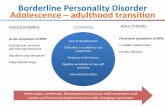
Neuroimaging and genetics of borderline personality disorder: a review
Transcript of Neuroimaging and genetics of borderline personality disorder: a review
162 Rev Psychiatr Neurosci 2007;32(3)
© 2007 Canadian Medical Association
Borderline personality disorder (BPD) is a highly prevalent psychiatric disorder that carries a severe risk factor for adolescent and youngadult suicide. Relatively little research has examined its biological etiology. Differences in the volume and activity in brain structuresrelated to emotion and impulsivity have been observed between individuals who have BPD and those who do not. The present studyseeks to assess current research on the neuroanatomical differences observed between individuals with and without BPD and the genesthat may play a role in the development of this disorder.
Le trouble de la personnalité limite (TPL) est une affection psychiatrique très répandue qui comporte un facteur de risque grave de suicidechez les adolescents et les jeunes adultes. Il s’est fait relativement peu de recherche sur son étiologie biologique. On a observé des dif-férences entre les sujets aux prises avec le TPL et ceux qui n'en sont pas atteints au niveau du volume et de l’activité de structures ducerveau reliées à l’émotion et à l’impulsivité. La présente étude vise à évaluer la recherche courante sur les différences neuro-anatomiquesobservées entre des sujets avec et sans TPL, ainsi que sur les gènes qui peuvent intervenir dans le développement de ce trouble.
Review PaperExamen critique
Neuroimaging and genetics of borderline personalitydisorder: a review
Eric Lis, BSc; Brian Greenfield, MD; Melissa Henry, PhD; Jean Marc Guilé, MD; Geoffrey Dougherty, MD
Lis, Greenfield, Henry — Faculty of Medicine, McGill University; Greenfield, Dougherty — Montréal Children’s Hospital; Guilé — Douglas Hospital, Montréal, Que.
Introduction
Borderline personality disorder (BPD) is prevalent, affecting asmany as 1% to 2% of the general population,1 and this inci-dence rises as high as 15% to 20% in psychiatric settings.2 BPDis associated with high rates of suicide — nearly all BPD pa-tients have experienced suicidal ideation and almost 10% com-mit suicide by adulthood.3 Although psychosocial causes ofBPD have been explored in many studies, relatively little dataexist regarding biological causes. The neurological and geneticfactors of BPD have not yet been fully explored, perhaps be-cause it is difficult to find BPD subjects to participate or be-cause the technologies used are relatively young. The study ofsuch factors may be a key to drawing new insights into thecauses, comorbidities and treatments of BPD.
Methods
We reviewed research on BPD, using the PubMed and
PsycINFO databases. Relevant articles were found between1980 and 2006, although we did not restrict our search to aparticular time period. We selected about 49 relevant articles,using the following 3 processes: 1) we cited selected articlesusing a combination of the search terms “borderline person-ality disorder,” “BPD,” “MRI,” “fMRI,” “imaging,” “PET,”“genetics,” “neuroanatomy,” “5-HTT,” “serotonin,”“dopamine,” “MAOA,” “amygdala” and “prefrontal”; 2) wesearched through articles and books cited as significant byrecent authors; 3) from the articles we accumulated, we se-lected the first authors who were the earliest to demonstratea given finding with a sufficient sample size. We did not citereplicated articles that did not demonstrate new findings.The articles we reviewed are summarized in Table 1 andTable 2.
Overall, use of neuroimaging in the study of BPD datesback only a few years. BPD has been linked to the amygdalaand limbic systems of the brain, the centres that control emo-tion and, particularly, rage, fear and impulsive automatic
Correspondence to: Eric Lis, Faculty of Medicine, McGill University, 144 Fairview, Montréal QC H9A 1V6; fax 514 412-4250;[email protected]
J Psychiatry Neurosci 2007;32(3):162-73.
Medical subject headings: diagnostic imaging, genetics, personality disorder.
Submitted Aug. 15, 2006; Revised Oct. 14, 2006; Accepted Oct. 30, 2006
Neuroimaging and genetics of BPD
J Psychiatry Neurosci 2007;32(3) 163
reactions.21 Studies have shown that the hippocampus andamygdala may be as much as 16% smaller in people withBPD and have suggested that experiences of trauma maylead to these neuroanatomical changes.5 Positron emission to-mography (PET) scans have generally shown that peoplewith BPD show hypometabolism of glucose in their pre-frontal cortex and limbic system relative to people who don’thave BPD,12 suggesting that the disorder may result from afailure of the “rational” prefrontal cortex to regulate the “im-pulsive” limbic system.
One difficulty inherent in analyzing the data about neuro-logical changes associated with BPD is that much of the re-search is contradictory. For example, the anterior cingulatecortex has been shown to have hypometabolism or hyper-metabolism in different studies that used the same imagingtechnologies. Undoubtedly, this is partly owing to the com-plexity of imaging studies and the variety of possible con-founding factors, including the drugs a participant mighthave had in their system, the potential effect of any comorbidpsychiatric disorders on neurophysiology, and differences inimages introduced by different resolutions, head tilts or labo-ratory conditions. The contradiction might also be due to theheterogeneity of people with BPD. Vast differences can beobserved in manifestations of the disorder between 2 individ-uals,3 and it is reasonable to assume that there may be differ-ent neurological changes in a person who is highly impulsiveversus someone with primarily dissociative symptoms.
A related difficulty in this area is the question of whetherparticipants with comorbid psychiatric disorders should beexcluded. Because most people with BPD have an additionalmental disorder, frequently depression,3 excluding partici-pants with these disorders reduces the generalizability of astudy. Excluding people with multiple diagnoses ensuresthat abnormal brain volumes or metabolisms observed areassociated with BPD, rather than some other illness, but theresults may not apply precisely to the larger population ofBPD patients with comorbid disorders.
Historically, work linking BPD to brain dysfunction datesas far back as 1980,22 when it was postulated that there maybe a subgroup of patients whose illnesses had organic causes,such as brain injury. This prompted examinations of neu-ropsychological functioning in BPD patients. van Reekumand colleagues23 examined data from medical charts and in-terviews with 48 war veterans, mostly men, with a mean ageof 32 years. They found that BPD patients had a higherprevalence of brain injuries, developmental or acquired, thanhealthy control subjects and that greater brain dysfunction islinked to greater behavioural disturbances. This finding wasreplicated with a more representative group of participants24
but was limited because it was retrospective; the authorscould not demonstrate cause and effect (that brain injurieswere a cause of BPD rather than that impulsive people weremore likely to be in injurious situations). To address suchuncertainties, imaging techniques were used to examine neu-rological function. The earliest studies typically found noneuroanatomical differences between control subjects andBPD patients, or they found differences that failed to achievestatistical significance.25–27
Electroencephalographic (EEG) technology was applied toBPD by Zanarini and others,28 who found subtle abnormali-ties in the EEGs of patients with BPD. They suggested that,because childhood abuse is a known risk factor for the devel-opment of BPD, cranial trauma sustained during childhoodmay result in permanent functional abnormalities that wouldresult in BPD symptoms. With the improvement of EEG tech-nology, newer studies have been conducted. Working fromthe hypothesis that people with BPD have impeded matura-tion of higher-order consciousness, Meares and colleagues29
tested prefrontal cortical systems of coordination and integra-tion. They administered an auditory stimulus target detectiontask to subjects with BPD and used EEG to measure the P3event-related brain potential, which can be measured as 2components (P3a and P3b). They demonstrated that P3 isslightly delayed in BPD subjects and that, compared withage-matched healthy control subjects, the P3a of BPD subjectsshowed enhanced amplitude, failure of habituation and lackof temporal synchronicity with P3b. The authors suggestedthat these abnormalities indicated a general failure of coordi-nation among diverse cortical networks. Further, on measur-ing and qualifying the characteristic P3 of people from variousage groups, BPD patients were found to exhibit a P3 profile ofpeople younger than themselves (i.e., failure of maturation andthus possibly failure of development of a sense of self). Thisstudy diagnosed patients using the Diagnostic and StatisticalManual of Mental Disorders (DSM), third edition, revised (DSM-III-R30) rather than the DSM, fourth edition (DSM-IV).31
Early attempts to use neuroimaging technology to studyBPD, in conjunction with early EEG studies that demon-strated neurological abnormalities in BPD patients, laid thegroundwork for more studies as imaging technologies im-proved. Higher-resolution, more easily accessible technologybegan to show structures in the brain that were abnormal inBPD patients. PET studies suggested that BPD patients hadabnormalities in the frontal and temporal lobes. Two majorworks12,32 found that patients with BPD showed relatively lowglucose metabolism in various brain structures, including thefrontal cortex (dorsolateral frontal cortex) and limbic system(anterior cingulate cortex), as well as structures strongly asso-ciated with the limbic system (the basal ganglia and the thala-mus) during the resting state. In contrast, Juengling andcolleagues17 found hypermetabolism in the anterior cingulateand in several frontal cortex structures (superior frontalgyrus, right inferior frontal gyrus and opercular part of theright precentral gyrus). Hypometabolism was demonstratedin the limbic structure of the left hippocampus and in the leftcuneus, an occipital structure involved in visual processing.
