Linkage disequilibrium analyses in the Costa Rican population suggests discrete gene loci for...
-
Upload
independent -
Category
Documents
-
view
3 -
download
0
Transcript of Linkage disequilibrium analyses in the Costa Rican population suggests discrete gene loci for...
Original article 159
Linkage disequilibrium analyses in the Costa Ricanpopulation suggests discrete gene loci for schizophreniaat 8p23.1 and 8q13.3Consuelo Walss-Bassa, Ana Patricia Monterod, Regina Armase,Albana Dassoria, Salvador A. Contrerasa, Wei Liua, Rolando Medinaa,Douglas Levinsonf, Mariana Pereirad, Ivannia Atmellad, Lisa NeSmitha,Robin Leachb, Laura Almasyc, Henriette Raventosd and Michael A. Escamillaa,b
Linkage studies using multiplex families have repeatedly
implicated chromosome 8 as involved in schizophrenia
etiology. The reported areas of linkage, however, span a
wide chromosomal region. The present study used the
founder population of the Central Valley of Costa Rica
and phenotyping strategies alternative to DSM-IV
classifications in attempts to further delimitate the
areas on chromosome 8 that may harbor schizophrenia
susceptibility genes. A linkage disequilibrium screen
of chromosome 8 was performed using family trios of
individuals with a history of psychosis. Four discrete
regions showing evidence of association (nominal P values
less than 0.05) to the phenotype of schizophrenia were
identified: 8p23.1, 8p21.3, 8q13.3 and 8q24.3. The region
of 8p23.1 precisely overlaps a region showing strong
evidence of linkage disequilibrium for severe bipolar
disorder in Costa Rica. The same chromosomal regions
were identified when the broader phenotype definition of
all individuals with functional psychosis was used for
analyses. Stratification of the psychotic sample by
history of mania suggests that the 8q13.3 locus may be
preferentially associated with non-manic psychosis.
These results may be helpful in targeting specific areas
to be analyzed in association-based or linkage
disequilibrium-based studies, for researchers who
have found evidence of linkage to schizophrenia on
chromosome 8 within their previous studies. Psychiatr
Genet 16:159–168 �c 2006 Lippincott Williams & Wilkins.
Psychiatric Genetics 2006, 16:159–168
Keywords: association, Costa Rica, linkage disequilibrium, mania, psycho-sis, schizophrenia
Departments of aPsychiatry, bCellular and Structrual Biology, University of TexasHealth Science Center at San Antonio, cSouthwest Foundation for BiomedicalResearch, San Antonio, Texas, dCenter for research in Cellular and MolecularBiology, University of Costa Rica, San Jose, Costa Rica, eLangley PorterPsychiatric Institute, University of California at San Francisco, San Francisco,California and fDepartment of Psychiatry, Stanford University, Stanford, California,USA.
Correspondence and requests for reprints to Michael Escamilla, 7703 Floyd CurlDrive, San Antonio, TX 78229-3900, USATel: + 1 210 562 5111; fax: + 1 210 562 5114;e-mail: [email protected]
Sponsorship: This work was supported in part by National Institute of HealthGrants R01-MH61884 and K01 MH01453 (M.A.E.), the NARSAD YoungInvestigator Award (M.A.E.), the Howard Hughes Medical Foundation, the Friendsof Psychiatry (UTHSCSA Department of Psychiatry), the International Center forGenetic Engineering and Biotechnology Project CRP/COS98-01 (H.R.), and aNational Institute of Health Minority Supplement Award 3 R01-Mh61884 toC.W.B.
IntroductionSchizophrenia (SC), a devastating mental illness that
affects around 1% of the population worldwide, is among
the most costly and debilitating of the psychiatric
disorders (Kessler et al., 1995; Wyatt et al., 1995). Although
genetic factors are known to play an important role, the
identification of such genes, and the molecular mechan-
isms of the disease, have remained elusive. This can be
due to the fact that numerous genes of minor effect are
involved in its etiology (Pulver et al., 2000), together with
environmental factors (Howes et al., 2004). Furthermore,
different combinations of disease susceptibility genes are
also expected. The complex inheritance and genetic
heterogeneity would explain the difficulties in replicating
linkage studies of SC. Nevertheless, through the use of
narrower and more precise phenotypes, certain broad
chromosomal regions have shown, in more than one
independent study, evidence of linkage at levels of
significance considered suggestive or significant by
Lander and Kruglyak (1995). The small arm of chromo-
some 8 (8p) is one such region (Pulver et al., 1995;
Kendler et al., 1996; Blouin et al., 1998; Shaw et al., 1998;
Brzustowicz et al., 1999; Gurling et al., 2001).
Most of the early studies searching for SC susceptibility
genes were carried out using large multiplex families. In
family linkage studies, mapping signals generally span
many centi-Morgans resulting in broad areas of possible
linkage (up to 20 cM or larger). The fact that earlier
studies predominantly used multiplex mapping, together
with the use of different sample sizes, analytic and family
ascertainment strategies, phenotype designation methods
0955-8829 �c 2006 Lippincott Williams & Wilkins
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
and inaccurate marker maps could account for the wide
area of positive linkage results spanning chromosome
8p. It is also possible that the chromosome 8p region
may potentially harbor several predisposition genes.
Supporting the latter possibility, several candidate genes
in the 8p region have recently been reported to be
associated with SC (Stefansson et al., 2002; Gerber et al.,2003; Katsu et al., 2003; Yang et al., 2003; Nakata and
Ujike, 2004).
One potentially useful method, both to map at a genome
level and to map at narrow regions where SC suscept-
ibility genes are located on chromosome 8, is to perform
systematic linkage disequilibrium (LD) analyses. The
present study performed an LD screen for SC genes on
chromosome 8 using a sample of individuals with a history
of psychosis, descendant from the founding population of
the Central Valley of Costa Rica (CVCR). The CVCR
population is an ideal one for performing LD analysis at
the genome screening level because of its structure,
origin and well documented genealogical information
(Escamilla et al., 1999; Ophoff et al., 2002; Mathews et al.,2004). A subset of the present day CVCR inhabitants are
descended from a small group of founders dating back to
the first Spanish settlement in 1569, approximately 20
generations ago (Escamilla et al., 1996). This type of
isolated expansion is ideal for detecting founder haplo-
types in genetic illnesses; compared with the few other
isolated populations in the world, such as Finland, regions
of the Netherlands and French Canada, and the Amish,
Costa Rica’s expansion has been the greatest and from
the fewest number of founders (Escamilla et al., 2001).
