Fast T1- and T2-weighted pulmonary MR-imaging in patients with bronchial carcinoma
-
Upload
independent -
Category
Documents
-
view
2 -
download
0
Transcript of Fast T1- and T2-weighted pulmonary MR-imaging in patients with bronchial carcinoma
European Journal of Radiology 53 (2005) 478–488
Fast T1- and T2-weighted pulmonary MR-imagingin patients with bronchial carcinoma
M. Botha,∗, J. Schultzeb, M. Reutera, B. Bewigc, R. Hubnerc,I. Bobisc, R. Nothc, M. Hellera, J. Biederera
a Department of Diagnostic Radiology, University Hospital Schleswig-Holstein, Campus Kiel, Arnold-Heller-Strasse 9, 24105 Kiel, Germanyb Department of Radiation Therapy, University Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germanyc Department of Internal Medicine, University Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany
Abstract
Purpose: A prospective study to evaluate the diagnostic potential and limitations of three fast MRI sequences in patients with bronchialcarcinoma based on the comparison with spiral CT.Material and methods:Three fast chest MRI sequences from 20 patients with central or peripheral bronchial carcinoma were evaluated by twoobservers for relation of tumour to adjacent structures, lymph node enlargement, additional pulmonary lesions and artefacts. The informationf TR/TE4 trix 192× esR ated by alls pared to CTs ediastinall n imagingl entiationb quenceiC bronchialc sue froma©
K
1
lfacss
l ofthatn of
ailedournt lo-d tobjectiled
lungiation
0d
rom MR-imaging was compared with the results from spiral CT. MRI comprised a T1-3D-GRE breath-hold examination (“VIBE”,.5/1.9 ms, flip-angle 12◦, matrix 502× 512, 2.5 mm coronal slices), a breath-hold, T2-HASTE sequence (TR/TE 2000/43 ms, ma256, 10 mm coronal slices) and a respiration-triggered T2-TSE sequence (TR/TE 3000–6000/120 ms, matrix 270× 512, 6 mm transvers
lices). The FOV was adapted individually (380–480 mm).esults:The presence of the primary bronchial carcinoma and infiltration of thoracic structures by tumour tissue could be demonstrequences. VIBE sequence was more suitable for detecting small pulmonary nodules than the other MRI examinations, but comtill 20% of these lesions were missed. Contrary to VIBE and T2-weighted TSE scans, HASTE sequence was limited in imaging mymph nodes due to missing relevant findings in 2/20 patients. HASTE images significantly provided the lowest rate of artefacts iung parenchyma (P < 0.001 in peripheral parenchyma), but spatial resolution was limited in this sequence. Concerning the differetween tumour and adjacent atelectasis (n= 8), T2-weighted TSE imaging was superior to CT and VIBE in all cases and to HASTE se
n 4/8 patients.onclusion:The combination of VIBE and HASTE sequence allows for an adaequate imaging of thoracic processes in patients witharcinoma, limited only in visualizing small pulmonary nodules. To obtain more detail resolution and to differentiate tumour tisdjacent atelectasis, T2-TSE examination may be added in selected cases.2004 Elsevier Ireland Ltd. All rights reserved.
eywords:Bronchial carcinoma; Lung; MRI; CT
. Introduction
Bronchial carcinoma is one of the most frequent ma-ignant tumours worldwide regarding incidence and caseatality rate. Twenty percent of all lung cancers are classifieds small-cell carcinoma, usually treated by radiation orhemotherapy. The remaining entities, classified as non-mall-cell lung cancers, are divided into adenocarcinoma,quamous cell carcinoma and large cell carcinoma. In this
∗ Corresponding author. Tel.: +49 43 1597 3153; fax: +49 43 1597 3151.E-mail address:[email protected] (M. Both).
group, surgical resection is potentially therapeutic. Althese types of bronchial carcinoma have in commonthe prognosis is basically dependent on the extensiothe malignant process. Imaging has to provide detinformation about the anatomical extension of the tumand about metastatic spread to lymph nodes and distacalisations. Effective surgical treatment is usually limiteearly stages[1,2]. Cases of advanced disease may be suto palliative radiation therapy. In any circumstance, detaknowledge about localisation and dissemination ofcancer is essential for adequate surgery or planning radfields[1,3].
720-048X/$ – see front matter © 2004 Elsevier Ireland Ltd. All rights reserved.oi:10.1016/j.ejrad.2004.05.007
M. Both et al. / European Journal of Radiology 53 (2005) 478–488 479
A number of different diagnostic procedures for the eval-uation of primary tumour expansion and detection of thoraci-cal metastases are available[4]. At present, the basic imagingmodality is spiral computed tomography (CT). Nevertheless,the reported accuracies concerning mediastinal and chest wallinfiltration (39–86%) and the accuracies of lymph node stag-ing with CT (40–90%) are limited[1,5]. Since CT imagingrequires ionising radiation and since application of CT con-trast agents is limited in patients with allergies to ionizedcontrast media or in patients with renal insufficiency, alter-native imaging methods to help for diagnosis and staging arealways of interest.