The ability of PET scans to observe brain activity in re-sponse to particular stimuli has allowed them to be used toexamine neural correlates of particular BPD symptoms, aswell as the illness itself (for example, Schmahl andcolleagues10). Fear of abandonment is a major symptom ofBPD, so the researchers presented scripts of abandonment sit-uations to 20 women with a history of abuse, 10 of whom hadBPD and 10 control women without BPD. In women withBPD, they observed increased activation (increased bloodflow) of the bilateral dorsolateral prefrontal cortex and right
cuneus and decreased activation in the medial prefrontal cor-tex and various structures involved primarily in visualprocessing, including the left fusiform gyrus, left visual asso-ciation cortex and left middle temporal gyrus. Women withand without BPD showed deactivation in the right precuneus(whose function has not yet been proven but which is be-lieved to be a limbic structure) and the right caudate (in-volved primarily in voluntary movement), suggesting thatthese areas play a role in a generalized response to memoriesof abandonment nonspecific to BPD.
In one of the most recent PET studies of BPD, Lange andcolleagues18 examined 17 female inpatients (mean age 32 yr)with dissociative symptoms and various other comorbid dis-orders, excluding only participants with neurological or psy-chotic diseases. Compared with healthy control subjects, the
patients with BPD demonstrated reduced glucose metabo-lism in right-sided ventromedial temporal and left-sided me-dial parietal or posterior cingulate cortices, areas associatedwith limbic function and memory. Further, memory perfor-mance was positively correlated with metabolism, suggestinga functional implication of the metabolic abnormalities.
The development of magnetic resonance imaging (MRI) asan alternative to CT, PET and EEG allowed researchers tomeasure the volumes of structures in the brain more effec-tively, with a clearer distinction between grey matter, whitematter and cerebrospinal fluid and with generally superiorresolution.33 Perhaps the first published MRI-based investiga-tion of brain abnormalities in people with BPD was Lyoo andcolleagues.8 They recruited 25 people with BPD (diagnosedaccording to the DSM-III34) and 25 control subjects without
Lis et al
164 Rev Psychiatr Neurosci 2007;32(3)
Table 1: Summary of papers relating to anatomic brain changes
Study Design Subjects Objective/hypothesis Results Limitations
Brambilla et al4 MRI:hippocampus,amygdala,dorsolateralprefrontalcortex, temporallobes, basalganglia
10 participants (6 F) withvarious comorbidities, drug-free 2 mo
Examine hippocampal andamygdala volume reductionin BPD associated withchildhood abuse;investigate areas importantin the regulation of emotionand impulsivity
Decreased hippocampusvolumes in BPD patients,especially those withchildhood abuse; enlargedputamen volumes in BPDespecially with comorbidsubstance use disorders
Small sample size
Driessen et al5 MRI:hippocampus,amygdala,temporal lobes,prosencephalon
21 F with BPD, 21-40 yr,previously without comorbidpsychiatric disorders
Volumes of studied brainstructures will be smallerthan in control subjects
Significantly reducedvolumes of both brainstructures (left hemispherehippocampus reduced15.7%, right hemispherehippocampus reduced15.8%, left hemisphereamygdala reduced 7.9%,right hemisphere amygdalareduced 7.5%); meanhippocampal volumenegatively correlated withduration of abuse in history
Did not assess for pastdepression; did notcontrol for history ofpsychotropic drug use
Hazlett et al6 MRI: measuregrey and whitematter in BAswithin thecingulate
50 patients (18-52 yr,mean 33) with variouscomorbidities, assessedwith DSM-III criteria; 13 hadSPD, 37 did not
Examine grey and whitematter volume within BAs ofthe cingulate gyrus andfrontal lobe, examinecomorbidity by subgroupinginto BPD patients with SPDand those without
Reduced cingulate grey andincreased white mattervolume in BA 24 and 31;BPD without SPD groupshowed this abnormality inBA 24 but 31 was spared;BPD with SPD group hadreduced grey matter volumein both; grey matter loss inBA 31 was greater in theBPD with SPD subjectsthan BPD only subjects
DSM-III diagnoses
Irle et al7 MRI: parietalcortex, hippo-campus
30 F inpatients; excludedfor history of neurologicaldisease, electro-encephalographabnormalities indicative oftemporal lobe epilepsy,hyperintense MRI signals,psychotic disorders;patients tested were alsodiagnosed with PTSD,panic disorder, generalizedanxiety disorder, OCD,major depression,somatization disorder,anorexia, depersonalizationdisorder, dissociativeamnesia, dissociativeidentity disorder
Examine anatomicalchanges in BPD via MRI
Reduced size of the rightparietal cortex, strongerparietal leftwardasymmetry; reducedleftward asymmetryassociated with strongerpsychotic symptoms andmore schizoid personalitytraits; smaller hippocampalvolumes associated withstronger clinical symptoms
High prevalence of axis1 disorders in theparticipants might haveadded confounds butmade the sample morerepresentative of BPD;only F tested
Neuroimaging and genetics of BPD
J Psychiatry Neurosci 2007;32(3) 165
any signs of BPD or neurological dysfunction. They com-pared images of the frontal and temporal lobes, lateral ventri-cles and overall cerebral hemispheres, demonstrating thatBPD patients showed significantly reduced frontal lobe vol-ume (6.2%) without other significant differences. Althoughinnovative in its use of MRI, this study was limited in its gen-eralizability because participants who demonstrated a historyof axis I or axis II mental disorders other than BPD were ex-cluded. The second limitation of this study was that head tiltduring scanning was not corrected for, and subject move-ment or head rotation might have added measurement error.The authors also noted that, while differences in grey andwhite matter were not analyzed as part of the study, the rela-tive amounts may make a difference in the results. The au-thors proposed that reduced frontal lobe volume may be as-sociated with impulse control failures of people with BPD,given that people with frontal lobe damage due to trauma of-ten display lack of impulse control.35
Building on the work of Lyoo and colleagues,8 Driessenand others5 used MRI to specifically study the limbic struc-tures of the hippocampus and amygdala. They recruited 21female patients (aged 21–40, mean 29.9 yr) with BPD withoutcomorbid psychotic disorders (i.e., schizophrenia or majordepressive disorder with psychotic symptoms as assessedwith the DSM-IV) and compared them with control subjectswithout BPD or other mental illness. Patients with BPDshowed significantly reduced volumes of both brain struc-tures (left hemisphere hippocampus reduced 15.7%, righthemisphere hippocampus reduced 15.8%, left hemisphereamygdala reduced 7.9% and right hemisphere amygdalareduced 7.5%). No significant difference in volumes were ob-served within the groups. BPD patients with comorbid post-traumatic stress disorder (PTSD) showed no significant dif-ferences from those without PTSD. Mean hippocampalvolume was negatively correlated with duration of abuse inthe patient’s history, and correlations between amygdala
Table 1 continued
Study Design Subjects Objective/hypothesis Results Limitations
Lyoo et al8 MRI: frontallobes, temporallobes, lateralventricles,cerebral hemi-spheres
25 subjects from inpatientand outpatient wards, withno other current axis 1 or 2illnesses
Volumes of the frontal andtemporal lobes of the brainmay change in BPDsubjects
Reduced frontal lobevolume (6.2%); no othersignificant differences
Participants wereexcluded if theydemonstrated a historyof axis I or axis IImental disorders otherthan BPD; head tiltduring scanning notcorrected for; differen-ces in grey and whitematter not analyzed
Rusch et al9 Voxel-basedmorphometricstudy
20 BPD patients (F, meanage 29.3 yr) with variouscomorbidities; excluded forhistory of loss ofconsciousness and coma,schizophrenia, bipolardisorder, alcohol/drugabuse, current majordepression, currentanorexia; participantspsychotropic-free for 2 wkand had completedschooling
