Review For reprint orders, please contact
-
Upload
independent -
Category
Documents
-
view
1 -
download
0
Transcript of Review For reprint orders, please contact
For reprint orders, please contact [email protected]
365
Review
www.expert-reviews.com ISSN 1476-0584© 2011 Expert Reviews Ltd10.1586/ERV.10.172
Despite recommendations to expand influenza vaccine coverage in the USA to 85% of the popu-lation, less than 40% received the vaccine in the 2008–2009 season [1]. Indeed uptake of influenza vaccine among the high-risk groups in the USA has not changed over the past decade [2]. Recently, a number of innovative influenza vaccines have been licensed for prophylaxis of seasonal and pandemic influenza using split antigens contain-ing novel adjuvants [3–5]. Such vaccines have the potential to broaden the use of influenza vaccines by providing improved immunogenicity and pro-tection against both vaccine and variant strains. In addition, adjuvanted influenza vaccines allow for antigen sparing in pandemic situations.
Phobia of needles is often cited as an obstacle to influenza vaccine usage in infants and adults [6,7]. Less invasive routes of administering influenza vaccines may also increase vaccine acceptance and compliance [8]. To address this need, alternative methods of immunization have been explored for influenza vaccines, including transcutaneous [9],
intranasal [10], sublingual [11] and oral [12] routes. FluMist™ (MedImmune, MD, USA), an intra-nasally delivered live-attenuated influenza vac-cine (LAIV), is the only noninjectable influenza vaccine licensed for human use [13].
Early studies demonstrated that intranasally administered inactivated whole-influenza viruses were capable of inducing significant protective immune responses in humans [14,15]. Currently licensed inf luenza vaccines are inactivated detergent-split virus preparations containing the hemagglutinin protein; however, split-influenza vaccines are generally less immunogenic via the intranasal route and require mucosal adjuvants to elicit strong protective immune responses. The most investigated of such adjuvants have been cholera toxin (CT) and Escherichia coli heat labile toxin (LT) and their variants [16,17]. Indeed an intranasal virosomal influenza vac-cine containing LT was licensed in Switzerland based on a successful clinical development pro-gram [18]. Nevertheless, this vaccine was taken
David Burt†1, Corey Mallett1, Martin Plante1, Joseph Zimmermann1, Krikor Torossian1 and Louis Fries2 1GlaxoSmithKline Biologicals of North America, Research and Development, 525 Cartier boulevard. West Laval, Quebec, Canada, H7V 3S8 2GlaxoSmithKline Biologicals of North America, Global Clinical Research and Development, 6996 Columbia Gateway Drive, Suite 103, Columbia, MD 21046-3303, USA†Author for correspondence:Tel.: +1 450 978 6322 Fax: +1 450 978 6340 [email protected]
The development of a safe and effective non-live intranasal influenza vaccine has been an elusive target in vaccinology for many decades. It is perceived that intranasal immunization, by offering a more convenient and less invasive vaccination modality, will boost vaccination rates against influenza, a disease that continues to inflict a significant annual health and economic burden worldwide. Intranasal immunization may also confer additional immunoprotective benefits by eliciting mucosal secretory antibodies at the site of entry of the virus, which are typically more broadly cross-reactive and cross-protective compared with those induced by systemic routes of vaccination. This property is highly desirable for confering improved protection against variant strains of influenza virus. Here we review the current status of intranasal proteosome-based influenza vaccines that comprise commercial detergent-split influenza antigens and proteosome adjuvants derived from purified bacterial outer membrane proteins. We demonstrate that these vaccines exhibit the desired advantages expected from immunization via the intranasal route. Furthermore, in clinical trials proteosome-based influenza vaccines were shown to be safe and protective in humans. The future possibilities for commercializing intranasal proteosome–influenza vaccines are also discussed.
Keywords: influenza vaccine • intranasal immunization • mucosal immunity • proteosome-based adjuvants
Proteosome-adjuvanted intranasal influenza vaccines: advantages, progress and future considerationsExpert Rev. Vaccines 10(3), 365–375 (2011)
Expert Rev. Vaccines 10(3), (2011)366
Review Burt, Mallett, Plante, Zimmermann, Torossian & Fries
off the market since it was associated with an increased incidence of Bell’s palsy [8,19]. It has also been demonstrated that LT and CT are transported to the olfactory region of rodent brains following intranasal administration [20]. Other mucosal intranasal adjuvants that have been examined with influenza vaccines include detoxi-fied lipopolysaccharide (LPS) [21], TLR-9 agonist [22], immunos-timulatory complexes [23], MF59 emulsion [24], TLR-3 agonists [25] and chito san [26]. Currently, there are no adjuvanted non-living intranasal influenza vaccines approved for use in humans.
Apart from providing a less invasive method of immunization compared with intramuscular vaccines, intranasal vaccines offer additional immunological and potentially improved protective advantages. The intranasal and gut epithelia constitute areas of follicular-associated lymphoid tissue that contain the full array of immune-competent cells needed to generate an immune response. These cells include B cells that produce polymeric IgA (pIgA), which is secreted into the mucosal lumen providing protective immunity at the site of entry of many pathogens including respiratory viruses [27]. Intranasal influenza vaccines have been shown to induce both serum IgG and pIgA, which are important for protection of the lower and upper respiratory tracts, respectively [28].
Polymeric IgA is five- to ten-times more efficient than mono-meric IgA and IgG at neutralizing influenza virus in vivo [29]. In an influenza model, pIgA was five-times more effective than monomeric IgA in inhibiting hemagglutination of red cells by influenza virus and seven- to ten-times more effective than monomeric IgA in virus neutralization [30].
Studies in mouse models of influenza confirmed by various investigators have shown mucosal immunization to be more cross-reactive (and cross-protective) than serum antibodies against variant strains of influenza. This heterosubtypic cross-protection correlated with the ability of the vaccines to produce secretory IgA (sIgA) [31], and was induced by intranasal but not subcuta-neous immunization with seasonal [32] and pandemic influenza antigens [33]. Intriguingly, in one report, intranasally adminis-tered seasonal strains also protected mice against H5N1 chal-lenge suggesting that the mucosal route may offer significantly enhanced protection against both heterotypic and drift variants of influenza [34].
Evidence of heterosubtypic responses have also been observed in humans in clinical trials involving intranasal LAIV. Both cross-reac-tive hemagglutination inhibition (HAI) [35] and cross-protection [36] were reported against variant strains not in the vaccine.
The mechanism for this superior crossreactivity and protection is not clear but may be related to the higher avidity of the pIgA and/or the ability of sIgA to inhibit viral replication intracellularly as it translocates from the basal to apical surface of respiratory epithelial cells [37,38].
This article describes the development progress and current status of intranasal influenza vaccines that utilize commercial detergent-split-influenza antigen and a class of adjuvants known as proteosomes, derived from extracted bacterial outer membrane proteins (OMPs). These proteosome-based vaccines have been used successfully in preclinical and clinical trials and offer an attractive non-live intranasal influenza vaccine alternative.
