Citrate Toxicity During Massive Blood Transfusion - Notify ...
The incidence/window period model and its use to assess the risk of transfusion-transmitted human...
-
Upload
independent -
Category
Documents
-
view
3 -
download
0
Transcript of The incidence/window period model and its use to assess the risk of transfusion-transmitted human...
TRANSFUSION MEDICINE
REVIEWS Vol 11, No 3 JUL Y 1997
The I n c i d e n c e / W i n d o w Per iod M o d e l and its Use to Assess the Risk of T r a n s f u s i o n - T r a n s m i t t e d H u m a n I m m u n o d e f i c i e n c y
Virus and Hepat i t i s C Virus I n f e c t i o n
Steven Kleinman, Michael P. Busch, James J. Korelitz, and George B. Schreiber
A CCURATE ESTIMATES of transfusion-trans- mitted risks are important to enable policy
makers to evaluate the expected benefit and costs of proposed interventions to further reduce transfusion- transmitted infection risk, as well as to allow patients and physicians to make informed decisions about whether to receive an allogeneic transfusion
/ . .
or to select another therapeutic option. Although each donated unit of blood is tested for
evidence of infection by specific viral agents, there are at least four potential reasons why transmission of these viral agents still might occur. The primary reason is that the donor has negative laboratory test results during the early stages of infection, known as the window period. A second factor contributing to the risk of transfusion-transmitted infection 'for some agents is the existence of a chronic carrier state in which a clinically asymptomatic donor will persistently test negative on a donation screening assay. Thirdly, a viral agent may have a large enough degree of genetic diversity so that labora- tory screening tests fail to identify som~ infectious donors who harbor a particular atypical genetic variant. A fourth factor contributing theoretically to a possible transfusion-transmitted infection is labo- ratory error in performing the screening tests; however, given the low prevalence of infected donors and the high accuracy of automated testing, the occurrence of such errors is thought to be extremely rare.
The most scientifically accurate method of di- rectly establishing transfusion-transmitted infec- tion risk is to perform a prospective controlled study of transfusion recipients. In this type of study,
blood specimens are obtained before transfusion and at periodic intervals posttransfusion; such studies are further strengthened when serum samples from recipients and/0r donors are frozen so that they may be reevaluated when more sensitive blood screening tests become available. Since the mid 1970s, the National Heart, Lung, and Blood Insti- tute has funded three such studies: The Transfusion Transmitted Virus Study (TTVS; recipients trans- fused from 1974 through 1979), the Transfusion Safety Study (recipients transfused in 1984 and 1985), and the Frequency of Agents Communicated by Transfusion Study (recipients transfused from 1985 to 1991). 1-3 In addition, investigators at the National Institutes of Health (NIH) Clinical Center have performed ongoing studies of the incidence of posttransfusion hepatitis for the past two decades. 4
A second direct method of determining risk involves screening donor units with sensitive labo- ratory tests that are not used routinely in donor testing. This approach requires large numbers of samples to be tested in a real time mode before the
From the Retrovirus Epidemiology Donor Study and from Westat Inc, Rockville, MD; Irwin Memorial Blood Centers, San Francisco, CA, the University of California at San Francisco, San Francisco, CA; the American Red Cross Greater Chesa- peake and Potomoc Region, Baltimore, MD; the American Red Cross Southeastern Michigan Region, Detroit, All; the Ameri- can Red Cross Southern California Region, Los Angeles, CA; the Oklahoma Blood Institute, Oklahoma City, OK," and the National Heart, Lung, and Blood Institute, Bethesda, MD.
Address reprint requests to Steven Kleinman, MD, 1281 Roekcrest Ave, Victoria, British Columbia, V9A 4W4, Canada.
Copyright �9 1997 by W.B. Saunders Company 0887- 7963/97/1103-0001 $3.00/0
Transfusion Medicine Reviews, Vol 11, No 3 (July), 1997: pp 155-172 155
156 KLEINMAN ET AL
routine release of blood components for distribu- tion. Such studies are logistically difficult in the current climate of intense regulatory scrutiny.
Ironically, because transfusion transmitted risks are currently so low in developed countries, it is exceedingly difficult to accurately measure these risks. Such measurement would require very large sample sizes and would be extremely expensive, and it is unlikely that prospective studies of transfu- sion recipients or large-scale parallel evaluations of donor samples with research tests will be con- ducted in the forseeable future. Therefore, it is necessary to rely on other methods that use indirect measures to assess risk: methods that generate a risk estimate by making reasonable assumptions and then applying appropriate calculations to spe- cific well-defined data sets.
A recent approach, employed by investigators from the Retrovirus Epidemiology Donor Study (REDS) and independently by the Centers for Disease Control and Prevention (CDC), has been to estimate risk by using an incidence/window period model. 5,6 The model is applicable to any transfu- sion transmissible agent that is characterized by a window period before detection by blood screening assays. This article provides a detailed description of various aspects of this model as used by REDS investigators including the various assumptions on which it is based, the methods used to collect the data and calculate risk, and the strengths and limitations of the approach. Residual risk estimates for human immunodeficiency virus (HIV) and hepatitis C virus (HCV) are reported and are compared with previously published estimates. Because the method of determining the incidence rate for hepatitis B virus (HBV) infection is based on the incidence of a transient marker (HBsAg), the application of the model to HBV infection is more complex and is reviewed elsewhere. 7
Before considering the model in detail, several general methodological issues warrant consider- ation. Although transfusion-transmitted risk esti- mates yield a single best estimate of risk (known as the point estimate), they usually include wide ranges or confidence limits resulting from the very low rates of 'risk being measured and the need to estimate certain variables. Risk estimates are sensi- tive to the screening tests used and must be revised when newer, more sensitive donor screening or laboratory testing protocols are adopted. Because estimates may have been obtained in particular
geographic areas, caution must be exercised in generalizing the results to other locations. Nonethe- less, the incidence/window period model is able to address some of these issues. The method allows for data to be updated and expanded over time, yielding tighter confidence intervals. Time trends can also be examined and risk estimates can also be compared across different geographic regions that have used the same method.
Studies reported in the late 1960s through the mid 1980s expressed infection risk o n ' a per- recipient basis. This method of reporting data made it difficult to compare the risk for patients receiving different numbers of transfusion. More recently, it has become standard practice to express the risk of infection on a per-unit or per-blood component basis; ie, the risk per unit is a given percentage (for example, 0.001%) or 1 in a given number (for example, 1 in 100,000). It is important to remember" that when such per-unit risk estimates are presented to an individual patient or a physician, the risk needs to be adjusted for the number of units (or more precisely, the number of donor exposures) to be received by that particular patient. The math- ematically correct way to determine per-patient risk is as follows, where p represents the probability of infection with a given blood unit and n represents the number of units transfused: the probability that a single unit is free of infection is ( l - p), the .probability that all n units that the recipient re- ceives would be infection free is ( l - p)n and, therefore, the probability that a recipient would get infected would be one minus the probability that he would not get infected or l - ( l - p ) n . Because transfusion risks are small (eg, < 1%), this formula simply reduces to p • n; therefore, the per-patient risk can be obtained by multiplying the per-unit risk by the number of units transfused.
PRINCIPLES OF THE INCIDENCE/WINDOW PERIOD MODEL
Two common measures of risk in medical re- search are prevalence and incidence. Prevalence provides information on the number and percent- age o f people who are currently affected by a particular condition (eg, the percentage of donors who have antibodies to an infectious disease agent). Although prevalence has obvious importance in estimating the current magnitude of a health prob- lem, it does not provide any indication of when an infection occurred, which is crucial in the blood
INCIDENCE/WINDOW PERIOD MODEL FOR TX RISK 157
donor setting. People who were infected long ago will present as prevalent cases but their donations will test positive and will be discarded. Therefore, the use of prevalence data to project transfusion- transmitted viral risk would be likely to overesti- mate the true risk.
A more important question relates to the rate at which negative donors are becoming positive, or seroconverting. Whereas people who have serocon- verted will test positive and their donations will be excluded, donors who are very recently infected may be in the window period when their donations are infectious but not yet detectable by current tests. The rate of observed seroconversion is termed the incidence and is an important variable that can be used to estimate the number of infectious, seronegative donations.
The incidence rate measures the number of new events that occur within a given time period. The two key features of an incidence rate worth empha- sizing are that it measures a change in a person's status (eg, change from noninfectious to infectious) and that the time period in which the change occurs must be specified. Both of these features are critical for estimating the risk that a donor will be infec- tious but seronegative at the time of donation.
Definition and Calculation of Incidence Rate in Repeat Donors
The incidence rate is defined as the number of newly infected donors divided by the observed person-time at risk. To be counted as an incident donor and included in the numerator, a donor first must have given a seronegative donation at one point in time and then subsequently given a sero- positive donation. Therefore, by definition the incidence is calculated from repeat donorS (or more specifically, from donors who give more than one donation during the study period).
