Successful prevention of ventilator-associated pneumonia in an intensive care setting
-
Upload
independent -
Category
Documents
-
view
1 -
download
0
Transcript of Successful prevention of ventilator-associated pneumonia in an intensive care setting
FIedDS
AE0
C
0
CC
d
Successful preventionof ventilator-associated pneumoniain an intensive care setting
Alexandre R. Marra, MD,a Ruy Guilherme Rodrigues Cal, MD,a Claudia Vallone Silva, RN,b Raquel Afonso Caserta, PT,aAngela Tavares Paes, PhD,c Denis Faria Moura Jr, RN,a Oscar Fernando Pavao dos Santos, MD,a,d Michael B. Edmond, MD,MPH, MPA,e and Marcelino Souza Durao, MDa,d
Sao Paulo, Brazil, and Richmond, Virginia
romsrael
Pesadeepa
choo
ddrinste565
onfl
196
opyont
oi:1
Background: Ventilator-associated pneumonia (VAP) is one of the most common health care-associated infections (HAIs) in criticalcare settings.Objective: Our objective was to examine the effect of a series of interventions, implemented in 3 different periods to reduce theincidence of VAP in an intensive care unit (ICU).Methods: A quasiexperimental study was conducted in a medical-surgical ICU. Multiple interventions to optimize VAP preventionwere performed during different phases. From March 2001 to December 2002 (phase 1: P1), some Centers for Disease Control andPrevention (CDC) evidence-based practices were implemented. From January 2003 to December 2006 (P2), we intervened in theseprocesses at the same time that performance monitoring was occurring at the bedside, and, from January 2007 to September 2008(P3), we continued P2 interventions and implemented the Institute for Healthcare Improvement’s ventilator bundle plus oral de-contamination with chlorhexidine and continuous aspiration of subglottic secretions.Results: The incidence density of VAP in the ICU per 1000 patient-days was 16.4 in phase 1, 15.0 in phase 2, and 10.4 in phase 3,P 5 .05. Getting to zero VAP was possible only in P3 when compliance with all interventions exceeded 95%.Conclusion: These results suggest that reducing VAP rates to zero is a complex process that involves multiple performance mea-sures and interventions.
Key Words: Ventilator associated pneumonia; critical care prevention; health care associated infection; ventilator bundle; infection control.Copyright ª 2009 by the Association for Professionals in Infection Control and Epidemiology, Inc.(Am J Infect Control 2009;37:619-25.)
Ventilator-associated pneumonia (VAP) is one of themost common health care-associated infections (HAIs)in critical care settings.1 Overall, VAP contributes tohigh mortality in adult intensive care patients2 and isthe leading cause of death among HAIs.3 The Centersfor Disease Control and Prevention (CDC) guidelines
the Intensive Carea and Infection Control Units,b Hospitalita Albert Einstein, Sao Paulo, Brazil; Instituto Israelita de Ensinoquisa (IIEP), Sao Paulo, Brazilc; Division of Nephrology Universi-Federal de Sao Paulo, Sao Paulo, Brazil (UNIFESP-EPM)d; andrtment of Internal Medicine Virginia Commonwealth Universityl of Medicine, Richmond, VA.e
ess correspondence to Alexandre R. Marra, MD, Av. Albertin, 627/701- No. 5 Andar-Bloco B, Sao Paulo, Brazil, CEP
1-901. E-mail: [email protected].
icts of interest: None to report.
-6553/$36.00
right ª 2009 by the Association for Professionals in Infectionrol and Epidemiology, Inc.
