High HIV Prevalence, Suboptimal HIV Testing, and Low Knowledge of HIV-Positive Serostatus Among...
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of High HIV Prevalence, Suboptimal HIV Testing, and Low Knowledge of HIV-Positive Serostatus Among...
High HIV Prevalence Suboptimal HIV Testing and LowKnowledge of HIV-Positive Serostatus Among Injection DrugUsers in St Petersburg Russia
Linda M NiccolaiDepartment of Epidemiology and Public Health Center for Interdisciplinary Research on AIDSYale School of Public Health 60 College Street New Haven CT 06520 USA
Olga V ToussovaThe Biomedical Center St Petersburg Russia
Sergei V VerevochkinThe Biomedical Center St Petersburg Russia
Russell BarbourDepartment of Epidemiology and Public Health Center for Interdisciplinary Research on AIDSYale School of Public Health 60 College Street New Haven CT 06520 USA
Robert Heimer andDepartment of Epidemiology and Public Health Center for Interdisciplinary Research on AIDSYale School of Public Health 60 College Street New Haven CT 06520 USA
Andrei P KozlovThe Biomedical Center St Petersburg RussiaLinda M Niccolai Lindaniccolaiyaleedu
AbstractThe purpose of this analysis was to estimate human immunodeficiency virus (HIV) prevalence andtesting patterns among injection drug users (IDUs) in St Petersburg Russia HIV prevalenceamong 387 IDUs in the sample was 50 Correlates of HIV-positive serostatus includedunemployment recent unsafe injections and historycurrent sexually transmitted infectionSeventy-six percent had been HIV tested but only 22 of those who did not report HIV-positiveserostatus had been tested in the past 12 months and received their test result Correlates of thismeasure included recent doctor visit and having been in prison or jail among men Among the 193HIV-infected participants 36 were aware of their HIV-positive serostatus HIV prevalence ishigh and continuing to increase in this population Adequate coverage of HIV testing has not beenachieved resulting in poor knowledge of positive serostatus Efforts are needed to betterunderstand motivating and deterring factors for HIV testing in this setting
KeywordsRussia Injection drug users HIV prevalence HIV testing HIV serostatus Knowledge
copy Springer Science+Business Media LLC 2008Correspondence to Linda M Niccolai Lindaniccolaiyaleedu
NIH Public AccessAuthor ManuscriptAIDS Behav Author manuscript available in PMC 2011 June 16
Published in final edited form asAIDS Behav 2010 August 14(4) 932ndash941 doi101007s10461-008-9469-y
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
IntroductionTesting for human immunodeficiency virus (HIV) infection to increase individualsrsquoawareness of HIV-positive serostatus is a key component of the global strategy to reduce theimpact of the AIDS pandemic (Janssen et al2001 UNAIDS 2004 WHO 2002) Earlydetection of HIV infection in individuals is essential for providing linkages to HIV-relatedsupport care and treatment and for preventing further spread of infection Individuals whoknow they are infected can adopt behaviors such as reducing the frequency of unprotectedintercourse and not sharing injecting equipment that will reduce the likelihood oftransmission to other individuals A recent meta-analysis of studies in the United Statesfound that individuals substantially reduce HIV sex risk behaviors after becoming aware ofHIV-positive serostatus (Marks et al 2005) Furthermore another meta-analysis concludedthat behavioral interventions are efficacious in reducing unprotected sex acts among HIV-positive individuals (Crepaz et al 2006) Another way in which knowledge of HIV-positiveserostatus may reduce HIV risk behaviors is through disclosure of positive serostatus to sexor drug partners so that partners may make informed decisions about risk-reductionstrategies Though the evidence for risk reduction in partnerships in which disclosure hasoccurred is more equivocal (Crepaz and Marks 2002) at a minimum it allows for adiscussion about risk reduction Finally there is strong evidence that injection drug users(IDUs) adopt drug-related HIV risk-reduction strategies such as lowered rates of distributiveneedle and syringe sharing when they know they are HIV-positive this is known asldquoinformed altruismrdquo (Des Jarlais et al 2004)
The Russian Federation is an important context in which to examine HIV testing andknowledge of HIV-positive serostatus Russia has had explosive growth in its HIV epidemicsince experiencing the dramatic social and economic change that began in the 1990sAccording to the Russian Federal AIDS Center the cumulative number of officiallyregistered people with HIVAIDS increased from asymp2000 to 417715 from 1996 to 2007(AFEW 2007) making the epidemic in Russia one of the fastest growing epidemicsobserved anywhere in the world (WHO 2005) An estimated 560000ndash1600000 individualsare currently living with HIVAIDS and the adult prevalence is estimated to beapproximately 1 (WHO 2006) The epidemic has been concentrated largely among IDUs(Lowndes et al 2003 Rhodes et al 2002 Shaboltas et al 2006) and currently IDUscomprise approximately 85 of the cumulative number of registered AIDS cases (WHO2005) The HIV epidemic in St Petersburg one of the largest cities in Russia (population42 million) mirrors that of the Russian Federation with HIV prevalence among selectsamples of IDU increasing from lt5prior to 2000 to 30 in 2003 (Abdala et al 2003Shaboltas et al 2006) This dramatic increase in prevalence indicates a very high incidenceand is clearly cause for concern
Little is known about HIV testing patterns and knowledge of HIV-positive serostatus amongIDUs in St Petersburg Therefore the objectives of the present analyses were to (1) providean updated estimate of HIV prevalence among IDUs for the city of St Petersburg (2)describe HIV testing patterns and correlates and (3) estimate accuracy of knowledge ofpositive serostatus These results are needed to better understand the course of the HIVepidemic in St Petersburg and to develop targeted areas for prevention
MethodsThese analyses were based on data collected as part of a larger and ongoing multi-site studycalled Sexual Acquisition and Transmission of HIV-Cooperative Agreement Program(SATH-CAP) The study takes place in St Petersburg Russia and three other field sites inthe USA present analyses are restricted to data collected at the St Petersburg site from
Niccolai et al Page 2
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
November 2005ndashDecember 2006 The overall goal of SATH-CAP is to better understandhow patterns of sexual and drug use behaviors along with other social and environmentalfactors influence the spread of HIVAIDS from people currently at high risk for HIVAIDS(drug users (DUs) and men who have sex with men (MSM)) to other members of the generalpopulation
ParticipantsThe goal of participant recruitment was to achieve a representative sample of DU from thecity of St Petersburg Participants were recruited into the SATH-CAP study using a dual-component form of respondent driven sampling (RDS) (Heckathorn 1997 2007) RDS is achain referral sampling methodology that uses dual incentives and structured coupondisbursement procedures for peer referrals in order to reduce biases that are typicallyinherent in samples of hidden populations Traditional RDS methods were modified in thisstudy to recruit both additional members of the target population (DUs and MSM) as well assex partners of participants Briefly a number of ldquoseedsrdquo who were known DUs or MSMwere recruited by the study staff enrolled and given coupons with study locationinformation to give to their peers (other members of the target population and their sexpartners) Initial seeds included participants from previous studies at the research site(Shaboltas et al 2006) or referrals from agencies providing services to DUs Peers and sexpartners then called the site to schedule an appointment and presented the coupon at thestudy site for eligibility screening and enrollment When potential participants arrived at theproject site the purpose of the study and study procedures were explained and interestedindividuals provided informed consent Participation was confidential Upon completion ofall study procedures participants were reimbursed with gifts worth approximately US$10containing cell phone cards or personal care items They were also given subway tokenscondoms and HIV prevention information
Forty-eight seeds were enrolled and 35 (73) recruited at least one other participantAmong those who recruited at least on other participant (ldquoproductive seedsrdquo) the meannumber of participants recruited from a single seedrsquos chain of recruits was 5 and the medianwas 14 The maximum number of people enrolled in a single seedrsquos chain was 165(minimum = 1) The distribution of the number of waves which can be thought of as ldquostepsrdquofrom the seed in this sample was as follows mean 28 median = 2 minimum = 1maximum = 14 A total of 522 participants were enrolled The eligibility criterion forinclusion in the present analysis was reporting ever having injected drugs which included387 participants (non-IDUs MSM and sex partners were excluded)
MeasuresParticipants completed structured interviews using computer assisted survey interviewingtechnology on laptop computers that took approximately 60ndash120 min to complete Data usedin the present analyses included demographics drug and sex behaviors structural and healthservice utilization and HIV testing history measures Demographic variables included sexage and current housing and employment status Drug use behaviors included use in thepast 30 days age at first use duration of use frequency of use in past 30 days number ofIDU partners in the past 30 days having a new IDU partner in past 30 days and unsafeinjections in past 30 days (defined as sharing needles without using bleach using a singlesyringe to mix or divide drugs or sharing cookers cotton or water) Sex behaviors includedage at first sex number of sex partners in past 6 months new sex partners in past 6 monthshaving ever had sex with a male (among men) and having ever exchanged money or goodsfor sex (among women) and having ever been pregnant Structural and service utilizationvariables included history of incarceration number of doctor visits in past year havinghealth insurance and having ever received drug treatment Questions about HIV testing
Niccolai et al Page 3
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
included having ever been previously tested for HIV number of times tested date of lasttest and knowledge of test results
Results from HIV and sexually transmitted infection (STI) testing were also included in thepresent analyses Pre-test HIV counseling was conducted a blood specimen was collected totest for HIV syphilis hepatitis B and C viruses and a urine specimen was collected to testfor chlamydia and gonorrhea Serum specimens were tested for HIV antibodies by enzyme-linked immunosorbent assay (ELISA) using commercially licensed reagents includingGenscreen HIV 12 (BioRad France) andor Vironostika HIV Uni-Form II plus 0(Biomerieux The Netherlands)Non-reactive specimens were considered to be HIV-negative Specimens that were reactive were further tested with Western blot analysis usingNew Lav Blot HIV-1 (BioRad France) STI testing was done for syphilis gonorrhea andchlamydia Serum samples were tested for syphilis with rapid plasma reagin test (RPR)(Macro-Vue RPR Card Tests Becton Dickinson USA) and Treponema pallidum particleagglutination assay (TPPA) (Serodia-TPPA Fujirebio Japan) samples were consideredpositive for history of syphilis if reactive on both tests Urine specimens were tested forchlamydia and gonorrhea using polymerase chain reaction (Amplicor CTNG Roche USA)All participants were invited to return to the site for post-test counseling to get HIV and STItest results and referrals for additional medical and social services were provided as needed
Statistical AnalysisThe sample was described on demographic drug use and sex behaviors and serviceutilization variables using standard descriptive statistics Participants were considered HIV-positive if their ELISA reactive specimens were confirmed by Western blot To estimatecorrelates of HIV-positive serostatus bivariate and multivariate logistic regression wereused Examined correlates included the demographic drug use and sex behaviors prevalentSTI variables and structural and service utilization variables described above Our initialmodeling strategy was intended to be an exploratory analysis of behavioral correlates Thefinding that none of the behavioral correlates were associated led us to speculate thatstructural factors may be important thus our modeling strategy was revised to includestructural variables Continuous variables were dichotomized for two reasons First becausethe outcome of interest was dichotomous the logistic regression modeling producesestimates that can be interpreted as odds ratios these estimates are most easily interpretedwith dichotomous covariates that compare one level of the covariate to the other levelSecond dichotomizing covariates provides greater statistical power in the regression modelsby minimizing the levels of stratification We used a priori meaningful cut points fordichotomizing Covariates that were associated in the bivariate analysis using the criticalvalue of P lt 020 were included in the initial multivariate model A backward selectionprocedure eliminated covariates that did not remain significant using the critical value of P lt005 to arrive at the final multivariate model
Patterns of HIV testing were described using proportions and medians to estimate theprevalence of having ever been tested the frequency of testing time since last test andknowledge of positive serostatus Bivariate and multivariate logistic regression were used todetermine correlates of having had a recent HIV test (in the past 12 months) and havingreceived results among individuals who self-reported being HIV-negative using the samemodeling strategy described above To estimate the accuracy of knowledge of positive HIVserostatus we related self-reported status to laboratory results using blood specimenscollected at the time of the interview We estimated with a 95 confidence interval theproportion of HIV-infected individuals who self-reported correct knowledge of their HIV-positive status
Niccolai et al Page 4
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Because we used RDS for recruitment of IDUs weighting procedures are available (RDSAnalyzing Tool RDSAT software version 56) to adjust the sample for recruitmentprobabilities to obtain estimates that are representative of the underlying target populationUsing a weighting procedure that took into account our modified RDS methodology wefound that the weighted and unweighted estimates of sex age and HIV status proportions inthis sample did not differ substantially unweighted estimates for proportions male lt25years of age and HIV-infected were 74 33 and 50 respectively compared toweighted estimates of 75 32 and 49 respectively Furthermore estimation of 95confidence intervals for each of these estimates indicated substantial overlap and a similarrange between weighted and unweighted bounds due to virtually identical standarddeviations of weighted and unweighted estimates (data not shown) Therefore we usedunweighted estimates for all subsequent analyses
ResultsParticipant Characteristics and HIV Prevalence
The sample (n = 387) was predominantly male (74) and the mean age was 288 (standarddeviation 65) years Nearly one-third (31) of the sample was currently employed full- orpart-time The vast majority of the sample 91 reported injection drug use in the past 30days and 80 reported injecting heroin Nearly half the sample (48) reported age at firstinjection 18 years or younger The median time since initiating injection drug use was 8years and 65 reported at least one instance of some form of unsafe injection in the past 30days Age at first sex was15 years or younger for 53 of the sample 38 had multiple sexpartners and 49 had a new sex partner in the past 6 months Eleven male IDUs (4)reported having ever had male sex partners and 7 female IDUs (7) reported having everreceived money or other goods as payment for sex due to these low numbers these factorswere not considered covariates in subsequent analyses Health care utilization characteristicsare as follows 56 had a doctor visit in the past 12 months 79 had health insurance and30 had ever received drug treatment Thirty-seven percent of the sample had ever been inprison or jail
Eighteen percent (n = 68) of the sample tested positive for syphilis chlamydia or gonorrheaA total of 196 specimens were ELISA positive for HIV and 1 was indeterminate Of the 197specimens tested by Western blot 193 were positive 3 were indeterminate and 1 wasnegative We considered the indeterminate results to be negative (by excluding them fromthe numerator but including them in the denominator) to produce a conservative estimateand thus estimated HIV prevalence to be 50 (193387) A total of 290 participants (75)returned for their HIV test results Correlates are presented in Table 1 In the adjustedanalysis current unemployment (OR = 197 95 CI = 126ndash308 P lt 01) reporting unsafeinjections in past 30 days (OR = 154 95 CI = 10 236 P lt 05) and prevalent infectionwith chlamydia or gonorrhea or prevalent or past diagnosis of syphilis (OR = 196 95 CI= 112ndash342 P lt 05) were associated with HIV-positive serostatus
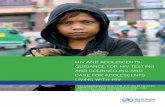
HIV Testing Patterns and CorrelatesSeventy-six percent (76) of the sample reported having ever been tested for HIV prior toenrollment in the present study Of those who had been tested (n = 295) the median numberof previous tests was 2 (range 1ndash55) and 36 of the sample had only been tested once Themedian time since last test was 8 months (range 0ndash96) and 30 had not been tested in thepast 12 months Twenty-four percent of those who had been tested reported knowing thatthey were HIV-positive 60 reported that they were HIV-negative and 17 did not knowtheir status (Fig 1)
Niccolai et al Page 5
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
To examine factors associated with HIV testing patterns we considered the outcome ofinterest to have been tested in the past year and received test results among those who didnot self-reported HIV-positive serostatus (n = 315) Sixty-nine individuals (22) had beentested in the past 12 months and received their test result Results of the bivariate analysisare presented in Table 2 To account for the association with having ever been pregnant amultivariate model on the entire sample was run without this covariate and stratified modelswere run for men and women separately (Table 3) In the entire sample only having adoctor visit in the past12 months remained significantly associated with recent testing (OR =306 95 CI = 168ndash559 P lt 01)Among men having a doctor visit in the past 12 months(OR = 366 95 CI = 175ndash770 P lt 01) and history of incarceration (OR = 212 95 CI= 108ndash442 P lt 05) were associated with recent testing and among women having everbeen pregnant was marginally associated (OR = 356 95 CI = 074ndash172 P lt 10)
Knowledge of HIV-Positive SerostatusAccuracy of knowledge of positive serostatus is depicted Fig 1 Of the 72 who self-reportedpositive serostatus 70 (97) were HIV-positive by serology Among the 315 participantswho did not report positive serostatus 123 (24) were HIV-positive This included 30participants who reported not knowing their status (60 of this group) 52 participants whoreported having never been tested (57 of this group) and 41 participants who reportedthey were HIV-negative (24 of this group) The proportion of HIV-infected participantswho self-reported that they knew they were HIV-infected was 36 (70193) with a 95confidence interval of 30ndash43 In other words 64 (123193) of HIV-positive individualsin this sample did not know their HIV status
DiscussionA key finding of this study is the HIV prevalence estimate of 50 among IDUs in StPetersburg Russia This updated estimate shows steady increase in comparison withprevious estimates of 11 from data collected in 2000 (Abdala et al 2003) and 30 fromdata collected in 2002 (Shaboltas et al 2006) and indicates continued growth of thisexplosive epidemic It is noteworthy that the study conducted in 2002 also relied heavily onchain referral sampling to access a similar population suggesting a degree of comparabilityin these samples Though we are unable to assess the temporal relationships betweencovariates and HIV status due to the cross-sectional nature of this study the significantlyhigher reporting of recent unsafe injections among those who are HIV-positive signalsconcern for continued transmission While we do not know the injection behaviors ofparticipants during the time in which they acquired HIV their current behaviors suggest thatthe potential for secondary transmission to their drug partners is high Similarly theassociation between STI (history of syphilis or current chlamydiagonorrhea) and HIVinfection suggests a possible role of sexual transmission of HIV among IDU in thispopulation either as a risk factor in the past or signaling the potential for future spread Theextent to which the epidemic will continue to grow and spread to the general population isan important and urgent question that the larger study on which this analysis was based isdesigned to address
