Papageorgiou SN. Meta-analysis for orthodontists: Part I – How to choose effect measure and...
Transcript of Papageorgiou SN. Meta-analysis for orthodontists: Part I – How to choose effect measure and...
Meta-analysis for orthodontists: Part I – How tochoose effect measure and statistical modelSpyridon N. Papageorgiou1,2
1Department of Orthodontics; 2Department of Oral Technology, School of Dentistry, University of Bonn, Bonn, Germany
Systematic reviews ideally provide a comprehensive and unbiased summary of existing evidence from clinical studies,
whilst meta-analysis combines the results of these studies to produce an overall estimate. Collectively, this makes them
invaluable for clinical decision-making. Although the number of published systematic reviews and meta-analyses in
orthodontics has increased, questions are often raised about their methodological soundness. In this primer, the first
steps of meta-analysis are discussed, namely the choice of an effect measure to express the results of included studies,
and the choice of a statistical model for the meta-analysis. Clinical orthodontic examples are given to explain the
various options available, the thought process behind the choice between them and their interpretation.
Key words: Effect measure, orthodontics, meta-analysis, fixed-effect, random-effects
Received 2 March 2014; accepted 5 June 2014
Introduction
Systematic reviews summarise qualitatively the results of
multiple studies, providing the highest grade of evidence
to develop clinical guidelines. Meta-analysis goes one step
further, to the quantitative synthesis of studies in order to
provide an overall summary. Although the number of
published systematic reviews and meta-analyses in
orthodontics has increased, questions about the metho-
dological soundness of some have been raised.
In this paper, the first steps of meta-analysis will be
discussed in the context of: (1) the choice of an effect
measure to express the results of included studies and (2)
selection of an appropriate model for subsequent statistical
synthesis. For readers not familiar with meta-analysis, a
short description of the forest plot and of between-study
heterogeneity will also be given. Meta-analyses will be
covered that compare two groups; either an intervention
group versus a placebo/control group or an intervention
group versus another intervention group. Meta-analyses of
data from a single group (i.e. event rates, means of groups,
etc.), meta-analyses of diagnostic accuracy or network
meta-analyses will not be covered. Furthermore, emphasis
will be given on basic principles, which can be easily
applied in the freely-available program Review Manager
(RevMan) (Review Manager, 2012) available from the
Cochrane Collaboration.
It is beyond the scope of this article to analytically
describe the stages of a systematic review and when it is
sensible to perform a meta-analysis or not. Interested
readers should refer to the Cochrane Handbook for
Systematic Reviews of Interventions (Higgins and
Green, 2011) and to the PRISMA statement (Preferred
Reporting Items for Systematic Reviews and Meta-
Analyses) (Liberati et al., 2009), where further details
can be found on how to respectively conduct and reportsystematic reviews and meta-analyses.
Effect measuresThe first step in meta-analysis is to identify all relevant
studies evaluating the same measure in order to directlycompare and eventually synthesise them. There are a
wide array of effect measures that can be used, but this
paper will focus on five of the most common:
(i) those for continuous outcomes (such as ANBangle): mean difference (MD) (also known as
difference in the means) and standardised mean
difference (SMD),
(ii) those for binary (dichotomous) outcomes (such as
bracket failure): odds ratio (OR), relative risk
(RR) (also known as risk ratio) and risk difference
(RD) (also known as absolute risk reduction).
Continuous outcomes
Effect measures. If all included studies measure the same
continuous outcome and use the same measurement
INVITATION TO SUBMIT Journal of Orthodontics, Vol. 41, 2014, 317–326
Address for correspondence: Spyridon N. Papageorgiou, DDS,
Department of Orthodontics, School of Dentistry, University of
Bonn, Welschnonnenstr. 17, 53111, Bonn, Germany.
Email: [email protected]# 2014 British Orthodontic Society DOI 10.1179/1465313314Y.0000000111
scale, then the obvious effect measure to use is the MD,
which is the mean of the intervention group minus
the mean of the control group in each study (or vice
versa):
MD~Meanintervention{Meancontrol,
and has the same units as the outcome measured.