0.1016/j.ajic.2009.03.009
describe many different interventions for preventingVAP in intensive care units (ICUs).4 Each of these recom-mendations is categorized on the basis of existing scien-tific evidence, theoretical rationale, applicability, andpotential economic impact. However, there is little ro-bust evidence to guide the choice of interventions toimplement to decrease VAP rates.5,6
As part of the 5 Million Lives campaign, endorsed byleading US agencies and professional societies, TheInstitute for Healthcare Improvement (IHI) (http://www.i-hi.org/ihi) recommends thatall ICUs implement a ventila-tor bundle to reduce the incidence of VAP to zero.7
However, there is also no robust evidence to support atleast 2 of the 4 key components (deep venous thrombosisand peptic ulcer prophylaxis).5 Although it is unclearwhether there is any association between deep venousthrombosis and peptic ulcer prophylaxis with decreasingrates of ventilator-acquired pneumonia, the IHI recom-mends that, when applied as a package of interventionsfor ventilator care, the rate of pneumonia decreases pre-cipitously.7-9 The purpose of this prospective, quality
619
620 Marra et al. American Journal of Infection ControlOctober 2009
improvement study was to examine the effect of a seriesof interventions, implemented in 3 different periods toreduce the incidence of VAP in an ICU.
METHODS
Setting and study design
A time series study was conducted in a 38-bed, med-ical-surgical ICU of a tertiary care, private hospital inSao Paulo, Brazil. This is an open staffing model ICUwhere approximately 2200 patients are admitted annu-ally. Because this study was considered a quality im-provement project, it was not submitted to ourInstitutional Review Board. This study was carried outin 3 phases: phase 1 (March 2001 to December 2002),phase 2 (January 2003 to December 2006), and phase3 (January 2007 to September 2008).
In phase 1, we implemented head of the bed eleva-tion (HOB) and other CDC evidence practices for pre-vention of VAP,3 including (1) no routine changing ofhumidified ventilator circuits, (2) periodically drainingand discarding condensate collecting in the ventilatortubing, and (3) changing the heat-and-moistureexchangers when they malfunction mechanically orbecome visibly soiled. All of these process measureswere audited twice yearly in a small sample of me-chanically ventilated patients at random intervals. Wethen provided feedback via e-mail on compliancewith these processes for the ICU team (doctors, nurses,and respiratory therapists).
In phase 2, the same infection control practiceswere performed. In addition, we began to interveneto improve compliance with these processes at thesame time that performance monitoring was occur-ring at the bedside. The rates of process measure com-pliance were also provided in the same fashion as inphase 1.
In phase 3, after the hospital’s chief executive officerarticulated zero tolerance for VAP, we continued inter-vening in these processes in the same way it was per-formed in phase 2; however, the intensity increasedmonth by month. In April 2007, we implemented theIHI ventilator bundle (elevation of the head of thebed,; daily ‘‘sedation vacations’’ and assessment ofreadiness to extubate, peptic ulcer disease prophylaxisand deep venous thrombosis prophylaxis) for all ICUpatients requiring mechanical ventilation. This ventila-tor bundle was monitored each weekday by an ICUnurse. The nurse intervened in this process at thesame time that performance monitoring was occurringat the bedside if non-compliance with an element ofthe bundle was detected (eg, sedation was not stopped).Prior to the start of the phase 3, we delivered a briefpresentation to the ICU staff on VAP, reviewed thestudy protocol, and encouraged participation in our
‘‘ventilator bundle—getting to zero’’ program. Everymonth, we provided feedback on compliance withthe bundle components via e-mail for the ICU team(doctors, nurses, and respiratory therapists). Also, weprovided posters in the ICU with bar graphs displayingcompliance with process of care measures. In theseposters, we also provided the VAP rate determined bysurveillance conducted by infection control and hospi-tal epidemiology personnel. We continued to intervenein the other CDC evidence-based practices for preven-tion of VAP described in P1 and P2; however, these pro-cess measures were observed, and interventions weredone monthly.
Other interventions to control VAP in the ICU wereimplemented during phase 3 of the study. In October2007, oral decontamination with chlorhexidine 0.12%was introduced for all mechanically ventilated ICUpatients. In February 2008, the continuous aspirationof subglottic secretions (CASS) endotracheal tube wasimplemented for patients requiring mechanical venti-lation and suspected to require ventilation for a periodlonger than 24 hours.
Definitions
VAP surveillance was performed by trained infec-tion control professionals using the US Center forDisease Control and Prevention (CDC) definition10
for the 3 phases of the study, and the incidence ofVAP was expressed as cases of VAP per 1000 ventila-tor-days.
