Evidence- Based Practice - Johns Hopkins Medicine
-
Upload
khangminh22 -
Category
Documents
-
view
1 -
download
0
Transcript of Evidence- Based Practice - Johns Hopkins Medicine
EBP: Best Practices for Completing Root Cause Analysis (RCA) of Hospital Acquired Pressure Injury Stage 3 or Greater (HAPI 3+)
Helen Borte BSN, RN, BMTCN; Retzer Cariaga, DNP, MPH, RN; Holley Farley, MSN, RN; Rachel Moseley, MS, BSN, RN, CWON, APHN; Alphie Rahman, DNP, APRN, CNS, CCRN; Lindsay Rice, BSN, RN, CWCN; Allison Spingler, Esq., RN; Cynthia A Walker, MSN, APRN-CNS, CWON
The Johns Hopkins Hospital, Johns Hopkins Bayview Medical Center
IntroductionA root cause analysis (RCA)provides insight into practice andprocess that may shed light oncorrectable systems issues aimedat prevention of future patientharm. At JHHS, varyingaccountability structures andprocesses for completing an RCAfor HAPI 3+ existed. A teamcollaborated to conduct an EBPreview using the JHEBP Model toharmonize the process withinmultiple system entities.
MethodsWhat are best practices forcompleting RCA for HAPI 3+?
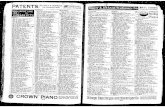
Per literature review:• Total results: 97• Total after title screen: 12• Total after abstract screen: 9• Total after appraisal: 6• 6 articles included in evidence:
3 level IIIA, 3 level IIIB
ResultsCreation and implementationof a collaborative revised HAPI3+RCA process, with standardizedtools to guide the user on tieredLevel A, Level B, and Level Cassessments, including:• Type of information/chart
review required• Role/stakeholders involved in
each review level• Timeframes for completion
Discussion
This process was translated intopractice at JHHS with JHM HAPI3+ RCA Toolkit intranet site. Thistoolkit contains:• Process Map• Instructions with Fast Facts• RCA forms for each level A, B,
and C RCA• Flyer• Implementation
presentation• Recorded webinar
Level A RCA
•All HAPI 3+•Unit Rep•Within 4 Days
Level B RCA
•Unit WTA or Champion•Within 7-10 Days•Validated by Wound Nurse
Level C RCA
•Led by Patient Safety, Risk Mgmt., and Quality Improvement
•Within 60 Days
Synthesis
The literature revealed a tiered approach toperforming a RCA with different levels ofinvestigation. These tiers, or levels, are based uponseverity of injury and preventability. This processincludes identifying and engaging differentstakeholders for each level, escalating as neededbased upon findings from the previous level, anddeveloping a corrective action plan as indicated.
An EBP Project: What is the Best Music Listening Intervention for Patients Recovering In the Post Anesthesia Care Unit (PACU)?
Patricia Anne Bulacan BSN RN CCRN;Maria Liza Anicoche MSN RN ACNS-BC CPAN CAPA: Marie Kelly Webber MSN RN M.MUS, MA.T Integrated Music;
Laura Kaiser MSN RN CPAN; Sylvia Urso BSN RN; Ivy Mendoza BSN RN; Rollie Asperin BSN RN CPAN CAPA
Perioperative Services, The Johns Hopkins Hospital, Baltimore, MD
ResultsIntroduction
In the Weinberg PACU, patients who were having laparoscopic radical prostatectomies experience severe pain which caused them to have an increase length of stay and excessive amounts of opioids. Additionally, these patients had high levels of anxiety due to potential urinary incontinence and sexual dysfunction from the surgery. Perianesthesia nurses questioned what complementary evidence could support a non-pharmacologic approach to reducing anxiety and post-operative pain.
The aim of the study was to determine the best music listening intervention for patients recovering in the PACU.
Practice QuestionWhat is the best music listening intervention comparing
preferred patient – selection music versus relaxation breathinginstructional narrative over minimalistic hypnotic music forpatients recovering in the PACU?
Search StrategyThe literature search yield 1006 articles and only 20 were
appropriate articles that met our PICO criteria. The evidencesearch strategy range from 2012-2020. The data basesearches were PUBMED, CINAHL, Jonna Briggs Institute, andCochrane Review data bases were searched. The key meshterms used were: music, music listening, music therapy,intervention, surgery, PACU, post-operative, randomizedcontrolled trials, anxiety, pain and pain management.
Level and Quality of Appraised Evidence
Text Box, tables or figures
SynthesisMusic listening has been shown to attenuate SNS and activate
PSNS activities, resulting in a reduction of anxiety and improved relaxation in patients (Kavak et al., 2020). Pain and anxiety are most effectively controlled with music-listening during the pre-operative phase (Hole, Hirsch, Ball & Meads, 2015); preoperative anxiety can alter, inform, and intensify postoperative pain and medication requirements (Stamenkovic, Rancic, Latas, Neskovic, Rondovic & Wu, 2018). Additionally, music has consistently shown improved pain and anxiety management in post-operative settings (Poulsen & Coto, 2018). The synthesis of evidence revealed two evidence based music listening interventions: 1. Preferred music listening method and 2. relaxation breathing over minimalistic hypnotic music for therapeutic interventions to reduce anxiety and pain.
Recommendations for Translation into Practice The evidence recommends to conduct a randomized comparative clinical trial comparing two methods of music listening: patient preferred
music listening via Spotify versus relaxation breathing narrative over minimalistic music. The study should identify the best cost- effective music listening intervention to decrease patient’s anxiety and post anesthesia pain management.
ReferencesKavak Akelma, F., Altınsoy, S., & Arslan, M. T. (2020). Effect of favorite music on postoperative anxiety and pain. Der Anaesthesist, 69, 198–204. Bojorquez, G., Jackson, K. & Andrews, A. (2020). Music therapy for surgical patients: Approach for managing pain and anxiety. Critical Care Nursing Quarterly, 43, 81-85. Watts, S., Leydon, G. & Birch, B. (2014) Depression and anxiety in prostate cancer: A systematic review and meta-analysis of prevalence rates.BMJ Open, 4:e0 Gelatti, F., Viganò, C., Borsani, S., Conistabile, L., & Bonetti, L. (2020). Efficacy of live versus recorded harp music in reducing preoperative stress and fear related to minor surgery: A pilot study. Alternative Therapies in Health & Medicine, 26(3), 10–15 Peng, C.S., Baxter, K., & Lally, K.M. (2019). Music intervention as a tool in improving patient experience in palliative care. American Journal of Hospice and Palliative Medicine, 36(1): 45–49. Hole, J., Hirsch, M., Ball. E. & Meads, C. (2015). Music as an aid for postoperative recovery in adults: A systematic review and meta-analysis. Lancet, 386:1659-71. Poulsen, M. & Coto, J. (2017). Nursing music protocol and postoperative pain. American Society for Pain Management Nursing, 19(2): 172-176. Bradt, J., Dileo, C., & Shim, M. (2013). Music interventions for preoperative anxiety. The Cochrane database of systematic reviews, 6: CD006908. Ni, C.H., Tsai, W.H., Lee, L.M., Kao, C.C. & Chen, Y.C. (2012). Minimising preoperative anxiety with music for day surgery patients: A randomised clinical trial. Journal of Clinical Nursing, 21(5-6): 620-5. Mok, E., & Wong, K.Y. (2003). Effects of music on patient anxiety. AORN journal, 77(2), 396–410. Chen, L.., Wang, T.F., Shih, Y.N. & Wu, L.J. (2013). Fifteen-minute music intervention reduces pre-radiotherapy anxiety in oncology patients. European Journal of Oncology, 17: 436-441 Kipnis, G., Tabak, N., Koton, S. (2016). Background music playback in the preoperative setting: Does it reduce the level of preoperative anxiety among candidates for elective surgery? Journal of Perianesthesia Nursing, 31(3): 209–216.Uğraş, G.A., Yıldırım, G., Yüksel, S., Öztürkçü, Y., Kuzdere, M. & Öztekin, S.D. (2018). The effect of different types of music on patients’ preoperative anxiety: a randomized controlled trial. Complement Therapies in Clinical Practice, 31:158–163 McClurkin SL, Smith CD (2016) The duration of self-selected music needed to reduce preoperative anxiety. Journal of Perianesthesia Nursing, 31(3):196–208 Attias, S., Boker, L. K., Arnon, Z., Ben-Arye, E., Bar'am, A., Sroka, G., Matter, I., Somri, M., & Schiff, E. (2016). Effectiveness of integrating individualized and generic complementary medicine treatments with standard care versus standard care alone for reducing preoperative anxiety. Journal of Clinical Anesthesia, 29: 54-64.
Author (Year)
Year Design/Method
Sample/Setting
Major Variables Studied & definitions Measurements & Data Analysis Results/Findings Evidence
6 American Academy of Pediatrics 2015 Conducted 50 year retrospective study (1961-2014) Evaluated risk of pediatric surgical patients’ morbidity/mortality Perioperative/Anesthesia Care Environment
Perioperative:Pre-Operative;Intra-Operative;Post Anesthesia Care Unit; Outside OR requiring anesthesia
Pediatric Preoperative Risk Factors Morbidity MortalityRespiratory ComplicationsCPR arrests
Pediatric surgical patients’ morbidity and mortality: infants 1 month-1 year have 4 times higher risk of anesthesia cardiac arrest than 1-18 years
AAP guiding principles:Facility/Medical staff policiesClinical privileges:Pain managementCompetency of anesthesia and nursing staff
Critical elements for the pediatric perioperative anesthesia environment. PediatricsLevel IV-A
1 American Society of PeriAnesthesia Nurses 2019 Evidence-based Pediatric Position Statement Perianesthesia nurses preoperative/ preanesthesia of children assessment
Nurses specializing in preparing children for surgery focus on respiratory system and airway management
Evidence-based interpretive statements Perianesthesia nurses will be knowledge in the assessment and care of the pediatric patient and their family
2019-2020 Perianesthesia Nursing Standards, Practice Recommendations and Interpretive Statements, 114-116Level IV-A.
32 Beck K 2012 Clinical review of risk factors in children with upper respiratory infections (URIs)
Pediatric surgical patients with “child-specific risk factors;” Surgery/anesthesia-specific risk factors”
Risk factors; type of surgery: URIs, co-existing pulmonary; Morbidity MortalityRespiratory Complications
Decision algorithm: child with URI presents to surgeryperioperative respiratory adverse events (PRAE)
Expert opinion: literature review: research studies, case studies, quality improvement studies, systematic reviews, clinical practice guidelines
Anesthesia in children with a cold.Pediatric AnesthesiaLevel IV-A
33 Brockmann PE, Bertrand P, Castro-Rodriguez JA 2014 Systematic Review of risk factors associated with asthma and obstructive sleep apnea
Electronic searches 968 citations with 17 studies selected; PRISMA format
Asthma, snoring, sleep disordered breathing (SDB), obstructive sleep apnea
Data extraction 17 articles: 13 not possible; 5 only asthma; 1 SBD; 3 same cohort studies
Children with asthma risk factor more likely to have habitual snoring and SDB
Influence of asthma on sleep disordered breathing in children: A systematic review. Sleep MedicineLevel III-A
24 Chattopadhyay S, Rudra A, Sengupta S 2013 Clinical review of risk factors for laryngospasm after anesthesia
Anesthesia and PACU settings with children Common airway complication and potentially like-threatening
Occurs most often on emergence; 10-fold increase in second hand smoke exposure
Risk factors include: Age – infants and young children, higher ASA, upper respiratory infection (URI)
Laryngospasm in paediatric anaesthesia: A review. Int J Anes ResLevel V-A
35 Chiswell C, Akram Y 2018 Systematic review conducted with the PRISMA guidelines with the two authors
6875 titles identified for eligibility; 28 fitting relevant review; studies identified and 15 studies qualified for the systematic review
Children 0-22 years, mean 5.8 yrs; Biologic and clinical outcomes;Levels of smokingOxygen desaturation, laryngospasms
Significant for 2.5 times likely for children to experience laryngospasms with exposure to second hand smoke
Environmental tobacco smoke exposure increases the risk of PRAE in the PACU and negative surgical outcomes
Impact of Environmental tobacco smoke exposure on anesthesia/ surgical outcomes in children: A systemic review and meta-analysis. Arch Dis Child Level III-A
2 Christensen R, Voepel-Lewis T, Lewis I, Ramachandran SK Malviya S
2013 United States retrospective review of the reported pediatric PACU patients’ morbidity and mortality from cardio-pulmonary arrests (CPAs) *Primary purpose to analyze the “nature of PACU arrests - Secondary purpose to describe pediatric survival following PACU CPAs
29 cases of CPA in the PACU; Ages birth to 17 yrs PACUs that reported pediatric CPR arrests (AHA CPA Registry)
Anesthesia-related pediatric CPR arrests in PACU:multicenter CPA registry - 27 cases;Children <5 yearsInfants < 1 year78% Underlying co-morbidities44% Respiratory most frequent
Descriptive statistics; Odds ratios with confidence intervals calculated survivors & Non-survivorsChi-Square, t-test, Mann-Whitney U-test; p value of <0.05 statisticallysignificant
27 CPA events: 67% in patients <5 years & 30% <1 years; Nonsurvival older age p<0.02Weekend occurrence p<0.01Nonpediatric setting p=0.02Occurrence at night p=0.04
Pediatric cardiopulmonary arrest in the postanesthesia care unit: Analysis of data from the AHA get with the guidelines –Resuscitation registry. Pediatric AnesthesiaLevel III-A
25 Cote V, Ruiz AG, Perkins J, Sillau S, Friedman NR 2015 Retrospective chart review 9038 patients under two years of age undergoing tonsillectomy under general anesthesia for obstructive sleep disordered breathing
Identify predictors of risk factors for upper airway obstruction complication postoperatively in the PACU
The odds of patients with syndromes or craniofacial anomalies were 11 times greater (p <0.0001) in this sample
Risk factors include: under 2 years of age, OSA severity, African-American, prematurity, daycare, Downs Syndrome
Characteristics of children under 2 years of age undergoing tonsillectomy for upper airway obstruction. Int J Ped Otorhinolaryngology Level III-A
26 Gleich SJ, Olson MD, Sprung J, Weingarter T N, Schroeder DR, Warner DO, Flick RP,
2012 100 severely obese children who were matched to normal weigh children undergoing tonsillectomies from January 1996 to December 31, 2005
100 Severely obese children 100 normal weigh children in Mayo Clinic having tonsillectomies
Age, BMIACo-morbidities:Reactive airway disorders, URISDB, Hypotonia;PACU respiratory complications
Frequencies with central tendencyTwo-tailed t test, p value< 0.05Multivariable logistic regression
PACU respiratory complications: airway obstruction, bronchospasm, aspiration, hypoxemia (<90% on room air) tracheal intubation
Perioperative outcomes of severely obese children undergoing tonsillectomy. Pediatric AnesthesiaLevel III-A
27 Graaff J C, Sarfo M, Wolfawinkel LV, Werff, DBM, Schouten ANJ
2015 Prospective Dutch study (January 2007 to August 2013); 20-item complication list (incidents affected safety of children under the care of the anesthesiologist) of critical events in 10 categories
The Netherlands pediatric anesthesia critical incidents voluntary reported occurred over a 6-year period of time with 1214 critical incidents reported
Pediatric respiratory emergencies, age infants less <1 year, ASA III and IV status, emergency proceduresDefined critical anesthesia events post surgeries
Sex: male 0.95ASA III/IV p <0.001Age: Infant p <0.001Urgency Surgery P <0.001
Respiratory events were the highest critical incidents reported; Higher incidence laryngospasmsInfants <1 year of age, ASA III & IV, emergency surgeries greatest risk for critical incidents
Anesthesia-related critical incidents in the perioperative period in children; a proposal for anesthesia-related reporting system for critical incidents in children. Pediatric AnesthesiaLevel III-A
28 Hampson-Evans D, Morgan P, Farrar M 2008 Pediatric expert opinion clinical article explored cause of pediatric laryngospasms
Collaborative anesthesia pediatric simulation project for pediatric anesthetists
Young children up to age 9 years correlated w/17 laryngospasm events in 1000 anesthetics
Exposure to URIs 96/1000 anesthetics; greater incidence with exposure to passive tobacco smoke
Risk factors include: young age, recent URI, exposure to cigarette smoke. obstructive lung or pulmonary disease,
