Mechanisms of acquired resistance to insulin-like growth factor 1 receptor inhibitor in MCF-7 breast...
-
Upload
independent -
Category
Documents
-
view
2 -
download
0
Transcript of Mechanisms of acquired resistance to insulin-like growth factor 1 receptor inhibitor in MCF-7 breast...
PRECLINICAL STUDIES
Mechanisms of acquired resistance to insulin-like growthfactor 1 receptor inhibitor in MCF-7 breast cancer cell line
Roudy Chiminch Ekyalongo & Toru Mukohara &
Yu Kataoka & Yohei Funakoshi & Hideo Tomioka &
Naomi Kiyota & Yutaka Fujiwara & Hironobu Minami
Received: 15 May 2012 /Accepted: 9 July 2012 /Published online: 25 July 2012# Springer Science+Business Media, LLC 2012
Summary The purpose of this study was to clarify the mech-anism of acquired resistance to the insulin-like growth factor-1receptor (IGF-1R) tyrosine kinase inhibitor NVP-AEW541.We developed an acquired resistant model by continuouslyexposing MCF-7 breast cancer cells to NVP-AEW541(MCF-7-NR). MCF-7 and MCF-7-NR were comparativelyanalyzed for cell signaling and cell growth. While phosphory-lation of Akt was completely inhibited by 3 μM NVP-AEW541 in both MCF-7 and MCF-7-NR, phosphorylationof S6K remained high only in MCF-7-NR, suggesting a dis-connection betweenAkt and S6K inMCF-7-NR. Consistently,the mTOR inhibitor everolimus inhibited phosphorylation ofS6K and cell growth equally in both lines. Screening of bothlines for phosphorylation of 42 receptor tyrosine kinases withand without NVP-AEW541 showed that Tyro3 phosphoryla-tion remained high only in MCF-7-NR. Protein expression ofTyro3 was found to be higher in MCF-7-NR than in MCF-7.
Gene silencing of Tyro3 using siRNA resulted in reduced cellgrowth and cyclin D1 expression in both lines. While Tyro3expression was inhibited by NVP-AEW541 and everolimus inMCF-7, it was reduced only by everolimus in MCF-7-NR.These findings suggested that cyclin D1 expression was regu-lated in a S6K/Tyro3-dependent manner in both MCF-7 andMCF-7-NR, and that the disconnection between IGF-1R/Aktand S6Kmay enable MCF-7-NR to keep cyclin D1 high in thepresence of NVP-AEW541. In summary, acquired resistanceto NVP-AEW541 appears to result from IGF-1R/Akt-indepen-dent activation of S6K and expression of Tyro3 and cyclin D1.
Keywords Breast cancer . Insulin-like growth factor-1receptor . NVP-AEW541 . Resistance . Tyro3
Introduction
The last decade has seen the successful introduction ofmolecularly targeted agents, particularly small-molecule re-ceptor tyrosine kinase inhibitors (RTK-Is), into the treatmentof solid tumors in clinical settings. These useful agentsinclude lapatinib, which inhibits human epidermal growthfactor receptor 2 (HER2) with gene-amplification in breastcancer [1]; erlotinib and gefitinib, which inhibit epidermalgrowth factor receptor (EGFR) with somatic mutations innon-small cell lung cancer (NSCLC) [2, 3]; and imatiniband sunitinib, which inhibit KIT with somatic mutations ingastrointestinal stromal tumors (GIST) [4]. Despite theseagents’ promising efficacy, however, virtually all metastaticpatients eventually relapse due to resistance acquired bytumors after exposure to RTK-Is.
One relatively common mechanism of acquired resistanceto RTK-Is involves secondary mutations on the target RTK,and has been identified for erlotinib and gefitinib in NSCLCand for imatinib in GIST [5, 6]. These secondary mutations are
Electronic supplementary material The online version of this article(doi:10.1007/s10637-012-9855-1) contains supplementary material,which is available to authorized users.
R. C. Ekyalongo : T. Mukohara (*) :Y. Kataoka :Y. Funakoshi :H. Tomioka :N. Kiyota :Y. Fujiwara :H. MinamiDivision of Medical Oncology/Hematology, Department ofInternal Medicine, Kobe University Graduate School of Medicine,7-5-2, Kusunoki-cho, Chuo-ku,Kobe 650-0017, Japane-mail: [email protected]
T. Mukohara :H. MinamiCancer Center, Kobe University Hospital,7-5-2, Kusunoki-cho, Chuo-ku,Kobe 650-0017, Japan
Present Address:Y. FujiwaraDivision of Internal Medicine and Thoracic Oncology,National Cancer Center Hospital,5-1-1, Tsukiji, Chuo-ku,Tokyo 104-0045, Japan
Invest New Drugs (2013) 31:293–303DOI 10.1007/s10637-012-9855-1
believed to prevent the RTK-I from accessing the ATP bindingpocket in their target RTK. On the other hand, acquired resis-tance to erlotinib and gefitinib in NSCLC has also been shownto be caused by cross-talk between MET receptors and EGFRfamily members [7]. However, these mechanisms explain onlysome cases of acquired resistance to RTK-Is.
Insulin-like growth factor-1 receptor (IGF-1R) is a po-tential therapeutic target RTK designated for clinical testing.Once the ligands of IGF-IR, IGF-1 or IGF-2 bind to thereceptor’s extracellular domain, the receptor is autophos-phorylated and activated. Adaptor molecules such as insulinreceptor substrate-1 (IRS-1) or IRS-2 are then tyrosine-phosphorylated and mediate downstream signaling, includ-ing phosphatidylinositol 3-kinase (PI3K)/Akt and Ras-Raf-MEK-ERK1/2 pathways [8]. Findings from a number ofpreclinical studies have suggested the benefit of targetingIGF-1R as a strategy for treating some types of aggressivecancer such as multiple myeloma [9], Ewing’s sarcoma [10],and ovarian and breast cancers [11, 12]. For example, inbreast cancer, IGF-1R protein expression is elevated in 39 %to 93 % of tumors [13, 14]. IRS-1 is reported to be frequent-ly phosphorylated in breast cancer tumors [15], and proteinlevels have been correlated with shorter disease-free surviv-al in a subgroup of breast cancer patients [16].