Microbiologic methods
All isolates were identified by manual or automatedmethods and confirmed by using the Vitek 2 system(bioMerieux Vitek, Inc., Hazelwood, MO).
Statistical analysis
Comparisons between phase 1 versus phase 2 andphase 2 versus phase 3 regarding compliance withVAP process measures and in-hospital mortality inVAP patients were performed using the x2 test. ANOVAwas performed for comparing the means of incidencedensity of VAP in the ICU per 1000 ventilator-days inthe 3 different phases.
We used segmented regression analysis of inter-rupted time series11 to assess the changes in VAP afterimplementation of the ventilator bundle, oral decon-tamination with chlorhexidine 0.12%, and CASS en-dotracheal tube for patients requiring mechanicalventilation, conforming to the interventional phasesoccurring from April 2007 to September 2008. We ad-justed a segmented regression model that allows usto analyze a reduction (or an increase) of VAP ratein each of the study segments separately: (1)
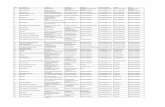
Table 1. Characteristics of both phases in the ICU during the study period
Phases
P1 P2 P3
Patient days 14,362 36,511 16,953
Ventilator days 5680 15,419 5971
Ventilator utilization ratio 0.40 0.42 0.35
Compliance with process measures, n (%)
HOB observations 526/710 (74.1) 239/267 (89.5) 7030/7264 (96.8)
Daily ‘‘sedation vacations’’ — — 3592/3632 (98.9)
Gastric prophylaxis — — 3602/3632 (99.2)
DVT/PE prevention — — 3476/3632 (95.7)
Ventilator circuits without changes 214/304 (70.4%) 67/111 (60.4) 695/704 (98.7)
HMEs changed — 105/146 (71.9) 658/704 (93.5)
Ventilator-circuit–tubing condensate — — 484/525 (92.2)
CASS endotracheal tube — — 149
Number of VAPs 91 224 62
VAP rate per 1000 ventilator-days, mean (SD) 16.4 (7.6) 15.0 (9.2) 10.4 (8.1)
In-hospital mortality in VAP patients, n (%) 41/91 (45) 91/224 (41) 22/61 (36)
NOTE. P1 5 phase 1 (March 2001 to December 2002). P2 5 phase 2 (January 2003 to December 2006). P3 5 phase 3 (January 2007 to September 2008).
HOB, head of the bed; HMEs, heat-and-moisture exchangers; CASS, continuous aspiration of subglottic secretions; DVT/PE, deep venous thrombosis/pulmonary embolism; SD, stan-
dard deviation.
www.ajicjournal.orgVol. 37 No. 8
Marra et al. 621
ventilator bundle only, April 2007 to October 2007;(2) ventilator bundle 1 chlorhexidine, November2007 to February 2008; (3) ventilator bundle 1 chlo-rhexidine 1 CASS endotracheal tube, March 2008 toSeptember 2008.
In a segmented regression modelling, 2 parameters(intercept and slope) are estimated for each segment.The intercept (b0) is the value of the series at the begin-ning of a given time interval, and the slope (b1) is theexpected change of the measure (VAP rate) for every in-crease of 1 unit of time (eg, a month). Therefore, posi-tive and negative slopes correspond to increase anddecrease of VAP rate, respectively.
All tests of statistical significance were 2-sided witha significance level set at .05. All the data analyses wereperformed using SPSS 16.0 (SPSS, Inc, Chicago, IL) andSAS 9.1 (SAS Institute Inc, Cary, NC).
