Mutational spectrum of COH1 and clinical heterogeneity in Cohen syndrome
-
Upload
independent -
Category
Documents
-
view
4 -
download
0
Transcript of Mutational spectrum of COH1 and clinical heterogeneity in Cohen syndrome
ELECTRONIC LETTER
Mutational spectrum of COH1 and clinical heterogeneity inCohen syndromeW Seifert, M Holder-Espinasse, S Spranger, M Hoeltzenbein, E Rossier, H Dollfus, D Lacombe,A Verloes, K H Chrzanowska, G H B Maegawa, D Chitayat, D Kotzot, D Huhle, P Meinecke,B Albrecht, I Mathijssen, B Leheup, K Raile, H C Hennies, D Horn. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
J Med Genet 2006;43:e22 (http://www.jmedgenet.com/cgi/content/full/43/5/e22). doi: 10.1136/jmg.2005.039867
Cohen syndrome (CS) is an autosomal recessive disorderwith variability in the clinical manifestations, characterised bymental retardation, postnatal microcephaly, facial dys-morphism, pigmentary retinopathy, myopia, and intermittentneutropenia. Mutations in the gene COH1 have been foundin an ethnically diverse series of patients. Brief clinicaldescriptions of 24 patients with CS are provided. The patientswere from 16 families of different ethnic backgrounds andbetween 2.5 and 60 years of age at assessment. DNAsamples from all patients were analysed for mutations inCOH1 by direct sequencing. Splice site mutations werecharacterised using reverse transcriptase PCR analysis fromtotal RNA samples. In this series, we detected 25 differentCOH1 mutations; 19 of these were novel, including 9nonsense mutations, 8 frameshift mutations, 4 verified splicesite mutations, 3 larger in frame deletions, and 1 missensemutation. We observed marked variability of developmentaland growth parameters. The typical facial gestalt was seen in23/24 patients. Early onset progressive myopia was presentin all the patients older than 5 years. Widespread pigmen-tary retinopathy was found in 12/14 patients assessed over5 years of age. We present evidence for extended allelicheterogeneity of CS, with the vast majority of mutationsleading to premature termination codons in COH1. Our dataconfirm the broad clinical spectrum of CS with some patientslacking even the characteristic facial gestalt and pigmentaryretinopathy at school age.
Cohen syndrome (CS; MIM #216550) is an uncommonautosomal recessive disorder with variability in theclinical manifestations including psychomotor retarda-
tion, microcephaly, typical facial dysmorphism, progressivepigmentary retinopathy appearing at mid-childhood, earlyonset and severe myopia, and intermittent neutropenia.1–4
The characteristic craniofacial appearance includes down-wards slanting and wave shaped palpebral fissures, shortphiltrum, heavy eyebrows, thick hair, and prominent nasalbase. Finnish patients present with a homogeneous pheno-type as result of a specific allele. However, a broad clinicalspectrum in non-Finnish cases and the age dependentappearance of some clinical signs may contribute to a delayin making the diagnosis.
Recently, the CS phenotype was found to be associatedwith mutations in the gene COH1 in different populations.5–8
COH1 maps to chromosome 8q22 and codes for various spliceforms. It comprises up to 62 exons and its longest transcriptis 14 093 nucleotides in length with an open reading frame of4022 codons.5 COH1 encodes a potential transmembraneprotein presumably involved in vesicle mediated sorting and
intracellular protein transport.5 9 10 The mouse homologue ofCOH1 is widely expressed in neurones of the postnatal andadult brain suggesting a role in neuronal differentiation.8
This suggests that COH1 primarily has a function inpostmitotic cells, which may be the reason for the postnatalmicrocephaly seen in CS.8
Overall, more than 50 COH1 mutations have been reportedin association with CS. Most are termination mutations andpredicted to result in a null allele, while missense mutationsand larger deletions are less common.
To determine the variability of the clinical manifestationsand the spectrum of mutations associated with this conditionwe investigated 24 patients with CS from 16 families, with awide range of geographical and ethnic origins.
