Regulations (WA)1965 and Poisons
Amendment Regulations (No 5) (WA) 2010 Therapeutic Goods Act 1989 Occupational Safety and Health Act 1984.
3. DEFINITIONS
Administration May be defined as the actual giving of a medication orally, by
injection, per rectum or other route.
Approved health service
Those listed in the Starter Pack approval list Appendix 1.
Authorised person
The designated controller (RN/midwife) of the Schedule S4R and S8 keys has knowledge at all times of who is carrying the keys. i.e. may delegate keys to another RN/Midwife but remains responsible for the S4R and S8 keys.
Competency Possess the knowledge, skills and behavioural attributes to perform a task.
Competent Demonstrate the minimum nursing or midwifery standard for effective work performance.
Direct supervision
Direct supervision is considered to be in the company of a RN.or medical practitioner or visually via the Emergency Telehealth Service.
Dispense Means supply the medicine or poison on and in accordance with a prescription given by a medical practitioner, nurse practitioner or dentist.
Dosage Administration Aid
A medication aid is a pre-packed medication dose in a container identified for a specific individual. It is used to support safe administration of medications. The client/ resident/ patient’s name, medication name, dose and time the medication is to be given is to be clearly labelled on the preparation dispensed by the pharmacist. May also include a pharmacy filled aid e.g. Webster Pak®.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 5 of 50
Dosage unit Means an individual dose of a poison and includes a tablet,
capsule, cachet, single dose powder, or a single dose sachet of powders or granules.
Medication support for UHWs
Medication prompting is described as assisting the client/ resident/ patient with self-medication and involves:
i. reminding and/or prompting the client to take the medication ii. assisting (if needed) with opening of medication containers
for the client, and iii. other assistance not involving medication administration.
Standing Orders
A written document that contains instructions for the administration of medications in a defined clinical situation. Standing orders specify the condition for which the orders apply and stipulate the medication to be given, dosage and route of administration. Their use is limited to the treatment of identified acute medical conditions at designated remote area nursing posts.
Supply Includes distribute and sell but not the administration to a patient of any substance specified in any of the Schedules to the Act by a medical practitioner, nurse practitioner or dentist, or by a registered nurse or registered midwife when acting under the direction of a medical practitioner, shall not be deemed to be supplying within the meaning of these regulations.
Time-critical medicines
Medicines where delayed or early administration by more than 30 minutes may cause harm or sub-therapeutic effect.
4. ROLES AND RESPONSIBILITIES
It is a role of the registered nurse (RN), nurse practitioner (NP) and midwife, eligible midwife and in limited situations, enrolled nurse (EN), to administer medication in accordance with legislative requirements. All nurses and midwives must undertake the National Inpatient Medication Chart (NIMC) and Medication Safety Course. This is a once only assessment via WACHS Learning and Development (L&D) unit unless medication errors occur requiring individual performance review. 4.1 Registered Nurse and Midwife
4.1.1 The RN and midwife are responsible for medication administration which also includes the medication history (see section 5.3).
4.1.2 A RN or midwife may administer unrestricted Schedule 2, 3 or 4 medications including oral, topical, vaginal, rectal, sublingual, buccal, intranasal, transdermal and oxygen therapy alone.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 6 of 50
4.1.3 Vaccinations may be administered by some RNs and Midwives. Refer to section 14
4.1.4 A RN or midwife may administer intramuscular, intravenous, subcutaneous injections medications alone when checked by a second nurse, medical officer or pharmacist.
4.1.5 A first year RN must administer intravenous drugs under the supervision of a more senior RN. This requirement ceases once the 1st year RN has been assessed as competent in intravenous medication administration.
4.1.6 In some circumstances, e.g. Multipurpose sites (MPS), community clinic, small hospital or nursing post, the ability to check the medication with a second nurse may not always be possible. In this instance the second checker is not required.
4.1.7 Schedule 8 medications when checked by an RN or midwife must be administered by two nurses, one of whom must be a RN or midwife. Refer to section 18.
4.1.8 The RN or midwife may administer Schedule 8 IV narcotic bolus and infusion when deemed competent in the administration. Refer sections 18, 19.
4.1.9 A RN working in a designated remote area nursing post: i. must attend training and assessment and maintain competency in
Pharmacotherapeutics for Remote Area Nurses (refer to learning and development site (or provide evidence of recognition prior learning in pharmacotheraputics e.g. successful completion of pharmacotherapeutics Nurse Practitioner units of study) to administer medications in accordance with Appendix 5 Standing Orders A
ii. in accordance with the Poisons Reg 36(1)(c)(i), may provide up to three days' supply of a Schedule 4 medication.
iii. may supply S2 and S3 medications refer to WA Health, Operational Instruction OP 0302/93 Supply of 2nd Schedule and 3rd Schedule Medications from Remote Area Nursing Posts to guide best practice for designated remote area nursing posts.
4.1.10 The only medications that may be charted by a RN or midwife are those designated as:
i. ‘Nurse initiated’ as described in this policy - see Appendix 3 ii. ‘Verbal orders’ as described in this policy - sections 8
4.2 Direct Entry Midwife (who is not a registered nurse)
4.2.1 The Poisons Regulations allow a midwife (who is not an RN) to
administer a Schedule 4 medicine on the prescription of a medical practitioner, NP or dentist. However midwives need to work within their scope of practice and only administer medications to women and neonates during the peri partum period. Medication administration in any other circumstance must be under direct supervision of a RN.
4.2.2 A midwife (who is not an RN) is not permitted to supply a patient with an ‘approved starter pack’ (Poisons Regulations (WA) 1965 Regulation 36AA), or psychiatric starter pack.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 7 of 50
4.3 Enrolled Nurse
4.3.1 All ENs are expected to have relevant medication administration competence. Those ENs who have not yet completed the required units
will have the following notation against their name on the Nursing and Midwifery Board of Australia Register ‘Does not hold a Board approved qualification in medication administration’.
4.3.2 The EN can administer medications alone within their scope of practice including oral, transdermal, topical, ear, eye, inhaled, nebulised, vaginal, rectal, sublingual, buccal, and intranasal unrestricted Schedule 2, 3 or 4 medications.
4.3.3 The EN can administer intramuscular, subcutaneous injections when these have been checked by a second person who must be an RN, medical officer or pharmacist.
4.3.4 An EN may administer medications to paediatric patients, but the medications must be checked by an RN, and must be checked at the bedside by both parties.
4.3.5 To administer intravenous therapy and medications, the EN must complete an intravenous (IV) medication training and competency program. The EN may only administer intravenous therapy via peripheral devices, excluding Peripherally Inserted Central Catheters and Central Venous Lines.
4.3.6 An EN without an IV medication competency may be allocated to patients who have IV infusions, but will not be responsible for the IV therapy delivery.
4.3.7 An EN with an IV medication competency (refer to 4.3.5) may administer IV therapy, including setting the rate; add to a mini bag and administer a bolus dose
4.3.8 An EN working within their scope of practice in a renal dialysis unit may administer intravenous therapy, under RN supervision.
4.3.9 An EN may take care of a patient receiving IV narcotic infusion, cytotoxic or epidural therapies however these therapies are the exclusive responsibility of a RN or midwife.
4.3.10 An EN may not care for unstable patients who are receiving high risk drug infusions with low therapeutic index that are dependent on monitored drug levels or dose adjusted dependant on frequent patient observations.
4.3.11 An EN may check Schedule 8 medication but cannot administer a Schedule 8 medication. The exception being an EN may administer a dosage administration aid containing a Schedule 8.
4.3.12 Under no circumstances is the EN to hold the Schedule 8 keys.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 8 of 50
4.4 Enrolled Nursing or Registered Nursing or Midwifery Students
A student EN, registered nursing or midwifery student may check and administer medications under the supervision of an RN or midwife, provided the student is directly supervised at all times by an RN or midwife. 4.4.1 A student can sign the medication chart; however this must be
countersigned by the supervising RN or midwife. 4.4.2 The student must have completed the relevant theoretical preparation. 4.4.3 Where there is a requirement for two nurses in medication
administration, the student cannot be one of those two unless the second nurse is only required to check the medication.
4.4.4 A registered nursing student is able to administer Schedule 8 medication and complete the Schedule 8 register but this must be countersigned by the supervising RN or midwife and second RN or midwife who is the checker.
4.4.5 Student midwives who are RNs can administer drugs as per RNs. Only administration of maternity specific drugs and epidurals by a student midwife require direct supervision of a midwife.
4.4.6 An EN student may be the third checker of a Schedule 8 medication and complete the Schedule 8 register but cannot administer a Schedule 8 medication.
4.4.7 An EN student cannot be supervised by another EN 4.5 Unregulated Health Worker
An Unregulated Health Worker (UHW) includes: patient care assistant (PCA); assistant in nursing (AIN); Home and Community Care (HACC) support worker and an aboriginal health care worker (AHW). 4.5.1 Unregulated health workers are individually accountable for their own
actions and are accountable for undertaking activities as delegated by an RN or midwife and their employer for delegated actions (ANMC 2007).
4.5.2 The UHW is required to provide evidence of completion of a Care Worker Medication Administration Competency Package to their employer from an approved registered training organisation or from an approved WACHS assessor (e.g. HACC Community West Inc.), prior to undertaking medication administration.
4.5.3 A delegated UHW who has been deemed competent can assist with medication support and administration as per the example HACC Medication Support and Administration Policy (read “this organisation = WACHS”), including documentation e.g. medication signing sheet.
4.5.4 If medication prompting support is being provided the client/resident/patient retains all responsibility for their medications.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 9 of 50
4.5.5 If a dose administration aid includes Schedule S4R or S8 the contents
of the aid may be given by the UHW (see section 18.3 In Hostel and Aged Care Facility).
4.5.6 In a community setting the UHW is supported by the example HACC Medication Support and Administration Policy (3.5.3) to provide medication support (see section 3 for definition) as delegated. Medications are only given and signed for: i. if there is a client assessment, and ii. consent is signed by the client and HACC provider on a WACHS
form refer to Aged Care Residential Manual - RC 26 Ability to Self-Medicate (page 298), and
iii. a medication plan is documented. 4.5.7 The UHWs who provide care to Department of Veterans Affairs Clients
(DVA) community care clients are not permitted to manage or administer prescribed medications as per a care plan, as outlined in the Community Nursing Guidelines 2010 (Section 6.3.2.4 page 34).
5. PRINCIPLES OF MEDICATION ADMINISTRATION
5.1 Administration Standards
The following standards apply to the administration of medication:
5.1.1 Prior to administering any medication a RN, midwife, NP or EN must: i. know the legislation relating to medication administration ii. know the medication, its therapeutic purpose, usual dose,
frequency and route of administration, specific precautions, contraindications, monitor for side effects and adverse reactions
iii. know the correct storage conditions of medications iv. ensure the medication order is legible, complete, correct and has a
legible signature of the medical practitioner. The RN, midwife and EN must not, under any circumstances amend a prescription written by a medical practitioner or nurse practitioner. However the RN or midwife may change the administration time on the medication chart.
v. adhere to the following six (6) principles of medication administration: 1. Right medication 2. Right individual (in accordance with WA Health, Operational
Directive OD 0312/10 Western Australian Patient Identification Policy
3. Right dose 4. Right time 5. Right route 6. Right documentation
vi. consult appropriate resources and references. (refer to section 1)
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 10 of 50
vii. Refer to the Australian Commission on Safety and Quality in Health
Care Recommendations for Terminology, Abbreviations and Symbols used in Medicines Documentation.
5.1.2 All medication including unscheduled medicines such as vitamins and
complementary medicines, Schedules 2, 3, 4 and 8, and oxygen must be written on an approved WACHS 170 series Medication Chart.
5.1.3 A RN, midwife and EN can only administer medication to a patient in a hospital if the medication is authorised in writing on the approved WACHS MR170 series Medication Chart or a WACHS approved electronic prescribing system. The documentation exceptions are aged care and MPS where an alternative approved chart may be used e.g. Webster Pak ® signing sheet.
5.1.4 Assess for efficacy of the medication and document in patient notes. 5.1.5 Report to the prescriber any side effects or adverse reactions
experienced by the patient and document the episode and nursing actions in the patient's medical record (Refer to section 7.1.3).
5.1.6 Administration of medications involving routes such as peripherally inserted central catheter or infusion port, intrathecal, epidural or regional blocks (e.g. femoral nerve block) is an advanced practice role (Refer to section 17.7). Administration of medications via these routes must be subject to providing demonstrated evidence of attainment of WACHS endorsed self-directed learning packages and/or competencies.
5.1.7 Administration of oral, enteral or nebuliser solutions - use of oral syringes. Refer to WA Health High Risk Medication Policy, WACHS High Risk Medications Procedure and section 16
5.2 National Inpatient Medication Charts
Use of the National Inpatient Medication Charts are a national standard for both prescribers and staff to enable safer prescribing and administration of medications. Guidelines for use of the National In-patient Medication Charts in WA are provided. In Western Australia these currently include WACHS medical record 170 series charts for: short and long stay adult and paediatric charts; anticoagulant medication and residential aged care. 5.2.1 Medication charts due to expire in the following 48 hours, are to be
brought to the medical practitioner’s attention by nursing staff caring for the patient to enable revision and rewriting.
5.2.2 All anticoagulant therapy is to be administered via the WACHS Anticoagulant Medication Chart (Refer to section 17).
5.3 Medication History and Management Plan
Nurses and midwives in partnership with the hospital pharmacists and/or medical practitioners complete a medication history, to inform care planning and documentation.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 11 of 50
Nurses and midwives are guided by the Medication Management Plan principles outlined in Pharmaceutical Benefit Scheme Reform in accordance with the Australian Pharmaceutical Advisory Council Guidelines for Continuity of Medication Management. Where a pharmacist is not available on site, the guidelines require nursing staff to ensure medication reconciliation occurs, and patients are charted for correct medications on admission. Discharge medication information should be included in the patients discharge summary by the pharmacist or medical practitioner.
5.3.1 Document an accurate medication history for all inpatients by an
appropriately qualified professional, as soon as possible but within 24 hours of admission. Only use the front of a WACHS MR170 series Medication Chart or a Medication Management Plan (where available).
5.3.2 Medication history is the documentation of all medications (including over-the-counter medications and complementary therapies) that a patient is taking at the time of hospital admission or presentation and includes any recently ceased or changed medications.
5.3.3 On admission, check any known allergies or drug sensitivities and document previous adverse drug reactions and allergies. Ensure correct identification e.g. red wrist band, alert labels. Document any adverse drug reactions (ADR) that may arise during admission.
5.3.4 Ensure the patient and family/ carer understand why the medication has been prescribed.
5.4 Patient’s Self Medication 5.4.1 The medical practitioner is to document on the medication chart if the
patient can self-medicate. 5.4.2 If the medical practitioner has documented such, the patient is to be
advised by the EN, RN or midwife of the safety plan for the storage of medications at the bedside, such as the medications are to be kept on the person of the patient or stored in their bedside locked drawer, not in plain view of other persons.
5.4.3 The EN, RN or midwife is to confirm all self administration medication and document on the medication chart using the appropriate code.
5.4.4 Schedule 4Restricted and Schedule 8 medications must not be left with patient (refer to sections 18 and 20).
5.4.5 Legal responsibility remains with the hospital or facility for the correct administration of patient medication.
5.4.6 Nursing and midwifery staff need to exclude evidence of delirium or temporary confusional state in situations where patients are usually self-medicating such as in a residential setting e.g. low care hostel (For community aged care settings also refer to section 4.5.5).
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 12 of 50
5.5 Withholding Medication
Guidelines for use of the National In-patient Medication Charts in WA - Appendix A provides information on withholding medications. 5.5.1 A RN or midwife may withhold the administration of a medication if:
i. the order is not legible ii. there is some doubt about the medication order or dosage iii. it is not possible to identify the prescribing doctor iv. an identified side effect occurs or has occurred previously, or v. a change in the patient’s condition warrants doing so.
5.5.2 If the medication is withheld due to above, the RN or midwife must seek clarification of the order as soon as practicable, and must document this on the medication chart and patient progress notes.
5.5.3 When patients are fasting, it is the responsibility of the RN or midwife to check with the medical practitioner which medications should continue to be administered unless indicated on the medication chart.
5.6 Correct Documentation
Time-critical medicines (refer to section 3 Definitions) must not be delayed or administered early by more than 30 minutes. Non-time-critical medicines will depend on the frequency of dosing.
i. For medicines administered more frequently than daily but less frequently than four hourly – may be administered within 60 minutes of the scheduled time;
ii. For medicines administered daily or less frequently – may be administered within two (2) hours of the scheduled time.
5.6.1 The person who administers the medication must document the exact time of administration and sign the medication chart (e.g. medication due 0800 and given at 0830; the time of 0830 must be recorded and signed).
5.6.2 When two people have checked a medication, both are required to sign the medication chart after administration (see section 13 & 16 S4R and S8).
5.6.3 Where alternative routes (oral/ PR) or a dose range (e.g. 5 -10mg) are ordered, the route chosen and the dose given must also be documented on the MR170 series medication chart.
5.6.4 When PRN medications are given, the reason why they are given and the results obtained are to be documented in the patient progress notes.
5.6.5 If a medication is not given, the reason is to be documented on the medication chart and patient progress notes using only the codes supplied on the WACHS medication charts.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 13 of 50
5.7 Discharge, Transfer, or Non-admitted Patient Medication Planning
Discharge planning ensures medication or a prescription change to a medication is available in a timely manner on discharge and facilitates responsible supply of patient medications. 5.7.1 It may be necessary for the medical practitioner to dispense, where a
pharmacist or retail pharmacy is unavailable, sufficient medication on discharge until a discharge prescription can be filled. The medical practitioner is to make a written record of the medication dispensed at the time of supply. The medication is to be labelled in accordance with the Poisons Act 1964 and Poisons Regulations 1965.
5.7.2 A NP is authorised to prescribe and dispense a range of medication within their scope of practice, in accordance with Poisons Reg 40 (1) (aa).
5.7.3 Nurses and midwives are not authorised to “dispense” medications to a patient leaving the hospital. This does not include the administration of prescribed starter packs as described in section 10.
5.7.5 The supply of starter pack medication to non-admitted patients is to take place, when necessary, through the Emergency Department or a Designated Remote Area Nursing Post.
5.7.6 If the patient is transferred to another ward, their admission medications are to be transferred with them.
5.7.7 After discharge, any unclaimed medications are to be forwarded to the pharmacy department for disposal.
5.8 Fees and Charges for Medication
Medication and supply for inpatients and outpatients are in accordance with the following Department of Health Operational Directives:
i. WA Health Administrative Circular A 7652 Supply of Drugs and Medications.
ii. WA Health Operational Instruction 0280/93 Drug Supplies To Outpatients of Health Department Of Western Australia Government Non-Teaching Hospitals And Nursing Posts
5.9 Patient Education
5.9.1 Discharge education is to be documented in the patient’s health record
by the medical practitioner, RN, midwife or pharmacist providing discharge medication education. Ensure the patient/carer:
i. understands what the medications are for, how and when to administer them.
ii. receives Consumer Medication Information (CMI) sheets or other drug information leaflets as appropriate. (Refer to eMIMs online CMI sheets)
iii. have own medication brought to hospital, returned by a RN or midwife if indicated, on discharge, except S4R and S8 medications (refer to section 20 Schedule 8 and Schedule 4R).
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 14 of 50
5.9.2 The patient/carer must be given information on the storage, preparation,
measuring and administration techniques for medications that they will be administering at home.
5.9.3 If administration devices are required, instructions for use, cleaning or maintenance must be given.
6. MEDICATION ERRORS 6.1 All medication incidents and near misses must be reported immediately to the
medical practitioner and shift coordinator/ line manager. The patient is to be immediately assessed and monitored for any adverse effects of incidents or errors. Also refer to sections 7 and section 21 Evaluation.
6.2 An incident occurs when any of the following occur: i. there is a deviation from a documented standard (policy, procedure), ii. a medication is omitted and the appropriate code has not been used, as per
the medication chart codes, iii. a medication is not signed for iv. medications are not given within 30 minutes for time critical medications, or
two (2) hours for all others of the specified time, except where there is a planned change due to patient circumstances,
v. a medication is given on the wrong date, vi. an incorrect medication is administered, vii. an incorrect dose is administered, viii. the medication is given by the incorrect route, ix. a medication is administered to the wrong patient, x. an intravenous infusion is administered at the wrong rate, and/or xi. where an adverse reaction requires treatment or cessation of the drug.
6.3 The medication given and/ or adverse drug reaction must be properly
recorded in the patient’s health record. In the case of an adverse drug reaction, an appropriate Adverse Drug Reaction Alert card may be completed.
6.4 Documentation must be completed as soon as practicable and be reported via
the clinical incident management system (refer to section 21 Evaluation).
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 15 of 50
7. MEDICATION PRESCRIBERS
7.1 The governance of monitoring authorised prescribers (NSQHSS 4 Medication
Safety 4.3.2) is the responsibility of the regional medical and nurse directors.
7.1.1 Prescribing medications is the responsibility of health professionals who are endorsed to prescribe medications in line with their APHRA registration e.g. medical practitioners, nurse practitioners, There are also a limited number of nurse initiated medications schedule 2 and 3 medications that can be prescribed by any RN (See Appendices 3a and 3b and section 11) and remote area nurses (see section 4.1.9)
7.1.2 Eligible midwives may prescribe in accordance with the NMBA National Prescribing Formulary for Eligible Midwives with a scheduled medicines endorsement - NMBA Prescribing formulary for eligible midwives.
7.1.3 The clinician responsible for the patient is required to report adverse drug reactions in collaboration with the Regional Pharmacist to the Australian Government, Department of Health and Ageing, TGA, Adverse Drug Reactions Advisory Committee (ADRAC) in accordance with ADRAC requirements.
7.2 Labelling of medications other than starter packs
7.2.1 A medical practitioner, NP or a RN working at a remote area nursing post (section 4.1.9) is to label a supplied medication in accordance with Poisons Reg 21 in “English” with: i. the words “Keep out of reach of children” ii. the name and strength or amount of each poison in the preparation,
or the trade name and strength of the preparation (unless the trade name also uniquely identifies the strength, in which case only the trade name need be given)
iii. the name of the patient iv. date of supply, and a number identifying the prescription or supply
which corresponds to the patient’s records v. the name and address of the designated health site or remote area
nursing post, from which it is supplied vi. the directions for use vii. the total quantity contained, and viii. in an approved and appropriately safe container.
7.2.2 External use: where the medication is for human external use only, it must include the words “Not to be taken”.
7.2.3 Where a medication is included in Poisons Standard 2010, Part 2 Sub-paragraph 14(2) Appendix K of the Standard for the Uniform Scheduling of Medicines and Poisons (SUSMP), in accordance with Poison Reg 21A, the package must bear the statement: “This medication may cause drowsiness. If affected do not drive a motor vehicle or operate machinery. Avoid alcohol.”
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 16 of 50
7.2.4 Plain Packaging
The Poisons Reg 19AA prohibits the use of envelopes, plastic bags, paper bags or cardboard boxes for supply of medication unless the medication is also strip packaged (in foil or in individually sealed amounts). The risk associated with supply of loose tablets in an envelope, bag or box is high. The use of a container with a name previously embossed or permanently marked is also prohibited (refer also to storage and transport section 20).
7.3 Registered Nurse’s Legal Responsibility 7.3.1 Should an RN be required to assist a medical practitioner in the
dispensing of a Schedule 4 or Schedule 8 medication to a non-admitted patient, the dispensed item is to be handed to the medical practitioner for supply by him/her to the patient or prepared under the direct visual supervision of the medical practitioner.
7.3.2 Nothing in the above precludes an RN from administering a medication to a non- admitted patient when acting under the direction of a medical practitioner.
8. VERBAL ORDERS
8.1 An RN (including a remote area nurse), midwife or NP may receive a
medication order for an inpatient or a non-admitted patient from a medical practitioner, NP or eligible midwife verbally, by telephone or other electronic means. The nurse who receives a ‘verbal order’ must:
i. confirm and record the identity of the prescriber ii. records the prescription in writing on the medication chart and repeat the
prescription back to the prescriber iii. second checker (RN, midwife, NP or EN, or pharmacist) confirms the
order with the prescriber. iv. both nurses must ensure the verbal order is recorded and signed on the
medication chart. v. exemption of second checker (see section 4.1.8).
8.2 The verbal order must be signed on the medication chart, or otherwise
confirmed in writing, within 24 hours by the prescriber. If the prescriber does not sign the original verbal order within a 24 hour period:
i. If order required beyond 24 hours must be reordered, or ii. In some instances where a health service may be covered utilising an on
call doctor in a single location or telehealth, telephone orders may be electronically transmitted via fax, email, or endorsed electronic system e.g. MMeX to the doctor’s location for signing and then faxed back for inclusion in the medical record in accordance with WA Health Information Circular IC 0179/14 Guidelines for the Transmission of Client Identifiable Health Information by Facsimile Machine.
iii. If electronic transmission occurs the hard copy document with the doctor’s original signature MUST be kept at the site from which the doctor authorised the medication order.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 17 of 50
iv. If the medication order is required to be continued beyond 24 hours it
must be reordered within the relevant section of the National Inpatient Medication Chart (NIMC)
9. DESIGNATED REMOTE AREA NURSING POST An RN working at a Designated Remote Area Nursing Post is authorised to supply a poison, not being a psychoactive poison in accordance with the Poisons Reg 36(1)(d):
i. Three (3) days medication supply, or ii. Where the poison is supplied in prepacked individual packs, one individual
standard pack iii. For the treatment of an acute medical condition in compliance with the
written standing orders of a medical practitioner which have been as approved by the CEO, or
iv. For the treatment of an acute medical condition in compliance with oral instructions of a medical practitioner for that particular patient.
