The Bioartificial Pancreas: Progress and Challenges
Transcript of The Bioartificial Pancreas: Progress and Challenges
968
DIABETES TECHNOLOGY & THERAPEUTICSVolume 7, Number 6, 2005© Mary Ann Liebert, Inc.
The Bioartificial Pancreas: Progress and Challenges
SEDA KIZILEL, Ph.D.,1 MARC GARFINKEL, M.D.,1 and EMMANUEL OPARA, Ph.D.2
ABSTRACT
Diabetes remains a devastating disease, with tremendous cost in terms of human sufferingand healthcare expenditures. A bioartificial pancreas has the potential as a promising approachto preventing or reversing complications associated with this disease. Bioartificial pancreatic con-structs are based on encapsulation of islet cells with a semipermeable membrane so that cellscan be protected from the host’s immune system. Encapsulation of islet cells eliminates the re-quirement of immunosuppressive drugs, and offers a possible solution to the shortage of donorsas it may allow the use of animal islets or insulin-producing cells engineered from stem cells.During the past 2 decades, several major approaches for immunoprotection of islets have beenstudied. The microencapsulation approach is quite promising because of its improved diffusioncapacity, and technical ease of transplantation. It has the potential for providing an effectivelong-term treatment or cure of Type 1 diabetes.
INTRODUCTION
DIABETES MELLITUS represents a major publichealth problem, as it is the most frequent
endocrine disease in industrialized countries.1,2
According to the latest estimates, the numberof people with this disease worldwide is 177million, and this figure will double by the year2025.3 The complications of diabetes are asso-ciated with multiple medical problems relatedto ophthalmic, renal, neurological, cerebrovas-cular, cardiovascular, and peripheral vasculardisease.4–9 The economic burden of diabetes isrelated to its management, to the treatment ofits secondary complications, and to resultantproductivity loss.10 While one estimate showsthat the cost of treating diabetes in the UnitedStates in 1997 was $44 billion,3 another study
has shown that it cost about $100 billion to treatdiabetes and its complications in this countryin 1992.10
Type 1 diabetes, also previously known asinsulin-dependent diabetes mellitus, occurswhen pancreatic islet cells are unable to pro-duce insulin. Consequently, the blood glucoseconcentration becomes high while tissues arestarving for metabolic fuel. In Type 2 diabetes,previously referred to as non–insulin-depen-dent diabetes, the body continues to make atleast some insulin, but is unable to respondproperly to the action of insulin produced bythe pancreas. The Diabetes Control and Com-plications Trial11 showed that an improvedmetabolic control was achieved using intensiveinsulin treatment in Type 1 diabetes patients.However, the aggressive management of dia-
1Section of Transplantation, Department of Surgery, The University of Chicago, Chicago, Illinois.2Pritzker Institute of Biomedical Science and Engineering, Illinois Institute of Technology, Chicago, Illinois.
Review
6019_13_p968-985 12/21/05 3:09 PM Page 968
betes with exogenous insulin only delayed theprogression and development of complicationsof this disease. Also, intensive insulin treat-ment could only be applied to fewer than 10%of patients due an increased risk of severeepisodes of hypoglycemia. Furthermore, it ap-pears that C-peptide, a cleavage product fromthe processing of pro-insulin to insulin, pre-vents diabetes and hyperglycemia-inducedvascular and neural dysfunction in animal andclinical models of diabetes and should there-fore be used in combination with insulin tomaintain vascular and neural functions as wellas blood glucose levels.12–15
Advances in transplantation and in im-munosuppression have made pancreas trans-plantation another treatment option for Type 1diabetes. The main objective for pancreas trans-plantation is to achieve normal level of glucosein the blood and to free the patient from ex-ogenous insulin requirements based on multi-ple finger stick glucose measurements.16 Eventhough successful pancreas transplantationprovides normal glucose homeostasis, the requirement of lifelong immunosuppressionmakes it unclear whether transplantation is ad-vantageous over continued insulin treatment.17
Also, because of the need for immunosuppres-sion, most pancreas transplantations have beendone simultaneously with a kidney transplantin patients who have advanced nephropathy.18
In contrast to pancreas transplantation, islettransplantation requires no major surgery.Also, islet transplantation offers an alternativeto exogenous insulin treatment, as it can resultin better glycemic control19 and potentiallyavoids surgical complications associated withwhole-organ pancreas transplantation. It isknown that islet cell transplantation can pre-vent, and, in some cases, reverse existing com-plications of diabetes probably because of therole played by C-peptide.20 However, majorchallenges remain to be addressed before islettransplantation can be used routinely and ap-plied more widely to patients with diabetes.One major barrier is the shortage of humanpancreas as a source of islet cells. Also, lifelonguse of immunosuppressive drugs to overcomethe rejection of transplanted tissue poses a sig-nificant risk to patients, as the use of glucocor-ticoids and cyclosporine have dose-dependent
deleterious effects on glucose homeostasis and�-cell function, and result in increased inci-dences of infection and cancer.20–24 The intro-duction of the steroid-free immunosuppressivedrug regimen has resulted in long-term graftsurvival of islets with concomitant control ofblood glucose levels.25 However, this immuno-suppressive drug regimen is also not withoutrisks to graft recipients.26
The routine application of islet transplanta-tion would be tremendously enhanced by anunlimited supply of donor tissue, a standardimplantation procedure, and the ability tomaintain the transplanted tissue without the re-quirement of immunosuppressive drugs.27 Toachieve these goals, immunoisolation (encap-sulation) of islet cells has been proposed to pro-tect cells from attack by the host immune sys-tem. Using immunoisolation of the islets,chronic administration of immunosuppressivedrugs can be theoretically eliminated or mini-mized, as transplanted cells are separated fromthe host immune system by a biocompatibleand semipermeable membrane.28,29 Moreover,immunoisolation of pancreatic islet cells fortransplantation into patients with diabetes the-oretically permits grafting of xenogenic islets,thus expanding the potential supply of donorislet tissue.25 Hence, immunoisolation couldopen up the possibility of using islets harvestedfrom animals, or insulin-producing cells engi-neered from stem cells without the requirementof immunosuppression of transplant recipi-ents. Porcine and bovine insulin amino acid se-quences have considerable sequence homologywith human insulin,30 and therefore pigs andcows are considered attractive as options forxenogeneic donors.
One important consideration in using mi-croencapsulated islets is defining the optimalsite for transplantation. To date, most researchhas considered peritoneal cavity as the optimalsite for implantation of encapsulated islets, asit is possible to transplant microcapsules intothe peritoneal cavity using a simple procedurethat could be suitable for routine outpatientuse.29,31–34 Also, this site allows for implanta-tion of high numbers of islets, which can be re-trieved by peritoneal lavage35 if necessary.36
However, this site limits graft viability becauseof low blood supply, oxygen tension, and con-
THE BIOARTIFICIAL PANCREAS 969
6019_13_p968-985 12/21/05 3:09 PM Page 969
centration of essential minerals.34 In addition,the release of insulin from the peritoneal cav-ity to the blood stream is delayed comparedwith hormones released to the portal vein.37
Also, peritoneal macrophages have a high tox-icity against encapsulated islets.38
Several researchers have also explored theportal vein of the liver as an alternative site fortransplantation of immunoisolated islets.39
Based on its double vascularization (hepaticartery and portal vein), the intraportal locationhas a high oxygen and nutrient supply, whichcould be beneficial for the performance and thelongevity of microencapsulated cells.39 Also,the liver is considered to be an immunologi-cally privileged site.40 But, even more clinicallyrelevant, is the use of percutaneous transhep-atic catheterization, which provides relativelysimple, inexpensive, and non-surgical access tothe liver.41 In addition, The International IsletRegistry reports more C-peptide-positive cases(more than 0.5 ng/mL) 1 year after transplan-tation into the portal vein than from any othersite.42
This article reviews the recent progress andchallenges remaining for the successful devel-opment of a bioartificial pancreas, and dis-cusses the requirements to bring this technol-ogy closer to clinical application.
HISTORICAL DEVELOPMENT
The pancreatic origin of diabetes was dis-covered in 1889 by Mering and Minkowski,when surgical removal of the pancreas causeddogs to develop diabetes. In 1913, Murlin andKramer prepared extracts of bovine pancreasto lower the blood glucose in a dog with dia-betes. However, the benefit of the extract wasexplained by the presence of lactate. Finally, in1922, Banting and Best developed a method forpreparing a pancreatic extract, and a few yearslater, injection of the active factor in this extract,insulin, became the main therapy for Type 1 di-abetes.
As of today, the treatment options for Type1 diabetes are exogenous insulin with externalglucose monitoring, whole-organ pancreastransplantation, islet cell transplantation, the ar-tificial pancreas, and the bioartificial pancreas.
Among these treatments, the bioartificialpancreas avoids the use of immunosuppressivedrugs while providing moment-to-momentglucose homeostasis consistent with a well-functioning native pancreas. It is important inthis context to distinguish between the terms“artificial pancreas” (sometimes called “me-chanical artificial pancreas”) and “bioartificialpancreas.”
