Fibrilación auricular en pacientes hospitalizados ... - RUC - UDC
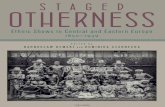
Staged Cheek-to-Nose and Auricular Interpolation Flaps
-
Upload
independent -
Category
Documents
-
view
4 -
download
0
Transcript of Staged Cheek-to-Nose and Auricular Interpolation Flaps
Staged Cheek-to-Nose and Auricular Interpolation FlapsTRI H. NGUYEN, MD
Department of Dermatology, The University of Texas M. D. Anderson Cancer Center, Houston, Texas
BACKGROUND. Staged interpolation flaps are priceless options inskin cancer reconstruction. Their value lies in their flexibility,reach, reliability, and ability to repair distant, complex facialdefects. Familiar interpolation flaps to dermatologic surgeonsinclude the paramedian forehead flap, cheek-to-nose interpola-tion flaps, and auricular staged flaps.OBJECTIVE. In this special reconstructive issue, the paramedianforehead flap is discussed separately. This article highlights thecheek-to-nose and auricular interpolation flaps as applied to skincancer defects. Design considerations, anatomic basis, execution,and the distinctions of each repair are presented.
MATERIALS AND METHODS. Patients with facial defects from Mohsmicrographic surgery serve to illustrate the surgical techniques ofeach repair.RESULTS. With meticulous planning and thoughtful execution,cheek-to-nose and auricular staged flaps are capable of restoringboth function and cosmesis. Several surgical stages are necessary,and an adequate supporting infrastructure is essential for an opti-mal outcome.CONCLUSION. Skin cancer patients with complex facial wounds fromMohs micrographic surgery may be assured of the highest possiblecure rate. Further, their esthetic and functional reconstructive goalsmay be achieved with staged flaps for the nose and ear.
© 2005 by the American Society for Dermatologic Surgery, Inc. • Published by BC Decker IncISSN: 1076–0512 • Dermatol Surg 2005;31:1034–1045.
TRI H. NGUYEN, MD, HAS INDICATED NO SIGNIFICANT INTEREST WITH COMMERCIAL SUPPORTERS.
IN THE algorithm of facial reconstruction, staged cheek-to-nose and auricular pedicle flaps are invaluable. Theyare also known as indirect, interpolation, and sometimesaxial pattern repairs. Their attributes permit the repair ofcomplex nasal and auricular wounds while preservingimportant anatomic landmarks. All interpolation flapsshare in common the following: (1) the flap donor site isdistant and not contiguous with the defect and (2) two ormore surgical stages are required for reconstruction. Addi-tionally, the flap pedicle may be based on a named vesseland its tributaries, making flap viability more reliable thanrandom pattern flaps. Interpolation flaps are often used toreconstruct entire subunits. Loss of up to 50% or more ofa subunit, for example, may be better repaired if the resid-ual tissue is excised. In facial cancer reconstruction, famil-iar interpolation flaps include (1) the paramedian foreheadflap (PFF), (2) cheek interpolation, and (3) auricular flaps.
Preoperative Consultation for InterpolationFlaps
All patients and their caretakers should understand thatinterpolation flaps require a minimum of two separatestages. Stage I initially covers the defect. Stage II (typically3 weeks or later) divides the pedicle and completes the flap
inset. Realistically, however, additional revision stages orinterventions are common to optimize results. Before pedi-cle detachment, facial appearances may be dramaticallyaltered, which may be a shock for the unprepared patient.Interference with social functions, wearing glasses, driv-ing, working, and exercise are all relevant issues, especiallyfor the PFF. Prior to flap execution, reviewing photographsof representative repairs will greatly enhance a patient’spreparation.1–4
Cheek-to-Nose Interpolation Flap: Stage I
Application
The cheek-to-nose interpolation flap (CIF) may reconstructthe ala, columella, nasal sill, and, less ideally, small defectsof the nasal tip. Defects for the CIF are usually smaller thanthose requiring a PFF. Strictly alar wounds, for example,are ideal candidates (Figure 1). The medial cheek skinclosely simulates alar skin in texture, color, and sebaceous-ness. The soft cheek skin contracts and trapdoors morereadily than forehead skin, a feature that can be exploitedfor the alar lobule. An advantage of the CIF over otheroptions for the ala is preservation of the alar groove.5 Thissulcus is difficult to restore once blunted by single-stagerepairs (melolabial transposition flap), with resulting alargroove asymmetry and suboptimal cosmesis.6 The potentialfor terminal hair transfer to the nose is relevant with theCIF in men, in whom bearded hairs are often present at themedial cheek.
