Minichromosome maintenance complex component 8 (MCM8) gene mutations result in primary gonadal...
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of Minichromosome maintenance complex component 8 (MCM8) gene mutations result in primary gonadal...
ORIGINAL ARTICLE
Minichromosome maintenance complex component8 (MCM8) gene mutations result in primarygonadal failureYardena Tenenbaum-Rakover,1,2 Ariella Weinberg-Shukron,3,4 Paul Renbaum,3
Orit Lobel,3,4 Hasan Eideh,5 Suleyman Gulsuner,6 Dvir Dahary,7 Amal Abu-Rayyan,8
Moien Kanaan,8 Ephrat Levy-Lahad,3,4 Dani Bercovich,9 David Zangen10
▸ Additional material ispublished online only. To viewplease visit the journal online(http://dx.doi.org/10.1136/jmedgenet-2014-102921).
For numbered affiliations seeend of article.
Correspondence toDr Yardena Tenenbaum-Rakover, Pediatric EndocrineUnit, Ha’Emek Medical Center,Afula 18101, Israel;[email protected]
YT-R, AW-S, DB and DZcontributed equally.
Received 26 November 2014Revised 3 March 2015Accepted 25 March 2015
To cite: Tenenbaum-Rakover Y, Weinberg-Shukron A, Renbaum P,et al. J Med Genet PublishedOnline First: [please includeDay Month Year]doi:10.1136/jmedgenet-2014-102921
ABSTRACTBackground Primary gonadal failure is characterisedby primary amenorrhoea or early menopause in females,and oligospermia or azoospermia in males. Variants ofthe minichromosome maintenance complex component 8gene (MCM8) have recently been shown to besignificantly associated with women’s menopausal agein genome-wide association studies. Furthermore,MCM8-knockout mice are sterile. The objective of thisstudy was to elucidate the genetic aetiology of gonadalfailure in two consanguineous families presenting asprimary amenorrhoea in the females and as small testesand azoospermia in a male.Methods and results Using whole exome sequencing,we identified two novel homozygous mutations in theMCM8 gene: a splice (c.1954-1G>A) and a frameshift(c.1469-1470insTA). In each consanguineous family themutation segregated with the disease and both mutationswere absent in 100 ethnically matched controls. The splicemutation led to lack of the wild-type transcript and threedifferent aberrant transcripts predicted to result in eithertruncated or significantly shorter proteins. Quantitativeanalysis of the aberrantly spliced transcripts showed asignificant decrease in total MCM8 message in affectedhomozygotes for the mutation, and an intermediatedecrease in heterozygous family members. Chromosomalbreakage following exposure to mitomcyin C wassignificantly increased in cells from homozygous individualsfor c.1954-1G>A, as well as c.1469-1470insTA.Conclusions MCM8, a component of the pre-replicationcomplex, is crucial for gonadal development andmaintenance in humans—both males and females. Thesefindings provide new insights into the genetic disorders ofinfertility and premature menopause in women.
INTRODUCTIONFetal sex differentiation occurs via multiple genesthat affect the development of germ cells, theirmigration to the urogenital ridge, and the differen-tiation and formation of testis or ovary from thebipotential gonad.1–3 Studies in knockout mousemodels have indicated that following the appropri-ate formation and migration of germ cells, severaltranscription factors, such as empty spiracleshomeobox 2 (Emx2), Wilms tumour 1 (WT1), andLim homeobox 9 (Lhx9), enable formation of theurogenital ridge from the intermediate mesodermand, consequently, bipotential gonad development.
The bipotenial gonad differentiates into testes inthe presence of sex region Y (SRY). Differentiationinto ovaries occurs when the SRY domain islacking,2 but discovery of the roles of WNT4 (MIM3603490), R-spondin 1 (RSPO1 (MIM 609595)),forkhead transcription factor L2 (FOXL2 (MIM305597)), and β catenin has suggested that ovariandevelopment is an active process rather than just adefault pathway.2 4 Clinically, primary gonadalinsufficiency is characterised by high serumgonadotropin concentrations and a lack of spontan-eous pubertal development, associated in femaleswith primary or secondary amenorrhoea, uterinehypoplasia, infertility and early menopause. Inmales, testicular insufficiency is associated withunderdeveloped testes, oligospermia or azoosper-mia. Primary ovarian insufficiency (POI) resultsfrom either ovarian dysgenesis with depletion ofthe primordial follicular pool, or diminished size ofthe pool due to accelerated atresia. To date, agenetic cause has been determined in only a fewcases of POI:5 the most common one involves Xchromosome abnormalities as in Turner syndrome,or X-linked genes, in particular fragile X mentalretardation 1 (FMR1 (MIM 309550)) and bonemorphogenetic protein 15 (BMP15 (MIM300247)).5 Additional genes have been identified inthe last few years, including: FOXL2, the folliclestimulating hormone (FSH) receptor (FSHR (MIM136435)), newborn ovary homeobox (NOBOX(MIM 610934)), nuclear receptor subfamily(NROB1/DAX1 (MIM 300473)),6 steroidogenicfactor 1 (SF1/NR5A1 (MIM 184757)),7 PSMC3IP(MIM 608665),8 and very recently, the STAG3gene,9 but the transcriptional cascade of ovariandevelopment is still poorly understood.Genome-wide association studies (GWAS) aimed atidentifying factors that determine the length of thereproductive lifespan and the aetiology ofpremature ovarian failure have revealed a few spe-cific single nucleotide polymorphisms (SNPs)within genes (eg, SYCP2L, UIMCI, and MCM8)10
that are significantly associated with age of meno-pause. Interestingly, only a few families have beenreported in which both genders are affected withprimary gonadal failure, but their genetic aetiologyremains unexplained in most cases.In the present study, using whole exome sequen-
cing (WES), we describe two novel mutations in
Tenenbaum-Rakover Y, et al. J Med Genet 2015;0:1–9. doi:10.1136/jmedgenet-2014-102921 1
Developmental defects JMG Online First, published on April 14, 2015 as 10.1136/jmedgenet-2014-102921
Copyright Article author (or their employer) 2015. Produced by BMJ Publishing Group Ltd under licence.
group.bmj.com on April 15, 2015 - Published by http://jmg.bmj.com/Downloaded from
the minichromosome maintenance complex component 8 gene(MCM8), leading to primary gonadal failure in humans, bothmales and females. Both the splice mutation, c.1954-1G>A,and a frameshift mutation, c.1469-1470insTA, compromiseMCM8 function and lead to chromosomal instability.