The denominator of the incidence is based on the
amount of time observed among all donors who gave at least two donations during the study peroid. (This is termed person-time.) Table 1 provides an example in which there are two incident donors (donor C and donor D) among a total of four donors. One overly simplistic approach is to calcu-: late the proportion of infected donors, ie, two out of four donors, or 50%, and to equate this with the incidence; this approach treats each of the four donors equally although they were observed for different amounts of time (eg, donor A was ob- served to remain seronegative for approximately 24 months whereas donor B was observed for only 12 months). This method of calculation is inadequate because the incidence must account for variations in donation intervals: This is done by summing the amount of time observed from each donor (person- time between first and last donations). A slight adjustment is made for seroconverfing donors by assuming they seroconverted at the midpoint be- tween their last seronegafive donation and seroposi- tive donation. The amount of person-time added to the denominator in these cases is stopped at this midpoint, because the seroconverted donor is now no longer "at risk" of seroconverting. To calculate risk from potentially transfusable units, an adjusted incidence variable, which takes into consideration whether the previous seronegative unit met all requirements for transfusion, needs to be calcu- lated. In this modification, all donations from a given donor are evaluated sequentially and an interval is included in the calculation only if the first donation of the interval was nonreactive on all standard serological screening tests and not ex- cluded by the confidential unit exclusion (CUE) process.
As seen in Tables 1 and 2, the incidence is computed by dividing the number of incident cases by the cumulative total of person-time at risk; in our hypothetical example, the incidence is calcu-
Table 1. Example of Incidence Rate Calculation
First Donation Last Donation Incident ]]me Interval Person-Months
Donor Date Result Date Result Case (months) (at risk)*
A January 1991 nonreactive January 1993 nonreactive no 24 24 B January 1991 nonreactive January 1992 nonreactive no 12 12
C April 1991 nonreactive December 1992 positive yes 20 10
D March 1992 nonreactive November 1992 positive yes 8 4
Note: There are two incident cases observed during 50 person-months at risk. Incidence = 2 seroconverting (SC) persons/50
person-months = 0.04 SC per month. *For seroconverting donors (donors C and D) person-months are tabulated assuming that seroconversion occurred at the midpoint
between their seronegative and seropositive donations.
158 KLEINMAN ET AL
Table 2. Calculations Used in the Incidence/Window Period Model
number of seroconverting (SC) donors
Incidence = person-years of Observation of donor population
Adjusted incidence -
number of SC donors whose previous donations were seronegative for all markers
person-years of observation
Risk (per unit)* = adjusted incidence • w indow period t
(expressed as fraction of year)
New test yield (.pet unit)* = Adjusted incidence
• Decrease in w indow periodll (fraction of year)
Annual yield of proposed new tests = new test yield
• annual number of donations ~
or annual number of components w
*Usually expressed as risk per 108 units.
~Time from exposure or infectiousness to seroconversion
(see text). *Usually expressed as yield per 107 units.
New test relative to standard blood screening assay.
REDS uses 12 million donations or 18 million components for this calculation.
lated as 2/50 = 0.04 seroconverting persons per person-month or, as the "persons" cancel out each other, 0.04 seroconversions (SC) per month. When the incidence is small and constant over the study period, the incidence is approximately equal to a probability. 8 In this example, the 0.04 SC per month incidence could be interpreted as the prob- ability of seroconversion within 1 month being equal to 0.04, or 4%. Turning to a more realistic example (see next section), results from REDS show an HIV incidence of 4.01 per 100,000 person-years, or a probability of seroconverting within 1 year equal to 0.0041%.
Source of REDS Incidence Data
REDS is conducted at five blood centers in different parts of the United States: the Irwin Memorial Blood Centers in San Francisco, CA; the Oklahoma Blood Institute in Oklahoma City, OK; and the American Red Cross Blood Services in the Greater Chesapeake and Potomac (Baltimore, MD), the Southeastern Michigan (Detroit, MI), and South- eru California (Los Angeles, CA) Regions. Westat, Inc, Rockville, MD is the coordinating center. Incidence data presented in this review were ob- tained from allogeneic and apheresis donors who donated at least twice during the study period
(between January 1, 1991 and December 31, 1993 for HIV and between April 1992 [the introductory date of HCV EIA-2 (enzyme immunoassay) test- ing] and December 31, 1993 for HCV). Before accepting a case as a seroconversion, a detailed review of screening and confirmatory test results was conducted to exclude any possible false posi- tive results. Person-years of observation were summed for all donors with two or more donations, and incidence data were expressed per 100,000 person-years.
Window Period Estimates
The infectious window period can be defined as the interval between the time a donor becomes infectious and the time that a particular laboratory test becomes positive. This infectious window period will differ from the more conventional window period (defined as the interval between the time the donor acquired the infection and the development of a positive laboratory test)'if there is a lag between the acquisition time of infection and the donor's ability to transmit the infection to others by blood transfusion. Theoretically such a lag would exist if, on initial exposUre to the viral agent, the donor were able to sequester the virus in the organs of the immune system before becoming viremic. Experimental animal evidence suggests that the difference between the conventional and infectious windows for retroviruses may range from 2 to 14 days. 9
Accurate measurement of the infectious window period would ideally require the establishment of the date of the individual's initial exposure to the infectious agents, the time when the individual becomes infectious, and the collection of multiple serial samples from the individual at closely spaced intervals (a few days to a week) for several weeks to several months after infection to precisely define the date of seroconversion to each marker. Such samples would need to be collected from a large number of such individuals to accurately establish the mean and range of the exposure and infectious window periods.l~
There are two types of sample sets that fit these ideal criteria fairly well. One source is samples from transfusion recipients who were prospectively enrolled in transfusiol.a transmission studies before the availability of specific viral ~screening assays. When these samples are retrospectively tested, recipients who seroconverted or became polymer-
INCIDENCE/WINDOW PERIOD MODEL FOR TX RISK 159
ase chain reaction (PCR) positive can be detected; the date of infection in such cases is definitively known (ie, the date of transfusion), and samples collected at fairly closely spaced intervals are available. However, the number of infected indi- viduals identified in such studies is small, and the samples most often must be obtained from limited repository resources. Such cohorts exist for HCV, HBV, and HTLV-I (Human T-cell lymphotropic vim s type 1), but not for HIM. 1,4,tl A second sample source is from paid plasmapheresis donors. Many of these donors donate up to twice a week for long periods and there continue to be a significant number of new infections in this population. Impor- tantly, these infections reflect contemporary rather than historical events, and sample volumes may be large (often entire units of plasma axe available from 10 or more serial donations before seroconver- sion). However, it is not usually possible to estab- lish the date of initial infection in these donors with certainty; rather, this date must be inferred from the earliest detection of viral nucleic acid by PCR or other methods. Because of this imprecision with regard to date of exposure, these types of samples are better suited for determining the ability of a new laboratory test to shorten the window relative to a test with an already established window period. When neither of these sample sources have been available, approaches using alternative sources of data have been used (see section on HIV window period later in this article).
Calculation of Transfusion-Transmitted Risk
When the incidence is small (such as in the case of HIV in blood donors) it is essentially eq'uivalent to a probability or risk. 8 ff the HIV incidence is 4.01 per 100,000 person-years (or a probability of 0.0041%), then the risk of a person seroconverting within a 1-year period can be equivalently ex- pressed as 1 in 25,000. Commonly, incidences (or probabilities) are used to predict the future, such as to estimate that 1 in 25,000 donors will become infected within the next year. However, the same incidence could also be interpreted as 1 in 25,000 donors were infected within the past year. The reason for thisdistinction is that, in the blood donor setting, the key question is not, what is the probabil- ity that a donor will become infected after donating blood? What is the probability that a donor was infected before donating blood? ff a donor was infected long enough ago, the serological, test will
be positive and the donation will not enter the blood supply. Hypothetically, if all donors infected more than 2 months ago now test positive, then the relevant question is What is the probability that a person donating blood today was infected within the past 2 months? Only such an infected donor might test negative thereby resulting in transfusion of the unit. In our example in which the risk of being infected within the past year is 1 in 25,000, the risk of being infected within 2 months (one sixth of that time) is one sixth of that risk, or 1 in 150,000.
Likewise, when the risks are small, we can estimate the risk of being infected within any specified time period to be directly proportional to the risk calculated on a per-year basis. However, one additional adjustment must be made before multiplying the observed incidence by the window period. The risk to the transfusion recipient will be overestimated if the observed incidence is not first adjusted to eliminate those seroconverting donors whose potentially infectious seronegative unit was removed from distribution before transfusion (be- cause of an abnormal result based on another laboratory screening assay or by a positive re- sponse to confidential unit exclusion). This ad- justed incidence is then multiplied by the window period expressed as a fraction of a year (Table 2). This product is the probability that a seroconverting donor gave an infectious unit of blood that was transfusable: In other words, this is the per-unit risk for infection.