If all included studies measure the same continuous
outcome, but do not use the same measurement scale,
then there are two options. The first is to convert the
data, so that all results are on the same scale. If this is
not possible, then the SMD can be used. This is the MD
standardised (adjusted) by the units of the standard
deviation. There are many standardised effect measures
(Cohen’s d, Hedge’s g, Glass’s d, etc.) (Borenstein et al.,
2008), but this paper will focus on Hedge’s g, which
includes an adjustment for small sample bias and is used
by default in RevMan. SMD does not have the same
units as any of the original scales, but is measured in
standardised measurement units. Both the MD and
SMD are absolute comparative measures and, if MD 5
0 or SMD 5 0, then there is no difference between the
two compared groups.
SMD~Meanintervention{Meanintervention
Pooled standard deviation of both groups
Interpretation. In order to illustrate the differences
between these two measures, suppose we have a meta-
analysis of four randomised controlled trials, where
patients are allocated either to a bite-wafer group or
to a non-wafer group during debonding and perception of
pain is measured by means of a questionnaire. Let us say
that all the trials measured pain with a Visual Analogue
Scale (VAS) (Huskisson, 1974), where a horizontal
100 mm line is plotted with ‘no pain’ on the left and
‘worst pain imaginable’ on the right and the patients
quantify their pain experience on this line. If we find an
MDwafer–control of 210 mm, this means that ‘on average,
patients allocated to the wafer group experienced less pain
during debonding by 10 mm in the VAS scale compared to
patients allocated to the control group’ or alternatively ‘on
average, the bite-wafer reduced pain during debonding by
10 mm in the VAS scale’. You will notice the word ‘on
average’. This means that we are talking about differences
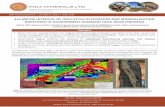
in means (Figure 1) and that not all the wafer patients
experienced less pain than the control patients (hence the
overlap between the curves).
However, if two out of the four trials measured pain
with a VAS scale (in mm) and the other two trials
measured pain with a Likert scale (Likert, 1932) (where
pain is measured in a 5-level scale with a score up to 5)
then the MD cannot be used. In this case, the SMD can
be used for the meta-analysis. If by combining all
four trials using the SMD as a measure, we find a
SMDwafer–control of 20.5, this means that ‘on average,
patients allocated to the wafer group experienced less pain
during debonding by 0.5 standardised measurement units
compared to the patients allocated to the control group’.
One will notice that the interpretation of the effect
measure will depend upon several factors, including the
direction of the scale (higher VAS 5 more pain), the
length of the scale (for VAS, 0 to 100 mm), the minimally
important difference (clinical judgement) and if the
outcome is beneficial (for example, mandibular growth)
or harmful (for example, pain). The interpretation of
SMD is not straightforward and it often makes sense to
back-transform the resulting SMD in one of the original
scales to communicate the results (here, either the VAS or
the Likert scale).
Data needed. For any continuous outcome, indepen-
dently of whether the MD or the SMD is to be used, the
following data are needed: the sample size, the mean and a
measure of variation (standard deviation or standard
error) for both the intervention and the control group.
Many other data formats can be used for data input in
meta-analysis (P, t value, median, interquartile range,
MD, ratio of means, ratio of geometric means), but these
go beyond the scope of this article. It is important also
to know that the SMD does not correct for different
directions among scales. If the used scales run in different
directions, you have to alter the direction of the results, by
multiplying with 21. Finally, conventional meta-analysis
methods rely on the broad assumption that the results are
normally distributed. If concrete indications of skewness
Figure 1 Illustration of the mean difference based on thedescribed fictional bite-wafer trial. The left distributiondepicts the pain experienced during debonding from thepatients in the wafer group and the right distribution depictsthe pain experienced during debonding from the patients inthe control group
318 Papageorgiou Invitation to Submit JO December 2014
are found, it is advisable to get formal statistical advice
before proceeding.
Binary outcomes
Effect measures. For binary outcomes, the three most
widely-used measures are the OR, the RR, and the RD. In
order to understand these three measures, we need to
introduce the concepts of odds and risks. Suppose we have
a fictional randomised controlled trial, where 100 patients
with a class II malocclusion and increased overjet are
allocated either to an early-phase Twin Block treatment orto an untreated control group (to then be treated com-
prehensively later). The measured outcome is the inci-
dence of new incisal trauma, measured as trauma or no
trauma. We can see the results of this trial in the form of a
262 contingency table, which provides the standard data
needed to input binary outcomes for meta-analysis
(Table 1) and includes the events and sample size of
each group. According to the results, 12/50 (24%) of thetreated patients and 24/50 (48%) of the control patients
experienced some kind of incisal trauma during the
follow-up.