Proteosome-based adjuvantsProteosomes are hydrophobic nanoparticles comprising of OMPs with trace amounts of purified lipooligosaccharide (LOS), particularly from Neisseria meningitidis [39,40].
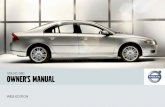
Two forms of proteosome-adjuvanted vaccines shown schemati-cally in Figure 1 have been explored. Proteosome–antigen com-plexes are defined as proteosomes noncovalently associated via interactions with hydrophobic domains of the proteosome OMP and amphophilic antigens (such as viral membrane glycopro-teins [41,42], lipopeptides [43] and lipid oligosaccharides [44]). Briefly, these preparations are produced by mixing antigen with deter-gent-solubilized proteosomes and removing detergent by dialysis (Figure 1A). A second class of proteosome adjuvants are pre-formed soluble proteosome–LPS particles that are mixed with antigen (Figure 1B). An example of this type of adjuvant is protollin [45], which comprises proteosomes noncovalently associated with LPS from Shigella flexneri, originally developed as a intranasal vaccine for shigellosis [44]. In animal model systems, mucosally adminis-tered proteosome vaccines have successfully induced strong sys-temic and mucosal immune responses against various types of antigen and have provided protection against infectious challenges with bacteria and viruses [42–48].
Mechanism of adjuvant action Evidence from a variety of studies suggests that proteosome OMP alone or formulated with LPS (e.g., protollin) stimulate innate immune responses leading to enhanced adaptive immunity.
The major protein components of proteosomes derived from N. meningitidis are the OMPs PorA (class 1) and PorB (class 2) and the class 4 protein [40,49]. PorB has been identified as an agonist for TLR-2 [50]. LOS (in proteosomes) and LPS (in protollin) are agonists for TLR-4 and CD14 [51]. Stimulation of these receptors can increase MHC class I and II expression on antigen-presenting cells, elicit proinflammatory cytokines that secondarily upregu-late the IL-2 receptor, B7.2 (CD86) and adhesion molecules, and stimulate maturation of dendritic cells [52].
Proteosome–antigen complexes induce secretion of TNF-a and IL-6 from adherent cells from human peripheral blood mono-nuclear cells (PBMCs) and macrophage-like cell lines [Plante M,
Unpublished Observations]. These responses were blocked by anti-TLR-1 or 2 antibodies while anti-TLR-4 or anti-CD14 had little effect. By contrast, protollin activated monocyte cell lines through TLR-1, -2 and-4 [Larocque D, Unpublished Observations], implicating a role for LPS and OMPs in the immunostimulatory activity of this adjuvant.
Recently, proteosome adjuvants were shown to induce the expres-sion of proinflammatory cytokines IL-6, IL-1b and IL-17 in mouse lungs following intranasal administration [Bélanger B, Manuscript
Submitted]. This was paralleled by the increased expression of the neutrophil chemoattractants CXCL1, CXCL2 and CCL20 ligand, which are known to be expressed on lymphocytes and dendritic cells. Furthermore, granulocyte colony-stimulating factor expression was highly upregulated by intranasally administered proteo some-based adjuvants. These results suggest a role for the IL-23/IL-17 axis in the mode of action of proteosome-based adjuvants.
www.expert-reviews.com 367
ReviewProteosome-adjuvanted intranasal influenza vaccines
Proteosomes also facilitate the uptake of vaccines into mucosal surfaces. The effects of proteosome adjuvants on follicle-associated epithelium (FAE) and resident dendritic cells (DCs) in vivo were studied using mouse Peyer’s patches [53]. Proteosomes accelerated the transepithelial transport of latex microparticles by M cells and also induced the migration of DCs into the FAE. Both effects were
dependent on expression of TLR-2. Intraepithelial DCs captured both latex microparticles and proteosomes [53].
Preclinical immunogenicity & protectionThe first evidence that proteosomes could be used as effective adjuvants for influenza antigens came from studies with synthetic
Extraction and purificationof OMPs
Extraction and purificationof OMPs
Detergent solubilized OMPs
Detergent-solubilized OMPs
Mixing and dialysis to remove detergent
Extraction and purificationof LPS
LPS
Protollin
Protollin-adjuvanted influenza vaccine(OMP–LPS complex + HA)
Mixing and dialysisto remove detergent
Influenza virus
Influenza virus
Split influenza antigen
Split influenza antigen
Proteosome adjuvanted influenza vaccine (OMP–HA complex)Detergent split of virus and
purification of influenza proteins
Detergent split of virus andpurification of influenza proteins
Neisseria meningitidis
Neisseria meningitidis
Shigella flexneri
Proteosome-based influenza vaccine
Protollin-based influenza vaccine
Expert Rev. Vaccines © Future Science Group (2011)
Figure 1. Preparation of proteosome-based influenza vaccines. Two varieties of proteosome-adjuvanted influenza vaccines are discussed in this article. (A) Proteosome–influenza complexes are produced by formulating detergent-solubilized endogenous lipooligosaccharide-depleted Neisseria meningitidis OMPs with influenza split antigen and removing detergent [55]. (B) Protollin is produced by formulating LPS with detergent-solubilized N. meningitidis OMPs [45]. On removal of detergent, a stable and soluble OMP–LPS is produced. Protollin influenza vaccine is prepared by mixing preformed protollin with influenza split antigen immediately prior to immunization. HA: Hemagglutination; LPS: Lipopolysaccharide; OMP: Outer membrane protein.
Expert Rev. Vaccines 10(3), (2011)368
Review Burt, Mallett, Plante, Zimmermann, Torossian & Fries
peptides representing either influenza B-cell epitopes on HA or CD4+ and CD8+ epitopes within the nucleoprotein [54]. Such peptides anchored to proteosomes were able to induce partially protective immune responses in mice. However, the use of pep-tide-based influenza vaccines as vaccine antigens for humans may not be the preferred strategy owing to HLA polymorphism in the human population.
We examined the ability of proteosome-based adjuvants to aug-ment the immunogenicity and efficacy of intranasal influenza HA that have either been licensed or that are under develop-ment for use in humans as split-influenza or recombinant antigen. Proteosome influenza formulations were prepared by formulating detergent-split monovalent antigens, seasonal trivalent influenza antigens or baculovirus-expressed recombinant HA (rHA) with proteosomes to achieve various HA:OMP ratios [55,56]. Vaccines comprised of split antigens or rHA mixed with protollin were also examined [45].
The proteosome-based vaccines induced high levels of virus-specific HAI serum antibodies comparable to those induced by split-influenza antigen given by the intramuscular route.
Furthermore, in contrast to split antigen given intramuscularly, only proteosome-formulated or protollin-mixed split-antigen vac-cines were capable of inducing significant levels of influenza-specific IgA in mouse lungs and intranasal washes. Production of these antibodies required that the split-influenza antigen be formulated with proteosomes or mixed with protollin since split-influenza antigen alone given intranasally did not induce significant amounts of serum HAI antibodies and no mucosal IgA [45,55,56].