Pediatric laryngospasm. Pediatric AnesthesiaLevel V-A
15 Horwood L, Nguyen H P, Brown K, Paci P, Constantin EC
2013 Retrospective cohort study.Canadian tertiary care center.
594 Children aged 0 to 18 years who underwentT&A at our institution from 2002 to 2006
Risk factor variables include: Obesity, asthma, neuro-muscular disease, pulmonary disease, airway & craniofacial abnormalities,
Evaluated: ethnicity and major PACU T&A respiratory complications for 23% of African American children preoperative sickle cell test (TestSC). Sensitivity 96%; Specificity 93%; PPV 77%
74 of 594 (12.5%)children experience major respiratory events; African American ethnicity is risk factor;Risk factors also reported in this cohort study:Age <2 yearsMale sexObeseModerate to severe OSA
African American ethnicity as a risk factor for respiratory complicationsfollowing adenotonsillectomy. JAMA OtolaryngologyLevel III-A
30 Hui JW, Ong J, Herdegen JJ, Kim H, Codispoti CD, Katantari V
2017 Retrospective reviewed of patients with risk factors diagnosed with polysomnogram (PSG) and chronic rhinoisinusitis (CRS) endoscopic surgeries
916 patients with CRS were evaluated for Obstructive sleep apnea (OSA)
Investigated the risk for OSA in White patients versus African American patients who had CSR
Adjusted odds ratio of 1.98 (95% CI), 1.19-3.29). Patients with CSR without nasal polyps were at higher risk for OSA – odds ratio 1.63 (95% CI, 1.02-2.61)
African American patients with CSR were at a significantly higher risk for OSA compared to white patients
Risk of obstructive sleep apnea in African American patients with chronic rhinoisinusitis.Ann Allergy Asthma ImmunolLevel III-A
23 Jones DT, Bhattacharyya N 2006 Prospective pediatric cohort underwent surgical procedures mask anesthesia; American Thoracic Society Children’s questionnaire on environmental and respiratory factors. Double-blinded outcomes to adverse airway events intraoperatively and PACU for patients with and without passive smoke exposure
Prospective cohort of 405 children who underwentsurgical procedures under mask anesthesia
Children exposed to second hand smoke and children not exposed to second hand smoke compared to those not exposed to second hand smoke. Children exposed to one cigaretteper day or exposed to smoking within the 12 months beforesurgery
Airway complications in PACU higher for all outcome measures for PSE children (allP < 0.005) PACU, breath holding (P < 0.086).Intraoperative laryngospasm and airway obstruction were 4.9 & 2.8 times more likely with PSE than non-exposure to PSE
Pediatric patients with passive smoke exposure have significantlyincreased rates of perioperative airway complicationsas compared with children without passive smokeexposure.
Passive smoke exposure as a risk factor forairway complications during outpatientpediatric procedures Otolaryngology–Head and Neck SurgeryLevel III-A
10 Kiekkas P, Stephanopoulos N, Bakalis N, Kefaliakos, A, Konstantinou E
2016 Systematic review inclusion criteria: January 1990-April 2014; Of 169 titles, 16 selected and 9 total studies included and appraised
Sample: patients aged 1-19 years;BMI > 85- 95 percentile
Search terms: obesity overweight, severe obesity, abdominal obesity, perioperative adverse respiratory events, hypoxemia, pediatric, children
Significant univariate and multivariate associations between obesity and overall perioperative adverse respiratory events (PARE)
Obesity was independently associated with PAREs and asthma, sleep-disordered breathing, and OSA
Perioperative adverse respiratory events in overweight/obese children: Systematic review. JoPAN, 31(1), 11-22Level III-A
9 Kurtz MP, McNamara ER, Schaeffer AJ, Logvinenko T, Nelson CP
2015 In 2012, queried the NSQIP data base for complications in 2871 children whose body mass index was above the 95th percentile and overweight > 85th percentile. (CDC definitions). Secondary descriptive statsMultivariate and odds ratio
Pediatric ages 2-18: investigated 2871 patients having genital, abdominal with/ without bowel involvement, surgeries.
BMIPediatric patients 2-18 yearsUrologic procedures; post-operative events
BMI significant risk factorBMI >85% percentile (Odds Ratio 1.36, CI 1.03-1.8, p=0.035; wound complications Odds ratio 2.36, CI 95%, 1.28-4.35, p=0.006
Results: Overweight/obese factors increased the odds of overall complications by 36% and of wound complications by 136%Conclusion: “BMI in the pediatric NSQIP urologic population found
Funded by National Institute of Diabetes, Digestive, and Kidney Diseases Assoc: Peds postoperative events: NSQIP. J Pediatric UrologyLevel II-A
29 Lee LK, Bernardo MK, Grogan TR, Elashoff DA 2017 Prospective study to validate COLDS score in 536 pediatric patients; multi variate regression to create an optimized score
536 pediatric patients under age of 6 years having sedation and/or general anesthesia
Patient risk factors: age (0-2 yr n=217,2-4 yr n=145, 4-6 yr n=174),male, ASA II, URI (n=139), lung disease,
PRAE = 17.8% (93 of 522 patientsCOLDS score predicted bronchospasm, oxygen desaturation, and beta-agonistic therapy; performed best in children under 2 years
COLDS score had potential to be valuable risk assessment tool for prediction of perioperative respiratory adverse events;Good predictive value potential for risk assessment perioperative respiratory adverse events.
Perioperative respiratory adverse event risk assessment in Children with upper respiratory tract infection: Validation of the COLDS score, Pediatric AnesthesiaLevel III-A
31 Lewanda AF, Matisoff A, Revenis M, Harahsheh A, Futterman C, Nino G, Greenberg J, Myseros J S, Rosenbaum KN, Summar M
2016 Expert clinical review article Downs syndrome children Cervical spine instability, cardiovascular abnormalities, pulmonary hypertension. Upper airway obstruction
Downs syndrome children have multiple anatomical and physiologic abnormalities predisposes them to respiratory complications
Downs syndrome risk factor places these children at greater risk for upper airway problem in the PACU
Preoperative evaluation and comprehensive assessment for children with Down syndrome. Pediatric Anesthesia Level V-A
3 Lian C, Xie Z, Wang Z, Li J, Huang C, Zhang J, Lu K, Li L, Zhu B, Ma D, Li J, Lian Q, Shang GW
2016 Retrospective study to analyze pediatric preoperative risk factors to predict postoperative ICU admissions and perioperative deaths
263,607 pediatric surgical patients from 1-14 years of age old in eight hospitals in China
1812 pediatric patients admitted to ICU postoperatively with variables: age, ASA physical status, prematurity, SPO2 and unfasted status
6626 admitted to ICU or died; Using multiple logistic regression analysis revealed age, ASA physical status, prematurity, SPO2 and unfasted status were independent risk factors
Study revealed that age, ASA physical status, SpO2 prematurity, and unfasted status are risk factors to predict postoperative ICU admission and death in pediatric patients.
Pediatric preoperative risk factors to predict postoperative ICU admission and death from multicenter retrospective study. Paediatric Anaesthesia, 26, 637-643
Level III-A
7 Malviya S, Voepel-Lewis T, Chiravuri SD, Gibbons K, Chimbira WT, Nafiu OO
2011 Risk Assessment Tool Descriptive statisticsNARCO is:N = NeurologicalA= AirwayR= RespiratoryC= CardiovascularO= Other
340 consecutive surgical cases were selected from a cohort of birth to 18 yr undergoinggeneral anesthesia with risk factors identify respiratory adverse events
Adverse events (AE), hospitallength of stay, admission status.
NARCO correlated with ASA-PS (r¼0.664; P<0.01) supporting its criterion validity.coefficients0.71–0.96; k 0.43–0.87
Measures of exact agreement were slightly better for NARCO compared with ASA-PS. Scores; correlated significantly with perioperative escalation of care, adverse events (AE), LOS
Preliminary psychometric evaluation ofnewly developed and specific measures of perioperative riskfor children using the NARCO. BJALevel III-A
20 Oofuvong M, Geater AF, Chongsuvivatwong V, Chanchayanon T, Sriyanaluk B, Saefung B, Nuanjun K
2015 12 month prospective matched cohort pediatric same day surgery study at a tertiary hospital in Thailand1.Compared excess hospital length of stay direct costs; who had complications; were admitted2.Compared indirect costs of parents loss of income due to missing work, transportation, hotelN= 430 subjects with 215 matched pairs
Prospective matched cohort study;430 children enrolled (215 matched pairs)Children less than 15 years of age undergoing anesthesia;Random selection outpatient surgery
Children less than 15 years of age; general anesthesia; ASA physical status;Outpatient surgery Length of stay(LOS); Hospital costs and indirect costs
Multivariate analysis; Odds ratio 2.56, 96% confidence interval for hospital stay after surgery; indirect costs 1.58, p=0.003
Results1.Thirty percent higher excess hospital costs; 58% higher indirect costs over the discharged ambulatory surgery2.Young age less than one year old3.Induction with propofol higher excess costs
Applicable to US. First study that looks at direct and indirect costs related to length of stay and respiratory events LOS excess costs; attributable to respiratory events in children. Anesthesia-AnalgesiaLevel III-A
8 Scherrer D, Mallory, MM, Cravero JP, Lowrie L, Hertzog JH, Berkenbosch JW
2015 Retrospective chart review on pediatric patients who had sedation for procedures; Descriptive statistics
28,792 patient records were eligible of which 5153 patients were obese (17.9%), predominately male
Procedural nursing interventions on obese children who more frequently required airway interventions: repositioning, suctioning, jaw thrust, airway adjuncts and bag-valve- mask
Multivariate regression analysis Results: Multivariate regression analysis demonstrated that obesity to be independently associated with minor and moderate respiratory adverse events.Obesity is an independent risk factor for adverse respiratory events
The impact of obesity on pediatric procedural sedation-related outcomes: Results from the pediatric sedation research consortium. Paediatric AnesthesiaLevel III-A
5 Subramanyam R, Yeramaneni S, Hossain MM, Anneken AM, Varughese A
2016 Perioperative respiratory adverse events in pediatric ambulatory anesthesia: Development and validation of a risk prediction tool.
19,059 patients from quality improvementdatabase. Predictor variables were age, sex, ASA physical status, morbid obesity, preexistingpulmonary disorder, preexisting neurologic disorder
Composite PRAE defined presence of any 1 of following PACU events:bronchospasm, apnea, laryngospasm, prolonged oxygen requirement.Development and validation of the risk prediction tool for PRAE
Model C-statistic and corresponding SE for validation cohort was 0.64 ± 0.01 and 0.63 ± 0.02, respectively. Sensitivity and SEof risk prediction tool to identify children at risk for PRAE 77.6 ± 0.02 in the derivationcohort and 76.2 ± 0.03 in validation cohort.
Predictor variables were: age <3 yr, sex, severe obesity, ASA II & III physical status, pre-existing pulmonary disorder, preexisting neurologic/ neuromuscular disorders
Perioperative respiratory adverse events in pediatric ambulatory anesthesia: Development and validation of a risk prediction tool. Anesthesia and AnalgesiaLevel III-A
12 Thongyam A, Marcus CL, Lockman JL, Cornaglia MA, Cardoff A, Gallagher PR, Shults J, Traylor JT, Rizzi MD, Elden L
2014 One of few prospective, observational cohort studies evaluating the relationship between children who had polysomnograms (PSG) with post- operative complications.
