Peri-nuclear antibodies correlate with survival in Greek primary biliary cirrhosis patients
Vitamin E deficiency and psychomotor dysfunction in adults with primary biliary cirrhosis
-
Upload
independent -
Category
Documents
-
view
4 -
download
0
Transcript of Vitamin E deficiency and psychomotor dysfunction in adults with primary biliary cirrhosis
Am J C/in Nuir 1990;52:383-90. Printed in USA. © 1990 American Society for Clinical Nutrition 383
Vitamin E deficiency and psychomotor dysfunctionin adults with primary biliary cirrhosis13
Amelia MArria, Ralph E Tarter, Vijay Warty, and David H Van Thiel
ABSTRACT The purpose of this study was to determine
the prevalence of vitamin E deficiency in adults with chronic
cholestatic liver disease and to quantify the association betweentheir psychomotor performance and vitamin E status. In 42female patients with primary bibiary cirrhosis, 43.5% met two
standard criteria for vitamin E deficiency. Vitamin E-deficientpatients performed less well than did healthy control subjects
on six of eight neuropsychologic tests of psychomotor capacity
(p < 0.01). Vitamin E-sufficient patients did not differ signifi-
cantly from normal control subjects. Serum vitamin E concen-trations were significantly bower in the group classified as sig-
nificantly psychomotor-impaired by two independent neurop-sychologists (blind to vitamin E status) whereas liver-injurymeasures failed to distinguish between these two groups. Pa-
tients with bow serum vitamin E exhibited clinically evident
neurobogic abnormalities. These data suggest that vitamin E
deficiency may, in part, underlie psychomotor and neurologicdisturbances found in adult patients with chronic chobestatic
biverdisease. Am JClin Nutr l990;52:383-90.
KEY WORDS Vitamin E, cholestatic disease, neuropsy-chologic impairment, primary bibiary cirrhosis
Introduction
Chronic vitamin E deficiency in animals produces severeneurobogic impairment that is characterized by progressive cer-
ebellar atrophy, proximal muscle weakness, ataxia, and are-flexia (1-3). Preliminary reports in the medical literature havedocumented the presence of an analogous neurologic syn-
drome in children who have cystic fibrosis (4) or chronic chole-stasis (5, 6). These batter conditions, among other concomitantdiseases, are associated with a disturbance in fat absorption.
Early correction ofbiochemicab vitamin E deficiency can ame-
liorate neurologic disturbances in children who have severe
cholestasis (7). In cases where children are nonresponsive tointramuscular preparations, an oral supplement was shown to
correct the biochemical vitamin E deficiency as well as improve
neurologic functioning (8).
Several case studies demonstrated that a vitamin E defi-ciency and associated neurobogic symptoms frequently occur
in adults with chronic cholestasis (9, 10). In one large study,
Sokol et al (1 1) reported that 17% ofa sample (n =42) of adults
with primary biliary cirrhosis had vitamin E deficiency. The
severity of vitamin E deficiency in his sample was related to
both the severity and duration of his subjects’ illness; however
the neurologic status of all the subjects was not described.
Knight et al (12) recently reported a vitamin E-deficient adultpatient with primary bibiary cirrhosis who had evidence of se-
vere neurologic disturbance. Jeffrey et al ( 13) also examinedthe vitamin E status ofadult patients (n =142) with liver dis-
ease. They reported that 44% of patients with primary biliarycirrhosis and 32% with other cholestatic liver diseases in theirsample were vitamin E deficient. Five oftheir patients had cvi-
dence for a mild mixed sensorirnotor peripheral neuropathy.They concluded, however, that the neurologic symptoms in
these patients could not be attributable solely to vitamin E de-ficiency. Therefore, a more comprehensive investigation isneeded to clarify the association between vitamin E deficiency
and neurologic impairment in such patients. Munoz et al (14)recently reported a bower prevalence ofvitamin E deficiency ina sample of patients with primary biliary cirrhosis; however,decreased gastrointestinal absorption of vitamin E was ob-
served.
Our ongoing studies of adults with cholestatic liver disease(who were being evaluated as potential candidates for liver
transplantation) have revealed the presence of psychomotorimpairments that occur in the absence ofovert hepatic enceph-alopathy (1 5-1 7). In light of recent findings documenting the
occurrence of a vitamin E deficiency in patients with chronic
cholestasis, we hypothesized that the psychomotor impair-
ments observed in these individuals are, at least in part, rebated
to a vitamin E deficiency and are not due solely to a subclinicalhepatic encephalopathy. To date, the relationship between vi-
tamin E deficiency and neuropsychobogic function has notbeen examined in a group ofadult patients.
This study had three purposes: 1) to establish the presence
and severity ofvitamin E deficiency in a group ofadult patientswith chronic cholestatic liver disease, 2) to document the asso-
ciation between vitamin E status and biochemical measures of
liver injury, and 3) to determine the association between vita-
mm E status and the psychomotor functioning ofthese patients
as measured by their performance on a battery of psychomotor
I From the Departments of Psychiatry. Pathology. and Medicine,University ofPittsburgh School of Medicine.
2Supported by grants AM32556-Ol, AAO66O1-Ol, and DK39789
from the National Institutes of Health.3 Address reprint requests to AM Ama, University of Pittsburgh
School of Medicine, Department of Psychiatry, 201 DeSoto Street,Pittsburgh, PA I 5213.
