Exploring the Use of Thermal Infrared Imaging in Human Stress Research
Transcript of Exploring the Use of Thermal Infrared Imaging in Human Stress Research
THERMAL SIGNATURE OF FEAR CONDITIONING IN MILD POSTTRAUMATIC STRESS DISORDER
A. DI GIACINTO, * M. BRUNETTI, G. SEPEDE,A. FERRETTI AND A. MERLA
ITAB – Institute for Advanced Biomedical Technologies, University ofChieti-Pescara, Italy
Department of Neuroscience and Imaging, University ofChieti-Pescara, Italy
Abstract—Fear conditioninghas beenproposed as an impor-tant factor involved in the etiology of posttraumatic stressdisorder (PTSD). We examined fear processing in PTSDpatients with mild symptoms and in individuals who did notdevelop symptoms (both groups consisting of victims of abank robbery), through the study of fear-conditionedresponse.Conditioned responseswerequantifiedby theskinconductance response (SCR) and the facial thermalresponse, the latter beingmeasured by high-resolution func-tional thermal infrared (fIR) imaging. We found: (a) a changeof the physiological parameters with respect to the baselinecondition in both control subjects and PTSD patients duringthe conditioning phase; (b) the permanence of the condition-ing effect in themaintenance phase in both control and PTSDpatients; (c) patients and controls did differ for the variationacross the phases of the physiological parameters ratherthan for their absolute values, showing that PTSD patientshad a prolonged excitation and higher tonic component ofautonomic activity. These results, although preliminary, indi-cate that the analysis of SCRand facial thermal responsedur-ing the conditioning paradigm is a promising psychometricmethod of investigation, even in the case of low level of PTSDsymptomseverity. To the best of our knowledge, this study isthefirst attempt to discriminate between control subjects andPTSD patients with mild symptoms through infrared thermalimaging. It may suggest feasible approaches for diagnosticscreening in the early phases of the disorder and in theassessment of preventive measures and therapies.! 2014 IBRO. Published by Elsevier Ltd. All rights reserved.
Key words: conditioning, emotion, thermal imaging, posttraumatic stress disorder (PTSD).
FEAR IS AN EVOLUTIONARY RESPONSE
Transient fear state is an advantage mechanism, whichcould turn into a pathological condition if occurring forlong-term. Pathological fear is a distinctive feature ofpatients suffering from post-traumatic stress disorder(PTSD), a clinical condition characterized by bothpsychological and physiological components. Indeed,PTSD patients present symptoms involving intrusivere-experiencing of traumatic events, avoidance ofreminders, emotional numbing and hyper-arousal(American Psychiatric Association, 2000, Diagnostic andStatistical Manual of Mental Disorders, 4th ed.DSM-IV-TR).
According to the DSM IV, PTSD patients may presenthigh physiological arousal (Criterion B5) to situations thathave low similarity with the experienced trauma, but thatcould overlap or share with them particular sensoryimpressions (e.g., similar color, smell or sound; Ehlersand Clark, 2000). Furthermore, exaggerated startleresponse (Criterion D5) expressed by significantincreases in the autonomic nervous system (ANS)response is usually observed.
Fear conditioning is a basic form of associativelearning, well studied at both the behavioral and neurallevels (Maren and Quirk, 2004; Quirk et al., 2006;Burgos-Robles et al., 2007), to investigate theaugmented physiological and emotional reactivity inPTSD patients (Foa et al., 1992; Rasmusson andCharney, 1997; Quirk and Mueller, 2008).
From a fear conditioning point of view, a traumaticevent serves as an unconditioned stimulus (US) thatelicits an unconditioned response like fear and higharousal. The US is associated with any stimuli (sights orsmells) present in the traumatic environment. As aconsequence, such stimuli could become conditionedstimuli (CS). Thereafter, despite the absence of the US,CS–US association produces conditioned responses,e.g. intense fear, at those stimuli similar to thosepresented in the traumatic context. Therefore theconditioned response persists even after the terminationof the conditioning (Fendt and Fanselow, 1999; LeDoux,2000), becoming a persistent conditioned response inPTSD (Friedman, 2006; Amstadter et al., 2009).Conversely, repeated presentations of the CS withoutthe US extinguishes the fear responses elicited by theCS (Brooks and Bouton, 1993) and it may represent amodel for the emotional regulation in healthy individuals,as the fear response is attenuated or extinguished bythe absence of the fear-related stimuli. Habituation
http://dx.doi.org/10.1016/j.neuroscience.2014.02.0090306-4522/! 2014 IBRO. Published by Elsevier Ltd. All rights reserved.
*Corresponding author. Address: Institute for Advanced BiomedicalTechnologies, University ‘‘G. D’Annunzio’’ of Chieti, Via dei Vestini,33, 66013 Chieti (CH), Italy. Tel: +39-0871-3555304; fax: +39-0871-3556930.E-mail address: [email protected] (A. Di Giacinto).Abbreviations: ANOVA, analysis of variance; ANS, autonomic nervoussystem; ASR, Acoustic Startle Response; CAPS, Clinician-Administered PTSD Scale; CS, conditioned stimulus; fIR, functionalinfrared imaging; GSR, Galvanic Skin Response; PTSD, post-traumaticstress disorder; SCR, skin conductance response; US, unconditionedstimulus.