The mechanical artificial pancreas consists ofa glucose sensor, an insulin pump, and a com-puter, which determines the rate of insulin de-livery. The sensor may be implanted in thevena cava, and may require periodic replace-ment. The development of a glucose biosensorhas been challenged by the difficulty of creat-ing a sensitive, stable, and accurate sensor, de-spite the capability of a mechanical artificialpancreas to regulate glucose levels. An error insensing, computation, or delivery could resultin insulin overdosing, which could be poten-tially risky with life-threatening hypogly-cemia,43–46 an unacceptable potential side effectof an artificial pancreas. It is also very difficultto produce a mechanical artificial pancreas thatresponds quickly enough to changes in bloodsugar (islets respond in less than 10 min).47
In contrast, a bioartificial pancreas is a de-vice that substitutes for the endocrine portionof the pancreas. Devices in this category con-tain synthetic materials and functional isletsencapsulated within a semipermeable mem-brane to protect cells from the host immune re-sponse. The semipermeable membrane permitsexchange of nutrients, glucose, and insulinwith the host, but excludes the diffusion of im-munoglobulins, complement, and white bloodcells. The device may be implanted into a vas-cularized site48,49 or into the peritoneal cavity.36
The idea of using ultrathin polymer mem-brane microcapsules was proposed by Chang50
in 1964 for the immunoprotection of trans-planted cells. Nearly 2 decades later, the con-cept of bioencapsulation was successfullyshown to maintain glucose homeostasis in ratswith diabetes using encapsulated allogeneicislets.32 When alginate microcapsules contain-ing islets were implanted in rats, normal bloodglucose levels were achieved for 13 weeks. Themicrocapsule used in that study consisted of aninner alginate core surrounded by a polylysine
KIZILEL ET AL.970
6019_13_p968-985 12/21/05 3:09 PM Page 970
membrane, which was then surrounded by anouter polyethyleneimine coating. In later stud-ies, the outer layer was replaced by the morebiocompatible alginate coating because of aninflammatory reaction induced by polyethyl-eneimine.51 Since then, a variety of studies havebeen performed to understand the require-ments for successful transplantation of encap-sulated islet cells, but there is still a need forconvincing evidence of success of encapsulatedislet transplantation in either non-human pri-mates or humans.49
IMPEDIMENTS TO THE PROGRESS OFCELL ENCAPSULATION TECHNOLOGY
Fibrotic overgrowth of the implanted micro-capsules is one of the major obstacles to pro-gress in cell encapsulation technology. Invari-ably, the materials used for encapsulation arenot completely inert, and can induce foreignbody and inflammatory reactions. As a result ofthis fibrous tissue overgrowth, the diffusion ofnutrients, oxygen, hormones, and waste prod-ucts through the capsule is diminished, and en-capsulated islets are destroyed because of hy-poxia, starvation, and the secretion of nitricoxide by the stimulated macrophages.52 This fi-brotic reaction to implanted microcapsules hadpreviously been associated with commerciallyavailable alginate with high mannuronic acidcontent, which activates macrophages in vivo,resulting in fibroblast proliferation and even-tual overgrowth.53 However, later studies didnot support that notion.33 It has also beenshown that polylysine may cause a fibrotic re-sponse through the induction of cytokines.54
Another important component of capsulardesign is permselectivity. Most capsule designsare based on the presumption that the effec-tiveness of immunoisolation of a polymer cap-sule is closely related to the pore size of the cap-sule membrane.55–57 However, pore sizes ofpolymer membranes are not homogeneous bynature, and consist of a broad spectrum ofsizes.58 Total immunoprotection of encapsu-lated cells can only be provided if the polymermembrane does not have any pores larger thanthe antibody complement component.59 Thisfact has been largely ignored by researchers
and has resulted in inconsistent findings in thefield.60–66
Mechanism of immunologic attack of allograftsand xenografts
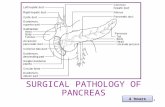
With regard to specific immunologic attackof encapsulated cell implants, there are differ-ences in the immune protection requirement ofallografts versus xenografts. An allograft is agraft between genetically different individualswithin the same species, while a xenograft is agraft between individuals from differentspecies. Allograft rejection occurs as result ofactivation of cellular immunity by interactionsof host T cells with a graft, while humoral im-munity, including antibodies and complementproteins, is responsible for the rejection ofxenografts.67,68 In the direct pathway of anti-gen presentation, the T cell receptor recognizesT cells presented by donor-type antigen-pre-senting cells along with Class I or II major his-tocompatibility complex (MHC) molecules.The idea of immunoisolation using a polymermembrane is to separate allogeneic or xeno-geneic tissue from the immune system of therecipient. Therefore, microencapsulation ofislets within effective permselective mem-branes would prevent contact with im-munoglobulin, complement components, andinflammatory cells. However, there is also a po-tential immune response towards antigensshed by encapsulated allogeneic or xenogeneiccells. Such antigens could be therapeutic agentthemselves, cell surface molecules, or cell com-ponents (phospholipids, DNA), includingthose released upon cell death. Shedding ofantigens from encapsulated cells would initiatea molecular tissue response around the im-plant, which could affect the viability and func-tion of the encapsulated cells. As a result of thisimmunological reaction, these shedded anti-gens may be internalized, processed, and pre-sented in association with host Class II MHCmolecules (macrophages and dendritic cells) tohost CD4� helper T cells (Fig. 1). The recogni-tion of antigens through this indirect pathwaymay lead to the activation of T helper cells,which then secrete cytokines and regulate cell-mediated immune response and inflamma-tion.69,70 Small molecules, such as reactive oxy-
THE BIOARTIFICIAL PANCREAS 971
6019_13_p968-985 12/21/05 3:09 PM Page 971
gen species and cytokines, may also passthrough the polymer membrane and damagethe transplanted tissue.
Owing to the complexity of the immune re-sponse mechanism, it is important to under-stand the mechanism of immune protection,and considerable efforts have been made to in-vestigate this issue. Chen et al.71 developed celllines that have resistance to cytokines and oxy-gen radical-induced damage. Recently, macro-phage depletion has also been used as a tool toprotect xenografts from immune destruction. Ithas been found that depletion of peritonealmacrophages with clodronate liposomes im-proved the survival of macroencapsulatedporcine neonatal pancreatic cell clusters.35
Safley et al.72 evaluated the cellular immune re-sponse in non-obese diabetic (NOD) mice aftertwo different pathways of T cell co-stimulationwere blocked. Alginate–poly-L-lysine-encapsu-lated porcine islet xenografts were trans-planted intraperitoneally in NOD mice treatedwith CTLA4-immunoglobulin to block CD28/B7 and with anti-CD154 monoclonal antibodyto inhibit CD40/CD40–ligand interactions. Itwas concluded that blocking two differentpathways of T cell co-stimulation inhibited Tcell-dependent inflammatory responses, and
significantly prolonged the survival of encap-sulated islet xenografts.
Another approach to improving the survivalof microencapsulated islets can be to use localimmunosuppression. Studies have shown thatpreimplantation of an immunoisolating deviceimproved the survival of an encapsulated isletgraft and reduced fibroblast outgrowth.73 Func-tional capsules may also be designed to releasethe immunosuppressive agent in a controlledmanner. Local immunosuppression induced us-ing this approach may prevent the occurrenceof an undesirable reaction around the implant.
Inflammatory reaction in response to the im-plantation of cell-free capsules involves a se-quence of events similar to a foreign body re-action, starting with an acute inflammatoryresponse and leading to a chronic inflamma-tory response or granulation tissue develop-ment and fibrous capsule development. The in-tensity and duration of each of these responsesare dependent upon several factors, such as theextent of injury created in the implantation,biomaterial chemical composition, surface free energy, surface charge, porosity, surfaceroughness, and implant size and shape.74,75 Thebiocompatibility of the material is determinedby the extent and deviation from the optimalwound healing conditions.76
Sources of donor islets
Despite all of the advances in islet transplan-tation and in encapsulation technology, somechallenges must be still overcome before thebioartificial pancreas can be broadly applied.The most significant of these challenges is theshortage of donor islets. This shortage is the motivation for researchers to find alternativesources of insulin-producing cells. Promisingapproaches for resolving this problem are dif-ferentiation of stem cells into cells with �-cell-like characteristics77–80 and genetic engineeringof adult cells for secretion of recombinant in-sulin.81–86 Based on similarities between mech-anisms that control the development of both theadult pancreas and the central nervous system,methods promoting neural differentiation ofembryonic stem cells have been adapted by re-searchers to derive insulin-producing cells.87–91
Hori et al.92 investigated the possibility of di-recting neural progenitors to develop into glu-
KIZILEL ET AL.972
FIG. 1. Schematic representation of antigen recognitionvia (A) the direct pathway and (B) the indirect pathway.APC, antigen-presenting cells; TCR, T cell receptor.
6019_13_p968-985 12/21/05 3:09 PM Page 972
cose-responsive insulin-producing cells usinginductive signals involved in normal pathwaysof islet development. Compared with othermethods for insulin-producing cell develop-ment from human stem cells,91,93 the methoddeveloped by this group produced insulin atthe highest levels yet achieved from an ex-pandable, human stem cell-derived tissue.However, the method developed in the studystill needs to be improved, perhaps through theaddition of glucagon-like peptide-1, trans-forming growth factor-� ligands, or other fac-tors to potentiate �-cell maturation, growth,and insulin secretion.94–96
Gene therapy has also been suggested as atreatment of insulin-dependent diabetes melli-tus. This strategy can be applied by preventingthe autoimmune destruction of �-cells,97,98 byregenerating �-cells,99,100 or by engineering in-sulin-secreting surrogate �-cells.99,101–103 Sapiret al.104 recently suggested the potential use ofadult human liver as an alternate tissue for au-tologous �-cell-replacement therapy. Usingpancreatic and duodenal homeobox gene 1(PDX-1) and soluble factors, they managed toinduce a comprehensive developmental shift ofadult human liver cells into functional insulin-producing cells. According to the findings ofthat study, PDX-1-treated human liver cells ex-pressed insulin, stored it in defined granules,and secreted the hormone in a glucose-regu-lated manner. When these cells were implantedunder the renal capsule of immunodeficientmice with diabetes, the cells ameliorated hy-perglycemia for prolonged periods of time. Thetechnique offers both the potential of a cell-re-placement therapy for patients with diabetesand allows the patient to be the donor of his orher own insulin-producing tissue.
Intestinal K cells have also been engineeredto express and secrete insulin in a glucose de-pendent manner, generating functional �-cells.105,106 With the development of robust andsafe gene therapy, this strategy may lead to ef-fective therapy in the future.
Preservation of encapsulated cell systems
The last challenge for a bioartificial pancreasto become a routine clinical application is thelong-term cryopreservation of encapsulatedcells. Validated technologies are required for
long-term preservation of encapsulated cell sys-tems to maintain a product inventory, and in or-der to meet end-user demands. One of the cur-rent strategies for overcoming the problem ofcryopreservation of tissue is the reduction of cry-oprotectant [dimethyl sulfoxide (DMSO)] con-centration or complete replacement by equallypowerful substances. Recent work in Dr. Opara’slaboratory has demonstrated that cryopreserva-tion of islet cells cultured overnight in the pres-ence of 10% polyvinylpyrrolidone yielded higherintact islet recovery compared with islets frozenin the presence of DMSO and glycerol.107 Thelower islet cell integrity and function were ex-plained on the basis of hypothesis that low-mo-lecular-weight compounds, such as DMSO andglycerol, permeate the cell and interact hy-drophobically with intracellular proteins, whichresults in perturbed cytoskeletal architecture ofthe frozen cells and diminished islet cell integrityand function.