10. APPROVED STARTER PACKS An RN at an approved health service (Appendix 1) as per Poisons Reg 36AA may give an approved starter pack (Appendix 2) to a non-admitted inpatient, if verbally instructed to do so by a medical practitioner or nurse practitioner, who need not be present at the health service. 10.1 Approved Starter Pack Supply
10.1.1 An approved starter pack is centrally prepared by WACHS Pharmacy and contains a medication supplied in a prepacked individual pack and does not exceed three days' worth of medication in accordance with Poisons Reg 36AA.
10.1.2 Within 72 hours of giving a starter pack instruction, a medical
practitioner or NP must provide to the health service a signed, written confirmation of the instruction including the following, (Poisons Reg 36AA) the: i. name of the medical practitioner or NP ii. name of the RN to whom the starter pack instruction was given iii. name of the patient iv. date and time when the instruction was given v. details of the approved starter pack vi. any relevant directions for use that were to be given to the patient,
and vii. any other information that the medical practitioner considers relevant.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 18 of 50
10.2 Before Giving an Approved Starter Pack 10.2.1 Before giving an approved starter pack to a patient, the RN must label it
with the patients name, date provided and name of prescribing medical practitioner or nurse practitioner.
i. keep the Supply Book for at least two years after the last entry is made, for accountable auditing and
ii. the name and address of the patient iii. the approved name and strength or amount of the poison or iv. if the brand name uniquely identifies the strength of the poison, that
brand name v. the date and time at which the approved starter pack is to be given
to the patient vi. the name of the medical practitioner vii. any directions for use given by the medical practitioner viii. a unique number identifying the entry in the Supply Book, and ix. the RN’s name and signature. x. document dispensing of starter pack in the patient’s MR5 or in
MR170 series medication chart. 10.3 Provision of a Psychiatric Starter Pack
Currently, there are no sites designated within WACHS for provision of psychiatric starter packs in accordance with the Poisons Regulations.
11. NURSE INITIATED NON PRESCRIPTION MEDICATIONS
11.1 An EN (under RN delegation), RN or midwife may administer a non-prescription
medication (Appendix 3 Nurse Initiated Medications). 11.1.1 The medication is recorded on the patient’s medication chart by an RN
or midwife in the adult nurse initiated medication section or the paediatric once only section.
11.1.2 The medical practitioner is advised as soon as possible (and a record made in the MR170 series medication chart.
11.1.3 If required on a regular basis, the medication is to be countersigned by the medical practitioner, and subsequently written up by the medical practitioner in the medication chart. (Refer Appendices 3a and 3b.)
11.2 If the patient requires two or more doses of these medications, the medical
practitioner is to be requested to review the patient. 11.3 Topical unscheduled products are not required to be individually listed in
Appendices 3a and 3b and may be given at the discretion of the RN. These products must be charted in the relevant section of the patient’s medication chart.
11.4 Supply of nurse initiated non-prescribed medication is subject to availability on
the regional formulary. 11.5 The WA Country Health Service supports the use of Nicotine Replacement
Therapy for inpatients. Refer to: Clinical Guidelines and Procedures for the Management of Nicotine Dependent Inpatients.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 19 of 50
12. NURSE INITIATED STI TREATMENT CODE
12.1 The WA Country Health Service nurses – STI and trachoma located at
Department of Health Structured Administration and Supply Arrangement website under CEO of Health SASA establishes the competencies which must be achieved and criteria to be met by a RN to administer single dose combination therapy (e.g. ZAP Pack) for chlamydia and gonorrhoea in accordance with the Poisons Regulations 1965.
12.2 A combination therapy pack may be administered for the treatment of chlamydia
and gonorrhoea in the Goldfields, Kimberley, Midwest and Pilbara regions and in accordance with the treatment indications and guidelines of the Silver Book and relevant recommendations in Silver Book Supplement. 12.2.1 A RN must only initiate treatment of adult clients and mature minors
aged fourteen (14) years or older, and 12.2.2 The ZAP Pack must be administered under direct observation of the
RN. The RN must not supply a ZAP Pack for an unsupervised client to self-administer.
13. GUIDELINES FOR USE OF OXYGEN
The WA Health, Operational Directive OD 0397/12 Use of Acute Oxygen Therapy in Western Australian Hospitals provide guidelines for the management of patients requiring acute oxygen therapy. 13.1 No patient should be denied oxygen therapy in an emergency. 13.2 Patients commenced on acute oxygen therapy should be assessed and
reviewed promptly, carefully and regularly as per the oxygen orders. 13.3 Once the patient is stable, oxygen therapy must be prescribed on a dedicated
oxygen prescription sticker by a doctor or NP and reviewed daily. Refer to the WACHS endorsed SMHS Respiratory Devices NPS or Princess Margaret Hospital (PMH), Oxygen Therapy, Section 7.2.1, 7.2.2 and 7.2.2.1, nursing standard of practice within the practice context and clinical equipment available for the WACHS sites.
14. VACCINATIONS/IMMUNISATIONS A WACHS RN fulfilling the requirements specified in the Vaccination Administration Code 2012 are authorised to administer vaccines in accordance with Regulation 37B of the Poisons Regulation 1965. 14.1 Vaccines are a Schedule 4 medication and can be administered by:
i. RN or midwife under the direction of a medical practitioner, or written prescription
ii. RN or midwife (e.g. community health nurses/ infection control nurses/ occupational health nurses) working within WACHS who have completed an accredited immunisation training program, as outlined in the Vaccination Administration Code 2012
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 20 of 50
14.2 Key areas of competence are outlined in 2012 Vaccination Administration
Code.
14.3 Vaccinations /immunisations may be administered as per WA Health, Operational Directive 0415/13 Guidelines for Department of Health Vaccination Programs – School and Community Health Immunisation.
14.4 Refer also to the WACHS endorsed Australian Immunisation Handbook.
15. COMPLEMENTARY MEDICINES
Complementary medicines may contain active substances. Administration of any complementary-type medicines must be authorised by the medical practitioner and accurately documented on the medication chart. Complementary therapies will not be supplied, but patients own medication may be administered if charted.
16. PRESCRIBING NUTRITIONAL SUPPLEMENTS Care is required when administering oral nutritional supplements. The same requirements for safer prescribing and administration of medicines apply to nutritional products. A separate order chart is required for oral nutrition supplements and enteral feeding products. Also refer to WA Health High Risk Medication Policy and WACHS High Risk Medications Procedure. Refer to section 5.1.7 Administration of oral, enteral or nebuliser solutions - use of oral syringes.
17. HIGH RISK MEDICATIONS
Medication safety alerts and notices are issued from the Australian Commission on Safety and Quality in Health Care website and WA Department of Health operational directives in response to reported incidents or for medicines with known high risks. Medication safety alerts advise action to prevent future adverse medicine events or to lessen the risk of such events occurring. High risk medicines include:
i. those with a low therapeutic index; and ii. the following categories (A PINCH): Anti-infective agents, Anti-psychotics,
Potassium, Insulin, Narcotics, Chemotherapy, Heparin and other anticoagulants. iii. those that present a high risk when administered by the wrong route or when
other systems error occur.
17.1 Anti-infective agents 17.1.1 Antibiotic selection
Antibiotic selection, dose and duration should follow the antimicrobial creed:
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 21 of 50
M. Microbiological Guides where possible (Therapeutic Guidelines Antibiotic current edition refer to section 1.)
I. Indications should be evidence based N. Narrowest spectrum D. Dosage appropriate for site and type of infection M. Minimize duration of therapy (see 17.1.2.1) E. Ensure monotherapy where possible.
17.1.2 Automatic Stop Order for Antibiotics An automatic stop-order may apply to the administration of intravenous, oral and topical antibiotics. 17.1.2.1 Wherever possible, a specific termination date is to be
written on the medication chart. If no specific date is given: i. an oral or topical antibiotic order has a seven (7) day
stop-order ii. an IV antibiotic order has a minimum third daily review
unless otherwise documented iii. if continuation required the prescription has to be re-
written if further administration is required 17.1.2.2 The prescriber is to be informed immediately prior to the
implementation of the automatic stop-order. If the antibiotic is to be continued, and the prescriber is unavailable to rewrite the prescription, the prescription should be recorded as an interim medication order
17.1.2.3 Where long term antibiotic administration is indicated, a specific endorsement to this effect is to appear on the medication chart, together with the date on which administration is to be reviewed.
17.2 Guidelines for Midazolam for Adult or Paediatric Sedation
Refer to WACHS specific adult and paediatric sedation procedures. Also, where appropriate, refer to the Sedation for Mental Health Patients Awaiting RFDS Transfer from Remote Regions Guideline and related documents in HealthPoint. 17.2.1 Intravenous Midazolam for adult sedation should only be used in
situations where there is: i. continuous cardiorespiratory monitoring, and ii. resuscitation equipment, and iii. availability of the specific antidote, and iv. registered nurses with the appropriate competencies, and v. a medical officer readily available per phone, in person or on the
Emergency Telehealth Service. 17.2.2 Paediatric patients prescribed intravenous Midazolam in anticipation
of a seizure require the above with the exception of continuous cardiorespiratory monitoring unless the patient is already sedated. Refer to PMH guidelines endorsed for use in WACHS for paediatric seizure management.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 22 of 50
17.3 Potassium Chloride Intravenous potassium chloride is to be stored, prescribed and administered in accordance with the Western Australian Guidelines for Use of Intravenous Potassium Chloride. Refer to WA Health High Risk Medication Policy and WACHS High Risk Medications Procedure.
A rapid potassium replacement/administration must only be administered in exceptional circumstances (i.e. resuscitation) under direct supervision or direct verbal prescription during a medical emergency by a senior medical consultant (FACEM, intensivist or paediatrician).
17.3.1 Paediatric administration of Molar potassium (10 mL ampoules of 10mmol of potassium chloride); rapid potassium replacement/ administration must only be prescribed and administered in exceptional circumstances under the direct supervision of the consultant. Refer to: PMH Pharmacy IV Potassium Chloride Policy.
17.4 Insulin
For all WACHS insulin guidelines refer to WACHS Ward Imprest Insulin Guideline; Insulin Infusion Guidelines and Insulin Infusion Order Chart (adults) MR157A.
17.5 Narcotics (opioids) For safe and appropriate pain management in WACHS sites consult medical staff, regional anaesthetist or Acute Pain Service. Also refer to the WACHS endorsed clinical practice policy: Emergency Care Acute Pain Management Manual. 17.5.1 Refer to Section 18 Schedule 8 17.5.2 Patient Controlled Analgesia. To ensure the prescription, administration
and monitoring of patients receiving intravenous patient controlled analgesia (with the main focus on opioids) is safe and appropriate refer
to OD 0416/13 Prescription and management of intravenous patient controlled analgesia.
17.5.3 Paediatric intermittent Morphine bolus protocol. Refer to the PMH Acute Pain Service Intermittent Morphine bolus protocol for infants greater than 6 months, children and adolescents.
17.6 Chemotherapy
17.6.1 Staff administering chemotherapy in WACHS utilise the endorsed Cancer Institute NSW - Standard Cancer Treatments - eviQ for use in clinical practice. Chemotherapy infusion rates must be verified by referring to the WACHS endorsed Cancer Institute NSW - Standard Cancer Treatments - eviQ for use in clinical practice (see also section 19.1.2).
17.6.2 Vincristine is neurotoxic and must only be administered intravenously. Sentinel events associated with the inadvertent intrathecal administration of vincristine result in a fatal outcome in 85% of cases with devastating neurological effects in the few survivors. Refer to WACHS Chemotherapy Administration - WACHS Clinical Practice Standard.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 23 of 50
17.7 Heparin and other anticoagulants
Refer to the WACHS endorsed NHMRC Prevention of Venous Thromboembolism Guidelines which contains the VTE Prevention Guideline and Clinician Summary and WACHS MR170C Anticoagulation Medication Chart.
17.8 Systems
This includes extra precautions for reducing oral medication wrong route or use of infusion pumps (refer to section 19). 17.8.1 Intrathecal Medication The administration of medication via the intrathecal route is considered
an advanced practice skill to be undertaken only by an intrathecal qualified RN. Refer to WACHS Chemotherapy Administration - WACHS Clinical Practice Standard
17.8.2 Epidural Therapy Administration of medications via the epidural route is considered an
advanced practice skill to be undertaken only by a WACHS certified competent RN or midwife.
17.8.3 Medication Restrictions to Nurse Administered IV Bolus Treatment An RN or midwife may prepare and administer a bolus IV medication,
in accordance with the prescriber’s instructions (including initial doses) - with the exceptions of the following groups of medications listed below, unless under the direct supervision of a medical practitioner, or direct verbal prescription by a medical practitioner during a medical emergency.
A patient is to be on cardiac monitor for both the administration of
Inotropes and Cardioactive drugs with a defibrillator in close proximity.
Medication Group
Examples (NOT to be administered by a nurse as an IV bolus)
Inotropes Dopamine, dobutamine, adrenaline, noradrenaline Cardioactive agents
Beta blockers, phenytoin, adenosine, verapamil, flecainide, digoxin, amiodarone
Anaesthetic agents Propofol, ketamine,
Paralysing agents (only applies to paediatric patients)
This list is not exhaustive and other agents are potentially dangerous in paediatric situations. Refer to section 1 links. Also PMH Paediatric Nursing Practice Manual section 2.1 Prescribing and Administering Medications
17.8.4 Infusion Pumps Refer to section 19
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 24 of 50
18. RECORDABLE DRUGS INCLUDING CONTROLLED DRUGS / DRUGS OF ADDICTION
18.1 Schedule 4 Restricted Medications The Operational Directive OD 0528/14 Storage and recording of Restricted Schedule 4 (S4R) medicines provides guidance for the management of Schedule 4 restricted (S4R) medicines. Also refer to WACHS specific procedure for Requisitioning and Receipt of Schedule S4R and 8 Medications and Ordering of Pharmacy Imprest Supplies Procedure. Some S4R medications are open to abuse, such as benzodiazepines and tramadol, and the traditional storage and record keeping requirements for a Schedule 4 medicine are inadequate to provide the level of accountability required within the public health system.
18.1.2 Recording of Schedule 4 Restricted Medication All transactions of S4R medications are to be recorded in the respective
drugs register or software approved by the hospital or Chief Pharmacist.
18.1.2.1 Administration of a S4R medicine requires one nurse and a single signature in the register. (Department of Health WA, 2014, Operational Directive OD 0528/14 Storage and recording of Restricted Schedule 4 (S4R) medicines. (see section 4) However, some regions may have a local site procedure which requires two nurses to check and sign the register.
18.1.2.2 A minimum daily stock check of each item is required (OD 0528/14) with names and signatures of two people or more frequently if instructed by a local site procedure. Some regions also require two nurses to check with two signatures in the register). The exception is single nursing post if the staff member has not changed where S4Rs will be checked weekly. Checks will also occur when change of staff occurs as part of the handover process. Refer to WACHS specific procedure for Requisitioning and Receipt of Schedule S4R and 8 Medications and Ordering of Pharmacy Imprest Supplies Procedure.
18.1.2.3 Exemption to second checker refer to 4.1.8.
18.2 Schedule 8 Medications
18.2.1 Only a medical practitioner, nurse practitioner or dentist can prescribe/order a Schedule 8 (S8) medication (refer to section 7).
18.2.2 A medical practitioner, pharmacist, dentist, RN, midwife or NP (see section 4) can administer a S8 medication on a prescription in accordance with Poisons Reg 42.
18.2.3 Intravenous Schedule 8 Medication. Refer to section 19 Intravenous Infusion and Intravenous Additive and Bolus Dose.
18.2.4 All patients presenting for emergencies who require a S8 medication are to be examined by a medical practitioner (in person or via Telehealth); a nurse practitioner (in person only); or admitted on the instruction of a medical practitioner as an inpatient and examined as soon as practicable (not more than 24 hours) Refer to OD 0141/08 - Code of practice for the handling of Schedule 8 medicines (drugs of addiction) in hospitals and nursing posts, and OD 0142/08 - Administration of Schedule 8 Medicines to Patients Attending for Emergencies. Refer also to section 8 Verbal Orders.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 25 of 50
18.2.5 Ongoing prescription for a Schedule 8 medicine within the ED In hospitals without on-site medical staff and where a medical
practitioner, practising at the hospital, has decided that a patient is to receive an ongoing prescription for a S8 medicine within the ED, then this must have prior approval of the Regional Medical Director, and this plan must be reviewed every 12 months by the medical practitioner or WACHS medical health service provider Department of Health WA, 2008, Operational Directive OD 0142/08 - Administration of Schedule 8 Medicines to Patients Attending for Emergencies.
18.2.6 Dispensing of Schedule 8 medication to a non-admitted patient This may only be undertaken by a medical practitioner. Only the amount
of medication required to treat the patient until a community pharmacy re-opens is to be provided. The medical practitioner is to make a written record of the medication dispensed at the time of supply. These must be labelled in accordance with the Poison Act and Regulations and be dispensed in an approved container. Details of Schedule 8 medications dispensed to patients must be reported to the Pharmaceutical Services Branch of WA Health Department.
18.2.7 Recording of a Schedule 8 Medication
18.2.7.1 An RN or midwife must record each transaction involving a drug
of addiction in the register in accordance with the Poisons Reg 44 (3) as per the requirements of the approved S8 register HA14.
18.2.7.2 In accordance with Poisons Reg 44B (6), an authorised person (see definitions), where a pharmacist is not available may correct an error in a register – if on paper, by making a marginal or foot note and initialling and dating the note.
18.2.7.3 An inventory of drugs of addiction held in stock must be made in accordance with the Poisons Reg 45 as follows:
i. When about to relinquish control of drugs of addiction, or ii. Where a health care facility has an authorised person
present 24/7 a minimum of one full inventory is completed every 24 hours, or
iii. By any person who assumes control (see definitions) of drugs of addiction, and the result of that inventory is to be recorded in the Register.
18.3 Administering Schedule 4 Restricted or Schedule 8 medications from
dose administration aids in hostel and aged care facilities.
18.3.1 The resident’s medication aid signing sheet (provided by the packing pharmacist) must be signed by the person providing medication support i.e. UHW (refer to section 4.5)
18.3.2 All dose administration aids containing S4R or S8 medications need to meet auditable accountability requirements. They must be securely stored, balance recorded and disposed of in accordance with the usual storage / recording / disposal requirements for S4R or S8 medications.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 26 of 50
The auditing requirements include: i. where medication support is provided by an UHW only, a site
procedure exemption may be required from OD 0528/09 and OD 0141, respectively, from checking the S4R or S8 when contained in an individual patient’s dose administration aid.
ii. the UHW providing medication support must report any inappropriate breach of integrity of the medication administration aid. Refer to section 20 Reporting of Medication Stock Discrepancies.
18.4 Patient Discharge and Schedule 8 Medication
Dispensed S8 discharge medications not given to the patient on discharge can be collected by a person nominated by the patient or sent by courier at the discretion of the pharmacist or senior nurse on duty. Medications must be placed in a plain, unmarked packaging such as a brown paper bag for transport in accordance with this policy (see Packaging section 7.2.4).
18.5 Storage, transfer or disposal of medication refer to section 20
19. INTRAVENOUS (IV) ADMINISTRATION
19.1 Intravenous therapy and infusion and bolus medication administration
19.1.1 A valid prescription is required for intravenous (IV) therapy, infusions and bolus medications. A valid prescription contains the following: i. name of drug ii. dosage iii. rate of administration iv. any diluent volume v. frequency of dosage, and vi. method of administration.
19.1.2 It must be ordered by the medical practitioner and charted on: i. The Intravenous Fluid Chart, including infusion rates. Refer to:
Appendix 6 Calculating Rate of Flow for IV Infusions; ii. Intravenous Additives section of WACHS 170 series medication
chart, or iii. A specific chemotherapy order chart. (refer to section 17.6)
19.1.3 Intravenous therapy, infusions and bolus medications are to be checked at the bedside by two (2) nurses, one of whom must be an RN or midwife, except in the case of section 4.1.8. It is the responsibility of the second nurse checker, to adhere to the following:
i. Observe the written order ii. Observe the preparation of the drug iii. Identify the patient at the bedside with the person administering drug iv. Check known allergies prior to administration of medication v. Check and confirm the rate / dose vi. Observe the initiation of the drug administration, and vii. Write signature, initial and document on the WACHS Series 170
medication chart and/or Fluid Therapy Order Chart.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 27 of 50
19.1.4 Where a medication is administered via an IV infusion, the RN or midwife is to ensure an additive label is completed and attached to the infusion bag, syringe or pump. The label must be completed and signed by two nurses, one of whom is an RN or midwife. (refer to section 19.5 labelling of intravenous medications)
19.1.5 Intravenous S8 infusions may be administered by an RN, midwife or NP. This must be via a lockable infusion pump or syringe driver (refer also to PCA OD). The RN or midwife must monitor and document on the observation and response chart throughout the administration of the infusion and escalate as per the early recognition and response to clinical deterioration site escalation process.
19.1.6 The use of a burette is to prevent accidental rapid infusion of large fluid/ drug volumes. All IV infusions must be connected to a burette with the exception of the following:
i. Those going through an infusion pump ii. Non additive intravenous fluids with a volume less than 500mL
(adult only). iii. Blood products. iv. Resuscitation fluids.
19.1.6.1 Paediatric IV fluid administration 19.1.6.1.1 Every patient under the age of 16 years receiving
(ongoing) IV therapy must have an infusion pump, if a pump is not available i.e. in operating room/ recovery area a burette must be used. Refer also to IV pump section 19.4
19.1.6.1.2 For safety reasons, all children 12 years and under must have a burette, where the duration of IV therapy is greater than two hours irrespective of whether antibiotics are pushed or infused via the B line.
19.1.6.1.3 Babies under 18 months of age must NOT have antibiotics infused via the burette (due to excessive fluid volume). Alternative options are either: i. use the ‘B’ line. ii. ‘push’ the drug manually if this is permissible. or iii. use a syringe pump
19.1.7 All IV therapy, including those with additives (if prepared immediately before use) must be used within 24 hours of commencement, or changed.
19.1.8 Specialised medication guidelines* for intravenous infusion, guidelines and checklists include (but are not limited to):
i. Infliximab Guideline and Pre-Infusion Checklist MR 173a ii. Natalizumab Guideline and Pre-Infusion Checklist MR 173b iii. Iron Polymaltose Guideline and Pre-Infusion Checklist MR173c iv. Phosphate Guideline v. Rituximab Guideline and Pre-Infusion Checklist MR173d vi. Nurse Compounding of Antibiotics in Elastomeric Devices
Guideline
* (use search option in HealthPoint using the term ‘specialised medication’ for new guidelines)
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 28 of 50
19.2 IV Flushes
19.2.1 Sodium Chloride 0.9% Injection for IV flush maybe given without prescription to maintain venous access patency (minimum once in 24 hours) and flushing, prior to and post prescribed medication. Consider compatible diluents refer to Australian Injectable Drug Handbook. Refer to RPH PIVC CPS
19.2.2 Volume of Sodium Chloride 0.9% Injection for adult patients 5 - 30mL. 19.2.3 Volume for paediatric patients, Sodium Chloride 0.9% Injection refer to
weight related volumes in the Guide for flush solutions and volumes in the PMH Nursing Practice Manual section 2.3.8 (see link above).
19.2.4 The RN is to ensure all IV cannulae are not flushed using any residual medication in order to avoid an adverse reaction.
19.3 Intravenous Additives and Bolus Dose
19.3.1 Only a RN or midwife may administer the first dose of IV medication
provided they operate within their individual scope of practice and ensure: i. that there is a clear process for the Early Recognition and
Response to Clinical Deterioration site clinical escalation process should an emergency occur
ii. they confirm that the patient is not allergic to the medication iii. they access information regarding the effects, side effects,
precautions, contraindications and the required patient monitoring/care specific to the medication is readily available refer to section 1
iv. is aware of the anaphylaxis flowchart Appendix 7 v. The medical practitioner prescribing the medication is aware the
medication is about to be given and is available at the hospital to respond should an emergency situation arise, or the Early Recognition and Response to Clinical Deterioration site clinical escalation process is initiated to contact of the medical practitioner in the event of an emergency
vi. Refer also to sections 17.2 Midazolam for sedation and 17.8 re bolus high risk drugs.
19.3.2 Allergic and anaphylactic reactions may occur at the second or third
dose of antibiotic administration and the nurse must always remain vigilant when monitoring the patient.
19.3.3 Bolus medication doses are only to be introduced into an IV line or
burette containing other medications when the line is flushed with compatible IV fluid before and after the administration of the bolus dose, unless specific compatibility information on the combination is available or provided by the pharmacy department. Refer also to section 19.1.6.1 for paediatric considerations.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 29 of 50
19.3.4 Provided a valid prescription exists, a RN or midwife may add any
prescribed therapeutic substance to a mini bag including the first dose with the exceptions of medications that may be considered to pose an occupational risk these include but are not limited to: Asparaginase; Azathioprine; Ganciclovir; cytotoxic drugs; targeted therapies including but not limited to monoclonal antibodies, kinase inhibitors and anti-angiogenesis agents - unless a risk assessment has been undertaken on the specified medication and there is a WACHS Specialised Medication guideline published.
19.3.5 The therapeutic substance must be prepared immediately prior to use.
19.4 Infusion Pump Safety Information
The Hospira Plum A+ infusion pump is a volumetric delivery device that is designed to ensure accurate and controlled administration of intravenous fluids, additives and medications. This pump is used across all of WA Health and must be operated as per system operating manual for Hospira Plum A+ 19.4.1 It is the nurse's responsibility to check the rate of infusion and to ensure
that the pump is working efficiently at all times. Refer also to the WACHS clinically endorsed policy SMHS Plum A + Volumetric Pump Nursing Practice Standard in addition follow the specific paediatric information regarding the B line in section 19.4.4 below.
19.4.2 Confirmation of drug / fluid compatibility, concentration, delivery rates
and volumes are suitable for piggyback or concurrent administration must be undertaken before administration.