A substantial proportion of IDUs in this sample from St Petersburg had not been tested forHIV ever or recently or received their test results Overall 24 had never been tested andamong those who had been tested 30 had not done so in the past year and 17 had notreceived test results These results are comparable to earlier findings from other Russiancities One study conducted in 2003 in the three Russian cities of Moscow Barnaul andVolgograd reported that 25ndash48 of IDUs had not been tested for HIV in the past year andthat 66 of HIV-positive IDUs were unaware of their HIV-positive serostatus (Rhodes et al2006) Our findings contribute to this growing body of knowledge by examining testing
Niccolai et al Page 6
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
patterns in a different city and by examining correlates neither of which had previouslybeen done Also given the highly dynamic and rapidly increasing HIV epidemic in Russiaour analysis that provides an updated estimate is needed to continually monitor the situationSadly our findings suggest that previously limited testing coverage has not increased overtime despite continued growth of the epidemic It should also be noted that our estimate of24 having never been tested is substantially higher than the 7 estimate from 5 US cities(Heimer et al 2007) This relatively low frequency of HIV testing has persisted in a high-risk group despite an emphasis on routine HIV testing in Russia According to the WHOapproximately 20 million HIV tests are conducted annually in Russia (WHO 2005) acountry that has a total population of approximately 142 million Though voluntarycounseling and testing (VCT) is guaranteed by Russian law this may not be widelyaccessible or conducted on a truly voluntary basis Furthermore IDUs may not seek HIVtesting for a variety of reasons For example substantial stigma in the general populationtoward people with HIVAIDS may make knowing onesrsquo status undesirable (Balabanova etal 2006) Lack of access to affordable antiretroviral treatment may be another barrier toaccessing VCT to learn onersquos status The WHO currently estimates that approximately 10of those in need of antiretroviral treatment receive it in Russia (WHO 2006) in large partbecause generic drugs are not registered and treatment is not affordable to many RussiansHowever increased governmental commitments to and financial support for treatment inRussia have recently occurred and these efforts are likely to increase the proportion ofpeople who may receive treatment As this occurs the acceptability of HIV testing becomesincreasingly important
The finding that none of the demographic or drug and sex risk behaviors was correlated withHIV testing patterns is evidence of our limited understanding of motivations for and barriersto HIV testing The lack of identified behavioral correlates in the present study may reflectthe large volume of routine tests that is conducted in Russia This is supported by ourfinding that having a recent doctor visit history of incarceration and having been pregnantmdashall events that provide contact with institutions (medical or other) that provide routinetestingmdashwere in fact associated with recent testing It is possible that structuralcharacteristics are more important determinants of HIV testing than individual preferencesthough this has not been adequately studied
Despite the large-scale national investment in routine HIV testing the low testing and returnrates have resulted in poor knowledge of positive HIV serostatus among IDUs in StPetersburg We found that 24 of individuals who self-reported that they were HIV-negative were actually HIV-positive this proportion was substantially higher amongindividuals who had been tested but not received results (60) and individuals who hadnever been tested (57) Overall nearly two-thirds (64) of HIV-infected individuals didnot know their positive serostatus These findings are also comparable to findings in otherstudies from the region including the same proportion (two-thirds) of IDUs being unawareof positive HIV status in the Russian three city study (Rhodes et al 2006) and three-quartersof IDUs being unaware of their positive status in another Russian city (Rhodes et al 2002)Again it is discouraging that these estimates have not improved as the epidemic hascontinued to expand These findings have implications for secondary prevention in thatindividuals who do not know they are HIV-positive may not ad opt risk-reduction behaviorsthat can prevent transmission of HIV to their drug and sex partners The usefulness of thistype of secondary prevention has been evaluated and reviewed in other countries (Crepaz etal 2006 Marks et al 2005) but has not been evaluated in the Russian setting
Several possible limitations of these findings should be noted First our results may notgeneralize to IDUs outside of St Petersburg though they may apply to areas of similarepidemiologic characteristics and others are encouraged to consider the applicability of
Niccolai et al Page 7
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
these findings to their own settings Given the recent rapid rise in HIV in this region and thepossible substantial role this region may play in the current wave of the HIV pandemic ourfindings provide insight into strategies that may be needed to reduce the impact of HIVincluding HIV testing Second though our recruitment strategy (RDS) is designed toachieve a representative sample of the underlying population the degree to which thisoccurred is unknown although the initial weighting analysis suggests heterophily at a levelconsistent with achieving representativeness (Heckathorn 2002) Third HIV testing historywas obtained by self-report and may be subject to unintentionally inaccurate responses dueto misreport or forgetting On the other hand the effect of intentional misreport due to socialdesirability should be minimized by the anonymous nature of data collection and use ofCASI technology Fourth the lack of identified significant correlates of HIV testing patternsmay be due to insufficient sample size for the required statistical power or loss ofinformation resulting from dichotomization of covariates Despite these potentialmethodological limitations these results present the first look at HIV testing patterns amongIDU in St Petersburg a large city with a high burden of HIV infection and an updatedprevalence estimate from earlier reports
ConclusionsThese data show sub-optimal coverage of HIV testing in a high-risk population in a settingof explosive growth and they also reflect our limited understanding of motivations anddeterrents for HIV testing Future work must address targeted testing and counselingprograms and understanding attitudes toward HIV testing by IDUs in Russia includingperceptions of the relative balance between potential benefits and harms This will becomeincreasingly important as progress in antiretroviral scale-up increases Until this occursemphasizing the potential benefit of knowing onersquos status for secondary prevention may beuseful Finally addressing the issue of stigma toward people living with HIVAIDS isanother great but necessary challenge in increasing the acceptability of HIV testing amongIDUs in Russia
AcknowledgmentsThis work was supported by a grant from National Institutes of Health (U01DA017387) to Yale School ofMedicine and The Biomedical Center The authors acknowledge the dedication of the SATH-CAP research team atthe Biomedical Center St Petersburg Russia The authors also thank investigators at other sites of the SATH-CAPresearch project including RAND Corporation Research Triangle Institute University of California at Los Angelesand University of Illinois Chicago
ReferencesAbdala N Carney JM Durante AJ Klimov N Ostrovski D Somlai AM et al Estimating the
prevalence of syringe-borne and sexually transmitted diseases among injection drug users in StPetersburg Russia International Journal of STD and AIDS 2003 14697ndash703 [PubMed14596774]
AIDS Foundation East-West Officially registered HIV cases in Russian Federation 1 January 1987ndash31May 2007 as reported by the Russian Federal AIDS Center 2007 Available at httpwwwafeworg
Balabanova Y Coker R Atun RA Drobniewski F Stigma and HIV infection in Russia AIDS Care2006 18846ndash852 [PubMed 16971297]
Crepaz N Lyles CM Wolitski RJ Passin WF Rama SM Herbst JH et al Do preventioninterventions reduce HIV risk behaviors among people living with HIV A metanalytic review ofcontrolled trials AIDS (London England) 2006 20143ndash157
Crepaz N Marks G Towards an understanding of sexual risk behavior in people living with HIV Areview of social psychological and medical findings AIDS (London England) 2002 16135ndash149
Niccolai et al Page 8
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Des Jarlais DC Perlis T Arasteh K Hagan H Milliken J Braine N et al ldquoInformed altruismrdquo andldquopartner restrictionrdquo in the reduction of HIV infection in injecting drug users entering detoxificationtreatment in New York City 1990ndash2001 Journal of Acquired Immune Deficiency Syndromes2004 35158ndash166 [PubMed 14722449]
Heckathorn DD Respondent-driven sampling A new approach to the study of hidden populationsSocial Problems 1997 44174ndash199
Heckathorn DD Respondent-driven sampling II Deriving valid population estimates from chainreferral samples of hidden populations Social Problems 2002 4911ndash34
Heckathorn DD Extensions of respondent-driven sampling Analyzing continuous variables andcontrolling for differential recruitment Sociological Methodology 2007 37151ndash208
Heimer R Grau LE Curtin E Khoshnood K Singer M Assessment of HIV testing of urban injectiondrug users Implications for expansion of HIV testing and prevention efforts American Journal ofPublic Health 2007 97110ndash116 [PubMed 17138916]
Janssen RS Holtgrave DR Valdiserri RO The serostatus approach to fighting the HIV epidemicprevention strategies for infected individuals American Journal of Public Health 2001 911019ndash1024 [PubMed 11441723]
Lowndes CM Renton A Alary M Rhodes T Garnett G Stimson G Conditions for widespreadheterosexual spread of HIV in the Russian Federation Implications for research monitoring andprevention The International Journal on Drug Policy 2003 1445ndash62
Marks G Crepaz N Senterfitt JW Janssen RS Meta-analysis of high-risk sexual behaviors in personsaware and unaware they are infected with HIV in the United States Journal of Acquired ImmuneDeficiency Syndromes 2005 39446ndash453 [PubMed 16010168]
Rhodes T Lowndes CM Judd A Mikhailova LA Sarang A Rylkov A et al Explosive spread andhigh prevalence of HIV infection among injecting drug users in Togliatti City Russia AIDS(London England) 2002 16F25ndashF31
Rhodes T Platt L Maximova S Koshkina E Latishevskaya N Hickman M et al Prevalence of HIVhepatitis C and syphilis among injecting drug users in Russia A multi-city study Addiction(Abingdon England) 2006 101252ndash266
Shaboltas AV Toussova OV Hoffman IF Heimer R Verevochkin SV Ryder RW et al HIVprevalence social demographic and behavioral correlates and recruitment methods amonginjection drug users in St Petersburg Russia Journal of Acquired ImmununodeficiencySyndromes 2006 41657ndash663
United Nations Joint Program on HIVAIDS UNAIDSWHO policy statement on HIV testing 2004World Health Organization WHO consultation on increasing access to HIV testing and counseling
2002World Health Organization Russian Federation Summary country profile for HIVAIDS treatment
scale-up 2005World Health Organization Epidemiologic fact sheet 2006 Russian Federation 2006
Niccolai et al Page 9
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig 1Classification of IDUs by HIV testing and HIV status(n = 387)
Niccolai et al Page 10
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
IntroductionTesting for human immunodeficiency virus (HIV) infection to increase individualsrsquoawareness of HIV-positive serostatus is a key component of the global strategy to reduce theimpact of the AIDS pandemic (Janssen et al2001 UNAIDS 2004 WHO 2002) Earlydetection of HIV infection in individuals is essential for providing linkages to HIV-relatedsupport care and treatment and for preventing further spread of infection Individuals whoknow they are infected can adopt behaviors such as reducing the frequency of unprotectedintercourse and not sharing injecting equipment that will reduce the likelihood oftransmission to other individuals A recent meta-analysis of studies in the United Statesfound that individuals substantially reduce HIV sex risk behaviors after becoming aware ofHIV-positive serostatus (Marks et al 2005) Furthermore another meta-analysis concludedthat behavioral interventions are efficacious in reducing unprotected sex acts among HIV-positive individuals (Crepaz et al 2006) Another way in which knowledge of HIV-positiveserostatus may reduce HIV risk behaviors is through disclosure of positive serostatus to sexor drug partners so that partners may make informed decisions about risk-reductionstrategies Though the evidence for risk reduction in partnerships in which disclosure hasoccurred is more equivocal (Crepaz and Marks 2002) at a minimum it allows for adiscussion about risk reduction Finally there is strong evidence that injection drug users(IDUs) adopt drug-related HIV risk-reduction strategies such as lowered rates of distributiveneedle and syringe sharing when they know they are HIV-positive this is known asldquoinformed altruismrdquo (Des Jarlais et al 2004)
The Russian Federation is an important context in which to examine HIV testing andknowledge of HIV-positive serostatus Russia has had explosive growth in its HIV epidemicsince experiencing the dramatic social and economic change that began in the 1990sAccording to the Russian Federal AIDS Center the cumulative number of officiallyregistered people with HIVAIDS increased from asymp2000 to 417715 from 1996 to 2007(AFEW 2007) making the epidemic in Russia one of the fastest growing epidemicsobserved anywhere in the world (WHO 2005) An estimated 560000ndash1600000 individualsare currently living with HIVAIDS and the adult prevalence is estimated to beapproximately 1 (WHO 2006) The epidemic has been concentrated largely among IDUs(Lowndes et al 2003 Rhodes et al 2002 Shaboltas et al 2006) and currently IDUscomprise approximately 85 of the cumulative number of registered AIDS cases (WHO2005) The HIV epidemic in St Petersburg one of the largest cities in Russia (population42 million) mirrors that of the Russian Federation with HIV prevalence among selectsamples of IDU increasing from lt5prior to 2000 to 30 in 2003 (Abdala et al 2003Shaboltas et al 2006) This dramatic increase in prevalence indicates a very high incidenceand is clearly cause for concern
Little is known about HIV testing patterns and knowledge of HIV-positive serostatus amongIDUs in St Petersburg Therefore the objectives of the present analyses were to (1) providean updated estimate of HIV prevalence among IDUs for the city of St Petersburg (2)describe HIV testing patterns and correlates and (3) estimate accuracy of knowledge ofpositive serostatus These results are needed to better understand the course of the HIVepidemic in St Petersburg and to develop targeted areas for prevention
MethodsThese analyses were based on data collected as part of a larger and ongoing multi-site studycalled Sexual Acquisition and Transmission of HIV-Cooperative Agreement Program(SATH-CAP) The study takes place in St Petersburg Russia and three other field sites inthe USA present analyses are restricted to data collected at the St Petersburg site from
Niccolai et al Page 2
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
November 2005ndashDecember 2006 The overall goal of SATH-CAP is to better understandhow patterns of sexual and drug use behaviors along with other social and environmentalfactors influence the spread of HIVAIDS from people currently at high risk for HIVAIDS(drug users (DUs) and men who have sex with men (MSM)) to other members of the generalpopulation
ParticipantsThe goal of participant recruitment was to achieve a representative sample of DU from thecity of St Petersburg Participants were recruited into the SATH-CAP study using a dual-component form of respondent driven sampling (RDS) (Heckathorn 1997 2007) RDS is achain referral sampling methodology that uses dual incentives and structured coupondisbursement procedures for peer referrals in order to reduce biases that are typicallyinherent in samples of hidden populations Traditional RDS methods were modified in thisstudy to recruit both additional members of the target population (DUs and MSM) as well assex partners of participants Briefly a number of ldquoseedsrdquo who were known DUs or MSMwere recruited by the study staff enrolled and given coupons with study locationinformation to give to their peers (other members of the target population and their sexpartners) Initial seeds included participants from previous studies at the research site(Shaboltas et al 2006) or referrals from agencies providing services to DUs Peers and sexpartners then called the site to schedule an appointment and presented the coupon at thestudy site for eligibility screening and enrollment When potential participants arrived at theproject site the purpose of the study and study procedures were explained and interestedindividuals provided informed consent Participation was confidential Upon completion ofall study procedures participants were reimbursed with gifts worth approximately US$10containing cell phone cards or personal care items They were also given subway tokenscondoms and HIV prevention information
Forty-eight seeds were enrolled and 35 (73) recruited at least one other participantAmong those who recruited at least on other participant (ldquoproductive seedsrdquo) the meannumber of participants recruited from a single seedrsquos chain of recruits was 5 and the medianwas 14 The maximum number of people enrolled in a single seedrsquos chain was 165(minimum = 1) The distribution of the number of waves which can be thought of as ldquostepsrdquofrom the seed in this sample was as follows mean 28 median = 2 minimum = 1maximum = 14 A total of 522 participants were enrolled The eligibility criterion forinclusion in the present analysis was reporting ever having injected drugs which included387 participants (non-IDUs MSM and sex partners were excluded)
MeasuresParticipants completed structured interviews using computer assisted survey interviewingtechnology on laptop computers that took approximately 60ndash120 min to complete Data usedin the present analyses included demographics drug and sex behaviors structural and healthservice utilization and HIV testing history measures Demographic variables included sexage and current housing and employment status Drug use behaviors included use in thepast 30 days age at first use duration of use frequency of use in past 30 days number ofIDU partners in the past 30 days having a new IDU partner in past 30 days and unsafeinjections in past 30 days (defined as sharing needles without using bleach using a singlesyringe to mix or divide drugs or sharing cookers cotton or water) Sex behaviors includedage at first sex number of sex partners in past 6 months new sex partners in past 6 monthshaving ever had sex with a male (among men) and having ever exchanged money or goodsfor sex (among women) and having ever been pregnant Structural and service utilizationvariables included history of incarceration number of doctor visits in past year havinghealth insurance and having ever received drug treatment Questions about HIV testing
Niccolai et al Page 3
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
included having ever been previously tested for HIV number of times tested date of lasttest and knowledge of test results
Results from HIV and sexually transmitted infection (STI) testing were also included in thepresent analyses Pre-test HIV counseling was conducted a blood specimen was collected totest for HIV syphilis hepatitis B and C viruses and a urine specimen was collected to testfor chlamydia and gonorrhea Serum specimens were tested for HIV antibodies by enzyme-linked immunosorbent assay (ELISA) using commercially licensed reagents includingGenscreen HIV 12 (BioRad France) andor Vironostika HIV Uni-Form II plus 0(Biomerieux The Netherlands)Non-reactive specimens were considered to be HIV-negative Specimens that were reactive were further tested with Western blot analysis usingNew Lav Blot HIV-1 (BioRad France) STI testing was done for syphilis gonorrhea andchlamydia Serum samples were tested for syphilis with rapid plasma reagin test (RPR)(Macro-Vue RPR Card Tests Becton Dickinson USA) and Treponema pallidum particleagglutination assay (TPPA) (Serodia-TPPA Fujirebio Japan) samples were consideredpositive for history of syphilis if reactive on both tests Urine specimens were tested forchlamydia and gonorrhea using polymerase chain reaction (Amplicor CTNG Roche USA)All participants were invited to return to the site for post-test counseling to get HIV and STItest results and referrals for additional medical and social services were provided as needed
Statistical AnalysisThe sample was described on demographic drug use and sex behaviors and serviceutilization variables using standard descriptive statistics Participants were considered HIV-positive if their ELISA reactive specimens were confirmed by Western blot To estimatecorrelates of HIV-positive serostatus bivariate and multivariate logistic regression wereused Examined correlates included the demographic drug use and sex behaviors prevalentSTI variables and structural and service utilization variables described above Our initialmodeling strategy was intended to be an exploratory analysis of behavioral correlates Thefinding that none of the behavioral correlates were associated led us to speculate thatstructural factors may be important thus our modeling strategy was revised to includestructural variables Continuous variables were dichotomized for two reasons First becausethe outcome of interest was dichotomous the logistic regression modeling producesestimates that can be interpreted as odds ratios these estimates are most easily interpretedwith dichotomous covariates that compare one level of the covariate to the other levelSecond dichotomizing covariates provides greater statistical power in the regression modelsby minimizing the levels of stratification We used a priori meaningful cut points fordichotomizing Covariates that were associated in the bivariate analysis using the criticalvalue of P lt 020 were included in the initial multivariate model A backward selectionprocedure eliminated covariates that did not remain significant using the critical value of P lt005 to arrive at the final multivariate model
