Parental Burden Associated with Borderline Personality Disorder in Female Offspring
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Parental Burden Associated with Borderline Personality Disorder in Female Offspring
59
Journal of Personality Disorders, 25(1), 59–74, 2010© 2011 The Guilford Press
From James J. Peters Veterans Affairs Medical Center, Mount Sinai School of Medicine.
Address correspondence to Marianne Goodman, MD, James J. Peters Veterans Affairs Medi-cal Center, 130 W. Kingsbridge Rd., Bronx, NY 10468; E-mail: [email protected]
Parental Burden associated with Borderline Personality disorder in Female oFFsPring
Marianne Goodman, MD, Uday Patil, MA, Joseph Triebwasser, MD, Perry Hoffman, PhD, Zachary A. Weinstein, BA, and Antonia New, MD
To identify aspects of parental burden associated with borderline per-sonality disorder (BPD), an anonymous internet survey linked to BPD support websites was developed for parents to complete on their BPD offspring and unaffected siblings. The questions cover aspects of the child’s life from pregnancy through young adulthood, and query about the impact of the child’s BPD on six domains of the parent’s life, includ-ing physical and emotional health, marriage, job, standard of living, social life, and career trajectory. Additionally, financial burden was as-sessed with questions pertaining to insurance and out-of pocket costs associated with the BPD disorder. BPD offspring were identified by meeting diagnostic criteria embedded within the survey and having been given a diagnosis of BPD by a professional at some point in their life. We report on 233 female offspring meeting strict criteria for BPD. Par-ents of daughters with BPD endorsed varying levels of impact on the six domains comprising burden with the largest impact on emotional health which was impacted in over 88% of the respondents. Over 50% of parents endorsed four or greater of the six burden items. Particular aspects of the offspring’s BPD symptom profile correlated with intensity of parental burden included including problems in adolescence with acting out behavior (p < .000), property destruction (.003), delusional symptoms (.007), and hallucinatory symptoms (.008). A subgroup of respondents provided data on specific financial ex-penses. The average and median out-of-pocket expense was $60,087, and $10,000. Insurance costs totaled an average of $108,251 with a mean of $20,000. The average cost per year after diagnosis was $14,606 out-of-pocket and $45,573 billed to insurance. The median cost per year after diagnosis was $3,667 out-of-pocket, and $12,500 billed to insurance. After adjusting for household income, a female proband who had been raped incurred roughly $40,000 more in BPD-related costs, while a diagnosis of conduct disorder led to about $50,000 in addi-tional costs. Parents of female offspring with BPD experience burden in multiple
60 GOODMAN ET AL.
domains of their life and many have incurred substantial financial ex-pense. Increasing awareness of co-morbid conditions in the BPD pro-band that significantly increase parental burden may be indicators for the provision of increased family support.
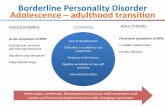
Borderline personality disorder (BPD) is a debilitating illness marked by emotional dysregulation, stormy relationships, suicidal tendencies, and overt physical and/or verbal aggression (DSM-IV, 1994) as well as fre-quently poor functional outcomes (Bagge et al., 2004). Because of this, the disorder poses profound challenges to families of afflicted individuals. A detailed description and the expense of this burden has not been exten-sively investigated in family members of BPD patients. There is, however, a wealth of literature that examines the stress on family members who provide care for individuals with severe mental illness (Baronet, 1999; Harvey, Burns, Fahy, Manley, & Tattan, 2001; Liu et al., 2007; Ostman & Hansson, 2004; Tsang, Tam, Chan, & Cheung, 2003; Veltman, Cameron, & Stewart, 2002). More specifically, the relationship between dimensions of family care giving and care giving distress has been assessed in depres-sion (van Wijngaarden, Schene, & Koeter, 2004) and schizophrenia (Schene, van Wijngaarden, & Koeter, 1998) suggesting that overall care-taking scores were related to patient symptomatology and number of con-tact hours between patient and caregiver.
Family burden (FB) has traditionally been defined as either objective or subjective (Hoenig & Hamilton, 1966). Objective FB refers to the daily re-sponsibilities incumbent on family members caring for the relative, while subjective FB refers to how family members feel about their role as care-givers. Generally, the FB literature has been either exploratory in nature or has assessed burden through specific models of coping strategies. While many of the findings have been inconsistent due to varying ap-proaches, there have been a few salient conclusions. First, caretaker bur-den has been correlated with high levels of psychological distress (Coyne et al., 1987; Noh & Turner, 1987; Szmukler et al., 1996; Baronet, 1999). Second, the burden of the caretaker is greater if his appraisal of this role is negative (Ostman & Hansson, 2004).
Baronet’s literature review reported that subjective FB is often due to the disruptive behaviors of the patient and that patient’s symptomatology is a reliable predictor of FB (Baronet, 1999). However, Harvey et al. found that disruptive behavior is not positively correlated with the caregiver’s appraisal of burden (Harvey et al., 2001). Using the stress-coping model (Szmukler et al., 1996), Harvey et al. (2001) reported that the caregiver’s appraisal was more negative if the patient could not perform expected du-ties (e.g., if there was unemployment and poor social functioning). Tsang et al. (2003) reported that FB results from financial burden, social stigma, and lack of appropriate healthcare facilities.