Relationship between 369 children PSG and <3 years obesity, severe obstructive sleep apnea (SOSA).
The authors present different professional medical OSA guidelines: ASA, AAP and American Academy of Otolaryngology Head and Neck Surgery
Measurement reported in percentages; Odds ratios. Respiratory events: laryngospasm bronchospasm, hypoxemia, hypercapnia with critical interventions.
Results: Respiratory most frequent cause of CPAs; Recommend RRT’s in PACU; African American children higher risk respiratory complications “craniofacial structure”, ventilatory drive, exposure to environmental allergens
Predictors of Perioperative resp complications in adenotonsillectomy for obstructive sleep apnea: A prospective study. Otolaryngology Head Neck SurgeryLevel III-A
4 Von Ungern-Sternberg, BS, Ramgolam A, Hall GL, Sly PD, Habre W
2015 Immunological (IgE) markers improve prediction of PRAE. Children 1 month to 16 years with URI, wheezing, asthma, hay fever, exposure to second hand smoke. Venous blood samples taken at time of IV insertion
119 Children aged 1 month - 16 years with URI, wheezing previous history of asthma, hay fever, exposure to second hand smoke. Exclusion cardiac disease.
Children with risk factors: URIs, wheezing previous history of asthma, hay fever, exposure to second hand smoke
Screen by asking parents about H&P risk factors compared to Biomarkers (IgE blood levels) Correlated adverse respiratory events Analyzed binary logistic regression and Receiver operating characteristic (ROC) curve analysis. SPSS version 22
Results reported that identification of risk factors (exposure second hand smoke exposure, asthma, hay fever, URIs) were superior to using IGE serum markers. Also the more risk factors children had the greater the prediction of respiratory adverse events
Peri-operative adverse respiratory events in children. AnesthesiaLevel III-A
32 White KK, Bompadre V, Goldberg MJ, Bober MB, Cho T, Hoover-Fong JE, Irving M et al.
2017 Delphi Method used to author this consensus practice guideline to improve the clinical outcomes in the perioperative management of skeletal dysplasia patients
Expert opinion of a panel of 13 multidisciplinary international experts for the two round Delphi study
Preoperative assessment of patients’ risk factors: Second round of the Delphi study identified perioperative assessment and management EBP guidelines for the skeletal dysplasia patients
PACU providers should be prepared to manage airway issues- difficulty with cervical spine mobility; laryngotracheal malacia;Respiratory – obstructive lung disease; snoring, OSA; abnormalities of the bronchial tree
Best practices in peri-operative management of patients with skeletal dysplasias. Am J Med GenetLevel IV-A
P = Surgical patientsI = Music listeningC = Comparing preferred music vs relaxation/breathing music O = Music listening outcomes: Decrease anxiety and improve pain management
Developing Nurse Preceptors: Why It Matters?Grace Carter, MSN, RN, CPN1; Kelly Lykens, BSN, RN, CPN11; Lisa Smith, MSN, RN2; Jackie Bradstock, BSN, RN, PCCN3; Linda Fair, MAS, RN, CCRN-CMC3;
Periwinkle Mackay, MSN, RN, CCRN4 ; Heather Watson, Ph.D., MSN, RN5; Madeleine Whalen, MSN/MPH, RN, CEN5
1 JH Bloomberg Children’s Center, 2 Bayview Medical Center, 3 Johns Hopkins Hospital, 4 Suburban Hospital, 5 Johns Hopkins Health System
BackgroundPreceptor programs across the Johns Hopkins Health System are highly variable. There is no standardization of Preceptor selection Training Ongoing education Validation of competency skills.These inconsistencies can adversely affect: the preceptor program itself the nurses who serve as preceptors the training and retention of newly
hired nursesPreceptors are critically important to the success of new nurses and for succession planning within the nursing profession.
MethodsExtensive literature review using the Johns Hopkins EBP Model focused on: Best practices for hospital-based nursing
preceptor programs Development Ongoing support Essential competencies
Of initial 2273 articles, 115 were appraised and synthesized to generate recommendations
RecommendationsHigh-level features of the evidence includes the following recommendations: Standard criteria for preceptor selection A structured preceptor training program On-going preceptor support including
continuing education & peer support networks
Structured tools, checklists, and pathways for preceptors to use as teaching guides, with clear expectations for preceptors and preceptees
Preceptor scheduling allowing adequate time for teaching, skill development, evaluation, and paperwork while providing patient care.
A standard process for preceptor evaluation and feedback
Preceptor recognition, rewards and/or compensation
Next StepsA robust preceptor program can reduce levels of: Preceptor burnout Inadequately prepared nurses Inconsistent nursing practices Staff turnover Cost of training/hiring
Level III n=54
Level IV n=1
Level V n=52
Level II n=7
Level I n=1
Present findings to CNO’s Prepare to publish to professional journal Design materials/resources for the program Create a low-risk pilot preceptor program Evaluate data from low-risk pilot program If successful, standardize across JHHS
What are the best practices for establishing and
maintaining a hospital-based nursing preceptor
program?
Reference List available upon request from [email protected]
EBP: Best Practices in Clinical Nurse Peer FeedbackKelly Connor, MSN, RN, NPD-BC; Patty Dawson, MSN, RN; Elizabeth Gabriel, BSN, RN, RN-BC; Kim Kuperman, MSN, RN, NPD-BC;
Catherine Lindauer, DNP, RN, CEN; Joanna Little, BSN, RN, RNC-NIC, C-ELBW; Karin Nevius, MSN, RN, CCRN-K; Linda Sayre, MS, RN, NE-BC;Amy Sawyerr, MPH, BSN, RN, RNC-LRN; Stephanie Wilmer, MSN, RN
Johns Hopkins Health System
IntroductionGiving and receiving peer feedback is aprofessional responsibility and is anANCC©, Magnet Recognition Program®requirement at all levels of nursing practicefrom bedside to CNO. Currently across theJHHS there is variation in how peerfeedback is collected and shared with directcare nursing staff. This project aimed todefine a harmonized, evidence-basedstrategy for peer feedback at the clinicalnurse level.
Methods
ResultsPeer feedback should reflect AmericanNurses Association (ANA) guidelines: apeer is someone of the same rank, istimely and continuous, used for learning,not anonymous and considers thenurse’s developmental level. The use ofpeer feedback should include writtenguidelines with a standardized tool, andcan be applied at mid-cycle ofevaluation.
DiscussionDevelop and pilot a harmonizedelectronic clinical nurse peer feedbacktool and process across the 6 JH affiliatehospitals for full implementation in theFY22 mid-year evaluation cycle. Mid-year peer feedback gives nurses theopportunity to enhance theirprofessional development goals beforethe annual review. The tool should beautomated, reflect key performancestandards of the clinical nurse role andinclude written guidelines. Education willneed to focus on non-anonymous natureand use in developing professionaldevelopment goals.
PICO: What are the best practices forimplementation of clinical nurse peerfeedback in inpatient and outpatientsettings to establish and sustain programuptake?
Literature Search:• Total Results: 700
Total Results after title screen: 52• Total after Abstract screen: 23• Total after appraisal: 12• 12 articles included in evidence: Level
IIIB=1; Level IIIC=1; Level VB=7; Level VB/C or C=3
The literature revealed that nursing peer feedback should reflect ANA guidelines:
A peer is someone of the same rank Peer feedback is practice-focused Is timely, routine, and continuous Fosters a continuous learning culture
of patient safety and best practice Feedback is not anonymous Incorporates the nurse’s
developmental level
Best Practices for Identifying Sex Trafficking Among Patients Visiting the Adult Emergency DepartmentEmma Crabo, MSN, RN, DNP-C; Leah Eickhoff, MSN, RN; Jazzolynn Kelly, MSN, RN, MPH, DNP-C; Heather Zimmie, MSN, RN;
Diana Baptiste, DNP, RN, CNE; Nancy Goldstein, DNP, ANP-BC, RNC, CNE; Barbara Maliszewski, MS, RN, NEA-BC
Introduction & Background PICO Question Recommendations for Practice
• Growing prevalence of sex trafficking (ST) in the U.S. (Figure 1)• Up to 88% of trafficked persons visit the Emergency Department
(ED) during captivity • Health care professionals (HCP) not identifying ST patients• Current screening tools have high rate of false negatives• ST screening and education not standardized
How does the implementation of multi-faceted screening models for sex trafficking in adult
emergency departments, versus use of standardized lists of screening questions,
improve identification of sex trafficked patients?
Key Findings and Results
Search Methodology
Methods and Procedures
We would like to thank our clinical facility for their guidance, and Tatiana Baiza and Nicole Bilger for input into the project.
• Half of female ST victims have visited the ED• Screening tools should be regionally tailored• Multifaceted approach yields better outcomes than simple
screening tool• Standardized list of screening questions is insufficient to identify
ST• HCPs must prioritize comfortability of patients, recognize
indicators, evaluate medical needs, and be prepared to deploy resources
• Improved ST identification through HCP training
Recommendations for Future Research
• Use of silent notification tools • Translation of validated screening tools into other languages• Design of multi-faceted screening tools for ST • Effectiveness of current screening tools• Value of teaching strategies for HCPs and ED personnel
Acknowledgements
References available upon request
Databases used: PubMed, CINAHL, Embase, Scopus, Web of ScienceSearch terms: Emergency Service, Hospital” OR "emergency room" OR "emergency unit" OR "emergency department*" OR "emergency service" OR "emergency ward*" OR "accident & emergency" OR "accident and emergency" OR "A&E" AND "Mass Screening" OR screen OR identify AND "Human Trafficking” OR "human traffic" OR "sex traffic*" OR "people traffic*" OR "trafficking in sex" OR "trafficking in people”Inclusion criteria: Peer-reviewed journals; English only; Published in 2016 or later
Best practices for ST screening in adult EDs Topic of Interest
Literature search for information relevant to PICO question
Literature Search
Through Covidence, 170 articles identified; team analysis resulted in 12 publications
Review & Analysis
Synthesis yielded recommendations on best-practice approach to ST screeningSynthesis
Findings consolidated and presentedPresentation
Dissemination to adult EDs; increase detection, treatment, and referral of ST victims
Future Application
Implement mechanism for ST detection
Invest in multifaceted screening tool
Build rapport with patients before asking safety
questions
Provide ST-specific trainings
Figure 1. Trafficked victims most likely to be used for sexual exploitation
Background Conclusions
Design and Methods
Recommendations
Results
Results
Problem:• Pressure injury (PI) is high, ranging from 18% to 29.5% among
cardiac surgery patients (Rao et al., 2016).• The Johns Hopkins Hospital CVSICU rarely achieve benchmark.• ICU LOS >5-7 days accounted for >66.7% of the PI in the
CVSICU over the last year.• Sacral deep tissue injuries (DTI) were the most prevalent.Aim:• To reduce the incidence rate of pressure injury in the CVSICU by
5% over a 10-week period using a bundle of best-practices.
Study Design: Single group, pre-post, evidence-based practice (EBP)Duration: 10 weeksEBP Bundle of Interventions:1. Pre-op screening2. Air-fluidized specialty bed for “highest risk” patients3. Standardized prevention tool4. Weekly wound rounds by wound champions5. Education to CVOR and CVSICU staff
• Wound treatment savings= ~ $373,610 over 10 weeks (Padula et. al, 2018). 1-year projection: $1,941,628.00.
• Screening tool & standardization early, patient-centered interventions.
• “Prevention” costs increased, however we decreased “treatment” costs.
• Insurance reimbursement may improve over the long-term. • More research is needed:
1. Screening tool validation (population-specific)2. Prevention: Short-term & long-term phases
Study Limitations:• Project design non-experimental, randomized.• Screening tool lacked validation for validity and reliability.• COVID-19 ECMO population included in screening population,
although not truly “cardiac surgery” in origin.
Tim Madeira, DNP, CRNP, APRN-CNS, CCRN, PCCN; Ashley Coco, RN, BSN; Nancy Sujeta, RN, BSN, WOCN; Jessica Groom, RN, BSN, WOCN; Scott Burkett, BSIE, CSSBB; Mary Beth Riegel, MSN, RN, CNOR; Carla Aquino, DNP, RN
Pressure Injury Prevention in Cardiac Surgery Using Risk Factor Assessment and Standardization
The Johns Hopkins Hospital – Cardiovascular Surgical Intensive Care Unit (CVSICU)
Control Chart of Pressure Injury Defects By Project Phase• Screen all pre-operative patients for risk factors.• Use air-fluidized specialty beds as a prevention tool.• Use sacral bordered silicone foam dressings on all patients.• Use silicone-based foam dressings to pressure points.• Implement weekly wound rounds with a champion group.• Educate & intervene across the OR and ICU phases of care.
Pressure Injury Count By Project Phase
59%
59% pressure injury incidence rate reduction from baseline to intervention
Almost 1 out of 3 patients screened positive as
“high risk”
Significant reduction p=0.009
Exploring Best Practices in Ethics Rounds in the Surgical ICUAshly Nealon, RN, BSN
Department of Surgery, The Johns Hopkins Hospital, Baltimore, MD
ResultsIntroductionPatients, family members and staffoften face complex ethicalchallenges related to patient care,communication and moral distressin the Intensive Care Unit.
Multidisciplinary Ethics roundswere instated in the SICU toidentify and address issues relevantto the health, wellbeing and safetyof all patients and staff.
Practice QuestionWhat are the best practices foridentifying ethical concerns in theadult inpatient SICU population?
