Molecular Markers of Breast Cancer Cells Identified in Fine Needle Aspiration Samples from Resected...
-
Upload
independent -
Category
Documents
-
view
1 -
download
0
Transcript of Molecular Markers of Breast Cancer Cells Identified in Fine Needle Aspiration Samples from Resected...
Objective
To analyze a procedure for breast cancer that requires per-formance of a molecular test before extensive intraoperativeexamination, fine needle aspiration cytology (FNAC) ofsurgically removed sentinel lymph nodes (SLNs).
Study Design
The diagnostic accuracy of ex-tensive histologic examinationand immunohistochemistry(IHC) of 101 SLNs from 98breast carcinoma patients werecompared with that of theevaluation of 2 specific mRNAmarkers by reverse transcrip-tase polymerase change reac-tion (mammaglobin andMUC-1). Cell specimens wereobtained by FNAC of the SLNs immediately before freez-ing.
Results
Metastases were detected on frozen sections in 19 cases(18.81%). IHC on serial sections confirmed the metastasesand showed micrometastases or isolated tumor cells in 24
SLNs (23.76%). Mammaglobin was expressed in 20FNAC specimens (19.80%). MUC-1 assay was positive in11 cases only (10.89%).
Conclusion
This technique allows a complete histologic examinationwithout sacrifice of part of theSLN and at the same time is avaluable diagnostic adjunct tothe detection of occult tumorcells. Moreover, it is less ex-pensive and time consumingthan extensive IHC. (ActaCytol 2006;50:271–276)
Keywords: breast cancer;sentinel lymph node biop-sy; aspiration biopsy, fine-
needle; polymerase chain reaction.
Sentinel lymph node (SLN) biopsy represents a newstandard of care for patients with clinically lymph
node negative breast cancer. Many institutions havecompleted their validation trials for this procedureand offer SLN biopsy alone, with no further axillary
This technique allows a completehistologic examination withoutsacrificing part of the SLN and
simultaneously provides avaluable diagnostic adjunct for
the detection of occult tumor cells.
From the Department of Pathology and Laboratory Medicine, Policlinico Multimedica, Milan, Italy.
Drs. Cannone and Rispoli are Molecular Biologists.
Dr. Oliveri is Biologist.
Drs. Roz, Ferrarese and Alexiadis are Assistant Pathologists.
Dr. Barberis is Director.
Address correspondence to: Massimo C. P. Barberis, M.D., Department of Pathology and Laboratory Medicine, Policlinico Multimedica, ViaFantoli 16/15, 20138 Milan, Italy ([email protected]).
Financial Disclosure: The authors have no connection to any companies or products mentioned in this article.
Received for publication February 6, 2005.
Accepted for publication July 19, 2005.
0001-5547/06/5003-0271/$19.00/0 © The International Academy of Cytology ACTA CYTOLOGICA 271
Molecular Markers of Breast Cancer CellsIdentified in Fine Needle Aspiration Samplesfrom Resected Sentinel Lymph Nodes
Maria Cannone, Sc.D., Claudio Oliveri, Sc.D., Elena Roz, M.D., Francesca Rispoli,Sc.D., Stefania Ferrarese, M.D., Spyridon Alexiadis, M.D., and Massimo C. P. Bar-beris, M.D.
MOLECULAR TECHNIQUES
DO NOT
DUPLICA
TE
© Cop
yrigh
ted
Mat
erial
surgery for SLN-negative patients.The histologic examination of SLN may be per-
formed on permanent sections of formalin-fixed andparaffin-embedded tissue or intraoperatively on fro-zen sections. This method has the advantage of allow-
ing immediate axillary dissection and avoiding reoper-ation. However, the frozen section is subject to falsenegative results, costly and time consuming.
To avoid an unacceptably high number of false neg-ative diagnoses, many institutions use the extensive in-traoperative examination of SLN proposed by Viale etal.1-3 According to these authors, the general concor-dance between the intraoperative examination ofSLNs and axillary node status is 96.7% and the truefalse negative rate 3.2%.