If we express the trauma experience in both groups
with odds, then:
N The odds of trauma in the Twin Block group are:
OddsTwin Block~EventsTwin Block
No-eventsTwin Block
~12
38~0:316 or 31:6%
N The odds of trauma in the control group are:
Oddscontrol~Eventscontrol
No-eventscontrol~
24
26~0:923 or 92:3%
N And the OR is simply the ratio of the odds for the two
groups:
OR~OddsTwin Block
Oddscontrol~
0:316
0:923~0:342
Expressed as risks (or probabilities), the same results
will be:
N The risk of trauma in the Twin Block group is:
RiskTwin Block~EventsTwin Block
SampleTwin Block
~12
50~0:240 or 24%
N The risk of trauma in the control group is:
Riskcontrol~Eventscontrol
Samplecontrol~
24
50~0:480 or 48%
N And the RR is simply the ratio of the risks for the two
groups:
RR~RiskTwin Block
Riskcontrol~
0:240
0:480~0:500
N Finally, the RD is the difference of the risks for the
two groups:
RD~RiskTwin Block{Riskcontrol
~0:240{0:480~{0:240 or {24:0%
Another illustrative measure for binary outcomes is the
Number Needed to Treat (NNT); however, this cannot
be directly used in the meta-analysis. Rather, the results
from the other measures have to be converted in the
NNT. NNT gives the number of patients you would have
to treat with the intervention (instead of leaving them
untreated) to prevent one additional event and is there-fore, very helpful for the clinical translation of results.
N The NNT is traditionally calculated as the reciprocal
of the RD, so in our example:
NNT~1
RD~
1
0:240~4:17,
which is always rounded up to the next number, so 5:
However, this assumes a constant RR (meaning that
the benefits/harms of a treatment are the same among
both low-risk and high-risk patients); but this is a bigassumption (Sackett et al., 1997). The aim of evidence-
based medicine is to individualise existing clinical knowl-
edge in order to satisfy the needs and preferences of each
individual patient (Glasziou et al., 1998).
Table 1 Fictional data for a randomised controlled trial, where 100 patients are allocated to either a Twin Block treatment or to an
untreated control group in order to avoid incisal trauma
Event (trauma) No event (no trauma) Total
Intervention (Twin Block) 12 38 50
Control (untreated) 24 26 50
Total 36 64 50
JO December 2014 Invitation to Submit Choice of effect and model in meta-analysis 319
N Therefore, Furukawa et al. (2002) proposed the
calculation of an individualised NNT based on the
Patient’s Expected Event Rate (PEER) and either
the RR or the OR:
NNT~1
PEER|(1{RR)or
NNT~1{PEERzOR|PEER
PEER|(1{OR)|(1{PEER)
Therefore, suppose we want to calculate the NNT for
two patient examples: (a) for a quiet late-adolescent
patient with increased overjet and a PEER for trauma of
0.3 (low-risk patient) and (b) for a rather energetic pre-
adolescent patient, who plays rugby and has a PEER for
trauma of 0.6 (high-risk patient).
N For the low-risk group we would have:
NNTlow risk~1
0:3|(1{0:5)~
1
0:3|0:5
~1
0:15~6:67 rounded up to 7:
N And for the high-risk group we would have:
NNThigh risk~1
0:6|(1{0:5)~
1
0:6|0:5
~1
0:3~3:33, rounded up to 4:
Interpretation. The interpretation of the four measures is
quite different. First of all, one must bear in mind that the
OR and the RR are relative measures, while the RD and
NNT are absolute measures. This means that for the
interpretation of the OR and the RR, we need to subtract
the calculated value from the no-effect value, which is OR
5 1 or RR 5 1:
N OR{1~0:342{1:000~{0:658 or 265.8%
This means that ‘the odds of trauma among patients
treated with Twin Block were reduced by 65.8% compared
to the odds among the control patients’ or ‘Twin Block
treatment reduced the odds of trauma by 65.8% of the
odds in untreated patients’.
N RR{1~0:500{1:000~{0:500 or 250.0%
This means that ‘the trauma risk of patients treated with
Twin Block was reduced by 50% compared to the risk of
untreated patients’ or that ‘Twin Block treatment reduced
the risk of trauma by 50% of the trauma risk in untreated
patients’.
