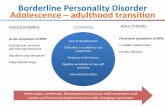
Screening for Borderline Personality Disorder in Outpatient Youth
Transcript of Screening for Borderline Personality Disorder in Outpatient Youth
Journal of Personality Disorders, 22(4), 353–364, 2008 2008 The Guilford Press
SCREENING FOR BORDERLINE PERSONALITYDISORDER IN OUTPATIENT YOUTH
Andrew M Chanen, MBBS, MPM, FRANZCP,Martina Jovev, PhD, Danica Djaja, BmedSci,Emma McDougall, BSc, Hok Pan Yuen, MSc,David Rawlings, DPhil, and Henry J Jackson, PhD, FAPS
Young people with borderline personality disorder (BPD) commonlyseek help but often go unrecognized. Screening offers a means of identi-fying individuals for more detailed assessment for early interventionand for research. Aims: This study compared the McLean Screening In-strument for Borderline Personality Disorder (MSI-BPD), BorderlinePersonality Questionnaire (BPQ), the BPD items from the InternationalPersonality Disorder Examination Screening Questionnaire and theBPD items from the Structured Clinical Interview for DSM-IV Axis IIdisorders (SCID-II) Personality Questionnaire. Method: 101 outpatientyouth (aged 15–25 years) completed the screening measures and wereinterviewed, blind to screening status, with the SCID-II BPD module.The screening measures were readministered two weeks later to assesstest-retest reliability. Results: All four instruments performed similarlybut the BPQ had the best mix of characteristics, with moderate sensi-tivity (0.68), the highest specificity (0.90), high negative predictive value(0.91) and moderate positive predictive value (0.65). Compared to theother three instruments, the BPQ had the highest overall diagnostic ac-curacy (0.85), a substantially higher kappa (0.57) with the criterion di-agnosis, the highest test-retest reliability (ICC = 0.92) and the highest in-ternal consistency (α = 0.92). The only clear difference to emerge in theReceiver Operator Curve (ROC) analysis was that the BPQ significantlyoutperformed the MSI (p = 0.05). Conclusion: Screening for BPD in out-patient youth is feasible but is not a replacement for clinical diagnosis.
Borderline personality disorder (BPD) usually emerges during adolescenceand is associated with serious morbidity, such as mood, anxiety, and sub-stance use disorders, along with severe impairment of psychosocial func-
From The ORYGEN Research Centre, Department of Psychiatry, University of Melbourne,Melbourne, Australia (A. M. C., M. J., D. D., E. M., H. P. Y.); ORYGEN Youth Health, Mel-bourne, Australia (A. M. C.); and The School of Behavioral Science, The University of Mel-bourne, Melbourne, Australia (D. R., H. J. J.).
The authors thank all participants in this study and the staff of ORYGEN Youth Health.Thanks also to Dr. Louise McCutcheon for training and supervision of the diagnostic assess-ments. The ORYGEN Research Centre is supported by funding from the Colonial Foundation,Melbourne, Australia.
Address correspondence to Dr Andrew M Chanen, ORYGEN Research Centre, Locked Bag10, Parkville, Victoria, Australia 3052; E-mail: [email protected]
353
354 CHANEN ET AL.
tioning (Chanen, Jovev, & Jackson, 2007). A substantial body of evidenceindicates that BPD diagnostic criteria are no less reliable, valid, and stableprior to age eighteen years than they are in adulthood (Chanen et al.,2004; Chanen, Jovev, & Jackson, 2007; Westen, Shedler, Durrett, Glass,& Martens, 2003). BPD affects 0.9% (Lewinsohn, Rohde, Seeley, & Klein,1997) to 3% (Bernstein et al., 1993) of community-dwelling teenagers (sim-ilar to the prevalence in adults; Lenzenweger, Lane, Loranger, & Kessler,2007) but this rises to 10.8% (Bernstein et al., 1993) to 14% (Chabrol,Montovany, Chouicha, Callahan, & Mullet, 2001) if lower symptom thresh-olds are used. In clinical samples, the limited data suggest a prevalence of11% in adolescent outpatients (Chanen et al., 2004), 49% in adolescentinpatients (Grilo, Becker, Fehon, et al., 1996) and 42% in young adult in-patients (Grilo, Becker, Edell, & McGlashan, 1996).