Evidence Level & Quality
SynthesisThe complexity of patient care in the ICU can leadto uncertainty about goals of care and prognosis.As trusted clinicians, nurses share theresponsibility of maintaining a practiceenvironment that fosters safe, quality patient care.
Research shows that effective approaches forinterprofessional ethics education of ICU cliniciansare lacking. However, regular ethics rounds havebeen found to help staff feel valued, decreasemoral distress, and help clinical staff gain a betterunderstanding of ethical concepts and language.
Incorporating clinical ethics support services hasbeen shown to help staff improve ethicalcompetence, build trust among clinicians and getissues resolved earlier.
Recommendations for Translation into Practice Recommendations include proactive multidisciplinary ethics rounds in the ICU setting; inclusionof demographic data including code status, decision making capacity, advanced directives andemergency contacts in the ICU daily goals checklist; and staff education around ethical language,principles and resources. Continued research and quality improvement projects arerecommended to address ethical concerns and staff resilience.
References & Search Strategy
Using Evidence-Based Practice to Prevent Unintentional Retained Foreign Objects (URFOs)
Mary Beth Riegel, MSN, RN, CNOR
The Johns Hopkins Hospital – Cardiovascular Thoracic Operating Room
Results
Introduction• An unintentional retained foreign object (URFO) is an item
used during a surgical procedure left in the patient after theincision is closed. These items include sponges, needles,instruments, and fragments of these items.
• The physical, emotional, and economic consequences to thepatient brought on by URFOs result from pain, infections,obstructions, reoperations, increased hospital length ofstays, readmissions, disability, and loss of time from work.Healthcare institutions are impacted financially by lawsuitsand the loss of revenue from second party payers (AORN,2020).
• The Joint Commission has identified retained surgical itemsas a sentinel event, which is a patient safety event thatresults in severe, temporary harm, permanent harm, ordeath (TJC, 2013).
Practice Question• The Johns Hopkins Hospital (JHH) has recently seen an
increase in the incidences of URFOs throughout the hospitalduring fiscal year 2020 compared to fiscal years 2018 and2019. In the CVT OR, there were three documented URFOsduring CY 2019.
• As part of the hospital’s yearly quality and patient safetygoals, URFO incidence needed to decrease in the JHH ORs.
• Using evidence-based practice, what changes in processesor practices could be made to decrease the incidence ofURFOs.
Search Strategy• This literature search was done through the WelchWeb
Digital Library at Johns Hopkins.• The databases searched included CINAHL Plus, PubMed,
Scopus, and the Cochrane.• The time frame used was January 2010 through February
2020.• The following keywords were used: retained surgical items,
surgical count procedure, surgical instruments, foreignbodies, postoperative complications, adjunct technology,and human error. Combinations of these keywords werealso used to decrease the number of results.
Level and Quality of Included Evidence• All articles had to be research studies or systematic reviews. There was no
randomized control research related to URFOs because it would be unethical toinflict harm as a result.
• Additional inclusion criteria were studies related to URFOs in the OR, the countingprocess, causative factors, and adjunct technology.
• Exclusion criteria included studies done in procedural areas or labor and delivery andthose involving broken catheters, guidewires, or instruments.
• The twenty articles were summarized using The Johns Hopkins Evidence-BasedPractice Model Individual Evidence Table.
• Of the twenty studies, nineteen were quantitative, and one was qualitative. Inaddition, three articles were a meta-analysis of prior studies done. All were rated asa IIIA or IIIB for strength and quality.
Synthesis• This review has shown that there are a multitude of studies
related to URFOs with more research being done by nurses.• In the past, research has concentrated on the incidence of
URFOs, identifying risk factors, and the clinical manifestations.The more recent research emphasizes human factors and theprevention of errors during the counting process, and the useof adjunct technology to identify URFOs before the incision isclosed.
• Since the incidence of URFOs is very low, the sample sizeswere smaller, and the direct causation of variables cannot beproven.
• Many studies relied on reporting the event to TJC, a hospital,or a database making it susceptible to selection bias.
Recommendations for Translation into Practice The following were identified as actions needed to minimize contributing factors associated with the incidence of URFOs:
• implement a standardized, evidence-based URFO policy and annual education competencies for all staff across all Johns Hopkins Medical System ORs and procedural areas to standardize the counting process;
• initiation of a URFO Procedure Checklist when a miscount is identified so reconciliation is consistent throughout the ORs;• implementation of a Root Cause Analysis (RCA) with the surgical team involved in a URFO or near-miss within 24 to 48 hours to identify the causes or
possible strategies for prevention and track on the Perioperative Dashboard;• in collaboration with the Armstrong Institute, initiate Speed Feedback Sessions with the Cardiac OR team so they can practice communication, feedback
skills in addition to speaking up; and• investigate the pros and cons of the use of adjunct technology.
References
Conner, R. (Ed.). (2020). Guidelines for perioperative practice 2020.Denver, CO: Association of Perioperative Registered Nurses (AORN).
Edel, E. M. (2012). Surgical count practice variability and the potentialfor retained surgical items. AORN Journal, 95(2), 228-238.
The Joint Commission (2013). Preventing unintended retained foreignobjects. The Joint Commission Sentinel event Alert, 51. Retrievedfrom https://www. Joint commission.org/en/resources /patient-safety-topics /sentinel-event/
Kleiner, C., Link, T., Maynard, M. T., & Carpenter, K. H. (2014).Coaching to improve the quality of communication duringbriefings and debriefings. AORN Journal, 100(4), 358-368.
Norton, E. K., Martin, C., & Micheli, A., J. (2012). Patients count on it:An initiative to reduce incorrect counts and prevent retainedsurgical items. AORN Journal, 95(1), 109-120.
Steelman, V.M. (2019). Retained Surgical Items: Evidence Review andRecommendations for Prevention. AORN Journal, 110(1), 92-96.
Nurse-Driven Telemetry Removal ProtocolDarshani Samaroo, BSN, RN, Clinical Team Lead & Regina Morales, BSN, RN, Clinical Manager
3800 Acute Medical Telemetry Unit, Suburban Hospital/Johns Hopkins Medicine, Bethesda, MD
Results
Introduction and Description of the Problem
Appropriateness of telemetry, alarm weariness and a shortage of telemetry-ready beds prompted two clinical nurses to investigate the feasibility of creating a nurse-driven telemetry protocol. Anecdotally the impression was patients stayed on telemetry until discharge without clear criteria for why telemetry was initiated and when it could be removed. Additionally, concern was expressed about the over-monitoring leading to alarm fatigue and desensitization.
Practice QuestionWill the implementation of an evidence-based nurse-driven telemetry removal protocol facilitate timelier discontinuation of telemetry and reduce alarm fatigue?
Search StrategyA literature review was conducted spanning 2015-2020. Databases accessed were ProQuest, CINAHL Plus, Cochrane, Embase, and PubMed, and Scopus. The main search concepts included nurse-driven, telemetry removal, alarm fatigue, telemetry criteria, telemetry standards. Six articles were found relating to our question.
Level and Quality of Included Evidence
The literature review did not yield high quality results. All six articles were level 5A-B. One article represented American Heart Association guidance on telemetry indications. The remaining articles were non-research and were quality improvement initiatives.
SynthesisThere is clear guidance on criteria for telemetry monitoring. Quality improvement projects targeted removal protocols for the purpose of reducing alarm fatigue, reducing inappropriate telemetry use, reducing overall expenditures, and reducing unnecessary monitoring. Literature demonstrates using multimodal interventions that include indication based ordering, automatic discontinuation, routine review of use and appropriateness, and education offer the organization the benefits of cost savings and assurance of telemetry availability. Evidence also suggests alarm fatigue is associated with overuse of telemetry. Establishment of clear protocols will lead to fewer monitored patients, fewer alarms, and a reduction in alarm weariness.
Recommendations for Translation into Practice
Evidence exists that initiation of clear protocols will guide practitioners on appropriateness of telemetry and could also offer a framework for removal of monitoring. Empowering nurses to use an evidence based tool for removal can assist in reduction of alarms, over use of monitoring, and a potential cost savings.
ReferencesPerrin, K., Ernst, N., Nelson, T., Sawyer, M., Pfoh, E., & Cvach,
M. (2017). Effect of a nurse-managed telemetry discontinuation protocol on monitoring duration, alarm frequency, and adverse patient events. Journal of Nursing Care Quality, 32, 126-133. DOI:10.1097/NCQ.0000000000000230
Yeow, R., Strohbehn, G., Kagan, C., Petrilli, C., Krishnan, J., Edholm, K., …Pahwa, A. (2018). Eliminating inappropriate telemetry monitoring: an evidence-based implementation guide. JAMA Intern Med., 178, 971-978. DOI:10.1001/jamainternmed.2018.2409.
Flanders, K. & Hudson, Z. (2020). Appropriate use of telemetry in the acute care setting. Nursing Management, 51, 44-51. DOI:10.1097/01.NUMA.0000659452.24567.3b.
Compliance Strategies for Completion of Essential Hygiene Protocols in Pediatric Oncology Population Cristina Suarez MSN, RN, CPHON, CPN, Lindsay Jones BSN, RN, CPN, CHPPN, Nicole Robertson BSN, RN, CPHON, Jean Bruce MSN, RN, CPON, Cheryl Shepherd MBA, BS, RN, CPHON, Kara Dixon, BSN, RN, CPN. Cancer and Blood Disorder Institute, Johns Hopkins All Children’s Hospital, St. Petersburg FL
The Centers for Disease Control reports Central Line Associated Bloodstream Infections (CLABSI’s) are responsible for thousands of deaths each year and increased length of stay and cost. Over 50% of children with hematologic malignancies experience infection during treatment (Bailey et al., 2009). Evidence supports a reduction in CLABSIs by implementing essential hygiene protocols (daily baths, twice daily tooth brushing, sodium bicarbonate rinses and lip balm and oral moisturizer Kemp et al., 2019). In our unit, we have found that compliance with these essential hygiene protocols is difficult to maintain.
What are the best strategies to ensure compliance of the essential hygiene protocols in the pediatric oncology population on a daily basis?
Practice Question (PICOT)
Introduction
Search StrategiesA thorough literature search was performed using CINAHL Plus, PubMed, and Cochrane Database. The literature review included quality improvement projects, peer reviewed journals, and published protocols for oncology patients. Current best practices at other national children’s hospitals were also examined (Kemp et al., 2019).
Synthesis
Recommendations
Bailey, L., Reilly, A.F, & Rheingold, S. R (2009). Infections in pediatric patients withhematologic malignancies. Seminars in Hematology, 46, 313–324. https://doi.org/10.1053/j. seminhematol.2009.03.010Central line-associated bloodstream infection (CLABSI). (2019, April 19). Centers for Disease Control. https://www.cdc.gov/hai/bsi/bsi.htmlKemp, G., Hallbourg, M., Altounji, D., & Secola, R. (2019). Back to basics: CLABSI reduction through implementation of an oral care and hygiene bundle. Journal of Pediatric Oncology Nursing, 36(5), 321-326. https://doi.org/10.1177/1043454219849583Linder, L. A., Gerdy, C., Abouzelof, R., & Wilson, A. (2016). Using practice-based evidence to improve supportive care practices to reduce central line–associated bloodstream infections in a pediatric oncology unit. Journal of Pediatric Oncology Nursing, 34(3), 185-195. https://doi.org/10.1177/1043454216676838
Level and Quality of Included Evidence
There is a lack of published research that addresses how to consistently complete daily oral/hygiene protocols in the pediatric oncology population. A barrier that was identified determined that these tasks are often delegated to the family members to increase parental involvement in care, however parental compliance is often not ideal as key elements are time and again missed or excluded entirely (Linder et al., 2016). Key elements often missed included mouth rinses, tooth brushing, and bathing.
Due to the lack of evidence/recommendations for increasing compliance of these hygiene protocols, and the identified barrier with parental involvement after the implementation of the Patient & Family Agreement, we are proposing the implementation of a dedicated hygiene tech in this population to promote the completion and compliance of the essential hygiene protocol. The tech would perform the essential hygiene protocols, encourage parental participation, and reinforce patient/parent education as appropriate.
The level of evidence evaluated included one quality improvement project (Level 5) and one evidence-based practice project (Level 5).
References
Mentoring Practice Based LeadersHeather Watson, Ph.D., MSN, RN, Jennifer Zeller, MS, CRNP, Lynn Thomas, MSN, RN, NRP, CCRN, CCEMTP, Erin Tobat, MSN, RN,
CCRN-CSC, Meghan Schott, BSN, RN, and Sarah Trandel, DNP, FNP-BCJohns Hopkins Health System, UM St. Joseph Medical Center, Luminis Health AAMC, TidalHealth Peninsula Regional MC,
UM St. Joseph Medical Center, Johns Hopkins Health System
ResultsIntroductionMentorship is well recognized as a key element for professional development in nursing. Mentorship can be defined as the guidance provided by a mentor, especially by an experienced person in an organization.
• Historically tend to be self-selected with no formalized structure
• Students and graduate nurses have pseudo mentors more focused on clinical skills
• Practice settings and organizations lack mentoring structure for leadership skills and career development
Practice QuestionThe purpose of our project was to explore the experiences of nurses regarding mentorship and conduct an Evidence-based literature review to answer the PICO question, “What are best practices for mentoring nurse leaders in a practice setting?”
Search StrategyArticles were included if published within the last 10 years, peer reviewed, and written in English. Databases searched included CINAHL, PubMed, and Cochrane. Search terms included nurse mentoring and mentorship and mentors, hospital mentorship for nurses, mentoring for clinical practice nurses, mentoring for advance practice nurses, NOT students, NOT new graduates, NOT faculty.