Any competing method for imaging and staging of lungcancer such as magnetic resonance imaging (MRI) wouldhave to match the results that can be achieved with spiral CT[5].
The limitations to MRI of lung parenchyma arewell known. Due to its low proton density and strongsusceptibility- and motion-artefacts the lung remains a mostdifficult terrain for this modality. Nevertheless, the contin-uous development of MRI has markedly improved the spa-tial resolution of imaging pulmonary structures in healthysubjects and in patients with lung disease[6–9]. Differentnew sequences, each with specific advantages and disadvan-tages, have been proposed. Leutner and Schild stated thatT2-weighted turbo spin echo sequences should be includedih TE)p mai ease[ th-h pre-s rmall sses[ alsob noma[
ncea logi-c ntiono pacto l car-c
2
2
n age6 arci-n RIa reads (= sw ses,
bronchial carcinoma was proven histologically by biopsy be-fore MRI was performed. Patients with conditions preclud-ing from MRI (cardiac pacemaker, severe claustrophobia,weighting more than 120 kg) were not included into the study.Informed consent was obtained from all patients after the pro-cedure had been fully explained, thus the requirements of thelocal ethics committee were fulfilled.
2.2. MRI protocol
Patients were examined with commercial 1.5 T MRI unit(Magnetom Vision, Siemens, Erlangen, Germany) with amaximum gradient strength of 25 mT/m and rise time of600�s using the body phased array coil.
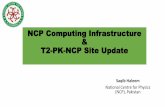
MRI was acquired with a coronal breathhold T1-weighted3D-GRE examination (volumetric interpolated breath-holdexamination (VIBE)); Siemens, Erlangen, Germany withTR/TE 4.5/1.9 ms, flip-angle 12◦, matrix 502× 512 (interpo-lated, slice thickness 2.5 mm), a coronal breathhold, cardiac-triggered T2-weighted half Fourier acquisition RARE se-quence (HASTE; Siemens, Erlangen, Germany with TR/TE2000/43 ms, matrix 192× 256, 10 mm slices) and arespiration-triggered T2-weighted fast spin-echo sequence(T2-TSE with TR/TE 3000–6000/120 ms, Matrix 270×512,6 mm slices) in transverse orientation (Fig. 1).
The 3D-GRE was applied to acquire three coronal slabso slabt eren -holdt mid-m labsw mmo lim-i sec-o
venc eachs theb tionb ther erea uesl qui-s pira-t L-)d
ndH tionw 380t
2
ectorr -g col-
n every pulmonary imaging protocol[7]. Also breath-holdalf-Fourier single-shot turbo spin-echo sequence (HASrovided a practical means for MRI of lung parenchy
n healthy subjects and in patients with pulmonary dis10]. Recently, in particular volumetric interpolated breaold technique with fast 3D GRE sequences has beenented as a fast, promising sequence in imaging no
ung parenchyma as well as pathologic pulmonary proce11–13]. Beside clinical indications, this sequence haseen discussed as a tool for screening for bronchial carci
12].Until now, the comparison of T2-TSE-, HASTE-seque
nd interpolated breath-hold technique in imaging pathoal pulmonal processes has not been performed. The intef this prospective study was to evaluate the clinical imf these three MRI-sequences in patients with bronchiainoma based on the comparison with spiral CT.
. Materials and methods
.1. Patients
Twenty consecutive patients: 16 male, 4 female, mea6 years (range: 55–82 years) suffering from bronchial coma (maximum size: 1.6–19.5 cm) were studied with Mnd CT of the thorax within 2 weeks. The diagnosesmall cell carcinoma (n = 8), squamous cell carcinoman7) and adenocarcinoma (n = 5). MRI and CT protocolere performed for accepted clinical indications. In all ca
f 80 mm thickness with 20 s breath-hold time for eacho cover the lung completely. Five to six acquisitions weeded, if 40 mm slabs were applied to reduce the breath
ime frame to 11 s. The first slab was centered on theediastinum and the tracheal bifurcation. Additional sere positioned anterior or posterior to this slab. A 10verlap was applied to avoid sampling errors at the slab
ts. Numeric slab positioning in 2.5 mm steps permittedndary reformations of the whole volume.
The T2-HASTE series was applied with slabs of seoronal slices and a breath-hold time frame of 18 s forlab. For respiration-triggered imaging with T2-TSE,reathing cycle was monitored with a pneumatic respiraelt. Image acquisition was started automatically whenespiration curve indicated 80% expiration. TR-values wdapted to the individual breathing cycle. With TR-val
imited to 50% of the respiration period (6–10 s), the acition segments would be completed before the next insion. The phase-encoding axis was oriented in right-left (Rirection. No contrast agents were administered.
The field of view for the coronal images with 3D-GRE aASTE and for the T2-TSE images in transverse orientaas adapted individually to each patient and ranged from
o 480 mm covering the lungs and the mediastinum.