Received March 23, 1989.Accepted for publication October 1 1, 1989.
by guest on Septem
ber 27, 2015ajcn.nutrition.org
Dow
nloaded from
1. Trailmaking A
2. Trailmaking B
3. Symbol-digit-modalities test
4. Groovedpegboard
(dominant)
5. Grooved
pegboard
(nondominant)
6. Finger tapping
7. Pursuit rotor
(dominant)
8. Pursuit rotor
(nondominant)
384 ARRIA ET AL
tests. The investigation of neurologic sequelae in adults with
vitamin E deficiency would extend the findings ofother studies
on children as well as demonstrate the need for treatment ofvitamin E deficiency in chronic liver disease.
Methods
Patients
Forty-two women admitted consecutively to Presbyterian
University Hospital ofthe University ofPittsburgh Health Sci-
ences Center, Pittsburgh, with a biopsy-proven diagnosis of pri-mary biliary cirrhosis composed the experimental group. In
each case, the biopsy was performed by one ofthe authors and
confirmed independently by a staff pathologist. All patients
were determined to have stage four primary biliary cirrhosis
with the exception oftwo who had stage three. All patients were
admitted to evaluate their candidacy for orthotopic liver trans-
plantation. Patients were aged 45.6 ± 7. 1 y (i ± SD). Fifteen
community-dwelling normal females aged 40.3 ± 8.4 y served
as control subjects. They were recruited by advertisement.None of the subjects had a history of neurobogic injury or dis-
ease, alcoholism, or significant medical history other than liverdisease. The subjects in both groups are participants in an on-
going series of investigations approved by the University ofPittsburgh Institutional Review Board in 1982 that are directedat clarifying hepatic-cerebral interactions. All subjects gave vol-
untary informed written consent before their participation in
this study.
Neither the control subjects nor the patient sample were tak-
ing any vitamin supplements at the time of study. Mean dailydietary intakes the following nutrients for the hospital patientswere as follows: 1675 kcal, 188.5 g carbohydrates, 60.0 g fat,
58.5 g protein, 3. 1 mg vitamin E, and 1469 �tg RE vitamin A.
Determination ofvitamin E status
Venous blood was obtained from each subject after an over-
night fast. Serum samples were frozen immediately after sepa-
ration from the cellular components of blood and were pre-
vented from having contact with light. The samples were
thawed immediately before they were extracted and assayed forthe measurement of the serum vitamin E concentration ac-cording to the method ofChow and Omaye (18).
We used high-performance liquid chromatography (Model
4000, Perkin-Elmer Corp, Norwalk, CT) with a C18 Bondapak
analytical column (Waters Chromatography Division, Milli-
pore Corp, Milford, MA) and a guard column packed with C18
Corasil (Waters Chromatography Division). Standard samplesof vitamin E of known concentrations were assayed at the be-ginning and end ofeach run to ensure the accuracy ofthe mea-
surements obtained. The internal standard used was retinyl ac-etate. The retention time for a-tocopherol by use of thismethod and equipment is 37 mm.
Serum lipids were extracted by the method ofBligh and Dyer(19) and were assayed by the method of Chiang et al (20). Inhyperlipidemic states, which commonly occur in patients withprimary biliary cirrhosis, the ratio ofvitamin E to total lipid is
thought to provide a better indication ofvitamin E status thanis the serum vitamin E concentration alone (1 1). Therefore thisratio was determined for each subject studied.
The determination of patients’ vitamin E status was made
TABLE 1
Description of neuropsychologic tests ofpsychomotor capacity
This test requires the subject to traverse a
complex spatial field by serially connectingnumbers. The time required to complete the
task is recorded.This test is given subsequent to Trailmaking A
and requires the subject to alternate numbersand letters in a manner similar to that used in
Trailmaking A. The letters and numbers arearranged haphazardly on a sheet of paper.
The time required to complete the task is
recorded.This test requires sustained attention and visual-
scanning abilities. The subject must write insequence, as rapidly as possible, numbers thatcorrespond to a particular symbol. Theperson must continuously scan the symbol-number matchings at the top ofa page, whileplacing in a row ofboxes below the correctnumber where only the symbol is present.
The number ofcorrect responses obtained in90 5 15 recorded.
This test measures eye-hand coordination. The
subject is required to insert pegs into a formboard having notched holes. The pegs can
thus only be placed in the form board in a
certain way. The time required to place all ofthe pegs in the pegboard for the dominanthand is recorded.
This test is identical to the test above, performed
with the nondominant hand.
This test ofsimple motor speed consists of atelegraph key attached to a counter. Thesubject is instructed to tap the key as quickly
as possible. Five trials, each of 10 s duration,are given for each hand. The score is the meannumber ofkey depressions or taps across five
trials for both hands.This apparatus for measuring perceptual motor
tracking consists ofa black rotating turntableof3O-cm diameter on which is painted a 1.3-cm-diameter silver circle at the periphery.The subject is required to hold a metal stylus
positioned on the circle while the disc rotatesfor 20 s at 20 rpm. The duration ofcontact onthe circle is recorded for each trial and themean score obtained across 10 consecutivetrials for the dominant hand is determined.
This test is identical to the test above, performed
with the nondominant hand.
during their first week of admission along with all other bio-chemical liver function and injury measures. These latter mdi-
ces ofliver function were performed by routine methods.