Volume reduction andpossibly loss of cortical greymatter density inhippocampus, amygdala,left orbitofrontal and rightanterior cingulate cortex
Volume reduction inbasolateral amygdale; nodifferences in regionalcortical grey or white matterdensity or volume
Excluded currentdepression andanorexia; VBM limits:eliminates rater biasand error but its abilityto detect subtledifferences not yetbeen proven sufficiently
Schmahl et al10 MRI: amygdalaandhippocampus
10 F with BPD and historyof sexual or childhoodabuse; exclusion for organicmental disorder, history ofhead trauma, currentalcohol abuse, history ofpsychotic disorder
Smaller hippocampal andamygdala volumes in BPDpatients
Supported hypothesis Small sample, historyof psychotropicmedication and/or druguse in most patients
Tebartz van Elstet al11
MRI:hippocampus,amygdala, andorbitofrontal,dorsolateralprefrontal, andanteriorcingulate cortex
Eight F patients with BPD,aged 20-40 yr, finishedregular schooling, nopsychotropic drugs for 2 wk;exclusion criteria: lifetimediagnosis of schizophrenia,bipolar I disorder,alcohol/drug abuse in past6 mo, current anorexia,major depression
Smaller amygdala andhippocampus in BPDpatients, differences inprefrontal lobe
No significant difference intotal brain volume; 20%–21% reduction ofhippocampal and 23%–25%reduction amygdalavolumes; 24% reduction ofthe left OFC, 26% reductionof the right ACC; amygdalavolumes of both sidescorrelated with leftorbitofrontal volume;positive correlation betweenno. of self-injuriousincidents and bilateralanterior cingulated volume
Did not separate greyfrom white matter.Cannot specify whichof the different gyricontributed most to thereported volume loss;exclusion reducedgeneralizability
F = female; BPD = borderline personality disorder; BA = Brodmanní s area; DSM-III = Diagnostic and Statistical Manual of Mental Disorders, third edition; SPD = schitzotypal personalitydisorder; PTSD = posttraumatic stress disorder; OCD = obsessive–compulsive disorder; VBM = voxel-based morphometry; OFC = orbitofrontal cortex; ACC = anterior cingulate cortex.
Lis et al
166 Rev Psychiatr Neurosci 2007;32(3)
Table 2: Summary of papers relating to functional brain changes
Study Design Subjects Objective/hypothesis Results Limitations
De la Fuenteet al12
PET: metabolismduring resting state,closed eyes,unplugged ears,dimmed lights, lowambient noise, after2 h fast
10 patients (8 F) 24-45 yrexcluded for current axis Idisorders and majordepression, abnormalneurology or history of headtrauma, abnormalities onstandard blood test or ECG;10 d washout for psychotropicmedication
Study regional cerebralmetabolism in BPD withPET
Hypometabolism in thedorsolateral part of thefrontal cortex, anteriorcingulate cortex, basalganglia and thalamus
Frontal cortexhypometabolism isprobably a nonspecificfinding, common tomany mental illnesses;DSM-III used fordiagnoses
Doneganet al13
fMRI: response to afixation point or tohappy, sad, fearfulfacial expressions
15 right-handed subjects (13F), mean age approx. 35 yr,treated in the last 6 mo;excluded for organic mentalimpairment, schizophrenia,and substance intoxication.Also excluded if unable torefrain from abusingsubstances for a 2-wk periodbefore the experiment orunable to undergo scanning
Amygdala hyperreactivityin BPD patientscontributes tohypervigilance, emotionaldysregulation, disturbedinterpersonal relations
Greater left amygdalaactivation to facial emotionv. fixation point; debriefingrevealed that some BPDpatients had difficultydisambiguating neutralfaces or found themthreatening
Did not exclude basedon most mentaldisorders (nearly everyparticipant wascomorbid for at least 1personality disorder).Some participantswere takingmedications that mighthave altered results
Driessenet al14
fMRI: metabolismwhile patientsrecalled traumaticepisodes
12 BPD patients (F) withtrauma and previouslytreated; excluded forendocrine system disorders,malignant diseases, livercirrhosis, neurologicaldiseases, loss ofconsciousness, mentalretardation, current infectiousdiseases, anorexia,schizophrenia, schizoaffectivedisorders, MDD withpsychotic symptoms
Traumatic memory in BPDpatients is associated withactivation patternsdifferent from thoseassociated with negativebut nontraumatic memoryand that PTSD modifiesthese patterns
Activation of theorbitofrontal cortex in bothhemispheres, activation ofBroca’s area in patientswith BPD without PTSD,minor activation of the OFC,no activation of Broca’sarea in patients with BPDand PTSD
Small sample size
Goethalset al15
Brain perfusionSPECT: investigatedwhether BPD andantisocial personalitydisorder showunusual patterns ofperfusion
37 patients APD (25 M, meanage 32.3 yr) admitted forimpulsive behaviour andfound to show as BPD;excluded for axis I diagnosis,inability to go medication-free,brain lesions found (CT); 27patients were BPD, 10 wereAPD
Confirm the existence of aparticular pattern ofcerebral perfusion in BPDand APD withoutcomorbid axis I disorders,substance abuse, ortraumatic brain injury
Reduced regional cerebralblood flow in the right lateraltemporal cortex and thepolar and ventrolateral partsof the right prefrontal cortex
Exclusion ofcomorbidities; lack ofsex- and age-matchedhealthy controls;absence of apsychiatric controlpopulation (wouldhave shown whetherreduced CBF was anonspecific psychiatricfinding)
Herpertz etal16
fMRI: amygdala whileemotionally aversiveimages are displayedto participants
6 BPD patients (F) whodisplayed no comorbid mentalillness
BPD subjects will show ahigher degree of activationin limbic/paralimbicstructures in response toaversive images
Elevated blood oxygenationlevel dependent fMRI signalin the amygdala in bothhemispheres, unusualactivation in the prefrontalcortex (medial andinferolateral portions)
Small sample size, nopatients withcomorbidities, noanalysis of the effect ofparticipants’ phase oftheir menstrual cycles
Juenglinget al17
PET: frontal andprefrontal metabolismduring restingconditions
12 F, mean age 25 yr, free ofpsychotropic-free for4 wk; excluded for lifetimeschizophrenia, bipolardisorder, alcohol/drug abusein the last 6 mo, currentanorexia, major depression
Replicate results of De laFuente et al,12
demonstrate alterations infunction in prefrontalcortex, anterior cingulate,hippocampus
Glucose metabolismincreased in the anteriorcingulate, the superiorfrontal gyrus bilaterally, theright inferior frontal gyrusand the opercular part ofthe right precentral gyrus,and decreased in leftcuneus and lefthippocampus
Small sample size;exclusion ofcomorbidities
Lange et al18 PET: metabolism inthe right temporalpole/anterior fusiformgyrus and leftprecuneus andposterior cingulatecortex and correlatewith failures ofmemory
17 F inpatients (mean age 32yr) with strong dissociativesymptoms and memorydeficits who had participatedin Irle et al7; excluded forneurological disease,psychotic disorder; variouscomorbid mental illnessesrepresented
Investigate whether brainglucose metabolism isreduced in temporo-parietal cortices of BPDsubjects with dissociativesymptoms; investigatewhether temporo-parietalmetabolic changes arerelated to clinicalsymptoms and to memorydeficits of BPD subjects
Reduced glucosemetabolism in right-sidedventromedial temporal andleft-sided medialparietal/posterior cingulatecortices; memoryperformance correlated withmetabolic activity inventromedial and lateraltemporal cortices (poorermemory performance iscorrelated to lowermetabolism)
High comorbidity rate
Neuroimaging and genetics of BPD
J Psychiatry Neurosci 2007;32(3) 167
volume and duration of abuse were insignificant. This studyaddresses several of the limitations of earlier studies. In addi-tion to using the DSM-IV to define BPD, rather than theDSM-III, it corrected for head tilt and used less stringent ex-clusion criteria. The study is limited because the functioningof the brain regions studied was not assessed, thus the au-thors could not state whether the reduced volume had afunctional impact or whether volume reductions were acause or an effect of BPD.