PARENTAL BURDEN 61
There is limited literature that specifically assesses the FB associated with caring for BPD patients. Hoffman, Buteau, Hooley, Fruzzetti, and Bruce (2003) found that family members who are more knowledgeable re-garding BPD tend to experience more FB, depression, and levels of dis-tress while caring for a family member with BPD. Schiers and Bok (2007) reported that caretakers of BPD patients score higher on all symptom di-mensions of the Symptom Checklist (SCL-90) when compared to the gen-eral population. Gunderson and Lyoo (1997) reported that individuals with BPD rated their family environments more negatively than a com-parison group without BPD, but this negative family perception was not found for the parents of offspring with BPD who rated their family envi-ronment similar to normative families. Given the known difficulties inher-ent in this disorder for patients and clinicians (Gunderson, 2009), it is surprising that little has been written regarding family burden in BPD and highlights the need for additional research.
The present study investigates subjective FB through the use of an on-line questionnaire. Respondents were parents of probands diagnosed with BPD. We created our own burden assessment measure in order to gather information not currently available in existing scales (e.g., financial im-pact) and to accommodate the use of the internet to gather survey respon-dents. The survey was created to measure the level of burden experienced by the family members who care for BPD patients and to determine cor-relates of FB in BPD. To our knowledge, the present study is the first to examine BPD-associated FB in BPD and to examine the impact of off-spring’s BPD on varying facets of parental life including marriage, physi-cal and emotional health, standard of living, social life, and career trajec-tory. In addition, the survey assessed an array of child and adolescent experiences of the proband in efforts to question whether the presence of particular developmental events preceding the diagnosis of BPD influence family burden, an area about which virtually nothing is known. Such in-formation may help direct attention to the need for additional family sup-port during these high-risk times. Data also was collected on out-of pock-et and insurance costs for treatment of the BPD proband.
Recent studies support the reliability and validity of utilizing the Inter-net for data collection (Gosling, Vazire, Srivastava, & John, 2004; Miller et al., 2002), as well as the effectiveness of polling adult participants over the Internet (Alexander & Trissel, 1996; Bäckström, 2007; Rochlen, McKelley, Suizzo, & Scaringi, 2008; Srivastava, John, Gosling, & Potter, 2003). While we relied solely on parents’ reports of their children, we believe this has provided us with reliable data, as evidenced by numerous studies demon-strating a high level of agreement between parental ratings of their chil-dren’s behavior and the behaviors and feelings the children truly exhibit, especially in instances of disordered behavior (Cantwell, Lewinsohn, Rohde, & Seeley, 1997; Hartung, McCarthy, Milich, & Martin, 2005; Sourander & Piha, 1997).
62 GOODMAN ET AL.
methodsWe developed a forty-five minute, anonymous Internet survey containing approximately 109 questions for parents to complete on their BPD off-spring. A link to the survey was located on the website of the National Education Alliance for Borderline Personality Disorder (NEA-BPD), an or-ganization offering support and educational services to families of BPD patients. The website contains over 179 pages and an extensive library of audio and video presentations by noted researchers in the field, and at-tracts approximately 7,821 unique visitors per month. Visitors from the 50 United States and 100 non-U.S. countries have used the site.
To solicit participants, a recruiting message was used on a prominent part of the NEA-BPD home page. The message asked parents to “share your family’s unique experience with BPD in order to help researchers ex-ploring early symptoms of the disorder and the impact of a child’s BPD.” Potential respondents clicked on a button and were taken to SurveyMon key.com, where the actual survey was situated. SurveyMonkey is a widely accepted tool for self-administered electronic surveys and facilitated data collection. Respondents supplied no identifying data. The first page de-scribed the survey, intent of the research and provided contact phone numbers for questions. Respondents could only proceed to the actual sur-vey if they designated a willingness to participate on a consent form.
Embedded within the survey was a diagnostic screen adapted from the ten-item McLean Screening Instrument for Borderline Personality Disor-der (MSI-BPD; Zanarini et al., 2003). In individuals with treatment histo-ries, MSI-BPD scores of seven and above yield good sensitivity (.81) and specificity (.85; Zanarini et al., 2003). In order to achieve the desired spec-ificity for BPD proband cases, we required both a score of seven or above on the MSI-BPD and a formal diagnosis of BPD by a professional at some point in the proband’s life. Data about offspring who had been given a di-agnosis of BPD in the past but who scored six or below on the MSI- BPD, as well as data about offspring without a formal BPD diagnosis but who scored seven or above on the MSI-BPD screen, were not analyzed. Surveys containing less than an 80% completion rate were discarded.
The survey contained questions on various clinical features, psychiatric and medical history, and family burden. Questions on various aspects of clinical features were sorted into four distinct developmental periods of the child’s life: birth, infancy, & toddlerhood (less than 5 years old), child-hood (between 5 and 13), and adolescence (between 14 and 19). The birth epoch consisted of two items inquiring about difficult pregnancy and/or labor. The infancy & toddlerhood epoch consisted of questions on affective lability (e.g., unusual moodiness), developmental delay (e.g. social delay in preschool, and separation anxiety (e.g., inability to self-soothe). An exam-ple question read, “Did you notice anything unusual during the first year, such as the inability to self-soothe?” The childhood epoch included ques-tions regarding academic difficulties (e.g., poor grades, special education),
PARENTAL BURDEN 63
interpersonal problems (e.g., few friends, conflict with authority, bully perpetrator), and affective lability, among others. The adolescent epoch included questions on impulsive behavior (e.g., promiscuity), victimization (e.g., rape, assault), self-harm (e.g., cutting, suicide attempt), self-image concerns (e.g., anorexia), psychotic features (e.g., hallucinations), inter-personal problems, and affective lability.
