Effects of Adipose Tissue-Derived Stem Cell Therapy After Myocardial Infarction: Impact of the Route...
-
Upload
unescfaculdade -
Category
Documents
-
view
1 -
download
0
Transcript of Effects of Adipose Tissue-Derived Stem Cell Therapy After Myocardial Infarction: Impact of the Route...
Journal of Cardiac Failure Vol. 16 No. 4 2010
Effects of Adipose Tissue-Derived Stem Cell Therapy AfterMyocardial Infarction: Impact of the Route of Administration
MONTSERRAT RIGOL, MVD, PhD,1,7 NURIA SOLANES, MVD, PhD,*,1 JORDI FARRE, PhD,2 SANTIAGO ROURA, PhD,2
MERCE ROQUE, MD, PhD,1 ANTONIO BERRUEZO, MD, PhD,1 NEUS BELLERA, MD,3 LAURA NOVENSA, MVD,1
DAVID TAMBORERO, BENG, PhD,1 CRISTINA PRAT-VIDAL, PhD,2 MA ANGELES HUZMAN, MVD,1 MONTSERRAT BATLLE,PhD,1 MARGO HOEFSLOOT, MD,4 MARTA SITGES, MD, PhD,1 JOSE RAMIREZ, MD, PhD,5 ANA PAULA DANTAS, PhD,1
ANNA MERINO, MD, PhD,5 GINES SANZ, MD, PhD,6 JOSEP BRUGADA, MD, PhD,1 ANTONI BAYES-GENIS, MD, PhD,2
AND MAGDA HERAS, MD, PhD1
Barcelona, Spain; Amsterdam, the Netherlands; Madrid, Spain; Mallorca, Spain
From the 1Instiques Agustı Pi Sugram, CardiologyBarcelona, Spain;celona, Spain; 4Acsterdam, the NetClınic, Barcelona,culares, Madrid,(CIBERES), Mallo
Manuscript recNovember 26, 200
Reprint requestTorax, Hospital CSpain. Tel: 34-93-
ub.es
ABSTRACT
Background: Cell-based therapies offer a promising approach to reducing the short-term mortality rateassociated with heart failure after a myocardial infarction. The aim of the study was to analyze histologicaland functional effects of adipose tissue-derived stem cells (ADSCs) after myocardial infarction and com-pare 2 types of administration pathways.Methods and Results: ADSCs from 28 pigs were labeled by transfection. Animals that survived myocar-dial infarction (n 5 19) received: intracoronary culture media (n 5 4); intracoronary ADSCs (n 5 5);transendocardial culture media (n 5 4); or transendocardial ADSCs (n 5 6). At 3 weeks’ follow-up, intra-coronary and transendocardial administration of ADSCs resulted in similar rates of engrafted cells (0.85[0.19-1.97] versus 2 [1-2] labeled cells/cm2, respectively; P 5 NS) and some of those cells expressedsmooth muscle cell markers. The intracoronary administration of ADSCs was more effective in increasingthe number of small vessels than transendocardial administration (223 6 40 versus 168 6 35 vessels/mm2;P ! .05). Ejection fraction was not modified by stem cell therapy.Conclusions: This is the first study to compare intracoronary and transendocardial administration ofautologous ADSCs in a porcine model of myocardial infarction. Both pathways of ADSCs delivery arefeasible, producing a similar number of engrafted and differentiated cells, although intracoronary admin-istration was more effective in increasing neovascularization. (J Cardiac Fail 2010;16:357e366)Key Words: Experimental study, intracoronary, transendocardial, neovascularization.
Stem cell therapy offers a promising approach to reduceshort-term mortality associated with heart failure after amyocardial infarction. Several stem cell types have beenidentified as suitable for regenerative cell therapy and
tut Clınic del Torax, Institut d’Investigacions Biomedi-nyer, Hospital Clınic, Barcelona, Spain; 2ICREC Pro-Service, Hospital de la Santa Creu i Sant Pau, ICCC,3Servei de Cardiologia, Hospital de Vall d’Hebron, Bar-ademic Medical Center, University of Amsterdam, Am-
herlands; 5Centre de Diagnostic Biomedic, HospitalSpain; 6Centro Nacional de Investigaciones Cardiovas-Spain; and 7Ciber de Enfermedades Respiratorias
rca, Spain.eived September 3, 2009; revised manuscript received9; revised manuscript accepted December 9, 2009.
s: Montserrat Rigol, MVD, PhD, Institut de Clınic dellınic de Barcelona, Villarroel, 170, 08036 Barcelona,2279305; Fax: 34-93-4514148. E-mail: mrigol@clinic.