.3. CT protocol
CT scans were performed on a commercial single detow spiral CT scanner (Somatom Plus-STM, Siemens, Erlanen, Germany). The whole lung was scanned with a beam
480 M. Both et al. / European Journal of Radiology 53 (2005) 478–488
Fig. 1. MRI of the lung in a 55-year-old patient (small cell carcinoma adjacent to the right hilus, invasion of the mediastinum (patient 4,Tables 1 and 2)):3D-GRE (VIBE) (a), HASTE (b) and T2-TSE sequence (c). Additional to the protocol, coronal slices also have been acquired in T2-TSE imaging to facilitatecomparison. 3D-GRE and T2-TSE scans are superior in outlining anatomical structures. Artefacts are negligible in HASTE sequence, while in VIBE andT2-TSE sequence especially imaging of the left lung is impaired by ghosting and breathing artefacts. Pleural effusion, separated in the apex of the chest, ismost easily seen in (b) and (c).
limation of 8 mm and a table speed of 12 mm/s (rotation-time1 s, pitch factor 1.5, 210 mA s, 137 kV) from the lung apicesto the diaphragm. All scans were obtained with intravenousapplication of 60 ml iodinated contrast agent (Imagopaque300TM, Nycomed, Ismaning, Germany) and a fixed scan de-lay 20 s. Images were reconstructed with an increment 6 mm(overlapping reconstruction) with a slim reconstruction pro-file and an edge-enhancing algorithm at a matrix of 512×512 pixels.
2.4. Image analysis
MRI and CT were assessed by two blinded observers onconsensus (J.B. and M.B.) at random order. CT was defined as
the reference imaging modality to evaluate the different MRI-sequences. No surgical-pathologic staging was performed.
A structured report was provided for each examination.Assessment of the primary tumour was performed with re-gard to its relations to adjacent structures. Local mediastinalinvasion by tumor tissue was stated in case of replacementof fat or of other mediastinal structures, tumour contactinga vessel like the aorta more than 90◦ of the circumferenceor contiguity to mediastinal structures more than 3 cm[4](Fig. 2). Chest wall invasion was assumed if rib destruc-tion, soft tissue masses in the chest wall or a long lengthof contact between tumor and chest wall were found[2]. Ad-ditional pulmonary masses or nodules and pleural effusionswere recorded. The maximum transverse diameter of pul-
M. Both et al. / European Journal of Radiology 53 (2005) 478–488 481
Fig. 2. HASTE (a), VIBE (b) and T2-TSE (c) sequence as well as CT (d) demonstrate a small cell carcinoma (patient 12,Tables 1 and 2) with long distancecontiguity to the pericardium as a sign of infiltration.
monary nodules was measured in CT as well as in the MRIsequences. Atelectases were judged to be partial (segmentaland lobar) or total. Hilar and mediastinal lymph nodes wereassessed and regarded as enlarged if the diameter was morethan 10 mm in the transverse plane. As far as examined, wealso evaluated upper abdomen and osseous structures in bothMR and CT imaging to detect distant metastases in theseregions.
T2-TSE-, HASTE- and VIBE-sequence were evaluatedwith regard to artefacts due to breathing or cardiac pulsation.In all 20 patients, each lobe of the long (central parenchymaseparated), mediastinum and the primary tumour were scoredfor the presence of artefacts (score 0: no artefacts, score 1:minor artefacts, score 2: strong artefacts, score 3: severe arte-facts, imaging quality insufficient for diagnostic purposes).Spatial resolution of the three MRI-sequences was rated inthe area of the primary bronchial carcinoma (score 0: sharpcontours, score 1: images slightly blurred, score 2: imagesseverely blurred, score 3: insufficient demarcation of find-ings).
The significance of differences between the scores for arte-facts and spatial resolution were calculated with two-sidedStudent’s pairedt-test.
These observations were used to discuss the contributionof each sequence to the whole examination.
3. Results
In all patients, the reports from MRI and CT agreed in thediagnosis of a pulmonary mass, most probably a bronchialcarcinoma. In each case, the presence of bronchial carcinomacould be confirmed by biopsy and histopathologic work up.The proven histology is listed inTable 1.
Examination times for VIBE sequence ranged from 5 to10 min and for respiration-gated T2-weighted TSE imagesfrom 20 to 30 min. HASTE imaging of the lung was feasiblewithin 5 min.
3.1. Diagnoses based on imaging findings
The clinical results from MRI readings (infiltration of tho-racic structures by the primary tumour, mediastinal lymphnodes and additional findings) and the comparison with re-sults from CT scanning are listed inTable 2.
482 M. Both et al. / European Journal of Radiology 53 (2005) 478–488
Table 1Clinical data of 20 patients in the study group
Patient Sexa Age Histologyb Primary tu-mour site
Maximumdiameterc
1 m 76 Squamous cell Central 242 m 71 Squamous cell Central 553 f 55 Small cell Central 804 m 55 Small cell Central 1005 m 82 Squamous cell Peripheral 166 f 77 Adenocarcinoma Peripheral 457 m 65 Small cell Central 248 m 75 Squamous cell Central 759 m 59 Squamous cell Central 33
10 m 81 Adenocarcinoma Peripheral 3711 m 65 Adenocarcinoma Central 2012 f 58 Small cell Central 6413 f 62 Adenocarcinoma Peripheral 5514 m 59 Squamous cell Peripheral 2015 m 66 Adenocarcinoma Peripheral 1916 m 59 Small cell Central 12517 m 61 Small cell Central 3418 m 72 Squamous cell Peripheral 4819 m 63 Small cell Central 12020 m 64 Small cell Central 195
a m: male, f: female.b Type of the bronchial carcinoma, histologically proven.c Maximum size of the primary tumour in cm, measured by CT in the
transverse plane.
