Pneumonia Prevention to Decrease Mortality in Intensive Care ...
-
Upload
khangminh22 -
Category
Documents
-
view
2 -
download
0
Transcript of Pneumonia Prevention to Decrease Mortality in Intensive Care ...
M A J O R A R T I C L E
Pneumonia Prevention to Decrease Mortality inIntensive Care Unit: A Systematic Review andMeta-analysis
Antoine Roquilly,1 Emmanuel Marret,3 Edward Abraham,4 and Karim Asehnoune1,2
1Service d’Anesthésie Réanimation Hôtel-Dieu, Nantes University Hospital, 2UPRES EA3826, Faculty of Médecine of Nantes, and 3Department ofAnesthesiology and Critical Care, Tenon University Hospital, University Pierre et Marie Curie, Paris, France; and 4Wake Forest School of Medicine,Winston-Salem, North Carolina
(See the Editorial Commentary by Klompas on pages 76–8.)
Background. To determine the strategies of prevention of hospital-acquired pneumonia that reduce mortality inintensive care unit (ICU).
Methods. We followed PRISMA (Preferred Reported Items for Systemic Reviews and Meta-Analyses) guide-lines. We searched MEDLINE and the Cochrane Controlled Trials Register (through 10 June 2014) as well as refer-ence lists of articles. We included all randomized controlled trials conducted in critically ill adult patientshospitalized in ICUs and evaluating digestive prophylactic methods (selective digestive decontamination [SDD],acidification of gastric content, early enteral feeding, prevention of microinhalation); circuit prophylactic methods(closed suctioning systems, early tracheotomy, aerosolized antibiotics, humidification, lung secretion drainage, sil-ver-coated endotracheal tubes) or oropharyngeal prophylactic methods (selective oropharyngeal decontamination,patient position, sinusitis prophylaxis, subglottic secretion drainage, tracheal cuff monitoring). One reviewer extract-ed data that were checked by 3 others. The primary outcome was the mortality rate in the ICU.
Results. We identified 157 randomized trials to pool in a meta-analysis. The primary outcome was available in145 studies (n = 37 156). The risk ratio (RR) for death was 0.95 (95% confidence interval [CI], .92–.99; P = .02) in theintervention groups. In subgroup analysis, only SDD significantly decreased mortality compared with control(n = 10 227; RR, 0.84 [95% CI, .76–.92; P < .001]). The RR for in-ICU death was 0.78 (95% CI, .69–.89; P < .001;I2 = 33%) in trials investigating SDD with systemic antimicrobial therapy and 1.00 (.84–1.21; P = .96; I2 = 0%) with-out systemic antimicrobial therapy.
Conclusions. Selective digestive decontamination with systemic antimicrobial therapy reduced mortality andshould be considered in critically ill patients at high risk for death.
Keywords. hospital-acquired pneumonia/prevention; mortality; selective digestive decontamination; mechanicalventilation.
Hospital-acquired pneumonia (HAP), and notably ven-tilator-associated pneumonia, developing as a conse-quence of lung bacterial colonization, alters clinically
important outcomes, including duration of mechanicalventilation, length of stay in the intensive care unit(ICU), and mortality rates [1–3]. HAP is associatedwith use of antibiotics that may increase the risk of mul-tiple-drug-resistant bacteria in ICUs, and the increase inmedical costs is estimated to be to $20 000 per episode ofHAP [4]. Given HAP-associated morbidity, the preven-tion of HAP has been the focus of numerous studies incritically ill patients and remains a controversial issue.
Bacterial colonization of the oropharynx and subse-quent microaspirations are initial events that lead toHAP [5–7]. The prevention of such events was therefore
Received 22 January 2014; accepted 4 August 2014; electronically published 24September 2014.
Correspondence: Karim Asehnoune, MD, PhD, CHU de Nantes, Service d’Anes-thésie Réanimation, 1 Pl Alexis Ricordeau, 44093 Nantes Cedex 1, France ([email protected]).
Clinical Infectious Diseases® 2015;60(1):64–75© The Author 2014. Published by Oxford University Press on behalf of the InfectiousDiseases Society of America. All rights reserved. For Permissions, please e-mail:[email protected]: 10.1093/cid/ciu740
64 • CID 2015:60 (1 January) • Roquilly et al
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
proposed as a method for reducing the rate of HAP and presum-ably for reducing associated morbidity and mortality. Three mainapproaches have been evaluated: (1) diminishing the microaspi-ration of digestive flora; (2) reducing the volume of oropharyn-geal secretions aspirated into the lungs; and (3) inhibitingovergrowth or alterations in the microbiome in the oropharynxor larynx. Several meta-analyses of approaches to reducing the in-cidence of HAP conclude to a reduction in the risk of infection ofsuch strategies. However, international recommendations for theprevention of HAP provide different conclusions [8–11] and donot state which intervention is mandatory or superior to the oth-ers. The combination of several strategies for preventing HAPfailed to improve mortality rates [12], and nonadherence to inter-national guidelines for HAP prevention is common [13].
We have hypothesized that all the preventive strategies do notequally alter the risk of death. Because many interventions areoften poorly applied in clinical practice, it is important to deter-mine the most effective interventions that should be implementedin critically ill patients. We thus performed a systematic review todetermine which method is the most effective for decreasingmor-tality rates. The rates of HAP, duration of mechanical ventilation,and ICU length of stay were also evaluated as secondary criteria.