METHODSFurther information can be found in the online supplementarymethods. This study was approved by Shaare Zedek andHa’Emek Medical Centers Institutional Review Board and theNational Helsinki Committee for Genetic Studies. Informedconsent and blood samples were obtained from the study parti-cipants and 100 unrelated healthy controls of Arab origin.
Genetic studiesGenomic DNA was extracted from peripheral blood mono-nuclear cells. Chromosome microarray analysis (CMA) was per-formed on genomic DNA extracted from peripheral bloodmononuclear cells in families A and B. Affymetrix cytogenetic2.7 M arrays were used with the Human Mapping Cytogenetic2.7 M Assay Kit according to the manufacturer’s standardprotocol. Results were analysed with the AffymetrixChromosome Analysis Suite (genome build 37) V.31NA.
For homozygosity mapping, DNA samples were genotypedwith the Affymetrix Gene Chip 250 K/750K Nsp SNP array. SNPdata were analysed using KinSNP11 and examined for informativegenomic regions >2Mb that were homozygous and sharedamong affected individuals, but not by their unaffected siblings.WES in family A was used to search for candidate variants in theaffected female proband (figure 1A, V-1). WES in family B wasused to search for shared candidate variants in the three affectedsisters (figure 1B, IV-2, IV-3 and IV-4). Genomic DNA librarieswere created following standard protocols. Libraries were enrichedusing Nextera Exome enrichment kit (62 Mbp; Illumina) andsequenced on HiSeq2500 (2×170 bp PE run) at a 83× meancoverage. Reads were aligned to the human genome (hg19; NCBIbuild 37; February 2009). (Exome filtering criteria for both fam-ilies are detailed in table 1, see online supplementary tables S1 andS2). In family A, Sanger sequencing was used to validate all codingand splicing variants that were homozygous, had a positive loga-rithm of odds (LOD) score, and were absent or found at very lowfrequencies in dbSNP, Exome variant server (http://evs.gs.washington.edu/EVS/) and 1000 Genomes (see online supplemen-tary table S1). In family B, Sanger sequencing was performed forthe MCM8 c.1469-1470insTA mutation in all available samples(figure 1B, D). PCR products were sequenced using BigDyeTerminator V.3.1. Sequence analysis was performed on an AppliedBiosystems 3130xl Genetic Analyzer. Both MCM8 c.1954-1G>Aand MCM8 c.1469-1470insTAwere analysed in 100 Arab controlsby either PstI digestion or a Gene-Scan assay, respectively. TheGene-Scan PCR products were analysed on the 3130xl GeneticAnalyzer with GeneScan 500 ROX size standards. Results wereanalysed using GeneScan analysis software.
RNA and cDNA studiesRNAwas extracted from peripheral blood leucocytes drawn intoTempus Blood RNA Tubes using the Applied Biosystems TempusBlood RNA kit. RNAwas reverse-transcribed using random hex-amers in the presence of RNase inhibitor (rRNasin, Promega). Infamily A, cDNAwas amplified by PCR with primers surroundingthe MCM8 mutation located in intron 14 at c.1954-1 (see onlinesupplementary table S3). PCR products were sequenced usingBigDye Terminator V.3.1. Quantitative real-time PCR analysis(qRT-PCR) was performed using primers spanning exon 7 and
exon 8 of MCM8 (see online supplementary table S3). Reactionswere performed using Power SYBR master mix (AppliedBiosystems) on the ABI PRISM 7000/7900 Sequence Detector(Applied Biosystems). MCM8 threshold cycle (Ct) values werenormalised to the Ct values of the housekeeping gene GAPDH ineach relevant sample. Relative mRNA levels were quantifiedusing the comparative method (ABI PRISM 7700 SequenceDetection System 1997) and calculated as 2−ΔCt. Experimentswere performed at least three times on all family members andhealthy controls. MCM8 expression in ovarian tissue was assessedby performing PCR reactions surrounding exons 12 and 15 ofMCM8 in an IGROV-1 ovarian carcinoma cell line.
Chromosomal instability studiesWe assayed DNA repair capabilities of lymphocytes cultured inperipheral blood karyotyping medium with phytohaemagglu-tinin (cat# 01-201-1, Biological Industries Ltd, Israel) in thepresence of mitomycin C (MMC) from Streptomyces caespitosus(cat# m0503-2 mg, Sigma) at increasing concentrations: 0, 150and 300 nM.12 Cells were harvested after 72 h of incubation at37°C and dropped onto microscope slides. At least 10 meta-phase spreads per sample were evaluated under the microscopefor aberrations. Two-tailed t test assuming equal variance wasused to compare the two cell lines at each concentration.
RESULTSClinical presentationsFamily ATwo siblings from a highly consanguineous Arab family pre-sented with gonadal failure. The oldest sister (V-1; figure 1A)was completely prepubertal with primary amenorrhoea at15 years of age. Her karyotype was 46,XX. Her gonadotropinvalues were elevated, consistent with primary ovarian failure(table 2). At her last visit, at 22 years of age, her pubertal devel-opment was at Tanner stage B2 and P5. Her 21-year-old brother(V-2; figure 1A), born small for gestational age (weight 1900 g),had neonatal hypocalcaemic seizures (treated with calcium andvitamin D), mild ventricular septal defect (VSD), right aorticarch and T cell derived immune deficiency, and was diagnosedwith DiGeorge syndrome (22q11 microdeletion) by fluorescencein situ hybridisation (FISH). His karyotype was 46,XY. At theage of 17 years and at his last visit at 21 years of age, his puber-tal development was at Tanner stage 5 for pubic hair and peniledevelopment but his testicular volume was only 3 mL, asconfirmed by ultrasound. High basal and GnRH-stimulatedgonadotropins and azoospermia consistent with primary testicu-lar failure (table 2). The father underwent delayed puberty, and,in addition, at the age of 49 years, his serum FSH concentra-tions were high at 21.2 mIU/L (normal male range 1.5–12.4 mIU/L), with normal luteinising hormone (LH) and testos-terone concentrations. The mother had delayed menarche at theage of 15 years but ever since then has had regular menses anda normal hormonal profile (age 40 years). Both parents werenegative for the 22q11 microdeletion. There were two add-itional siblings: a 10-year-old brother with a small VSD butotherwise no somatic phenotype and a normal prepubertalgonadotropin response to GnRH stimulation; and a 14-year-oldbrother (V-3, figure 1A) with a normal age related hormonalprofile. No known history of malignancies was reported in theextended family.