In 11 patients, CT revealed infiltration of different thoracicstructures. All of these findings could be reliably demon-strated by T2-TSE- HASTE- and VIBE-sequence. Therewere no signs of tumour infiltration in MR imaging which didnot correlate with CT. Therefore, the sensitivity and specifityof each MRI sequence in detecting signs of invasive tumourtissue was 100%, compared to CT.
Beside primary bronchial carcinoma, 15 additional pul-monary nodules (3–21 mm) were found in five patients in CT.VIBE-sequence succeeded in imaging 80% (12/15) of thesenodules, the minimum diameter was 4 mm. T2-TSE- andHASTE-sequence proved to visualize pulmonary nodules assmall as 5 mm with a lesser overall detection rate (T2-TSE:7/15 nodules, HASTE: 9/15 nodules). Total nodules in a pa-tients lungs were depicted in 3/5 patients by VIBE-sequenceand in only 1/5 patients by T2-TSE-and HASTE-sequence,respectively. False positive findings were integrated into theevaluation of artefacts.
In the category “detection of maximum mediastinal lymphnode”, the performance of HASTE-sequence was limiteddue to missing relevant lymph node findings in 2/20 (10%)patients, compared to CT. Including lymph nodes with amaximum transverse diameter≤10 mm, HASTE-sequenceeven failed in 5/20 cases (25%), while with T2-TSE-imagingin only one patient (5%) small mediastinal lymph nodes(≤10 mm) could not be detected.
uldb find-i
Additional findings included atelectases (n = 8), pleuraleffusion (n = 2), adrenal metastases (n = 2) and a liver cyst(n = 1). These diagnoses were stated by CT as well as by allapplied MRI scans.
In patients with tumour-associated atelectasis (n= 8), MRI(particularly T2-TSE-, but also HASTE-sequence) provided abetter demarcation of atelectasis against tumor. T2-weightedTSE imaging was superior to CT and VIBE in all cases andto HASTE sequence in 4/8 patients, but this did not affectthe diagnosis in regards of the invasive character of advancedmalignant processes.
3.2. Artefacts and spatial resolution
With regard to comprehensive scoring of breathing andcardiac pulsation artefacts HASTE-scans provided the lowestartefact scores compared to the other MRI sequences in allparts of the lung (Table 3). The average total artefact scorefor HASTE ranged from 0 to 1.1 while T2-TSE and VIBEreached 0.9–1.8 and 1.0–1.5, respectively. The differencesbetween the sequences were highly significant (P< 0.001) inperipheral parenchyma. In the central parts of the lung, totalartefacts were significantly lower in HASTE- than in VIBE-sequence (P < 0.05), while differences to the T2-TSE-scanswere not significant
Total artefacts in mediastinal structures were comparablei mours tala
ves-s acts.P ver0 er-a d byt
thatH anyt geso 0.3,b ng(
aryb E-s e (av-e ages cesb
4
n ofp pa-t l-i MRI-a cient
Using VIBE-sequence, the maximum lymph node coe detected in all cases, but there was one false positive
ng.
n all evaluated sequences. Concerning the primary tuite, HASTE was superior to T2-TSE and to VIBE (tortefact score 0.6 for HASTE,P < 0.05).
In all MRI-sequences, artefacts related to cardiac andel pulsation were more prominent than breathing artefulsation artefacts ranged from 0.1 to 0.9 for HASTE o.9–1.5 for VIBE to 0.9–1.7 for T2-TSE, respectively. Ovll, the resulting total artefact scores were predominate
he contribution of pulsation artefacts.Further detailed analysis of artefacts revealed
ASTE-scans were not affected by breathing artefacts inhoracic region. Minor breathing artefacts occurred in imabtained with the VIBE-sequence ranging from 0.1 tout were still significantly lower than in T2-TSE imagi0.4–1.3 for T2-TSE,P < 0.05) [Table 3].
Detail resolution at the tumour site (the area of the primronchial carcinoma), was significantly inferior in HASTcans (average score 1.6) compared to VIBE-sequencrage score 0.9,P < 0.05 and to T2-TSE-sequence (avercore 0.7,P < 0.001). There were no significant differenetween VIBE- and T2-TSE-images.