To gauge the magnitude of transfusion transmis- sion of a given viral agent, the per-unit risk can be multiplied by an estimate of the number of blood donations or components collected in a time period (eg, annually). For example, if the risk for HIV transmission is 1 in 493,000 and if there are 18 million components collected each year in the United States, then there would be approximately 37 infectious window period components entering the blood supply each year) With this model, the number of window period donations (ie, the num- ber of donations from infected donors who are not yet testing positive) depends directly and equally on the incidence and the window period. For example, if the window period is halved, the number of window period donations is halved. Likewise, for any fixed window period, if the incidence is reduced by "X%," the number of window period donations also is reduced b y "X%."
160 KLEINMAN ET AL
Risk Reduction by Introduction of New Tests
In the past, prevalence calculations derived from the number of detected seropositive donated units have been misused to evaluate measures to reduce transfusion transmitted risk. More appropriately, incidences can be combined with performance information on new assays to assess the yield of a proposed new test. Theoretically, risk reduction information could be obtained without knowledge of the actual length of the window period. For example, if all that were known was that a new test could detect HIV infection 6 days earlier than existing tests, we could make the following calcula- tion: If the HIV incidence is 4.01 per 100,000 person-years, and if there are 18 million compo- nents collected per year, then the yield of the new test would be [(4.0/102 p-y) • (year/365 days) • (6 days) • (18,000,000 components/year) = 12 com- ponents/year implying that 12 more infectious components might be detected by the new test annually.
The preceeding example refers to the best avail- able information concerning the ability of the HIV p24 antigen test to shorten the window relative to detection by the most sensitive third generation anti-HIV assay. 12 The same approach could be applied for other agents or tests using the appropri- ate estimates for the incidences and the shortening of the Window period. Furthermore, by comparing tlle cost of implementing a proposed new test with the projected yield from shortening the window period, cost-benefit information can be obtained.
Critical Data Elements to Complete the Model
At the time of a blood donation, a donor may be asked if he or she has previously donated and, if so, to provide the date of their last donation. This information could be used to derive an incidence but only if it is assumed that the prior donation was seronegative and that the donor accurately recol- lects the date of prior donation. If one or both of these assumptions are not true, the incidence esti- mate could be severely biased. Therefore, a system that documents and links an individual's multiple donation dates and test results is required for reliable incidence estimates. Given the low rates of seroconversion (SC) for known agents, a large donor and donation database is necessary to estab- lish reasonable confidence intervals around the point estimate for incidence.
Accurate information about the window period
is the second critical element of the model because the risk is obtained by multiplying the number of window period days (expressed as a fraction of a year) by the adjusted incidence. Wide confidence limits around the window period estimate will result in wide confidence limits for the per-unit risk estimate.
In performing risk reduction estimates with regard to the yield of a new version of an existing assay or the addition of a second test for a known agent, the critical data element is the reduction in the number of window period days relative to the previous testing algorithm. If this is known, the calculation can be reliably performed, although the length of the absolute window period for the new test has not been prospectively determined.
Assumptions of the Model
There are several important assumptions assocf- ated with the incidence/window period model. It will provide a reliable estimate of recipient risk only if the other theoretical causes for risk are absent or of considerably less importance. The model will accurately predict risk, provided that there is not an immuno-silent carrier state for the agent, that there are not missed infections caused by genetic diversity, and that laboratory errors occur at an insignificant rate. These potential sources of risk must be evaluated for each viral agent of concern; to the extent that any of these other sources of risk are substantial, they must be added to the incidence/window period model risk estimate to accurately predict overall transfusion risk.
The incidence calculation assumes that the inci- dence among donors is constant throughout the time period of study. This assumption is more likely to hold for relatively short and recent time intervals (eg, 1.991 to 1993) than for extended intervals that include periods of dynamic change in the donor population with respect to risk behavior or viral penetrance (eg, 1985 to 1993 for HIV infection). In the latter case, statistical techniques (eg, stratification, multivariable models, and soon) should be applied to incidence calculations to account for suspected changes in the incidence over time. Likewise, these statistical techniques can be applied to examine and adjust for differences in incidences that may 'exist by gender, age, race/ ethnicity, geographic region, and so on, assuming such demographic data are available. Another poten-
INCIDENCE/WINDOW PERIOD MODEL FOR TX RISK 161
tially relevant factor is a donor's frequency of donation and their interdonation intervals, which could be evaluated in the same manner as other donor covariates.
A problematic aspect of the model relates to the assumption that a recently infected donor is as likely to donate in the early interval after infection as he or she is subsequently. Consider the example of the donor whose HIV seropositive donation was made 180 days after his seronegative donation. Using a window period for HIV infection of 22 days, his infection may have occurred from day - 2 1 to day 159 ( 1 8 0 - 21). However, several factors may exist to bias when such a donor was likely to have made his donation. If, for example, the donor recently engaged in a high risk activity and is donating blood specifically to learn his HIV status, he may be more likely to present for donation very soon after the exposure; hence, he might be more likely than our model predicts to have been infected in the 21 days before his donation. On the other hand, if recent infection results in an illness that precludes donation, he may be less likely to donate during this infectious seronegative window. Thus, depending on the circumstances and timing of the donor's situation, the calculated incidence based on an assumed steady state rate of donations could produce either an overestimate or underestimate of the true inci- dence.
Incidence is a measure of the rate of change per unit of time. Consequently, people must be evalu- ated on at least two occasions to document the length of time under observation (the denominator) and whether or not seroconversion occurred (the numerator). For single time donors (ie, donors listed as first time in the blood donation database or repeat donors if they do not return t0' donate a second time during the observed study period), the information needed for calculating incidences does not exist in the database. Nevertheless, an inci- dence rate must exist for first time donors, although by definition it is not observable. Because it has been well documented that the prevalence of infec- tious disease markers is significantly higher among first time donors than for repeat donors, it has been generally assumed that the same is true for inci- dence. However, data for examining this issue are sparse. One older study, using data based on the relative prevalence of anti-HIV seropositivity among first-time and repeat donors at the time of HIV
antibody test implementation in 1985, has sug- gested that the HIV incidence among first-time donors is 1.8 times greater than that for repeat donors; however, there are no recent data to support this figure nor are there comparable data for agents other than HIV. 13 It has been well established that the percentage of the total donation pool contrib- uted by donations from first time donors is approxi- mately 20%. 14 Therefore, even if we assume that the relative incidence between first-time and repeat donors is 1.8, the overall incidence requires only slight adjustment (eg, the rate in repeat donors would be multiplied by 1.16 to estimate the inci- dence for all donors). More generally, the observed incidence in repeat donors should be multiplied by (0.8 + 0.2k), where k is the relative incidence among first-time donors compared with repeat donors. Approaches using laboratory tests for H1V that distinguish recent from older infections are currently being developed to permit an incidence to be calculated in first time donors; once refined, such testing may provide additional insight as to how to address this issue for other agents as well.
TRANSFUSION TRANSMITTED HIV INFECTION
HIV Risk From Screened Donations
From 1986 to 1992, two prospective studies were conducted with the aim of defining the risk of transfusion-transmitted H1V infection. The first study, performed in the Baltimore and Houston areas, involved testing patients for anti-HIV-1 before and after cardiac surgery. 3 Observed serocon- versions in recipients were investigated to rule out other risk factors, and donors in those cases were traced to further document the source of recipient infection. Two cases of HIV-1 infection were documented after transfusion of 120,000 units of blood; seroconverting donors were identified in both cases. The risk from this study was estimated as 1 in 60,000 (upper 95% confidence interval (CI): 1 in 19,000) In the other study, performed from 1987 tO 1993 in the San Francisco Bay Area, viral culture and PCR analyses were used to detect HIV-1 in pooled, peripheral blood mononuclear cells derived from 200,000 anti-HIV-negative do- nations. Only a single infected seronegative dona- tion was identified in 1987. After adjusting for assay sensitivity and the pooled analyses, a risk estimate of 1 in 160,000 units was calculated (upper 95% CI: 1 in 128,000). ~5,16 Other estimates of HIV risk were also published in the 1980s; these
162 KLEINMAN ET AL
studies used various assumptions and calculations to generate risk estimates ranging from 1 in 40,000 units to 1 in 153,000 units. 13,17,18 It should be noted that all of these studies were conducted before the introduction of more sensitive recombinant antigen based third generation anti-HIV tests that are capable of detecting early IgM and IgG responses to HIV infection.