Gene mapping studies in non-psychiatric disorders in this
population have also led to significant findings, leading to
eventual identification of disease genes for inherited
deafness (Leon et al., 1992) and familial telangiectasia
(Uhrhammer et al., 1995).
Chromosome 8 is of special interest for those studying
psychiatric disorders (especially those involving psycho-
sis) in the CVCR. A genome-wide LD screen of severe
bipolar disorder (BP) conducted in this population
reported the most significant finding to be on a well
delimited region on chromosome 8p (Ophoff et al., 2002).
Patients with severe BP, such as those studied in the
CVCR, often have psychotic episodes (Escamilla et al.,2002) and share clinical and epidemiological features of
SC (Boteva and Lieberman, 2003). In addition to
investigating whether evidence for specific SC loci could
be found on chromosome 8 in the CVCR population, we
also wished to investigate whether SC patients would
show LD to the same region that has been shown to be in
LD with severe BP in this population (Ophoff et al.,2002). Other loci have been found in common between
SC and severe BP in samples from this population
(Freimer et al., 1996; Escamilla et al., 1999, 2001; DeLisi
et al., 2002; Walss-Bass et al., unpublished observation)
and other populations (Gershon and Badner, 2001).
Although formal criteria for defining SC have been
developed and the diagnosis using current classification
systems is highly reliable (Nurnberger et al., 1994),
naturalistic studies of BP and SC have suggested that
alternate classifications may better define the underlying
types of psychotic disorder (Kendler et al., 1998; Swann etal., 2001). To further try to understand the nature of the
phenotypes showing LD to various loci on chromosome 8
in the CVCR, an alternative phenotyping strategy was
also used. First, individuals with a history of psychosis
[regardless of DSM-IV (Diagnostic and statistical manual
of mental disorders – fourth edition) category] were
analyzed for evidence of LD on chromosome 8. Next, it
was hypothesized that the presence or absence of mania
in the course of chronic psychotic illness might better
define homogeneous subtypes of psychotic disorder, in a
manner that is obfuscated when using DSM-IV classifica-
tions. Division of the ‘psychotic disorder’ group into two
more genetically homogeneous groups, if successful,
should result in (i) distinct genetic loci showing LD to
each of the two subtypes, and (ii) more power to detect
loci (i.e. a smaller sample of a more homogeneous
phenotype should have as much power to detect LD as
a larger sample that is not as genetically homogeneous).
The results of this study support a locus for SC at the
same location as a locus for severe BP in the CVCR
population, on chromosome 8p23.1. Supportive evidence
for other possible SC loci at two other chromosome 8
regions is also reported. Finally, we report a unique locus
on 8q, which demonstrates LD to ‘non-manic’ psychotic
disorders.
MethodsAll study participants (154 probands and 289 relatives)
were recruited in accordance with the principles of the
Declaration of Helsinki and with approval from the
Institutional Review Boards of the University of Costa
Rica and the University of Texas Health Science Center
at San Antonio. Probands were recruited independently
from one another from psychiatric hospitals and clinics in
the CVCR. All probands had disease onset by the age of
40 years, a history of at least one psychiatric hospitaliza-
tion, a discharge diagnosis of SC, bilineal Spanish
surnames and a current residence in the CVCR.
Furthermore, we performed genealogical analysis to
determine the ancestry of all participants in our study
(Table 1, section A). Two hundred and eighty-nine
parents and first-degree relatives of probands were
recruited where possible to permit determination of the
genetic phase and to allow for family-based LD analyses.
These additional participants were not diagnosed or
assessed for psychiatric disorders. The breakdown of
160 Psychiatric Genetics 2006, Vol 16 No 4
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
family pedigrees recruited for our study is shown in Table
1, section B).
As in previous LD studies of BP in this population
(Escamilla et al., 1996, 1999), each proband was
interviewed by a bilingual psychiatrist who was blind to
the previous history of the participant, using the
Diagnostic Interview for Genetic Studies (Nurnberger
et al., 1994). Medical records (inpatient and outpatient)
were also abstracted for each proband. An interview
with a close relative, using a Spanish version of the
Family Interview for Genetic Studies was also completed
for each proband. All 154 probands were diagnosed
using a best-estimate diagnostic process like the one
described in previous CVCR studies (Escamilla et al.,1996, 1999). The process arrives at a lifetime consensus
diagnosis or diagnoses using the DSM-III-R, DSM-IV
and RDC systems. For each proband, the best estimators
also diagnosed whether manic and/or depressive syn-
dromes (as defined by the DSM-IV) had been present
during the course of the disorder. Each proband was also
evaluated at the best estimate for a history of psychosis,
as defined by a history of hallucinations, delusions,
disorganized thinking or behavior (symptoms 1–4 of
category A of DSM-IV SC). All probands had a history
of psychosis.
Best-estimate consensus diagnoses of the 154 probands
recruited for this study are shown in Table 1 (section C).
All 154 probands had a history of psychosis. Seventy-two
of the 154 probands had both a history of psychosis and at
least one manic syndrome during the course of their
illness and 82 had never met full criteria for a manic
syndrome (DSM-IV criteria). Of the 72 participants who
had histories of both psychosis and mania, 14 had final
consensus DSM-IV diagnoses of bipolar type I disorder
(BPI), 19 were diagnosed with schizoaffective bipolar
disorder (SABP), and 39 were diagnosed with SC. When
probands had both manic syndromes and psychotic
episodes, and the psychoses lasted more than 2 weeks
in the absence of mood syndromes, the DSM-IV allows a
diagnosis of either SC or SABP to be given. In deciding
between SC and SABP for such cases, using DSM-IV
criteria, SABP was operationalized as a case in which the
affective syndromes (manias and depressions) had been
present for 30% or more of the entire illness. This
operationalization is consistent with the Family Interview
for Genetic Studies and the Diagnostic Interview for
Genetic Studies, which query this item, and with current
classifications used in the NIMH Genetics Initiative
studies of Schizophrenia (Levinson and Escamilla,
personal communications).
Genotyping
A genomewide survey of background LD in the CVCR
population showed that LD extended to distances of 2–
7 cM in 310 of 1012 adjacent marker pairs (Service et al.,1999). We therefore expected that, if there is a founder
mutation in the CVCR that influences SC, using a marker
density of 5 cM and the sample described above, we
would have reasonable power, as a first pass, to identify
loci most likely to be in LD with genes influencing our
diagnoses of interest.