Neuropsychologic assessments
Table 1 lists the eight tests of psychomotor functioning thatwere administered to each subject. The tests were given by
trained psychotechnicians who were unaware of the nutrition
status of the patients. Each test session lasted ‘-P40 mm. Theinvestigators have years ofexperience in conducting neuropsy-
by guest on Septem
ber 27, 2015ajcn.nutrition.org
Dow
nloaded from
59.5% 40.5%� �1
n=14
50
40
30
20
10-
w-I0�
U)
U-
0I-zw0
w0�
50
40
30
20
10
50.0%
n=13
n=8 n=8
n=11
I.
50.0%
n=6
n=3
0.0- 0.4-
0.4 0.8
VITAMIN E AND PSYCHOMOTOR DYSFUNCTION 385
n=6
nn=5n=3 n=3nnn0-7 7- 11.6- 16.3-21- 25.5-
11.6 16.3 21 25.5 39.5
SERUM ALPHA-TOCOPHEROL (umol/L)
0.8- 1.2- 1.6- 2.0-
1.2 1.6 2.0 2.2
VITAMIN E: TOTAL CIRCULATING LIPIDS
(a) (b)
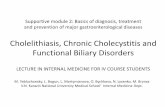
FIG 1. Percent sample of patients with primary biliary cirrhosis at different concentrations of vitamin E as mea-sured by serum a-tocopherol alone and the ratio of vitamin E to total circulating lipids. The shaded bars representvitamin E-deficient subjects and the clear bars represent vitamin E-sufficient subjects.
chologicab assessments with this particular hospitalized popula-
tion. The technicians are personally trained and supervised,
and testing sessions are spread out over time to avoid any
effects of fatigue on performance and to ensure accuracy of the
results.
These tests were chosen for this study for several reasons.First, all were demonstrated to be valid measures of psychomo-tor capacity and sensitive measures ofcerebral injury (2 1 ). Sec-ond, they were shown to surpass the sensitivity of the clinical
neurobogic examination for the detection ofsubcbinical hepatic
encephabopathy (22). Third, they are the techniques of choice
for quantitating psychomotor and cognitive capacity (23).Fourth, performance scores obtained by patients on neuropsy-
chologic tests were shown to be predictive ofoccupational and
social functioning (24). And fifth, the results obtained from a
neuropsychologic assessment can have an important bearing
on comprehensive medical management, especially when ca-pabibity (eg, driving a car) or safety (eg, operating power tools)
are considered (25). Thus, for both empirical and practical rca-sons, neuropsychobogic tests are ideal for quantifying psycho-motor capacity.
Rating by clinical neuropsychologists
Two independent clinical neuropsychobogists were given thescores on the psychomotor tests for each patient. They were
asked to classify each patient as having either a clinically sig-nificant psychomotor deficit or normal psychomotor function-
ing. Each clinician was blind to the identity and nutrition status
ofthe patient.
Neurologic examination
Patients with suspected vitamin E deficiency defined by avitamin E concentration < 1 1.6 �mol/L were given a routine
neurobogic examination by a staff neurologist. Electroencepha-
bogram (EEG) results on 18 of these 19 patients were also ob-
tamed. Thirteen patients with sufficient vitamin E concentra-
tions were also given a formal clinical neurologic examination.
Statistical analysis
Statistical analyses were performed by use ofSPSS software(SPSS, Inc, Chicago) on a DEC-10 mainframe computer. Pear-son product-moment correlations were employed to analyzethe relationship between biochemical measures and vitaminstatus. Two-tailed t tests for independent samples were utilized
to compare mean scores for the three groups studied on the
eight psychomotor tests and to compare the group of patientsclassified by two neuropsychologists as having a clinically sig-
nificant impairment with the group classified as normal.
Results
Figure 1 illustrates both the prevalence and severity of vita-mm E deficiency in the study sample of patients with primary
biliary cirrhosis. The mean serum a-tocopherol concentration
for the group was 1 1.61 ± 8.36 �mol/L (1 ± SD) and the ratio
of vitamin E to lipid (expressed as mg/g) was 0.93 ± 0.68. Therecognized concentrations (26) used to define vitamin E defi-
ciency are a serum vitamin E concentration < 1 1.6 1 �zmol/Land a ratio of vitamin E to lipid < 0.80. Over 30% of primary
biliary cirrhosis patients had serum vitamin E concentrations< 6.97 j�mol/L and a ratio of vitamin E to total lipids < 0.4.
Overall, 43.5% (n =19) ofthe primary biliary cirrhosis sample
met both standard criteria for vitamin E deficiency. This subset
ofpatients was used for further analysis because, by all criteria,no ambiguity about their vitamin E deficiency exists. Those
by guest on Septem
ber 27, 2015ajcn.nutrition.org
Dow
nloaded from
386 ARRIA ET AL
t Significantly different from the deficient group, p < 0.03.