Studies were performed in vivo to investigate the involvement of TLR-2 and -4 in the adjuvanticity of proteosome-based influ-enza vaccines [Plante M, Unpublished Data]. Anti-influenza IgG responses were induced in C3H wild-type animals by intra nasal administration of influenza antigen given with protollin but were significantly reduced in C3H/HeJ mice that have a missense mutation in their TLR-4 gene and thus fail to respond to LPS. Conversely, proteosome-formulated influenza antigen induced
equivalent strong anti-influenza responses in both C3H/HeJ and C3H wild-type mice. These data indicate a role for TLR-4 in the systemic antibody response stimulated by protollin (probably due to the presence of LPS) but not for proteosomes that have depleted LOS levels. These results confirm the TLR–ligand usage of these adjuvants observed in in vitro studies (see ‘Mechanism of adjuvant action’ section).
Proteosome-based influenza vaccines also modulated influ-enza virus-specific cytokine responses towards a type 1 pheno-type, which is in contrast to the type 2-biased responses elicited by antigen alone given intranasally or by the intramuscular route [45,55,56].
Intranasal administration of influenza-split antigens with proteosome-based adjuvants completely protected mice against live virus challenge, as measured by mortality and weight loss [45,55,56]. The proteosome split-influenza formulation pro-tected mice against homologous virus to the same extent as split-influenza alone given intramuscularly [55]. Importantly, purified A/Texas/91 H1N1 baculovirus expressed rHA antigen mixed with protollin completely protected mice against chal-lenge with a H1N1 homotypic drift strain, A/Taiwan/86 [45]. Interestingly, rHA given via the intramuscular route only par-tially protected the mice against mortality and morbidity. At the equivalent dose of rHA, the protollin-adjuvanted intrana-sal formulation induced fourfold higher HAI titers, 17-fold higher lung IgA titers and fourfold higher IFN-g compared with antigen alone given intramuscularly [45]. One or a com-bination of these enhanced immune responses may explain the improved protection induced by the intranasal protollin-adjuvanted vaccine.
Licensed influenza vaccines are presently given as a triva-lent formulation of H1, H3 subtype and type B antigens. Proteosome-based vaccines prepared with each of the three influenza strains and given in combination intranasally induced serum HAI and mucosal IgA responses against each HA sero-type equivalent to levels induced by the individual formulations [Jones D, Unpublished Data].
Table 1. Safety profile of the proteosome–influenza vaccine in humans.
Type of finding Frequency (%) Severity Description
Immediate complaints† 5–20 Mild Local burning and itching of nose, throat or eyes. Frequency similar to placebo
Objective local reactions‡ 5–19
0–19
Mild
Minor
Nasal inflammation or discharge. No difference in frequency or severity between the first and second treatments or the vaccine and placeboAsymptomatic cervical lymph node enlargement. Frequency similar in vaccine and placebo
Subjective reactogenicity findings§ 25–33
20–56
Mild
Mild
Headache and fatigue. No association with vaccineRunny nose, stuffiness, nasal itching and sneezing. Modest increase in vaccine versus placebo without dose response. Frequency in vaccine lower at second versus first dose
†30 min after dosing.‡Physician findings 7 days after dosing.§7 days after dosing.Summary of findings from various clinical trials in 1300 healthy adults representing approximately 1600 doses of active product. Data from [46,60,61].
www.expert-reviews.com 369
ReviewProteosome-adjuvanted intranasal influenza vaccines
Additional murine preclinical studies were performed to mimic the situation in humans where repeated vaccination with influenza vaccine containing a new variant strain occurs on an annual basis. Mice were re-immunized with a intranasal proteosome–influenza vaccine 9 months after receiving either the identical proteosome vaccine, or exposure to antigens of a drifted strain of influenza given in the form of either an intra-nasal proteosome–influenza vaccine or a standard intramuscular split-influenza vaccine, or live influenza virus [57]. In each of these experimental situations, high levels of serum HAI and mucosal IgA antibody were induced against the heterosubtypic re-immunizing strain in the proteosome. These data indicate that yearly administration of intranasal proteosome–influenza vaccine does not suppress specific immune responses against the most recent strain, irrespective of the form of influenza antigen originally administered.
The ferret is a recognized animal model for use in devel-oping influenza vaccines. Unlike mice, they are susceptible to infection by nonadapted human strains of influenza [58]. We assessed the ability of intranasal immunization of ferrets with a monovalent proteosome–influenza preparation to reduce virus shedding following challenge with homologous live influenza. Prechallenge levels of serum HAI antibodies were significantly higher in proteosome–influenza immunized ferrets compared with those produced by ferrets that were nonimmunized or that received the same dose of HA antigen alone via the intra-muscular route. Furthermore, virus shedding was significantly reduced in the animals that received the proteosome formu-lation compared with the phosphate-buffered saline controls [Fries L, Unpublished Data].
Nonclinical toxicity studiesSince the proteosome-formulated influenza vaccines were more advanced in the development pipeline they were prioritized over the protollin-mixed vaccines for clinical evaluation. Prior to investigation in humans, good laboratory practice-compliant toxicity studies were performed to evaluate the safety of proteo-some–influenza vaccines when given intranasally. Vaccines were prepared by a good manufacturing practice process.
Since BALB/c mice exhibit strong immune responses to pro-teosome–influenza vaccines, all studies performed in these ani-mals immunized with these vaccines have shown protection against influenza challenge. Importantly, this strain of mouse is particularly susceptible to the translocation of intranasally administered LT and CT to the olfactory region of the brain and has been recommended as a suitable model to assess the toxicity of intranasally administered products [101].
Three administrations of test article were examined given at 14-day intervals (a maximum of two immunizations are expected to be given to humans in a single season). No active treatment-related changes in weight, food consumption or clini-cal signs were observed [Fries L, Unpublished Data]. There were no gross or histopathologic findings of the nose, paranasal tissues, respiratory tract, olfactory bulb or CNS that occurred with a frequency or relation to dosage that suggested causation by the
vaccine. The no-observed adverse effect level (NOAEL) was at least 100-fold greater, on a µg/kg basis, than the maximum projected human dose.
CNS translocation studiesNasally administered influenza vaccines adjuvanted with bacte-rial toxins such as CT and LT are known to translocate to the brain in mice [20] and to be associated with increased incidence of Bell’s Palsy in humans [19]. The mechanism of translocation in mice appears to be through binding to GM1-gangliosides and retrograde transport to the olfactory region via neurons that extend into the intranasal cavity [20]. While there is no mechanistic rationale for intranasally administered proteo-somes to reach the brain, we nevertheless performed studies to investigate this possibility. Polyvalent rabbit antisera spe-cific for either influenza HA, proteosome OMPs or CT were used to detect these materials in the brains of treated mice via immunohistochemistry. Results indicated that neither HA or proteosome proteins could be detected in brain tissue after administration of proteosome–influenza vaccines. Conversely, CT could be detected when administered alone or with intra-nasal proteosome–influenza vaccines [Plante M, Unpublished Data]. Similarly we could find no evidence that protollin migrates to the brain after intranasal administration [Plante M, Unpublished
Data] [59]. Combined with data from the previously described GLP nonclinical toxicity studies described above, these find-ings demonstrated that unlike CT and LT adjuvanted influenza vaccine, proteosome–influenza vaccines do not translocate to the brain and do not induce histopathology in the olfactory bulb or CNS.
