Response inhibition deficits in unaffected first-degree relatives of patients with borderline...
Transcript of Response inhibition deficits in unaffected first-degree relatives of patients with borderline...
Neuropsychology
Response Inhibition Deficits in Unaffected First-DegreeRelatives of Patients With Borderline PersonalityDisorderAnthony C. Ruocco, Lise Laporte, Jennifer Russell, Herta Guttman, and Joel ParisOnline First Publication, May 21, 2012. doi: 10.1037/a0028715
CITATIONRuocco, A. C., Laporte, L., Russell, J., Guttman, H., & Paris, J. (2012, May 21). ResponseInhibition Deficits in Unaffected First-Degree Relatives of Patients With BorderlinePersonality Disorder. Neuropsychology. Advance online publication. doi: 10.1037/a0028715
Response Inhibition Deficits in Unaffected First-Degree Relatives ofPatients With Borderline Personality Disorder
Anthony C. RuoccoUniversity of Toronto Scarborough
Lise Laporte, Jennifer Russell, and Herta GuttmanMcGill University Health Centre, Montreal, Quebec, Canada
Joel ParisSMBD-Jewish General Hospital, Montreal, Quebec, Canada
Objective: Impulsiveness is a heritable feature of borderline personality disorder (BPD) which aggregatesin families affected with the illness. Whereas BPD patients show deficits on neuropsychological tests ofresponse inhibition, it is unknown whether these deficits are also present in their first-degree biologicalrelatives who are at an increased genetic risk for this illness. The purpose of the current study was toidentify and characterize a subgroup of BPD patients with pronounced response inhibition deficits, andsecondarily, to estimate the relative recurrence risk of these deficits among affected families. Method:Thirty-nine pairs of female BPD probands and their unaffected first-degree biological sisters wererecruited from hospital outpatient clinics. Participants completed the Conners’ Continuous PerformanceTest (CPT) and the Barratt Impulsiveness Scale-11. Results: BPD relatives made a similar number ofcommission errors on the CPT compared to healthy controls with no personal or family history ofpsychiatric illness; however, cluster analysis revealed a subgroup of BPD relatives who displayedclinically elevated commission errors and atypically fast RTs to target stimuli, indicating a genuineresponse inhibition deficit. The estimated relative recurrence risk for response inhibition deficits for allsibling pairs on the CPT was moderate at � � 4.55. Conclusions: These findings suggest that responseinhibition deficits are pronounced in some BPD relatives, may be heritable between siblings, arenonredundant with diagnostic status, and show promise as candidate neuropsychological endophenotypesfor BPD.
Keywords: borderline personality disorder, response inhibition, impulsivity, endophenotype
Borderline personality disorder (BPD) is a severe form of men-tal illness characterized by pervasive difficulties with impulsivity,cognition, affectivity, and interpersonal relations (American Psy-chiatric Association, 2000). This illness is associated with highrates of suicide, comorbidity with other psychiatric disorders,extensive mental health services utilization, and functional disabil-ity (Leichsenring, Leibing, Kruse, New, & Leweke, 2011; Skodolet al., 2005; 1999). Approximately 1% of the general population isaffected by BPD (Lenzenweger, Lane, Loranger, & Kessler, 2007),although it is more prevalent in psychiatric settings, representingupward of 10% of outpatients and 15–25% of inpatients (Gunder-son, 2009). Their high rates of suicidality and deficient cognitivefunctioning, particularly impulsivity, rank BPD patients among thehighest users of public mental health services (Comtois et al.,2003).
Impulsivity represents one of the most pressing concerns forBPD because it places patients at an increased risk for physicalharm, whether self-inflicted or as a consequence of other danger-ous and risky behaviors. At the phenotypic level, impulsivity is amultidimensional construct which encompasses several interre-lated traits, including urgency (tendency to commit acts rashly asa result of negative affect), lack of premeditation (tendency to actwithout planning), lack of perseverance (inability to remain fo-cused on a boring or difficult task), and sensation seeking (ten-dency to enjoy and pursue exciting activities as well as an open-ness to try new experiences which may be dangerous; seeWhiteside & Lynam, 2001). For patients with BPD, impulsivity isthought to be an outgrowth of symptoms that appear in childhoodand are shaped over the course of development through interac-tions between temperamental and environmental risk factors(Paris, 2005). A long-term prospective follow-up study by Links,Heslegrave, and van Reekum (1999) revealed that impulsivitysymptoms were not only stable over 7 years in a cohort of BPDpatients, but that they were also highly predictive of BPD psycho-pathology at follow-up, more so than any other aspects of thedisorder. Impulsive personality traits also appear to be geneticallytransmitted in BPD families, as first-degree biological relatives ofBPD probands exhibit higher levels of trait impulsiveness, even ascompared with relatives of patients with schizophrenia and majormood disorders (Silverman et al., 1991).
Anthony C. Ruocco, Department of Psychology, University of TorontoScarborough, Toronto, ON, Canada; Lise Laporte, Jennifer Russell, andHerta Guttman, Department of Psychiatry, McGill University Health Cen-tre, Montreal, Quebec, Canada; Joel Paris, Department of Psychiatry,SMBD-Jewish General Hospital, Montreal, Quebec, Canada.
Correspondence concerning this article should be addressed to AnthonyC. Ruocco, Department of Psychology, University of Toronto Scarbor-ough, Toronto, ON, M1C 1A4. E-mail: [email protected]
Neuropsychology © 2012 American Psychological Association2012, Vol. 00, No. 00, 000–000 0894-4105/12/$12.00 DOI: 10.1037/a0028715
1
Neural Correlates of Response Inhibition in BPD
Response inhibition, one facet of impulsivity, may be evaluatedusing a variety of neuropsychological tests. Among the mostcommon of these are continuous performance tests, go/no-gotasks, stop-signal tasks and the Stroop test, all of which requireparticipants to inhibit a response according to specific task param-eters (Epstein, Johnson, Varia, & Conners, 2001). Functional neu-roimaging studies of healthy human participants using variants ofthese tasks reveal a complex network of neural systems supportingresponse inhibition processes. The results of these studies indicatethat discrete frontal cortical regions are engaged during responseinhibition, namely, the medial, ventrolateral, and dorsolateral pre-frontal cortex, as well as premotor and supplementary motor areas(Konishi et al., 1999; Konishi, Nakajima, Uchida, Sekihara, &Miyashita, 1998; Mostofsky et al., 2003; Watanabe et al., 2002).Other regions associated with performance on response inhibitiontasks include the insula, inferior parietal lobule, temporoparietaljunction, and occipitotemporal area (Nakata et al., 2008). Thefailure to inhibit a response (i.e., a commission) appears to berelated to activity within the anterior cingulate cortex, presupple-mentary motor area, insula, thalamus, and right inferior parietallobe (Hester, Fassbender, & Garavan, 2004; Lutcke & Frahm,2008).
Functional neuroimaging studies of response inhibition haveilluminated the neural basis of impulse control deficits in BPD. Apositron emission tomography study of BPD patients found thatcommission errors on a laboratory measure of response inhibitionwere associated with lower alpha-[(11)C]MTrp trapping in themedial frontal gyrus, anterior cingulate gyrus, temporal gyrus, andstriatum (Leyton et al., 2001). Functional MRI has also been usedto investigate the neural correlates of response inhibition in BPD.Using a classic go/no-go task, Völlm and colleagues (2004) foundthat BPD patients showed a less focal pattern of functional acti-vation in the prefrontal cortex compared with healthy individuals.Specifically, BPD patients showed a more bilateral and extendedpattern of activation involving the medial, superior, and inferiorfrontal gyri, and extending to the anterior cingulate cortex. Toexamine the influence of emotions on inhibitory control in patientswith BPD, Silbersweig and colleagues (2007) used an emotionalvariant of the go/no-go task. They found that under conditions ofresponse inhibition and negative emotion, BPD patients demon-strated relative decreases in ventromedial prefrontal cortex activ-ity, including the medial orbitofrontal cortex and subgenual ante-rior cingulate. Together, these studies suggest decreased efficiencyof inhibitory control in patients with BPD as reflected in reducedactivation of the prefrontal cortex under conditions of responseinhibition.