Neuroscience 266 (2014) 216–223
216
allows individuals to ignore innocuous events byproducing a progressive decline in response to repeatedpresentations of a neutral stimulus via non-associativelearning (Hettema et al., 2003). Therefore, deficits in theextinction of the fear responses may reflect an abnormalemotional regulation similar to what observed in thePTSD patients (Sherin and Nemeroff, 2011).
Functional imaging studies have shown a correlationbetween blood-oxygen-level-dependent (BOLD) signal inthe amygdala and the skin conductance response(SCR) amplitude and occurrence in response to thepresentation of emotional stimulus (Liberzon et al.,2000; Williams et al., 2001; Hoffman et al., 2007).These responses include increases in ANS arousal(such as sweating, heart rate, blood pressure) and therelease of stress hormones (LeDoux, 1998). Theenhanced amygdala activity together with arousalsystems excitation are thought to allow the cortex todistinguish fear signals from other arousal responses tonovel stimuli (Damasio, 1995; LeDoux, 1996).
Previous studies about idiographic trauma imageryhave shown that PTSD patients report more pronouncedheart rate acceleration than control subjects andstronger facial expressions of displeasure concordantwith more extreme aversive ratings (Pitman et al., 1987;Cuthbert et al., 2003; Pole, 2007). Patients also exhibit astronger startle reflex response than controls duringidiographic threat-related imagery, consistent withenhanced limbic (in particular, amygdalar) andparalimbic activation. Indeed, PTSD patients interpretinnocuous stimuli as a potential threat (Lanius et al.,2006; Brunetti et al., 2010). An example of this is theAcoustic Startle Response (ASR), which consists of asequence of reactions caused by muscular and neuralresponses to sudden and intense acoustic stimuli.Conversely to healthy controls, a lack of habituation tothe ASR has been reported in PTSD patients, thusindicating a difficult evaluation of the sensory stimuli andof the appropriate mobilizing levels of neural andphysiological reactivity (Van der Kolk, 2003; Gloveret al., 2011). SCRs to subliminal salient emotional stimuliwere also delayed in PTSD patients with damage in theleft or right amygdala (Glascher and Adolphs, 2003).
Furthermore, PTSD patients show higher levels ofarousal in response to both conditioned (CS+) andunconditioned (US) stimuli (Peri et al., 2000; Orr et al.,2000; Norrholm et al., 2011) in paradigms based onfear-potentiated startle response, that is characterizedby the increase in the magnitude of the acoustic startlereflex elicited from a CS previously paired with an US.
In this pilot study, we wanted to assess whether thepsychophysiological responses of PTSD patients withmild symptoms during a new variant of conditioningparadigm differ from those observed in the subjects whodid not develop symptoms. To this end we measuredboth the SCR and the facial thermal response, the latterbeing measured by high-resolution functional thermalinfrared (fIR) imaging (Merla and Romani, 2007).
In fact, fIR imaging has proven to be a robust andecologically valid method to monitor an individual’sarousal through the effects that the autonomic activity
exerts on the facial cutaneous temperature (Shastriet al., 2009; Ebisch et al., 2012; Manini et al., 2013). Inparticular, we focused on the tonic component of theSCR, which is the slowly changing component of thesignal and it is related to the arousal level of the subject(Lim et al., 1997), and on the nose tip temperature,which is closely related to the tonic component of theSCR (Shastri et al., 2009).
We expected that mild PTSD patients would havehigher tonic average values in the conditioning andmaintenance phases than controls. Moreover, we didexpect to find reduced differences between conditioningand maintenance phases in patients with respect tocontrols. The same hypotheses hold for the nose tiptemperature.
EXPERIMENTAL PROCEDURES
Subjects
Ten PTSD patients and 10 healthy controls (Table 1)were recruited for this study. All the participants werebank clerks, victims of one or more armed bankassaults in the last 10 months before the experiments(range of 2–18 months). All participants underwent to anextensive clinical examination carried out by an expertpsychiatrist (GS) and a clinical psychologist (MB).
A broader range of traumatic event types, includingcar accidents and criminal attacks, was assessed usingthe event checklist of the Clinician Administered PTSDScale (CAPS) (Blake et al., 1998). Standardized clinicalinstruments were used for the assessment of DSM-IVdiagnoses by trained researchers: CAPS (Blake et al.,1990; Pieraccini et al., 1999) for the diagnosis andquantification of PTSD and related dissociative features(MB) and Mini International Neuropsychiatric Interviews(MINI) (Sheehan et al., 1994; Conti et al., 1999) fordiagnoses of DSM-IV Axis I disorders (GS). At the timeof the present study, participants met DSM IV diagnosticcriteria for the following current co-morbid diagnoses:dysthymia (n= 1 PTSD subject), agoraphobia withouthistory of panic attack disorder (n= 1 PTSD subject),and social phobia (n= 1 control subject). None of the
Table 1. Demographic and clinical characteristics of the two subjectgroups
Variable PTSD group
(n= 10)
Control group
(n= 10)
Mean age in years (SD) 39.7 (6.34) 36.8 (12.1)
Mean school educ. in years
(SD)
16 (2.5) 14 (2.1)
Females N (%) 6 (60) 6 (60)
Nicotine dependence N (%) 4 (40) 4 (40)
Trauma load [mean number
(range)]
5 (1–8) 4 (1–5)
CAPS PTSD symptom
score, mean (SD)
30.8* (11.2) 6.2* (6.9)
CAPS= Clinician Administered PTSD Scale.* Indices represent the results of ANOVA: (F(1,18) = 34.9, p 6 0.01).