As early as 1988, case reports of transfusion- transmitted acquired immunodeficiency syndrome (AIDS) from HIV seronegative blood were being investigated by CDC. 17 Through June 1992, CDC had received 201 AIDS case reports in which the only acknowledged mode of HIV exposure was one or more transfusions received from 1986 through 1991.19 However, when CDC reinvestigated 106 of these cases, 55 (52%) were reclassified as not transfusion associated, either because no transfu- sion was given, or because another more probable mode of HIV exposure existed. An additional 34 cases (32%) involved persons who had received earlier transfusions of unscreened blood or who were transfused in foreign countries. Thus, only 14 of the 106 investigated cases (13%) initially re- ported to be caused by infections from screened blood transfusions were confirmed. In many of these cases, an infected donor was identified who had given blood shortly after a high-risk exposure, ie, in the preseroconversion infectious window period. After adjustment for noninvestigated cases, the CDC investigators estimated that from 1986 through 1991 approximately five AIDS cases per year were caused by infections from anti-HIV- screened blood transfusions. The most recent unpub- lished data indicate that there have now been a cumulative total of 38 documented cases of AIDS resulting from anti-HIV-screened blood transfu- sions since 1985 (Dr M. Chamberland, CDC, personal communication).
Potential Reasons for Continued Transmission of HIV by Transfusion
The possible existence of asymptomatic, long- term HIV infection in which the infected person never develops or loses HIV antibody is of great potential significance to transfusion safety. A few reports in the late 1980s claimed that immuno- silent carriers were not uncommon; however, the most prominent initial study that identified this phenomenon using viral culture techniques was unable to reproduce its results on subsequent
fol low-up. 20,21 Furthermore, numerous subsequently reported studies of persons at high risk for acquir- ing HIV infection failed to detect HIV nucleic acid (PCR) positive, antibody negative individuals. 22,z3 In the late 1980s, a single study also reported four cases in which the testing of serial frozen reposi- tory samples appeared to indicate the loss of HIV antibody (sero-reversion) in healthy high-risk indi- viduals. 24 However, these findings could not be replicated using the much larger database of HIV antibody test results in United States Army-person- nel and these investigators indicated that apparent seroreversion was likely due to sample mislabeling or clerical error. 25 These accumulated data were sufficiently convincing for the Food and Drug Administration (FDA) in 1992 to shorten the required deferral period for some individuals with HIV risk factors. It was reasoned that such persons, if infected, would show positive HIV antibody results within 12 months of their last exposure. 26 More recently, isolated case reports have docu- mented the rare existence of HIV infection without antibody production in asymptomatic and symptom- atic immunocompetent persons? 7,28 All such cases reported to date have progressed rapidly to disease, precluding long-term blood donation by these indi- viduals. Furthermore, the rarity of such cases despite intense surveillance efforts to identify them over the last decade indicates that this is not a significant source of transfusion-transmitted HIV infection.
The importance of HIV .genetic variation for transfusion safety relates to whether screening assays can detect antibody to the array of subtypes that may be present in the ethnically and geographi- cally diverse population that donates blood. HIV could be transmitted if a donor were infected with an atypical genetic variant that was undetectable by current HIV antibody screening assays. HIV can be classified into broad groups based on nucleic acid sequence analysis of envelope (env) and core (gag) genes; HIV-1 and HIV-2 are at the extremes of this diversity. The HIV-1 family is phylogenetically subclassified into main (M) and outlier (O) groups. Group M is further divided into at least 8 distinct subtypes, or clades, designated A through H. The outlier HIV- 1 group (Group O) is also composed of a set of divergent clades. 29,3~ Group M clades are widely distributed geographically and show evolv- ing distributions in different parts of the world after seeding of the epidemic in different geographic
INCIDENCE/WINDOW PERIOD MODEL FOR TX RISK 163
regions by distinct "founder" viruses. Recombi- nant viral strains, with genetic regions derived from multiple clades have also recently been observed. 31
At present, HIV-1 clade B is by far the predomi- nant subtype in the United States; consequently, the initially developed antibody assays used HIV-1 Clade B viral lysate as antigen. Subsequent genera- tions of assays used recombinant antigens corre- sponding to immunodominant regions of gag and env also derived from HIV-1 clade B prototypes. Fortunately, these assays have been shown to be highly sensitive to infection caused by HIV-1 clades A through H. However, the assays fail to detect occasional samples from more diverse vari- ants, such as HIV-2 and HIV-1 group 0 . 32,33
HIV-2 was discovered in 1985 in West Africa and subsequently was found in western Europe, where a number of infected blood donors have been detected and cases of transfusion transmission have been documented. HIV-1 and HIV-2 are approxi- mately 50% homologous at the nucleic acid se- quence level, and they cross-react immunologically to a great extent (particularly the gag and polymer- ase antigens). For this reason, up to 90% of sera from HIV-2-infected persons test positive on FDA- licensed HIV- 1-based assays, with variable reactiv- ity on HIV-1 Western blots. 32 However, because the sensitivity of these assays to HIV-2 is less than 100%, a combined assay using both HIV-1 and HIV-2 antigens was introduced into routine blood donor screening in the United States in 1992. With the introduction of this assay, HIV-2 risk from transfusion transmission has been confined to win- dow period cases, this risk is so small as to not be measurable. In 4 years of HIV-2 testing, only one
HIV-2 infected blood donor has been reported. 34 This is not surprising, because the total number of HIV-2 infections in the United States is quite low.
In mid-1994, French investigators first reported that some persons infected with HIV-:I group O, then a recently described variant endemic in the central African countries of Cameroon and Gabon (with rare immigrant cases in Europe), tested negative on a number of HIV-1 antibody and HIV-1/HIV-2 antibody combination assays. Assays using synthetic peptides or recombinant antigens on the solid phase, and those using the so-called third-generation "antigen-sandwich" format, were particularly prone to false negative results. These results prompted test manufacturers in Europe to enhance their assays' sensitivity to unusual HIV
variants like group O; however, these modified assays have not yet been approved for use in the United States. In July 1996, the first case of non-transfusion-associated group O infection in North America was published. 35 Nevertheless, be- cause of the rarity of group O infection and the ability of current antibody assays to cross-react with some group-O-infected donors, the contribu- tion of such genetically divergent infections to transfusion-transmitted HIV risk will be negligible.
Finally, given the low prevalence of HIV, the contribution of test error is expected to be trivial. Consequently, window period transmission is by far the predominant source of transfusion-transmit- ted HIV in developed countries.
Defining the HIV Window Period
The first approach used to generate an estimate for the infectious window period preceding HIV seroconversion was based on exploiting the math- ematical relationship between the window period, the interdonation interval (ie, the interval between seronegative and seropositive donations in an HIV seroconverting donor), and whether the seronega- tive unit transmitted HIV infection to a recipient. Because HIV transmission or its lack could be determined by testing recipients of potentially infectious units from donors who later serocon- verted, and because the interdonation interval for each donor was known, the duration of the window period could be estimated. To accomplish this, a large scale multicenter study was conducted to trace previous recipients of components from 701 blood donors who had seroConverted to anti-HIV positivity before 1991. 36 These investigations yielded 182 seroconverting donors for whom the sero-status of one or more recipients was deter- mined. Of the 182 recipients of donations from seroconverting donors, 39 (20%) were infected with HIV. The recipient infection rate (and hence the HIV infectivity status of the donor) correlated inversely with the time interval between the sero- positive and seronegative donations (eg, interval <90 days, 76%; 91 to 180 days, 28%; >180 days, 11%). Not surprisingly, the donors wi th longer interdonation intervals had a greater likelihood of acquiring their HIV infection some time after their donation of a seronegative unit. Mathematical modeling using maximum likelihood techniques yielded an estimated median 45-day infectious window period, with an upper 95% confidence
164 KLEINMAN ET AL
limit of 141 days. Separate analysis of data from donations given before and after April 1987, when second generation anti-HIV EIAs were introduced, showed that this change resulted in a reduction of the estimated median infectious window period from 56 days (pre-1987) to 42 days (post-1987).