Family BThree sisters from a highly consanguineous Arab family(figure 1B, not related to family A) presented consecutively at the
2 Tenenbaum-Rakover Y, et al. J Med Genet 2015;0:1–9. doi:10.1136/jmedgenet-2014-102921
Developmental defects
group.bmj.com on April 15, 2015 - Published by http://jmg.bmj.com/Downloaded from
age of 14.5–15 years with delayed puberty, primary amenorrhoea,hypergonadotrophic hypogonadism, absence of ovaries, and asmall uterus at both ultrasound and MRI imaging (table 2). Apartfrom delayed pubertal signs, the medical history and physicalexamination were unremarkable. The karyotype was 46,XX andSRY testing was negative. They responded well to oestrogenand progesterone replacement therapy, achieved normal heightand pubertal development (Tanner stage 5 for breast and pubichair), and experienced regular menstrual cycles. The parents andan older healthy sister had normal pubertal development and anormal hormonal profile. Following the diagnosis of POI in thethree sisters, two paternal female cousins aged 30 and 28 yearswere diagnosed with primary hypergonadotrophic hypogonadism.No known history of malignancies was reported in the extendedfamily.
Copy number variation analysisWe first performed CMA analysis on both affected siblings fromfamily A and on the three affected sisters from family B (figure
1A, cases V-1 and V-2, and figure 1B, cases IV-2, IV-3 and IV-4);as expected, in patient V-2 from family A, who was previouslydiagnosed with DiGeorge syndrome, we identified a 2.724 Mbdeletion in 22q11.21 (chr22:19 040 100–21 457 100, genes:DGCR11, SERPIND1, ARVCF, COMT, PI4KAP1, UFD1L,FLJ39582, RIMBP3B, ZNF74, and SLC7A4). He also had a427 kb duplication in chromosome 6q27 (chr6:170 300 320–170 827 320, genes: FAM120B, TBP, PDCD2, DLL1,LOC154449, and PSMB1). His non-gonadal phenotype is con-sistent with the 22q deletion, whereas genes in the duplicated6q27 region have not been reported to cause similar features orgonadal effects. Furthermore, these genomic rearrangementswere not found in his sister, V-1, whose CMA revealed no signifi-cant duplications or deletions. No significant copy number varia-tions (CNVs) were observed in family B.
Homozygosity mappingHomozygosity mapping in family B identified approximately32 Mb of homozygous regions, including two large regions on
Figure 1 Family pedigrees and MCM8 mutation sequencing. (A) Pedigree of family A. Affected siblings V-1 and V-2 are homozygous for theMCM8 c.1954-1G>A mutation (V- variant, N-normal). The parents (IV-1 and IV-2), and the healthy brother V-3 are heterozygous carriers. (B)Pedigree of family B. Affected siblings IV-2, 3 and 4 and affected cousins IV-6 and 7 are homozygous for the MCM8 c.1469-1470insTA mutation.The parents (III-1 and III-2), healthy aunt III-3 and a healthy brother (IV-5) are heterozygous. An older healthy sister (IV-1) is wild type. (C) Sangersequencing in family A of the genomic MCM8 c.1954-1G>A mutation at chr20:5966317, showing the mutation at the acceptor splice site betweenintron 14 and exon 15. First row: sequence from an unrelated wild-type (WT) individual, with the WT G allele at the splice site (surrounded by ablack square). Second row: sequence from a carrier parent, harbouring both the WT G allele and the mutant A allele (R, surrounded by a blacksquare). Third row: sequence from an affected individual, harbouring the mutated base A on both alleles at the splice site (surrounded by a blacksquare). Intron–exon junction is marked by a black vertical line at the right of the mutated base. (D) Sanger sequencing in family B of the genomicMCM8 c.1469-1470insTA mutation at chr20: 5958595, showing the 2 bp insertion and the frameshift it causes. First row: sequence from anunrelated WT individual. WT amino acid codons are marked above the WT sequence. Second row: sequence from a carrier parent, harbouring boththe WT allele and the mutant 2 bp insertion allele. Both the WT amino acid codons and the mutated codons that are generated by the insertionallele are marked above the sequence. Third row: sequence from an affected individual, harbouring the mutated 2 bp insertion on both alleles (theinserted 2 bp are surrounded by a black square). The new amino acid codons which are generated by the insertion allele are marked above thesequence.
Tenenbaum-Rakover Y, et al. J Med Genet 2015;0:1–9. doi:10.1136/jmedgenet-2014-102921 3
Developmental defects
group.bmj.com on April 15, 2015 - Published by http://jmg.bmj.com/Downloaded from
chromosomes 17 and 18, but no candidate genes in theseregions were related to gonadal dysgenesis.
Whole exome sequencingFamily AWES was performed on genomic DNA from the female probandin family A (figure 1A, V-1). Applying the filters indicated above,13 homozygous coding variants with a quality score >10, LODscore >0, and frequency ≤1% were identified (table 1). Sangersequencing confirmed that the proband (V-1) was indeed homo-zygous for 12/13 variants, but her affected brother (V-2) waseither heterozygous or wild type for 12 of these variants. Only anovel homozygous MCM8 IVS14-1G>A (c.1954-1, G>A)variant at the canonical acceptor splice site of intron 14(genomic position chr20:5966567 G>A dbSNP IDrs138761187, NM_001281520.1, NP_001268449) segregatedwith the disease in family A (see online supplementary table S1).Both affected siblings were homozygous for this mutation,whereas the parents (IV-1 and IV-2) and the healthy brother(V-3) were heterozygous (figure 1A, C). The MCM8 c.1954-1G>A splice site mutation (rs138761187) has been reported, inthe heterozygote state, in 1/8599 (0.012%) European Americansand in 0/4066 African Americans, in the Exome Variant Server(National Heart, Lung, and Blood Institute (NHLBI) ExomeSequencing Project (http://evs.gs.washington.edu/EVS)) and in1/4545 (0.022%) in the 1000 Genomes project. No homozy-gotes are reported in any database, and it was not identified in100 ethnically matched healthy control subjects.
Family BWES was performed on genomic DNA from three affectedfemales (figure 1B, IV-2, 3 and 4), one healthy sister (IV-1), andthe parents (III-1 and III-2). Only a novel homozygous MCM8c.1469-1470insTA 2-bp frameshift mutation (genomic positionchr20:5958595 insTA, NM_001281520.1, NP_001268449)segregated with the disease in this family (table 1). All affectedindividuals were homozygous for the MCM8 c.1469-1470insTA
mutation (IV-2, 3, 4, 6 and 7), whereas the parents (III-1 andIII-2), a healthy unaffected aunt (III-3), and the unaffectedbrother (IV-5) were heterozygous. The unaffected sister (IV-1)was wild type (figure 1B, D). Although the probable inheritancemodel in this family is homozygosity for an autosomal recessiveallele, we searched for both compound heterozygous and denovo heterozygous mutations in the affected sisters and nomutations were found to fit these models (see online supplemen-tary table S2). The frameshift c.1469-1470insTA mutation ispredicted to generate a premature stop codon 88 amino acidsdownstream, p.Leu491Ilefs*88. This variant has not beenreported in any database and was absent in 100 ethnicallymatched healthy control subjects.