A. Di Giacinto et al. / Neuroscience 266 (2014) 216–223 217
participants had been previously treated withpsychopharmacologic interventions.
All the subjects were right-handed (EdinburghInventory). Exclusion criteria included seizure disorder,progressive neurological and/or systemic disorders,significant unstable concurrent medical illness, hormonereplacement therapy, electroconvulsive or light therapy,administration of concomitant medication that could altermood (e.g. benzodiazepines, antidepressants, moodstabilizers, stimulants, and steroids) within 30 days priorto screening, history of any substance/alcohol abuse ordependence within the past 6 months (nicotinedependence was allowed and balanced betweengroups). In addition, all participants had no overt historyof cardiovascular, immunological or dermatologicaldiseases potentially impacting the normal cutaneousthermoregulation (i.e., diabetes, scleroderma, lupus,Raynaud’s Phenomenon) (Harding, 2007).
The demographic variables of the resulting two groupswere comparable (Table 1).
On the average, the CAPS index of severity of PTSDwas 30.8 (SD = 11.2) in the PTSD group and 6.2(SD = 6.9) in the control group. A one-way analysis ofvariance (ANOVA) confirmed the statistical significanceof the difference between the two average scores[F(1–18) = 34.9 p< 0.01].
All subjects received detailed explanations about thestudy design and provided written informed consentaccording to the Declaration of Helsinki (World MedicalAssociation Declaration of Helsinki, 1997). The protocolwas approved by the local Ethics Committee of theUniversity of Chieti-Pescara, Italy).
Stimuli and experimental design
Gray scale images of five different target faces (twoangry, two happy and one neutral) were selected from astandard set of pictures of facial affect (Ekman et al.,1983). The five faces were arranged in a series with apre-defined order of visualization, which was keptconstant through all the experimental procedure.
The series was presented 12 times and grouped inphases as follows:
– Baseline: 4 series repetitions, with no sound paired tothe images;
– Conditioning: 4 series repetitions, with 80-db whitenoise burst (US) paired to the fifth face. The soundlasted for the whole image presentation;
– Maintenance: 4 series repetitions, with no soundpaired to the images (CS).
Two successive faces were presented 18 s apart. Agray screen was presented during the interval betweentwo successive face images. Each series lasted 90 s,while the whole procedure lasted 1080 s. Each imagewas presented for 2 s and preceded by a fixation whitecircle or triangle, presented for 0.5 s. Participants wereasked to count the number of triangles or circles thatpreceded the presentation of the faces. This task wasonly intended to keep the attention of the participants onthe stimulus as the real functional and conditioningstimulus was represented by the sudden andunexpected white noise burst (US) during the view ofthe fifth image of the seconds four series repetition (seeFig. 1).
The visual stimuli were presented usingPresentation, a program produced by MATLAB (http://www.mathworks.com/). The stimuli were projected on a2100 LCD monitor, at a distance of 70 cm, while thesound was delivered through a surround speakersystem.
Physiological recordings
Thermal imaging. Prior to testing, each subject wasleft to acclimate for 10–20 min to the experimental roomand to allow the baseline skin temperature to stabilize.The recording room was set at standardizedtemperature (23 "C), humidity (50–60%), and withoutdirect ventilation. The subjects comfortably sat on achair during both acclimation and measurement periods,without any restriction to body movement.
Thermal IR imaging was performed by means of adigital thermal camera (FLIR SC3000, FlirSystems,Sweden), with a Focal Plane Array of 320 ! 240 QWIP
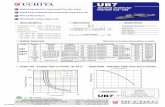
Fig. 1. Experimental paradigm. Upper panel: The series of the five faces and the presentation timing. The speaker icon on the fifth face identifiesthe acoustic stimulation (US). Bottom panel: The three experimental phases (baseline, conditioning, maintenance). Each phase comprises fourrepetitions of the five images series.
218 A. Di Giacinto et al. / Neuroscience 266 (2014) 216–223
detectors, capable of collecting the thermal radiation inthe 8–9 m band, with a 0.02-s time resolution, and0.02 K temperature sensitivity. The thermal cameraresponse was blackbody-calibrated to nullify noise-effects related to the sensor drift/shift dynamics andoptical artifacts. Sampling rate for thermal imaging wasset at 10 frames/s in order to correct for thedisplacement between images frame by frame usinganatomical landmarkers based on the subject’s noseprofile (Ebisch et al., 2012).
