Using Nominal Group Technique to investigate the views of people with intellectual disabilities on...
-
Upload
independent -
Category
Documents
-
view
4 -
download
0
Transcript of Using Nominal Group Technique to investigate the views of people with intellectual disabilities on...
Using Nominal Group Technique to investigate the views of people
with intellectual disabilities on end-of-life care provision
Irene Tuffrey-Wijne, Jane Bernal, Gary Butler, Sheila Hollins & Leopold Curfs
Accepted for publication 6 November 2006
Irene Tuffrey-Wijne BSc RN RNMH
Research Fellow
Division of Mental Health, St George’s,
University of London, London, UK
Jane Bernal MB ChB MRCPsych
Honorary Senior Lecturer
Division of Mental Health, St George’s,
University of London, London, UK
Gary Butler
Training Advisor
Division of Mental Health, St George’s,
University of London, London, UK
Sheila Hollins MBBS FRCPsych FRCPCH
Professor of Learning Disabilities
Division of Mental Health, St George’s,
University of London, London, UK
Leopold Curfs
Professor of Learning Disabilities
Department of Clinical Genetics, University
Maastricht/Academic Hospital Maastricht,
Maastricht, The Netherlands
Correspondence to I. Tuffrey-Wijne:
e-mail: [email protected]
TUFFREY-WIJNE I . , BERNAL J. , BUTLER G., HOLLINS S. & CURFS L. (2007)TUFFREY-WIJNE I. , BERNAL J. , BUTLER G. , HOLLINS S. & CURFS L. (2007)
Using Nominal Group Technique to investigate the views of people with intellectual
disabilities on end-of-life care provision. Journal of Advanced Nursing 58(1), 80–89
doi: 10.1111/j.1365-2648.2007.04227.x
AbstractTitle. Using Nominal Group Technique to investigate the views of people with
intellectual disabilities on end-of-life care provision
Aim. This paper is a report of a study using the Nominal Group Technique as a
method to elicit the views of people with intellectual disabilities on sensitive issues,
in this example end-of-life care provision.
Background. Establishing consumer views is essential in providing appropriate end-
of-life care, yet people with intellectual disabilities have historically been excluded
from giving their opinion and participating in research.
Methods. Nominal Group Technique was used in three groups, with a total of 14
participants who had mild and moderate intellectual disabilities. This technique
involves four steps: (1) silent generation of ideas, (2) round robin recording of ideas;
(3) clarification of ideas and (4) ranking of ideas (voting). Participants were pre-
sented with an image of a terminally ill woman (Veronica), and were asked: ‘What
do you think people could do to help Veronica?’
Findings. Participants generated a mean of nine individual responses. The highest
rankings were given to issues around involvement in one’s own care, presence of
family and friends, offering activities to the ill person, and physical comfort meas-
ures.
Conclusion. People with mild and moderate intellectual disabilities are capable of
expressing their views on end-of-life care provision, and should be asked to do so.
The Nominal Group Technique presents an effective and acceptable methodology in
enabling people with intellectual disabilities to generate their views.
Keywords: attitudes, death and dying, learning disabilities, Nominal Group Tech-
nique, palliative care, patient participation, qualitative approaches
Background
There has been a growing emphasis in recent decades on the
importance of obtaining consumer input around healthcare
delivery (Crawford et al. 2002). Where traditionally the
shaping of healthcare services may have been based
exclusively around the views of professionals, it is now
standard practice to take account of consumer preferences,
for example through consumer forums. Most healthcare
services in Western countries have seen a proliferation of
tools measuring the appropriateness, effectiveness and quality
of healthcare services and interventions (Streiner & Norman
RESEARCH METHODOLOGYJAN
80 � 2007 The Authors. Journal compilation � 2007 Blackwell Publishing Ltd
1995, Bowling 2002). People with intellectual disabilities
have historically been excluded from decision-making about
the delivery of services that affect their lives, generally based
on the presumption that they are incapable of forming an
opinion around their own problems and needs. Although
there is growing emphasis in the Western world on inclusion,
empowerment and self-advocacy (Department of Health
2001, Marks & Heller 2003, Brandon 2005), reports of
meaningful involvement of people with intellectual disabil-
ities in the shaping of healthcare services remain scarce
(Young & Chesson 2006).
Dramatic demographic changes over the past century
have resulted in increased longevity for people with
intellectual disabilities, with patterns of mortality and
morbidity now approaching those of the rest of the
population (Tuffrey-Wijne et al. in press). Little is known
about the palliative care provision for this client group, and
in particular, around the appropriateness of end-of-life care
currently being provided. This is a pertinent issue: as both
intellectual disability services and palliative care services are
faced increasingly with the prospect of providing prolonged
end-of-life care for people with intellectual disabilities, they
need to find ways of tailoring such care to their clients’
needs.
When it comes to palliative care, ascertaining consumer
views and satisfaction with services presents particular
challenges, yet in this area of health care, too, consumer
input has become an important factor (Small & Rhodes
2000, Aspinal et al. 2003). If both user-involvement and
person-centred care are taken seriously, it seems imperative
to establish the views of people with intellectual disabilities
on what they value at the end of life. The importance of this is
exemplified in studies that have shown discrepancies between
the views of patients and those of staff or relatives about
factors considered important at the end of life (Payne et al.