RESULTS
Compliance with process measures in eachphase
In phase 1, the infection control (IC) process mea-sures for analysis included 710 HOB elevation observa-tions (74.1% compliance) and 304 ventilator circuitswithout changes (70.4% compliance). In phase 2, therewere 267 HOB elevation observations (89.5% compli-ance), 111 ventilator circuits without changes (60.4%compliance), and 146 heat-and-moisture exchangerschanged (71.9% compliance). In phase 3, more intenseobservations were performed; there were 7264 HOB el-evation with 96.8% compliance and 3632 daily seda-tion vacations, gastric prophylaxis opportunities, anddeep venous thrombosis/pulmonary embolism (DVT/
PE) prevention opportunities with 98.9%, 99.2%, and95.7% compliance, respectively. There were also 704ventilator circuits without changes with 98.7% compli-ance, 704 heat-and-moisture exchangers changed with93.5% of compliance, and 525 ventilator-circuit-tubingcondensate with 92.2% compliance. CASS endotra-cheal tube was performed in 149 patients in phase 3(Table 1). Since October 2007, all patients requiring me-chanical ventilation received oral decontaminationwith chlorhexidine 0.12%.
Incidence density of VAP and in-hospitalmortality of VAP patients
The mean incidence density of VAP per 1000 ventila-tor-days in the ICU was 16.4 in phase 1 (14,362 patient-days), 15.0 in phase 2 (36,511 patient-days), and 10.4 inphase 3 (16,953 patient-days), P 5 .05. The ventilator uti-lization ratio, the number of VAPs, ventilator-days, andin-hospital mortality of VAP patients for each phase ofthe study are shown in Table 1. There was no significantdifference in hospital mortality of VAP patients betweenP1 and P2, P 5 .47, and between P2 and P3, P 5 .51.
Getting to zero VAP was possible only in phase 3when there was greater than 95% compliance withthe ventilator bundle, oral decontamination with chlo-rhexidine 0.12%, and continuous aspiration of CASS(Fig 1). In addition to this, we continued to evaluateventilator circuits without changes, heat-and-moistureexchangers changes, and ventilator-circuit-tubingcondensate.
Segmented regression analysis showed in the firstsegment (ventilator bundle) a statistically significant in-crease in VAP rate (b1 5 2.59; P 5 .001). However, in the
0,010,020,030,040,050,060,070,080,090,0
100,0
apr/2
007
may/20
07jun
/07jul
/07
aug/2
007
sep/2
007
oct/2
007
nov/0
7
dec/2
007
jan/08
feb/20
08
mar/08
apr/2
008
may/20
08jun
/08jul
/08
aug/2
008
sep/2
008
0,0
5,0
10,0
15,0
20,0
25,0
30,0
Bundle compliance (%)VAP/1,000 ventilator-days
oral decontamination with chlorhexidine 0.12 (since October/2007)
continuous aspiration of subglottic secretions (CASS) endotracheal tube (since February/2008)
Fig 1. Bundle compliance and ventilator-associated pneumonia (VAP) rate per 1000 ventilator-days from April 2007to September 2008.
Segmented 1: 1=2.59; p=0.001Segmented 2: 2=-2.30; p=0.27Segmented 3: 3=-0.76; p=0.18
-5
0
5
10
15
20
25
0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18
21
3
Fig 2. Segmented regression of ventilator-associated pneumonia (VAP) rate per 1000 ventilator-days from April 2007to September 2008.
622 Marra et al. American Journal of Infection ControlOctober 2009
second segment (ventilator bundle 1 chlorhexidine)and in the third segment (ventilator bundle 1 chlo-rhexidine 1 CASS endotracheal tube), the slopes werenegative (b1 5 22.30 in the second segment andb1 5 20.76 in the third segment), indicating that therewas a reduction in VAP rate; however, this was not sta-tistically significant as seen in Fig 2.
Microbiologic features
As seen in Table 2, more than one quarter of thepathogens were not identified. Fifty-seven percent
(57.1%) of all the microorganisms identified in phase1 were gram negative, followed by gram-positive orga-nisms (30.8%) and fungi (12.1%). In phase 2, almost69% (68.8%) of microorganisms identified were gramnegative, followed by gram-positive organisms (23.4%)and fungi (7.8%). In phase 3, 61.5% of microorganismsidentified were gram negative, followed by gram-positive organisms (25.0%) and fungi (13.5%).
Staphylococci accounted for over 25% of the gram-positive pathogens in the 3 phases. The most prevalentpathogens overall were Pseudomonas aeruginosa,Acinetobacter baumannii, and Klebsiella pneumoniae.