Several cautions regarding interpretation of this lookback-derived window period estimate should be raised. The viremic preseroconversion window period determined by the lookback methodology should not be equated with the time period from exposure to seroconversion. Data from animal models indicate that there is a period of days to weeks after exposure, during which the virus is replicating in regional lymphoid tissue before dis- seminating into peripheral blood. 9 Therefore, the "exposure4o-seroconversion" window period is necessarily longer than the "infectious" window period. Second, these data relate to infections transmitted by intravascular infusions of several hundred milliliters of blood from a donor who was in the dynamic preseroconversion window phase of infection. Extrapolation of these data to other exposure routes and inoculation volumes (eg, needlestick exposure, injection drug use, or sexual exposure) should, therefore, be made with cau- tion. l0
With the introduction of more sensitive third generation HIV antibody assays in 1992, it was apparent that the window period for HIV detection would be shortened. However, because of the relatively low number of expected annual HIV seroconversions, it was recognized that it would not be possible to repeat a similar lookback study to calculate this new window period. Therefore, an alternative approach was developed based on deter- mining the degree of shortening of the window period by third generation assays, relative to previ- ously used versions of the antibody test. This involved the testing of samples obtained from HIV high-risk cohort studies. Such studies, involving hundreds or even thousands of high-risk individu- als, collect and store cryopreserved specimen at regular intervals (usually 3 to 6 month s) from each subject at each visit. The methodology used in these window period studies was to obtain presero- conversion and seroconversion samples from such repositories. These samples were tested with im- proved sensitivity antibody assays as well as with direct viral assays, thereby determining the capac- ity of such assays to detect infection earlier than
pre-existing antibody tests. The first such study used multiple HIV assays, including third-genera- tion anti-HIV tests, p24 antigen, and DNA and RNA PCR, to test serial samples from 81 serocon- vertors who had been enrolled in three separate cohort studies. 37 Based on a model in which the assay results were analyzed relative to the inter- bleed interval for these 81 seroconverters, a 19.7- day reduction (95% CI of 7.7 days to 31.6 days) in the HIV-1 preseroconversion window period by third-generation HIV antibody assays was~ estab- lished. This 20-day improvement when subtracted from the previously determined 42-day window results in the current estimate of a 22-day window. These findings have recently been confirmed by a similar analysis conducted using 394 seroconvert- ing subjects from six cohort studies; this study showed a window period reduction of 21.6 days and a narrowing of the 95% CI caused by the larger sample size (95% CI of 16.5 days to 28.3 days). 38
REDS Data on HIV Incidence and Risk
During a 3-year period of the REDS protocol, 586,507 people who donated blood more than once made a total of 2,318,356 allogeneic donations. The crude incidence rate for HIV infection was 4.01 per 100,000 person-years, determined by dividing the 33 persons who seroconverted to HIV by the 822,494 person-years of observation. Al-
though 33 donors seroconverted, the most recent seronegative donation was not transfusable in six cases, either because it tested positive for another marker (elevated alanine amino transference (ALT) level in one case, positive hepatitis B core antibody (anti-HBc) in two cases, positive Hepatitis B surface Antigen in one case or because of confiden- tial unit exclusion in two cases). This resulted in a 16% decrease in the adjusted incidence rate from 4.01 to 3.37 per 100,000 person-years (95% CI of 2.22 to 4.76); this is an estimate of the probability that a donor who gave a transfusable donation was infected in a subsequent 1-year period. To deter- mine the risk that the donor was already infected and in the infectious, seronegative window, the adjusted incidence rate was multiplied by 0.061 (the 22-day window period [range 6 to 38 days] expressed as a fraction of a year) yielding a residual risk 'of 2.03 per million donations (range 0.36 to 4.95 per million). The point estimate for the risk of a transfusable HIV seronegative unit transmitting HIV infection is 1 in 493,000. 5
INCIDENCE/WINDOW PERIOD MODEL FOR TX RISK 165
Recently, investigators from the CDC and the American Red Cross used similar methodology to arrive at a comparable risk for HIV transmission of 1 in 450,000 to 1 in 660,000 units. 6 The concor- dance of these two recent risk estimates, each obtained at a limited number of blood centers using data obtained in the early 1990s, suggests that they are likely to be generalizable on a national level. Data from both of these studies were obtained before the introduction of the HIV p24 antigen test in routine blood donor screening; they should be adjusted downward by a factor of 27% (6 days/22 days) to account for the estimated additional frac- tional reduction of the window period by p24 antigen testing. 12 Using the REDS point estimate, this yields a per-unit risk of 1 in 677,000.
When compared with earlier estimates from the late 1980s, the estimated risk for HIV transmission has decreased by fivefold to tenfold. This decrease is primarily caused by the improved sensitivity of anti-HIV screening assays to detect HIV infection earlier in the window period, thereby reducing the number of HIV infectious units transfused. A second factor that may have also contributed to this decrease is a lowered HIV incidence in blood donors because of more effective deferral of indi- viduals at risk for HIV infection; however, the significance of this factor is uncertain. Although it is clear that the seroprevalence of HIV infection has markedly decreased in donors over the last decade, 39 similar data on incident HIV infection have been more difficult to obtain. A report from Los Angeles showed that the incidence of HIV infection in blood donors during 1987 to 1989 decreased from that detected in the first 2 years of HIV antibody screening, 4~ suggesting that a de- crease in the number of donations made in the HIV window period played a role in enhancing blood safety before the development of more sensitive HIV antibody assays.
Evaluation of Surrogate Procedures for Decreasing HIV Risk
Anti-HBc testing was implemented nationally in the United States in the mid 1980s as a surrogate test for non-A, non-B hepatitis, and not as a surrogate test for HIV infection. Nevertheless it was observed that 30% to 40% of HIV seropositive donors tested positive for anti-HBc, suggesting that the test might have value in decreasing the risk of transfusion-transmitted HIV infection. 41 However,
a valid evaluation of the effectiveness of anti-HBc testing for this purpose requires a determination of whether units donated during the seronegative window period would be interdicted from transfu- sion because of positive surrogate test results. Therefore, by defining the population of HIV seroconverting donors, it becomes possible to evalu- ate the utility of anti-HBc testing with respect to HIV window period donations. Similarly, the effi- cacy of CUE can be evaluated using the same methodology. REDS data, as presented above, indicate that each of these two approaches had only a 6.1% yield (2 of 33 HIV seroconverting donors by each approach). Similar data fo r the perfor- mance of anti-HBc testing was obtained by a joint CDC and American Red Cross investigation during the 1987 through 1990 timeframe when anti-HBc- positive donors were not discouraged from return- ing to donate; they found that 17.7% of HIV seroconverters had anti-HBc-positive results on their HIV seronegative donation. 42 If we perform transfusion risk calculations applying REDS data to the incidence/window period model and assume that the CUE procedure had not been in place (ie, leading to the transfusion of two additional units from HIV seroconverting donors) we calculate an HIV risk of 2.17 per million donations (rather than 2.03 per million); this 0.14 per million increase translates to transfusing one additional HIV infec- tious unit per 7.14 million blood donations. For discontinuation of anti-HBc testing, REDS data indicate an increased risk of 6.1% whereas CDC data indicate increased risk of 17.7%; therefore, the estimate for increased HIV risk associated with discontinuation of anti-HBc testing ranges from one additional HIV infectious unit transfused per 2.78 million to 7.14 million donations. The yield of either CUE or anti-HBc testing in preventing HIV infection, therefore, can be seen to be exceedingly low; similarly, additional analyses of related data show extremely low projected yields for both positive predictive value and cost effectiveness of either of these procedures. 43,44
The Potential Impact of HIV p24 Antigen Testing and HIV RNA Testing
The incidence/window period model can also be employed to project the yield of direct virus detection assays (p24 antigen and HIV RNA ampli- fication assays), which are able to detect infected donors earlier than routine anti-HIV screening. 5
166 KLEINMAN ET AL
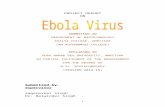
Projections of yield can then be combined with reactive rates for each test to project their positive predictive values, or with testing cost and disease outcome data to project their cost-effectiveness. 45 As discussed above, studies of seroconverting plasma donor panels have yielded estimates for the duration of p24 antigen and RNA positivity preced- ing antibody seroconversion (Fig 1). The most recent study, based on 51 such panels, indicates that p24 antigen is detected 5.0 days (95% CI: 3.4 to 7.3 days) before antibody detection by IgM-sensitive, antigen sandwich format HIV-1/2 EIAs, whereas RNA is detected approximately 8.1 days (95% CI: 5.1 to 12.8 days) before IgM seroconversion. 46 Similar estimates are available from analyses of preseroconversion samples from individuals en- rolled in high-risk cohort studies: p24 antigen pre-IgM EIA window period, 9.2 days (95% CI: 6.1 to 13.9 days); RNA pre-IgM EIA window period, 11.8 days (95% CI: 8.0 to 17.3 days). 38,46 p24 antigen and RNA-positive preseroconversion win- dow period estimates would be about 10 days longer than the above projections relative to anti- HIV-1 or anti-HIV-1/2 EIAs not optimized for IgM detection.