Since Driessen and colleagues, other researchers have con-ducted similar MRI studies, including Tebartz van Elst andcolleagues11 who studied 8 female patients aged between 20
and 40 years, excluding those with a lifetime diagnosis ofschizophrenia, bipolar I disorder, alcohol or drug abuse inthe past 6 months, current anorexia or current major depres-sion. The researchers demonstrated 20%–21% reductions ofhippocampal volume and 23%–25% reductions of amygdalavolume in people with BPD. They also demonstrated 24% re-ductions of the left orbitofrontal cortex (OFC, a frontal cortexstructure implicated in decision-making and believed to bepart of the limbic system) and 26% reductions of the right an-terior cingulate cortex. This study was limited because greyand white matter were not separated; thus it could not bespecified which gyri contributed to volume loss. The study
Table 2 continued
Study Design Subjects Objective/hypothesis Results Limitations
Schmahlet al10
PET: blood flow whilelistening to stories ofneutral or personalabandonment
10 F with BPD and 10 withoutBPD but with history ofabuse, recruited throughnewspapers and flyers;excluded for serious medicalor neurologicsl illness, organicmental disorder or comorbidpsychotic disorders, retainedmetal, history of head trauma,loss of consciousness,cerebral infectious disease,dyslexia; most participantshad comorbidities, such aslifetime or current MDD andPTSD
Exposure to scripts ofabandonment situationswill result in decreasedblood flow in medialprefrontal cortex, fusiformgyrus, and visualassociation cortex and inincreased activation indorsolateral prefrontalcortex in F with BPD
Exposure to scripts ofabandonment resulted inincreased activation of thebilateral dorsolateralprefrontal cortex anddecreased activation in theleft fusiform gyrus, leftvisual association cortex,medial prefrontal cortex andalterations in blood flow inother areas that were nothypothesized, includingdeactivation in left middletemporal gyrus andactivation in right cuneus;both groups showeddeactivation in rightprecuneus and rightcaudate, suggesting ageneralized response tomemories of abandonmentnonspecific to BPD
Pilot study; smallsample size; nearly allBPD subjects weretaking psychotropicmedication during theinvestigation controland experimentalgroups not matchedfor comorbid disorders
van Elstet al19
Hydrogen-1 magneticresonancespectroscopy withvaried echo time:measurement of NAAconcentrations inprefrontal cortex ofBPD patients
12 unmedicated F BPDpatients previously treated viadialectical behaviour therapy;excluded for lifetimeschizophrenia, bipolardisorder, learning disorders,alcohol/drug abuse in past6 mo, current severeanorexia, major depression
Short and long echo timeMRS to investigate frontaland striatal brainpathology as a possiblecause of the glucosehypometabolism, lookingespecially at NAA as ametabolite
Reduction of the absoluteNAA concentrations in thedorsolateral prefrontalcortex which suggestshypometabolism, lowneuronal density, andpossibly neurodegenration.No differences inNAA/creatine orcholine/creatine ratios(which suggests thatlooking at these rations is ofno use for BPD)
Looked only atprefrontal cortex dueto time constraints, socannot comment onother brain areas ofinterest (such asorbitofrontal cortex andamygdala); excludeddepression patients
Völlm et al20 fMRI: BPD or APDpatients scannedduring a Go/No Gotask to observeactivation associatedwith impulsivity
8 personality disorder patients(7 BPD) with variouscomorbid axis II disorders;excluded for history ofsignificant head injury, historyof neurologicalillness/pathological MRI scan,use of illicit substance in thepast 2 mo, alcohol intake> 20 units/wk, current moderateor severe depression, manicor psychotic illness, currentantidepressant medicationand any contraindication forMRI scanning
Attenuated orbitofrontalcortex responses duringperformance of aGo/NoGo task comparedwith healthy controlsubjects
More widespread activationof prefrontal and temporalareas than healthy control;in control subjects, mainfocus of activation duringinhibition was rightdorsolateral and the leftorbitofrontal cortex; inpatients, observed morebilateral and extendedactivation across themedial, superior and inferiorfrontal gyri extending to theanterior cingulate
Small sample, with 2disorders as the mainfocus; patients withsevere depressionexcluded; nodifference inimpulsivity betweenpatients and healthycontrol subjects(probably due to lowpower and patientsunderreportingimpulsivity); impulsivitymanifests differently indifferent disorders andmay not be the samesymptom in APD andBPD
PET = positron emission tomography; F = female; ECG = electrocardiogram; BPD = borderline personality disorder; DSM-III = Diagnostic and Statistical Manual of Mental Disorders, thirdedition; fMRI = functional MRI; M = male; MDD = major depressive disorder; PTSD = posttraumatic stress disorder; OFC = orbitofrontal cortex; SPECT = single photon emissioncomputed tomography; APD = antisocial personality disorder; CBF = cerebral bloodflow; MRS = magnetic resonance spectroscopy; NAA = N-acetylaspartate.
was additionally limited because it used a small sample size(n = 8). The generalizability was stronger than some previousstudies because patients with a lifetime history of depressionwere included (4 of 8 participants had experienced major de-pression in their lifetime). Brambilla and colleagues4 laterstudied volume abnormalities in the putamen, a structure as-sociated with the caudate and part of the basal ganglia that isbelieved to play a role in reinforcement learning and which isparticularly vulnerable to abnormal enlargement in alcoholand drug abusers. Examining 10 subjects with BPD(6 women, aged 18–45 yr) with various comorbid disorderswithout taking medication for 2 months, they demonstratedthat BPD patients had decreased hippocampal volume (espe-cially those who were abused as children) and increasedputamen volume (especially in substance users). They didnot find volume differences in the amygdala or other struc-tures that were noted by other investigators. The authorssuggested that ongoing studies with larger sample sizes areneeded to address conflicting results obtained by these differ-ent studies.
Even more recently, Irle and colleagues7 tested 30 womenwith BPD and demonstrated that, relative to control subjects,they showed reduced volume of the right parietal cortex.They further demonstrated a stronger parietal leftwardasymmetry in BPD patients, with reduced leftward asymme-try appearing related to stronger psychotic symptoms andmore schizoid personality traits. The study replicated thefinding that hippocampus size was reduced in people withBPD, with reduced volume being related to stronger trauma-related clinical symptoms. The authors speculated that a re-duced leftward asymmetry of temporoparietal cortices maybe a risk factor for developing psychotic symptoms aftertrauma and abuse, whereas increased leftward parietal cortexasymmetry may be protective. In line with Tebartz van Elstand others,11 this study excluded people with neurologicaldisease and psychotic disorders but included many DSM dis-eases, such as major depression (lifetime and current), PTSD,generalized anxiety disorder, somatization disorder,anorexia, depersonalization disorder and even dissociativeidentity disorder. These authors noted that, as with moststudies on the neuroimaging of BPD patients, they testedonly women but that temporoparietal cortex asymmetry hasbeen shown to vary considerably with sex.
Current research has moved increasingly toward examin-ing volume reductions in different subgroups of BPD, as inthe work of Hazlett and colleagues.6 These researchers exam-ined differences between people with BPD and withoutcomorbid schitzotypal personality disorder (SPD). The inves-tigators used MRI to examine the overall cingulate gyrusgrey and white matter volume and volume of Brodmann’sareas 24 and 31 in the cingulate gyrus, comparing BPD sub-jects with healthy control subjects and subjects with BPDboth with and without SPD. They found that BPD subjectshad overall reduced grey and increased white matter volumein areas 24 and 31. Patients with BPD without SPD, however,had these reductions in area 24 while area 31 was spared; pa-tients with BPD and SPD had reduced grey matter volume inboth areas. Grey matter volume reduction in area 31 was
greater in the BPD and SPD group than in the BPD withoutSPD group, while the whole BPD group did not differ fromcontrol subjects in overall prefrontal brain or cingulate vol-ume. These findings suggest that BPD patients do not differfrom control subjects in the total volume of their cingulategyri but that relative grey and white matter volumes in cer-tain parts of that gyrus may be abnormal. The authors arguedthat it makes sense that area 24 (in the anterior cingulate, as-sociated with recognition of affect) would show such abnor-malities in all BPD patients, whereas abnormalities in area 31(in the posterior cingulate, associated with affective process-ing) would be less abnormal in people with BPD withoutSPD. This study used the DSM-III-R to assess patients andprovides insight into possible subgroupings of BPD.