MCM8 c.1954-1 G>A cDNA analysisTo confirm that the MCM8 c.1954-1 G>A mutation affects spli-cing, MCM8 cDNA was amplified and sequenced in all sampledindividuals from family A (figure 2A). Whereas in normal con-trols there was a single transcript of the expected length, in theaffected homozygotes (family A, V-1 and V-2) there were threedifferent MCM8 transcripts: one of seemingly similar size to thewild type, and two shorter transcripts which were not present innormal controls (figure 2B). Sequencing revealed that all threeMCM8 transcripts produced from the mutant allele differ fromthe wild type, either by usage of alternative splice sites in exon15 or by skipping exon 15 entirely (figure 2C): (1) the largesttranscript (figure 2A, transcript b) is only 1 bp shorter than thewild type, based on an alternative splice site 1 nucleotide intoexon 15—this results in a frameshift leading to a premature stopcodon after six alternative codons, p.Val652Trpfs*6; (2) thesecond transcript (figure 2A, transcript c) is the product of analternative splice site 39 nucleotides into exon 15, predicted todelete the first 13 amino acids in exon 15 (in frame), leaving therest of the protein intact, p.(Val652_Gln664del); (3) the smallesttranscript (figure 2A, transcript d) is produced by complete skip-ping of exon 15, predicted to delete (in frame) 70 amino acidsfrom the protein, p.(Val652_Glu721del).
Semi-quantitative analysis of c.1954-1 G>A cDNAtranscriptsTo determine the relative amounts of the alternative transcriptsderived from the mutant MCM8 c.1954-1 G>A allele, we per-formed semi-quantitative analysis of cDNA from homozygouscompared to heterozygous and wild-type (WT) samples in familyA (figure 2D). The main alternative transcript in homozygous indi-viduals was the one lacking exon 15 due to complete skipping ofthis exon (p.(Val652_Glu721del), transcript d, 55%). The twoother transcripts—alternative splice site 1 bp into exon 15 (p.Val652Trpfs*6, transcript b) and alternative splice site 39 bp intoexon 1 (p.(Val652_Gln664del), transcript c)—accounted for 35%and 10% of the mutantMCM8 c.1954-1,G>A alleles, respectively.NoWTcDNAwas identified in c.1954-1 G>A homozygotes.
qRT-PCR analysis of c.1954-1 G>A mRNATo determine whether the MCM8 c.1954-1 G>A splice muta-tion affects the total amount of MCM8 mRNA and quantify thiseffect, we performed qRT-PCR using primers spanning exons 7and 8 of MCM8 (see online supplementary table S3), which arepresent in all alternatively spliced MCM8 transcripts and arelocated upstream of the splice mutation we identified.Experiments were performed at least three times, each time onboth homozygous individuals from family A, three heterozygousfamily members (two parents and one healthy brother), andthree unrelated wild-type samples from the same ethnic
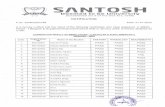
Table 1 Next generation whole exome data filtering criteria
Filtering criteria, family ANumber ofvariants V-1
Total number of variants 24 050Coding missense, nonsense, splice and frameshift only 12 576Homozygous variants 4706Variant quality >10LOD score > 0
1295
Frequency ≤1% 15Exclude polymorphic repeats 13Segregated with the disease in the family 1
Filtering criteria, family B
Number of variants
IV-2 IV-3 IV-4
Total number of variants 193 481 189 325 269 432Coding missense, nonsense, splice andframeshift only
15 472 15 367 15 532
Homozygous variants 5038 5196 5414Shared variants 3417Frequency ≤1% 373Not homozygous in healthy sister IV-1 or inparents III-1 and III-2
1
LOD, logarithm of odds.
4 Tenenbaum-Rakover Y, et al. J Med Genet 2015;0:1–9. doi:10.1136/jmedgenet-2014-102921
Developmental defects
group.bmj.com on April 15, 2015 - Published by http://jmg.bmj.com/Downloaded from
background. We found a significant (p=0.002) threefolddecrease in the quantity of MCM8 mRNA in mutant homozy-gous individuals from family A compared to WT controls.Heterozygote values were intermediate (figure 2E). The MCM8gene normally undergoes alternative splicing, resulting in severalWT transcripts, but according to published expression data,exons 12–16 are present in all of them.
MCM8 expression in ovarian tissueTo assess directly the expression of exons 12 and 15 of MCM8in ovarian tissue, we prepared cDNA from an IGROV-1 ovarian
carcinoma cell line and amplified the segment flanking exon 12and exon 15, confirming that these exons are indeed expressedin ovarian tissue. Exons 12–16 were expressed in all of the alter-native splicing transcripts of the gene.
Chromosomal instability studiesGiven MCM8’s crucial role in homologous recombinationmediated DNA repair, we assessed chromosomal breakagerepair of both MCM8 c.1954-1G>A and MCM8c.1469-1470insTA mutations. DNA repair capabilities wereassessed in peripheral lymphocytes exposed to MMC.