TABLE 2Pearson product-moment correlations between biochemical measures
ofliver function and vitamin E status in females with primary biliary
cirrhosis
Serum
a-tocopherol
Ratio of vitamin
E to total lipids
Prothrombin time 0. 18 0.24
Ammonia (fasting) 0.04 0.06Total bilirubin -0.5 1 (p = 0.00 1) -0.39 (p = 0.013)
Alkaline phosphatase -0.08 0.27Alanine transaminase -0. 1 1 -0.26Indocyanine green clearance
at 20 mm -0.38 (p = 0.025) -0.37 (p = 0.034)Albumin 0.27 -0.07
-yGlobulin 0.15 0.11
Aspartate transaminase -0. 17 -0.27
‘y Glutamyl peptidetransferase 0.53(p=0.OOl) 0.14
who met neither criteria for a deficiency (n =1 5) composed
the vitamin E-sufficient group and served as the liver-disease
control group in the analyses. Although it has been argued that
the ratio of vitamin E to lipid is a better indicator of vitamin E
status than is serum vitamin E concentration alone, it is impor-
tant to note that in the current study the ratio provided no more
information than did the serum concentration alone.
The duration of symptomatic disease for the whole sample
was 5.0 ± 3.7 y. Duration was defined as the number of years
based on self report since the patient first experienced symp-
toms such as pruritus, fatigue, or jaundice, which eventuallyled to a biopsy-confirmed diagnosis. Overall, we found that
there was no significant correlation between reported duration
ofsymptomatic disease and either the serum vitamin E concen-
tration or the ratio of vitamin E to total lipid. In our sample,
duration was also unrelated to severity ofdisease because none
of the correlations between duration and biochemical mea-
sures ofliver function were statistically significant.
Of all the liver-function and injury indices measured and
shown in Table 2, only the serum vitamin E concentration and
the ratio of vitamin E to total lipids were found to be signifi-
cantly correlated inversely with indocyanine green clearance
and total bilirubin, suggesting that chobestasis is the probablemechanism responsible for both the altered liver function and
the vitamin E deficiency. The serum vitamin E concentration,but not the ratio of vitamin E to lipid, was significantly corre-bated directly with the concentration of serum a-glutamyl
transpeptidase (GGTP) activity. This finding may be con-
founded by the finding that the GGTP also correlated signifi-
cantly with total lipids (r = 0.56, p < 0.01). Thus, the elevated
GGTP may be the result ofan increased serum lipid concentra-
tion rather than increased vitamin E. This hypothesis is sup-
ported by the fact that the measure of vitamin E status that
adjusts for this phenomenon, ie, the ratio of vitamin E to total
lipid, did not correlate with GGTP.
The means and SDs ofeach liver-injury variable assessed forthe vitamin E-deficient and vitamin E-sufficient groups are
shown in Table 3. The only variable that significantly differs
between the two groups is bibirubin. The groups also did not
differ in age and duration ofsymptomatic disease.Table 4 presents the results ofthe analyses, which documents
group differences on the psychomotor tests. On six ofthe eight
tests the vitamin E-deficient group performed significantly
more poorly than did the healthy control subjects; in contrast,
only one statistically significant difference was observed be-
tween the normal control subjects and the subjects with pri-
mary bibiary cirrhosis who did not have biochemical evidence
for vitamin E deficiency.
The classification of the patients by two independent neu-
ropsychologists on the basis oftheir scores on the psychomotor
tests yielded two groups. One group (n = 19) was classified by
both clinicians as having a clinically significant psychomotor
impairment. The second group (n = 1 5) was found by both
clinicians to be performing within normal limits. Interrater re-
liability was 78.7%. These two groups ofpatients, referred to as
the impaired group and the normal group, were compared by
age, duration ofsymptomatic disease, biochemical measures of
liver function, and vitamin E status. As is shown in Table 5,serum vitamin E concentration is the only measure that was
significantly different between the two groups.
Subjects who met criteria for a serum vitamin E deficiency
underwent a routine formal neurologic examination. The re-
sults of the examination along with clinical information on
each patient are shown in Table 6. The three patients with no
detectable amount of vitamin E all showed signs of hyper-
reflexia. One of these patients could not perform tandem gait
accurately and had an observed sensory boss to pinprick stimu-
bation. One patient with very bow vitamin E had positive aster-
ixis, hand tremor, severe ataxia, and hyperreflexia with cbonus.
Hand tremor was also seen in another patient with very lowvitamin E. One 34-y-old patient with borderline vitamin E de-
ficiency was areflexic on three offour deep-tendon reflexes and
had evidence ofperipheral neuropathy upon eletromyographictesting. Hyperreflexia ofthe upper extremities was seen in only
one patient in this group, and two others had mild hyperreflexiathroughout. One patient with low serum vitamin E but a nor-
mal ratio of vitamin E to lipid reported experiencing loss of
balance, and another patient with similar vitamin E status had
proximal median and ulnar mononeuropathy, mild axonal
TABLE 3Clinical measures and liver-injury indices for vitamin E-deficient andvitamin E-sufficient patients*
Vitamin E
deficient
Vitamin Esufficient
Normal
range
Age(y) 45.5 ± 5.9 47.9 ± 7.6 -
Duration of symptomatic
disease(y) 6.3 ± 3.2 8.2 ± 4.2 -
Prothrombintime(s) 13.9±2.2 13.1 ± 1.8 10.5-13.5
Fasting ammonia(zmol/L) 47 ± 19 58 ± 22 5-50
Totalbilirubin(umol/L) 258 ± 11 1 133 ± 123t 2-18
Alkaline phosphatase (�kat/L) 1 1 .9 ± 7.4 9.4 ± 4.7 0.5-2.0
‘y-Glutamyl transpeptidase
(�kat/L) 6.7 1 ± 6.22 9.39 ± 9.77 0-0.50
Alanine transaminase (�zkat/L) 1.5 ± 0.7 1.3 ± 0.7 0-0.58
Aspartate transaminase (�kat/L) 2.87 ± I . 15 2.43 ± 1 .50 0-0.58
Indocyanine green (% retention
at 20 mm) 39.3 ± 12.7 30.8 ± 18.6 0-4
Serum albumin (g/L) 3 1 ± 6 29 ± 4 36-52
yGlobulin(g/L) 22±5 25±1 6-16
Total lipids (gIL) 7.3 ± 3.7 5.2 ± 1 .2 2.0-4.0
by guest on Septem
ber 27, 2015ajcn.nutrition.org
Dow
nloaded from
*�±SD.