Neuropsychological Studies of Response Inhibition inBPD
Patients with BPD display neuropsychological deficits in arange of cognitive domains, including mental speed, attention/working memory, auditory (verbal) and visual memory, visuospa-tial/constructional skills, and several executive functions (for areview, see Ruocco, 2005). Most neuropsychological studies sug-gest that executive dysfunction may form the core cognitive deficitin patients with BPD, with impairments in response inhibition
perhaps the most central (McCloskey et al., 2009; Posner et al.,2002; Rubio et al., 2007). Indeed, adequate inhibitory control iscritical for efficient performances on many neuropsychologicaltests of executive functioning, and reduced inhibition in BPD maytherefore impact performance on tests which rely on these abilities.Response inhibition has been evaluated in BPD using a variety ofneuropsychological tasks tapping a number of related cognitivedomains, including motor response control, planning and problem-solving, and decision-making. Continuous performance tests(CPT; Conners, 2000; Dougherty, 1999) are among the most wellvalidated tests of motor response control, as well as vigilance andsustained attention (Riccio, Reynolds, Lowe, & Moore, 2002).These tasks typically present target and nontarget stimuli on amonitor and examinees are required to provide a specified re-sponse to target stimuli while withholding responses to nontargetstimuli. Among a sample of adolescent inpatients with disruptivebehavior disorders, Swann, Bjork, Moeller, and Dougherty (2002)found a robust relationship between CPT commission errors (i.e.,“false alarms”) and elevated BPD symptoms. Paris, Zelkowitz,Guzder, Joseph, and Feldman (1999) investigated a group ofchildren with BPD psychopathology and discovered high levels ofabnormal performance on the CPT compared with nonborderlinechildren. Adults with BPD also show high levels of impulsiveresponding on the CPT, behaviors which are correlated with self-report measures of motoric, nonplanning, and cognitive impulsiv-ity (McCloskey et al., 2009; Rubio et al., 2007). The Stroop Test,a task requiring the inhibition of a prepotent response (i.e., read-ing), has been employed in several studies of BPD patients, withboth positive and negative results (Domes et al., 2006; Ruocco,2005). Whereas some studies have found a deficit on the inhibitioncondition of this task (Swirsky-Sacchetti et al., 1993), particularlyunder conditions of negative emotionality (Arntz, Appels, &Sieswerda, 2000; Sieswerda, Arntz, Mertens, & Vertommen,2007), others studies have not confirmed this effect or foundisolated deficits in word- or color-reading speed (Kunert, Druecke,Sass, & Herpertz, 2003; Wingenfeld et al., 2009).
A variety of other response control tasks have yielded moreconsistent findings. The Attention Network Test (Fan, McCan-dliss, Sommer, Raz, & Posner, 2002) measures three attentionalnetworks comprised of alerting, orienting, and conflict resolution/executive attention. To evaluate the conflict network, a target issurrounded by flankers which are incongruent with the target.Several studies have evaluated BPD patients using this paradigm(Fertuck, Lenzenweger, & Clarkin, 2005; Lampe et al., 2007;Posner et al., 2002; Rusch et al., 2007). In comparison to healthycontrols, BPD patients have typically showed isolated deficits inconflict resolution, with poorer performance associated withgreater levels of BPD psychopathology. On variants of the classicgo/no-go task, BPD patients demonstrate a higher frequency ofcommission errors, which are not accounted for by slowed re-sponse latencies (Dinn et al., 2004; Kaiser et al., 2008; Rentrop etal., 2008). Results with the stop-signal task are less consistent,although there is evidence that increased RTs to stop signals maybe related to elevated levels of BPD psychopathology (Jacob et al.,2010; Lampe et al., 2007; Nigg, Silk, Stavro, & Miller, 2005;Rubio et al., 2007). Response inhibition has also been evaluatedusing tests of planning and problem-solving, such as the Tower ofLondon (Culbertson & Zillmer, 2001). BPD patients typicallyrequire more steps to arrive at target solutions than healthy con-
2 RUOCCO, LAPORTE, RUSSELL, GUTTMAN, AND PARIS
trols (Bazanis et al., 2002; Beblo et al., 2006). They also showprotracted first-move initiation times, suggesting that while BPDpatients may take longer to deliberate before beginning to solveproblems, they nevertheless tend to solve them in an inefficientand often ineffective manner (Ruocco, 2005). There is also evi-dence for distinct subpopulations of BPD patients who show moresevere deficits on the Tower of London but minimal levels ofbehavioral impulsivity based on self-report measures (Bustamanteet al., 2009). Decision-making abilities have also been investigatedin BPD to determine whether patients make more impulsivechoices under conditions of heightened risk (Bechara, Damasio,Tranel, & Damasio, 1997). Compared with healthy controls, BPDpatients consistently make more disadvantageous decisions (i.e.,choices that present the largest magnitudes of gain but also thegreatest long-term loss) (Haaland & Landro, 2007; Maurex et al.,2009; Schuermann, Kathmann, Stiglmayr, Renneberg, & Endrass,2011; Van den Eynde et al., 2008), a bias which may also char-acterize other Cluster B (i.e., antisocial, narcissistic, histrionic) aswell as Cluster C (anxious-fearful) personality disorders (Ruocco,McCloskey, Lee, & Coccaro, 2009).
Impulsivity as a Candidate Endophenotype for BPD
BPD is strongly influenced by genetic factors. Risk for theillness is transmitted in families (Zanarini, Barison, Frankenburg,Reich, & Hudson, 2009), and the concordance rate for BPD amongmonozygotic twin pairs is 35% (Nigg & Goldsmith, 1994). Thestrongest evidence for BPD’s heritability is found in specific traitswhich delineate the illness, namely, impulsiveness, emotional in-stability, and identity disturbance (Livesley, Jang, Jackson, &Vernon, 1993; Silverman et al., 1991). Attempts to link specificgenetic polymorphisms with BPD, however, have met with limitedsuccess. Nevertheless, the bulk of the evidence implicates genesinvolved in the regulation of specific monoamine neurotransmit-ters: dopamine, serotonin, and norepinephrine (Nemoda et al.,2010; Ni et al., 2006; Ni, Chan, Chan, McMain, & Kennedy, 2009;Ni et al., 2007; Tadic et al., 2009). In particular, decreased sero-tonin neurotransmission in the prefrontal cortex has been linked todifficulties regulating impulsive behavior in BPD patients (Soloff,Meltzer, Greer, Constantine, & Kelly, 2000).
Several factors may help explain why it has been difficult toisolate specific susceptibility genes for BPD. First, the phenotypicstructure of BPD is such that there are several combinations ofsymptoms which may lead to a single diagnosis of this illness. Thisdiagnostic heterogeneity may obscure significant biological vul-nerabilities that may be present for specific subsets of BPD pa-tients. Second, it may be the case that specific BPD traits showmore compelling links with specific genes than the full-blownillness itself, as has been found with angry-impulsive BPD traits(Joyce et al., 2009). Third, the discrete traits and symptoms whichmake up BPD may themselves represent complex clinical pheno-types that are likely tied to multiple genes, which as a consequenceincrease the complexity of genetic analyses.