Adolescents and young adults with BPD commonly seek help (Chanen,Jovev, et al., 2007; Zanarini, Frankenburg, Khera, & Bleichmar, 2001).However, they often go unrecognized (Chanen, Jovev, et al., 2007), in partbecause personality disorder (PD) diagnosis is seen as controversial priorto age eighteen (Paris, 2003) and is often discouraged. Consequently,many clinicians lack training or experience in making PD diagnoses inthis age group. However, BPD traits also show considerable flexibility andmalleability in young people (Lenzenweger & Castro, 2005), making this akey period in which to intervene.
We have previously concluded that the available evidence supports thedevelopment and evaluation of early intervention programs for BPD inyouth (Chanen, McCutcheon, Jovev, Jackson, & McGorry, 2007). How-ever, recognition of the disorder, especially in adolescent clinical services,presents a significant barrier to the development of such programs. Theuse of a screening measure offers a means of drawing clinicians’ attentionto the diagnosis in young people and also a potentially efficient means ofidentifying individuals for more detailed assessment for early interventionprograms and for research. Screening, however, is not a replacement forrigorous diagnosis.
Screening usually involves a trade off between sensitivity (the true posi-tive rate) and specificity (the true negative rate). For screening in outpa-tient youth, a desirable test would have high sensitivity and a high nega-tive predictive value (NPV; probability that a negative test means theperson does not have the condition). In other words, it would detect nearlyall the “true” cases of BPD and when the test is negative, one could beconfident that a person does not have BPD. However, one possible cost ofthis approach might be tolerating a low positive predictive value (PPV; highfalse positive rate).
There are numerous interview and self-report screening tools for PDs(Morse & Pilkonis, 2007) but fewer specifically for BPD (Poreh et al., 2006).Some investigators have used BPD scales derived from the items in generalscreening measures for PDs (e.g., Patrick, Links, Van Reekum, & Mitton,1995; Trull, 1995), while others have developed measures specifically forBPD (e.g., Leichsenring, 1999; Poreh et al., 2006; Zanarini et al., 2003).
SCREENING FOR BPD 355
Also, studies are not always directly comparable, as they have used vari-ous definitions of BPD for their criterion diagnosis, including different ver-sions of the DSM, the ICD, and Kernberg’s Borderline Personality Organi-zation (Kernberg, 1986). Moreover, it is possible that these criteriondiagnoses will also vary according to the instruments used to measurethem.
Of the instruments designed to measure DSM-IV BPD, the McLeanScreening Instrument for Borderline Personality Disorder (MSI-BPD;Zanarini et al., 2003) and the Borderline Personality Questionnaire (BPQ;Poreh et al., 2006) have shown particular promise in screening for youthwith DSM-IV BPD but neither has been evaluated in psychiatric outpa-tients. This report examines the performance of four candidate screeningmeasures for BPD in a sample of outpatient youth (aged 15–25 years),against a criterion diagnosis of Structured Clinical Interview for DSM-IVAxis II disorders (SCID-II; First, Gibbon, Spitzer, Williams, & Benjamin,1997) BPD.
METHODPARTICIPANTS
The study took place at ORYGEN Youth Health, the government-funded,youth (aged 15–24) mental health service for western metropolitan Mel-bourne, Australia. Exclusion criteria for the study included: (1) intellectualdisability; (2) substance intoxication or withdrawal on the day of the proce-dure and (3) meeting criteria for ORYGEN’s first episode psychosis service,the Early Psychosis Prevention and Intervention Centre (EPPIC; McGorry,Edwards, Mihalopoulos, Harrigan, & Jackson, 1996).