Summary of the LiteratureThe literature consisted of primarily Level 3 and Level 5 articles which revealed-• Lack of consistent best practices for mentoring
nurses in leadership within the clinical practice setting
• Mentorship is valued and supported • Benefits of a mentoring program include
1. Effective communication2. Coping skills3. Increased confidence4. Job satisfaction5. Retention6. Problem solving
• A formalized approach using theoretical frameworks and validated tools is well received
• Mentors are described as experts, senior, or experienced, and could be from within or external to the chain of command
References
After reviewing the literature, it is apparent that whilementorship is important for the professional development ofnurse leaders in clinical settings, further research is necessaryto understand the key components needed to develop asustainable leader mentoring model. We offer the followingrecommendations based on the results of the literaturereview and the survey, including over 200 comments providedby nurses in clinical settings.
Survey Results
317 Articles
identified, removed 3 duplicates, 314 titles reviewed
79 Abstracts screened, 19 articles underwent full review
13 Articles included 2 Research 2 Opinion 6 QI 3 Reviews
A 16 question survey was administered in both academic and non-academic health care settings. There were 11 multiple-choice questions and 5 open ended questions. The survey targeted experienced nurses and those with joint appointments. We excluded new graduates and students. We received 98 responses, and of those, 44 completed the open ended questions.
Scan QR code for Survey Questions
0
10
20
30
40
50
60
70
80
Do you have a mentor(s)? Formal organizational mentoring?Yes No
Characteristics of Nurse Leaders Surveyed (N=98)
%Years of Experience
< 10 1911-20 24>20 55
RoleClinical Nurse 42Director/CNO 14APRN 4Other 25
Education LevelAssociates Degree 4Bachelors Degree 33Masters Degree 50Doctorate Degree 11
Length of Mentorship (n=44)< 3 years 50.53-5 years 13.25-10 years 5.6Other 30
Q12• Assigned• Happened organically• Asked
Q13
• Time • Not knowing who or what to
ask for • No one available
Q14• Professional Growth• Support• Transitioning to new roles
Q15• Reciprocal learning• Advancement opportunities• Support
Q16• Good communicator• Patience• Knowledgeable
Open Ended Themes (n=44)“Throughout my career, I have sought out nurses who have qualities I admire, or skills I would like to develop and have asked a lot of questions. I guess a barrier would be no formal structure for this process, but that also allows flexibility and ability to "adopt" several mentors for different purposes.”
“The newly promoted nurse relies on guess-work as to who to go to for support, and may not accurately identify areas in which he/she needs to grow and develop. Often people new to a role say they "don't know what they don't know". A formal mentorship program would help focus efforts to grow nurses, rather than a hit or miss approach.”
Develop or adapt a paired mentor model for practice settings
The model should be specifically for leadership development
Mentors should be chosen based on attributes as well as experience
Provide time for mentorship to occur
Base the mentorship model on leadership competencies
Educate nurses on mentoring value
Scan the QR code for references.
We acknowledge the guidance and support from the UM Nurse Leadership Institute in the development of this project.
Discussion
Maternal Child Health – OB , Johns Hopkins Bayview Medical Center, Baltimore, MDIntroduction
Problem Statement:Nursing documentation of infant feeding times, LATCH score, and stool assessment do not meet regulatory best practice standards leading to increased incidences of formula supplementation and delay of discharge
Lean MethodsDefine: key metric is % shifts with feeding assessment documentation meeting expectations benchmark 95%Measure: 30 chart audits/month for infants>34 weeks on couplet careAnalyze:• Engaged staff “your ideas are the best ideas”• Engaged leadership in system improvement • Identified Waste (time studies)• Managed the Project
• CUSP team• A3
Improve:• Staff education and visual cues• Newborn Nursery interdepartmental
workgroup• Audits/Accountability
• 1st deficit emailed care team • 2nd deficit staff member audits 3
charts with CUSP team member• 3rd deficit manager conversation
Control/Sustainability • Educating Travelers and new staff• Celebrate successes, perfect charts - Applause• Quarterly audits
ResultsIncreased total number of shifts with feeding assessment documentation meeting expectations at or near 95% benchmark.
DiscussionLean processes helped to engage leadership and staff in this improvement project. Staff was eager to participate as evidenced by a 50% increase in CUSP membership. An A3 and data tracking graphs illustrated progress towards the goals. Accountability was the biggest factor in changing culture and meeting the benchmark. Developing the CUSP team’s working understanding of Lean tools and principles sets the stage for better management of future projects.
Lean methods were successfully used to change unit culture
around infant feeding assessment and documentation.
Accountability was the key!
0.000
0.200
0.400
0.600
0.800
1.000
1.200
Oct-19 Nov-19 Dec-19 Jul-20 Aug-20 Sep-20 Oct-20 Nov-20 Dec-20 Jan-21 Feb-21 Mar-21 Apr-21 May-21 Jun-21
% shifts with documentation
Feeding Times Latch Stool
Lean Management of Infant Feeding Assessment
Susan Aronson BSN RNC-OB c-EFM , Katharine Giancola MSN RN IBCLC CPPS c-EFM c-ONQS
Audi
t Too
l
Bedside Report ImplementationJessica Barkdoll, MS, RN, CVRN-BC, Cora Lehet MSN, RN, CNL, Allison Wells, BSN, RN
BackgroundPatient safety events with IV drips, central
lines, and procedural sites on a 32-bed cardiac telemetry/IMC unit indicated a need for
consistent nursing report to include assessment of these items.
Aim of the Project
Interventions• BSR team created
• BSR/safety check in-services
• Hybrid BSR- IMC safety checks only
• Streamlined report
• BSR video presented to staff
• 8 successful BSR audits required for entire
unit- a Success Factor goal
• Nursing leadership & BSR team members
performed 25 audits
Data Collection and Analysis
• Pre-survey of nurses
• HERO system event review
• Success Factor goal compliance
• Leadership audit compliance
Implications for Practice
Lessons Learned
Full bedside implementation versus slow introduction via hybrid method led to program success
Unit leadership support is pivotal for achievement of BSR
Results• Pre-survey revealed 73% of RNs
did not want to change existing report
• HERO data identified multiple good catches during BSR
• 100% of RNs received a rating of “meets expectations” or higher for Success Factor goal
• Improved compliance resulted in a new unit culture
Offgoing RN
Oncoming RN
Report in patient’s room?
YesNoNeeded reminder
Hourly rounding card adjusted appropriately?
YesNoNeeded reminder
Fall Status relayed/bed alarm checked
YesNoN/A
Lines/tubes/wounds/post-procedure siteschecked
YesNoUnable to assess
White board updated with oncoming RN name?
YesNo
Drips double-checked scanned for handoff in MAR
YesNoN/A
Department of Medical Nursing, Johns Hopkins Hospital, Baltimore, MD
Improve communication, accountability, patient satisfaction,
and patient safety by initiating a standardized report style utilizing bedside report (BSR) with
safety checks
References by request
BSR can lead to identification of
patient safety events and improves
communication between the RNs and
patients/family members
Effectiveness of Novel Instructional Methods for Fire Drills in the Perioperative Environment: A Quality Improvement Project.
Nechama Brilliant, BSN, RN, CNOR, Jamelia Maher, BSN, RN, CNOR & Sheila Sanariz, MSN, RNPerioperative Department, The Johns Hopkins Hospital, Baltimore, MD
ResultsBackgroundCreate a robust learning experiences to support competencies and engage staff to retain knowledge of emergency protocols for fire safety in the perioperative environment.
Aim of the ProjectThe aim of the project is to explore novel instructional methods that fit best with the delivery of fire drill exercises. It reviews staff’s knowledge for managing fires in the perioperative environment, fire safety and emergency protocols.
Description of the Intervention• Reviewed current literature.• Chose a game-based learning to
incorporate. • Formulated an escape room and
a scavenger hunt.• Team facilitators identified for each unit
and provided instructions.• Representatives from HEIC and
Perioperative educators served as a resource during the fire drill.
• A survey was distributed to the staff to evaluate the effectiveness of the activity.
Description of Data Collection and AnalysisFire escape room activity evaluation was created using Microsoft Forms which include demographics, level of satisfaction with the activity and degree to which learning needs were met. The survey was distributed to staff following the activity. The survey was analyzed using automated settings of Microsoft Forms. Themes were extracted from the qualitative portion of the survey.
Implications for PracticeFires that occur in the operating room remain in the high risk, low frequency, and time sensitive category. It is imperative to explore creative ways to engage staff to retain vital information such as policies, procedures and location of emergency equipment for managing fire safety in the perioperative environment.
Lessons LearnedTo ensure success of the project, validate technical aspects of the project and provide clear written instructions explaining the mechanics of the game, rewards and role of each team member.
ReferencesAssociation of Perioperative Nurses (AORN). (2021).
Environment of care: fire safety. AORN Guidelines for Perioperative Practice. Retrieved from http://online.statref.com/Home/Resolve?id=54383&grpalias=JHU
Malicki,A., et. al. (2020). Gamification in nursing: an integrative literature review. Journal of Con. Educ. In Nursing. 51(11). 509-515.
The Joint Commission (TJC, 2021). General requirements-clinical impact LS.02.01.10. Retrieved from General Requirements - Clinical Impact | The Joint Commission
Outcomes Measures or Results• There were a total of 45 responses.• Largest group of participants have more than ten years of
clinical experience. • 73% of respondents were nurses. • Participants rated their level of satisfaction:
o Overall rating of 4.2/5 when compared to previous year’s activity.
o 84% of staff strongly agreed or agreed that the activity met their learning needs.
o 15% of the staff were undecided.
Team working together to solve puzzle in escape room Fire Drill Escape Room Kit
Emergency Debriefing in PCCU Quality Improvement Shelby Cahill, BSN, RN & Marcus Dyson, MBA
Progressive Cardiac Care Unit, The Johns Hopkins Hospital, 1800 Orleans St. Baltimore, MD 21
IntroductionPrompt delivery of high-quality cardiopulmonary resuscitation (CPR) can dramatically improve survival outcomes. The Johns Hopkins Hospital’s (JHH) Progressive Cardiac Care Unit (PCCU) is dedicated to providing quality care support by evidenced based practices
After reevaluating our processes, we recognized: • The sporadic nature of our data collection• Post-CODE feedback to staff was delayed by weeks• Rapid-response teams (RRTs) events received little to
no feedback.
This project aims to demonstrate how the implementation of a debriefing tool and consistent feedback can improve emergency culture, patient outcomes, and staff engagement.
Methods• ACLS Champion was identified
• The “PCCU Post-Emergency Debriefing Tool,” a form used to detail the emergency event, express the need for follow-up, and surface any concerns was created
• Within the same shift of a CODE/RRT response, the charge nurse would invite PCCU staff, providers, pharmacy and any other key member involved to participate in a feedback discussion, all of which include the successes, learning opportunities, and gratitude using the new debriefing tool
• The Lead Clinical Nurse would further investigate the “CPR Report Cards” and annotate performance deficiencies compared against the American Heart Association’s (AHA) “Get With the Guidelines”
• Afterwards, the reviewing nurse would then distribute an email to the PCCU staff with the following: a summary of the event, the “CPR Report Cards,” the team’s performance compared to guidelines, any learning opportunities and he summary of the debriefing, including the gratitude for the team’s efforts
• The Emergency Management Committee (EMC) was created to implement and enforce debriefing compliance
Results
DiscussionBy providing consistent post-emergency debriefings and feedback PCCU saw:• Enhanced information-sharing • Guideline awareness and compliance• Gained staff trust • Improvement in CPR performance during
emergencies
Post-emergency debriefing is not enough to change unit culture and ensure debriefing compliance.
Consistent feedback about performance and support is imperative to improve the quality of emergency
performance.
Calendar Year Number of emergencies
Emergency debrief forms
received
Percentage of emergencies
debriefed
2019 54 5 14%2020 162 56 34%2021 YTD 79 53 67%
*Survey results per PCCU’s nurses, clinical technicians, and certified nursing externs in 2021• 96.43% Felt debriefings are held consistently• 92.86% Post CODE/RRT feedback given in timely manner• 92.14% More comfortable doing CODEs/RRTs after debriefing• 82.14% Debriefings are a safe space to discuss QI• 75% More aware of CPR Guidelines after post-CODE email• 67% Debriefings give recognition to team members• 57.14% Learn something with every debriefing session
[DATE: 6/13/2021] RECOREDED ON THE BATHROOM FLOOR
Distribution of Compressions by Rate:
Too Slow: 3.0% Normal: 85.2% Too Fast: 11.9%
Distribution of Compressions by Depth:
Too Shallow: 44.6%In Range: 53.6%Too Deep: 1.8%
Distribution of Compressions by Depth:
Too Shallow: 26.8%In Range: 15.0%Too Deep: 58.2%
Distribution of Compressions by Rate:
Too Slow: 5.0% Normal: 43.8% Too Fast: 51.3%
Distribution of Compressions by Rate:
Too Slow: 2.2% Normal: 74.4% Too Fast: 23.4%
Distribution of Compressions by Depth:
Too Shallow: 7.8%In Range: 40.0%Too Deep: 52.2%
DATE: [1/4/2019] [DATE: 9/29/2020]
Contact information
How to read CPR cardCreated by Heather Newton
Example Post-Code Feedback Email
References Available Upon Request
Changes to alarm priority reduce alarm fatigueShelby Cahill, BSN, RN, Paula Murray, MSN, CVRN, NPD-BC, Maria Moning, BSN, RN, Tania Randell, MS, RN, ACCNS
Department of Medicine, Johns Hopkins Hospital, Baltimore, MD
Problem/Background PCCU nurses and techs noticed that codes
and bed exit alarms (BEA) had the same alert on new iphones:
This resulted in alarm fatigue and a delay in response to several emergencies.
Intervention Leadership nurses reassessed BEA levels in
collaboration with JHH Alarm Committee.