DNA from a total of 443 people, of which 154 were
diagnosed probands, was genotyped. Marker order,
heterozygosity and sex-averaged distance from the p-
terminal are listed in Fig. 1. Genotyping was initially
performed using 30 fluorescently labeled microsatellite
markers of the highest heterozygosity available, spaced at
an average of 5 cM. Follow-up genotyping was then
performed using closely spaced microsatellite markers
positioned in the areas where positive evidence of
association was initially obtained (Table 2). Standard
polymerase chain reaction (PCR) was performed using
the ABI 877 automated thermocycler (Applied Biosys-
tems, Foster city, CA, USA) or the PE 9700 PCR
instrument (Applied Biosystems, Foster city, CA, USA).
Amplified fragments were analyzed on the ABI 377
sequencer (Applied Biosystems, Foster city, CA, USA)
and genotypes were assigned using GENESCAN and
GENOTYPER software. Each genotype was scored
separately by two individuals, who were blind to the
diagnosis of the participants. Genotypes were compared
using a software program, discrepancies were discussed
and final genotypes agreed upon. Genotypes were
checked for violations of Mendelian inheritance by the
PEDSYS program INFER. A total of four families were
discarded from statistical analyses owing to recurrent
Mendelian discrepancies.
Table 1 Diagnostic and family structure information
Proband information n
A. AncestryAt least four great-grandparents born in the CentralValley of Costa Rica
152a
All known ancestors from the Guanacaste area ofCosta Rica
2
Total 154B. Family structure
Both parents sampled 45At least one parent sampled 62No parents, but one or more siblings sampled 13No relatives available 34Total 154
C. DSM-IV diagnosis of probandsSchizophrenia 105Schizoaffective bipolar 19Schizoaffective depressed 6Bipolar disorder I 14Major depressive episode with psychosis 6Psychosis not otherwise specified 4Total 154
aNine of the probands had incomplete information to ascertain complete ancestryof the great-grandparents. DSM-IV, Diagnostic and statistical manual of mentaldisorders – fourth edition.
LD analysis of chromosome 8 in Costa Rica Walss-Bass et al. 161
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
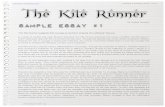
Fig. 1
II
IV
I
Region
Ideogram
8p23+38p23+2
8p23+1
8p22
8p21+2
8p11+18q11+1
8q12+38q13+18q13+28q13+3
8p21+1
8p12
8p11+238p11+228p11+21
8q11+21
8q11+22
8q11+23
8q12+18q12+2
8q21+118q21+128q21+13
8q21+2
8q21+3
8q22+18q22+2
8q22+3
8q23+18q23+2
8q23+3
8q24+118q24+12
8q24+13
8q24+21
8q24+228q24+23
8q24+3
8p21+3
D8 S 264
D8 S 277
D8 S 1825
D8 S 503
D8 S 542
D8 S 516D8 S 1721
D8 S 520D8 S 552D8 S 549
D8 S 261
D8 S 282D8 S 1786D8 S 1734
D8 S 1771
D8 S 1820D8 S 505
D8 S 532D8 S 285D8 S 260
D8 S 1841D8 S 1767
D8 S 1117D8 S 543D8 S 1795
D8 S 279
D8 S 1144D8 S 1705
D8 S 1757
D8 S 275D8 S 271D8 S 270D8 S 1762
D8 S 1784D8 S 1779
D8 S 514D8 S 1799
D8 S 284
D8 S 256D8 S 272
Heterozygosity
D8 S 1837
D8 S 1743D8 S 1836
0.73
8.34
15.38
16.19
16.1917.00
17.00
20.6126.4331.73
37.0441.5542.8545.41
46.26
50.0556.04
60.8764.7571.00
79.3682.26
83.5085.2387.54
87.54
91.4694.61
96.21
97.28
98.88102.6
103.69
112.42118.15123.54
130.00133.64
143.82148.12
154.02
156.59162.94
165.93
0.83
0.73
0.710.610.74
0.600.71
0.770.800.61
0.790.70
0.740.86
0.670.770.750.80
0.830.78
0.820.79
0.680.68
0.740.66
0.88
0.760.840.80
0.750.770.79
0.770.68
0.760.760.84
0.830.83
0.80
0.810.83
0.84
D8 S 258
Marker pter (cM)
III
Chromosome 8 schizophrenia susceptibility loci in Costa Rica. Boxed numbers to the left of the chromosome ideogram represent chromosomalareas with positive association in our present study. Markers are positioned according to genetic distance (cM) from the p-terminal. Marker positionsand heterozygosity are from Marshfield.
162 Psychiatric Genetics 2006, Vol 16 No 4
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Statistical analysis
Potential LD was evaluated between markers and a
putative disease locus by the T1 and T3 tests of
association implemented in the program CLUMP (Sham
and Curtis, 1995). Both tests evaluate whether particular
alleles at a locus are overrepresented on disease chromo-
somes, compared with non-disease chromosomes. The T3
statistic is most powerful when one allele at a particular
marker is associated with the disease, while the T1
statistic looks at whether allele frequencies are statisti-
cally different from one group to another. The T1 and T3
CLUMP tests thus offer compensatory strengths and
weaknesses when used in the search for genes in a
complex disease. At the time this study was originally
designed, newer family-based association tests that can
accommodate multiple affected family members, such as
FBAT (Laird et al., 2000), were not available. Our design
therefore focused on one affected individual (i.e. the
proband) per family and used the CLUMP test as our
primary method of analysis. Current and future studies in
this population sample will diagnose all individuals within
these families and will probably use FBATor other similar
analyses to assess the association between markers and
phenotypes of interest.