Table 2. Characteristics of pathogens causing VAP during the 3 study phases in ICU patients
P1 P2 P3
Pathogen N % N % N %
Gram-positive 28 100 33 100 13 100
CNS 7 25.0 4 12.1 – –
Enterococcus spp 5 17.9 6 18.2 2 15.4
Staphylococcus aureus 7 25.0 21 63.6 9 69.2
Streptococcus spp 9 32.1 2 6.1 2 15.4
Gram-negative 52 100 97 100 33 100
Acinetobacter baumannii 12 23.1 18 18.6 6 18.2
Alcaligenes xylosoxidans 2 3.8 – – – –
Burkholderia cepacia – – 1 1.0 – –
Citrobacter freundii – – 1 1.0 – –
Citrobacter koseri – – 1 1.0 – –
Enterobacter aerogenes 3 5.8 1 1.0 2 6.1
Enterobacter cloacae 1 1.9 7 7.2 – –
Escherichia coli – – 2 2.1 2 6.1
Flavimonas oryzihabitans – – 2 2.1 – –
Klebsiella pneumoniae 6 11.5 12 12.4 5 15.1
Klebsiella oxytoca 2 3.8 – – 1 3.0
Morganella morganii 1 1.9 2 2.1 1 3.0
Neisseria spp 2 3.8 – – – –
Proteus spp 2 3.8 – – 1 3.0
Pseudomonas aeruginosa 18 34.6 36 37.1 6 18.2
Pseudomonas fluorescens – – 1 1.0 – –
Serrratia marcescens – – 3 3.1 2 6.1
Sphingomonas paucimobilis – – 1 1.0 – –
Stenotrophomonas maltophilia 3 5.8 9 9.3 7 21.2
Fungi 11 100 11 100 7 100
Aspergillus spp – – – – 1 14.3
Candida albicans 5 45.4 5 45.4 4 57.1
Candida glabrata – – 2 18.2 – –
Candida krusei – – 1 9.1 1 14.3
Candida tropicalis 4 36.4 3 27.3 1 14.3
Candida spp 2 18.2 – – – –
Identified agent 91 76.5 141 56.4 53 71.6
No identified agent 28 23.5 109 43.6 21 28.4
CNS, coagulase-negative staphylococci.
www.ajicjournal.orgVol. 37 No. 8
Marra et al. 623
DISCUSSION
This study demonstrates that VAP prevention usingthe majority of evidence-based measures for control-ling this HAI in the ICU is a difficult process that in-volves the accountability of many health careworkers who care for ventilated patients. We felt an ur-gent need to implement a new approach because ourrates of VAP were extremely high, although we hadbeen trying to control this infection since 2001. Our ex-perience shows that it is not enough to control HOB oronly to implement the IHI ventilator bundle as somecenters have advocated.6,7 We believe that, by gettingthe involvement of all members of the ICU team, we ul-timately had success in applying all these process mea-sures over several years.