An endophenotype approach (Gottesman & Gould, 2003) mayhelp overcome many of the barriers encountered on the pathwaytoward deconstructing the genetic architecture of BPD. Perfor-mance on neuropsychological tests show promise as candidateendophenotypes for BPD, most especially measures of responseinhibition (Ruocco, 2005). Deficits on laboratory tests of response
inhibition may thus serve as putative neurocognitive liabilitymarkers for BPD, and there is mounting evidence to support thispossibility (McCloskey et al., 2009). According to Gottesman andGould (2003), two of the defining characteristics of endopheno-types are that they are heritable and found in first-degree biologicalrelatives of BPD patients at a higher rate than in the generalpopulation. Whereas several neuropsychological studies have nowconfirmed the presence of response inhibition deficits in patientswith BPD, it remains to be determined whether these deficits,albeit to a lesser degree, may also be found in their biologicalrelatives. Furthermore, estimates of the relative recurrence risk ofthese deficits among BPD relatives have yet to be examined.
The primary aim of the current study was to evaluate responseinhibition deficits in the first-degree biological relatives of BPDpatients using a well-validated measure of response inhibition(Conners, 2000). We hypothesized that relatives of BPD patientswould show deficits in response inhibition on this task whencompared to a group of nonpsychiatric controls. Considering theheterogeneity of neuropsychological response inhibition deficitseven within BPD patient samples (Bustamante et al., 2009;Ruocco, 2005), we decided to perform a cluster analysis among thesample of BPD relatives to explore possible latent subgroupswhich may show more pronounced deficits on this task. Thesecond aim of this study was to calculate the relative recurrencerisk of response inhibition deficits among all sibling pairs in orderto estimate the likelihood of recurrence of these deficits within thesame pedigree, and determine whether these deficits among rela-tives are nonredundant with the BPD diagnosis.
Method
Sample and Participant Selection
Thirty-nine pairs of female BPD probands and their unaffectedfirst-degree biological sisters were drawn from psychiatric clinicsacross a large urban area. Detailed sampling procedures have beenreported previously (Laporte, Paris, Russell, & Guttman, 2011).Informed consent was obtained from each participant after theprocedures were fully explained. Institutional review boards at allhospitals from which patients were recruited, as well as the Re-search Ethics Board at McGill University, approved the study. Allparticipants received an honorarium for their participation.Twenty-four female participants without a personal or familyhistory of psychiatric illness were recruited as healthy controlsfrom the University of Toronto Scarborough. Research ethicsapproval was obtained from the University of Toronto and allparticipants provided written informed consent to participate inthis study. Probands, relatives, and healthy controls completed theCPT as part of a larger battery of neuropsychological tests andpsychiatric assessments, with the healthy controls recruited as partof a separate family protocol that incorporated a similar battery ofassessments. Healthy controls were younger (M � 21.4 years,SD � 6.3) than probands (M � 29.7 years, SD � 7.9, p � .001)and relatives (M � 30.3, SD � 7.7, p � .001). To control for ageeffects, all CPT analyses used age- and gender-adjusted T-scoresbased on normative data provided in Conners (2000).
3RESPONSE INHIBITION AND BORDERLINE PERSONALITY
Assessments and Measures
Diagnostic interviews. For a diagnosis of BPD, probandswere required to meet DSM–IV (First, Spitzer, Gibbon, & Wil-liams, 1996) criteria by scoring 8 out of a possible 10 on theDiagnostic Interview for Borderline Personality Disorder–Revised(DIB-R; Zanarini, Gunderson, & Frankenburg, 1989). BPD rela-tives also completed the DIB-R to determine their affected status.From an initial sample of 39 sibling pairs, three pairs were ex-cluded because probands and siblings were concordant for a diag-nosis of BPD. Additionally, three relatives were excluded becausethey met criteria for current alcohol or substance dependence. Thefinal sample comprised 33 BPD probands and 33 unaffected rel-atives. The Structured Clinical Interview for DSM–IV (SCID; Firstet al., 1996) was used to screen for severe psychopathology (i.e.,psychosis, substance dependence, severe eating disorders). Anexperienced clinician (JP) with previously established interraterreliability administered the diagnostic interviews. Exclusion crite-ria for all participants were organic brain syndromes and mentalretardation. The nonpsychiatric comparison group was carefullyevaluated for major psychiatric illness (i.e., psychosis, substanceuse, current mood disturbance) using the SCID and were free ofillicit substances at the time of testing based on urine drug screens.
Conners’ Continuous Performance Test-II. The Conners’CPT (Conners, 2000) was administered to all participants as ameasure of response inhibition, vigilance, and sustained attention.Testing was carried out with participants seated at a computer in aquiet room. Examiners ensured that all participants understood testinstructions prior to beginning the testing session. Participantswere required to press the space bar on a keyboard when any letterappeared on the computer monitor except for the target letter X.There were four interstimulus intervals (ISI’s): 1, 2, and 4 seconds.Stimuli were displayed for 250 milliseconds. The task comprisedsix blocks and three subblocks, each of which contained 20 trials(letter presentations). The different ISI’s were presented in avariable order between blocks. The total time to complete the taskwas 14 minutes. The primary measure of response inhibition wasthe number of commission errors. A commission error was definedas a response (space bar press) given after an X appeared on thescreen. Participants’ responses on these trials were presumed toreflect failures of response inhibition because the task instructionswere to withhold responses to these stimuli. In addition to com-mission errors, the CPT provides a variety of other performancemeasures, including reaction time (RT), omission errors, andchanges in RT speed (i.e., Hit Reaction Time Block Change) andconsistency (i.e., Hit Standard Error Block Change) as the testprogresses and for different ISI’s. Raw scores for participants’performances on the CPT were transformed to age- and gender-adjusted T-scores which have a mean of 50 and a standard devi-ation of 10.
Barratt Impulsiveness Scale-11 (BIS-11). The BIS-11 is anobjective self-report rating scale of impulsiveness. Participantswere asked to rate how much or how frequently each item de-scribed them. They used a rating scale ranging from 0 (rarely) to3 (almost always). Factor analytic studies of the BIS-11 indicatethat the scale measures three interrelated constructs: attentional,motor, and nonplanning impulsiveness (Patton, Stanford, & Bar-ratt, 1995).
Statistical Analyses
Primary contrasts of relatives and nonpsychiatric controls werecarried out with the Mann–Whitney U test for Independent Sam-ples (two-sided) as the distributions of scores for the CPT indiceswere not normally distributed. A standardized test statistic (z-score) and asymptotic significance value (p value) was reportedfor nonparametric analyses. To reduce spurious findings in theseexploratory analyses, a Bonferroni correction was implementedwith test statistics considered significant if they exceeded a p valueof .005. A two-step cluster analysis based on CPT commissionerrors was used to investigate possible latent subgroups of relativeswith response inhibition deficits. The resulting distributions ofcommission errors for these clusters were normal and of equivalentvariance; thus, they were compared with independent samples ttests (two-sided). Secondary analyses comparing probands withrelatives and controls were also carried out using Mann–WhitneyU tests. Estimated relative recurrence risk for response inhibitiondeficits was calculated as (concordant pairs/[concordant � non-concordant pairs])/proportion affected in the comparison group.