To determine whether the association detected by the
CLUMP analyses was due to LD, the likelihood-ratio test
of LD (measured by the parameter l), implemented in
DISLAMB (Terwilliger, 1995), was performed. The
likelihood-ratio test of LD has been previously used to
Table 2 Results of T1 and T3 CLUMP analyses (P values) for schizophrenia and psychosis in the Central Valley of Costa Rica
Markers Schizophrenia Psychosis
Initial screen Follow-upmarkers
pter (n = 105) All (n = 154) Mania (n = 72) No mania (n = 82)
cM T1 T3 TI T3 T1 T3 T1 T3
D8S264 0.730 NS NS NS NS NS NS NS NSD8S277 8.340 NS NS NS NS NS 0.0839 NS NS
D8S1825 15.38 NS NS 0.082 NS 0.008 0.034 NS NSD8S542 16.19 0.036 0.008 0.090 0.031 0.019 0.084 0.063 0.027
D8S503 16.19 0.019 0.044 NS NS NS NS NS NSD8S516 17.00 NS NS 0.092 NS NS NS NS NSD8S1721 17.00 NS NS NS NS NS NS NS NS
D8S520 20.61 NS NS NS NS NS NS NS NSD8S552 26.43 NS NS NS NS NS NS NS NSD8S549 31.73 NS NS NS NS NS NS NS NSD8S261 37.04 NS NS NS NS NS NS NS NS
D8S258 41.55 0.049 0.080 0.055 NS NS NS NS NSD8S282 42.85 0.092 0.048 NS 0.028 NS NS 0.057 0.033
D8S1786 45.41 NS NS NS NS NS NS NS NSD8S1734 46.26 NS NS NS NS NS NS NS NSD8S1771 50.05 NS NS NS NS NS NS NS NSD8S1820 56.04 NS NS NS NS NS NS NS NSD8S505 60.87 NS NS NS NS NS NS 0.068 NSD8S532 64.75 NS NS NS NS NS NS NS NSD8S285 71.00 0.059 0.062 0.0699 0.065 NS NS 0.071 0.026
D8S260 79.36 NS NS NS NS NS NS NS NSD8S1841 82.26 NS NS NS 0.030 NS 0.0789 NS 0.088D8S1767 83.51 NS NS NS NS NS NS NS NSD8S1117 85.23 0.098 NS 0.010 0.076 0.039 NS 0.034 0.047
D8S543 87.54 0.023 0.049 0.0280 0.035 NS NS 0.002 0.009
D8S1795 87.54 NS NS NS NS NS NS NS NSD8S279 91.46 NS NS NS NS NS NS NS NSD8S1144 94.61 NS NS NS NS NS NS NS NS
D8S1705 96.21 NS NS NS NS NS NS 0.001 0.012
D8S1757 97.28 NS NS NS NS NS NS NS NSD8S275 98.88 NS 0.071 NS NS NS NS NS 0.041
D8S271 102.6 NS NS NS NS NS NS NS NSD8S270 103.6 NS NS 0.098 NS NS NS NS NSD8S1762 112.4 NS NS NS NS NS NS NS NSD8S1784 118.1 NS NS NS NS NS NS NS NSD8S1779 123.5 NS NS NS NS NS NS NS NSD8S514 130.0 NS NS NS NS 0.089 NS NS NSD8S1799 133.6 NS NS NS NS NS NS NS NSD8S284 143.8 NS NS NS NS NS NS NS NSD8S256 148.1 NS NS NS NS NS NS NS NSD8S272 154.0 NS NS NS NS NS NS NS NSD8S1837 156.5 NS NS NS NS NS NS NS NSD8S1743 162.9 NS NS NS NS NS NS NS NSD8S1836 165.9 0.026 0.039 0.015 0.010 NS NS 0.070 0.051
Only P values less than 0.1 are listed. Genetic distances for each marker from the pter are from Marshfield. Numbers in bold are those with P < 0.05. All, all diagnosis witha history of psychosis; NS, non-significant.
LD analysis of chromosome 8 in Costa Rica Walss-Bass et al. 163
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
assess LD of BP disorder in the Costa Rican population
(Escamilla et al., 1999). In that study, simulation tests
were performed to determine the power to detect LD
using different sample sizes and phenocopy rates. It was
found that with a sample of 90 patients and their
relatives, assuming a phenocopy rate of 50%, a suggestive
level of association (Pr 0.05) could be detected 82% of
the time. Increasing the sample size to 200 improved the
power to detect LD to 99% of the time. Given that the
sample size in our present study is 105 SC patients from
the same Costa Rican population, and that parental
alleles were available in the majority of the individuals
(through either direct genotyping or inference), we felt
that by establishing an a priori level of significance of
P = 0.05 we would be able to detect LD over 82% of the
time, if 50% of the individuals have the same mutation.
Alleles from chromosomes of ‘affected’ persons were
compared with non-transmitted parental chromosomes,
using the CLUMP and DISLAMB tests modified to allow
analysis of DNA from affected individuals whose parents
were not available (Escamilla et al., 1999). Whenever
possible, if both parents were not available, additional
siblings of the affected individual were genotyped to
permit inference of the parental alleles.
Initially, the phenotype of interest studied was SC, as
defined by the DSM-IV by best-estimate consensus. To
maximize the power of analysis and because of the fact
that the population sample contained several individuals
whose parents were not available for analysis, the sample
group used for the control chromosomes included non-
transmitted chromosomes from the parents of probands
of all diagnoses. The allele frequency distribution (for
each marker tested) from this group was not statistically
different from that of the parents of SC probands only. It
was therefore felt that the sample of parents of all
diagnosis was from the same population pool as the
sample of parents of SC probands only. To address the
possibility of population stratification, however, LD
analysis of the markers that showed positive results in
the CLUMP tests was performed using the more
conservative transmission disequilibrium test of Spielman
et al. (1993), which uses only affected subjects with both
parents available for genotyping.
Given the symptomatic and syndromal overlaps between
SC, BP and other psychotic disorders, an alternate
phenotyping strategy was also pursued. A more general-
ized ‘psychosis’ (all psychotic disorders) phenotype was
analyzed for evidence of LD. Subsequently, this sample
was divided into those with and those without a history of
mania (full manic syndrome or episode, by consensus
diagnosis). The ‘psychosis’ sample included all 154
probands, all of who had a history of psychosis (by best-
estimate consensus). Forty-seven percent of these
individuals had a history of full mania (‘manic psychosis’
sample), while 53% had a psychotic disorder with no
previous history of mania. The control sample of non-
transmitted chromosomes remained the same for each
subset.
ResultsResults from the T1 and T3 CLUMP analyses are shown
in Table 2. Markers listed in the first column are those in
the initial 5 cM screen, while markers listed in the second
column are follow-up markers in the regions where
evidence of association was initially seen. For simplicity
purposes, only P values less than 0.10 are listed [others
are listed as non–significant (NS)] and P values less than
0.05 are displayed in bold.
From the initial 5 cM screen, evidence of association
(Pr 0.05) with the SC phenotype (105 affected
individuals) was obtained at four markers, representing
four distinct chromosomal regions (see Fig. 1 for position
of markers along the chromosome): region I: 8p23.1
(D8S542), region II: 8p21.3 (D8S282), region III: 8q13.3
(D8S543) and region IV: 8q24.3 (D8S1836). The
strongest evidence of association was obtained at
D8S542 for the SC category (P = 0.008 for T3). Of the
markers that suggested positive association to the SC
phenotype, D8S542 and D8S543, of regions I and III,
respectively, also showed evidence of association by the
more conservative transmission disequilibrium test ana-
lysis (P = 0.032 and 0.033, respectively). When the
phenotype of ‘psychosis’ was analyzed (154 individuals),
the same four markers showed evidence of association at
Pr 0.05. No additional markers showed evidence of
association to the ‘psychosis’ phenotype.