Numerous other imaging methods exist and, while tech-nologies such as MRI and functional MRI (fMRI) are mostcommon, other technologies have recently been used to addto the body of research on BPD. Rusch and colleagues9 usedvoxel-based morphometry (VBM) to examine brain struc-tures that MRI had shown lose volume in BPD patients. Theyselected VBM as their tool because it offers objective and au-tomated measurement of changes in grey and white matterdensity and volume. Using this highly sensitive technologyto compare the volume and density of the grey and whitematter of BPD patients with control subjects, the researchersfound significant volume reductions in the area of the baso-lateral amygdala and no differences in regional cortical greyor white matter density or volume. They did not confirmright amygdala volume loss or abnormalities in the pre-frontal areas and suggested that this may be due to differentmethodologies used in different studies.
The increasing availability of data regarding anatomicchanges in the brain led to an investigation of physiologicalchanges, particularly with fMRI. Whereas MRI scans had be-gun to demonstrate anatomical abnormalities in the brains ofpeople with BPD, fMRI allowed researchers to observeneural activation within the structures of interest. The func-tion of the amygdala as a centre of emotion regulation andthe evidence of structural abnormalities in the amygdala incases of BPD made it a natural structure for fMRI investiga-tion. Herpertz and colleagues16 first recruited 6 women withBPD who displayed no comorbid mental illness and 6 age-matched healthy control subjects. They then presentedemotionally aversive and neutral slides and compared theamygdala functioning of both groups. It was demonstratedthat participants with BPD showed an elevated blood oxy-gen–level dependent fMRI signal in the amygdala in bothhemispheres and activation in the prefrontal cortex (medialand inferolateral portions) in response to aversive slides. Ex-perimental and control groups both demonstrated increasedactivation in the temporo-occipital cortex, but the experimen-tal group showed increased activation in the fusiform gyrusas well. The authors suggested that the increased activity inthe amygdala demonstrates that BPD patients experience anexaggerated emotional response even to mild stimuli andthat “abnormal” prefrontal cortical modulation of the indi-vidual’s perceptions may result in that individual focusingexcessively on emotionally relevant stimuli in the environ-
Lis et al
168 Rev Psychiatr Neurosci 2007;32(3)
Neuroimaging and genetics of BPD
J Psychiatry Neurosci 2007;32(3) 169
ment. The major limitation of this study was its sample sizeof only 6 participants, none of whom had comorbid mentalillness. Additionally, this study did not analyze the effect ofthe participants’ phase of their menstrual cycles, which theauthors indicated may be a source of error. Estrogen levelscan influence cerebral perfusion, and while this effect shouldbe miniscule in a small brain structure such as the amygdala,it should be investigated.
Inspired by the earlier studies, Donegan and colleagues13
used fMRI scanning to observe the brains of people with BPDwhen presented with emotional facial expressions. Fifteenright-handed participants (13 female, mean age 35 yr) wererecruited, excluding those with organic mental impairment,schizophrenia, substance intoxication, inability to refrainfrom abusing substances for a 2-week period before the ex-periment or inability to undergo fMRI scanning. Participantswere shown a neutral stimulus (a fixation point) or a happy,sad or fearful facial expression; relative brain activation wasmeasured. All participants predictably showed greater activ-ity in the left amygdala in response to faces than to fixationpoints. Whereas control participants’ activation did not ex-ceed threshold criteria set by the researchers, subjects withBPD demonstrated activity in excess of the researchers’ crite-ria. In addition to the amygdala, high activity was observedin the limbic structures of the regions containing the dorsalborder of the amygdala, the bed nucleus of the stria termi-nalis, the lateral hypothalamic nuclei, the nucleus basalis (aproposed integrator of limbic information) and in the frontallobes. Further, during the debriefing, BPD participants re-vealed that they had difficulty disambiguating neutral faces,interpreting them as unnecessarily negative or finding themthreatening, which might have implications for the anxietyand social difficulties often observed in BPD. This study in-cluded participants with numerous comorbidities, for whichthe authors compensated with post hoc analyses, suggestingthat none of the other disorders were responsible for a signif-icant alteration in their results, except possibly PTSD. The ef-fect of PTSD did not reach significance but did suggest thatamygdala reactivity may be bilateral for patients with BPDbut not PTSD and lateralized to the left hemisphere for sub-jects with BPD and PTSD. The sample size tested makes itdifficult to conduct such analyses, and investigating the effectof PTSD on a larger group would be useful.
Evidence of the significance of the presence or absence ofPTSD grew with the efforts of Driessen and colleagues.14
They recruited 12 women with BPD who had experiencedtrauma (aged 21–40 yr, mean 33 yr) and who had variouscomorbidities. The authors interviewed the participants toobtain cues about traumatic memories and aversive but non-traumatic memories and observed them via fMRI during re-call of those memories. The researchers observed activationof the orbitofrontal cortex in both hemispheres and activationof Broca’s area in patients with BPD without PTSD and ob-served only a minor activation of the orbitofrontal cortex andno activation of Broca’s area in patients with BPD and PTSD.Because all BPD patients tested had experienced trauma butnot all had PTSD, the authors argued that presence or ab-sence of comorbid PTSD may be an important subgroup
classification for the diagnosis and treatment of BPD. Likemost studies of the MRI and fMRI of BPD, this study waslimited by a small sample size.
It has become increasingly common for BPD to be exam-ined in terms of its symptoms, rather than as a disorder inand of itself. This has proven to be true in the study of impul-sivity, which is a feature of several personality disorders.Völlm and colleagues20 examined 8 patients with BPD or anti-social personality disorder (APD) or both (7 with BPD and 3with APD, with some overlap between disorders) andscanned them during a Go/No Go task in which participantshad to restrain their behaviour. They found that, whilehealthy control participants demonstrated activity in theirright dorsolateral and left orbitofrontal cortex, patients withimpulsive personality disorders exhibited more widespreadactivity, with more bilateral activation from their medial, su-perior and inferior frontal gyri to their anterior cingulate gyri.The implication of this study is that BPD patients may notonly demonstrate abnormal metabolism in normal cortical ar-eas but may also activate improper cortical areas entirely or,due to inefficient cortical processing, activate a wider corticalarea to achieve the same regulation.
As with neuroanatomy, metabolism in the brain has beenstudied with technologies other than fMRI and PET. Onesuch study was conducted by van Elst and others19 and usedmagnetic resonance spectroscopy to examine metabolites inthe brain as a measure of metabolism. Using short echo timesingle voxel spectroscopy, 12 female BPD patients with nodepression were found to have 19% reductions in N-acetyl-aspartate concentrations in the dorsolateral prefrontal cortex.Deficiency of this metabolite suggests a lower density of neu-rons and disturbed neuronal metabolism, consistent withresults obtained by other imaging techniques. These re-searchers examined only one frontal subregion and thuscould not comment on whether similar deficiencies might beobserved in other areas where abnormalities have beenlinked to BPD. Another technology that has been used tostudy BPD is brain perfusion single photon emission com-puted tomography (SPECT), which is particularly well suitedto observing local metabolism and is useful in differentiatingAlzheimer’s disease from strokes and other dementias.36 Us-ing SPECT, Goethals and colleagues15 demonstrated that pa-tients with BPD or ADP both show reduced regional cerebralblood flow in the right lateral temporal cortex and the polarand ventrolateral right prefrontal cortex. This study included2 disorders because its focus was to explain the impulsive be-haviours common to both, and it broadens the field of re-search by considering BPD in terms of symptoms that itshares with other very different disorders. Because this studyexcludes participants with comorbid axis I disorders, its gen-eralizability is limited.