Clinical studies Intranasal proteosome–influenza vaccines have been tested for safety, immunogenicity and efficacy in various Phase I and II human clinical trials involving more than 1800 healthy subjects of 3–65 years of age. To date, there have been no studies in children under 3 years of age or in high-risk groups.
The studies discussed later in this article involved healthy adults and included the testing of monovalent [60] and trivalent [46] prote-osome-formulated influenza split-antigens given as one (7.5–45 µg HA/dose) or two (15–30 µg HA/dose) doses at 14-day intervals. Two of the studies were placebo-controlled, randomized, double-blind, in-patient virus challenges of subjects [61] and a third study evaluated the efficacy of the vaccine in a field study setting [62].
Intranasal vaccines were administered at 100–140 µl per nostril using a metered-dose nasal spray pump [60] delivering the vaccine in droplets of mean particle size of between 40 and 50 µm. Less than 10% of droplets were of diameter ≤10 µm, ensuring that the vaccine was distributed mainly in the nasal pharynx.
Safety in humansProteosome influenza vaccines were consistently well tolerated in all clinical studies (TABle 1). Mild and reversible local reactogencity was observed in 20–56% of subjects but these were not statisti-cally different from placebo (phosphate-buffered isotonic saline).
Expert Rev. Vaccines 10(3), (2011)370
Review Burt, Mallett, Plante, Zimmermann, Torossian & Fries
Symptoms included runny and/or stuffy nose, nasal burning or itching, or sneezing [46,60,61]. The frequency of these complaints generally did not show a significant association with active treat-ment or a clear dose response.
Headache and fatigue were the most common systemic symp-toms. Fever was uncommon and low grade. None of these obser-vations were associated with active treatment. These safety results compare favorably with those reported in a similar age group that received FluMist, the licensed intranasal live-attenuated influenza vaccine [63].
Proteosome-influenza vaccines have demonstrated a benign safety profile in humans. After approximately 1600 doses in 1300 volunteers there has been no evidence of association with wheezing or reactive airway disease. Indeed, there has been a persistent decrease in all respiratory system adverse events in all proteosome–influenza groups, which has been observed repeat-edly (even outside the winter influenza season) and has, in studies of adequate size, attained significance.
Immunogenicity in humansVirus-specific antibody responses were measured 14 days after each dose of vac-cine and in some studies at intervals up to 140 days post primary immunization. Standard HAI was measured in serum, and sIgA was determined in nasal washes or saliva by kinetic ELISA assay specific for sIgA [45].
Intranasal proteosome–inf luenza vac-cines consistently induced signif icant increases in serum HAI and sIgA against all strains.
A monovalent prototype proteosome split-influenza (H1N1) vaccine was first tested in two randomized blinded com-parator-controlled trials in healthy adults 18–45 years of age [60]. Safety and immu-nogenicity of the proteosome split-influ-enza vaccine formulated at a 4:1 HA:OMP ratio was compared with control groups that received the same antigen either as split-influenza antigen administered alone intranasally or trivalent inactivated influ-enza vaccine (TIV) given intramuscularly in subjects with pre-immunization HAI titers of <40 and in unselected subjects. The proteosome–influenza vaccines were immunogenic in both the naive and the unselected populations. Up to 60% of the naive subjects induced significant rises in serum HAI of ≥fourfold and up to 88% of the subjects showed significant increases in mucosal IgA. As demonstrated in the pre-clinical studies, formulation of the antigen with proteosomes was necessary to achieve this response since the split-influenza anti-
gen given alone intranasally did not produce significant increases in either serum or mucosal parameters. While the intramuscular TIV was highly immunogenic in terms of magnitude and fre-quency of the serum HAI response (≥fourfold in up to 92% of the subjects), it failed to induce significant increases in mucosal IgA. Generally, the two-dose proteosome–influenza regimens induced higher mucosal IgA and serum responses compared with single-dose schedules. The serum HAI and nasal sIgA responses induced by the proteosome split-influenza vaccine were long-lived and remained significantly elevated throughout the testing period of up to 126 days. This is a critically impor-tant finding since it suggests that proteosome-based intranasal influenza vaccines can induce potentially protective immune responses in the serum and mucosal compartments that persist through a typical influenza season. There was no significant rise in antibody responses to the proteosome OMPs and no impact of pre-existing anti-OMP antibodies in the response to the associated influenza antigen.
Per
cen
t la
bo
rato
ry-c
on
firm
ed in
flu
enza
illn
ess
Prec
halle
nge
HA
I
Prechallenge virus-specific nasal sIgA
5 to 19
20 to 79
80 to 320LowMid
High
80
70
60
50
40
30
20
10
0
Figure 2. Contribution of virus-specific serum hemagglutination inhibition and nasal secretory IgA to protection against influenza challenge. Data described in [61] was further analyzed to determine the correlation between laboratory-confirmed influenza illness and prechallenge nasal sIgA and corresponding serum HAI in human subjects who received a trivalent proteosome–influenza vaccine. Healthy adults received one or two intranasal doses of proteosome vaccine containing A/Panama/207/99 H3N2 on days 0 and 14 prior to challenge with with the homologous egg-grown H3N2 virus on day 42. Logistic regression model analysis gave p-values of 0.0007 (HAI) and 0.0051 (sIgA) for one covariant and 0.0016 (HAI) and 0.014 (sIgA) for two covariants indicating significant correlation between protection against laboratory-confirmed influenza and HAI and sIgA either individually or together. HAI: Hemagglutination inhibition; sIgA: Secretory IgA. Data taken from [61].
www.expert-reviews.com 371
ReviewProteosome-adjuvanted intranasal influenza vaccines
In a subsequent placebo-controlled study, the safety and immuno gencity of an intranasal proteosome trivalent split-influ-enza vaccine was evaluated in healthy adults [46]. Importantly, statistically significant serum and mucosal responses were dem-onstrated against each of the two A and the B strain. A total of 60% of the subjects responded with a ≥fourfold increase in serum HAI against the A strains. As often observed for TIV, the frequency of the serum response was lower (33%) for the type B strain. Consistent with the monovalent study, the two-dose regi-men (30 µg HA × 2) gave the highest significant mucosal IgA response (up to 80% responders) that persisted up to at least 140 days post immunization. It is noteworthy that ≥60% of subjects entering the study without protective titers (≤40 HAI) responded with either HAI, sIgA or both to the nasal proteasome vaccines, suggesting that they had achieved potentially protective levels of anti-influenza antibodies.