VITAMIN E AND PSYCHOMOTOR DYSFUNCTION 387
t Significantly different from the impaired group, p = 0.03.:t Expressed as mg/g.
TABLE 4Performance scores on neuropsychologic tests for normal, healthy control subjects, primary biliary cirrhosis(PBC) patients with vitamin E
deficiency, and PBC patients without vitamin E deficiency
Neuropsychologic testHealthy control
subjects Vitamin E deficient Vitamin E sufficient
Visuomotor efficiencyTrailmaking A 26.87 ± 6.7 36.22 ± 9.4 (1 = 3.38) 34.7 1 ± 1 1.0 (NS)Trailmaking B 57.00 ± 10.3 98.05 ± 31.8 (t = 5.28) 77.14 ± 32.5 (NS)Symbol digit 55.60 ± 7.2 39.16 ± 10.1 (t = 5.55) 44.07 ± 6.4 (NS)
Simple motor speedFinger tapping (right and left hands) 84.50 ± 1 1.2 82.94 ± I 3.9 (NS) 84.29 ± 8.8 (NS)
Fine-motor coordinationGrooved pegboard
Dominant hand 6 1.80 ± 8.3 79.05 ± 10. 1 (1 = 5. 16) 76.67 ± 22. 1 (NS)
Nondominant hand 65.43 ± 7.3 87.95 ± 2 1 .7 (1 = 4.2 1) 85.00 ± 22.6 (1 = 2.87)Eye-hand coordination
Pursuit rotor
Dominant hand 15.90 ± 2.8 12.64 ± 2.9 (t = 2.99) 13.43 ± 4.9 (NS)Nondominant hand 15.37 ± 3.1 12.46 ± 3.5 (NS) 12.99 ± 5.4 (NS)
* i�± SD. All t values indicate significant differences from control subjects, p < 0.01.
loss, and observed demyelination. EEG results interestingly re-
vealed generalized dysrythmia in 6 of the 18 vitamin E-defi-
cient patients and another had asymmetric dysrhythmia.
Results from the clinical neurological examination on 13 vi-
tamin E-sufficient patients (by serum criteria) are presentedin Table 7. Hyperreflexia was observed in two patients, andhyporeflexia was reported in two patients. The serum vitaminE concentration in both patients with hyporeflexia was 11.84�tmol/L, which is just above the standard serum criterion for
deficiency. Decreased motor strength was also observed in one
sufficient patient who also was hyporeflexic.
TABLESLiver-injury measures for patients classified as having a clinically
significant psychomotor impairment and patients classified as normal
by two independent clinical neuropsychologists
Clinically
impairedClinically
normal
Age (y) 45.5 ± 5.9 47.9 ± 7.6Duration ofsymptomatic disease (y) 6.8 ± 3.0 6.8 ± 4.4Prothrombin time (s) 13.8 ± 1.0 13.5 ± 2.4Fasting ammonia (umol/L) 56 ± 24 48 ± 18
Total bilirubin (umol/L) 239 ± 145 195 ± 121Alkaline phosphatase (zkat/L) 10.2 ± 7.7 1 1 .2 ± 4.9
‘1 Glutamyl transpeptidase (�zkat/L) S. 19 ± 3.89 10.44 ± 9.55Alanine transaminase (�tkat/L) 1.23 ± 0.52 1.42 ± 0.77
Aspartate transaminase (�zkat/L) 2.48 ± 0.90 2.41 ± 1.15Indocyanine green (% retention at
20 mm) 39. 1 ± 12.8 32.3 ± 16.8Serum albumin (giL) 29 ± 6 32 ± 5.y Globulin (g/L) 23 ± 6 23 ± 8Total lipids (gIL) 5.2 ± 2.5 6.6 ± 3.2
Serum vitamin E (�mol/L) 8.36 ± 6.04 14.40 ± 9.29tRatio ofvitamin E to total lipidsf 0.7 ± 0.6 1.1 ± 0.8
Discussion
The results ofthis study demonstrate that a vitamin E-defi-
ciency state exists in a high proportion of adult patients who
have chronic advanced cholestatic liver disease. The preva-
lence and severity ofvitamin E deficiency in the sample studiedis striking and, although considerably greater than that re-
ported by Sokol et al (1 1), it is consistent with the recent reportby Knight et al (12). Perhaps this discrepancy can be explained
by the fact that the study population, consisting of potentialliver-transplant candidates (most of whom had end-stage pri-
mary bibiary cirrhosis), was considerably more ill than were thepopulations studied previously.
