Repeat Valvular Operations: Bench Optimization of Conventional Surgery
-
Upload
sacklerinstitute -
Category
Documents
-
view
1 -
download
0
Transcript of Repeat Valvular Operations: Bench Optimization of Conventional Surgery
DOI: 10.1016/j.athoracsur.2005.11.030 2006;81:1279-1283 Ann Thorac Surg
Gianfederico Possati Fabiana Girola, Mariantonietta Piscitelli, Mario Perisano, Lorenzo Martinelli and
Nicola Luciani, Giuseppe Nasso, Amedeo Anselmi, Franco Glieca, Mario Gaudino, Repeat Valvular Operations: Bench Optimization of Conventional Surgery
http://ats.ctsnetjournals.org/cgi/content/full/81/4/1279located on the World Wide Web at:
The online version of this article, along with updated information and services, is
Print ISSN: 0003-4975; eISSN: 1552-6259. Southern Thoracic Surgical Association. Copyright © 2006 by The Society of Thoracic Surgeons.
is the official journal of The Society of Thoracic Surgeons and theThe Annals of Thoracic Surgery
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from
RCNMMDC
crpm
a2U
iiauiI
IfgptftrwbrqAfppsm
A
ACI
©P
DIO
VA
SCU
LAR
epeat Valvular Operations: Bench Optimization ofonventional Surgery
icola Luciani, MD, Giuseppe Nasso, MD, Amedeo Anselmi, MD, Franco Glieca, MD,ario Gaudino, MD, Fabiana Girola, MD, Mariantonietta Piscitelli, MD,ario Perisano, MD, Lorenzo Martinelli, MD, and Gianfederico Possati, MD
epartment of Cardiovascular Medicine, Division of Cardiac Surgery, Catholic University of the Sacred Heart, and Department of
ardiovascular Sciences, Unit of Cardiac Surgery, Campus Bio-Medico University of Rome, Rome, Italymc
pamiecagcp
CA
R
Background. Repeat heart valve operations have be-ome a quite common procedure. We reviewed our expe-ience with reoperative valvular surgery during a 6-yeareriod to assess the risk factors affecting in-hospitalortality and medium-term survival.Methods. A series of 316 redo procedures performed ontotal of 290 patients in the period between 1997 and
002 at our institution was retrospectively analyzed.nivariate and multivariable analyses were performed.Results. In-hospital mortality was 3.8%; overall mortal-
ty at the end of a 30-month follow-up was 9.3%. Wedentified advanced New York Heart Association class,dvanced age, depressed ejection fraction, emergent orrgent presentation, impairment of renal function, and
nvolvement of tricuspid valve as predictors of mortality.
n contrast, duration of cardiopulmonary bypass andM
Hwfaimcs
tsbiotatIad2
CIp(
atholic University of the Sacred Heart, Largo A. Gemelli, 8, 00168 Rome,taly; e-mail: [email protected].
2006 by The Society of Thoracic Surgeonsublished by Elsevier Inc
ats.ctsnetjournDownloaded from
ultiple valve procedure were not associated with in-reased short-term risk.
Conclusions. The present study is characterized byarticular attention in reducing confounding variablesnd biases correlated to heterogeneities. The main deter-inants of mortality are related to the degree of patients’
llness rather than to inherent technical factors of reop-rations. Although highest-risk individuals (previousoronary artery bypass grafting or coexistence of aorticneurysm) were excluded from the study, our data sug-est that patients undergoing isolated redo valvular pro-edures now face operative risks that are comparable torimary intervention.
(Ann Thorac Surg 2006;81:1279–83)
© 2006 by The Society of Thoracic Surgeonsmprovements of surgical techniques and prolongedlife expectancy in the population have increased the
requency of heart valve reoperations (HVRs) [1]. Despitelobal amelioration of results of heart valve surgery, redorocedures still carry specific risk factors for inherent
echnical problems [2]. Traditionally operative mortalityor HVRs has been reported to be higher in comparisono primary procedures [1, 3, 4]. Furthermore, the patientseferred to undergo HVR are noticeably heterogeneousith respect to indications, surgical history, and comor-idity. We performed a retrospective review of hospitalecords for 290 patients who underwent first or subse-uent HVR in our institution between January 1997 andugust 2002. We sought to ascertain among candidates
or isolated valvular reoperation (1) whether surgical risk,ostoperative morbidity, and mid-term results are com-arable to those of primary surgery, and (2) whichpecific technical factors can influence operativeortality.
ccepted for publication Nov 8, 2005.
ddress correspondence to Dr Luciani, Dept of Cardiovascular Medicine,
aterial and Methods
ospital records of 316 consecutive HVR proceduresere retrospectively analyzed. Patients were selected
rom the pool of 780 overall redo procedures performedt our institution in the 1997 through 2002 period, accord-ng to the following inclusion criteria: (1) use of full
edian sternotomy plus normothermic or hypothermicardiopulmonary bypass; and (2) use of the same surgicaltrategy at first intervention.