Questions pertaining to psychiatric and medical history included items on evaluation, assessment, and treatment. Furthermore, respondents were asked to rate their satisfaction with the proband’s overall clinical treatment and overall health. Both items were rated on five-point Likert scales, and were rated as (1) Very Satisfied, (2) Satisfied, (3) Neutral, (4) Unsatisfied, or (5) Very Unsatisfied. An overall satisfaction index was cre-ated from the two individual items.
FB-related questions specifically queried on the impact of the child’s ill-ness on the respondent’s marriage, physical health, emotional health, standard of living, social life, and career trajectory. These items were open to the interpretation of the respondent, as no clarifying or prompting in-formation was provided alongside the question. A burden severity index was calculated by adding the number of individual FB items that were endorsed. Respondents were also queried on expenses (out-of-pocket and insurance) related to the proband’s illness. While costs were not assigned to any specific categories, we assumed that approximately 54% of the stat-ed costs were secondary to psychiatric hospitalization fees, based on a report by van Asselt, Dirksen, Arntz, and Severens (2007).
Statistical Package for Social Sciences (SPSS, version 16) was used for statistical analyses. Data analysis included descriptive statistics aggregat-ing and summarizing item responses, and nonparametric partial correla-tions between burden intensity and individual survey items. Separate analyses were conducted to assess costs associated with BPD. Data was drawn from ANOVA techniques, grouped by clinical variables, and run on cost figures. These figures were first log-transformed, making the skewed distribution more symmetric. All significance tests run were two-tailed and tested against a .01 significance level. More conservative techniques, such as the Bonferroni or Holm-Bonferroni correction, were found to be overly restrictive of the significance test results. However, we see the need for correction during multiple comparisons, and this self-derived correc-tion level was used to reduce the familywise error rate while allowing us meaningful results.
resultsWhile 950 surveys were completed, only 711 had usable data. Surveys with incomplete responses were excluded. Of the 711 surveys, 566 per-tained to female probands. Of these 566, 233 were defined as having strictly defined BPD; i.e., had been given a BPD diagnosis by a profes-
64 GOODMAN ET AL.
sional and scored seven or higher on the MSI-BPD. A total of 333 cases did not meet these criteria; i.e., they either had (1) an official, profession-ally-given, lifetime diagnosis of BPD but a sub-threshold score on the MSI-BPD, or (2) an above-threshold score on the MSI-BPD, but have not been given a lifetime diagnosis of BPD, or (3) neither an official diagnosis of BPD nor a threshold score on the MSI-BPD. Approximately 1 in 40 com-pleted surveys yielded a male BPD proband. These numbers are insuffi-cient for detailed statistical analyses at this time.
SAMPLE
The 233 BPD female probands had a mean age of 24.2 years old, with a median age of 22 and range of 12 to 55 years old. The mean age of BPD diagnosis by a professional was 20.0 years old, with a median age of 18 and a range of 10 to 47 years old. Female probands met an average of 8.77 MSI-BPD screen items. They had been psychiatrically hospitalized an av-erage of 3.4 times; 94.4% of the sample had had at least one psychiatric hospitalization. Female proband characteristics are summarized in Table 1. Co-morbid disorders are presented in Table 2.
Parents completing the surveys were primarily female (94.6%) with a mean age of 51.3 +/- 8.8 years old. They were predominantly white (91.6%), married (66.4%), and Christian (73.5%). Approximately 1/3 had college degrees and 52.9% had annual household incomes greater than $75,000 (see Table 3). Ninety-six point 4 percent were the biological parent.
taBle 1. Proband characteristics
Age n = 229 Mean 24.17 SD 8.49 Median 22.00 Range 12–55Age at BPD Dx n = 151 Mean 20.00 SD 6.01 Median 18.00 Range 10–47MSI-BPD Items n = 233 Mean 8.77 SD 1.05 Median 9.00 Range 7–10Hospitalizations n = 233 Mean 3.40 SD 3.62 Median 3.00 Range 0–25 % with at least one 94.4Suicide Attempts n = 92 Mean 3.14 SD 3.47 Median 2.00 Range 1–24
Note. Figures are drawn from the number of valid responses within the total sample of 233 unique responses.
PARENTAL BURDEN 65
FAMILY PSYCHIATRIC HISTORY CHARACTERISTICS
Respondents noted high levels of psychiatric history in family members. This included lifetime rates of Major Depressive Disorder (58.8%), Bipolar Disorder (31.3%), Substance Abuse or Dependence (47.2%), and personal-ity disorder (15.9%). Thirty point 5 percent reported family members who had lifetime histories of psychiatric hospitalization. The survey neither as-sessed the relationship of a psychiatrically ill family member to the pro-band, nor measured whether the family member was a first- or second-degree relative.