By multiplying the REDS-derived HIV inci- dence rate by the fraction of a year that direct virus detection assays detect a seroconvertor in the viremic, preseroconversion window period, the
yield of the assays can be projected. The projection for the p24 antigen yield of about six infected donors per year among the 12 million voluntary donations in the United States is consistent with the results of the large United States studies from the late 1980s that failed to detect p24 antigen-positive, anti-HIV-negative donors, as well as with extrapo- lations from high HIV incidence settings (Thailand, India, and emergency room) in which the p24 antigen has been implemented in pilot research protocols. 12 Based on these low yield projections and correspondingly poor projections for the posi- tive predictive value and cost-effectiveness of p24 antigen screening of United States donorsY the FDA Blood Products Advisory Committee recom- mended against implementation of p24 antigen screening in mid-1995. However, the FDA subse- quently recommended implementation of the test, after congressional criticism that the yield projec- tions were theoretical and likely underestimates, and that cost-effectiveness analyses were inappro- priately considered given the FDA's charter to focus only on safety and efficacy. As a result, p24 antigen EIAs were licensed by the FDA for donor screening in the spring of 1996 and implemented immediately.
Implementation of p24 antigen screening has presented the unusual opportunity to empirically validate a projection of the incidence/window pe-
2 2 d a y s 4
Infectious
1
10
1 1 d a y s (
d /
/ /
/ /
/ /
/ ." , ". \ ,
20 30 40- 50 60
Days post-infectiousness (calculated)
Fig 1. 13me course of appear- ance and dynamics of HIV RNA (solid line), p24 antigen (dotted line), and antibody detectable by IgM-sensitive, third-generation EIAs (dashed line). Day 0 repre- sents time point at which a re- cently infected person is esti- mated to be infectious (viremicl as a blood donor.36 Horizontal arrows represent (l i duration of overall viremic window period preceding antibody (< - - - ) , (2) duration of RNA detectability be- fore antibody (~) , and (3) dura- tion of p24 antigen-positive/anti- HIV-negative window period (<. �9 .). Data from Petersen et a136 and Busch et al. z7
INCIDENCE/WINDOW PERIOD MODEL FOR TX RISK 167
riod model. During the first 6 months of screening, over 3 million volunteer donations were tested by the American Red Cross, with only one p24 antigen-positive-antibody-negative-infected do- nor identified. 47 Thus, the model may have overes- timated, rather than underestimated, yield. In retro- spect, the steady state assumption of the model, ie, that seroconverting donors will attempt donations at a consistent rate during the preseroconversion period, may not apply to the antigenemic phase of primary HIV infection. This phase of HIV infection is frequently characterized by clinical or subclini- cal illness ,(the acute HIV syndrome), 48 and, there- fore, antigenic donors may self-defer or may be deferred at an attempted donation because of fevers or histories of recent night sweats. From a policy development perspective, it is important that the projection was conservative and, therefore, served the decision-making process well. Given that HIV RNA is only detectable several days earlier than p24 antigen, it is not surprising that projections for the yield of HIV RNA screening are similarly low (`10 to 12 infected seronegative donors per year). However, the focus of nucleic acid screening assay development is a multiplex screening system target- ing HIV, HCV, HBV, and perhaps other agents. Consequently, both government and industry re- sources are now focused toward a goal of nucleic acid screening of donors by the year 2,000.
TRANSFUSION-TRANSMITTED HCV INFECTION
Previous Studies to Define HCV Risk
The risk of non-A, non-B hepatitis transmission has decreased dramatically over the past 20 years. In the late 1970s, two independent prospective recipient follow-up studies documented this risk to be 7% to 10% per recipient in multitransfused patients. 1,4 Anti-HCV testing of linked donor- recipient sample sets in these studies retrospec- tively established that approximately 90% of cases
49 50 were because of HCV infection. . The changes in blood donor screening that were introduced to prevent transfusion transmitted AIDS in 1983 as well as the implementation of surrogate testing (ALT and anti-HBc) for non-A, non-B hepatitis in 1987 were estimated to have reduced non-A, non-B transfusion risk by approximately 50% from pre- 1983 levels to a per-unit risk of 0.2% to 1% in 1989.
The impact of implementing surrogate testing
and the first generation of anti-HCV EIA testing (EIA-1) was shown in a prospective recipient follow-up study of cardiac surgery patients that spanned the years of 1985 to 1991. 51 In this study, a comparison was made between the risk of HCV transmission from three types of transfused prod- uqts: blood that was not screened for non-A, non-B hepatitis, blood that was tested by ALT and anti- HBc, and blood that was tested using these two surrogate tests plus anti-HCV EIA-1. In the initial publication of this study, it was reported that the per-unit risk decreased from 0.45% per unit presur- rogate testing to 0.19% with surrogate testing and to 0.03% after anti-HCV EIA-1 testing. Subse- quently, when recipient samples were reevaluated using a more sensitive anti-HCV EIA-2 test, it was found that the per-unit risk from EIA-l-screened donor blood was twice as high as previously reported with a per-unit risk of 0.06% (1 in 1,672 units). 52 This and other studies confirmed that anti-HCV EIA-1 testing lowered the risk of HCV transmission by 80% from its presurrogate testing levels. 53
The predicted transfusion safety impact of the implementation of the improved multi-antigen sec- ond generation anti-HCV EIA (EIA-2) was shown in a prelicensure study of this test in 1991. 49 This study detected 1.2 additional HCV-infected donors (not detected by EIA-1) per 1,000 donors tested; these initial observations were later confirmed by several other investigators who reported a similar additional yield when EIA-2 testing was performed on inventory units previously screened negative by EIA-1 testing. 54 The additional yield was due primarily to the ability of the EIA-2 test to detect chronic HCV infections missed by EIA-1.
Potential Reasons for Continued Transmission of HCV by Transfusion
HCV has now been classified into six distinct genotypes and the virus has shown an ability to exist in multiple quasi-species within a given infected host. 55 Nevertheless, the recombinant HCV antigens used in the multi-antigen EIA-2 and the newer EIA Version 3.0 tests appear to detect patient antibody regardless of the infecting genotype. Currently, HCV genetic variants do not seem to pose a risk for transfusion transmission.
The contribution of testing error to HCV infec- tion must be given some consideration. Because there is a substantial prevalence of anti~HCV
168 KLEINMAN ET AL
confirmed positive donated units (0.1% to 0.2%), this prevalence would need to be multiplied by the estimated rate of laboratory testing error to quantify this phenomenon. Initial attempts at this quantifica- tion indicate that testing error may account for some HCV transmission but that it makes only a small contribution to overall r i sk . 56
On the other hand, there are data to strongly support the view that some chronic HCV carriers may not be detectable by current screening assays but nevertheless may be capable of transmitting HCV. In 1992, CDC investigators reported that 10% of patients with community-acquired symp- tomatic HCV infection were negative by anti-HCV EIA-2 tests but positive by plasma RNA PCR or by immunofluorescence antibody assay using infected hepatocytes as antigen. 57 This pattern persisted on follow-up sampling. Other investigators have re- ported similar individuals .58 However, no study has either corroborated or refuted the CDC's reported rate of immunosilent HCV infection, making it difficult to establish the relative importance of the chronically infected, antibody-negative donor to transfusion safety. This phenomenon may also have been observed in the older TTVS and NIH prospec- tive recipient follow-up studies, In 8% to 12% of cases in which recipients seroconverted to HCV after transfusion and in which samples from all donors were available, testing of these frozen donor sera by second generation anti-HCV assays failed to detect any HCV-infected donors. 49,5~ However, there are several possible explanations for this observation; these include donors who were chronic undetectable carriers, donors who were in the HCV window period, or the occurrence of recipient infection from a source other than blood transfu- sion.
Previous data documenting the risk of HCV infection after EIA-1 screening (1 in 1,650 units) was combined with an estimate of the percentage of residual HCV infections detected by EIA-2 testing, but not by EIA-1 test!ng, in the TTVS study (64%) to derive a per-unit risk from EIA-2-screened blood donations of approximately 1 in 5,000 (range i in 2,000 to 1 in 6,000).49.59 Since the' implementa- tion of EIA-2 testing in 1992, this estimated risk has been widely quoted.