The other promising technical improvementof the cryopreservation technology is the re-duction of total sample volume. Miniaturizationof the cryosubstrates from 1 mL to microlitersreduces temperature gradients in cryosub-strates, which makes it possible to achievehigher freezing rates and more homogeneousfreezing of the sample.108 Islets cryopreservedwith this strategy were highly functional evenwith the lower DMSO concentrations.109
Misler et al.110 studied stimulus–secretioncoupling in whole islets as well as single � cellsfrom carefully selected cryopreserved andthawed human islets of Langerhans. They foundthat without using any of the recent advances incryopreservation technique, cryopreserved andthawed human islets, which were selected basedon their smooth surface and diameter, re-sponded to glucose in a calcium- and metabolic-dependent fashion. In another study by vonMach et al.,111 viability of pancreatic islets aftercryopreservation was correlated negatively withtheir size, and suppression of insulin release wasnot observed for islets �300 �m.
DIFFERENT FORMS OF BIOARTIFICIALPANCREAS
Various configurations have been studied forthe purpose of immunoisolation of islets. These
THE BIOARTIFICIAL PANCREAS 973
6019_13_p968-985 12/21/05 3:09 PM Page 973
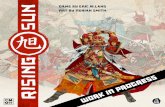
include biohybrid vascular devices, extravas-cular chambers, and encapsulation.112,113 En-capsulation is the technique of islet im-munoisolation using biopolymeric spheres ofdifferent sizes. Currently, results in rodentsand dogs with diabetes indicate that sphericalmicro- and macrocapsules appear to have thehighest therapeutic potential.60,65,114 A micro-capsule typically contains only a few hundredcells or a single islet, and to provide a thera-peutic dosage, tens of hundreds of thousandsof cells are required. In contrast, macrocapsulesemploy much larger depots to contain the fulltherapeutic dosage in one or a few implants.
Macrocapsules are shaped as cylinders orplanes, and typically one dimension is in therange of 2–6 mm (Fig. 2a).115,116 One advantageof the implantation of macrocapsules is the easeof retrieval in case of complications. However,despite reports of reduced risks in the implan-tation of macrocapsules, it has been shown thatmacroencapsulated islets have significantly im-paired insulin secretion because of necrosis inthe center of aggregated islet clumps as a re-sult of diffusion limitations of nutrients andoxygen.116,117
Encouraging results have been obtained byimmobilization of the islets in a matrix beforefinal macroencapsulation.115,118 Limited diffu-sion of nutrients, as well as slow exchange ofglucose and insulin, occurs as a result of rela-tive large surface-to-volume ratio of these de-vices. To ensure sufficient nutrient and oxygendiffusion to the cells, islet cell density withinthe macrocapsules is kept to around 5–10% ofthe volume fraction. This approach, however,requires the implantation of large devices in or-der to provide adequate masses of insulin-pro-ducing cells, and large grafts are not practicaland cannot be transplanted in conventionalsites.119
In contrast, microencapsulation offers an op-timal volume-to-surface ratio for fast exchangeof hormones and nutrients without a large de-vice. The technique involves enclosure of oneor two islets within small spheres, which havediameters of less than 1 mm (Fig. 2b). Also, be-cause of reduced volume of the islet transplants,and in contrast to macroencapsulated islets, mi-crocapsules can theoretically be transplanted indelicate sites, such as the portal vein. The trans-
plantation of microcapsules into the peritonealcavity, an outpatient-based procedure,33,120–122
makes it particularly attractive to patients anddoctors. Interestingly, intraperitoneally im-planted microencapsulated islets have shownpromising results in large animal122–124 modelsas well as in limited clinical trials.33
TECHNIQUES INMICROENCAPSULATION
Materials used for microencapsulation
Various materials have been used as biopoly-meric coats in islet microencapsulation. Thesehave included alginate, agarose, tissue-engi-neered chondrocytes, polyacrylates,125,126 andpoly(ethylene glycol) (PEG).
Alginate–polylysine-based microencapsula-tion of islets, first described by Lim and Sun,32
has been found not to interfere with cellular func-tion, and these microcapsules have been shownto be stable for years in small and large animalsas well as in human beings.127–132 Alginate is alinear polysaccharide extracted from seaweed.133
It is composed of three types of 1 � 4-linkedpolyuronic acid blocks containing poly-L-gu-luronic acid segments (G blocks), poly-D-ma-nuronic acid segments (M blocks), and segmentsof alternating L-guluronic and D-mannuronicacid residues, and it has gel-forming propertiesin the presence of most polyvalent cations.133,134
Impurities, such as monomers, catalysts, and ini-tiators present in synthetic polymers, may con-tribute to the failure of the encapsulated islet im-
KIZILEL ET AL.974
(a) Macroencapsulation
(b) Microencapsulation
FIG. 2. Immunoisolated islets within (a) membrane dif-fusion chambers (macrocapsules) and (b) microcapsules.
6019_13_p968-985 12/21/05 3:09 PM Page 974
plants.135 Other impurities, such as pyrogens andmitogens, can be found in polymers derivedfrom natural substances, such as seaweed.135 Upto 90% of the impurities can be removed by elec-trophoresis or by the Klock extraction purifica-tion procedure.130,135 Conflicting reports exist onwhether alginate with high M blocks or high Gblocks results in increased fibrosis.53 It has beenshown, however, that the inflammatory re-sponse to alginate becomes less with purifica-tion, irrespective of the composition used.36,136
The immunoisolating permselectivity of al-ginate microcapsules can be achieved by soak-ing the initial alginate beads in 0.05–0.1%polylysine dissolved in normal saline for 6–20min. This occurs as a result of the binding ofnegatively charged carboxyl groups on the al-ginate to positively charged �-amino groups onthe amino acid polymer. The droplets are againrinsed with normal saline, followed by the ad-dition of an outer alginate layer by soaking ina lower concentration of 0.06–0.25% sodium al-ginate for 4 min. It is extremely important thatthe outer coating of alginate on top of thepolylysine membrane is complete. In the caseof incomplete cover of the polylysine coatingand when an impure alginate is used for theouter coating, microcapsules may become com-pletely covered by cell overgrowths within 1week of transplantation because of the inflam-matory reactions attributable to polylysine andthe impurities in the alginate.137 To dissolve theintracapsular sodium alginate by chelation ofthe cross-linking calcium, the resulting micro-capsules are treated with 55 mM sodium cit-rate for 7 min. The hollow microcapsules con-taining a few islets are then washed with saline(Fig. 3). It appears that liquefaction of the in-ner alginate core of microcapsules is requiredfor optimal function of the enclosed islets.138
One successful transplantation of encapsulatedislets performed with this technique was re-ported by a team of investigators at Duke Uni-versity. The encapsulated islets were madewith an outer alginate coating and inner poly-L-ornithine layer for permselectivity. To liquefythe inner alginate core of each bead a salt treat-ment was used. After transplantation, encap-sulated islet cells were shown to keep a baboonwith diabetes from requiring exogenous in-sulin for more than 9 months.122
For a capsule to be stable in vivo it has to bewater insoluble, as capsule dissolution willelicit a continuing inflammatory response andwill ultimately expose the transplanted cells tothe host. Both alginate and polylysine are wa-ter-soluble polymers and are both expected toelicit an inflammatory or foreign body re-sponse. However, findings indicate that thepolyelectrolyte complex formed during encap-sulation is biocompatible and less soluble inwater than the individual components.62,139,140
Differences in biocompatibility were also notedbetween empty and cell-containing capsules inNOD mice,141,142 which could be due to the dif-ficulty of producing reproducible cell-contain-ing capsules. For better biocompatibility, onegroup has suggested the use of high guluronicacid-containing alginates,53 while anothergroup modified alginate–polylysine capsuleswith PEG.132 An alternative approach has beenchosen to obtain stronger and more biocom-patible microcapsules using synthetic poly-acrylates such as the water-insoluble syntheticcopolymer hydroxyethyl methacrylate-methylmethacrylate.143 This research group has se-lected the acrylate monomers because of theirdiversity and has shown that mammalian cells
THE BIOARTIFICIAL PANCREAS 975
FIG. 3. Microencapsulation of islets with alginate–polylysine.
6019_13_p968-985 12/21/05 3:09 PM Page 975
may be microencapsulated in uncharged andpolyelectrolyte polymer, in polyelectrolytecomplexes, and inside a cohesive precipitatefrom a destabilized emulsion, without loss ofviability.
Polymerization of acrylamide monomer onislet cells encapsulated in agarose microsphereshas also been reported.144 However, whenpolymerization is in direct contact with tissue,this can generate excessive local heating andcytotoxicity.145 Poly(styrene sulfonic acid), oneof the most potent complement-interactingpolymers, was selected for the purpose of con-suming cytolytic complement activity andmixed with agarose for the preparation of mi-crobeads to protect xenogeneic islets in micewith diabetes from the humoral immune reac-tion.63,146 Antibodies and complement proteinsplay a major role in the rejection of xenografts.Binding of antibodies to the antigens on thexenogeneic cell surface cannot alone damagethe islet cell. For destruction of the xenogeneiccells to occur, complement activation by anti-gen–antibody complexes present on the cellsurface is required.147 Various polymers bear-ing hydroxyl groups such as regenerated cel-lulose, cellulose acetate, and poly(ethylene-co-vinyl alcohol) activate the complement systemthrough the alternative pathway,148 whereasother polymers bearing sulfonic acid or sulfategroups strongly interact with complement pro-teins and decrease the cytolytic complement ac-tivity.149
As previously noted, a fibrotic reaction afterimplantation would limit the diffusion of es-sential nutrients or metabolites, leading to re-duced viability or impaired functional activityof the encapsulated cells. Several studies havereported the usefulness of coating membranesurfaces with poly(ethylene oxide) (PEO) in or-der to reduce protein adsorption and associ-ated fibrotic reaction.150 This was achieved byexposing the poly(acrylonitrile-vinyl chloride)membrane surface to amine-terminated PEOafter acid hydrolysis of the nitrile group to acarboxylic acid. Membrane surfaces were alsoexposed to PEO-succinimide after base reduc-tion to an amine.151 The in vivo responseproved that a smaller number of macrophagesand foreign body giant cells were present onthe PEO-grafted membrane surface without
any change in transport properties. The otherapplication to modify the membrane surfacewas achieved by synthesizing a graft copoly-mer having poly-L-lysine as the backbone andthe monomethoxy PEG as pendant chains. Mi-crocapsules with sodium alginate were formedusing this polycationic copolymer, which dem-onstrated reduced protein adsorption, comple-ment binding, and cell adhesion in vitro com-pared with materials with unmodified poly-L-lysine.132
That artificial materials used for immuno-isolation purposes are not completely inert andcan induce foreign body and inflammatory re-actions have led researchers to study tissue-en-gineered capsules of rat chondrocytes. Polloket al.126 proposed the encapsulation of isletswith a layer of chondrocytes and their matrixto prevent immunorecognition and destructionof transplanted allogeneic or xenogeneic islets.This investigation demonstrated the mem-brane’s ability as an immunoisolation barrierby utilizing the immunoprivileged propertiesof the chondrocyte matrix. This approachmight offer a therapeutic advantage for pa-tients with diabetes, using the patient’s ownchondrocytes from a cartilage biopsy specimenas the encapsulation material.