MATERIALS AND METHODS
Data Source and SearchesWe followed PRISMA (Preferred Reported Items for SystemicReviews and Meta-Analyses) guidelines were followed duringthe design and implementation of this meta-analysis (Supple-mentary Table 1). We attempted to identify all relevant studiespublished in English regardless of publication status (publishedor in press). We considered abstracts presented at scientificmeetings <3 years earlier (Society Of Critical Care Medicine,European Society of Intensive Care Medicine, Societé Françaised’Anesthesie Reanimation, Societé de Reanimation de LangueFrançaise). PubMed (MEDLINE/Index Medicus) and theCochrane Controlled Trials Register were searched for studiespublished from January 1969 through 10 June 2014. The Med-ical Subject Heading terms used for the search were pneumoniaand intensive care units with the limit “adult 19+ years.” The“related articles” hyperlinks in MEDLINE were explored for ad-ditional references. The reference lists of all selected trials andprevious published meta-analysis were checked for additionalreferences. We contacted authors to identify unpublished data.
Study SelectionThe authors selected all randomized trials that evaluated any ofthe following strategies in adult patients (aged ≥18 years) hos-pitalized in ICUs: acidified enteral feeding, selective digestivedecontamination (SDD), early enteral feeding, postpyloricenteral feeding, decreased gastric retention, probiotic/symbiotic
therapies, ulcer prophylaxis, aerosolized antibiotics, closed suc-tioning systems, early tracheotomy, humidification, phytotherapy(ginger extract), physiotherapy, positive end-expiratory pressure(PEEP), tracheal saline instillation, silver-coated endotrachealtubes), selective oropharyngeal decontamination (SOD), patientposition, sinusitis prophylaxis, subglottic secretion drainage, andtracheal cuff monitoring. Studies using a cluster-randomizationprocedure were included in the main analysis, but a sensitiveanalysis with exclusion of such studies was planned a priori.Pediatric patients were excluded from the study.
Data Extraction and Quality AssessmentOne author (A. R.) checked all titles and abstracts of the articlesidentified from the database research and examined in full allrandomized trials potentially eligible for the review. Quality as-sessment for each study was performed by 2 unblinded investi-gators (A. R. and K. A.). Any disagreement among the 2 authorswas resolved by discussion. Persistent disagreement was settledby discussion with other authors (E. M. and E. A.) after separatereview of the report.
One author (A. R.) designed a standard data extraction form,and other authors (E. M., E. A., and K. A.) amended and vali-dated the design of the form before abstraction of data. One au-thor (A. R.) extracted the following data from each eligiblestudy: first author, year of publication, quality assessment bythe Cochrane Collaboration’s risk of bias tool, type of interven-tion, inclusion criteria, criteria used for HAP diagnosis, numberof patients, number of HAP cases, duration of mechanical ven-tilation and of ICU stay, and ICU mortality rate. Data were ex-tracted from the tables, figures, text of the manuscript, and/orfrom previous meta-analysis that included the selected trial.
Data Synthesis and AnalysisThe primary evaluation criterion was the rate of in-ICU deaths, thatis, the ICU mortality rate. When no information was available onin-ICU deaths, the rate of in-hospital death was considered if pro-vided.When trials had 2 control arms, the numbers of deaths in thecontrol arms were pooled. The other end points analyzed includedthe incidence of HAP, the duration of mechanical ventilation, andthe ICU length of stay (or duration of hospitalization, as provided).
Statistical AnalysesAll statistical analyses were performed using Review Managersoftware (version 5.1.6; Cochrane Collaboration; NordicCochrane Centre) or Stata software (version 10.1; StataCorp).For dichotomous data (mortality and HAP), we calculated therisk ratio (RR) with 95% confidence intervals (CIs). To estimatethe clinical relevance of a beneficial effect on mortality, we cal-culated the number needed to treat with 95% CIs, using RR andcontrol event rates if the RR was significant. For continuousdata, weighted mean differences with 95% CIs were calculated.
Pneumonia Prevention • CID 2015:60 (1 January) • 65
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
Heterogeneity was determined using the I2 statistics. All pooledestimates used the randomeffectsmodel. A sensitivity analysis wasachieved with the exclusion of cluster-randomized trial [14].
In exploratory analyses, we compared the effects of SDD onmortality rates, based on the administration of systemic antimi-crobial therapy (or not), population (trauma and surgical vsmedical or mixed population), sample size (>200 or <200 pa-tients), and risk of bias (double blinding and randomization).To evaluate publication bias for trials that studied SDD, we con-structed a funnel plot and carried out Egger regression interceptand Begg rank correlation tests to assess asymmetry. The preci-sion of each trial was evaluated according to the standard errorof logarithm RR. Egger test and Begg rank test results were con-sidered significant at P < .10 because these tests have low power.We finally performed a meta-regression analysis to explore thepossible interaction between the mortality rate (baseline risk) in
the control group and the effect of SDD. Differences were con-sidered statistically significant at P < .05.
Role of the Funding SourceNone of the institutions/sponsors of individual author had anyrole in thedesignandconduct of the study; collection,management,analysis, and interpretation of the data; or preparation, review, orapproval of the manuscript. The corresponding author had full ac-cess to all the data in the study and had final responsibility for thedecision to submit the manuscript for publication.