For the interpretation of RD, no subtraction is
needed, so the interpretation would be that:
N ‘on average, patients treated with Twin Block had 24%
lower risk of trauma’ or ‘Twin Block treatment reduced
the trauma risk by 24 percentage points’
Finally, the interpretation of the individualised NNTs, is
that:
N ‘one would have to treat four high-risk patients or seven
low-risk patients with increased overjet with a Twin
Block, instead of leaving them untreated, in order to
prevent one new case of incisal trauma’.
How to choose a summary measure? Ideally, a summary
measure should have consistency, desirable mathematical
properties and ease of interpretation (Higgins and Green,
2011). A summary of the introduced effect measures is
provided in Table 2. The choice of a summary measure
for the meta-analysis of continuous outcomes is straight-
forward. In contrast, the choice of a measure for binary
outcomes has been the focal point of much discussion.
However, the selection of an effect measure for meta-
analysis should be based on empirical evidence (Walter,
2000) and not solely on theoretical or statistical
grounds. According to existing empirical studies
(Engels et al., 2000; Deeks, 2002; Furukawa et al.,
2002), the following recommendations can be made
about the choice of effect measure for binary outcomes:
(i) the use of RD should be avoided,
(ii) the RR for harm (i.e. incidence of incisal trauma)
is preferable to the use of RR for benefit
(avoidance of incisal trauma),
(iii) a convenient approach is to use the RR for the
statistical pooling and then use the patient’s
expected event rate to individualise the NNT for
application into practice.
Many researchers prefer to use OR as a measure in meta-
analysis on the grounds that it is often reported as
adjusted OR resulting from a logistic regression. How-
ever, there exist also several methods to calculate adjusted
RRs [Mantel–Haenszel method, log-binomial regres-
sion, Poisson regression with robust standard error, etc.
(McNutt et al., 2003; Greenland, 2004; Knol, 2012)].
Adding to that, statisticians argue that the OR might not
be the most suitable measure to express the results of
interventional trials or systematic reviews of such trials
(Fleiss, 1981; Sinclair and Braken, 1994; Feinstein, 1999).
For case-control studies and logistic regression, the use of
ORs is inevitable, as the OR is the best estimate of RR
that can be obtained (Deeks, 1998). However, the use of
OR should be avoided in cohort or randomised studies
320 Papageorgiou Invitation to Submit JO December 2014
(Sackett et al., 1996; Knol, 2012). Grimes and Shulz (2008)
advocate the use of RRs for epidemiological studies
together with the corresponding Confidence Intervals
(CIs), whenever possible. In both clinical trials and sys-
tematic reviews of trials there is no reason for compromis-
ing interpretation by reporting results in odds rather than
risks (Sinclair and Bracken, 1994; Sackett et al., 1996).
Finally, it is crucial for the reader to understand that every
estimate (continuous or binary) from any study is
uncertain, and should be always presented with a CI.