1996, Steinhauser et al. 2000a, Catt et al. 2005).
Palliative care is ‘an approach that improves the quality of
life of patients and their families facing the problems
associated with life-threatening illness’ (World Health
Organisation 2002). Inherent in this definition is the need
to establish what constitutes ‘quality of life’ for an individual.
During the past decade, the concept of ‘quality of life’ has
gained prominence in intellectual disability services, with a
growing emphasis on the need for quality of life applications
to be the basis for intervention and support (Schalock et al.
2002, Brown & Brown 2005). Whilst this is mostly hailed in
the literature as a positive development, it can also be
contentious, with concerns being raised that seeking to define
‘quality of life’ may lead to other people deciding what
constitutes a good quality of life for people with intellectual
disabilities, rather than empower people with intellectual
disabilities themselves (Northway & Jenkins 2003). From
this perspective too, then, ascertaining the views of people
with intellectual disabilities themselves on end-of-life care is
crucial, as they will be the experts on their own ‘quality of
life’.
Participative research, in which people with intellectual
disabilities are participants or even researchers themselves, is
gaining recognition (Kiernan 1999, Rodgers 1999, Walmsley
& Johnson 2003, Walmsley 2004). It is clear that people with
intellectual disabilities can and do express their views with
authority. However, in the area of palliative care, they have
been totally excluded; many are still being protected from
knowledge about death and dying (Todd 2004). Establishing
the views of people with intellectual disabilities about what is
important in end-of-life care provision may seem too difficult
a challenge. Apart from the existing taboos around death,
questions around palliative care may seem too abstract for
this client group. In addition, ethical concerns around
research involving people with intellectual disabilities in
questions around death and dying may seem prohibitively
challenging.
In other populations (such as hospice patients or the
elderly), views about end-of-life care have been elicited using
interviews (Townsend et al. 1990, Payne et al. 1996, Steinha-
user et al. 2000b, Vig et al. 2002), focus groups (Steinhauser
et al. 2000b, Tong et al. 2003) or postal questionnaires
(Steinhauser et al. 2000a). The choice of methodology for a
population of people with intellectual disabilities needs careful
consideration (Lindop 2006); some of the methods used in the
above studies are inappropriate for this group without major
adaptations.
The Nominal Group Technique
The Nominal Group Technique (NGT) was initially devel-
oped by Delbecq et al. (1975) as an organizational planning
tool. In healthcare settings, it has been used widely for
evaluating education (Davis et al. 1998, Lloyd-Jones et al.
1999, Lancaster et al. 2002, Dobbie et al. 2004), whilst it has
also been employed as a method for problem identification
and problem-solving in consumer groups (Miller et al. 2000,
Shewchuk & O’Connor 2002, Dewar et al. 2003). NGT
combines quantitative and qualitative data collection in small
groups of stake holders and typically involves four steps: (i)
silent generation of ideas by each individual; (ii) round-robin
recording of ideas; (iii) structured and time-limited discussion
of ideas; (iv) selection and ranking of ideas (voting) (Moore
1987). The advantages of this highly structured methodology
over Delphi and focus groups or brainstorming include an
JAN: RESEARCH METHODOLOGY The views of people with intellectual disabilities on end-of-life care provision
� 2007 The Authors. Journal compilation � 2007 Blackwell Publishing Ltd 81
avoidance of one individual monopolising the discussion,
allowing all participants to contribute equally, producing a
large pool of items, and being easy to implement (Gallagher
et al. 1993). A literature search produced highly limited
descriptions of the use of NGT with groups of people with
intellectual disabilities; one example is a study by Bostwick
and Foss (1981), who used it to identify major problems
faced by people with mild and moderate intellectual disabil-
ities in the domains of employment, community living and
social relationships.
The study
Aim
The aim of this study was to investigate the use of the
Nominal Group Technique as a method to elicit the views of
people with intellectual disabilities on sensitive issues, in this
example end-of-life care provision.
Participants
The participants were a convenience sample of 14 people
recruited from a London theatre company for people with
intellectual disabilities, aged between 25 and 45 years. We
had no access to their clinical notes, but they all functioned
within the mild/moderate range of intellectual disabilities
(mental retardation) as defined by ICD-10 (World Health
Organisation 1992). Two members of the research team
(including GB, who has intellectual disabilities himself)
visited the theatre company to explain the study to three
different groups of about 18 people, asking them to volunteer
to participate in the study by joining a data collection session
the following week. The topic and the research question were
explained explicitly. The researchers clarified that partici-
pants’ views were important and would be widely dissemin-
ated, albeit anonymized. The aim was to establish groups of
six participants, bearing in mind that the ideal group size for
NGT is between five and nine participants (Moore 1987).
Two groups produced six volunteers; in the third group more
people volunteered, and staff at the theatre company selected
those who were, in their opinion, most able to cope with the
topic and verbalize their ideas. The researchers were not
aware of participants’ personal bereavement history, but staff
were asked to indicate whether, given people’s personal
histories, they thought it was appropriate for them to
participate. This did not lead to anyone being excluded.