In our previous study, we evaluated the effect of thenovel IGF-1R kinase inhibitor NVP-AEW541 in a largepanel of breast cancer cell lines [17]. Results showed thatIGF-1R expression was not the sole determiner of sensitivityto NVP-AEW541; in fact, sensitivity to this compound wasonly noted in the MCF-7 cell line, the only line which co-expresses high levels of both IGF-1R and IRS-1. We alsoshowed that NVP-AEW541 disrupted complexes of IRS-1and PI3K (p85) in MCF-7 cells [17]. Taken together, thesefindings suggested that co-expression of IGF-1R and IRS-1may indicate functioning IGF-1R signaling and therefore actas a biomarker for predicting the efficacy of NVP-AEW541.However, despite the importance of identifying mechanismsof acquired resistance to molecularly-targeted agents in ad-vance of or in parallel with clinical development, few studieshave yet examined these mechanisms for IGF-1R inhibitors.
Here, to identify mechanisms of acquired resistance to NVP-AEW541 and to develop ameans of overcoming this resistance,we developed a model of acquired resistance using the MCF-7cell line by continuously exposing cells to NVP-AEW541.
Materials and methods
Cell culture and development of cell line resistantto NVP-AEW541
MCF-7, MDA-MB-231, CAMA-1, ZR75-30, BT474,T47D, and HCC1954 breast cancer cell lines were
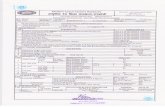
purchased from the American Type Culture Collection(ATCC, Manassas, VA). To generate a cell line resistant toNVP-AEW541, MCF-7 cells were continuously cultured instepwise dial-up dosages of NVP-AEW541 (starting dose:1 μM, gradually increasing up to 5 μM). To examine for thepresence of a resistant clone, MTS assays were performedevery five passages (see below for description). Cells devel-oped sufficient resistance for our study after 12 months’drug exposure (Fig. 1) and were designated as “MCF-7-NR.” MCF-7 parental cells were concomitantly maintainedwithout NVP-AEW541, and drug sensitivity was comparedwith NVP-AEW541-conditioned cells. No significantchange in sensitivity to NVP-AEW541 was observed inparental cells during the drug exposure period (data notshown).
Before every experiment using this new MCF-7-NRline, the cells were allowed to grow under drug-freeconditions for at least 4 days. Both the MCF-7 parentline and MCF-7-NR were maintained in RPMI 1640(Cellgro; Mediatech, Inc., Herdon, CA, USA) supple-mented with 10 % FBS (Gemini-Bio-Products, Inc.,Woodland, CA, USA), 100 units/ml penicillin, 100units/ml streptomycin, and 2 mM glutamine. Estradiolwas not supplemented in maintenance media or in anyexperiments. All cells were grown at 37 °C in a humid-ified atmosphere with 5 % CO2 and were in logarithmicgrowth phase upon initiation of experiments. ParentalMCF-7 cells were passaged for ≤3 months before freshcells were obtained from frozen early-passage stocksreceived from the source.
NVP-AEW541 ( M)
% o
f con
trol
MCF-7
MCF-7-NR
μ
Fig. 1 Development of MCF-7-NR. MCF-7 cells were continuouslyexposed to increasing concentrations (1–5 μM) of NVP-AEW541.MCF-7 and NVP-AEW541-conditioned MCF-7 cells were then furthercultured in 10 % FBS-containing media for 5 days in the presence ofvarious concentrations of NVP-AEW541. The percentage of viablecells is shown relative to that of the untreated control and plotted onthe y-axis, and NVP-AEW541 concentrations are plotted on the x-axis.Each data point represents the mean value and standard deviation of 6–12 wells. After 12 months’ incubation, cells were designated as MCF-7-NR
294 Invest New Drugs (2013) 31:293–303
Drugs
NVP-AEW541 and everolimus (RAD001) were kindlyprovided by Novartis Pharma (Basel, Switzerland).Stock solution was prepared in dimethyl sulfoxide(DMSO) and stored at −20 °C. The EGFR/HER2 inhib-itor lapatinib and Akt inhibitor perifosine were pur-chased from BioVision (Mountain View, CA, USA).Perifosine and lapatinib were reconstituted in PBS andDMSO, respectively, and stored at −20 °C. All drugswere diluted in fresh media before each experiment.
Cell growth assay
Cell growth was determined using an MTS assay kit(Promega, Madison, WI, USA), which determined thenumber of viable cells by a colorimetric method basedon the bioreduction of 3-(4,5-dimethylthiazol-2yl)-5-(3-carboxyme-thowyphenyl)-2-(4-sulfophenyl)-2H-tetrazoli-um (MTS) to a soluble formazan product detected spec-trophotometrically at a wavelength of 490 nm.
MCF-7 or MCF-7-NR diluted in 10 % FBS-containing maintenance media (160 μL/well) were plat-ed in 96-well flat-bottom plates (Corning, Inc., Corning,NY, USA) and incubated for 24 h at 37 °C in 5 %CO2. The cell culture media was then replaced with10 % FBS-containing media with or without the indi-cated drugs until final analysis. The number of cellsrequired to obtain an optical density (OD) of 1.3–2.2,the linear range of the assay, was determined in apreparatory experiment to be 2000 cells/well (data notshown). Each experiment was repeated at least threetimes.
Western blot
Cells were washed once with ice-cold PBS and scrapedimmediately after adding lysis buffer (20 mM tris [pH7.5], 150 mM sodium chloride, 2 mM EDTA, 10 %glycerol, 1 % NP40) containing protease and phospha-tase inhibitor (100 mM NaF, 1 mM phenylmethylsul-fonyl fluoride [PMSF], 1 mM Na3VO4, 2 μg/mlaprotinin, 5 μg/ml leupeptin). Cell lysates were centri-fuged at 14,000 × g for 10 min at 4 °C to pelletinsoluble material, and supernatant was collected asprotein extract.