Figure 2 cDNA analysis of family 1. (A) MCM8 gDNA: Schematic representation of wild-type (WT) and c.1954-1G>A-associated transcripts in theMCM8 gene. (A) Normally spliced WT exon 15, resulting in a 358 bp PCR product. Transcripts observed with the c.1954-1G>A mutation; (B)alternative exon 15 acceptor splice site at +1 bp into exon 15; (C) alternative exon 15 acceptor splice site at +39 bp into exon 15; (D) skipping ofexon 15. MCM8 protein: Schematic representation of the MCM8 protein and its known domains. Marked by a purple oval is the MCM domain,typical of all proteins in the MCM family, which resides between amino acids 402 and 609. Exons 14 to 16 are marked by blue squares and thedashed lines mark the regions in the protein that are translated from these exons. (B) Alternative splice products observed using exon 14/16 PCRprimers (as described in A) viewed on a 3% agarose gel. Lane 1, wild type; lane 2, heterozygous c.1954-1G>G/A; lane 3, homozygousc.1954-1G>A. Transcripts a (wild type) and b (del 1 bp) are indistinguishable on this gel. (C) Sequencing of alternative splice transcripts purifiedfrom gel shown in panel B. The expected amino acid sequence of the aberrant splicing in the mutant transcripts is shown above thechromatograms. Transcript b: premature protein truncated after six alternative codons; transcript c: deletion of 13 amino acids; transcript d: deletionof 70 amino acids as a result of exon 15 skipping. (D) Semi-quantitative analysis of WT and mutant MCM8 transcripts. Shown are the cDNA of thec.1954-1G>A homozygote (Hom), the heterozygous (Het) parents, and the WT individuals, amplified with exon 14/16 primers. The homozygousmutant sample does not contain any WT transcript (358 bp). Percentage of each mutant transcript in the homozygous sample is indicated. (E)Quantitative real-time PCR analysis of MCM8 mRNA in family A. Homozygous MCM8 c.1954-1G>A samples contain threefold less mRNA than theWT samples, including no WT allele. Heterozygous values are intermediate. The decrease in mRNA quantity in homozygous MCM8 c.1954-1G>Asamples is significant compared with both WT and heterozygous values. aIndicates significant p value in comparison between WT and heterozygouslevels; bindicates significant p value in comparison between heterozygous and homozygous levels; and cindicates significant p value in comparisonbetween WT and homozygous levels. SD is represented as error bars. SEM for homozygous and heterozygous values is 0.05 and 0.1, respectively.Experiments were performed at least three times, each time on two homozygous individuals, three heterozygous family members (two parents andone healthy brother), and three unrelated WT samples from the same ethnic background.
Tenenbaum-Rakover Y, et al. J Med Genet 2015;0:1–9. doi:10.1136/jmedgenet-2014-102921 5
Developmental defects
group.bmj.com on April 15, 2015 - Published by http://jmg.bmj.com/Downloaded from
Chromosomes derived from WTcontrols showed a few chromo-somal breaks at 150 and 300 nM MMC (figure 3A–C), whereaschromosomes derived from homozygous individuals of bothfamilies showed a significantly increased number of breaks percell at both 150 and 300 nM MMC (Family A 150 nM:Homozygous affected V-1: 3.8±3.3; V-2: 2.4±0.9 vs WTcontrol: 0.25±0.44, p=1.17e−05, 300 nM: Homozygousaffected V-1: 11.6±3.5; V-2: 11.8±3.3 vs WT control: 1.5±1.3, p=5.19e−15. Family B 150 nM: Homozygous affectedIV-3: 4.4±3.4 vs WT control: 0.25±0.44, p=9.2e−06, 300 nM:Homozygous affected IV-3: 12.9±5.9 vs WT control: 1.5±1.3,p=6.18e−09) (figure 3A–C, E). Heterozygous carriers showedan intermediate number of breaks per cell at both 150 and300 nM MMC (figure 3A–E). These results indicated impairedrepair of chromosome breaks in homozygotes for both MCM8c.1954-1G>A and MCM8 c.1469-1470insTA mutations.
DISCUSSIONThe reported novel homozygous splicing and frameshift mutationsin MCM8 implicate the MCM family of proteins in gonadalfailure in humans, both male and female. The MCM8c.1954-1G>A mutation identified in family A results in lack ofnormal MCM8 transcript and leads to production of three aber-rant MCM8 transcripts with significant reduction in the total
amount of MCM8 mRNA. This might be due to nonsensemediated decay in the frame-shifted transcripts, and/or reducedstability of the in-frame deleted transcripts. The MCM8c.1469-1470insTA mutation identified in family B results in aframeshift and premature stop codon 88 amino acids downstream.
MCM8 and MCM9 were the last genes to be discovered in theevolutionarily conserved family of eight proteins (MCM2–9)characterised by Walker A and B motifs for ATP hydrolysis andzinc- and arginine-finger motifs.13–15 Proteins MCM2–7 arerelated to each other and form a family of DNA helicases impli-cated in the initiation of DNA synthesis.
The functions of MCM8 and MCM9 are only partiallyknown, as they have only been studied to a limited extent in celllines and animal models. MCM8 is conserved in most eukaryoticspecies; it is located at chromosome band 20p12.3–13, and con-sists of 19 exons.15 Studies of MCM8 from Xenopus,16 17
Drosophila,18 chicken DT40 cells,19 and mice20 have demon-strated its crucial role in homologous recombination mediatedDNA repair during gametogenesis. Furthermore, MCM8- andMCM9-deficient mice had chromosome damage and werehypersensitive to replication stress, hallmarks of unrepaireddouble-strand breaks.20
While the current study was under review, an MCM8 mis-sense mutation was reported in three sisters of a
Figure 3 Chromosomal breakage analysis in chromosomes derived from peripheral lymphocytes of individuals in families A and B. (A) Number ofbreaks per cell in homozygous and heterozygous individuals from family A, compared to a wild-type (WT) control. (B) Number of breaks per cell inhomozygous and heterozygous individuals from family B, compared to a WT control. aIndicates significant p value in comparison between WT andheterozygous; bindicates significant p value in comparison between heterozygous and homozygous; and cindicates significant p value in comparisonbetween WT and homozygous. At least 10 metaphases were counted per individual. (C) WT chromosomes exposed to 300 nM mitomycin C (MMC).(D) Heterozygous chromosomes. (E) Homozygous chromosomes. Arrows indicate the observed chromosomal breaks.
6 Tenenbaum-Rakover Y, et al. J Med Genet 2015;0:1–9. doi:10.1136/jmedgenet-2014-102921
Developmental defects
group.bmj.com on April 15, 2015 - Published by http://jmg.bmj.com/Downloaded from
consanguineous family affected with POI21 and MCM9 muta-tions were identified in two families with POI.22 Interestingly,the novel MCM8 splice mutation we report is the only muta-tion described to cause gonadal dysgenesis in a male subject aswell, whereas the mutations described in MCM9 have onlybeen described in females. This is compatible with the mouseknockout model in which only MCM8-deficient male micewere sterile, whereas MCM9-deficient males were fertile.20
Although the two proteins could act independently, it has beenshown that together they form a stable complex that isrequired for DNA repair.18–20
Male MCM8-knockout mice have 50% lower testicularvolume and arrested spermatogenesis in meiotic prophase I. Theovaries of newborn female MCM8-knockout mice contain fewer
small-size oocytes with condensed nuclei, indicating that apop-tosis is already occurring at birth. Later in life, MCM8-knockoutfemales have arrested primary follicles, and by adulthood theyhave no observable follicles at all. Furthermore, 100% of thefemales develop ovarian adenomas.20
Interestingly, the late testicular apoptosis observed inMCM8-mutated mice20 suggests that the gonadal failure is anevolving process. Indeed, the homozygous affected male infamily A (V-2) had ‘normal’ pubertal development until17 years of age, when small testes and primary testicular failurebecame evident, suggesting that the gonadal failure developedgradually over a period of years. Moreover, the normal maleserum testosterone concentrations indicated preserved Leydigcell function.