Many reports emphasize the role of immunohisto-chemistry (IHC) in detecting micrometastases inSLNs and have recommended performing immunore-actions for epithelial markers (cytokeratins) directlyon frozen or permanent sections.4,5 However, the useof this technique does not surmount the need for ex-tensive sectioning of the node. The costs and the timerequired for IHC are high and not sustainable formany institutions.
More sensitive, polymerase chain reaction (PCR)–based methods for the detection of metastatic cells arenow available, permitting the amplification of cancercell–specific mRNA messages by the reverse tran-scriptase (RT)–PCR assay. Even if an ideal tumormarker, consistently expressed in tumor samples andnot at all in normal and/or reactive lymph nodes, re-mains to be identified, human mammoglobin(hMMG) now represents the most specific mRNAmarker of the lymphatic spread of breast cancercells.6-8 Molecular tests are usually performed on un-fixed moieties or parts of SLNs; otherwise, when theSLN is intraoperatively examined, the discarded,trimmed tissue between the sections chosen for stain-ing can be retrieved for molecular assays. Therefore,part of the SLN is not histologically examined, and amicrometastatic focus could be missed. To overcomethis drawback, we devised a procedure for performingthe molecular test before the extensive intraoperative
examination: fine needle aspiration cytology (FNAC)of the surgically removed SLN.
In this study we compared the results obtained byintraoperative histology of SLNs with the hMMG-mRNA and mucinlike carcinoma-associated antigen(MUC1) mRNA detection by RT-PCR performed onFNAC of the same SLNs.
Materials and Methods
From January 2003 to July 2004, 98 women withbreast cancer underwent surgery for intraoperativesentinel lymph node biopsy, completion level I/II ax-illary lymphadenectomy in histologically positivecases and breast-conserving surgery. The mean agewas 57.9 years (range, 28–84).
SLNs were located by peritumoral injection of a ra-dioactive colloid (30–40 Mbq of unfiltered 99Tc sulfurcolloid in 6–8 mL) or by patent blue. Lymphoscintig-raphy was performed for patients who underwent ra-dioactive colloid injection. Intraoperative localizationof the SLNs was performed with a hand-held gammaprobe or by visualizing the blue-stained lymphaticsand lymph nodes. One hundred twenty-one SLNswere sent for pathologic evaluation.
The working tablet and the examination gloves ofthe pathologist were washed with RNAse. FNACspecimens were obtained from each lymph node usinga 25-gauge needle connected to a 10-mL syringe, im-mediately dissolved in Trizol reagent (Life Technolo-gies, Rockville, Maryland, U.S.A.) and preserved at −80°C in RNA-free tubes.
Histologic examination was performed followingthe protocol proposed by Viale et al.1-3 The perinodalfat was excised, and then the SLN was bisected alongits longitudinal axis and embedded in OCT (Bio-Optica, Milan, Italy). Sections 2–4 mm thick were cutat 100-mm intervals until the SLN was completelyand serially sectioned. Moreover, in each case, addi-tional sections were obtained at 200-mm intervals andimmunostained with anticytokeratin pool (Epos anti-cytokeratins, DakoCytomation, Glostrup, Denmark).In this way an immunostained section was positionedbetween 2 hematoxylin-eosin (HE)–stained sections.
After cell homogenization in 1 mL of Trizol, 200mL of chloroform was added to each tube; the tubeswere centrifuged at 2–8°C. The cells in aqueous phasecontaining RNA were transferred in a new tube andprecipitated with isopropyl alcohol by centrifugationat 2–8°C. RNA was pelleted with 75% ethanol by vor-texing and centrifuged under the same conditions asabove mentioned. At the end, the RNA pellet wasbriefly dried and resuspended in RNAse-free water(DEPC treated). One microgram of total RNA wasretrotranscribed with random examers with the Gene-Amp Gold RNA-PCR core kit (PE Biosystems, Foster
272
Cannone et al
ACTA CYTOLOGICA Volume 50 Number 3 May–June 2006
In selected cases [the technique]could be used in association withultrasonographically guided SLNFNA to obtain information on thepresurgical status of the axillary
lymph nodes.