Protein extract samples were separated using electropho-resis on 7.6 % sodium dodecyl sulfate-polyacrylamide gelsand transferred to polyvinylidene fluoride (PVDF) mem-branes, which were subsequently probed with one of theprimary antibodies. Phospho-IGF-1 receptor β (tyr1135/1136)/Insulin Receptor β (tyr1150/1151) (19H7) IGF-1 re-ceptor β, phospho-IRS-1 (Ser636/639), phospho-IRS-1
(Ser612), IRS-1, phospho-IRS-2 (Ser731), IRS-2,phospho-Akt (Ser473), phospho-Akt (Thr308), Akt,phospho-Tuberin/TSC-2 (Thr1463), phospho-PRAS40(Thr246), phospho-p70 S6 Kinase (S6K) (Thr389), p70S6K, Rheb, Tyro3, and ergenhor Cyclin D1 (DCS6) werepurchased from Cell Signaling Technology (Beverly, MA,USA). Phospho-ERK1/2 (pTpY185/187) and ERK1/2 anti-bodies were purchased from Invitrogen (Carlsbad, CA,USA), and β-actin from Sigma-Aldrich (St. Louis, MO,USA). Each targeted protein was detected using AmershamECL plus Western Blotting Detection Reagents (GE Health-care, Buckinghamshire, UK).
The results are representative of at least two repeatedexperiments. Immunoblots for all repeated experimentswere quantified using ImageJ software (nih.gov).
Phospho-RTK array
Protein extracts were prepared as described above fromMCF-7 and MCF-7-NR cells incubated with and with-out 3 μM of NVP-AEW541 for 24 h. After measuringprotein concentration, 500 μg of total protein was ap-plied to a Human Phospho-RTK array (R&D Systems,Minneapolis, MN, USA), which screens 42 differentphosphorylated human RTKs on the same nitro-cellulose membrane. These experiments were conductedin accordance with the manufacturer’s instructions.
SiRNA transfection
A Tyro3 small interfering RNA (siRNA) Kit was pur-chased from Invitrogen. SiRNAs targeting IRS-2 werepurchased from Ambion Life Technologies (Carlsbad,CA). Optimal conditions for gene knockout were deter-mined by multiple pilot experiments before transfectionin accordance with the manufacturer’s instructions.Briefly, cells were incubated for 24 h at 37 °C in 6-cm plates (Corning) until 50 % to 60 % confluencebefore being transiently transfected with siRNA for24 h using Lipofectamine 2000 reagent (Invitrogen).The cells were then subjected to immunoblot analysisor serial MTS assay. Of three Tyro3 siRNA clonespurchased, the clone AACAAGUUUGGCCACGUGUGGAUGG and AUCACUUCUUCCCACUCCAAGAUGA were selected for efficient knockout. Of twoIRS-2 siRNAs clones purchased, the clone ACUG-CUGCCUGAACAUCAA was selected. To minimizethe risk of sequence-independent effects in our siRNAanalysis, the stealth RNAi negative control low GCduplex (Invi t rogen) was used in each siRNAexperiment.
Invest New Drugs (2013) 31:293–303 295
Results
Persistent S6K phosphorylation in MCF-7-NR treatedwith NVP-AEW541
We established the NVP-AEW541-resistant MCF-7 cell lineMCF-7-NR by continuously exposing parent cells to NVP-AEW541 as described in Materials and Methods (Fig. 1). Toidentify signs of differential cell signaling between MCF-7and MCF-7-NR cells, we examined the expression andphosphorylation levels of IGF-1R and representative down-stream signaling molecules in 10 % FBS-containing mediawith and without 3 μM of NVP-AEW541.
Results showed that protein expression of IGF-1R, thetarget of NVP-AEW541, was preserved in MCF-7-NR atlevels equivalent to those in the MCF-7 parent line (Fig. 2a).While baseline phosphorylation of IGF-1R was equivalentin both cell lines and was fully inhibited on treatment withNVP-AEW541, expression and phosphorylation of IRS-1was significantly reduced in MCF-7-NR compared to MCF-
7 (Fig. 2a). These findings support the hypothesis that IRS-1may be a key determinant of sensitivity to NVP-AEW541,as we proposed in our previous study [17]. On the otherhand, while phosphorylation of IRS-2 was inhibited byNVP-AEW541 in parental cells, it remained high in MCF-7-NR (Fig. 2a). To explore the possibility of involvement ofIRS-2 in the resistance mechanism, IRS-2 was knockeddown using siRNA, but no decrease in the phosphorylationof downstream molecules or growth rate were observed(Supplemental figure 1).
Examination of downstream molecules showed that ex-pression and phosphorylation of ERK1/2 was drasticallyreduced in MCF-7-NR cells compared with MCF-7, a phe-nomenon which was not affected by NVP-AEW541 treat-ment. Interestingly, while treatment with 3 μM NVP-AEW541 resulted in almost complete inhibition of Aktphosphorylation in both lines, phosphorylation of S6K,which is generally considered to lie downstream of Akt,remained high only in MCF-7-NR cells (Fig. 2a), suggestingthat phosphorylation of S6K may be independent of Akt in
phospho-Akt(Ser473)
Akt
phospho-S6K(Thr389)
S6K
β-actin
NVP-AEW541 - - + - - +
MCF-7 MCF-7-NR
- + + - + +IGF-1
phospho-IGF-1R(Tyr1135/1136)
IGF-1R
phospho-IRS-1(Ser612)
IRS-1
phospho-Akt(Ser473)
Akt
phospho-mTOR (Ser2448)
mTOR
phospho-S6K(Thr389)
S6K
phospho-ERK1/2(Thr185/Tyr187)
ERK1/2
β-actin
NVP-AEW541(3 μμM) - + - +
MCF-7 MCF-7-NR
phospho-IRS-2(Ser731)
IRS-2
phospho-Akt(Thr308)
phospho-IRS-1(Ser636/639)
a b
Fig. 2 Effects of NVP-AEW541 on phosphorylation of IGF-1R anddownstream signaling molecules in MCF-7 and MCF-7-NR lines. aCells grown in 10 % FBS-containing media with and without 3 μMNVP-AEW541 for 6 h were lysed and immunoblotted for each protein.Blots were stripped and re-probed for β-actin as a loading control. b
Cells were serum-starved overnight and then grown in the presence orabsence of 3 μM NVP-AEW541 for 2 h followed by IGF-1 (50 ng/ml)stimulation for 15 min. Western blots are shown for phospho- and totalAkt and S6K, and β-actin as a loading control
296 Invest New Drugs (2013) 31:293–303
this line. To more strongly focus on ligand-dependent cellsignaling, we next serum-starved MCF-7 and MCF-7-NRcells overnight and stimulated them with IGF-1 for 15 minwith or without 2 h pre-exposure to 3 μM NVP-AEW541,then analyzed cell lysates by Western blot (Fig. 2b). Con-sistent with the finding in 10 % FBS-containing media,while IGF-1-dependent phosphorylation of Akt wasinhibited with NVP-AEW541 in both lines, inhibition ofS6K phosphorylation occurred only in MCF-7, but not inMCF-7-NR.