PEG is another polymer that has been uti-lized for the purpose of encapsulating islets. Inorder to obtain stable and biocompatible gelswithout any cytotoxicity generation, Pathak etal.152 and Cruise et al.153 reported rapid pho-topolymerization of water-soluble PEG-basedmacromers in direct contact with islet cells.PEG is biocompatible, nontoxic, non-immuno-genic, and hydrophilic and can be chemicallycross-linked into hydrogels for a variety of ap-plications.154,155 Diffusion profiles of proteinsthrough PEG diacrylate hydrogels showed thatgels formed with the proper formulation werecapable of being immunoprotective. The semi-permeable properties of cross-linked PEG hy-drogels made by interfacial photopolymeriza-tion of PEG diacrylate were also studied byCruise et al.156 by forming hydrogels uponpoly(vinylidiene fluoride) microporous filters.This approach allowed them to study the effectof molecular weight and concentration of thePEG diacrylate on the diffusivity of biologicalmolecules.
KIZILEL ET AL.976
6019_13_p968-985 12/21/05 3:09 PM Page 976
Techniques used for droplet generation
The other major consideration in microen-capsulation technology is how to get the cellsinto the individual polymer capsules. Tech-niques to form such a physical barrier includeair-jet syringe pump droplet generator, inter-facial photopolymerization, and selective with-drawal.
One of the main devices used for microen-capsulation of islets with alginate–polylysine isthe air-jet syringe pump droplet generator.157
The device consists of an air jacket surround-ing an alginate nozzle through which alginatesolution is injected.158,159 Islets are suspendedin a solution of 1.4–3% sodium alginate, andspherical droplets of this suspension areformed by an air-jet syringe pump generator.As alginate droplets are forced out of the endof the needle by the syringe pump, the dropletsare pulled off by the shear forces set up by theflowing air stream. The size of the sphericaldroplets is controlled by adjusting the flow rateof the air jacket. The spherical droplets are col-lected in a funnel containing HEPES acid buffersupplemented with 1.1% CaCl2 solution, whichtransformed alginate droplets into rigid beadsby gelation.110 Excess fluid is drained with theaid of a filtering device consisting of a nylonmesh and a stopcock at the exit end of the fun-nel, and the droplets are washed in normalsaline.
As noted earlier, an air jet-syringe pump ex-trusion method generates gel droplets contain-ing entrapped islets from the suspension of theislets in aqueous sodium alginate solution.However, there are various constraints con-cerning the use of this procedure to producemicrocapsule diameters of less than 700 �m. Toform perfectly spherical capsules, the viscosityof the gel-forming liquid must be greater than30 cp. Also, to prevent the blockage of the nee-dle by the islets, the minimum internal diame-ter of the needle must be greater than 300 �m.Finally, the volumetric airflow rate must re-main below 2,000 mL/min in order to producecapsules of uniform diameter. This procedurewas improved by employing an electrostaticdroplet generator to form uniform, smooth,and perfectly spherical microcapsules having adiameter about 150–500 �m.160 A droplet,
which is charged with high static voltage, issuspended from a needle and attracted to a col-lecting vessel with opposing polarity. Once thevoltage threshold potential is passed, thedroplet moves from the needle to the collect-ing vessel. Droplets with predetermined sizesmay be repeatedly generated as the voltagepulse height, pulse frequency and length, andextrusion rate of the droplets are adjustable. Asshown in Figure 4, droplets are formed as theplunger is driven by the syringe pump and ex-pelled towards a collecting vessel containing ahardening solution, which may be aqueous cal-cium chloride in the case of an aqueous dropletforming liquid containing sodium alginate.Negative polarity was attached to the needle,while positive polarity was attached to themetal ring. As the voltage applied duringdroplet formation is a static voltage, the via-bility of the encapsulated islets is not compro-mised.
Biomolecules such as proteins and cells canalso be deposited as patterned droplets ontosurfaces for the development of cell-basedbiosensing devices for applications such ashigh-throughput drug screening.161 There arenumerous techniques for microfabrication ofpatterned polymer surfaces for protein deliv-ery. Lithographic techniques and microcontactprinting have been most widely used to gen-erate patterned droplets of cells.162–168 PEG hy-
THE BIOARTIFICIAL PANCREAS 977
FIG. 4. Schematic representation of an electrostaticdroplet generator.
6019_13_p968-985 12/21/05 3:09 PM Page 977
drogel is the most commonly used material forcell patterning purposes. In the case of surface-initiated photopolymerization of PEG, the tech-nique involves immobilization of initiator ontoa substrate surface using a stamp such aspoly(dimethyl siloxane), followed by polymer-ization of precursor solution.169 One recentstudy focused on the cellular delivery based onmicro- and nanotechnology.170 To provide animmunoisolating microenvironment for isletcells, nanoporous biocapsules were bulk andsurface micromachined to present uniform andwell-controlled pore sizes. The designs of themembranes with defined nanopores were fab-ricated using a thermally grown silicon oxidesandwiched between two structural layers ofsilicon.
Another technique used to generate dropletsof encapsulated islet cells was proposed byCruise et al.153 using interfacial photopolymer-ization. The technique involves physical ad-sorption of the initiator eosin Y on the islet cellsurface, which then allows polymerization tooccur on the islet–prepolymer interface. The in-terfacial photoinitiation process employed withthis technique results in conformal coating ofcross-linked PEG-based hydrogel on the isletcell surface.
The process of selective withdrawal is an-other novel method reported recently for thepurpose of coating cell clusters, such as isletcells.171 Briefly, the process involves the inser-tion of a tube into a container such that its tipis suspended at a specific height above an in-terface separating two immiscible fluids (Fig.5). In the case of a low fluid withdrawal rate,only the upper fluid (oil) is withdrawn throughthe tube. Increasing the fluid flow rate or de-
creasing the height of the tip above the inter-face results in a transition where the lower liq-uid (water) is incorporated in a thin spoutalong with the oil. The technique was demon-strated through encapsulation of a poppy seedin a poly(styrenesulfonic acid). The particleswere coated with the prepolymer solution,which has styrene sulfonic acid sodium saltand triethylene glycol diacrylate, and mixedwith the initiator eosin Y and co-initiator tri-ethanolamine used for the purpose of initiatingpolymerization.171 After the selective with-drawal step, the coated particles were collectedand photopolymerized with a halogen lamp.The technique could also be used to encapsu-late cells through surface initiated photopoly-merization of PEG. The photoinitiator eosin Ycould be immobilized on the islet cell surfacethrough covalent attachment,169 and after theselective withdrawal process, cells could be col-lected and illuminated for 2–3 min with an ar-gon ion laser in order to cross-link the coataround the cells.
CONCLUSIONS
The successful development of a bioartificialpancreas involves several considerations. Twomajor obstacles in islet transplantation are thelimited supply of islet cells and the use of im-munosuppressive drugs to prevent transplantrejection. It is hoped that the use of encapsu-lated islets as a form of bioartificial pancreaswould overcome these obstacles. Three poten-tial sources of islet cell tissue, including humanor allogeneic cells, porcine or xenogenic cells,and engineered cells, are currently under in-vestigation. Among these sources, human isletcells would be the least immunogenic; how-ever, there is a shortage of pancreata retrievedfrom human cadaveric donors, and these cellshave a limited secretory capacity and life span.The use of porcine islet cells could be a betteroption, because these are readily available, andthere is an unlimited supply of donors. How-ever, one major concern about the use of isletsharvested from pigs has been the possibility oftransmittance of porcine endogenous retro-viruses (PERVs) to humans during transplan-tation. This concept arose from studies on the
KIZILEL ET AL.978
Water
Oil
To pump
FIG. 5. Diagram of the selective withdrawal apparatus.
6019_13_p968-985 12/21/05 3:09 PM Page 978
infection of humans and immunodeficient miceafter pig cell xenotransplantation.172,173 Thereare studies, however, showing no possibility oftransmission of PERVs from pigs to human re-cipients of islet xenografts.120,174,175 Indeed, onerecent study showed that the porcine genomeharbors a limited number of infectious PERVsequences, which suggests that many breeds ofpig fail to produce PERVs capable of infectinghuman cells even in laboratory testing.176 Thisraises the possibility of using special breeds ofpig for an unlimited supply of islet cells for en-capsulation and use as a bioartificial pancreasin clinical xenotransplantation.
The other attractive approach to generate un-limited supply of islets is the use of embryonicstem cells, which have the ability to differenti-ate into a variety of cell lineages in vitro. Re-cent studies in small animals showing success-ful transplantation of pancreatic stem cellssuggest that this approach could provide anunlimited source of allogeneic insulin-produc-ing tissue in the future.177–179
The maintenance of cell viability is anotherimportant concern in the development of a suc-cessful bioartificial pancreas. When cells are en-capsulated and implanted in an environmentwithout a natural circulation, lack of an ade-quate supply of oxygen and nutrients results incell necrosis, making implantation unsuccess-ful. To improve long-term islet survival andfunction, vascularization of transplanted isletshas been proposed.180–182 An ideal architecturefor implantation would be to promote vascu-larization around encapsulated cells using anovel approach. Recently, a technique to formcovalently bonded multilayers of PEG hydro-gels has been developed. This approach maybe used to encapsulate cells with bilayers suchthat outer layer would promote vascularizationaround the inner layer.183,184
There are other areas of urgent need for thesuccessful development of a bioartificial pan-creas through islet cell microencapsulation. Allcurrent techniques for cell microencapsulationare slow in producing desirable microcapsules,requiring days to generate enough encapsu-lated islets for one transplantation.185 An idealprocedure for routine use of encapsulated isletswould require the development of massivelyparallel concepts in microencapsulation, which
would generate sufficient quantities of micro-capsules for multiple transplantations in a mat-ter of minutes. In the absence of a techniquebased on such a principle, there is a need foran adequate procedure for long-term storage ofencapsulated cells to enhance their use fortransplantation. It is also highly desirable to de-velop rapid in vitro techniques for determina-tion of the functional viability of encapsulatedislets prior to transplantation.