. Discussion
Reliable imaging is indispensable to the determinatiorognosis and to the selection of adequate therapy in
ients with bronchial carcinoma[4,14]. The standard modaty is spiral CT, although several studies have presentedssessment of bronchial carcinoma as a similarly effi
M.B
othetal./E
uropeanJournalofR
adiolog
y53(2005)
Table 2Imaging findings as demonstrated by the applied MRI sequences and by CT
Patient Infiltration of thoracic structures Mediastinal lymph nodes: discordance to CT Additional findings
CT VIBE HASTE T2-TSE VIBE HASTE T2-TSE CT VIBE HASTE T2-TSE
1 Main bronchus Main bronchus Main bronchus Main bronchus × − − − −2 Main bronchus Main bronchus Main bronchus Main bronchus× Adrenal met.
segm. atelect.+
Adrenal met.segm. atelect.+
Adrenal met.segm. atelect.++
Adrenal met.segm. atelect.+++
3 Main bronchusmediast.pleura
Main bronchusmediast.pleura
Main bronchusmediast.pleura
Main bronchusmediast.pleura
Segm. atelect.−
Segm. atelect.++
Segm. atelect.+++
Segm. atelect.+++
4 Mediastinum Mediastinum Mediastinum Mediastinum Pleuraleffusion segm.atelect.−
Pleuraleffusion segm.atelect. +
Pleuraleffusion segm.atelect. +++
Pleural effu-sion segm.atelect. +++
5 − − − − − − − −6 − − − − × − − − −7 − − − − − − − −8 Mediastinum
tracheaMediastinumtrachea
Mediastinumtrachea
Mediastinumtrachea
One pulm.nodule
One pulm.nodule
− −
9 Mediastinum Mediastinum Mediastinum Mediastinum × Liver cyst Liver cyst Liver cyst Liver cyst10 − − − − Four pulm.
nodulesTwo pulm.nodules
One pulm.nodule
One pulm.nodule segm.atelect. ++
11 − − − − Adrenal met. Adrenal met. Adrenal met. Adrenal met.12 Pericardium Pericardium Pericardium Pericardium Segm. atelect.
−Segm. atelect.+
Segm. atelect.+
Segm. atelect.+++
13 Lower lobebronchus
Lower lobebronchus
Lower lobebronchus
Lower lobebronchus
Lobar atelect.−
Lobar atelect.−
Lobar atelect.+++
Lobar atelect.+++
14 − − − − × − − − −15 − − − − × × − − − −16 Main bronchus
mediastinumMain bronchusmediastinum
Main bronchusmediastinum
Main broncmediastinu
17 − − − −
18 − − − −
19 Mediastinumdesc. aortaoesophagus
Mediastinumdesc. aortaoesophagus
Mediastinumdesc. aortaoesophagus
Mediastinudesc. aortaoesophagu
20 Mediastinumthoracic wall
Mediastinumthoracic wall
Mediastinumthoracic wall
Mediastinuthoracic wa
(×) Discordant mediastinal lymph node findings in MRI compared to Csufficient, (+++) excellent.
478–488
483
husm
Pleuraleffusion lobaratelect.−
Pleuraleffusion lobaratelect.−
Pleuraleffusion lobaratelect. ++
Pleural ef-fusion lobaratelect. +++
Eight pulm.nodules
Eight pulm.nodules
Seven pulm.nodules
Five pulm.nodules
One pulm.nodule
− − −
m
s
Total atelect.−
Total atelect. + Total atelect. + Total atelect.++
mll
One pulm.nodule segm.atelect.−
One pulm.nodule segm.atelect. +
One pulm.nodule segm.atelect. ++
One pulm.nodule segm.atelect. ++
T; met.: metastasis, atelect.: atelectasis, segm.: segmental. Differentiation of atelectasis from tumour: (−) not possible, (+) limited, (++)
484 M. Both et al. / European Journal of Radiology 53 (2005) 478–488
Table 3Average artefact score as found in the study group in different pulmonary localisations
Pulsation artefacts Breathing artefacts Total artefacts
VIBE HASTE T2-TSE VIBE HASTE T2-TSE VIBE HASTE T2-TSE
Right upper lobe 1.2 0.1 1.2 0.2 0 0.9 1.3 0.1 1.3Right middle lobe 1.5 0.2 1.7 0.3 0 1.2 1.5 0.2 1.8Right lower lobe 1.3 0.2 1.4 0.3 0 1.3 1.3 0.2 1.5Left upper lobe 1.4 0.2 1.5 0.2 0 1.0 1.4 0.2 1.6Left lower lobe 1.4 0.4 1.4 0.3 0 1.3 1.4 0.4 1.6Central parenchyma 1.5 0.9 1.3 0.1 0 0.7 1.5 0.9 1.3Mediastinum 1.1 1.1 0.9 0.1 0 0.4 1.1 1.1 0.9Bronchial carcinoma 0.9 0.6 1.1 0.1 0 0.7 1.0 0.6 1.2
Score 0: no artefacts, score 1: minor artefacts, score 2: strong artefacts, score 3: severe artefacts, imaging quality insufficient for diagnostic purposes.
method [5,15]. While recently the feasibility and ef-fectiveness of low-dose CT algorithms in screening forbronchial carcinoma is evaluated in several studies[16],pulmonary MR screening has not been subject to clinicalstudies.