Address correspondence and reprint requests to: Tri H. Nguyen,MD, Department of Dermatology, The University of Texas M. D.Anderson Cancer Center, 1515 Holcombe, Box 434, Houston, TX77030, or e-mail: [email protected].
Dermatol Surg 31:8 Part 2:August 2005 NGUYEN: STAGED INTERPOLATION FLAPS 1035
Anatomy
Unlike the PFF’s pedicle, which actually contains thesupratrochlear artery, the CIF relies on myocutaneous per-forators and tributaries from the angular artery for its via-bility. As a result, its vascular reliability is less than that ofthe PFF.
Flap and Pedicle Design
Although a PFF template matches exactly its defect, theCIF should be 1 mm larger than the ala in all dimensionsto compensate for eventual contraction.7 A material suchas suture foil or Telfa (Tyco Healthcare Group LP, Mans-field, MA, USA) will best reproduce the spherical dimen-sions of the ala and is modeled after the contralateral nor-mal side. Although the flap template should account forany anticipated removal of subunit tissue, any excision ofthe residual ala should wait until flap viability is ensuredat the time of pedicle division. CIF dimensions may beexpanded to cover alar defects with small extensions ontothe nasal sidewall but not the lateral cheek. A cheekadvancement flap is more appropriate for the latter por-tion. If covering extends across the alar groove, then sub-sequent stages are needed to recreate this sulcus.
Cartilage structural grafts are also important consider-ations with the CIF.8,9 They especially prevent contractile
elevation of the alar rim and collapse of the nasal valve.Some contraction effect is inevitable and even desirable torestore the lobular ala. Excessive contraction, however,(prevented by the cartilage graft) results in a ball-like domerather than an esthetic lobule. Any batten graft should belong enough to span the entire alar length and support theoverlying flap. It should also be wide enough (1 cm) tospan the alar lobule to resist the contractile forces of heal-ing. Sculpting may be needed to create a graft that is 1 mmthick and has beveled edges and a curvature to match thealar convexity. The cartilage graft should be securedwithin a pocket in the alar base laterally and to the nativealar cartilage medially. Further, it must be positioned asclose as possible to the alar margin for rim support.
An accurate template should be positioned along themedial cheek and melolabial fold and the flap outlines repro-duced. The widest part of the template should be across orslightly above the oral commissure (Figure 2). Longerdesigns (flap below the oral commissure) are usually unnec-essary but are still viable. Cutaneous triangles are thendrawn above and below the flap outline as standing cones inan elliptical excision. The superior triangle should taperbelow the alar-cheek sulcus to avoid blunting of this land-mark. It must be stressed that although the proximal skin tri-angle is small, the underlying pedicle itself should be widerand deeper during development (Figure 3). These designsfacilitate primary closure of the donor site without unto-ward lip or alar groove distortion.
The proximal pedicle of the CIF may be developed to beeither myocutaneous or myosubcutaneous. With the myocu-taneous pedicle, all layers are harvested (skin, subcutis, somemuscle) contiguously. A myosubcutaneous pedicle, however,consists of only the subcutis and some underlying muscle,without the overlying skin. Portions of the levator labii supe-
Figure 1. Mohs defect encompassing the subtotal alar dimension.
Figure 2. Template position for a cheek interpolation flap; notethe structural cartilage graft in place for alar rim stability and flapsupport.
1036 NGUYEN: STAGED INTERPOLATION FLAPS Dermatol Surg 31:8 Part 2:August 2005
rioris alequae nasi provide the muscle component in bothdesigns. The myocutaneous design is easier to harvest butplaces greater metabolic demands on the pedicle (nourishesboth the flap and the overlying skin). The myosubcutaneouspedicle is technically more challenging but may providegreater mobility and viability. With the myosubcutaneousdesign, if necrosis does occur at the distal flap, then proxi-mal skin is not available to salvage the repair.
Regardless of the design, adequate flap reach should betested prior to incision with a suture or stretched gauze.The CIF rotates counterclockwise from the right cheek fora right-sided defect and clockwise from the left cheek fora left-sided defect. Template orientation should reflect thisrotational movement.
Anesthesia
A CIF requires less adjunctive anesthesia or sedation thana PFF. At most, oral anxiolysis with benzodiazepines(midazolam, lorazepam) is all that is needed in addition tolocal anesthesia. Nerve blocks of the infraorbital andexternal nasal nerve will augment patient comfort but areusually not necessary.
Execution
Prior to the first incision, all design elements should bemeasured and remeasured, and anesthesia must be com-plete. The execution sequence I use is (1) cartilage supportand nasal lining restoration (if needed), (2) flap harvestingand pedicle mobilization, (3) defect preparation, (4) flappreparation and inset, (5) donor site closure, and (6) post-operative care.