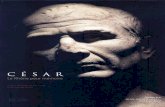
Reading a forest plotBefore advancing from expressing all studies in the same
measure to the statistical pooling of measures, we need
to take a look at the forest plot, which is the standard
graphical output of a meta-analysis. A forest plot from a
Cochrane systematic review (Thiruvenkatachari et al.,
2013) is replicated in Figure 2, highlighting its various
components. In this meta-analysis, three randomised
controlled studies are pooled, which allocated patients
to functional appliance treatment or to an untreated
control group and measured the patients’ ANB angle
post-treatment. As can be seen, the raw data from each
study (left) are re-expressed with the effect measure
(right) and then all effect measures are pooled across
studies (middle). This summary estimate is depicted as a
diamond at the bottom of the forest plot. In this data
synthesis, weights are assigned to the studies, according
to the model that is used (here fixed-effect model):
Table 2 Summary of the three assessed effect measures for binary outcomes
Odds ratio (OR) Relative risk (RR) Risk difference (RD)
Characteristics Definition Odda/Oddb Riska/Riskb Riska–Riskb
Range 1/‘ to ‘ 0 to ‘ 21 to 1
No-effect value 1 1 0
Consistency (similar
despite variation in
baseline risk)
(z) Yes (z) Yes (2) No
Mathematical
properties
Bounded (z) No (2) Yes (as risks range
0 to 1); switching event
and no-event can avoid
this problem
(2) Yes (risks
range 0 to 1)
Collapsibility (calculated
effect is unaffected
by adjustments)
(2) No (z) Yes (2) No
Constrained predictions (2) Yes; absolute benefit
when control group event
rate is 0 and 100%
– –
Relatively homogenous (z) Yes (z) Yes (2) Less homogenous
than OR and RR
(Engels et al., 2000;
Deeks, 2002)
Simple variance estimator (z) Yes (z) Yes (2) No
Symmetry (Effectevent
and effectno-event are
symmetrical)
(z) Yes (reciprocal) (2) No (z) Yes (change of sign)
Other (2) Does not approximate
well the RR with event
rates greater than 10–15%
(Altman et al., 1998)
(2) Can behave paradoxically
with chained or conditional
probabilities, in which case
the RR is more transparent
(Newcombe, 2006)
– –
Interpretation Easily understood (2) No; often misinterpreted
as RR by authors and readers
(Sackett et al., 1996)
(z) Yes (z) Yes
JO December 2014 Invitation to Submit Choice of effect and model in meta-analysis 321
Weightfixed�effect~1
variance
Then the pooled summary estimate is:
Pooled effect~sum of (estimate|weight)
sum of weights
Heterogeneity between studiesAs we can see from the forest plot (Figure 2), even
though the studies have similar intervention and control
groups, the effect estimates (here the MDs) vary across
them, a phenomenon termed between-study heterogeneity.Sources for this variation between the study results can
include clinical diversity (regarding patients, interventions
or outcomes), methodological differences (variation in
study design, conduct, attrition, etc.) or statistical hetero-
geneity (variability that could be expected entirely from
chance). Heterogeneity can be ‘eyeballed’ from the overlap
of the 95% CIs across studies. If the 95% CIs of the studies
have poor overlap, this generally indicates the presence
of heterogeneity. There are more sophisticated ways to
identify and quantify heterogeneity (Higgins and Green,
2011), but they will not be discussed here. However, it is
important to know that heterogeneity plays a major role
in meta-analysis. As can be logically expected, extreme
heterogeneity between studies can make them incompatible
with each other. When extreme heterogeneity exists, one can
choose to:
1. check the data again (for mistakes in the data
extraction or data input);
2. not to pool at all the studies;
3. ignore the heterogeneity (not advisable);
4. exclude outlying studies from the analysis (not
advisable);
5. change effect measure (not advisable);
6. encompass heterogeneity with a random-effects model;
Figure 2 Example of a meta-analysis forest plot including its various components. CI, confidence interval; N, sample size; SD,standard deviation; UK, United Kingdom; H0, null hypothesis; MD, mean difference; SMD, standardised mean difference; RD, riskdifference; RR, risk ratio; OR, odds ratio
322 Papageorgiou Invitation to Submit JO December 2014
7. explore sources of heterogeneity that can explain thevariability (subgroup analysis, meta-regression, etc).
Finally, the role of heterogeneity in the meta-analysis
depends heavily on the statistical model that is used.
Statistical model for the meta-analysisThere are two main models used in meta-analysis: the
fixed-effect model and the random-effects model. These
two models rely on different assumptions and are
fundamentally different, both in the synthesis and their
interpretation.
A fixed-effect model is based on the assumption that
every study is evaluating a common (‘fixed’) treatment
effect. This means that the effect of treatment is the same in
all studies. To put it simply, the only difference betweenthe identified studies is the random error (sampling
variation) and if all studies had an infinitely large sample
of patients, they would also yield identical results. The
pooled diamond in the fixed-effect meta-analysis repre-
sents this one ‘fixed’ treatment effect and the 95% CI
represents how uncertain we are about the estimate. In this
model our goal is to compute the common effect measure
for the identified population, and not to generalise to otherpopulations. It should be clear, however, that this situation
is relatively rare. The vast majority of cases will more
closely resemble those discussed immediately below.