Follow-up markers
Additional, follow-up markers (markers in close proximity to
markers that tested positive on the initial screen) were
tested for regions I, II and III. In each case, at least one
additional marker, closely linked to the screening markers in
those regions, gave additional evidence of association to SC
or to all psychosis categories (D8S503 in region I, D8S258 in
region II, and D8S1841 and D8S1117 in region III).
Analyses of psychoses with and without a history
of mania
Stratification of the total ‘psychosis’ sample by the
presence or absence of mania yielded two additional
regions, which had not passed our a priori threshold for
association to the ‘SC’ or the ‘all psychosis’ phenotypes
(Table 2). These two additional loci, 8q12.1 (D8S285)
and 8q21.13 (D8S1705 and D8S275), showed possible
association to the ‘no history of mania’ psychosis
phenotype (n = 82) at levels of significance of P < 0.05.
Regions I, II, III and IV, which had shown evidence of
possible association to the ‘all psychosis’ and ‘SC’
164 Psychiatric Genetics 2006, Vol 16 No 4
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
phenotypes, all showed evidence of association at
Pr 0.05 to this phenotype (psychosis without mania)
as well. The strongest evidence of association to this
phenotype was at 8q21.13 (P = 0.001 at D8S1705).
For the ‘psychosis with mania’ group (n = 72), only
regions I and III showed association at levels less than
Pr 0.05. Region I showed the strongest evidence of
association to the psychosis with mania phenotype
(P = 0.008 at D8S1825 and P = 0.019 at D8S542).
Results from the DISLAMB analysis are shown in Table 3
for all diagnostic categories. For simplicity purposes, only
l values greater than 0 are displayed. P values less than
0.05 are displayed in bold. Except for region IV, at 8q24.3,
evidence of LD (l> 0) was obtained in the same regions
that displayed positive association to SC and psychosis
(either stratified or overall). Only two regions, however,
met the criteria for LD at a significance level of P < 0.05:
region I (D8S503), at 8p23.1 was seen to be in LD with
SC (P = 0.0270). In region III, at 8q13.3, markers
D8S1841 and D8S543 were in apparent LD with SC
(P = 0.0398 and 0.0191 respectively), while markers
D8S1117 and D8S543 appeared to be in LD with overall
psychosis (P = 0.0230 and 0.0240, respectively). Inter-
estingly, when the psychotic sample was stratified to
include only non-manic individuals, all three of the region
III markers displayed P values less than 0.05 (P = 0.0350,
0.01176 and 0.0044 for markers D8S1841, D8S1117 and
D8S543, respectively).
Table 3 Results of DISLAMB analysis (k and P values) for schizophrenia and psychosis in the Central Valley of Costa Rica
Markers Schizophrenia Psychosis
Initial screen Follow-upmarkers
pter (n = 105) All (n = 154) Mania (n = 72) No mania (n = 82)
cM l P l P l P l P
D8S264 0.730 NS NS NS NS NS NS NS NSD8S277 8.340 NS NS NS NS NS NS NS NS
D8S1825 15.38 NS NS NS NS NS NS NS NSD8S542 16.19 0.0464 0.4009 NS NS 0.0502 0.3592 NS NS
D8S503 16.19 0.1465 0.0270 0.0900 0.3935 NS NS 0.1155 0.1887D8S516 17.00 NS NS NS NS NS NS NS NSD8S1721 17.00 NS NS NS NS NS NS NS NS
D8S520 20.61 NS NS NS NS NS NS NS NSD8S552 26.43 NS NS NS NS NS NS NS NSD8S549 31.73 NS NS NS NS NS NS NS NSD8S261 37.04 NS NS NS NS NS NS NS NS
D8S258 41.55 NS NS NS NS NS NS NS NSD8S282 42.85 0.1147 0.3363 0.1103 0.2909 NS NS 0.1490 0.1144
D8S1786 45.41 NS NS NS NS NS NS NS NSD8S1734 46.26 NS NS NS NS NS NS NS NSD8S1771 50.05 NS NS NS NS NS NS NS NSD8S1820 56.04 NS NS NS NS NS NS NS NSD8S505 60.87 NS NS 0.1310 0.1931 0.1928 0.0727 0.0221 0.4390D8S532 64.75 NS NS NS NS NS NS NS NSD8S285 71.00 0.1407 0.1856 0.1530 0.1324 0.3338 0.2638 0.1693 0.1005D8S260 79.36 NS NS NS NS NS NS NS NS
D8S1841 82.26 0.2073 0.0398 0.1850 0.0550 NS NS 0.2250 0.0350
D8S1767 83.51 0.1780 0.2196 0.1890 0.1505 0.2016 0.1968 0.1785 0.2583D8S1117 85.23 0.1780 0.0850 0.2096 0.0230 0.1661 0.1857 0.2454 0.0176
D8S543 87.54 0.2009 0.0191 0.1805 0.0240 NS NS 0.2565 0.0044
D8S1795 87.54 NS NS NS NS NS NS NS NSD8S279 91.46 NS NS NS NS NS NS NS NSD8S1144 94.61 NS NS NS NS NS NS NS NS
D8S1705 96.21 NS NS NS NS NS NS NS NSD8S1757 97.28 NS NS NS NS NS NS NS NS
D8S275 98.88 0.1614 0.1101 0.1192 0.2806 0.1614 0.1686 NS NSD8S271 102.6 NS NS NS NS NS NS NS NS
D8S270 103.6 NS NS NS NS NS NS NS NSD8S1762 112.4 NS NS NS NS NS NS NS NSD8S1784 118.1 NS NS NS NS NS NS NS NSD8S1779 123.5 NS NS NS NS NS NS NS NSD8S514 130.0 NS NS NS NS NS NS NS NSD8S1799 133.6 NS NS NS NS NS NS NS NSD8S284 143.8 0.1119 0.0982 NS NS NS NS NS NSD8S256 148.1 NS NS NS NS NS NS NS NSD8S272 154.0 NS NS NS NS NS NS NS NSD8S1837 156.5 NS NS NS NS NS NS NS NSD8S1743 162.9 NS NS NS NS NS NS NS NSD8S1836 165.9 NS NS NS NS NS NS NS NS
Only l values more than 0 and P values less than 0.1 are listed. Genetic distances for each marker from the pter are from Marshfield. Numbers in bold are those withP < 0.05. All, all diagnosis with a history of psychosis; NS, non-significant.