Because of limited resources, the only room available for
conducting the study was up stairs; regrettably, this led to one
person being excluded because of mobility problems. Partic-
ipants were given an explanatory letter to take home and
share with their family or carers, detailing the context and
content of the study. Carers were alerted to the possible need
of participants to discuss at home the issues raised in the
study, and were asked to contact the research team if they
had any concerns. No concerns were raised by family, carers
or staff.
Data collection
Data were collected on three consecutive days in 2006. Four
volunteers decided not to attend, stating a reluctance to
discuss death and dying on that particular day. This left a
total of 14 participants (two groups of four and one group of
six). All had verbal skills, although some lacked literacy
skills. Staff were asked to be alert to possible signs of distress
following to study, and the research team offered to de-brief
participants if needed. One person showed signs of distress
after the information session; staff supported her in talking
about her own losses. Participants received a small gift token
at the completion of the NGT session.
Nominal Group Technique
Nominal Group Technique is a single-question technique,
and its success depends on the unambiguity of a question that
can generate a wide range of answers. For this study, a
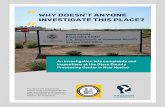
picture of a woman resting in an armchair was selected
(Figure 1), accompanied by the following statement and
question: ‘This is Veronica. Veronica is very ill. She is not
going to get better. The doctor knows that she is going to die.
What do you think people should do to help Veronica?’ The
question was piloted with two colleagues who had intellec-
tual disabilities, and who provided feedback on the appro-
priateness and accessibility of the question. Training for the
co-researchers (JB and GB) and two research assistants was
provided by the principal researcher (IT).
Each session was led by IT and GB, and supported by two
other members of the research team. A member of staff from
the theatre company was also present, but did not take part in
the data collection. After introductions, the participants were
shown the picture and asked the question.
Step 1: generating ideas
The objective of this part is to facilitate contributions from all
group members. Each participant worked individually with a
researcher, who wrote down the participants’ ideas verbatim.
To reduce the likelihood of bias through researcher influence,
facilitators had been instructed not to question participants’
answers nor make any suggestions. It was stressed that all
I. Tuffrey-Wijne et al.
82 � 2007 The Authors. Journal compilation � 2007 Blackwell Publishing Ltd
ideas were important and would be documented; there was
no limit to the number of ideas one individual could give.
Some participants had to wait until a researcher was available
to record their ideas. Most participants seemed pleased with
themselves after completing this step, smiling and giving
comments like ‘I did really well’.
Step 2: round robin recording of ideas
It was explained that this part of the process was to map the
group’s thinking, and to generate as wide as possible a range
of ideas from which participants could later choose the most
important ones. Participants were asked to read out (or to be
helped to read) one idea in turn, which was written verbatim
onto a flip chart. Some participants contributed new ideas,
inspired by those of other group members; these were also
recorded. No discussions or questions were permitted at this
stage. Each idea was affirmed; for example, when one parti-
cipant laughed at another’s idea of ‘an outing, like shopping
or going out for lunch’, commenting that Veronica surely
couldn’t do this as she was terminally ill, the group leader
noted that there may well be some terminally ill people who
would find the idea helpful.
Step 3: clarification
The group leader read through all the ideas written on the flip
charts, and asked for clarification where necessary. For
example, one participant who had suggested ‘lie in peace’ was
asked whether this meant ‘being in a peaceful room’, and
clarified that she meant ‘lie in peace after she dies’. Another
participant explained to the group what ‘make a will’ meant.
Step 4: voting
Whilst participants had lunch, the research team combined
the group’s ideas, collapsing similar ideas and simplifying the
wording. These were printed out onto separate pieces of
paper for each participant, producing sets of ‘voting slips’.
Participants were asked to select, individually, the five ideas
they thought were most important, putting all other slips of
paper aside. They were then asked to rank the ideas, giving a
score of 5 to the top idea, 4 to the next important idea, and so
on. Participants put the slips into voting boxes of decreasing
size, labelled 5 to 1. All researchers circulated the room
during this task, giving assistance where needed. Whilst some
participants could manage the task unaided, most (in par-
ticular those who lacked literacy skills) needed one to one
support. In most cases, the facilitating researcher read out
each idea and asked the participant whether to shortlist it or
not; the non-shortlisted ideas were removed, and the process
repeated until only five ideas remained. Many participants
found a comparison with the voting system at the Eurovision
Song Contest helpful, where the best song is given maximum
points.
Participants assisted in counting the votes. At the close of
the sessions, groups were asked for verbal feedback in
response to the simple question ‘What was it like for you to
be in this study?’ The whole process took around 2 hours,
including lunch.
Ethical considerations
Despite repeated efforts, we could find no ethics committee
responsible for work undertaken with the theatre company,
as this was a private company not governed by health or
social services. In recognition of the sensitive nature of this
study, we sought advice from the chairperson of the South
East London Multi-centre Research Ethics Committee to
ensure that the study was conducted with due regard for
ethical issues, particularly concerning informed consent,
minimizing harm, and follow-up. This study is part of a
larger programme of work by the research team, consisting of
Figure 1 The NGT question. ‘This is Veronica. Veronica is very ill.