Results
Comparisons of BPD Relatives and Controls
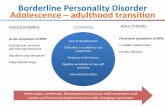
The mean performances of BPD relatives across CPT indiceswere within the average range based on normative data provided inConners (2000). Whereas healthy controls and relatives did notdiffer significantly in their performance on the commission errorsindex of the CPT, the effect size difference fell within the “me-dium” range (Cohen’s d � �.43). Relatives were also more thanfive times as likely to demonstrate a “markedly atypical” (T � 65;Conners, 2000) number of commission errors compared to healthycontrols with no personal or family history of psychiatric illness(21% vs. 4%, respectively), although this difference did not reachstatistical significance, �2 � 3.34, df � 1, p � .067. As can be seenin Figure 1, across most CPT indices, the performance of BPDrelatives largely fell intermediate to that of probands and nonpsy-chiatric controls. Effect size differences (Cohen’s d) betweenrelatives and controls for the remaining CPT indices were asfollows: Omissions (d � �.14), Hit Reaction Time (d � �.12),Hit Reaction Time Standard Error (d � �.14), Detectability (d ��.49), Perseverations (d � �.12), Hit Reaction Time BlackChange (d � �.001), Hit Standard Error Block Change (d ��.01), Hit Reaction Time Interstimulus Change (d � .46), HitStandard Error Interstimulus Change (d � .88).
Cluster Analysis of Commission Error Performance
We conducted a two-step cluster analysis of BPD relatives’commission error scores using PASW Statistics 18, Release Ver-sion 18.0.0 (SPSS, Inc., 2009, Chicago, IL, www.spss.com). Thetwo-step cluster analysis procedure was used to reveal naturalgroupings (or clusters) among BPD relatives that would otherwisenot be apparent. The algorithm employed by the cluster analysisprocedure used Euclidian as the distance measure and Schwartz’sBayesian Inference Criterion (BIC) to determine the optimal num-ber of clusters (Judge, Griffiths, Hill, Lutkepohl, & Lee, 1980). Inthe first “autoclustering” stage, the BIC for each number of clus-
4 RUOCCO, LAPORTE, RUSSELL, GUTTMAN, AND PARIS
ters within a specified range (in this case, 10) is calculated andused to find the initial estimate for the number of clusters (seeTable 1). The ratio of change in BIC at each successive mergingrelative to the first merging determines the initial estimate. In thesecond stage, the initial estimate is refined by finding the largestrelative increase in distance between the two closest clusters ineach hierarchical clustering stage. This two-step cluster analysisyielded a two-cluster solution with good cohesion and separation(average Silhouette � 0.70). The first cluster (n � 15) was
characterized by a normatively average number of CPT commis-sions errors (mean T-score � 4 3.66, SD � 5.56), whereas thesecond cluster (n � 18) showed clinically elevated scores on theCPT commission errors index (mean T-score � 64.36, SD � 7.54;see Table 2). This difference in performance between the BPDrelatives clusters was very robust, clinically meaningful, and sta-tistically significant, t(47) � 11.05, p � .001. Analysis of theclusters revealed that the group with elevated commission errorswas more inattentive (d’; Mann–Whitney U, z � 4.59, p � .001)
Figure 1. Comparison of BPD probands and relatives with nonpsychiatric controls on the Conners’ ContinuousPerformance Test (Conners, 2000). Note: Scores are plotted in the direction of negative scores representingworse performance (not applicable to Response Bias scale). RT � reaction time; SE � standard error; ISI �interstimulus interval.
Table 1Results of Auto-Clustering Process in Two-Step Cluster Analysis
Number of clustersSchwarz’s Bayesian
Inference Criterion (BIC)BIC
changeaRatio of BIC
changesbRatio of
Euclidian measurec
1 29.42 22.6 �6.8 1.0 2.23 25.3 2.8 �0.4 1.74 30.2 4.9 �0.7 1.35 36.3 6.1 �0.9 3.16 42.9 6.6 �1.0 1.17 49.5 6.6 �1.0 1.88 56.4 6.9 �1.0 1.19 63.3 6.9 �1.0 1.3
10 70.2 6.9 �1.0 1.0
a The changes are from the previous number of clusters in the table. b The ratios of changes are relative to thechange for the two cluster solution. c The ratios of distance measures are based on the current number ofclusters against the previous number of clusters.
5RESPONSE INHIBITION AND BORDERLINE PERSONALITY
and produced atypically fast RTs (Mann–Whitney U, z � 3.58,p � .001). There was no difference between the clusters withregard to demographic variables or self-reported impulsiveness onthe BIS-11 (all ps � .05).
BPD Probands Versus Relatives and Controls
Probands made more commissions (Mann–Whitney U, z �2.01, p � .045) and were more inattentive (d’; Mann–Whitney U,z � 2.84, p � .005) compared with nonpsychiatric controls.Probands did not differ from relatives on any of the CPT indices(all ps � .05). On the BIS-11, probands reported more impulsive-ness than relatives across all subscales, including nonplanning,t(64) � 4.05, p � .001 (probands M � 28.9, SD � 4.6, relativesM � 24.0, SD � 5.2), attentional, t(64) � 6.79, p � .001 (pro-bands M � 22.7, SD � 3.2, relatives M � 16.3, SD � 4.4), andmotor impulsiveness, t(64) � 3.25, p � .002 (probands M � 25.5,SD � 5.4, relatives M � 21.4, SD � 4.8).
Relative Recurrence Risk of Response InhibitionDeficits
Relative recurrence risk (�) is the probability that a deficitaffecting a proband will appear in other members of the samepedigree. BPD probands and relatives were designated as beingaffected if they showed a response inhibition deficit defined as acommissions error score greater than two standard deviationsabove the mean for the normative group (i.e., an age- and gender-adjusted T-score �70 on the Commissions scale of the CPT).Based on this cut-off value, 18.2% of probands and 12.1% ofrelatives were affected. Nine percent of the sibling pairs wereconcordant for these deficits, and by definition, 2% of the norma-tive sample obtained scores greater than a T-score of 70 on theCommissions scale of the CPT (none of our healthy controls whohad no personal or family history of psychiatric illness had scoresabove T � 70). Given this proportion of concordant sibling pairs
and the base rate of this deficit in the general population, therelative recurrence risk of response inhibition deficits within thissample of BPD probands and their first-degree biological siblingswas moderate at � � 4.55.
Discussion
The primary aim of the current study was to investigate thepresence of neuropsychological response inhibition deficits in thefirst-degree biological relatives of BPD probands by exploringpossible latent subgroups of relatives which may otherwise not beapparent. We found overall comparable performance betweenBPD relatives and nonpsychiatriccontrols on the CPT commissionerrors index; however, cluster analysis revealed a subgroup ofrelatives with clinically elevated response inhibition deficits. Theperformance of these relatives on the CPT could be characterizedas genuinely impulsive, as they showed atypically fast RTs totarget stimuli and a very large number of commission errors(Conners, 2000). This is consistent with the general pattern ofperformance of BPD probands on similar tests of response inhibi-tion (Rentrop et al., 2008). Relatives counted among the clusterwith significant response inhibition deficits also showed signs ofinattentiveness on the CPT as indicated by poorer discriminabilitybetween target and nontarget stimuli. This group, however, did notshow elevated levels of behavioral impulsivity as assessed by theBIS-11, perhaps suggesting that these neuropsychological deficitsare not necessarily manifested in overt signs of impulsive behaviorin this group of relatives. Indeed, whereas neuropsychological testsof response inhibition bear some relationship with the phenotypicstructure of impulsive personality traits, these tests actually mea-sure specific aspects of the latent construct of impulsivity and assuch do not completely overlap with self-report assessments (Cy-ders & Coskunpinar, 2011).