PARENTAL SATISFACTION
Parents were not satisfied with clinical treatment or with their children’s overall psychiatric health (see Table 4). On average, respondents rated their satisfaction with clinicians with a score of 3.24 (Unsatisfied to Neu-tral), and their satisfaction with their child’s health with a score of 3.67 (Unsatisfied to Neutral). 37.9% of respondents were either Unsatisfied or Very Unsatisfied with the circumstances.
taBle 2. lifetime Psychiatric disordersin Female BPd offspring (n = 233)
Major Depressive Disorder 77.7% n = 181Bipolar Disorder 57.1% n = 133Psychotic Spectrum Disorders 7.7% n = 18Anxiety Disorders 49.4% n = 115Attention-Deficit/Hyperactivity Disorder 33.9% n = 79Oppositional Defiant Disorder 15.5% n = 36Conduct Disorder 8.2% n = 19
taBle 3. Parent demographics
Age n = 221 Mean 51.32 SD 8.82 Range 32–79Gender n = 224 Female 94.6% n = 212Relationship n = 221 Birth Parent 96.4% n = 213Marital n = 226 Married 66.4% n = 150 Divorced: 16.4% n = 37Income n = 215 <25K 9.8% n = 21 25–50K 18.1% n = 39 50–75K 19.1% n = 41 75–100K 20.9% n = 45 100–200K 20.9% n = 45 200K+ 11.1% n = 24Education n = 224 HS Diploma or Less 10.7% n = 24 Some College 28.6% n = 64 College Degree 34.4% n = 84 Graduate Degree 26.3% n = 59Race n = 226 White 91.6% n = 207Religion n = 223 Christian 73.5% n = 164Immigrant n = 226 Immigrant 6.2% n = 14
Note. Figures are drawn from the number of valid responses within the total sample of 233 unique responses.
66 GOODMAN ET AL.
PARENTAL BURDEN
Parents endorsed varying levels of impact of their child’s BPD on the six domains comprising burden, including marriage, physical health, stan-dard of living, social life, career trajectory, and emotional health (see Table 4). Emotional health was affected most severely, with over 88% of survey completers endorsing this item, while physical health strain was reported by over 58% of respondents. Deleterious impact on relationships was also pronounced, with over 56% noting effects on their marriage and slightly over 59% reporting a burden on their social life. Financial burden, mea-sured by an impact on standard of living, was noted by 44.2% of respon-dents, while an impact on one’s career trajectory was described by slightly over 36%. Over 53% of the respondents selected four or more individual burden items, and one third endorsed five or more individual burden items, suggesting that having offspring with BPD influences multiple fac-ets of parental life.
Individual items of mental health symptomatology for each epoch, in-cluding birth, infancy/toddlerhood, childhood, and adolescence were cor-related with overall severity of burden to identify particularly strong cor-relates of parental burden. Covariates included age of child, age of parent, income bracket, and education bracket. As expected, there were no sig-nificant correlations for any items during the birth, infancy/toddlerhood, and childhood epochs. During adolescence, however, several items were correlated with intensity of parental burden (see Table 5), including prob-
taBle 4. Parental Burden (n = 233)
Burden Items Marriage 56.2% n = 131 Physical Health 58.4% n = 136 Standard of Living 44.2% n = 103 Social Life 59.2% n = 138 Career Trajectory 36.5% n = 85 Emotional Health 88.8% n = 207Severity Index Number of total items endorsed None 6.0% n = 14 1 13.7% n = 32 2 10.7% n = 25 3 15.9% n = 37 4 20.2% n = 47 5 21.0% n = 49 All 6 12.4% n = 29Satisfaction Scales Clinician Satisfaction How satisfied have you been with Mean: 3.24 “Unsatisfied” this child’s clinicians? S.D.: 1.18 to “Neutral” n = 221 Median: 3 “Neutral”Proband Satisfaction Overall satisfaction with child Mean: 3.67 “Unsatisfied” S.D.: 0.97 to “Neutral” n = 230 Median: 4 “Unsatisfied”
Note. Satisfaction Scale is rated as follows: (1) Very Satisfied; (2) Satisfied; (3) Neutral; (4) Unsatisfied; (5) Very Unsatisfied
PARENTAL BURDEN 67
lems with acting out behavior (p < .000), property destruction (.003), delu-sional symptoms (.007), and hallucinatory symptoms (.008). Trend-level correlations were also found between burden and adolescent verbally abu-sive behavior (.015), anorexia (.018), and homicidality (.019). Surprisingly, correlations with items pertaining to suicidality, self-injury, and victimiza-tion were not significant. Burden severity was, however, correlated with bipolar disorder comorbidity (.000).