In summary, a potential cure for Type 1 di-abetes could be the use of bioartificial pancre-atic constructs based on insulin-secreting cells(allogeneic or xenogeneic islet cells) that are im-munoisolated with the microencapsulationtechnique. Additionally, enhanced survival ofthe graft might be supported with a novel ap-proach to induce neovascularization, whichcould make this technology a clinical reality inthe near future. This will in turn serve as animportant progress in cell therapy for the treat-ment of diabetes as well as other diseases, suchas cancer, hemophilia, liver failure, and Parkin-son’s disease.
REFERENCES
1. Kleinman JC, Donahue RP, Harris MI, Finucane FF,Madans JH, Brock DB: Mortality among diabetics ina national sample. Am J Epidemiol 1988;128:389–401.
2. Drury TF: Disability among adult diabetics. In: Na-tional Diabetes Group, eds. Diabetes in America: Di-abetes Data Compiled. Publication 85-1468. Bethesda,MD: National Diabetes Data Group, 1985.
3. World Health Organization: Definition, Diagnosisand Classification of Diabetes Mellitus and Its Com-plications. Report of a WHO Consultation. Geneva:World Health Organization, 1999.
4. Nathan DM: Long term complications of diabetesmellitus. N Engl J Med 1993;328:1676–1685.
5. Barrett-Connor E, Orchard T: Insulin-dependent di-abetes mellitus and ischemic heart disease. DiabetesCare 1985;8:65–70.
6. Barret-Conor E, Khaw KT: Diabetes mellitus and in-dependent risk factor for stroke. Am J Epidemiol1988;128:116–123.
7. Bild DE, Selby JV, Sinnock P, Browner WS, Brave-man P, Showstack JA: Lower extremity amputationin people with diabetes: epidemiology and preven-tion. Diabetes Care 1989;12:24–29.
8. Geiss LS, Herman WH, Teutsch SM: Diabetes andrenal mortality in the United States. Am J PublicHealth 1985;75:1325–1326.
THE BIOARTIFICIAL PANCREAS 979
6019_13_p968-985 12/21/05 3:09 PM Page 979
9. Moss SE, Klein R, Klein BE: The incidence of visionloss in a diabetic population. Ophthalmology 1988;95:1340–1348.
10. Rubin RJ, Altman WM, Mendelson DN: Health careexpenditures for people with diabetes mellitus. JClin Endocrinol Metab 1994;78:809A–809F.
11. Diabetes Control and Complications Trial ResearchGroup: The effect of intensive treatment of diabeteson the development and progression of long-termcomplications in insulin-dependent diabetes melli-tus. N Engl J Med 1993;329:977–986.
12. Ido Y, Vindignia A, Chang K, Stramm L, Chance R,Heath WF, DiMarchi RD, Di Cera E, Williamson JR:Prevention of vascular and neural dysfunction in di-abetic rats by C-peptide. Science 1997;277:563–566.
13. Johansson BL, Borg K, Fernqvist-Forbes E, KernellA, Odergren T, Wahren J: Beneficial effects of C-pep-tide on incipient nephropathy and neuropathy in pa-tients with Type 1 diabetes mellitus. Diabet Med2000;17:181–189.
14. Hansen A, Johansson BL, Wahren J, Bibra HV: C-peptide exerts beneficial effects on myocardial bloodflow and function in patients with Type 1 diabetes.Diabetes 2002;51:3077–3082.
15. Ekberg K, Brismar T, Johansson BL, Jonsson B, Lind-ström P, Wahren J: Amelioration of sensory nervedysfunction by C-peptide in patients with Type 1 di-abetes. Diabetes 2003;52:536–541.
16. Sutherland DE, Gruessner RW, Gruessner AC: Pan-creas transplantation for treatment of diabetes mel-litus. World J Surg 2001;25:487–496.
17. Venstrom JM, McBride MA, Rother KI, Hirshberg B,Orchard TJ, Harlan DM: Survival after pancreastransplantation in patients with diabetes and pre-served kidney function. JAMA 2003;290:2817–2823.
18. Sutherland DE, Stratta RJ, Gruessner AC: Pancreastransplant outcome by recipient category: singlepancreas versus combined kidney-pancreas. CurrOpin Organ Transplant 1998;3:231–241.
19. de Groot M, Schuurs TA, van Schilfgaarde R: Causesof limited survival of microencapsulated pancreaticislet grafts. J Surg Res 2004;121:141–150.
20. Kendall WFJ, Opara EC: Immunoisolation tech-niques for islet cell transplantation. Expert Opin BiolTher 2002;2:503–511.
21. Alejandro R, Feldman EC, Bloom AD, Kenyon NS:Effects of cyclosporin on insulin and C-peptide se-cretion in healthy beagles. Diabetes 1989;38:698–703.
22. Gunnarsson R, Klintmalm G, Lundgren G, WilczekH, Ostman J, Groth CG: Deterioration in glucose me-tabolism in pancreatic transplant recipients given cy-closporine. Lancet 1983;2:571–572.
23. Schlumpf R, Largiader F, Uhlschmid GK, Baum-gartner D: Is cyclosporine toxic for transplanted pan-creatic islets? Transplant Proc 1986;28:1169–1170.
24. Van Schilfgaarde R, van der Burg MPM, vanSuylichem HG, Goosen HG, Frolich M: Does cy-closporine influence beta cell function? TransplantProc 1986;28:1175–1176.
25. Shapiro AM, Lakey JR, Ryan EA, Korbutt GS, Toth E,Warnock GL, Kneteman NM, Rajotte RV: Islet trans-plantation in seven patients with Type I diabetesmellitus using a glucocorticoid-free immunosup-pressive regimen. N Engl J Med 2000;343:230–238.
26. Ryan EA, Lakey JRT, Paty BW, Imes S, Korbutt GS,Kneteman, NM, Bigam D, Rajotte RV, Shapiro AM:Successful islet transplantation: continued insulin re-verse provides long-term glycemic control. Diabetes2002;51:2148–2157.
27. Brunicardi FC, Mullen Y: Issues in clinical islet trans-plantation. Pancreas 1994;9:281–290.
28. De Vos P, Van Schilfgaarde R: Biocompatibility is-sues. In: Chick WL, ed. Cell Encapsulation Technol-ogy and Therapeutics. Boston: Birkhauser, 1999:63–79.
29. De Vos P, Van Straaten JF, Nieuwenhuizen AG, deGroot M, Ploeg RJ, De Haan BJ, Van Schlifgaarde R:Why do microencapsulated islet grafts fail in thepresence of fibrotic overgrowth? Diabetes 1999;48:1381–1388.
30. Ortiz C, Zhang D, Xie Y, Davisson VJ, Ben-AmotzD: Identification of insulin variants using Ramanspectroscopy. Anal Biochem 2004;332:245–252.
31. Lanza RP, Ecker DM, Kuhtreiber WM, Marsh JP,Ringeling J, Chick WL: Transplantation of islets us-ing microencapsulation: studies in diabetic rodentsand dogs. J Mol Med 1999;77:206–210.
32. Lim F, Sun AM: Microencapsulated islets as bioarti-ficial endocrine pancreas. Science 1980;210:908–910.
33. Soon-Shiong P, Heintz RE, Merideth N, Yao QX, YaoZW, Zheng TL, Murphy M, Moloney MK, SchmehlM, Harris M, Mendez R, Mendez R, Sandford PA:Insulin independence in a type I diabetic patient af-ter encapsulated islet transplantation. Lancet1994;343:950–951.
34. Zekorn TD, Horcher A, Siebers U, Federlin K, Bret-zel RG: Synergistic effect of microencapsulation andimmunoalteration on islet allograft survival in bioar-tificial pancreas. J Mol Med 1999;77:193–199.
35. Omer A, Keegan M, Czismadia E, De Vos P, VanRooijen N, Bonner-Weir S, Weir GC: Macrophage de-pletion improves survival of porcine neonatal pan-creatic cell clusters contained in alginate macrocap-sules transplanted into rats. Xenotransplantation2003;10:240–251.
36. de Vos P, Hamel AF, Tatarkiewicz K: Considerationsfor successful transplantation of encapsulated pan-creatic islets. Diabetologia 2002;45:159–173.
37. De Vos P, Vegter D, De Haan BJ, Strubbe JH, Brug-gink JE, Van Schilfgaarde R: Kinetics of intraperi-toneally infused insulin in rats. Functional implica-tions for the bioartificial pancreas. Diabetes 1996;45:1102–1107.
38. Kessler L, Jesser C, Lombard Y, Karsten V, BelcourtA, Pinget M, Poindron P: Cytotoxicity of peritonealmurine macrophages against encapsulated pancre-atic rat islets: in vivo and in vitro studies. J Leuk Biol1996;60:729–736.
KIZILEL ET AL.980
6019_13_p968-985 12/21/05 3:09 PM Page 980
39. Toso C, Oberholzer J, Ceausoglu I, Ris F, Rochat B,Rehor A, Bucher P, Wandrey C, Schuldt U, BelengerJ, Bosco D, Morel P, Hunkeler D: Intra-portal injec-tion of 400 � microcapsules in a large animal model.Transplant Int 2003;16:405–410.
40. Qian JH, Hashimoto T, Fujiwara H, Hamaoka T:Studies on the induction of tolerance of alloantigens.I. The abrogation of potentials for delayed-type-hy-persensitivity responses to alloantigens by portal ve-nous inoculations with allogeneic cells. J Immunol1985;134:3656–3661.
41. Alejandro R, Mintz DH, Noel J, Latif Z, Koh N, Rus-sell E, Miller J: Islet cell transplantation in Type I diabetes mellitus. Transplant Proc 1987;19:2359–2361.
42. Brendel MD, Hering B, Schultz AO, Bretzel RG: International Islet Transplant Registry. Newsletter 8. Giessen, Germany: Justus-Liebig-University ofGiessen, 1999.
43. Pfeiffer EF: Artificial pancreas, glucose sensors andthe impact upon diabetology. Int J Artif Organs1993;16:636–644.
44. Pfeiffer EF, Kerner W, Beischer W: Substitution ofislet cell function by mechanical device: extracorpo-real artificial pancreas. Adv Exp Med Biol 1979;119:501–508.