Patterns of HIV testing were described using proportions and medians to estimate theprevalence of having ever been tested the frequency of testing time since last test andknowledge of positive serostatus Bivariate and multivariate logistic regression were used todetermine correlates of having had a recent HIV test (in the past 12 months) and havingreceived results among individuals who self-reported being HIV-negative using the samemodeling strategy described above To estimate the accuracy of knowledge of positive HIVserostatus we related self-reported status to laboratory results using blood specimenscollected at the time of the interview We estimated with a 95 confidence interval theproportion of HIV-infected individuals who self-reported correct knowledge of their HIV-positive status
Niccolai et al Page 4
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Because we used RDS for recruitment of IDUs weighting procedures are available (RDSAnalyzing Tool RDSAT software version 56) to adjust the sample for recruitmentprobabilities to obtain estimates that are representative of the underlying target populationUsing a weighting procedure that took into account our modified RDS methodology wefound that the weighted and unweighted estimates of sex age and HIV status proportions inthis sample did not differ substantially unweighted estimates for proportions male lt25years of age and HIV-infected were 74 33 and 50 respectively compared toweighted estimates of 75 32 and 49 respectively Furthermore estimation of 95confidence intervals for each of these estimates indicated substantial overlap and a similarrange between weighted and unweighted bounds due to virtually identical standarddeviations of weighted and unweighted estimates (data not shown) Therefore we usedunweighted estimates for all subsequent analyses
ResultsParticipant Characteristics and HIV Prevalence
The sample (n = 387) was predominantly male (74) and the mean age was 288 (standarddeviation 65) years Nearly one-third (31) of the sample was currently employed full- orpart-time The vast majority of the sample 91 reported injection drug use in the past 30days and 80 reported injecting heroin Nearly half the sample (48) reported age at firstinjection 18 years or younger The median time since initiating injection drug use was 8years and 65 reported at least one instance of some form of unsafe injection in the past 30days Age at first sex was15 years or younger for 53 of the sample 38 had multiple sexpartners and 49 had a new sex partner in the past 6 months Eleven male IDUs (4)reported having ever had male sex partners and 7 female IDUs (7) reported having everreceived money or other goods as payment for sex due to these low numbers these factorswere not considered covariates in subsequent analyses Health care utilization characteristicsare as follows 56 had a doctor visit in the past 12 months 79 had health insurance and30 had ever received drug treatment Thirty-seven percent of the sample had ever been inprison or jail
Eighteen percent (n = 68) of the sample tested positive for syphilis chlamydia or gonorrheaA total of 196 specimens were ELISA positive for HIV and 1 was indeterminate Of the 197specimens tested by Western blot 193 were positive 3 were indeterminate and 1 wasnegative We considered the indeterminate results to be negative (by excluding them fromthe numerator but including them in the denominator) to produce a conservative estimateand thus estimated HIV prevalence to be 50 (193387) A total of 290 participants (75)returned for their HIV test results Correlates are presented in Table 1 In the adjustedanalysis current unemployment (OR = 197 95 CI = 126ndash308 P lt 01) reporting unsafeinjections in past 30 days (OR = 154 95 CI = 10 236 P lt 05) and prevalent infectionwith chlamydia or gonorrhea or prevalent or past diagnosis of syphilis (OR = 196 95 CI= 112ndash342 P lt 05) were associated with HIV-positive serostatus
HIV Testing Patterns and CorrelatesSeventy-six percent (76) of the sample reported having ever been tested for HIV prior toenrollment in the present study Of those who had been tested (n = 295) the median numberof previous tests was 2 (range 1ndash55) and 36 of the sample had only been tested once Themedian time since last test was 8 months (range 0ndash96) and 30 had not been tested in thepast 12 months Twenty-four percent of those who had been tested reported knowing thatthey were HIV-positive 60 reported that they were HIV-negative and 17 did not knowtheir status (Fig 1)
Niccolai et al Page 5
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
To examine factors associated with HIV testing patterns we considered the outcome ofinterest to have been tested in the past year and received test results among those who didnot self-reported HIV-positive serostatus (n = 315) Sixty-nine individuals (22) had beentested in the past 12 months and received their test result Results of the bivariate analysisare presented in Table 2 To account for the association with having ever been pregnant amultivariate model on the entire sample was run without this covariate and stratified modelswere run for men and women separately (Table 3) In the entire sample only having adoctor visit in the past12 months remained significantly associated with recent testing (OR =306 95 CI = 168ndash559 P lt 01)Among men having a doctor visit in the past 12 months(OR = 366 95 CI = 175ndash770 P lt 01) and history of incarceration (OR = 212 95 CI= 108ndash442 P lt 05) were associated with recent testing and among women having everbeen pregnant was marginally associated (OR = 356 95 CI = 074ndash172 P lt 10)
Knowledge of HIV-Positive SerostatusAccuracy of knowledge of positive serostatus is depicted Fig 1 Of the 72 who self-reportedpositive serostatus 70 (97) were HIV-positive by serology Among the 315 participantswho did not report positive serostatus 123 (24) were HIV-positive This included 30participants who reported not knowing their status (60 of this group) 52 participants whoreported having never been tested (57 of this group) and 41 participants who reportedthey were HIV-negative (24 of this group) The proportion of HIV-infected participantswho self-reported that they knew they were HIV-infected was 36 (70193) with a 95confidence interval of 30ndash43 In other words 64 (123193) of HIV-positive individualsin this sample did not know their HIV status
DiscussionA key finding of this study is the HIV prevalence estimate of 50 among IDUs in StPetersburg Russia This updated estimate shows steady increase in comparison withprevious estimates of 11 from data collected in 2000 (Abdala et al 2003) and 30 fromdata collected in 2002 (Shaboltas et al 2006) and indicates continued growth of thisexplosive epidemic It is noteworthy that the study conducted in 2002 also relied heavily onchain referral sampling to access a similar population suggesting a degree of comparabilityin these samples Though we are unable to assess the temporal relationships betweencovariates and HIV status due to the cross-sectional nature of this study the significantlyhigher reporting of recent unsafe injections among those who are HIV-positive signalsconcern for continued transmission While we do not know the injection behaviors ofparticipants during the time in which they acquired HIV their current behaviors suggest thatthe potential for secondary transmission to their drug partners is high Similarly theassociation between STI (history of syphilis or current chlamydiagonorrhea) and HIVinfection suggests a possible role of sexual transmission of HIV among IDU in thispopulation either as a risk factor in the past or signaling the potential for future spread Theextent to which the epidemic will continue to grow and spread to the general population isan important and urgent question that the larger study on which this analysis was based isdesigned to address
A substantial proportion of IDUs in this sample from St Petersburg had not been tested forHIV ever or recently or received their test results Overall 24 had never been tested andamong those who had been tested 30 had not done so in the past year and 17 had notreceived test results These results are comparable to earlier findings from other Russiancities One study conducted in 2003 in the three Russian cities of Moscow Barnaul andVolgograd reported that 25ndash48 of IDUs had not been tested for HIV in the past year andthat 66 of HIV-positive IDUs were unaware of their HIV-positive serostatus (Rhodes et al2006) Our findings contribute to this growing body of knowledge by examining testing
Niccolai et al Page 6
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
patterns in a different city and by examining correlates neither of which had previouslybeen done Also given the highly dynamic and rapidly increasing HIV epidemic in Russiaour analysis that provides an updated estimate is needed to continually monitor the situationSadly our findings suggest that previously limited testing coverage has not increased overtime despite continued growth of the epidemic It should also be noted that our estimate of24 having never been tested is substantially higher than the 7 estimate from 5 US cities(Heimer et al 2007) This relatively low frequency of HIV testing has persisted in a high-risk group despite an emphasis on routine HIV testing in Russia According to the WHOapproximately 20 million HIV tests are conducted annually in Russia (WHO 2005) acountry that has a total population of approximately 142 million Though voluntarycounseling and testing (VCT) is guaranteed by Russian law this may not be widelyaccessible or conducted on a truly voluntary basis Furthermore IDUs may not seek HIVtesting for a variety of reasons For example substantial stigma in the general populationtoward people with HIVAIDS may make knowing onesrsquo status undesirable (Balabanova etal 2006) Lack of access to affordable antiretroviral treatment may be another barrier toaccessing VCT to learn onersquos status The WHO currently estimates that approximately 10of those in need of antiretroviral treatment receive it in Russia (WHO 2006) in large partbecause generic drugs are not registered and treatment is not affordable to many RussiansHowever increased governmental commitments to and financial support for treatment inRussia have recently occurred and these efforts are likely to increase the proportion ofpeople who may receive treatment As this occurs the acceptability of HIV testing becomesincreasingly important
The finding that none of the demographic or drug and sex risk behaviors was correlated withHIV testing patterns is evidence of our limited understanding of motivations for and barriersto HIV testing The lack of identified behavioral correlates in the present study may reflectthe large volume of routine tests that is conducted in Russia This is supported by ourfinding that having a recent doctor visit history of incarceration and having been pregnantmdashall events that provide contact with institutions (medical or other) that provide routinetestingmdashwere in fact associated with recent testing It is possible that structuralcharacteristics are more important determinants of HIV testing than individual preferencesthough this has not been adequately studied
Despite the large-scale national investment in routine HIV testing the low testing and returnrates have resulted in poor knowledge of positive HIV serostatus among IDUs in StPetersburg We found that 24 of individuals who self-reported that they were HIV-negative were actually HIV-positive this proportion was substantially higher amongindividuals who had been tested but not received results (60) and individuals who hadnever been tested (57) Overall nearly two-thirds (64) of HIV-infected individuals didnot know their positive serostatus These findings are also comparable to findings in otherstudies from the region including the same proportion (two-thirds) of IDUs being unawareof positive HIV status in the Russian three city study (Rhodes et al 2006) and three-quartersof IDUs being unaware of their positive status in another Russian city (Rhodes et al 2002)Again it is discouraging that these estimates have not improved as the epidemic hascontinued to expand These findings have implications for secondary prevention in thatindividuals who do not know they are HIV-positive may not ad opt risk-reduction behaviorsthat can prevent transmission of HIV to their drug and sex partners The usefulness of thistype of secondary prevention has been evaluated and reviewed in other countries (Crepaz etal 2006 Marks et al 2005) but has not been evaluated in the Russian setting
Several possible limitations of these findings should be noted First our results may notgeneralize to IDUs outside of St Petersburg though they may apply to areas of similarepidemiologic characteristics and others are encouraged to consider the applicability of
Niccolai et al Page 7
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
these findings to their own settings Given the recent rapid rise in HIV in this region and thepossible substantial role this region may play in the current wave of the HIV pandemic ourfindings provide insight into strategies that may be needed to reduce the impact of HIVincluding HIV testing Second though our recruitment strategy (RDS) is designed toachieve a representative sample of the underlying population the degree to which thisoccurred is unknown although the initial weighting analysis suggests heterophily at a levelconsistent with achieving representativeness (Heckathorn 2002) Third HIV testing historywas obtained by self-report and may be subject to unintentionally inaccurate responses dueto misreport or forgetting On the other hand the effect of intentional misreport due to socialdesirability should be minimized by the anonymous nature of data collection and use ofCASI technology Fourth the lack of identified significant correlates of HIV testing patternsmay be due to insufficient sample size for the required statistical power or loss ofinformation resulting from dichotomization of covariates Despite these potentialmethodological limitations these results present the first look at HIV testing patterns amongIDU in St Petersburg a large city with a high burden of HIV infection and an updatedprevalence estimate from earlier reports
ConclusionsThese data show sub-optimal coverage of HIV testing in a high-risk population in a settingof explosive growth and they also reflect our limited understanding of motivations anddeterrents for HIV testing Future work must address targeted testing and counselingprograms and understanding attitudes toward HIV testing by IDUs in Russia includingperceptions of the relative balance between potential benefits and harms This will becomeincreasingly important as progress in antiretroviral scale-up increases Until this occursemphasizing the potential benefit of knowing onersquos status for secondary prevention may beuseful Finally addressing the issue of stigma toward people living with HIVAIDS isanother great but necessary challenge in increasing the acceptability of HIV testing amongIDUs in Russia
AcknowledgmentsThis work was supported by a grant from National Institutes of Health (U01DA017387) to Yale School ofMedicine and The Biomedical Center The authors acknowledge the dedication of the SATH-CAP research team atthe Biomedical Center St Petersburg Russia The authors also thank investigators at other sites of the SATH-CAPresearch project including RAND Corporation Research Triangle Institute University of California at Los Angelesand University of Illinois Chicago
ReferencesAbdala N Carney JM Durante AJ Klimov N Ostrovski D Somlai AM et al Estimating the
prevalence of syringe-borne and sexually transmitted diseases among injection drug users in StPetersburg Russia International Journal of STD and AIDS 2003 14697ndash703 [PubMed14596774]
AIDS Foundation East-West Officially registered HIV cases in Russian Federation 1 January 1987ndash31May 2007 as reported by the Russian Federal AIDS Center 2007 Available at httpwwwafeworg
Balabanova Y Coker R Atun RA Drobniewski F Stigma and HIV infection in Russia AIDS Care2006 18846ndash852 [PubMed 16971297]
Crepaz N Lyles CM Wolitski RJ Passin WF Rama SM Herbst JH et al Do preventioninterventions reduce HIV risk behaviors among people living with HIV A metanalytic review ofcontrolled trials AIDS (London England) 2006 20143ndash157
Crepaz N Marks G Towards an understanding of sexual risk behavior in people living with HIV Areview of social psychological and medical findings AIDS (London England) 2002 16135ndash149
Niccolai et al Page 8
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Des Jarlais DC Perlis T Arasteh K Hagan H Milliken J Braine N et al ldquoInformed altruismrdquo andldquopartner restrictionrdquo in the reduction of HIV infection in injecting drug users entering detoxificationtreatment in New York City 1990ndash2001 Journal of Acquired Immune Deficiency Syndromes2004 35158ndash166 [PubMed 14722449]
Heckathorn DD Respondent-driven sampling A new approach to the study of hidden populationsSocial Problems 1997 44174ndash199
Heckathorn DD Respondent-driven sampling II Deriving valid population estimates from chainreferral samples of hidden populations Social Problems 2002 4911ndash34
Heckathorn DD Extensions of respondent-driven sampling Analyzing continuous variables andcontrolling for differential recruitment Sociological Methodology 2007 37151ndash208
Heimer R Grau LE Curtin E Khoshnood K Singer M Assessment of HIV testing of urban injectiondrug users Implications for expansion of HIV testing and prevention efforts American Journal ofPublic Health 2007 97110ndash116 [PubMed 17138916]
Janssen RS Holtgrave DR Valdiserri RO The serostatus approach to fighting the HIV epidemicprevention strategies for infected individuals American Journal of Public Health 2001 911019ndash1024 [PubMed 11441723]
Lowndes CM Renton A Alary M Rhodes T Garnett G Stimson G Conditions for widespreadheterosexual spread of HIV in the Russian Federation Implications for research monitoring andprevention The International Journal on Drug Policy 2003 1445ndash62
Marks G Crepaz N Senterfitt JW Janssen RS Meta-analysis of high-risk sexual behaviors in personsaware and unaware they are infected with HIV in the United States Journal of Acquired ImmuneDeficiency Syndromes 2005 39446ndash453 [PubMed 16010168]
Rhodes T Lowndes CM Judd A Mikhailova LA Sarang A Rylkov A et al Explosive spread andhigh prevalence of HIV infection among injecting drug users in Togliatti City Russia AIDS(London England) 2002 16F25ndashF31
Rhodes T Platt L Maximova S Koshkina E Latishevskaya N Hickman M et al Prevalence of HIVhepatitis C and syphilis among injecting drug users in Russia A multi-city study Addiction(Abingdon England) 2006 101252ndash266
Shaboltas AV Toussova OV Hoffman IF Heimer R Verevochkin SV Ryder RW et al HIVprevalence social demographic and behavioral correlates and recruitment methods amonginjection drug users in St Petersburg Russia Journal of Acquired ImmununodeficiencySyndromes 2006 41657ndash663
United Nations Joint Program on HIVAIDS UNAIDSWHO policy statement on HIV testing 2004World Health Organization WHO consultation on increasing access to HIV testing and counseling
2002World Health Organization Russian Federation Summary country profile for HIVAIDS treatment
scale-up 2005World Health Organization Epidemiologic fact sheet 2006 Russian Federation 2006
Niccolai et al Page 9
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig 1Classification of IDUs by HIV testing and HIV status(n = 387)
Niccolai et al Page 10
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
November 2005ndashDecember 2006 The overall goal of SATH-CAP is to better understandhow patterns of sexual and drug use behaviors along with other social and environmentalfactors influence the spread of HIVAIDS from people currently at high risk for HIVAIDS(drug users (DUs) and men who have sex with men (MSM)) to other members of the generalpopulation
ParticipantsThe goal of participant recruitment was to achieve a representative sample of DU from thecity of St Petersburg Participants were recruited into the SATH-CAP study using a dual-component form of respondent driven sampling (RDS) (Heckathorn 1997 2007) RDS is achain referral sampling methodology that uses dual incentives and structured coupondisbursement procedures for peer referrals in order to reduce biases that are typicallyinherent in samples of hidden populations Traditional RDS methods were modified in thisstudy to recruit both additional members of the target population (DUs and MSM) as well assex partners of participants Briefly a number of ldquoseedsrdquo who were known DUs or MSMwere recruited by the study staff enrolled and given coupons with study locationinformation to give to their peers (other members of the target population and their sexpartners) Initial seeds included participants from previous studies at the research site(Shaboltas et al 2006) or referrals from agencies providing services to DUs Peers and sexpartners then called the site to schedule an appointment and presented the coupon at thestudy site for eligibility screening and enrollment When potential participants arrived at theproject site the purpose of the study and study procedures were explained and interestedindividuals provided informed consent Participation was confidential Upon completion ofall study procedures participants were reimbursed with gifts worth approximately US$10containing cell phone cards or personal care items They were also given subway tokenscondoms and HIV prevention information