All interventions were performed by the same surgicaleam. Patient characteristics and indications for redourgery are highly variable in previously reported data-ases [5]. In our study, exclusion criteria were the coex-
stence of coronary artery disease with or without historyf coronary surgery, aortic aneurysm, and any concomi-ant procedure other than valvular, including ventricularneurysmectomy and excision of cardiac neoplasms, ei-her at the previous procedure or at reintervention. Thenstitutional Review Board of the Catholic Universitypproved the retrospective and anonymous treatment ofata without need for individual consent on March 22,005.
linical Evaluation and Surgical Methodsntraoperative transesophageal echocardiography waserformed. For patients at high risk of reentry injuries
patients with close adhesions between the sternum and
0003-4975/06/$32.00doi:10.1016/j.athoracsur.2005.11.030
by on June 2, 2013 als.org
tlmnfpcccpbucaotarr[c
ali(aal
aelcfpiy
DIwdlPlaaaMtsdfiatca
SDbCstctic(puoac0fCl
R
T3IwpTvspuf
hato
TC
V
AMLBNC
L
CdNY
1280 LUCIANI ET AL Ann Thorac SurgREPEAT VALVULAR OPERATIONS 2006;81:1279–83
CA
RD
IOV
ASC
ULA
R
he ascending aorta, and patients with tricuspid valveesion), femorofemoral cannulation and deep hypother-
ia with circulatory arrest were instituted before ster-otomy [6]. When possible, valve procedure was per-
ormed without complete mobilization of the heart torevent injuries to the myocardium, great vessels, andoronary arteries during intrapericardial dissection. As-ending aorta cannulation and right atrial or bicavalannulation were adopted for extracorporeal circulation,lus normothermic antegrade and retrograde multidoselood cardioplegia. Mild systemic hypothermia wassed. Ventricular venting was achieved through the as-ending aorta /or the right superior pulmonary vein. Theortic valve was accessed through low transverse aortot-my and the pulmonary valve by analogous incision onhe pulmonary trunk. The atrioventricular valves wereccessed through right atriotomy (tricuspid) and throughight atriotomy plus septal incision (mitral). Operativeisk was standardized through the EuroSCORE system7]. Low-dose aprotinin (2,000,000 U before initiation ofardiopulmonary bypass) was used until January 1998.
Postoperative complications and valvular morbiditiesnd mortality were defined in compliance with the pub-ished guidelines [8]. Cardiac events were analyzed asncluded in one of the following groups: cardiac deathincluding valve-related cardiac death), sudden death,nd valve-related complications (including structuralnd nonstructural dysfunction, valve thrombosis, embo-ism, bleeding, operated valve endocarditis).
Follow-up was carried out by periodic examinationsfter discharge, each including physical examination,lectrocardiogram, and cardiac ultrasonography. The fol-ow-up period lasted 26 � 2 months and was 100%omplete among patients alive at each time interval. Theollow-up was started immediately after discharge of theatients operated on in January 1997 and was completed
n January 2005 for the last patients operated on in theear 2002.