LD analysis of chromosome 8 in Costa Rica Walss-Bass et al. 165
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
DiscussionThe current study utilized an LD approach to screen for
possible SC loci in the CVCR, using an a priori threshold
of P < 0.05. The results of this study suggest two discrete
loci (8p23.1 and 8q13.3) that are most likely to harbor SC
susceptibility genes on chromosome 8, in the Costa Rican
population, as well as two additional loci on chromosome
8 meriting further investigation for psychosis-related
phenotypes. Evidence for both association and LD at
these loci are not at the levels typically required to prove
significant evidence of linkage at the genome screen
level. In addition, as the statistical tools used in this study
(CLUMP T1, CLUMP T3 and DISLAMB tests) are not
independent of each other, corrections for multiple
testing were not applied. Given the size of the sample
involved in this study, and the anticipated complexity of
SC at the genetic level, strongly significant evidence of
LD will require larger samples, additional (haplotype-
based) analyses or additional statistical tools. This study
presents an approach to identifying genes for complex
disorders within a founder-type population (Escamilla etal., 1996), by using a genome screening approach with
previously defined levels of significance (based on the
sample size and power calculations) to identify regions
showing possible LD. The intention of the study is to
identify possible gene loci, which will then be followed
up by more intensive study to identify predisposition
genes within the population of interest.
Several studies have reported linkage of SC to chromo-
some 8p, beginning with a study by Pulver et al. (1995),
conducted in pedigrees drawn from the northeast United
States. Since then, numerous studies using different
populations have reported linkages of SC to 8p (Kendler
et al., 1996; Blouin et al., 1998; Kaufmann et al., 1998; Shaw
et al., 1998; Brzustowicz et al., 1999; Gurling et al., 2001).
Most of the studies point to the region of 8p22-21,
although in two studies, the region of possible linkage
extends as far as 8p23-11 (Kaufmann et al., 1998; Gurling
et al., 2001). In addition, a genome wide screen for severe
BPI in the CVCR population showed evidence for a
possible BPI gene locus on 8p (Ophoff et al., 2002). Given
these interesting findings from previous studies, this
study analyzed a new set of individuals with a history of
psychosis from the CVCR, predominantly those with SC,
in order to identify possible discrete genetic loci for
psychotic disorders along chromosome 8, using LD
screening techniques.
This study identified four distinct chromosomal regions
showing possible association with putative SC genes on
chromosome 8: region I at 8p23.1, region II at 8p21.3,
region III at 8q13.3 and region IV at 8q24.3. Expansion of
the phenotype, to include all available individuals with
any history of psychosis (SC, BPI, schizoaffective bipolar,
schizoaffective depressed, psychosis not otherwise speci-
fied, major depression with psychosis), resulted in the
same four regions showing association. Only region I
(D8S542) showed stronger evidence of association (by an
order of magnitude) when the narrower phenotypic
definition (SC) was used. Except for region IV, all regions
in which association was detected in the current study
overlap with regions previously reported to be in linkage
with SC (Kendler et al., 1996; Blouin et al., 1998;
Kaufmann et al., 1998; Brzustowicz et al., 1999; Gurling
et al., 2001). The regions suggested by these earlier
studies cover wide areas, expanding over up to 50 cM,
leading to difficulties in fine mapping and gene
identification. The existence of several susceptibility
genes in a relatively small chromosomal region may
increase the power to find positive linkage signals in the
area, which may be the reason why chromosome 8 has
been continuously reported to be associated with SC.
When LD techniques are used in isolated populations,
finer localization of susceptibility loci may be achieved
and more than one gene can be identified in a given
chromosomal region. The current results suggest there
may indeed be more than one SC gene locus on
chromosome 8, even in a relatively homogeneous
population such as the CVCR. One should interpret the
findings of the current study with caution however, given
the low thresholds set for identifying possible SC loci.
The strongest evidence of association with SC and/or all
psychosis in the current study was obtained in the area of
region I. Three back-to-back markers in our study
(D8S1825, D8S542 and D8S503) gave positive evidence
of association in this region, and D8S503 also showed
evidence of LD (by DISLAMB) to the SC phenotype.
Marker D8S503 is the same marker that yielded the most
significant finding of association in a genome-wide LD
screen of BPI in the CVCR population (Ophoff et al.,2002). Furthermore, it is interesting that the evidence of
association in this area, at marker D8S1825, appears to
increase by an order of magnitude when the affected
sample includes only cases with a history of mania. These
results, together with the previous findings of linkage of
this region with SC (Kaufmann et al., 1998; Gurling et al.,2001) and BP (Ophoff et al., 2002), indicate that the
Region I loci may be associated with psychosis (in
particular psychotic disorders which have shown a history
of mania at some point), rather than to SC or BP
specifically.
The present results provide evidence of association with
SC and/or psychosis in the region of 8p21.3 (Region II,
D8S258 and D8S282). Stratification of the affected
psychotic sample showed segregation of association at
this locus, which appeared to be preferentially associated
with non-manic psychosis.
The current study provides substantial evidence for a SC
locus in Region III (from 82.26 to 87.54 cM on the
166 Psychiatric Genetics 2006, Vol 16 No 4
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Marshfield map). Three markers in this region pass the a
priori thresholds (Pr 0.05) for association and LD
(D8S1841, D8S1117 and D8S543). The level of evidence
for LD at these markers appears to increase when the
phenotype of ‘psychotic disorder’ without a history of
mania is analyzed, suggesting this locus may be relevant
primarily for non-manic psychotic disorders. Two addi-
tional markers, approximately 10 cM centromeric to
D8S543, D8S1705 and D8S275, which did not appear
to be associated with the SC or overall psychosis
phenotypes, also appeared to be associated with non-
manic psychosis. Whether these markers represent
association to yet another susceptibility gene on chromo-
some 8 or are associated to the same putative gene as
markers D8S543 and D8S1117 remains to be determined.
In the case of Region IV, the only reports of association
with psychotic disorders near this area come from linkage
studies with BP (Cichon et al., 2001; Dick et al., 2003).
These studies obtained positive linkage in the region of
8q24, approximately 17 cM away from marker D8S1836,
the marker yielding positive association in the current
study. As Region IV in our current study has only one
marker showing possible association to SC and no marker
showing evidence of LD at Pr 0.05, the evidence for a
SC locus in the CVCR is the least compelling of the four
regions. Additional markers, tightly linked to D8S1836,
need to be analyzed in order to evaluate whether this
region merits further study with regard to SC or other
psychotic phenotypes.
In the present study, evidence of association at a P value
of < 0.05 was not found in the region where the
neuregulin 1 gene is located (Stefansson et al., 2002).
Evidence of association (by CLUMP) and LD (by
DISLAMB) for marker D8S505, which is approximately
0.4 cM from neuregulin 1, however, was found at
significance levels slightly above 0.05. Furthermore, the
likelihood-ratio test revealed l values > 0 in this region.