If the study of neurological abnormalities of BPD can besaid to be in its early stages, the study of genes associatedwith BPD is even less advanced. The heritability of BPD hasbeen suggested to be moderate to high, based on findings ofconcordance between monozygotic twins in the area of 35%(examining 92 twin pairs) and dizygotic twins in the area of7% (examining 129 twin pairs),37 although previous studies
by the same researcher and with much smaller samplesfound no concordance between monozygotic twins.38 Currentresearch has suggested several promising directions for in-vestigating genetic causes of BPD, although presently no spe-cific genes have been clearly suspected as being causative.Because it is a disorder of great complexity commonly associ-ated with multiple comorbid conditions and is linked to envi-ronmental stressors, research on genetic factors has tended toinvestigate the genetic etiology of individual symptomsrather than the disease as a whole. Evidence suggests thatmany of the major symptoms or dimensions of BPD arehighly heritable, including impulsiveness39 and aggression.40
The genes that so far appear to be most persuasively linkedto BPD are involved in the serotonin system. In monkeys,low levels of serotonin metabolites in the cerebral spinal fluid(CBS) have been associated with unusually high impulsiveaggression and self-destructive behaviour, moderatedstrongly by the presence or absence of a nurturing atmos-phere and secure attachments.41 Monkeys with short allelesfor the serotonin 5-hydroxytryptamine (5-HT) transportergene 5-HTT appear to be at elevated risk of developingsymptoms analogous to BPD when taken from their naturalmothers and raised in nonnurturing environments (peergroups or an inanimate mother), an effect that is largelynegated when matched control monkeys are raised by theirown nurturing mothers.42
In humans, the gene-linked polymorphic region of the 5-HT transporter gene serotonin transporter gene promoterpolymorphism (5-HTTLPR) has been found to have shortand long alleles as well. The short allele has been associatedwith violent behaviour in humans by Retz and colleagues,43
who demonstrated that, among criminal offenders, violentoffenders were more likely to possess the short allele, al-though this accounted for only 5% of the variance of violentbehaviour. In people with eating disorders, the less efficientshort polymorphism has been found to be associated withhigher rates of comorbidity with BPD and aggressive impul-sivity in general.44 Steiger and colleagues reported that everyparticipant in their study with BPD had the short allele (al-though not all who had the short allele had BPD), and noparticipants with the long allele were found to have BPD co-morbid with their eating disorder. The 5-HTTLPR region isexpressed differently in different populations, and its associa-tion with BPD may be limited to certain diagnostic popula-tions (such as groups of patients with eating disorders) butstill has clear implications for the presence of BPD in a sizableclinical population. The effectiveness of selective serotoninreuptake inhibitors (SSRIs) such as fluoxetine in the treat-ment of mood shifts and depression in patients with BPDlends credence to researchers who argue that serotonin dys-function plays a role in BPD.45
Related to the serotonergic system, dopamine dysfunctionhas been suggested as a factor in BPD symptoms as well.Dopamine is thought to play a role in emotional informationprocessing and impulsivity, as well as in general cognition.Although evidence for dopamine dysfunction as a factor inBPD is mostly circumstantial, hyperactive dopamine functionhas been proposed as a potential cause of, for example,
hyperactive amygdala function, leading to emotional dysreg-ulation and negative reactions to social situations.46 Theremay be cause for future research to investigate dopamine’seffect on the development of BPD.
Genes involved in the production of monoamine oxidase-A (MAOA) may also be involved in the development of BPD.The MAOA gene encodes MAOA enzyme, a potent metabo-lizer of norepinepherine, serotonin and dopamine, amongother neurotransmitters. Caspi and colleagues47 demon-strated that people with genetic polymorphisms resulting inMAOA deficiency who are abused as children are signifi-cantly more likely to show criminal behaviour than are thosewho were also abused but had normal or elevated MAOAlevels; this indicates that MAOA may protect against nega-tive outcomes of childhood abuse. When BPD patients weretested for the MAOA gene, they were found to not differ sig-nificantly from healthy control subjects.48 The MAOA genecontinues to be of interest to researchers studying the devel-opment of aggression, impulsivity and criminality in abusedchildren.
Summary
In summary, research from a biological perspective has pro-vided several findings about BPD. PET studies have demon-strated that BPD patients show relatively low metabolism inthe dorsolateral frontal cortex, anterior cingulate cortex, basalganglia, thalamus, right-sided ventromedial temporal cortex,left-sided medial parietal/posterior cingulate cortex, hip-pocampus and left cuneus. Other studies have shown hyper-metabolism in the anterior cingulate gyrus, superior frontalgyrus, right inferior frontal gyrus and opercular part of theright precentral gyrus. PET studies have further shown hyper-activation of the bilateral dorsolateral prefrontal cortex andright cuneus and decreased activation in the medial prefrontalcortex in BPD patients who were presented with scripts ofabandonment. These data suggest that, in BPD patients, areasof the brain that are used to regulate and control emotion arehypometabolic and that activation of limbic areas, when it oc-curs, is excessive. This might reflect a failure of rationalthought to control emotional thought, leading to the emo-tional instability that is characteristic of BPD.
MRI studies have demonstrated that people with BPDhave reduced volume in the frontal lobe, bilateral hippocam-pus, bilateral amygdala (a reduced volume that has notalways been replicated in MRI studies), left orbitofrontal cor-tex, right anterior cingulate cortex, and right parietal cortexand increased putamen volume. In the cingulate gyrus ofpeople with BPD, the volume of which is generally shown tobe abnormal, Brodmann’s areas 24 and 31 showed reducedgrey and increased white matter volume; patients with BPDwithout comorbid SPD showed reduced grey matter in area24 but not 31; those with both BPD and SPD had reducedgrey matter volume in both areas. These data show abnor-malities in limbic structures, particularly areas involved innegative affect. Although causality cannot be inferred, thedata suggest that the anatomical changes are associated withthe physiological changes.
Lis et al
170 Rev Psychiatr Neurosci 2007;32(3)
Neuroimaging and genetics of BPD
J Psychiatry Neurosci 2007;32(3) 171
fMRI studies have demonstrated that people with BPDshow hypermetabolism in the amygdala bilaterally and ab-normal activation in the medial and inferolateral prefrontalcortex and fusiform gyrus in response to emotionally aver-sive slides. In response to faces, people with BPD show exces-sive activity in the amygdala, the bed nucleus of the striaterminalis, the lateral hypothalamic nuclei, the nucleus andthe frontal lobes. During recall of traumatic memories, pa-tients with BPD without PTSD have shown greater activationof the orbitofrontal cortex in both hemispheres and Broca’sarea, relative to patients with BPD and PTSD. These physio-logical data confirm and supplement PET data and again il-lustrate hyperactivation of limbic structures.
Other imaging technologies have demonstrated several ab-normalities. Patients with BPD show deficiencies in N-acetyl-aspartate concentrations in the dorsolateral prefrontal cortex,suggesting a lower density of neurons and disturbed neu-ronal metabolism (magnetic resonance spectroscopy). Inaddition, they show volume reductions in the basolateralamygdala (voxel-based morphometry). Finally, patients withBPD or APD show reduced regional cerebral blood flow inthe right lateral temporal cortex and the polar and ventrolat-eral right prefrontal cortex (SPECT), suggesting that these ar-eas are linked to impulsivity but that abnormalities thereinare not specific to BPD. These data supplement otheranatomical and physiological findings.
Research has most strongly implicated the serotonin trans-porter gene 5-HTT in the development of BPD, shorter allelesof which have been associated with lower levels of serotoninand greater impulsive aggression; genes for dopamine andMAOA may yet prove to have an etiological role. Geneticfindings further consolidate the evidence that there are bio-logical (not only psychological) differences between peoplewith and without BPD.