efinitionsn-hospital or operative mortality was defined as deathithin 30 days from surgery. Renal insufficiency wasefined as postoperative increase of the serum creatinine
evel of at least 2 mg/dL greater than preoperative.erioperative stroke was defined as a new focal neuro-
ogic deficit or coma, lasting more than 24 hours, associ-ted with recent ischemic cerebral lesion demonstratedt computed tomography, which was evident at patient’swakening or occurred later in postoperative course.ediastinitis was defined as deep sternal wound infec-
ion with involvement of the substernal planes andystemic signs of sepsis, and associated with sternalehiscence or instability. Myocardial infarction was de-ned as occurrence of regional hypokinesia or dyskinesiat echocardiography, creatine kinase MB fraction greaterhan 4% of the total blood level of creatine kinaseoncentration, and ST-segment elevation followed by
ppearance of new Q waves on the electrocardiogram. (ats.ctsnetjournDownloaded from
tatistical Methodsata were stored and processed in an electronic data-ase, using SPSS 10.1 for Windows software (SPSS,hicago, IL). Continuous data are presented as mean �
tandard deviation. For group comparisons, unpaired �2
est and Student’s t test were adopted for discrete andontinuous variables, respectively. All tests were two-ailed. Univariate analysis was performed for the follow-ng variables: diabetes, advanced New York Heart Asso-iation class, depressed left ventricular ejection fraction�0.40), impaired renal function preoperatively, cardio-ulmonary bypass (CPB) time greater than 120 minutes,rgent or emergent presentation, history of more thanne surgical procedure, and combined valve proceduret any of the redo interventions, with death as theategorical response variable (cutoff probability value,.02). Given the high number of censored observations,actors associated with mortality were then included in aox proportional hazards regression analysis. The alpha
evel was 0.05.
esults
wo hundred ninety patients who underwent a total of16 HVR procedures were included in the present study.n the same period 1,508 isolated valvular proceduresere performed in our unit. Baseline features of theopulation and comorbidity profile are presented inable 1. Eleven patients (3.8%) had undergone a failedalve repair at first cardiac procedure. One hundredixty-four patients (56%) underwent one HVR only, 76atients (26%) underwent two HVRs, 48 patients (14%)nderwent three HVRs, and 10 patients (3%) underwent
our HVRs.At first reoperation a total of 13 Brompton pulmonary
omografts were explanted from the aortic position and 5ortic homografts were explanted from the aortic posi-ion. Among mechanical prostheses explanted in theverall 316 reinterventions, 24% were Sorin Bicarbon
able 1. Baseline Demographics and Preoperativeomorbidities
ariable Result
ge (years) 60.3 � 2.1ale sex 151 (52.1%)
VEF 0.48 � 0.04lood creatinine (mg/dL) 1.3 � 0.5YHA III or IV 143 (49.3%)omorbiditiesIDDM 1NIDDM 48COPD 15
ogistic EuroSCORE (%) 16 � 6
OPD � chronic obstructive pulmonary disease; IDDM � insulin-ependent diabetes mellitus; LVEF � left ventricular ejection fraction;IDDM � non–insulin-dependent diabetes mellitus; NYHA � Nework Heart Association.
Sorin Biomedica, Saluggia, Italy), 21% were St. Jude
by on June 2, 2013 als.org
M1TBs4w(pabEwnIpBHwCpp
wdtmctdidhw3wtirph3vmr
io
awO2w7thepvetpcvmqssM
ppipr
C
Rwsblrmmu
TDS
IIII
N
TM
DNLARE
T
a
�a
1281Ann Thorac Surg LUCIANI ET AL2006;81:1279–83 REPEAT VALVULAR OPERATIONS
CA
RD
IOV
ASC
ULA
R
edical prostheses (St. Jude Medical Inc, St Paul, MN),9% were Sulzer Carbomedics (Carbomedics Inc, Austin,X), 16% were Bjork-Shiley (Bjork-Shiley spherical valve,jork-Shiley convexocave valve, or Bjork-Shiley Mono-trut 70° convexoconcave valve; Shiley Inc, Irvine, CA),% were Starr-Edwards (Baxter Healthcare Corp, Ed-ards Division, Irvine, CA), 10% were Sorin Monoleaflet
Sorin Biomedica), 5% were Lillehei-Kaster tiliting-diskrostheses (LKP, Medical Inc, Inner Grove Heights, MN),nd 1% were Omniscience valves (Medical Inc). Amongiologic prostheses explanted, 55% were Carpentier-dwards porcine valves (Baxter Healthcare Corp), 25%ere Mitroflow pericardial prostheses (Mitroflow Inter-ational Inc, Richmond, BC, Canada), 8% were Hancock