Table 2 Summary of clinical, hormonal and imaging resultsCase 1 (V-1, family A) Female Case 2 (V-2, family A) Male Case 3 (IV-3, family B) Female
Clinical findingsAge at presentation 15 years 2 weeks 14.5 yearsPresenting symptom Primary amenorrhoea Hypocalcaemic seizures Primary amenorrhoeaOther clinical abnormalitiesCardiac Normal VSD and right aortic arch NormalKidney Agenesis of left kidney Normal NormalLung Normal Bronchiectasis due to recurrent pneumonia NormalHearing Mild conductive high frequency hearing
loss in left earNormal Normal
Immune system Normal T cell immune deficiency NormalNeurology Temporal epilepsy Normal Normal
Mild mental retardation Mild mental retardation NormalHeight (cm) (at last visit) 163 (0.33 SD) 161 (−2.5 SD) 158 (−0.7 SD)Weight (kg) (at last visit) 40.5 (−1.3 SD) 43.3 (−4.4 SD) 54 (0.3 SD)Pubertal signs (at last visit) Tanner stage P5, B2* Tanner stage P5, testicular volume 3 Tanner B3* P3*Dysmorphic features Elongated face, hypertelorism and long
fingersThin face, vitiligo spot on forehead, narrowchest with small nipples
None
Hormonal resultsGnRH stimulation testAge (years) 15 18 14.5Basal LH (mIU/L) 31.7 21.3 60Peak LH (mIU/L) 120 84.6 NABasal FSH (mIU/L) 146 46.8 94Peak FSH (mIU/L) >150 80.4 NA
Oestradiol (pmol/L)/testosterone (nmol/L)
<183 13.9 <183
ACTH stimulation testBasal cortisol (nmol/L) 358 378 NAPeak cortisol (nmol/L) 613 616 NA
AMH (ng/mL) Undetectable 3.06 NAImagingSonography No ovary and no uterus (15, 17, 18 years) Homogeneous testis in 2.6 cm volume (19 years) No ovaries , small prepubertal uterus length
5 cm (14.5 years)No ovary, 6 mm long uterus with 4 mmmucosa (20 years)
MRIPelvic No ovary or uterus and rudimentary
vagina (17 years)NA
Brain Normal ND NAGenetic evaluationKaryotype 46, XX 46, XY 46, XX22q11del No Yes NoMCM8 gene mutation c.1954-1G>A/c.1954-1G>A c.1954-1G>A/c.1954-1G>A c.1469-1470insTA/c.1469-1470insTA
*On hormonal replacement therapy.Normal range: LH (mIU/L), male: 1.5–9.3, female: 1.9–12.5; FSH (mIU/L), male: 1.4–18, female: 2.5–10; testosterone (nmol/L): 8.3–28.8; oestradiol (pmol/L): 40.4–605.5; AMH (ng/mL),male: 0.7–19, female: 0.9–9.5.ACTH, adrenocorticotropic hormone; AMH, anti-Müllerian hormone; FSH, follicle stimulating hormone; GnRH, gonadotropin releasing hormone; LH, luteinising hormone; NA, notavailable; ND, not detectable; VSD, ventricular septal defect.
Tenenbaum-Rakover Y, et al. J Med Genet 2015;0:1–9. doi:10.1136/jmedgenet-2014-102921 7
Developmental defects
group.bmj.com on April 15, 2015 - Published by http://jmg.bmj.com/Downloaded from
GWAS aimed at identifying genes associated with earlymenarche or menopause have revealed SNPs in MCM8 asso-ciated with either late age of menopause and higher folliclecounts, or increased probability (by up to 85%) of early meno-pause.10 23–28 Interestingly mutations in STAG3, also encoding aprotein that is important in meiosis, namely a meiosis-specificsubunit of the cohesion ring, was recently reported in a largeconsanguineous family of Arab-Palestinian origin with inheritedPOI.9 That report, together with our findings, suggest that add-itional unexplained cases of ovarian dysgenesis, as well as pre-mature menopause, might be attributed to defects in the meioticprocess.
MCM8 has been shown to be involved in homologous recom-bination mediated DNA repair during gametogenesis and insomatic cell DNA repair, functions that are associated withgenomic instability and higher tumour susceptibility,16 as femaleMCM8-knockout mice all developed adenomas, and 50% ofthem developed sex cord stromal tumours later in life.20 Ourresults, which showed increased chromosomal breaks per cell inhomozygote chromosomes of both mutations, along withsimilar results from the other very recently reported MCM8 andMCM9 mutations,21 22 and the development of ovarian aden-omas and carcinomas in MCM8-deficient female mice, stronglyindicate close monitoring and possibly even removal of non-functioning gonads in cases with MCM8 mutations.Additionally, since chromosomes derived from heterozygousindividuals (in our two families) also displayed some increasednumber of chromosomal breaks per cell compared to controls,it is possible that delayed phenotypes might also manifest laterin life in heterozygous carriers—as observed in the delayedpuberty and the elevation of gonadotropins at 49 years of age inthe father IV-2 in family A.
In family A, POI was associated with additional clinical fea-tures, including hearing loss, agenesis of the left kidney andtemporal epilepsy (in case V-1), and mild mental retardation inboth siblings. Whether these clinical findings can be attributedto the identified MCM8 gene mutation or are related to themorbidity associated with the familial consanguinity has yet tobe defined. Interestingly, the affected male (V-2) had 22q11delwhich, in addition to gonadal failure, presented with DiGeorgesyndrome phenotype. We speculate that this gene deletionmight be caused by the MCM8 gene mutation, resulting ingenetic instability due to meiotic DNA repair defect.