SCR. The SCR reflects the activation of the ANS. Weused SCR as a verification of the facial thermal response.SCR was recorded using the ADInstruments PowerLab16/30 system, following standard published guidelines(Gutrecht, 1994). Silver electrodes were taped to thepalmar surface of the participant’s left hand II and IVfingers. The participants wore the electrodes for a fewminutes before the recording was initiated to achievesignal stabilization and individual calibration. Data wereregistered at 1-KHz sample-rate and processed with aMatlab (The Mathworks Inc.) custom program.
Tonic component of SCR has been computedaccording to (Lim et al., 1997). The average tonicvalues for each phase were then computed.
Data analysis
A visual inspection of the changes in facial thermalimprints in the subjects was performed to qualitativelyinvestigate their autonomic responses throughout theexperiment.
This visual analysis was followed by a quantitativeestimation of temperature variations in relevant facialregions of interest. Thermal facial imprints andvariations in cutaneous temperature of facial regionswere analyzed using custom-made Matlab programs(http://www.mathworks.com).
In order to quantify the thermal variations, changes incutaneous temperature for specific facial regions ofinterest were calculated. In particular we focused ouranalysis on the nose tip by choosing a circular region,
inscribed in the thermal nose profile, and notoverlapping with the nostrils (Fig. 2).
In order to correct for the displacement betweenlocations of the regions of interest in the successiveframes, we applied the motion correction and imageregistration procedure described by Ebisch et al. (2012).The procedure allows to properly re-align regions ofinterest by means of the automatic recognition andidentification of anatomical (nose and nostril profiles)and artificial landmarkers (Fig. 2).
Nose tip was selected according to previous studies inhumans and primates (Shastri et al., 2009; Nhan andChau, 2010; Kuraoka and Nakamura, 2011; Ebischet al., 2012; Manini et al., 2013). It has been shown thatthe nose tip temperature depends on the activation ofthe sympathetic nervous system in response toemotional or distressing stimuli and reflects sympatheticalpha-adrenergic vasomotor effects (Merla and Romani,2007; Nakanishi and Imai-Matsumura, 2008; Shastriet al., 2009; Nhan and Chau, 2010; Kuraoka andNakamura, 2011; Ebisch et al., 2012). Furthermore,sympathetic stimulation of the blood vessels can alsohave smaller vasodilatory effects via cholinergic andbeta-adrenergic receptor action (Smith and Kampine,1990).
In order to check for proper acclimatization ofsubjects, we assessed ‘‘at the intra-individual level’’whether the facial skin temperature did not varysignificantly or presented drifts during a 90-s periodimmediately preceding the experiment.
Then, we divided the whole time course of thetemperature signal into three segments, eachcorresponding to the experimental phases: (1) baseline(i.e., first four repetitions of the image series); (2)conditioning (i.e., second four repetitions of the imageseries with the sound paired with the fifth image); (3)maintenance (i.e., the last four repetitions of the imageseries with no sound paired to the images).
In order to identify the presence and timing for thenose tip temperature changes in response to thepresentation of the stimuli, we carried out multiplecomparison tests between the 10 s preceding and the
Fig. 2. Facial thermal changes in a representative subject. On the left: the average temperature before the acoustic stimulation (US); on the right:soon after the acoustic stimulation (US). A general temperature drop can be observed over the whole face, with the onset of sudomotor response ashighlighted by the dotted pattern of the temperature associated with the emotional sweating response. In particular, while the cheeks do not changetheir average temperature values and pattern, nose tip, perioral, maxillary and forehead regions clearly present a temperature decrease due to theappearance of colder dotted spots. The temperature decrease is particularly appreciable on the nose tip, where blue areas can be easily spotted.The circles over the face are paper markers put on to facilitate the tracking of the region of interest along the procedure. The black-contour circularregion on the nose tip is the region of interest from which the temperature data have been extracted.
A. Di Giacinto et al. / Neuroscience 266 (2014) 216–223 219
10 s following each stimulus delivery. Results fromthe ANOVA rejected the hypothesis of equality of themeans of the distributions. Dunnett’s t-test showed thatstimulus-related skin temperature variations occurredwithin the first 10 s. Therefore, for further analysis, wedecided to take into account 100 frames for eachexperimental phase (baseline, conditioning,maintaining), equally spaced in time. This procedureaccounted for the participants’ potential motion andvocalizations in the ecological experimental setting byexcluding frames affected by short-lasting motion orvocalization artifacts (Ebisch et al., 2012). Thus, a totalof 300 frames (data points) were obtained for eachparticipant for the analysis of the experimental phases.
In order to verify whether there was a significantmodulation of the physiological parameters during theexperimental phases and the baseline period in thenose tip, and whether PTSD and control groups differedin terms of SCR and fIR imaging variables during theexperimental phases, a 2-group (patients, controls) "3-phase (baseline, conditioning, maintenance) ANOVAwas conducted (level of significance a = 0.05). Thenormality of distribution was assessed by means ofKolmogorov–Smirnov test. Duncan’s post hoc test wasused to inspect the group " phase significant interactions.
Table 2 reports the SCR and fIR imaging variablesused for the data analysis.
RESULTS
Consistent with the study hypothesis, the conditioningphase induced a significant change of the physiologicalparameters with respect to the baseline condition (seeFig. 2 and Table 3).