She is not going to get better. The doctor knows that she is going to
die. What do you think people should do to help Veronica?’
JAN: RESEARCH METHODOLOGY The views of people with intellectual disabilities on end-of-life care provision
� 2007 The Authors. Journal compilation � 2007 Blackwell Publishing Ltd 83
in-depth investigation of the perspectives of people with
intellectual disabilities on end-of-life care. This wider body of
research has been rigorously reviewed and approved by the
South East London Multi-centre Research Ethics Committee
(Tuffrey-Wijne & Davies 2007).
Data analysis
Scores were added up for each idea, and the ideas were
ranked with the highest total score first, producing a list of
the groups’ ‘top ideas’. Identical scores were given the same
ranking number, although an idea that had more individual
votes was listed higher (for example, a score of 5 made up of
one vote of five points was lower on the list than one made up
of two votes of two and three points).
Results
Participants generated a mean of nine individual responses
(range 4–16). Identical responses were eliminated from the
group’s list, and collapsing ideas resulted in reducing the
number of ideas by half, leaving a total of 25, 17 and 15 ideas
respectively (See Table 1).
Participants appeared to have varying approaches to
answering the NGT question. Some searched the picture for
clues to what Veronica might want, resulting in suggestions
such as ‘close the window, give her a drink, keep her warm,
go to bed, someone to look after her dog when she goes to
hospital’. Others seemed to remember what happened when
they themselves had been ill: ‘give her a magazine, send cards
and flowers, watch TV’. A few participants based suggestions
on their experiences of the terminal illness of someone close
to them, for example: ‘Go into a nursing home’ and ‘Support
the parents because they are going to lose a daughter’.
The ideas put forward by the 14 participants were wide
ranging, covering several areas for end-of-life care provision.
These include factors associated with physical illness (medical
treatment, pain relief, food and drink, keeping warm),
involvement (tell her what is going on, listen to her wishes),
relationships (have family and friends around, phoning
friends, comfort and touch), organising supporting care (help
in the house, nursing presence, walk the dog, go to a nursing
home), keeping active and occupied (work, outings, TV,
magazines), atmosphere (lively, friendly, emotionally sup-
portive) and preparation for death (organize the funeral,
support the family, say goodbye).
The number of times an idea was suggested was no
indication of the final ranking of the idea; one of the highest
scores was given to an item that was suggested by only one
Table 1 Results
(a) Top 10 ideas for each group (with total score)
Group 1 (four participants)
1. Someone to listen to her wishes (7)
2. Make her comfortable and warm (5)
3. Have family and friends around (5)
3. Help her to go to work (5)
3. Ring an ambulance (5)
3. Care for her (5)
7. Help her to learn new things (4)
7. Hospital treatment (4)
7. Someone to walk her dog (4)
10. Help her family not to be scared (3)
Group 2 (six participants)
1. A ‘get well’ card, flowers and chocolate (17)
2. Get her a phone with credit so she can talk to her friends (14)
3. Get her family, sisters and neighbours (10)
4. Give her something she likes doing
(music, magazines, TV, book etc.) (10)
5. Ask her what she wants (6)
5. Give her medicine (6)
7. A nurse to come into the house and look after her (6)
8. Give her a cuddle and a kiss (5)
9. Get her something for her headaches (4)
9. Keep her warm enough (4)
Group 3 (four participants)
1. Tell her what is going on. Show her signs and pictures (9)
1. Support the parents; tell them what is going on (9)
3. Make her comfortable (8)
4. Have neighbours and friends around (6)
5. Go and do something (exercise, shopping and lunch) (5)
5. Someone to look after her (maybe a nurse) (5)
7. Organize the funeral (4)
8. Keep the pain away (4)
8. Someone to help her if she is feeling sad (4)
10. Go to bed, go to sleep (4)
(b) Other ideas (not in the top 10)
Be lively, happy, laughing
Help her to relax
Go into a nursing home
Someone living with her
Help with the housework
Give her food and drink
Lie in peace (after she dies)
Say goodbye
Check if she is hearing or not
An animal keeping her company
Make a will
Be friendly
Hold her hand
(c) Ideas with highest rankings across all groups
Involvement in one’s own care
Presence of family and friends
Offering activities to the ill person
Physical comfort measures
I. Tuffrey-Wijne et al.
84 � 2007 The Authors. Journal compilation � 2007 Blackwell Publishing Ltd
person, but then had all six group members voting for it
(Get her a phone with credit so she can talk to her friends),
whereas the same group did not give any votes to an item
suggested by all six group members (Give her food and
drink). Likewise, issues around involvement in one’s own
care were put forward by only one participant in each group,
yet in all groups received a relatively high number of votes,
ranking first in two groups. Other issues with the highest final
rankings in all three groups were the presence of family and
friends, and offering activities to the ill person. Physical
comfort measures (other than medication or pain relief) also
scored highly in two groups [See Table 1(c)].
Evaluating the session, all participants said that they had
enjoyed it, using words like ‘fun’ and ‘exciting’. They
particularly liked the opportunity to give their ideas and
voting. Participants commented that the process seemed
difficult at first, but once they had started they found it easy
to complete. Other comments included ‘it was good to learn
about it’ and ‘it gets you thinking about yourself’.