The MCM8 gene, transcribed into several alternatively splicedtranscripts, is widely expressed in human tissues, including theovaries and testes. Most transcripts include all 19 exons, butmay differ in the length of their untranslated regions or in theinclusion of extra exons between exons 8 and 12. The splicemutation reported here, at chr20:5966317, is at the acceptorsplice site before exon 15, which is present in all transcripts ofthe MCM8 gene in the different tissues. It was expressed inRNA extracted from peripheral blood leucocytes as well as froman ovarian cell line. Nevertheless, the exact function of theamino acid sequence encoded by exon 15—that is, amino acids652–722 of the MCM protein—is unknown. Although thesplice mutation, which eliminates exon 15 from the protein orgenerates a premature stop codon in this exon after six aminoacids (from position 652 to 658), is not thought to affect theknown functional domain of the protein (amino acids 402 to609), we assume that it must have an important role given itsubiquitous tissue expression, its evolutionary sequence conserva-tion across species, and the chromosomal instability observed inhomozygous mutant cells. The frameshift mutation reportedhere occurs in exon 12 of the MCM8 gene and disrupts the
MCM8 protein in the middle of its MCM domain (amino acids402–609), which contains Walker A- and Walker B-type nucleo-tide binding motifs. This domain is conserved throughout allMCM proteins (MCM2–9) and is crucial for their functionality.
In summary, we identified novel splice and frameshift muta-tions in the MCM8 gene underlying primary gonadal failure inhumans of both sexes. In view of the major role of MCM8 inthe development and maintenance of gonads in mice, ourfinding of mutations in this gene leading to a human clinicalphenotype might serve as a basis for elucidation of the geneticcauses of other cases of POI and male infertility. Together withGWAS implicating an association between MCM8 SNPs and ageof menopause, our findings provide important evidence thatMCM8 is essential for human gonadal development and main-tenance, and suggest its relevance in the larger context forreproductive lifespan in humans.
Author affiliations1Pediatric Endocrine Unit, Ha’Emek Medical Center, Afula, Israel2The Rappaport Faculty of Medicine, Technion, Haifa, Israel3Medical Genetics Institute, Shaare Zedek Medical Center, Jerusalem, Israel4Hebrew University Medical School, Jerusalem, Israel5Palestinian Medical Complex, Ramallah, USA6Departments of Medicine (Medical Genetics) and Genome Sciences, University ofWashington, Seattle, Washington, USA7Toldot Genetics Ltd., Hod Hasharon, Israel8Hereditary Research Laboratory, Bethlehem University, Bethlehem, Palestine9Tel Hai College and GGA (Galilee Genetic Analysis lab), Tel Hai, Israel10Division of Pediatric Endocrinology, Hadassah Hebrew University Medical Center,Jerusalem, Israel
Acknowledgements We thank Professor Serge Amselem for his constructivecomments and suggestions, Camille Vainstein for professional language editing, andthe families for participating in and providing samples for this study.
Contributors All authors contributed to this manuscript. Planning: YT-R, DZ,AW-S, EL-L and DB. Conducting: YT-R, AW-S, DB, DD, OL, SG, AA-R, MK, HE,PR and DZ. Reporting: YT-R, DZ, AW-S and EL-L.
Funding This study was supported by the Legacy Heritage Biomedical Program ofthe Israel Science Foundation (grant 1531/2009 to DZ), by a grant from the USAgency for International Development (USAID) program for Middle East RegionalCooperation (TA-MOU-10-M30-021 to EL-L and MK), and the Academic committeof Ha'Emek Medical Center (to YT-R).
Competing interests None declared.
Ethics approval Shaare Zedek and Ha’Emek Medical Center Institutional ReviewBoard and the National Genetic Committee.
Patient consent Obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES1 MacLaughlin DT, Donahoe PK. Sex determination and differentiation. N Engl J Med
2004;350:367–78.2 Biason-Lauber A. Control of sex development. Best Pract Res Clin Endocrinol Metab
2010;24:163–86.3 Hughes IA. Disorders of sex development: a new definition and classification. Best
Pract Res Clin Endocrinol Metab 2008;22:119–34.4 Monget P, Bobe J, Gougeon A, Fabre S, Monniaux D, Dalbies-Tran R. The ovarian
reserve in mammals: a functional and evolutionary perspective. Mol Cell Endocrinol2012;356:2–12.
5 Persani L, Rossetti R, Cacciatore C. Genes involved in human premature ovarianfailure. J Mol Endocrinol 2010;45:257–79.
6 Qin Y, Choi Y, Zhao H, Simpson J-L, Chen ZJ, Rajkovic A. NOBOX homeoboxmutation causes premature ovarian failure. Am J Hum Genet 2007;81:576–81.
7 Lourenço D, Brauner R, Lin L, De Perdigo A, Weryha G, Muresan M, Boudjenah R,Guerra-Junior G, Maciel-Guerra AT, Achermann JC, McElreavey K, Bashamboo A.Mutations in NR5A1 associated with ovarian insufficiency. N Engl J Med2009;360:1200–10.
8 Zangen D, Kaufman Y, Zeligson S, Perlberg S, Fridman H, Kanaan M,Abdulhadi-Atwan M, Abu Libdeh A, Gussow A, Kisslov I, Carmel L, Renbaum P,Levy-Lahad E. XX ovarian dysgenesis is caused by a PSMC3IP/HOP2 mutation thatabolishes coactivation of estrogen-driven transcription. Am J Hum Genet2011;89:572–9.
8 Tenenbaum-Rakover Y, et al. J Med Genet 2015;0:1–9. doi:10.1136/jmedgenet-2014-102921
Developmental defects
group.bmj.com on April 15, 2015 - Published by http://jmg.bmj.com/Downloaded from
9 Caburet S, Arboleda VA, Llano E, Overbeek P-A, Barbero JL, Oka K, Harrison W,Vaiman D, Ben-Neriah Z, García-Tuñón I, Fellous M, Pendás AM, Veitia RA,Vilain E. Mutant cohesin in premature ovarian failure. N Engl J Med2014;370:943–9.
10 Carty CL, Spencer KL, Setiawan VW, Fernandez-Rhodes L, Malinowski J, Buyske S,Young A, Jorgensen NW, Cheng I, Carlson CS, Brown-Gentry K, Goodloe R, Park A,Parikh NI, Henderson B, Le Marchand L, Wactawski-Wende J, Fornage M, MatiseTC, Hindorff LA, Arnold AM, Haiman CA, Franceschini N, Peters U, Crawford DC.Replication of genetic loci for ages at menarche and menopause in the multi-ethnicPopulation Architecture using Genomics and Epidemiology (PAGE) study. HumReprod 2013;28:1695–706.
11 Amir el AD, Bartal O, Morad E, Nagar T, Sheynin J, Parvari R, Chalifa-Caspi V.KinSNP software for homozygosity mapping of disease genes using SNPmicroarrays. Hum Genomics 2010;4:394–401.