Experimental human challenge & efficacy studiesTo evaluate whether the observed immune responses in the serum and mucosal compartments were sufficient to protect against influenza infection, an experimental challenge study was performed.
Human in-patient immunization and virus challenges were undertaken in healthy adults to examine the efficacy of a triva-lent intranasal proteosome–influenza formulation against a live influenza virus homologous to the H3N2 strain included in the vaccine [61]. Subjects were selected for HAI titers <20 against the challenge strain and given either a single dose equivalent to 30 µg HA or two doses of either 15 or 30 µg HA on days 0 and 14. Subjects were challenged on days 40–42 with 105.5 egg infec-tious dose
50 wild-type A/Panama/2007/99. Approximately 70%
of the subjects that received either one or two doses of the active treatment responded with HAI titers ≥40 against the challenge strain compared with 4% that received placebo. Nasal wash sIgA was significantly increased 1.63-fold and 2.47-fold for one and two doses, respectively, compared with placebo. The two-dose regimens were 100% protective against febrile illness with lab-oratory-confirmation of influenza while the single dose showed 65% efficacy. There were no statistical differences in clinical end points between the low- and high-dose regimens. Importantly, we were able to demonstrate that serum and mucosal antibody responses significantly contributed to protection – both individu-ally and in an additive manner (Figure 2). For example, subjects with pre-challenge serum HAI titers of less than 20 HAI and the lowest levels of sIgA were poorly protected whereas individuals with the same range of HAI titers but with the highest levels of sIgA were protected. Conversely, subjects with the lowest levels of sIgA were not protected unless they had concomitant HAI responses of ≥20. Although the subjects in this study were chal-lenged experimentally with live virus and not by natural exposure, these results suggest that intranasal proteosome–influenza vac-cines can be efficacious despite inducing serum HAI titers below the threshold presumed to correlate with protection (≥40). This protection appears to be due to the ability of these vaccines to induce significant levels of mucosal sIgA in the respiratory tract.
A trivalent intranasal proteosome–influenza vaccine was further examined in a double-blind, placebo-controlled trial involving 1,349 healthy subjects 18–49 years of age over the 2003/2004 influenza season in the western hemisphere [62]. Subjects received placebo or 30 µg HA either as a single dose or in two iterations of 15 µg given 14 days apart. HAI and IgA responses were consist-ent with previous studies. Statistically significant rises in serum HAI and salivary sIgA were observed for each of the three strains. Importantly, the two-dose regimen showed no advantage over a single vaccination. Unfortunately, this study was impacted by a number of factors including an atypical early influenza epi-demic, a poor match between the vaccine antigen and circulat-ing virus strains and a low rate of confirmed influenza illness in the study population (~2% placebo rate). Nevertheless, the vaccines demonstrated 56–68% efficacy against influenza-like illness and laboratory-confirmed influenza infection as assessed by positive virus culture or reverse transcriptase-PCR [62]. These results compared favorably with an efficacy of 40–60% in a US study for TIV based on laboratory-confirmed influenza reports during the same season [64].
Expert commentary The LAIV vaccines FluMist [65] and Nasovac™ (Serum Institute of India Ltd., licensed in Pune, India [66]) are currently the only intranasal vaccines approved for use in humans; however, there is ongoing research to develop safe and effective non-live intra-nasal vaccines. Non-live vaccines present no risk of transmission of live virus following vaccination. Shedding of vaccine virus was observed particularly in young children for 1 day after receiving LAIV [63], posing the potential risk of reassortment with wild-type virus and infection of unvaccinated subjects, especially the immu-nosuppressed. Another advantage of non-live influenza vaccines is the potential to tolerate a wider range of storage conditions com-pared with LAIV. For example, the proteosome–influenza vaccines used in the aforementioned clinical studies were stable for at least 1 month at room temperature [White G, Unpublished Observations]. The live-attenuated vaccines require storage at 2–8°C [67].
In addition, while safe and highly effective at preventing influ-enza infection in children between 15 months and 6 years of age [68], LAIVs are less effective in older populations and are not approved for individuals 50 years of age or older [63]. This reduced efficacy in the elderly is possibly due to suppression of vaccine virus replication necessary to stimulate immunity. Although not studied specifically at this stage, safe adjuvanted intranasal influ-enza vaccines such as the proteosome-based variety would not be impacted in the same manner by pre-existing mucosal antibod-ies. Furthermore, their intrinsic immunostimulatory properties may help to overcome the reduced responsiveness of the elderly to influenza vaccines [69].
An important consideration for the future clinical develop-ment of intranasal influenza vaccines is the need to better define immuno logical correlates of protection. For example, while the proteosome–influenza vaccines induced consistent seroconversion in adults as measured by serum HAI, this was at a lower frequency (in up to 30–60% of subjects) than that normally seen in the same
Expert Rev. Vaccines 10(3), (2011)372
Review Burt, Mallett, Plante, Zimmermann, Torossian & Fries
Key issues
• The uptake of influenza vaccines in the general population is below the coverage levels recommended by health agencies.
• Improvements in the efficacy of influenza vaccines and in the way that they are administered may increase their acceptability and result in increased coverage in communities.
• Currently, licensed inactivated influenza vaccines are administered intramuscularly and protect by inducing mainly systemic immune responses.
• Intranasally delivered inactivated influenza vaccines induce both systemic and mucosal immune responses including secretory IgA in respiratory tissues where the influenza virus infects.
• Mucosal immune responses against influenza tend to be more cross-reactive and cross-protective against variant strains of the virus compared with influenza-specific systemic responses.
• The development of a safe and effective inactivated intranasal influenza vaccine offers the potential for a less invasive, more acceptable and broadly protective influenza vaccine.
age group immunized with TIV (70–90%) [70]. Nonetheless, pro-teosome–influenza vaccines demonstrated efficacy of up to 100% in a human experimental challenge study and protection in a field trial during a season where the circulating H3N2 strain was dif-ferent to the H3N2 strain in the vaccine. These results argue that historical immunological correlates of protection based on serum HAI alone, as used for intramuscular TIV vaccines, may not apply to intranasal vaccines. The immune responses induced by proteo-some vaccines in the clinical trials described in this article were comparable or higher than those achieved by the commercial LAIV FluMist in the same age groups [63]. Despite showing high efficacy rates in infants and healthy adults, there has been no consistent cor-relation between fourfold rise in serum HAI and protective efficacy for live-attenuated vaccines [63]. Correlates of protection defined by immune markers other than serum HAI such as nasal or salivary sIgA could provide an alternative biomarker. Experience from the cold-adapted influenza vaccine trials suggest that any detectable level of virus-specific local IgA can be correlated with suppression of both disease and virus shedding [71]. In the proteosome–influ-enza human challenge study, either sIgA (in the absence of protec-tive levels of HAI) or HAI alone or in combination with mucosal antibody correlated with protection against laboratory-confirmed influenza and illness. These results suggest that for intranasal inac-tivated influenza vaccines it may be possible to define immune correlates of protection based on various combinations of serum HA titers and sIgA levels. Such biomarkers may become useful surrogates for large and expensive human efficacy trials and in re-registration trials that are required in some countries.