19.4.3 All infusions of drugs are to be administered directly after reconstitution
and connection. The delay function of the pump must not be used. 19.4.4 Paediatric IV infusions use of the B line The Plum Manual states a 3ml syringe is the smallest that can be used
on the Plum A+ pump. However the small syringe will increase resistance when drawing fluid into the cassette generating an occlusion alarm. Therefore the manufacturer suggests using a 10mL syringe to deliver small doses such as 3mL - no accuracy will be lost and occlusion alarms may be prevented.
The clave port should always be flushed following delivery of drug through the B line, particularly if a small volume has been programmed. This will clear the Clave and ensure that no sediment builds up. You could leave the delivery syringe on when VTBI complete, back prime with 1mL then deliver it to clear line.
Refer also to section 19.1.6.1 for paediatric considerations.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 30 of 50
19.4.5 Pressure Settings Check the distal pressure setting each time an infusion is commenced, if required the limit can be changed manually. Note: The pump defaults to medium (258 mmHg) when it is switched on. If required, the distal pressure limit can be changed manually. The formula to determine distal pressure limit is M.A.P x 3. e.g. MAP = 80 x 3 = 240 mmHg.
i. paediatrics, limit is to be reduced to 90 mmHg (except some PICC lines which require higher pressures.
ii. neonates, the limit is usually 60mm/Hg 19.5 Labelling, Changing Infusions and Intravenous Lines
19.5.1 In the case of infusions - an Intravenous Additive Label must be
completed and attached to the mini bag/ burette/syringe 19.5.2 When changing infusions and IV lines the following applies:
i. IV infusion bags and syringes are to be changed every 24 hours. ii. IV fluid bags must not be taken down and reused once insertion
port has been punctured. iii. IV fluid bags must be discarded if the bag integrity is breached, i.e.
the bag is punctured or leaking. iv. Continuous IV lines are to have a completed IV change sticker
attached to the line and are to be changed every 72 hours. v. Intermittent IV lines are to have a completed IV change sticker
attached to the line and are to be changed every 24 hours, and vi. Time and date of the change is to be recorded on the label and
signed when completed on the nursing care plan. vii. IV fluids in warming cabinets to remain in outer packaging to be
labelled with a date timeframe of two (2) weeks, and discarded if not used after the two week timeframe.
19.5.3 Minimum labelling requirements are outlined in OD 385/12 Updated:
national recommendations for user-applied labelling of injectable medicines, fluids and lines
20. STORAGE OF MEDICATIONS
20.1 Bedside Storage When medications are stored and administered at the bedside, the storage unit must be locked at all times and key/code or swipe card held by a RN, midwife, EN or NP.
20.1.1 Two nurses (exception section 4.1.8), one of whom must be a RN, midwife or EN, must check the medications to be placed in the medication drawer. The practice of double checking placement in the drawer against the WACHS series 170 medication chart on admission or stock replacement is a requirement to avoid human error in medication incidents.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 31 of 50
20.1.2 Blister strips may be taken out of the packet and placed in the patient’s medication drawer, but the strip is not to be cut. Identification of the drug name, strength, batch number and expiry date are to be retained.
20.1.3 Medication drawers are to be emptied on discharge or transfer of the
patient. 20.1.4 Bedside medication drawers are for medications only. Other items e.g.
watch and other valuables are not to be stored in bedside patient medication drawers.
20.2 Storage of Patient’s Own Medication
20.2.1 These medications must not be used by the patient while in hospital, unless the medication is unavailable from the pharmacy.
20.2.2 Staff are to encourage family/ carer to take medications home after
medication reconciliation has occurred. (refer to section 5) 20.2.3 The EN, RN or midwife must document in the patient medical record or
medication chart the location of a patient’s medication - on admission and discharge, including any medications taken home by carer.
20.2.4 Patient’s own S4R or S8 medication storage: Dispensed controlled drugs must be separated from the remainder of the
discharge drugs and stored in the controlled drugs locked cupboard or safe. A note is to identify the presence of dispensed controlled drugs.
20.2.4.1 Any S4R or S8 medications are to be stored in the locked S4R
or S8 controlled drug cupboard/safe in a tamper proof bag and documented in the Register of Drugs of Addiction. i. The tamper proof bag contents should be recorded and then
stored in the safe. Only the seal and bag number need to be checked each safe check after this.
ii. If tamper proof bags are not available then each drug needs to be recorded on a separate page in the register of Drugs of Addiction and checked during the ward checking regime. (refer to section 18.2.7.3)
20.2.5 On discharge, two (2) persons check dispensed S4R or S8 medications
(one of which must be an RN) returned to the patient, and documented in the Register of Drugs of Addiction. Except in the case of a single RN site (refer to section 4.1.7)
20.3 Storage of controlled drugs
20.3.1 Storage of S4R and S8 medicines are to be stored in separate cupboards,
securely attached to a wall or floor in a secure storage area not accessible to the public. (OD0528/14)
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 32 of 50
20.4 Keys and Access to Controlled Drug Keys
20.4.1 Keys/codes are required to ensure locks to the S4R and S8 medication
cupboards are keyed separately and key/code is to be kept on the person of the nurse in charge, or their delegate who may be an RN or midwife. (OD0528/14)
20.4.2 The S4R and S8 keys/codes are to be kept on separate key rings
(OD0528/14)
20.4.4 In outpatient areas with after hour storage, controlled drugs keys are to remain in the control of an RN or pharmacist e.g. a key safe.
20.4.5 The receipt of a S4R or S8 medication (including any patient's own
medicines) is to be signed by two people (except section 4.1.8) in accordance with local policy.
20.5 Transfer of controlled drug keys
20.5.1 In sites where there is not a RN on duty 24 hours per day, 7 days per
week, the key to the drug safe must at all times remain under the control of an authorised person (see definitions). The RN may retain possession of the keys while off duty.
20.5.2 If a spare key is available this is to be held by the Regional Pharmacist. 20.5.3 Under no circumstances may the key be left with unauthorised persons
such as police or staff of another agency. If the RN is leaving the area and it is necessary to transfer the key to another person, arrangements must be made to transfer the key to the regional pharmacist. If this is not possible, the key is to be transferred to a senior nurse at another WACHS facility, provided that the regional pharmacist is aware and approves of the arrangement.
20.5.4 The Poisons Regulations require that a stocktake is taken when control of
the key is transferred. Ideally, the stocktake is to be conducted jointly by the two parties involved. Where this is not possible because transfer of the key occurs at a location removed from the drug safe: i. the nurse relinquishing control is to conduct a stocktake, record the
results in the drug register, and the balances on hand at the time of checking, and,
ii. the nurse accepting control must conduct a stock control using the drug register on arrival on site.
iii. any discrepancies discovered must be reported. Refer to section 20.8
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 33 of 50
20.6 Transfer of recordable medication including Controlled Drugs
20.6.1 Movement of recordable stock between hospital wards or between the pharmacy and wards on the same site is to be documented in the Register as well as in a transaction record, such as the Requisition for Drugs of Addiction Form, with the supplier and receiver both signing the requisition form and the receiving register.
20.6.2 Transfer of recordable medications from one site to another
i. Only in urgent situations may recordable medications be sought from another site outside of working hours. Recordable medications may only be supplied with the approval of both the requesting and receiving site nurse managers.
ii. Must be requested on an appropriate requisition form which has been appropriately authorized, and the details of the transaction must be recorded in the drug register of both the requesting and receiving site.
iii. The regional pharmacy must be faxed a copy of this requisition to alert the pharmacists to the transaction.
iv. It is the responsibility of the lending site to replace any stock transferred via a faxed requisition to the Regional Pharmacy during working hours.
20.6.3 If a recordable medication is to be obtained from another ward, a
requisition must be completed. i. The requisition, the medication chart and Register must be taken to
the ward where the medication is being transferred from. ii. The acquired recordable medication is recorded as "transferred" on
both registers. The requisition number is recorded under “req. no” and amount issued is recorded in the “amount issued from stock” column in the ward the stock is removed from. The date, amount and requisition number are recorded in the “received” columns in the receiving wards book.
iii. The RN or midwife removing the stock must accompany the nurse receiving the stock to the receiving ward and confirm the balance is correct.
iv. The recordable medication can then be checked and administered in the usual way.
20.7 Disposal of Drugs of Addiction and Poisons Included in Schedule 4
Restricted and Schedule 8
20.7.1 A S4R or S8 medicine is to be administered immediately after preparation or drawing up into a syringe and any unused portion discarded and recorded. If incremental dose is required the RN must stay with the patient.
20.7.2 If the full amount of a S8 medication is drawn up and not administered, the
same two (2) persons (one of which must be an RN) are required to witness the disposal of this drug. This should be recorded in the discarded column of the register.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 34 of 50
20.7.3 Where a partial amount of a solid dose form (e.g. tablet or lozenge) of a S4R or S8 is used the balance of the solid dose form should be destroyed and discarded in a manner preventing diversion. This should be recorded in the discard column in the register.
20.7.4 If a S4R or S8 medication has been unused (i.e. seal intact) it can be returned to stock. The medication must be re-entered into the Register of Drugs of Addiction with date, time, patient name and the statement "returned to stock". Two persons involved in the initial preparation must sign the entry.
20.7.5 Exemption of second checker. Refer to section 4.1.7 20.7.6 Expired stock is to be returned to the pharmacy or, in hospitals without
a pharmacist on site, the regional pharmacist is to be notified to arrange transfer or disposal. Medications dispensed to aged care facility residents by a retail pharmacy may be returned to the retail pharmacy for disposal in this circumstance the retail pharmacy must be contacted to arrange for the secure collection disposal of the medications.
20.8 Reporting Of Schedule 4 Restricted and 8 Medication Stock Discrepancies
20.8.1 All discrepancies (lost, stolen or theft) in the stock of S4R and S8 medications are required to be investigated and reported. OD0377/12 Reporting of medicine discrepancies in public hospitals and licensed private facilities which provide services to public patients in Western Australia.
20.8.2 If the discrepancy involves a clinical incident, an incident form must be completed. Poisons Reg 45(2) requires that the authorised person (Regional Pharmacist or as per individual regional processes) immediately notify clinical governance who would then report to the CCC and CEO in writing. Refer to: i. Flowchart: Investigating and reporting loss in public hospitals and
private facilities treating public patients and complete ii. Form: S8 & R4 medicine discrepancy /loss report.
20.9 Medication Fridge
20.9.1 Medications deemed suitable to be stored in a ward medication fridge must be securely stored and managed in accordance with legislation, licensing permit requirements, manufacturers’ recommendations and local WACHS pharmacy procedures.
20.9.2 All medications, including vaccines, stored in the ward medication fridges must meet cold chain storage requirements, where applicable.
20.9.3 All staff handling these pharmaceutical items are responsible for maintaining cold chain integrity and utilising the record sheets for temperature monitoring.
20.10 Transport
Refer to regional pharmacist for information on transporting medication. The use of plain packaging and a reputable post/courier is the responsibility of each WACHS facility when transporting medication. Refer to WACHS Requisitioning and Receipt of Schedule S4R and 8 Medications and Ordering of Pharmacy Imprest Supplies Procedure for district sites.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 35 of 50
Where stock discrepancy is identified e.g. drugs dispatched but not delivered/ received, the Post/Courier and WACHS persons involved must investigate and report the discrepancy and involve senior staff in accordance with local procedure. (refer to section 20.8) A S8 and S4R medications are not to be transported between facilities by a staff member other than a medical practitioner or pharmacist, and should generally be consigned by post or courier. Medications to be secured appropriately in tamperproof/tamper evident packaging prior to plain-packaging (refer to section 7.2.4). Refer also to WACHS Requisitioning and Receipt of Schedule S4R and 8 Medications and Ordering of Pharmacy Imprest Supplies Procedure.
21. EVALUATION
Medication incidents are the second most commonly reported incidents in Australian hospital incident monitoring systems. Organisations can learn about the safety of medication management processes by reviewing incidents and undertaking in depth analyses of incidents causing, or with the potential to cause, patient harm (NSQHSS 4). 21.1 Compliance
Compliance with this medication policy is to be measured by the number of medication incidents, adverse events and near misses relating to inappropriate medication administration by a RN, midwife, EN or NP and reported through the Clinical Incident Monitoring system. Specific national audit tools are available for medication safety e.g. aged care audit tool, high risk areas i.e. oncology and antithrombotic therapy.
WACHS sites are encouraged to participate in the Medication Safety Self-Assessment® for Australian Hospitals. This audit reviews a sample of medication charts to:
i. evaluate the effect of NIMC safety features ii. identify areas for improvement iii. provide a baseline for NIMC use and quality improvement initiatives. iv. improve the safety of medication charting.
21.2 Mitigation strategies
21.2.1 Site and regional review of incident reports, adverse events and near misses using Failure Modes and Effects Analysis (FMEA) identify: i. trends in the type and causes of errors, ii. particular areas in the medication management pathway where
incidents are occurring, or iii. specific medicines involved. (ref NSQHSS 4)
21.2.2 Regions include specific issues in the WACHS Riskbase risk register 21.2.3 Site nurse managers and pharmacists communicate to the workforce
and students about medication incidents and actions and proposed practice changes to reduce occurrence. (NSQHHS 4 - 4.4.2).
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 36 of 50
REFERENCES Aged Care Act 1997 and Quality of Care Principles Quality of Care Amendment
Principles 2011 (No. 1). (Australian Government). Australian Commission on Safety and Quality in Healthcare (ACSQHC) 2011 National
Safety and Quality Health Service Standards, ACSQHC, Sydney. Australian Health Practitioner Regulation Agency (AHPRA) 2008, Code of Ethics and
Professional Code of Conduct for Nurses. Australian Health Practitioner Regulation Agency, Australia.
Australian Nursing and Midwifery Council, 2007, National Framework for the Development of Decision-making Tools for Nursing and Midwifery Practice.
Australian Pharmaceutical Advisory Council, 2005, Guiding principles to achieve continuity in medication management, Department of Health and Ageing, Canberra.
Burridge N & Deigun D (eds.) 2011, Australian Injectable Drugs Handbook Society of Hospital Pharmacists of Australia.
Cancer Institute NSW n.d. - Standard Cancer Treatments - eviQ for use in clinical practice Carers Recognition Act (WA) 2004 Office of Health Protection. 2013 Australian Immunisation Handbook10th ed.,
Department of Health and Ageing: Canberra WA Health, Administrative Circular A 7652 Supply of Drugs and Medications. WA Health, Operational Instruction 0280/93 Drug Supplies To Outpatients of Health
Department Of Western Australia Government Non-Teaching Hospitals And Nursing Posts WA Health Operational Circular OP 1988/05 Scope of Enrolled Nursing Practice and
Enrolled Nurse Competencies. WA Health Information Circular IC 0179/14 Guidelines for the Transmission of Client
Identifiable Health Information by Facsimile Machine. WA Health, Operational Directive OD 0141/08 - Code of practice for the handling of
Schedule 8 medicines (drugs of addiction) in hospitals and nursing posts WA Health, Operational Directive OD 0142/08 Administration of Schedule 8 medicines
to patients attending for emergencies. WA Health, Operational Directive OD 0528/14 Storage and recording of Restricted
Schedule 4 (S4R) medicines Australian Commission on Safety and Quality in Health Care Recommendations for
Terminology, Abbreviations and Symbols used in Medicines Documentation. WA Health, Operational Directive OD 0312/10 Western Australian Patient Identification
Policy WA Health, Operational Directive OD 0377/12 Reporting of medicine discrepancies in
public hospitals and licensed private facilities which provide services to public patients in Western Australia and Flowchart: Investigating and reporting loss in public hospitals and private facilities treating public patients
3 WA Health, Operational Directive OD 0385/12 Updated: national recommendations for
user-applied labelling of injectable medicines, fluids and lines WA Health, Operational Directive OD 0397/12 Use of Acute Oxygen Therapy in
Western Australian Hospitals WA Health, Operational Directive 0414/13 Smoke Free WA Health System Policy. WA Health, Operational Directive 0415/13 Guidelines for Department of Health
Vaccination Programs – School and Community Health Immunisation.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 37 of 50
WA Health, Operational Directive OD 0416/13 Prescription and management of intravenous patient controlled analgesia
Department of Health WA 2011, Clinical Guidelines and Procedures for the Management of Nicotine Dependent Inpatients. Perth, Department of Health.
Department of Health WA n.d., Smoke Free WA Health System Policy, Guidelines for the management of nicotine withdrawal and cessation support in nicotine dependent patients. Perth, Department of Health.
Department of Veterans’ Affairs. 2010, Guidelines for the provision of community nursing services. Australian Government.
Health Practitioner Regulation National Law (WA) Act 2010. National Health and Medical Research Council. 2009. Clinical practice guideline for the
prevention of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to Australian hospitals. Melbourne: National Health and Medical Research Council: Canberra
National Institute of Clinical Studies 2011 Emergency Care Acute Pain Management Manual national emergency care Pain management initiative. National Health and Medical Research Council: Canberra.
Nursing and Midwifery Board of Australia n.d. Prescribing Formulary for eligible Midwives with a scheduled medicines endorsement.
Occupational Safety and Health Act 1984. (Western Australia). Office of Safety and Quality in Healthcare, 2008, National Inpatient Medication Chart
(NIMC) Standardised Charts and Guidelines (for adults, paediatric, neonatal and adult anticoagulant). Perth, Department of Health.
Office of the Chief Nursing Officer. 2003, Guiding Framework for the Implementation of Nurse Practitioners in Western Australia, Perth, Department of Health WA.
Poisons Act 1964. (Perth, Western Australia Government) Poisons Amendment Regulations 2010, Perth, Western Australia Government Poisons Regulations 1965. (Perth, Western Australia Government) Princess Margaret Hospital, 2011, Nursing Practice Manual drug and intravenous
therapy section 2. Royal Perth Hospital, 2012, Clinical Practice Standard for insertion and management of
a Peripheral Intravenous Cannula (PIVC). Royal Perth Hospital, 2010(revised version), RPH Policy Manual (V3 2007) Safe use of
medication refrigerators.
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 38 of 50
The Office of Safety and Quality in Healthcare 2012, Safer Guidelines for the WA
National Inpatient Medication Chart: Guidelines for use of the WA NIMC including the long stay NIMC. Department of Health WA
Therapeutic Goods Administration, 2010, Advisory Committee on the Safe Use of Medicines. Department of Health and Ageing, Canberra.
WA Country Health Service, 2007, Smoke Free WA Health System Policy Implementation Procedure.
WA Health High Risk Medication Policy WACHS High Risk Medications Procedure WACHS Chemotherapy Administration - WACHS Clinical Practice Standard
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 39 of 50
APPENDIX 1 STARTER PACK APPROVAL SITE LIST Albany Hospital Warden Avenue ALBANY WA 6330 Augusta Multi-Purpose Health Service Donovan Street AUGUSTA WA 6290 Bayulu Remote Area Health Service via FITZROY CROSSING WA 6765 Beacon Nursing Post Lindsay Street BEACON WA 6472 Bencubbin Nursing Post 79 Monger Street BENCUBBIN WA 6477 Beverly Health Service Sewell Street BEVERLEY WA 6304 Boddington Hospital Hotham Avenue BODDINGTON WA 6390 Boyup Brook Hospital Hospital Drive BOYUP BROOK WA 6244 Bremer Bay Health Centre 29 John Street BREMER BAY WA 6338 Bridgetown Hospital Peninsula Road BRIDGETOWN WA 6255 Brookton Nursing Home Lennard Street BROOKTON WA 6306 Broome Hospital Robinson Street BROOME WA 6725 Bruce Rock Hospital 35 Dunstall Street BRUCE ROCK WA 6418
Burringurrah Nsg Post Burringurrah Community Aboriginal Corporation UPPER GASCOYNE WA 6705 Collie Health Service Deakin Street COLLIE WA 6225 Coonana Nursing Post Coonana Community COONANA WA 6431 Coolgardie Health Centre Wilkie St COOLGARDIE WA 6429 Coral Bay Nursing Post Coral Bay Shopping Centre CORAL BAY WA 6701 Corrigin Hospital 49 Kirkwood Street CORRIGIN WA 6375 Cue Nursing Post Victoria Street CUE WA 6640 Cunderdin Hospital Cubbine Road CUNDERDIN WA 6407 Dalwallinu Hospital PO BOX 115 DALWALLINU WA 6609 Denmark Health Service Scotsdale Road DENMARK WA 6333 Derby Hospital Clarendon Street DERBY WA 6728 Dongara MPS 48 Blenheim Road DONGARA WA 6525 Donnybrook Hospital Bentley Street DONNYBROOK WA 6239
Dumbleyung Hospital McIntyre Street DUMBLEYUNG WA 6350 Dundas Health Service Talbot Street NORSEMAN WA 6443 Eneabba Nursing Post Grover Street ENEABBA WA 6518 Esperance Community Health Forrest St ESPERANCE WA 6450 Esperance Hospital Hicks St ESPERANCE WA 6450 Exmouth Hospital Lyons Street EXMOUTH WA 6707 Fitzroy Crossing Hospital Fallon Road FITZROY CROSSING WA 6765 Gnowangerup Hospital Yougenup Road GNOWANGERUP WA 6335 Goldfields Population Health 36-42 Ware St KALGOORLIE WA 6430 Goomalling Hospital PO BOX 107 GOOMALLING WA 6460 Halls Creek Hospital 70 Roberta Avenue HALLS CREEK WA 6770 Harvey Hospital 45 Hayward Street HARVEY WA 6220
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 40 of 50
Hedland Health Campus Colebach Way South Hedland WA 6722 Jerramungup Health Centre - Kokoda Road JERRAMUNGUP WA 6337 Junjuwa Remote Area Health Service Junjuwa via FITZROY CROSSING WA 6765 Jurien Bay Health Centre Whitfield Street JURIEN BAY WA 6516 Kalbarri Health Centre Kaiber Street, KALBARRI WA 6536 Kalgoorlie-Boulder Community Health 36-42 Ware St KALGOORLIE WA 6430 Kalumburu Remote Area Health Service Kalumburu WA 6740 Kambalda Health Centre Gumnut Place KAMBALDA WA 6444 Katanning Health Service Clive Street KATANNING WA 6317 Kellerberrin Health Services 51-53 Gregory Street KELLERBERRIN WA 6410 Kojonup Hospital Spring Street KOJONUP WA 6395 Kondinin Hospital Graham Street KONDININ WA 6367
Koorda Community Health Centre 21 Allenby Street KOORDA WA 6475 Kukerin Health Centre Manser Street KUKERIN WA 6352 Kununoppin and Districts Health Service Leake Street KUNUNOPPIN WA 6489 Kununurra Hospital 96 Coolibah Drive KUNUNURRA WA 6743 Lake Grace Hospital Stubbs Street LAKE GRACE WA 6353 Laverton Community Health Laver Place LAVERTON WA 6440 Laverton Hospital Beria Road LAVERTON WA 6440 Leeman Nursing Post Lot 692 Morcombe Road LEEMAN WA 6514 Leinster Nursing Post Link Road LEINSTER WA 6437 Leonora Community Health 96 Tower St LEONORA WA 6438 Leonora Hospital Sadie Canning Drive LEONORA WA 6438 Lombadina Remote Area Health Service LOMBADINA WA 6725 Looma Remote Area Health Service LOOMA via DERBY WA 6728
Marble Bar Nursing Post 2 Francis Street MARBLE BAR WA 6760 Margaret River Hospital Farrelly Street MARGARET RIVER WA 6285 Meekatharra Hospital Savage Street MEEKATHARRA WA 6642 Menzies Nursing Post Sandstone Road MENZIES WA 6436 Merredin Health Services Kitchener Road MERREDIN WA 6415 Mingenew Nursing Post 80 Philip Street MINGENEW WA 6522 Moora Hospital PO BOX 154 MOORA WA 6510 Morawa and Districts Health Service Caulfield Road MORAWA WA 6623 Mount Magnet Nursing Post Cnr Welcome & Criddle Sts MOUNT MAGNET WA 6638 Mukinbudin Health Service Ferguson Street MUKINBUDIN WA 6479 Mullewa Health Service Elder Street MULEWA WA 6535 Nannup Hospital Carey Street NANNUP WA 6275
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 41 of 50
Narembeen Health Svcs Ada Street NAREMBEEN WA 6369 Narrogin Hospital Williams Road NARROGIN WA 6312 Nickol Bay Hospital Millstream Road KARRATHA WA 6714 Newman Hospital Mindarra Street NEWMAN WA 6753 Noonkanbah Remote Area Health Service via FITZROY CROSSING WA 6765 North Midlands Health Service Thomas Street THREE SPRINGS WA 6519 Northampton Hospital Stevens Street Northampton WA 6535 Northam Hospital PO BOX 312 Northam WA 6401 Northcliffe Nursing Post Wheatley Coast Road NORTHCLIFFE WA 6262 Norseman Comm.Health 72-74 Princep St NORESMAN WA 6443 Norseman Hospital Talbot St NORSEMAN WA 6443 Nullagine Nursing Post 2 Cooke Street NULLIGINE WA 6758 One Arm Point Comm. Remote Area Health ONE ARM POINT WA 6725 Onslow Hospital Second Avenue ONSLOW WA 6710
Paraburdoo Hospital Rocklea Road PARABURDOO WA 6754 Pemberton Northcliffe Health Service Railway Crescent PEMBERTON WA 6260 Pingelly Hospital Stratford Street PINGELLY WA 6308 Plantagenet Hospital Langton Road MOUNT BARKER WA 6324 Quairading Hospital Harris Street QUAIRADING WA 6383 Ravensthorpe Health Service Morgan Street RAVENSTHORPE WA 6346 Roebourne Hospital 42-44 Hampton Street ROEBOURNE WA 6718 Sandstone Nursing Post 120 Payne Street SANDSTONE WA 6639 Shark Bay Nursing Post 35 Hughes Street DENHAM WA 6537 Southern Cross Health Service Coolgardie Road SOUTHERN CROSS WA 6426 Tambellup Nursing Post Norrish Street TAMBELLUP WA 6320 Tom Price Hospital Mine Road TOM PRICE WA 6751 Wagin Hospital Warwick Street WAGIN WA 6315
Walpole Nursing Post South Coast Highway WALPOLE WA 6398 Wangkatjungka Remote Area Health Service via FITZROY CROSSING WA 6765 Warmun Remote Area Health Service - Ord Street WARMUN WA 6743 Warren Hospital Hospital Avenue MANJIMUP WA 6258 Wheatbelt Health Region Furnival Street NARROGIN WA 6312 Wickepin Community Health Centre Wogolin Road WICKEPIN WA 6370 Williams Health Centre Adams Street WILLIAMS WA 6391 Wongan Hills Hospital PO BOX 250 WONGAN HILLS WA 6603 Wyalkatchem-Koorda and Districts Hospital Honour Street WYALKATCHEM WA 6485 Wyndham Hospital Minderoo Road WYNDHAM WA 6740 Yalgoo Nursing Post Stanley Street YALGOO WA 6635 Yandeyarra Community Health Clinic Great Northern Highway De Grey WA 6722 York Hospital Trews Road YORK WA 6302
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 42 of 50
Appendix 2 - "APPROVED STARTER PACKS" AS AT 18 SEPTEMBER 2013
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 43 of 50
Appendix 2 continued
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request This information is available in alternative formats upon request
Page 44 of 50
APPENDIX 3a NURSE INITIATED MEDICATIONS NON-PRESCRIBED
SCHEDULE 2 and 3 MEDICATIONS FOR ADULT PATIENTS The following medications may be administered to an adult patient by a RN, or an EN (after consultation with an RN) who has undertaken an assessment of the patient without a medical officer's written or verbal order, as per section 8. Subsequent repeat dose require medical review. Therefore any S2-3 preparation that is only provided in a multi dose pack is not included in this list (e.g. anti-fungal preparations). Supply of nurse initiated non-prescribed medication is subject to availability on regional formulary. The RN is accountable for their practice including adhering to Section 5 principles of medication administration. The administration of these medications must be documented on the ‘Once Only and Pre-Operative Medication’ section of the MR170 series medication chart. Nicotine replacement therapy may only be administered as per DOH Clinical guidelines and procedures for the management of Nicotine dependent inpatients (see section 11). Analgesics / Anti-inflammatory Paracetamol mixture or tablets (500mg) Aspirin 300mg Ibuprofen 200-400mg Topical Lignocaine 2% gel for wound
management only Antihistamine Loratidine 10mg Fexofenadine 60mg Promethazine 10-25mg
Bowel Stimulants Docusate (Coloxyl oral or rectal formula) Paraffin emulsion (Agarol mixture) Docusate with Senna (Coloxyl with
senna) Senna tablets Bisacodyl tablets Fruit Laxative (Nulax) Bulk Laxatives Fibre supplements (Metamucil,
Benefibre) Sterculia (Normacol, Granacol) Movicol
Enemas and Suppositories Microlax enema Glycerin suppositories Bisacodyl suppositories 10mg Antacids Aluminium hydroxide (GavisconTM, MylantaTM) Ocular Ocular lubricants – Polytears Fluorescein Sodium 2% stain (emergency
department only)
Respiratory Salbutamol MDI with spacer Nebulised saline Incidentals Glucose oral solution Carbotest Sodium citro-tartrate (Citravescent/Ural/
Uricalm) Saliva Substitute Antiseptic throat lozenges (Capitol) Sodium citrate 8.8% 0.3M (single dose) Pholcodine linctus Senega and ammonia mixture Glyceryl trinitrate sublingual Simethicone capsules Hyoscine butylbromide 20mg Hirudoid/Lasonil Head Lice Treatments
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request
This information is available in alternative formats upon request
Page 45 of 50
APPENDIX 3b NURSE INITIATED NON-PRESCRIBED SCHEDULE 2 and 3 MEDICATIONS FOR PAEDIATRIC PATIENTS
The following medications may be administered to a paediatric patient by a RN, who has undertaken an assessment of the patient without a Medical Officers written or verbal order, as per section 8. Subsequent repeat dose require medical review. Therefore any S2-3 preparation that is only provided in a multi dose pack is not included in this list (e.g. anti-fungal preparations). Supply of nurse initiated non-prescribed medication is subject to availability on regional formulary. The RN is accountable for their practice including adhering to Section 5 Principles of medication administration. The RN must consult the appropriate endorsed for use in WACHS administration of medications handbook e.g. Royal Children’s Hospital Melbourne paediatric pharmacopeia (see section 1) for weight related dosing schedule. The administration of these medications must be included in the ‘Once Only and Pre-Operative Medication’ section of the WACHS MR170D medication chart including documenting the basis for dose calculation e.g. mg/kg. Analgesics/ Anti-inflammatory Paracetamol oral or rectal Ibuprofen Topical Local Anaesthetics e.g. Eutectic Mixture of Local Anaesthetics (EMLA) Sucrose 25% solution Antihistamine Loratadine Respiratory Salbutamol (inhalational) Nebulised saline Incidentals Wax removal ear drops (e.g. Cerumol®; Waxsol®) NaCl 0.9% nose drops Artificial tears (ointment and drops) Glycerine suppository (infant/child/adult) Head Lice Treatments
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request
This information is available in alternative formats upon request
Page 46 of 50
APPENDIX 4 - DESIGNATED REMOTE AREA NURSING POSTS Please refer to Appendix 1 of Registered nurses – remote area nursing posts (Word 97KB) located at Department of Health Structured Administration and Supply Arrangement website under CEO of Health SASA
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request
This information is available in alternative formats upon request
Page 47 of 50
APPENDIX 5 - SUPPLY BY REGISTERED NURSES AT REMOTE AREA NURSING POSTS Please refer to Registered nurses – remote area nursing posts (Word 97KB) located at Department of Health Structured Administration and Supply Arrangement website under CEO of Health SASA
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request
This information is available in alternative formats upon request
Page 48 of 50
APPENDIX 6 - DRUG AND IV FLOW CALCULATIONS 6.1 Calculating Rate of Flow for Intravenous Infusions Check the delivery rate of the giving set used for infusion (i.e. drops per mL). Formula is as follows: Rate of flow = Volume x Drops/minute
Time in Hours x 60 Or Time [hours] = Volume x Drops/mL
Rate in Drops / mL x 60 mL/hr = Volume or Volume x 60
Time (hrs) Time (mins)
The rate for IV medications going through a pump is also to be checked by an RN and a second nurse in order to avoid any errors in the rate programmed into the pump.