357
evaluated in animals and humans.1e3 One of the typesmost often used for cell therapy is mesenchymal stem cellsisolated from bone marrow, given their capacity to prolifer-ate, migrate, differentiate into several cell types, and
Supported by grants from Fondo de Investigacion Sanitaria [PI060110];Sociedad Espanola de Cardiologıa [2006]; Societat Catalana de Cardiolo-gia [2006]; Hipertension Esencial: Red de Analisis de Canales ionicos dela musculatura Lisa arterial y su Explotacion terapeutica Sistematica[HERACLES, RD06/0009/0008]; Ciber de Enfermedades Respiratorias[06/06/0028], Red tematica de investigacion cooperativa de la salud[RD06/0003/0008], Fundacio Marato TV3 (2007, Malaltires Cardiovascu-lar) and SAF2008-05114-C02-01
* Both authors contributed equally to this study.1071-9164/$ - see front matter� 2010 Elsevier Inc. All rights reserved.doi:10.1016/j.cardfail.2009.12.006
358 Journal of Cardiac Failure Vol. 16 No. 4 April 2010
maintain their differentiation properties despite aging.4 Re-cently, the adipose tissue has been shown to be a good al-ternative for obtaining multipotent cells, called adiposetissue-derived stem cells (ADSCs),5 because a larger num-ber of cells can be easily harvested using standard fat ex-traction techniques and the ADSCs proliferate morerapidly in vitro compared with bone marrow cells. More-over, it has been demonstrated in small animal modelsthat ADSCs enhance neovascularization and have the po-tential to differentiate into endothelial and cardiomyocytephenotypes.6,7
The objective of cardiac cell therapy is to deliver the ad-equate number of cells and to achieve a high number ofimplanted cells in the affected myocardium. The main ad-ministration routes are intravenous, intracoronary, and in-tramyocardial. Peripheral venous infusion is the simplesttechnique;8 however, the more complex intracoronary andintramyocardial administration routes can direct cells intocoronary circulation or target myocardium. Several recentexperimental and clinical studies have established the useof intracoronary and intramyocardial pathways to deliverstem cells as feasible and safe.9,10 However, very few stud-ies have compared various routes of administration in thesame experimental model11,12 and to our knowledge nostudies specifically compare intracoronary and intramyo-cardial administration of ADSCs in large animals or hu-mans.
Therefore, the aim of the present research was to analyzethe histological and functional effects of ADSCs in a por-cine model of myocardial infarction and determine whetherthe administration route affected outcomes.
Methods
Experimental Animals
The study protocol was approved by our Institutional ReviewBoard and Ethics Committee. The conditions for the 28 femaleLandrace x Large White pigs (30 6 3 kg) used in this study con-form to the ‘‘Guiding Principles in the Use and Care of Animals’’published by the National Institutes of Health (NIH PublicationNo. 85-23, revised 1996).
Experimental Design
The 19 animals surviving initial induced myocardial infarctionwere distributed into 4 treatment groups, according to the admin-istration of culture medium or ADSCs: 1) intracoronary culturemedium without cells (icCM, n 5 4); 2) intracoronary ADSCs(icADSCs, n 5 5); 3) transendocardial culture medium withoutcells (teCM, n 5 4); and 4) transendocardial ADSCs (teADSCs,n 5 6), and followed for 3 weeks after ADSCs or culture mediumadministration.
Subcutaneous Adipose Tissue Collection and CellCulture
All animals were anaesthetized as previously described.13 Sub-cutaneous adipose tissue was excised through an incision in theneck area and kept at 4 �C in culture medium supplementedwith antibiotics (penicillin-streptomycin).
Tissue specimens were rinsed with phosphate-buffered salinebuffer, minced, and processed as described.14 Adhered cellswere maintained in a-MEM supplemented with 10% fetal bovineserum and 1% penicillin-streptomycin (Invitrogen, Carlsbad, CA)under standard culture conditions. Third-passage cells were usedto analyze expression of mesenchymal lineage markers, b-Galac-tosidase (b-Gal) labeling, and in vivo administration.
Characterization of ADSCs
Cells were immunostained as previously described15 using spe-cific monoclonal antibodies: CD90 (BD Pharmingen, Palo Alto,CA), CD45, and CD14 (AbD serotec, Oxford, UK), and conju-gated with fluorescein isothiocyanate or phycoerythrine. Flow cy-tometry levels of each antigen were expressed as a percentage ofpositive cells normalized with respect to each immunoglobulin Gisotype control (AbD serotec). A Coulter EPICS XL flow cytom-eter (Beckman Coulter, Fullerton, CA) was used for data acquisi-tion; analysis was carried out using Expo32 software (BeckmanCoulter).
Cell labelling
Three days before in vivo administration, some of the culturedADSCs (2 � 106 cells) were transfected with a construct carryingthe Escherichia coli lacZ gene encoding b-Gal by nonviral Nucle-ofector technology (Lonza Cologne AG, Cologne, Germany) ac-cording to the manufacturer’s instructions.
Two days after transfection, labeled and unlabeled cells weretrypsinized and counted; cell viability was evaluated by trypanblue exclusion method and a hemocytometer (only viabilitiesgreater than 90% were accepted for cell injection). After that, cellswere resuspended in DMEM until injection.