Cartilage and Lining RestorationCartilage grafts or nasal lining should be secured first tominimize closure delays. Cartilage grafts may be structural(added for a supportive role even when native cartilage is
intact) (see Figure 2) or restorative, replacing what wasremoved. Structural purposes include (1) bracing theheavy flap tissue, (2) maintaining the patency of the inter-nal nasal valve and airway (of utmost importance in nasalreconstruction), (3) minimizing scar contraction, and (4)restoring contour projection (nasal tip). Donor sites forcartilage grafts may include the antihelix and the conchalbowl from one or both ears (Figure 4). Incisions for har-vest may be anterior or posterior. Anterior incisions areeasier for access, but scars are more noticeable than pos-terior incisions. Antihelical cartilage is excellent for long,straight segments, whereas conchal cartilage is ideal forgrafts that demand more curvature and substance.8,9 Sep-tal and costal cartilages may also be harvested to supportlarger defects. However, if the defect is extensive enoughto require more complex lining and structural support, aPFF is often preferred over a CIF. The subject of nasal lin-ing is beyond the scope of this article. General options,however, for smaller mucosal defects (< 1 cm) include (1)a turnover hinge flap, (2) turndown of a forehead flapextension, (3) a full-thickness skin graft (FTSG), and (4)bipedicle vestibular skin advancement flap. Larger liningrestoration may require (1) a turnover forehead flap, (2) aseptal mucoperichondrial hinge flap, (3) a composite sep-tal chondromucosal pivotal flap, and (4) a larger FTSGvascularized by an overlying PFF.10
Figure 4. Anterior approach to auricular cartilage harvesting. Conchalskin is elevated and cartilage with perichondrium is removed forgrafting.
Figure 3. Narrow cutaneous triangle with broader underlyingmyocutaneous pedicle.
Flap Harvest and Pedicle MobilizationThe CIF should overlie the defect without tension (Figure 5).A scoring (superficial) incision to outline the template and itstriangles begins the flap harvest. These shallow marks delin-eate the flap outlines should the pen markings be blurred.Incisions are then carried to the subcutaneous fat, and the dis-tal flap and its distal triangle are undermined sharply to leavea thin layer of subdermal fat. The distal triangle (dog-ear)may either be excised during flap elevation or preserved as anextension, to be used for either additional reach or for grasp-ing during mobilization.
Initial sharp, superficial undermining transitions toblunt, deeper dissection to create a myosubcutaneous ormyocutaneous pedicle. This transition occurs as onereaches the proximal half of the pedicle. Muscle fibers areincorporated into the pedicle whenever possible, but toodeep undermining should be avoided (see Figure 5).Undermining for the CIF is similar to that for an islandpedicle flap at the alar-facial sulcus. As the flap is elevated,hook counter traction to retract the upper cutaneous lipmedially and the cheek laterally will aid in exposure of thelevator muscles, angular artery, and its perforators. TheCIF should reach the defect with no tension. If tensionpersists, then a temporary suspension stitch from themedial cheek to the alar base can lift the CIF to the ala.
Defect PreparationWith the flap reach and pedicle secured, the flap dimen-sion is again compared with the defect plus any plannedsubunit enlargement. Undermining is needed peripheral tothe defect, and wound borders are trimmed. The alardefect requires minimal preparation except for peripheralundermining. Lining and cartilage support should be inplace and wound edges trimmed. Beveled edges should berevised to be perpendicular except for near the alar rim,where a beveled edge is desirable for a smoother approxi-mation with the flap. The CIF’s edge should correspond-ingly be reverse-beveled to fit the distal wound. If possible,
defect corners are angulated, which theoretically mini-mizes trapdoor contraction. Although some excise residualsubunit tissue at the time of flap inset, I defer this step untilstage II (pedicle division), when flap survival may be bet-ter assessed. Only when adequate cover is ensured shouldthe remaining subunit tissue be removed.
Flap Preparation and InsetPrior to any suturing, the flap thickness must be revised tofit the defect. Additional trimming may be needed of theunderlying fat, leaving a thin subdermal layer. Aggressivedebulking to a thin subdermal layer is possible as long asthe pedicle is richly vascularized and other confoundingfactors, such as smoking, are not present. However, unlikethe PFF, the risk of necrosis is present. Notation of pinpointbleeding of the distal flap should be maintained to minimize the risk of flap necrosis. Constant reference to thedefect is mandatory to prevent excessive thinning. Theflap’s leading edge should be reverse-beveled to promote aflush approximation. Flap inset begins with simple or horizontal mattress interrupted epidermal sutures to secureits leading edge with the defect. If dermal buried sutures areplaced, then poliglecaprone 25 (Monocryl, Ethicon,Somerville, NJ, USA) is preferred owing to its minimal tissue reaction, a desirable feature on the sebaceous nose.11
Dermal sutures contribute to flap security and minimizeincision line separation. The proximal flap as it abuts thenasofacial sulcus or a superior aspect of the alar groove isnot sutured until pedicle division.