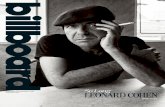
METHODSPatientsThis study included 24 patients from 16 families (17 maleand 7 female patients, ranging in age from 2.5 to 60 years).The diagnosis of CS was based on clinical manifestationsincluding developmental delay/mental retardation and atleast two of three criteria: typical facial gestalt (fig 1),pigmentary retinopathy or myopia, and neutropenia (table 1).There were 12 non-consanguineous families, comprisingthree French families (one with two affected children andtwo with one affected child each), three German families(two with one affected child and one with five affected malemembers), one Turkish family (one affected child), oneBelgian family (one affected child), one family of English andGerman origin (one affected child), one Canadian familyfrom English/Scottish descent (one affected child), and twoPolish families (with one and two affected children,respectively). The four consanguineous families reportedwere all Turkish (two with affected sibling pairs and twowith one affected child each).
Clinical assessments were carried out on all patients by atleast one of us. Blood samples were collected from theparents and from affected and unaffected siblings. Signedinformed consents were obtained from the parents of theaffected and unaffected children.
Mutation analysisGenomic DNA was isolated from peripheral blood usingstandard techniques. For mutation screening, 62 exons andfive potential alternative exons including their flanking splicesites, and the predicted promoter region of COH1 wereanalysed. Primer pairs for genomic amplification weregenerated on the basis of the sequence of a chromosome 8genomic contig (GenBank accession numberNT_008046.15).7 All primer sequences are available on
Abbreviations: CS, Cohen syndrome
1 of 6
www.jmedgenet.com
request. PCR products were purified using exonuclease I andshrimp alkaline phosphatase, and then sequenced directlywith a commercial kit (BigDye Terminator cycle sequencingkit, version 1.1, Applied Biosystems) and analysed on anautomated DNA analyser (model 3730; Applied Biosystems).
RT analysisTotal RNA was extracted from peripheral blood, and reversetranscription (RT) perfomed using commercial kits (PAXgeneblood RNA validation kit, PreAnalytiX and Omniscript RT kit,Qiagen). Primer pairs for cDNA amplification were designedfrom the sequence of the full length COH1 transcript(GenBank accession number NM_017890.3). Analysis ofPCR products was performed by purifying single bands fromagarose gel using a gel extraction kit (QIAquick; Qiagen), andsequenced directly as described above.
RESULTSClinical dataIn our series of 24 patients with CS from 16 families, weobserved marked variability of developmental and growthparameters (table 1). At the time of assessment, short stature(height at or below the third centile) was present in 16 of 24cases. Postnatal microcephaly was found in 20 of 24 patients.Truncal obesity was documented in the majority of patientsanalysed (17/24). Mental retardation and intellectual impair-ment varied from moderate to severe. All but one of thepatients (patient 2-2) learned to walk independently. Themajority of patients achieved verbal communication skillsand most used short sentences at mid-childhood. However,two adult patients (2-2 and 2-3) and two 5 year old patients(14-1 and 15-2) were non-verbal. Stereotypic movementswere seen in patients 5 and 15-2.
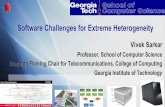
Typical craniofacial features were seen in 23/24 patients(fig 1). Patient 6, who presented with everted lips, bulbousnasal tip, and normal appearing philtrum, lacked the facialgestalt characteristic of CS (fig 2). The affected siblings of
family 2 were 44 and 60 years old at assessment and bothhad the characteristic facial features of CS including shortphiltrum and downwards slanting palpebral fissure.
Progressive visual disability was a consistent finding. Anearly onset of progressive myopia with refractive errorsranging from 20.3 to 28 dioptres was evident in all thepatients older than 5 years. Patient 8-2 was too young toassess this clinical sign. Retinal examination had beenperformed on all study patients. All but two of the patientsolder than 5 years had widespread pigmentary retinopathywith vessel attenuation and optic pallor. Two siblings (13-1and 13-2) had normal retinal examinations at the ages of16.5 and 14.5 years. Electrodiagnostic tests have not beencarried out on these two patients but functional impairmentsuch as nyctalopia was not recorded. Six patients between 3.5and 5 years of age had normal retinas on ophthalmologicalexamination. The adult patients assessed by us showedprogressive ophthalmological changes. Severe retinochoroidalatrophy, generalised bone spiculae-like pigment accumula-tions, cataracts, and optic nerve pallor were found in twoaffected brothers aged 53 and 44 years (2-4 and 2-5,respectively). The ophthalmological abnormalities led to totalblindness in mid-adulthood in patients 2-1 and 2-5.