Infarct Procedure
An intracardiac echocardiogram (AcuNav Catheter, BiosenseWebster Inc, Diamond Bar, CA) was performed and from offlineanalysis we measured end diastolic (LVEDV) and systolic(LVESV) volumes and left ventricular ejection fraction (LVEF)by the Simpson method. Myocardial infarction was then inducedby placing an angioplasty catheter into the middle segment ofthe left anterior descending (LAD) artery and inflating it for 90minutes, followed by reperfusion.16 During the procedure, antico-agulant doses of unfractionated heparin are given intravenously3000 U as a bolus at the beginning of the infarction induction fol-lowed by 1000 U/h until the end of the surgery. Aspirin 500 mg isgiven on a daily from day 1 to sacrifice.
Intracoronary or Transendocardial Administration ofAutologous Adipose Tissue-derived Stem Cells
One week after myocardial infarction, LVEDV, LVESV, andLVEF were again measured by echocardiogram and culture me-dium or ADSCs were administered by intracoronary or transendo-cardial means.
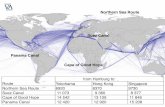
For intracoronary administration, a balloon catheter was placedinto the proximal segment of the LAD, inflated for 2 minutes toinfuse 2 mL of culture medium or ADSC suspension (Fig. 1A),then deflated; myocardium was perfused for 2 minutes. This cyclewas completed 7 times to deliver 14 mL of culture medium orADSC solution (total 16 6 11 million ADSCs). LAD patency af-ter intracoronary administration was assessed by angiography.
Transendocardial administration was guided by an electroana-tomical mapping system (Carto, Biosense Webster Inc, Diamond
Fig. 1. Intracoronary and transendocardial administration of adipose tissue-derived stem cells. (A) Angiography shows a catheter ballooninflated into the proximal segment of the left anterior descending artery to infuse culture media or adipose tissue-derived stem cell suspen-sion. (B) Right anterior oblique projection of 3-dimensional Carto voltage map of the left ventricle to identify areas of infarcted (gradedcolors, bipolar voltage #1.5 mV) and normal (purple, bipolar voltage O1.5 mV) myocardium. (C) Representative histological sectionshows the presence of ink in the myocardium after its transendocardial injection by Myocath catheter. Hematoxylin and eosin stain. Orig-inal magnification: 10�.
Adipose Tissue-Derived Stem Cell Therapy � Rigol et al 359
Bar, CA). Three-dimensional geometry and a voltage map of theleft ventricle were constructed using a 3.5-mm tip catheter (Navis-tar, Biosense Webster Inc) to identify infarct (voltage !0.5 mV)and normal myocardium (voltage O1.5 mV), and carefully defineborder zones (voltage between 0.5 and 1.5 mV) (Fig. 1B). Admin-istration of culture medium or ADSCs (23 6 8 million) in the in-farct and border zones was achieved by 14 injections of 0.5 mLeach (Myocath catheter, Bioheart, Florida, FL). Adequacy ofthis method was tested by injecting ink through the Myocath cath-eter into the left ventricle of one additional pig; the histologicalstudy showed ink in the targeted regions (Fig. 1C).
No significant differences existed between icADSC andteADSC groups in the number of total administered cells.
Follow-up and Harvesting of Specimens for HistologicalAnalysis
At 3 weeks, animals were returned for cardiac catheterizationand echocardiography and then euthanized. The hearts wereimmediately excised and prepared for histological analysis. Eachharvested heart was cut into 7 to 8 transversal slices (9 mm thick)from the apex to the base (Fig. 2). Each transversal slice was cutinto 4 sections: free wall, anterior wall, posterior wall, and septum;the apex was cut in half. Representative samples of kidney, lung,intestine, spleen, and liver were obtained to determine the pres-ence of b-Gal positive cells. For each animal, 30 to 34 sectionsfrom heart and 5 sections from studied organs were fixed by im-mersion in 10% buffered formalin and embedded in paraffin.
Infarct Size
Infarcted and noninfarcted myocardium areas were delineatedand calculated in each transversal slice using morphometric anal-ysis software (AnalySIS, Olympus Optical, Hamburg, Germany).The percentage of left ventricle infarction was calculated as: [in-farct area/(infarct area þ noninfarcted myocardium area)] � 100.
Determination of Cellular Engraftment
For each animal, 5-mm-thick histological sections (30 to 34from heart and 5 from studied organs) were layered in poly-L-lysineecoated glass slides for b-Gal staining (Roche Diagnostics
SL, Sant Cugat del Valles, Barcelona, Spain) counterstainedwith eosin. ADSCs grafted in the myocardium and in the studiedorgans were visible by the blue color resulting from b-Gal enzymeexpression. The histological sections were carefully examined andthe total number of b-Galepositive cells was expressed as countsper cm2. The number of engrafted cells was evaluated by 2 inde-pendent investigators blinded to the treatment administered (87%agreement).