Forty-eight seeds were enrolled and 35 (73) recruited at least one other participantAmong those who recruited at least on other participant (ldquoproductive seedsrdquo) the meannumber of participants recruited from a single seedrsquos chain of recruits was 5 and the medianwas 14 The maximum number of people enrolled in a single seedrsquos chain was 165(minimum = 1) The distribution of the number of waves which can be thought of as ldquostepsrdquofrom the seed in this sample was as follows mean 28 median = 2 minimum = 1maximum = 14 A total of 522 participants were enrolled The eligibility criterion forinclusion in the present analysis was reporting ever having injected drugs which included387 participants (non-IDUs MSM and sex partners were excluded)
MeasuresParticipants completed structured interviews using computer assisted survey interviewingtechnology on laptop computers that took approximately 60ndash120 min to complete Data usedin the present analyses included demographics drug and sex behaviors structural and healthservice utilization and HIV testing history measures Demographic variables included sexage and current housing and employment status Drug use behaviors included use in thepast 30 days age at first use duration of use frequency of use in past 30 days number ofIDU partners in the past 30 days having a new IDU partner in past 30 days and unsafeinjections in past 30 days (defined as sharing needles without using bleach using a singlesyringe to mix or divide drugs or sharing cookers cotton or water) Sex behaviors includedage at first sex number of sex partners in past 6 months new sex partners in past 6 monthshaving ever had sex with a male (among men) and having ever exchanged money or goodsfor sex (among women) and having ever been pregnant Structural and service utilizationvariables included history of incarceration number of doctor visits in past year havinghealth insurance and having ever received drug treatment Questions about HIV testing
Niccolai et al Page 3
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
included having ever been previously tested for HIV number of times tested date of lasttest and knowledge of test results
Results from HIV and sexually transmitted infection (STI) testing were also included in thepresent analyses Pre-test HIV counseling was conducted a blood specimen was collected totest for HIV syphilis hepatitis B and C viruses and a urine specimen was collected to testfor chlamydia and gonorrhea Serum specimens were tested for HIV antibodies by enzyme-linked immunosorbent assay (ELISA) using commercially licensed reagents includingGenscreen HIV 12 (BioRad France) andor Vironostika HIV Uni-Form II plus 0(Biomerieux The Netherlands)Non-reactive specimens were considered to be HIV-negative Specimens that were reactive were further tested with Western blot analysis usingNew Lav Blot HIV-1 (BioRad France) STI testing was done for syphilis gonorrhea andchlamydia Serum samples were tested for syphilis with rapid plasma reagin test (RPR)(Macro-Vue RPR Card Tests Becton Dickinson USA) and Treponema pallidum particleagglutination assay (TPPA) (Serodia-TPPA Fujirebio Japan) samples were consideredpositive for history of syphilis if reactive on both tests Urine specimens were tested forchlamydia and gonorrhea using polymerase chain reaction (Amplicor CTNG Roche USA)All participants were invited to return to the site for post-test counseling to get HIV and STItest results and referrals for additional medical and social services were provided as needed
Statistical AnalysisThe sample was described on demographic drug use and sex behaviors and serviceutilization variables using standard descriptive statistics Participants were considered HIV-positive if their ELISA reactive specimens were confirmed by Western blot To estimatecorrelates of HIV-positive serostatus bivariate and multivariate logistic regression wereused Examined correlates included the demographic drug use and sex behaviors prevalentSTI variables and structural and service utilization variables described above Our initialmodeling strategy was intended to be an exploratory analysis of behavioral correlates Thefinding that none of the behavioral correlates were associated led us to speculate thatstructural factors may be important thus our modeling strategy was revised to includestructural variables Continuous variables were dichotomized for two reasons First becausethe outcome of interest was dichotomous the logistic regression modeling producesestimates that can be interpreted as odds ratios these estimates are most easily interpretedwith dichotomous covariates that compare one level of the covariate to the other levelSecond dichotomizing covariates provides greater statistical power in the regression modelsby minimizing the levels of stratification We used a priori meaningful cut points fordichotomizing Covariates that were associated in the bivariate analysis using the criticalvalue of P lt 020 were included in the initial multivariate model A backward selectionprocedure eliminated covariates that did not remain significant using the critical value of P lt005 to arrive at the final multivariate model
Patterns of HIV testing were described using proportions and medians to estimate theprevalence of having ever been tested the frequency of testing time since last test andknowledge of positive serostatus Bivariate and multivariate logistic regression were used todetermine correlates of having had a recent HIV test (in the past 12 months) and havingreceived results among individuals who self-reported being HIV-negative using the samemodeling strategy described above To estimate the accuracy of knowledge of positive HIVserostatus we related self-reported status to laboratory results using blood specimenscollected at the time of the interview We estimated with a 95 confidence interval theproportion of HIV-infected individuals who self-reported correct knowledge of their HIV-positive status
Niccolai et al Page 4
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Because we used RDS for recruitment of IDUs weighting procedures are available (RDSAnalyzing Tool RDSAT software version 56) to adjust the sample for recruitmentprobabilities to obtain estimates that are representative of the underlying target populationUsing a weighting procedure that took into account our modified RDS methodology wefound that the weighted and unweighted estimates of sex age and HIV status proportions inthis sample did not differ substantially unweighted estimates for proportions male lt25years of age and HIV-infected were 74 33 and 50 respectively compared toweighted estimates of 75 32 and 49 respectively Furthermore estimation of 95confidence intervals for each of these estimates indicated substantial overlap and a similarrange between weighted and unweighted bounds due to virtually identical standarddeviations of weighted and unweighted estimates (data not shown) Therefore we usedunweighted estimates for all subsequent analyses
ResultsParticipant Characteristics and HIV Prevalence
The sample (n = 387) was predominantly male (74) and the mean age was 288 (standarddeviation 65) years Nearly one-third (31) of the sample was currently employed full- orpart-time The vast majority of the sample 91 reported injection drug use in the past 30days and 80 reported injecting heroin Nearly half the sample (48) reported age at firstinjection 18 years or younger The median time since initiating injection drug use was 8years and 65 reported at least one instance of some form of unsafe injection in the past 30days Age at first sex was15 years or younger for 53 of the sample 38 had multiple sexpartners and 49 had a new sex partner in the past 6 months Eleven male IDUs (4)reported having ever had male sex partners and 7 female IDUs (7) reported having everreceived money or other goods as payment for sex due to these low numbers these factorswere not considered covariates in subsequent analyses Health care utilization characteristicsare as follows 56 had a doctor visit in the past 12 months 79 had health insurance and30 had ever received drug treatment Thirty-seven percent of the sample had ever been inprison or jail
Eighteen percent (n = 68) of the sample tested positive for syphilis chlamydia or gonorrheaA total of 196 specimens were ELISA positive for HIV and 1 was indeterminate Of the 197specimens tested by Western blot 193 were positive 3 were indeterminate and 1 wasnegative We considered the indeterminate results to be negative (by excluding them fromthe numerator but including them in the denominator) to produce a conservative estimateand thus estimated HIV prevalence to be 50 (193387) A total of 290 participants (75)returned for their HIV test results Correlates are presented in Table 1 In the adjustedanalysis current unemployment (OR = 197 95 CI = 126ndash308 P lt 01) reporting unsafeinjections in past 30 days (OR = 154 95 CI = 10 236 P lt 05) and prevalent infectionwith chlamydia or gonorrhea or prevalent or past diagnosis of syphilis (OR = 196 95 CI= 112ndash342 P lt 05) were associated with HIV-positive serostatus
HIV Testing Patterns and CorrelatesSeventy-six percent (76) of the sample reported having ever been tested for HIV prior toenrollment in the present study Of those who had been tested (n = 295) the median numberof previous tests was 2 (range 1ndash55) and 36 of the sample had only been tested once Themedian time since last test was 8 months (range 0ndash96) and 30 had not been tested in thepast 12 months Twenty-four percent of those who had been tested reported knowing thatthey were HIV-positive 60 reported that they were HIV-negative and 17 did not knowtheir status (Fig 1)
Niccolai et al Page 5
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
To examine factors associated with HIV testing patterns we considered the outcome ofinterest to have been tested in the past year and received test results among those who didnot self-reported HIV-positive serostatus (n = 315) Sixty-nine individuals (22) had beentested in the past 12 months and received their test result Results of the bivariate analysisare presented in Table 2 To account for the association with having ever been pregnant amultivariate model on the entire sample was run without this covariate and stratified modelswere run for men and women separately (Table 3) In the entire sample only having adoctor visit in the past12 months remained significantly associated with recent testing (OR =306 95 CI = 168ndash559 P lt 01)Among men having a doctor visit in the past 12 months(OR = 366 95 CI = 175ndash770 P lt 01) and history of incarceration (OR = 212 95 CI= 108ndash442 P lt 05) were associated with recent testing and among women having everbeen pregnant was marginally associated (OR = 356 95 CI = 074ndash172 P lt 10)
Knowledge of HIV-Positive SerostatusAccuracy of knowledge of positive serostatus is depicted Fig 1 Of the 72 who self-reportedpositive serostatus 70 (97) were HIV-positive by serology Among the 315 participantswho did not report positive serostatus 123 (24) were HIV-positive This included 30participants who reported not knowing their status (60 of this group) 52 participants whoreported having never been tested (57 of this group) and 41 participants who reportedthey were HIV-negative (24 of this group) The proportion of HIV-infected participantswho self-reported that they knew they were HIV-infected was 36 (70193) with a 95confidence interval of 30ndash43 In other words 64 (123193) of HIV-positive individualsin this sample did not know their HIV status
DiscussionA key finding of this study is the HIV prevalence estimate of 50 among IDUs in StPetersburg Russia This updated estimate shows steady increase in comparison withprevious estimates of 11 from data collected in 2000 (Abdala et al 2003) and 30 fromdata collected in 2002 (Shaboltas et al 2006) and indicates continued growth of thisexplosive epidemic It is noteworthy that the study conducted in 2002 also relied heavily onchain referral sampling to access a similar population suggesting a degree of comparabilityin these samples Though we are unable to assess the temporal relationships betweencovariates and HIV status due to the cross-sectional nature of this study the significantlyhigher reporting of recent unsafe injections among those who are HIV-positive signalsconcern for continued transmission While we do not know the injection behaviors ofparticipants during the time in which they acquired HIV their current behaviors suggest thatthe potential for secondary transmission to their drug partners is high Similarly theassociation between STI (history of syphilis or current chlamydiagonorrhea) and HIVinfection suggests a possible role of sexual transmission of HIV among IDU in thispopulation either as a risk factor in the past or signaling the potential for future spread Theextent to which the epidemic will continue to grow and spread to the general population isan important and urgent question that the larger study on which this analysis was based isdesigned to address
A substantial proportion of IDUs in this sample from St Petersburg had not been tested forHIV ever or recently or received their test results Overall 24 had never been tested andamong those who had been tested 30 had not done so in the past year and 17 had notreceived test results These results are comparable to earlier findings from other Russiancities One study conducted in 2003 in the three Russian cities of Moscow Barnaul andVolgograd reported that 25ndash48 of IDUs had not been tested for HIV in the past year andthat 66 of HIV-positive IDUs were unaware of their HIV-positive serostatus (Rhodes et al2006) Our findings contribute to this growing body of knowledge by examining testing
Niccolai et al Page 6
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
patterns in a different city and by examining correlates neither of which had previouslybeen done Also given the highly dynamic and rapidly increasing HIV epidemic in Russiaour analysis that provides an updated estimate is needed to continually monitor the situationSadly our findings suggest that previously limited testing coverage has not increased overtime despite continued growth of the epidemic It should also be noted that our estimate of24 having never been tested is substantially higher than the 7 estimate from 5 US cities(Heimer et al 2007) This relatively low frequency of HIV testing has persisted in a high-risk group despite an emphasis on routine HIV testing in Russia According to the WHOapproximately 20 million HIV tests are conducted annually in Russia (WHO 2005) acountry that has a total population of approximately 142 million Though voluntarycounseling and testing (VCT) is guaranteed by Russian law this may not be widelyaccessible or conducted on a truly voluntary basis Furthermore IDUs may not seek HIVtesting for a variety of reasons For example substantial stigma in the general populationtoward people with HIVAIDS may make knowing onesrsquo status undesirable (Balabanova etal 2006) Lack of access to affordable antiretroviral treatment may be another barrier toaccessing VCT to learn onersquos status The WHO currently estimates that approximately 10of those in need of antiretroviral treatment receive it in Russia (WHO 2006) in large partbecause generic drugs are not registered and treatment is not affordable to many RussiansHowever increased governmental commitments to and financial support for treatment inRussia have recently occurred and these efforts are likely to increase the proportion ofpeople who may receive treatment As this occurs the acceptability of HIV testing becomesincreasingly important
The finding that none of the demographic or drug and sex risk behaviors was correlated withHIV testing patterns is evidence of our limited understanding of motivations for and barriersto HIV testing The lack of identified behavioral correlates in the present study may reflectthe large volume of routine tests that is conducted in Russia This is supported by ourfinding that having a recent doctor visit history of incarceration and having been pregnantmdashall events that provide contact with institutions (medical or other) that provide routinetestingmdashwere in fact associated with recent testing It is possible that structuralcharacteristics are more important determinants of HIV testing than individual preferencesthough this has not been adequately studied
Despite the large-scale national investment in routine HIV testing the low testing and returnrates have resulted in poor knowledge of positive HIV serostatus among IDUs in StPetersburg We found that 24 of individuals who self-reported that they were HIV-negative were actually HIV-positive this proportion was substantially higher amongindividuals who had been tested but not received results (60) and individuals who hadnever been tested (57) Overall nearly two-thirds (64) of HIV-infected individuals didnot know their positive serostatus These findings are also comparable to findings in otherstudies from the region including the same proportion (two-thirds) of IDUs being unawareof positive HIV status in the Russian three city study (Rhodes et al 2006) and three-quartersof IDUs being unaware of their positive status in another Russian city (Rhodes et al 2002)Again it is discouraging that these estimates have not improved as the epidemic hascontinued to expand These findings have implications for secondary prevention in thatindividuals who do not know they are HIV-positive may not ad opt risk-reduction behaviorsthat can prevent transmission of HIV to their drug and sex partners The usefulness of thistype of secondary prevention has been evaluated and reviewed in other countries (Crepaz etal 2006 Marks et al 2005) but has not been evaluated in the Russian setting
Several possible limitations of these findings should be noted First our results may notgeneralize to IDUs outside of St Petersburg though they may apply to areas of similarepidemiologic characteristics and others are encouraged to consider the applicability of
Niccolai et al Page 7
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
these findings to their own settings Given the recent rapid rise in HIV in this region and thepossible substantial role this region may play in the current wave of the HIV pandemic ourfindings provide insight into strategies that may be needed to reduce the impact of HIVincluding HIV testing Second though our recruitment strategy (RDS) is designed toachieve a representative sample of the underlying population the degree to which thisoccurred is unknown although the initial weighting analysis suggests heterophily at a levelconsistent with achieving representativeness (Heckathorn 2002) Third HIV testing historywas obtained by self-report and may be subject to unintentionally inaccurate responses dueto misreport or forgetting On the other hand the effect of intentional misreport due to socialdesirability should be minimized by the anonymous nature of data collection and use ofCASI technology Fourth the lack of identified significant correlates of HIV testing patternsmay be due to insufficient sample size for the required statistical power or loss ofinformation resulting from dichotomization of covariates Despite these potentialmethodological limitations these results present the first look at HIV testing patterns amongIDU in St Petersburg a large city with a high burden of HIV infection and an updatedprevalence estimate from earlier reports
ConclusionsThese data show sub-optimal coverage of HIV testing in a high-risk population in a settingof explosive growth and they also reflect our limited understanding of motivations anddeterrents for HIV testing Future work must address targeted testing and counselingprograms and understanding attitudes toward HIV testing by IDUs in Russia includingperceptions of the relative balance between potential benefits and harms This will becomeincreasingly important as progress in antiretroviral scale-up increases Until this occursemphasizing the potential benefit of knowing onersquos status for secondary prevention may beuseful Finally addressing the issue of stigma toward people living with HIVAIDS isanother great but necessary challenge in increasing the acceptability of HIV testing amongIDUs in Russia
AcknowledgmentsThis work was supported by a grant from National Institutes of Health (U01DA017387) to Yale School ofMedicine and The Biomedical Center The authors acknowledge the dedication of the SATH-CAP research team atthe Biomedical Center St Petersburg Russia The authors also thank investigators at other sites of the SATH-CAPresearch project including RAND Corporation Research Triangle Institute University of California at Los Angelesand University of Illinois Chicago
ReferencesAbdala N Carney JM Durante AJ Klimov N Ostrovski D Somlai AM et al Estimating the
prevalence of syringe-borne and sexually transmitted diseases among injection drug users in StPetersburg Russia International Journal of STD and AIDS 2003 14697ndash703 [PubMed14596774]
AIDS Foundation East-West Officially registered HIV cases in Russian Federation 1 January 1987ndash31May 2007 as reported by the Russian Federal AIDS Center 2007 Available at httpwwwafeworg
Balabanova Y Coker R Atun RA Drobniewski F Stigma and HIV infection in Russia AIDS Care2006 18846ndash852 [PubMed 16971297]