45. Kruse-Jarres JD, Braun G, Naegele R, Bresch M,Lehmann U: Blood glucose monitoring and com-puter regulation by means of an artificial endocrinepancreas. Horm Metab Res Suppl 1979;8:42–45.
46. Kerner W, Beischer W, Herfarth C, Pfeiffer EF: Ap-plication of an artificial endocrine pancreas in themanagement of the diabetic surgical patient. HormMetab Res Suppl 1979;8:159–161.
47. Hunkeler D: Allo transplants xeno: as bioartificial or-gans move to the clinic. Ann N Y Acad Sci 2001;944:1–6.
48. Encapsulation & immunoprotective strategies ofislet cells. Diabetes Technol Ther 2002;4:361.
49. Prokop A: Bioartificial pancreas: materials, devices,function and limitations. Diabetes Technol Ther2001;3:431–449.
50. Chang TMS: Semipermeable microcapsules. Science1964;146:524–525.
51. Sun AM, O’Shea GM, Goosen MF: Injectable mi-croencapsulated islet cells as bioartificial pancreas.Appl Biochem Biotechnol 1984;10:87–99.
52. Wiegand F, Kroncke KD, Kolb-Bachofen V: Macro-phage generated nitric-oxide as cytptoxic factor indestruction of alginate-encapsulated islets. Trans-plant Proc 1993;56:1206–1212.
53. Soon-Shiong P, Otterlie M, Skjak-Braek G, SmidsrodO, Heintz R, Lanza RP, Espevik T: An immunologicbasis for the fibrotic reaction to implanted micro-capsules. Transplant Proc 1991;23:758–759.
54. Strand BL, Ryan TL, In’t Veld P, Kulseng B, RokstadAM, Skjak-Brek G, Espevik T: Poly-L-lysine inducesfibrosis on alginate microcapsules via the inductionof cytokines. Cell Transplant 2001;10:263–275.
55. De Vos P, Wolters GHJ, Fritschy WM, Van Schilf-gaarde R: Obstacles in the application of microen-capsulation in islet transplantation. Int J Artif Organs1993;16:205–212.
56. Goosen MFA: In: Lanza RR, Chick WL, eds. Im-munoisolation of Pancreatic Islets. Austin, TX: R.G.Landes Co., 1994:21–44.
57. Soon-Shiong P, Feldman E, Nelson R, Heintz R, YaoQ, Yao Z, Zheng T, Merideth N, Skjak-Braek G, Es-pevik T, Smidsrod O, Sandford P: Long-term rever-sal of diabetes by the injection of immunoprotectedislets. Proc Natl Acad Sci U S A 1993;90:5843–5847.
58. Lanza R, Langer R, Chick WL: Principles of TissueEngineering, 2nd ed. Orlando, FL: Academic Press,2000.
59. Colton CK, Avgoustiniatos ES: Bioengineering in de-velopment of the hybrid artificial pancreas. J Bio-mech Eng 1991;113:152–170.
60. Brissova M, Lacik I, Powers AC, Anilkumar AV,Wang TG: Control and measurement of permeabil-ity for design of microcapsule cell delivery system.J Biomed Mater Res 1998;39:61–70.
61. Cole DR, Waterfall M, McIntyre M, Baird JD: Mi-croencapsulated islet grafts in the BB/E rat: a possi-ble role for cytokines in graft failure. Diabetologia1992;35:231–237.
62. Fan MY, Lum Z, Levesque L, Tai IT, Sun AM: Re-versal of diabetes in BB rats by transplantation of en-capsulated rat islets. Diabetes 1990;39:519–522.
63. Iwata H, Takagi T, Kobayashi K, Oka T, Tsuki T, ItoF: Strategy for developing microbeads applicable toislet xenotransplantation into a spontaneous diabeticNOD mice. J Biomed Mater Res 1994;28:1201–1207.
64. Lanza RR, Chick WL, eds.: Immunoisolation of Pan-creatic Islets. Austin, TX: R.G. Landes Co., 1994.
65. Lacik I, Brissova M, Anilkumar AV, Powers AC,Wang TG: New capsule with tailored properties forthe encapsulation of living cells. J Biomed Mater Res1998;39:52–60.
66. Lum ZP, Tai P, Krestow I, Tai T, Sun AM: Xenograftsof microencapsulated rat islets into diabetic mice.Transplant Proc 1992;53:1180–1183.
67. Iwata H, Murakami Y, Ikada Y: Control of comple-ment activities for immunoisolation. Ann N Y AcadSci 1999;875:7–23.
68. Paul LC: Mechanism of humoral xenograft rejection.In: Cooper DKC, Kemp E, Reemtsma K, White D,eds. Xenotransplantation. Berlin: Springer-Verlag,1991:47–67.
69. Auchincloss HJ, Moses R, Conti D, Sundt T, SmithC, Sachs DH, Winn HJ: Rejection of transgenic skinexpressing a xeno-class I antigen is CD4-dependentand CD8-independent. Transplant Proc 1990;22:1059–1060.
70. Sayegh MH, Watschinger B, Carpenter CB: Mecha-nisms of T cell recognition of alloantigen. The roleof peptides. Transplantation 1994;57:1295–1302.
71. Chen G, Hohmeier HE, Gasa R, Tran VV, NewgardCB: Selection of insulinoma cell lines with resistance
THE BIOARTIFICIAL PANCREAS 981
6019_13_p968-985 12/21/05 3:09 PM Page 981
to interleukin-1beta- and gamma-interferon-inducedcytotoxicity. Diabetes 2000;49:562–570.
72. Safley SA, Kapp LM, Tucker-Burden C, Hering B,Kapp JA, Weber CJ: Inhibition of cellular immuneresponses to encapsulated porcine islet xenograftsby simultaneous blockade of two different costimu-latory pathways. Transplantation 2005;79:409–418.
73. Rafael E, Wu GS, Hultenby K, Tibell A, WernersonA: Improved survival of macroencapsulated islets ofLangerhans by preimplantation of the immunoiso-lating device: a morphometric study. Cell Transplant2003;12:407–412.
74. Anderson JM: Inflammatory response to implants.ASAIO Trans 1988;34:101–107.
75. Anderson JM: Mechanisms of inflammation and in-fection with implanted devices. Cardiovasc Pathol1993;2(Suppl):33S–41S.
76. Anderson JM: Biocompatibility of tissue engineeredimplants. In: CW Patrick Jr, AG Mikos, LV McIntire,eds. Frontiers in Tissue Engineering. Oxford: Else-vier Science, 1998:152–165.
77. Bonner-Weir S, Sharma A: Pancreatic stem cells. JPathol 2002;197:519–526.
78. Lumelsky N, Blondel O, Laeng P, Velasco I, RavinR, McKay R: Differentiation of embryonic stem cellsto insulin-secreting structures similar to pancreaticislets. Science 2001;292:1389–1394.
79. Peck AB, Cornelius JG, Schatz D, Ramiya VK: Gen-eration of islets of Langerhans from adult pancreaticstem cells. J Hepatobil Pancreat Surg 2002;9:704–709.
80. Ramiya VK, Maraist M, Arfors KE, Schatz DA, PeckAB, Cornelius JG: Reversal of insulin-dependent di-abetes using islets generated in vitro from pancre-atic stem cells. Nat Med 2000;6:278–282.
81. Chen R, Meseck ML, Woo SL: Auto-regulated he-patic insulin gene expression in type I diabetic rats.Mol Ther 2001;3:584–590.
82. Lee HC, Kim SJ, Kim KS, Shin HC, Yoon JW: Re-mission in models of Type I diabetes by gene ther-apy using a single-chain insulin analogue. Nature2000;408:483–488.
83. Tang SC, Sambanis A: Development of geneticallyengineered human intestinal cells for regulated in-sulin secretion using rAAV-mediated gene transfer.Biochem Biophys Res Commun 2003;303:645–652.
84. Tang SC, Sambanis A: Preproinsulin mRNA engi-neering and its application to the regulation of in-sulin secretion from human hepatomas. FEBS Lett2003;537:193–197.
85. Thule PM, Liu JM: Regulated hepatic insulin genetherapy of STZ-diabetic rats. Gene Ther 2000;7:1744–1752.
86. Thule PM, Liu J, Philips LS: Glucose regulated pro-duction of human insulin in rat hepatocytes. GeneTher 2000;7:205–214.
87. Lumelsky N, Blondel O, Laeng P, Velasco I, RavinR, McKay R: Differentiation of embryonic stem cellsto insulin secreting structures similar to pancreatic-islets. Science 2001;292:1389–1394.
88. Hori Y, Rulifson IC, Tsai BC, Heit JJ, Cahoy JD, KimSK: Growth inhibitors promote differentiation of in-sulin-producing tissue from embryonic stem cells.Proc Natl Acad Sci U S A 2002;99:16105–16110.
89. Blyszczuk P, Czyz J, Kania G, Wagner M, Roll U, St-Onge L, Wobus AM: Expression of Pax4 in embry-onic stem cells promotes differentiation of nestin-positive progenitor and insulin-producing cells. ProcNatl Acad Sci U S A 2003;100:998–1003.
90. Moritoh Y, Yamato E, Yasui Y, Miyazaki S, MiyazakiJ: Analysis of insulin-producing cells during in vitrodifferentiation from feeder-free embryonic stemcells. Diabetes 2003;52:1163–1168.
91. Segev H, Fishman B, Ziskind A, Shulman M, It-skovitz-Eldor J: Differentiation of human embryonicstem cells into insulin-producing clusters. Stem Cells2004;22:265–274.
92. Hori Y, Gu X, Xie X, Kim SK: Differentiation of in-sulin-producing cells from human neural progenitorcells. PLoS Med 2005;2:e103.
93. Assady S, Maor G, Amit M, Itskovitz-Eldor J, Sko-recki KL, Tzukerman M: Insulin production by hu-man embryonic stem cells. Diabetes 2001;50:1691–1697.
94. Xu G, Stoffers DA, Habener JF, Bonner-Weir S: Ex-endin-4 stimulates both beta-cell replication andneogenesis, resulting in increased beta-cell mass andimproved glucose tolerance in diabetic rats. Diabetes1999;48:2270–2276.
95. Gromada J, Brock B, Schmitz O, Rorsman P:Glucagon-like peptide-1: regulation of insulin secre-tion and therapeutic potential. Basic Clin PharmacolToxicol 2004;95:252–262.
96. Harmon EB, Apelqvist AA, Smart NG, Gu X, Os-borne DH, Kim SK: GDF11 modulates NGN3� isletprogenitor cell number and promotes beta-cell dif-ferentiation in pancreas development. Development2004;131:6163–6174.