Clinical satisfaction and burden severity were negatively correlated (.002), indicating that the greater the dissatisfaction with clinical treat-ment quality and accessibility, the greater the perceived parental burden. Moreover, burden severity and family expenditures related to BPD were highly correlated (.004).
taBle 5. Partial correlations Between diagnoses/clinicalFeatures and Burden severity index (n = 204)
item correlation significance
Lifetime Diagnoses Bipolar Disorder .246 .000** ADHD .175 .012* Anxiety Disorders .148 .034* Psychotic Spectrum Disorders .118 .090 Oppositional Defiant Disorder .070 .317 Major Depressive Disorder .062 .374 Conduct Disorder .059 .403Clinical Features in Adolescence Acting Out .252 .000** Property Destruction .206 .003** Delusions .187 .007** Hallucinations .183 .008** Verbally Abusive .170 .015* Anorexic Features .165 .018* Homicidality .163 .019* Impulsivity .116 .096 Rape Victim .095 .176 Alcohol or Substance Abuse .091 .194 Bulimic Features .083 .236 Aggression .083 .237 Violence Victim -.071 .311 Promiscuity .058 .404 Suicidality .054 .443 Thoughts .061 .381 Threats .104 .136 Plans .112 .110 Attempts .046 .512 Animal Cruelty .050 .472 Pregnancy -.045 .516 Deliberate Self-Harm .044 .530 Cutting .1187 .091 Burning –.010 .8887 Head Banging -.095 .176 Fighting .039 .583 Police Arrests .032 .652 STIs .026 .711
Note. Covariates include age of child, age of parent, income bracket, and education bracket**p < .01; *p < .05
68 GOODMAN ET AL.
FINANCIAL COSTS
Respondents were asked regarding out-of-pocket expenses and insurance costs related to the treatment and care of the BPD proband (see Table 6). Fifty-seven percent of respondents reported details on out-of-pocket ex-penses, 3% reported no expenses, and 40% declined to answer. Similarly, 39% reported data on insurance costs, 4% reported no expenses, and 57% declined to answer. Of those who reported expenses, the average out-of-pocket expense was $60,087, and insurance costs totaled an average of $108,251. The average cost per year after diagnosis was $14,606 out-of-pocket and $45,573 billed to insurance. As the distribution of costs is skewed heavily to the right, median values are more representative of the true financial burden. Of those who reported expenses, the median out-of-pocket expense was $10,000, and insurance costs totaled a median of $20,000. The median cost per year after diagnosis was $3,667 out-of-pocket, and $12,500 billed to insurance.
Table 7 lists differences between BPD-related expenditures across various diagnoses and clinical features. One covariate, household income bracket, was included in the models to factor out confounding effects. There were significant cost differences between probands who were victims of rape dur-ing adolescence compared to those who were not raped (p < .006). After ad-justing for household income, a proband who had been raped in adoles-cence incurred roughly $40,000 more in BPD-related costs, while a diagnosis of conduct disorder led to about $50,000 in additional costs.
taBle 6. Financial Burden
Out-Of-Pocket n = 130 Mean: $56,604 Standard Deviation: $165,078 Per year after Dx: * $15,934 Per hospitalization: ** $11,119 Median: $10,000 Per year after Dx: * $3,667 Per hospitalization: ** $2,700Financial Burden Average cost, per household, directly related to treatment of BPD in proband Range: $100–1,400,000 Insurance n = 90 Mean: $108,251 Standard Deviation: $328,920 Per year after Dx: * $53,297 Per hospitalization: ** $15,756 Median: $20,000 Per year after Dx: * $12,500 Per hospitalization: ** $3,729 Range: $400–3,000,000
Note. Years after diagnosis resulted from difference between proband’s current age and age at diagnosis, rounded up to nearest whole number.*Derived from subsample (Out-of-Pocket, n = 88; Insurance, n = 59)**Derived from subsample (Out-of-Pocket, n = 125; Insurance, n = 86) 54% of total expenditure assumed to be hospitalization costs (van Asselt & Dirksen, 2007)
PARENTAL BURDEN 69
discussionThis anonymous Internet survey of parental viewpoints regarding their female offspring with BPD provides novel and important data on the de-gree and types of burden experienced by parents caring for a child with this disorder. Strengths of this study include the large number of respon-dents and probands, assessment of multiple facets of burden and collec-tion of data on both insurance and out-of pocket expenditures. Our strin-gent criteria for inclusion in the BPD group, including MSI-BPD scores cut-offs of seven and above and a formal diagnosis of BPD by a clinician, further strengthens the project design.
Our main finding is a detailed description of the negative impact of car-ing for a BPD child on a parent’s life, with assessment of six differing do-mains. Difficulty with emotional wellbeing was most widely endorsed (>88%) but physical health problems (59%) and damage to the marriage (56%) also were reported by the majority of parental respondents. A burden severity index was calculated by adding the number of individual burden
taBle 7. Financial Burden differences across diagnoses/clinicalFeatures (anoVa) (n = 136)
differenceitem difference (adjusted) F significance
Lifetime Diagnoses Conduct Disorder $67,870 $48,757 4.782 .031* Anxiety Disorders 3.127 .079 Bipolar Disorder 2.198 .141 Major Depressive Disorder 2.105 .149 ADHD 2.078 .152 Psychotic spectrum disorders 1.511 .221 Oppositional Defiant Disorder 0.362 .548Clinical Features in Adolescence Rape Victim $22,716 $40,253 7.656 .006** Deliberate Self-Harm $17,533 $17,066 5.165 .025* Cutting $17,812 $16,960 5.3 .023* Burning 0.696 .406 Head Banging 0.319 .573 Alcohol or Substance Abuse $17,369 $18,765 4.654 .033* Homicidality 2.752 .099 Pregnancy 1.916 .169 STIs 1.892 .171 Hallucinations 1.722 .192 Bulimic Features 1.647 .198 Fighting 1.314 .254 Suicidality 1.268 .262 Thoughts 0.5 .481 Threats 0.917 .340 Plans $33,876 $38,027 11.84 .001** Attempts 2.39 .124 Property Destruction 1.234 .269 Promiscuity 0.772 .381 Animal Cruelty 0.773 .381 Violence Victim 0.764 .384 Impulsivity 0.705 .403 Anorexic Features 0.583 .447
Note. Household income bracket included as covariate. F values evaluated at 1 of 136 degrees of freedom.**p < .01; *p < .05
70 GOODMAN ET AL.
items selected, with a maximum score of 6. Over 53% of respondents en-dorsed 4+ items. Our data suggest that caretaking for a BPD child affects multiple domains of functioning, similar to the findings of Schiers & Bok.