Of 238 referrals to ORYGEN, 89 (37.4%) could not be located for re-search interview, 4 (1.7%) had moved away from the service, 24 (10.1%)refused to participate, 5 were not approached for clinical reasons (2.1%),and 1 (0.4%) was excluded for intellectual disability. After complete de-scription of the study to the participants, written informed consent wasobtained from 115 participants (48.3%) or from their parent or guardian,where appropriate. Fourteen participants (5.9% of referrals) could not belocated subsequently, leaving 101 participants available for the analysis.
Seventy-three (72.3%) participants were female. The mean age of thesample was 18.8 years (SD = 2.8; range 15–25). Twenty-two participants(21.8%) met DSM-IV criteria for BPD ( ≥ 5 BPD criteria). The most commonAxis I diagnoses in the sample were mood disorders (n = 56), anxiety disor-ders (n = 52), substance dependence (n = 21) and eating disorders (n = 19).
MEASURESScreening Measures. The MSI-BPD (Zanarini et al., 2003) is a ten-item
screening measure specifically for BPD. The questions are based upon asubset of the questions that comprise the borderline module of the Diag-nostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini,
356 CHANEN ET AL.
Frankenburg, Sickel, & Yong, 1996). It includes eight items for each of thefirst eight DSM-IV criteria for BPD and two items for the ninth criterionof paranoia/dissociation. In a sample of adults with treatment historiesresponding to advertisements, the MSI-BPD had good sensitivity (0.81)and specificity (0.85) against a criterion diagnosis of DIPD BPD. Encourag-ingly, for the aims of the present study, in post hoc analyses of participantsaged 18–25 years, these figures rose to 0.9 (sensitivity) and 0.93 (specific-ity). Predictive values, accuracy and Cohen’s Kappa are not reported byZanarini and colleagues but can be calculated for the overall sample of200 from the data provided (PPV 0.93; NPV 0.67; accuracy 0.83; kappa0.62). Internal consistency of the MSI was found to be acceptable (α =0.74).
The BPQ (Poreh et al., 2006) is an 80-item true/false self-report measurecomprising nine subscales corresponding to the nine DSM-IV BPD criteria.These are labeled impulsivity (9 items), affective instability (10 items),abandonment (10 items), unstable relationships (8 items), self-image (9items), self-mutilation (7 items), emptiness (10 items), intense anger (10items) and quasi-psychotic states (7 items). The BPQ’s psychometric prop-erties were established using four normal samples, with mean ages from19.32 years (SD = 2.91) to 21.73 years (SD = 5.81). The BPQ has high in-ternal consistency (Kuder-Richardson coefficient = 0.94) and convergentvalidity with the MMPI-2 BPD scale (r = 0.85), along with satisfactory crite-rion validity (tau = 0.51) using the Diagnostic Interview for Borderline Pa-tients (Gunderson, Kolb, & Austin, 1981).
In addition, the BPD items from the screening questionnaires for twoother common semi-structured interviews for PD were chosen, the Inter-national Personality Disorder Examination Screener (IPDE-S; Loranger,1999) and the Structured Clinical Interview for DSM-IV Axis II PersonalityQuestionnaire (SCID-II PQ; First et al., 1997), the latter of which ismatched to the SCID-II which was used as the criterion diagnosis for thepresent study.
The IPDE-S contains nine BPD items (IPDE-BPD), corresponding to eachof the nine DSM-IV BPD criteria, in a true/false response format. TheSCID-II PQ contains fifteen BPD items (SCID-II PQ-BPD) in a yes/no re-sponse format, corresponding to the nine DSM-IV BPD criteria. EachDSM-IV criterion has one question, except for criteria three (identity distur-bance, four questions), five (recurrent suicidal behavior, two questions) andeight (inappropriate anger, three questions). Psychometric data are notavailable for the IPDE-BPD or SCID-II PQ-BPD used as stand alone screen-ing instruments.
DIAGNOSTIC INTERVIEW
Axis I diagnoses were obtained using the Structured Clinical Interview forDSM-IV axis I disorders-patient version (SCID-I/P; First, Gibbon, Spitzer,& Williams, 1996).