Donor ClosureThe secondary cheek defect is undermined laterally andclosed in a layered fashion. Lateral tenting of the oralcommissure is common with large donor defects. However,the dynamic strength of the orbicularis oris muscle ensurescorrection of this temporary distortion.
Postoperative Care
Postoperative bleeding at the sides of the exposed pediclemay occur. For hemostasis, the exposed pedicle may bewrapped in Surgicel or Surgicel Nu-Knit (Somerville), anoxidized cellulose gauze. Removal of Surgicel with dress-ing changes causes less discomfort than petrolatumgauze.12 Bacitracin ointment and Xeroform petrolatumgauze (Sherwood Medical, St. Louis, MO, USA) may coverthe remaining sites under a pressure dressing. Often a sim-ple petrolatum or antibiotic ointment layer and routinepressure dressing, removed in 24 hours, will suffice. AXeroform roll may also be fashioned and placed within theaffected nostril as part of a bilayer dressing. This is espe-cially useful if skin grafts were placed internally for lining.Nausea and vomiting, as well as significant pain, are rarewith the CIF. Any discomfort is often associated with thecartilage donor site rather than the flap location. Inspira-tion may seem hampered despite cartilage grafting and is
Dermatol Surg 31:8 Part 2:August 2005 NGUYEN: STAGED INTERPOLATION FLAPS 1037
Figure 5. Flap movement should be without tension. Note arrowhighlighting muscle fibers at base of pedicle.
1038 NGUYEN: STAGED INTERPOLATION FLAPS Dermatol Surg 31:8 Part 2:August 2005
due to the transient surgical edema. Compared with thePFF, patients have substantially fewer lifestyle interrup-tions with the CIF in terms of work, wearing glasses, anddriving. Still, patients should be discharged with a driverto home or to a local residence in the charge of a caretaker,given the CIF’s relative complexity and potential for com-plications. Patients are seen in 5 to 7 days for sutureremoval. A telephone call by the surgeon the night of sur-gery, with emergency contact numbers provided postoper-atively, greatly reassures the patient.
Cheek-to-Nose Interpolation Flap: Stage II
The second stage of pedicle division and inset usually occursafter 3 weeks (Figure 6). Intermediate-stage thinning shouldbe avoided because the pedicle is not as robust as with thePFF. If the flap is fully viable at 3 weeks, then the remainingalar tissue underneath the pedicle may be resected to permitfull subunit repair (Figure 7). All but a 1 to 2 mm rim of thealar base should be preserved (see Figure 7). This alar stumpserves as an anchor for the CIF and maintains the difficultto recreate lateral alar groove. Additional tissue removalshould be mindful of any recently placed cartilage support.Airway patency should again be confirmed. As in stage I, areverse bevel at the flap’s edges (especially at the alar rim)will create a flush fit with the residual defect. Surgical recre-ation of the alar groove, if necessary, should be deferreduntil a third stage. Aggressive thinning of the flap usuallymay be performed in stage II, along with any revisions tocartilage grafts and lining. A third stage may also berequired for additional flap thinning and cartilage grafts ifnecessary. A three-stage approach is also useful for patientsat high risk of flap necrosis.
Although uncommon, flap necrosis is seen more with theCIF than the PFF and is often due to a thin pedicle (subcu-taneous rather than myosubcutaneous pedicle) (Figure 8).Necrosis is usually partial and involves the distal edge (Fig-ure 9). Pedicle division should be deferred for an additional2 weeks and flap viability reassessed. The nonviable tissuemay be gently curetted to determine its depth. If superficial,the wound may heal by second intention. If necrosis isdeeper, then this portion may be trimmed and the proximalflap advanced for replacement provided that adequate flaptissue and mobility remain. Necrosis is not fatal, however,and esthetic recovery may still be possible (Figure 10).
Two postoperative issues pertain to the cheek and melo-labial fold in stage II: too full or too flat. At the time ofpedicle detachment, there may be significant soft tissuecongestion at the flap base, which may result in asymmet-ric fullness of the ipsilateral cheek–melolabial fold. Mostof this swelling resolves with time, but revisions may beneeded. Conversely, if the pedicle base is too close to thealar-facial sulcus, then the natural fullness of this regionmay be asymmetrically flattened with pedicle excision. Ifthe pedicle is properly positioned, then its base should be
divided sharply and not inset into the cheek (Figure 11). Ifthe cheek-fold complex appears too flat, however, thenpartial pedicle inset to restore fullness may be considered.Inevitably, the lower cheek–melolabial fold will be slightlyflatter and less pronounced than the contralateral side.Alar restoration can be exceptional (Figure 12).