Duration ofsymptomatic disease was found not to correlatewith vitamin E status in the sample studied. It cannot be cx-
trapolated, however, that vitamin E status is not related to se-
verity ofdisease because, in our sample, duration ofdisease was
not correlated with any index of liver injury. Duration, as itwas defined in the study and used clinically, conceivably could
include a number of years when a person is relatively asymp-
tomatic. For our purposes, it might have been more useful todefine duration as the number of years from the time when
symptoms became persistent enough to require hospitaliza-tion, ie, duration ofthe present episode.
Both serum vitamin E and the ratio of vitamin E to totallipid correlated with indocyanine green clearance and total bili-rubin, an indication that with increasing severity of disease,
one is at higher risk for developing vitamin E deficiency. Of allofthe liver-injury measures assessed, total bilirubin concentra-tion was the only variable that significantly differed betweenthe vitamin E-sufficient and vitamin E-deficient group. Thisfinding supports the theory that cholestasis is the primarymechanism for both hyperbibirubinemia and decreased vita-
mm E.
The neurobogic sequelae of a vitamin E deficiency in thissample are consistent with other case reports and the recentstudy by Knight et al (12). Neurobogic symptomatology inadults may have different characteristics than those symptoms
by guest on Septem
ber 27, 2015ajcn.nutrition.org
Dow
nloaded from
388 ARRIA ET AL
TABLE 6Clinical information and results ofthe neurologic examination on 19 patients with low serum vitamin E concentrations
Duration of
symptomatic Serum
Ratio of
vitamin E to Sensory Motor
Deep tend on reflexes
Ankle KneeSubject Age disease vitamin E total lipids Bilirubin Orientationt Tremorf losst strength Biceps Triceps jerk jerk EEG�
y �v �zmo//L �moI/L
I 29 6 9.1 0.62 348.8 0 0 0 5/5 2+ 2+ 2+ 2+ 0
2 38� 4 6.7 1.00 249.7 0 0 0 5/5 2+ 2+ 2+ 2+ 0
3 4611 3 10.2 1.41 218.9 0 0 0 5/5 2+ 2+ 2+ 2+ 1
4 45 12 10.4 0.71 1 18.1 0 0 0 5/5 1+ 1+ 2+ 2+ 0
5 43 6 10.4 1.04 236.0 0 0 0 5/5 2+ 2+ 2+ 2+ 1
6 48 5 9.1 0.49 254.8 0 0 0 5/5 3+ 3+ 3+ 3+ 1
7 34 9 1 1.4 0.97 147.1 0 0 0 5/5�I 0 2+ 0 0 2
8 48 5 6.0 0.58 282.2 0 0 0 5/5 2+ 2+ 2+ 2+ 1
9 48 5 0.0 0.00 302.7 0 0 I 5/5 2+ 2+ 4+ 4+ 1
10 45 3 5.6 0.29 162.5 0 0 0 5/5 3+ 3+ 3+ 3+ 0
I I 39 8 3.5 0.34 499.3 0 0 0 5/5 2+ 2+ 2+ 2+ 0
12 48 2 10.7 1.23 153.9 0 0 0 5/5 2+ 2+ 2+ 2+ 0
13 51 10 0.0 0.00 90.6 0 0 0 5/5 3+ 3+ 3+ 3+ 0
14 41 8 2.6 0.29 383.0 1 Itt 0 4/5 3+ 3+ 3+ 4+ff 0
15 54 5 0.0 0.00 88.9 0 0 0 5/5 3/4+ 3/4+ 3/4+ 3/4+ 0
16 46 13 7.0 0.50 176.1 0 0 0 5/5 2+ 2+ 2+ 2+ 0
17 45 10 3.3 0.29 345.4 0 0 0 4/5 2+ 2+ 2+ 2+ 1
18 36 4 2.8 0.23 277.0 0 1 0 5/5 2+ 2+ 2+ 2+ 0
19 51 7 7.9 0.29 188.1 0 0 0 5/5 2+ 2+ 2+ 2+ NA�
S Expressed as mg/g.
t 0, normal; 1, symptom observed.
1:Electroencephalogram. 0, normal; I , grade I with generalized dysrhythmia; 2, asymmetric dysrhythmia.
§ Proximal median and ulnar mononeuropathy; mild axonal loss and demyelination.
II Selfreported difficulty with balance.#{182}Evidence ofperipheral neuropathy on electromyographic testing.
** Could not perform tandem gait accurately.tt Severe ataxia, positive asterixis.if With clonus.
§� Not available.
found in children with vitamin E deficiency. More extensiveinvestigation of the neurobogic status of adults with vitamin E
deficiency needs to be conducted to define symptoms rebated
directly to vitamin E deficiency and those that could be relatedmore directly to hepatic encephalopathy. This study quantifies
psychomotor neuropsychologic deficits in individuals with ad-vanced primary biliary cirrhosis and a concomitant vitamin E
deficiency as compared with normal healthy adults. The psy-
chomotor performance of the vitamin E-sufficient group fellbetween the vitamin E-deficient group and the normal controlsubjects. The differences between the two primary biliary cir-rhosis groups was not statistically significant. There are trendsin the data of Tables 3 and 4 despite the absence of statisticalsignificance between the vitamin E-sufficient and -deficient
groups with primary bibiary cirrhosis (PBC). Perhaps with a
larger sample size, statistical differences would be revealed.Biochemical measures related to vitamin E status, namely
bilirubin and indocyanine green clearance, did not correlatewith neuropsychobogic test performance. Bilirubin was signifi-
cantly higher in the vitamin E-deficient group and possibly
could be reflective of more severe liver injury and thus de-creased psychomotor performance of this group. However, a
more probable explanation is that the neurologic symptoms area result of a combination of liver dysfunction and vitamin Edeficiency, both ofwhich contribute to the presence of psycho-
motor deficits. The finding that the serum vitamin E concentra-tion was the only variable that was significantly different in the
group classified as having a clinically significant psychomotorimpairment reinforces the association between vitamin E defi-
ciency and psychomotor impairment.