DO NOT
DUPLICA
TE
© Cop
yrigh
ted
Mat
erial
City, California, U.S.A.) as described in the manufac-turer’s instructions and checked for integrity by am-plification for GAPDH using the specific primers:GAPDH forward 5´-CCACCCATGGCAAATT C CATGGCA-3´ and GAPDH reverse 5´-CTAGACGGCAGGTCAGGTCCACC-3´. The 599–base pair(bp) PCR product was analyzed on a 2% agarose gelstained with ethidium bromide.
For gene expression studies, 10% of cDNA was firstsubjected to hMMG nested PCR using specificprimers: MMG forward 5´-CAGCGGCTTCCTT-GATCCTTG-3´ and MMG reverse 5´-TAGCAGG-TTTCAACAATTGTC-3´ for outer amplificationand MMG forward 5´-AGCACTGCTACGCAGG-CTCT-3´ and MMG reverse 5´-ATAAGAAAGAGA-AGGTGTGG-3´ for inner amplification. A 329-bpPCR fragment was analyzed on a 2% agarose gelstained with ethidium bromide.
The second time, all RNA samples were evaluatedfor MUC-1 tumor marker using specific primers:MUC-1 primer forward 5´-CAGTTGTCTACTG-GGGTCTC-3´ and MUC 1 primer reverse 5´-TTCTCGGAAGGCCAGAGTCA-3´. Samples wereconsidered positive when a 248-bp fragment was visu-alized on 2% agarose gel stained with ethidium bro-mide. The reaction conditions are detailed in Table I.
The sensitivity of RT-PCR experiments was initial-ly established by performing RT-PCR analysis onRNA extracted from serial dilution of MCF-7 cellswith lymphocytes obtained from normal, controllymph nodes as previously described.9 To check thespecificity we examined 20 lymph nodes obtainedfrom patients without cancer who had undergone ab-dominal surgery. To avoid cross-contamination, RNAextraction, RT-PCR assay and analysis of the PCRfragment were carried out in separate rooms.
The stage of disease in patients with positive SLNswas reported according to the new American JointCommittee on Cancer breast cancer staging system.10
Results
The diameter of the SLNs ranged from 0.5 to 2 cm(mean, 1.2). The mean of the frozen sections obtainedwas 52, with 26 immunostains (range, 25–120 sectionsand 12–60 immunostains). Twenty SLNs (16.52%)were negative for GAPDH expression and were notconsidered in the study. Therefore, our data refer to101 SLNs.
The 20 control specimens obtained from non-can-cer patients were negative for hMMG and MUC-1 ex-pression.
Metastases were detected on frozen sections in 19cases (18.81%). In 12 of 19 cases (63.1%) they wereobserved on the first H-E–stained section.
Extensive IHC confirmed the metastases andshowed micrometastases or isolated tumor cells (ITC)in 24 SLNs (23.76%); IHC upstaged 5 SLNs (4.95%),the true false negative specimens in H-E serial sec-tions.
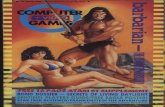
hMMG was expressed in 20 FNAC specimens(19.80%) (Figure 1). In 4 cases a positive molecularassay was confirmed by IHC that detected ITC in his-tologically negative specimens.
In one histologically negative and immunohisto-chemically positive case, tumor marker expression wasnegative. Two other cases of SLNs with mi-crometastatic foci were negative for hMMG expres-sion but immunohistochemically positive. Two SLNswith obvious metastatic localization were negative forhMMG and MUC-1.