Discussion
Several possible issues are raised by this body of research.First, it is apparent that there is disagreement and sometimesoutright contradiction between different neuroimaging stud-ies, even between those using the same technology and theo-retically similar procedures. Studies select people with BPDon the assumption that such people represent the whole ofthe population. However, minute differences in samplingbias might considerably impact data obtained. For example,it remains a contentious issue in imaging whether patientswith common comorbidities should be included in studies.Understandably, someone with BPD and major depressionmight have different neuroanatomical abnormalities fromsomeone who has BPD and PTSD. Including people with co-morbid disorders makes it more difficult to attribute ob-served differences to a single disease; however, we wonderwhether it is possible for someone to have BPD without co-morbid depression, given the disrupted lifestyle and inter-personal stresses that these people have. It seems reasonableto suggest that a full understanding of BPD requires that pa-tients with comorbid disorders be included, and there ap-pears to be a general trend in research to include such
patients. Other possible sources of conflicting data might in-clude such confounds as, for example, how to persuade aclinically impulsive patient to lie still while an image is taken,and if they move, might this result in minute (or large) differ-ences? Given the variety of factors that might influence theresults of a neuroimaging study, it may not be a surprise tosee even completely opposing results. Such confusion under-scores the importance of replication in this area. Future meta-analyses should attempt to remove interstudy variability byapplying statistical techniques that take sample size (and thequestion of inadequate sampling) into account, particularlygiven the small sample sizes common to costly and time-consuming neuroimaging studies.
Imaging technology has shown that structures that havereduced volume in BPD patients may show hypermetabo-lism. Perhaps some of the lost volume in these structures (no-tably, the amygdala) may be lost inhibitory neurons, and thislost inhibition could result in impulsive behaviour and overlynegative attributions. An apt analogy may be that of a horseand rider: in BPD patients, affective brain structures (thehorse) run wild, while the cognitive areas (the rider) areasleep, paralyzed or otherwise unable to reign in this excessactivity.
We also wonder whether different developmental abnor-malities may lead to different clinical manifestations of BPDand, specifically, if chronic versus acute abuse in childhoodmay be associated with different imaging abnormalities inadulthood.
What do the neuroimaging findings mean? How can werelate the structural and functioning abnormalities of theamygdala with the functional abnormalities of the frontalcortex? Is it possible that the limbic overreactivity over-whelms the frontal cortex, shutting it off? Alternatively,could the absence of frontal cortex restraints create a voidcompensated for by an overactive amygdala? Answeringthese questions requires the integration of findings fromgenetic and endophenotypic analyses. For example, impul-sivity, aggression and nonwelfare affect are cardinal compo-nents of the BPD endophenotype. Although it has beenhypothesized that we can link those components to a commongenetic coding for serotonin, a definitive model of this linkhas not yet been devised; we are only in the beginning stagesof neuroimaging.
To determine what research design would help advanceour understanding of this disorder across the lifespan, wemust reconcile the tension between examining the broadersyndrome under investigation and the symptoms associatedwith that disorder. If the chosen strategy were to first focuson the syndrome, we risk losing sight of the symptoms. Itmight be wiser to study the syndrome’s specific componentswith the intent of examining all possible evidence before de-ciding how to proceed. That approach would argue in favourof a continued thrust to further study such BPD symptoms asimpulsivity. Such an approach gains support from a geneticperspective, because genes appear to be more proximally re-lated to symptoms than to the broader endophenotypes.
Accordingly, an ideal research design would include con-sideration of molecular genetics, fMRI findings and a charac-
Lis et al
172 Rev Psychiatr Neurosci 2007;32(3)
terization of symptoms. Choosing a comparison groupwould require consideration of potential confounds andwhether it would be more productive to compare BPD withanother syndrome (e.g., depression) with the risk of substan-tial endophenotypic overlap, or to another symptom, withthe risk of genetic overlap. Whichever approach is taken, ef-forts should be made to represent as many endophenotypicvariants as possible, with a preparedness to measure each ge-netically and via neuroimaging.
There are advantages and disadvantages to approachingthe study of BPD in terms of its individual symptoms or as asyndrome. Because BPD is a complex disorder with a rangeof common manifestations, it can be tempting to attempt tobreak the disorder down and, for example, study it in termsof impulsivity alone. This is an approach that lends itself wellto research, since it is often easier to quantify a participant’simpulsivity than it is to establish a confident diagnosis of apersonality disorder. Further, a study that examines onesymptom of a larger disorder has the opportunity to establishfindings or suggest implications regarding other disordersthat may share that symptom (as demonstrated by authorswhose studies of BPD have given insight into APD as well).There are, however, drawbacks to this approach. BPD is acollection of symptoms, and focusing exclusively on any onesymptom at the expense of others has the risk of collectingdata that may miss some insight. Studying impulsivity in aperson with BPD may fail to uncover results related to the in-teraction of impulsivity with depression. An impulsive per-son with BPD might indulge in self-harm, whereas someonewith APD does not, which suggests that the same basicsymptom (and presumably similar neuroanatomical dysfunc-tion) manifests differently because it interacts with othersymptoms, such as depression or self-loathing. To create afull picture of this disorder, it is necessary to study BPD asboth a syndrome and through individuals’ symptoms.
Another important question raised by this research iswhether there are neuroanatomical differences between pa-tients who remit at different times? Few neuroimaging or ge-netic studies include a longitudinal component, often becausenot enough time has passed for a longitudinal component tobe meaningful. Links and Heslegrave49 found that, after 10years, roughly one-half of BPD patients remit. Paris50 foundthat this rate increased with age: by age 40 years, most BPDpatients no longer met the criteria for the disorder. Most par-ticipants in the research we examined were aged between 20and 30 years, so it is easy to imagine that some of them mighthave been nearer to remission than others. This caused us towonder whether it could have influenced the results, orwhether the severity of neuroanatomical abnormalitieschange over time as people overcome their symptoms. Itwould be interesting for future studies to return to their par-ticipants after 2 years and examine who, if anyone, no longermeets diagnostic criteria.
Most BPD research to date has focused on adults and, bydefinition, BPD emerges in late adolescence or early adult-hood.31 BPD-like symptoms in children are often classified asborderline syndrome of childhood rather than BPD, and incertain cases, the child might more appropriately be labelled
by another name.51 Future research exploring BPD-likesymptoms in younger patients will contribute to an under-standing of this disorder and its development. Further, itmay be useful to researchers who study the neurological andgenetic etiology of BPD to explore whether the known ab-normalities are exclusive to adults with BPD or are found inchildren as well.
References
1. Torgersen S. Epidemiology. In: Oldham JM, Skodol AE, BenderDS, editors. Textbook of Personality Disorders. Arlington: AmericanPsychiatric Publishing; 2005. p. 129-41.
2. Gunderson JG. Borderline personality disorder: a clinical guide. Wash-ington: American Psychiatric Press; 2001. p. 37.
3. Skodol AE, Gunderson JG, Pfohl B, et al. The borderline diagnosisI: psychopathology, comorbidity, and personality structure. BiolPsychiatry 2002;51:936-50.
4. Brambilla P, Soloff PH, Sala M, et al. Anatomical MRI study of bor-derline personality disorder patients. Psychiatry Res 2004;131:125-33.
5. Driessen M, Herrmann J, Stahl K, et al. Magnetic resonance imag-ing volumes of the hippocampus and the amygdala in womenwith borderline personality disorder and early traumatization.Arch Gen Psychiatry 2000;57:1115-22.
6. Hazlett EA, New AS, Newmark R, et al. Reduced anterior and pos-terior cingulate grey matter in borderline personality disorder. BiolPsychiatry 2005;58:614-23.
7. Irle E, Lange C, Sachsse U. Reduced size and abnormal asymmetryof parietal cortex in women with borderline personality disorder.Biol Psychiatry 2005;57:173-82.
8. Lyoo IK, Han MH, Cho DY. A brain MRI study in subjects withborderline personality disorder. J Affect Disord 1998;50:235-43.
9. Rusch N, van Elst LT, Ludaescher P, et al. A voxel-based morpho-metric MRI study in female patients with borderline personalitydisorder. Neuroimage 2003;20:385-92.
10. Schmahl CG, Elzinga BM, Vermetten E, et al. Neural correlates ofmemories of abandonment in women with and without borderlinepersonality disorder. Biol Psychiatry 2003;54:142-51.
11. Tebartz van Elst L, Hesslinger B, Thiel T, et al. Frontolimbic brainabnormalities in patients with borderline personality disorder: avolumetric magnetic resonance imaging study. Biol Psychiatry2003;54:163-71.
12. De la Fuente JM, Goldman S, Stanus E, et al. Brain glucose metabo-lism in borderline personality disorder. J Psychiatr Res 1997;31:531-41.
13. Donegan NH, Sanislow CA, Blumberg HP, et al. Amygdala hyper-reactivity in borderline personality disorder: implications for emo-tional dysregulation. Biol Psychiatry 2003;54:1284-93.