Feedback from staff at the theatre company suggested that
none of the participants showed any signs of distress
following the NGT sessions, although some talked about
friends or relatives who had died and of whom the study had
reminded them. During the sessions, however, several
participants asked whether Veronica (the woman in the
picture) was a real person, and commented how sad her
situation was. The researchers stressed that Veronica was not
real, and compared the picture to ‘a story’, which participants
seemed to find helpful and reassuring.
Discussion
Our findings show that the people with intellectual disabil-
ities who participated were able to think about a difficult and
often taboo topic, such as death and dying. They were not
only able to give their opinions and show an ability to think
about a wide variety of issues that may be of importance in
end-of-life care, but relished the opportunity to do so. One
important question to ask is whether the ideas put forward by
our participants, or their prioritization, were affected by the
presence of intellectual disability. Of particular interest is the
relatively high ranking in all groups of issues of involvement,
and the emphasis on practical measures and keeping occu-
pied; it could be hypothesized that people with intellectual
disabilities give greater priority to these issues than those
without such disabilities. The findings further suggest that it
may be important, when supporting people with intellectual
disabilities who are terminally ill, to consider not only who
are the important people in a person’s life (and ensure that
these are encouraged to offer support), but also what kind of
activities the person enjoyed previously, and hence to what
extent this can be built into their end-of-life support. Choice
in palliative care is often not only concerned with obvious
issues such as planning funerals, but also with day-to-day
issues related to the use of available time; for example, people
suffering from cancer-related fatigue may be helped to plan
their activities through energy-conservation measures (Barnes
& Bruera 2002, Lipman & Lawrence 2004).
Direct comparisons of the findings with a general popula-
tion would only be possible in a larger study involving
participants with and without intellectual disabilities. Stein-
hauser et al. (2000a) found that seriously ill patients
suggested similar factors to be of importance at the end of
life, including help with symptoms or personal care, prepar-
ation for the end of life and being treated as a ‘whole person’
(such as humour, dignity, presence of close friends and
having someone who will listen). Catt et al. (2005) used NGT
to assess older people’s attitudes to end-of-life issues, and
found that they valued choice, dignity, addressing social
isolation, involvement and preparation for death. It seems
likely that several attributes, including participants’ social
and family roles, their own experiences of death and dying,
and closeness to death, affect the findings of such studies. It is
also interesting to note that both Steinhauser et al. (2000a)
and Catt et al. (2005) made comparisons with the views of
healthcare professionals, and found discrepancies with the
responses of patients and older people themselves. This is a
pertinent issue for people with intellectual disabilities, who
may be less involved in decisions about their own care and
support, and more dependent on decisions made by carers
and professionals.
Our findings provide a strong argument for involvement of
people with mild and moderate intellectual disabilities who
are facing a life-threatening illness in establishing priorities
for their own care. This has implications for nurses and other
healthcare professionals in a wide range of settings, including
acute settings, primary care, palliative care and intellectual
disability services. They need to try and find appropriate
methods and approaches to enable people with intellectual
disabilities to express their views and wishes. Apart from the
option of straightforward discussions, one way of achieving
this may be to use part of the technique described here, by
showing the person an image of someone in a situation
similar to themselves and asking what this fictional person
might need and want. Our findings suggest that many people
with intellectual disabilities base their answers on personal
experience; it is, therefore, likely that people who themselves
are terminally ill could identify with the image and answer
accordingly. The use of pictures to enable people with
intellectual disabilities to talk about cancer has been found to
JAN: RESEARCH METHODOLOGY The views of people with intellectual disabilities on end-of-life care provision
� 2007 The Authors. Journal compilation � 2007 Blackwell Publishing Ltd 85
be effective (Tuffrey-Wijne et al. 2006). Any measures taken
to establish the views of people with intellectual disabilities
about their own end-of-life care necessitates the presence of
staff who are skilled and sensitive, and this may have
implications for training and staff support. Nurses need to be
aware, however, that openness about death and dying can be
contentious amongst families and carers, and good collabor-
ation between everyone involved in a person’s care is crucial
(Tuffrey-Wijne 2003, Todd 2004, Brown et al. 2005).
Using NGT
Despite the particular context and limited sample size, affect-
ing representativeness of this study, the methods used in this
study may be generalizable and thus of interest to nurses and
other healthcare practitioners who are working with people
with intellectual disabilities and endeavouring to establish user
perspectives. This study could be regarded as a pilot study for
the use of NGT in this context; it is therefore important to
describe some of the methodological issues that emerged.
Moore (1987) states that ‘NGT is easy to learn and use,
(and) groups enjoy participating in an NGT because they
realize they have been unusually productive in a relatively
brief time’ (p 35). For people with intellectual disabilities,
who have seldom been asked for their opinion and have been
excluded from participating in research, the experience of
giving and ranking ideas may be particularly empowering. It
is crucial to create a safe and structured environment within
the group, calling for a skilled and experienced group
facilitator. NGT is a highly structured approach, which
may be particularly suitable for people with intellectual
disabilities. In a discussion of interviewing people with
intellectual disabilities, Booth and Booth (1994) note a
tendency to answer questions with a single word or a short
phrase, and a responsive rather than a proactive style. They
recommend that ‘techniques other than just talking have to
be used to engage the informant’ (p. 421). Sigelman et al.