Resistance of MCF-7-NR to the Akt inhibitor perifosine
To validate the Akt-independent phosphorylation of S6K inthe MCF-7-NR line, we treated MCF-7 and MCF-7-NRcells with increasing concentrations of the Akt inhibitorperifosine, and noted the inhibition of phospho-Akt from aconcentration of 10 μM in both lines (Fig. 3a). In contrast,while S6K phosphorylation decreased in parallel with that
of Akt in MCF-7 cells, relatively little reduction in S6Kphosphorylation was noted in MCF-7-NR cells, with adecrease only evident at 50 μM of perifosine (Fig. 3a).We next evaluated perifosine-induced growth inhibitionusing an MTS assay. Consistent with findings for S6Kphosphorylation in Western blot analysis, MCF-7-NRwas found to be less sensitive to perifosine than theMCF-7 parent line (Fig. 3b).
Effect of everolimus on MCF-7-NR cell growth
As S6K was suspected to play a central role in thedevelopment of acquired resistance to NVP-AEW541,we next tested the mTOR inhibitor everolimus aloneor in combination with NVP-AEW541 in MCF-7 andMCF-7-NR lines.
In both lines, treatment with 1 μM everolimus in-duced complete inhibition of S6K phosphorylation(Fig. 4a) and an increase in Akt phosphorylation,
Perifosine(μμg/ml) 0 10 25 50 0 10 25 50
MCF-7 MCF-7-NR
phospho-Akt(Ser473)
phospho-S6K(Thr389)
β-acitin
0
20
40
60
80
100
120
Perifosine (μΜ)
% o
f con
trol
MCF-7
MCF-7-NR
10 20 40 800
a
b
Fig. 3 Effect of Akt inhibitor perifosine on phosphorylation of Aktand S6K and cell growth in MCF-7 and MCF-7-NR lines. a Cellsgrown in 10 % FBS-containing media for 6 h with and withoutperifosine were lysed and immunoblotted for phospho-Akt andphospho-S6K. Blots were stripped and re-probed for β-actin as aloading control. The immunoblot was quantified by densitometry.Perifosine concentrations were plotted on the x-axis, and ratio ofphospho-S6K/phospho-Akt was plotted on the y-axis as the average
of the ratio to the untreated control. Standard deviation from repeatedexperiments is shown as error bars. b Cells were grown in 10 % FBS-containing media for 5 days in the presence of various concentrationsof perifosine. The percentage of viable cells is shown relative to that ofthe untreated control and plotted on the y-axis, and concentrations ofeach drug are plotted on the x-axis. Each data point represents themean value and standard deviation of 6–12 replicate wells
Invest New Drugs (2013) 31:293–303 297
possibly due to a well-characterized positive feedbackloop from S6K through Akt [18]. In addition, thisincrease in Akt phosphorylation was suppressed in bothlines on co-treatment with 3 μM NVP-AEW541(Fig. 4a). In the MTS assay using these drugs, ever-olimus was equally effective in MCF-7 and MCF-7-NRcells (Fig. 4b), and growth inhibition in both linesappeared correlated with decreased phosphorylation ofS6K but not Akt (Fig. 4a and b).
Persistent Tyro3 phosphorylation in presenceof NVP-AEW541 in MCF-7-NR
Given that several preclinical studies have shown that alter-native signals from other RTKs can induce resistance tocertain RTK-Is [7, 19, 20], we used a phospho-RTK arrayto explore the phosphorylation profile of other RTKs withand without treatment of 3 μM NVP-AEW541 in MCF-7and MCF-7-NR cells. Baseline phosphorylation of IGF-1Rwas equivalent in both lines and completely inhibited onadministration of 3 μM NVP-AEW541 (Fig. 5), findingsconsistent with our earlier Western blot analysis (Fig. 2a).HER3 phosphorylation was decreased in MCF-7 and slight-ly increased in MCF-7-NR cells on treatment with NVP-AEW541. Because HER3 lacks kinase activity by itself, itmust be coupled with one of the other HER family membersto be activated, such as EGFR and HER2. We thereforetreated MCF-7-NR with 1 μM lapatinib, an EGFR/HER2
phospho-Akt(Ser473)
phospho-S6K(Thr389)
β-actin
Everolimus
MCF-7 MCF-7-NR
NVP-AEW541 - + - + - + - +- - + + - - + +
0
20
40
60
80
100
120
% o
f con
trol
control NVP EVE NVP /EVE
MCF-7
MCF-7-NR
Akt
S6K
a b
Fig. 4 Effect of the mTOR inhibitor everolimus on phosphorylation ofS6K and Akt and cell growth in MCF-7 and MCF-7-NR. a Cells grownin 10 % FBS-containing media for 6 h with and without 1 μM ever-olimus alone or in combination with 3 μM NVP-AEW541 were lysedand immunoblotted for phospho- and total-Akt, and S6K, after whichblots were stripped and re-probed for β-actin as a loading control. b
Cells were grown in 10 % FBS-containing media for 5 days with andwithout 1 μM everolimus alone or in combination with 3 μM NVP-AEW541. The percentage of viable cells is shown relative to that of theuntreated control and plotted on the y-axis, and drugs applied areplotted on the x-axis. Each data point represents the mean value andstandard deviation of 6–12 replicate wells
MCF-7 control
IGF-1R
Internal positive control
Tyro3HER3
EGFR
MCF-7 NVP
MCF-7-NR control
MCF-7-NR NVP
Fig. 5 Phosphorylation profiles of 42 RTKs in MCF-7 and MCF-7-NR lines with and without 3 μM NVP-AEW541. Protein extractsprepared from each cell line grown in 10 % FBS-containing mediumwere applied to phospho-RTK arrays
Fig. 6 Effect of Tyro3 knock-down on cell signaling and cell growthin MCF-7 and MCF-7-NR lines. a On Day 0, cells were treated withTyro3 siRNA. On Day 1, cells were treated with the indicated drugs for6 h before being lysed and immunoblotted for phosphorylated S6K,Akt, and ERK1/2 and cyclin D1. Blots were then stripped and re-probed for β-actin as a loading control. b Mechanism of MCF-7-NR’sescape from IGF-1R-dependent control of cell growth and expressionof Tyro3 and cyclin D1. c Cells grown in 10 % FBS-containing mediafor 24 h with and without 1 μM everolimus or 3 μM NVP-AEW541were lysed and immunoblotted for Tyro3, phospho- and total-S6K,after which blots were stripped and re-probed for β-actin as a loadingcontrol. The immunoblot was quantified by densitometry. Drugs ap-plied were plotted on the x-axis, and level of each phospho-protein wasplotted on the y-axis as the average of ratio to untreated control.Standard deviation from repeated experiments is shown as error bars.d On Day 0, cells were treated with Tyro3 or negative control siRNA.On Days 1 through 4, cells were subjected to serial MTS assay withand without NVP-AEW541. Daily OD values are shown on the y-axis.Each data point represents the mean value and standard deviation of 6–12 replicate wells
b
298 Invest New Drugs (2013) 31:293–303
TKI, combined with 3 μM NVP-AEW541, and found thatthe combination failed to overcome acquired resistance toNVP-AEW541 in MCF-7-NR cells when evaluated usingthe MTS assay (data not shown). With regard to Tyro3,phosphorylation remained high in MCF-7-NR cells regard-less of treatment with NVP-AEW541, while phosphoryla-tion was relatively low in MCF-7 cells (Fig. 5).