As described in the methods section, this initial screen
has substantial power to detect loci (at P < 0.05) only for
loci in which 50% or more of the participants have
inherited a SC predisposition gene in common from a
specific CVCR ancestor. SC susceptibility genes shared
by less than 50% of the participants may still show
evidence of LD (and association) in this sample, but will
not necessarily pass the ‘0.05’ threshold. Given the prior
evidence (Stefansson et al., 2002) for the involvement of
neuregulin 1 in SC, and the results found for D8S505 in
the current study, further investigation of the neuregulin
1 gene region in this population is warranted.
In conclusion, this report presents the results of a LD
analysis of chromosome 8 using a founder population and
detailed phenotype analysis to identify discrete regions
most likely to harbor genes for psychotic disorders on
chromosome 8. The least stringent screen in this study
(5 cM screen) identified four distinct chromosomal
regions showing evidence of association to the phenotype
of SC in the CVCR. When more stringent evidence is
required (more than one closely linked marker showing
evidence of association at P < 0.05, at least one of those
markers showing evidence of association using the more
conservative transmission disequilibrium test, and at least
one of those markers showing evidence of LD at P < 0.05,
the present study identifies two distinct regions, 8p23.1
and 8q13.3, as the strongest candidates for further
attempts at identifying SC genes in the CVCR. The
8q13.3 locus may contain two discrete genes related to
non-manic psychotic disorders. In addition, three other
loci, including the neuregulin 1 locus, merit further study
within this population, in order to determine whether
preliminary evidence of association to SC in this sample
reflects actual SC gene loci or false positives. The
statistical significance of our results should be considered
relative but not absolute, as the P values are not corrected
for multiple testing nor confirmed by simulation. Future
analyses of this and other ‘founder’ populations, with
more finely spaced markers, utilization of newer statis-
tical techniques (such as FBAT) that permit multiple
affected individuals to be included in family-based
association analyses, as well as expansion of the sample
and comparison with genome wide results, should be
undertaken to further prioritize regions for future study.
The results of the present study also suggest that the use
of the mania syndrome to refine the psychosis phenotype
may provide a means of improving the methodology used
to identifying genes that underlie the psychotic spectrum
of psychiatric illnesses.
AcknowledgementsWe are indebted to the patients and family members who
participated in this study. We also thank the hospitals and
clinics of Costa Rica (in particular, the Instituto Nacional
de Psiquiatria in Pavas and the Hospital Calderon Guardia
in San Jose) and their excellent clinical staffs for making
this study possible. We also acknowledge the contribu-
tions of the following clinical and statistical researchers to
the completion of this project: Dr Israel Katz (San
Francisco General Hospital, San Francisco, California),
Drs Sophia Vinogradov and Carol Mathews (University of
California at San Francisco), Dr Jean Jacques Garbarz
(Department of Mental Health, San Francisco, Califor-
nia), Dr Rodolfo Salazar-Fonseca (University of Costa
Rica), Drs Rigoberto Castro and J. Saenz (Instituto
Nacional de Psiquiatria de Costa Rica), Drs Alec Miller
and Charles Bowden (University of Texas Health Science
Center at San Antonio) and Maureen O’Connell (South-
west Foundation for Biomedical Research. We thank the
following for their assistance with laboratory work (DNA
extraction, marker testing and creation of cell cultures)
critical to the success of the study: Reinaldo Pereira
LD analysis of chromosome 8 in Costa Rica Walss-Bass et al. 167
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
(University of Costa Rica), Yazmin Ench and Julie
Wisdom (University of Texas Health Science Center at
San Antonio).
ReferencesBlouin JL, Dombroski BA, Nath SK, Lasseter VK, Wolyniec PS, Nestadt G, et al.
(1998). Schizophrenia susceptibility loci on chromosomes 13q32 and 8p21.Nat Genet 20:70–73.
Boteva K, Lieberman J (2003). Reconsidering the classification of schizophreniaand manic depressive illness: a critical analysis and new conceptual model.World J Biol Psychiatry 4:81–92.
Brzustowicz LM, Honer WG, Chow EW, Little D, Hogan J, Hodgkinson K,Bassett AS (1999). Linkage of familial schizophrenia to chromosome 13q32.Am J Hum Genet 65:1096–1103.
Cichon S, Schumacher J, Muller DJ, Hurter M, Windemuth C, Strauch K, et al.(2001). A genome screen for genes predisposing to bipolar affective disorderdetects a new susceptibility locus on 8q. Hum Mol Genet 10:2933–2944.
DeLisi LE, Mesen A, Rodriguez C, Bertheau A, LaPrade B, Llach M, et al. (2002).Genome-wide scan for linkage to schizophrenia in a Spanish-origin cohortfrom Costa Rica. Am J Med Genet 114:497–508.
Dick DM, Foroud T, Flury L, Bowman ES, Miller MJ, Rau NL, et al. (2003).Genomewide linkage analyses of bipolar disorder: a new sample of 250pedigrees from the National Institute of Mental Health Genetics Initiative. AmJ Hum Genet 73:107–114.
Escamilla MA, Spesny M, Reus V, Gallegos A, Meza L, Molina J, et al. (1996). Useof linkage disequilibrium approaches to map genes for bipolar disorder in theCosta Rican population. Am J Med Genet 67:244–253.
Escamilla MA, McInnes LA, Spesny M, Reus V, Service SK, Shimayoshi N, et al.(1999). Assessing the feasibility of linkage disequilibrium methods formapping complex traits: an initial screen for bipolar disorder loci onchromosome 18. Am J Hum Genet 64:1670–1678.
Escamilla MA, Batki S, Reus VI, Spesny M, Molina J, Service S, et al. (2002).Comorbidity of bipolar disorder and substance abuse in Costa Rica:pedigree- and population-based studies. J Affect Disord 71:71–83.
Escamilla MA (2005). Population isolates: their special valve for locating genesfor bipolar disorder. Bipolar Disord 3(6):299–317.
Freimer NB, Reus V, Escamilla MA, McInnes LA, Spesny M, Leon P, et al. (1996).Genetic mapping using haplotype, association and linkage methodssuggests a locus for severe bipolar disorder (BP1) at 18q22-q23. NatGenet 12:436–441.
Gerber DJ, Hall D, Miyakawa T, Demars S, Gogos JA, Karayiorgou M, Tonegawa S(2003). Evidence for association of schizophrenia with genetic variation in the8p21.3 gene, PPP3CC, encoding the calcineurin gamma subunit. Proc NatlAcad Sci USA 100:8993–8998.