Other immunological responses including virus-specific neu-tralizing antibody and cell-mediated immunity should also be fur-ther examined in this regard. Cell-mediated immunity responses may also contribute to protection by accelerating recovery from infection [72]. Increases in influenza-specific IFN-g-secreting CD4+ and CD8+ T cells were detected in children and infants following intranasal immunization with LAIV vaccine [73]. While not explored thoroughly in humans, proteosome-based vaccines induce strong IFN-g-secreting T-cell responses in animals [45,55].
Five-year view Overall, the preclinical and clinical results produced to date for proteosome-based influenza vaccines support their feasibility as efficacious, inactivated intranasal subunit vaccine alternatives
against influenza. There are a number of possible strategies to fully exploit the potential of the proteosome-based adjuvant tech-nology for a commercial nasal influenza vaccine. Despite their impressive clinical safety, immunogenicity and efficacy results, the proteosome vaccines used were produced using a process that requires a relatively lengthy formulation process to produce the OMP–HA vaccine, resulting in some loss of HA. In preclini-cal studies we demonstrated that similar or superior protective immune responses can be achieved with split-influenza antigen or rHA mixed prior to immunization with pre-formed proteosome–LPS (protollin) [45] that contains agonists for TLR-4 in addition to TLR-2. We have generated similar results with a protollin-like adjuvant comprised of OMP and LOS from N. meningitidis [Zimmermann J, Unpublished Data]. This alternative type of proteo-some-based vaccine could be produced without loss of HA and could be simpler to manufacture – an important factor consider-ing the tight timelines under which influenza vaccines need to be manufactured and released. Furthermore, the potential for an enhanced protective immune response would be advantageous for an intranasal pandemic influenza vaccine where antigen-sparing is important. It is noteworthy that protollin has been tested previ-ously by the intranasal route in humans as a vaccine for shigellosis and was well tolerated at levels of LPS of at least 0.4 mg [74].
AcknowledgementsThe authors would like to acknowledge all of their colleagues and collabora-tors for their contribution towards this body of work especially George Lowell, former Chief Scientific Officer of ID Biomedical, and David Jones, former senior scientist of ID Biomedical.
Financial & competing interests disclosureAll authors are currently employees of GlaxoSmithKline Biologicals of North America and inventors on patents related to the proteosome technology. D Burt, M Plante, J Zimmermann, K Torossian and L Fries are eligible for GSK stock options. The authors have no other relevant affiliations or finan-cial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock own-ership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
www.expert-reviews.com 373
ReviewProteosome-adjuvanted intranasal influenza vaccines
ReferencesPapers of special note have been highlighted as:• of interest•• of considerable interest
1 Fiore AE, Shay DK, Broder K et al.; Centers for Disease Control and Prevention. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR 58, 1–52 (2009).
2 Centers for Disease Control and Prevention (CDC). Influenza vaccination coverage among children and adults – United States, 2008–09 influenza season. MMWR 58, 1091–1095 (2009).
3 Gasparini R, Laghi-Pasini F, Staniscia T et al. A. MF59-adjuvanted H5N1 vaccine induces immunologic memory and heterotypic antibody responses in non-elderly and elderly adults. PLoS One 4(2), e4384 (2009).
4 Walker WT, Oeser C, Reiner A et al. Safety and immunogenicity of AS03B adjuvanted split virion versus non-adjuvanted whole virion H1N1 influenza vaccine in UK children aged 6 months-12 years: open label, randomised, parallel group, multicentre study. Br. Med. J. 340, c2649 (2010).
5 Baras B, Bouveret N, Devaster JM et al. A vaccine manufacturer’s approach to address medical needs related to seasonal and pandemic influenza viruses. Influenza Other Respi. Viruses 2(6), 251–260 (2008).
6 Nir Y, Paz A, Sabo E, Potasman I. Fear of injections in young adults: prevalence and associations. Am. J. Trop. Med. Hyg. 68(3), 341–344 (2003).
7 Breau L, McGrath PJ, Craig K, Santor D, Cassidy KL, Reid G. Facial expression of children receiving immunizations: a principal components analysis of the child facial coding system. Clin. J. Pain 17(2), 178–186 (2001).
8 Sendi P, Locher R, Bucheli B et al. Intranasal influenza vaccine in a working population. Clin. Infect. Dis. 38(7), 974–980 (2004).
9 Glenn GM, Thomas DN, Poffenberger KL et al. Safety and immunogenicity of an influenza vaccine A/H5N1 (A/Vietnam/1194/2004) when coadministered with a heat-labile enterotoxin (LT) adjuvant patch. Vaccine 27(Suppl. 6), 60–66 (2009).
10 Tamura S. Studies on the usefulness of intranasal inactivated influenza vaccines. Vaccine 28(38), 6393–6397 (2010).
11 Song JH, Nguyen HH, Cuburu N et al. Sublingual vaccination with influenza virus protects mice against lethal viral infection. Proc. Natl Acad. Sci. USA 105(5), 1644–1649 (2008).
12 Prabakaran M, Madhan S, Prabhu N, Geng GY, New R, Kwang J. Reverse micelle-encapsulated recombinant baculovirus as an oral vaccine against H5N1 infection in mice. Antiviral Res. 86(2), 180–187 (2010).
13 Ambrose CS, Luke C, Coelingh K. Current status of live attenuated influenza vaccine in the United States for seasonal and pandemic influenza. Influenza Other Respi. Viruses 2(6), 193–202 (2008).
14 Waldman RH, Bond JO, Levitt LP et al. An evaluation of influenza immunization. influence of route of administration and vaccine strain. Bull. World Health Organ. 41(3), 543–548 (1969).
15 Liem KS, Jacobs J, Marcus EA, van Strik R. The protective effect of intranasal immunization with inactivated influenza virus vaccine. Postgrad. Med. J. 49(569), 175–179 (1973).
16 Lycke N, Holmgren J. Strong adjuvant properties of cholera toxin on gut mucosal immune responses to orally presented antigens. Immunology 59(2), 301–308 (1986).
17 Sixma TK, Kalk KH, van Zanten BA et al. Refined structure of Escherichia coli heat-labile enterotoxin, a close relative of cholera toxin. J. Mol. Biol. 230(3), 890–918 (1993).
18 Glück U, Gebbers JO, Glück R. Phase 1 evaluation of intranasal virosomal influenza vaccine with and without Escherichia coli heat-labile toxin in adult volunteers. J. Virol. 73(9), 7780–7786 (1999).
19 Mutsch M, Zhou W, Rhodes P et al. Use of the inactivated intranasal influenza vaccine and the risk of Bell’s palsy in Switzerland. N. Engl. J. Med. 350(9), 896–903 (2004).