Determination of Cellular Phenotype
Double fluorescent immunohistochemistry was performed usingmouse monoclonal antieb-Gal antibody (1:100 dilution) (Abcamplc, Cambridge, UK) and rabbit polyclonal anti-Troponin I (TnI)antibody (1:200 dilution) (Santa Cruz Biotechnology Inc, SantaCruz, CA) or rabbit polyclonal anti-alpha smooth muscle actin(SMA) antibody (1:100 dilution) (Abcam plc). Double-positivecells (b-Gal and SMA; b-Gal and TnI) were evaluated with confo-cal microscopy (Leica Microsystems GmbH, Wetzlar, Germany)by 2 investigators blinded to the treatment administered.
Vascular Density
The density and size of blood vessels were evaluated in 5 histo-logical sections per animal from the infarct border zone. Doubleimmunohistochemistry was performed using mouse monoclonalanti-SMA antibody (1:100 dilution) and rabbit polyclonal anti-von Willebrand factor antibody (undiluted) (both from DakoDenmark, Glostrup, Denmark). Five areas of each slide were pho-tographed under light microscopy at �200 magnification, andblindly analyzed (AnalySIS, Olympus Optical, Hamburg,Germany).
Vessels were defined as small (15 mm or less in diameter) orlarge (O15 mm). The number of small, large and total (small þlarge) vessels was expressed as counts per mm2.
Statistical Analysis
Quantitative variables are presented as mean 6 SD values ormedian (quartiles 1 through 3) when criteria for normal distribu-tion of data were not met. Student’s unpaired t-test was usedto compare quantitative variables between 2 groups and
Fig. 2. Representative images showing macroscopic characteristics of myocardial infarction. On the left, dotted line shows myocardialinfarct location. On the right, transversal slice sections of the left ventricle show transmural infarction involving septal and anterolateralwalls (pale areas). L, the free wall; A, the anterior wall; P, the posterior wall; T, the septum.
360 Journal of Cardiac Failure Vol. 16 No. 4 April 2010
Mann-Whitney U test when data were not normally distributed.Analysis of variance and Bonferroni post-hoc procedures wereused to compare quantitative variables between the 4 study groupsand Kruscal-Wallis and Mann-Whitney U tests when criteria fornormal distribution of data were not met. A P value !.05 wasconsidered significant. Calculations were performed using theSPSS/PC statistical package.
Results
During the induction of myocardial infarction in 28 ani-mals, 9 animals experienced ventricular fibrillation that didnot respond to external defibrillation (32% mortality). The19 survivors had no adverse events during intracoronaryor transendocardial administration of ADSCs. AfterADSC administration and at 3 weeks’ follow-up, all ani-mals had normal coronary angiograms.
Characteristics of ADSCs
A few fibroblast-like cells appeared attached and formeda complete monolayer 7 days after establishment of pri-mary cell cultures (Fig. 3A). At passage 3, primary culturesof ADSCs were homogeneously positive for CD90 (98.2 ±0.2%) and negative for CD45 (0.2 ± 0.2%) and CD14 (0.6 ±0.2%), averaging 57 ± 6% b-Gal positive cells after admin-istration (Fig. 3B).
Infarct Size
Macroscopic infarcts were observed in all hearts. AllLADs were patent until sacrifice. Left ventricle infarctionwas 19 ± 10%, 24 ± 1%, 22 ± 12%, and 20 ± 10% foricCM, icADSCs, teCM, and teADSCs groups, respectively,without differences between groups.
ADSCs Engraftment and Phenotype afterAdministration
At 3 weeks, histological staining by b-Gal showedADSCs in left ventricular myocardium in the icADSCand teADSC groups (Figs. 3C and 3D, respectively). En-grafted ADSCs were localized (80 6 16% and 79 6 32%for icADSC and teADSC groups, respectively) in theborder zone of the infarction and close to vessels. Therewere no significant differences between icADSC andteADSC groups in the number of engrafted cells (0.85[0.19-1.97] versus 2 [1-2] labeled cells/cm2, respectively;P 5 NS). No engrafted ADSCs were found in kidney,lung, intestine, spleen, and liver samples.
Confocal microscopy demonstrated specific colocaliza-tion of b-Galepositive cells with stain for SMA in theicADSC and teADSC groups, showing the smooth musclephenotype of ADSC positive cells (Figs. 4A and 4C).
Fig. 3. Representative images showing adipose tissue-derived stem cells (ADSCs) in culture before (A) and after b-Gal staining (B). (C, D)Histological sections stained by b-Gal and counterstained with eosin show ADSCs expressing b-Gal (blue) engrafted in the border zone ofthe infarcted myocardium after intracoronary (C) and transendocardial (D) administration. Original magnification of 200� on the left and400� zoom on the right.
Adipose Tissue-Derived Stem Cell Therapy � Rigol et al 361
However, no colocalization of b-Gal positive cells withstain for TnI could be found (Figs. 4B and 4D).
Vascular Density
The total vessel count using histochemical staining forvon Willebrand factor and SMA was significantly greaterin icADSC than in icCM and teADSC groups. The highestnumber of small vessels was observed in the icADSCgroup. No significant differences existed between teADSCand teCM groups in the number of total and small vessels;large vessels count was similar in all study groups (Table 1,Fig. 5).