273
Molecular Markers of Breast Cancer
Volume 50 Number 3 May–June 2006 ACTA CYTOLOGICA
Table I Thermal Conditions for PCR Amplification
Initial Cycle No. of Final
Marker denaturation conditions cycles extension
GAPDH 94°C × 5 min 94°C × 30 sec 40 72°C × 7 min
64°C × 30 sec
72°C × 30 sec
MMG 94°C × 5 min 94°C × 30 sec 25 72°C × 7 min
Outer 58°C × 30 sec
72°C × 30 sec
94°C × 5 min 94°C × 30 sec 40 72°C × 7 min
Inner 55°C × 30 sec
72°C × 30 sec
MUC1 94°C × 5 min 94°C × 30 sec 30 72°C × 7 min
50°C × 30 sec
72°C × 30 sec
Figure 1 Agarose gel electrophoresis of amplified products by
RT-PCR analysis of MMG mRNA expression in axillary lymph nodes.
Lanes are consecutively numbered above their start line. The
molecular weight marker (lane 8) is a 100-bp ladder. Lanes 1–4 are
329-bp products corresponding to mammoglobin expression. Lane
5 contains no band, corresponding to lymph nodes obtained from
noncancer patients (node-negative controls). Lanes 6 and 7 are
negative controls (no cDNA added during RT-PCR).
DO NOT
DUPLICA
TE
© Cop
yrigh
ted
Mat
erial
MUC-1 assay was positive in 11 cases (10.89%). In1 histologically negative SLN, MUC-1 mRNA wasdetected, but both IHC and hMMG were positive.Only 1 case was positive for hMMG and was histolog-ically and immunohistochemically negative. If wecompare the results obtained by the extensive use ofIHC with those obtained by the other techniques andconsider IHC the gold standard in detecting ITC andmicrometastases in SLNs, the sensitivity and specific-ity values of the HE-stained frozen sections and ofamplification for hMMG and MUC-1 mRNA were:frozen, 82.75% and 100%; hMMG, 82.75% and98.71%; MUC-1, 68.11% and 100%, respectively.
Discussion
In spite of published studies, there is no consensus onthe optimal handling of SLNs. The protocols are usu-ally tailored to the institution’s goals, organization ofsurgical activities and cost analysis. The pathologicmethods used to assess SLNs can influence the inter-pretation of the results reported in the literature andjustify the differences in the evaluation of the sensitiv-ity of the procedure.1,11-16,20
In our study the extensive use of IHC confirmedthat the intraoperative examination of axillary SLNsusing serial sectioning is feasible and effective. How-ever, RT-PCR is more sensitive than immunohisto-chemistry in detecting tumor cells.18-20
A review of the literature reveals that different re-sults from such heterogeneous methodologies may bedue to the fact that not all SLN tissue is histopatho-logically assessed.9,14 Usually a moiety of the SLN isused for molecular studies, and this sample is lost forserial sectioning. To overcome this drawback, we useFNAC of the surgically removed SLN before the ex-tensive intraoperative examination; in this way themolecular test can be considered an important, ad-junctive tool in the definition of the pathologic stageaccording to the TNM staging system (N0
(mol+)).We used hMMG since it was suggested to be a su-
perior marker for PCR detection of breast cancermetastases in SLN.6 hMMG is a highly glycosylated,low-molecular-weight protein and member of theuteroglobin family with unknown functions. HMMGmRNA expression has been found in 70–80% of pri-mary and metastatic breast cancer.16-18,21 Unfortu-nately, it is not universally expressed in breast cancersbecause these tumors are highly heterogeneous bygene expression profiling; therefore, additional mark-ers are needed for a sensitive assay to detect breastcancer cells.22 MUC is a well-known marker of breastcancer23; MUC RNA has been used by several re-searchers, usually in multigene RT-PCR, to detectbreast cancer cells in lymph nodes and in peripheralblood.24-27
The feasibility and reliability of the proposedmethod was confirmed by the relatively high percent-age (83.47%) of successful amplification forGAPDH2, a housekeeping gene product, and by con-firmation of the result of hMMG-positive cases thatwere subsequently used as positive controls.