RESULTS
Identification of the TrialsFigure 1 presents the overall search approach. Our initialsearches identified 1113 studies in MEDLINE and 465 studies
Figure 1. Literature search and study selection. Asterisks indicate studies providing the primary outcome, intensive care unit (ICU) mortality rate. Ab-breviations: PEEP, positive end-expiratory pressure; SDD, selective digestive decontamination; SOD, selective oropharyngeal decontamination. aTotal 146studies because one study comparing 1 control group to 2 intervention groups (1 digestive method and 1 oro-pharyngeal method) was counted twice.
66 • CID 2015:60 (1 January) • Roquilly et al
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
in the Cochrane Controlled Trials Register. After duplicate titlesand abstracts were removed, 1220 citations were excluded (1041nonrandomized trials and 179 irrelevant citations). The remain-ing 278 studies were considered potentially eligible and wereaccessed for full-text review. After exclusion of 117 trials (103nonrandomized, 8 without outcomes of interest, 6 with ab-stracts >3 years old), we included 157 evaluable trials, ofwhich 145 provided the mortality rate.
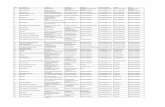
Description of Recorded Outcomes and Tested InterventionsSupplementary Table 2 summarizes the characteristics of theincluded clinical trials. Fifteen trials (9.6%) had >2 arms: 7(5%) compared 1 control group with 2 interventional groupscombined for analysis, 1 (1%) compared 1 control group with2 interventional groups considered separately for the analysis;5 (3.2%) compared 1 interventional group with 2 control
groups combined for analysis. For 2 trials with a 2 × 2 design,the 3 intervention groups (two groups with one of the inter-ventions and one group with the association of the twointerventions) were combined and compared with the double-dummy (none of the intervention) group. One trial with a2 × 2 design compared patients who received continuous sub-glottic secretion drainage or control and ulcer prophylaxiswith either H2-receptor antagonist or aluminate, no placebowas used for ulcer prophylaxis, and only 2 arms were thus con-sidered for the analyses (subglottic secretion drainage vscontrol).
Description of ParticipantsFifteen studies (9.6%) included medical ICU patients, 46(29.2%) included surgical or trauma ICU patients, and 96(61.1%) included mixed ICU populations.
Figure 2. Hospital mortality rates in critically ill patients receiving a strategy for preventing hospital-acquired pneumonia. All pooled estimates used the randomeffects model. Boldface P values indicate significant differences (P < .05). Abbreviations: CI, confidence interval; ET, endotracheal tube; NA, not applicable; PEEP,positive end-expiratory pressure; RCT, randomized controlled trial; SDD, selective digestive decontamination; SOD, selective oropharyngeal decontamination.
Pneumonia Prevention • CID 2015:60 (1 January) • 67
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
Risk of Bias in the Included StudiesThe risks for bias are presented in Supplementary Table 3. All stu-dies were randomized; the risk of bias for allocation concealmentwas low in 98 studies (62%). The risks of performance (double-blind study) and detection bias (blinding of outcome assessment)were low in 52 (33.1%) and 89 (56.7%) of the studies, respectively.
Effect of InterventionsPrimary Outcome: In-ICU DeathsWe computed data from 145 randomized trials (37 156 pa-tients). The in-ICU mortality rate was 4079 of 18 838 (21.6%)in the experimental groups versus 4160 of 18 318 (22.7%) incontrols (RR, 0.95 [95% CI, .92–.99; P = .02; I2 = 4%]; numberneeded to treat, 89 [95% CI, 50–443]). The results for each in-tervention analyzed separately are provided in Figure 2 (andSupplementary Figure 1 for forest plots of each interventionseparately). Except SDD, no tested strategy significantly de-creased ICU mortality rates.
In the 30 trials (10 227 patients) investigating SDD versusstandard care or placebo, the in-ICU mortality rate for treatedvs control patients was 1051 of 5326 (19.7%) versus 1143 of4901 (23.3%) (RR, 0.84 [95% CI, .76–.92]; number needed totreat, 27 [95% CI, 18–54]) (Figure 3A) [14–43]. The benefit ofSDD for in-ICU mortality rates remains significant after exclu-sion of the cluster-randomized trial (603 of 3209 [18.8%] vs 686of 2880 [23.8%]; RR, 0.82 [95% CI, .68–.95, P < .001]) (Supple-mentary Table 4). The funnel plot showed no evidence forasymmetry and does not suggest publication bias or otherbias (Egger test, P = .17; Begg test, P = .69) (Figure 3B). In sub-group analyses, the RR for in-ICU death was 0.78 (95% CI,.69–.90; P < .001; I2 = 40%) in trials investigating SDD with sys-temic antimicrobial therapy and 1.01 (95% CI, .85–1.21; P = .91;I2 = 0%) in trials without systemic antimicrobial therapy (Sup-plementary Tables 4 and 5). Given the risk of selection of resis-tant bacteria with antimicrobial therapies [44], defining thepopulation in which SDD is more effective is an important inassessing the use of such therapy. We thus investigated the as-sociation between the effects of SDD and mortality rate in thecontrol group (a proxy for baseline risk). In meta-regressionanalysis, there was a trend toward a positive interaction betweenthe rate of death in the control groups and benefit from SDD(P = .07; Figure 3C).