BEA iphone alert was re-prioritized from criticalto a less urgent-sounding important tone:
• Pilot in PCCU• Department of Medicine (DOM)
Intervention created a distinction between BEAs and critical alarms that signify an emergency
Conducted Qualtrics survey pre/post in PCCU and DOM
Comparison of pre/post fall rates
Results
Discussion Conducting a pilot assists in identifying
barriers and potential deficiencies of the larger project.
Standardization of survey questions may have produced more consistent analysis.
Following a QI planning structure may have assisted with depth of data and ease of obtaining results.
This QI project positively impacted: nursing's perception of
BEA frequency alarm fatigue alarm identification Fall rates decreased in PCCU
but increased in DOM
PCCU was impacted more favorably than DOM, indicating that determinants of alarm fatigue are multifactorial
Alarm priority must continue to be a collaborative decision with nursing at the forefront.
Critical Alarms from iPhone
Bed Exit Code/ERT Staff Emergency
Lavatory Emergency
Aim of the Project1. Improve patient safety2. Decrease alarm fatigue3. Maintain or reduce fall rates Q1 - How frequently does a “Bed Exit” alarm notification alert you via the iPhone during your shift?
Q3 PCCU - How much do you feel alarm fatigue with the iPhones since the bed exit alarm was change from critical to important?
PCCU Post
Q2 - The iPhone alert system in the has distinct tones that allow me to identify the level of the alarm quickly
PCCU Post
Responses:PCCU (pre n= 23, post n= 26) DOM (pre n= 126, post n= 101)
Responses Q1-3 shown in bar graphs
Q3 DOM - Q3 - To what extent do you agree with the following statement: My alarm fatigue during a normal 12 hour shift has decreased since the bed exit alarm changed.
References available upon request
DOM Post
DOM Post
DOM Pre
DOM Pre
PCCU Post
DOM Pre
PCCU Pre26% Agree
PCCU Pre22%
6-10 times per shift
74%More than 10 times per shift
Q3 - How much do you feel alarm fatigue with the iPhones?Q3 - How much do you feel alarm fatigue with the iPhones?
PCCU Pre
48%severe
44%moderate
DOM Post- not asked
Marifi Castillo, BSN RN CAPA; Waiman Sin, BSN RN-BC; Kristy Wormack, BSN RN CPAN; Ashley Greene, RN CPANPerioperative Services, The Johns Hopkins Hospital, Baltimore, MD
ResultsBackgroundTransfemoral Arteriogram is a minimally invasive
interventional procedure which utilizes VCD to achievehemostasis. Post procedure patient discomfort arises due torestrictions in position and prolonged bedrest.
There are two standards of care in the post proceduremanagement of patients post transfemoral arteriogram (PTFA).IR and NIR practice the two-hour supine with HOB flat, elevatethe HOB to thirty degrees for an hour, then ambulatethereafter.
The Johns Hopkins Hospital Zayed 5 Prep/PACU nursesrecover interventional cardiac patients post procedure withHOB in flat position for one hour and progressively elevate HOBevery thirty minutes, then ambulate after two hours.
Aim of the ProjectTo determine whether flat bedrest and ambulation
time frames could safely be reduced by one hour after transfemoral arteriography with vascular closure device.
Description of InterventionThe literature search yielded 892 articles and there were
only 12 appropriate articles that met the PICO criteria. Thefollowing Mesh terms were used: post angiography, closuredevice, transfemoral access, early ambulation, early discharge.The evidence reviewed range from 2006 to 2019. PUBMED,CINAHL, Jonna Briggs, and Cochrane Review databases weresearched.
Description of Data Collection and Analysis
The study revealed that reducing flat bedrest and ambulation by anhour is safe, feasible, increases patient comfort and decreases hospitalstay, therefore improving patient satisfaction. Further evaluation tostandardize the protocol to early ambulation and discharge could be costeffective due to decreased utilization of resources, manpower, and lengthof hospital stay. Finally, the CVIL and the IR post transfemoral arteriogramwith vascular closure device’s protocols will now be standardized andcomparable across the two specialty Prep/PACU units.
Implications for PracticeThe strength of evidence revealed ten years of studies
recommends it was safe to ambulate within 120 minutes PTFA withVCD. Roebuck, et al., disclosed there were no discernable difference incomplications when mobilizing patients two hours versus four hoursPTFA.
Larsen et al., concluded that immediate mobilization PTFA withAngioseal showed no increased risk of bleeding vs standard practicewith bedrest. It is imperative that the practice across JHH are alignedwith a standard protocol.
Results of the study are to be disseminated with JHH IR and NIRproviders as well as across the JHH Health System.
Acknowledgement
Plan Do Study Act (PDSA) format was utilized which compares the current IR practiceinstructing patients on three-hour bedrest while maintaining supine head of bed (HOB)in flat position for two hours then elevating the HOB to 30 degrees for one additionalhour vs implementing two-hour bedrest while maintaining supine HOB in flat position forone hour then elevating the HOB to 30 degrees for an additional hour.
Data collection included monitoring the BP, HR, RR, femoral pulse check, femoral groinsite check pain score, and patient satisfaction.
Data revealed the average minutes post transfemoral sheath removal to HOB elevationto thirty degrees is 69.95 min and the PACU discharge criteria met average time is 108minutes.
ReferencesAbdollahi, A.A., Mehranfard, S., Behnampour, N., Kordnejad, A.M. (2015) Effect of positioning and earlyambulation on coronary angiography complications: a randomized clinical trial. Journal of Caring Sciences, 4(2),125-134.Augustin, A.C., Schaan de Quadros, A., Sarmento-Leite, R.E. (2010) Early sheath removal and ambulation inpatients submitted to percutaneous coronary intervention: a randomized controlled trial. International Journal ofNursing Practice, 47, 939-945.Engelbert, T., Scholten, A., Thompson, K., Spivack, A., et al. (2010) Early ambulation after percutaneous femoralaccess with use of closure devices and hemostatic agents. Annals of Vascular Surgery, 24, 518-523.Fereidouni, Z., Morandini, M.K., Kalyani, M.N. (2019) The efficacy of interventions for back pain in patients aftertransfemoral coronary angiography: a rapid systematic review. Journal of Vascular Nursing,37, 52-57.Lai, Y-C., Kao, H-L., Lin, M-S., et al. (2008) The angio-seal arterial closure device for early ambulation afterelective percutaneous coronary intervention in patients receiving low-dose enoxaparin. The Journal ofInternational Medical research, 36, 1077-1084.Larsen, E.N., Hansen, C.B., Thayssen, P., Jensen, L.O. (2014) Immediate mobilization after coronary angiographyor percutaneous coronary intervention following hemostasis with the angioseal vascular closure device (theMOBS study). European Journal of Cardiovascular Nursing, 13(5), 466-472.Roebuck, A., Jessop, S., Turner, J., Caplin, J.L. (2000) The safety of two-hour versus four-hour bed rest afterelective 6-French femoral cardiac catheterization. Coronary Health Care, 4, 169-173.Sekhar, A., Sutton, B.S., Raheja, P., Mohsen, A., et al. (2016) Femoral arterial closure using ProgGlide is moreefficacious and cost-effective when ambulating early following cardiac catheterization. IJC Heart andVasculature, 13, 6-13.Tonetti, D.A., Ferari, C., Perez, J., Ozpinar, A., et al. (2018) Validation of an extrinsic compression and earlyambulation protocol after diagnostic transfemoral cerebral angiography: a 5-year prospective series. JNeurointervent Surg, 11, 837-840.Watanabe, S., Yamamoto, A., Torigoe, T., Kanki, A., et al. (2013) Transfemoral intra-arterial chemotherapy forhead and neck cancer using a 3-French catheter system: Comparison with a 4-French catheter sytem. KawasakiMedical Journal, 39(4), 119-125.
Early Ambulation of Patients with Post Transfemoral Arteriography with Vascular Closure Device (VCD): A Quality Improvement Project
Lessons Learned• Initiating the study was relatively straightforward.• IR providers and Z3 Prep/PACU staff worked
collaboratively during the implementation of the QI project.
• The activity did not pose greater risks than those presented by the current routine clinical care established in the Zayed 5 CVIL Prep/PACU interventional cardiac procedures.
0
10
20
30
40
50
60
70
80
90
100
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24
Min
utes
Patients post transfemoral srteriogram with closure device
Time frame of HOB elevation post sheath removal
0
50
100
150
200
250
300
350
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24
Min
utes
Patients post transfemoral arteriogram with clodure device
PACU Discharge Criteria Met
Outcome Measures/ Results
Zayed 3 Prep/PACU Nurses and staff, Interventional Radiology Providers esp Dr Singh and Dr Hong, IR Nurses andStaff, and Zayed 5 Prep PACUs for sharing their current standard protocol. Myrna Mamaril,, DNP, RN,CPAN, CAPA,FAAN, NEA-BC Patricia Ryan MSN, MHA, RN,and Lynnae Elliotte,RN, MSN ( Z3 Manager)
Implementation of a Fast Track Chair in a Hospital-Based Cancer Center to Increase Efficiency and Decrease Patient Wait Times
K. Alice Catches, BSN, RN, OCNMedical Oncology Clinical Coordinator, Sibley Memorial Hospital, Washington, DC
Results
Background• Sibley’s Cancer Center has been experiencing
considerable growth since 2016 (as much as 30% between FY19 and FY20).
• Infusion Center Visits are comprised of:• Intravenous infusions (chemotherapy, blood
transfusions, electrolytes, etc.), intravesical treatments, and injections
• Infusion Nurse Assignments:• 1 RN: 5-7 patients, staggered appts, acuity-based
• Scheduling Process:• Patients scheduled into one of six “chairs” based
on expected appt duration: • Fast track (15 minutes), 1 hour, 2 hour, 3
hour, 4-5 hours, 6 hours• 34 infusion rooms available
Project Goals• Decrease patient wait times• Increase patient satisfaction• Increase nurse satisfaction
Implementation• Fast track chair – back to back injections – 1 nurse• Daily injection volume calculated • De-coupled appointments – required at least 90
minutes between lab and injection appt• RN: Patient ratio for injections – established a
standard daily volume for one nurse• Designated days of the week to maximize nurse
capacity• Workflow changes:
• Release all medications to give pharmacy time to verify Rx
• Purchased two Pyxis refrigerators to give nurses ability to remove medications without relying on pharmacy to prepare first
Description of Data Collection and Analysis
• Data Collection• Wait time (appt check-in to first med given)• Long wait times (45 mins for an injection)• Nurses caring for infusion patients take longer to get
to injection patients• Data Analysis
• Labs/provider visit/treatment on same day highly correlated with increased wait times• i.e. Procrit – requires lab parameters to be drawn
and met• RN delays related to care for other patients• Pharmacy verification process
• RN “releases” medication for pharmacy to review and verify
Implications for Practice• Using our fast track injection process, assigning a nurse to
administer injections only:• Reduces patient wait times• Increases the capacity of infusions and injections• Increases number of available rooms for patients getting
infusions• Decreases pharmacy time spent handling medications
• Decoupling appointments: Not permitting patients to wait for lab results in an infusion chair:
• Allows for adequate time to receive results and make treatment adjustments, if necessary
• Increases volume of patients treated daily• Decreases wait times from appt time to first medication
administration time
ReferencesEdwards, L., Hermis, K., LeGette, C. R., Lujan, L. A., & Scarlett, C. (2017). Acuity-Based Scheduling. Clinical journal of oncology nursing, 21(2).Looker, S., French, H. S., Eastman, J., Anderson, K., Smith, E., & Jensen, P. (2016). Development of a fast track process within an ambulatory chemotherapy unit [Abstract 12]. In Oncology Nursing Forum (Vol. 43, p. E82).Atchison, E. A., Omar, A. F., Iezzi, R., Barkmeier, A. J., & Bakri, S. J. (2017). Outcomes of an intravitreal injection clinic. Retina, 37(7), 1371-1376.
Results
• The above chart shows a comparison of the injection visit times between fiscal year 20 (blue) and fiscal year 21(yellow). In July of FY20, our average wait time for injection appointments was 28 minutes.
• In March of FY20, when preparation for the impact of Covid-19 began, we began to see fewer appointments overall, and at that time, we implemented the fast track chair.
• One barrier to decreasing patient wait times with Covid-19 was the added necessity of disinfecting waiting areas and reducing the volume of patients in our waiting areas to allow for social distancing.
• As the patients began to return to the clinic you can see our wait times increase again. We believe this increase was related to the adjustments in managing the influx of patient volumes, new cleaning procedures, and intensive screening processes.
• As you view the progression of FY21 in yellow, you can see that we are adjusting to the new processes and have regained our strides in decreasing the average injection appointment time.
1817
14 1312 12 12 11
28
25
22 2122 22
18
11
9
13 13
16.4
0
5
10
15
20
25
30
Jul Aug Sep Oct Nov Dec Jan Feb Mar Apr May Jun
Injection Visit Duration
FY21 FY20
July 2019 (FY20)Monthly Stats
July 2020 (FY20) Monthly Stats
Infusion Patients: 1,072 patients824 infusions248 injections
1,558 patients1,251 infusions307 injections
Average Wait Time for Injections:
28 minutes 17.8 minutes
Injection Chair Turnover:
10.6 patients per day 32 patients per day
Utilizing Innovative Ideas to Decrease Central Line Associated Blood Stream Infections (CLABSI) in the Surgical Intensive Care Unit by use of Prevention Education Mobile Cart
Heather Cullen BSN, RN, CCRN; Samantha Young MSN, CCNS, ACNPS,CCRN; Stephanie Gray BSN, RN; Madison Goundry BSN, RN Weinberg Intensive Care Unit, The Johns Hopkins Hospital, Baltimore, MD
Results
Problem The Weinberg Intensive Care Unit
(WICU) had an increasing number of CLABSIs in 2020.
Continual onboarding of new hires and travel nurses.