Parents of BPD offspring completing this survey were recruited using a website offering support to family members seeking advice and help. Those parents who proceeded to complete the survey were clearly motivated, ei-ther hoping that their responses might help clarify their child’s condition or that their answers might help others. This may represent a more severely burdened subgroup of parents of offpsring with BPD or a subgroup of par-ents who are over-involved with their BPD offspring. However our data do document the impairment in multiple domains experienced by this group of parents and the considerable sums of money for the care of their ill child.
The results of this survey identify several features of adolescent BPD females, including acting out behaviors, property destruction, delusions and hallucinations, as being significantly correlated with overall parental burden severity, as is a co-morbid diagnosis of bipolar disorder. These findings support previous research suggesting that disruptive behavior correlates strongly with family burden (Harvey et al., 2001), but also high-lights the importance of the effects of other psychiatric symptoms. Delu-sions and hallucinations are not central to the BPD diagnosis and may represent co-morbid Axis I conditions. While only 8% of parents endorsed a lifetime history of a schizophrenic disorder, the psychotic symptomatol-ogy correlating with burden intensity may possibly be attributed to fea-tures of major depressive disorder or bipolar episodes, substance induced psychosis or captured in the ninth BPD criterion of transient psychotic episodes. In fact, recent research in BPD highlights psychotic-like symp-toms as an important target dimension (Grooten et al., 2008), and advo-cates the use of antipsychotics in the treatment of BPD (Pascual et al., 2008). Others contend that there exists an under appreciation of psy-chotic symptomatology in BPD and the mood dysregulation connected to psychotic symptomatology (Benvenuti et al., 2005). Taken together, our data support this idea of developing a clearer understanding of the rela-tionship between psychotic symptomatology and BPD outcome, as hal-lucinations and delusions in adolescence are significant contributors to parental burden. Alternative hypotheses for the psychotic symptomatol-ogy during adolescence include psychotic features of associated axis I mood disorders and substance abuse. While our data highlight high life-time co-morbidities of bipolar disorder (57%) and major depression (78%), we can not ascertain from the current survey whether these disorders oc-curred at the time of adolescence during the periods of endorsed psy-chotic symptomatology. Our data does indicate that alcohol and sub-stance abuse problems in adolescence were endorsed by 40% of parents however its precise relationship with adolescent psychotic features re-mains unclear.
Surprisingly, adolescent suicide and self-injurious behavior were not significant contributors to the family burden severity index. The suicidal and self-injurious behaviors that were assessed in this survey occurred
PARENTAL BURDEN 71
solely during the adolescent epoch. This explains the lower incidence of suicide (93 of 233 or 40%) than is typical for clinical BPD samples. How-ever, the burden severity that is being assessed corresponds to the pres-ent time frame. It is possible that adolescent features of the disorder (i.e., adolescent suicidality and self injurious behavior) do not significantly af-fect current burden levels which are likely more influenced by overall psy-chiatric severity as reflected by co-morbidity and associated psychiatric symptomatology such as psychosis. One limitation of this study design is that the survey did not quantify current symptom severity in the proband.
While overall burden severity was not affected by these two adolescent variables, parental financial expenditures were affected by adolescent sui-cidal plans and DSH. Such behaviors added $38 thousand and $17 thou-sand dollars to BPD related costs respectively (see Table 7).
Dissatisfaction with the BPD proband’s clinicians was correlated with parental burden. This finding underscores the importance of quality treat-ment for BPD, which for many is currently not available. Even for those in treatment, struggles with health care providers, and the quest for dignity can complicate treatment efforts (Perseius, Ekdahl, Asberg, & Samuels-son, 2005). Our survey was not designed to query specific reasons for dis-satisfaction, but this is an important topic for future investigations.
Parental reports of average and median total out-of-pocket expenses of $60,087 and $10,000 or $14,606 average and $3,667 median per year after BPD diagnosis, and average and median insurance costs of $108,251 and $20,000 or $45,573 average and $12,500 median per year after BPD diagnosis begin to describe the financial costs of treating this disorder, both to insurance companies and individual families struggling with non-covered health-care costs. The highly skewed nature of this data suggests that there exist individuals with BPD with extensive treatment resource utilization. We found that co-morbid conduct disorder and the presence in adolescence of a rape or suicide plan significantly contribute to the overall costs of the disorder. These data indicate particular profiles of BPD sub-jects resulting in increased parental financial burden; such information may be useful to clinicians, family therapists, insurance companies, and BPD advocacy groups.