We consider the extensive use of IHC as the goldstandard in detection of isolated tumor cells and mi-crometastases in SLNs; concordance with the molec-ular assay on FNAC was obtained in 19 of the 24 pos-itive SLNs (79.1%). In 2 cases IHC detected isolatedtumor cells in the marginal sinus of the SLN, and in 1a micrometastatic focus was present. Probably smallaggregates of tumor cells escape FNAC and give falsenegative results. In the remaining 2 cases, obviousmetastatic deposits were not detected with the molec-ular assays. It is well known that molecular diagnostictests are potentially of higher sensitivity than IHC,but unfortunately the application of RT-PCR forbreast cancer detection is hampered by lack of specif-ic markers; in fact, neither hMMG nor MUC-1 iden-tifies all breast cancers.22,25-27
In our series MUC-1 showed very low sensitivity,and its application in a multigene assay should be dis-couraged. In contrast, hMMG proved to be the mostuseful and reliable marker.
In conclusion, extensive use of IHC can reduce thenumber of the false negative results in detecting ITCand micrometastases in routine frozen sections. Theincreased yield on serial sectioning with H-E and IHChas been reported variously, ranging from 7% to 33%(4.9% in our series).28-30 However, the pathologic im-portance of ITC and micrometastases in SLNs andtheir impact on the natural history of the disease arestill being debated. At present the presence of anytumor in the lymph node, regardless of the size, mustbe considered a metastasis in light of what it impliesabout tumor biology,31 but whether these foci havesignificant metastatic potential is unclear, and thus noclear prognostic value for patient survival has beenshown for the identification of ITC and micrometas-tases.32
Our tissue-sparing molecular assay gives encourag-ing results. Our method is very simple, quick and notas expensive as the extensive use of IHC. At our insti-tution an IHC stain with anticytokeratin pool is avail-able at a cost of US$12.30, whereas the assays forGAPDH and hMMG RNA RT-PCR (extraction andamplification) cost US$36.80. A mean of 26 IHCstains for SLN costs of US$314.60, 10 times morethan the molecular test.
In > 16% of cases, FNAC was inadequate, as con-firmed by amplification for a housekeeping gene. Thiswas due to the difficulty of obtaining sufficient mate-rial from small, soft SLNs and to the excessively deli-
274
Cannone et al
ACTA CYTOLOGICA Volume 50 Number 3 May–June 2006
DO NOT
DUPLICA
TE
© Cop
yrigh
ted
Mat
erial
cate needling of the pathologist, worried about caus-ing tissue artifacts. More accurate selection of samplecandidates for the molecular test could reduce the per-centage of failures reported in the present study,which was based on 98 consecutive surgical proce-dures.
In the future the development of rapid RT-PCRprotocols might provide the platforms for realizinghighly sensitive intraoperative analysis of SLNs andgaining prognostic information on the necessity of ax-illary dissection.
Although the clinical and prognostic relevance of apositive molecular test in histologically negative casesshould be further investigated, these preliminary datacould have a dual impact on SLN examination. First,this technique allows a complete histologic examina-tion without sacrificing part of the SLN and simulta-neously provides a valuable diagnostic adjunct for thedetection of occult tumor cells. Second, in selectedcases it could be used in association with ultrasono-graphically guided SLN FNA to obtain informationon the presurgical status of the axillary lymph nodes.