A random-effects model does not assume that one
‘fixed’ treatment effect really exists. Under this model,
proposed by DerSimonian and Laird (DerSimonian and
Laird, 1986), the true treatment effects in the individual
studies may be different from each other. Between-studyheterogeneity is incorporated into the weight assigned to
each study:
Weightrandom-effects~1
variancezheterogeneity parameter
In this case the meta-analysis does not calculate a singleestimate, but rather a distribution of treatment effects
(usually assumed to be normally-distributed). That means
that the diamond in the random-effects meta-analysis
represents the mean and the dispersion of the different
treatment effects and not a single ‘fixed’ treatment effect.
Additionally, 95% predictive intervals should always be
calculated for random-effects meta-analyses (Higgins
et al., 2009). These predictive intervals incorporate iden-tified heterogeneity and answer the question: ‘based on
existing evidence, what effect can I expect my treatment
to have in a future application?’ by providing a range of
plausible effects. However, the calculation of predictive
intervals for the random-effects model is not currently
available in RevMan (possibly to be incorporated in a
forthcoming release) and one must use another statistical
package or perform it manually.
There are many methods to calculate and pool effect
measures in RevMan. For the fixed-effect model, the
inverse variance method is a straightforward method that
can be used generally in most situations by weighing
studies according to their precision (the reciprocal of
variance). The Mantel–Haenszel method (Mantel and
Haenszel, 1959; Greenland and Robins, 1985) is a good
method for reviews with few events or small studies
(default method in RevMan). For ORs, there is also the
Peto method (Yusuf et al., 1985), which is a good method
for studies with few events, small effects (OR close to 1)
and similar numbers in the experimental and control
group. For the random-effects model there are two
options (Mantel–Haenszel and inverse variance), but the
difference between them is trivial.
Comparing the results of the two models, the fixed-
effect model gives almost always, narrower CIs for the
pooled estimate than the random-effects model.
Additionally, as under the fixed-effect assumption the
random error is the only source of variability, large and
more precise studies are given more weight with this
model than with the random-effects model. As stated
before, the results of the two models are heavily
influenced by the existence of heterogeneity. When no
heterogeneity is identified, both models give relatively
similar results. However, when heterogeneity is present,
then a random-effects model is much more conservative
compared to a fixed-effect model (wider CIs and larger P
values). The two models also differ, when the meta-
analysis results are related to study size (Papageorgiou
et al., 2014a), as the random-effects model gives relatively
more weight to smaller studies.
In practice, people tend to interpret both models simi-
larly, which is wrong. To illustrate the different interpreta-
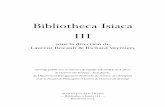
tion of the two models, the abovementioned meta-analysis
from Figure 2 is replicated in a simplified form in Figure 3,
both with fixed-effect and random-effects models. The
pooled diamonds for the two meta-analyses are graphi-
cally ‘augmented’ to illustrate the thought process behind
them. In the upper meta-analysis, where a fixed-effect
model is used, we would interpret the results as follows:
(i) functional appliance treatment has exactly the
same effect on the ANB angle in every included
clinical setting (one ‘fixed’ distribution),
(ii) our best estimate of this effect is an average
reduction in ANB angle of 0.89u compared to
untreated patients.
In the lower analysis, where a random-effects model is
used, our interpretation would be the following:
JO December 2014 Invitation to Submit Choice of effect and model in meta-analysis 323
(i) the effect of functional appliance treatment varies
among the included clinical settings (different
distributions),
(ii) the average of the various effects is a reduction in
ANB angle of 1.35u compared to untreated patients.
Comparing the two models, we see that with the random-
effects model:
(i) less weight is given to the biggest study (Florida
1998 study) than with the fixed-effect model,
(ii) the 95% CI of the overall estimate is wider than
with the fixed-effect model,
(iii) the MD moves more to the left compared to the
fixed-effect model, as the imprecise UK 2009
study influences the results more and finally
(iv) the test for the overall effect is now less significant.
The use of a fixed-effect model is not unproblematic, as
many researchers argue that heterogeneity is inevitable
in a meta-analysis. Especially for orthodontic clinical
research, a random-effects model can be in most cases
easier to justify than a fixed-effect model, as factors like
different populations, different chronological/skeletal age
and growth potential, different experimental settings,
clinician preferences and experience, appliance design,
Figure 3 Forest plot of the meta-analysis from Figure 2 with either a fixed-effect model (above) or with at random-effectsmodel. IV, inverse variance; CI, confidence interval
324 Papageorgiou Invitation to Submit JO December 2014
patient compliance and biological response to treatment
might come into play.