High levels of Axis I co-morbidity were endorsed in this sample. This may reflect a sample of more severely ill offspring with co-morbid Axis1 and II pathology, a profile consistent with data from the Children in the Community Study (Chen et al., 2006) that identifies the most negative adult quality of life in the adolescents with Axis I and II co-morbidities. Alternatively, misdiagnosis and incorrect reporting of diagnoses may be explaining this result. Unfortunately, the anonymous nature of this sur-vey does not allow for corroboration of the reported clinical diagnoses.
There are several limitations of this study. The use of an internet survey assessing parent’s opinions and feedback creates limits on the validity of collected data on offspring diagnoses. The inclusion of a BPD self-report measure that is completed by the parent was included to bolster the reli-ability. However, there may exist differences in results from MSI-BPD pa-
72 GOODMAN ET AL.
rental report as compared to patient self-report, particularly with items that refer to internal experiences such as emptiness.
The survey contained no measures of parental psychopathology. We were concerned that such questioning might be offensive to parents who come to the NEA-BPD website seeking advice, support, and explanations for their children’s disorder and might be sensitive to suggestions that early abuse was the culprit. It is also possible that parents may distort the dysfunction of their offspring, thereby skewing the results. However as-sessing parental input is a validated approach to assessing clinical data in child and adolescent populations (Cantwell et al., 1997; Hartung et al., 2005; Sourander & Piha, 1998). Also, the parents who completed the sur-veys were mostly educated white females with access to the Internet. We cannot predict how generalizable our results are to other ethnic groups or individuals with differing socioeconomic profiles. Additionally, the survey respondents were primarily mothers, which reflect the general composi-tion of individuals who frequent the NEA-BPD website. The surprising low levels of paternal and step-parent involvement in the study may reflect their more limited involvement with their BPD children, use of internet, or ability to ask for help. These possibilities could be more directly tested in future studies.
Our calculation of financial costs is limited by the reporting accuracy of the survey respondent. We hoped that the anonymous format of the sur-vey would allow parents to respond honestly about costs; however we do not know how well their answers reflect actual costs. Forty perrcent of survey respondents did not complete the questions pertaining to financial costs. There are likely several reasons for this including not wanting to take the additional time required to make the calculations, not knowing the answers pertaining to costs and expenditures, or feeling that this in-formation is private, Future studies might validate parental responses us-ing insurance company records.
This anonymous Internet survey of parents with BPD offspring docu-ments the burden experienced by caretakers of children with this disor-der. These data may be useful to individuals who work with families, prompting identification of high-risk families for whom support and treat-ment may be beneficial.
reFerences
American Psychiatric Association. (1994). Di-agnostic and statistical manual of men-tal disorders (4th ed.). Washington, DC: Author.
Alexander, R. B., & Trissel, D. (1996). Chron-ic prostatitis: results of an Internet survey. Urology, 48, 568–574.
Bäckström, M. (2007). Higher-order factors in a five-factor personality inventory and its relation to social desirability.
European Journal of Psychological As-sessment, 23, 63–70.
Bagge, C., Nickell, A., Stepp, S., Durrett, C., Jackson, K., & Trull, T. J. (2004). Bor-derline personality disorder features predict negative outcomes 2 years later. Journal of Abnormal Psychology, 113, 279–288.
Baronet, A. M. (1999). Factors associated with caregiver burden in mental ill-
PARENTAL BURDEN 73
ness: A critical review of the research literature. Clinical Psychology Review, 19, 819–841.
Benvenuti, A., Rucci, P., Ravani, L., Gonnelli, C., Frank, E., Balestrieri, M., et al.(2005). Psychotic features in border-line patients: is there a connection to mood dysregulation? Bipolar Disor-ders, 7, 338–43.
Cantwell, D. P., Lewinsohn, P. M., Rohde, P., & Seeley, J. R. (1997). Correspon-dence between adolescent report and parent report of psychiatric diagnostic data. Journal of the American Acade-my of Child Adolescent Psychiatry, 36, 610–619.
Chen, H., Cohen, P., Crawford, T. N., Kasen, S., Johnson, J. G., & Berenson, K. (2006). Relative impact of young adult personality disorders on subsequent quality of life: findings of a communi-ty-based longitudinal study. Journal of Personality Disorders, 20, 510–523.
Coyne, J. C., Kessler, R. C., Tal, M., Turn-bull, J., Wortman, C. B., & Greden, J. F. (1987). Living with a depressed per-son. Journal of Consulting and Clinical Psychology, 55, 347–352.
Gosling, S. D., Vazire, S., Srivastava, S., & John, O. P. (2004). Should we trust web-based studies? A comparative analysis of six preconceptions about internet questionnaires. The American Psychologist, 59, 93–104.
Grootens, K. P., van Luijtelaar, G., Buitelaar, J. K., van der Laan, A., Hummelen, J. W., & Verkes, R. J. (2008). Inhibi-tion errors in borderline personality disorder with psychotic-like symp-toms. Progress in Neuro-psychophar-macology and Biological Psychiatry, 32, 267–273.
Gunderson, J. G. (2009). Borderline person-ality disorder: ontogeny of a diagnosis. The American Journal of Psychiatry, 166, 530–539.
Gunderson, J. G., & Lyoo, I. K. (1997). Fam-ily problems and relationships for adults with borderline personality dis-order. Harvard Review of Psychiatry, 4, 272–278.