• AssociationofBell’spalsywithtoxinadjuvants.
20 van Ginkel FW, Jackson RJ, Yuki Y, McGhee JR. Cutting edge: the mucosal adjuvant cholera toxin redirects vaccine proteins into olfactory tissues. J. Immunol. 165(9), 4778–4782 (2000).
21 Baldridge JR, Yorgensen Y, Ward JR, Ulrich JT. Monophosphoryl lipid A enhances mucosal and systemic immunity to vaccine antigens following intranasal administration. Vaccine 18(22), 2416–2425 (2000).
22 Xiaowen Z, Qinghua Y, Xiaofei Z, Qian Y. Co-administration of inactivated avian influenza virus with CpG or rIL-2 strongly enhances the local immune response after intranasal immunization in chicken. Vaccine 27(41), 5628–5632 (2009).
23 Hu KF, Lövgren-Bengtsson K, Morein B. Immunostimulating complexes (ISCOMs) for nasal vaccination. Adv. Drug Deliv. Rev. 51(1–3), 149–159 (2001).
24 Boyce TG, Hsu HH, Sannella EC et al. Safety and immunogenicity of adjuvanted and unadjuvanted subunit influenza vaccines administered intranasally to healthy adults. Vaccine 19(2–3), 217–226 (2000).
25 Ichinohe T, Watanabe I, Ito S et al. Synthetic double-stranded RNA poly(I:C) combined with mucosal vaccine protects against influenza virus infection. J. Virol. 79(5), 2910–2919 (2005).
26 Jabbal-Gill I, Fisher A, Illum L et al. Effective nasal influenza vaccine delivery using chitosan. Vaccine 23(35), 4367–4374 (2005).
27 Kiyono H, Fukuyama S. NALT-versus Peyer’s-patch-mediated mucosal immunity. Nat. Rev. Immunol. 4(9), 699–710 (2004).
28 Renegar KB, Small PA Jr, Boykins LG, Wright PF. Role of IgA versus IgG in the control of influenza viral infection in the murine respiratory tract. J. Immunol. 173(3), 1978–1986 (2004).
29 Mazanec MB, Lamm ME, Lyn D, Portner A, Nedrud JG. Comparison of IgA versus IgG monoclonal antibodies for passive immunization of the murine respiratory tract. Virus Res. 23(1–2), 1–12 (1992).
•• ShowsthesuperiorabilityofsecretoryIgAtoneutralizeinfluenzavirusin vivo.
30 Renegar KB, Jackson GD, Mestecky J. In vitro comparison of the biologic activities of monoclonal monomeric IgA, polymeric IgA, and secretory IgA. J. Immunol. 160(3), 1219–1223 (1998).
31 Liew FY, Russell SM, Appleyard G, Brand CM, Beale J. Cross-protection in mice infected with influenza A virus by the respiratory route is correlated with local IgA antibody rather than serum antibody or cytotoxic T cell reactivity. Eur. J. Immunol. 14(4), 350–356 (1984).
32 Tamura SI, Asanuma H, Ito Y et al. Superior cross-protective effect of nasal vaccination to subcutaneous inoculation with influenza hemagglutinin vaccine. Eur. J. Immunol. 22(2), 477–481 (1992).
Expert Rev. Vaccines 10(3), (2011)374
Review Burt, Mallett, Plante, Zimmermann, Torossian & Fries
33 Ichinohe T, Kawaguchi A, Tamura SI et al. Intranasal immunization with H5N1 vaccine plus poly I:poly C12U, a Toll-like receptor agonist, protects mice against homologous and heterologous virus challenge. Microbes Infect. 9(11), 1333–1340 (2007).
34 Tumpey TM, Renshaw M, Clements JD, Katz JM. Mucosal delivery of inactivated influenza vaccine induces B-cell-dependent heterosubtypic cross-protection against lethal influenza A H5N1 virus infection. J. Virol. 75(11), 5141–5150 (2001).
35 Mendelman PM, Rappaport R, Cho I et al. Live attenuated influenza vaccine induces cross-reactive antibody responses in children against an a/Fujian/411/2002-like H3N2 antigenic variant strain. Pediatr. Infect. Dis. J. 23(11), 1053–1055 (2004).
36 Belshe RB, Gruber WC, Mendelman PM et al. Efficacy of vaccination with live attenuated, cold-adapted, trivalent, intranasal influenza virus vaccine against a variant (A/Sydney) not contained in the vaccine. J. Pediatr. 136(2), 168–175 (2000).
37 Asahi Y, Yoshikawa T, Watanabe I et al. Protection against influenza virus infection in polymeric Ig receptor knockout mice immunized intranasally with adjuvant-combined vaccines. J. Immunol. 168(6), 2930–2938 (2002).
38 Taylor HP, Dimmock NJ. Mechanism of neutralization of influenza virus by secretory IgA is different from that of monomeric IgA or IgG. J. Exp. Med. 161(1), 198–209 (1985).
• EvidenceforabilityofsecretoryIgAtoneutralizeinfluenzavirusintracellularly.
39 Lowell GH, Smith LF, Seid RC, Zollinger WD. Peptides bound to proteosomes via hydrophobic feet become highly immunogenic without adjuvants. J. Exp. Med. 167(2), 658–663 (1988).
40 Wetzler LM. Immunopotentiating ability of neisserial major outer membrane proteins. Use as an adjuvant for poorly immunogenic substances and potential use in vaccines. Ann. NY Acad. Sci. 15(730), 367–370 (1994).
• EvidencethatPorBoutermembraneproteinisanagonistforTLR-2.
41 VanCott TC, Kaminski RW, Mascola JR et al. HIV-1 neutralizing antibodies in the genital and respiratory tracts of mice intranasally immunized with oligomeric gp160. J. Immunol. 160(4), 2000–2012 (1998).
42 Cyr SL, Jones T, Stoica-Popescu I et al. Intranasal proteosome™-based respiratory syncytial virus (RSV) vaccines protect BALB/c mice against challenge without eosinophilia or enhanced pathology. Vaccine 25(29), 5378–5389 (2007).
43 Batzloff MR, Yan H, Davies MR et al. Toward the development of an antidisease, transmission-blocking intranasal vaccine for group a streptococcus. J. Infect. Dis. 192(8), 1450–1455 (2005).
44 Mallett CP, Hale TL, Kaminski RW et al. Intransal or intragastric immunization with proteosome-Shigella lipopolysaccharide vaccines protects against lethal pneumonia in a murine model of Shigella infection. Infect. Immun. 63(6), 2382–2386 (1995).
45 Jones T, Cyr S, Allard F, Bellerose N, Lowell GH, Burt DS. Protollin™: a novel adjuvant for intranasal vaccines. Vaccine 22(27–28), 3691–3697 (2004).