Contribution of Tyro3 in resistance to NVP-AEW541
To determine the role of Tyro3 in acquired resistance toNVP-AEW541, we evaluated Tyro3 expression andknocked it down using siRNA in MCF-7 and MCF-7-NR(Fig. 6a). Baseline expression of Tyro3 was higher in MCF-7-NR than parental MCF-7. Treatment with NVP-AEW541resulted in reduced Tyro3 expression and S6K phosphory-lation only in MCF-7, and not in MCF-7-NR (Fig. 6a). Twoclones of Tyro3 siRNA successfully inhibited expression ofTyro3 in both MCF-7 and MCF-7-NR. Interestingly, theexpression levels of Tyro3 appeared in parallel with that ofcyclin D1, a key G1-S cell cycle modulator (Fig. 6a).
Based on the finding that only in MCF-7 Tyro3 expres-sion was inhibited by NVP-AEW541, accompanied by in-hibition of S6K phosphorylation, we next tested the effect ofeverolimus on Tyro3 expression in MCF-7 and MCF-7-NR.Treatment with everolimus resulted in reduced phosphory-lation of S6K and expression of Tyro3 in both MCF-7 andMCF-7-NR to a similar degree, suggesting that Tyro3 ex-pression is regulated in a S6K-dependent manner (Fig. 6band 6c).
In serial MTS assay, slowing of growth rate with 3 μMNVP-AEW541 was observed only in MCF-7, and not inMCF-7-NR (Fig. 6d), findings consistent with those inWestern blot (Fig. 6a). Further, two clones of Tyro3 siRNAinhibited both MCF-7 and MCF-7-NR (Fig. 6d), findingsagain consistent with those in Western blot (Fig. 6a).
Taken together, these findings suggested that cyclin D1expression is regulated in an S6K/Tyro3-dependent mannerin MCF-7 even before developing resistance to NVP-AEW541, at least in part, and that the disconnection be-tween IGF-1R/Akt and S6K in MCF-7-NR may allow thecells to maintain cyclin D1 at a high level even in thepresence of NVP-AEW541, and to thereby become resistantto it (Fig. 6b).
Discussion
In the present study, we identified a mechanism of acquiredresistance to the IGF-1R inhibitor NVP-AEW541 whichinvolves persistent IGF-1R/Akt-independent S6K activationin the presence of NVP-AEW541. We also found that S6Kregulates Tyro3 expression and that Tyro3 in turn regulates
cyclin D1 expression, such that the disconnection betweenIGF-1R/Akt and S6K enables MCF-7-NR to maintain highlevels of cyclin D1 in the presence of NVP-AEW541. Thesefindings explain resistance to IGF-1R, at least in part(Fig. 6b).
While we noted equal inhibition of Akt phosphorylationby NVP-AEW541 between MCF-7 and MCF-7-NR lines,S6K phosphorylation was unaffected by the compound onlyin MCF-7-NR cells (Fig. 2). We also demonstrated that theAkt inhibitor perifosine inhibited phosphorylation of S6Kand cellular growth to a lesser extent in MCF-7-NR than inMCF-7 cells, despite observations of a similar trend in Aktphosphorylation suppression between the two cell lines(Fig. 3). Taken together, these data suggest a disconnectionbetween Akt and S6K in MCF-7-NR.
A previous study showed that prostaglandin F2 (PGF2)in luteal cells stimulates TSC-2 phosphorylation, therebyleading to activation of S6K in an Akt-independent andERK-dependent manner [21]. However, we found thatTSC-2 expression and phosphorylation levels in MCF-7-NR cells were similar between MCF-7 and MCF-7-NRlines, and that phosphorylation of TSC-2 was equallyinhibited by NVP-AEW541 in both lines (Supplementalfigure 2). Further, no differences were found in phosphory-lation levels of the Akt substrate PRAS40 or Rheb, a targetof TSC-2 GAP activity, between MCF-7 and MCF-7-NRlines (Supplemental figure 2). Other reported mechanismsof Akt-independent mTOR/S6K activation include S6K ac-tivation by the ternary complex of FKBP 12-rapamycin-associated protein and S6K mediated by p85 PI3K regula-tory subunit [22] and Bcr-Abl-driven mTOR/S6K activationvia phospholipase C-γ1 (PLC-γ1) in leukemia cells [23].Additional mechanisms of Akt-independent S6K phosphor-ylation in MCF-7-NR are currently being investigated in ourlaboratory.