I (Medtronic Inc, Minneapolis, MN), 10% were Labcororcine prostheses (Labcor Laboratories, Belo Horizonte,razil), and 2% were Prima Edwards Stentless (Baxterealthcare Corp). Among implanted prostheses, 36%ere Sorin Bicarbon mechanical valves, 29% were Sulzerarbomedics mechanical valves, 21% were Hancock IIorcine bioprosthesis, and 14% were Medtronic Intactorcine bioprosthesis (Medtronic Inc) (Table 4).The duration of first-implanted prosthesis was higherhen malfunction was caused by primary failure (meanuration, 103 � 24 months), and shorter when malfunc-
ion was caused by endocarditis (mean duration, 37 � 25onths). Cardiopulmonary bypass time and aortic cross-
lamp time ranged from 81 to 263 minutes (mean dura-ion, 139 � 24 minutes) and from 42 to 187 minutes (meanuration, 92 � 16 minutes), respectively. Unexpected
njuries to the heart or great vessels occurred in 2 patientsuring repeat median sternotomy; however, catastrophicemorrhage did not occur in any patient, and no deathas related to reentry injury. In-hospital mortality was
.8% (11 of 290 patients). Causes of in-hospital deathere multiorgan failure in four cases, myocardial infarc-
ion in three, stroke in two, and intractable respiratorynsufficiency in two. After the intervention, 4 patientsequired revision for control of bleeding. The meanostoperative chest tube output was 521 � 174 mL. Meanospital stay was 8 � 5 days. Intensive care unit stay was� 3 days (Table 5). The interval between the initial
alve operation and the first HVR ranged from 1.5onths to 21 years (mean interval, 8.3 years). Mortality
ose progressively with increasing number of HVRs.New York Heart Association functional classification
mproved with time in all survivors (Table 2). At the end
able 2. New York Heart Association Functional Classistribution Among Surviving Patients Before and Afterurgery
NYHA Class Preoperative At Discharge End of Follow-up
V 34 (12%) 0 0II 86 (30%) 6 (2%) 2 (1%)I 125 (43%) 50 (18%) 46 (17%)
45 (15%) 223 (80%) 221 (82%)
YHA � New York Heart Association.
f the follow-up, freedom from valve repeat reoperationLA
ats.ctsnetjournDownloaded from
t 4 years was 83%. Four patients (15% of all deaths) diedithin 2 months after discharge of left ventricular failure.verall mortality at the end of the follow-up period was
7 of 290 patients (9%). Causes of death after dischargeere cardiac related in 9 cases and noncardiac related in
. Replacement of a mechanical valve rather than of aissue valve was associated with higher risk at follow-up;owever, this advantage was offset by a higher risk ofarlier valve failure associated with bioprostheses. Coxroportional hazards regression analysis identified ad-anced New York Heart Association class, depressedjection fraction, advanced age, nonelective presentation,ricuspid valve involvement, and renal insufficiency asredictors of mortality (Table 3). Meanwhile protractedardiopulmonary bypass time, diabetes, and multiplealve procedure were not associated with higher risk ofortality. Causes of second reoperation were more fre-
uently prosthetic valve dysfunction owing to thrombo-is; the survival after second reoperation is comparable tourvival after first and third reintervention (see Kaplan-
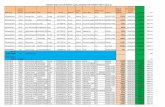
eier analysis).Figure 1 shows the influence of the number of redo
rocedures on survival. Although the small number ofatients with history of three or four reinterventions may
mpair the reliability of our analysis, we found thoseatients undergoing four reinterventions to be at highestisk of death.
omment
edo interventions have been traditionally associatedith high surgical risk and major challenges for the
urgeon compared with a primary procedure. This coulde partially ascribed to the frequently severe conditions
eading to redo procedure. The majority of deaths inecent series are because of cardiac causes, especiallyyocardial failure, which reflects the severely compro-ised hemodynamic conditions of the patients presently
ndergoing HVRs. Specific technical features must be
able 3. Cox Proportional Hazards Regression Model forortality Risk Factors in the Whole Study Populationa
Explanatory Variable Odds Ratios95% Confidence
Interval p Value
iabetes 1.41 0.08–2.33 0.47YHA III or IV 8.39 3.44–10.27 0.016VEF � 0.40 3.21 1.48–7.02 0.0079ge � 75 y 5.15 3.26–7.84 0.027enal insufficiency 3.18 1.9–3.66 0.023mergent or urgentpresentation
7.59 4.94–13.71 0.004
ricuspid valveinvolvement
9.16 2.91–8.97 0.03
No hazards regression was performed for cardiopulmonary bypass time120 minutes or combined valve procedure as they were not significant
t univariate analysis.