A common mistake to be avoided is to test for
heterogeneity and then select a fixed-effect or a random-
effects model according to the test results (Borenstein
et al., 2008; Higgins and Green, 2011; Papageorgiou,
2013; Papageorgiou et al., 2014b). This is problematic
for a number of reasons. The choice of model should be
pre-specified a priori (in the protocol) if possible, by
contemplating the review question you have asked, the
studies you intend to include, and if logically you expect
them to be very diverse. You either ‘believe’ in hetero-
geneity a priori or not at all. As an alternative, one
can apply and present both fixed and random-effects
analyses and compare their results and the role of
heterogeneity. This is also often performed to check the
robustness of the results (sensitivity analysis). How-
ever, the interpretation for each model is different, as
discussed earlier, and this could confuse the reader.
The biggest limitation of the fixed-effect model is that
existing means for the identification of heterogeneity are
very imprecise (Hardy and Thompson, 1998), meaning
that heterogeneity is very likely to exist, whether we find it
or not. In this case ignoring heterogeneity might lead to
false positive results and threatens the validity of the meta-
analysis. For example, an empirical study of meta-analyses
on psychology found that the calculated 95% CIs from the
fixed-effect model were considerably narrower than they
actually were (Schmidt et al., 2009). It is generally ‘safer’ to
use a random-effects model, as it gives similar results to the
fixed effect model in case of homogeneity, but deals much
better with the heterogeneity. Finally, a random-effects
model is also better at the generalizability of the meta-
analysis results, as it covers more clinical scenarios and
therefore, is more useful in evidence-based decision-
making in orthodontics.
ConclusionsRegarding the choice of effect measure:
N For continuous outcomes either the mean difference
or the standardised mean difference can be used,
according to the measurement scale used.
N For binary outcomes, the use of relative risk seems to
be preferable to the use of OR or RD based on
empirical and epidemiological grounds. Re-expressing
the results into the individualised number needed to
treat aids in the clinical translation.
Regarding the choice of a statistical model:
N The choice of model should be pre-specified, where
possible.
N A fixed-effect model is by definition difficult to apply in
orthodontic clinical research, as many factors can result
in between-study variability and absolutely controlled
experimental conditions are almost impossible.
N A random-effects model is easier to justify clinically in
orthodontics and is generally more conservative thana fixed-effect model, reducing the risk of spurious
findings.
N The results of a random-effects model must be
interpreted accordingly, as the average of the various
treatment effects among the included trials and, if
possible, be accompanied by 95% predictive intervals.
Disclaimer StatementsContributors Mr Papageorgiou wrote and revised the
first manuscript and is the guarantor.
Funding None
Conflicts of interest None
Ethics approval No ethical approval needed.
Acknowledgements
I would like to thank Martyn Cobourne for his helpfulcomments on the earlier version of this manuscript.
ReferencesAltman DG, Deeks JJ, Sackett DL. Odds ratios should be avoided when events
are common. BMJ 1998; 317: 1318.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-
analysis. Chichester: John Wiley & Sons. 2008.
Deeks J. When can odds ratios mislead? Odds ratios should be used only in case-
control studies and logistic regression analyses. BMJ 1998; 317: 1155–1156.
Deeks JJ. Issues in the selection of a summary statistic for meta-analysis of
clinical trials with binary outcomes. Stat Med 2002; 21: 1575–1600.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials
1986; 7: 177–188.
Engels EA, Schmid CH, Terrin N, Olkin I, Lau J. Heterogeneity and statistical
significance in meta-analysis: an empirical study of 125 meta-analyses. Stat
Med 2000; 19: 1707–1728.
Feinstein AR. Indexes of contrast and quantitative significance for comparisons
of two groups. Stat Med 1999; 18: 2557–2581.
Fleiss J. Statistical Methods for Rates and Proportions. 2nd edn. New York:
John Wiley and sons. 1981.
Furukawa TA, Guyatt GH, Griffith LE. Can we individualize the ’number
needed to treat’? An empirical study of summary effect measures in meta-
analyses. Int J Epidemiol 2002; 31: 72–76.
Glasziou P, Guyatt GH, Dans AL, Dans LF, Straus S, Sackett DL. Applying the
results of trials and systematic reviews to individual patients. ACP J Club
1998; 129: A15–A16.