The SCID-II is a 120-item semi-structured interview which assesses for
SCREENING FOR BPD 357
all DSM-IV PDs. In the present study, the BPD module was administeredblind to screening status. In the SCID-II, each DSM-IV PD item is scoredon a three-point scale (1 = absent, 2 = subthreshold or 3 = present). Incommon with previous literature (Bernstein, Cohen, Skodol, Bezirganian, &Brook, 1996), a PD feature was scored positive if it was present for two yearsand did not occur exclusively during an axis I disorder. This is one yearlonger than that required for adolescents in the DSM-IV. A score of three onat least five out of nine BPD items was required for a diagnosis of BPD.
PROCEDURE
The study was approved by the Northwestern Mental Health Research andEthics Committee. After complete description of the study to the partici-pants, written informed consent was obtained from participants or from aparent or guardian, where appropriate. All participants were remuneratedAU$35 to cover expenses.
Participants completed the first set of questionnaires and two semi-struc-tured interviews (SCID-I/P and SCID-II). The self-report questionnaires werereadministered to all participants two weeks after (mean duration = 13.7days, SD = 15.5) their initial assessment. The order of presentation of ques-tionnaires in each set were randomized using www.randomizer.org (Ur-baniak, Plous, & Lestik, 2003).
DATA ANALYSIS
All data were analyzed using Statistical Package for the Social Sciences, Ver-sion 12.0 (SPSS 12.0) and S-PLUS 6.2 for Windows (Insightful Corporation,2003). The test-retest reliability of the four self-report instruments was ex-amined by looking at the agreement between time 1 (T1) and time 2 (T2) interms of the individual items and the total score. For the individual items,the percentage of participants showing the same response at T1 and T2 wascalculated for each instrument and appropriate summary statistics werecomputed. In terms of the total scores, Intraclass Correlation Coefficient(ICC) was used to measure the agreement between each instrument at T1and at T2. The internal consistency for the self-report measures was com-puted using Cronbach’s alpha reliability coefficient and the inter-item corre-lation was analyzed using Pearson’s product moment correlation.
The performance of each screening instrument was evaluated by com-puting the value of sensitivity, specificity, PPV, and NPV for that instru-ment. Receiver Operator Curve (ROC) analysis was used to obtain informa-tion regarding all possible pairs of achievable sensitivity and specificityvalues for each screening instrument. This analysis also determined theoptimal cut-off score for each instrument to obtain the best value of sensi-tivity and specificity. The kappa statistic was also used as a measure ofagreement between the criterion diagnosis and each of the screening in-struments, employing Fleiss’ (1986) guidelines (poor agreement: <0.40, fairto good agreement: 0.40–0.75, excellent agreement: >0.75).
358 CHANEN ET AL.
RESULTSCOMPARING BPD SCREENING INSTRUMENTS WITH SCID-IICRITERION DIAGNOSIS
Figure 1 shows a plot of the ROC curves of the four instruments basedupon the total scores of each instrument. A ROC curve is a plot of the truepositive rate (sensitivity) against the false positive rate (1-specificity) for allthe possible cut-off points of an instrument. The optimal screening mea-sure would have a true positive rate of 100% and a false positive rate of0%, which would be indicated by a curve in the top left corner of the plotor as close to this point as possible. Figure 1 shows that the BPQ is com-pletely above the SCID-II PQ and MSI and nearly completely above IPDE.The IPDE and MSI are quite close to each other with the IPDE being abovethe MSI for most of the plot. There is also a considerable crossover betweenthe SCID-II-PQ and each of the IPDE and MSI.
Statistical tests were carried out to test for the difference between thecurves in terms of the area under the curves. The only significant compari-son is that between BPQ and MSI (p = 0.05), which together with the re-sults in Figure 1, indicate that the BPQ is significantly better than the MSI
FIGURE 1. ROC curves for the four BPD screening instruments with the criterion diagnosisof SCID II BPD.