12 Oostra AB, Nieuwint AW, Joenje H, de Winter JP. Diagnosis of Fanconi anemia:chromosomal breakage analysis. Anemia 2012;2012:238731.
13 Maiorano D, Lutzmann M, Méchali M. MCM proteins and DNA replication. CurrOpin Cell Biol 2006;18:130–6.
14 Gozuacik D, Chami M, Lagorce D, Faivre J, Murakami Y, Poch O, Biermann E,Knippers R, Bréchot C, Paterlini-Bréchot P. Identification and functionalcharacterization of a new member of the human Mcm protein family: hMcm8.Nucleic Acids Res 2003;31:570–8.
15 Johnson EM, Kinoshita Y, Daniel DC. A new member of the MCM proteinfamily encoded by the human MCM8 gene, located contrapodal toGCD10 at chromosome band 20p12.3–13. Nucleic Acids Res 2003;31:2915–25.
16 Gambus A, Blow JJ. Mcm8 and Mcm9 form a dimeric complex in Xenopus laevisegg extract that is not essential for DNA replication initiation. Cell Cycle2013;12:1225–32.
17 Kanemaki MT. The dimeric Mcm8–9 complex of Xenopus laevis likelyhas a conserved function for resistance to DNA damage. Cell Cycle2013;12:1338–9.
18 Blanton HL, Radford SJ, McMahan S, Kearney HM, Ibrahim JG, Sekelsky J. REC,Drosophila MCM8, drives formation of meiotic crossovers. PLoS Genet 2005;1:e40.
19 Nishimura K, Ishiai M, Horikawa K, Fukagawa T, Takata M, Takisawa H, KanemakiMT. Mcm8 and Mcm9 form a complex that functions in homologous recombinationrepair induced by DNA interstrand crosslinks. Mol Cell 2012;47:511–22.
20 Lutzmann M, Grey C, Traver S, Ganier O, Maya-Mendozam A, Ranisavljevic N,Bernex F, Nishiyama A, Montel N, Gavois E, Forichon L, de Massy B, Méchali M.MCM8- and MCM9-deficient mice reveal gametogenesis defects and genomeinstability due to impaired homologous recombination. Mol Cell 2012;47:523–34.
21 AlAsiri S, Basit S, Wood-Trageser MA, Yatsenko SA, Jeffries EP, Surti U, KettererDM, Afzal S, Ramzan K, Faiyaz-Ul Haque M, Jiang H, Trakselis MA, Rajkovic A.Exome sequencing reveals MCM8 mutation underlies ovarian failure andchromosomal instability. J Clin Invest 2015;125:258–62.
22 Wood-Trageser MA, Gurbuz F, Yatsenko SA, Jeffries EP, Kotan LD, Surti U, KettererDM, Matic J, Chipkin J, Jiang H, Trakselis MA, Topaloglu AK, Rajkovic A. MCM9mutations are associated with ovarian failure, short stature, and chromosomalinstability. Am J Hum Genet 2014;4:754–62.
23 Schuh-Huerta SM, Johnson NA, Rosen MP, Sternfeld B, Cedars MI, Reijo Pera RA.Genetic markers of ovarian follicle number and menopause in women of multipleethnicities. Hum Genet 2012;131:1709–24.
24 He C, Murabito JM. Genome-wide association studies of age at menarche and ageat natural menopause. Mol Cell Endocrinol 2014;382:767–79.
25 Murray A, Bennett CE, Perry JR, Weedon MN, Jacobs PA, Morris DH, Orr N,Schoemaker MJ, Jones M, Ashworth A, Swerdlow AJ, ReproGen Consortium.Common genetic variants are significant risk factors for early menopause: resultsfrom the Breakthrough Generations Study. Hum Mol Genet 2011;20:186–92.
26 Stolk L, Zhai G, van Meurs JB, Verbiest MM, Visser JA, Estrada K, Rivadeneira F,Williams FM, Cherkas L, Deloukas P, Soranzo N, de Keyzer JJ, Pop VJ, Lips P,Lebrun CE, van der Schouw YT, Grobbee DE, Witteman J, Hofman A, Pols HA,Laven JS, Spector TD, Uitterlinden AG. Loci at chromosomes 13, 19 and 20influence age at natural menopause. Nat Genet 2009;41:645–7.
27 Chen CT, Fernández-Rhodes L, Brzyski RG, Carlson CS, Chen Z, Heiss G, North KE,Woods NF, Rajkovic A, Kooperberg C, Franceschini N. Replication of loci influencingages at menarche and menopause in Hispanic women: the Women’s HealthInitiative SHARe Study. Hum Mol Genet 2012;21:1419–32.
28 Hartge P. Genetics of reproductive lifespan. Nat Genet 2009;41:637–8.
Tenenbaum-Rakover Y, et al. J Med Genet 2015;0:1–9. doi:10.1136/jmedgenet-2014-102921 9
Developmental defects
group.bmj.com on April 15, 2015 - Published by http://jmg.bmj.com/Downloaded from
in primary gonadal failurecomponent 8 (MCM8) gene mutations result Minichromosome maintenance complex
and David ZangenAmal Abu-Rayyan, Moien Kanaan, Ephrat Levy-Lahad, Dani BercovichRenbaum, Orit Lobel, Hasan Eideh, Suleyman Gulsuner, Dvir Dahary, Yardena Tenenbaum-Rakover, Ariella Weinberg-Shukron, Paul
published online April 14, 2015J Med Genet
http://jmg.bmj.com/content/early/2015/04/14/jmedgenet-2014-102921Updated information and services can be found at:
These include:
MaterialSupplementary
.DC1.htmlhttp://jmg.bmj.com/content/suppl/2015/04/14/jmedgenet-2014-102921Supplementary material can be found at:
References
#BIBLhttp://jmg.bmj.com/content/early/2015/04/14/jmedgenet-2014-102921This article cites 28 articles, 6 of which you can access for free at:
serviceEmail alerting
box at the top right corner of the online article. Receive free email alerts when new articles cite this article. Sign up in the
CollectionsTopic Articles on similar topics can be found in the following collections
(241)Clinical genetics (504)Reproductive medicine
(1194)Molecular genetics (558)Immunology (including allergy) (825)Genetic screening / counselling
Notes
http://group.bmj.com/group/rights-licensing/permissionsTo request permissions go to:
http://journals.bmj.com/cgi/reprintformTo order reprints go to:
http://group.bmj.com/subscribe/To subscribe to BMJ go to:
group.bmj.com on April 15, 2015 - Published by http://jmg.bmj.com/Downloaded from