LV Function
Baseline LVEDV, LVESV and LVEF are shown inTable 2. There were no significant differences between
groups (analysis of variance, P 5 NS). Myocardial infarc-tion significantly increased LVESV and, as a consequence,reduced LVEF at 1 week; amount of infarcted myocardiumwas similar for all groups. At 3 weeks, there was no signif-icant change in LVEDV, LVESV, and LVEF in any groupand no significant differences between groups (Table 2).
Discussion
This is the first study to compare intracoronary and trans-endocardial administration of autologous ADSCs in a por-cine model of myocardial infarction. Our results showthat both pathways are feasible, with a similar number ofengrafted and differentiated ADSCs at 3 weeks follow-up,although intracoronary administration of ADSCs moreeffectively increased the number of newly formed vessels.
Fig. 4. Confocal microscopy images of double fluorescent immunohistochemistry with antibodies against b-Gal and alpha smooth muscleactin (SMA) (A, C) or Troponin I (TnI) (B, D), obtained from the border zone of the infarcted myocardial. Arrows indicate colocalization ofb-Galepositive cells with stain for SMA (A, C). However, there is no colocalization of b-Galepositive cells and TnI (B, D). DAPI, stainingfor nuclei; merge, merged image.
362 Journal of Cardiac Failure Vol. 16 No. 4 April 2010
This is a relevant finding because it may positively affectlong-term prognosis.
Engraftment, Differentiation, and Neovascularization
Experience with ADSCs is scarce in large animals buthas been reported in small animal models of myocardialinfarction.6,17e19 The only previous study conducted ina porcine model of acute myocardial infarction also demon-strated, as we observed, that intracoronary administration ofADSCs significantly increased small vessels in the infarct
border zone.20 Interestingly, we have demonstrate, for thefirst time, better vascular density after intracoronary thantransendocardial administration of ADSCs. However, bothadministration routes resulted in a similar low number ofengrafted cells, distributed principally in the infarct borderzone. As in previous studies,18,20 our histological analysisconfirmed that some of those engrafted cells expressedsmooth muscle cell markers and were incorporated intothe blood vessel wall. Although engraftment and differenti-ation of ADSCs were similar for intracoronary and transen-docardial administration, that intracoronary infusion
Table 1. Vascular Density in the Infarct Border Zone at 3Weeks after ADSC Delivery, Expressed as Vessels per mm2
IntracoronaryAdministration
TransendocardialAdministration
CultureMedium(Control)
n 5 4ADSCsn 5 5
CultureMedium(Control)
n 5 4ADSCsn 5 6
Small vessels 141 6 26 223 6 40* 162 6 37 168 6 35Large vessels 31 6 4 38 6 11 32 6 14 34 6 5Total number
of vessels172 6 25 261 6 40* 194 6 24 201 6 34
ADSC, adipose tissue-derived stem cells.Results presented as mean 6 SD.*P ! .05 vs. intracoronary administration of culture medium and trans-
endocardial administration of ADSCs.
Adipose Tissue-Derived Stem Cell Therapy � Rigol et al 363
produced more neovascularization suggests that injectingcells into the coronary circulation and leaving them to actfreely has a more beneficial effect than directly injectingthem into the affected area. One could speculate that thismay be partially the result of a paracrine action, as sup-ported by different experimental reports,19,21,22 which coulddiffer by administration pathway. However, the design ofour study precludes evaluation of this possibility. Indeed,further large animal studies should investigate whether in-tracoronary administration of ADSCs induces a differentparacrine action than the transendocardial route, and
Fig. 5. Microphotographs representing the comparative results of vascunary administration of culture media. (B) Intracoronary administration oadministration of culture media. (D) Transendocardial administration ointracoronary administration of ADSCs. Original magnification: 100�.
whether this is related to neovascularization after myocar-dial infarction.
We did not observe transdifferentiation of engraftedADSCs into cardiomyocytes after intracoronary or transen-docardial administration. Although previous studies usingother types of stem cells have found engrafted cells that ex-pressed cardiomyocyte markers,22e24 our results are consis-tent with the findings of Valina et al20 in a similar animalmodel. Similarly, studies in small animal models foundno cardiac myocyte differentiation of engrafted cells.19,21
Schuleri et al.25 in a porcine model of myocardial infarc-tion, reached similar conclusions and suggested that in-creased neovascularization and tissue perfusion afterintramyocardial administration of bone marrow mesenchy-mal stem cells could occur before significant cardiomyo-genesis.