After pedicle division, additional revisions may beneeded, such as dermabrasion (6 to 8 weeks from stage I), de-epilation, and contouring. After 8 weeks, however, fur-
Figure 6. Stage II: complete survival at 3 weeks permitting pedicledivision and enlargement of a subunit defect if needed.
Figure 7. Conservation of alar base while excising remainder of alarsubunit.
ther tuning should be deferred for several months to per-mit flap maturity and scar evolution. Early interventionfor self-resolving issues leads only to unnecessary mor-bidity. A functional airway should always be evaluatedprior to any intervention. The CIF and PFF have similarapplications. Factors favoring either the CIF or the PFF
are discussed in Table 1. The CIF is an excellent, althoughless robust, flap than the PFF for paranasal defects.Defects resurfaced with the CIF tend to be smaller, lesscomplex, and more distal (infratip and columella) or lat-eral (ala) than those for the PFF. The CIF demands fewerlifestyle disruptions and donor site morbidity. It may beless suitable, however, in younger patients who do nothave a pronounced melolabial fold because the donor sitescar remains conspicuous for years. A viable alternative to
Dermatol Surg 31:8 Part 2:August 2005 NGUYEN: STAGED INTERPOLATION FLAPS 1039
Figure 8. A fragile pedicle lacking in muscle bulk because of super-ficial dissection.
Figure 9. Partial flap necrosis at distal insertion.
Figure 10. One-year postoperative result of a cheek-to-nose stagedrepair.
Figure 11. Primary closure of donor cheek without inset of pedicle.
1040 NGUYEN: STAGED INTERPOLATION FLAPS Dermatol Surg 31:8 Part 2:August 2005
the CIF for comparable alar defects is a one-stage subcu-taneous hinge flap in combination with full-thickness skingrafting.13–15
Interpolation Flaps for Auricular Defects
Application
Staged interpolation flaps are flexible options for eardefects of varying complexity and location. Wounds alongthe helical rim, ear lobe, antihelix, and conchal bowl mayall be resurfaced with either preauricular or postauricularinterpolation flaps. Interpolation flaps for the ear are oftenreserved for cosmetically sensitive patients or for func-tional restoration. Skin grafts, one-stage flaps, or second-intention healing are often acceptable for others becausethe ear may be partially hidden with longer hair (espe-cially in women). The wearing of glasses or hearing aids isan important consideration in reconstructive counseling.
Anatomy
For behind the ear, retroauricular tributaries of the poste-rior auricular artery serve as a rich blood supply to thepedicle. Preauricular staged flaps rely on branches of thesuperficial temporal or transverse facial artery. These
named arteries are branches of the external carotid andare usually not directly contained within the pedicles. Thevascular supply, therefore, is more analogous to randompattern flaps.
Flap and Pedicle Design
Substantial loss of cartilage can be tolerated withoutadverse sequelae for most ear defects. After all, the ear isan excellent donor site for cartilage grafts in nasal recon-struction. If the primary defect involves complete loss of aportion of the helical rim and a small amount of cartilage,the flap may be folded onto itself to provide adequatethickness and support without a free cartilage graft. Car-tilage replacement, however, may be useful for support ifdesired or necessary for larger defects involving the supe-rior helical dome or convexity, superior helical crus andscapha, or significant portions of the midantihelix. Carti-lage in these cases may restore esthetic contour (helicaldome) and/or structural integrity and stability.
There are many design variations for staged auricularflaps, and these are summarized in Table 2.16–22 Because adiscussion of all variations is not possible in this article,the most common retroauricular interpolation flap (RIF)will be highlighted. This version is most applicable to full-thickness defects along the helical rim, ear lobule, or anti-helix and will nourish cartilage grafts, although rarely nec-essary, if needed. An interesting single-stage version is alsopossible for earlobe recreation.16 The donor site for an RIFis the retroauricular ear, sulcus, and scalp (Figure 13). Theadvantages of the RIP are that the donor scar is easily hid-den, available well-matched tissue is often abundant, andthe vascularity is rich. High esthetic and functional resultsare obtainable.