Defining the HCV Window Period
The HCV window period has been defined using panels of sera collected at intervals of 2 to 4 weeks as part of prospective post-transfusion hepatitis
recipient follow-up studies. In contrast to the HIV window period, the HCV window period has been calculated from the time of HCV exposure to the time of antibody detectability; therefore, this win- dow period theoretically may overestimate the period of infectivity. Data from 21 post-transfusion cases in Spain indicate a mean window period to detectable antibody by anti-HCV EIA-2 of 82 days (range of 26 to 118 days), whereas data from a smaller series of nine cases from the Netherlands indicate a mean of 95 days and a similarly wide range (54 to 192 days). 6~ Unpublished data from an additional 25 cases are in agreement with the published series. 63
Another relevant window period that has been calculated from these same sample sets is the window period to HCV seroconversion using the EIA Version 3.0 assay. As compared with EIA-2 testing, approximately 25% of patients had thei~ HCV infection detected a mean of 26 days earlier using EIA Version 3.0, whereas the remaining patients were detected simultaneously by both assays. Projected to the entire sample set, the mean window period using EIA Version 3.0 was 70 days, a 12-day reduction from the EIA 2.0 window. 6~
REDS Data on HCV Incidence and Risk
REDS HCV incidence data were calculated for a 21-month period in which anti-HCV EIA-2 screen- ing was performed (April 1992 through December 1993). 5 The crude incidence rate for HCV infection was 4.84 per 100,000 person-years, determined by dividing the 16 persons who seroconverted to HCV by the 330,924 person-years of observation. Al- though 16 donors seroconverted, the most recent seronegative donation was not transfusable in 2 cases because of low level ALT elevations. This resulted in an 11% decrease in the adjusted inci- dence rate from 4.84 to 4.32 per 100,000 person- years (95% CI of 2.35 to 6.87). To determine the risk that the donor was already in the infectious seronegative window, the adjusted incidence rate was multiplied by .225 (the 82-day window period [range 54 to 192 days] expressed as a fracdon of a year) yielding a residual risk estimate Of 9.70 per million donations (range 3.47 to 36.11 per million). Thus, the point estimate for the risk of an infectious window period HCV seronegative unit transmitting HCV infection with ALT testing in place is 1 in 103,000. A similar risk estimate can also be calcu- lated for the EIA Version 3.0 test using a window period of 70 days; this yields a per-unit risk
INCIDENCE/WINDOW PERIOD MODEL FOR TX RISK 169
estimate that is diminished by 15%, to 1 in 121,000 per unit.
The REDS HCV risk estimate is substantially lower than the previously reported 1 in 5,000 per-unit risk, which was based on the hypothesis of the existence of significant numbers of chronic, antibody-negative HCV carriers. Given the rarity of HCV transmission reported since the initiation of EIA-2 testing, as evidenced by 0 cases in over 650 recipients in a contemporary, prospective NIH study, 64 (Dr Harvey Alter, personal communica- tion) we postulate that the fi'equency of immunosi- lent infections is less than the originally reported 10%; however, it is not possible currently to quantify it more precisely. Therefore, we are left with a very wide range of possible HCV risk, ranging from 1 in 5,000 to 1 in 103,000 per unit.
Evaluation of Surrogate Procedures (ALT Testing) for Decreasing HCV Risk
The value of surrogate tests (ALT and anti-HBc) in decreasing the risk of post-transfusion non-A, non-B hepatitis by at least 30% before the availabil- ity of anti-HCV testing has been well validated in two prospective recipient follow-up studies. 51,65 Its retrospective value was further substantiated with data obtained after implementation of HCV donor screening, which showed that approximately 55% of first-time donors who are anti-HCV positive are also positive by one or both of these assays. 49 In contrast, several lines of evidence suggest that these surrogate assays have very little use in the era of anti-HCV screening. A reanalysis of samples from the TTVS indicated that surrogate marker testing would not have prevented any cases of HCV that were not also prevented by anti-HCV screen- ing. 5~ Two prospective studies in countries in which surrogate testing had not been implemented also showed lack of efficacy of either surrogate test.65,67
REDS incidence and risk estimates have been used to more precisely quantitate the contribution of ALT testing (in the era of anti-HCV EIA-2 screening) in prevention of window period HCV transmission. 61 REDS evaluated the two-level ALT screening algorithm employed by blood banks: discard the unit if the ALT is above the lower cutoff level and discard the unit and deferral of the donor if the ALT is above the higher cutoff level (in which the value is routinely set at twice the lower cutoff level). REDS data were used to directly calculate the impact of eliminating the low level, but retain-
ing the high level, ALT cutoff. The risk of window period HCV transmission in this scenario was calculated to change from 9.7 units per million to 11.0 units per million, an increase of 1.3 HCV infectious units per million donations. In contrast, the contribution to HCV risk of donors with high level ALT elevations could not be calculated di- rectly because all such donors were deferred after their initial ALT elevated donation and, therefore, could not be evaluated for seroconversion. An adjustment factor for these donors was calculated based on the observation that, in first-time donors, the prevalence of anti-HCV in donors with high- level ALT elevations was 3.4 times more frequent than the anti-HCV prevalence in donors with low level ALT elevations. Applying this adjustment, it was projected that totally discontinuing ALT test- ing would increase HCV risk to 12.5 units per million, a 2.8 per million unit increase. An NIH Consensus Conference panel considered these data in conjunction with data concerning the large number of discarded units and deferred donors caused by the poor specificity of ALT testing and concluded that ALT testing of donated blood should be discontinued. 68
The Potential Impact of HCV RNA Testing to Shorten the Window
Plasma HCV RNA PCR testing will reliably detect HCV infection early in the antibody negative window period. Studies of chimpanzees who were very frequently sampled have detected HCV RNA within a few days to 2 weeks after exposure. 69 Data from human post-transfusion studies also detect RNA within 2 weeks of exposure64; in one series, PCR was positive approximately 59 days before detection of anti-HCV 5 (Fig 2). Therefore, the estimated reduction in risk with PCR testing is 72% (59 days of 82 days), giving an expected per-unit residual risk of 2.72 per million. When projected over 12 million donations, it is estimated that 84 HCV infectious window period units would be detected by HCV RNA PCR testing annually in the United States.
FINAL COMMENTS
The incidence/window period model has several distinct advantages over many of the methods that have previously been used to estimate transfusion risk. It allows the formulation of risk estimates for multiple agents using a single, database that can be obtained from information that is routinely avail-
INCIDENCE/WINDOW PERIOD MODEL FOR TX RISK 171
10. Busch MR Satten GA: Time course of viremia and antibody seroconversion following primary HIV infection: Implications for management of exposed health care workers. Am J Med, 102:51-58, 1997
11. Manns A, Wilks RJ, Murphy EL, et al: A prospective study of transmission by transfusion of HTLV-I and risk factors associated with seroconversion. Int J Cancer 35:91-97, 1992
12. Busch MP, Alter HJ: Will human immunodeficiency virus p24 antigen screening increase the safety of the blood supply and, if:so, at what cost? Transfusion 35:536-539, 1995 (editorial)
13. Cummings PD, Wallace EL, Schorr JB, et al: Exposure of patients to human immunodeficiency virus through the transfu- sion of blood components that test antibody negative. N Engl J Med 321:941-946, 1989
14. Murphy EL, Bryzman S, Williams AE, et al: Demo- graphic determinants of Hepatitis C virus seroprevalence among blood donors. JAMA 275:995-1000, 1996
15. Busch MP, Eble BE, Khayam-Bashi H, et al: Evaluation of screened blood donations for human immtmodeficiency virus type 1 infection by cultnre and DNA amplificatiofi of pooled ceils. N Engl J Med 325:1-5, 1991
16. Vyas GN, Rawal BP, Busch MP: The risk of HIV transmission by screened blood. N Engl J Med 334:992, 1996 (letter)
17. Ward JW, Holmberg SD, Allen JR, et al: Transmission of human immunodeficiency virus by blood transfusions screened as negative for HIV antibody. N Engl J Med 318:473-478, 1988