Routes of Administration
To our knowledge, no other studies have compared dif-ferent types of ADSC delivery in large animal models orhumans. Although different methods of stem cell adminis-tration have been compared in swine models of myocardialinfarction, these studies focused on other stem cellstypes.11,12,26 Freyman et al11 evaluated 3 methods of stemcell delivery after myocardial infarction, including intra-coronary and endocardial pathways using allogeneic bonemarrow mesenchymal stem cells rather than ADSCs.They found intracoronary injection to be most efficient in
lar density in the infarct border zone for all groups. (A) Intracoro-f adipose tissue-derived stem cells (ADSCs). (C) Transendocardialf ADSCs. The number of newly formed vessels was higher after
Table 2. Left Ventricular Volumes and Ejection Fraction Measured by Intracardiac Echocardiography
Intracoronary Administration Transendocardial Administration
Culture Medium(Control)
n 5 4ADSCsn 5 5
Culture Medium(Control)
n 5 4ADSCsn 5 6
BaselineLVEF (%) 78 6 3 79 6 2 84 6 3 80 6 4LVEDV (mL) 31.9 6 4.4 30.7 6 4.2 39.8 6 6.5 34.7 6 4.6LVESV (mL) 6.9 6 1.6 6.5 6 1.5 6.1 6 0.7 6.9 6 1.6
1 week after infarct inductionLVEF (%) 45 6 1* 48 6 2* 50 6 5* 51 6 6*LVEDV (mL) 29.3 6 0.6 28.3 6 3.0 32.4 6 4.0 37.2 6 7.7LVESV (mL) 16.0 6 0.2* 14.6 6 1.6* 16.0 6 0.2* 19.6 6 6.8*
3 weeks after administrationLVEF (%) 49 6 2* 49 6 10* 51 6 8* 51 6 12*LVEDV (mL) 27.3 6 3.9 32.0 6 4.8 34.1 6 5.9 38.4 6 13.9LVESV (mL) 13.8 6 1.3* 16.2 6 2.7* 16.6 6 3.2* 17.7 6 2.9*
Results presented as mean 6 SD.*P ! .05 vs. baseline.
364 Journal of Cardiac Failure Vol. 16 No. 4 April 2010
terms of engraftment but also associated with a higher inci-dence of decreased coronary blood flow. Our study did notobserve this no-reflow phenomenon, but 5 times fewer cellswere administrated. Similar to our study and that of Frey-man et al, Gavira et al26 found that the transendocardialroute was safe and well tolerated in their comparison ofthe efficacy of surgical and percutaneous administrationof autologous skeletal myoblast in a chronic myocardial in-farction model. However, in a rat model of chronicinfarction, Fukushima et al27 recently reported that intra-myocardial injection of bone marrow cells induced proar-rhythmia effects, which the intracoronary route mightavoid. However, this finding in a rat model could be as-cribed to the many morphological and physiological differ-ences in the cardiovascular system between small and largeanimal models.
LV Function
Beneficial effects of different types of stem cells on car-diac function have been reported in animals and humans.21,
26, 28, 29 Some experimental studies have suggested that in-creased neovascularization after stem cell therapy was themain impetus for improved cardiac function19e22. In ourstudy, the beneficial effect of intracoronary administrationof ADSCs on neovascularization did not translate at 3weeks’ follow-up into significant improvement in cardiacfunction, taking into account that LV volumes and LVEFrepresent a gross estimation of LV contractile function. In-deed, it has been shown that quantitative assessment of re-gional systolic function might be more sensitive than globalLVEF for evaluating the slight changes in contractile func-tion induced by stem cell therapy.30 Although our resultsare similar to those reported in some animal studies,31,32
we do not exclude the possibility that the increased neovas-cularization we observed may translate into long-term func-tional benefits, either by new myocyte formation or byreducing negative remodeling.
Engraftment of ADSCs in Other Organs
Our study did not find labeled ADSCs in the representa-tive kidney, lung, intestine, spleen, and liver samples. Otherinvestigators analyzed the whole organ and observed a re-distribution of stem cells to non-target organs such as theliver, kidney, lung, and spleen.11,33,34 The effects of en-grafted cells in these remote organs are unknown. However,the methods used to track the injected cells differed; insome cases, permitting evaluation of the complete organ.Because our study could only analyze representative sam-ples, we cannot exclude the possibility of ADSC uptakeby remote organs after both intracoronary and transendo-cardial deliveries.
Study Characteristics and Limitations
Several stem cell labelling tags have been used in exper-imental studies and all methods have some limitations. Wechose electroporation because no virus is required and forits safer, fast manipulation of cells, high proportion oftransfected ADSCs, and expression of the b-Gal enzymeat 3 weeks after the administration of cells.
The optimal number of injected ADSCs is still controver-sial. For intracoronary administration, we chose to injectfewer than 20 million cells because ADSCs are particularlylarge and a higher number of this type of cells occluded ar-teries (1 animal not included). In this respect, Valina et al20
observed the no-reflow phenomenon after intracoronary ad-ministration of more than 10 million ADSCs. Finally, wedecided on a short-term survival study in an effort to under-stand early effects of ADSC administration. However, thislimits our ability to determine the possible benefits of ourobserved results at longer follow-up.
Conclusion
In summary, the present study shows that both intracoro-nary and transendocardial techniques of ADSCs delivery
Adipose Tissue-Derived Stem Cell Therapy � Rigol et al 365
after acute myocardial infarction are feasible. At 3 weeks’follow-up, both techniques resulted in similar rates of en-grafted cells, mainly in the infarct border zone, and someof these ADSCs were incorporated into newly formed ves-sels. We also identified better neovascularization resultswith intracoronary administration of ADSCs. Future studiesare required to understand the mechanisms involved in neo-vascularization and their effects on LVEF in a long-termsurvival model.