Secondary OutcomesThe HAP rate was reported in 148 trials (28 856 patients); HAPwas diagnosed in 2156 of 14 457 patients (14.9%) assigned totreatment versus 2994 of 13 799 (21.7%) who received controltherapy (RR, 0.69 [95% CI, .63–.75; P < .001]; χ2 = 391[P < .001; I2 = 63%]). When each intervention is analyzed sepa-rately (Figure 4), the RR for HAP was reduced in trials evaluat-ing SDD versus placebo (P < .001), postpyloric versus gastric
enteral feeding (P = .02), PEEP versus no PEEP (P = .02), tra-cheal saline instillation versus standard secretion drainage(P = .009), aerosolized antibiotic versus placebo (P = .04), sil-ver-coated versus classic endotracheal tube (P = .002), SOD ver-sus standard oral care (P < .001), and subglottic versus routinesecretion drainage (P < .001).
The duration of mechanical ventilation was reported in 85studies (23 691 patients) and showed high heterogeneity acrossstudies (I2 = 84%). The duration of mechanical ventilation wasreduced in the intervention groups compared with the controlgroups (weighted mean difference, −0.75 days (95 CI%, −1.16to −.35; P < .001). When each intervention is analyzed sepa-rately (Figure 5), the duration of mechanical ventilation was re-duced in trials evaluating SDD versus standard care or placebo(P = .003) and physiotherapy versus standard care (P = .03).
The duration of the ICU stay was reported in 82 studies(22 718 patients). It was reduced in the intervention groupscompared with the control groups (weighted mean difference,−1.13 days [95 CI%, −1.70, −.57; P < .001; I2 = 89%]). Wheneach intervention is analyzed separately (Figure 6), the durationof ICU stay was reduced in trials evaluating phytotherapy (gin-ger extract) versus placebo (P < .001) or SOD versus standardoral care (P = .03).
DISCUSSION
For this systematic review, we performed an extensive literaturesearch with few limits regarding publication status, therebyminimizing the risk of missing important studies. This meta-analysis shows that SDD is the main intervention decreasingthe mortality rate in critically ill patients.
It is widely accepted that HAP increases morbidity and mor-tality rates in critically ill patients [45, 46]. In the current results,there is a paradox between the sharp reduction in the rate ofHAP and the small reductions in death rates and time on ven-tilators [47]. This paradox may be attributable to the systemicdiffusion of prophylactic antibiotics used for the SDD [48,49], which can alter the accuracy of the bacteriological samplesand thus increase the rate of false-negatives in the diagnosis ofHAP. Moreover, the diagnosis of HAP has a low specificity andhigh interobserver variability [50], and there are major discrep-ancies between the clinical diagnoses of HAP and the autopsyfindings in critically ill patients [51, 52]. We thus used mortalityrate as the primary outcome in this meta-analysis, because it al-lows us to control the risk of detection bias associated with thediagnosis of HAP, notably in open-label trials.
Previous reviews and meta-analyses have already reported areduction in the risk of death with SDD [53]. In clinical practice,however, SDD is rarely used in ICUs [54] and was not even con-sidered in a recent European survey that evaluated the approach-es for HAP prevention in ICUs [55].The most likely explanation
68 • CID 2015:60 (1 January) • Roquilly et al
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
Figure 3. Intensive care unit (ICU) mortality rates in trials evaluating selective digestive decontamination. A, Forest plot for mortality in randomizedclinical trials evaluating the effects of digestive decontamination in critically ill patients [14–43]. B, Funnel plot for mortality rates in randomized controlledtrials depicts the effects of digestive decontamination on mortality. The x-axis represents the effect; the y-axis, precision. C, Meta-regression analysisexploring the interaction between survival benefit with digestive decontamination and the incidence of mortality in the control group (y =−0.83x + 1.107;P = .07). Abbreviations: CI, confidence interval; M-H, Mantel-Haenszel; RR, risk ratio; SE (Log RR), standard error of the logarithm of the risk ratio.
Pneumonia Prevention • CID 2015:60 (1 January) • 69
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
Figure 4. Hospital-acquired pneumonia in critically ill patients receiving a strategy for preventing hospital acquired pneumonia. All pooled estimates used the random effects model. Boldface P values indicatesignificant differences (P < .05). Abbreviations: CI, confidence interval; ET, endotracheal tube; NA, not applicable; PEEP, positive end-expiratory pressure; RCT, randomized controlled trials; SDD, selective digestivedecontamination; SOD, selective oropharyngeal decontamination.
70•
CID
2015:60(1
January)
•Roquilly
etal
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
for the infrequent use of SDD is concern about the risk foremerging antimicrobial resistance during treatment [44, 56,57]. However, in the largest trial of SDD [14], the percentagesof resistant bacteria causing ICU-acquired bacteremia were notsignificantly altered in patients treated with SDD, compared withcontrols. Moreover, in a recent meta-analysis including microbi-ological data issue from 35 studies, no relationship was foundbetween the use of SDD and development of antimicrobial-resistance in pathogens [58]. In the subgroup of patients with in-fection due to gram-negative bacteria, SDD was associated with adecreased risk of resistance to cephalosporins and quinolones[58]. This surprising result may be explained by the reductionin the total daily doses of antibiotics that has been reportedwith SDD [14]. The lack of a proof for increased antimicrobialresistance in numerous studies suggests that the perceived riskof selection of resistant bacteria does not justify the low rate ofSDD use in clinical practice. However, the long-term risk of
emergence of resistance needs to be better investigated beforewe can rule out this potential side effect of SDD.