Supporting the importance of mTOR-S6K signaling indeveloping acquired resistance to NVP-AEW541, we foundthat the mTOR inhibitor everolimus with and without NVP-AEW541 inhibited cellular growth equally in both MCF-7and MCF-7-NR lines (Fig. 4b). Further, treatment witheverolimus alone increased Akt phosphorylation in both celllines (Fig. 4a), likely due to positive feedback [24], suggest-ing that downstream S6K rather than Akt itself is a keymediator in controlling cellular growth in these lines. Thesefindings are consistent with those of our previous study,which found that the in vitro growth inhibitory effect oftrastuzumab was more closely correlated with inhibition ofphosphorylation of S6K than of Akt in HER2-amplifiedbreast cancer cells [25]. Further, promising efficacy wasobserved in phase II trials on administration of everolimuscombined with trastuzumab in HER2-positive metastaticbreast cancer patients who experienced disease progressionduring or after trastuzumab therapy [26]. These findings
300 Invest New Drugs (2013) 31:293–303
support the notion that mTOR/S6K signaling plays an es-sential role in cellular growth in breast cancer and raises thepossibility that loss of mTOR/S6K signal control by RTKsmay be a common mechanism of acquired resistance toRTK-targeted therapy.
In the present study, we observed the contribution of thenovel RTK Tyro3, also known as Dtk or Sky, to acquiredresistance to NVP-AEW541. Tyro3 is part of a receptortyrosine kinase subfamily known as the “Tyro3, Axl, andMer (TAM)” subfamily. TAM subfamily members havebeen shown to be involved in oncogenic activities such asproliferation [27], anti-apoptosis [27, 28], and migration[29–31]. Among TAM subfamily members, Axl has beenthe most closely studied, and researchers have extensivelyexamined this protein’s involvement in the mechanisms ofacquired resistance to cytotoxic chemotherapeutic agents inseveral human cancers, including myeloid leukemia [32, 33]and lung adenocarcinoma [34, 35]. Very few studies havereported the involvement of Tyro3 in upstream regulation ofsolid tumors [36–38], however, and no study has reportedS6K-dependent Tyro3 expression or its contribution to re-sistance to TKIs. However, a recent preclinical study dem-onstrated that alternative signaling from Axl was able toinduce resistance to lapatinib in HER2-amplified breastcancer cells [20], suggesting that signals from TAM sub-family members might contribute to acquired resistance tosmall molecule RTK-Is more commonly than presumed.
Several limitations of this study warrant mention. First,the use of only one pair of parental and acquired-resistancecell lines only for NVP-AEW541 precludes much general-ization of the results. Although we found only MCF-7 to besensitive to NVP-AEW541 among 16 lines tested previous-ly, several other studies have detected similar sensitivity inother lines [39–41]. Development of an acquired-resistancemodel out of these cell lines may aid in determining whetheror not our present findings are a general phenomenon.Additionally, while many other IGF-1R TKIs are underclinical development [42], it is not known if the findingsof our current study are applicable to acquired resistance tothese compounds. Further, the lack of in vivo experiments inour study limits the clinical applicability of our findings.
Second, because we did not use a cloning process toestablish MCF-7-NR, the cell line potentially involves mul-tiple clones with different resistance mechanisms. Cloningfrom a single cell suspension of MCF-7-NR may allow thedifferentiation of different mechanisms.
Third, while MCF-7-NR showed higher Tyro3 expres-sion than MCF-7, suggesting an enhanced role of Tyro3 incell growth when cells acquire resistance to NVP-AEW541,the role of Tyro3 in primary resistance to NVP-AEW541and its potential as a new therapeutic target remain to beclarified. When we exploratory screened Tyro3 expressionin 6 other breast cancer cell lines, defined in our previous
study as NVP-AEW541 resistant cells [17], various expres-sion levels were observed (Supplemental figure 3).
Fourth, consistent with previous studies which focusedon the effect of IGF-1R inhibitors, including ours [17], wedid not add supplemental estradiol in any experiments inthis study. However, MCF-7 is known to be an estrogen-responsive cell line and several studies have suggested thatestradiol might potentiate IGF-1R signaling through upre-gulation of IGF-1R or IRS-1 in the cell line [43, 44].Therefore, the use of supplemental estradiol might havechanged our findings.
In summary, IGF-1R/Akt-independent activation ofmTOR/S6K by an as-yet-undefined mechanism appears toinduce acquired resistance to NVP-AEW541. This is at leastpartially explained by the fact that in both MCF-7 and MCF-7-NR expression of Tyro3 and subsequently cyclin D1 iscontrolled in an S6K-dependent fashion, such that IGF-1R/Akt-independent activation of mTOR/S6K in MCF-7-NRmaintains high levels of cyclin D1 in the presence ofNVP-AEW541. Consistently, we found that the mTOR in-hibitor everolimus may have therapeutic value in overcom-ing this resistance. Although the validity of these findingsrequires confirmation in further preclinical and clinical tri-als, our observations may lead to individualized use ofNVP-AEW541 and the development of “back-up drugs”against tumors that acquire resistance to NVP-AEW541.
Acknowledgment This study was supported by the Global Centersof Excellence Program (H.M.), Grant-in-Aid for Scientific Research(C) (T.M.) and Grant-in-Aid for Young Scientists (B) (T.M) from theMinistry of Education, Culture, Sports, Science and Technology ofJapan, and Research Grant from Takeda Science Foundation (T.M).
Conflict of interest The authors declare that they have no conflict ofinterest.