6.2 Drug Calculation Formula
Dose required = Number of tablets to be administered Stock Strength
Dose Required x Volume of Stock Strength = Volume to administer Stock Strength
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request
This information is available in alternative formats upon request
Page 49 of 50
APPENDIX 7 - ANAPHYLAXIS FLOWCHART (Modified to remove administration of Epipens within hospitals)
27/11/2007 3:27 pmDocument valid at:
This information is available in alternative formats upon request
This information is available in alternative formats upon request
Page 50 of 50
APPENDIX 8 - POLICY REVIEW CONTRIBUTORS
With thanks to the contributions from individual submissions and the tireless work of Medication Review Group 2012/2013. 1. Shirilee Kerrison (Chair) Coordinator of Nursing and Midwifery - WACHS Central
Office 2. Pamela Coates Senior Project Officer Nursing and Midwifery - Central Office 3. Ruth Littler, WACHS Aged Care Project Officer - WACHS Central Office 4. Kerry Fitzsimmons Pharmacist Office of Safety and Quality DOH 5. Meeghan Clay Pharmacist - Great Southern 6. John Van der Post FACEM Albany - Great Southern) 7. Marianne Slattery Regional Nurse Director - South West 8. Naomi Lillywhite Chief Pharmacist Bunbury - South west. 9. Mair Jones Nurse Educator - South West 10. Diana Ellison DON/HSM Quairading - Wheatbelt 11. Chris Cream Regional Nurse Director, Midwest (proxy Sue Hogan) 12. Janine Glasson Clinical Nurse/CNI, Geraldton - Midwest 13. Ken Thomson Mental Health Manager, Geraldton 14. Peter Barrett Regional Medical Director - Goldfields 15. Karine Miller regional Coordinator of Population Health, Goldfields 16. Krysten Todd Registered Nurse Hedland Health Campus, Pilbara 17. Geraldine Rolfe Mental Health Manager, Broome 18. Scott Stokes Nurse Practitioner Paediatric – Kimberley; (Proxy Angela Fisher NP) 19. Ruth Bath DON/HSM Kununurra
Specific subject matter expert consultations: 20. Peggy Briggs Rural Cancer Nurse Coordinator, WACHS Perth 21. Kate Reynolds Senior Midwifery Project Manager, WACHS Perth 22. Garth Hetherington, FACEM lead WACHS 23. Siva Balu Psychiatric Kimberley 24. Linda Smith HACC project officer; Carol Fryer Community West auditor
Title: Medication Administration Policy Contact: WACHS Great Southern Regional Chief Pharmacist (M. Clay)
Directorate: Medical Services TRIM Record Number: ED-CO-13-124530 Version: 7.00 Date Published: 25 January 2018
Date of Last Review: January 2018 Date Next Review: June 2018
27/11/2007 3:27 pmDocument valid at:
This document can be made available in alternative formats upon request
from a person with a disability.
© WA Country Health Service
27/11/2007 3:27 pmDocument valid at:
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 1 of 43 Date Next Review: March 2021
Effective: 2 April 2020
Assessment and Management in the Emergency Department - Clinical Practice Standard
1. Purpose
The purpose of this policy is to: Ensure evidence based minimum practice standards for the triage, assessment,
care and management of unplanned patient presentations to emergency facilities.
Minimise unwanted variation in clinical practice (overuse, misuse and underuse).
Ensure safe, effective and efficient health outcomes, minimising preventable harm and decreasing wastage therefore reducing health expenditure.
Ensure each presentation is newly assessed as a unique episode of illness/injury.
Ensure appropriate documentation and clinical handover.
2. Scope
The scope of this policy relates to all medical, nursing and midwifery staff employed within WACHS. All health care professionals are to work within their scope of practice appropriate to their level of training and responsibility and the scope of their professional registration as documented by the Australian Health Practitioner Regulation Agency.
2.1 Out of scope:
Planned outpatient presentations such as wound or X-ray reviews are documented on the MR5 Outpatient Notes or identified in the Planned Return Visit vs Emergency attendance field in webPAS.
When the ED is the only provider of elective testing i.e. ECG, spirometry etc. Refer also to WACHS Emergency Department Acute and Outpatient Activity Guideline.
Pregnant women 20 weeks gestation or more, presenting to the ED at a hospital with a maternity ward with a pregnancy related condition should be sent straight to maternity for midwifery assessment. Refer to Appendix 6 – Pregnant Women 20 Weeks or More Presenting to a Maternity Site.
3. Communicating for Safety in the Emergency Department
To minimise the risks arising from patient aggression: The triage area should be as private as possible for easy staff egress and
duress capability.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 2 of 43 Date Next Review: March 2021
Refer to local Code Black procedure. Each site should have a local management plan for identifying and managing patients know to be at risk of aggression towards hospital staff.
It is mandatory for all ED clinicians to be trained in aggression management. Refer to the Chief Psychiatrist of Western Australia, DOH Principles and Best
Practice for the Care of People Who May be Suicidal. Refer to the WACHS Working in Isolation – Minimum Safety and Security
Standards for All Staff Policy. Early notification of the Emergency Telehealth Service (ETS). Documentation of
telephone conversation including handover of patient.
3.1 Clinical Handover
In all cases clinical handover must include information exchange between all disciplines as per the National Safety and Quality Healthcare Service (NSQHS) Standard- Communicating for Safety, and MP 0095/19 Clinical Handover Policy using the iSoBAR framework.
3.2 Consent to Treatment
Patients undergoing procedures in the ED must be provided with full information and their consent documented as per MP 0657/18 Consent to Treatment Policy. The policy provides guidelines for those unable to provide consent on their own behalf and for life-threatening emergency situations.
3.3 Partnering with Consumers
Ensure measures are in place to maintain patient privacy and dignity. Offer the presence of a chaperone where appropriate to patient and clinician requirements, refer to the WACHS Chaperone Policy. Provide the opportunity for an accredited interpreter and/ or Aboriginal Liaison Officer where appropriate to the patient’s language or communication requirements.
4. Triage Process
4.1 Triage Competency
At least one Registered Nurse performing triage must have: Completed the WACHS Triage competency Australia Government, Department
of Health and Ageing, Emergency Training Education Kit (ETEK) as outlined in the WACHS Capabiliti Learning Management System (NEDT EL2).
Current Basic Life Support (BLS REABL EL2) competency. Advanced Life Support - Adult competency where possible. Advanced Life Support - Paediatric competency where possible. ETS Help – Triage (ETS0013EL1) at sites where applicable. Recognised prior learning of an accepted triage education course is accepted.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 3 of 43 Date Next Review: March 2021
Note: Sites which roster two nurses per shift are to ensure one holds a current triage competency. A staff member who is yet to achieve triage competency must seek guidance from either the triage competent nurse onsite or through ETS. All nursing staff at ETS are triage competent.
4.2 Initial Referral
Regardless of referral or mode of transport to the ED, all patient contacts with the triage nurse must be documented on the MR1 WACHS Emergency Department Notes. The process for managing emergency department presentations is defined in Appendix 2 - Management of Patient Presentations to ED throughout WACHS.
4.3 Telephone
The receiving clinician should quickly establish if the caller requires an emergency vehicle to attend.
If yes, document the patients’ name, phone and address details and transfer them to ‘000’ immediately.
Do not hang up until they are connected to the emergency vehicle provider. If necessary place hospital response teams on standby e.g. trauma team, local
GP as per local procedure. Consider early notification of ETS (Emergency Telehealth Service)
4.4 General call for non- emergency advice
Redirect caller to HealthDirect – Telephone: 1800 022 222, Hearing Impaired Text Telephone (TTY): 1800 022 226.
4.5 Mental Health Call for non-emergency advice
Redirect caller to WA RuralLink (specialist after-hours mental health) – Telephone: 1800 552 002, Hearing Impaired Text Telephone (TTY): 1800 720 101.
Child and Adolescent Acute Response Team 1800 048 636.
5. Emergency Triage and Immediate Management
5.1 Triage – Primary Survey
All patients are to be assessed on arrival to the health care facility, according to the ATS guidelines.
Rapid visual survey of Airway, Breathing, Circulation, Disability and Exposure (ABCDE) assessment is to occur.
The most urgent and high risk clinical features determine the ATS category, with consideration of mechanism of injury and co-morbidities. Relief of pain is a legitimate reason for a higher ATS category.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 4 of 43 Date Next Review: March 2021
Triage does not require formal physiological observations. Palpation of pulses can ascertain quality and rate of heart rate, condition of skin (cool, dry etc.).
Commence nurse-initiated care activities i.e. first-aid, pain relief, or escalation of care as indicated.
ATS CategoryMaximum waiting time for assessment and treatment
Performance indicator threshold
1 Immediate 100%2 10 minutes 80%3 30 minutes 75%4 60 minutes 70%5 120 minutes 70%
Refer to Appendix 3 - Australasian Triage Score Categories and Appendix 4 - Triage Clinical Descriptors.
5.2 Nursing documentation
The triage assessment and ATS code allocated must be recorded on the MR1 WACHS Emergency Department Notes. Refer also to the OD 0590/15 Recording and Reporting of Clinical Care Commencement Date and Time in the Emergency Department.
5.3 Nursing observations
A Nurse is to be notified of: Any patient who cannot be seen within the recommended ATS timeframes must
be commenced on a MR140A WACHS Observation and Response Chart series, appropriate to age – (Adult Chart for 16 years and over if deemed mature / appropriate).
All patients in the waiting room must be re-assessed once the triage time has expired as per the table above.
Observations in the waiting room are done as per ATS criteria unless the patient’s clinical condition dictates more frequent observations: ATS 3 - every 30 minutes ATS 4 - every 60 minutes (1 hourly) ATS 5 - two hourly.
Escalation of abnormal observations should be as per the ORC criteria and documented on the MR1.
5.4 Medical Officer or Nurse Practitioner Notifications
A Medical Officer (MO) is to be notified of: All patients categorised as ATS category 1-2.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 5 of 43 Date Next Review: March 2021
A Medical Officer (MO) or Nurse Practitioner (NP) is to be notified of: All patients categorised as ATS category 3-5. Any patient who re-presents with 48 hours for the same condition. Any presentation in which the provisional diagnosis is not clear. All patients who meet Trauma Team Notification criteria as per the trauma
descriptors in Appendix 4 - Triage Clinical Descriptors and complete the MR2 WACHS Emergency Department Trauma Notes.
Additional triage indicators which require review by or discussion with a MO or NP are listed in Appendix 5 - Triage Risk Factor Indicators or Review or Discussion with Medical Officer (MO) / ED Nurse Practitioner (NP).
Where a local MO or NP are not available, contact Regional Resource Centre (RRC) MO or hub hospital (Wheatbelt), Emergency Telehealth Service (ETS) or Royal Flying Doctor (RFDS).
Refer to local practice and ETS guidelines Appendix 11 - Emergency Telehealth Service Referral Process for referral process to ETS escalation of care.
5.5 Mental health considerations
Key considerations for triage of mental health presentations: The usual primary-survey approach to assessing all incoming patients is to be
complete prior to commencing mental health assessment. The higher ATS (general or mental health specific) is documented and acted upon to expedite appropriate review and treatment.
Mental health triage is based on assessment of observed and reported clinical features and undertaking WACHS BACPAC Mental State Assessment.
The allocation of a triage code must be based on clinical criteria that are consistent with ATS descriptors for mental health presentations. Refer to Appendix 4 - Triage Clinical Descriptors.
Refer to WACHS Mental Health Care in Emergency Departments and General Wards Policy.
Where indicated complete an MR46 WACHS Suicide Risk Assessment and Safety Plan.
Adult and paediatric community mental health links for Child and Adolescent Acute Response Team and RuralLink (free call 1800 552 002 or
[TTY] 1800 720 101). People presenting with mental health problems and associated risk to self or
others may be treated under Duty of Care, or by reference to the MH Act 2014: “Emergency Psychiatric Treatment (EPT)”. Refer to Appendix 1 - Definitions.
5.6 Paediatric presentations
For the purpose of emergency presentations to ED a paediatric presentation is any child under the age of 18 years. Key considerations for triage of paediatric presentations:
The clinical priorities and the principles of urgency for infants, children and adolescents are the same as those for adults.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 6 of 43 Date Next Review: March 2021
Determining the urgency will require recognition of serious illness, some features of which may be different in infants and children. Refer to Appendix 4 - Triage Clinical Descriptors and Appendix 5 - Triage Risk Factor Indicators for Review or Discussion with Medical Officer / ED Nurse Practitioner. Where applicable refer to OD 0606/15 Guidelines for Protecting Children and WACHS WebPAS Child at Risk Alert Procedure.
The value of parents, carers or significant others and their capacity to identify deviations from normal in their child’s level of function should not be underestimated.
Infants that are preterm must be placed on the age adjusted appropriate MR 140 Paediatric Observation and Response Chart. Refer to section 15. Related Forms.
5.7 Dead on arrival
Refer to WACHS Care of the Deceased Policy and the related suite of procedures and forms.
5.8 Did not wait
Refer WACHS Management and Review of “Did Not Wait” Patients that Present to Emergency Services Policy.
5.9 Primary Assessment
Primary Assessment must involve: A systematic physiologic assessment. A full set of physiological observations. The patient’s presenting complaint, past history, current medications and
allergies.
Relevant clinical care pathways should be implemented at this point.
5.10 Secondary Assessment
The secondary survey/assessment builds upon the primary assessment: Once immediate life-threatening issues have been treated. Includes a further complete physical examination to ensure that no injuries have
been missed.
Other considerations that may apply include Emergency Telehealth Referral Process, Advanced Health Directives (AHD), WebPAS risk alerts, cultural needs and Next of Kin.
A clinician working within their scope of practice may commence specific clinical care using established protocols, procedures or endorsed guidelines.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 7 of 43 Date Next Review: March 2021
6. Management of Pregnant or Postnatal Women
6.1 Principle of triage assessment for pregnant and postnatal women
There are no ATS categories specific to pregnancy related conditions. Some guidance is provided in Chapter 9 of the Emergency Triage Education Kit and the following: For presentations to ED with a maternity service – Refer to Appendix 7 –
ED Obstetric Triage Pathway. For presentations to ED with a no maternity service – Refer to Appendix
8 – ED Obstetric Triage Pathway for Non-maternity Service Sites. The triage nurse must confirm the gestation using Estimated Due Date
(EDD); this is calculated from the first day of the Last Normal Menstrual Period (LNMP) or an EDD by first trimester ultrasound scan.
All pregnant women 20 weeks or more need to be triaged and then follow Appendix 7 – ED Obstetric Triage Pathway and commenced on a MR140B WACHS Maternal Observation & Response Chart.
Assessment of pregnant women who are more than 20 weeks or postnatal is not within the scope of nurses and midwives.
Postnatal women include those who present up to six weeks after giving birth.
For women who are obviously in labour and birth appears imminent refer to the WACHS Management of Imminent Unplanned Birth at Non-Birthing Service Sites Policy.
All women of child-bearing age are to be considered to be pregnant until proven otherwise.
6.2 Clinical telephone advice
If the caller does not require an emergency vehicle, either direct the caller to: The maternity service they are booked to give birth at, OR HealthDirect as per ‘General Medical’ telephone referrals.
6.3 Nursing assessment of pregnant woman 20 weeks and over
Triage in the emergency department. Refer to Appendix 9 – Nursing History for a Pregnant Woman. A single fetal heart rate by Doppler does not constitute an assessment of fetal
wellbeing and should not be routinely undertaken by non-midwives and non-obstetric doctors as: They may not know normal /abnormal parameters. There is no ability to act on an abnormal fetal heart. If the fetal heart cannot be found, which may be due to inadequate
technique rather than absence of a fetal heart, is may be distressing for the mother and possibly the staff.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 8 of 43 Date Next Review: March 2021
A single fetal heart rate tells you only that the baby is alive at the time it is taken and an ill baby can still die shortly thereafter.
Cardiotocograph monitoring should not be ordered by non-midwives and non-obstetric doctors.
6.4 Vaginal examinations of pregnant woman 20 weeks and over
Assessment should be made on the woman’s presenting symptoms and vaginal examination should not influence management or decision making.
Vaginal examination should not be undertaken by non-midwives and non-obstetric doctors, as the assessment is very likely to be inaccurate and therefore misguide appropriate management / transfer. Cervical status can change rapidly so may be falsely reassuring. Risks of introducing infection to the mother and/ or fetus. Risks of causing rupture of membranes. Risks of increasing likelihood of preterm labour /birth. Risks of causing haemorrhage if placental location is not known. Unnecessary discomfort and exposure to the woman.
It is outside the scope of practice for a Registered Nurse whom is not a Registered Midwife to undertake a vaginal examination in this context and any requests for the Registered Nurse to undertake this procedure must be declined.
6.5 Symptoms requiring obstetric / midwifery consult:
Pregnant women can present with symptoms that may appear to a non-midwife nurse and non-obstetric doctors to be unrelated to the pregnancy.
Refer to Appendix 6 – Symptoms in the Pregnant or Postnatal Woman Requiring Obstetric MP and/or Midwifery Consultation before Discharge from the ED.
These symptoms can be associated with significant maternal or fetal complications and as such require consultation with either an obstetric medical practitioner or midwife.
Refer to Appendix 8 – Pathway for Obstetric or Midwifery Advice for ED / ETS Staff at a Non-maternity Site.
7. Implementing and Evaluation of Care
7.1 Planning
Following the secondary survey / assessment an individualised management plan is to be documented, at a minimum, including:
Patient history and presence of comorbidities (MR1). Differential diagnoses. Treatment for pre-existing and current condition. Including emulation of treatment by patient response.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 9 of 43 Date Next Review: March 2021
Medications (MR170 series). Frequency and type of observations. Psychosocial and cultural factors that could influence patient care planning and
treatment. Patient education and consent. Any limits on interventions associated with AHDs or similar. Diagnostics undertaken and process of review. Refer to the General, Paediatric and Mental Health General Management
Principles e.g. actions and considerations - Appendix 10 - General Management Principles.
8. Admission, Transfer and Discharge Planning and Disposition
8.1 Decision to admit
Ensure that a complete iSoBAR handover occurs between the ED and the ward. Refer to MP0095/19 Clinical Handover Policy.
8.2 Decision to transfer
Refer to the WACHS Assessment and Management of Interhospital Patient Transfers Policy. The most senior WACHS clinician at the site, including ETS, is responsible for care and decision to transfer as per the policy.
WACHS Link is a model for transferring emergency and urgent patients requiring tertiary level care.
Patients awaiting transfer must continue to receive regular observations, escalation and treatment until care is handed over to the retrieval team.
8.3 Decision to discharge
A decision to discharge a patient from the emergency department in rural facilities can only be taken by a MO, NP or senior Registered Nurse, after a comprehensive secondary assessment.
If the patient has ongoing significant symptoms and the diagnosis is unclear, the patient must be discussed with a MO/NP prior to discharge.
Discharge of children aged < 2 years by a NP or senior Registered Nurse must be in consultation with a MO either onsite, by phone or by ETS.
Considerations should include the suitability of the patient’s proposed residence, the availability of safe transport and the availability of supervision or carer support according to the identified discharge needs.
Patients and carers must be provided with a ED discharge summary, written information and education for their condition and information as to how to provide consumer experience feedback.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 10 of 43 Date Next Review: March 2021
8.4 Discharge against medical advice
Wherever possible, liaise with MO to review patient prior to patient leaving hospital. Refer to WACHS Admission, Discharge and Intra-hospital Transfer CPS.