Crepaz N Lyles CM Wolitski RJ Passin WF Rama SM Herbst JH et al Do preventioninterventions reduce HIV risk behaviors among people living with HIV A metanalytic review ofcontrolled trials AIDS (London England) 2006 20143ndash157
Crepaz N Marks G Towards an understanding of sexual risk behavior in people living with HIV Areview of social psychological and medical findings AIDS (London England) 2002 16135ndash149
Niccolai et al Page 8
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Des Jarlais DC Perlis T Arasteh K Hagan H Milliken J Braine N et al ldquoInformed altruismrdquo andldquopartner restrictionrdquo in the reduction of HIV infection in injecting drug users entering detoxificationtreatment in New York City 1990ndash2001 Journal of Acquired Immune Deficiency Syndromes2004 35158ndash166 [PubMed 14722449]
Heckathorn DD Respondent-driven sampling A new approach to the study of hidden populationsSocial Problems 1997 44174ndash199
Heckathorn DD Respondent-driven sampling II Deriving valid population estimates from chainreferral samples of hidden populations Social Problems 2002 4911ndash34
Heckathorn DD Extensions of respondent-driven sampling Analyzing continuous variables andcontrolling for differential recruitment Sociological Methodology 2007 37151ndash208
Heimer R Grau LE Curtin E Khoshnood K Singer M Assessment of HIV testing of urban injectiondrug users Implications for expansion of HIV testing and prevention efforts American Journal ofPublic Health 2007 97110ndash116 [PubMed 17138916]
Janssen RS Holtgrave DR Valdiserri RO The serostatus approach to fighting the HIV epidemicprevention strategies for infected individuals American Journal of Public Health 2001 911019ndash1024 [PubMed 11441723]
Lowndes CM Renton A Alary M Rhodes T Garnett G Stimson G Conditions for widespreadheterosexual spread of HIV in the Russian Federation Implications for research monitoring andprevention The International Journal on Drug Policy 2003 1445ndash62
Marks G Crepaz N Senterfitt JW Janssen RS Meta-analysis of high-risk sexual behaviors in personsaware and unaware they are infected with HIV in the United States Journal of Acquired ImmuneDeficiency Syndromes 2005 39446ndash453 [PubMed 16010168]
Rhodes T Lowndes CM Judd A Mikhailova LA Sarang A Rylkov A et al Explosive spread andhigh prevalence of HIV infection among injecting drug users in Togliatti City Russia AIDS(London England) 2002 16F25ndashF31
Rhodes T Platt L Maximova S Koshkina E Latishevskaya N Hickman M et al Prevalence of HIVhepatitis C and syphilis among injecting drug users in Russia A multi-city study Addiction(Abingdon England) 2006 101252ndash266
Shaboltas AV Toussova OV Hoffman IF Heimer R Verevochkin SV Ryder RW et al HIVprevalence social demographic and behavioral correlates and recruitment methods amonginjection drug users in St Petersburg Russia Journal of Acquired ImmununodeficiencySyndromes 2006 41657ndash663
United Nations Joint Program on HIVAIDS UNAIDSWHO policy statement on HIV testing 2004World Health Organization WHO consultation on increasing access to HIV testing and counseling
2002World Health Organization Russian Federation Summary country profile for HIVAIDS treatment
scale-up 2005World Health Organization Epidemiologic fact sheet 2006 Russian Federation 2006
Niccolai et al Page 9
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig 1Classification of IDUs by HIV testing and HIV status(n = 387)
Niccolai et al Page 10
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
included having ever been previously tested for HIV number of times tested date of lasttest and knowledge of test results
Results from HIV and sexually transmitted infection (STI) testing were also included in thepresent analyses Pre-test HIV counseling was conducted a blood specimen was collected totest for HIV syphilis hepatitis B and C viruses and a urine specimen was collected to testfor chlamydia and gonorrhea Serum specimens were tested for HIV antibodies by enzyme-linked immunosorbent assay (ELISA) using commercially licensed reagents includingGenscreen HIV 12 (BioRad France) andor Vironostika HIV Uni-Form II plus 0(Biomerieux The Netherlands)Non-reactive specimens were considered to be HIV-negative Specimens that were reactive were further tested with Western blot analysis usingNew Lav Blot HIV-1 (BioRad France) STI testing was done for syphilis gonorrhea andchlamydia Serum samples were tested for syphilis with rapid plasma reagin test (RPR)(Macro-Vue RPR Card Tests Becton Dickinson USA) and Treponema pallidum particleagglutination assay (TPPA) (Serodia-TPPA Fujirebio Japan) samples were consideredpositive for history of syphilis if reactive on both tests Urine specimens were tested forchlamydia and gonorrhea using polymerase chain reaction (Amplicor CTNG Roche USA)All participants were invited to return to the site for post-test counseling to get HIV and STItest results and referrals for additional medical and social services were provided as needed
Statistical AnalysisThe sample was described on demographic drug use and sex behaviors and serviceutilization variables using standard descriptive statistics Participants were considered HIV-positive if their ELISA reactive specimens were confirmed by Western blot To estimatecorrelates of HIV-positive serostatus bivariate and multivariate logistic regression wereused Examined correlates included the demographic drug use and sex behaviors prevalentSTI variables and structural and service utilization variables described above Our initialmodeling strategy was intended to be an exploratory analysis of behavioral correlates Thefinding that none of the behavioral correlates were associated led us to speculate thatstructural factors may be important thus our modeling strategy was revised to includestructural variables Continuous variables were dichotomized for two reasons First becausethe outcome of interest was dichotomous the logistic regression modeling producesestimates that can be interpreted as odds ratios these estimates are most easily interpretedwith dichotomous covariates that compare one level of the covariate to the other levelSecond dichotomizing covariates provides greater statistical power in the regression modelsby minimizing the levels of stratification We used a priori meaningful cut points fordichotomizing Covariates that were associated in the bivariate analysis using the criticalvalue of P lt 020 were included in the initial multivariate model A backward selectionprocedure eliminated covariates that did not remain significant using the critical value of P lt005 to arrive at the final multivariate model
Patterns of HIV testing were described using proportions and medians to estimate theprevalence of having ever been tested the frequency of testing time since last test andknowledge of positive serostatus Bivariate and multivariate logistic regression were used todetermine correlates of having had a recent HIV test (in the past 12 months) and havingreceived results among individuals who self-reported being HIV-negative using the samemodeling strategy described above To estimate the accuracy of knowledge of positive HIVserostatus we related self-reported status to laboratory results using blood specimenscollected at the time of the interview We estimated with a 95 confidence interval theproportion of HIV-infected individuals who self-reported correct knowledge of their HIV-positive status
Niccolai et al Page 4
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Because we used RDS for recruitment of IDUs weighting procedures are available (RDSAnalyzing Tool RDSAT software version 56) to adjust the sample for recruitmentprobabilities to obtain estimates that are representative of the underlying target populationUsing a weighting procedure that took into account our modified RDS methodology wefound that the weighted and unweighted estimates of sex age and HIV status proportions inthis sample did not differ substantially unweighted estimates for proportions male lt25years of age and HIV-infected were 74 33 and 50 respectively compared toweighted estimates of 75 32 and 49 respectively Furthermore estimation of 95confidence intervals for each of these estimates indicated substantial overlap and a similarrange between weighted and unweighted bounds due to virtually identical standarddeviations of weighted and unweighted estimates (data not shown) Therefore we usedunweighted estimates for all subsequent analyses
ResultsParticipant Characteristics and HIV Prevalence
The sample (n = 387) was predominantly male (74) and the mean age was 288 (standarddeviation 65) years Nearly one-third (31) of the sample was currently employed full- orpart-time The vast majority of the sample 91 reported injection drug use in the past 30days and 80 reported injecting heroin Nearly half the sample (48) reported age at firstinjection 18 years or younger The median time since initiating injection drug use was 8years and 65 reported at least one instance of some form of unsafe injection in the past 30days Age at first sex was15 years or younger for 53 of the sample 38 had multiple sexpartners and 49 had a new sex partner in the past 6 months Eleven male IDUs (4)reported having ever had male sex partners and 7 female IDUs (7) reported having everreceived money or other goods as payment for sex due to these low numbers these factorswere not considered covariates in subsequent analyses Health care utilization characteristicsare as follows 56 had a doctor visit in the past 12 months 79 had health insurance and30 had ever received drug treatment Thirty-seven percent of the sample had ever been inprison or jail
Eighteen percent (n = 68) of the sample tested positive for syphilis chlamydia or gonorrheaA total of 196 specimens were ELISA positive for HIV and 1 was indeterminate Of the 197specimens tested by Western blot 193 were positive 3 were indeterminate and 1 wasnegative We considered the indeterminate results to be negative (by excluding them fromthe numerator but including them in the denominator) to produce a conservative estimateand thus estimated HIV prevalence to be 50 (193387) A total of 290 participants (75)returned for their HIV test results Correlates are presented in Table 1 In the adjustedanalysis current unemployment (OR = 197 95 CI = 126ndash308 P lt 01) reporting unsafeinjections in past 30 days (OR = 154 95 CI = 10 236 P lt 05) and prevalent infectionwith chlamydia or gonorrhea or prevalent or past diagnosis of syphilis (OR = 196 95 CI= 112ndash342 P lt 05) were associated with HIV-positive serostatus
HIV Testing Patterns and CorrelatesSeventy-six percent (76) of the sample reported having ever been tested for HIV prior toenrollment in the present study Of those who had been tested (n = 295) the median numberof previous tests was 2 (range 1ndash55) and 36 of the sample had only been tested once Themedian time since last test was 8 months (range 0ndash96) and 30 had not been tested in thepast 12 months Twenty-four percent of those who had been tested reported knowing thatthey were HIV-positive 60 reported that they were HIV-negative and 17 did not knowtheir status (Fig 1)
Niccolai et al Page 5
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
To examine factors associated with HIV testing patterns we considered the outcome ofinterest to have been tested in the past year and received test results among those who didnot self-reported HIV-positive serostatus (n = 315) Sixty-nine individuals (22) had beentested in the past 12 months and received their test result Results of the bivariate analysisare presented in Table 2 To account for the association with having ever been pregnant amultivariate model on the entire sample was run without this covariate and stratified modelswere run for men and women separately (Table 3) In the entire sample only having adoctor visit in the past12 months remained significantly associated with recent testing (OR =306 95 CI = 168ndash559 P lt 01)Among men having a doctor visit in the past 12 months(OR = 366 95 CI = 175ndash770 P lt 01) and history of incarceration (OR = 212 95 CI= 108ndash442 P lt 05) were associated with recent testing and among women having everbeen pregnant was marginally associated (OR = 356 95 CI = 074ndash172 P lt 10)
Knowledge of HIV-Positive SerostatusAccuracy of knowledge of positive serostatus is depicted Fig 1 Of the 72 who self-reportedpositive serostatus 70 (97) were HIV-positive by serology Among the 315 participantswho did not report positive serostatus 123 (24) were HIV-positive This included 30participants who reported not knowing their status (60 of this group) 52 participants whoreported having never been tested (57 of this group) and 41 participants who reportedthey were HIV-negative (24 of this group) The proportion of HIV-infected participantswho self-reported that they knew they were HIV-infected was 36 (70193) with a 95confidence interval of 30ndash43 In other words 64 (123193) of HIV-positive individualsin this sample did not know their HIV status
DiscussionA key finding of this study is the HIV prevalence estimate of 50 among IDUs in StPetersburg Russia This updated estimate shows steady increase in comparison withprevious estimates of 11 from data collected in 2000 (Abdala et al 2003) and 30 fromdata collected in 2002 (Shaboltas et al 2006) and indicates continued growth of thisexplosive epidemic It is noteworthy that the study conducted in 2002 also relied heavily onchain referral sampling to access a similar population suggesting a degree of comparabilityin these samples Though we are unable to assess the temporal relationships betweencovariates and HIV status due to the cross-sectional nature of this study the significantlyhigher reporting of recent unsafe injections among those who are HIV-positive signalsconcern for continued transmission While we do not know the injection behaviors ofparticipants during the time in which they acquired HIV their current behaviors suggest thatthe potential for secondary transmission to their drug partners is high Similarly theassociation between STI (history of syphilis or current chlamydiagonorrhea) and HIVinfection suggests a possible role of sexual transmission of HIV among IDU in thispopulation either as a risk factor in the past or signaling the potential for future spread Theextent to which the epidemic will continue to grow and spread to the general population isan important and urgent question that the larger study on which this analysis was based isdesigned to address
A substantial proportion of IDUs in this sample from St Petersburg had not been tested forHIV ever or recently or received their test results Overall 24 had never been tested andamong those who had been tested 30 had not done so in the past year and 17 had notreceived test results These results are comparable to earlier findings from other Russiancities One study conducted in 2003 in the three Russian cities of Moscow Barnaul andVolgograd reported that 25ndash48 of IDUs had not been tested for HIV in the past year andthat 66 of HIV-positive IDUs were unaware of their HIV-positive serostatus (Rhodes et al2006) Our findings contribute to this growing body of knowledge by examining testing
Niccolai et al Page 6
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
patterns in a different city and by examining correlates neither of which had previouslybeen done Also given the highly dynamic and rapidly increasing HIV epidemic in Russiaour analysis that provides an updated estimate is needed to continually monitor the situationSadly our findings suggest that previously limited testing coverage has not increased overtime despite continued growth of the epidemic It should also be noted that our estimate of24 having never been tested is substantially higher than the 7 estimate from 5 US cities(Heimer et al 2007) This relatively low frequency of HIV testing has persisted in a high-risk group despite an emphasis on routine HIV testing in Russia According to the WHOapproximately 20 million HIV tests are conducted annually in Russia (WHO 2005) acountry that has a total population of approximately 142 million Though voluntarycounseling and testing (VCT) is guaranteed by Russian law this may not be widelyaccessible or conducted on a truly voluntary basis Furthermore IDUs may not seek HIVtesting for a variety of reasons For example substantial stigma in the general populationtoward people with HIVAIDS may make knowing onesrsquo status undesirable (Balabanova etal 2006) Lack of access to affordable antiretroviral treatment may be another barrier toaccessing VCT to learn onersquos status The WHO currently estimates that approximately 10of those in need of antiretroviral treatment receive it in Russia (WHO 2006) in large partbecause generic drugs are not registered and treatment is not affordable to many RussiansHowever increased governmental commitments to and financial support for treatment inRussia have recently occurred and these efforts are likely to increase the proportion ofpeople who may receive treatment As this occurs the acceptability of HIV testing becomesincreasingly important
The finding that none of the demographic or drug and sex risk behaviors was correlated withHIV testing patterns is evidence of our limited understanding of motivations for and barriersto HIV testing The lack of identified behavioral correlates in the present study may reflectthe large volume of routine tests that is conducted in Russia This is supported by ourfinding that having a recent doctor visit history of incarceration and having been pregnantmdashall events that provide contact with institutions (medical or other) that provide routinetestingmdashwere in fact associated with recent testing It is possible that structuralcharacteristics are more important determinants of HIV testing than individual preferencesthough this has not been adequately studied
Despite the large-scale national investment in routine HIV testing the low testing and returnrates have resulted in poor knowledge of positive HIV serostatus among IDUs in StPetersburg We found that 24 of individuals who self-reported that they were HIV-negative were actually HIV-positive this proportion was substantially higher amongindividuals who had been tested but not received results (60) and individuals who hadnever been tested (57) Overall nearly two-thirds (64) of HIV-infected individuals didnot know their positive serostatus These findings are also comparable to findings in otherstudies from the region including the same proportion (two-thirds) of IDUs being unawareof positive HIV status in the Russian three city study (Rhodes et al 2006) and three-quartersof IDUs being unaware of their positive status in another Russian city (Rhodes et al 2002)Again it is discouraging that these estimates have not improved as the epidemic hascontinued to expand These findings have implications for secondary prevention in thatindividuals who do not know they are HIV-positive may not ad opt risk-reduction behaviorsthat can prevent transmission of HIV to their drug and sex partners The usefulness of thistype of secondary prevention has been evaluated and reviewed in other countries (Crepaz etal 2006 Marks et al 2005) but has not been evaluated in the Russian setting
Several possible limitations of these findings should be noted First our results may notgeneralize to IDUs outside of St Petersburg though they may apply to areas of similarepidemiologic characteristics and others are encouraged to consider the applicability of
Niccolai et al Page 7
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
these findings to their own settings Given the recent rapid rise in HIV in this region and thepossible substantial role this region may play in the current wave of the HIV pandemic ourfindings provide insight into strategies that may be needed to reduce the impact of HIVincluding HIV testing Second though our recruitment strategy (RDS) is designed toachieve a representative sample of the underlying population the degree to which thisoccurred is unknown although the initial weighting analysis suggests heterophily at a levelconsistent with achieving representativeness (Heckathorn 2002) Third HIV testing historywas obtained by self-report and may be subject to unintentionally inaccurate responses dueto misreport or forgetting On the other hand the effect of intentional misreport due to socialdesirability should be minimized by the anonymous nature of data collection and use ofCASI technology Fourth the lack of identified significant correlates of HIV testing patternsmay be due to insufficient sample size for the required statistical power or loss ofinformation resulting from dichotomization of covariates Despite these potentialmethodological limitations these results present the first look at HIV testing patterns amongIDU in St Petersburg a large city with a high burden of HIV infection and an updatedprevalence estimate from earlier reports
ConclusionsThese data show sub-optimal coverage of HIV testing in a high-risk population in a settingof explosive growth and they also reflect our limited understanding of motivations anddeterrents for HIV testing Future work must address targeted testing and counselingprograms and understanding attitudes toward HIV testing by IDUs in Russia includingperceptions of the relative balance between potential benefits and harms This will becomeincreasingly important as progress in antiretroviral scale-up increases Until this occursemphasizing the potential benefit of knowing onersquos status for secondary prevention may beuseful Finally addressing the issue of stigma toward people living with HIVAIDS isanother great but necessary challenge in increasing the acceptability of HIV testing amongIDUs in Russia