Need for consistent CLABSI prevention education.
Aim of the Project
The aim was to create standardized education, accessible to all WICU staff 24/7, that could be measured and tracked.
Description of the Intervention
Utilizing Johns Hopkins Hospital’s Epidemiology and Infection Control (HEIC) CLABSI prevention toolkits, a self guided mobile education cart was created.
Each drawer contained guidelines from Hopkins policies, vendor handouts, quizzes and skill sign offs. A competency packet guided learning and tracked completion.
Staff had four months to complete.
Description of Data Collection and Analysis A pre and post Likert survey was sent
to nurses and clinical technicians asking them to rank comfort level regarding central line maintenance and CLABSI prevention.
Topics that fewer than 75% staff rated “moderately comfortable” were identified as areas to improve.
WICU CLABSI rates were tracked pre, during and post intervention.
Implications for Practice
The CLABSI cart creates an easily accessible resource for CLABSI education that can be utilized anytime and anywhere on the unit.
All staff are educated on the same material and completion can be measured and tracked.
Increased education on CLABSI prevention can help to improve patient outcomes.
Lessons Learned Educational material will need to be
checked at a scheduled time to assure it is up to date with Hopkins policies.
A process will need to be implemented to assure all new hires complete CLABSI cart.
Temporary staff have found this educational cart useful and informative.
References available upon request
Outcomes Measures
Pre surveys were distributed with a 73%(N=43) response rate and post surveys with a 71%(N=39) response rate. All survey questions showed an increase in comfort level post intervention.
The WICU had 5 CLABSIs from Jan 2020-Nov 2020 and zero CLABSIs from implementation in Dec 2020 through July 2021.
The Period of Purple Crying: Education Intervention for Staff and CaregiversElizabeth Curley, MSN, RN, CPN, Kris Schaum-Comegys, MS, RN, & Jennifer Polk, BSN, RN
Pediatrics, Johns Hopkins Children Center, Baltimore MD
ResultsBackgroundShaken baby syndrome (SBS) and abusive head trauma (AHT) is an unfortunate form of child abuse that plagues our communities for infants/children under two years of age. By bringing the PURPLE program to the forefront of health care workers education, we provide needed education for soothing and coping during periods of unexpected, evening crying and long-lasting unsettledness within our infants. Safety is key for all parents and childcare providers for our infants and children well-being.
Aim of the ProjectTo train our staff on how to educate parents/caregivers on the normal progression of newborn development, including the normal periods of increased crying that their infant may display, and strategies to cope with these times.
InterventionThe PURPLE program, an evidence-based educational program from the National Center on Shaken Baby Syndrome, was used. Following training sessions, nurses on Bloomberg 9N provided this education to the families of all admitted patients under the age of six months (corrected gestational age).
Description of Data Collection and AnalysisBefore the program's official roll-out, we surveyed all nursing staff to determine baseline knowledge and perceptions of SBS and AHT. A post-survey was completed, and data was compared. All programs were signed out to collect data about age of infant and who received the education. SPSS was used to evaluate data using Mann-Whitney U analysis.
Implications for PracticeThe program should be rolled out across JHCC to reach the greatest number of individuals. The program offers all the tools for implementation. Additionally, staff feel that it is easy to provide to families. The overall cost of the programs ranges from $2.00-$3.50, thus project is relatively inexpensive to implement.
Lessons LearnedStaff resistance to change can be detrimental to program success. Audits, clear expectations, and staff buy-in were necessary. Audits provided just-in-time education and reminders to staff to complete education with families. Frequent check-ins from staff allowed us to determine ways to help improve compliance.
ReferencesRabbitt, A.L., Bretl, D., Parker, M. Yan, K., & Zhang, L. (2018). Assessment of
maternal knowledge and confidence about abusive head trauma and coping with infant crying before and after infant safety education in the neonatal intensive care unit. The Journal of Perinatal & Neonatal Nursing, 32(4), 373-381.
Duzinski, S.V., Guevara, L. M., Barczyk, A.N., Garcia, N.M., Cassel, J. L., & Lawason, K. A. (2018). Effectiveness of a pediatric abusive head trauma prevention program among Spanish-speaking mothers. Hispanic Health Care International, 16(1), 5-10.
Nocera, M., Shanahan, M., Murphy, R.A., Sullivan, K. M., Barr, M., Price, J., & Zolotor, A. (2016). A statewide nurse training program for a hospital based infant abusive head trauma prevention program. Nurse Education in Practice, 16(1), e1-e6.
Outcomes Measures or ResultsStaff feels more confident in providing education on the developmental crying curve after introducing the program (p < 0.001). Additionally, staff feels that our SBS/AHT education for patient families has dramatically improved (p < 0.001). Program was delivered to 109 families with 40.4% of programs being delivered to families of patients less than 1 month old.
Baseline Knowledge of Staff
Have you received any SBS/AHT education in the past 3 years?, n (%)
Yes 13 (35.14)
No 24 (64.86)
Have you heard of the Period of PURPLE Crying before?, n (%)
Yes 6 (16.2)
No 25 (67.6)
Unsure 6 (16.2)
Figure 1. Period of PURPLE Program Acronym
Table 1. Baseline Knowledge of Staff on
SBS & AHTFigure 2 & 3. Results from Staff Surveys
Foley Maintenance and CAUTI PreventionKatherine D’Auria, Raphael Oguariri, and Kathrine Carongoy. Adult Surgical Unit [4800].
Suburban Hospital | Johns Hopkins Medicine
Background
One of the most prevalent healthcare-acquired illnesses is catheter-associated urinary tract infection (CAUTI).Infections caused by indwelling urethral catheter (Foley catheter) devices are a major concern for infection prevention efforts in health care. CAUTIs currently account for 20% of hospital acquired bacteremia, increased length of stay, and increased mortality of the inpatient population. CAUTIs can be prevented if the CAUTI prevention guideline is followed.
The goals of this study are: • To reduce catheter associated urinary tract infections
(CAUTI) in adult surgical unit (4800).• Reduce comorbidity and mortality of patients.• Empower staff and patients to take an active role in
infection prevention.
Analyze: October 2020—January 12, 2021
• Control Group: 25 patients surveyed• No CAUTIs during control period
Process Map /Value Stream Map (VSM)
ConclusionPost intervention, there was improvement in bags remaining off the floor, being <2/3 full, completion/documentation of perineal care, and cleanliness of catheter tubing. The unit recorded no CAUTI pre and post intervention. Nurses and techs will be responsible for maintaining foley catheters. CAUTI champion for unit will continue to conduct random assessments and implement interventions with staff.
Post-Intervention Results• Treatment Group: 30 patients surveyed
• Areas of improvement: foley bags off the floor, bags less than 2/3 full, pericare completion, cleanliness of tubing
• Areas that worsened: necessity of foley catheter & presence of securing device
• No CAUTIs from January 13-June 2020
Education/Intervention: January 13—June 2021• Address any existing practice issues in relation to foley care or
maintenance in real time• Place foley care calendar on patient doors during Infection
Control’s trial period• Remind staff during AM and PM huddles that catheters will be
assessed• Discuss audit findings with nurse and tech in real time• Have staff incorporate pericare into shift handoff and assess
catheter together• Educate patients in real time the importance of maintaining
proper positioning of catheter
Obtain current number of CAUTI during
October 2020-January 12 2021 (control group)
Randomly audit charts of adults with
indwelling urinary catheters
Determine deficits of care
Discuss with patients, nurses, and techs ways to improve practice or documentation in real
time
Evaluate outcomes
24 25 2522
25 24
6
23
1 0 0 3 0 1
19
205
1015202530
yes no
28 28 30 29 30 299
30
2 2 0 1 0 1 21 00
10203040
yes no
# oc
curr
ence
s
# oc
curr
ence
sMethods
This was a PRE-POST study design.
Random audits of patient charts and Foley Care Calendar documentation will be completed in order to establish baseline information that gives insight into how compliant current processes are.
• Assess foley in person.• Review documentation of nurses and techs.• Synthesize compliance to catheter maintenance policies.• Calculate total number of CAUTIs during October 2020-
January 2021 (control) and January 2021-June 2021 (intervention)
Key Metrics
• Total # of unit CAUTIs in control and intervention groups.• Compliance with catheter maintenance and
documentation.• Assessment of data provided on Foley Care Calendar
Improving New Graduate Nurses’ Anxiety Surrounding Pediatric End-of-Life Care Using Simulation
Kelsey Davis, DNP, ARNP, CPNP-AC; Michelle Cook, MS, RN, NPD-BC, CHPPN; Jennifer R. Dungan, PhD, RN Pediatric Intensive Care Unit, Johns Hopkins All Children’s Hospital, St. Petersburg FL
Caring for dying children can be a traumatic experience which may lead to nurse anxiety and burnout, fueled by a lack of end-of-life education
To determine if a simulation-based educational program for new graduate nurses (NGN) in the critical care areas at an academic pediatric hospital can reduce anxiety regarding end-of-life (EOL) care.
Objective
Background
Intervention
Practice Implications
Sustainability Plan
• Offering as an optional activity through annual ELNEC conference hosted at JHACH• Potential for inclusion on a volunteer basis or as a computer-based training module• Dissemination through publishing findings in an academic journal
Data Analyzation
Data Collection
NGNs participated in a 4-hour educational offering which included both a case study & a simulation component. Case studies provided NGNs with information to practice in the sim-lab. Both sims utilized live actors as parents/caregivers.
• NGN anxiety was measured utilizing the State Trait Anxiety Index (STAI) ©• STAI has ability to measure both state and trait anxiety. For purposes of this project, only state
(situational) anxiety was measured (STAI-Y1). • Scores range from 20-80, 20 being anxiety-absent and 80 being highest possible anxiety. Cut-off for
probable clinical anxiety on STAI-Y1 is a score of 41. • NGNs filled out the STAI-Y1 as both the pre and post test.
Pre-program anxietyMean: 48.25 (range 33-70)62.5% scored above 41
Post-program anxiety:Mean 36.63 (range 28-44)37.5% scored above 41
Mean change:11.62 points24.1% decrease
Case Study 1Reviewed withdrawal of life
sustaining measures, the SPIKES method of difficult communication,
EOL Symptom management, memory work, post mortem care,
and hospital policy.
Case Study 2Reviewed death by neurologic basis & hospital policy, as well as briefly
reiterated content reviewed in Case Study 1.
Simulation 1NGNs practiced explaining brain
death testing and patient prognosis utilizing the SPIKES method of communication.
Simulation 2NGNs practiced participating in
withdrawal of life sustaining treatment including palliative
extubation, memory work, EOL symptom management, and
post mortem care.
• Educating NGNs to improve the end-of-life experience for themselves, patients, and families has great potential for positive impact..
• Utilizing simulation to enhance learner engagement in the unique and sensitive clinical circumstance of pediatric EOL may reduce workplace anxiety and lead to better nurse retention.
Above: NGNs were shown a video of a nurse performing EOL care prior to completing
the pre-test STAI-Y1.
ReferencesCrowe, S., Sullivant, S., Miller-Smith, L., & Lantos, J.D. (2017). Grief and burnout in the PICU. Pediatrics. 139(5):1-5.Ercan, I., Hafizoglu, S., Ozkaya, G., Kirli, S., Yalcintas, E., & Akaya, C. (2015). Examining cut-off values for the state-trait anxiety index. Revista Argentina de Clinica
Psicologica, 24(2):143-148.Koutsimani, P., Montgomery, A., & Georganta, K. (2019). The relationship between burnout, depression, and anxiety: A systematic review and meta-analysis. Frontiers in
Psychology, 10, 284. https://doi.org/10.3389/fpsyg.2019.00284Spielberger, C.D. (2015). State-Trait Anxiety Inventory for Adults Manual. Mind Garden, Inc.
A Multi-Disciplinary Initiative to Improving Management of Heart Failure Patients on a Medical Telemetry Unit Marcia Dawson, MS, RN-BC, NE, Lavina Patel, BSN-RN, Ishaan Gupta, MDMedicine A, Johns Hopkins Bayview Medical Center, Baltimore, Maryland
Results
IntroductionHeart Failure (HF) is becoming more prevalent in the U.S. and is costly in terms of mortality rates and health care services. It is one of the most common causes of hospitalization and readmission. A collaborative approach among RNs, PCTs, and providers initiated a heart failure project on a medical telemetry unit that focused on education for patients, families, and staff. Why Make A Change?•Inconsistent intake and output documentation•Inconsistent daily weight documentation•Difficulty in identifying heart failure patients and creating educational plans •Increase in heart failure 30-day readmission rates
Objectives• Enhance documentation of intake and output and daily
weights • Enhance staff understanding of roles in disease
management• Improve patient and family understanding of disease
through adequate education and resources• Improve inpatient management for this patient population• Reduce hospital readmission rates for HF exacerbations
Interventions and MethodsStaff Education
Nursing and Providers
Interventions & MethodsNursing and provider education continued A heart failure registry was created in electronic health record, EPIC to identify
patients with HF. A red, heart-shaped sticker is placed on their door name tags. Patients were assigned HF education within 24 hours of admission on to the unit.Patient Care Technician (PCT) Education PCTs recorded I&O Q4H on all heart failure patients. RNs communicated with PCTs about patients who are on HF education program.
Night shift PCT obtains standing weight in morning, encourage and educate patients on how to accurately obtain their weight at home.
Outcome
HCAHPs–A closer look at FY2021 to current performance in the following metrics showed improvements in the following:
Significance•Outcomes suggests improvement in HCAHPs and documentation compliance on patient education since the start of the project which supports objectives. •HF survival skill education documentation is influenced by recent COVID pandemic. •Future data should focus on hospital readmission rates.