Narrow hands and feet were found in all patients.Progressive kyphoscoliosis developed after the age of 40 yearsin patients 2-4 and 2-5 but was also present in an affectedteenager (patient 6). Neutropenia defined as a neutrophilcount ,1.56109/l was shown in the majority of patientsanalysed for that clinical sign (14/16 patients).
Hypogonadotropic hypogonadism, severe and completegrowth hormone deficiency, insulin resistance, and compen-satory hyperinsulinemia were found in patient 10.
Molecular analysisWe analysed all 24 patients by direct genomic sequencing ofthe whole coding region including the exon splice sites andthe promoter region. In the full length transcript of COH1, we
Figure 1 Typical facial features of patients with CS. Shown are patients 8-1 (A), 8-2 (B), 11 (C), 7 (D), 9 (E), 15-1 (F), 2-5 (G), and 2-4 (H). Signedinformed consents were obtained from the parents of the affected children and guardians of affected adults for publication of the images.
2 of 6 Seifert, Holder-Espinasse, Spranger, et al
www.jmedgenet.com
Table
1Su
mm
ary
ofth
ecl
inic
alfin
ding
sin
24
patie
nts
with
CS
from
16
fam
ilies
Patie
ntO
rigin
Con
san-
gui
nity
Sex
Age
at
ass
essm
ent
(yea
rs)
Mic
ro-
cepha
lySh
ort
statu
reTr
unca
lob
esity
Age
first
walk
edSp
eech
dev
elop
men
tTy
pic
al
faci
esM
yopia
(dio
ptr
es)
PR
Narr
owha
nds
/fee
tN
eutr
o-pen
iaM
isce
llane
ous
1G
erm
an/
Engl
ish
2M
5+
22
3ye
ars
Sent
ence
s+
20.3
2+
+
2-1
Ger
man
2M
60
22
+C
hild
hood
Sent
ence
s+
++
+N
ATo
talb
lindn
ess
2-2
Ger
man
2M
44*
22
+N
ow
alki
ngN
osp
eech
+N
AN
A+
NA
2-3
Ger
man
2M
56
2+
2C
hild
hood
No
spee
ch+
NA
NA
+N
A2-4
Ger
man
2M
53
++
+C
hild
hood
Sing
lew
ords
++
(.2
7)
++
+C
atar
acts
,ky
phos
colio
sis
2-5
Ger
man
2M
44
++
2C
hild
hood
Sent
ence
s+
+(.