(1981, 1982) found that a structured approach to questioning
produced the highest responsiveness. They conclude that
although open-ended questions were more difficult for
respondents, these were preferable to yes/no questions,
because of a tendency among people with intellectual
disabilities to respond ‘Yes’ regardless of the question. In
the light of these findings, it seems that NGT has great
potential for use with people with intellectual disabilities.
Following our study, a number of observations and
recommendations for further studies can be made. Whilst
certain ideas were consistent between groups in this study,
each group came up with entirely new suggestions, indicating
that saturation of ideas had not been reached. Considering
the fact that many participants voted for ideas that were
generated by others, it may be worth repeating the study with
other groups of people with intellectual disabilities until
saturation is reached, to develop a forced choice inventory
based on the most consistently high-ranking ideas that could
then be used by larger groups of participants (Bostwick &
Foss 1981).
The process of sorting and ranking ideas was the most
challenging for the participants, particularly for those who
lacked literacy skills. Confronted with a large number of
pieces of paper with printed text, some participants struggled
with the need to compare and prioritize sometimes abstract
concepts. A simple picture or other visual reminder on each
voting slip might be a source of bias, as some participants
might simply vote for the most attractive picture, but this risk
may outweigh the disadvantages of only using written text. It
would reduce the need for facilitator input (which is in itself a
potential source of bias), as well as enabling those with more
severe intellectual disabilities to participate. Other threats to
reliability include the possibility that participants might
choose randomly when confronted with a ranking decision;
this could be detected by measures to reduce bias, for
example, asking the person to do the task twice (Streiner &
Norman 1995).
Repeating NGT with different groups presents problems
with data analysis, as each group generates different lists of
items that are then difficult to compare. In collapsing the
individual responses into more general ideas for voting
purposes, we considered it important to remain as close as
possible to participants’ original ideas, resulting in slight
variations in wording, although concepts may have been
similar between groups (e.g. ‘someone to listen to her wishes’
and ‘ask her what she wants’). Having groups of only four
participants affects the validity of the final rankings, as even
one (possibly random) vote could move an item towards the
top of the list. Again, developing a standard set of items that
could then be voted on by larger groups of participants would
overcome the problem of analysis, although it may reduce
‘ownership’ (and therefore acceptability) of the process if
participants have not had a chance to generate their own ideas.
We recommend that when conducting NGT sessions with
people with intellectual disabilities, inviting eight participants
to each group is ideal; it is possible to accommodate eight
people in a group, whilst non-attendance should not reduce
the size of the group too much.
This study was conducted with people with mild and
moderate intellectual disabilities. To participate, a certain
level of verbal ability and a capacity to express ideas is
essential, although it may be possible for people without such
ability to take part in the final steps (voting). NGT in this
I. Tuffrey-Wijne et al.
86 � 2007 The Authors. Journal compilation � 2007 Blackwell Publishing Ltd
format is not suitable for people with severe and profound
intellectual disabilities, who will have difficulty conceptual-
izing the question; to establish their views on end-of-life care
provision, a different methodology may be more appropriate;
one possibility would be participant observation (Angrosino
2004, Tuffrey-Wijne & Davies 2007).
Study limitations
Threats to validity and reliability have already been noted
above. Given the limited sample size, the findings need to be
treated with caution and are not easily generalizable. It is
worth noting, in particular, that people with intellectual
disabilities are a highly heterogeneous group, with wide
variations not only in level of intellectual ability and ability to
think in abstract concepts, but also in their own personal
experiences of death and dying. These variations may all
affect the way participants prioritize end-of-life care issues. It
is also worth noting that the participants in this study, as
members of a theatre company, were used to working in
groups and generating ideas.
Conclusion
The study demonstrates that people with mild and moderate
intellectual disabilities are capable of giving their opinion,
and indeed should be asked to do so. This paper presents a
template for researchers, service managers and healthcare
providers who wish to assess the views of people with
intellectual disabilities about care and services provided. The
tools presented here are eminently transferable and can be
employed in other domains affecting the lives of people with
intellectual disabilities. More work is clearly warranted in the
important area of end-of-life care, particularly concerning
factors (such as age, life experience, level of intellectual
ability and social role) that affect the way people prioritize
issues. If we have demonstrated that people with intellectual
disabilities can contribute ideas about a taboo subject, such
as death and dying, then nurses and other health and social
care professionals have an obligation to involve them in
decisions about their care.
Acknowledgements
We are indebted to the participants and staff at the Theatre
Company in London for their generous help with this study.
Thanks to Michael Woodman for secretarial and technical
support, and help with data collection. The picture of
Veronica is taken from the book Getting On With Cancer
(Donaghey et al. 2002), with kind permission from the
publishers.
Author contributions
IT, JB and GB were responsible for the study conception and
design and IT was responsible for the drafting of the
manuscript. IT, JB and GB performed the data collection
and IT performed the data analysis. JB and LC made critical
revisions to the paper. SH and LC supervised the study.