SCREENING FOR BPD 359
in terms of the overall diagnostic accuracy when all the possible cut-pointsof these two instruments are taken into account.
In practice, however, only one cut-point would be used for each instru-ment. Thus another way of comparing the different instruments is to selectthe “best” cut-point of each instrument and evaluate its performance.Since the different points on a ROC curve represent trade-offs betweenthe true positive rate and the false positive rate, the “best” cut-point de-pends on the relative importance of these two rates. One reasonable wayto choose the best point is to select the point closest to the top left corner,as shown in Figure 1. The results for these “best” cut-points are shown inTable 1. Examination of kappa statistic suggests that most of the instru-ments show moderate agreement (kappa between 0.40 and 0.75) with thecriterion diagnosis (SCID II), with the BPQ appearing to show the bestagreement. Poor agreement (kappa <0.40) was obtained for the MSI. Thus,the results indicate that the BPQ is the best of the four screening mea-sures tested in this study as, (1) its ROC curve is completely above ornearly completely above the other curves, (2) it has the highest specificityvalue, the highest PPV and the highest kappa value (Table 1) and (3) itssensitivity value and NPV are comparable to those of the other measures.
TEST-RETEST RELIABILITY OF THE BPDSCREENING INSTRUMENTS
This was examined by looking at the agreement between T1 and T2 interms of individual items and in terms of the total score. In terms of indi-vidual items, the percentage of participants who showed agreement be-tween the two occasions in their responses was calculated for each item.All of the four instruments had very similar percentages of participantsgiving the same response on both occasions, with approximately 85% ofthe participants showing agreement between the two occasions when aver-aged over the items within each instrument. In terms of the total scores,the ICC values were computed as a measure of agreement between the twooccasions. Table 1 shows that the lowest ICC value was obtained for MSI,followed by IPDE, SCID-II PQ and BPQ, respectively. Both the averageagreement of 85% and the high ICC values therefore suggest good test-retest reliability for all four instruments, particularly the BPQ.
INTERNAL CONSISTENCY OF THE BPD SCREENING INSTRUMENTS
Cronbach’s alpha coefficient was used as a measure of the internal consis-tency for the four BPD screening instruments (see Table 1). Using 0.70 asan acceptable value for the alpha coefficient (Nunnally, 1978), the majorityof the other measures with the exception of IPDE, appear to have goodinternal consistency. Note that the alpha coefficient is related to the lengthof an instrument in the sense that a longer instrument will generally givea higher coefficient. So the alpha value of the BPQ is not directly compara-ble with those of the other measures.
TABLE 1. “Best” Cut-Points as Derived from Time 1 Data, Internal Consistency and Test-Retest Reliability
Negative Positive OverallNumber “Best” predictive predictive diagnostic Kappa
Instrument of items cut-point Sensitivity Specificity value value accuracy (se) Alpha ICC
0.45IPDE-BPD 9 >6 0.77 0.77 0.92 0.49 0.77 0.61 0.83(0.09)0.45SCID-II PQ-BPD 15 >12 0.64 0.85 0.89 0.54 0.80 0.88 0.87(0.10)0.35MSI 10 >7 0.68 0.75 0.89 0.43 0.73 0.78 0.78(0.09)0.57BPQ 80 >56 0.68 0.90 0.91 0.65 0.85 0.92 0.92(0.10)
Note. ICC denotes intraclass correlation
SCREENING FOR BPD 361
DISCUSSIONThe main finding from this study is that all four instruments performedsimilarly, with moderate sensitivity, moderate to high specificity, highNPVs, low to moderate PPVs, moderate agreement with the criterion diag-nosis (except the MSI), acceptable to high internal consistency (except theIPDE-BPD) and good test-retest reliability. However, there are noteworthydifferences that might favor one instrument over another.