27)
++
+C
atar
acts
,to
talb
lindn
ess,
kyph
osco
liosi
s3
Engl
ish/
Scot
tish
2F
9+
+2
2.5
year
sSe
nten
ces
++
++
+Ju
veni
lerh
eum
atoi
dar
thri
tis,
infla
mm
ator
ybo
wel
dise
ase
4Tu
rkis
h2
M5.5
++
22
year
sSe
nten
ces
+2
5+
++
5Po
lish
2F
5+
2+
2ye
ars
Sing
lew
ords
+2
3+
++
Ster
eoty
pic
mov
emen
ts6
Fren
ch2
M17
++
+22
mon
ths
Sent
ence
s2
24
++
2Sc
olio
sis
7Be
lgia
n2
F15
++
+D
elay
edD
elay
ed+
++
++
Aut
istic
feat
ures
8-1
Fren
ch2
M7
++
+D
elay
edD
elay
ed+
++
++
8-2
Fren
ch2
M3.5
++
+D
elay
edD
elay
ed+
22
++
9Fr
ench
2F
16.5
++
+D
elay
edD
elay
ed+
++
++
10
Ger
man
2M
15.5
++
+5.5
year
sSi
ngle
wor
ds+
++
++
Hyp
ogon
adis
m,
grow
thho
rmon
ede
ficie
ncy
11
Ger
man
2M
11.5
++
+D
elay
edSe
nten
ces
+2
8+
++
Ster
eoty
pic
mov
emen
ts12
Turk
ish
+M
28
++
+12
mon
ths
Sent
ence
s+
210/2
7+
+2
13-1
Turk
ish
+F
16.5
++
+16
mon
ths
Sing
lew
ords
+2
52
+N
A13-2
Turk
ish
+M
14.5
++
+13
mon
ths
Sing
lew
ords
+2
42
+N
A14-1�
Polis
h2
M5
+2
+20
mon
ths
No
spee
ch+
23.5
/22.5
2+
+14-2�
Polis
h2
M3
+2
+3
year
sSi
ngle
wor
ds+
26.5
/24.0
2+
+15-1
Turk
ish
+F
82
++
2ye
ars
Sent
ence
s+
+2`
+N
A15-2
Turk
ish
+F
5+
22
2ye
ars
No
spee
ch+
26
2+
NA
Uni
late
ralp
tosi
s,st
ereo
typi
cm
ovem
ents
16
Turk
ish
+M
2.5
+2
22.5
year
sSi
ngle
wor
dsat
2.5
year
s+
NA
NA
+N
A
*Die
ddu
eto
ileus
atag
eof
44
year
s;�t
hese
patie
nts
wer
ere
port
edas
fam
ily8
byH
enni
eset
al7bu
tonl
yon
em
utat
ion
had
been
iden
tifie
dat
that
time;
`las
tret
inal
exam
inat
ion
atag
eof
4ye
ars.
PR,p
igm
enta
ryre
tinop
athy
;.N
A,n
otav
aila
ble.
Mutational spectrum of COH1 and clinical heterogeneity in Cohen syndrome 3 of 6
www.jmedgenet.com
identified 25 different mutations; 19 of these were novel,including 9 nonsense mutations, 8 frameshift mutations, 4verified splice site mutations, 3 larger in frame deletions, and1 missense mutation identified in two unrelated families. Themutations identified are summarised in table 2. Eachmutation cosegregated in the respective family in all casesand was not seen in 150 chromosomes from control subjects.
Heterozygous mutation c.1563GRA identified in family 1affected the last base pair of exon 11 (table 2). To analysewhether the mutation caused an altered splicing of COH1, weperformed RT-PCR on a total RNA sample from peripheral
blood of patient 1. Amplified cDNA with primers located inexons 8 and 16 showed the regularly processed product in avery low level. Amplification with primers placed in exon 8and intron 11 resulted in a mutant cDNA fragment.Sequencing demonstrated an abnormal transcript includingmore than 177 bp of the intron 11, resulting in a new readingframe of 19 codons followed by a stop codon in intron 11.
In family 9, we identified a heterozygous mutation,c.7322_7322+1delGGinsATGGAGC (table 2), at the splicedonor site. RNA analysis with primers located in exons 39and 45 and in exon 39 and intron 40, respectively, showedlack of splicing with an altered codon 2441, followed by 35novel codons and a stop codon. A heterozygous splice donorsite mutation c.2934+1_2934+2delGT was identified in family11 (table 2). We identified complete skipping of exon 20 withprimers located in exons 19 and 24. Consequently, the alteredtranscript lacked 110 nucleotides. Mutation c.6732+1GRA,first reported by Kohlemainen et al,6 changed the splice donorsite of intron 37 (family 3; table 2). Total RNA from theaffected individual analysed with primers located in exons 35and 39 revealed a cryptic splice site in intron 37. The defectivesplicing leads to an addition of four bases into the COH1transcript. The sequence of the cryptic splice site (GTGGGT)is consistent with the consensus motif (GURAGU) at five ofsix positions, including the highly conserved dinucleotide GTat the beginning.