These results argue for a nutritionally mediated psychomo-tor deficit, rather than a solely hepaticalby determined mecha-nism, and extend previous research citing the occurrence of
similar neurobogic symptoms in children with diseases of fatmalabsorption. The mechanism by which neurologic dysfunc-
tion occurs as a result of a vitamin E deficiency is not corn-
pletely understood but accumulating evidence from studies
performed both in vitro and in vivo suggests that the antioxida-
tive properties of vitamin E may serve to protect neuronalmembranes from free radical degeneration, and that when vita-
mm E deficiency exists, nerve tissue is susceptible to peroxida-tive injury (27-29).
In patients with chronic advanced cholestatic liver disease,
portal systemic encephalopathy has been postulated as the pri-mary factor underlying the characteristic neurologic and neu-ropsychobogic disturbances. However, the findings from this
study support the hypothesis that a vitamin E deficiency may,at least in part, contribute to the psychomotor dysfunction ob-
served in individuals with advanced primary biliary cirrhosis.There may be several etiobogic factors involved in the develop-ment ofcognitive deficits observed in chronic-liver-disease pa-tients. It is important to emphasize that vitamin E deficiency is
perhaps one of several contributory factors that interact andresult in cognitive disturbance.
by guest on Septem
ber 27, 2015ajcn.nutrition.org
Dow
nloaded from
VITAMIN E AND PSYCHOMOTOR DYSFUNCTION 389
TABLE 7
Clinical information and results ofthe neurologic exam on I 3 patients with sufficient concentrations ofvitamin E
Duration of
symptomatic Serum
Ratio of
vitamin E to Total Sensory Motor
Deep tendo n reflexes
Ankle Knee
Subject Age disease vitamin E total lipids bilirubin Orientationt TremorJ losst strength Biceps Triceps jerk jerk EEG�
y y �mo1/L �imol/L
1 39 9 13.9 1.08 15.4 0 0 0 5/5 2+ 2+ 2+ 2+ 0
2 46 3 16.7 1.81 47.9 0 0 0 5/5 2+ 2+ 2+ 2+ 03 39 2 21.4 1.85 143.6 0 0 0 5/5 2+ 2+ 2+ 2+ 04 53 9 16.5 1.78 331.7 0 0 0 5/5 2+ 2+ 3+ 3+ 0
5 33 1 12.9 0.75 236.0 0 0 0 5/5 2+ 2+ 2+ 2+ 0
6 53 I I 19.6 1.83 39.3 0 0 0 5/5 2+ 2+ 2+ 2+ 17 59 9 11.8 1.03 111.2 0 0 0 3/4 1+ 1+ 0 2+ 0
8 45 3 25.8 2.16 15.4 0 0 0 5/5 2+ 2+ 2+ 2+ 0
9 44 4 1 1.8 1.8 218.9 0 0 0 5/5 2+ 2+ 2+ 2+ 0
10 36 10 11.8 1.02 263.3 0 0 0 5/5 1+ 1+ 1+ 1+ 0
II 48 4 15.8 1.34 352.3 0 01 0 5/5 2+ 2+ 2+ 2+ 0
12 59 15 23.7 2.15 13.7 0 0 0 5/5 2+ 2+ 3+ 3+ 0
13 46 6 20.5 1.13 309.5 0 OIl 0 5/5 2+ 2+ 2+ 2+ 0
* Expressed as mg/g.
t 0, normal; I, symptom observed.
t See Table 6.
§ Mild astenxis.
0 Mild difficulty on tandem walking.
In summary, the present findings underscore the need for
further investigations of the relationships among nutrient de-ficiencies, hepatobibiary dysfunction, and nervous system in-tegrity. At a practical level the results of this study emphasize
the need for a comprehensive and interdisciplinary approach
to patient management, one that includes a comprehensive nu-trition assessment. The early diagnosis and treatment of vita-mm E deficiency in patients with cholestatic liver disease mayhave important ramifications for mitigating bong-term neuro-logic sequebae. El
References
1. MachIm U, Filipski R, Nelson JS. Effects ofa prolonged vitaminEdeficiency in the rat. J Nutr 1977; 107:1200-8.
2. Pappenheimer AM, Goettsch M. A cerebellar disorder in chicks,
apparently ofnutritional origin. J Exp Med 1931; 53: 1 1-26.
3. Nelson JS, Fitch CD, Fischer VW, et al. Progressive neuropatho-logic lesions in vitamin E deficient rhesus monkeys. J Neuropathol
Exp Neurol 198 l;40:166-86.4. Elias E, Muller DPR, Scott J. Association ofspinocerebellar disor-
ders with cystic fibrosis or chronic childhood cholestasis and verylow serum vitamin E. Lancet 1981;2:13l9-2l.