18. Kleinman S, Secord K: Risk of human immnnodefi- ciency virus transmission by anti-HIV negative blood. Transfu- sion 28:499-501, 1988
19. Selik RM, Ward JW, Buehler JW: Trends in transfusion- associated acquired immunodeficiency syndrome in the United States, 1982 through 1991. Transfusion 33:890-893, 1993
20. Imagawa DT, Lee MH, Wolinsky SM, et al: Human immnnodeficiency virus type 1 infection in homosexual men who remain seronegative for prolonged periods. N Engl J Med 320:1458-1462, 1989
21. Imagawa D, Detels R: HIV-1 in seronegative homosexual men. N Engl J Med 325:1250-1251, 1991
22. Jackson JB: Human imnmnodeficiency virus indetermi- nate western Nots and latent HIV infection. Transfusion 32:497- 499, 1992
23. Lifson AR, Stanley M, Pane J, et al: Detection of human immunodeficiency virus DNA using the polymerase chain reaction in a well-characterized group of homosexual and bisexual men. J Infect Dis 161:436-439, 1990
24. Farzadagen H, Polis MA, Wolinsky SM; et al: Loss of human immunodeficiency virus type 1 antibodies with evidence of viral infection in asymptomatic homosexual men: A report from the Multicenter AIDS Cohort Study. Ann Intern Med 108:785-790, 1988
25. Roy MJ, Damalo JJ, Burke DS: Absence of true serorever- sion of HIV-1 antibody in seroreactive individuals. JAMA 269:2786-2789, ,1993
26. Center for Biologics Evaluation and Research, FDA: Revised recommendations for the prevention of human immuno- deficiency ,/~rus (HIV) transmission by blood and blood prod- ucts, Rockville, MD April 23, 1992
27. Centers for Disease Control and Prevention: Persistent lack of detectable HIV-1 antibody in a person with HIV
infection--Utah, 1995. Morb Mortal Wldy Rep 45:181-185, 1996
28. Soriano V, Dronda F, Gonzales-Lopez A, et al: I-IIV-1 causing AIDS and death in a seronegative individual. Vox Sang 67:410-411, 1994
29. Korber BTM, MacInnes K, Smith RF, et al: Mutational trends in V3 loop protein sequences observed in different genetic lineage of human immunodeficiency virus type 1. J Virol 68:6730-6744, 1994
30. Nkengasong IN, Janssens W, Heyndricks L, et al: Geno- typicsubtypes of HIV-1 in Cameroon. AIDS 8:1405-1412, 1994
31. Sabino EC; Shpaer EG, Morgado MG, et al: Identifica- tion of human immunodeficiency virus type 1 envelope genes recombinant between subtypes B and F in two epiderniologi- cally linked individuals from Brazil. J Viro168:6340-6346, 1994
32. O'Brien TR, George JR, Holmberg SD: Human imnmno- deficiency virus type 2 infection in the United States: Epidemiol- ogy, diagnosis, and public health implications. JAMA 267:2775- 2779, 1992
33. Loussert-Ajaka I, Ly TD, Chaix M, et al: HIV-1/HIV-2 seronegativity in HIV-1 subtype O infected patients. Lancet 343:1393-1394, 1994
34. Centers for Disease Control and Prevention: Update: HIV-2 infection among blood and plasma donors--United States, June 1992 to June 1995. Morb Mortal Wkly Rep 42:603-606, 1995
35. Centers for Disease Control and Prevention: Identifica- tion of HIV-1 Group O infection Los Angeles County, Califor- nia, 1996. Morb Mortal Wkly Rep 45:561-564, 1996
36. Petersen LR, Satten GA, Dodd RI et al and the HIV Seroconversiou Study Group: Duration of time from onset of human immunodeficiency virus type 1 infectiousness to develop- ment of detectable antibody. Transfusion 34:283-289, 1994
37. Busch MP, Lee LLL, Satten GA, et al: Time course of detection of viral and serological markers preceding HIV-1 seroconversion; implications for blood and tissue donor screen- ing. Transfusion 35:91-97, 1995
38. Busch MP, Herman SA, Henrard DR, et al: Time course and kinetics of HIV viremia during primary infection. Third Conference on Retroviruses and Opportunistic Infections, Wash- ington, DC, Jan 1996 p 60 (abstr 38)
39. Lackritz EM, Kennedy MB, Doll LS, et al: Risk behav- iors and test seeking among HIV-1 positive blood donors. Transfusion 35:42S, 1995 (abstr, suppl)
40. Kleinman S, Secord K, Doyle M: Demographic profile and motivation for donation in donors who have seroconverted for HIV. Transfusion 28:29S, 1988 (abstr, suppl)
41. Zuck TF: Silent sequences and the safety of blood transfusions. Ann Intern Med 108:895-897, 1988
42. Busch MP: HIV and blood transfusions: Focus on seroconversion. Vox Sang 67:13-18, 1994 (suppl 3)
43. Korelitz JJ, Busch MP, Kleinman SH, et al: Relationship between antibody to hepatitis B core antigen and retroviral infections in blood from volunteer donors. Transfusion 36:232- 237, 1996
44. Korelitz JJ, Williams AE, Busch MP, et al: Demographic characteristics and prevalence of serologic markers among donors who use the confidential unit exclusion process: The retrovirus epidemiology donor study. Transfusion 34:870-876, 1994
45. AuBuchon JP, Birkmeyer JD, Busch MP: Cost-effective-
172 KLEINMAN ET AL
ness of expanded HIV test protocols for donated blood. Transfu- sion 37:45-51, 1997
46. Busch ME Satten GA, Herman SA, et al: Time course and kinetics of HIV viremia during primary infection. Transfu- sion 37:41S, 1996 (suppl, abstr)
47. Strainer SL, Salemi BL, Sievert WS, et al: Evaluation of US blood donations testing positive for HIV-1 p24 antigen. Transfusion 37:38S, 1996 (Suppl, abstr)
48. Kinloch S, Pert-in L, Hirschel B: The risk of HIV transmission by screened blood. N Engl J Med 334:992, 1996 (letter)
49. Kleinman S, Alter H, Busch M, et al: Increased detection of hepatitis C virus (HCV)-infected blood donors by a multiple- antigen HCV enzyme immunoassay. Transfusion 32:805-813, 1992
50. Aach RD, Stevens CE, Hollinger FB, et al: Hepatitis C virus infection in post-transfusion hepat i t is-An analysis with first- and second-generation assays. N Engl J Med 325:1325- 1329, 1991
51. Donahue JG, Munoz A, Ness PM, et al: The declining risk of post-transfusion hepatitis C virus infection. N Engl J Med 327:369-373, 1992
52. Nelson KE, Donahue JG, Stambolis V: Post-transfusion hepatitis C virus infection. N Engl J Med 327:1601-1602, 1992 (letter)
53. Esteban JI, Gonzales A, Heruandez JM, et al: Open prospective efficacy trial of anti-HCV screening of blood donors to prevent post-transfusion hepatitis, in Hollinger FB, Lemon SM, Margolis HS (eds): Viral Hepatitis and Liver Disease. Baltimore, MD, Williams and Wilkens, 1991, p 441
54. Cyrus S, Swenson S, Dembowski J: Removal of HCV infected donors with use of second generation anti-HCV EIA. Transfusion 32:36S, 1992 (abstr, suppl)
55. Simmonds P, Holmes EC, Cha TA, et al: Classification of Hepatitis C virus into six major genotypes and a series of subtypes by phylogenetic analysis of the NS-5 region. J Gen Viro174:2391-2399, 1993
56. Busch MP, Watanabe K, Smith JW, et al: False negative testing errors in routine viral screening. Transfusion 37:59S, 1996 (abstr, suppl)
57. Alter MJ, Margolis HS, Krawczynski K, et al: The natural history of community-acquired hepatitis C in the United States. N Engl J Med 327:1899-1905, 1992
58. Sugitani M, Shindo M, Inchauspe G, et al: Sensitivity of serological assays to identify blood donors with hepatitis C viraemia. Lancet 339:1018-1019, 1992
59. Kleinman S, Busch J, Holland P: Post-transfusion hepati- tis C virus infection. New Engl J Med 327:1601, 1992 (letter)
60. Barrera JM, Francis B, Ercilla G, et al: Improved detection of anti-HCV In post-transfusion hepatitis by a third generation ELISA. Vox Sang 68:15-18, 1995
61. Busch MR Korelitz JJ, Kleinman SH, et al: Declining value of alanine aminotransferase in screening of blood donors to prevent posttransfusion hepatitis B and C virus infection. Transfusion 35:903-910, 1995
62. Lelie PN, Cuypers HTM, Reesnick HW, et al: Patterns of serological markers in transfusion-transmitted hepatitis C infec- tion using second generation HCV assays. J Med Virol 37:203- 209, 1992
63. Busch MR Lee SR: Yield of HCV EIA 3.0 vs 2.0 for detection of seroconverting donors. Transfusion 37:51S, 1996 (abstr, suppl)
64. Alter HJ: To C or not to C: These are the questions. Blood 85:1681-1695, 1995
65. Blajchman MA, Bull SB, Feinman SV: Post-transfusion hepatitis: Impact of non-A, non-B surrogate tests. Lancet 345:21-25, 1995
66. Mosley JW, Huang W, Strata DO: Donor levels of serum alanine aminotransferase activity and antibody to hepatitis B core antigen associated with recipient hepatitis C and non-B, non-C outcomes. Transfusion 36:776-781, 1996
67. Esteban JI, Camps J, Genesca J, et al: Hepatitis C and B: New development, in Nance SJ, (ed): Blood Safety: Current Challenges. Bethesda, MD, American Association of Blood Banks, 1992, pp 45-96
68. National Institutes of Health: Infectious disease testing for blood transfusions. NIH Consensus Statement Jan 9-11, Betbesda, MD 13:1-27, 1995
69. Farci P, London WT, Wong DC, et al: The natural history of infection with hepatitis C virus in chimpanzees: Comparison of serologic responses measured with first and second genera- tion assays and relationship to viremia. J Infect Dis 165:1006- 1011, 1992