9. Staffing Requirements
Refer to the WACHS Emergency Care Capability Framework Report and Emergency Care Minimum Requirements Matrix for minimum medical and nursing staffing requirements in emergency departments.
9.1 Triage Nurse
The triage nurse is to be a qualified and experienced registered nurse level 1.2 or above and competent as documented in Section 4 Triage Process.
Sites which roster two nurses per shift must ensure one nurse is triage competent.
The enrolled nurse may be the first person to document an initial assessment. The enrolled nurse must then immediately notify an appropriate triage competent registered nurse or nurse practitioner of the patient’s arrival and the findings of the initial assessment.
The registered nurse or nurse practitioner is then required to attend the patient to complete a triage assessment.
10.Records ManagementAll WACHS corporate records must be stored in the approved Electronic Documents and Records Management System. Refer to WACHS Records Management Policy and Health Record Management Policy.
11.EvaluationMonitoring of compliance with this document is to be carried out by Regional Nursing and Midwifery Directors and Regional Medical Directors. Refer to the facility audit schedule WACHS Recognising and Responding to Acute Deterioration Audit specific to Emergency Department patients.
12.Standards
National Safety and Quality Health Service Standards: 2.1, 5.4, 6.1.Aged Care Accreditation Standards: 1, 2, 3, 5, 8.National Standards for Mental Health Services: 10.3, 10.4, 10.5.National Standards for Disability Services: 1, 5, 6.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 11 of 43 Date Next Review: March 2021
13.Compliance Monitoring
Performance and evaluation of triage practices are to be monitored through site, regional and central level governance processes including: Clinical audit of triage using the agreed WACHS audit tool and process
http://wachs.hdwa.health.wa.gov.au/?id=3136 Review of key performance indicators such as Percentage of emergency
department patients seen within recommended times by triage category and WA Emergency Access Target (WEAT) within the Health Service Performance Report (HSPR)
Review of any clinical incidents involving triage.
14.Legislation
(Accessible via: Western Australian Legislation or ComLaw) sites) Carers Recognition Act 2004 Children and Community Services Act 2004 Civil Liability Act 2002 Criminal Code Act Compilation Act 1913 Disability Services Act 1993 Equal Opportunity Act 1984 Equal Opportunity Regulations 1986 Guardianship and Administration Act 1990 Health Practitioner Regulation National Law (WA) Act 2010 Mental Health Act 2014 Occupational Safety and Health Act 1984 Occupational Safety and Health Regulations 1996 Pharmacy Act 1964 Poisons Act 1964 Poisons Regulations 1965 Privacy Act 1988 Public Sector Management Act 1994 State Records Act 2000
15.References
Department of Health and Ageing Emergency Triage Education KitDOH Guidelines for Protecting ChildrenWACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response policy (2018)WACHS Emergency Department Acute and Outpatient Activity GuidelineWACHS Clinical observations and Assessments Clinical Practice Standard (physiological (vital signs), neurovascular, neurological and fluid balance)
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 12 of 43 Date Next Review: March 2021
WA health system Credentialing and Defining Scope of Clinical Practice PolicyWA health system Clinical Governance, Safety and Quality Policy FrameworkWA health system Information Management Policy Framework
16.Related Forms
MR1 WACHS Emergency Department NotesMR1B Chest Pain Pathway – All patients presenting with chest pain are to be commenced on the MR1B chest pain pathway. At any stage of the ED episode, if the MO or NP deems that the patient does not need to continue on the pathway, they can be discharged from the pathway.MR140 WACHS Medical Emergency Response / Code Blue RecordMR140A Adult Observation and Response Chart (A-ORC)MR140B Maternal Observation and Response Chart (M-ORC)MR140C Additional Maternal Observation ChartMR140D Paediatric Observation and Response Chart (N-ORC)MR140E Paediatric Observation and Response Chart (P-ORC - under 3 months)MR140F Paediatric Observation and Response Chart (P-ORC - 3-12 months)MR140G Paediatric Observation and Response Chart (P-ORC - 1-4 yrs)MR140H Paediatric Observation and Response Chart (P-ORC - 5-11 yrs)MR140I Paediatric Observation and Response Chart (P-ORC - 12+ yrs)MR170.1 Medication History and Management PlanMR170A National Inpatient Medication Chart - Adult Short StayMR170C Anticoagulant Medication ChartMR170D National Inpatient Medication Chart - Paediatric Short StayMR170E National Inpatient Medication Chart - Paediatric Long StayMR172A and B - Tenecteplase forms – Any patient who presents with an acute myocardial infarction requiring thrombolysis is to have their treatment assessed and managed as per the MR172a and MR172b formMR2 WACHS Emergency Department Trauma Chart (Adult) – All major trauma is to be documented on the MR2 trauma sheetMR111 WACHS Nursing Admission, Screening and Assessment Tool or MR111P WACHS Paediatric Nursing Admission/Discharge Assessment form - As a minimum complete the comprehensive skin assessment, Braden score, malnutrition screening tool, and falls risk assessment. MR184 WACHS Inter-hospital Clinical Handover formPatient Transfer Envelope Checklist
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 13 of 43 Date Next Review: March 2021
WACHS Safe Transport and Transfer of Country Mental Health Patients Flowchart.MR36 WACHS Discharge Against Medical Advice FormMR46 WACHS Suicide Risk Assessment and Safety Plan
17.Related Policy DocumentsWACHS BACPAC Mental State Assessment.WACHS Chaperone PolicyWACHS Webpas Child at Risk Alert ProcedureWACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response PolicyWACHS Clinical observations and Assessments Clinical Practice Standard (physiological (vital signs), neurovascular, neurological and fluid balance)WACHS Mental Health Care in Emergency Departments and General Wards PolicyWACHS Working in Isolation - Minimum Safety and Security Standards for All Staff Policy
18.Policy FrameworkClinical Governance, Safety and QualityInformation Management
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 14 of 43 Date Next Review: March 2021
19.Appendices
Appendix 1 DefinitionsAppendix 2 Management of Presentations to ED in WACHS FacilitiesAppendix 3 Australasia Triage Score Categories Appendix 4 Triage Clinical DescriptorsAppendix 5 Triage Risk Factor Indicators for Review or Discussion with Medical
Officer / ED Nurse PractitionerAppendix 6 Symptoms Requiring Either Obstetric MP and/or Midwifery
Consultation before Discharge from the EDAppendix 7 Obstetric Triage Pathway for EDs in a Maternity HospitalAppendix 8 Pathway for Obstetric / Midwifery Advice by ED or ETS Staff at a
Non-maternity SiteAppendix 9 Nursing History for a Pregnant WomanAppendix 10 General Management Principles - General, Paediatric and Mental
Health - ATS 1 to 5 Appendix 11 Emergency Telehealth Service Referral Process
This document can be made available in alternative formats on request for a person with a disability
Contact: WACHS Coordinator of Nursing (V. Bloom)Directorate: Nursing and Midwifery Services EDRMS Record # ED-CO-16-73455
Version: 2.00 Date Published: 2 April 2020Copyright to this material is vested in the State of Western Australia unless otherwise indicated. Apart from any fair dealing for the purposes of private study, research, criticism or review, as permitted under the provisions of the Copyright Act 1968, no part may be reproduced or re-used for any purposes whatsoever without written permission of the State of Western Australia.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 15 of 43 Date Next Review: March 2021
Appendix 1 – Definitions
Advanced Life Support
Involves the management of a cardiac arrest or other medical emergencies in a clinical setting, and includes recognition of the critically ill patient, airway management (including LMA at some sites), resuscitation procedures, defibrillation and basic drug therapy.
Carer Carers provide unpaid care and support to family members and friends who have a disability, mental illness, chronic condition, terminal illness, an alcohol or other drug issue or who are frail aged (Carers Australia, 2015).
Close on call Appropriate health practitioner available to attend site within 10 minutes.
Consumer
A person who uses, or may potentially use, health services. Depending on the nature of the health service organisation, this person may be referred to as a patient, a client, a consumer, a customer or some other term. Consumers also include families, carers, friends and other support people, as well as representatives of consumer groups.
Continuous visual surveillance Patient is under direct visual observation at all times.
Direct supervision Direct supervision is considered to be in the company of an RN or medical practitioner or visually via an emergency tele-health service.
Emergency psychiatric treatment
Sections 202 – 204 of the MHA 2014 allow for emergency psychiatric treatment to be provided to a patient without informed consent: where treatment needs to be provided to save the person’s life, or where treatment needs to be provided to prevent the person from behaving in a way that is likely to result in serious physical injury to the person or another person.The MO who provides emergency psychiatric treatment must make a record of that treatment (Form 9A). A copy of the form must be provided to the person, the Chief Psychiatrist and, if the person is a mentally impaired accused, to the Mentally Impaired Accused Review Board. (OD 0657/16).
Triage system The process by which a clinician assesses a patient’s clinical urgency.
Triage A triage system is the basic structure in which all incoming patients are categorised into groups using a standard urgency rating scale or structure.
Urgency
Urgency is determined according to the patient’s clinical condition and is used to ‘determine the speed of intervention that is necessary to achieve an optimal outcome’. Urgency is independent of the severity or complexity of an illness or injury. For example, patients may be triaged to a lower urgency rating because it is safe for them to wait for an emergency assessment, even though they may still eventually require a hospital admission for their condition or have significant morbidity and attendant mortality.
WACHS Clinical Practice Standard – Assessment and Management in the Emergency Department
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: September 2019 Page 16 of 43 Date Next Review: March 2021
Appendix 2 - Management of Patient Presentations to ED in WACHS Facilities
INITIAL REFERRALTelephone Self Presentation
Caller needing an emergency vehicle to attend?
Yes No
Scheduled Appointment?No Yes
Is the patient stable?
Yes
No
DO NOT Triage (MR1) - instead
complete an MR5
EMERGENCY TRIAGE(Primary Survey – ABCD)
PRIMARY ASSESSMENTS.A.M.P.L.E. & ADPIE
NOTIFICATIONS
SECONDARY ASSESSMENT
ED DISCHARGE PLANNING AND DISPOSITION
Neuro-logicalTrauma Eye ENT Cardio-
vascular Renal Respir-atory
Gastro-intestinal
Repro-ductive
Musculo-skeletal
Integu-ment
Mental Health
Direct them to call ‘000’ immediately
Redirected to Clinical Resources e.g. HealthDirect and Rural Link, Clinics. This may also include directing them to present
to your Health Facility
Observation and Response Early Recognition Escalation Criteria MER / CODE BLUE ACTIVATION
NOTIFICATIONS
NOTIFICATIONS
PATIENT MONITORING
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: September 2019 Page 17 of 43 Date Next Review: March 2021
Appendix 3 - Australasian Triage Score Categories
The time allocated to each ATS category describes the maximum time a patient can safely wait for medical assessment and treatment (ACEM 2013 & 2016). All ATS 1-3 and any in Appendix 5 must be reviewed by MO or NP.
ATS DESCRIPTION OF CATEGORYRESPONSEKey Performance Indicator
National Target Times
1 Immediately life-threatening - Conditions that are threats to life (or imminent risk of deterioration) and require immediate aggressive treatment.
Immediate - Simultaneous assessment and treatment
100%
2
Imminently life-threatening condition or deteriorating so rapidly that there is the potential of threat to life/foetus/organ system failure or important time-critical intervention e.g. antidote, thrombolysis, or human practice mandates the relief of very severe discomfort/pain or distress. Pain score 7-10 (severe)
Within 10 minutes - Assessment and treatment
80%
3Potentially life-threatening – may progress to life or limb threatening, or may lead to significant morbidity, or potential for adverse outcome or time-critical treatment; or human practice mandates the relief of severe discomfort or distress. Pain score 4-6 (moderate).
Within 30 minutes - Assessment and treatment
75%
4
Potentially life-serious condition may deteriorate, or possible adverse outcome or time-critical treatment; Symptoms moderate or prolonged or situational urgency or significant complexity or severity likely to require complex work-up and consultation and/or inpatient management or human practice mandates the relief of severe discomfort or distress. Pain score 1-3 (mild)
Within 60 minutes - Assessment and treatment start
70%
5
Less urgent - the patient’s condition is chronic or minor enough that symptoms or clinical outcome will not be significantly affected if assessment and treatment are delayed or clinic-administrative problems e.g. request for prescription only; results review; medical certificate. Pain score 0 (no pain)
Within 120 minutes - Assessment and treatment start
70%
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 18 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors – Airway and Breathing(Note: This list is not exhaustive; advice should be sought for any other concern relating to safety of a patient (ACEM 2016).
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
AIRWAY
ALL P
ATIE
NTS
Immediate risk to airway:
Completely obstructed Partially obstructed Threatened airway
(swelling / facial burns) or airway management required
Patent Airway risk– severe
stridor or drooling with distress
Partially obstructed with moderate respiratory distress
Patent Partially obstructed
with mild respiratory distress
Able to verbalise
Patent Foreign body
aspiration with no respiratory distress
Patent
BREATHING ADUL
TS
Extreme respiratory distress:
Absent respiration/respiratory arrest
RR<10 or >36 Hypoventilation SpO2
<85%
Severe respiratory distress:
RR <10 or >29-35 SpO2 85-90%
Moderate Respiratory Distress:
Moderate shortness of breath
RR 25-29 SpO2 91 – 94%
Mild or no Respiratory Distress:
- RR 20-24 - SpO2>94% Chest injury without
rib pain or respiratory distress
Difficulty swallowing, no respiratory distress
No respiratory distress
RR 10-20 Sp02>94%
For additional information on paediatric patients please refer to Emergency Triage Education Kit – Chapter 8: Paediatric Triage.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 19 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Breathing Continued
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
BREATHING
PAED
IATR
IC
Extreme respiratory distress:
Absent respiration Hypoventilation Severe respiratory
distress e.g. severe use accessory muscle, severe retraction, acute cyanosis
RR and SpO2 dependant on parameters for ORC age range
Severe respiratory distress:
Moderate use accessory muscles, moderate retraction, skin pale
RR and SpO2 dependant on parameters for ORC age range
Mild-moderate respiratory distress:
Mild use accessory muscles, mild retraction, skin pink
RR and SpO2 dependant on parameters for ORC age range
No Respiratory Distress:
RR and SpO2 dependant on parameters for ORC age range
No respiratory distress
For additional information on paediatric patients please refer to Emergency Triage Education Kit – Chapter 8: Paediatric Triage.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 20 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Circulation
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
CIRCULATION
ADUL
TS
Severe circulatory compromise:
Absent circulation/Cardiac arrest
SBP<90 Heart rate<40 or
>140 Uncontrolled
haemorrhage
Moderate circulatory compromise:
Clammy, mottled skin, skin pale, cool, poor perfusion
Heart rate <50 or 120-140
Hypotension SBP<90 or Hypertension SPB 200+
Severe blood loss Chest pain Fever 38° C+ with
signs of lethargy (any age)
Suspected sepsis (haemo-dynamically unstable)
Febrile neutropenia- immunosuppressed, oncology or steroid therapy
Hypothermia <35.0°C
Mild circulatory compromise:
Palpable peripheral pulses, skin pale, warm
Mild tachycardia HR 110-119
Severe hypertension SBP 160-200
Moderately severe blood loss – any cause
Suspected sepsis (haemodynamically stable)
Persistent vomiting Dehydration
No circulatory compromise:
Skin pink and warm, no alteration in vital signs
Mild haemorrhage Vomiting or
diarrhoea without dehydration
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 21 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Circulation Continued
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
CIRCULATION
Paediatric signs and symptoms (s/s) of dehydration:
- ↓LOC/activity- Cap refill> 2 secs- Dry mucous
membranes - Absent tears- Sunken eyes/
fontanelles- ↓Tissue turgor- Deep respirations- Thready/weak pulse- Tachycardia- ↓Urine output / <4
wet nappies in 24hrs
- Weight loss >4-5%
PAED
IATR
IC
Severely Shocked Child:
Absent circulation Significant
bradycardia e.g. <60 in an infant
Severe haemodynamic compromise (absent peripheral pulses, skin pale, cold, moist mottled, significant tachycardia as per ORC for age range; capillary refill >4 seconds)
Uncontrolled haemorrhage
Moderate circulatory compromise:
Skin pale, cool, moderate tachycardia as per ORC for age range, capillary refill 2-4 seconds
>6 s/s dehydration Fever with signs of
lethargy/ increased irritability (any age)
Any neonate or corrected preterm age < 28 days
Age < 3 months and febrile (38.0°C)
Age < 5 years, febrile (38.5°C) and with signs of lethargy or increased irritability or rash or co-morbidities
Mild circulatory compromise:
Palpable peripheral pulses, skin pale, warm
Mild tachycardia as per ORC for age range
3-6 s/s dehydration
No circulatory compromise:
Palpable peripheral pulses, skin pink warm and dry as per ORC for age range)
<3 s/s dehydration
No s/s of dehydration
For additional information on paediatric patients please refer to Emergency Triage Education Kit – Chapter 8: Paediatric Triage.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 22 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Disability
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
DISABILITY ADUL
TS
AVPU- Unresponsive Glasgow Coma Score
GCS< 8 Ongoing/prolonged
seizure Pupils: fixed and
dilated (Indication of possible drug overdose or head trauma)
IV drug overdose and unresponsive or hypoventilation
AVPU- responds to pain only
GCS 9 – 12 Drowsy, decreased
responsiveness of any cause
Sudden severe headache with altered GCS
BSL <3 or >19 mmol Suspected provisional
diagnoses (Acute stroke, meningococcemia)
Significant sedative or other toxic ingestion
Significant or dangerous envenomation
AVPU- responds to voice
GCS >13 Sudden severe
headache with normal GCS
BSL > 16-18 mmol Head injury with short
loss of consciousness, now alert
Seizure, now alert Suspected stroke
Normal GCS or no acute change to usual GCS
AVPU - Alert Minor head injury,
no loss of consciousness
Normal GCS
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 23 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Disability and Pain
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
DISABILITYPA
EDIA
TRIC
GCS <8 Ongoing / prolonged
seizure
GCS 9 – 12 Severe decreases in
activity (no eye contact, decreased muscle tone)
Significant sedative or other toxic ingestion
Significant / dangerous envenomation
GCS >13 Moderate decrease in
activity (lethargic, eye contact when disturbed)
Normal GCS or no acute change in usual GCS
Mild decrease in activity (quiet but eye contact, interacts with parents)
Normal GCS No alteration
to activity (playing, smiling)
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 24 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Neurovascular and Trauma
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
PAIN
ALL P
ATIE
NTS
Very severe pain (pain score 7-10) requiring analgesia, affecting physical capacity emotions and or behaviour. Including possible: cardiac cause, acute myocardial infarction, AMI, PE, aortic dissection, pulmonary embolus, aortic dissection, abdominal aortic aneurysm, ectopic pregnancy, ischaemic leg, ischaemic gut, renal colic, dislocated hip or shoulder
Moderate severe pain (pain score 4-6) requiring analgesia
Chest pain likely non-cardiac
Abdominal pain without high risk features of moderate-severe pain or patient age >65 years
Moderate pain (pain score 1-3) some risk features and/or requiring analgesia
Non-specific abdominal pain
Minimal pain
For additional information on paediatric patients please refer to Emergency Triage Education Kit – Chapter 8: Paediatric Triage.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 25 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Neurovascular and Trauma
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
NEUROVASCULAR
ALL P
ATIE
NTS
Severe neurovascular compromise; pulseless, cold, nil sensation, nil movement, cap refill
Moderate neurovascular compromise; pulse present or acutely absent, cool, sensation, movement and / or cap refill
Mild neurovascular compromise; pulse present, normal/ sensation, movement and/or cap refill
Tight cast- with no neurovascular impairment
Swollen ‘hot’ joint/s
No neuro-vascular compromise
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 26 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Neurovascular and Trauma
TRAUMAALL PATIENTS
- Major multi trauma
Major multi trauma (requiring rapid organised response)
Severe localised trauma – major fracture, amputation
Suspected testicular torsion
Moderate limb injury – deformity, severe laceration, crush injury
Trauma – high risk history with no other high-risk features
Child at risk of abuse/suspected non-accidental injury
Minor limb trauma – sprained ankle, possible fracture
uncomplicated laceration requiring investigation or intervention
Minor wounds – small abrasions, minor lacerations (not requiring suturing)
Major trauma criteria ATS1 or 2:- Penetrating injury- Fall > 3 metres (paediatric fall >1m)- MCA > 60kph; MBA / cyclist > 30kph; Pedestrian- Explosion- Ejection/rollover- Prolonged extrication (>30min)- Death in same vehicle
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 27 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Ophthalmic and High Risk History or Clinico-Administrative
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
OPHTHALMICALL PATIENTS
Penetrating eye injury Chemical Injury (Acid or
alkali splash to eye) – requiring irrigation
Sudden loss of vision or pain with or without injury
sudden onset of pain, blurred vision AND red eye
Suspected endophthalmitis post eye procedure (post cataract, post intravitreal injection)
Sudden abnormal vision with or without injury
Moderate eye pain e.g. blunt eye injury, flash burns, foreign body
Eye inflammation or foreign body with normal vision
Low-risk history and now asymptomatic
Minor symptoms of existing stable illness or low risk condition.
Patient requesting medical certificates, prescriptions.
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 28 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Neurovascular and Trauma
HIGH RISK HISTORY orCLINICO-ADMINSTRATIVEALL PATIENTS
Child protection issues
No safe environment to discharge patient to
Stable neonate
Patients presenting as worker’s compensation
Any other reason for concern requiring MO review
Parental concern (mandatory MO or NP review)
Age >65 or <1monthChemical exposure
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 29 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Mental Health
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
MENTAL HEALTHALL PATIENTS
Risk:Definite danger to life (self or others). Severe behavioural disorder. Immediate threat of dangerous violence.
Observed: Extreme or Violent
behaviour Possession of
weapon Self-destruction in
ED Displays extreme
agitation or restlessness
Bizarre/disoriented behaviour
Reported: Verbal commands
to do harm to self or others, that the person is unable to resist (command hallucinations)
Risk: Probable risk of danger (self or others)
Observed: Severe agitation/
restlessness Physically/verbally
aggressive Confused/unable to
cooperate Hallucinations/delusions/
paranoia Requires or has required
restraint / containment High risk of absconding
and not waiting for treatment
Reported: Attempt at self-harm /
threat of self-harm Immediate threat of harm
to others Unable to wait safely
Risk: Possible danger to self or others; very distressed; risk of self-harm or has deliberately self-harmed
Observed: Agitated/restless Intrusive behaviour Confused Withdrawn/ambivalenc
e about treatment Not likely to wait for
treatment Potentially aggressive
Reported: Suicidal ideation Situational crisis
Presence of psychotic symptoms:
Hallucinations Delusions Paranoid ideas
Risk:Under observation and/or no immediate risk to self or others.
Observed: No agitation/
restlessness Irritable without
aggression Cooperative Patient provides
coherent history
Reported: Semi urgent mental
health problem Pre-existing mental
health disorder Symptoms of
anxiety or depression, without suicidal ideation
Willing to wait
Risk:No danger to self or others. No acute distress or behavioural disturbance
Observed: Cooperative Communicative
and able to engage in developing management plan
Able to discuss concerns
Compliant with instructions
Reported: Pre-existing non-
acute mental health disorder with chronic psychotic symptoms, social crisis, clinically well patient
If in police custody or on Mental Health forms consider clinical escalation
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 30 of 43 Date Next Review: March 2021
Appendix 4 - Triage Clinical Descriptors Mental Health Continued
Category 1(immediate)
Category 2(10 minutes)
Category 3(30 minutes)
Category 4(60 minutes)
Category 5(120 minutes)
MENTAL HEALTHALL PATIENTS
Risk:Definite danger to life (self or others). Severe behavioural disorder. Immediate threat of dangerous violence.
Observed: Recent violent
behaviour
Risk: Possible danger to self or others; very distressed; risk of self-harm or has deliberately self-harmed
Observed: Thought disordered Bizarre/agitated
condition Presence of mood
disturbance: Severe symptoms of
depression Withdrawn/uncommuni
cative and/or anxiety Elevated or irritable
mood
Risk:No danger to self or others. No acute distress or behavioural disturbance
Observed: Request for
medication Minor adverse
effect of medicationIf in police custody or on
Mental Health forms consider clinical escalation
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: January 2020 Page 31 of 43 Date Next Review: March 2021
Appendix 5 - Triage Risk Factor Indicators for Review or Discussion with Medical Officer / ED Nurse Practitioner(Note: This list is not exhaustive and in addition to the items described, advice is to be sought for any other concern relating to the health or safety of a patient.)
Airway / Breathing Cardiovascular Neurosensory Trauma Any patient on oxygen Apnoeic / cyanotic episode History of severe/anaphylactic
allergy response and presenting with allergic reaction
Asthma not relieved by actions outlined in the patient’s emergency / national asthma action plan
audible wheeze, snoring in presenting complaint
Irregular pulse rate, that is not normal for the patient
Unexplained fall in urine output (< 10ml in 3 hrs)
First convulsion Seizure activity-
intermittent Collapse Loss of sensation in any
body part Decreased / loss of
movement or weakness in any body part
Any head and eye injury
Injury to chest, abdomen or neck
Alleged / suspicion of physical and / or sexual assault
Paediatric Medical History Infection Seizure activity Decreased intake / output Red currant jelly stool Bile stained vomit Actual / potential effects of drugs / alcohol Age < 2 years any discharge Age <1 month (including corrected age) with:
Febrile convulsions Acute changed to feeding pattern Acute change to sleeping pattern
Any undifferentiated diagnosis
Exacerbation of chronic condition, where the patient’s care plan identifies need for medical review.