Our hospital is engaged in a patient safety programthat is a resource from the IHI. This was one of our rea-sons for adopting the ‘‘VAP—getting to zero’’ goal as a
quality indicator for patient safety in our ICU. However,Ucxkay et al5 called attention to the problems with usingVAP as a quality indicator, including difficulties with thecase definition and risk adjustment. Moreover, Edmondhas pointed out that a ‘‘getting to zero’’ approach can beassociated with adverse unintended consequences.12
Eliminating HAIs has been identified as an importantpriority in many hospitals,13,14 especially since therewas a decision in the United States by Medicare to nolonger provide increased payments for VAP or centralline-associated bloodstream infections. In Brazilianhospitals, this has not yet happened, although our hos-pital’s chief executive officer and senior managementare responsible for ensuring that the health care sys-tem supports an infection prevention and control pro-gram to effectively prevent VAP.13
We believe that, to control VAP in the ICU, it is notsufficient to implement 1 measure, or even the IHIbundle, but rather it requires a culture change
624 Marra et al. American Journal of Infection ControlOctober 2009
involving the entire ICU team (doctors, nurses, respira-tory therapists). Further reductions occurred after theimplementation of the CASS endotracheal tube andoral decontamination with chlorhexidine 0.12%.Other publications have reported the utility of theCASS endotracheal tube in reducing VAP15,16 or delay-ing VAP episodes17 in the ICU. Oral decontaminationwith chlorhexidine in different concentrations18-20 isalso considered a strategy for reducing the incidenceof VAP; however, our study evaluates concomitant im-plementation of the CASS endotracheal tube and oraldecontamination with chlorhexidine. We did not finda statistically significant difference applying the venti-lator bundle, chlorhexidine, and CASS endotrachealtube in our ICU for explaining the VAP rate reductionusing a segmented regression analysis. One possibleexplanation may be the short interval period betweenthe 3 segments analyzed from April 2007 to Septem-ber 2008, for the implementation of the bundle, chlo-rhexidine, and CASS endotracheal tube in these 3different periods. Although we have not demonstrateda statistically significant finding using the segmentedregression analysis for VAP prevention, we haveachieved a zero infection rate by applying all theVAP prevention measures that are recommended inthe literature.4-7
It is important to note that our VAP surveillance wasperformed by trained infection control professionalsusing the CDC definition10 for the 3 phases of thestudy. With the increasing pressure being placed onhospitals to report measures of quality, includingVAP, there is a risk that hospital staff will subcon-sciously interpret the VAP definition in a way to min-imize their apparent VAP rates.21 Interestingly, ourVAP rates have a high proportion of non-identifiedagents (around one quarter of the cases) and Candidapneumonia (around 10% of VAP cases) in the 3phases, suggesting that the CDC definition can overes-timate the number of VAP cases. The lack of specificclinical signs and better culture diagnostic methodsleads to a variability in the diagnosis of VAP amongdifferent ICUs.22 Despite the problems associatedwith considering VAP as a good quality indicator, weachieved successful prevention of VAP in the ICU set-ting. We are completely aware that we may not be ableto sustain zero VAP rates indefinitely, but our goal is tosustain a nearly perfect compliance with the ventila-tor bundle and maintain ICU team motivation forVAP prevention.
There are several limitations to this study. This is nota randomized trial but a quasiexperimental, interrup-ted time series study. Quasiexperimental study designsare frequently used when it is not logistically feasibleto conduct a controlled trial. Thus, other unmeasuredfactors might have occurred coincident with the
interventions that occurred since April 2007 (imple-mentation of the ventilator bundle), resulting in a de-crease in VAP rates in our ICU. However, this seemsunlikely because there had been no decrease in VAPrates previously over the last several years (Table 1).Finally, because this intervention was performed at asingle medical center, these results may not be general-izable to other hospitals. Despite the limitations, ourstudy has broadened support for the concept that con-trolling VAP rates requires multiple performance mea-sures and quality improvement efforts. The processand outcome measures for VAP presented here are de-rived from published guidelines and other relevant lit-erature. Reporting both process and outcome measuresto senior hospital leadership, nursing leadership, andclinicians who care for patients at risk for VAP in theICU can be a good strategy for successfully reducingthis infection.
References
1. Richard MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infec-
tions in combined medical-surgical intensive care units in the United
States. Infect Control Hosp Epidemiol 2000;21:510-5.
2. Garrouste Orgeas M, Timsit JF, Soufir L, Tafflet M, Adrie C, Philippart
F, et al. Impact of adverse events on outcomes in intensive care unit
patients. Crit Care Med 2008;36:2041-7.
3. Warren DK, Shukla SJ, Olsen MA, Kollef MH, Hollenbeak CS, Cox MJ,
et al. Outcome and attributable cost of ventilator-associated pneumo-
nia among intensive care unit patients in a suburban medical center.
Crit Care Med 2003;31:1312-7.
4. Centers for Disease Control and Prevention. Guidelines for prevent-
ing healthcare-associated pneumonia, 2003: recommendations of
CDC and the Healthcare Infection Control Practices Advisory Com-
mittee (HICPAC). MMWR Morb Mortal Wkly Rep 2004;53:1-36.