AcknowledgmentsThis work was supported by a grant from National Institutes of Health (U01DA017387) to Yale School ofMedicine and The Biomedical Center The authors acknowledge the dedication of the SATH-CAP research team atthe Biomedical Center St Petersburg Russia The authors also thank investigators at other sites of the SATH-CAPresearch project including RAND Corporation Research Triangle Institute University of California at Los Angelesand University of Illinois Chicago
ReferencesAbdala N Carney JM Durante AJ Klimov N Ostrovski D Somlai AM et al Estimating the
prevalence of syringe-borne and sexually transmitted diseases among injection drug users in StPetersburg Russia International Journal of STD and AIDS 2003 14697ndash703 [PubMed14596774]
AIDS Foundation East-West Officially registered HIV cases in Russian Federation 1 January 1987ndash31May 2007 as reported by the Russian Federal AIDS Center 2007 Available at httpwwwafeworg
Balabanova Y Coker R Atun RA Drobniewski F Stigma and HIV infection in Russia AIDS Care2006 18846ndash852 [PubMed 16971297]
Crepaz N Lyles CM Wolitski RJ Passin WF Rama SM Herbst JH et al Do preventioninterventions reduce HIV risk behaviors among people living with HIV A metanalytic review ofcontrolled trials AIDS (London England) 2006 20143ndash157
Crepaz N Marks G Towards an understanding of sexual risk behavior in people living with HIV Areview of social psychological and medical findings AIDS (London England) 2002 16135ndash149
Niccolai et al Page 8
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Des Jarlais DC Perlis T Arasteh K Hagan H Milliken J Braine N et al ldquoInformed altruismrdquo andldquopartner restrictionrdquo in the reduction of HIV infection in injecting drug users entering detoxificationtreatment in New York City 1990ndash2001 Journal of Acquired Immune Deficiency Syndromes2004 35158ndash166 [PubMed 14722449]
Heckathorn DD Respondent-driven sampling A new approach to the study of hidden populationsSocial Problems 1997 44174ndash199
Heckathorn DD Respondent-driven sampling II Deriving valid population estimates from chainreferral samples of hidden populations Social Problems 2002 4911ndash34
Heckathorn DD Extensions of respondent-driven sampling Analyzing continuous variables andcontrolling for differential recruitment Sociological Methodology 2007 37151ndash208
Heimer R Grau LE Curtin E Khoshnood K Singer M Assessment of HIV testing of urban injectiondrug users Implications for expansion of HIV testing and prevention efforts American Journal ofPublic Health 2007 97110ndash116 [PubMed 17138916]
Janssen RS Holtgrave DR Valdiserri RO The serostatus approach to fighting the HIV epidemicprevention strategies for infected individuals American Journal of Public Health 2001 911019ndash1024 [PubMed 11441723]
Lowndes CM Renton A Alary M Rhodes T Garnett G Stimson G Conditions for widespreadheterosexual spread of HIV in the Russian Federation Implications for research monitoring andprevention The International Journal on Drug Policy 2003 1445ndash62
Marks G Crepaz N Senterfitt JW Janssen RS Meta-analysis of high-risk sexual behaviors in personsaware and unaware they are infected with HIV in the United States Journal of Acquired ImmuneDeficiency Syndromes 2005 39446ndash453 [PubMed 16010168]
Rhodes T Lowndes CM Judd A Mikhailova LA Sarang A Rylkov A et al Explosive spread andhigh prevalence of HIV infection among injecting drug users in Togliatti City Russia AIDS(London England) 2002 16F25ndashF31
Rhodes T Platt L Maximova S Koshkina E Latishevskaya N Hickman M et al Prevalence of HIVhepatitis C and syphilis among injecting drug users in Russia A multi-city study Addiction(Abingdon England) 2006 101252ndash266
Shaboltas AV Toussova OV Hoffman IF Heimer R Verevochkin SV Ryder RW et al HIVprevalence social demographic and behavioral correlates and recruitment methods amonginjection drug users in St Petersburg Russia Journal of Acquired ImmununodeficiencySyndromes 2006 41657ndash663
United Nations Joint Program on HIVAIDS UNAIDSWHO policy statement on HIV testing 2004World Health Organization WHO consultation on increasing access to HIV testing and counseling
2002World Health Organization Russian Federation Summary country profile for HIVAIDS treatment
scale-up 2005World Health Organization Epidemiologic fact sheet 2006 Russian Federation 2006
Niccolai et al Page 9
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig 1Classification of IDUs by HIV testing and HIV status(n = 387)
Niccolai et al Page 10
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
Because we used RDS for recruitment of IDUs weighting procedures are available (RDSAnalyzing Tool RDSAT software version 56) to adjust the sample for recruitmentprobabilities to obtain estimates that are representative of the underlying target populationUsing a weighting procedure that took into account our modified RDS methodology wefound that the weighted and unweighted estimates of sex age and HIV status proportions inthis sample did not differ substantially unweighted estimates for proportions male lt25years of age and HIV-infected were 74 33 and 50 respectively compared toweighted estimates of 75 32 and 49 respectively Furthermore estimation of 95confidence intervals for each of these estimates indicated substantial overlap and a similarrange between weighted and unweighted bounds due to virtually identical standarddeviations of weighted and unweighted estimates (data not shown) Therefore we usedunweighted estimates for all subsequent analyses
ResultsParticipant Characteristics and HIV Prevalence
The sample (n = 387) was predominantly male (74) and the mean age was 288 (standarddeviation 65) years Nearly one-third (31) of the sample was currently employed full- orpart-time The vast majority of the sample 91 reported injection drug use in the past 30days and 80 reported injecting heroin Nearly half the sample (48) reported age at firstinjection 18 years or younger The median time since initiating injection drug use was 8years and 65 reported at least one instance of some form of unsafe injection in the past 30days Age at first sex was15 years or younger for 53 of the sample 38 had multiple sexpartners and 49 had a new sex partner in the past 6 months Eleven male IDUs (4)reported having ever had male sex partners and 7 female IDUs (7) reported having everreceived money or other goods as payment for sex due to these low numbers these factorswere not considered covariates in subsequent analyses Health care utilization characteristicsare as follows 56 had a doctor visit in the past 12 months 79 had health insurance and30 had ever received drug treatment Thirty-seven percent of the sample had ever been inprison or jail
Eighteen percent (n = 68) of the sample tested positive for syphilis chlamydia or gonorrheaA total of 196 specimens were ELISA positive for HIV and 1 was indeterminate Of the 197specimens tested by Western blot 193 were positive 3 were indeterminate and 1 wasnegative We considered the indeterminate results to be negative (by excluding them fromthe numerator but including them in the denominator) to produce a conservative estimateand thus estimated HIV prevalence to be 50 (193387) A total of 290 participants (75)returned for their HIV test results Correlates are presented in Table 1 In the adjustedanalysis current unemployment (OR = 197 95 CI = 126ndash308 P lt 01) reporting unsafeinjections in past 30 days (OR = 154 95 CI = 10 236 P lt 05) and prevalent infectionwith chlamydia or gonorrhea or prevalent or past diagnosis of syphilis (OR = 196 95 CI= 112ndash342 P lt 05) were associated with HIV-positive serostatus
HIV Testing Patterns and CorrelatesSeventy-six percent (76) of the sample reported having ever been tested for HIV prior toenrollment in the present study Of those who had been tested (n = 295) the median numberof previous tests was 2 (range 1ndash55) and 36 of the sample had only been tested once Themedian time since last test was 8 months (range 0ndash96) and 30 had not been tested in thepast 12 months Twenty-four percent of those who had been tested reported knowing thatthey were HIV-positive 60 reported that they were HIV-negative and 17 did not knowtheir status (Fig 1)
Niccolai et al Page 5
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
To examine factors associated with HIV testing patterns we considered the outcome ofinterest to have been tested in the past year and received test results among those who didnot self-reported HIV-positive serostatus (n = 315) Sixty-nine individuals (22) had beentested in the past 12 months and received their test result Results of the bivariate analysisare presented in Table 2 To account for the association with having ever been pregnant amultivariate model on the entire sample was run without this covariate and stratified modelswere run for men and women separately (Table 3) In the entire sample only having adoctor visit in the past12 months remained significantly associated with recent testing (OR =306 95 CI = 168ndash559 P lt 01)Among men having a doctor visit in the past 12 months(OR = 366 95 CI = 175ndash770 P lt 01) and history of incarceration (OR = 212 95 CI= 108ndash442 P lt 05) were associated with recent testing and among women having everbeen pregnant was marginally associated (OR = 356 95 CI = 074ndash172 P lt 10)
Knowledge of HIV-Positive SerostatusAccuracy of knowledge of positive serostatus is depicted Fig 1 Of the 72 who self-reportedpositive serostatus 70 (97) were HIV-positive by serology Among the 315 participantswho did not report positive serostatus 123 (24) were HIV-positive This included 30participants who reported not knowing their status (60 of this group) 52 participants whoreported having never been tested (57 of this group) and 41 participants who reportedthey were HIV-negative (24 of this group) The proportion of HIV-infected participantswho self-reported that they knew they were HIV-infected was 36 (70193) with a 95confidence interval of 30ndash43 In other words 64 (123193) of HIV-positive individualsin this sample did not know their HIV status
DiscussionA key finding of this study is the HIV prevalence estimate of 50 among IDUs in StPetersburg Russia This updated estimate shows steady increase in comparison withprevious estimates of 11 from data collected in 2000 (Abdala et al 2003) and 30 fromdata collected in 2002 (Shaboltas et al 2006) and indicates continued growth of thisexplosive epidemic It is noteworthy that the study conducted in 2002 also relied heavily onchain referral sampling to access a similar population suggesting a degree of comparabilityin these samples Though we are unable to assess the temporal relationships betweencovariates and HIV status due to the cross-sectional nature of this study the significantlyhigher reporting of recent unsafe injections among those who are HIV-positive signalsconcern for continued transmission While we do not know the injection behaviors ofparticipants during the time in which they acquired HIV their current behaviors suggest thatthe potential for secondary transmission to their drug partners is high Similarly theassociation between STI (history of syphilis or current chlamydiagonorrhea) and HIVinfection suggests a possible role of sexual transmission of HIV among IDU in thispopulation either as a risk factor in the past or signaling the potential for future spread Theextent to which the epidemic will continue to grow and spread to the general population isan important and urgent question that the larger study on which this analysis was based isdesigned to address
A substantial proportion of IDUs in this sample from St Petersburg had not been tested forHIV ever or recently or received their test results Overall 24 had never been tested andamong those who had been tested 30 had not done so in the past year and 17 had notreceived test results These results are comparable to earlier findings from other Russiancities One study conducted in 2003 in the three Russian cities of Moscow Barnaul andVolgograd reported that 25ndash48 of IDUs had not been tested for HIV in the past year andthat 66 of HIV-positive IDUs were unaware of their HIV-positive serostatus (Rhodes et al2006) Our findings contribute to this growing body of knowledge by examining testing
Niccolai et al Page 6
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
patterns in a different city and by examining correlates neither of which had previouslybeen done Also given the highly dynamic and rapidly increasing HIV epidemic in Russiaour analysis that provides an updated estimate is needed to continually monitor the situationSadly our findings suggest that previously limited testing coverage has not increased overtime despite continued growth of the epidemic It should also be noted that our estimate of24 having never been tested is substantially higher than the 7 estimate from 5 US cities(Heimer et al 2007) This relatively low frequency of HIV testing has persisted in a high-risk group despite an emphasis on routine HIV testing in Russia According to the WHOapproximately 20 million HIV tests are conducted annually in Russia (WHO 2005) acountry that has a total population of approximately 142 million Though voluntarycounseling and testing (VCT) is guaranteed by Russian law this may not be widelyaccessible or conducted on a truly voluntary basis Furthermore IDUs may not seek HIVtesting for a variety of reasons For example substantial stigma in the general populationtoward people with HIVAIDS may make knowing onesrsquo status undesirable (Balabanova etal 2006) Lack of access to affordable antiretroviral treatment may be another barrier toaccessing VCT to learn onersquos status The WHO currently estimates that approximately 10of those in need of antiretroviral treatment receive it in Russia (WHO 2006) in large partbecause generic drugs are not registered and treatment is not affordable to many RussiansHowever increased governmental commitments to and financial support for treatment inRussia have recently occurred and these efforts are likely to increase the proportion ofpeople who may receive treatment As this occurs the acceptability of HIV testing becomesincreasingly important
The finding that none of the demographic or drug and sex risk behaviors was correlated withHIV testing patterns is evidence of our limited understanding of motivations for and barriersto HIV testing The lack of identified behavioral correlates in the present study may reflectthe large volume of routine tests that is conducted in Russia This is supported by ourfinding that having a recent doctor visit history of incarceration and having been pregnantmdashall events that provide contact with institutions (medical or other) that provide routinetestingmdashwere in fact associated with recent testing It is possible that structuralcharacteristics are more important determinants of HIV testing than individual preferencesthough this has not been adequately studied
Despite the large-scale national investment in routine HIV testing the low testing and returnrates have resulted in poor knowledge of positive HIV serostatus among IDUs in StPetersburg We found that 24 of individuals who self-reported that they were HIV-negative were actually HIV-positive this proportion was substantially higher amongindividuals who had been tested but not received results (60) and individuals who hadnever been tested (57) Overall nearly two-thirds (64) of HIV-infected individuals didnot know their positive serostatus These findings are also comparable to findings in otherstudies from the region including the same proportion (two-thirds) of IDUs being unawareof positive HIV status in the Russian three city study (Rhodes et al 2006) and three-quartersof IDUs being unaware of their positive status in another Russian city (Rhodes et al 2002)Again it is discouraging that these estimates have not improved as the epidemic hascontinued to expand These findings have implications for secondary prevention in thatindividuals who do not know they are HIV-positive may not ad opt risk-reduction behaviorsthat can prevent transmission of HIV to their drug and sex partners The usefulness of thistype of secondary prevention has been evaluated and reviewed in other countries (Crepaz etal 2006 Marks et al 2005) but has not been evaluated in the Russian setting
Several possible limitations of these findings should be noted First our results may notgeneralize to IDUs outside of St Petersburg though they may apply to areas of similarepidemiologic characteristics and others are encouraged to consider the applicability of
Niccolai et al Page 7
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
these findings to their own settings Given the recent rapid rise in HIV in this region and thepossible substantial role this region may play in the current wave of the HIV pandemic ourfindings provide insight into strategies that may be needed to reduce the impact of HIVincluding HIV testing Second though our recruitment strategy (RDS) is designed toachieve a representative sample of the underlying population the degree to which thisoccurred is unknown although the initial weighting analysis suggests heterophily at a levelconsistent with achieving representativeness (Heckathorn 2002) Third HIV testing historywas obtained by self-report and may be subject to unintentionally inaccurate responses dueto misreport or forgetting On the other hand the effect of intentional misreport due to socialdesirability should be minimized by the anonymous nature of data collection and use ofCASI technology Fourth the lack of identified significant correlates of HIV testing patternsmay be due to insufficient sample size for the required statistical power or loss ofinformation resulting from dichotomization of covariates Despite these potentialmethodological limitations these results present the first look at HIV testing patterns amongIDU in St Petersburg a large city with a high burden of HIV infection and an updatedprevalence estimate from earlier reports
ConclusionsThese data show sub-optimal coverage of HIV testing in a high-risk population in a settingof explosive growth and they also reflect our limited understanding of motivations anddeterrents for HIV testing Future work must address targeted testing and counselingprograms and understanding attitudes toward HIV testing by IDUs in Russia includingperceptions of the relative balance between potential benefits and harms This will becomeincreasingly important as progress in antiretroviral scale-up increases Until this occursemphasizing the potential benefit of knowing onersquos status for secondary prevention may beuseful Finally addressing the issue of stigma toward people living with HIVAIDS isanother great but necessary challenge in increasing the acceptability of HIV testing amongIDUs in Russia
AcknowledgmentsThis work was supported by a grant from National Institutes of Health (U01DA017387) to Yale School ofMedicine and The Biomedical Center The authors acknowledge the dedication of the SATH-CAP research team atthe Biomedical Center St Petersburg Russia The authors also thank investigators at other sites of the SATH-CAPresearch project including RAND Corporation Research Triangle Institute University of California at Los Angelesand University of Illinois Chicago
ReferencesAbdala N Carney JM Durante AJ Klimov N Ostrovski D Somlai AM et al Estimating the
prevalence of syringe-borne and sexually transmitted diseases among injection drug users in StPetersburg Russia International Journal of STD and AIDS 2003 14697ndash703 [PubMed14596774]
AIDS Foundation East-West Officially registered HIV cases in Russian Federation 1 January 1987ndash31May 2007 as reported by the Russian Federal AIDS Center 2007 Available at httpwwwafeworg
Balabanova Y Coker R Atun RA Drobniewski F Stigma and HIV infection in Russia AIDS Care2006 18846ndash852 [PubMed 16971297]
Crepaz N Lyles CM Wolitski RJ Passin WF Rama SM Herbst JH et al Do preventioninterventions reduce HIV risk behaviors among people living with HIV A metanalytic review ofcontrolled trials AIDS (London England) 2006 20143ndash157
Crepaz N Marks G Towards an understanding of sexual risk behavior in people living with HIV Areview of social psychological and medical findings AIDS (London England) 2002 16135ndash149
Niccolai et al Page 8
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Des Jarlais DC Perlis T Arasteh K Hagan H Milliken J Braine N et al ldquoInformed altruismrdquo andldquopartner restrictionrdquo in the reduction of HIV infection in injecting drug users entering detoxificationtreatment in New York City 1990ndash2001 Journal of Acquired Immune Deficiency Syndromes2004 35158ndash166 [PubMed 14722449]
Heckathorn DD Respondent-driven sampling A new approach to the study of hidden populationsSocial Problems 1997 44174ndash199
Heckathorn DD Respondent-driven sampling II Deriving valid population estimates from chainreferral samples of hidden populations Social Problems 2002 4911ndash34
Heckathorn DD Extensions of respondent-driven sampling Analyzing continuous variables andcontrolling for differential recruitment Sociological Methodology 2007 37151ndash208
Heimer R Grau LE Curtin E Khoshnood K Singer M Assessment of HIV testing of urban injectiondrug users Implications for expansion of HIV testing and prevention efforts American Journal ofPublic Health 2007 97110ndash116 [PubMed 17138916]
Janssen RS Holtgrave DR Valdiserri RO The serostatus approach to fighting the HIV epidemicprevention strategies for infected individuals American Journal of Public Health 2001 911019ndash1024 [PubMed 11441723]
Lowndes CM Renton A Alary M Rhodes T Garnett G Stimson G Conditions for widespreadheterosexual spread of HIV in the Russian Federation Implications for research monitoring andprevention The International Journal on Drug Policy 2003 1445ndash62