History rheumatic fever or prosthetic valve
Representation with similar or same symptoms within 48 hours
Age >65
Oedema of bony areas around facial sinuses
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 32 of 43 Date Next Review: March 2021
Appendix 6 – Symptoms in the Pregnant or Postnatal Woman Requiring Either Obstetric MP and/or Midwifery Consultation before Discharge from the ED
Presenting Symptoms (pregnant) Possible Complications
Any symptoms below should prompt the triage RN to take a BP:
Headache, or Blurred vision / visual disturbance, or Epigastric pain, or Hyper-reflexia / hypertonus, or Swelling of hands, face or legs, or Proteinuria
Blood pressure 140/90 or more, or increase of 30/15 mmHg above pre-pregnancy BP
Pre-eclampsia Pregnancy Induced
Hypertension Eclampsia (seizure) HELLP syndrome (haemolysis,
elevated liver enzymes, low platelets) – can result in DIC (disseminated intravascular coagulopathy)
Diagnostic tests required: FBC LFTs Coag profile PCR
Any abdominal pain: Intermittent, or Crampy, or Constant, or with or without back pain, or Rigid abdomen, not relaxing Epigastric pain
Early labour including preterm Placental abruption Chorioamnionitis Epigastric pain – can be a sign
of severe pre-eclampsia
UTI symptoms under 37 weeks: Frequency, or Burning, or Offensive urine, or Cloudy urine
UTI is the most common trigger of preterm labour
Preterm labour can only be excluded by Obstetric consult
Gastroenteritis associated with intermittent abdominal pain less than 37 weeks
Sepsis (can be afebrile) Gastro may trigger preterm
labour
Any fluid loss per vagina (or loss suspected by the woman): Spotting, or Bleeding, or Clear or coloured or offensive fluid
Early labour (including preterm) Ruptured membranes Chorioamnionitis Placental abruption – can
trigger coagulopathy Massive maternal haemorrhage
Woman complains of reduced (less than normal or change in type) or absent fetal movements
Unwell fetus requires biophysical profile by Obstetric Sonographer
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 33 of 43 Date Next Review: March 2021
Presenting Symptoms (pregnant) Possible Complications
Woman complains of reduced (less than normal or change in type) or absent fetal movements
Unwell fetus Requires biophysical profile by
obstetric sonographerAny abdominal trauma, particularly arising from: MVA / seatbelt Fall Assault
Placental abruptionPotential outcomes: Concealed massive maternal
haemorrhage Unwell fetus / death Preterm labour Severe coagulopathy
Umbilical cord prolapsed from the vaginaPostnatal up to 6 weeks Possible Complications
Any symptoms below should prompt the triage RN to take a BP:
Headache, or Blurred vision / visual disturbance, or Epigastric pain, or Hyper-reflexia / hypertonus, or Swelling of hands, face or legs, or Proteinuria
Blood pressure 140/90 or more, or increase of 30/15 mmHg above Pre-pregnancy BP
Hypertension due to pre-eclampsia can re-bound after birth (generally on the 3rd of 4th day within the first week)
Hx of epidural or spinal for birth: Pain or inflammation at the epidural / spinal site, or Sensory or motor deficits in the lower limbs (one or both), or
Fever 38 or more
Epidural haematoma or epidural abscess
Discuss with Anaesthetist
Unwell with temperature greater than 38 or less than 35.5 twice
Sepsis
Changes to vaginal loss: Increased bleeding or clots since birth, orOffensive vaginal discharge
Retained products of conception
Endometritis Retained vaginal pack (if
required perineal suturing)
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 34 of 43 Date Next Review: March 2021
Presenting Symptoms (pregnant) Possible Complications
Any signs of endometritis – mild fever or lower abdominal pains
Any symptoms of urinary retention / incontinence: Dribbling or Urge incontinence or Small volumes or Bladder pain or Dysuria or Frequency or Haematuria.
Bladder over-distension injury (particularly if Hx Epidural)
Birth trauma (particularly if Hx instrumental vaginal birth or caesarean)
UTI
Pregnant or Postnatal up to 6 weeks
Symptoms of postnatal depression 1 in 5 women at risk
Red or hot or tender spots on calves Deep vein thrombus
Red or hot or tender spot/s on breast/s+/- Fever or flu like symptoms Mastitis or breast abscess
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 35 of 43 Date Next Review: March 2021
Appendix 7 - Obstetric Triage Pathway for EDs with a Maternity Service
WACHS Assessment and Management in the Emergency Department Clinical Practice Standard
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 36 of 43 Date Next Review: March 2021
Appendix 8 – Pathway for Obstetric / Midwifery Advice by ED or ETS Staff at a Non-maternity Service Sites
WACHS Clinical Practice Standard – Assessment and Management in the Emergency Department
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 37 of 43 Date Next Review: March 2021
Appendix 9 – Nursing History for a Pregnant Woman
1. What date is your baby due? If due date known – use a pregnancy wheel to calculate gestation based on
due date and current date If due date not known –
o If date that last menstrual period started is known then use a pregnancy wheel to determine due date and current gestation
o Has she seen a doctor or midwife this pregnancyo Has she had an ultrasound done anywhere?o Assess abdomen (if normal BMI),
fundus felt above umbilicus = more than 20 weeks Fundus felt below umbilicus = less than 20 weeks
2. How many pregnancies have you had (Gravida)? How many births have you had after 2O weeks (Parity)?
If they have had a baby before, o did they have any complications in pregnancy or during birtho have they had any caesarean births
3. Have you had any antenatal visits in this pregnancy? Where was your antenatal care? Where are you booked to have your birth? Have you had any problems with this pregnancy
4. If more than 26 weeks – have you felt your baby moving today?5. Have you had any blood or fluid leaking from your vagina?
Describe how much? Can you show me? If yes, place a pad in situ and reassess after lying down for 30 minutes
6. Have you had any abdominal pain? Is the pain constant? Is the pain intermittent or crampy? Is there a pattern to the pain? Tell me
when a pain comes and when it goes (time the frequency of the pain while assessing the woman)?
If they have had a labour / birth before – does it feel like pains in your last labour?
7. Do you have any of the following (if yes, requires a BP check)? Headache Spots before your eyes Swelling in face or hands Pitting oedema of legs Epigastric pain
WACHS Clinical Practice Standard – Assessment and Management in the Emergency Department
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 38 of 43 Date Next Review: March 2021
Appendix 10 - General Management Principles – ATS 1 – Adult & Paediatric – Mental Health
ATS Category General (adult and paediatric) Mental Health
1
Action: Continuous cardiac monitoring, SpO2
MET call activation Transfer the patient to the resuscitation area
immediately Alert the resuscitation nurse and medical
staff immediately for commencement of immediate simultaneous assessment and treatment
Activate local emergency response protocols (If not on site immediately contact ETS/ RRC/RFDS for assistance/advice).
Consider: Alerting theatre Radiology and pathology for
emergency intervention Alerting ambulance service / RFDS for
emergency transfer dependent on local service capacity.
Supervision: Continuous visual surveillance
Action: Alert medical staff immediately Alert community mental health team / RuralLink (Free call
1800 552 002 – TTY 1800 720 101) Child and Adolescent Acute Response Team 1800048636 as appropriate to day, time and site.
Provide safe environment for patient or others Alert senior nurse to prepare for personnel to assist with any
required emergency psychiatric treatment.
Consider: Calling an emergency Code Black for assistance, as per local
procedure, if required Calling police +/- security if staff or patient safety is
compromised Intoxication by drugs and alcohol may cause escalation in
behaviour that requires management Use of WACHS Sedation for mental health patients awaiting
RFDS transfer from remote regions guideline.
WACHS Clinical Practice Standard – Assessment and Management in the Emergency Department
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 39 of 43 Date Next Review: March 2021
Appendix 10 - General Management Principles - ATS 2
ATS Category General (adult and paediatric) Mental Health
2
Action: Transfer the patient to the resuscitation /
treatment area immediately Continuous cardiac monitoring, SpO2 Triage nurse to weigh child/infant Alert a registered nurse for commencement
of immediate simultaneous assessment and treatment
Alert medical staff immediately for commencement of assessment and treatment
Activate local emergency response protocols. (If not on site immediately contact ETS/ RRC/RFDS for assistance/advice)
Consider: Alerting theatre for emergency intervention. Alerting ambulance service/RFDS for
emergency transfer dependent on local service capacity.
Supervision: Continuous visual surveillance.
Action: Alert medical staff immediately, for prompt assessment for
consideration of referral under the Mental Health Act. Alert community mental health team/RuralLink/ (Free call
1800 552 002 – TTY 1800 720 101) Child and Adolescent Acute Response Team 1800048636 as appropriate to day, time and site
Provide safe environment for patient or others Use defusing techniques (oral medication, time in quieter
area) Alert senior nurse to prepare for personnel to assist with any
required emergency psychiatric treatment Prompt assessment for patient recommended.
Consider: If diffusing techniques ineffective, escalate care Police +/- security/ additional staff until patient sedated Intoxication by drugs and alcohol may cause escalation in
behaviour that requires management.
WACHS Clinical Practice Standard – Assessment and Management in the Emergency Department
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 40 of 43 Date Next Review: March 2021
Appendix 10 - General Management Principles – ATS 3
ATS Category General (adult and paediatric) Mental Health
3
Action: Transfer the patient to the treatment area as
appropriate Triage nurse to weigh child/infant. Commence first aid and comfort measures
(ice for pain and swelling, sling for arm) Hand over patient to a nurse or MO for
consideration of assessment and treatment If patient able to remain in waiting room,
triage nurse to observe patient and perform physiological observations and document at 30 minute intervals.
Supervision: Close visual observation at a maximum of 10 minute intervals
must be documented - do not leave in the waiting room without support person
Action: Alert community mental health team/RuralLink (Free call 1800
552 002 – TTY 1800 720 101) Child and Adolescent Acute Response Team 1800048636 as appropriate to day, time and site
Ensure safe environment for patient and others.
Consider: Clinical escalation if evidence of increasing behavioural
disturbance, such as restlessness, intrusiveness, agitation, aggressiveness, increasing distress or threats of harm to self or others
Alert nurse coordinator / security that patient is in the department, for code black preparedness
Intoxication by drugs and alcohol may cause escalation in behaviour that requires management.
WACHS Clinical Practice Standard – Assessment and Management in the Emergency Department
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 41 of 43 Date Next Review: March 2021
Appendix 10 - General Management Principles – ATS 4
ATS Category General (adult and paediatric) Mental Health
4
Action: Patient may wait in the waiting room, advise
patient may not to drink or eat anything until assessed (presentation dependent)
Triage nurse to weigh child/infant Commence first aid and comfort measures
e.g.: ice for pain and swelling, elevation of swollen limb, clean dressing and patient applied pressure
Hand over patient to a nurse or MO for prioritisation of assessment and treatment
If patient able to remain in waiting room, triage nurse to observe the patient and perform physiological observations and document at hourly intervals.
Supervision: Intermittent regular observation at a maximum of 30 minute
intervals, must be documented.
Action: Discuss with community mental health team/RuralLink (Free
call 1800 552 002 – TTY 1800 720 101) Child and Adolescent Acute Response Team 1800048636 as appropriate to day, time and site. May not occur if patient’s treating General Practitioner is the Visiting Medical Practitioner who assesses the patient
Referral information must be provided to consumer prior to discharge.
Consider: Clinical escalation if evidence of increasing behavioural
disturbance, such as restlessness, intrusiveness, agitation, aggressiveness, increasing distress
Referral for follow-up with community mental health team on discharge / admission
Intoxication by drugs and alcohol may cause escalation in behaviour that requires management.
WACHS Clinical Practice Standard – Assessment and Management in the Emergency Department
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 42 of 43 Date Next Review: March 2021
Appendix 10 - General Management Principles – ATS 5
ATS Category General (adult and paediatric) Mental Health
5
Action: Patient may wait in the waiting room, advise
patient may not to drink or eat anything until assessed (presentation dependent)
Triage nurse to weigh child/infant Commence first aid and comfort measures
e.g. ice for pain and swelling, elevation of swollen limb, clean dressing and patient applied pressure
Hand over patient to nurse or MO for prioritisation of assessment and treatment
If patient able to remain in waiting room, triage nurse to observe the patient and perform physiological observations and document at two hourly intervals observe the patient .
Supervision: General observation -routine waiting room check at 30 minute
intervals, must be documented
Action: Discuss with community mental health team/RuralLink (Free
call 1800 552 002 – TTY 1800 720 101) Child and Adolescent Acute Response Team 1800048636 as appropriate to day, time and site
Refer to treating team if case-managed Referral information must be provided to consumer prior to
discharge.
WACHS Clinical Practice Standard – Assessment and Management in the Emergency Department
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: February 2020 Page 43 of 43 Date Next Review: March 2021
Appendix 11 – Emergency Telehealth Service Referral Process
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 1 of 32 Date Next Review: December 2019
Effective: Effective: 29 January 2018
Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response Policy
1. Background This policy addresses the requirements for early recognition of acute physiological deterioration and clinical escalation, including Medical Emergency Response (MER) for adult, maternity, newborn and paediatric patients, inclusive of mental health inpatients and aged care residents within WACHS healthcare facilities. Where a MER is required outside the health campus, ambulance assistance is to be sought by dialling 000 (WACHS staff may be first responders). Consistent with the National Consensus Statement: Essential Elements for Recognising and Responding to Clinical Deterioration, each WACHS healthcare facility must have a formal documented escalation procedure that is appropriate to the size, role and staffing mix of the hospital, which sets out actions required to respond to different levels of abnormal physiological observations. The processes should be documented using the relevant endorsed templates (See Appendices 1-4). Early intervention has been shown to reduce mortality and morbidity in the critically ill patient. The decision to initiate a MER call is made in response to established criteria on the observation and response charts and in consideration of the situation at the time e.g. staff available/staffing mix. This Policy does not include the processes to recognise and escalate mental state deterioration.
2. Policy Statement
This policy is to be read in conjunction with National Consensus Statement: Essential Elements for Recognising and Responding to Clinical Deterioration, and the WA Health Acute Deterioration Policy and Guideline (pending publication).
2.1 Observation and Response Charts The following observation and response charts are endorsed for use in WACHS:
Adult Observation and Response Chart (AORC, MR 140a) Maternal Observation and Response Chart (MORC, MR140b) Newborn Observation and Response Chart (NORC, MR140d). This chart
is for use in newborns <1 month in Special Care Nursery, and newborns on the postnatal ward if perinatal risk factors are identified (e.g. any resuscitation at birth, meconium stained liquor, risk of early onset sepsis, <37 weeks gestation, <2500g) and/or an observation is abnormal. Refer to WACHS Recognition and Management of the Newborn at Clinical Risk Policy.
Paediatric Observation and Response Charts (PORC, MR 140e – i)
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 2 of 32 Date Next Review: December 2019
Modifications In keeping with the WA Health Acute Deterioration Policy and Guideline, modifications to the response criteria can only be made in exceptional circumstances and should only be made by consultants, or by the most senior doctor available in smaller sites. Modifications can only be made following a full review of the patient, and with sound clinical rationale and justification documented. Where a health service is covered utilising a senior doctor whom is remotely on call in a single location or Emergency Telehealth Service, the modification (i.e. written on the front of ORC) may be electronically transmitted via fax, email, or endorsed electronic system e.g. MMeX to the doctor’s location for signing and then faxed back for inclusion in the medical record in accordance with IC 0179/14 Guidelines for the Transmission of Client Identifiable Health Information by Facsimile Machine. If electronic transmission occurs the hard copy document with the doctor’s original signature MUST be kept at the site from which the doctor authorised the modification.
2.2 Escalation and Medical Emergency Response Procedures
2.2.1 Escalation of Physiologically Deteriorating Patient Each site is to identify the internal and external contacts to assist with any adult, maternal or paediatric escalation and MER procedures. At some sites Medical Review and MER may be via telephone or videoconference e.g. Emergency Telehealth Service.
Escalation and MER processes are to be completed for each WACHS clinical site, and each WACHS site providing an emergency service. The processes should be documented using the relevant endorsed templates (See Appendices 1-4).
If at any time, the escalation process is not progressing in a timely manner, the staff member may contact the Regional Director Nursing & Midwifery or Medical Director for advice or assistance.
Remote Area Nurses (RANs) are encouraged to maintain one point of contact and only contact the Medical Officer (MO), Director of Nursing (DON) or Hospital Service Manager (HSM) on call for the site. The MO is responsible for contacting the specialist/s for further advice. RANs and contact MO/DON/HSMs are to make use of conference phone calls where possible, and include specialists and transport service officers in discussions regarding patient management with a view to minimising the number of phone calls and relayed messages required to provide optimal care. WACHS endorses the Australian and New Zealand Committee on Resuscitation (ANZCOR) guidelines and flowcharts for Basic and Advanced Life Support (Adult, Infants and Children). See Appendices 5-7.
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 3 of 32 Date Next Review: December 2019
WACHS endorses both the ANZCOR Newborn guidelines and flowcharts (Appendix 8) and the King Edward Memorial Hospital Resuscitation Algorithm for the Newborn. When applied, the information contained in these guidelines must take account of the context and scope of practice, level of service delivery and facility capacity.
2.2.2 Medical Emergency Response A Code Blue emergency call should be placed for all patients with MER criteria (purple zone observations, or red zone on PORC series), airway threat, respiratory or cardiac arrest, sudden fall in consciousness, oxygen saturations ≤ 84%, seizure, unattended medical review or you or a family member are concerned.
All MER calls are to be documented on either the – MR 140 Medical Emergency Response (MER) / Code Blue Record MR 75B Newborn Medical Emergency Response (MER) Record
The senior nurse is to ensure a MER record form is completed for every MER. All MER events require a regional process for clinical review, and results should be tabled at appropriate regional committees.
The outcome and events preceding every MER are to be assessed by a senior nurse or medical officer to determine if a clinical incident has occurred. Where a clinical incident is considered to have occurred this is to be reported in the Datix Clinical Incident Management System (CIMS) and investigated in accordance with the Operational Directive OD 0611/15 WA Health Clinical Incident Policy.
2.2.3 Call and Respond Early (CARE) Call CARE is a consumer-centred approach allowing patients, their families or carers to call for assistance when they feel they are worried. CARE is an additional protective process that supports established strategies to improve the recognition and response to physiological deterioration.
CARE comprises 3 steps: Step 1- Reminds the patient, their family or carer to talk to the nurse, midwife or doctor caring for them if they have any concerns about the health of themselves or their loved one. Step 2 - Encourages the patient, family member or carer to ask to speak to the shift coordinator /nurse/midwife in charge if they still have concerns and feel that these have not been addressed by their primary carer. Step 3 - Provides the ability for the patient, family or carer to make a CARE call and speak to another clinician if they still have concerns that they don't feel have been adequately addressed.
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 4 of 32 Date Next Review: December 2019
When a CARE call is made, a senior staff member should listen to the concerns of the person who made the CARE Call, and make a full assessment of the patient’s situation, liaising with the treating medical team and other health care providers as required.
2.3 Clinical Area Specific Information/Special Considerations
2.3.1 Maternity and Newborns Maternity and newborn care is a specialised area and is often already staffed by the most appropriate responders to physiological deterioration. Specialist staff are to be contacted immediately in the event of suspected physiological deterioration e.g. on call midwife, on-call obstetric medical officer, paediatric medical officer. For obstetric or newborn emergencies, immediate advice regarding the most appropriate management plan including stabilisation and transfer is available by:
Contacting the regional obstetrician and/or paediatrician on call King Edward Memorial Hospital on-call consultant (08) 6458 2222. Neonatal Emergency Transport Service (NETSWA) 1300 638 792.
WACHS has endorsed the clinical guidelines produced by KEMH including Resuscitation Algorithm for the Newborn, and the ANZCOR2 guidelines for Newborn Life Support Flowchart (Appendix 8). 2.3.2 Paediatric Special considerations for paediatric patients are addressed in the various age appropriate paediatric observation and response charts. The paediatric escalation and MER procedure templates (Appendix 2 and 4) are aligned with the ‘actions required’ described on the escalation zone criteria section in paediatric charts. WACHS has endorsed the ANZCOR2 guidelines and Advanced Life Support for Infants and Children Flowchart for basic and advanced life support (see Appendices 5 and 7) to guide practice.
2.3.3 Emergency Department All patients that present to WACHS facilities that provide emergency care will have observations recorded on the WACHS observation and response charts at the time of primary assessment, and no patient should be discharged or transferred from ED with abnormal vital signs without a medical review and a comprehensive management plan which may include modifications and follow up if required. Sites are required to document their escalation and MER processes on the Emergency Department - Adult and Maternity, or Paediatric Observation and Response Escalation and MER templates (Appendices 3 and 4). Note: The observation and response charts, and escalation and MER process templates are not for use when triaging patients. Refer to Triage, Assessment and Management in the Emergency Department - Clinical Practice Standard.
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 5 of 32 Date Next Review: December 2019
2.3.4 Mental Health There is overwhelming evidence indicating poor physical health outcomes for people with mental illness, often as the result of a delay in recognising and escalating the patient’s physiological deterioration. This Policy applies to all WACHS mental health patients. If the patient’s mental health condition is hindering the escalation of their physiological deterioration, consider the following use or review of PRN and routine medications contact:
the patients treating psychiatrist or the local mental health team or RuralLink (Free call 1800 552 002 – [TTY] 1800 720 101).
2.3.5 Theatre and Recovery These are specialised areas in which the most appropriate respondents to clinical deterioration are often present, thus it may not always be appropriate to call the MER team. Local escalation plans for the area are to be followed.
2.3.6 Older Person An atypical disease presentation is the most common illness presentation in the elderly. Vague and nonspecific complaints are not to be dismissed as they may be signs of a medical emergency. An acute deterioration of mental state is an early marker of a serious condition. Early recognition and escalation can improve the older person’s health outcomes and reduce rates of co morbidities for treatable geriatric syndromes. If an atypical presentation of illness in an older person, or changes in vital signs are identified, or if staff are concerned about the person, a senior nurse must undertake full assessment and a medical officer must review the person (see Appendix 9).
2.4 Equipment
2.4.1 Refrigerated Medications Resuscitation medications that require refrigeration are to be stored in an appropriate area that is easily accessible in the event of a MER. The team leader is to ensure that these medications accompany the MER team to the patient.
2.4.2 Resuscitation Equipment WACHS Resuscitation Trolley Standardisation lists (Appendix 10-14) provide the recommended minimum content for MER at all sites. The standardised lists ensure provision in all clinical areas for access to resuscitation equipment and drugs consistent with the ANZCOR Standards for
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 6 of 32 Date Next Review: December 2019
Resuscitation: Clinical Practice and Education 2014, recommendations and suggested equipment.3 All clinical staff are to be familiar with the location and appropriate use of
resuscitation equipment including competency requirements. This information is to be provided to staff during orientation.
Portable oxygen and suction must be available, and in good working order
Resuscitation equipment including defibrillator is to be checked by the nurse/midwife who has the delegated clinical responsibility for the area. Frequency of checking: – As a minimum of daily or after use (except Nursing Posts where
checking is to be once per week). – Every shift where an area/bay is designated for emergency services or
critical care, and staff are rostered on a shift by shift basis in the area. – Checking of all defibrillators is to occur as per the manufacturer’s
guidelines. Refer to BioClinical Services Clinical Equipment User Manual Library
Where a problem is identified, the problem and the actions taken are to be documented.
2.5 Communication and Documentation
Ensure accurate documentation in patient notes and use of iSoBAR for all communication including transfer of care to another facility, clinical care coordination team, or with transport providers (e.g. ambulance personnel, RFDS) occurs in accordance with the -
Operational Directive OD 0484/14 Clinical Handover Policy WACHS Assessment and Management of Interhospital Patient Transfers
Policy and MR184 WACHS Inter-hospital Clinical Handover Form
All MER calls are to be documented on either the – MR 140 Medical Emergency Response (MER) / Code Blue Record MR 75B Newborn Medical Emergency Response (MER) Record
Refer to 2.2.2 Medical Emergency Response
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 7 of 32 Date Next Review: December 2019
3. Definitions
ALS Advanced Life Support Clinical Incident A clinical incident is an event or circumstance resulting from
health care which could have, or did lead to unintended and/or unnecessary harm to a patient/consumer8.
Medical Review The patients admitting doctor, medical team or Emergency Telehealth Service or RFDS reviews the patient, or adequately assesses the patient by phone or videoconference within 30 minutes. The most senior nurse/midwife available must be aware the medical review has been requested.
Code Blue The call code made for a Medical Emergency Response (MER) within the WACHS Emergency (Disaster) Management Policy6 consistent with the Australian Standard AS4083-2010 Planning for emergencies – health care facilities.
Medical Emergency Any event in which trained personnel are required to respond to a medical crisis1. Includes Acute Myocardial Infarction, Sepsis and Stroke
Medical Emergency Response (MER)
The system for providing emergency assistance to patients whose condition is deteriorating. On the Adult Maternal & Newborn Observation and Response Chart (AORC/MORC/NORC) this is represented by the purple section, and on the Paediatric Observation and Response Charts (PORC) this is represented by the red section
Medical Emergency Response Team (MER Team)
The defined team/personnel required to respond to a medical emergency response as defined on the site escalation procedure.
Medical Officer Includes all types of medical officers including District Medical officer (DMO), Health Service Medical Practitioner (HSMP), Senior Medical Practitioner (SMO), Resident Medical Officer (RMO), Registrar, Consultant, Visiting Medical Officer/Practitioner (VMO or VMP), Fellow of the Australasian College of Emergency Medicine (FACEM) or General Practitioner (GP).
Newborn An infant from birth to aged less than 28 completed days. ORC Observation and Response Chart Senior Nurse/Midwife
Depending on the size of the service, this includes the senior nurse / midwife on duty, e.g. shift coordinator; after hours Nurse Manager; Clinical Nurse Manager (CNM); after hours CNM; DON/HSM.
Senior Nurse/Midwife Review
The most senior nurse/midwife available (after hours nurse manager or clinical nurse manager) is to review the patient and, if required contact the medical officer to determine if a clinical review is required.