14. Driessen M, Beblo T, Mertens M, et al. Posttraumatic stress disor-der and fMRI activation patterns of traumatic memory in patientswith borderline personality disorder. Biol Psychiatry 2004;55:603-11.
15. Goethals I, Audenaert K, Jacobs F, et al. Brain perfusion SPECT inimpulsivity-related personality disorders. Behav Brain Res 2005;157:187-92.
16. Herpertz SC, Dietrich TM, Wenning B, et al. Evidence of abnormalamygdala functioning in borderline personality disorder: a func-tional MRI study. Biol Psychiatry 2001;50:292-8.
17. Juengling FD, Schmahl C, Hesslinger B, et al. Positron emission to-mography in female patients with borderline personality disorder.J Psychiatr Res 2003;37:109-15.
Acknowledgements: We acknowledge McGill University and theCanadian Institutes of Health Research (CIHR) for funding this pro-ject via the CIHR Health Professional Student Research bursary.
Competing interests: None declared.
Contributors: Mr. Lis and Dr. Greenfield designed the study. Mr. Lisand Drs. Greenfield and Guilé aquired the data; Mr. Lis, Ms. Henryand Dr. Dougherty analyzed the data. Dr. Lis and Dr. Greenfieldwrote the article, and all authors revised it. All authors gave final ap-proval for the article to be published.
Neuroimaging and genetics of BPD
J Psychiatry Neurosci 2007;32(3) 173
18. Lange C, Kracht L, Herholz K, et al. Reduced glucose metabolismin temporo-parietal cortices of women with borderline personalitydisorder. Psychiatry Res 2005;139:115-26.
19. van Elst LT, Thiel T, Hesslinger B, et al. Subtle prefrontal neu-ropathology in a pilot magnetic resonance spectroscopy study inpatients with borderline personality disorder. J NeuropsychiatryClin Neurosci 2001;13:511-4.
20. Völlm B, Richardson P, Stirling J, et al. Neurobiological substratesof antisocial and borderline personality disorder: preliminary re-sults of a functional fMRI study. Crim Behav Ment Health 2004;14:39-54.
21. Bear MF, Connors BW, Paradiso MA. Neuroscience: exploring thebrain. 2nd ed. Baltimore: Lippincott, Williams and Wilkins; 2001.p. 443-4.
22. Andrulonis PA, Glueck BC, Stroebel CF, et al. Organic brain dys-function and the borderline syndrome. Psychiatr Clin North Am1981;4:47-66.
23. van Reekum R, Conway CA, Gansler D, et al. Neurobehavioralstudy of borderline personality disorder. J Psychiatry Neurosci1993;18:121-9.
24. van Reekum R, Links PS, Finlayson MAJ, et al. Repeat neurobe-havioral study of borderline personality disorder. J Psychiatry Neu-rosci 1996;21:13-20.
25. Snyder S, Pitts WM Jr, Gustin Q. CT scans of patients with border-line personality disorder. Am J Psychiatry 1983;140:272.
26. Schulz SC, Koller MM, Kishore PR, et al. Ventricular enlargementin teenage patients with schizophrenia spectrum disorder. Am JPsychiatry 1983;140:1592-5.
27. Adamec RE, Stark-Adamec C, Saint-Hilaire JM, et al. Basic scienceand clinical aspects of procaine HCl as a limbic system excitant.Prog Neuropsychopharmacol Biol Psychiatry 1985;9:109-19.
28. Zanarini MC, Kimble CR, Williams AA. Neurological dysfunctionin borderline patients and axis II control subjects. In: Silk KR, edi-tor. Biological and Neurobehavioral studies of borderline personality dis-order. Washington: American Psychiatric Press; 1994. p. 159-75.
29. Meares R, Melkonia D, Gordon E, et al. Distinct pattern of p3aevent-related potential in borderline personality disorder. Neurore-port 2005;16:289-93.
30. American Psychiatric Association. Diagnostic and statistical manual ofmental disorders. 3rd ed, revised. Washington: The Association; 1987.
31. American Psychiatric Association. Diagnostic and statistical manualof mental disorders. 4th ed. Washington: The Association; 1994.
32. Goyer PF, Andreason PJ, Semple WE, et al. Positron-emission to-mography and personality disorders. Neuropsychopharmacology1994;10:21-8.
33. Na C, Doraiswamy PM, Lee KH, et al. Magnetic resonance imag-ing in biological psychiatry. Prog Neuropsychopharmacol Biol Psychi-atry 1991;15:581-93.
34. American Psychiatric Association. Diagnostic and statistical manual
of mental disorders. 3rd ed. Washington: The Association; 1980.35. Damasio AR, Tranel D, Damasio H. Individuals with sociopathic
behavior caused by frontal damage fail to respond autonomicallyto social stimuli. Behav Brain Res 1990;41:81-94.
36. Dougall NJ, Bruggink S, Ebmeier KP. Systematic review of the di-agnostic accuracy of 99mTc-HMPAO-SPECT in dementia. Am JGeriatr Psychiatry 2004;12:554-70.
37. Torgersen S, Lygren S, Oien PA, et al. A twin study of personalitydisorders. Compr Psychiatry 2000;41:416-25.
38. Torgersen S. Genetic and nosological aspects of schizotypal andborderline personality disorders: a twin study. Arch Gen Psychiatry1984;41:546-54.
39. Coccaro EF, Bergeman CS, Kavoussi RJ. Heritability of aggressionand irritability: a twin study of the Buss-Durkee aggression scalesin adult male subjects. Biol Psychiatry 1997;41:273-84.
40. Coccaro EF, Bergeman CS, McClearn GE. Heritability of irritableimpulsiveness: a study of twins reared together and apart. Psychia-try Res 1993;48:229-42.
41. Gabbard GO. Mind, brain, and personality disorders. Am J Psychia-try 2005;162:648-55.
42. Bennett AJ, Lesch KP, Heils A, et al. Early experience and sero-tonin transporter gene variation interact to influence primate CNSfunction. Mol Psychiatry 2002;7:118-22.
43. Retz W, Retz-Junginger P, Supprian T. Association of serotonintransporter promoter gene polymorphism with violence: relationwith personality disorders, impulsivity, and childhood ADHDpsychopathology. Behav Sci Law 2004;22:415-25.
44. Steiger H, Joober R, Israël M, et al. The 5HTTLPR polymorphism,psychopathologic symptoms, and platelet [3H-] paroxetine bind-ing in bulimic syndromes. Int J Eat Disord 2005;37:57-60.
45. Goodman M, New A, Siever L. Trauma, genes, and the neurobiol-ogy of personality disorders. Ann N Y Acad Sci 2004;1032:104-16.
46. Friedel RO. Dopamine dysfunction in borderline personality disor-der: a hypothesis. Neuropsychopharmacology 2004;29:1029-39.
47. Caspi A, McClay J, Moffitt TE, et al. Role of genotype in the cycleof violence in maltreated children. Science 2002;297:851-4.
48. Posner MI, Rothbart MK, Vizueta N, et al. An approach to thepsychobiology of personality disorders. Dev Psychopathol 2003;15:1093-106.
49. Links PS, Heslegrave RJ. Prospective studies of outcome. Under-standing mechanisms of change in patients with borderline per-sonality disorder. Psychiatr Clin North Am 2000;23:137-50.
50. Paris J. Implications of long-term outcome research for the man-agement of patients with borderline personality disorder. Harv RevPsychiatry 2002;10:315-23.
51. Ad-Dab’bagh Y, Greenfield B. Multiple complex developmentaldisorder: the “multiple and complex” evolution of the “childhoodborderline syndrome” construct. J Am Acad Child Adolesc Psychiatry2001;40:954-64.
CANADIAN COLLEGE OF NEUROPSYCHOPHARMACOLOGY
30TH ANNUAL SCIENTIFIC MEETING
Banff, AlbertaJune 15–19, 2007
Banff Conference Centre
The 2007 Annual Meeting of the Canadian College of Neuropsychopharmacology will be held June 15th to June 19th,2007, at the Banff Conference Centre in beautiful Banff, Alberta, Canada (www.banffcentre.ca).
For further information and contacts, see our Web site (www.ccnp.ca).