46 Langley JM, Halperin SA, McNeil S et al. Safety and immunogenicity of a Proteosome™-trivalent inactivated influenza vaccine, given nasally to healthy adults. Vaccine 24(10), 1601–1608 (2006).
47 Pasetti MF, Resendiz-Albor A, Ramirez K et al. Heterologous prime-boost strategy to immunize very young infants against measles: pre-clinical studies in rhesus macaques. Clin. Pharmacol. Ther. 82(6), 672–685 (2007).
48 Hu MC, Jones T, Kenney RT, Barnard DL, Burt DS, Lowell GH. Intranasal Protollin-formulated recombinant SARS S-protein elicits respiratory and serum neutralizing antibodies and protection in mice. Vaccine 25(34), 6334–6340 (2007).
49 Lynch EC, Blake MS, Gotschlich EC, Mauro A. Studies of porins: spontaneously transferred from whole cells and reconstituted from purified proteins of Neisseria gonorrhoeae and Neisseria meningitidis. Biophys. J. 45(1), 104–107 (1984).
50 Massari P, Henneke P, Ho Y, Latz E, Golenbock DT, Wetzler LM. Cutting edge: immune stimulation by neisserial porins is Toll-like receptor 2 and MyD88 dependent. J. Immunol. 168(4), 1533–1537 (2002).
51 Chow JC, Young DW, Golenbock DT, Christ WJ, Gusovsky F. Toll-like receptor-4 mediates lipopolysaccharide-induced signal transduction. J. Biol. Chem. 274(16), 10689–10692 (1999).
52 Faure E, Thomas L, Xu H, Medvedev A, Equils O, Arditi M. Bacterial lipopolysaccharide and IFN-gamma induce Toll-like receptor 2 and Toll-like receptor 4 expression in human endothelial cells: role of NF-kappa B activation. J. Immunol. 166(3), 2018–2024 (2001).
53 Chabot SM, Chernin TS, Shawi M et al. TLR-2 activation by proteosomes promotes uptake of particulate vaccines at mucosal surfaces. Vaccine 25(29), 5348–5358 (2007).
54 Levi R, Aboud-Pirak E, Leclerc C, Lowell GH, Arnon R. Intranasal immunization of mice against influenza with synthetic peptides anchored to proteosomes. Vaccine 13(14), 1353–1359 (1995).
55 Plante M, Jones T, Allard F et al. Nasal immunization with subunit proteosome influenza vaccines induces serum HAI, mucosal IgA and protection against influenza challenge. Vaccine 20(1–2), 218–225 (2001).
56 Jones T, Allard F, Cyr SL et al. A nasal Proteosome™ influenza vaccine containing baculovirus-derived hemagglutinin induces protective mucosal and systemic immunity. Vaccine 21(25–26), 3706–3712 (2003).
57 Lowell GL, Burt D, White G, Fries L. Proteosome technology for vaccines and adjuvants. In: New Generation Vaccines. Levine M (Ed.). Marcel Decker Inc., NY, USA, 271–282 (2004).
58 Reuman PD, Keely S, Schiff GM. Assessment of signs of influenza illness in the ferret model. J. Virol. Methods 24(1–2), 27–34 (1989).
59 Frenkel D, Puckett L, Petrovic S et al. A nasal proteosome adjuvant activates microglia and prevents amyloid deposition. Ann. Neurol. 63(5), 591–601 (2008).
60 Treanor J, Nolan C, O’Brien D et al. Intranasal administration of a proteosome–influenza vaccine is well-tolerated and induces serum and nasal secretion influenza antibodies in healthy human subjects. Vaccine 24(3), 254–262 (2006).
61 Fries L, Lambkin R, Gelder C et al. FluInsure™, an inactivated trivalent influenza vaccine for intranasal administration, is protective in human challenge with A/Panama/2007/99 (H3N2) virus. Presented at: International Conference on Options for the Control of Influenza V. Okinawa, Japan, 7–11 October 2003.
www.expert-reviews.com 375
ReviewProteosome-adjuvanted intranasal influenza vaccines
•• Firstdemonstrationofprotectiveefficacyofproteosome–influenzavaccineinhumans.
62 Langley JM, Akoi F, Ward BJ et al. A nasally administered trivalent inactivated influenza vaccine is well tolerated, stimulates both mucosal and systemic immunity, and potentially protects against influenza illness. Vaccine 29(10), 1921–1928 (2011).
63 Ambrose CS, Luke C, Coelingh K. Current status of live attenuated influenza vaccine in the United States for seasonal and pandemic influenza. Influenza Other Respi. Viruses. 2(6), 193–202 (2008).
64 Herrera GA, Iwane MK, Cortese M et al. Influenza vaccine effectiveness among 50–64-year-old persons during a season of poor antigenic match between vaccine and circulating influenza virus strains: Colorado, United States, 2003–2004. Vaccine 25(1), 154–160 (2007).
65 Belshe RB, Mendelman PM, Treanor J et al. The efficacy of live attenuated, cold-adapted, trivalent, intranasal influenza virus vaccine in children. N. Engl. J. Med. 338(20), 1405–1412 (1998).
66 Jabbal-Gill I. Nasal vaccine innovation. J. Drug Targeting 18(10), 771–786 (2010).
67 FluMist™, Influenza Vaccine Live, Intranasal. Prescribing Information. MedImmune, Gaithersburg, MD, USA (2007).
68 Rhorer J, Ambrose CS, Dickinson S et al. Efficacy of live attenuated influenza vaccine in children: a meta-analysis of nine randomized clinical trials. Vaccine 27(7), 1101–1110 (2009).
69 Govaert TM, Thijs CT, Masurel N et al. The efficacy of influenza vaccination in elderly individuals. A randomized double-blind placebo-controlled trial. JAMA 272, 1661–1665 (1997).
70 Ruben FL. Prevention and control of influenza. Role of vaccine. Am. J. Med. 82(6A), 31–34 (1987).
71 Johnson PR, Feldman S, Thompson JM, Mahoney JD, Wright PF. Immunity to influenza A virus infection in young children: a comparison of natural infection, live cold-adapted vaccine, and inactivated vaccine. J. Infect. Dis. 154(1), 121–127 (1986).
72 McMichael AJ, Gotch FM, Noble GR, Beare PA. Cytotoxic T-cell immunity to influenza. N. Engl. J. Med. 309(1), 13–17 (1983).
73 Forrest BD, Pride MW, Dunning AJ et al. Correlation of cellular immune responses with protection against culture-confirmed influenza virus in young children. Clin. Vaccine Immunol. 15(7), 1042–1053 (2008).
74 Fries LF, Montemarano AD, Mallett CP, Taylor DN, Hale TL, Lowell GH. Safety and immunogenicity of a proteosome-Shigella flexneri 2a lipopolysaccharide vaccine administered intranasally to healthy adults. Infect. Immun. 69(7), 4545–4553 (2001).
Website
101 Safety evaluation of toxin adjuvants delivered intranasally www.niaid.nih.gov/topics/entericDiseases/Documents/intranasal.pdf