We did not find any between-group effect in terms ofabsolute values of SCR and average temperature.Conversely, the two groups did differ when comparing
the variation across the phases of the physiologicalparameters.
When analyzing the variation of SCR, we found asignificant group " phase interaction [F(2, 38) = 13.3,p= 4.7 ! 10#5]: in PTSD patients the conditioning vs.baseline SCR variation (DSCRbc) and the maintenancevs. baseline SCR variation (DSCRbm) were significantlyhigher with respect to controls.
The same results were found when comparing thegroups in terms of temperature variations [F(2,38) = 5.7, p= 6.7 ! 10#3]: the PTSD patients showedhigher conditioning vs. baseline (Tbc) and maintenancevs. baseline (Tbm) variations with respect to controls.
These results suggest that the effects of conditioningwere larger and more persistent in PTSD. In agreementwith the study hypothesis, the observed variations inSCR and temperature parameters are opposite, as anincreased SCR signal corresponds to a diminished nosetip temperature (Shastri et al., 2009).
DISCUSSION
In the present pilot study, we used thermal imaging to testthe hypothesis that the psychophysiological response of agroup of mild PTSD patients differs from the healthycontrols one during a new variant of conditioningparadigm. We chose thermal imaging, because it hasbeen shown to be a robust and ecologically validmethod to monitor individual’s arousal through theeffects that the autonomic activity exerts on the facialcutaneous temperature (Shastri et al., 2009; Maniniet al., 2013). We examined fear processing in PTSDthrough the study of the fear-conditioning responseusing a sudden acoustic stimulus as the US. Thischoice derived by literature on the ASR (Norrholm et al.,2011), characterized by reflexive response andmodulated under specific conditions in Pavlovianconditioning tasks (Davis, 1997). In the present studythe ASR (i.e. EMG response) was not measured, sincedependent measures of psychophysiological reactionwere represented by skin conductance and fIR imagingresponse.
The main findings of the current study are: (a) achange of the physiological parameters with respect tothe baseline condition in both control subjects andPTSD patients during the conditioning phase; (b) thepermanence of the conditioning effect in themaintenance phase in both control and PTSD patients;(c) patients and controls did differ for the variationacross the phases of the physiological parametersrather than for their absolute values, showing that PTSDpatients had a prolonged excitation of greater effectrepresented by the tonic component, either estimatedthrough the Galvanic Skin Response (GSR) and thethermal signal.
Results showed that all participants displayedunlearned response to US (conditioning phase).Furthermore, higher levels of arousal were observed tothe CS previously paired to the US (maintenancephase) with respect to the response to the baselinephase, thus indicating successful fear conditioning.
Table 2. Physiological variables included in the analysis
Variable Definition
SCR Tonic component of the skin conductance response
SCRb SCR at baseline
SCRc SCR during the conditioning phase
SCRm SCR during the maintaining phase
DSCRbc Conditioning vs. baseline SCR variation:
(SCRc # SCRb)/SCRb
DSCRbm Maintaining vs. baseline SCR variation:
(SCRm # SCRb)/SCRb
DSCRcm Conditioning vs. maintaining SCR variation:
(SCRc # SCRm)/SCRm
Tb Average temperature at baseline
Tc Average temperature during the conditioning phase
Tm Average temperature during the conditioning phase
DTbc Conditioning vs. baseline temperature variation:
(Tc # Tb)/Tb
DTbm Maintaining vs. baseline temperature variation:
(Tm # Tb)/Tb
DTcm Conditioning vs. maintaining temperature variation:
(Tc # Tm)/Tm
220 A. Di Giacinto et al. / Neuroscience 266 (2014) 216–223
In agreement with the study hypothesis, the resultssuggest that the observed variations in SCR andtemperature parameters are opposite, as an increasedSCR signal corresponds to a diminished nose tiptemperature (Shastri et al., 2009). Also, PTSD patientspresented larger variation of the signals across thephases. It seems that mild PTSD patients maintain ahigher level of attention to external stimuli compared tocontrol subjects and, at the same time, they exhibitamplified response to conditioning stimuli. Indeed,patients showed lack of habituation with respect to theperiodic stimulation, showing a prolonged excitation ofgreater effect represented by the tonic component of theGSR.
From a physiological point of view, the most markedobserved effect is the reduced skin temperature in theconsidered regions of the face (in particular the nose),synchronous to the activation (increase) of the averagelevel of the signal associated with the tonic component.PTSD patients seem to have a higher level of stresscompared to controls, as indicated by the decrease ofthe skin temperature, that in the presence of US tendsto decrease of up to #2 "C. The temperature of thenose tip, and generally of the skin surface, is known topresent lowering, during the phases of stress, causedby the activation of the sympathetic nerves (Williamset al., 2006).