Marks G Crepaz N Senterfitt JW Janssen RS Meta-analysis of high-risk sexual behaviors in personsaware and unaware they are infected with HIV in the United States Journal of Acquired ImmuneDeficiency Syndromes 2005 39446ndash453 [PubMed 16010168]
Rhodes T Lowndes CM Judd A Mikhailova LA Sarang A Rylkov A et al Explosive spread andhigh prevalence of HIV infection among injecting drug users in Togliatti City Russia AIDS(London England) 2002 16F25ndashF31
Rhodes T Platt L Maximova S Koshkina E Latishevskaya N Hickman M et al Prevalence of HIVhepatitis C and syphilis among injecting drug users in Russia A multi-city study Addiction(Abingdon England) 2006 101252ndash266
Shaboltas AV Toussova OV Hoffman IF Heimer R Verevochkin SV Ryder RW et al HIVprevalence social demographic and behavioral correlates and recruitment methods amonginjection drug users in St Petersburg Russia Journal of Acquired ImmununodeficiencySyndromes 2006 41657ndash663
United Nations Joint Program on HIVAIDS UNAIDSWHO policy statement on HIV testing 2004World Health Organization WHO consultation on increasing access to HIV testing and counseling
2002World Health Organization Russian Federation Summary country profile for HIVAIDS treatment
scale-up 2005World Health Organization Epidemiologic fact sheet 2006 Russian Federation 2006
Niccolai et al Page 9
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig 1Classification of IDUs by HIV testing and HIV status(n = 387)
Niccolai et al Page 10
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
To examine factors associated with HIV testing patterns we considered the outcome ofinterest to have been tested in the past year and received test results among those who didnot self-reported HIV-positive serostatus (n = 315) Sixty-nine individuals (22) had beentested in the past 12 months and received their test result Results of the bivariate analysisare presented in Table 2 To account for the association with having ever been pregnant amultivariate model on the entire sample was run without this covariate and stratified modelswere run for men and women separately (Table 3) In the entire sample only having adoctor visit in the past12 months remained significantly associated with recent testing (OR =306 95 CI = 168ndash559 P lt 01)Among men having a doctor visit in the past 12 months(OR = 366 95 CI = 175ndash770 P lt 01) and history of incarceration (OR = 212 95 CI= 108ndash442 P lt 05) were associated with recent testing and among women having everbeen pregnant was marginally associated (OR = 356 95 CI = 074ndash172 P lt 10)
Knowledge of HIV-Positive SerostatusAccuracy of knowledge of positive serostatus is depicted Fig 1 Of the 72 who self-reportedpositive serostatus 70 (97) were HIV-positive by serology Among the 315 participantswho did not report positive serostatus 123 (24) were HIV-positive This included 30participants who reported not knowing their status (60 of this group) 52 participants whoreported having never been tested (57 of this group) and 41 participants who reportedthey were HIV-negative (24 of this group) The proportion of HIV-infected participantswho self-reported that they knew they were HIV-infected was 36 (70193) with a 95confidence interval of 30ndash43 In other words 64 (123193) of HIV-positive individualsin this sample did not know their HIV status
DiscussionA key finding of this study is the HIV prevalence estimate of 50 among IDUs in StPetersburg Russia This updated estimate shows steady increase in comparison withprevious estimates of 11 from data collected in 2000 (Abdala et al 2003) and 30 fromdata collected in 2002 (Shaboltas et al 2006) and indicates continued growth of thisexplosive epidemic It is noteworthy that the study conducted in 2002 also relied heavily onchain referral sampling to access a similar population suggesting a degree of comparabilityin these samples Though we are unable to assess the temporal relationships betweencovariates and HIV status due to the cross-sectional nature of this study the significantlyhigher reporting of recent unsafe injections among those who are HIV-positive signalsconcern for continued transmission While we do not know the injection behaviors ofparticipants during the time in which they acquired HIV their current behaviors suggest thatthe potential for secondary transmission to their drug partners is high Similarly theassociation between STI (history of syphilis or current chlamydiagonorrhea) and HIVinfection suggests a possible role of sexual transmission of HIV among IDU in thispopulation either as a risk factor in the past or signaling the potential for future spread Theextent to which the epidemic will continue to grow and spread to the general population isan important and urgent question that the larger study on which this analysis was based isdesigned to address
A substantial proportion of IDUs in this sample from St Petersburg had not been tested forHIV ever or recently or received their test results Overall 24 had never been tested andamong those who had been tested 30 had not done so in the past year and 17 had notreceived test results These results are comparable to earlier findings from other Russiancities One study conducted in 2003 in the three Russian cities of Moscow Barnaul andVolgograd reported that 25ndash48 of IDUs had not been tested for HIV in the past year andthat 66 of HIV-positive IDUs were unaware of their HIV-positive serostatus (Rhodes et al2006) Our findings contribute to this growing body of knowledge by examining testing
Niccolai et al Page 6
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
patterns in a different city and by examining correlates neither of which had previouslybeen done Also given the highly dynamic and rapidly increasing HIV epidemic in Russiaour analysis that provides an updated estimate is needed to continually monitor the situationSadly our findings suggest that previously limited testing coverage has not increased overtime despite continued growth of the epidemic It should also be noted that our estimate of24 having never been tested is substantially higher than the 7 estimate from 5 US cities(Heimer et al 2007) This relatively low frequency of HIV testing has persisted in a high-risk group despite an emphasis on routine HIV testing in Russia According to the WHOapproximately 20 million HIV tests are conducted annually in Russia (WHO 2005) acountry that has a total population of approximately 142 million Though voluntarycounseling and testing (VCT) is guaranteed by Russian law this may not be widelyaccessible or conducted on a truly voluntary basis Furthermore IDUs may not seek HIVtesting for a variety of reasons For example substantial stigma in the general populationtoward people with HIVAIDS may make knowing onesrsquo status undesirable (Balabanova etal 2006) Lack of access to affordable antiretroviral treatment may be another barrier toaccessing VCT to learn onersquos status The WHO currently estimates that approximately 10of those in need of antiretroviral treatment receive it in Russia (WHO 2006) in large partbecause generic drugs are not registered and treatment is not affordable to many RussiansHowever increased governmental commitments to and financial support for treatment inRussia have recently occurred and these efforts are likely to increase the proportion ofpeople who may receive treatment As this occurs the acceptability of HIV testing becomesincreasingly important
The finding that none of the demographic or drug and sex risk behaviors was correlated withHIV testing patterns is evidence of our limited understanding of motivations for and barriersto HIV testing The lack of identified behavioral correlates in the present study may reflectthe large volume of routine tests that is conducted in Russia This is supported by ourfinding that having a recent doctor visit history of incarceration and having been pregnantmdashall events that provide contact with institutions (medical or other) that provide routinetestingmdashwere in fact associated with recent testing It is possible that structuralcharacteristics are more important determinants of HIV testing than individual preferencesthough this has not been adequately studied
Despite the large-scale national investment in routine HIV testing the low testing and returnrates have resulted in poor knowledge of positive HIV serostatus among IDUs in StPetersburg We found that 24 of individuals who self-reported that they were HIV-negative were actually HIV-positive this proportion was substantially higher amongindividuals who had been tested but not received results (60) and individuals who hadnever been tested (57) Overall nearly two-thirds (64) of HIV-infected individuals didnot know their positive serostatus These findings are also comparable to findings in otherstudies from the region including the same proportion (two-thirds) of IDUs being unawareof positive HIV status in the Russian three city study (Rhodes et al 2006) and three-quartersof IDUs being unaware of their positive status in another Russian city (Rhodes et al 2002)Again it is discouraging that these estimates have not improved as the epidemic hascontinued to expand These findings have implications for secondary prevention in thatindividuals who do not know they are HIV-positive may not ad opt risk-reduction behaviorsthat can prevent transmission of HIV to their drug and sex partners The usefulness of thistype of secondary prevention has been evaluated and reviewed in other countries (Crepaz etal 2006 Marks et al 2005) but has not been evaluated in the Russian setting
Several possible limitations of these findings should be noted First our results may notgeneralize to IDUs outside of St Petersburg though they may apply to areas of similarepidemiologic characteristics and others are encouraged to consider the applicability of
Niccolai et al Page 7
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
these findings to their own settings Given the recent rapid rise in HIV in this region and thepossible substantial role this region may play in the current wave of the HIV pandemic ourfindings provide insight into strategies that may be needed to reduce the impact of HIVincluding HIV testing Second though our recruitment strategy (RDS) is designed toachieve a representative sample of the underlying population the degree to which thisoccurred is unknown although the initial weighting analysis suggests heterophily at a levelconsistent with achieving representativeness (Heckathorn 2002) Third HIV testing historywas obtained by self-report and may be subject to unintentionally inaccurate responses dueto misreport or forgetting On the other hand the effect of intentional misreport due to socialdesirability should be minimized by the anonymous nature of data collection and use ofCASI technology Fourth the lack of identified significant correlates of HIV testing patternsmay be due to insufficient sample size for the required statistical power or loss ofinformation resulting from dichotomization of covariates Despite these potentialmethodological limitations these results present the first look at HIV testing patterns amongIDU in St Petersburg a large city with a high burden of HIV infection and an updatedprevalence estimate from earlier reports
ConclusionsThese data show sub-optimal coverage of HIV testing in a high-risk population in a settingof explosive growth and they also reflect our limited understanding of motivations anddeterrents for HIV testing Future work must address targeted testing and counselingprograms and understanding attitudes toward HIV testing by IDUs in Russia includingperceptions of the relative balance between potential benefits and harms This will becomeincreasingly important as progress in antiretroviral scale-up increases Until this occursemphasizing the potential benefit of knowing onersquos status for secondary prevention may beuseful Finally addressing the issue of stigma toward people living with HIVAIDS isanother great but necessary challenge in increasing the acceptability of HIV testing amongIDUs in Russia
AcknowledgmentsThis work was supported by a grant from National Institutes of Health (U01DA017387) to Yale School ofMedicine and The Biomedical Center The authors acknowledge the dedication of the SATH-CAP research team atthe Biomedical Center St Petersburg Russia The authors also thank investigators at other sites of the SATH-CAPresearch project including RAND Corporation Research Triangle Institute University of California at Los Angelesand University of Illinois Chicago
ReferencesAbdala N Carney JM Durante AJ Klimov N Ostrovski D Somlai AM et al Estimating the
prevalence of syringe-borne and sexually transmitted diseases among injection drug users in StPetersburg Russia International Journal of STD and AIDS 2003 14697ndash703 [PubMed14596774]
AIDS Foundation East-West Officially registered HIV cases in Russian Federation 1 January 1987ndash31May 2007 as reported by the Russian Federal AIDS Center 2007 Available at httpwwwafeworg
Balabanova Y Coker R Atun RA Drobniewski F Stigma and HIV infection in Russia AIDS Care2006 18846ndash852 [PubMed 16971297]
Crepaz N Lyles CM Wolitski RJ Passin WF Rama SM Herbst JH et al Do preventioninterventions reduce HIV risk behaviors among people living with HIV A metanalytic review ofcontrolled trials AIDS (London England) 2006 20143ndash157
Crepaz N Marks G Towards an understanding of sexual risk behavior in people living with HIV Areview of social psychological and medical findings AIDS (London England) 2002 16135ndash149
Niccolai et al Page 8
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Des Jarlais DC Perlis T Arasteh K Hagan H Milliken J Braine N et al ldquoInformed altruismrdquo andldquopartner restrictionrdquo in the reduction of HIV infection in injecting drug users entering detoxificationtreatment in New York City 1990ndash2001 Journal of Acquired Immune Deficiency Syndromes2004 35158ndash166 [PubMed 14722449]
Heckathorn DD Respondent-driven sampling A new approach to the study of hidden populationsSocial Problems 1997 44174ndash199
Heckathorn DD Respondent-driven sampling II Deriving valid population estimates from chainreferral samples of hidden populations Social Problems 2002 4911ndash34
Heckathorn DD Extensions of respondent-driven sampling Analyzing continuous variables andcontrolling for differential recruitment Sociological Methodology 2007 37151ndash208
Heimer R Grau LE Curtin E Khoshnood K Singer M Assessment of HIV testing of urban injectiondrug users Implications for expansion of HIV testing and prevention efforts American Journal ofPublic Health 2007 97110ndash116 [PubMed 17138916]
Janssen RS Holtgrave DR Valdiserri RO The serostatus approach to fighting the HIV epidemicprevention strategies for infected individuals American Journal of Public Health 2001 911019ndash1024 [PubMed 11441723]
Lowndes CM Renton A Alary M Rhodes T Garnett G Stimson G Conditions for widespreadheterosexual spread of HIV in the Russian Federation Implications for research monitoring andprevention The International Journal on Drug Policy 2003 1445ndash62
Marks G Crepaz N Senterfitt JW Janssen RS Meta-analysis of high-risk sexual behaviors in personsaware and unaware they are infected with HIV in the United States Journal of Acquired ImmuneDeficiency Syndromes 2005 39446ndash453 [PubMed 16010168]
Rhodes T Lowndes CM Judd A Mikhailova LA Sarang A Rylkov A et al Explosive spread andhigh prevalence of HIV infection among injecting drug users in Togliatti City Russia AIDS(London England) 2002 16F25ndashF31
Rhodes T Platt L Maximova S Koshkina E Latishevskaya N Hickman M et al Prevalence of HIVhepatitis C and syphilis among injecting drug users in Russia A multi-city study Addiction(Abingdon England) 2006 101252ndash266
Shaboltas AV Toussova OV Hoffman IF Heimer R Verevochkin SV Ryder RW et al HIVprevalence social demographic and behavioral correlates and recruitment methods amonginjection drug users in St Petersburg Russia Journal of Acquired ImmununodeficiencySyndromes 2006 41657ndash663
United Nations Joint Program on HIVAIDS UNAIDSWHO policy statement on HIV testing 2004World Health Organization WHO consultation on increasing access to HIV testing and counseling
2002World Health Organization Russian Federation Summary country profile for HIVAIDS treatment
scale-up 2005World Health Organization Epidemiologic fact sheet 2006 Russian Federation 2006
Niccolai et al Page 9
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig 1Classification of IDUs by HIV testing and HIV status(n = 387)
Niccolai et al Page 10
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
patterns in a different city and by examining correlates neither of which had previouslybeen done Also given the highly dynamic and rapidly increasing HIV epidemic in Russiaour analysis that provides an updated estimate is needed to continually monitor the situationSadly our findings suggest that previously limited testing coverage has not increased overtime despite continued growth of the epidemic It should also be noted that our estimate of24 having never been tested is substantially higher than the 7 estimate from 5 US cities(Heimer et al 2007) This relatively low frequency of HIV testing has persisted in a high-risk group despite an emphasis on routine HIV testing in Russia According to the WHOapproximately 20 million HIV tests are conducted annually in Russia (WHO 2005) acountry that has a total population of approximately 142 million Though voluntarycounseling and testing (VCT) is guaranteed by Russian law this may not be widelyaccessible or conducted on a truly voluntary basis Furthermore IDUs may not seek HIVtesting for a variety of reasons For example substantial stigma in the general populationtoward people with HIVAIDS may make knowing onesrsquo status undesirable (Balabanova etal 2006) Lack of access to affordable antiretroviral treatment may be another barrier toaccessing VCT to learn onersquos status The WHO currently estimates that approximately 10of those in need of antiretroviral treatment receive it in Russia (WHO 2006) in large partbecause generic drugs are not registered and treatment is not affordable to many RussiansHowever increased governmental commitments to and financial support for treatment inRussia have recently occurred and these efforts are likely to increase the proportion ofpeople who may receive treatment As this occurs the acceptability of HIV testing becomesincreasingly important
The finding that none of the demographic or drug and sex risk behaviors was correlated withHIV testing patterns is evidence of our limited understanding of motivations for and barriersto HIV testing The lack of identified behavioral correlates in the present study may reflectthe large volume of routine tests that is conducted in Russia This is supported by ourfinding that having a recent doctor visit history of incarceration and having been pregnantmdashall events that provide contact with institutions (medical or other) that provide routinetestingmdashwere in fact associated with recent testing It is possible that structuralcharacteristics are more important determinants of HIV testing than individual preferencesthough this has not been adequately studied
Despite the large-scale national investment in routine HIV testing the low testing and returnrates have resulted in poor knowledge of positive HIV serostatus among IDUs in StPetersburg We found that 24 of individuals who self-reported that they were HIV-negative were actually HIV-positive this proportion was substantially higher amongindividuals who had been tested but not received results (60) and individuals who hadnever been tested (57) Overall nearly two-thirds (64) of HIV-infected individuals didnot know their positive serostatus These findings are also comparable to findings in otherstudies from the region including the same proportion (two-thirds) of IDUs being unawareof positive HIV status in the Russian three city study (Rhodes et al 2006) and three-quartersof IDUs being unaware of their positive status in another Russian city (Rhodes et al 2002)Again it is discouraging that these estimates have not improved as the epidemic hascontinued to expand These findings have implications for secondary prevention in thatindividuals who do not know they are HIV-positive may not ad opt risk-reduction behaviorsthat can prevent transmission of HIV to their drug and sex partners The usefulness of thistype of secondary prevention has been evaluated and reviewed in other countries (Crepaz etal 2006 Marks et al 2005) but has not been evaluated in the Russian setting
Several possible limitations of these findings should be noted First our results may notgeneralize to IDUs outside of St Petersburg though they may apply to areas of similarepidemiologic characteristics and others are encouraged to consider the applicability of
Niccolai et al Page 7
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
these findings to their own settings Given the recent rapid rise in HIV in this region and thepossible substantial role this region may play in the current wave of the HIV pandemic ourfindings provide insight into strategies that may be needed to reduce the impact of HIVincluding HIV testing Second though our recruitment strategy (RDS) is designed toachieve a representative sample of the underlying population the degree to which thisoccurred is unknown although the initial weighting analysis suggests heterophily at a levelconsistent with achieving representativeness (Heckathorn 2002) Third HIV testing historywas obtained by self-report and may be subject to unintentionally inaccurate responses dueto misreport or forgetting On the other hand the effect of intentional misreport due to socialdesirability should be minimized by the anonymous nature of data collection and use ofCASI technology Fourth the lack of identified significant correlates of HIV testing patternsmay be due to insufficient sample size for the required statistical power or loss ofinformation resulting from dichotomization of covariates Despite these potentialmethodological limitations these results present the first look at HIV testing patterns amongIDU in St Petersburg a large city with a high burden of HIV infection and an updatedprevalence estimate from earlier reports