DISCUSSIONIn this paper, we report the clinical and molecular data on 24individuals with CS, from 16 families, caused by mutations inCOH1. Overall, 11 compound heterozygous cases, 4 homo-zygous cases with known consanguinity, and 1 homozygouscase with unknown consanguinity were observed. In onepatient (family 10), only one heterozygous mutation wasdetected. This patient was also assumed to be compoundheterozygous. The lack of a second pathogenic mutationpoints to the existence of further alternative exons and/orother transcripts of COH1.5 7 11 Alternatively, further muta-tions could reside within intronic sequences, which were
Figure 2 Facial dysmorphism differs in patient 6 by the presence ofeverted lips, bulbous nasal tip, and a normal philtrum. Signed informedconsent was obtained from the parents of the patient for publication ofthe image.
Table 2 Summary of mutations in COH1 identified in this study
Nucleotide exchange ExonAmino acid change/predicted consequence Genotype Family
c.1504CRT 11* p.Arg502X Heterozygous 3c.1563GRA 11 p.Lys521fsX20 Heterozygous 1c.2074CRT 15� p.Arg692X Heterozygous 8c.2516_4299del 18–28 p.Gly839fsX19 Heterozygous 14c.2727_2730dupGCTC 19* p.Asn911fsX3 Heterozygous 14c.2934+1_2934+2delGT 20 p.Gly942fsX14 Heterozygous 11c.2516_3083del 18–21 p.Gly839_Thr1027del Heterozygous 11c.4877_4879dupAAT 31 p.Tyr1627X Homozygous 12c.4923GRA 31 p.Trp1641X Heterozygous 2c.4955CRG 31 p.Ser1652X Heterozygous 2c.5152_5295del 33 p.Glu1718_Glu1765del Heterozygous 5c.5215_5232delAGTGTGGCTCAAGTTCAA 33 p.Ser1739_Gln1744del Heterozygous 10c.5426_5427dupAG 34� p.Gln1810fsX21 Heterozygous 8c.5461_5462insC 34 p.Arg1821fsX18 Heterozygous 6c.5920CRT 34 p.Arg1974X Heterozygous 5c.6732+1GRA 37` p.Val2245fsX17 Heterozygous 3c.7322_7322+1delGGinsATGGAGC 40 p.Ser2441fsX37 Heterozygous 9c.7153GRT 40 p.Glu2384X Heterozygous 9c.8292CRA 45 p.Cys2764X Homozygous 13c.8318CRT 45 p.Ser2773Leu Homozygous 15, 16c.10456_10457delAG 56 p.Leu3487fsX25 Homozygous 7c.11245GRT 58 p.Glu3749X Heterozygous 4c.11564_11565delAT 60 p.Tyr3855fsX30 Heterozygous 4c.11780delC + c.11783TGRAA 61 p.Thr3927fsX15 Heterozygous 1c.11907dupC 62` p.Ser3970fsX22 Heterozygous 6
*Mutation reported by Hennies et al;7 �Mutation reported by Kolehmainen et al;5 `Mutation reported byKolehmainen et al.6
4 of 6 Seifert, Holder-Espinasse, Spranger, et al
www.jmedgenet.com
analysed only at the conserved splice sites, or could representlarger deletions.
In total, we identified 25 different mutations, of which 19were novel (table 2). Most of the patients described herecarried mutations resulting in premature termination codons.This is consistent with previously reported cases. In total, 61of the 73 mutations in COH1 published to date resulted inpremature termination through frameshift or nonsensemutations,5–8 12 13 and six mutations are larger in framedeletions. Thus, the pathogenic implications of missensemutations associated with CS (6 of 73), identified only in twoof our cases, have still to be clarified. Several coding SNPsfound indicate that the COH1 product appears to have sometolerance to such variations (table 3).