References
1. Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, BajamondeA, Fleming T, EiermannW,Wolter J, PegramM, Baselga J, Norton L(2001) Use of chemotherapy plus a monoclonal antibody againstHER2 for metastatic breast cancer that overexpresses HER2. N EnglJ Med 344:783–792
2. Paez JG, Janne PA, Lee JC, Tracy S, Greulich H, Gabriel S,Herman P, Kaye FJ, Lindeman N, Boggon TJ, Naoki K, SasakiH, Fujii Y, Eck MJ, Sellers WR, Johnson BE, Meyerson M (2004)EGFR mutations in lung cancer: correlation with clinical responseto gefitinib therapy. Science 304:1497–1500
3. Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA,Brannigan BW, Harris PL, Haserlat SM, Supko JG, Haluska FG,Louis DN, Christiani DC, Settleman J, Haber DA (2004) Activat-ing mutations in the epidermal growth factor receptor underlyingresponsiveness of non-small-cell lung cancer to gefitinib. N Engl JMed 350:2129–2139
4. Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD,Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA, Singer S,Janicek M, Fletcher JA, Silverman SG, Silberman SL, Capdeville
Invest New Drugs (2013) 31:293–303 301
R, Kiese B, Peng B, Dimitrijevic S, Druker BJ, Corless C, FletcherCD, Joensuu H (2002) Efficacy and safety of imatinib mesylate inadvanced gastrointestinal stromal tumors. N Engl J Med 347:472–480
5. Kobayashi S, Boggon TJ, Dayaram T, Janne PA, Kocher O,Meyerson M, Johnson BE, Eck MJ, Tenen DG, Halmos B(2005) EGFR mutation and resistance of non-small-cell lung can-cer to gefitinib. N Engl J Med 352:786–792
6. Tamborini E, Bonadiman L, Greco A, Albertini V, Negri T, GronchiA, Bertulli R, Colecchia M, Casali PG, Pierotti MA, Pilotti S (2004)A new mutation in the KITATP pocket causes acquired resistance toimatinib in a gastrointestinal stromal tumor patient. Gastroenterology127:294–299
7. Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C,Park JO, Lindeman N, Gale CM, Zhao X, Christensen J, Kosaka T,Holmes AJ, Rogers AM, Cappuzzo F, Mok T, Lee C, Johnson BE,Cantley LC, Janne PA (2007) MET amplification leads to gefitinibresistance in lung cancer by activating ERBB3 signaling. Science316:1039–1043
8. Pollak MN, Schernhammer ES, Hankinson SE (2004) Insulin-likegrowth factors and neoplasia. Nat Rev Cancer 4:505–518
9. Maiso P, Ocio EM, Garayoa M, Montero JC, Hofmann F, Garcia-Echeverria C, Zimmermann J, Pandiella A, San Miguel JF (2008)The insulin-like growth factor-I receptor inhibitor NVP-AEW541provokes cell cycle arrest and apoptosis in multiple myeloma cells.Br J Haematol 141:470–482
10. Scotlandi K, Manara MC, Nicoletti G, Lollini PL, Lukas S, BeniniS, Croci S, Perdichizzi S, Zambelli D, Serra M, Garcia-EcheverriaC, Hofmann F, Picci P (2005) Antitumor activity of the insulin-likegrowth factor-I receptor kinase inhibitor NVP-AEW541 in muscu-loskeletal tumors. Cancer Res 65:3868–3876
11. Jin Q, Esteva FJ (2008) Cross-talk between the ErbB/HER familyand the type I insulin-like growth factor receptor signaling pathwayin breast cancer. J Mammary Gland Biol Neoplasia 13:485–498
12. Huang X, Gao L, Wang S, McManaman JL, Thor AD, Yang X,Esteva FJ, Liu B. Heterotrimerization of the growth factor receptorserbB2, erbB3, and insulin-like growth factor-i receptor in breastcancer cells resistant to herceptin. Cancer Res 70:1204–1214
13. Ibrahim YH, Yee D (2005) Insulin-like growth factor-I and breastcancer therapy. Clin Cancer Res 11:944s–950s
14. Shimizu C, Hasegawa T, Tani Y, Takahashi F, TakeuchiM,WatanabeT, Ando M, Katsumata N, Fujiwara Y (2004) Expression of insulin-like growth factor 1 receptor in primary breast cancer: immunohis-tochemical analysis. Hum Pathol 35:1537–1542
15. Chang Q, Li Y, White MF, Fletcher JA, Xiao S (2002) Constitutiveactivation of insulin receptor substrate 1 is a frequent event inhuman tumors: therapeutic implications. Cancer Res 62:6035–6038
16. Rocha RL, Hilsenbeck SG, Jackson JG, VanDenBerg CL, Weng C,Lee AV, Yee D (1997) Insulin-like growth factor binding protein-3and insulin receptor substrate-1 in breast cancer: correlation withclinical parameters and disease-free survival. Clin Cancer Res3:103–109
17. Mukohara T, Shimada H, Ogasawara N, Wanikawa R, ShimomuraM, Nakatsura T, Ishii G, Park JO, Janne PA, Saijo N, Minami H(2009) Sensitivity of breast cancer cell lines to the novel insulin-like growth factor-1 receptor (IGF-1R) inhibitor NVP-AEW541 isdependent on the level of IRS-1 expression. Cancer Lett 282:14–24
18. Liu P, Cheng H, Roberts TM, Zhao JJ (2009) Targeting the phos-phoinositide 3-kinase pathway in cancer. Nat Rev Drug Discov8:627–644
19. Lu Y, Zi X, Zhao Y, Mascarenhas D, Pollak M (2001) Insulin-likegrowth factor-I receptor signaling and resistance to trastuzumab(Herceptin). J Natl Cancer Inst 93:1852–1857
20. Liu L, Greger J, Shi H, Liu Y, Greshock J, Annan R, Halsey W,Sathe GM, Martin AM, Gilmer TM (2009) Novel mechanism of
lapatinib resistance in HER2-positive breast tumor cells: activationof AXL. Cancer Res 69:6871–6878
21. Arvisais EW, Romanelli A, Hou X, Davis JS (2006) AKT-independent phosphorylation of TSC2 and activation of mTORand ribosomal protein S6 kinase signaling by prostaglandin F2al-pha. J Biol Chem 281:26904–26913