The total defect is first assessed with respect to theanterior and posterior components of the primary defect.Stage I is aimed at repair of the anterior portion of the pri-mary defect, including the normally noticeable helicalrim. Final restoration of the helical rim and posterior pri-mary defect is accomplished at stage II. A template of theanterior defect and normally noticeable helical rim ismade in a fashion similar to the CIF. Alternatively, theauricle may be pressed against the scalp and the verticallength of the flap outlined. The template is placed in thepostauricular sulcus, usually with the anterior marginencompassing a small portion of the posterior ear skinwith a typical excellent color and thickness match. Theposterior ear, postauricular sulcus, and scalp skin usuallyprovide an excellent tissue match for ear defects (Figure 14).Care should be taken to prevent designing the flap toincorporate terminal scalp hair into the planned earreconstruction. For those with a hairline to the sulcus,other options, including a preauricular approach or otherreconstructive options, are best.
Figure 12. One-year postoperative result of cheek-to-ala stagedrepair.
Dermatol Surg 31:8 Part 2:August 2005 NGUYEN: STAGED INTERPOLATION FLAPS 1041
Anesthesia
Local anesthesia infiltration will suffice, and no adjunctivesedation is necessary in most patients.
Execution
Flap Harvest and Pedicle MobilizationAfter measuring and outlining the RIF, an incision ismade along the length (anterior leading border) of theflap. At both ends of this incision, perpendicular inci-sions are made through the retroauricular skin to thehairline if necessary, slightly widening the pedicle base asthe incisions extend posteriorly toward the scalp. Abridge of skin should remain between the primary andsecondary defect to prevent these two defects from gran-ulating together while waiting for stage II (see Figure 14).The flap is incised to ear perichondrium, sulcus, and
scalp subcutaneous fat or fascia. Carrying the dissectionto the fascia at the pedicle base ensures a rich blood sup-ply to the flap tip.
The flap is then elevated and transposed into the pri-mary defect. The secondary and primary anterior helicaldefect margins require only slight undermining to provideincreased flap mobility. The distal flap may be thinned ifneeded but is often not necessary owing to an excellentthickness match. After meticulous hemostasis, the flap istransposed into the primary anterior helical defect to thejunction of the usually non-noticeable posterior helicalrim-noticeable anterior rim. The RIF should reach thedefect with minimal to no tension.
Defect PreparationNo special defect preparation is normally required. Simi-lar to the CIF, beveled edges should be revised to be per-pendicular. If possible, defect corners are angulated, whichmay benefit final cosmesis.
Table 1. Comparison between the Cheek Interpolation Flap and the Paramedian Forehead Flap
Parameters Cheek Interpolation Flap (CIF) Paramedian Forehead Flap (PFF)
Applications Alar defects, columella, nasal sill. Nasal tip Nasal tip, infratip, ala. Less ideal: and dorsum wounds are better repaired nasal sidewall and dorsum,with the PFF. periorbital
Smaller defects, less complex Larger defects, multiple subunits
Pedicle creation and vascularity Tributaries of angular artery (not artery itself) Contains supratrochlear artery andand muscle perforators its tributaries. Dorsal nasal artery
Pedicle can be more difficult to develop as secondary blood supply.Vascularity less reliable, and flap is at more Vessel predictably identifiable and
risk in smokers more easily preservedVascularity robust, permitting
intermediate-stage revisions andlining with skin grafts
Postoperative morbidity Patients may wear glasses, drive Wearing glasses difficult withoutWork may be possible customized appliancesLess postoperative pain Work continuation unlikelyNausea, headache, and vomiting Pain is variable, often related to
are unusual cartilage donor siteHeadache, nausea, and vomiting
are uncommon but seen more with PFF than CIF
Cartilage grafts Nasal valve patency must be preserved Nasal valve patency must beCartilage needed in most alar repairs preserved
to balance contraction forces of healing Cartilage need will vary
Patient limitations Younger patients with less pronounced melolabial Vertical forehead height folds may have more visible donor scar determines reach to defect and
Terminal hair transfer more likely in men from is highly individualizedhair-bearing medial cheek Terminal hair transfer variable
depending on height of PFFdesign and degree of frontal scalp hair density
Flap Preparation and InsetPrior to any suturing, the flap is trimmed and thinned ifneeded for a perfect fit. The RIF drapes into the defect, andseveral interrupted epidermal sutures may be used to alignthe flap. Vertical or horizontal mattress sutures at the rimare essential for maximal eversion (Figure 15). The flap isthen sutured into the remaining anterior and helical rimportion of the primary defect in a manner similar to theCIF. Subcutaneous sutures are rarely needed. If a promi-nent helical rim curl exists, a few basting sutures at theantihelical groove should be considered to recreate thisnatural sulcus. Basting sutures placed during stage I can
usually be done without risk of necrosis owing to the richblood supply to the RIF.