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 8 of 32 Date Next Review: December 2019
4. Roles and Responsibilities STAFF MEMBER RESPONSIBILITIES
WARD NURSE (Enrolled Nurse, Registered Nurse, Registered Midwife)
Escalate response as per ORC or if concerned. Escalate response if family and or carer indicate
concern. Communicate effectively with Shift Coordinator Document observations and escalation of care
appropriately. Ensure resuscitation trolley nearby if deterioration
identified. Ensure patient notes and Observation and Response
Charts are available at bedside. Follow instruction by MER leader and deliver
appropriate care within their scope of practice Check and re-stock MER equipment daily (weekly for
Nursing Posts) and immediately following use. Report equipment issues to nursing manager.
SHIFT COORDINATOR (may be senior nurse, Remote Area Nurse, nurse practitioner or senior midwife)
Assess patient. Communicate to medical officer if medical review is
required. Initiate MER if need identified and if other staff have not
already done so. Contact other medical staff as requested by MER
leader (e.g. second MO, obstetrician, anaesthetist, surgeon).
Contact radiology, pathology and theatre team on call as required/available.
Initiate BLS and ALS (where competent) until MER Team arrives.
Communicate patient’s condition, history and progress to MER Team.
Complete and submit MR140 or MR75B (Newborn) Medical Emergency Response Record
MEDICAL OFFICERS
Provide appropriate medical intervention as required. Communicate effectively with the other members of the
team. Ensure adequate post MER follow up or appropriate
escalation of care.
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 9 of 32 Date Next Review: December 2019
MER TEAM LEADER This role is to be performed by the most experienced clinical expert available.
Be ALS (adult/paediatric/neonatal as required for the situation) competent and experienced staff member.
Communicate effectively with all team members. Identify the tasks or roles required specific to the
emergency. Identify and notify all available human resources
including ensuring sufficient and suitable medical, nursing and support personnel are called.
Coordinate and delegate roles in accordance with priority of need and in consideration of skill levels/competency/scope of practice of team members.
Delegate the retrieval of additional equipment/ medications to an appropriate nursing or other staff member.
Ensure situational awareness of immediate and surrounding environments including the delegation of care of all other patients to appropriate personnel.
Maintain a safe working environment
NOTE: If there are perceived issues around the decision to activate a MER, then
these are best discussed during debriefing in a safe environment.
5. Compliance Failure to comply with this policy may constitute a breach of the WA Health Code of Conduct (Code). The Code is part of the Employment Policy Framework issued pursuant to section 26 of the Health Services Act 2016 (HSA) and is binding on all WACHS staff which for this purpose includes trainees, students, volunteers, researchers, contractors for service (including all visiting health professionals and agency staff) and persons delivering training or education within WACHS. WACHS staff are reminded that compliance with all policies is mandatory.
6. Evaluation Governance and evaluation of recognition and response systems, including MER, involves data collection and interpretation at a site, regional and area level. This is to include: Audit using the agreed WACHS audit tools available on the WACHS Clinical
Deterioration intranet page to assess the: - documentation of recorded observations, as specified in the patient’s care
plan - appropriate recognition and escalation when observations fall into one of the
shaded zones on the observation and response charts.
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 10 of 32 Date Next Review: December 2019
To evaluate the use of the recognition and response systems, and any failures in these systems, the following investigations are to occur:
- All MERs and cardiac arrests for patients without an advance care directive or an agreed treatment-limiting order (such as Not for Resuscitation) require a full clinical review
- All missed MERs identified through audit require a full clinical review - All missed Medical Reviews identified through audit are to be followed up by
local investigation.
Review of the collated analysis of data from MER record forms every quarter at multidisciplinary meetings, with a summary of findings presented to Regional Safety and Quality Governance Groups.
Senior nurse is responsible for ensuring by audit, that compliance with checking of resuscitation equipment has been met.
7. Standards
National Safety and Quality Health Services (NSQHS) Standards Edition 1
NSQHS Standard 9: Recognising and Responding to Clinical Deterioration in Acute Health Care
National Safety and Quality Health Services (NSQHS) Standards Edition 2 Recognising and Responding to Acute Deterioration Standard
8. Legislation
(Accessible via: Government of Western Australia (State Law Publisher or ComLaw)
Health Services Act 2016 Carers Recognition Act 2004 Disability Services Act 1993 Guardianship and Administration Act 1990 Health Practitioner Regulation National Law (WA) Act 2010 Mental Health Act 2014 Poisons Act 1964 Poisons Regulations 1965 State Records Act 2000
9. References
1. Australian Standard AS4083-2010 Planning for emergencies – health care facilities
2. Australian and New Zealand Committee on Resuscitation (2016) Flowcharts. 3. Australian and New Zealand Committee on Resuscitation (2014) Standards for
Resuscitation: Clinical Practice and Education
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 11 of 32 Date Next Review: December 2019
4. Australian Commission on Safety and Quality in Health Care (2010). National consensus statement: Essential elements for recognising and responding to clinical deterioration. Canberra Australia.
5. Australian Commission on Safety and Quality in Health Care, National Safety and Quality Health Service Standards: Standard 9 Recognising and Responding to Clinical Deterioration
6. WACHS Emergency (Disaster) Management Arrangements Policy 7. Australian Commission on Safety and Quality in Health Care, Standard 9
Recognising and Responding to Clinical Deterioration in Acute Health Care: Safety and Quality Improvement Guide October 2012
8. Operational Directive OD 0611/15 Clinical Incident Management Policy (2015) 9. Operational Directive OD 0484/14 Clinical Handover Policy 10. WACHS Resuscitation Education and Competency Policy 11. Operational Directive OD 0501/14 Clinical Deterioration Policy
10. Related Forms MR 140 Medical Emergency Response / Code Blue Record MR 75B Newborn Medical Emergency Response (MER) Record MR140A Adult Observation & Response Chart AORC MR140B Maternal Observation and Response Chart MORC MR140D Newborn Observation & Response Chart NORC MR140E Paediatric Observation and Response Chart - Under 3 Months MR140F Paediatric Observation and Response Chart - 3 - 12 Months MR140G Paediatric Observation and Response Chart - 1 - 4 Years MR 140H Paediatric Observation and Response Chart - 5 - 11 Years MR140I Paediatric Observation and Response Chart - 12+ Years MR149 Neurovascular Observation Chart
11. Related Policy Documents
Chest Pain and Acute Coronary Syndrome Clinical Practice Standard Airway Management (Adult) Clinical Practice Standard Clinical Observations and Assessments Clinical Practice Standard Oxygen Therapy (Adults) Clinical Practice Standard Resuscitation, Education and Competency Assessment Policy Recognition and Management of the Newborn at Clinical Risk Policy Assessment and Management of Interhospital Patient Transfers Policy
12. Related WA Health System Policies
OD 0501/14 Clinical Deterioration Policy OD 0484/14 Clinical Handover Policy OD 0611/15 Clinical Incident Management Policy (2015)
13. WA Health Policy Framework Clinical Governance, Safety and Quality Policy Framework
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 12 of 32 Date Next Review: December 2019
14. Appendices
Appendix 1 Adult and Maternity Observation and Response Escalation and MER Template
Appendix 2 Paediatric Observation and Response Escalation and MER Template Appendix 3 Emergency Department - Adult and Maternity Observation and
Response Escalation and MER Template Appendix 4 Emergency Department - Paediatric Observation and Response
Escalation and MER Template Appendix 5 Basic Life Support Flowchart2 Appendix 6 Advanced Life Support for Adults Flowchart2 Appendix 7 Advanced Life Support for Infants and Children Flowchart2 Appendix 8 Newborn Life Support Flowchart2
Appendix 9 Clinical Deterioration and Early Response in the Older Person Appendix 10 Resuscitation Trolley Lists
This document can be made available in alternative formats on request for a person with a disability
Contact: Program Manager Clinical Quality and Performance (R. Fletcher) Directorate: Medical Services TRIM Record # ED-CO-13-52403
Version: 3.00 Date Published: 29 January 2018 Copyright to this material is vested in the State of Western Australia unless otherwise indicated. Apart from any fair dealing for the purposes of private study, research, criticism or review, as permitted under the provisions of the Copyright Act 1968, no part may be reproduced or re-used for any purposes whatsoever without written permission of the State of Western Australia.
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 13 of 32 Date Next Review: December 2019
Appendix 1 - Adult and Maternity Observation and Response Escalation and MER Template
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 14 of 32 Date Next Review: December 2019
Appendix 2 - Paediatric Observation and Response Escalation and MER Template
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 15 of 32 Date Next Review: December 2019
Appendix 3 - Emergency Department - Adult and Maternity Observation and Response Escalation and MER Template
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 16 of 32 Date Next Review: December 2019
Appendix 4 - Emergency Department - Paediatric Observation and Response Escalation and MER Template
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 17 of 32 Date Next Review: December 2019
Appendix 5 - Basic Life Support Flowchart
Source: https://resus.org.au/guidelines/flowcharts-3/
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
.
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 18 of 32 Date Next Review: December 2019
Appendix 6 - Advanced Life Support for Adults Flowchart
Source: https://resus.org.au/guidelines/flowcharts-3/
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 19 of 32 Date Next Review: December 2019
Appendix 7 - Advanced Life Support for Infants and Children
Source: https://resus.org.au/guidelines/flowcharts-3/
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 20 of 32 Date Next Review: December 2019
Appendix 8 - Newborn Life Support
Source: https://resus.org.au/guidelines/flowcharts-3/
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 21 of 32 Date Next Review: December 2019
Appendix 9 - Clinical Deterioration and Early Response in the Older Person
Adult Observation and Response Chart
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 22 of 32 Date Next Review: December 2019
Appendix 10 - Recommended Minimum Equipment – Adult MER Trolley Top of Trolley: Quantity Defibrillator 1
ECG Leads attached 1 Set Defibrillation pads attached 1 Set
IV Pole 1 Sharps Container Small 1 Bag-Valve Mask - Adult 1 Pressure Bag 1000ml 1 Goggles 2 Glucometer 1 Non Sterile Gloves box Small, Medium, Large 1 Each Calculator 1 Stethoscope 1 Right Side of Trolley: Quantity C-Size oxygen cylinder with oxygen nipple attached 1 Twin-o-vac suction unit with suction tubing & Yankauer sucker attached 1 Hudson mask Adult 1 Each Nasal Prongs Adult 1 Oxygen tubing 1 Nebuliser mask Adult 1 Left side of Trolley Quantity MR 140 Medical Emergency Response (MER)/Code Blue Record 2 Resus Trolley check list (Clip board) 1 ANZCOR Advanced Life Support for Adults Flowchart laminated 1 Draw 1: Drugs Quantity Adrenaline 1:1000/1ml 10 Adrenaline 1:10 000/10ml 5 Amiodarone 150mg/3ml 3 Atropine 600mcg/ 1ml 5 Adenosine 6mg/ 2ml 6 Aspirin 300mg 2 Calcium Gluconate 10ml 1 Glucose 25g in 50ml (50%) 1 Bottle Glucose 5% in 100ml 1 Bottle Glycerine Trinitrate S/L 1 Bottle Ipratropium 500mcg/2.5ml Nebules 2 Midazolam 5mg/5ml 2 Magnesium Sulphate 10mmol/5ml 2 Naloxone 400mcg/1ml 2 Normal Saline 10ml 10 Salbutamol Nebules 5mg/2.5ml 2 Water for Injection 10ml 4 Sodium Bicarbonate 8.4g/100ml 1 Bottle Alcohol swabs 10 Chlorhexidine swabs 2 ABG Syringe 2 Syringe 2, 5, 10, 20ml 5 each Syringe 50ml Luer Lock 1 Blunt Drawing up needle 18G 5
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 23 of 32 Date Next Review: December 2019
Draw 2: Simple Airway/ IV Quantity Non Rebreather Mask 1 Hudson Mask 1 Elastic bandage 1 Blood sample bottles Green, Purple, Blue 1 Each Blood Culture Bottles 1 Blood transfusion set 1 IVC 14, 16, 18,20G 3 Each IVC Dressing pack 1 IV Dressing Adult 5 IV Fluids administration/giving set 1 IV 3 Way taps 2 Micropore tape 1 Needle free bungs 3 Needles 21, 23 & 25G 5 Each Primary Pump (hand pump) IV infusion set 1 Pulse oximeter 1 Tourniquet 1 Yankauer Sucker 1 Draw 3: Advanced Airway/ Intubation Quantity Laryngoscope handle 1 Laryngoscope blade Mackintosh (Standard & Long) size 3 & 4 1 Each Batteries AA 6 Batteries C 2 Bougie 10Fr 1 Cobbs connector 1 CO2 Filter 1 CO2 Detector 1 Cotton ETT Tape 20 ETT Cuffed size 6, 6.5, 7.0, 7.5, 8, 8.5 & 9 1 Each Face masks for Bag-Valve Mask Size 4 & 5 1 Each LMA size 3, 4, & 5 1 Each Lubricant Sachet 5 Magill’s forceps 1 Nasogastric Tube10 & 12Fr 1 Each NPA Size 32 & 34G 1 Each OPA Size 3, 4 & 5 1 Each Stylet 10 & 14Fr 1 Each Suction Catheters 12 & 14Fr 1 Each Pen Torch 1 Draw 4: IV Fluids/ Intraosseous Quantity Normal Saline 0.9% 1000ml bag 1 Compound Sodium Lactate 1000ml bag 1 Glucose 5% 100ml bag 1 IIntraosseous Tray Intraosseous insertion device 1 Intraosseous needles 25mm, 45mm 2 each Chlorhexidine swab 5 IVC dressing pack 1 IV Extension tubing 25cm 2 Syringe 50ml Luer Lock 1 Needle free bung 1 Draw 5: Miscellaneous Quantity ECG Monitoring Dots 1 Packet Defibrillator printing paper 1 Refill Defibrillator Pads 1 Set Drug/Plain Labels 1 Roll
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 24 of 32 Date Next Review: December 2019
Recommended Minimum Equipment –Paediatric and Adult Trolley Top of Trolley: Quantity Defibrillator 1
ECG Leads attached 1 Defibrillation pads attached - Adult Defibrillation pads >15kg Defibrillation pads <15kg
1 set Each
IV Pole 1 Trauma Scissors 1 Sharps Container Small 1 Bag Valve Mask with size 4 Facemask attached 1 Bag Valve Mask- Paed 500ml with size 2 Facemask attached 1 Bag Valve Mask - Neonate 250ml with size 1 Facemask attached 1 Pressure Bag 500ml 1 Goggles 1 Glucometer 1 Non Sterile Gloves box - Small, Medium, Large 1 Calculator 1 Stethoscope 1 Right Side of Trolley: Quantity C-Size oxygen cylinder with oxygen nipple attached with Adult Hudson Mask attached 1 Twin-o-vac suction unit with suction tubing & Yankauer sucker Adult attached 1 Nasal Prongs Adult & Paediatric 1 Oxygen tubing 1 Nebuliser mask Adult & Paediatric 1 Left side of Trolley Quantity MR 140 Medical Emergency Response (MER)/Code Blue Record 2 Resus Trolley check list (Clip board) 1 ANZCOR Advanced Life Support for Adults & Advanced Life Support for Infants and Children Flowcharts laminated
1 Each
Paediatric Drug dose reference i.e. Broselow tape, Monash Drug book, Kidshealthwa Guidelines
1
Draw 1: Drugs Quantity Adrenaline 1:1000 10 Adrenaline 1:10 000 5 Amiodarone 150mg/3ml 3 Atropine 600mcg 5 Adenosine 6mg/2ml 6 Aspirin 300mg 2 Calcium Gluconate 10ml 1 Glucose 25g in 50ml (50%) 1 Bottle Glucose 10g in 100ml (10%) 1 Glucose 5% in 100ml 1 Bottle Magnesium Sulphate 10mmol/5ml 2 Naloxone 400mcg 2 Normal Saline 10ml 10 Sodium Bicarbonate 8.4g/100ml (8.4%) 1 Bottle Alcohol swabs 10 Chlorhexidine swabs 2 ABG Syringe 2 Syringe 2, 5, 10, 20ml 5 each Syringe 50ml Luer Lock 1 Blunt Drawing up needle 18G 5
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 25 of 32 Date Next Review: December 2019
Draw 2: Simple Airway/ IV Quantity Elastic bandage 1 Blood sample bottles Green, Purple, Blue - Adult & Paediatric 1 Each Blood Culture Bottles Adult & Paediatric 1 Blood transfusion set 1 IVC 14, 16 18, 20G, 22, 24G 3 each IVC Dressing pack 1 IV Dressing Adult & Paediatric 5 IV Fluids administration set 1 IV 3 Way tapes 2 Micropore tape 1 Needles 19, 21, 23, 25G 5 Each Needle free bungs 3 Primary Pump IV infusion set 1 IV Burette Paediatric 1 Pulse oximeter 1 Tourniquet 1 Draw 3: Advanced Airway/ Intubation Quantity Laryngoscope handle 1 Laryngoscope blade Macintosh- Standard & Long size 3 &4 1 each Batteries AA 6 Batteries C 2 Bougies 5 & 10Fr 1 Each Cobbs connector 1 CO2 Filter 1 CO2 Detector Easy Cap Adult & Paediatric 1 Each Face masks for Bag Valve mask 00,1,2, 3 & 5 1 Each Lubricant Sachet 5 Magills forceps Paediatric & Adult size 1 Nasogastric Tubes Size 6, 8, 10, & 12Fr 1 Each Suction Catheters 6, 8, 10, 12 & 14Fr 1 Each Pen Torch 1 Draw 4: IV Fluids/ Intraosseous/Miscellaneous Quantity Glucose 10% 500ml 1 Glucose 5% 100ml bag 1 Normal Saline 0.9% 500mls 1 Compound Sodium Lactate 1000ml bag 1 I/O Tray Quantity Intraosseous insertion device (drill) 1 Intraosseous needle 15mm, 25mm, 45mm, 2 each Chlorhexidine Swab 2 IVC Dressing pack 1 IV Extension tubing 25cm 1 Syringe 50ml Luer Lock 1 Needle free bung 1 Miscellaneous Quantity ECG Monitoring Dots - Adult & Paediatric 1 Packet Defibrillator printing paper 1 Refill Defibrillator Pads- spare Adult, <15kg, >15kg 1 Set Drug/Plain Labels 1 Roll
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 26 of 32 Date Next Review: December 2019
Draw 5: Paediatric Equipment Quantity Hudson mask Paediatric 1 each Nebuliser mask Paediatric 1 Nasal Prongs Paediatrics 1 Non Rebreather Mask Paediatric 1 Yankauer Sucker Paediatric 1 Laryngoscope short handle 1 Elastoplast tape 2.5cm 1 CO2 Detector Pedi Cap 1 each Tongue depressors 5 Blood Culture Bottles Paediatrics 1 IVC 18, 20, 22, 24 G 3 each IV Butterflies 21, 23, 25G 2 Each IV Dressing Paediatric 5 IV Arm board Neonate/Paediatric 1 Each IV Burette Paediatric 1 Stethoscope Paediatric 1 3-5kg Quantity Oropharyngeal Airway (OPA) Size 000, 00, 0 1 Each Nasopharyngeal Airway (NPA) 14Fr 1 Laryngeal Mask Airway (LMA) size 1 1 Stylet 5Fr 1 Endotracheal Tube (ETT) uncuffed 2.5 & 3 1 Each Miller Laryngoscope blade size 0 & 1 1 Each 6-11kg Quantity OPA Size 0, 1 1 Each NPA 14, 18Fr 1 Each LMA Size 1.5, 2 1 Each Stylet 5Fr 1 ETT uncuffed Size 3.5 & cuffed size 3, 3.5, 4 1 Each Miller Laryngoscope blade size 1 1 12-23kg Quantity OPA Size 1, 2 1 Each NPA 20, 22Fr 1 Each LMA Size 2, 2.5 1 Each Stylet 10Fr 1 ETT Cuffed size 4, 4.5, 5, 5.5 1 Each Mackintosh Laryngoscope Blade size 1 & 2 1 Each 24-42kg Quantity OPA Size 3 1 NPA 22, 24Fr 1 LMA Size 2.5, 3 1 Stylet 10Fr 1 ETT Cuffed size 5, 5.5, 6, 6.5, 7 1 Each Mackintosh Laryngoscope Blade size 2 & 3 1 Each
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 27 of 32 Date Next Review: December 2019
Recommended Minimum Equipment – Paediatric MER Trolley
Top of Trolley: Quantity Defibrillator 1
ECG Leads attached 1 set Defibrillation pads attached >15kg 1 Set Defibrillation pads <15kg 1 Set
Trauma Scissors 1 IV Pole 1 Sharps Container Small 1 Bag- Valve Mask- Adult- size 4 face mask attached 1 Bag- Valve Mask- Paed 500ml- size 2 face mask attached 1 Bag- Valve Mask- Neonate 250ml- size 1 face mask 1 Pressure Bag 500ml 1 Goggles 1 Glucometer 1 Non Sterile Gloves box Small, Medium, Large 1 Each Calculator 1 Stethoscope 1 Right Side of Trolley: Quantity C-Size oxygen cylinder with oxygen nipple attached 1 Twin-o-vac suction unit with suction tubing & yankauer sucker attached 1 Hudson mask Paediatric 1 Nasal Prongs Paediatric 1 Oxygen tubing 1 Nebuliser Mask Paediatric- 3 sizes 1Each Left side of Trolley Quantity MR 140 Medical Emergency Response (MER)/Code Blue Record 2 Resus Trolley check list (Clip board) 1 ANZCOR Advanced Life Support for Infants and Children Flowcharts laminated 1 Paediatric Drug dose reference i.e. Broselow tape, Monash Paediatric Emergency Book or kidshealthwa (PMH) Resuscitation Guideline
1
Draw 1: Drugs Quantity Adrenaline 1:1000/1ml 10 Adrenaline 1:10 000/10ml 5 Amiodarone 150mg/3ml 3 Atropine 600mcg/1ml 5 Adenosine 6mg/2ml 6 Calcium Gluconate 1g/10ml 1 Glucose 10g in 100ml (10%) 1 Glucose 25g in 50ml (50%) 1 Bottle Glucose 5% in 100ml 1 Bottle Ipratropium Bromide 500mcg/2.5ml Nebules 2 Midazolam 5mg/5ml- leave on to align with other trolleys 2 Magnesium Sulphate 10mmol/5ml 2 Naloxone 400mcg/1ml 2 Normal Saline 10ml 10 Sodium Bicarbonate 8.4g/100ml (8.4%) 1 Bottle Salbutamol Nebules 2.5mg/2.5mls & 5mg/2.5mls trolleys 2 Each Alcohol swabs 10 Chlorhexidine swabs 2 ABG Syringe 2 Syringe 2, 5, 10, 20ml 5 each Syringe 50ml Luer Lock 1 Blunt Drawing up needle 18G 5
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 28 of 32 Date Next Review: December 2019
Draw 2: Simple Airway/ IV Quantity Oxygen masks size 4 & 5 1 Non Rebreather Mask Paed 1 Elastic bandage 1 Blood sample bottles Green, Purple, Blue- Paediatric 1 Each Blood Culture Bottles Paediatrics 1 Blood transfusion set 1 set IVC 18,20, 22, 24 G 3 each IV Butterflies 21, 23, 25G 2 Each IVC Dressing pack 1 IV Dressing Paediatric 5 IV Arm board Neonate & Paediatric 1 Each IV Fluids administration set 1 IV Burette Paediatrics 1 IV 3 Way taps 2 Micropore tape 1 Needles 19, 25G 5 Each Needle free bungs 3 Pulse oximeter 1 Tourniquet 1 Yankauer Sucker - Paediatric & Adult size 1 Draw 3: Advanced Airway/ Intubation Quantity Laryngoscope short handle 1 Batteries AA 6 Batteries C 2 Bougies 5 & 10Fr 1 Each Cobbs connector 1 CO2 Filter 1 CO2 Detector Pedicap & Easy Cap 1 each Elastoplast tape 2.5cm 1 Face masks for Bag Valve Mask Size 00, 1, 2, 3, & 4 1Each Lubricant Sachet 5 Magill’s forceps- neonatal, paediatric & adult 1 Nasogastric Tubes Size 6, 8, 10, & 12Fr 1 Each Suction Catheters 6, 8, 10, 12 & 14Fr 1 Each Tongue depressors 5 Pen Torch 1
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 29 of 32 Date Next Review: December 2019
Recommended Minimum Equipment – Newborn MER Pack
Equipment (Top of Neonatal Resuscitation Cot) Quantity Overhead Heater 1 Dry warm towels 2 Stethoscope - Neonatal 1 Bag-Valve Mask Neonate 250ml with Size 00 Face Mask attached 1 T piece resuscitator with ventilator tubing and 00Face mask attached 1 Positive Pressure Ventilation Device (Neopuff or similar) 1 Air-Oxygen Blender 1 Oxygen Saturations machine with stick on probe attached 1 Infant Hudson mask with oxygen tubing attached 1 Infant nasal prongs 1 Gloves Sterile : Small, Medium, Large 1 each Goggles 2 Sharps container 1 (Back of resus Cot): Quantity Portable/Suction C-Size oxygen cylinder 1 Twin-o-vac suction unit with paediatric Yankauer attached 1 10Fr Y suction catheter 2 Meconium aspirator / hand suction device 1 (Left side of Resuscitation Cot) Quantity MR 75B Newborn Medical Emergency Response (MER) Record 2 Resus Trolley/Pack check list (Clip board) 1 ANZCOR Newborn Life Support Flowchart laminated 1 (Draw 1: Drugs or in Drugs box in pack) Quantity Adrenaline 1:10 000/10ml 2 Atropine 600mcg/1ml 2 Naloxone 400mcg/1ml 1 Normal Saline 10ml 5 Alcohol swabs 5 ABG Syringe 2 Syringe 2, 5, 10, 20ml Luer lock 1 each Blunt Drawing up needle 18G 2 (Draw 2: Simple Airway/ IV or within pack) Quantity Elastic bandage 1 Blood sample bottles Green, Purple, Blue 1 Each Blood Culture Bottles 1 set Blood transfusion set 1 IVC 25G 2 UVC Line 5fr 2 IVC Dressing pack 1 IV Dressing Paediatric/Umbilical Tape 2 IV Fluids administration set 1 IV 3 Way tap 2 Micropore tape 1 Needle free bungs 2 Needles 25G 2 Tourniquet 1 Scalpel Blade 1
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 30 of 32 Date Next Review: December 2019
(Draw 3: Advanced Airway/ Intubation or within Pack) Quantity Laryngoscope short handle 1 Laryngoscope blade Mackintosh size 00/0/1 1 Each Bougie 5Fr 1 CO2 Detector, Pedicap 1 ETT Uncuffed size 2.5, 3.0, 3.5 1 Each Face masks Bag-Valve Mask size 00/1 1 Each LMA size 1/ 1.5/2 1 Each Lubricant Sachet 2 Magill’s forceps neonatal size 1 Nasogastric Tube 6, 8Fr 1 Each Oropharyngeal Airway Size 000, 00, 0 1 Each Stylet 10Fr 1 Each Suction Catheters 6Fr, 8Fr, 10Fr 1 Each Pen Torch 1 Draw 4: IV Fluids/ Intraosseous/Miscellaneous Quantity Normal Saline 0.9% 500ml bag 1 Glucose 10% 100ml 1 Miscellaneous Defibrillator Pads Paediatric 1 set Glucometer 1 Drug labels 1 Roll
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 31 of 32 Date Next Review: December 2019
Recommended Minimum Equipment – Nursing Post/Small Centre MER Pack Equipment (Top of Trolley or external to Pack) Quantity Automated External Defibrillator 1
Defibrillation adult pads - attached 1 Set Defibrillation paediatric pads (easily accessible next to it) 1 Set
IV Pole 1 Trauma Scissors 1 Sharps Container Small 1 Bag- Valve Mask Adult with size 4 Face Mask attached 1 Bag- Valve Mask Paediatric 500ml with Size 2 Face Mask attached 1 Bag- Valve Mask-Neonate 250ml with Size 1 Face Mask attached 1 Pressure Bag 500ml 1 Goggles 1 Glucometer 1 Non- Sterile Gloves box- Small, Medium, Large 1 Each Calculator 1 Stethoscope 1 (Right Side of Trolley or external to pack): Quantity Portable suction/ C-Size oxygen cylinder with oxygen nipple attached 1 Twin-o-vac suction unit with suction tubing & Yankauer Sucker attached 1 Hudson mask Adult & Paediatric with Oxygen tubing attached 1 Each Nasal Prongs Adult & Paediatric 1 Each Nebulizer Masks Adult & Paediatric 1 Each (Left side of Trolley or within pack) Quantity MR 140 Medical Emergency Response (MER)/Code Blue Record 2 Resus Trolley check list (Clip board) 1 ANZCOR Advanced Life Support for Adults & Advanced Life Support for Infants and Children Flowcharts laminated
1 Each
Paediatric Drug dose reference i.e. Broselow tape, Monash Paediatric Emergency Book or kidshealthwa (PMH) Resuscitation Guideline
1
(Draw 1: Drugs or in Drugs box in pack) Quantity Adrenaline 1:1000/1ml 10 Adrenaline 1:10 000/10ml 5 Amiodarone 150mg/3ml 3 Adenosine 6mg/2ml 6 Aspirin 300mg 2 Atropine 600mcg/1ml 5 Calcium Gluconate 10ml 1 Glucose 10g in 100ml (10%) 1 Glucose 25g in 50ml (50%) 1 Glycerine Trinitrate S/L 1 Bottle Ipratropium Nebules 500mcg/2.5ml 2 Magnesium Sulphate 10mmol/5ml 2 Naloxone 400mcg/ 1ml 2 Water for injection 10ml 4 Normal Saline 10ml 10 Sodium Bicarbonate 8.4g/100ml (8.4%) 1 Bottle Salbutamol Nebules 5mg/2.5ml 2 Alcohol swabs 10 Syringe 2, 5, 10, 20 5 Each Syringe 50ml Luer Lock 1 Blunt Drawing up needle 18G 5
WACHS Clinical Escalation of Acute Physiological Deterioration including Medical Emergency Response (MER) Policy
Printed or saved electronic copies of this policy document are considered uncontrolled. Always source the current version from WACHS HealthPoint Policies.