References
1. Viale G, Mazzarol G, Bosari S: Intraoperative examination ofaxillary sentinel lymph nodes in breast carcinoma patients. Can-cer 1999;85:2433–2438
2. Veronesi U, Paganelli G, Viale G: Sentinel lymph node biopsyand axillary dissection in breast cancer: Results in a large series.J Natl Cancer Inst 1999;91:368–373
3. Viale G: The intraoperative examination of axillary sentinelnodes. Radiol Oncol 2000;34:261–264
4. Czerniecki BJ, Scheff AM, Callans LS: Immunohistochemistrywith pancytokeratins improves the sensitivity of sentinel lymphnode biopsy in patients with breast carcinoma. Cancer 1999;85:1098–1103
5. Pendas S, Dauway E, Cox CE, Giuliano R, Ku NN, SchreiberRH: Sentinel node biopsy and cytokeratin staining for the ac-curate staging of 478 breast cancer patients. Am Surg 1999;65:500–506
6. Min CJ, Tafra L, Verbanac KM: Identification of superiormarkers for polymerase chain detection of breast cancer metas-tases in sentinel lymph nodes. Cancer Res 1998;58:4581–4584
7. Grunewald K, Haun M, Hurbanek M, Fiegl M, Muller-Holz-ner E, Gunsilius E, Dunser M, Marth C, Gastl G: mammoglo-bin gene expression: A superior marker of breast cancer cells inperipheral blood in comparison to Epidermal-Growth-Factor-Receptor and Cytokeratin 19. Lab Invest 2000;80:1071–1077
8. Marchetti A, Buttitta F, Bertacca G, Zavaglia K, Bevilacqua G,Angelucci D, Viacava P, Naccarato A, Bonadio A, Barassi F, Fe-licioni L, Salvatore S, Mucilli F: mRNA markers of breast can-cer nodal metastases: Comparison between mammoglobin andcarcinoembryonic antigen in 248 patients. J Pathol 2001;195:186–190
9. Manzotti M, Dell’Orto P, Maisonneuve P, Zurrida S, MazzarolG, Viale G: Reverse transcription-polymerase chain reactionassay for multiple mRNA markers in the detection of breastcancer metastases in sentinel lymph nodes. Int J Cancer
2001;95:307–312
10. Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, HallerDG, Morrow M: AJCC Cancer Staging Manual. Sixth edition.New York, Springer-Verlag, 2002
11. Giuliano AE, Kirgan DM, Guenther JM, Morton DL: Lym-phatic mapping and sentinel lymphadenectomy for breast can-cer. Ann Surg 1994;220:391–398
12. Krag D, Weaver D, Ashikaga T, Moffat F, Klimberg VS, Shri-ver C, Feldman S, Kusminsky R, Gadd M, Kuhn J, Harlow S,Beitsch P: The sentinel node in breast cancer: A multicentervalidation study. N Engl J Med 1998;339:941–946
13. Weaver DL, Krag DN, Ashikaga T, Harlow SP, O’Connell M:Pathologic analysis of sentinel and nonsentinel lymph nodes inbreast carcinoma: A multicenter study. Cancer 2000;88:1099–1107
14. O’Hea BJ, Hill AD, El-Shirbiny AM, Yeh SD, Rosen PP, CoitDG, Borgen PI, Cody HS III: Sentinel lymph node biopsy inbreast cancer: Initial experience at Memorial Sloan-KetteringCancer Center. J Am Coll Surg 1998;186:423–427
15. Cody HS III, Borgen PI: State-of-the-art approaches to sen-tinel node biopsy for breast cancer: Study design, patient selec-tion, technique, and quality control at Memorial Sloan-Ketter-ing Cancer Center. Surg Oncol 1999;8:85–91
16. Veronesi U, Paganelli G, Galimberti V, Viale G, Zurrida S,Bedoni M, Costa A, de Cicco C, Geraghty JG, Luini A, Sacchi-ni V, Veronesi P: Sentinel-node biopsy to avoid axillary dissec-tion in breast cancer with clinically negative lymph nodes.Lancet 1997;349:1864–1867
17. Schoenfeld A, Luqmani Y, Smith D, O’Reilly S, Shousha S,Sinnett HD, Coombes RC: Detection of breast cancer mi-crometastases in axillary lymph nodes by using polymerasechain reaction. Cancer Res 1994;54:2986–2990
18. Noguchi S, Aihara T, Nakamori S, Motomura K, Inaji H,Imaoka S, Koyama H: The detection of breast carcinoma mi-crometastases in axillary lymph nodes by means of reverse tran-scriptase-polymerase chain reaction. Cancer 1994;74:1595–1160