Given concerns regarding acquisition of bacterial resistance,it has been suggested that SDD may be used in selected popu-lations, but little information is available regarding the popula-tions that could be eligible for SDD. In particular, medicalversus surgical reasons for ICU admission are not reliable crite-ria in selecting patients for SDD [59]. The result of the meta-regression (Figure 2C) suggests that SDD is more effective inpatients with a high risk of death. In 2 systematic reviews,SDD seemed particularly effective in patients with multipleorgan dysfunction syndrome or with a high risk for bacteremia[60]. Taken together, these data suggest that the use of SDDcould be limited to patients with a high risk of death, such asthose presenting with acute organ failure on admission.
Several regimens of SDD have been proposed, and the use ofa systemic antimicrobial therapy is one of the main differences
Figure 5. Duration of mechanical ventilation in critically ill patients receiving a strategy for preventing hospital-acquired pneumonia. All pooled estimatesused the random effects model. Boldface P values indicate significant differences (P < .05). Abbreviations: CI, confidence interval; ET, endotracheal tube; NA,not applicable; PEEP, positive end-expiratory pressure; RCT, randomized controlled trial; SDD, selective digestive decontamination; SOD, selective oropha-ryngeal decontamination; WMD, weighted mean difference.
Pneumonia Prevention • CID 2015:60 (1 January) • 71
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
between them. We found that systemic antimicrobial therapy isessential to a decrease in the risk of mortality. The recent dem-onstration that the distal respiratory flora is not distinct fromthe upper airway microbiome in healthy lungs [61, 62] suggeststhat HAP results from an increased population of distal lungbacteria rather than colonization from the digestive tract.This hypothesis can explain why the application of an oralpaste of nonabsorbable antibiotics, which has no effect onthe lung microbiome, is not sufficient to prevent HAP and re-duce the risk of death. Finally, the current results argue thatprotocols of SDD should always include a short course of sys-temic antimicrobial therapy and question the importance ofthe oral paste.
This meta-analysis has some limitations. First, our studycombined different types of interventions. This strategy of anal-ysis has already been used to estimate the attributable mortalityof HAP [46, 63], and it will enable intensivists to prioritize strat-egies for implementation in clinical practice. Second, the num-ber of patients in the SDD analyses is greater than the numberfor any other intervention, which results in a higher power forSDD than for other strategies. Thus, the current meta-analysescannot rule out the efficiency of strategies with fewer includedpatients. Third, the prevention of ventilator-associated pneu-monia was analyzed together with that of HAP. However, path-ogens involved in HAP are similar regardless of whether or notHAP is acquired during mechanical ventilation, thereby
Figure 6. Duration of ICU stay for critically ill patients receiving a strategy for preventing hospital-acquired pneumonia. All pooled estimates used therandom effects model. Boldface P values indicate significant differences (P < .05). Abbreviations: CI, confidence interval; ET, endotracheal tube; ICU, inten-sive care unit; NA, not applicable; PEEP, positive end-expiratory pressure; RCT, randomized controlled trial; SDD, selective digestive decontamination; SOD,selective oropharyngeal decontamination; WMD, weighted mean difference.
72 • CID 2015:60 (1 January) • Roquilly et al
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
suggesting that preventive strategies should be efficient withboth HAP and ventilator-acquired pneumonia [64]. Finally,the existing literature on SDD has mainly considered short-term impacts on morbidity and mortality rates. If SDD eventu-ally leads to increased prevalence of resistant bacteria, then theshort-term benefits could be reversed by increases in failure ofcurative antimicrobial therapy.
In conclusion, the current meta-analysis, which includes 157randomized studies, highlights the benefits preventing HAP indecreasing death rates in critically ill patients. When specific in-terventions are considered separately, SDD with systemic anti-microbial therapy should be considered first in critically illpatients, mainly in those with acute organ failure and at highrisk for death. Ongoing trials should (1) enhance the selectionof patients who may benefit from SDD and determine the min-imal efficient duration of systemic antimicrobial therapy;(2) compare systemic antimicrobial therapy, with or withoutdigestive decontamination; (3) determine the optimal antimi-crobial therapy in patients treated with SDD who develop asubsequent infection; and (4) assess the long-term risk foremergence of multiple-drug-resistant bacteria.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online(http://cid.oxfordjournals.org). Supplementary materials consist of dataprovided by the author that are published to benefit the reader. The postedmaterials are not copyedited. The contents of all supplementary data are thesole responsibility of the authors. Questions or messages regarding errorsshould be addressed to the author.