Gershon ES, Badner JA (2001). Progress toward discovery of susceptibilitygenes for bipolar manic-depressive illness and schizophrenia. CNS Spectr6(12):965–968.
Gurling HM, Kalsi G, Brynjolfson J, Sigmundsson T, Sherrington R, Mankoo BS,et al. (2001). Genomewide genetic linkage analysis confirms the presence ofsusceptibility loci for schizophrenia, on chromosomes 1q32.2, 5q33.2, and8p21-22 and provides support for linkage to schizophrenia, on chromosomes11q23.3-24 and 20q12.1-11.23. Am J Hum Genet 68:661–673.
Howes OD, McDonald C, Cannon M, Arseneault L, Boydell J, Murray RM (2004).Pathways to schizophrenia: the impact of environmental factors. Int JNeuropsychopharmacol vol 7(Suppl 1):S7–S13.
Katsu T, Ujike H, Nakano T, Tanaka Y, Nomura A, Nakata K, et al. (2003). Thehuman frizzled-3 (FZD3) gene on chromosome 8p21, a receptor gene forWnt ligands, is associated with the susceptibility to schizophrenia. NeurosciLett 353:53–56.
Kaufmann CA, Suarez B, Malaspina D, Pepple J, Svrakic D, Markel PD, et al.(1998). NIMH Genetics Initiative Millennium Schizophrenia Consortium:linkage analysis of African-American pedigrees. Am J Med Genet 81:282–289.
Kendler KS, MacLean CJ, O’Neill FA, Burke J, Murphy B, Duke F, et al. (1996).Evidence for a schizophrenia vulnerability locus on chromosome 8p in the
Irish Study of High-Density Schizophrenia Families. Am J Psychiatry153:1534–1540.
Kendler KS, Karkowski LM, Walsh D (1998). The structure of psychosis: latentclass analysis of probands from the Roscommon family study. Arch GenPsychiatry 55:492–499.
Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al.(1995). Lifetime and 12-month prevalence of DSM-III-R psychiatric disordersin the United States. Arch Gen Psychiatry 51:8–19.
Laird NM, Horvath S, Xu X (2000). Implementing a unified approach tofamily-based tests of association. Genet Epidemiol 19 (Suppl 1):S36–S42.
Lander E, Kruglyak L (1995). Genetic dissection of complex traits: guidelines forinterpreting and reporting linkage results. Nat Genet 11:241–247.
Leon PE, Raventos H, Lynch E, Morrow J, King MC (1992). The gene for aninherited form of deafness maps to chromosome 5q31. Proc Natl Acad SciUSA 89:5181–5184.
Mathews CA, Revs VI, Bejarano J, Escamilla MA, Fournier E, Herrera LD, et al.(2004). Genetic studies of europsychiatric disorders in Costa Rica: a modelfor the use of isolated populations. Psychiatr Genet 14(1):13–23.
Nakata K, Ujike H (2004). The human dihydropyrimidinase-related protein 2(DRP-2) gene on chromosome 8p21 is associated with paranoid-typeschizophrenia [Review]. Nihon Shinkei Seishin Yakurigaku Zasshi 24:33–37.
Nurnberger JI Jr, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG,Harkavy-Friedman J, et al. (1994). Diagnostic interview for genetic studies:rationale, unique features, and training, NIMH Genetics Initiative. Arch GenPsychiatry 51:849–859.
Ophoff RA, Escamilla MA, Service SK, Spesny M, Meshi DB, Poon W, et al.(2002). Genomewide linkage disequilibrium mapping of severe bipolardisorder in a population isolate. Am J Hum Genet 71:565–574.
Pulver AE, Lasseter VK, Kasch L, Wolyniec P, Nestadt G, Blouin JL, et al. (1995).Schizophrenia: a genome scan targets chromosomes 3p and 8p as potentialsites of susceptibility genes. Am J Med Genet 60:252–260.
Pulver AE, Mulle J, Nestadt G, Swartz KL, Blouin JL, Dombroski B, et al. (2000).Genetic heterogeneity in schizophrenia: stratification of genome scan datausing co-segregating related phenotypes. Mol Psychiatry 5:650–653.
Service SK, Temple-Lang DW, Freimer NB, Sandkuijl LA (1999). The genomewide distribution of background linkage disequilibrium in a population isolate.Hum Mol Genet 10:545–551.
Sham PC, Curtis DR (1995). An extended transmission/disequilibrium test (TDT)for multi-allelic marker loci. Ann Hum Genet 59:323–336.
Shaw SH, Kelly M, Smith AB, Shields G, Hopkins PJ, Loftus J, et al. (1998). Agenome-wide search for schizophrenia susceptibility genes. Am J Med Genet81:364–376.
Spielman RS, McGinnis RE, Ewens WJ (1993). Transmission test for linkagedisequilibrium: the insulin gene region and insulin dependent diabetesmellitus (IDDM). Am J Hum Genet 52:506–516.
Stefansson H, Sigurdsson E, Steinthorsdottir V, Bjornsdottir S, Sigmundsson T,Ghosh S, et al. (2002). Neuregulin 1 and susceptibility to schizophrenia. AmJ Hum Genet 71:877–892.
Swann AC, Janicak PL, Calabrese JR, Bowden CL, Dilsaver SC, Morris DD, et al.(2001). Structure of mania: depressive, irritable, and psychotic clusters withdifferent retrospectively-assessed course patterns of illness in randomizedclinical trial participants. J Affect Disord 67:123–132.
Terwilliger JD (1995). A powerful likelihood method for the analysis of linkagedisequilibrium between trait loci and one or more polymorphic marker loci.Am J Hum Genet 56:777–787.
Uhrhammer N, Lange E, Porras O, Naeim A, Chen X, Sheikhavandi S, et al.(1995). Sublocalization of an ataxia-telangiectasia gene distal to D11S384by ancestral haplotyping in Costa Rican families. Am J Hum Genet57:103–111.
Walss-Bass C, Escamilla MA, Raventos H, Montero PA, Armas R, Dassori A, et al.(2005). Evidence of genetic overlap of schizophrenia and bipolar disorder:linkage disequilibrium analysis of chromosome 18 in the Costa Ricanpopulation. Am J Med Genet 1398:54–60.
Wyatt RJ, Henter I, Leary MC, Taylor E (1995). An economic evaluation ofschizophrenia–1991. Soc Psychiatry Psychiatr Epidemiol 30:196–205.
Yang J, Si T, Ling Y, Ruan Y, Han Y, Wang X, et al. (2003). Association study ofthe human FZD3 locus with schizophrenia. Biol Psychiatry 54:1298–1301.
168 Psychiatric Genetics 2006, Vol 16 No 4
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.