These findings suggest that PTSD patients have ahigher level of arousal, reflected in a higher averagevalue of the tonic component, express more markedtemperature reactions and that these do not depend onthe stimulus itself. The ANS response and the selectivityof the emotional response to the acoustic stimulus (US)is abnormal in PTSD patients with mild symptoms. Asdemonstrated by other studies (Norrholm et al., 2011)these results confirm that PTSD is associated withenhanced fear learning and a greater ‘‘fear load’’ toextinguish after conditioned fear learning. We found
that, in PTSD patients, although with mild symptoms,ASN ‘‘attack–escape’’ response and selectivity of theemotional response to neutral stimuli are abnormal. Thiswould represent a neural correlate of acute generalizedthreshold ‘‘alert’’, which is typically observed in PTSD(Criterions B5 and D5, DSM IV), which could representa strategy to alert the body to a dangerous environmentafter emotional trauma.
This work indicates that the analysis of the activationof the ANS, through the study of SCR signals and facialthermal response, during the conditioning paradigm is apromising psychometric method of investigation. Indeed,we found robust effect sizes despite: 1. the small studysample; 2. the white noise acoustic stimulus, and 3. thelow level of severity of symptoms in PTSD patients.
The use of thermal imaging is showing great potentialfor medical diagnostic purposes in monitoring a widevariety of diseases impacting the normalthermoregulatory processes (Ring and Ammer, 2012). Itcould also provide a useful approach for psychometricpurposes and for the clinical practice. For stimuli ofdifferent nature, thermal imaging can record anddemonstrate the activation of the sympathetic nervoussystem. Therefore, in neuropsychology and clinicalneuropsychology, it may help for monitoring eitherphysiological responses or impaired one’s expressingdisturbance, anxiety or all of those psychologicalconditions in which the monitoring of physiologicalresponses can be representative of disease orpathological conditions. Such potential depends on thecapability provided for monitoring the emotionalreactions of the subject in a passive and non-invasivemodality, even with the subject unaware of themonitoring, even though ethical considerations shouldbe opportunely considered in this perspective.
Although the exploratory nature of this study and theneed for a further validation of the results in a largestsample of PTSD patients, our results indicate that
Table 3. Two-group (controls, patients) " 3-phase (baseline, conditioning, maintaining) ANOVA. HC = healthy controls. P = patients
Variables Groups Statistics
HC P ANOVA 2-group " 3-phase interaction
Mean (SD) Mean (SD) F p Duncan post hoc test significant results
SCR 20.60 8.7 ! 10#7 P SCRb< P SCRc
SCR b 8.6 (5.8) 4.5 (3.9) P SCRb< P SCRm
SCR c 9.7 (5.8) 10.5 (5.8)
SCR m 9.9 (6.3) 10.7 (6.5)
DSCR 13.34 4.7 ! 10#5 P DSCRbc > P DSCRcm
DSCRbc 0.2 (0.3) 2.3 (1.8) P DSCRbm < P DSCRcm
DSCRbm 0.2 (0.3) 2.4 (2.2) P DSCRbc > HC DSCRbc
DSCRcm 0.01 (0.1) 0.02 (0.2) P DSCRbm > HC DSCRbm
T 12.6 6.2 ! 10#5 HC Tc < HC Tb; HC Tm < HC Tb
Tb 35.7 (0.9) 36.4 (0.5) HC Tc < HC Tm
Tc 34.8 (1.0) 34.6 (0.5) P Tc < P Tb; P Tm < P Tb
Tm 35.2 (1.2) 34.8 (0.3)
DT 5.7 6.7 ! 10#3 HC DTcm < HC DTbc; HC DTcm < HC DTbm
DTbc 0.02 (0.01) 0.05 (0.01) P DTcm < P DTbc; P DTcm < P DTbm
DTbm 0.01 (0.02) 0.04 (0.01) P DTbc > HC DTbc
DTcm 0.00 (0.02) 0.01 (0.01) P DTbm > HC DTbm
A. Di Giacinto et al. / Neuroscience 266 (2014) 216–223 221
thermal imaging and fear-conditioning paradigms couldprovide an additional, or complementary to the actualstandards, criterion of investigation in anxiety disorder.To the best of our knowledge, this study is the firstattempt to discriminate between control subjects andpatients with PTSD (even with mild symptoms) throughinfrared thermal imaging. It may suggest feasibleapproaches for diagnostic screening in the early phasesof the disease and in the assessment of preventivemeasures and therapies. Furthermore, this methodologycould be extended to individuals who present criticalsymptoms but do not meet criteria for PTSD diagnosis.The lack of a systematic profile based on possibleeffects and symptoms of reaction to trauma can lead thehealth staff to produce an incorrect evaluation. Indeed, itis unclear how to distinguish a real pathological profilewith respect to an acute reaction that has not become achronic impairment. Since DSM IV criteria are veryrestrictive, a set of clinical and vegetative criteria thatclearly delineate between full pathological conditionsand transitory or partial trauma reactions could beidentified. Thermal imaging could represent a diagnostictool, fast and usable in different contexts, that can beadministered in order to identify vegetative parametersin traumatized domain. Moreover, usable information fordelineating predictive factors for PTSD development inthe acute phase after trauma response could beprovided by means of thermal imaging.
REFERENCES
Amstadter AB, Nugent NR, Koenen KC (2009) Genetics of PTSD:fear conditioning as a model for future research. Psychiatr Ann39:358–367.