97. Bach JF: Immunotherapy of insulin-dependent dia-betes mellitus. Curr Opin Immunol 2001;13:601–605.
98. Giannoukakis N, Rudert WA, Robbins PD, TruccoM: Targeting autoimmune diabetes with gene ther-apy. Diabetes 1999;48:2107–2121.
99. Docherty K: Gene therapy for diabetes mellitus. ClinSci (Lond) 1997;92:321–330.
100. Soria B, Skoudy A, Martin F: From stem cells to betacells: new strategies in cell therapy of diabetes mel-litus. Diabetologia 2001;44:407–415.
101. Selden RF, Skoskiewicz MJ, Russell PS, GoodmanHM: Regulation of insulin-gene expression. Impli-cations for gene therapy. N Engl J Med 1987;317:1067–1076.
102. Newgard CB: Cellular engineering and gene therapystrategies for insulin replacement in diabetes. Dia-betes 1994;43:341–350.
103. Halban PA, Kahn SE, Lernmark A, Rhodes CJ: Geneand cell-replacement therapy in the treatment oftype 1 diabetes: how high must the standards be set?Diabetes 2001;50:2181–2191.
KIZILEL ET AL.982
6019_13_p968-985 12/21/05 3:09 PM Page 982
104. Sapir T, Shternhall K, Meivar-Levy I, Blumenfeld T,Cohen H, Skutelsky E, Eventov-Friedman S, Bar-shack I, Goldberg I, Pri-Chen S, Ben-Dor L, Polak-Charcon S, Karasik A, Shimon I, Mor E, Ferber S:Cell-replacement therapy for diabetes: generatingfunctional insulin-producing tissue from adult human liver cells. Proc Natl Acad Sci U S A2005;102:7964–7969.
105. Fujita Y, Cheung AT, Kieffer TJ: Harnessing the gutto treat diabetes. Pediatr Diabetes 2004;5:57–69.
106. Cheung AT, Dayanandan B, Lewis JT, Korbutt GS,Rajotte RV, Bryer-Ash M, Boylan MO, Wolfe MM,Kieffer TJ: Glucose-dependent insulin release fromgenetically engineered K cells. Science 2000;290:1959–1962.
107. El-Shewy HM, Kendall WFJ, Darrabie M, Collins BH,Opara EC: Polyvinyl pyrrolidone: a novel cryopro-tectant in islet cell cryopreservation. Cell Transplant2004;13:237–243.
108. Zimmermann H, Katsen AD, Ihmig FR, Durst CHP,Shirley SG, Fuhr GR: First steps of an interdiscipli-nary approach towards miniaturised cryopreservationfor cellular nanobiotechnology. IEE Proc Nanobio-technol 2004;151:134–138.
109. Zimmermann H, Zimmermann D, Reuss R, FeilenPJ, Manz B, Katsen A, Weber M, Ihmig FR, EhrhartF, Gessner P, Behringer M, Steinbach A, Wegner LH,Sukhorukov VL, Vasquez JA, Schneider S, WeberMM, Volke F, Wolf R, Zimmermann U: Towards amedically approved technology for alginate-basedmicrocapsules allowing long-term immunoisolatedtransplantation. J Mater Sci Mater Med 2005;16:491–501.
110. Misler S, Dickey A, Barnett DW: Maintenance ofstimulus-secretion coupling and single beta-cellfunction in cryopreserved-thawed human islets ofLangerhans. Pflugers Arch 2005;450:395–404.
111. von Mach MA, Schlosser J, Weiland M, Feilen PJ,Ringel M, Hengstler JG, Weilemann LS, Beyer J,Kann P, Schneider S: Size of pancreatic islets ofLangerhans: a key parameter for viability after cry-opreservation. Acta Diabetol 2003;40:123–129.
112. Lanza RP, Chick WL: Transplantation of encapsu-lated cells and tissues. Surgery 1997;121:1–9.
113. Lanza RP, Chick WL: Immunoisolation strategies forthe transplantation of pancreatic islets. Ann N YAcad Sci 1997;831:323–331.
114. Wang TG: Progress in bioartificial pancreas. J RegenMed 2000;1:93–98.
115. Jain K, Yang H, Cai BR, Haque B, Hurvitz AI, DiehlC, Miyata T, Smith BH, Stenzel K, Suthanthiran M: Re-trievable, replaceable, macroencapsulated pancreaticislet xenografts. Long-term engraftment without im-munosuppression. Transplantation 1995;59:319–324.
116. Trivedi N, Keegan M, Steil GM, Hollister-Lock J,Hasenkamp WM, Colton CK, Bonner-Weir S, WeirGC: Islets in alginate macrobeads reverse diabetesdespite minimal acute insulin secretory responses.Transplantation 2001;71:203–211.
117. Lacy PE, Hegre OD: Maintenance of normoglycemiain diabetic mice by subcutaneous xenografts of en-capsulated islets. Science 1991;254:1782–1784.
118. Scharp DW, Swanson CJ, Olack BJ, Latta PP, HegreOD, Doherty EJ, Gentile FT, Flavin KS, Ansara MF,Lacy P: Protection of encapsulated human islets im-planted without immunosuppression in patientswith type I or type II diabetes and in nondiabeticcontrol subjects. Diabetes 1994;43:1167–1170.
119. van Suylichem PT, Strubbe JH, Houwing H, WoltersGH, van Schilfgaarde R: Insulin secretion by rat isletisografts of a defined endocrine volume after trans-plantation to three different sites. Diabetologia1992;35:917–923.
120. Elliott RB, Escobar L, Garkavenko O, Croxson MC,Schroeder BA, McGregor M, Ferguson G, BeckmanN, Ferguson S: No evidence of infection with porcineendogenous retrovirus in recipients of encapsulatedporcine islet xenografts. Cell Transplant 2000;9:895–901.
121. Sun YL, Ma X, Zhou D, Vacek I, Sun AM: Normal-ization of diabetes in spontaneously diabeticcynomologus monkeys by xenografts of microen-capsulated porcine islets without immunosuppres-sion. J Clin Invest 1996;98:1417–1422.
122. Kendall WF, Collins BH, Hobbs HA, Bollinger RR,Opara EC: Long-term normoglycemia induced bymicroencapsulated porcine islet xenotransplantationin a diabetic baboon [abstract]. Acta Chir Austriaca2001;33(Suppl 174):56.
123. Soon-Shiong P, Feldman E, Nelson R, KomtebeddeJ, Smidsrod O, Skjak-Braek G, Espevik T, Heintz R,Lee M: Successful reversal of spontaneous diabetesin dogs by intraperitoneal microencapsulated islets.Transplantation 1992;54:769–774.
124. Sun Y, Ma X, Zhou D, Vacek I, Sun AM: Normaliza-tion of diabetes in spontaneously diabetic cynomol-ogous monkeys by xenografts of microencapsulatedporcine islets without immunosuppression. J Clin In-vest 1996;98:1417–1422.
125. Uludag H, De Vos P, Tresco PA: Technology ofmammalian cell encapsulation. Adv Drug Deliv Rev2000;42:29–64.
126. Pollok JM, Kolin PA, Lorenzen M, Torok E, Kauf-mann PM, Kluth D, Bohuslavizki KH, Gundlach M,Rogiers X: Islets of Langerhans encapsulated with atissue engineered membrane of rat chondrocytesmaintain insulin secretion and glucose insulin feed-back for at least 30 days in culture. Transplant Proc2001;33:1713–1714.
127. Sandler S, Andersson A, Eizirik DL, Hellerstrom C,Espevik T, Kulseng B, Thu B, Pipeleers DG, Skjak-Braek G: Assessment of insulin secretion in vitrofrom microencapsulated fetal porcine islet like cellclusters and rat, mouse, and human pancreatic islets.Transplantation 1997;63:1712–1718.
128. Halle JP, Leblond FA, Pariseau JF, Jutras P, BrabantMJ, Lepage Y: Studies on small (�300 microns) mi-crocapsules: II—Parameters governing the produc-
THE BIOARTIFICIAL PANCREAS 983
6019_13_p968-985 12/21/05 3:09 PM Page 983
tion of alginate beads by high voltage electrostaticpulses. Cell Transplant 1994;3:365–372.
129. Duvivier-Kali VF, Omer A, Parent RJ, O’Neil JJ, WeirGC: Complete protection of islets against allorejec-tion and autoimmunity by a simple barium alginatemembrane. Diabetes 2001;50:1698–1705.
130. Klock G, Frank H, Houben R, Zekorn T, Horcher A,Siebers U, Wöhrle M, Federlin K, Zimmermann U:Production of purified alginates suitable for use inimmunoisolated transplantation. Appl MicrobiolBiotechnol 1994;40:638–643.
131. Kulseng B, Thu T, Espevik T, Skjk-Brk G: Alginatepoly-lysine microcapsules as immune barrier: per-meability of cytokines and immunoglobins over thecapsule membrane. Cell Transplant 1997;6:387–394.
132. Sawhney AS, Hubbell JA: Poly(ethylene oxide)-graft-poly(L-lysine) copolymers to enhance the bio-compatibility of poly(L-lysine)-alginate microcap-sule membranes. Biomaterials 1992;13:863–870.
133. Lim F: Microencapsulation of living mammaliancells. Adv Biotechnol Processes 1988;7:185–197.
134. Smidsrod O, Skjak-Braek G: Alginate as immobi-lization matrix for cells. Trends Biotechnol 1990;8:71–78.
135. Prokop A, Wang TG: Purification of polymers usedfor fabrication of an immunoisolation barrier. AnnN Y Acad Sci 1997;831:223–231.
136. Zekorn T, Klock G, Horcher A, Siebers U, Wohrle M,Kowalski M, Arnold M, Federlin K, Bretzel R, Zim-mermann U: Lymphoid activation by different crudealginates and the effect of purification. TransplantProc 1992;24:2952–2953.
137. Ricker A, Stockberger S: Hyperimmune response tomicroencapsulated xenogeneic tissue in NOD mice[abstract]. Diabetes 1986;35:61A.
138. Garfinkel MR, Harland RC, Opara EC: Optimizationof the microencapsulated islet for transplantation. JSurg Res 1998;76:7–10.
139. Ar’Rajab A, Bengmark S, Ahren B: Insulin secretionin streptozotocin-diabetic rats transplanted with im-munoisolated islets. Transplantation 1991;51:571–574.