Nearly all mutations except for those found in Finnishpatients5 6 were seen only once or in a few families. Fournovel splice site mutations (families 1, 3, 9, and 11) wereconfirmed on RNA analysis. The splice site mutationc.1563GRA (family 1) resulted in intron retention and anaberrant stop codon. The second splice site mutation,c.7322_7322+1delGGinsATGGAGC (family 9), led to intronretention with an aberrant stop after 2477 residues. Thesplice site mutation found in family 11(c.2934+1_2934+2delGT) resulted in exon skipping. Thefourth splice mutation, c.6732+1GRA (family 3), resultedin activation of a cryptic 59 splice site within the intronicsequence and a subsequent frameshift.
Our data help in defining the phenotypic spectrum of CS.Consistent with previously reported cases of CS,7 8 12 13 thepatients reported by us demonstrate an obviously broadphenotypic variability, in contrast to the patients withapparent founder mutations, who have a fairly homogeneousphenotype. Thus, COH1 mutations may be present in patientswith CS lacking either microcephaly or truncal obesity. Themajority of patients in our study showed short stature. Mostpatients reported by us (21/24) had moderate mentalretardation. Three patients were classified as having pro-found mental retardation with complete lack of speech, andone adult patient could not walk.
In previous studies early onset of high myopia andpigmentary retinopathy have been a hallmark of CS.14 15 Inall our patients older than 5 years, the severity of myopia wascomparable to that reported earlier.14 15 Pigmentary retino-pathy was not confirmed by retinal examination in twopatients who were teenagers at the time of assessmentsalthough these patients did not undergo electrodiagnostictesting. Thus, retinopathy present at school age may not to beobligatory for the diagnosis of CS.
Despite some variability in the facial appearance in CS,craniofacial abnormalities including wave shaped palpebralfissures and short philtrum were seen in almost all patientsand in different ethnic backgrounds.5–7 12 However, the facialdysmorphism may be subtle, which can lead to delay indiagnosis.12 In our opinion, despite mild hypertelorism, thefacial appearance of one patient reported by Falk et al12 (givenas sketch drawing in that report) is consistent with thetypical facial features of CS. One patient in this study (patient6) had facial features not typical of CS, including everted lips,bulbous nasal tip, and normal philtrum (fig 2). Therefore, thediagnosis of CS cannot be ruled out in the absence ofcharacteristic facial features.
Although no significant endocrinal abnormalities werefound in Finnish patients on the examination of pituitaryfunction,4 one of our patients, of German origin, showedgrowth hormone deficiency and hypogonadotropic hypo-gonadism.
Long term follow up and clinical information on patientsolder than 40 years are rare in the literature.3 Our patientsbetween 44 and 60 years of age show that the featurescharacteristic of CS remain in older patients, and can be usedin making the diagnosis even at that age. Total blindnessfound in two adult patients reported here contrasts with theFinnish group of CS patients, in whom marked deteriorationof visual function occurred over the age of 50 years, but nopatient was reported to be completely blind.3 However, onethird of CS patients from Britain were registered with severevisual impairment or blindness.16
Kyphoscoliosis was seen in three of our patients asteenagers or adults and this tends to be progressive throughadult life. As CS patients do not have life threateningdisorders and are generally in good health, their life spandoes not seem to be markedly reduced.
The detailed clinical information and the results of themolecular analysis of COH1 on patients with CS presentedhere enabled us to provide evidence of extended allelicheterogeneity as well as to obtain further informationregarding the clinical findings, particularly the facial features,in patients of different ethnic backgrounds.
ACKNOWLEGDEMENTSWe thank all patients and their families for their collaboration. Thiswork was supported by a grant from the DeutscheForschungsgemeinschaft to H C Hennies and D Horn.
Authors’ affiliations. . . . . . . . . . . . . . . . . . . . .