VEF � left ventricular ejection fraction; NYHA � New York Heartssociation.
by on June 2, 2013 als.org
tiwt
rcdastfc
smiccwTcc
ridwppstpcrmtnt[bslama[drssp
tpctpc
FntNt
TP
MATP
a
TP
C
SSMRRIR
1282 LUCIANI ET AL Ann Thorac SurgREPEAT VALVULAR OPERATIONS 2006;81:1279–83
CA
RD
IOV
ASC
ULA
R
aken into account in the surgical management of HVRs,ncluding extent of retrosternal and cardiac dissectionith the risk of reentry injuries, careful myocardial pro-
ection, and difficulties in the removal of air phase [9, 10].Marked heterogeneity of patients in need of HVR
enders the investigations in this field a methodologicalhallenge. To this concern, all individuals included in ouratabase (1) were affected by valvular disease and oper-ted on for isolated disease, (2) received full medianternotomy, (3) were operated on by a unique surgicaleam, and (4) were studied in a relatively short timerame (1997 through 2002). The exclusion of patients withoronary disease is a potential limitation to our conclu-
ig 1. Kaplan-Meier survival curves obtained on the basis of theumber of reinterventions. p � 0.05 at comparison of the curve for
he fourth redo with each of the other three curves (log-rank test).umber of patients at risk stratified according to number of reopera-
ions is reported.
able 4. Details of Location of Explanted and Implantedrostheses
Location
ValvesRemoved
atPrimarySurgery
Valves/ProsthesesRemoveda
MechanicalProsthesesImplanteda
BioprosthesesImplanteda
itral 150 183 119 64ortic 143 141 101 40ricuspid — 12 — 12ulmonary — 2 1 1
bAt first or subsequent reoperation.
ats.ctsnetjournDownloaded from
ion, given the recognized influence of ischemic cardio-yopathy on outcomes. Mortality reported by other
nvestigators ranges between 4% and 5% [5, 11], which isonsistent with the 3.8% in-hospital mortality in ourohort. We found a 2.4% in-hospital mortality associatedith first HVR and an overall mid-term mortality of 9.3%.hese results are similar to data published by Lytle andolleagues [12], Cohn and associates [13], Akins andoworkers [14], and Pansini and associates [15].
Recently a definite trend has been observed towardeduction of operative risk. Improvements in postoperativentensive care probably contributed to this tendency. Suchecrease in risk has been observed by several investigatorsho had included in their analysis even valvular redoatients affected by ischemic heart disease [11] and re-orted results globally comparable to ours. This agreementuggests that the amelioration of prognosis is real ratherhan attributable to selection of low-risk individuals in theresent work. Concerning mitral valve surgery, Potter andoworkers [16] and Matsuyama and colleagues [17] haveeported operative mortality rates comparable to the pri-ary procedure (4.7% versus 4.1%). Although reinterven-
ions for bioprosthetic failure are in most cases performedonelectively, operative mortality decreased from 10.8% in
he period 1987 through 1992 to 3.4% in 1993 through 200018]. Optimal management of prosthetic valve obstructionecause of thrombosis still remains controversial, althoughurgery is usually preferred. Our operative mortality wasower than the rates reported in similar settings by Rodautnd associates [19] and Deviri and colleagues [20]. Surgicalortality has markedly decreased during the last decade,
lthough preoperative functional class still affects survival21]. Heart valve reoperation for prosthetic valve endocar-itis is a procedure at highest risk, with operative mortalityates ranging between 20% and 65% [4], with a fall to 10% inome recent series [22], the latter consistent with our re-ults. This procedure is performed on systematically illatients and often in nonelective conditions.Our Cox proportional hazards regression model iden-
ified advanced New York Heart Association class, com-romised preoperative ejection fraction, advanced age,hronic renal insufficiency, emergent or urgent interven-ion, and tricuspid valve involvement as independentredictors of mortality in the overall population. Con-erning New York Heart Association classification, on the
able 5. Postoperative Complications in Overall Studyopulation
omplication Incidence
troke 8 (2.7%)epsis 5 (1.7%)yocardial infarction 2 (0.7%)
enal insufficiency 19 (6.5%)espiratory distress 15 (5.2%)
notropic support �24 hours 10 (3.4%)evision for bleeding 13 (4.5%)
asis of our experience we agree with others who recom-
by on June 2, 2013 als.org
msHYpWrwuapaoo
pipmiprstnmnt(dspvpoistliiemtfasitphihpf
R
1
1
1
1
1