This is the first study to our knowledge to investigate thepresence of neuropsychological deficits in the first-degree biolog-
Table 2Continuous Performance Test Indices and Borderline Personality Disorder Symptom Scales for Empirically Derived Clusters ofPatients’ Siblings
Cluster 1 (n � 15) Cluster 2 (n � 18) t p-value Cohen’s d
Conners’ Continuous Performance Test1
Commissions 44.2 (5.6) 64.0 (7.7) 8.3 �.001 2.94Omissions 48.0 (4.6) 64.8 (53.8) 1.2 .24 .44Detectability (d’) 46.6 (8.2) 61.1 (5.5) 6.0 �.001 2.08Response style (�) 53.8 (15.8) 47.4 (3.3) 1.7 .10 �.56Hit RT block change 44.9 (8.1) 51.1 (6.6) 2.4 .02 .84Hit RT SE block change 52.7 (6.2) 55.9 (10.0) 1.1 .30 .38Hit RT ISI change 51.4 (14.8) 45.0 (9.7) 1.5 .14 �.51Hit RT SE ISI change 47.0 (9.2) 43.7 (11.4) .90 .37 �.32Hit RT 53.7 (11.1) 40.4 (7.1) 4.2 �.001 �1.43Perseverations 50.2 (7.6) 52.2 (8.0) .74 .46 .26
Barratt Impulsiveness Scale-112
Nonplanning 25.0 (5.3) 23.2 (5.2) 1.0 .31 �.34Attentional 16.5 (5.3) 16.1 (3.5) .29 .78 �.09Motor 21.7 (4.8) 21.2 (5.0) .27 .79 �.10Total scale 63.5 (12.7) 60.6 (11.7) .69 .49 �.24
Note. Values represent means and standard deviations of T-scores adjusted for age and gender based on normative data provided in Conners (2000). RT �reaction time; SE � standard error; ISI � interstimulus interval.1 Age- and gender-adjusted T-scores. 2 Raw scores.
6 RUOCCO, LAPORTE, RUSSELL, GUTTMAN, AND PARIS
ical relatives of BPD patients. Considering the aggregation ofimpulsive personality traits in BPD families (Silverman et al.,1991) and the pronounced response control problems found onneuropsychological testing of BPD patients (Ruocco, 2005), theidentification of intermediate phenotypes of response inhibitiondeficits in relatives of BPD patients represents a critical stepforward in delineating endophenotypes for this illness. The find-ings of the current study suggest that impaired response inhibitionmay represent an important neuropsychological endophenotype forBPD. As these findings suggest, there may be a subset of BPDpatients who show clinically elevated response inhibition deficitsas reflected in increased commission errors and atypically fast RTsto target stimuli on the CPT. Our results are consistent withprevious neuropsychological findings indicating that specific sub-populations of BPD patients may be discernible based on neuro-psychological measures of planning and self-report assessments ofimpulsiveness (Bustamante et al., 2009). The response inhibitiondeficits detected in these unaffected BPD relatives may thus reflecta neurocognitive vulnerability marker for this illness. Repetition ofthe cluster structure in a separate sample of BPD relatives, how-ever, is necessary to validate the cluster solution and confirm thesefindings.
The second aim of the current study was to calculate the relativerecurrence risk of response inhibition deficits among BPD siblingpairs. Understanding the pattern of response inhibition deficitsamong relatives within affected families is potentially significantbecause strong estimates of recurrence risk for cognitive deficits inthis illness may increase the power of genetic linkage analyses forBPD (Risch & Merikangas, 1996). The observed relative recur-rence risk of � � 4.55 for response inhibition deficits in thesesibling pairs is consistent with more rigorous estimates of recur-rence risk for deficits on the CPT in other major psychiatric illness,such as schizophrenia (Egan et al., 2000). This moderate recur-rence risk estimate suggests that a deficit in response inhibitionmay serve as a promising neuropsychological endophenotypefor BPD because these deficits are nonredundant with diagno-sis, as even relatives with clinically elevated response inhibitiondeficits were not symptomatic for BPD. The results of thisstudy may thus provide important clues for future geneticresearch to isolate genes which confer susceptibility to BPD.
There are some limitations to the current study which should benoted. First, it is important to note that the nonsignificant primarycomparisons of relatives and controls on the CPT were likelyunderpowered. The effect size difference between the two groupson the commissions index, for example, fell within the “medium”range, suggesting that relatives may indeed show remarkable re-sponse inhibition deficits, although future studies with sufficientlylarge samples of first-degree relatives of BPD patients shouldconfirm these findings. Second, whereas commission errors on theCPT represent a useful measure by which to investigate responseinhibition deficits, other neuropsychological measures may alsoshed light on response control difficulties in BPD. Future researchshould investigate the performance of BPD relatives on otherclassic neuropsychological response inhibition measures (e.g., go/no-go and stop-signal tasks) and related tests of planning anddecision-making (e.g., tower tests and gambling tasks). Perfor-mance on these measures may provide greater information aboutthe nature of neuropsychological aspects of impulsiveness in rel-atives at genetic risk for BPD. Third, the healthy control group
included in this study was younger than the probands and relatives,which may have impacted our findings. T-scores transformed byage and gender based on comprehensive normative data were usedto adjust for these differences, although it remains possible that ourfindings may have been biased by age-related effects not ac-counted for by normatively standardized scores. Fourth, given thesusceptibility of BPD patients to behavioral dysregulation underconditions of negative affect (Gratz, Rosenthal, Tull, Lejuez, &Gunderson, 2006), integration of emotional stimuli with neuropsy-chological response inhibition measures may improve the preci-sion of neuropsychological instruments for identifying possibleendophenotypes for BPD. Indeed, underlying neurocognitive vul-nerabilities in BPD may be exacerbated by negative emotionswhether triggered by interpersonal rejection (Ruocco et al., 2010)or emotional invalidation (Woodberry, Gallo, & Nock, 2008).Emotional variants of the go/no-go task have also shown utility inidentifying response inhibition deficits in BPD (Silbersweig et al.,2007). Further research is needed to determine whether thesedeficits may also be present in unaffected relatives. Fifth, we wereunable to address the specificity of response inhibition deficits asan endophenotype for BPD. Future studies should incorporatedimensional measures of personality and psychopathology, as wellas investigate probands with other personality disorders (and theirbiological relatives), to assess the degree to which these findingsmight be associated with specific cross-cutting personality dimen-sions and psychopathology more generally. The use of dimen-sional measures of personality and psychopathology may alsoassist in assessing phenotypic similarities and differences betweenempirically derived subgroups of BPD relatives. Finally, func-tional brain imaging forms an important component of any strategyto link intermediate phenotypes with genetic risk in family mem-bers. To that end, studies incorporating response control measuresand brain imaging protocols will help shed light on brain regionsshowing functional abnormality in probands and relatives, evenwhen there are no apparent differences in behavioral performanceson these tasks.
Taken together, this research provides important informationabout the prominence of response inhibition deficits in BPD pro-bands and their unaffected first-degree relatives, highlighting thatsome relatives may be more vulnerable than others to cognitivedeficit. Additionally, these data suggest that neuropsychologicalresponse inhibition deficits may be moderately heritable in af-fected sibling pairs, and given that they are nonredundant withdiagnosis, may increase the power of genetic linkage analyses.Response inhibition deficits may thus serve as promising candidateneuropsychological endophenotypes for BPD, which may not onlyaid research to understand the genetic causes of this illness butpossibly improve efforts at early identification and intervention forat-risk individuals.
References
American Psychiatric Association. (2000). Diagnostic and statistical man-ual of mental disorders (4th ed.). Text revision. Washington, DC:Author.