Deficits of MRI owing to the low proton density of thelung parenchyma (resulting in a low signal-to-noise-ratio),
FEi
reduced T2∗ due to susceptibility artefacts at air-tissue inter-faces, motion artefacts due to breathing, ghosting related tothe pulsation of heart and vessels and long acquisition timeshave limited its clinical acceptance in imaging pulmonarydisease[7]. However, superior soft tissue contrast and the ab-sence of ionizing radiation[13,14] are inherent advantagesof MRI.
ig. 3. Small peripheral squamous cell carcinoma in the right upper lobe ofxcellent spatial resolution is obtained using VIBE sequence (a), while HAS
maging (c) does not provide additional advantages.
a 59-year-old patient (patient 14,Tables 1 and 2) who denied surgical resection.TE sequence (b) is superior in avoiding artefacts. Respiration-triggered T2-TSE
M. Both et al. / European Journal of Radiology 53 (2005) 478–488 485
Fig. 4. Small cell carcinoma (patient 20,Tables 1 and 2) with extensive, confluent mediastinal and hilar lymph node masses on the left side. A small pulmonarynodule (8 mm, white arrow) in the right upper lobe is visualized by all applied MRI sequences ((a) HASTE, (b) VIBE, (c) T2-TSE) and is proven by CT imaging(d).
The continuous development of MR-technology encour-aged us to conduct this study to estimate the clinical value ofpulmonary imaging in patients with bronchial carcinoma us-ing three fast MR-sequences at the current state of MR imag-ing technique. It was intended to evaluate the potential roleof each sequence to establish a standard protocol for imagingbronchial carcinoma and associated thoracic processes.
In this study, we combined a T1-weighted 3D-GRE se-quence with volumetric interpolation (“VIBE”), a breathhold,cardiac-triggered T2-weighted HASTE- and a T2-weightedTSE-sequence. MR imaging was performed without contrast-enhancement because according to recent literature, the min-imal improvement in sensitivity and specificity does not seemto warrant the routine use of gadolinium[14]. To reduce sam-pling errors in breath hold imaging, VIBE and HASTE scanswere performed in coronal orientation because the motionpattern of the lung during inspiration and expiration pre-dominantly implies expansion along the body axis[17]. In
T2-weighted TSE imaging, respiration triggering guaranteedimage acquisition in a constant phase of the breathing cy-cle. Thus, this sequence could be performed in the transverseorientation as CT.
3D-GRE sequences with short TR and TE initially weredeveloped for MR angiography[18]. As a substantial advan-tage of the presented 3D-GRE (VIBE) protocol, this sequencecan be applied as a breath-hold examination without cardiacor respiratory triggering to overcome artefacts from respira-tory motion.
Compared to fast two-dimensional GRE sequences, 3DGRE VIBE sequence appears superior due to the lesser re-duction of signal-to-noise-ratio with small voxel sizes[12].3D-GRE has been proven to provide high spatial resolution,good visualization of lung anatomy and low rates of artefactsin healthy volunteers[11]. These imaging qualities could beconfirmed in recent studies using 3D-GRE-sequences in awide spectrum of malignant and benign pulmonary diseases
486 M. Both et al. / European Journal of Radiology 53 (2005) 478–488
Fig. 5. Sixty-two-year-old patient with tumour associated lobar atelectasis (patient 13,Tables 1 and 2). CT imaging (a) is unable to differentiate tumourtissue from adjacent atelectasis reliably. Due to hyperintensity of obstructive atelectasis, T2-weigthed MR imaging (T2-TSE (b), HASTE (c)), provides betterseparation against tumour than CT and T1-GRE (VIBE) (d).
[12,13]. Besides these examinations in patients, the potentialability of VIBE-sequence to detect nodules smaller than 5mmwith high diagnostic accuracy has been also demonstrated bysimulated pulmonary nodules implanted in a porcine chestphantom[19].
In our study, this combination of angiographic capabilitiesand a high spatial resolution with reasonable soft tissue signal(Fig. 3) enabled VIBE scans to precisely visualize invasionof large vessels and other mediastinal structures. Pulmonarynodules as small as 4 mm were depicted more reliable byVIBE sequence than by the other evaluated MRI sequences.Compared to CT, missed pulmonal lesions could be corre-lated with the presence of artefacts in these regions retro-spectively. In patients with respiratory distress, thinner slabsof 40 mm had to be applied to reduce the breath-hold timeframe from 20 to 11 s. This is a limitation of our study becausethe comparability for motion artefacts scoring decreased dueto inconsistency of the VIBE protocol.