Notes
Author contributions. A. R., E. M., and K. A. designed and organizedresearch; acquired, analyzed and interpreted data; and wrote the manuscript.Emmanuel Marret performed the statistical analysis. E. A. provided criticalrevision of the manuscript for intellectual content. E. A. and K. A. supervisedthe study. K. A. had full access to all the data in the study and takes respon-sibility for the integrity of the data and the accuracy of the data analysis. Allauthors have agreed to submit data for publication.Disclaimer. The funders had no role in study design, data collection
and analysis, decision to publish, or preparation of the manuscript.Financial support. This work was supported by institutional and
departmental funds.Potential conflicts of interest. E. M. has been a consultant for Bayer.
K. A. has been on the speakers’ bureau for Fresenius and B. Braun Medicaland has been a consultant to Astellas Pharma. All other authors report nopotential conflicts.All authors have submitted the ICMJE Form for Disclosure of Potential
Conflicts of Interest. Conflicts that the editors consider relevant to the con-tent of the manuscript have been disclosed.
References
1. Mizgerd JP. Acute lower respiratory tract infection. N Engl J Med 2008;358:716–27.
2. Heyland DK, Cook DJ, Griffith L, Keenan SP, Brun-Buisson C. The at-tributable morbidity and mortality of ventilator-associated pneumonia
in the critically ill patient. The Canadian Critical Trials Group. Am JRespir Crit Care Med 1999; 159:1249–56.
3. Bekaert M, Timsit JF, Vansteelandt S, et al. Attributable mortality ofventilator-associated pneumonia: a reappraisal using causal analysis.Am J Respir Crit Care Med 2011; 184:1133–9.
4. Safdar N, Dezfulian C, Collard HR, Saint S. Clinical and economic con-sequences of ventilator-associated pneumonia: a systematic review. CritCare Med 2005; 33:2184–93.
5. Bonten MJ, Gaillard CA, de Leeuw PW, Stobberingh EE. Role of colo-nization of the upper intestinal tract in the pathogenesis of ventilator-associated pneumonia. Clin Infect Dis 1997; 24:309–19.
6. Ewig S, Torres A, El-Ebiary M, et al. Bacterial colonization patterns inmechanically ventilated patients with traumatic and medical head inju-ry: incidence, risk factors, and association with ventilator-associatedpneumonia. Am J Respir Crit Care Med 1999; 159:188–98.
7. Bonten MJM. Ventilator-associated pneumonia and the gastropulmo-nary route of infection: a pendulum. Am J Respir Crit Care Med2011; 184:991–3.
8. American Thoracic Society, Infectious Diseases Society of America.Guidelines for the management of adults with hospital-acquired, venti-lator-associated, and healthcare-associated pneumonia. Am J RespirCrit Care Med 2005; 171:388–416.
9. Torres A, Carlet J. Ventilator-associated pneumonia. European TaskForce on ventilator-associated pneumonia. Eur Respir J 2001; 17:1034–45.
10. Healthcare Infection Control Practices Advisory Committee, Centersfor Disease Control and Prevention. Guidelines for preventing health-care-associated pneumonia, 2003 recommendations of the CDC and theHealthcare Infection Control Practices Advisory Committee. RespirCare 2004; 49:926–39.
11. Dodek P, Keenan S, Cook D, et al. Evidence-based clinical practiceguideline for the prevention of ventilator-associated pneumonia. AnnIntern Med 2004; 141:305–13.
12. Bouadma L, Deslandes E, Lolom I, et al. Long-term impact of a multi-faceted prevention program on ventilator-associated pneumonia in amedical intensive care unit. Clin Infect Dis 2010; 51:1115–22.
13. Rello J. Why do physicians not follow evidence-based guidelines forpreventing ventilator-associated pneumonia? : a survey based on theopinions of an international panel of intensivists. Chest 2002;122:656–61.
14. de Smet AMGA, Kluytmans JAJW, Cooper BS, et al. Decontaminationof the digestive tract and oropharynx in ICU patients. N Engl J Med2009; 360:20–31.
15. Aerdts SJ, Clasener HA, van Dalen R, et al. Prevention of bacterial col-onization of the respiratory tract and stomach of mechanically ventilat-ed patients by a novel regimen of selective decontamination incombination with initial systemic cefotaxime. J Antimicrob Chemother1990; 26(suppl A):59–76.
16. Arnow PM, Carandang GC, Zabner R, Irwin ME. Randomizedcontrolled trial of selective bowel decontamination for prevention ofinfections following liver transplantation. Clin Infect Dis 1996; 22:997–1003.
17. Blair P, Rowlands BJ, Lowry K,Webb H, Armstrong P, Smilie J. Selectivedecontamination of the digestive tract: a stratified, randomized, pro-spective study in a mixed intensive care unit. Surgery 1991; 110:303–9.
18. Cerra FB, Maddaus MA, Dunn DL, et al. Selective gut decontaminationreduces nosocomial infections and length of stay but not mortality ororgan failure in surgical intensive care unit patients. Arch Surg 1992;127:163–7.
19. Cockerill FR, Muller SR, Anhalt JP, et al. Prevention of infection in crit-ically ill patients by selective decontamination of the digestive tract. AnnIntern Med 1992; 117:545–53.
20. de Jonge E, Schultz MJ, Spanjaard L, et al. Effects of selective decon-tamination of digestive tract on mortality and acquisition of resistantbacteria in intensive care: a randomized controlled trial. Lancet 2003;362:1011–6.