Arntz, A., Appels, C., & Sieswerda, S. (2000). Hypervigilance in border-line disorder: A test with the emotional Stroop paradigm. Journal ofPersonality Disorders, 14, 366–373. doi:10.1521/pedi.2000.14.4.366
Bazanis, E., Rogers, R. D., Dowson, J. H., Taylor, P., Meux, C., Staley,C., . . . Sahakian, B. J. (2002). Neurocognitive deficits in decision-
7RESPONSE INHIBITION AND BORDERLINE PERSONALITY
making and planning of patients with DSM-III-R borderline person-ality disorder. Psychological Medicine, 32, 1395–1405. doi:10.1017/S0033291702006657
Beblo, T., Saavedra, A. S., Mensebach, C., Lange, W., Markowitsch, H. J.,Rau, H., . . . Driessen, M. (2006). Deficits in visual functions andneuropsychological inconsistency in borderline personality disorder.Psychiatry Research, 145, 127–135. doi:10.1016/j.psychres.2006.01.017
Bechara, A., Damasio, H., Tranel, D., & Damasio, A. R. (1997). Decidingadvantageously before knowing the advantageous strategy. Science, 275,1293–1295. doi:10.1126/science.275.5304.1293
Bustamante, M. L., Villarroel, J., Francesetti, V., Rios, M., Arcos-Burgos,M., Jerez, S., . . . Silva, H. (2009). Planning in borderline personalitydisorder: Evidence for distinct subpopulations. World Journal of Bio-logical Psychiatry, 10, 512–517. doi:10.1080/15622970903079481
Comtois, K. A., Russo, J., Snowden, M., Srebnik, D., Ries, R., & Roy-Byrne, P. (2003). Factors associated with high use of public mentalhealth services by persons with borderline personality disorder. Psychi-atric Services, 54, 1149–1154. doi:10.1176/appi.ps.54.8.1149
Conners, C. K. (2000). Conners’ Continuous Performance Test II: Com-puter program for Windows technical guide and software manual.Toronto, Canada: Mutli-Health Systems.
Culbertson, W. C., & Zillmer, E. A. (2001). Tower of London - DrexelUniversity edition. Toronto, ON: Multi-Health Systems.
Cyders, M. A., & Coskunpinar, A. (2011). Measurement of constructsusing self-report and behavioral lab tasks: Is there overlap in nomotheticspan and construct representation for impulsivity? Clinical PsychologyReview, 31, 965–982. doi:DOI10.1016/j.cpr.2011.06.001
Dinn, W. M., Harris, C. L., Aycicegi, A., Greene, P. B., Kirkley, S. M., &Reilly, C. (2004). Neurocognitive function in borderline personalitydisorder. Progress in Neuro-Psychopharmacology and Biological Psy-chiatry, 28, 329–341. doi:10.1016/j.pnpbp.2003.10.012
Domes, G., Winter, B., Schnell, K., Vohs, K., Fast, K., & Herpertz, S. C.(2006). The influence of emotions on inhibitory functioning in border-line personality disorder. Psychological Medicine, 36, 1163–1172. doi:10.1017/S0033291706007756
Dougherty, D. M. (1999). IMT/DMT Immediate Memory Task & DelayedMemory Task: A research tool for studying attention and memoryprocesses. Houston, TX: University of Texas Health Sciences Center.
Egan, M. F., Goldberg, T. E., Gscheidle, T., Weirich, M., Bigelow, L. B.,& Weinberger, D. R. (2000). Relative risk of attention deficits in siblingsof patients with schizophrenia. The American Journal of Psychiatry,157, 1309–1316. doi:10.1176/appi.ajp.157.8.1309
Epstein, J. N., Johnson, D. E., Varia, I. M., & Conners, C. K. (2001).Neuropsychological assessment of response inhibition in adults withADHD. Journal of Clinical and Experimental Neuropsychology, 23,362–371. doi:10.1076/jcen.23.3.362.1186
Fan, J., McCandliss, B. D., Sommer, T., Raz, A., & Posner, M. I.(2002). Testing the efficiency and independence of attentional net-works. Journal of Cognitive Neuroscience, 14, 340 –347. doi:10.1162/089892902317361886
Fertuck, E. A., Lenzenweger, M. F., & Clarkin, J. F. (2005). The associ-ation between attentional and executive controls in the expression ofborderline personality disorder features: A preliminary study. Psycho-pathology, 38, 75–81. doi:10.1159/000084814
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. (1996). Structuredclinical interview for DSM-IV Axis I disorders—Patient edition (SCID-I/P, Version 2.0). New York, NY: Biometrics Research Department,New York State Psychiatric Institute.
Gottesman, I. I., & Gould, T. D. (2003). The endophenotype concept inpsychiatry: Etymology and strategic intentions. The American Journal ofPsychiatry, 160, 636–645. doi:10.1176/appi.ajp.160.4.636
Gratz, K. L., Rosenthal, M. Z., Tull, M. T., Lejuez, C. W., & Gunderson,J. G. (2006). An experimental investigation of emotion dysregulation in
borderline personality disorder. Journal of Abnormal Psychology, 115,850–855. doi:10.1037/0021-843x.115.4.850
Gunderson, J. G. (2009). Borderline personality disorder: Ontogeny of adiagnosis. The American Journal of Psychiatry, 166, 530–539. doi:10.1176/appi.ajp.2009.08121825
Haaland, V. O., & Landro, N. I. (2007). Decision making as measured withthe Iowa Gambling Task in patients with borderline personality disorder.Journal of the International Neuropsychological Society, 13, 699–703.doi:10.1017/S1355617707070890
Hester, R., Fassbender, C., & Garavan, H. (2004). Individual differences inerror processing: A review and reanalysis of three event-related fMRIstudies using the GO/NOGO task. Cerebral Cortex, 14, 986–994. doi:10.1093/cercor/bhh059
Jacob, G. A., Gutz, L., Bader, K., Lieb, K., Tuscher, O., & Stahl, C. (2010).Impulsivity in borderline personality disorder: Impairment in self-reportmeasures, but not behavioral inhibition. Psychopathology, 43, 180–188.doi:10.1159/000304174
Joyce, P. R., McHugh, P. C., Light, K. J., Rowe, S., Miller, A. L., &Kennedy, M. A. (2009). Relationships between angry-impulsive person-ality traits and genetic polymorphisms of the dopamine transporter.Biological Psychiatry, 66, 717–721. doi:10.1016/j.biopsych.2009.03.005
Judge, G. G., Griffiths, W. E., Hill, R. C., Lutkepohl, H., & Lee, T. C.(1980). The theory and practice of econometrics (2nd ed.). New York,NY: John Wiley and Sons.