Donor ClosureThe donor site requires no closure. Insertion of packingwith gauze described for the CIF is inserted into thepostauricular tunnel for hemostasis, comfort, and preven-tion of the primary to secondary defect wounds healing toone another. The packing is usually changed weekly.
Postoperative Care
Wound care is straightforward and similar to the CIF. Inplacing the postoperative dressing, the concavities around
1042 NGUYEN: STAGED INTERPOLATION FLAPS Dermatol Surg 31:8 Part 2:August 2005
Figure 13. Donor site for a staged retroauricular flap: the postau-ricular ear, sulcus, and scalp. The vertical height of the flap equalsthat of the defect on the helical rim. Courtesy of Tim Johnson, MD,Ann Arbor, MI.
Table 2. Auricular Interpolation Flaps
Design Comment References
Retroauricular to auricular flap Postauricular skin/mastoid flap is elevated to cover a helical rim 16, 17or antihelix defect
Ear is “pinned” posteriorly by flap until time of pedicle divisionRetroauricular pull-through flap Postauricular skin flap is pulled through an incision or existing 18, 19
defect to cover the anterior ear defectSome designs may be performed as one stage
Preauricular two-stage banner Preauricular cheek flap is transposed onto a lower helical rim or 15transposition flap earlobe defect
Preauricular donor skin is more abundant compared with postauricular skin
Tubed postauricular interpolation For helical rim defects with cartilage intact 20, 21flap Three-stage flap with 3 wk between each stage
Stage I (elevation): postauricular skin is harvested as a tube with pedicle attachments at both ends
Stage II (partial inset): tube is detached at one end and freed end is attached to helical rim defect
Stage III (complete inset): remaining end detached and sutured to defect
Figure 14. Flap inset with a skin bridge between the primary andsecondary defect. Note the mattress sutures at the helical rim formaximal eversion. Courtesy of Tim Johnson, MD, Ann Arbor, MI.
the ear and flap should be carefully padded with soft gauzeto create an even plane of pressure. A circumferential Ker-lix wrap (Kendall, Mansfield, MA, USA) is often useful tocomplete and secure the dressing. The dressing is removedin 24 hours, and the patient can bathe daily and wearglasses. The small 5-0 or 6-0 monofilament nonabsorbablesutures may remain in place until stage II without devel-opment of track marks or irritation if desired for addedflap security and ease.
RIF: Stage II
At 3 to 4 weeks, division of the pedicle is made at a point foradequate posterior primary defect coverage, thinned, curledover the helical rim, and sutured into the posterior margin ofthe primary defect (see Figure 15). Often this is not necessarybecause the posterior portion of the primary defect is usuallygranulating well. The remaining pedicle may be severed orreset into the secondary defect and sutured. Alternatively, thesecondary defect may be left to granulate. Additional revi-sion steps are rarely required with the RIF.
Final Perspectives
The RIF is an effective repair that has relatively little oper-ative morbidity. Given the abundant reservoir of postau-ricular and scalp tissue with a hairless zone in manypatients, defect coverage is ensured and donor site mor-bidity is negligible (Figure 16). The vascular pedicle forthis flap is random based, but flap necrosis is rare. Thefirst stage results in a natural-appearing ear, with themajority of the flap camouflaged behind the ear, minimiz-ing the patient’s self-consciousness and distortion that arenoted with other staged interpolation flaps (Figure 17).
Dermatol Surg 31:8 Part 2:August 2005 NGUYEN: STAGED INTERPOLATION FLAPS 1043
Figure 15. Stage II retroauricular flap: pedicle divided at a lengthsufficient to cover any remaining posterior helical wound. Anyresidual defect at the donor site heals by second intention. Cour-tesy of Tim Johnson, MD, Ann Arbor, MI.
Figure 16. Short-term postoperative result. Note excellent healingof the donor site. Courtesy of Tim Johnson, MD, Ann Arbor, MI.
Figure 17. (A and B) Long-term postoperative results. The contour,substance, and integrity of the helical rim have been maintained,and the cosmesis is excellent.
A
B
Variations of the RIF may be performed; other designs arementioned in Table 2 (Figures 18 and 19).
Conclusion
Staged pedicle flaps are priceless options for facial recon-struction. They enable both functional and esthetic repairsof difficult and large defects. These flaps cannot be per-formed without forethought for underlying infrastructure,such as cartilage and lining, especially for nasal wounds.Cutaneous surgeons involved with skin cancer are fullycapable of their execution and, in fact, have made sub-stantial contributions to the refinement of the aforemen-tioned repairs. Nuances in interpolation flap design sig-nificantly impact final outcome, and a careful study of theabove details is essential for success.