References
Angrosino M. (2004) Participant observation and research on intel-
lectual disabilities. In The International Handbook of Applied
Research in Intellectual Disabilities (Emerson E., Hatton C.,
Thompson T. & Parmenter T., eds), John Wiley & Sons Ltd,
Chichester, pp. 161–177.
Aspinal F., Addington-Hall J., Hughes R. & Higginson I. (2003)
Using satisfaction to measure the quality of palliative care: a review
of the literature. Journal of Advanced Nursing 42, 324–339.
Barnes E. & Bruera E. (2002) Fatigue in patients with advanced
cancer: a review. International Journal of Gynecological Cancer
12, 424–428.
What is already known about this topic
• Growing numbers of people with intellectual disabilities
face a prolonged terminal illness and are in need of
appropriately tailored end-of-life care.
• People with intellectual disabilities have traditionally
been excluded from expressing their views on issues that
affect their lives, and from participating in research.
• End-of-life care provision for this group has been based
on the views of professionals, rather than those of pa-
tients.
What this paper adds
• The views of people with intellectual disabilities on
death, dying and end-of-life care have not been inves-
tigated or described in the literature. This paper shows
that people with intellectual disabilities want to give
their views, and are capable of doing so.
• The use of Nominal Group Technique with people with
intellectual disabilities has been limited. This paper
describes clearly how the methodology can be used with
this group, thus providing a template for other
researchers and service providers who wish to establish
the views of people with intellectual disabilities on is-
sues around service delivery.
JAN: RESEARCH METHODOLOGY The views of people with intellectual disabilities on end-of-life care provision
� 2007 The Authors. Journal compilation � 2007 Blackwell Publishing Ltd 87
Booth T. & Booth W. (1994) The use of depth interviewing with
vulnerable subjects: lessons from a research study of parents with
learning difficulties. Social Science & Medicine 39, 415–425.
Bostwick D. & Foss G. (1981) Obtaining consumer input: two
strategies for identifying and ranking the problems of mentally
retarded adults. Education & Training of the Mentally Retarded
16, 207–212.
Bowling A. (2002) Research Methods in Health: Investigating Health
and Health Services, 2nd edn. Open University Press, Buckingham.
Brandon T. (2005) Empowerment, policy levels and service forums.
Journal of Intellectual Disabilities 9, 321–331.
Brown R. & Brown I. (2005) The application of quality of life.
Journal of Intellectual Disability Research 49, 718–727.
Brown H., Burns S. & Flynn M. (2005) Dying Matters: A Workbook
on Caring for People with Learning Disabilities Who are Ter-
minally Ill. The Mental Health Foundation, London.
Catt S., Blanchard M., Addington-Hall J., Zis M., Blizard B. & King
M. (2005) The development of a questionnaire to assess the atti-
tudes of older people to end-of-life issues (AEOLI). Palliative
Medicine 19, 397–401.
Crawford M., Rutter D., Manley C., Weaver T., Kamaldeep B.,
Fulop N. & Tyrer P. (2002) Systematic review of involving patients
in the planning and development of health care. British Medical
Journal 325, 1263–1265.
Davis D., Rhodes R. & Baker A. (1998) Curriculum revision:
reaching faculty consensus through the Nominal Group Technique.
Journal of Nursing Education 37, 326–328.
Delbecq A., Van de Ven A. & Gustafson D. (1975) Group Techniques
for Program Planning. Scott, Foresman and Company, Glenview, IL.
Department of Health (2001) Nothing About Us Without Us.
Department of Health, London.
Dewar A., White M., Posade S. & Dillon W. (2003) Using nominal
group technique to assess chronic pain, patients’ perceived chal-
lenges and needs in a community health region. Health Expecta-
tions 6, 44–52.
Dobbie A., Rhodes M., Tysinger J. & Freeman J. (2004) Using a
modified nominal group technique as a curriculum evaluation tool.
Family Medicine 36, 402–406.
Donaghey V., Bernal J., Tuffrey-Wijne I. & Hollins S. (2002) Getting
on with Cancer. Gaskell/St George’s Hospital Medical School,
London.
Gallagher M., Hares T., Spencer J., Bradshaw C. & Webb I. (1993)
The nominal group technique: a research tool for general practice?
Family Practice 10, 76–81.
Kiernan C. (1999) Participation in research by people with learning
disability: origins and issues. British Journal of Learning Disabil-
ities 27, 43–47.
Lancaster T., Hart R. & Gardner S. (2002) Literature and medicine:
evaluating a special study module using the nominal group tech-
nique. Medical Education 36, 1071–1076.
Lindop E. (2006) Research, palliative care and learning disability. In
Palliative Care for People with Learning Disabilities (Read S., ed.),
Quay Books, London, pp. 153–165.
Lipman A. & Lawrence D. (2004) The management of fatigue in
cancer patients. Oncology 18, 1527–1535.
Lloyd-Jones G., Fowell S. & Bligh J. (1999) The use of the nominal
group technique as an evaluative tool in medical undergraduate
education. Medical Education 33, 8–13.
Marks B. & Heller T. (2003) Bridging the equity gap: health pro-
motion for adults with intellectual and developmental disabilities.