Kaiser, S., Roth, A., Rentrop, M., Friederich, H. C., Bender, S., & Weis-brod, M. (2008). Intra-individual reaction time variability in schizophre-nia, depression and borderline personality disorder. Brain and Cogni-tion, 66, 73–82. doi:10.1016/j.bandc.2007.05.007
Konishi, S., Nakajima, K., Uchida, I., Kikyo, H., Kameyama, M., &Miyashita, Y. (1999). Common inhibitory mechanism in human inferiorprefrontal cortex revealed by event-related functional MRI. Brain, 122,981–991. doi:10.1093/brain/122.5.981
Konishi, S., Nakajima, K., Uchida, I., Sekihara, K., & Miyashita, Y.(1998). No-go dominant brain activity in human inferior prefrontalcortex revealed by functional magnetic resonance imaging. EuropeanJournal of Neuroscience, 10, 1209 –1213. doi:10.1046/j.1460-9568.1998.00167.x
Kunert, H. J., Druecke, H. W., Sass, H., & Herpertz, S. C. (2003). Frontallobe dysfunctions in borderline personality disorder? Neuropsychologi-cal findings. Journal of Personality Disorders, 17, 497–509. doi:10.1521/pedi.17.6.497.25354
Lampe, K., Konrad, K., Kroener, S., Fast, K., Kunert, H. J., & Herpertz,S. C. (2007). Neuropsychological and behaviouraldisinhibition in adultADHD compared to borderline personality disorder. Psychological Med-icine, 37, 1717–1729. doi:10.1017/S0033291707000517
Laporte, L., Paris, J., Russell, J., & Guttman, H. (2011). Psychopathology,trauma, and personality traits in patients with borderline personalitydisorder and their sisters. Journal of Personality Disorders, 25, 448–462. doi:10.1521/pedi.2011.25.4.448
Leichsenring, F., Leibing, E., Kruse, J., New, A. S., & Leweke, F. (2011).Borderline personality disorder. The Lancet, 377, 74–84. doi:10.1016/S0140-6736(10)61422-5
Lenzenweger, M. F., Lane, M. C., Loranger, A. W., & Kessler, R. C.(2007). DSM-IV personality disorders in the National ComorbiditySurvey Replication. Biological Psychiatry, 62, 553–564. doi:10.1016/j.biopsych.2006.09.019
Leyton, M., Okazawa, H., Diksic, M., Paris, J., Rosa, P., Mzengeza, S., . . .Benkelfat, C. (2001). Brain Regional alpha-[11C]methyl-L-tryptophantrapping in impulsive subjects with borderline personality disorder. TheAmerican Journal of Psychiatry, 158, 775–782. doi:10.1176/appi.ajp.158.5.775
Links, P. S., Heslegrave, R., & van Reekum, R. (1999). Impulsivity: Core
8 RUOCCO, LAPORTE, RUSSELL, GUTTMAN, AND PARIS
aspect of borderline personality disorder. Journal of Personality Disor-ders, 13, 1–9. doi:10.1521/pedi.1999.13.1.1
Livesley, W. J., Jang, K. L., Jackson, D. N., & Vernon, P. A. (1993).Genetic and environmental contributions to dimensions of personalitydisorder. The American Journal of Psychiatry, 150, 1826–1831.
Lutcke, H., & Frahm, J. (2008). Lateralized anterior cingulate functionduring error processing and conflict monitoring as revealed by high-resolution fMRI. Cerebral Cortex, 18, 508–515. doi:10.1093/cercor/bhm090
Maurex, L., Zaboli, G., Wiens, S., Asberg, M., Leopardi, R., & Ohman, A.(2009). Emotionally controlled decision-making and a gene variantrelated to serotonin synthesis in women with borderline personalitydisorder. Scandinavian Journal of Psychology, 50, 5–10. doi:10.1111/j.1467-9450.2008.00689.x
McCloskey, M. S., New, A. S., Siever, L. J., Goodman, M., Koenigsberg,H. W., Flory, J. D., & Coccaro, E. F. (2009). Evaluation of behavioralimpulsivity and aggression tasks as endophenotypes for borderline per-sonality disorder. Journal of Psychiatric Research, 43, 1036–1048.doi:10.1016/j.jpsychires.2009.01.002
Mostofsky, S. H., Schafer, J. G., Abrams, M. T., Goldberg, M. C., Flower,A. A., Boyce, A., . . . Pekar, J. J. (2003). fMRI evidence that the neuralbasis of response inhibition is task-dependent. Cognitive Brain Re-search. Cognitive Brain Research, 17, 419–430. doi:10.1016/S0926-6410(03)00144-7
Nakata, H., Sakamoto, K., Ferretti, A., Gianni Perrucci, M., Del Gratta, C.,Kakigi, R., & Luca Romani, G. (2008). Somato-motor inhibitory pro-cessing in humans: An event-related functional MRI study. Neuroimage,39, 1858–1866. doi:10.1016/j.neuroimage.2007.10.041
Nemoda, Z., Lyons-Ruth, K., Szekely, A., Bertha, E., Faludi, G., &Sasvari-Szekely, M. (2010). Association between dopaminergic poly-morphisms and borderline personality traits among at-risk young adultsand psychiatric inpatients. Behavioral and Brain Functions, 6, 4. doi:10.1186/1744-9081-6-4
Ni, X., Bismil, R., Chan, K., Sicard, T., Bulgin, N., McMain, S., &Kennedy, J. L. (2006). Serotonin 2A receptor gene is associated withpersonality traits, but not to disorder, in patients with borderline person-ality disorder. Neuroscience Letters, 408, 214 –219. doi:10.1016/j.neulet.2006.09.002
Ni, X., Chan, D., Chan, K., McMain, S., & Kennedy, J. L. (2009).Serotonin genes and gene-gene interactions in borderline personalitydisorder in a matched case-control study. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 33, 128–133. doi:10.1016/j.pnpbp.2008.10.022
Ni, X., Sicard, T., Bulgin, N., Bismil, R., Chan, K., McMain, S., &Kennedy, J. L. (2007). Monoamine oxidase a gene is associated withborderline personality disorder. Psychiatric Genetics, 17, 153–157. doi:10.1097/YPG.0b013e328016831c
Nigg, J. T., & Goldsmith, H. H. (1994). Genetics of personality disorders:Perspectives from personality and psychopathology research. Psycho-logical Bulletin, 115, 346–380. doi:10.1037/0033-2909.115.3.346
Nigg, J. T., Silk, K. R., Stavro, G., & Miller, T. (2005). Disinhibition andborderline personality disorder. Development and Psychopathology, 17,1129–1149. doi:10.1017/S0954579405050534
Paris, J. (2005). The development of impulsivity and suicidality in border-line personality disorder. Development and Psychopathology, 17, 1091–1104. doi:10.1017/S0954579405050510
Paris, J., Zelkowitz, P., Guzder, J., Joseph, S., & Feldman, R. (1999).Neuropsychological factors associated with borderline pathology in chil-dren. Journal of the American Academy of Child & Adolescent Psychi-atry, 38, 770–774. doi:10.1097/00004583-199906000-00026
Patton, J. H., Stanford, M. S., & Barratt, E. S. (1995). Factor structureof the Barratt impulsiveness scale. Journal of Clinical Psychology,51, 768 –774. doi:10.1002/1097-4679(199511)51:6�768::AID-JCLP2270510607�3.0.CO;2-1
Posner, M. I., Rothbart, M. K., Vizueta, N., Levy, K. N., Evans, D. E.,Thomas, K. M., & Clarkin, J. F. (2002). Attentional mechanisms ofborderline personality disorder. Proceedings of the National Academy ofSciences of the United States of America, 99, 16366–16370. doi:10.1073/pnas.252644699
Rentrop, M., Backenstrass, M., Jaentsch, B., Kaiser, S., Roth, A., Unger, J.,. . . Renneberg, B. (2008). Response inhibition in borderline personalitydisorder: Performance in a Go/Nogo task. Psychopathology, 41, 50–57.doi:10.1159/000110626
Riccio, C. A., Reynolds, C. R., Lowe, P., & Moore, J. J. (2002). Thecontinuous performance test: A window on the neural substrates forattention? Archives of Clinical Neuropsychology, 17, 235–272.