1
1
1
1
1
2
2
2
2
1283Ann Thorac Surg LUCIANI ET AL2006;81:1279–83 REPEAT VALVULAR OPERATIONS
CA
RD
IOV
ASC
ULA
R
end earlier reoperation in patients affected by progres-ive prosthetic valve dysfunction [11]. Performance ofVR before the patient enters a more advanced Nework Heart Association class may significantly improverognosis. The same can be said about ejection fraction.e report higher operative mortality among patients
equiring tricuspid valve surgery alone or in associationith other valve procedures as compared with patientsndergoing aortic or mitral re-replacement alone. Akinsnd coworkers [14] identified the number of previousrocedures as a risk factor for operative mortality (7.3%t first reintervention and 14.3% at the third). Conversely,ur data suggest that the risk is significantly increasednly in patients who underwent a fourth reintervention.We identified no technical element among factors
redictive of death. Fourth HVR and tricuspid valvenvolvement characterize populations at higher riskrobably as a consequence of the severely compromisedyocardial and general status of such patients. These
ndividuals are in our experience more likely to sufferulmonary complication, low-output status, and delayedecovery from the intensive care unit. The same is to beaid about the indications to redo surgery. Nevertheless,echnical problems associated with repeat median ster-otomy did not have a significant impact on our overallortality. We believe that the number of previous ster-
otomies does not increase the risk of reentry injuries tohe heart and great vessels. The morphology of the thoraxshort anteroposterior axis) and the kind of valvularisease (namely severe tricuspid lesion and aortic steno-is) play a main role in increasing this risk. Thereafter,reoperative computed tomographic scan is always ad-isable in redo patients but becomes mandatory in theresence of the above-mentioned conditions regardlessf the number of previous sternotomies. We report a low
ncidence of complications inherent to surgery itself,uch as intraoperative massive bleeding and mediastini-is. Furthermore, the adoption of the Harmonic scalpel isikely to contribute to reduction of postoperative morbid-ty [23]. The limited use of aprotinin among our patientss not likely to affect the reliability of our data of postop-rative bleeding. As a major conclusion of our study,ortality in redo valvular surgery fundamentally shares
he same risk factors as primary procedures. The need forour reinterventions still identifies a subgroup of patientst higher risk. Novel approaches such as ministernotomyolutions and robotic-aided surgery might decrease thencidence of satellite complications. However, conven-ional valvular surgery as described herein has beenrogressively optimized in the last few years, and in-ospital risk of HVRs is comparable to that for primary
nterventions if HVR is not delayed until clinical andemodynamic deterioration occurs. From a technicaloint of view, even minor improvements in surgical
acilities might improve results in these settings.
eferences
1. de Almeida Brandao CM, Pomerantzeff PMA, Souza LR, et
al. Multivariate analysis of risk factors for hospital mortalityats.ctsnetjournDownloaded from
in valvular reoperations for prosthetic valve dysfunction.Eur J Cardiothorac Surg 2002;22:922–6.
2. Morishita K, Mawatari T, Baba T, et al. Re-replacement forprosthetic valve dysfunction: analysis of long-term resultsand risk factors. Ann Thorac Surg 1998;65:696–9.
3. Beghi C, De Cicco G, Nicolini F, et al. Cardiac valve reop-erations: analysis of operative risk factors in 154 patients.J Heart Valve Dis 2002;11:258–62.
4. Bortolotti U, Milano A, Mossuto E, et al. Early and lateoutcome after reoperation for prosthetic valve dysfunction:analysis of 549 patients during a 26-years period. J HeartValve Dis 1994;3:81–7.
5. Jones JM, O’kane H, Gladstone DJ, et al. Repeat heart valvesurgery: risk factors and operative mortality. J Thorac Car-diovasc Surg 2001;122:913–8.
6. Luciani N, Nasso G, Piscitelli M, Possati G, Anselmi A.Computed tomography scan in redo valvular surgery. AnnThorac Surg 2005;80:2422–3.
7. Nashef SA, Roques F, Hamill BG, et al. Validation of Euro-pean System for Cardiac Operative Risk Evaluation (Euro-SCORE) in North American cardiac surgery. Eur J Cardio-thorac Surg 2002;22:101–5.
8. Edmunds LH Jr, Clark RE, Cohn LH, et al. Guidelines forreporting morbidity and mortality after cardiac valve oper-ations. J Thorac Cardiovasc Surg 1996;112:708–11.