W Seifert, H C Hennies, Cologne Center for Genomics, Universitat zuKoln, Koln, GermanyW Seifert, Faculty of Biology, Chemistry, and Pharmacy, Free Universityof Berlin, GermanyM Holder-Espinasse, Hopital Jeanne de Flandre, Genetique medicale,CHRU, Lille, FranceS Spranger, Praxis fur Humangenetik, Bremen, GermanyM Hoeltzenbein, Max Planck Institute for Molecular Genetics, Berlin,GermanyE Rossier, Department of Human Genetics, University of Ulm, GermanyH Dollfus, Centre de Reference pour les Affections GenetiqueOphtalmologiques, Service de Genetique Medicale, HopitauxUniversitaires de Strasbourg, Strasbourg, France
Table 3 Overview of all single nucleotidepolymorphisms and CS associated missense mutations inthe coding region of COH1
ExonNucleotideexchange
Alternativeresidues Source
Synonymous polymorphisms25 c.3855ARG p.Leu1248Leu rs169739139 c.7038ARG p.Val2346Val This study40 c.7227GRA p.Pro2409Pro This study52 c.9566TRC p.Ser3189Ser This study56 c.10140GRT p.Ala3380Ala This study57 c.10980TRC p.Pro3660Pro This study61 c.11640ARG p.Ser3880Ser rs7844645Non-synonymous polymorphisms17 c.2485GRA p.Ala829Thr This study18 c.2596GRA p.Val866Ile This study34 c.5980ARG p.Ile1994Val This study42 c.7751TRC p.Val2548Ala rs783387046 c.8465ARG p.Tyr2822Cys This study50 c.9098CRA p.Ala3033Glu rs699205952 c.9424ARG p.Ser3142Arg This study56 c.10294GRA p.Gly3432Arg rs6468694Potentially pathogenic missense mutations37 c.6578TRG p.Leu2193Arg Kolehmainen et al.5
39 c.7022ARG p.Tyr2341Cys Hennies et al.7
43 c.7934GRA p.Gly2645Asp Mochida et al.8
45 c.8318CRT p.Ser2773Leu This study46 c.8459TRC p.Ile2820Thr Falk et al.12
49 c.8978ARG p.Asn2993Ser Kolehmainen et al.6
Mutational spectrum of COH1 and clinical heterogeneity in Cohen syndrome 5 of 6
www.jmedgenet.com
D Lacombe, Service de Genetique Medicale, Hopital Pellegrin-Enfants,Bordeaux, FranceA Verloes, Unit of Clinical Genetics, Hopital Robert Debre and INSERMU676, Paris, FranceK H Chrzanowska, Department of Medical Genetics, Children’sMemorial Health Institute, Warsaw, PolandG H B Maegawa, D Chitayat, Department of Pediatrics, Division ofClinical and Metabolic Genetics, The Hospital for Sick Children,University of Toronto, Toronto, Ontario, CanadaD Kotzot, Division of Clinical Genetics, Department of Medical Genetics,Molecular and Clinical Pharmacology, Medical University of Innsbruck,AustriaD Huhle, Praxis fur humangenetische Beratung und Diagnostik, Wetzlar,GermanyP Meinecke, Altonaer Kinderkrankenhaus, Hamburg, GermanyB Albrecht, Institut fur Humangenetik, Universitat Essen, Essen, GermanyI Mathijssen, Academic Medical Centre, University of Amsterdam,Amsterdam, The NetherlandsB Leheup, Hopital de Brabois, Service de Genetique, Nancy, FranceK Raile, Department of Pediatric Endocrinology, University of Leipzig,Leipzig, GermanyD Horn, Institute of Medical Genetics, Charite, University Medicine ofBerlin, Germany
Competing interests: there are no competing interests.
Signed informed consents were obtained from the parents of the affectedand unaffected children and guardians of affected adults. The study wasapproved by the local ethics committee.
Correspondence to: Dr H C Hennies, Cologne Center for Genomics,University of Cologne, Zulpicher Str. 47, 50674 Koln, Germany;[email protected]
Received 28 November 2005Revised version received 25 January 2006Accepted for publication 25 January 2006
REFERENCES1 Cohen MM Jr, Hall BD, Smith DW, Graham CB, Lampert KJ. A new syndrome
with hypotonia, obesity, mental deficiency, and facial, oral, ocular, and limbanomalies. J Pediatr 1973;83:280–4.
2 Norio R, Raitta C, Lindahl E. Further delineation of the Cohen syndrome;report on chorioretinal dystrophy, leukopenia and consanguinity. Clin Genet1984;25:1–14.