Risch, N., & Merikangas, K. (1996). The future of genetic studies ofcomplex human diseases. Science, 273, 1516 –1517. doi:10.1126/science.273.5281.1516
Rubio, G., Jimenez, M., Rodriguez-Jimenez, R., Martinez, I., Iribarren,M. M., Jimenez-Arriero, M. A., . . . Avila, C. (2007). Varieties ofimpulsivity in males with alcohol dependence: The role of Cluster-Bpersonality disorder. Alcoholism: Clinical and Experimental Research,31, 1826–1832. doi:10.1111/j.1530-0277.2007.00506.x
Ruocco, A. C. (2005). The neuropsychology of borderline personalitydisorder: A meta-analysis and review. Psychiatry Research, 137, 191–202. doi:10.1016/j.psychres.2005.07.004
Ruocco, A. C., McCloskey, M. S., Lee, R., & Coccaro, E. F. (2009).Indices of orbitofrontal and prefrontal function in Cluster B and ClusterC personality disorders. Psychiatry Research, 170, 282–285. doi:10.1016/j.psychres.2008.12.003
Ruocco, A. C., Medaglia, J. D., Tinker, J. R., Ayaz, H., Forman, E. M.,Newman, C. F., . . . Chute, D. L. (2010). Medial prefrontal cortexhyperactivation during social exclusion in borderline personality disor-der. Psychiatry Research: Neuroimaging, 181, 233–236. doi:10.1016/j.pscychresns.2009.12.001
Rusch, N., Weber, M., Il’yasov, K. A., Lieb, K., Ebert, D., Hennig, J., &van Elst, L. T. (2007). Inferior frontal white matter microstructure andpatterns of psychopathology in women with borderline personality dis-order and comorbid attention-deficit hyperactivity disorder. Neuroim-age, 35, 738–747. doi:10.1016/j.neuroimage.2006.12.007
Schuermann, B., Kathmann, N., Stiglmayr, C., Renneberg, B., & Endrass,T. (2011). Impaired decision making and feedback evaluation in bor-derline personality disorder. Psychological Medicine, 41, 1917–1927.
Sieswerda, S., Arntz, A., Mertens, I., & Vertommen, S. (2007). Hypervigi-lance in patients with borderline personality disorder: Specificity, auto-maticity, and predictors. Behaviour Research and Therapy, 45, 1011–1024. doi:10.1016/j.brat.2006.07.012
Silbersweig, D., Clarkin, J. F., Goldstein, M., Kernberg, O. F., Tuescher,O., Levy, K. N., . . . Stern, E. (2007). Failure of frontolimbic inhibitoryfunction in the context of negative emotion in borderline personalitydisorder. The American Journal of Psychiatry, 164, 1832–1841. doi:10.1176/appi.ajp.2007.06010126
Silverman, J. M., Pinkham, L., Horvath, T. B., Coccaro, E. F., Klar, H.,Schear, S., . . . Siever, L. J. (1991). Affective and impulsive personalitydisorder traits in the relatives of patients with borderline personalitydisorder. The American Journal of Psychiatry, 148, 1378–1385.
Skodol, A. E., Gunderson, J. G., Shea, M. T., McGlashan, T. H., Morey,L. C., Sanislow, C. A., . . . Stout, R. L. (2005). The CollaborativeLongitudinal Personality Disorders Study (CLPS): Overview and impli-cations. Journal of Personality Disorders, 19, 487–504. doi:10.1521/pedi.2005.19.5.487
Skodol, A. E., Stout, R. L., McGlashan, T. H., Grilo, C. M., Gunderson,J. G., Shea, M. T., . . . Oldham, J. M. (1999). Co-occurrence of moodand personality disorders: A report from the Collaborative Longitu-dinal Personality Disorders Study (CLPS). Depression and Anxiety,10, 175–182. doi:10.1002/(SICI)1520-6394(1999)10:4�175::AID-DA6�3.0.CO;2-2
9RESPONSE INHIBITION AND BORDERLINE PERSONALITY
Soloff, P. H., Meltzer, C. C., Greer, P. J., Constantine, D., & Kelly, T. M.(2000). A fenfluramine-activated FDG-PET study of borderline person-ality disorder. Biological Psychiatry, 47, 540–547. doi:10.1016/S0006-3223(99)00202-4
Swann, A. C., Bjork, J. M., Moeller, F. G., & Dougherty, D. M. (2002).Two models of impulsivity: Relationship to personality traits and psy-chopathology. Biological Psychiatry, 51, 988–994. doi:10.1016/S0006-3223(01)01357-9
Swirsky-Sacchetti, T., Gorton, G., Samuel, S., Sobel, R., Genetta-Wadley,A., & Burleigh, B. (1993). Neuropsychological function in borderlinepersonality disorder. Journal of Clinical Psychology, 49, 385–396. doi:10.1002/1097-4679(199305)49:3�385::AID-JCLP2270490313�3.0.CO;2-4
Tadic, A., Victor, A., Baskaya, O., von Cube, R., Hoch, J., Kouti, I., . . .Dahmen, N. (2009). Interaction between gene variants of the serotonintransporter promoter region (5-HTTLPR) and catecholO-methyltransferase (COMT) in borderline personality disorder. Amer-ican Journal of Medical Genetics Part B: Neuropsychiatric Genetics,150B, 487–495. doi:10.1002/ajmg.b.30843
Van den Eynde, F., Senturk, V., Naudts, K., Vogels, C., Bernagie, K.,Thas, O., . . . Audenaert, K. (2008). Efficacy of quetiapine for impul-sivity and affective symptoms in borderline personality disorder. Journalof Clinical Psychopharmacology, 28, 147–155. doi:10.1097/JCP.0b013e318166c4bf
Völlm, B., Richardson, P., Stirling, J., Elliott, R., Dolan, M., Chaudhry, I.,. . . Deakin, B. (2004). Neurobiological substrates of antisocial andborderline personality disorder: Preliminary results of a functional fMRIstudy. Criminal Behaviour and Mental Health, 14, 39–54. doi:10.1002/cbm.559
Watanabe, J., Sugiura, M., Sato, K., Sato, Y., Maeda, Y., Matsue, Y., . . .Kawashima, R. (2002). The human prefrontal and parietal associationcortices are involved in NO-GO performances: An event-related fMRIstudy. Neuroimage, 17, 1207–1216. doi:10.1006/nimg.2002.1198
Whiteside, S. P., & Lynam, D. R. (2001). The Five Factor Model andimpulsivity: Using a structural model of personality to understand im-pulsivity. Personality and Individual Differences, 30, 669–689. doi:10.1016/S0191-8869(00)00064-7
Wingenfeld, K., Rullkoetter, N., Mensebach, C., Beblo, T., Mertens, M.,Kreisel, S., . . . Woermann, F. G. (2009). Neural correlates of theindividual emotional Stroop in borderline personality disorder. Psycho-neuroendocrinology, 34, 571–586. doi:10.1016/j.psyneuen.2008.10.024
Woodberry, K. A., Gallo, K. P., & Nock, M. K. (2008). An experimentalpilot study of response to invalidation in young women with features ofborderline personality disorder. Psychiatry Research, 157, 169–180.doi:10.1016/j.psychres.2007.06.007
Zanarini, M. C., Barison, L. K., Frankenburg, F. R., Reich, D. B., &Hudson, J. I. (2009). Family history study of the familial coaggregationof borderline personality disorder with axis I and nonborderline dramaticcluster axis II disorders. Journal of Personality Disorders, 23, 357–369.doi:10.1521/pedi.2009.23.4.357
Zanarini, M. C., Gunderson, J. G., & Frankenburg, F. R. (1989). Therevised diagnostic interview for borderlines: Discriminating BPD fromother Axis II disorders. Journal of Personality Disorders, 3, 10–18.doi:10.1521/pedi.1989.3.1.10
Received June 2, 2011Revision received April 20, 2012
Accepted April 26, 2012 �
10 RUOCCO, LAPORTE, RUSSELL, GUTTMAN, AND PARIS