Greenland S. Model-based estimation of relative risks and other epidemiologic
measures in studies of common outcomes and in case-control studies. Am
J Epidemiol 2004; 160: 301–305.
Greenland S, Robins JM. Estimation of a common effect parameter from sparse
follow-up data. Biometrics 1985; 41: 55–68.
Grimes DA, Schulz KF. Making sense of odds and odds ratios. Obstet Gynecol
2008; 111: 423–426.
Hardy RJ, Thompson SG. Detecting and describing heterogeneity in meta-
analysis. Stat Med 1998; 17: 841–856.
JO December 2014 Invitation to Submit Choice of effect and model in meta-analysis 325
Higgins JP, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects
meta-analysis. J R Stat Soc Ser A Stat Soc 2009; 172: 137–159.
Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of
Interventions Version 5.1.0 (updated March 2011). The Cochrane
Collaboration, 2011. Available from: www.cochrane-handbook.org
Huskisson EC. Measurement of pain. Lancet 1974; 2: 1127–1131.
Knol MJ. Down with odds ratios: risk ratios in cohort studies and randomised
clinical trials. Ned Tijdschr Geneeskd 2012; 156: A4775.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al.
The PRISMA statement for reporting systematic reviews and meta-
analyses of studies that evaluate health care interventions: explanation and
elaboration. J Clin Epidemiol 2009; 62: e1–e34.
Likert R. A technique for the measurement of attitudes. Arch Psychol 1932; 140:
1–55.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from
retrospective studies of disease. J Natl Cancer Inst 1959; 22: 719–748.
McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies
and clinical trials of common outcomes. Am J Epidemiol 2003; 157: 940–943.
Newcombe RG. A deficiency of the odds ratio as a measure of effect size. Stat
Med 2006; 25: 4235–4240.
Papageorgiou SN. Meta-analysis 101. Am J Orthod Dentofacial Orthop 2013;
144: 497.
Papageorgiou SN, Antonoglou G, Tsiranidou E, Jepsen S, Jager A. Bias and small-
study effects influence treatment effect estimates: a meta-epidemiological study
in oral medicine. J Clin Epidemiol 2014a. Epub ahead of print: DOI: 10.1016/
j.jclinepi.2014.04.002.
Papageorgiou SN, Papadopoulos MA, Athanasiou AE. Reporting character-
istics of meta-analyses in orthodontics: methodological assessment and
statistical recommendations. Eur J Orthod 2014b; 36: 74–85.
Review Manager (RevMan) [Computer program]. Version 5.2. Copenhagen:
The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Sackett DL, Deeks JJ, Altman D. Down with odds ratios! Evidence-Based Med
1996; 1: 164–167.
Sacket DL, Richardson WS, Rosenberg W, Haynes RB. Evidence-Based
Medicine: How to Practice and Teach EBM. New York: Churchill
Livingstone. 1997.
Schmidt FL, Oh IS, Hayes TL. Fixed- versus random-effects models in meta-
analysis: model properties and an empirical comparison of differences in
results. Br J Math Stat Psychol 2009; 62: 97–128.
Sinclair JC, Bracken MB. Clinically useful measures of effect in binary analyses
of randomized trials. J Clin Epidemiol 1994; 47: 881–90.
Thiruvenkatachari B, Harrison JE, Worthington HV, O’Brien KD. Orthodontic
treatment for prominent upper front teeth (Class II malocclusion) in
children. Cochrane Database Syst Rev 2013; 11: CD003452.
Walter SD. Choice of effect measure for epidemiological data. J Clin Epidemiol
2000; 53: 931–939.
Yusuf S, Peto R, Lewis J, Collins R, Sleight P. Beta blockade during and after
myocardial infarction: an overview of the randomised trials. Prog
Cardiovasc Dis 1985; 27: 335–371.
326 Papageorgiou Invitation to Submit JO December 2014











![[326-09]. Singh, Rana P.B. 2009. Transformation on the cradle of time; in, his: Banaras: Making of India’s Heritage City. Planet Earth & Cultural Understanding, Series Pub. 3. Cambridge](https://static.fdokumen.com/doc/165x107/633386afa290d455630a30e3/326-09-singh-rana-pb-2009-transformation-on-the-cradle-of-time-in-his.jpg)