S. Sokol Ri, Heubi JE, lannaccone 5, et al. Mechanism of causingvitamin E deficiency during chronic childhood cholestasis. Gastro-
enterology l983;85:l 172-82.
6. Rosenblum JL, KeatingJP, Prensky AL, et al. A progressive neuro-logic syndrome in children with chronicliverdisease. N Engl J Med
198 1;304:S0S-8.
7. Sokol Ri, Guggenheim M, lannaccone ST, et al. Improved neuro-logic function after long-term correction of vitamin E deficiencyin children with chronic cholestasis. N Engl J Med l985;313:1580-6.
8. Sokol Ri, Butler-Simon NA, Bettis D, et al. Tocopheryl polyethyl-ene glycol 1000 succinate therapy for vitamin E deficiency during
chronic childhood cholestasis: neurologic outcome. J Pediatr1987; 111:830-6.
9. Werlin SL, Harb JM, Swick H, et al. Neuromuscular dysfunction
and ultrastructural pathology in children with chronic cholestasisand vitamin E deficiency. Ann Neurol 1983; 13:29 1-6.
10. Harding AE, Matthews 5, Jones 5, et al. Spinocerebellar degenera-tion associated with a selective defect of vitamin E absorption. N
EnglJ Med 1985;3l3:32-5.1 1. Sokol Ri, Balistreri WF, Hoofnagle JH, et al. Vitamin E deficiency
in adults with chronic liver disease. Am J Clin Nutr l985;41:66-72.
12. Knight RE, Bourne AJ, Newton M, Black A, Wilson P. Lawson
MJ. Neurologic syndrome associated with low levels ofvitamin Ein primary biliary cirrhosis. Gastroenterology 1986;91:209-l 1.
13. Jeffrey GP, Muller DPR, Burroughs AK, et al. Vitamin E defi-
ciency and its clinical significance in adults with primary biliarycirrhosis and other forms of chronic liver disease. J Hepatol
1987;4:307- 17.
14. Munoz Si, Heubi JE, Balistreri WF, et al. Vitamin E deficiency inprimary biliary cirrhosis: gastrointestinal malabsorption, fre-quency and relationship to other lipid soluble vitamins. Hepatol-
ogy 1989;9:525-31.
15. Tarter RE, Hegedus AM, Van Thiel DH, et al. Nonalcoholic cir-rhosis associated with neuropsychological dysfunction in the ab-
sence of overt evidence of hepatic encephalopathy. Gastroenterol-ogy l984;86:l42l-7.
16. Hegedus AM, Tarter RE, Van Thiel DH, et al. Neuropsychiatric
characteristics associated with primary biliary cirrhosis. Int J Psy-chiatry Med 1984; 14:303-14.
17. Tarter RE, Hays AL, Sandford SL, et al. Cerebral morphologic sta-tus is predicted by liver injury severity in patients with nonalco-
holic cirrhosis. Lancet l986;2:893-S.
18. Chow F, Omaye S. Use ofantioxidants in the analysis of vitamins
A and E in mammalian plasma by high performance liquid chro-matography. Lipids 1983; 18:837-41.
19. Bligh EG, Dyer WJ. A rapid method of total lipid extraction and
purification. Can J Biochem Physiol 1959:37:91 1-7.
20. Chiang SP, Gessert CF. Lowry OH. Colorimetric determination ofextracted lipids. Randolph AFB, San Antonio, TX: Air University,1957.
2 1 . Gitlin N, Lewis DC, Hinkley L. The diagnosis and prevalence
by guest on Septem
ber 27, 2015ajcn.nutrition.org
Dow
nloaded from
390 ARRIA ET AL
of subclinical hepatic encephalopathy in apparently healthy encephalopathy. I. Nature ofcerebral functional defects and theirambulant, non-shunted patients with cirrhosis. J Hepatol 1986; effect on fitness to drive. Dig Dis Sci 198 l;26:622-30.3:75-82. 26. Horwitt MK, Harvey CC, Daum CH, et al. Relationship between
22. Rehnstrom S. SimertG, Hansson J, et al. Chronic hepatic encepha- tocopherol and serum lipid levels for determination of nutritionallopathy. A psychometrical study. Scand J Gastroenterol 1977; 12: adequacy. Ann NY Acad Sci l972;203:223-36.
305-1 1. 27. Yoshida S, Busto R, Watson BD, et al. Postischemic cerebral lipid
23. Goldstein C, Tarter R, Shelly C, et al. The Pittsburgh Initial Neuro- peroxidation in vitro: modification by dietary vitamin E. J Neuro-chem 1985;44:1�93-601.
psychological Testing System (PINTS): a neuropsychological 28. Demopoulos HB, Flamm ES, Pietronigro DD, et al. The free radi-
screen battery for psychiatric patients. J Behav Assess 1983; 5:227- cal pathology and the microcirculation in the major central ncr-38. vous system disorders. Acts Physiol Scand l98l;492:9l-l 19.
24. Lezak M. Neuropsychobogical assessment. 2nd ed. New York: Ox- 29. Hauswirth JW, Nair PP. Some aspects of vitamin E in the cx-
ford University Press, 1984. pression of biological information. Ann NY Acad Sci l972;203:
25. Schomerus H, Hamster W, Blunck H, et al. Latent portal-systemic 1 1 1-2.
by guest on Septem
ber 27, 2015ajcn.nutrition.org
Dow
nloaded from