The BPQ appears to have the best mix of characteristics, with moderatesensitivity, the highest specificity, high NPV and moderate PPV. It also hashigh internal consistency. Compared to the other three instruments, theBPQ has the highest overall diagnostic accuracy, a substantially higherkappa and the highest test-retest reliability. The only clear difference toemerge in the ROC analysis was that the BPQ significantly outperformedthe MSI. The main drawback of the BPQ for screening purposes is itslength, which might prove unacceptable to patients and to clinicians. How-ever, the BPQ has a simple yes/no response format that can be completedby the patient in around ten minutes and scored by the clinician in fiveminutes. This investment in time might be worthwhile when BPD identifi-cation and treatment is a higher priority, such as in specialist BPD treat-ment or research programs. When BPD is but one of many priorities, suchas in general clinical services, the SCID-II PQ-BPD might prove more suit-able.
For the MSI, the present study found that a slightly higher cut point (>7compared to ≥7 in Zanarini and colleagues’ study) gave the best balanceof sensitivity and specificity. In contrast to Zanarini and colleagues’ (2003)findings, we found only moderate sensitivity and specificity in our sample.We also found the opposite pattern of predictive values with a high NPVand low PPV, which better suits the intended purpose outlined in the in-troduction. Moreover, we found internal consistency was similar in bothstudies and test-retest reliability was good, although the lowest of the fourinstruments tested.
The relatively poor performance of the MSI might have been due to thechoice of the SCID-II as the criterion diagnosis. In Zanarini and colleagues’study, the criterion was the DIPD and the MSI questions are tightly linkedto this instrument. The slightly superior performance of the SCID-II PQ-BPD, compared to the MSI, might reflect its tight linkage to the questionsin the SCID-II criterion diagnosis. There are subtle but important differ-ences between the SCID-II and DIPD in their operational definitions of theDSM-IV BPD criteria. For example, angry outbursts are only assessed un-der the inappropriate anger criterion in the SCID-II, whereas in the DIPD,they contribute to the scoring of both the impulsivity and inappropriateanger items.
Another source of differences between the present study and that of Za-narini and colleagues is the sample itself. Zanarini and colleagues adver-tised for participants and selected those with treatment histories. In thepresent study, the sample was derived from acute referrals to a frontline
362 CHANEN ET AL.
youth mental health service. Zanarini and colleagues report that 69.5% ofparticipants met criteria for BPD, compared to 21.8% in the present study.Zanarini and colleagues’ prevalence is higher than base rates reported formost acute clinical services, including adolescent (Grilo, Becker, Fehon, etal., 1996), young adult (Grilo, Becker, Edell, et al., 1996) and adult (Widi-ger & Weissman, 1991) inpatient units. The performance of a screeningmeasure will vary according to the base rate of the diagnosis in question(Morse & Pilkonis, 2007). For a fixed test sensitivity and specificity, therarer the disorder, the lower the PPV of the test and this is the most likelyexplanation for the high PPV in Zanarini and colleagues’ study and the lowPPV in the present study.
The main strength of the present study is its use of actual outpatientsin a setting in which the screening measure will be used. However, we canonly comment to a limited extent upon the representativeness of the sam-ple. We have previously found that the presence and number of Axis I andII disorders in adolescent outpatients is significantly associated with fol-low-up contact difficulty and might lead to underestimation of the extentof psychopathology in a sample (Allott, Chanen, & Yuen, 2006). Anotherlimitation includes the requirement that participants complete all screen-ing measures (presented in random order) in one sitting. Therefore, thefindings might not reflect the performance of each measure when adminis-tered individually. Also, the IPDE-BPD and SCID-II PQ-BPD were actuallysubsets of items extracted from the corresponding original instruments. Itis unclear whether they would perform the same when administered intheir complete form. Another limitation is that the criterion diagnosis wasa semi-structured interview by a trained research assistant. It was neitheran expert clinical diagnosis nor a diagnosis using the Longitudinal ExpertAll Data (LEAD; Pilkonis, Heape, Ruddy, & Serrao, 1991) standard. More-over, the use of a categorical diagnosis of BPD means that “criterion nega-tive” participants might have had sub-syndromal BPD or other personalitypathology. In fact, a further 8 participants met 4 SCID-II BPD criteria anda further ten met 3 SCID-II BPD criteria.