The HASTE-sequence, a fast single-shot turbo spin echosequence, is described as a useful breath-hold T2-imagingprocess in lung parenchyma. Particularly due to a short echo
spacing, this pulse sequence is relatively resistant to inho-mogeneous magnetic susceptibility of the lung parenchyma[10,20]. Because water-rich processes show very high sig-nal intensity in HASTE-sequence, lung parenchymal lesionsappear bright when this sequence is applied. As a disadvan-tage of HASTE-sequence, soft-tissue resolution is usuallylimited due to T2 filtering effects (T2 decay in later echosduring data acquisition), resulting in blurred images[20,21].Consequently, spatial resolution in the area of the bronchialcarcinoma was inferior to VIBE and T2-TSE-series, and alsoassessment of mediastinal lymph nodes and pulmonal nod-ules was limited. On the other hand, the HASTE sequence wasas sensitive as the other sequences for infiltrative processes.In case of obstructive dystelectatic processes adjacent to tu-mour tissue, HASTE scans provided even better demarcationthan VIBE series since fluid containing atelectasis were pre-sented with high signal intensity. In our study, an importantadvantage of HASTE scans was the low rate of pulsation arte-facts and the absence of relevant respiratory motion artefacts(Figs. 1–5). This may be particularly valuable in patients withsevere pulmonary disease and respiratory distress.
M. Both et al. / European Journal of Radiology 53 (2005) 478–488 487
T2-weigthed turbo spin echo sequences are the most es-tablished modality in MR imaging of the thorax and havebeen described as basic in pulmonary imaging protocols dueto high spatial resolution and good imaging quality for me-diastinal structures as well as for the lung periphery[7,22].Using multiple acquisition T2-TSE series, in our study norelevant advantage could be revealed especially compared toVIBE-sequence. There was a tendency to provide better spa-tial resolution and a better score for pulsation artefacts in themediastinum than VIBE scans, but the degree of discordancebetween the two methods was not significant. The T2-TSE-sequence was superior to CT and the other MRI series inseparating tumour from atelectasis in 8 patients (Table 2)due to the hyperintense appearance of obstructive atelectasis(Fig. 5) [23], nevertheless this was not relevant for clinical di-agnosis in the presented cases. Disadvantages of respiration-triggered, high resolution T2-TSE-series are longer acquisi-tion times and a tendency to increased artefacts in peripherallung parenchyma compared to T1-GRE[22] and particularlyto the HASTE sequence.
As a limitation of our study, MRI and CT staging couldnot be compared to intraoperative findings because advanced,unresectable malignant processes were found in 16 patients.Three patients could not be treated surgically due to impairedhealth conditions, one patient refused surgical resection. Con-sequently, surgical-pathologic staging according to the inter-n d.
hi-l usings amicM
pop-u nityo eralt nces.N ith an tate-o R-i
E-s racicp or ani od-u gingm ions,b tientsw encei andb
lica-t ddi-t use-f ever,t arlym gingl e
with newly developed multiple detector row CT. Neverthe-less, as a contribution to the discussion, whether MRI withit’s unique properties like absence of ionizing radiation andexcellent soft tissue contrast may play a role in lung can-cer screening or not, the results of the present study give anoverview over what can be expected from MRI as a potentialscreening tool.
References
[1] Patz EF. Imaging bronchogenic carcinoma. Chest 2000;117(4(Suppl.1)):90S–5S.
[2] Haramati LB, White CS. MR imaging of lung cancer. MRI ClinNorth Am 2000;8(1):43–57.
[3] Krempien R, Schubert K, Latz D, Wenz F, Wannemacher M. Ra-diotherapy treatment simulation of bronchogenic carcinoma usingan open low-field magnetic resonance system. Strahlenther Onkol1999;175(6):279–83.
[4] Wunderbaldinger P, Bankier AA, Strasser G, Hoffmann U, Schafer-Prokop C, Herold CJ. Staging of bronchial carcinoma. Radiologe1999;39(7):525–37.
[5] Haberkorn U, Schoenberg SO. Imaging of lung cancer with CT, MRIand PET. Lung Cancer 2001;34(Suppl. 3):13–23.
[6] Kauczor HU, Kreitner KF. MRI of the pulmonary parenchyma. EurRadiol 1999;9(9):1755–64.
[7] Leutner C, Schild H. MRI of the lung parenchyma. Fortschr Roent-genstr 2001;173(3):168–75.
Care
Eur
[ naryTE)
[ ng ofnce.
[ MRtech-2–9.
[ linaseasel ob-
[ ndAm
[ m-bron-
[ ction
[ Q.nor-I. J
[ mag-adiol
[ latedntom:(2):
ational TNM-staging system staging was not performeMore detailed results in evaluating mediastinal and
ar lymph node metastases might have been obtaineduperparamagnetic ultra-small iron oxide particles, dynRI or PET[5,24,25].As a minor weakness of the present work, the study
lation is too small for further statistics. The inhomogef the study group allowed only to detect and judge gen
endencies in the performance of the applied MRI sequeevertheless, even if regarded as a collection of cases wumber of different findings, it represents the current sf-the-art of basic fast MRI sequences for pulmonary M
maging in patients with bronchial carcinoma.In conclusion, the combination of VIBE- and HAST
equences provides fast and sufficient imaging of thorocesses in patients with bronchial carcinoma, except f
nferior performance in detection of small pulmonary nles compared to CT. VIBE sequence is superior in imaediastinal lymph nodes and small intrapulmonary les
ut these potencies may be reduced by artefacts in paith respiratory distress. In these patients, HASTE sequ
s advantageous due to its limited susceptibility to motionreathing artefacts.