Acknowledgments
The authors are grateful to the Universitat de Barcelonamicroscopy service, Montse Vazquez and Nadia Castillofor assistance, and Elaine Lilly for English editing. Wewould also like to thank Antonio Diez and Antonio Bernadof the Centro Nacional de Investigaciones Cardiovascularesfor their advice on fluorescent immunohistochemistry andhelpful comments.
References
1. Agbulut O, Vandervelde S, Al Attar N, Larghero J, Ghostine S,
Leobon B, et al. Comparison of human skeletal myoblasts and bone
marrow-derived CD133þ progenitors for the repair of infracted myo-
cardium. J Am Coll Cardiol 2004;44:458e63.
2. Meyer GP, Wollert KC, Lotz J, Steffens J, Lippolt P, Fichtner S, et al.
Intracoronary bone marrow cell transfer after myocardial infarction.
Eighteen months’ follow-up data from the randomized, controlled
BOOST trial. Circulation 2006;113:1287e94.
3. Siminiak T, Fiszer D, Jerzykowska O, Grygielska B, Rozwadowska N,
Kalmucki P, et al. Percutaneous trans-coronary-venous transplantation
of autologous skeletal myoblasts in the treatment of post-infarction
myocardial contractility impairment: the POZNAN trial. Eur Heart
J 2005;26:1188e95.
4. Beeres SL, Atsma DE, van Ramshorst J, Schalij MJ, Bax JJ. Cell ther-
apy for ischaemic heart disease. Heart 2008;94:1214e26.
5. Lee RH, Kim B, Choi I, Kim H, Choi HS, Suh K, et al. Characteriza-
tion and expression analysis of mesenchymal stem cells from human
bone marrow and adipose tissue. Cell Physiol Biochem 2004;14:
311e24.
6. Planat-Benard V, Menard C, Andre M, Puceat M, Perez A, Garcia-
Verdugo JM, et al. Spontaneous cardiomyocyte differentiation from
adipose tissue stroma cells. Circ Res 2004;94:223e9.
7. Planat-Benard V, Silvestre JS, Cousin B, Andre M, Nibbelink M,
Tamarat R, et al. Plasticity of human adipose lineage cells towards en-
dothelial cells: physiology and therapeutic perspectives. Circulation
2004;109:656e63.
8. Halkos ME, Zhao ZQ, Kerendi F, Wang NP, Jiang R, Schmarkey LS,
et al. Intravenous infusion of mesenchymal stem cells enhances re-
gional perfusion and improves ventricular function in a porcine model
of myocardial infarction. Basic Res Cardiol 2008;103:525e36.
9. Fernandez-Aviles F, San Roman JA, Garcıa-Frade J, Fernandez ME,
Penarrubia MJ, de la Fuente L, et al. Experimental and clinical regen-
erative capability of human bone marrow cells after myocardial infarc-
tion. Circ Res 2004;95:742e8.
10. Fuchs S, Kornowski R, Weisz G, Satler LF, Smits PC, Okubagzi P,
et al. Safety and feasibility of transendocardial autologous bone mar-
row cell transplantation in patients with advanced heart disease. Am
J Cardiol 2006;97:823e9.
11. Freyman T, Polin G, Osman H, Crary J, Lu M, Cheng L, et al. A quan-
titative, randomised study evaluating three methods of mesenchymal
stem cell delivery following myocardial infarction. Eur Heart
J 2006;27:1114e22.
12. Tossios P, Krausgrill B, Schmidt M, Fischer T, Halbach M, Fries WU,
et al. Role of balloon occlusion for mononuclear bone marrow cell de-
position after intracoronary injection in pigs with reperfused myocar-
dial infarction. Eur Heart J 2008;29:1911e21.
13. Rigol M, Solanes N, Sionis A, Galvez C, Martorell J, Rojo I, et al.
Effects of cyclosporine, tacrolimus and sirolimus on vascular changes
related to immune response: an experimental study. J Heart Lung
Transplant 2008;27:416e22.
14. Martınez-Estrada OM, Munoz-Santos Y, Julve J, Reina M, Vilaro S.
Human adipose tissue as a source of Flk-1þ cells: new method of dif-
ferentiation and expansion. Cardiovasc Res 2005;65:328e33.
15. Farre J, Roura S, Prat-Vidal C, Soler-Botija C, Llach A, Molina CE,
et al. FGF-4 increases in vitro expansion rate of human adult bone
marrow-derived mesenchymal stem cells. Growth Factors 2007;25:
71e6.
16. Rigol M, Solanes N, Roque M, Farre J, Batlle M, Roura S, et al. Hae-
mosiderin deposits confounds tracking of iron-oxide labelled stem
cells. Transpl Proc 2008;40:3619e22.