Pneumonia Prevention • CID 2015:60 (1 January) • 73
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
21. de La Cal MA, Cerdá E, García-Hierro P, et al. Survival benefit in crit-ically ill burned patients receiving selective decontamination of the di-gestive tract: a randomized, placebo-controlled, double-blind trial. AnnSurg 2005; 241:424–30.
22. Ferrer M, Torres A, González J, et al. Utility of selective digestive decon-tamination in mechanically ventilated patients. Ann Intern Med 1994;120:389–95.
23. Flaherty J, Nathan C, Kabins SA, Weinstein RA. Pilot trial of selectivedecontamination for prevention of bacterial infection in an intensivecare unit. J Infect Dis 1990; 162:1393–7.
24. Fox MA, Peterson S, Fabri BM, van Saene HK. Selective decontamina-tion of the digestive tract in cardiac surgical patients. Crit Care Med1991; 19:1486–90.
25. Gastinne H, Wolff M, Delatour F, Faurisson F, Chevret S; French StudyGroup on Selective Decontamination of the Digestive Tract. A con-trolled trial in intensive care units of selective decontamination of thedigestive tract with nonabsorbable antibiotics. N Engl J Med 1992;326:594–9.
26. Godard J, Guillaume C, Reverdy ME, et al. Intestinal decontaminationin a polyvalent ICU: a double-blind study. Intensive Care Med 1990;16:307–11.
27. Hammond JM, Potgieter PD, Saunders GL, Forder AA. Double-blindstudy of selective decontamination of the digestive tract in intensivecare. Lancet 1992; 340:5–9.
28. Kerver AJ, Rommes JH, Mevissen-Verhage EA, et al. Prevention ofcolonization and infection in critically ill patients a prospective ran-domized study. Crit Care Med 1988; 16:1087–93.
29. Korinek AM, Laisne MJ, Nicolas MH, Raskine L, Deroin V, Sanson-Lepors MJ. Selective decontamination of the digestive tract in neurosur-gical intensive care unit patients: a double-blind, randomized, placebo-controlled study. Crit Care Med 1993; 21:1466–73.
30. Krueger WA, Lenhart FP, Neeser G, et al. Influence of combinedintravenous and topical antibiotic prophylaxis on the incidence ofinfections, organ dysfunctions, and mortality in critically ill surgicalpatients: a prospective, stratified, randomized, double-blind, placebo-controlled clinical trial. Am J Respir Crit Care Med 2002; 166:1029–37.
31. LingnauW, Berger J, Javorsky F, Lejeune P, Mutz N, Benzer H. Selectiveintestinal decontamination in multiple trauma patients: prospective,controlled trial. J Trauma 1997; 42:687–94.
32. Mandelli M, Mosconi P, Langer M, CigadaM. Prevention of pneumoniain an intensive care unit: a randomized multicenter clinical trial. Inten-sive Care Unit Group of Infection Control. Crit Care Med 1989;17:501–5.
33. Pneumatikos I, Koulouras V, Nathanail C, Goe D, Nakos G. Selectivedecontamination of subglottic area in mechanically ventilated patientswith multiple trauma. Intensive Care Med 2002; 28:432–7.
34. Quinio B, Albanèse J, Bues-Charbit M, Viviand X, Martin C. Selectivedecontamination of the digestive tract in multiple trauma patients: aprospective double-blind, randomized, placebo-controlled study.Chest 1996; 109:765–72.
35. Rocha LA, Martín MJ, Pita S, et al. Prevention of nosocomial infectionin critically ill patients by selective decontamination of the digestivetract: a randomized, double blind, placebo-controlled study. IntensiveCare Med 1992; 18:398–404.
36. Rodríguez-Roldán JM, Altuna-Cuesta A, López A, et al. Preventionof nosocomial lung infection in ventilated patients: use of an anti-microbial pharyngeal nonabsorbable paste. Crit Care Med 1990; 18:1239–42.
37. Sánchez García M, Cambronero Galache JA, López Diaz J, et al. Effective-ness and cost of selective decontamination of the digestive tract in critical-ly ill intubated patients: a randomized, double-blind, placebo-controlled,multicenter trial. Am J Respir Crit Care Med 1998; 158:908–16.
38. Silvestri L, van Saene HK, Milanese M, et al. Prevention of MRSA pneu-monia by oral vancomycin decontamination: a randomised trial. EurRespir J 2004; 23:921–6.
39. Stoutenbeek CP, van Saene HK, Little RA, Whitehead A; WorkingGroup on Selective Decontamination of the Digestive Tract. The effectof selective decontamination of the digestive tract on mortality in mul-tiple trauma patients: a multicenter randomized controlled trial. Inten-sive Care Med 2007; 33:261–70.
40. Ulrich C, Harinck-de Weerd JE, Bakker NC, Jacz K, Doornbos L,de Ridder VA. Selective decontamination of the digestive tract with nor-floxacin in the prevention of ICU-acquired infections: a prospectiverandomized study. Intensive Care Med 1989; 15:424–31.
41. Unertl K, Ruckdeschel G, Selbmann HK, et al. Prevention of coloniza-tion and respiratory infections in long-term ventilated patients by localantimicrobial prophylaxis. Intensive Care Med 1987; 13:106–13.