In patients with tumour associated atelectasis, the appion of respiration-triggered T2-weighted TSE scans in aion to the other sequences or to CT appears potentiallyul to separate tumour mass from atelectatic lung. Howhe performance of spiral CT in general can be only neatched at present and any improvements in MR ima
ike ECG-triggered 3D-sequences[26] will have to compet
[8] White CS. Magnetic resonance imaging of the chest. Respir2001;46(9):922–31.
[9] Ohno Y, Sugimura K, Hatabu H. MR imaging of lung cancer.J Radiol 2002;44(3):172–81.
10] Hatabu H, Gaa J, Tadamura E, et al. MR imaging of pulmoparenchym with a half-Fourier single-shot turbo spin-echo (HASsequence. Eur J Radiol 1999;29(2):152–9.
11] Biederer J, Graessner J, Heller M. Magnetic resonance imagithe lung with a volumetric interpolated 3D-gradient echo sequeFortschr Roentgenstr 2001;173(10):883–7.
12] Biederer J, Both M, Graessner J, et al. Lung morphology: fastimaging assessment with a volumetric interpolated breath-holdnique: initial experience with patients. Radiology 2002;226(1):24
13] Bader TR, Semelka RC, Pedro MS, Armao DM, Brown MA, MoPL. Magnetic resonance imaging of pulmonary parenchymal diusing a modified breath-hold 3D gradient-echo technique: initiaservations. J Magn Reson Imaging 2002;15(1):31–8.
14] Thompson BH, Stanford W. MR imaging of pulmonary amediastinal malignancies. Magn Reson Imaging Clin N2000;8(4):729–39.
15] Manfredi R, Pirronti T, Bonomo L, Marano P. Accuracy of coputed tomography and magnetic resonance imaging in stagingchogenic carcinoma. MAGMA 1996;4(3–4):257–62.
16] Diederich S, Wormanns D, Heindel W. Early lung cancer detewith low-dose CT: an update. Radiologe 2002;42(8):608–11.
17] Napadow VJ, Mai V, Bankier A, Gilbert RJ, Edelman R, ChenDetermination of regional pulmonary parenchymal strain duringmal respiration using spin inversion tagged magnetization MRMagn Reson Imaging 2001;13(3):467–74.
18] Leung DA, Debatin JF. Three-dimensional contrast-enhancednetic resonance angiography of the thoracic vasculature. Eur R1997;7(7):981–9.
19] Biederer J, Schoene A, Freitag S, Reuter M, Heller M. Simupulmonary nodules implanted in a dedicated porcine chest phasensitivity of MR imaging for detection. Radiology 2003;227475–83.
488 M. Both et al. / European Journal of Radiology 53 (2005) 478–488
[20] Yamashita Y, Yokoyama T, Tomiguchi S, Takahashi M, Ando M.MR imaging of focal lung lesions: elimination of flow and motionartefact by breath-hold ECG-gated and black-blood techniques onT2-weighted turbo SE and STIR sequences. J Magn Reson Imaging1999;9(5):691–8.
[21] Tang Y, Yamashita Y, Namimoto T, Abe Y, Takahashi M. LiverT2-weighted MR imaging: comparison of fast and conventionalhalf-Fourier single-shot turbo spin-echo, breath-hold turbo spin-echo, and respiratory-triggered turbo spin-echo sequences. Radiology1997;203(3):766–72.
[22] Biederer J, Reuter M, Both M, et al. Analysis of artefacts and detailresolution of lung MRI with breath-hold T1-weighted gradient-echoand T2-weighted fast spin-echo sequences with respiratory trigger-ing. Eur Radiol 2002;12(2):378–84.
[23] Gaeta M, Minutoli F, Ascenti G, et al. MR white lung sign: inci-dence and significance in pulmonary consolidations. J Comput AssistTomogr 2001;25(6):890–6.
[24] Bellin MF, Roy C, Kinkel K, et al. Lymph node metastases: safetyand effectiveness of MR imaging with ultrasmall superparamag-netic iron oxide particles: initial clinical experience. Radiology1998;207(3):799–808.
[25] Hasegawa I, Eguchi K, Kohda E, et al. Pulmonary hilar lymph nodesin lung cancer: assessment with 3D-dynamic contrast-enhanced MRimaging. Eur J Radiol 2003;45(2):129–34.
[26] Ohno Y, Adachi S, Motoyama A, et al. Multiphase ECG-triggered 3Dcontrast-enhanced MR angiography for evaluation of hilar and medi-astinal invasion of bronchogenic carcinoma. J Magn Reson Imaging2001;13(2):215–24.
















![bronchial-hygiene-therapy.ppt [Read-Only] - Semantic Scholar](https://static.fdokumen.com/doc/165x107/6317b9679076d1dcf80beb6a/bronchial-hygiene-therapyppt-read-only-semantic-scholar.jpg)