17. Cai L, Johnstone BH, Cook TG, Tan J, Fishbein MC, Chen PS, et al.
IFATS series: human adipose tissue-derived stem cells induce angio-
genesis and nerve sprouting following myocardial infarction, in con-
junction with potent preservation of cardiac function. Stem Cells
2009;27:230e7.
18. Miyahara Y, Nagaya N, Kataoka M, Yanagawa B, Tanaka K, Hao H,
et al. Monolayered mesenchymal stem cells repair scarred myocar-
dium after myocardial infarction. Nat Med 2006;12:459e65.
19. Schenke-Layland K, Strem BM, Jordan MC, DeEmedio MT,
Hedrick MH, Roos KP, et al. Adipose tissue-derived cells improve car-
diac function following myocardial infarction. J Surg Res 2009;153:
217e23.
20. Valina C, Pinkernell K, Song Y, Bai X, Sadat S, Campeau RJ, et al.
Intracoronary administration of autologous adipose tissue-derived
stem cells improves left ventricular function, perfusion, and remodel-
ling after acute myocardial infarction. Eur Heart J 2007;28:2667e77.
21. Li B, Zeng Q, Wang H, Shao S, Mao X, Zhang F, et al. Adipose tissue
stromal cells transplantation in rats of acute myocardial infarction.
Coron Artery Dis 2007;18:221e7.
22. Zhang D, Gai L, Liu H, Jin Q, Huang J, Zhu X. Transplantation of au-
tologous adipose-derived stem cells ameliorates cardiac function in
rabbits with myocardial infarction. Chin Med J 2007;20:300e7.
23. Kajstura J, Rota M, Whang B, Cascapera S, Hosoda T, Bearzi C, et al.
Bone marrow cells differentiate in cardiac cell lineages after infarction
independently of cell fusion. Circ Res 2005;96:127e37.
24. Orlic D, Kajstura J, Chimenti S, Jakoniuk I, Anderson SM, Li B, et al.
Bone marrow cells regenerate infracted myocardium. Nature 2001;
410:701e5.
25. Schuleri KH, Amado LC, Boyle AJ, Centola M, Saliaris AP,
Gutman MR, et al. Early improvement in cardiac tissue perfusion
due to mesenchymal stem cells. Am J Physiol Heart Circ Physiol
2008;29:H2002e11.
26. Gavira JJ, Perez-Ilzarbe M, Abizanda G, Garcıa-Rodrıguez A,
Orbe J, Paramo JA, et al. A comparison between percutaneous and
surgical transplantation of autologous skeletal myoblasts in a swine
model of chronic myocardial infarction. Cardiovasc Res 2006;71:
744e53.
27. Fukushima S, Varela-Carver A, Coppen SR, Yamahara K, Felkin LE,
Lee J, et al. Direct intramyocardial but not intracoronary injection of
bone marrow cells induces ventricular arrhythmias in a rat chronic
ischemic heart failure model. Circulation 2007;115:2254e61.
28. Krause U, Harter C, Seckinger A, Wolf D, Reinhard A, Bea F, et al.
Intravenous delivery of autologous mesenchymal stem cells limits in-
farct size and improves left ventricular function in the infracted por-
cine heart. Stem Cells Develop 2007;16:31e7.
29. Martin-Rendon E, Brunskill SJ, Hyde CJ, Stanworth SJ, Mathur A,
Watt SM. Autologous bone marrow stem cells to treat acute myocar-
dial infarction: a systematic review. Eur Heart J 2008;29:1807e18.
366 Journal of Cardiac Failure Vol. 16 No. 4 April 2010
30. Herbots L, D’hooge J, Eroglu E, Thijs D, Ganame J, Claus P, et al.
Improved regional function after autologous bone marrow-derived
stem cell transfer in patients with acute myocardial infarction: a ran-
domized, double-blind strain rate imaging study. Eur Heart J 2009;30:
640e1.
31. de Silva R, Raval AN, Hadi M, Gildea KM, Bonifacino AC, Yu ZF,
et al. Intracoronary infusion of autologous mononuclear cells from
bone marrow or granulocyte colony-stimulation factor-mobilized
apheresis product may not improve remodelling, contractile function,
perfusion, or infarct size in a swine model of large myocardial infarc-
tion. Eur Heart J 2008;29:1772e82.
32. Hashemi SM, Ghods S, Kolodgie FD, Parcham-Azad K, Keane M,
Hamamdzic D, et al. A placebo controlled, dose-ranging, safety study
of allogenic mesenchymal stem cells injected by endomyocardial delivery
after an acute myocardial infarction. Eur Heart J 2008;29:251e9.
33. Barbash IM, Chouraqui P, Baron J, Feinbert MS, Etzion S, Tessone A,
et al. Systemic delivery of bone marrow-derived mesenchymal stem
cells to the infracted myocardium: feasibility, cell migration, and
body distribution. Circ 2003;108:863e8.
34. Hofmann M, Wollert KC, Meyer GP, Menke A, Arseniev L,
Hertenstein B, et al. Monitoring of bone marrow cell homing into
the infarcted human myocardium. Circ 2005;111:2198e202.