Date of Last Review: December 2017 Page 32 of 32 Date Next Review: December 2019
(Draw 2: Simple Airway/ IV or within pack) Quantity Non Rebreather Mask Adult &Paediatric 1 Each Hudson Mask Adult & Paediatric 1 Each Elastic bandage 1 Blood sample bottles Green, Purple, Blue adult & paediatric 1 Each Blood Culture Bottles adult & paediatric 1 set Blood transfusion set 1 IVC 14, 16, 18,20, 22 & 24G 3 Each IVC Dressing pack 1 IV Dressing Adult/Paediatric 5 Each IV Fluids administration set 1 IV 3 Way tap 1 Micropore tape 1 Needle free bungs 3 Needles 19, 21, 23 & 25G 5 Each Primary Pump IV infusion set 1 IV Burette paediatric 1 Tourniquet 1 Yankauer Sucker Adult & Paediatric 1 Each (Draw 3: Advanced Airway/ Intubation or within Pack) Quantity Laryngoscope handle 1 Laryngoscope blade Mackintosh size 0, 1, 2, 3 & 4 1 Each Bougie 5, 10Fr 1 Each Cobbs connector 1 CO2 Detector, Adult & Pedicap 1 Each Cotton ETT Tape 20cm 1 ETT Uncuffed size 2.5, 3, 3.5 Cuffed 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7.0, 7.5, 8, 8.5 & 9 1 Each Face masks for BVM Size 00,1, 2, 3 & 5 1 Each LMA size 1.5, 2, 2.5, 3, 4, & 5 1 Each Lubricant Sachet 2 Magill’s forceps Adult & Paeds 1Each Nasogastric Tube 6, 8, 10 & 12Fr 1 Each NPA Size 14, 18, 20, 22, 24, 32 & 34G 1 Each OPA Size 000, 00, 0, 1, 2, 3, 4 & 5 1 Each Stylet 10 & 14Fr 1 Each Suction Catheters 6, 8, 10, 12 & 14Fr 1 Each Pen Torch 1 Draw 4: IV Fluids/ Intraosseous/Miscellaneous Quantity Normal Saline 0.9% 1000ml bag 1 Compound Sodium Lactate 1000ml 1 Glucose 5% 100ml bag 1 I/O Tray Intraosseous Insertion device (drill) 1 I/O Needle 15mm, 25mm & 45mm 2 Each Chlorhexidine Swab 2 IVC Dressing Pack 1 IV Extension tubing 25cm 2 Needle free bung 1 Syringe 50ml Luer Lock 1 Draw 5: Miscellaneous ECG monitoring dots 1 Packet Defibrillator printing paper 1 Refill Drug/Plain Labels 1 set Defibrillator Adult and Paediatric Pads - Spares 1 set
each
Date of Last Review: March 2017 Page 1 of 9 Date Next Review: March 2022
Effective: 4 April 2017
Resuscitation Education and Competency Assessment Policy
1. Background
The WA Country Health Service (WACHS) is committed to developing and fostering a culture of learning which encourages self-development and the assessment of clinical skills and knowledge in the resuscitation practices associated with newborns, infants, children and adults. This is centred on establishing learning and assessment programs to agreed standards and to ensure minimum safe practice. The agreed standard for resuscitation practices for WACHS is the Australian Resuscitation Council (ARC). Governance over learning and performance objectives is to be maintained by WACHS Central Office and Learning and Development, in accordance with the Guidelines of the ARC. WACHS is committed to ensuring the achievement of competency of staff who care for patients in an emergency situation. Resuscitation education programs within WACHS are based on a flexible learning framework that encourages individuals to seek learning opportunities in a format that reflects the principles of adult learning. Therefore, a variety of education opportunities and learning resources are available for WACHS staff to access for education in resuscitation. Achievement of competency can be obtained through an assessment process that ensures the national assessment principles of validity, reliability, flexibility and fairness are applied. Demonstrated competency through a sound process quantifies the achievement of the skills, knowledge and attitude of the elements of Basic Life Support (BLS), Advanced Life Support (ALS) and Newborn Resuscitation (NNR) practices. Demonstration of the evidence required for competency in all areas of resuscitation can occur through direct observation and supplementary and indirect methods that are ethical, manageable and cost effective.
2. Policy Statement It is WACHS policy that:
all resuscitation education and assessment programs must comply with ARC Guidelines
WACHS resuscitation education and assessment programs include Basic Life Support, Advanced Life Support (adult and paediatric) and Newborn Resuscitation.
in accordance with documentary evidence for Australian Health Practitioner Regulatory Agency (AHPRA) Continuous Professional Development (CPD) requirements of each National Board the individual employee and the organisation must maintain:
a record of attendance at BLS, ALS and NNR education sessions or other learning resource completion;
a record of currency of BLS, ALS and NNR competency employees must maintain their own records of completed learning activities
related to resuscitation.
Document valid at: 05/04/2017 7:38 am
WACHS Resuscitation Education and Competency Assessment Policy
Date of Last Review: March 2017 Page 2 of 9 Date Next Review: March 2022
Each resuscitation program has identified and endorsed learning and performance objectives. Successful completion of learning and assessment opportunities are to be recorded against the WACHS Learning and Development (L&D) codes as follows:
o Basic Life Support – REABL (adult); REPBL (paediatric) o Advanced Life Support – REALH (adult); REP (paediatric) o Newborn Resuscitation – REN
Skill levels are to be recorded as: 001/EL1 - Awareness 002/EL2 - Knowledge Tested 003 – Demonstrated Skills 004 – Assessor 005 - Trainer
the Newborn Resuscitation Program is to be conducted in accordance with the Australian Resuscitation Council Policy Statements and King Edward Memorial Policies Neonatal Resuscitation Policies - Section 1
a system is in place for ensuring access at all times to at least one clinician, either on-site or in close proximity, who can practise ALS (National Safety and Quality Health Service Standards)
3. Competency Requirements
The clinical workforce is required to demonstrate BLS competence annually
BLS competency assessment of clinicians are to include the successful demonstration of use of the Automated External Defibrillator (AED) available at their worksite.
Non-clinical staff BLS competency requirements are as directed by the site manager in accordance with Australian Resuscitation Council Policy Statements.
To allow delegation of roles and responsibilities to clinicians who can practise ALS, all nursing and medical staff that are expected to respond to a medical emergency are to demonstrate ALS competence annually (WACHS Emergency (Disaster) Management Arrangements Policy 2013).
All staff expected to respond as part of a Medical Emergency Team or working in an emergency department, high dependency or peri operative area are expected to demonstrate annual competence in ALS (ref: WACHS Emergency (Disaster) Management Arrangements Policy 2013).
All nursing, midwifery and medical staff who are attending obstetric deliveries, working in obstetric units or neonatal nurseries or attending at Lower Segment Caesarean Section are required to demonstrate Newborn Resuscitation competence annually. (ref: WACHS Emergency (Disaster) Management Arrangements Policy 2013; WACHS Professional Development Requirements for Midwives Policy 2013). Medical Staff are also to refer to WACHS Medical Credentialing and Compliance Requirement Guideline.
Document valid at: 05/04/2017 7:38 am
WACHS Resuscitation Education and Competency Assessment Policy
Date of Last Review: March 2017 Page 3 of 9 Date Next Review: March 2022
Shift coordinators responsible for the care of newborn and/or paediatric patients are to successfully demonstrate Newborn Resuscitation and/or Advanced Life Support (Paediatric) resuscitation competence annually.
3.1 Assessment of Competency
The International Consensus on Cardiopulmonary Resuscitation and Emergency Care Science with Treatment Recommendations (Sour et al.) demonstrates that skill retention deteriorates from six months after skill acquisition for basic and advanced life support techniques and therefore a minimum of 12 monthly reassessment is recommended. In WACHS, annual assessment of competence in Basic, Advanced (adult/paediatric) and Newborn Life Support is through successful completion of: theoretical assessment, and practical assessments that reflect the identified and endorsed performance
objectives for each competency area, and assessment is to be conducted by appropriately trained and qualified assessors
utilising the WACHS endorsed basic, advanced and/or new born resuscitation assessment tools located in the Learning and Development Portal.
3.2 Skills Recognition
Where a staff member can provide evidence of achieving competence through another recognised agency, the certificate is to be recognised, utilising the skills recognition process of ensuring validity, reliability, currency and transferability, providing the competency has been achieved within the preceding 12 months and meets all of the performance objectives defined for each area of competency.
A copy of the certificate is to be sent to the line manager and nurse educator or staff development nurse within each region as evidence of competency for recording into the appropriate documents and electronic record keeping tools for record keeping purposes.
Recognition of Prior Learning (RPL) will be issued for the following upon the receipt of evidence: BLS (REABL – adult BLS)– successful completion of WACHS BLS competency
assessment or any nationally endorsed qualification conducted by a registered Training Organisation that includes the Unit of Competency HLTCPR211A or successful completion of BLS competency at a WA Health Teaching Hospital. All other evidence will be mapped against the performance criteria for WACHS BLS.
BLS (REPBL – child BLS) – successful completion of WACHS BLS competency assessment or successful completion of BLS or Hospital Paediatric Life Support competency at Princess Margaret Hospital for Children/Perth Children’s Hospital. All other evidence will be mapped against the performance criteria for WACHS BLS
ALS (REALH - Adult only) – successful completion of WACHS ALS competency or Australian College of Critical Care Nurses (ACCCN) ALS Course. These programs include team leader and team member roles. Alternatively, successful completion of assessment at an accredited Australian Resuscitation Council ALS 1 (suitable for eam members) or ALS 2 Course (suitable for team leaders and/or MER team members). All other evidence will be mapped against the performance criteria for WACHS Adult ALS.
Document valid at: 05/04/2017 7:38 am
WACHS Resuscitation Education and Competency Assessment Policy
Date of Last Review: March 2017 Page 4 of 9 Date Next Review: March 2022
ALS (REP - paediatric only) – successful completion of WACHS ALS competency, successful completion of assessment at ACCCN Paediatric Life Support Course, successful completion of assessment at an Advanced Paediatric Life Support Course (APLS Australia/ New Zealand) or Paediatric Life Support Course (Princess Margaret Hospital for Children WA). All other evidence will be mapped against the WACHS performance criteria for WACHS Paediatric ALS.
Newborn Resuscitation (REN) – successful completion of WACHS Newborn Resuscitation Competency or successful completion of King Edward Memorial Hospital theoretical and practical competency assessment of Newborn Resuscitation. All other evidence will be mapped against the WACHS performance criteria for Newborn Resuscitation.
4. Roles and Responsibilities
4.1 Individual Staff As per the WACHS Code Blue/MER Policy and WACHS Disaster Management policy, all WACHS staff who may be required to, or are expected to respond to a clinical deterioration or medical emergency are to: actively access and participate in resuscitation learning and assessment activities be responsible for recording their own continuing professional development
activities participate in equipment checking procedures (where relevant) to ensure equipment
is functional report equipment problems via the relevant equipment maintenance process. New employees to WACHS who may be required to, or are expected to respond to a clinical deterioration or medical emergency are required to provide evidence of competence in BLS within six weeks of commencing employment. New employees to WACHS who may be required to, or are expected to respond to a clinical deterioration or medical emergency are required to provide evidence of competence in ALS (adult and/or paediatric) and/or Newborn Resuscitation competence within three months of commencing employment. All WACHS nursing staff should assess their BLS, ALS and NNR education and competency requirements against the Approved Area Master for their Clinical Unit Knowledge and Skills Scope of Practice Tool available on WACHS Nursing & Midwifery intranet webpage. 4.11 Medication Orders Where a medical emergency requires the administration of Adrenaline and/or Amiodarone, it is only to be administered by a Registered Nurse with a minimum of a doctors’ verbal order i.e. General Practitioner/Regional Resource Centre ED doctor, Emergency Telehealth (ETS) Service doctor Where a patient regularly presents with an episode of anaphylaxis and the patient usually self-administers an Adrenaline Epi-pen ™, they are to have a documented specific management plan provided by a medical officer for intramuscular adrenaline administration for treatment of his/her anaphylaxis presentation.
Document valid at: 05/04/2017 7:38 am
WACHS Resuscitation Education and Competency Assessment Policy
Date of Last Review: March 2017 Page 5 of 9 Date Next Review: March 2022
4.2 Operations Managers/ Line Managers The manager's responsibility is to: ensure supervised orientation to site resuscitation equipment and training resources
and associated processes and policies occurs perform a comprehensive risk analysis of training needs to ensure appropriate staff
are trained in resuscitation. e.g. small sites may utilise non-clinical staff trained in BLS to support clinical staff during a resuscitation event
develop a plan to ensure that the clinical workforce can initiate appropriate early interventions and respond with life-sustaining measures in the event of severe or rapid deterioration
ensure training is available for the clinical workforce, with the initial focus being on employed nursing, allied health and medical staff.
ensure staff are rostered appropriately to enable attendance at learning sessions or courses in order to achieve their resuscitation competency requirements
monitor compliance of competency achievement of individual staff, providing evidence to demonstrate that the clinical workforce is trained and proficient, and ensuring visibility of this data is available at local and regional governance levels for monitoring.
ensure that staff have access to an Assessor to allow on-site assessment of staff competence
implement equipment checking processes and monitor to ensure compliance facilitate the participation of all identified target group staff at assessment activities,
and liaise with the Learning and Development staff or Staff Development personnel
when required to ensure systems and equipment to support effective Learning and Assessment opportunities are maintained
ensure working parties and governance committees responsible for NSQHS Standard 9 include broad representation of medical and nursing disciplines to support the standardised processes across the region.
4.3 Assessors Assessors are key persons with well-developed personal competence in the area of which they are assessing and have responsibility to assess clinical competence within WACHS facilities in accordance with WACHS and ARC policy and guidelines.
These key persons must: be currently competent in the individual skill being assessed and be recommended as an Assessor by the line manager for the area /ward /hospital
and have completed local Assessor/Validator Competency or Certificate IV Workplace
Training and Assessment or equivalent, or Certificate IV Assessment Skill Set Program or
Graduate Certificate, Diploma or Masters in Education or EMST Instructor – Emergency Management of Severe Trauma (Royal Australasian
College of Surgeons); ACME Instructor – Acute and Complex Medical Emergencies (Australasian College of Emergency Medicine); EMAC Instructor – Effective Management of Anaesthetic Crisis (Australian and New Zealand College of Anaesthetists or
Document valid at: 05/04/2017 7:38 am
WACHS Resuscitation Education and Competency Assessment Policy
Date of Last Review: March 2017 Page 6 of 9 Date Next Review: March 2022
ACCCN or ARC current assessor. N.B. these WACHS employees working in the capacity as a WACHS site assessor are to use the WACHS endorsed learning and assessment tools only or
have completed recognition of prior learning process that has been endorsed by the regional L&D coordinator or Nurse Educator
check all candidate pre-requisites are successfully completed prior to undertaking assessment activities
check all equipment used in the practical assessment is in a safe, clean and functional condition prior to and following the assessment process
maintain accurate, confidential and legible documentation of all assessment activities
conduct all practical assessments in a safe, private and confidential, one-on-one environment in accordance with the endorsed performance criteria for each program area. Assessments must not occur on-mass i.e. multiple assessments must not occur simultaneously
ensure candidates are aware of the Appeals Process forward assessment results of successful candidates confidentially in accordance
with local processes for recording in the WACHS Learning Management System immediately and confidentially notify the candidate’s manager of persons that are
unsuccessful in achieving competency and the suggested pathway and plan for re-assessment
following completion of local recording and reporting requirements, return all completed and signed hard copies of practical assessment tools to the candidate.
All employees involved in assessment and training of resuscitation programs are to perform self-assessment to a level of Stage 5 (The Expert) according to the Benner’s Levels of Competence. Definitions available on the WACHS Nursing & Midwifery intranet webpage. All WACHS resuscitation assessors must supply evidence of currency of Assessor status and are to be recorded in the L&D system as the associated code level of 004, additionally trainers may also have a code level 005. Assessors need to supply evidence annually to their line manager of self-assessment and reflective practice activities in accordance with continuing professional development standards for professions governed through the Australian Health Practitioners Registration Authority (AHPRA). Assessors are not to undertake assessment responsibilities of others if their own competency status has lapsed. 4.4 Nurse Educators / Staff Development Nurses
The nurse educators / staff development nurses are to ensure: involvement in the development, implementation, evaluation and coordination of the
resuscitation education programs including the provision of flexible learning and assessment resources
the coordinator for each resuscitation program provides support for Managers and Assessors to allow on-site assessment
Document valid at: 05/04/2017 7:38 am
WACHS Resuscitation Education and Competency Assessment Policy
Date of Last Review: March 2017 Page 7 of 9 Date Next Review: March 2022
the program is flexible in delivery and can be accessed via various means; the program includes a skills recognition process learning and assessment resources including on-site manikins (low or high fidelity)
are readily available for staff, are in safe working order and are compliant with infection control policies and principles.
4.5 Regional Learning and Development The regional Learning and Development department is responsible for record keeping of the competency status of staff within their region in a format that is accessible by the appropriate managers and maintains confidentiality for individual staff members. 4.6 WACHS Learning and Development The WACHS L&D unit is responsible for the creation of codes for recording the completion of learning and assessment activities for all resuscitation programs across WACHS. The program development persons/team are responsible for the development of associated standardised learning and performance objectives.
5. Definitons
Advanced Life Support (ALS)
Includes advanced airway management, emergency ventilation, rhythm recognition, defibrillation, emergency pharmacology, teamwork in an emergency, post resuscitation care and special circumstances of paediatric and adult patients. ALS for nurses and medical officers includes defibrillation in manual and semi-automatic external defibrillation modes. Nurses should reflect on the Scope of Nursing Practic and Nursing Practice Standards (Nursing and Midwifery Board of Australia) to determine their performance requirements.
Automated External Defibrillation (AED)
External defibrillation using a voice prompting defibrillator which is pre-set to deliver a controlled shock to clients in Ventricular Fibrillation and rapid Ventricular Tachycardia only.
Basic Life Support (BLS) Cardiopulmonary Resuscitation (CPR) including of the adult, child and infant. Includes automated external defibrillation.
Close Proximity As defined in the staffing criteria outlined in the Code Blue/MER Policy requirements for individual site escalation templates – Appendix A
Manual Defibrillation External Defibrillation using a defibrillator in an operator-controlled function.
Document valid at: 05/04/2017 7:38 am
WACHS Resuscitation Education and Competency Assessment Policy
Date of Last Review: March 2017 Page 8 of 9 Date Next Review: March 2022
Medical Officer Medical staff who are responsible for the clinical care of a patient within a specified health care setting within the WACHS.
Newborn Resuscitation Resuscitation of the newborn (first hours of life) during the transitional period from intrauterine life.
Validation/Assessment Proven application of skills and knowledge within an identified framework that demonstrates competence in a given skill.
Validator / Assessor Persons with appropriate competency to assess the skills of others, must have competency in the skill to b validated as well as proven assessment skills.
6. Compliance
Failure to comply with this policy may constitute a breach of the WA Health Code of Conduct (Code). The Code is part of the Employment Policy Framework issued pursuant to section 26 of the Health Services Act 2016 (HSA) and is binding on all WACHS staff which for this purpose includes trainees, students, volunteers, researchers, contractors for service (including all visiting health professionals and agency staff) and persons delivering training or education within WACHS. WACHS staff are reminded that compliance with all policies is mandatory.
7. Evaluation Monitoring of compliance with point 3.1 is to be carried out by area/line managers. Compliance of resuscitation key performance indicators is 100%.
8. Legislation
Health Practitioner Regulation National Law (WA) Act 2010
9. References Australian Commission on Safety and Quality in Healthcare Australian Commission on Safety and Quality in Healthcare Recognition and Response to Clinical Deterioration Australian Flexible Learning Framework Australian Health Practitioner Regulation Agency Australian Resuscitation Council Guidelines International Liaison Committee on Resuscitation Sour, J., Mancini M.E., Bhanji F., Dennett J., Finn J., Huel-Ming Ma M., Perkins G.D., Rodgers D.L., Hazinski M.F., Jacobs I., Morley P.T.(2010). International Consensus on Cardiopulmonary Resuscitation and Emergency Care Science with Treatment Recommendations. Part 12 Education, implementation and teams.
Document valid at: 05/04/2017 7:38 am
WACHS Resuscitation Education and Competency Assessment Policy
Date of Last Review: March 2017 Page 9 of 9 Date Next Review: March 2022
King Edward Memorial Hospital Policies Nurses & Midwifery Board of Australia - National Framework for the Development of Decision-making Tools for Nursing and Midwifery Practice Princess Margaret Hospital for Children Policy – Resuscitation: MET and Code Blue – Responding to Clinical Deterioration
10. Related Policy Documents WACHS Clinical Escalation Including Code Blue Medical Emergency Response (MER) Policy WACHS Emergency (Disaster) Management Arrangements Policy WACHS Professional Development Requirements for Midwives Policy
11. Related WA Health Policies WA Health Clinical Deterioration Policy
12. WA Health Policy Framework Employment Policy Framework Clinical Governance, Safety and Quality Policy Framework.
This document can be made available in alternative formats on request for a person with a disability
Contact: Education Coordinator | Emergency Telehealth Service (L.Newman) Directorate: Nursing and Midwifery Services TRIM Record # ED-CO-13-108874
Version: 2.00 Date Published: 5 April 2017 Copyright to this material is vested in the State of Western Australia unless otherwise indicated. Apart from any fair dealing for the purposes of private study, research, criticism or review, as permitted under the provisions of the Copyright Act 1968, no part may be reproduced or re-used for any purposes whatsoever without written permission of the State of Western Australia.
Document valid at: 05/04/2017 7:38 am