References1. Sherris DA, Fuerstenberg J, Danahey D, Hilger PA. Reconstruction
of the nasal columella. Arch Facial Plast Surg 2002;4:42–6.2. Burget GC, Menick FG. The paramedian forehead flap. In: Burget
GC, Menick FG, editors. Aesthetic nasal reconstruction. St. Louis:Mosby; 1994. p. 57–91.
3. Boyd CM, Baker SR, Fader DJ, et al. The forehead flap for nasalreconstruction. Arch Dermatol 2000;136:1365–70.
4. Quatela VC, Sherris DA, Rounds MF. Esthetic refinements in fore-head flap nasal reconstruction. Arch Otolaryngol Head Neck Surg1995;121:1106–13.
5. Fader DJ, Baker SR, Johnson TM. The staged cheek-to-nose inter-polation flap for reconstruction of the nasal alar rim/lobule. J AmAcad Dermatol 1997;37:614–9.
6. Baker SR, Johnson TM, Nelson BR. The importance of maintain-ing the alar-facial sulcus in nasal reconstruction. Arch OtolaryngolHead Neck Surg 1995;121:617–22.
7. Burget GC, Menick FG. The superiorly based nasolabial flap: tech-nical details. In: Burget GC, Menick FG, editors. Aesthetic nasalreconstruction. St. Louis: Mosby; 1994. p. 93–115.
8. Ratner D, Skouge JW. Surgical pearl: the use of free cartilage graftsin nasal alar reconstruction. J Am Acad Dermatol 1997;36:622–4.
9. Byrd DR, Otley CC, Nguyen TH. Alar batten cartilage grafting innasal reconstruction: functional and cosmetic results. J Am AcadDermatol 2000;43(5 Pt 1):833–6.
10. Baker SR. Internal lining. In: Baker SR, Naficy S, editors. Principlesof nasal reconstruction. St. Louis: Mosby; 2002. p. 31–46.
11. Molea G, Schonauer F, Bifulco G, D’Angelo D. Comparative studyon biocompatibility and absorption times of three absorbablemonofilament suture materials (polydioxanone, poliglecaprone 25,glycomer 631). Br J Plast Surg 2000;53:137–41.
12. Shinkwin CA, Beasley N, Simo R, et al. Evaluation of Surgicel Nu-knit, Merocel and Vasoline gauze nasal packs: a randomized trial.Rhinology 1996;34:41–3.
13. Baker SR. Subcutaneous hinge cheek flaps. In: Baker SR, Naficy S,editors. Principles of nasal reconstruction. St. Louis: Mosby; 2002.p. 144–52.
14. Johnson TM, Baker SR, Brown MD, Nelson BR. Utility of the sub-cutaneous hinge flap in nasal reconstruction. J Am Acad Dermatol1994;30:459–66.
15. Menick FJ. A 10-year experience in nasal reconstruction with thethree-stage forehead flap. Plast Reconstr Surg 2002;109:1839–55;discussion 1856–61.
1044 NGUYEN: STAGED INTERPOLATION FLAPS Dermatol Surg 31:8 Part 2:August 2005
Figure 19. (A and B) Complete flap survival and match at the timeof stage II.
Figure 18. Variation (pull-through) of a retroauricular flap for ascaphoid fossa and antihelical defect. Courtesy of Tim Johnson, MD,Ann Arbor, MI.
B
A
Dermatol Surg 31:8 Part 2:August 2005 NGUYEN: STAGED INTERPOLATION FLAPS 1045
16. Tanner D, Leshin B. Utility of a bilayered transposition flap inreconstruction of lower third of the pinna. Dermatol Surg2000;26:687–9.
17. Johnson TM, Fader DJ. The staged retroauricular to auriculardirect pedicle (interpolation) flap for helical ear reconstruction. JAm Acad Dermatol 1997;37:975–8.
18. Butler CE. Extended retroauricular advancement flap reconstruc-tion of a full-thickness auricular defect including posteromedial andretroauricular skin. Ann Plast Surg 2002;49:317–21.
19. Azaria R, Amir A, Hauben DJ. Anterior conchal reconstructionusing a posteroauricular pull-through transpositional flap. PlastReconstr Surg 2004;113:2071–5.
20. Zenn MR. Helical advancement with a posterior auricular pull-through flap: a technique for reconstruction of combined helicaland scaphal defects. Aesthetic Plast Surg 1999;23:131–3.
21. Di Mascio D, Castagnetti F. Tubed flap interpolation in reconstruc-tion of helical and ear lobe defects. Dermatol Surg 2004;30(4 Pt1):572–8.
22. Field LM. The preauricular tubed pedicle flap. J Dermatol SurgOncol 1989;15:614–8.