19. Watson MA, Fleming TP: mammoglobin, a mammary specificmember of the uteroglobin gene family, is overexpressed inhuman breast cancer. Cancer Res 1996;56:860–865
20. Watson MA, Dintsis S, Darrow CM, Voss LE, DiPersio J,Jensen R: mammoglobin expression in primary, metastatic andoccult breast cancer. Cancer Res 1999;59:3028–3031
21. Houghton RL, Dillon DC, Molesh DA, Zehentner BK, Xu JC,Jiang J: Transcription complementarity in breast cancer: Appli-cation to detection of circulating tumor cells. Mol Diagn2001;6:79–91
22. Zehentner BK, Dillon DC, Yuqiu J, Jiangchun X, BenningtonA, Molesh DA, XinQun Z, Reed SG, Persing DH, HoughtonRL: Application of a multigene reverse transcription-PCR assayfor detection of mammoglobin and complementary transcribedgenes in breast cancer lymph nodes. Clin Chem 2002;48:1225–1231
23. Bombardieri E, Gion M: Mucin-like cancer associated antigen(MCA. as available circulating tumor marker for breast cancer.In Serological Cancer Markers. Edited by S Sell. Totowa, NewJersey, Humana Press, 1992, pp 341–354
24. Gillanders WE, Mikhitarian K, Hebert R, Mauldin PD, PaleshY, Walters C, Urist MM, Mann GB, Doherty G, HermannVM, Hill AD, Eremin O, El-Sheemy M, Orr RK, Valle AA,Henderson MA, Dewitty RL, Sugg SL, Frykberg E, Yeh K, Bell
275
Molecular Markers of Breast Cancer
Volume 50 Number 3 May–June 2006 ACTA CYTOLOGICA
DO NOT
DUPLICA
TE
© Cop
yrigh
ted
Mat
erial
RM, Metcalf JS, Elliott BM, Brothers T, Robison J, Mitas M,Cole DJ: Molecular detection of micrometastatic breast cancerin histopathology-negative axillary lymph nodes correlates withtraditional predictors of prognosis: An interim analysis of aprospective multi-institutional cohort study. Ann Surg 2004;239:828–837
25. Baker MK, Mikhitarian K, Osta W, Callahan K, Hoda R, Bres-cia F, Kenuper-Hall R, Mitas M, Cole DJ, Gillanders WE:Molecular detection of breast cancer cells in the peripheralblood of advanced-stage breast cancer patients using multi-marker real-time reverse transcription-polymerase chain reac-tion and a novel porous barrier density gradient centrifugationtechnology. Clin Cancer Res 2003;9:4865–4871
26. Zippelius A, Pantel K: RT-PCR based detection of occult dis-seminated tumor cells in peripheral blood and bone marrow ofpatients with solid tumors. Ann N Y Acad Sci 2000;906:110–123
27. Mitas M, Mikhitarian K, Walters C, Baron PL, Elliott BM,Brothers TE: Quantitative real time RT-PCR detection ofbreast cancer micrometastasis using a multigene marker panel.
Int J Cancer 2001;93:162–171
28. Zhang PJ, Reisner RM, Nangia R, Edge SB, Brooks JJ: Effec-tiveness of multilevel sectioning in detecting axillary nodal mi-crometastases: A retrospective study with immunohistochemi-cal analysis. Arch Pathol Lab Med 1998;122:687–690
29. Bedrosian I, Reynolds C, Mick R, Callans LS, Grant CS,Donohue JH, Farley DR, Heller R, Conant E, Orel SG, Law-ton T, Fraker DL, Czerniecki BJ: Accuracy of sentinel lymphnode biopsy in patients with large primary breast tumors. Can-cer 2000;88:2540–2545
30. Prognostic importance of occult axillary lymph node mi-crometastases in breast cancer: International (Ludwig). BreastCancer Study Group. Lancet 1990;335:1565–1568
31. Jannink I, Fan M, Nagy S, Rayudu G, Dowlatshahi K: Serialsectioning of sentinel nodes in patients with breast cancer: Apilot study. Ann Surg Oncol 1998;5:310–314
32. Strickland AH, Beechey-Newman N, Steer CB, Harper PG:Sentinel node biopsy: An in-depth appraisal. Crit Rev OncolHematol 2002;44:45–70
276
Cannone et al
ACTA CYTOLOGICA Volume 50 Number 3 May–June 2006
DO NOT
DUPLICA
TE
© Cop
yrigh
ted
Mat
erial