140. Calafiore R, Calcinaro F, Basta G, Pietropoalo M,Falorni A, Piermattei M, Brunetti P: A method forthe massive separation of highly purified, adultporcine islets of Langerhans. Metabolism 1990;39:175–181.
141. Carani BS, Edwin G, eds.: Annals of the New YorkAcademy of Sciences, Vol. 1037: Immunology of Di-abetes III. New York: New York Academy of Sci-ences, 2005.
142. Mazaheri R, Atkison P, Stiller C, Dupre J, Vose J,O’Shea G: Transplantation of encapsulated allo-geneic islets into diabetic BB/W rats. Effects of im-munosuppression. Transplantation 1991;51:750–754.
143. Sefton MV, Stevenson WTK: Microencapsulation oflive animal cells using polyacrylates. Adv Polym Sci1993;107:145–198.
144. Dupuy B, Gin H, Baquey C, Ducassou D: In situpolymerization of a microencapsulating medium
round living cells. J Biomed Mater Res 1988;22:1061–1070.
145. Gin H, Dupuy B, Baquey C, Ducassou D, AubertinJ: Agarose encapsulation of islets of Langerhans: re-duced toxicity in vitro. J Microencapsul 1987;4:239–242.
146. Takagi T, Iwata H, Tashiro H, Tsuji T, Ito F: Devel-opment of a novel microbead applicable to xeno-geneic islet transplantation. J Control Rel 1994;31:283–291.
147. Iwata H, Murakami Y, Ikada Y: Control of comple-ment activities for immunoisolation. Ann N Y AcadSci 1999;875:7–23.
148. Deppsich R, Goehl H, Ritz E, Haensch GM: Com-plement activation on artificial surfaces in biomed-ical therapies. In: Rother K, Till GO, Hänsch GM, eds.The Complement System, 2nd ed. Berlin: Springer-Verlag, 1998, pp. 487–504.
149. Pangburn MK: Alternative pathway: activation andregulation. In: Rother K, Till GO, Hänsch GM, eds.The Complement System, 2nd ed. Berlin: Springer-Verlag, 1998:93–115.
150. Chaikof EL: Engineering and material considera-tions in islet cell transplantation. Annu Rev BiomedEng 1999;1:103–127.
151. Shoichet MS, Winn SR, Gentile FT, Athavale S, Har-ris JM: Poly(ethylene oxide) grafted thermoplasticmembranes for use as cellular hybrid bioartificial or-gans in the central nervous system. Biotechnol Bio-engin 1994;43:563–572.
152. Pathak CP, Sawhney AS, Hubbell JA: Rapid pho-topolymerization of immunoprotective gels in con-tact with cells and tissue. J Am Chem Soc 1992;114:8311–8312.
153. Cruise GM, Hegre OD, Scharp DS, Hubbell JA: Asensitivity study of the key parameters in the inter-facial photopolymerization of poly(ethylene glycol)diacrylate upon porcine islets. Biotechnol Bioengin1998;57:655–665.
154. Harris JM: Poly(ethylene Glycol) Chemistry: Bio-technical and Biomedical Applications. New York:Plenum Press, 1992.
155. Sawhney AS, Pathak CP, Hubbell JA: Bioerodiblehydrogels based on photopolymerized poly(ethyl-ene glycol)-co-poly(�-hydroxy acid) diacrylatemacromers. Macromolecules 1993;26:581–587.
156. Cruise GM, Scharp DS, Hubbell JA: Characterizationof permeability and network structure of inter-facially photopolymerized poly(ethylene glycol) diacrylate hydrogels. Biomaterials 1998;19:1287–1294.
157. Wolters GH, Fritschy WM, Gerrits D, Van Schilf-gaarde R: A versatile alginate droplet generator ap-plicable for microencapsulation of pancreatic islets.J Appl Biomater 1992;3:281–286.
158. Opara EC: The therapeutic potential of islet celltransplants in the treatment of diabetes. Expert OpinInvest Drugs 1998;7:1–11.
159. Hobbs H, Kendall W, Darrabie M, Collins B, BridgesS, Opara EC: Substitution of polyornithine for
KIZILEL ET AL.984
6019_13_p968-985 12/21/05 3:09 PM Page 984
polylysine in alginate microcapsules [abstract]. Dia-betes 2000;49:A111.
160. Hommel M, Sun AM, Goosen MFA, inventors; Con-naught Laboratories Limited, assignee: Droplet gen-eration. US Patent 4,956,128. September 11, 1990.
161. Sundberg C: High-throughput and ultra-high-throughput screening: solution- and cell-based ap-proaches. Curr Opin Biotechnol 2000;11:47–53.
162. Kane RS, Takayama S, Ostuni E, Ingber DE, White-sides GM: Patterning proteins and cells using softlithography. Biomaterials 1999;20:2363–2376.
163. Singhvi R, Kumer A, Lopez GP, Stephanopoulos GN,Wang DIC, Whitesides GM, Ingber DE: Engineeringcell shape and function. Science 1994;264:696–698.
164. Amirpour ML, Ghosh P, Lackowski WM, CrooksRM, Pishko MV: Mammalian cell cultures on mi-cropatterned surfaces of weak-acid, polyelectrolytehyperbranched thin films on gold. Anal Chem2001;73:1560–1566.
165. Chen CS, Mrksich M, Huang S, Whitesides GM, In-gber DE: Micropatterned surfaces for control of cellshape, position, and function. Biotechnol Prog1998;14:356–363.
166. Ito Y: Surface micropatterning to regulate cell func-tions. Biomaterials 1999;20:2333–2342.
167. Koh W, Revzin A, Simonian A, Reeves T, Pishko M:Control of mammalian cell and bacteria adhesion onsubstrates micropatterned with poly(ethylene gly-col) hydrogels. Biomed Microdev 2003;5:11–19.
168. Matsuda T, Sugawara T: Development of surfacephotochemical modification method for micropat-terning of cultured cells. J Biomed Mater Res1995;29:749–756.
169. Kizilel S, Perez-Luna VH, Teymour F: Photopoly-merization of poly(ethylene glycol) diacrylate oneosin-functionalized surfaces. Langmuir 2004;20:8652–8658.
170. Desai TA, West T, Cohen M, Boiarski T, RampersaudA: Nanoporous microsystems for islet cell replace-ment. Adv Drug Deliv Rev 2004;56:1661–1673.
171. Cohen I, Li H, Hougland JL, Mrksich M, Nagel SR:Using selective withdrawal to coat microparticles.Science 2001;292:265–267.
172. Patience C, Takeuchi Y, Weiss RA: Infection of hu-man cells by an endogeneous retrovirus of pigs. NatMed 1997;3:282–286.
173. van der Laan LJW, Lockey C, Griffeth BC, Frasier FS,Wilson CA, Onions DE, Hering BJ, Long Z, Otto E,Torbett BE, Salomon DR: Infection by porcine endo-geneous retrovirus after islet xenotransplantation inSCID mice. Nature 2000;407:90–94.
174. Heneine W, Tibell A, Switzer WM, Sandstrom P,Rosales GV, Mathews A, Korsgren O, Chapman LE,Folks TM, Groth CG: No evidence of infection withporcine endogeneous retrovirus in recipients ofporcine islet-cell xenografts. Lancet 1998;352:695–699.
175. Paradis K, Langford G, Long Z, Heneine W, Sand-strom P, Switzer WM, Chapman LE, Lockey C,Onions D, Otto E: Search for cross species transmis-
sion of porcine endogeneous retrovirus in patientstreated with living pig tissue. The XEN 111 StudyGroup. Science 1999;285:1236–1241.
176. Niebert M, Rogel-Gaillard C, Chardon P, Tonjes RR:Characterization of chromosomally assigned repli-cation-component gamma porcine endogenousretroviruses derived from a large white pig and ex-pression in human cells. J Virol 2002;76:2714–2720.
177. Soria B, Roche E, Berna G, Leon-Quinto T, Reig JA,Martin F: Insulin secreting cells derived from embry-onic stem cells normalize glycemia in streptozotocininduced diabetic mice. Diabetes 2000;49:157–162.
178. Soria B, Andreu E, Berna G, Fuentes E, Gil A, Leon-Quinto T, Martin F, Montanya E, Nadal A, Reig JA,Ripoll C, Roche E, Sanchez-Andres JV, Segura J: En-gineering pancreatic islets. Pflugers Arch 2000;440:1–18.
179. Ramiya VK, Maraist M, Arfors KE, Schatz DA, PeckAB, Cornelius JG: Reversal of insulin dependent di-abetes using islets generated in vitro from pancre-atic stem cells. Nat Med 2000;6:278–282.
180. Zhang N, Richter A, Suriawinata J, Harbaran S, Al-tomonte J, Cong L, Zhang H, Song K, Meseck M,Bromberg J, Dong H: Elevated vascular endothelialgrowth factor production in islets improves isletgraft vascularization. Diabetes 2004;53:963–970.
181. Sigrist S, Mechine-Neuville A, Mandes K, CalendaV, Braun S, Legeay G, Bellocq JP, Pinget M, KesslerL: Influence of VEGF on the viability of encapsulatedpancreatic rat islets after transplantation in diabeticmice. Cell Transplant 2003;12:627–635.
182. Narang AS, Cheng K, Henry J, Zhang C, Sabek O,Fraga D, Kotb M, Gaber AO, Mahato RI: Vascularendothelial growth factor gene delivery for revascu-larization in transplanted human islets. Pharm Res2004;21:15–25.
183. Kizilel S: Theoretical and experimental investigationfor interfacial photopolymerization of poly(ethyleneglycol) diacrylate [Ph.D. thesis]. Chicago: BiomedicalEngineering, Illinois Institute of Technology, 2004.
184. Kizilel S, Sawardecker E, Teymour F, Perez-LunaVH: Sequential formation of covalently bonded hy-drogel multilayers through surface initiated pho-topolymerization. Biomaterials 2005 Sept 10 [Epubahead of print].
185. De Vos P, De Haan BJ, Van Schilfgaarde R: Upscal-ing the production of microencapsulated pancreaticislets. Biomaterials 1997;18:1085–1090.
Address reprint requests to:Emmanuel C. Opara, Ph.D.
Pritzker Institute of Biomedical Science &Engineering
Illinois Institute of Technology10 West 32nd Street, E1-116
Chicago, IL 60616
E-mail: [email protected]
THE BIOARTIFICIAL PANCREAS 985
6019_13_p968-985 12/21/05 3:09 PM Page 985