American Psychiatric Association: Diagnostic and statistical of mentaldisorders (2000) Fourth Edition-Text Revised (DSM IV-TR).Washington, DC: A.P.A.
Blake D, Weathers F, Nagy L, Kaloupek D, Klauminzer G, Charney D,Keane T (1990) A clinician rating scale for assessing current andlifetime PTSD: the CAPS-I. Behav Therapist 18:187.
Blake D, Weathers F, Nagy L, Kaloupek D, Charney D, Keane T(1998) Clinician Administered PTSD Scale (CAPS). Boston,VA: National Center for Post-Traumatic Stress Disorder,Behavioral Science Division.
Brooks DC, Bouton ME (1993) A retrieval cue for extinctionattenuates spontaneous recovery. J Exp Psychol Anim BehavProcess 19(1):77–89.
Brunetti M, Sepede G, Mingoia G, Catani C, Ferretti A, Merla A, DelGratta C, Romani GL, Babiloni C (2010) Elevated response ofhuman amygdala to neutral stimuli in mild post traumatic stressdisorder: neural correlates of generalized emotional response.Neuroscience 168(3):670–679.
Burgos-Robles A, Vidal-Gonzalez I, Santini E, Quirk GJ (2007)Consolidation of fear extinction requires NMDA receptor-dependent bursting in the ventromedial prefrontal cortex.Neuron 53(6):871–880.
Conti L, Rossi A, Donda P (1999). In: MINI 5.0 Italian version:‘‘Repertorio delle scale di Valutazione in Psichiatria’’ (Conti L.,ed), pp. 153, 174. SEE Firenze.
Cuthbert BN, Lang PJ, Strauss C, Drobes D, Patrick CJ, Bradley MM(2003) The psychophysiology of anxiety disorder: fear memoryimagery. Psychophysiology 40(3):407–422.
Damasio AR (1995) Descartes’ error: emotion, reason, and thehuman brain. London: Picador.
Davis M (1997) The neurophysiological basis of acoustic startlemodulation: research on fear motivation and sensory gating [p.69–96]. In: Lang PJ, Simons RF, Balaban MT, editors. Attentionand orienting: sensory and motivational processes. Mahwah, NewJersey: Lawrence Erlbaum Associates.
Ebisch SJ, Aureli T, Bafunno D, Cardone D, Romani GL, Merla A(2012) Mother and child in synchrony: thermal facial imprints ofautonomic contagion. Biol Psychol 89(1):123–129.
Ehlers A, Clark DM (2000) A cognitive model of posttraumatic stressdisorder. Behav Res Ther 38:319–345.
Ekman P, Levenson RW, Friesen WV (1983) Autonomic nervoussystem activity distinguishes among emotions. Science221(4616):1208–1210.
Fendt M, Fanselow MS (1999) The neuroanatomical andneurochemical basis of conditioned fear. Neurosci BiobehavRev 23(5):743–760.
Foa EB, Zinbarg R, Rothbaum BO (1992) Uncontrollability andunpredictability in post-traumatic stress disorder: an animalmodel. Psychol Bull 112(2):218–238.
Friedman M (2006) Post-traumatic and acute stress disorders: thelatest assessment and treatment strategies. 4th ed. Kansas City,Missouri: Dean Psych Press Corporation.
Glascher J, Adolphs R (2003) Processing of the arousal of subliminaland supraliminal emotional stimuli by the human amygdala. JNeurosci 23(32):10274–10282.
Glover EM, Phifer JE, Crain DF, Norrholm SD, Davis M, Bradley B,Ressler KJ, Jovanovic T (2011) Tools for translationalneuroscience: PTSD is associated with heightened fearresponses using acoustic startle but not skin conductancemeasures. Depress Anxiety 28(12):1058–1066.
Gutrecht JA (1994) Sympathetic skin response. J Clin Neurophysiol11(5):519–524.
Harding JR (2007) Raynaud’s phenomenon: cold hands = warmheart, but what about cold noses. Thermol Int 17(4):157.
Hettema JM, Annas P, Neale MC, Kendler KS, Fredrikson M (2003) Atwin study of the genetics of fear conditioning. Arch GenPsychiatry 60(7):702–708.
Hoffman KL, Gothard KM, Schmid MC, Logothetis NK (2007) Facial-expression and gaze-selective responses in the monkeyamygdala. Curr Biol 17:766–772.
Kuraoka K, Nakamura K (2011) The use of nasal skin temperaturemeasurements in studying emotion in macaque monkeys. PhysiolBehav 102(3–4):347–355.
Lanius RA, Bluhm R, Lanius U, Pain C (2006) A review ofneuroimaging studies in PTSD: heterogeneity of response tosymptom provocation. J Psychiatr Res 40(8):709–729.
LeDoux JE (1996) Emotional networks and motor control: a fearfulview. Prog Brain Res 107:437–446.
LeDoux JE (1998) Cognition and emotion: listen to the brain. In: LaneR, editor. Emotion and cognitive neuroscience. New York: OxfordU. Press.
LeDoux JE (2000) Emotion circuits in the brain. Annu Rev Neurosci23:155–184.