22. Gonzalez-Garcia A, Garrido E, Hernandez C, Alvarez B, JimenezC, Cantrell DA, Pullen N, Carrera AC (2002) A new role for thep85-phosphatidylinositol 3-kinase regulatory subunit linkingFRAP to p70 S6 kinase activation. J Biol Chem 277:1500–1508
23. MarkovaB, Albers C, Breitenbuecher F,Melo JV, Brummendorf TH,Heidel F, Lipka D, Duyster J, Huber C, Fischer T. Novel pathway inBcr-Abl signal transduction involves Akt-independent, PLC-gamma1-driven activation of mTOR/p70S6-kinase pathway. Onco-gene 29:739–751
24. Engelman JA (2009) Targeting PI3K signalling in cancer: oppor-tunities, challenges and limitations. Nat Rev Cancer 9:550–562
25. Kataoka Y, Mukohara T, Shimada H, Saijo N, Hirai M, Minami H.Association between gain-of-function mutations in PIK3CA andresistance to HER2-targeted agents in HER2-amplified breast can-cer cell lines. Ann Oncol 21:255–262
26. Nahta R, O’Regan RM. Evolving Strategies for Overcoming Re-sistance to HER2-Directed Therapy: Targeting the PI3K/Akt/mTOR Pathway. Clin Breast Cancer 10:S72–78
27. Shiozawa Y, Pedersen EA, Patel LR, Ziegler AM, Havens AM,Jung Y, Wang J, Zalucha S, Loberg RD, Pienta KJ, Taichman RS.GAS6/AXL axis regulates prostate cancer invasion, proliferation,and survival in the bone marrow niche. Neoplasia 12:116–127
28. Weinger JG, Gohari P, Yan Y, Backer JM, Varnum B, Shafit-ZagardoB (2008) In brain, Axl recruits Grb2 and the p85 regulatory subunit ofPI3 kinase; in vitro mutagenesis defines the requisite binding sites fordownstream Akt activation. J Neurochem 106:134–146
29. Gjerdrum C, Tiron C, Hoiby T, Stefansson I, Haugen H, Sandal T,Collett K, Li S, McCormack E, Gjertsen BT, Micklem DR, AkslenLA, Glackin C, Lorens JB. Axl is an essential epithelial-to-mesenchymal transition-induced regulator of breast cancer metas-tasis and patient survival. Proc Natl Acad Sci U S A 107:1124–1129
30. Li-Ping Z, Da-Lei Z, Jian H, Liang-Quan X, Ai-Xia X, Xiao-Yu D,Dan-Feng T, Yue-Hui Z. Proto-oncogene c-erbB2 initiates ratprimordial follicle growth via PKC and MAPK pathways. ReprodBiol Endocrinol 8:66
31. Scutera S, Fraone T, Musso T, Cappello P, Rossi S, Pierobon D,Orinska Z, Paus R, Bulfone-Paus S, Giovarelli M (2009) Survivaland migration of human dendritic cells are regulated by an IFN-alpha-inducible Axl/Gas6 pathway. J Immunol 183:3004–3013
32. O’Bryan JP, Frye RA, Cogswell PC, Neubauer A, Kitch B, ProkopC, Espinosa R 3rd, Le Beau MM, Earp HS, Liu ET (1991) axl, atransforming gene isolated from primary human myeloid leukemiacells, encodes a novel receptor tyrosine kinase. Mol Cell Biol11:5016–5031
33. Hong CC, Lay JD, Huang JS, Cheng AL, Tang JL, Lin MT, LaiGM, Chuang SE (2008) Receptor tyrosine kinase AXL is inducedby chemotherapy drugs and overexpression of AXL confers drugresistance in acute myeloid leukemia. Cancer Lett 268:314–324
34. Li Y, Ye X, Tan C, Hongo JA, Zha J, Liu J, Kallop D, Ludlam MJ,Pei L (2009) Axl as a potential therapeutic target in cancer: role ofAxl in tumor growth, metastasis and angiogenesis. Oncogene28:3442–3455
35. Lay JD, Hong CC, Huang JS, Yang YY, Pao CY, Liu CH, Lai YP,Lai GM, Cheng AL, Su IJ, Chuang SE (2007) Sulfasalazinesuppresses drug resistance and invasiveness of lung adenocarcino-ma cells expressing AXL. Cancer Res 67:3878–3887
36. Zhu S, Wurdak H, Wang Y, Galkin A, Tao H, Li J, Lyssiotis CA,Yan F, Tu BP, Miraglia L, Walker J, Sun F, Orth A, Schultz PG,Wu X (2009) A genomic screen identifies TYRO3 as a MITF
302 Invest New Drugs (2013) 31:293–303
regulator in melanoma. Proc Natl Acad Sci U S A 106:17025–17030
37. Sun WS, Fujimoto J, Tamaya T (2003) Clinical implications ofcoexpression of growth arrest-specific gene 6 and receptor tyrosinekinases Axl and Sky in human uterine leiomyoma. Mol HumReprod 9:701–707
38. Sun WS, Fujimoto J, Tamaya T (2003) Coexpression of growtharrest-specific gene 6 and receptor tyrosine kinases Axl and Sky inhuman uterine endometrial cancers. Ann Oncol 14:898–906
39. Hagerstrand D, Lindh MB, Pena C, Garcia-Echeverria C, Nister M,Hofmann F, Ostman A. PI3K/PTEN/Akt pathway status affects thesensitivity of high-grade glioma cell cultures to the insulin-like growthfactor-1 receptor inhibitor NVP-AEW541. Neuro Oncol 12:967–975
40. Guerreiro AS, Boller D, Shalaby T, Grotzer MA, Arcaro A (2006)Protein kinase B modulates the sensitivity of human neuroblastoma
cells to insulin-like growth factor receptor inhibition. Int J Cancer119:2527–2538
41. Attias-Geva Z, Bentov I, Fishman A, Werner H, Bruchim. IInsulin-like growth factor-I receptor inhibition by specific tyrosinekinase inhibitor NVP-AEW541 in endometrioid and serous papil-lary endometrial cancer cell lines. Gynecol Oncol
42. Weroha SJ, Haluska P (2008) IGF-1 receptor inhibitors in clinicaltrials–early lessons. J Mammary Gland Biol Neoplasia 13:471–483
43. Molloy CA, May FE, Westley BR (2000) Insulin receptorsubstrate-1 expression is regulated by estrogen in the MCF-7human breast cancer cell line. J Biol Chem 275:12565–12571
44. Maor S, Mayer D, Yarden RI, Lee AV, Sarfstein R, Werner H, PapaMZ (2006) Estrogen receptor regulates insulin-like growth factor-Ireceptor gene expression in breast tumor cells: involvement oftranscription factor Sp1. J Endocrinol 191:605–612
Invest New Drugs (2013) 31:293–303 303