Nursing Clinics of North America 38, 205–228.
Miller D., Shewchuk R., Elliot T. & Richards S. (2000) Nominal
group technique: a process for identifying diabetes self-care issues
among patients and caregivers. The Diabetes Educator 26,
305–314.
Moore C. (1987) Group Techniques for Idea Building. Sage Publi-
cations, London.
Northway R. & Jenkins R. (2003) Quality of life as a concept for
developing learning disability nursing practice? Journal of Clinical
Nursing 12, 57–66.
Payne S., Langley-Evans A. & Hillier R. (1996) Perceptions of a
‘good’ death: a comparative study of the views of hospice staff and
patients. Palliative Medicine 10, 307–312.
Rodgers J. (1999) Trying to get it right: undertaking research invol-
ving people with learning difficulties. Disability & Society 14,
421–433.
Schalock R., Brown I., Brown R., Cummins R., Felce D., Matikka L.,
Keith K. & Parmenter T. (2002) Quality of life: its con-
ceptualization, measurement and application. A consensus docu-
ment. Mental Retardation 40, 457–470.
Shewchuk R. & O’Connor S. (2002) Using congitive concept map-
ping to understand what health care means to the elderly: an
illustrative approach for planning and marketing. Health Market-
ing Quarterly 20, 69–88.
Sigelman C., Budd E., Spanhel C. & Schoenrock C. (1981) When in
doubt, say yes: acquiescence in interviews with mentally retarded
persons. Mental Retardation 19, 53–58.
Sigelman C., Budd E., Winer J., Schoenrock C. & Martin P. (1982)
Evaluating alternative techniques of questioning mentally retarded
persons. American Journal of Mental Deficiency 86, 511–518.
Small N. & Rhodes P. (2000) Too Ill to Talk? User Involvement and
Palliative Care. Routledge, London.
Steinhauser K., Christakis N., Clipp E., McNeilly M., McIntyre L. &
Tulsky J. (2000a) Factors considered important at the end of life by
patients, family, physicians, and other care providers. JAMA 284,
2476–2482.
Steinhauser K., Clipp E., McNeilly M., Christakis N., McIntyre L. &
Tulsky J. (2000b) In search of a good death: observations of pa-
tients, families, and providers. Annals of Internal Medicine 132,
825–832.
Streiner D. & Norman G. (1995) Health Measurement Scales, 2nd
edn. Oxford University Press, Oxford.
Todd S. (2004) Death counts: the challenge of death and dying in
learning disability services. Learning Disability Practice 7, 12–15.
Tong E., McGraw S., Dobihal E., Baggish R., Cherlin E. & Bradley
E. (2003) What is a good death? Minority and non-minority per-
spectives. Journal of Palliative Care 19, 168–175.
Townsend J., Fermont D., Dyer S., Karran O., Walgrove A. & Piper
M. (1990) Terminal cancer care and patients’ preference for place
of death: a prospective study. British Medical Journal 301, 415–
417.
Tuffrey-Wijne I. (2003) The palliative care needs of people with
intellectual disabilities: a literature review. Palliative Medicine 17,
55–62.
Tuffrey-Wijne I. & Davies J. (2007) This is my story: I’ve got cancer.
‘The Veronica Project’: and ethnographic study of the experiences
I. Tuffrey-Wijne et al.
88 � 2007 The Authors. Journal compilation � 2007 Blackwell Publishing Ltd
of people with learning disabilities who have cancer. British
Journal of Learning Disabilities 35, 7–11.
Tuffrey-Wijne I., Bernal J., Jones A., Butler G. & Hollins S. (2006)
People with intellectual disabilities and their need for cancer in-
formation. European Journal of Oncology Nursing 10, 106–116.
Tuffrey-Wijne I., Hogg J. & Curfs L. End-of-life and palliative
care for people with intellectual disabilities who have cancer or
other life-limiting illness: a review of the literature and available
resources. Journal of Applied Research in Intellectual Disabilities,
in press.
Vig E., Davenport N. & Pearlman R. (2002) Good deaths, bad
deaths, and preferences for the end of life: a qualitative study of
geriatric outpatients. Journal of the American Geriatrics Society
50, 1541–1548.
Walmsley J. (2004) Involving users with learning difficulties in health
improvement: lessons from inclusive learning disability research.
Nursing Inquiry 11, 54–64.
Walmsley J. & Johnson K. (2003) Inclusive Research with People
with Learning Disabilities. Jessica Kingsley Publishers, London.
World Health Organisation (1992) ICD-10: International Statistical
Classification of Diseases and Related Health Problems (10th
Revision). World Health Organisation, Geneva.
World Health Organisation (2002) National Cancer Control Pro-
grammes: Policies and Managerial Guidelines. World Health
Organisation, Geneva.
Young A. & Chesson R. (2006) Obtaining views on health care from
people with learning disabilities and severe mental health pro-
blems. British Journal of Learning Disabilities 34, 11–19.
JAN: RESEARCH METHODOLOGY The views of people with intellectual disabilities on end-of-life care provision
� 2007 The Authors. Journal compilation � 2007 Blackwell Publishing Ltd 89