3 Kivitie-Kallio S, Norio R. Cohen syndrome: essential features, natural history,and heterogeneity. Am J Med Genet 2001;102:125–35.
4 Kivitie-Kallio S, Eronen M, Lipsanen-Nyman M, Marttinen E, Norio R. Cohensyndrome: evaluation of its cardiac, endocrine and radiological features. ClinGenet 1999;56:41–50.
5 Kolehmainen J, Black GC, Saarinen A, Chandler K, Clayton-Smith J,Traskelin AL, Perveen R, Kivitie-Kallio S, Norio R, Warburg M, Fryns JP, de laChapelle A, Lehesjoki AE. Cohen syndrome is caused by mutations in a novelgene, COH1, encoding a transmembrane protein with a presumed role invesicle-mediated sorting and intracellular protein transport. Am J Hum Genet2003;72:1359–69.
6 Kolehmainen J, Wilkinson R, Lehesjoki AE, Chandler K, Kivitie-Kallio S,Clayton-Smith J, Traskelin AL, Waris L, Saarinen A, Khan J, Gross-Tsur V,Traboulsi EI, Warburg M, Fryns JP, Norio R, Black GC, Manson FD.Delineation of Cohen syndrome following a large-scale genotype-phenotypescreen. Am J Hum Genet 2004;75:122–7.
7 Hennies HC, Rauch A, Seifert W, Schumi C, Moser E, Al-Taji E, Tariverdian G,Chrzanowska KH, Krajewska-Walasek M, Rajab A, Giugliani R, Neumann TE,Eckl KM, Karbasiyan M, Reis A, Horn D. Allelic heterogeneity in the COH1gene explains clinical variability in Cohen syndrome. Am J Hum Genet2004;75:138–45.
8 Mochida GH, Rajab A, Eyaid W, Lu A, Al-Nouri D, Kosaki K, Noruzinia M,Sarda P, Ishihara J, Bodell A, Apse K, Walsh CA. Broader geographicalspectrum of Cohen syndrome due to COH1 mutations. J Med Genet2004;41:e87.
9 Redding K, Brickner JH, Marschall LG, Nichols JW, Fuller RS. Allele-specificsuppression of a defective trans-Golgi network (TGN) localization signal inKex2p identifies three genes involved in localization of TGN transmembraneproteins. Mol Cell Biol 1996;16:6208–17.
10 Brickner JH, Fuller RS. SOI1 encodes a novel, conserved protein that promotesTGN-endosomal cycling of Kex2p and other membrane proteins bymodulating the function of two TGN localization signals. J Cell Biol1997;139:23–36.
11 Velayos-Baeza A, Vettori A, Copley RR, Dobson-Stone C,Monaco AP. Analysis of the human VPS13 gene family. Genomics2004;84:536–49.
12 Falk MJ, Feiler HS, Neilson DE, Maxwell K, Lee JV, Segall SK, Robin NH,Wilhelmsen KC, Traskelin AL, Kolehmainen J, Lehesjoki AE, Wiznitzer M,Warman ML. Cohen syndrome in the Ohio Amish. Am J Med Genet A2004;128:23–8.
13 Kondo I, Shimizu A, Asakawa S. COH1 analysis and linkagestudy in two Japanese families with Cohen Syndrome. Clin Genet2005;67:270–2.
14 Summanen P, Kivitie-Kallio S, Norio R, Raitta C, Kivela T. Mechanisms ofmyopia in Cohen syndrome mapped to chromosome 8q22. Invest OphthalmolVis Sci 2002;43:1686–93.
15 Chandler KE, Biswas S, Lloyd IC, et al. The ophthalmic findings in Cohensyndrome. Br J Ophthalmol 2002;86:1395–8.
16 Chandler KE, Kidd A, Al-Gazali L, Kolehmainen J, Lehesjoki AE,Black GC, Clayton-Smith J. Diagnostic criteria, clinicalcharacteristics, and natural history of Cohen syndrome. J Med Genet2003;40:233–41.
6 of 6 Seifert, Holder-Espinasse, Spranger, et al
www.jmedgenet.com