Hartung, C. M., McCarthy, D. M., Milich, R., & Martin, C. A. (2005). A parent- adolescent agreement on disruptive behavior symptoms: A multitrait-mul-timethod model. Journal of Psychopa-thology and Behavioral Assessment., 27, 159–168.
Harvey, K., Burns, T., Fahy, T., Manley, C.,
& Tattan, T. (2001). Relatives of pa-tients with severe psychotic illness: Factors that influence appraisal of caregiving and psychological distress. Social Psychiatry and Psychiatric Epi-demiology, 36, 456–461.
Hoenig, J., & Hamilton, M. W. (1966). The schizophrenic patient in the commu-nity and his effect on the household. The International Journal of Social Psychiatry, 12, 165–176.
Hoffman, P. D., Buteau, E., Hooley, J. M., Fruzzetti, A. E., & Bruce, M. L. (2003). Family members’ knowledge about borderline personality disorder: Corre-spondence with their levels of depres-sion, burden, distress, and expressed emotion. Family Process, 42, 469–478.
Liu, M., Lambert, C. E., & Rohde, P. (2007). Caregiver burden and coping patterns of Chinese parents of a child with mental illness. International Journal of Mental Health Nursing, 16, 86–95.
Miller, E. T., Neal, D. J., Roberts, L. J., Baer, J. S., Cressler, S. O., Metrik, J., et al. (2002). Test-retest reliability of alcohol measures: Is there a difference be-tween internet-based assessment and traditional methods? Psychology of Addictive Behaviors: Journal of the So-ciety of Psychologists in Addictive Be-haviors, 16, 56–63.
Noh, S., & Turner, R. J. (1987). Living with psychiatric patients: Implications for the mental health of family members. Social Science and Medicine, 25, 263–272.
Ostman, M., & Hansson, L. (2004). Apprais-al of caregiving, burden and psycho-logical distress in relatives of psychiat-ric inpatients. European Psychiatry: The Journal of the Association of Euro-pean Psychiatrists, 19, 402–407.
Pascual, J. C., Soler, J., Puigdemont, D., Pérez-Egea, R., Tiana, T., Alvarez, E., & Pérez, V. (2008). Ziprasidone in the treatment of borderline personality disorder: A double-blind, placebo-con-trolled, randomized study. The Jour-nal of Clinical Psychiatry, 69, 603–608.
Perseius, K. I., Ekdahl, S., Asberg, M., & Samuelsson, M. (2005). To tame a vol-cano: Patients with borderline person-ality disorder and their perceptions of suffering. Archives of Psychiatric Nurs-ing, 19, 160–168.
Rochlen, A. B., McKelley, R. A., Suizzo, M.-A., & Scaringi, V. (2008). Predictors of relationship satisfaction, psycho-
74 GOODMAN ET AL.
logical well-being, and life satisfaction among stay-at-home fathers. Psychol-ogy of Men and Masculinity, 9, 17–28.
Scheirs, J. G., & Bok, S. (2007). Psychological distress in caretakers or relatives of pa-tients with borderline personality disor-der. The International Journal of Social Psychiatry, 53, 195–203.
Schene, A. H., van Wijngaarden, B., & Koeter M. (1998). Family caregiving in schizo-phrenia; Domains and distress. Schizo-phrenia Bulletin, 24, 609–618.
Sourander, A., & Piha, J. (1998). Three-year follow-up of child psychiatric inpatient treatment. European Child & Adoles-cent Psychiatry, 7, 153–162.
Srivastava, S., John, O. P., Gosling, S. D., & Potter, J. (2003). Development of per-sonality in early and middle adult-hood: Set like plaster or persistent change? Journal of Personality and So-cial Psychology, 84, 1041–1053.
Szmukler, G. I., Burgess, P., Herrman, H., Benson, A., Colusa, S., & Bloch, S. (1996). Caring for relatives with seri-ous mental illness: The development of the experience of caregiving inven-tory. Social Psychiatry and Psychiatric Epidemiology, 31, 137–148.
Tsang, H. W., Tam, P. K., Chan, F., &
Cheung, W. M. (2003). Sources of bur-dens on families of individuals with mental illness. International Journal of Rehabilitation Research, 26, 123–130.
van Asselt, A. D., Dirksen, C. D., Arntz, A., & Severens, J. L. (2007). The cost of bor-derline personality disorder: Societal cost of illness in BPD-patients. Euro-pean Psychiatry: The Journal of the Association of European Pyschiatrists, 22, 354–361.
van Wijngaarden, B., Schene, A. H., & Koeter, M. (2004). Family caregiving in depression: Impact on caregivers’ dai-ly life, distress and help seeking. Jour-nal of Affective Disorders, 81, 211–222.
Veltman, A., Cameron, J., & Stewart, D. E. (2002). The experience of providing care to relatives with chronic mental illness. The Journal of Nervous Mental Disease, 190, 108–114.
Zanarini, M. C., Vujanovic, A. A., Parachini, E. A., Boulanger, J. L., Frankenburg, F. R., & Hennen, J. (2003). A screen-ing measure for BPD: The McLean screening instrument for borderline personality disorder. (MSI-BPD). Jour-nal of Personality Disorders, 17, 568–573.