The present findings indicate that screening for BPD in outpatient youthis feasible and should help improve recognition of the disorder among cli-nicians. Based upon our findings the BPQ achieves the best balance ofthe desired properties in a screening instrument. However, its length is asignificant drawback and might preclude more widespread clinical appli-cation. Of the shorter instruments, the data favor the SCID-II BPD but thismight be dependent upon the choice of criterion diagnosis.
REFERENCES
Allott, K., Chanen, A., & Yuen, H. P. (2006). patients. Journal of Nervous and Men-tal Disease, 194, 958–961.Attrition bias in longitudinal research
involving adolescent psychiatric out- Bernstein, D. P., Cohen, P., Skodol, A., Bezir-
SCREENING FOR BPD 363
ganian, S., & Brook, J. (1996). Child- Grilo, C. M., Becker, D. F., Fehon, D. C.,Walker, M. L., Edell, W. S., McGlash-hood antecedents of adolescent per-
sonality disorders. American Journal of an, T. H., & et al. (1996). Gender differ-ences in personality disorders in psy-Psychiatry, 153, 907–913.
Bernstein, D. P., Cohen, P., Velez, C. N., chiatrically hospitalized adolescents.American Journal of Psychiatry, 153,Schwab-Stone, M., Siever, L. J., &
Shinsato, L. (1993). Prevalence and 1089–1091.Gunderson, J. G., Kolb, J. E., & Austin, V.stability of the DSM-III-R personality
disorders in a community-based sur- (1981). The diagnostic interview forborderline patients. American Journalvey of adolescents. American Journal
of Psychiatry, 150, 1237–1243. of Psychiatry, 138, 896–903.Insightful Corporation. (2003). S-PLUS forChabrol, H., Montovany, A., Chouicha, K.,
Callahan, S., & Mullet, E. (2001). Fre- Windows. Seattle, Washington: Insight-ful Corporation.quency of borderline personality disor-
der in a sample of French high school Kernberg, O. F. (1986). Severe personalitydisorders: Psychotherapeutic strate-students. Canadian Journal of Psychi-
atry, 46, 847–849. gies. New Haven, CT: Yale UniversityPress.Chanen, A. M., Jackson, H. J., McGorry,
P. D., Allott, K. A., Clarkson, V., & Leichsenring, F. (1999). Development andfirst results of the borderline personal-Yuen, H. P. (2004). Two-year stability
of personality disorder in older adoles- ity inventory: A self-report instrumentfor assessing borderline personalitycent outpatients. Journal of Personal-
ity Disorders, 18, 526–541. organization. Journal of PersonalityAssessment, 73, 45–63.Chanen, A. M., Jovev, M., & Jackson, H. J.
(2007). Adaptive functioning and psy- Lenzenweger, M. F., & Castro, D. D. (2005).Predicting change in borderline per-chiatric symptoms in adolescents with
borderline personality disorder. Jour- sonality: Using neurobehavioral sys-tems indicators within an individualnal of Clinical Psychiatry, 68, 297–
306. growth curve framework. Developmentand Psychopathology, 17, 1207–1237.Chanen, A. M., McCutcheon, L., Jovev, M.,
Jackson, H. J., & McGorry, P. D. Lenzenweger, M. F., Lane, M. C., Loranger,A. W., & Kessler, R. C. (2007). DSM-IV(2007). Prevention and early interven-
tion for borderline personality disor- Personality Disorders in the NationalComorbidity Survey Replication. Bio-der. Medical Journal of Australia, 187,
S18–S21. logical Psychiatry, 62, 553–564.Lewinsohn, P. M., Rohde, P., Seeley, J. R., &First, M. B., Gibbon, M., Spitzer, R. L., &
Williams, J.B.W. (1996). Structured Klein, D. N. (1997). Axis II psychopath-ology as a function of Axis I disordersclinical interview for DSM-IV Axis I dis-
orders-patient version (SCID-I/P). New in childhood and adolescence. Journalof the American Academy of Child andYork: Biometrics Research Depart-
ment, New York State Psychiatric In- Adolescent Psychiatry, 36, 1752–1759.Loranger, A. W. (1999). International Person-stitute.