5. Ucxkay I, Ahmed QA, Sax H, Pittet D. Ventilator-associated pneumonia
as a quality indicator for patient safety? Clin Infect Dis 2008;46:557-63.
6. Apisarnthanarak A, Pinitchai U, Thongphubeth K, Yuekyen C, Warren
DK, Zack JE, et al. Effectiveness of an educational program to reduce
ventilator-associated pneumonia in a tertiary care center in Thailand: a
4-year study. Clin Infect Dis 2007;45:704-11.
7. Youngquist P, Carroll M, Farber M, Macy D, Madrid P, Ronning J, et al.
Implementing a ventilator bundle in a community hospital. Jt Comm
J Qual Patient Saf 2007;33:219-25.
8. Babcock HM, Zack JE, Garrison T, Trovillion E, Jones M, Fraser VJ,
et al. An educational intervention to reduce ventilator-associated
pneumonia in an integrated health system: a comparison of effects.
Chest 2004;125:2224-31.
9. Dodek P, Keenan S, Cook D, Heyland D, Jacka M, Hand L, et al. the
Canadian Critical Care Trials Group; Canadian Critical Care Society.
Evidence-based clinical practice guideline for the prevention of venti-
lator-associated pneumonia. Ann Intern Med 2004;141:305-13.
10. Garner JS, Jarvis WR, Emori TB, Horan TC, Hughes JM. CDC defini-
tions for nosocomial infections. Am J Infect Control 1988;6:128-40.
11. Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented re-
gression analysis of interrupted time series studies in medication
use research. J Clin Pharm Ther 2002;27:299-309.
12. Edmond MB. Getting to zero: is it safe? Infect Control Hosp Epidemiol
2009;30:74-6.
13. Coffin SE, Klompas M, Classen D, Arias KM, Podgorny K, Anderson
DJ, et al. Strategies to prevent ventilator-associated pneumonia in
www.ajicjournal.orgVol. 37 No. 8
Marra et al. 625
acute care hospitals. Infect Control Hosp Epidemiol 2008;29:
S31-S40.
14. Assanasen S, Edmond MB, Bearman G. Impact of 2 different levels of
performance feedback on compliance with infection control process
measures in 2 intensive care units. Am J Infect Control 2008;36:
407-13.
15. Bouza E, Jesus Perez M, Munoz P, Rincon C, Barrio JM, Hortal J. Con-
tinuous aspiration of subglottic secretions (CASS) in the prevention of
ventilator-associated pneumonia in the postoperative period of major
heart surgery. Chest 2008;134:938-46.
16. Valles J, Artigas A, Rello J, Bonsoms N, Fontanals D, Blanch L, et al.
Continuous aspiration of subglottic secretions in preventing ventila-
tor-associated pneumonia. Ann Intern Med 1995;122:179-86.
17. Kollef MH, Skubas NJ, Sundt TM. A randomized clinical trial of contin-
uous aspiration of subglottic secretions in cardiac surgery patients.
Chest 1999;116:1339-46.
18. Tantipong H, Morkchareonpong C, Jaiyindee S, Thamlikitkul V. Ran-
domized controlled trial and meta-analysis of oral decontamination
with 2% chlorhexidine solution for the prevention of ventilator-
associated pneumonia. Infect Control Hosp Epidemiol 2008;29:131-6.
19. Chlebicki MP, Safdar N. Topical chlorhexidine for prevention of venti-
lator-associated pneumonia: a meta-analysis. Crit Care Med 2007;35:
595-602.
20. Koeman M, van der Ven AJ, Hak E, Joore JC, Kaasjager HA, de Smet
AM, et al. Oral decontamination with chlorhexidine reduces the inci-
dence of ventilator-associated pneumonia. Am J Respir Crit Care Med
2006;173:1348-55.
21. Klompas M, Platt R. Ventilator-associated pneumonia: the wrong
quality measure for benchmarking. Ann Intern Med 2007;147:803-5.
22. Klompas M, Kulldorff M, Platt R. Risk of misleading ventilator-
associated pneumonia rates with use of standard clinical and
microbiological criteria. Clin Infect Dis 2008;46:1443-6.