9. Rodewald G, Guntau J, Bantea C, et al. The risk of reopera-tion in acquired valvular heart disease. Thorac CardiovascSurg 1980;28:77–88.
0. Rossiter SJ, Miller DC, Stinson EB, et al. Aortic and mitralprosthetic valve reoperations: early and late results. ArchSurg 1979;114:1279–83.
1. Potter DD, Sundt TM, Zehr KJ, et al. Operative risk ofreoperative aortic valve replacement. J Thorac CardiovascSurg 2005;129:94–103.
2. Lytle BW, Cosgrove DM, Taylor PC, et al. Reoperations forvalve surgery: perioperative mortality and determinants ofrisk for 1,000 patients, 1958–1984. Ann Thorac Surg 1986;42:632–43.
3. Cohn LH, Aranki SF, Rizzo RJ, et al. Decrease in operativerisk of reoperative valve surgery. Ann Thorac Surg 1993:56:15–20.
4. Akins CW, Buckley MJ, Daggett WM, et al. Risk of reopera-tive valve replacement for failed mitral and aortic biopros-theses. Ann Thorac Surg 1998;65:1545–51.
5. Pansini S, Ottino G, Forsennati PG, et al. Reoperations onheart valve prostheses: an analysis of operative risk and lateresults. Ann Thorac Surg 1990;50:590–6.
6. Potter DD, Sundt TM III, Zehr JK, et al. Risk of repeat mitralvalve replacement for failed mitral valve prostheses. AnnThorac Surg 2004;78:67–72.
7. Matsuyama K, Matsumoto M, Sugita T, et al. Long-termresults of reoperative mitral valve surgery in patients withrheumatic disease. Ann Thorac Surg 2003;79:1939–43.
8. Jamieson WRE, Burr LM, Miyagishima MT, et al. Reopera-tion for bioprosthetic mitral valve structural failure—riskassessment. Circulation 2003;108(Suppl 2):98–102.
9. Rodaut R, Roques X, Lafitte S, et al. Surgery for prostheticvalve obstruction. A single center study of 136 patients. EurJ Cardiothorac Surg 2003;24:868–72.
0. Deviri E, Sareli P, Wisenbaugh T, Cronje SL. Obstruction ofmechanical heart valve prostheses: clinical aspects and sur-gical management. J Am Coll Cardiol 1991;17:646–50.
1. Lengyel M, Fuster V, Keltai M, et al. Guidelines for manage-ment of left-sided prosthetic valve thrombosis: a role ofthrombolytic therapy. J Am Coll Cardiol 1997;30:1521–6.
2. Lytle BW, Priest BP, Taylor PC, et al. Surgical treatment ofprosthetic valve endocarditis. J Thorac Cardiovasc Surg1996;111:198–210.
3. Luciani N, Anselmi A, Gaudino M, et al. Harmonic scalpelreduces bleeding and postoperatuve complications in redo
cardiac surgery. Ann Thorac Surg 2005,80:934–8.by on June 2, 2013 als.org
DOI: 10.1016/j.athoracsur.2005.11.030 2006;81:1279-1283 Ann Thorac Surg
Gianfederico Possati Fabiana Girola, Mariantonietta Piscitelli, Mario Perisano, Lorenzo Martinelli and
Nicola Luciani, Giuseppe Nasso, Amedeo Anselmi, Franco Glieca, Mario Gaudino, Repeat Valvular Operations: Bench Optimization of Conventional Surgery
& ServicesUpdated Information
http://ats.ctsnetjournals.org/cgi/content/full/81/4/1279including high-resolution figures, can be found at:
References http://ats.ctsnetjournals.org/cgi/content/full/81/4/1279#BIBL
This article cites 23 articles, 15 of which you can access for free at:
Citations
shttp://ats.ctsnetjournals.org/cgi/content/full/81/4/1279#otherarticleThis article has been cited by 11 HighWire-hosted articles:
Subspecialty Collections
http://ats.ctsnetjournals.org/cgi/collection/valve_disease Valve disease
following collection(s): This article, along with others on similar topics, appears in the
Permissions & Licensing
[email protected]: orhttp://www.us.elsevierhealth.com/Licensing/permissions.jsp
in its entirety should be submitted to: Requests about reproducing this article in parts (figures, tables) or
Reprints [email protected]
For information about ordering reprints, please email:
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from