First, M. B., Gibbon, M., Spitzer, R. L., ality Disorder Examination DSM-IV andICD-10 Interview. Florida: Psychologi-Williams, J.B.W., & Benjamin, L. S.
(1997). User’s guide for the structured cal Assessment Resources.McGorry, P. D., Edwards, J., Mihalopoulos,clinical interview for DSM-IV Axis II per-
sonality disorders. Washington, DC: C., Harrigan, S. M., & Jackson, H. J.(1996). EPPIC: An evolving system ofAmerican Psychiatric Press.
Fleiss, J. L. (1986). The design and analysis early detection and optimal manage-ment. Schizophrenia Bulletin, 22, 305–of clinical experiments. New York: John
Wiley & Sons. 326.Morse, J. Q., & Pilkonis, P. A. (2007). Screen-Grilo, C. M., Becker, D. F., Edell, W. S., &
McGlashan, T. H. (1996). Gender ing for personality disorders. Journalof Personality Disorders, 21, 179–198.differences in personality disorders
in psychiatrically hospitalized young Nunnally, J. (1978). Psychometric theory.New York: McGraw-Hill.adults. Journal of Nervous & Mental
Disease, 184, 754–757. Paris, J. (2003). Personality disorders over
364 CHANEN ET AL.
time: Precursors, course and outcome. Westen, D., Shedler, J., Durrett, C., Glass,S., & Martens, A. (2003). PersonalityJournal of Personality Disorders, 17,
479–488. diagnoses in adolescence: DSM-IVAxis II Diagnoses and an empiricallyPatrick, J., Links, P., Van Reekum, R., & Mit-
ton, M. (1995). Using the PDQ-R BPD derived alternative. American Journalof Psychiatry, 160, 952–966.scale as a brief screening measure in
the differential diagnosis of personality Widiger, T. A., & Weissman, M. M. (1991).Epidemiology of borderline personalitydisorder. Journal of Personality Disor-
ders, 9, 266–274. disorder. Hospital & Community Psy-chiatry, 42, 1015–1021.Pilkonis, P. A., Heape, C. L., Ruddy, J., &
Serrao, P. (1991). Validity in the diag- Zanarini, M. C., Frankenburg, F. R., Khera,G. S., & Bleichmar, J. (2001). Treat-nosis of personality disorders: The use
of the LEAD standard. Psychological ment histories of borderline inpa-tients. Comprehensive Psychiatry, 42,Assessment, 3, 46–54.
Poreh, A. M., Rawlings, D., Claridge, G., 144–150.Zanarini, M. C., Frankenburg, F. R., Sickel,Freeman, J. L., Faulkner, C., & Shel-
ton, C. (2006). The BPQ: A Scale for A. E., & Yong, L. (1996). The DiagnosticInterview for DSM-IV Personality Disor-the Assessment of Borderline Person-
ality Based on DSM-IV Criteria. Jour- ders. Belmont, MA: McLean Hospital,laboratory for the study of adult devel-nal of Personality Disorders, 20, 247–
260. opment.Zanarini, M. C., Vujanovic, A., Parachini, E.Trull, T. J. (1995). Borderline personality
disorder features in nonclinical young A., Boulanger, J. L., Frankenburg, F.R., & Hennen, J. (2003). A screeningadults: I. Identification and validation.
Psychological Assessment, 7, 33–41. measure for BPD: The McLean Screen-ing Instrument for Borderline Person-Urbaniak, G. C., Plous, S., & Lestik, M.
(2003). Research randomizer. Retrieved ality Disorder (MSI-BPD). Journal ofPersonality Disorders, 17, 568–573.May 17, 2005, from http://www.ran
domizer.org/