42. Verwaest C, Verhaegen J, Ferdinande P, et al. Randomized, controlledtrial of selective digestive decontamination in 600 mechanically ventilat-ed patients in a multidisciplinary intensive care unit. Crit Care Med1997; 25:63–71.
43. Wiener J, Itokazu G, Nathan C, Kabins SA, Weinstein RA. A random-ized, double-blind, placebo-controlled trial of selective digestive decon-tamination in a medical-surgical intensive care unit. Clin Infect Dis1995; 20:861–7.
44. Bouza E, Granda MJP, Hortal J, Barrio JM, Cercenado E, Muñoz P. Pre-emptive broad-spectrum treatment for ventilator-associated pneumoniain high-risk patients. Intensive Care Med 2013; 39:1547–55.
45. Rincón-Ferrari MD, Flores-Cordero JM, Leal-Noval SR, et al. Impact ofventilator-associated pneumonia in patients with severe head injury.J Trauma 2004; 57:1234–40.
46. Melsen WG, Rovers MM, Koeman M, Bonten MJM. Estimating the at-tributable mortality of ventilator-associated pneumonia from random-ized prevention studies. Crit Care Med 2011; 39:2736–42.
47. Klompas M. The paradox of ventilator-associated pneumonia preven-tion measures. Crit Care 2009; 13:315.
48. Gastinne H, Wolff M, Lachatre G, Boiteau R, Savy FP. Antibiotic levelsin bronchial tree and in serum during selective digestive decontamina-tion. Intensive Care Med 1991; 17:215–8.
49. Mol M, van Kan HJM, Schultz MJ, de Jonge E. Systemic tobramycinconcentrations during selective decontamination of the digestive tractin intensive care unit patients on continuous venovenous hemofiltra-tion. Intensive Care Med 2008; 34:903–6.
50. Klompas M. Interobserver variability in ventilator-associated pneumo-nia surveillance. Am J Infect Control 2010; 38:237–9.
51. Fábregas N, Ewig S, Torres A, et al. Clinical diagnosis of ventilator as-sociated pneumonia revisited: comparative validation using immediatepost-mortem lung biopsies. Thorax 1999; 54:867–73.
52. Tejerina E, Esteban A, Fernández-Segoviano P, et al. Accuracy of clinicaldefinitions of ventilator-associated pneumonia: comparison with autop-sy findings. J Crit Care 2010; 25:62–8.
53. Liberati A, D’Amico R, Pifferi S, Torri V, Brazzi L, Parmelli E. Antibioticprophylaxis to reduce respiratory tract infections and mortality inadults receiving intensive care. Cochrane Database Syst Rev 2009; 3:CD000022.
54. Bastin AJ, Ryanna KB. Use of selective decontamination of the digestivetract in United Kingdom intensive care units. Anaesthesia 2009;64:46–9.
55. Ricard J-D, Conti G, Boucherie M, et al. A European survey of nosoco-mial infection control and hospital-acquired pneumonia preventionpractices. J Infect 2012; 65:285–91.
56. Salgado CD, O Grady N, Farr BM. Prevention and control of antimicro-bial-resistant infections in intensive care patients. Crit Care Med 2005;33:2373–82.
57. Naiemi Al N. Emergence of multidrug-resistant gram-negative bacteriaduring selective decontamination of the digestive tract on an intensivecare unit. J Antimicrob Chemother 2006; 58:853–6.
58. Daneman N, Sarwar S, Fowler RA, Cuthbertson BH; SuDDICU Cana-dian Study Group. Effect of selective decontamination on antimicrobialresistance in intensive care units: a systematic review and meta-analysis.Lancet infect dis 2013; 13:328–41.
74 • CID 2015:60 (1 January) • Roquilly et al
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022
59. Melsen WG, de Smet A, Kluytmans JAJW, Bonten MJM; Dutch SOD-SDD Trialists’ Group. Selective decontamination of the oral and diges-tive tract in surgical versus non-surgical patients in intensive care in acluster-randomized trial. Br J Surg 2012; 99:232–7.
60. Silvestri L, van Saene HKF, Milanese M, Gregori D, Gullo A. Selectivedecontamination of the digestive tract reduces bacterial bloodstream in-fection and mortality in critically ill patients. Systematic review of ran-domized, controlled trials. J Hosp Infect 2007; 65:187–203.
61. Charlson ES, Bittinger K, Haas AR, et al. Topographical continuity ofbacterial populations in the healthy human respiratory tract. Am J Re-spir Crit Care Med 2011; 184:957–63.
62. Morris A, Beck JM, Schloss PD, et al. Comparison of the respiratory mi-crobiome in healthy non-smokers and smokers. Am J Respir Crit CareMed 2013; 187:1067–75.
63. Melsen WG, Rovers MM, Groenwold RH, et al. Attributable mortalityof ventilator-associated pneumonia: a meta-analysis of individual pa-tient data from randomised prevention studies. Lancet Infect Dis2013; 13:665–71.
64. Esperatti M, Ferrer M, Theessen A, et al. Nosocomial pneumonia inthe intensive care unit acquired by mechanically ventilated versusnonventilated patients. Am J Respir Crit Care Med 2010; 182:1533–9.
Pneumonia Prevention • CID 2015:60 (1 January) • 75
Dow
nloaded from https://academ
ic.oup.com/cid/article/60/1/64/2895643 by guest on 15 February 2022