ConclusionsThese data show sub-optimal coverage of HIV testing in a high-risk population in a settingof explosive growth and they also reflect our limited understanding of motivations anddeterrents for HIV testing Future work must address targeted testing and counselingprograms and understanding attitudes toward HIV testing by IDUs in Russia includingperceptions of the relative balance between potential benefits and harms This will becomeincreasingly important as progress in antiretroviral scale-up increases Until this occursemphasizing the potential benefit of knowing onersquos status for secondary prevention may beuseful Finally addressing the issue of stigma toward people living with HIVAIDS isanother great but necessary challenge in increasing the acceptability of HIV testing amongIDUs in Russia
AcknowledgmentsThis work was supported by a grant from National Institutes of Health (U01DA017387) to Yale School ofMedicine and The Biomedical Center The authors acknowledge the dedication of the SATH-CAP research team atthe Biomedical Center St Petersburg Russia The authors also thank investigators at other sites of the SATH-CAPresearch project including RAND Corporation Research Triangle Institute University of California at Los Angelesand University of Illinois Chicago
ReferencesAbdala N Carney JM Durante AJ Klimov N Ostrovski D Somlai AM et al Estimating the
prevalence of syringe-borne and sexually transmitted diseases among injection drug users in StPetersburg Russia International Journal of STD and AIDS 2003 14697ndash703 [PubMed14596774]
AIDS Foundation East-West Officially registered HIV cases in Russian Federation 1 January 1987ndash31May 2007 as reported by the Russian Federal AIDS Center 2007 Available at httpwwwafeworg
Balabanova Y Coker R Atun RA Drobniewski F Stigma and HIV infection in Russia AIDS Care2006 18846ndash852 [PubMed 16971297]
Crepaz N Lyles CM Wolitski RJ Passin WF Rama SM Herbst JH et al Do preventioninterventions reduce HIV risk behaviors among people living with HIV A metanalytic review ofcontrolled trials AIDS (London England) 2006 20143ndash157
Crepaz N Marks G Towards an understanding of sexual risk behavior in people living with HIV Areview of social psychological and medical findings AIDS (London England) 2002 16135ndash149
Niccolai et al Page 8
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Des Jarlais DC Perlis T Arasteh K Hagan H Milliken J Braine N et al ldquoInformed altruismrdquo andldquopartner restrictionrdquo in the reduction of HIV infection in injecting drug users entering detoxificationtreatment in New York City 1990ndash2001 Journal of Acquired Immune Deficiency Syndromes2004 35158ndash166 [PubMed 14722449]
Heckathorn DD Respondent-driven sampling A new approach to the study of hidden populationsSocial Problems 1997 44174ndash199
Heckathorn DD Respondent-driven sampling II Deriving valid population estimates from chainreferral samples of hidden populations Social Problems 2002 4911ndash34
Heckathorn DD Extensions of respondent-driven sampling Analyzing continuous variables andcontrolling for differential recruitment Sociological Methodology 2007 37151ndash208
Heimer R Grau LE Curtin E Khoshnood K Singer M Assessment of HIV testing of urban injectiondrug users Implications for expansion of HIV testing and prevention efforts American Journal ofPublic Health 2007 97110ndash116 [PubMed 17138916]
Janssen RS Holtgrave DR Valdiserri RO The serostatus approach to fighting the HIV epidemicprevention strategies for infected individuals American Journal of Public Health 2001 911019ndash1024 [PubMed 11441723]
Lowndes CM Renton A Alary M Rhodes T Garnett G Stimson G Conditions for widespreadheterosexual spread of HIV in the Russian Federation Implications for research monitoring andprevention The International Journal on Drug Policy 2003 1445ndash62
Marks G Crepaz N Senterfitt JW Janssen RS Meta-analysis of high-risk sexual behaviors in personsaware and unaware they are infected with HIV in the United States Journal of Acquired ImmuneDeficiency Syndromes 2005 39446ndash453 [PubMed 16010168]
Rhodes T Lowndes CM Judd A Mikhailova LA Sarang A Rylkov A et al Explosive spread andhigh prevalence of HIV infection among injecting drug users in Togliatti City Russia AIDS(London England) 2002 16F25ndashF31
Rhodes T Platt L Maximova S Koshkina E Latishevskaya N Hickman M et al Prevalence of HIVhepatitis C and syphilis among injecting drug users in Russia A multi-city study Addiction(Abingdon England) 2006 101252ndash266
Shaboltas AV Toussova OV Hoffman IF Heimer R Verevochkin SV Ryder RW et al HIVprevalence social demographic and behavioral correlates and recruitment methods amonginjection drug users in St Petersburg Russia Journal of Acquired ImmununodeficiencySyndromes 2006 41657ndash663
United Nations Joint Program on HIVAIDS UNAIDSWHO policy statement on HIV testing 2004World Health Organization WHO consultation on increasing access to HIV testing and counseling
2002World Health Organization Russian Federation Summary country profile for HIVAIDS treatment
scale-up 2005World Health Organization Epidemiologic fact sheet 2006 Russian Federation 2006
Niccolai et al Page 9
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig 1Classification of IDUs by HIV testing and HIV status(n = 387)
Niccolai et al Page 10
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
these findings to their own settings Given the recent rapid rise in HIV in this region and thepossible substantial role this region may play in the current wave of the HIV pandemic ourfindings provide insight into strategies that may be needed to reduce the impact of HIVincluding HIV testing Second though our recruitment strategy (RDS) is designed toachieve a representative sample of the underlying population the degree to which thisoccurred is unknown although the initial weighting analysis suggests heterophily at a levelconsistent with achieving representativeness (Heckathorn 2002) Third HIV testing historywas obtained by self-report and may be subject to unintentionally inaccurate responses dueto misreport or forgetting On the other hand the effect of intentional misreport due to socialdesirability should be minimized by the anonymous nature of data collection and use ofCASI technology Fourth the lack of identified significant correlates of HIV testing patternsmay be due to insufficient sample size for the required statistical power or loss ofinformation resulting from dichotomization of covariates Despite these potentialmethodological limitations these results present the first look at HIV testing patterns amongIDU in St Petersburg a large city with a high burden of HIV infection and an updatedprevalence estimate from earlier reports
ConclusionsThese data show sub-optimal coverage of HIV testing in a high-risk population in a settingof explosive growth and they also reflect our limited understanding of motivations anddeterrents for HIV testing Future work must address targeted testing and counselingprograms and understanding attitudes toward HIV testing by IDUs in Russia includingperceptions of the relative balance between potential benefits and harms This will becomeincreasingly important as progress in antiretroviral scale-up increases Until this occursemphasizing the potential benefit of knowing onersquos status for secondary prevention may beuseful Finally addressing the issue of stigma toward people living with HIVAIDS isanother great but necessary challenge in increasing the acceptability of HIV testing amongIDUs in Russia
AcknowledgmentsThis work was supported by a grant from National Institutes of Health (U01DA017387) to Yale School ofMedicine and The Biomedical Center The authors acknowledge the dedication of the SATH-CAP research team atthe Biomedical Center St Petersburg Russia The authors also thank investigators at other sites of the SATH-CAPresearch project including RAND Corporation Research Triangle Institute University of California at Los Angelesand University of Illinois Chicago
ReferencesAbdala N Carney JM Durante AJ Klimov N Ostrovski D Somlai AM et al Estimating the
prevalence of syringe-borne and sexually transmitted diseases among injection drug users in StPetersburg Russia International Journal of STD and AIDS 2003 14697ndash703 [PubMed14596774]
AIDS Foundation East-West Officially registered HIV cases in Russian Federation 1 January 1987ndash31May 2007 as reported by the Russian Federal AIDS Center 2007 Available at httpwwwafeworg
Balabanova Y Coker R Atun RA Drobniewski F Stigma and HIV infection in Russia AIDS Care2006 18846ndash852 [PubMed 16971297]
Crepaz N Lyles CM Wolitski RJ Passin WF Rama SM Herbst JH et al Do preventioninterventions reduce HIV risk behaviors among people living with HIV A metanalytic review ofcontrolled trials AIDS (London England) 2006 20143ndash157
Crepaz N Marks G Towards an understanding of sexual risk behavior in people living with HIV Areview of social psychological and medical findings AIDS (London England) 2002 16135ndash149
Niccolai et al Page 8
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Des Jarlais DC Perlis T Arasteh K Hagan H Milliken J Braine N et al ldquoInformed altruismrdquo andldquopartner restrictionrdquo in the reduction of HIV infection in injecting drug users entering detoxificationtreatment in New York City 1990ndash2001 Journal of Acquired Immune Deficiency Syndromes2004 35158ndash166 [PubMed 14722449]
Heckathorn DD Respondent-driven sampling A new approach to the study of hidden populationsSocial Problems 1997 44174ndash199
Heckathorn DD Respondent-driven sampling II Deriving valid population estimates from chainreferral samples of hidden populations Social Problems 2002 4911ndash34
Heckathorn DD Extensions of respondent-driven sampling Analyzing continuous variables andcontrolling for differential recruitment Sociological Methodology 2007 37151ndash208
Heimer R Grau LE Curtin E Khoshnood K Singer M Assessment of HIV testing of urban injectiondrug users Implications for expansion of HIV testing and prevention efforts American Journal ofPublic Health 2007 97110ndash116 [PubMed 17138916]
Janssen RS Holtgrave DR Valdiserri RO The serostatus approach to fighting the HIV epidemicprevention strategies for infected individuals American Journal of Public Health 2001 911019ndash1024 [PubMed 11441723]
Lowndes CM Renton A Alary M Rhodes T Garnett G Stimson G Conditions for widespreadheterosexual spread of HIV in the Russian Federation Implications for research monitoring andprevention The International Journal on Drug Policy 2003 1445ndash62
Marks G Crepaz N Senterfitt JW Janssen RS Meta-analysis of high-risk sexual behaviors in personsaware and unaware they are infected with HIV in the United States Journal of Acquired ImmuneDeficiency Syndromes 2005 39446ndash453 [PubMed 16010168]
Rhodes T Lowndes CM Judd A Mikhailova LA Sarang A Rylkov A et al Explosive spread andhigh prevalence of HIV infection among injecting drug users in Togliatti City Russia AIDS(London England) 2002 16F25ndashF31
Rhodes T Platt L Maximova S Koshkina E Latishevskaya N Hickman M et al Prevalence of HIVhepatitis C and syphilis among injecting drug users in Russia A multi-city study Addiction(Abingdon England) 2006 101252ndash266
Shaboltas AV Toussova OV Hoffman IF Heimer R Verevochkin SV Ryder RW et al HIVprevalence social demographic and behavioral correlates and recruitment methods amonginjection drug users in St Petersburg Russia Journal of Acquired ImmununodeficiencySyndromes 2006 41657ndash663
United Nations Joint Program on HIVAIDS UNAIDSWHO policy statement on HIV testing 2004World Health Organization WHO consultation on increasing access to HIV testing and counseling
2002World Health Organization Russian Federation Summary country profile for HIVAIDS treatment
scale-up 2005World Health Organization Epidemiologic fact sheet 2006 Russian Federation 2006
Niccolai et al Page 9
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig 1Classification of IDUs by HIV testing and HIV status(n = 387)
Niccolai et al Page 10
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
Des Jarlais DC Perlis T Arasteh K Hagan H Milliken J Braine N et al ldquoInformed altruismrdquo andldquopartner restrictionrdquo in the reduction of HIV infection in injecting drug users entering detoxificationtreatment in New York City 1990ndash2001 Journal of Acquired Immune Deficiency Syndromes2004 35158ndash166 [PubMed 14722449]
Heckathorn DD Respondent-driven sampling A new approach to the study of hidden populationsSocial Problems 1997 44174ndash199
Heckathorn DD Respondent-driven sampling II Deriving valid population estimates from chainreferral samples of hidden populations Social Problems 2002 4911ndash34
Heckathorn DD Extensions of respondent-driven sampling Analyzing continuous variables andcontrolling for differential recruitment Sociological Methodology 2007 37151ndash208
Heimer R Grau LE Curtin E Khoshnood K Singer M Assessment of HIV testing of urban injectiondrug users Implications for expansion of HIV testing and prevention efforts American Journal ofPublic Health 2007 97110ndash116 [PubMed 17138916]
Janssen RS Holtgrave DR Valdiserri RO The serostatus approach to fighting the HIV epidemicprevention strategies for infected individuals American Journal of Public Health 2001 911019ndash1024 [PubMed 11441723]
Lowndes CM Renton A Alary M Rhodes T Garnett G Stimson G Conditions for widespreadheterosexual spread of HIV in the Russian Federation Implications for research monitoring andprevention The International Journal on Drug Policy 2003 1445ndash62
Marks G Crepaz N Senterfitt JW Janssen RS Meta-analysis of high-risk sexual behaviors in personsaware and unaware they are infected with HIV in the United States Journal of Acquired ImmuneDeficiency Syndromes 2005 39446ndash453 [PubMed 16010168]
Rhodes T Lowndes CM Judd A Mikhailova LA Sarang A Rylkov A et al Explosive spread andhigh prevalence of HIV infection among injecting drug users in Togliatti City Russia AIDS(London England) 2002 16F25ndashF31
Rhodes T Platt L Maximova S Koshkina E Latishevskaya N Hickman M et al Prevalence of HIVhepatitis C and syphilis among injecting drug users in Russia A multi-city study Addiction(Abingdon England) 2006 101252ndash266
Shaboltas AV Toussova OV Hoffman IF Heimer R Verevochkin SV Ryder RW et al HIVprevalence social demographic and behavioral correlates and recruitment methods amonginjection drug users in St Petersburg Russia Journal of Acquired ImmununodeficiencySyndromes 2006 41657ndash663
United Nations Joint Program on HIVAIDS UNAIDSWHO policy statement on HIV testing 2004World Health Organization WHO consultation on increasing access to HIV testing and counseling
2002World Health Organization Russian Federation Summary country profile for HIVAIDS treatment
scale-up 2005World Health Organization Epidemiologic fact sheet 2006 Russian Federation 2006
Niccolai et al Page 9
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig 1Classification of IDUs by HIV testing and HIV status(n = 387)
Niccolai et al Page 10
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
Fig 1Classification of IDUs by HIV testing and HIV status(n = 387)
Niccolai et al Page 10
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 11
Tabl
e 1
Una
djus
ted
and
adju
sted
cor
rela
tes o
f HIV
-pos
itive
sero
stat
us a
mon
g in
ject
ion
drug
use
rs S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
87 u
nles
s oth
erw
ise
note
d)
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
Sex
Mal
e28
613
6 (4
8)
Ref
eren
t
Fem
ale
101
57 (5
6)
143
(09
1ndash2
26)
Age
le25
yea
rs12
762
(49
)R
efer
ent
gt25
yea
rs26
013
1 (5
0)
107
(07
0ndash1
63)
Cur
rent
ly e
mpl
oyed
Ful
l- or
par
t-tim
e11
945
(38
)R
efer
ent
Ref
eren
t
Not
em
ploy
ed26
414
6 (5
5)
204
(13
1ndash3
17)
1
97
(12
6ndash3
08)
IDU
pas
t 30
days
Yes
342
172
(50
)1
42(0
71ndash
284
)
No
3615
(42
)R
efer
ent
Age
at f
irst I
DU
le18
186
99 (5
3)
131
(08
8ndash1
95)
gt18
200
93 (4
7)
Ref
eren
t
Dur
atio
n of
IDU
le5
year
s10
642
(40
)R
efer
ent
gt5
year
s28
015
0 (5
4)
176
(11
2ndash2
77)
Freq
uenc
y of
IDU
in p
ast 3
0 da
ys
lt30
260
131
(50
)1
01(0
72ndash
142
)
ge30
118
56 (4
8)
Ref
eren
t
Num
ber o
f ID
U p
artn
ers p
ast 3
0 da
ys
le2
223
107
(48
)R
efer
ent
gt2
164
86 (5
2)
112
(08
6ndash1
47)
Uns
afe
inje
ctio
n in
pas
t 30
days
a
Yes
251
134
(53
)1
50(0
98ndash
228
)1
54(1
0ndash2
36)
No
136
59 (4
3)
Ref
eren
tR
efer
ent
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 12
Cov
aria
teT
otal
No
() H
IV+
uOR
95
CI
aOR
a95
C
I
New
inje
ctio
n pa
rtner
in p
ast 3
0 da
ys
Yes
275
131
(48
)R
efer
ent
No
112
62 (5
5)
136
(08
8ndash2
12)
Age
at f
irst s
ex
le15
185
96 (5
2)
Ref
eren
t
gt15
167
76 (4
6)
129
(08
5ndash1
96)
Num
ber o
f sex
par
tner
s pas
t 6 m
onth
s
le1
213
106
(50
)1
45(0
49ndash
097
)
gt1
130
59 (4
5)
Ref
eren
t
New
sex
partn
er p
ast 6
mon
ths
Yes
163
77 (4
7)
Ref
eren
t
No
172
85 (4
9)
109
(07
1ndash1
68)
STIb
Yes
6842
(62
)1
80(1
05ndash
307
)
196
(11
2ndash3
42)
No
319
151
(47
)R
efer
ent
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
7844
(56
)R
efer
ent
No
2112
(57
)1
03(0
39ndash
272
)
Ever
bee
n in
pris
on o
r jai
l
Yes
140
76 (5
4)
130
(08
6ndash1
98)
No
239
114
(48
)R
efer
ent
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
205
102
(50
)1
03(0
66ndash
151
)
No
163
81 (5
0)
Ref
eren
t
Hav
e he
alth
insu
ranc
e
Yes
306
155
(51
)1
19(0
73ndash
195
)
No
8037
(46
)R
efer
ent
Ever
rece
ived
dru
g tre
atm
ent
Yes
116
59 (5
1)
107
(06
9ndash1
65)
No
270
133
(49
)R
efer
ent
P lt
20
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 13
P lt
05
P
lt 0
1
a Def
ined
as s
harin
g ne
edle
s with
out u
sing
ble
ach
usi
ng a
sing
le sy
ringe
to m
ix o
r div
ide
drug
s or
shar
ing
cook
ers
cotto
n or
wat
er
b Def
ined
as h
isto
ry o
f syp
hilis
of c
urre
nt in
fect
ion
with
gon
orrh
ea o
r chl
amyd
ia a
s det
erm
ined
by
biol
ogic
al te
stin
g at
tim
e of
inte
rvie
w
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 14
Table 2
Unadjusted correlates of having been recently tested and having received test results among injection drugusers who did not self-report being HIV-infected St Petersburg Russia 2005ndash2006 (n = 315)
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Sex
Male 237 48 (20) 147 (081 270)
Female 78 21 (27) Referent
Age
le25 years 106 23 (22) 102 (058 182)
gt25 years 209 46 (22) Referent
Currently employed
Full- or part- time 104 26 (25) 135 (077 236)
Not employed 207 41 (20) Referent
IDU past 30 days
Yes 275 61 (22) Referent
No 33 6 (18) 128 (051 323)
Age at first IDU
le18 143 35 (24) Referent
gt18 171 33 (19) 135 (079 231)
Duration of IDU
le5 years 99 21 (21) 104 (058 185)
gt5 years 215 47 (22) Referent
Frequency of IDU in past 30 days
lt30 213 43 (20) 133 (075 238)
ge30 95 24 (25) Referent
Number of IDU partners past 30 days
le2 191 41 (21) 106 (061 182)
gt2 124 28 (23) Referent
Unsafe injection in past 30 daysa
Yes 197 40 (20) 129 (075 223)
No 118 29 (25) Referent
New injection partner in past 30 days
Yes 224 50 (22) 109 (060 198)
No 91 19 (21) Referent
Age at first sex
le15 151 33 (22) Referent
gt15 136 29 (21) 102 (058 180)
Number of sex partners past 6 months
le1 171 38 (22) 102 (057 182)
gt1 109 24 (22) Referent
New sex partner past 6 months
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 15
Covariate Total No () having been testedin past 12 months and
received test result
uOR 95 CI
Yes 131 26 (20) 102 (067 214)
No 141 32 (23) Referent
STIb
Yes 55 12 (22) 102 (050 204)
No 260 57 (22) Referent
Ever pregnant (women only)
Yes 59 19 (32) 356 (074 172)
No 17 2 (12) Referent
Ever been in prison or jail
Yes 107 29 (27) 165 (095 287)
No 201 37 (18) Referent
Doctor visit in past 12 months
Yes 152 46 (30) 306 (168 559)
No 145 18 (12) Referent
Have health insurance
Yes 245 58 (24) 164 (080 332)
No 69 11 (16) Referent
Ever received drug treatment
Yes 87 24 (28) 154 (089 273)
No 227 45 (20) Referent
P lt 20
P lt 05
P lt 01
aDefined as sharing needles without using bleach using a single syringe to mix or divide drugs or sharing cookers cotton or water
bDefined as history of syphilis of current infection with gonorrhea or chlamydia as determined by biological testing at time of interview
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Niccolai et al Page 16
Tabl
e 3
Adj
uste
d co
rrel
ates
for
the
entir
e sa
mpl
e an
d by
sex
of h
avin
g be
en re
cent
ly te
sted
and
hav
ing
rece
ived
test
resu
lts a
mon
g in
ject
ion
drug
use
rs w
ho d
idno
t sel
f-re
port
bein
g H
IV-in
fect
ed S
t Pe
ters
burg
Rus
sia
200
5ndash20
06 (n
= 3
15)
Tot
alM
enW
omen
OR
95
CI
OR
95
CI
OR
95
CI
Doc
tor v
isit
in p
ast 1
2 m
onth
s
Yes
306
(16
8ndash5
59)
3
66(1
75ndash
770
)
NS
No
Ref
eren
taR
efer
ent
Ever
bee
n in
pris
on o
r jai
l
Yes
NS
212
(10
8ndash4
42)
N
S
No
Ref
eren
t
Ever
pre
gnan
t (w
omen
onl
y)
Yes
NA
NA
356
(07
4ndash17
2)
b
No
Ref
eren
t
NS
not s
igni
fican
t in
final
mul
tivar
iate
mod
el
NA
not a
pplic
able
for i
nclu
sion
in in
itial
mul
tivar
iate
mod
el
P lt
10
P
lt 0
5
P
lt 0
1
a Estim
ates
are
the
sam
e as
una
djus
ted
beca
use
no o
ther
cov
aria
tes w
ere
reta
ined
in th
e m
odel
b Thou
gh th
is e
stim
ate
did
not a
chie
ve st
atis
tical
sign
ifica
nce
and
P lt
05
it is
pre
sent
ed b
ecau
se it
was
mar
gina
lly si
gnifi
cant
and
bas
ed o
n a
smal
ler s
ampl
e si
ze (f
or w
omen
onl
y n
= 9
9) a
nd it
was
the
mos
t sig
nific
ant c
ovar
iate
and
the
only
one
ass
ocia
ted
amon
g w
omen
at P
lt 2
0
AIDS Behav Author manuscript available in PMC 2011 June 16