Liberzon I, Taylor SF, Fig LM, Decker LR, Koeppe RA, Minoshima S(2000) Limbic activation and psychophysiologic responses toaversive visual stimuli. Interaction with cognitive task.Neuropsychopharmacology 23:508–516.
Lim CL, Rennie C, Barry RJ, Bahramali H, Lazzaro I, Manor B,Gordon E (1997) Decomposing skin conductance into tonic andphasic components. Int J Psychophysiol 25(2):97–109.
Manini B, Cardone D, Ebisch SJ, Bafunno D, Aureli T, Merla A (2013)Mom feels what her child feels: thermal signatures of vicariousautonomic response while watching children in a stressfulsituation. Front Hum Neurosci 25(7):299.
Maren S, Quirk GJ (2004) Neuronal signalling of fear memory. NatRev Neurosci 5(11):844–852.
Merla A, Romani GL (2007) Thermal signatures of emotional arousal:a functional infrared imaging study. Conf Proc IEEE Eng Med BiolSoc 2007:247–249.
222 A. Di Giacinto et al. / Neuroscience 266 (2014) 216–223
Nakanishi R, Imai-Matsumura K (2008) Facial skin temperaturedecreases in infants with joyful expression. Infant Behav Dev31(1):137–144.
Nhan BR, Chau T (2010) Classifying affective states using thermalinfrared imaging of the human face. IEEE Trans Biomed Eng57(4):979–987.
Norrholm SD, Jovanovic T, Olin IW, Sands LA, Karapanou I, BradleyB, Ressler KJ (2011) Fear extinction in traumatized civilians withposttraumatic stress disorder: relation to symptom severity. BiolPsychiatry 69(6):556–563.
Orr SP, Metzger LJ, Lasko NB, Macklin ML, Peri T, Pitman RK (2000)De novo conditioning in trauma-exposed individuals with andwithout posttraumatic stress disorder. J Abnorm Psychol109:290–298.
Peri T, Ben-Shakhar G, Orr SP, Shalev AY (2000) Psychophysiologicassessment of aversive conditioning in posttraumatic stressdisorder. Biol Psychiatry 47:512–519.
Pieraccini F, Bossini L, Lombardelli A, Dell’Erba A, Pappagallo E,Mantovani A, Castrogiovanni P (1999). In: CAPS Italian version:‘‘Repertorio delle scale di Valutazione in Psichiatria’’ (Conti L.,ed), pp:1253, 1272. SEE Firenze.
Pitman RK, Orr SP, Forgue DF, de Jong JB, Claiborn JM (1987)Psychophysiologic assessment of posttraumatic stress disorderimagery in Vietnam combat veterans. Arch Gen Psychiatry44:970–975.
Pole N (2007) The psychophysiology of posttraumatic stressdisorder: a meta-analysis. Psychol Bull 133(5):725–746.
Quirk GJ, Garcia R, Gonzalez-Lima F (2006) Prefrontal mechanismsin extinction of conditioned fear. Biol Psychiatry 60:337–343.
Quirk GJ, Mueller D (2008) Neural mechanisms of extinction learningand retrieval. Neuropsychopharmacology 33:56–72.
Rasmusson AM, Charney DS (1997) Animal models of relevance toPTSD. Ann N Y Acad Sci 21(821):332–351.
Ring EF, Ammer K (2012) Infrared thermal imaging in medicine.Physiol Meas 33(3):R33–R46.
Shastri D, Merla A, Tsiamyrtzis P, Pavlidis I (2009) Imaging facialsigns of neurophysiological responses. IEEE Trans Biomed Eng56:477–484.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, WeillerE, Hergueta T, Baker R, Dunbar GC (1994) The Mini InternationalNeuropsychiatric Interview (M.I.N.I.): the development andvalidation of a structured diagnostic psychiatric interview forDSM-IV and ICD-10. University of South Florida Institute forResearch in Psychiatry, Tampa, Florida and INSERM – Hopital dela Salpetriere, Paris, France.
Sherin JE, Nemeroff CB (2011) Post-traumatic stress disorder: theneurobiological impact of psychological trauma. Dialogues ClinNeurosci 13(3):263–278.
Smith JJ, Kampine JT (1990) Circulatory physiology, the essentials.3rd ed. Baltimore, MD: Williams and Wilkins.
Van der Kolk BA (2003) The neurobiology of childhood trauma andabuse. Child Adolesc Psychiatr Clin N Am 12(2):293–317.
Williams LM, Phillips ML, Brammer MJ, Skerrett D, Lagopoulos J,Rennie C, Bahramali H, Olivieri G, David AS, Peduto A, Gordon E(2001) Arousal dissociates amygdala and hippocampal fearresponses: evidence from simultaneous fMRI and skinconductance recording. Neuroimage 14(5):1070–1079.
Williams LM, Kemp AH, Felmingham K, Barton M, Olivieri G, PedutoA, Gordon E, Bryant RA (2006) Trauma modulates amygdala andmedial prefrontal responses to consciously attended fear.Neuroimage 29(2):347–357.
(Accepted 6 February 2014)(Available online 20 February 2014)
A. Di Giacinto et al. / Neuroscience 266 (2014) 216–223 223