Patient and Family Education ResourcesFolders Within 24 hours of admission, each patient receives a HF education packet that
contains information on the disease, nutrition, exercise, medications and logs for keeping track of weight and fluid intake. Patient education is performed at every interaction, when it is most relevant to the patient.
Fluid Intake Patients can be provided with measuring cups in order to help keep track of fluid
intake. Weight Scales provided upon discharge to patients that were financially unable to obtain
them. This will help promote self-management of their disease at home.
Outcome continued
Heart Failure Survival Skill education documentation References
69.33
83.64
37.73
83.33
97.37
52.72
0
20
40
60
80
100
Nurse Communication Discharge Information Care Transition
H-CAHPS FY2021 to FY2022 Performance Comparison-MEDICINE A
FY21
FY22
Center for Disease Control and Prevention (CDC). (2019). Heart Failure Fact Sheet. Retrieved from https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_heart_failure.htm
Kelly, S., Prasun, M., Lee, C., Jaarsma, T., Piano, M., & Albert, N. (2018). Nursing research in heartfailure care: A position statement of the American Association of Heart Failure Nurses (AAHRN). Heart & Lung, 47(2), 169-175.https://doi.org/10.1016/j.hrtlng.2018.01.003
Takeda, A., Martin, N., Taylor, R.S., & Taylor, S.J.C. (2019). Disease management interventions for heart failure.Cochrane Database of Systematic Reviews 2019, 1. DOI: 10.1002/14651858.CD002752.pub4.
Vasan, R. & Wilson, P. (2018). Epidemiology and causes of heart failure. UptoDate. Retrieved from https://www.uptodate.com/contents/epidemiology-and-causes-of-heart-
Paired sample t test of SCHFI 7.2 surveypre & post intervention (N = 9). Patient SC confidence score significantly improved.
State-wide database (HSCRC) showed:PCCU readmission rates for the pilot period (April 1- July 31) followed a similar trend to previous years
Nurse survey respondents felt…Accessing pilot materials was easyTeaching with materials was easyPatients responded well to teaching
Background
Interventions
Results
Discussion
• Hospital Heart Failure (HF) readmissionrates trend above the national benchmark of 20%.
• Improving patient self-care (SC) may be a way to influence readmission.
• The Teach-back method is a concise and effective way to prepare patients
Improve the quality and impact of HF
patient education and influence
readmissions by targeting patient self-care
knowledge and confidence through use of
a standardized education packet
• Pilot participants were introduced to the HF education packet
• Patients were instructed daily by bedside nurses using the teach-back method
• Administered Self-Care for Heart Failure Index (SCHFI) 7.2 pre & post intervention
• Nursing documentation audits were performed for pilot patients
• Anonymous follow-up nursing survey given
• One size does not fit all.
• Variables to consider for each patient:• Education level• Home resources • Stage of HF• Time since diagnosis• Level of motivation
• Nurses need guidance and a system for providing tailored HF education.
Laura Dobbyn, MSN Candidate, Tania Randell, MS, RN, ACCNS-AG, Maria Moning, BSN, RN, & Rebecca Polatkan, BSN, RN
Department of Medical Nursing, Johns Hopkins Hospital, Baltimore, MD
“Heal Your Heart”: A Heart Failure Patient Education Pilot
Aim
Pilot packetEvidence-based
Hospital approvedFifth-grade level
Standardized messageteach-back questions
Self-care topics-weight tracking
fluid trackingmedication safety
Allows practice ofself-care prior to
discharge
Presenting a heart failure self-care education tool using teach-back improves patient confidence in performing self-care at home.
References available upon request
Example of SCHFI 7.2 questions given to pilot patients
64% of nurses taught pilot materials 25% of nurses documented teaching
PERIOPERATIVE ENHANCED FAMILY COMMUNICATION : CREATING A STORY WITH TEXT MESSAGES
Annie P. Duremdes MSN-RN, Cyndi Bochniak BSN-RN CAPA, Sarah Pierorazio BSN-RN, Angel Shoemaker BSN-RN, Joe Rainwater, Kim Goldsborough DNP-RN
PERIOPERATIVE DEPARTMENT: ASU/OPERATING ROOM/POST-ANESTHESIA CARE UNIT
Introduction Can technology leverage communication
with families and care partners of patient in surgery during these challenging times?
How can we create and convey caring moments with random text messages?
The perioperative service activated the electronic family communication system (EFCS) in EMR during COVID 19
Providing updates that tells a “story” is a collection of text messages sent by nurses from ASU, OR, PACU to provide timely, instantaneous and meaningful information.
Methods Results• Actively utilizing EMR functionality of sending
a collection of text messages that tells a “story” enriches communication, supports core elements of PFCC, improve care with family engagement and therefore patient outcomes
• Use of mobile digital communications in addition to in person and phone call updates, can streamline and augment patient care, improve nurse, patient and family satisfaction
• Promotion of patient and family centered care through instantaneous sharing of perioperative information via text messaging
Discussion• As a process improvement initiative it’s a
continuous process to monitor, evaluate and sustain
• We identified our barriers and opportunities• OR staffing changes occurred in Jan-Feb.• Understanding the nursing workflow can
improve staff adoption of the new process• Staff like the immediate information sharing
but has expressed the limitation of sending one way communication
• A family phone update every 2 hours is still standard for the operating room nurses
• A phone update from the provider is a must
Desired Outcome Enhanced communication to families and
care partners during the pandemic Promote patient and family centered care
(PFCC) Promote safety by limiting distractions due
to frequent calls to the clinical areas
A COMPLETED PERIOPERATIVE TEXT COMMUNICATION “STORY”
Patient is in the OR –ASU Patient procedure has begun – OR Patient procedure is still in progress – OR Patient is doing well – OR/PACU Patient is in recovery room – PACU Transport to the unit – PACU Ready for pick up/discharge – PACU
Utilization of EFCS in EMR
• EVALUATE EMR UTILIZATION
• HCAHPS SURVEY• COMPLETED “STORY”• MESSAGES SENT• INCREASING ADOPTION
• CREATE CARING MOMENTS
• APPLY CONNECT, PARTNER, REFLECT COMMUNICATIONMODEL
• FOCUS GROUP
• ACTIVATE TEXT FUNCTIONALITY (EFCS)
• STAFF EDUCATION OF NEW PROCESS
• PILOT
• ENHANCE FAMILY COMMUNICATION
• TEAM BUILDING
PLAN DO
CHECKACT
0
500
1000
1500
2000
2500
3000
JUNE JUL AUG JAN FEB MAR
NUMBER OF TEXT MESSAGES SENT
1765
22782088
2556
1334
147
PRE DATA POST DATA
0
20
40
60
80
100
120
140
160
180
200
Jun-40 JUL150
AUG172
JAN152
FEB108
MAR155
NUMBER OF COMPLETED STORIES
References1. Hart, J., Turnbull, A., Oppenheim,I., & Courtright, K. (2020). Family centered
care during the COVID-19 era. Journal of Pain and Symptom Management. Vol. 60 No. 2 e93-e97.
2. Sitzman, K. & Watson, J. ( 2017). Watson’s Caring in the Digital World. New York: Springer Publishing.
3. Ray & Turkel (2014). Caring as emancipatory nursing praxis. The theory of relational caring complexity. Advances in Nursing Science. April-June; 37(2); 136-46
The Use of the Neiguan (P6) Acupressure Wristband as an Adjunct to Anti-emetic
Prophylaxis for the Reduction and/or Prevention of PONV in the High Risk
Outpatient Populationcredentials
ResultsBackgroundPostoperative Nausea and Vomiting (PONV) has a negative effect on patients
and is a complication of anesthesia often viewed by patients as more debilitating than postoperative pain. Despite anti-emetic administration, PONV still remains a problem. Symptoms can cause physical and mental distress and may prolong hospitalization, increasing health care costs. The risk of PONV ranges from 30% in the general surgical population and increases to 80% in the presence of specific risk factors.
There is evidence that the Neiguan Point (P6) acupressure wristband reduces PONV and increases comfort levels. Research has shown acupoint stimulation is a cost-effective, safe intervention either in conjunction with or in place of pharmaceutical practices.
This quality improvement project was designed to determine the effect of the acupressure wristband application on the high-risk outpatient’s perception, experience and/or intensity of PONV within the first 24 hours post operatively. A secondary outcome was to see if wearing the wristband improved comfort level, satisfaction and overall experience by decreasing the incidence and effects of PONV.
Project Design-Methodology
Data Analysis Implications for Practice
Lessons Learned
References
Outcomes Measures or Results
1.Unulu, kaya, The Effect of Neiguan Point (P6) Acupressure With Wristband on Postoperative Nausea, Vomiting, and Comfort Level. Journal of PeriAnesthesia Nursing 2018; 33:915
2.Molassiotis, Russell, Hughes, Breckons. The Effectiveness of Acupressure for the Control and Management of Chemotherapy-Related Acute and Delayed Nausea. Journal of pain and Symptom Management 2014; 47:13.
3.Sherif, Hedge, Mariswami, Ollapally, Validation of the Aphelscoring system for identification of High-risk patients for PONV. Karnataka Anesthesia Journal 2015; 1:115.
Data tool kit available here:
Comments received during the post op phone call were that some found the band tight and took it off. Some found the band a little tight at first but got used to it and left it on. Two patients said their hand started to swell and took off as instructed. Some patients said they were impressed that we offered a prevention/treatment option other than medications for PONV symptoms which added to their overall positive experience.
Sharon Ferguson BSN RN, PACU, Pre-Testing and Pre-Op Holding RN’s
Suburban Hospital Johns Hopkins Medicine,Bethesda MD 20814
A validated scoring tool (Simplified Apfel), was used to identify the high risk PONV patient as part of the preprocedural assessment. Pre-op holding and PACU RNs were instructed on proper application of the wristband.On the day of surgery, the pre-op holding RN provided written and verbal information on the possible benefits of wearing the wristband to the high-risk patients.
Exclusion criteria were developed and included: skin breakdown/rash on the wrist, limb alert, wrist or hand IV location, inpatients, patients with cognitive impairments, and surgery or regional blocks to the upper extremity. If no exclusion criteria were present and the patient was interested in participating, the band was placed and the patient was instructed to keep it on for 24 hours post op. The patient received anti-emetic therapy intra operatively and post operatively as needed.
The PACU RN confirmed proper placement and assessment of the wristband and provided additional instruction and education at time of discharge. Response to wearing the band on the occurrence of PONV and patient’s perception of their experience was assessed the following day by the PACU RN using the post op phone call data collection tool. Data was collected on 100 patients from 9/2020 through 5/2021.
This QI project was submitted and approved by the JHH IRB and deemed a quality improvement project.
1. The first goal was to identify the high-risk patient’s perception, experience and intensity of PONV symptoms • 26% strongly agreed band reduced intensity and/or amount of symptoms• 24% agreed band reduced intensity and/or amount of symptoms• 45% neither agreed or disagreed (due to also receiving anti-emetics)• 4% disagreed, 1% strongly disagreed50% reported reduced symptoms
2. The second goal was to determine if there was improved patient comfort level, patient satisfaction and overall patient care experience by decreasing the incidence and effects of PONV• 41% agreed• 22% strongly agreed• 30% neither agreed or disagreed• 6% disagreed, 1% strongly disagreed63% reported increased satisfaction and overall experience3. Patients rating of PONV symptoms post operatively were 64% had none, 4% had anticipated nausea, 10% had mild, 9% had moderate, 7% had great and 6% had severe.4. When asked if they would wear the band again if offered for another surgery, 93% 0f the participants answered yes. Since anti-emetics and wristbands were used together, we are unable to distinguish their independent efficacy. We can conclude that when used in conjunction, a high percentage believed that wearing the wristband benefited them and enhanced their overall experience.
Nurses should seek solutions to enhance patient comfort and to prevent nausea during the post-operative period. Wristband P6 point acupressure application is a non-pharmacologic, cost-effective intervention which based on our project results has positive benefits for the high risk PONV patient. This QI project has shown that patient’s perception of wearing the wristband had positive benefits and 93% would wear the band again which speaks to a demand for adjunct therapy. Offering an additional intervention allows the patient to be more engaged in their treatment and associated outcomes.
EMPOWERING PATIENTS: A HOME HEALTH CLINICIAN’S TOOLKIT Patricia Grimes MSN, RN Lead Clinical Nurse, Adult Home Health Services
Melissa Millard, MPH Senior Quality Safety Manager Brittany Cardoso, PT, DPT. Patient Experience Coach, Quality Safety Manager
Tammy Fallon, ADN. Clinical Manager Adult Home Health ServicesJohns Hopkins Home Care Group – Baltimore Maryland
Introduction
QI initiative: Integrate new Patient Empowerment practices into the Adult Home Health Clinician Patient Empowerment ToolkitGoals: Improve patient outcomes Achieve “Top-box” patient
satisfaction metrics.
Methods
Interdisciplinary team:refurbished existing & created new
patient empowerment toolsPatient Family Advisory Council:
Collaborated on toolkitEducated Clinicians Metrics Collected:
by outside vendors presented quarterly
Annual patient empowerment competency training
ResultsHH-CAHPS score “Communications between Providers and Patients”
increased: 90% to 93%SHP Readmission data- length of stay calendar year 2019 -2020
decreased: 33.05 to 30.54 days calendar year 2020 -2021
decreased: 30.54 to 27.31 daysConfounding Variables:
COVID19 pandemicCaregiver support
DiscussionTeach Back Training: Annual competency usingExperiential learning Home Observation Visit Data: Track & trend patient education: teach back & return demonstration quarterly Ongoing Data Review/Analysis:
Readmission data by diagnosisHH- CAHPS metrics
Develop additional STOP LIGHT zone tools:
Wound care – depression - HTN
IMPROVING PATIENT OUTCOMESIntegrating new patient
empowerment practices into the Adult Home Health Clinician/Patient
Empowerment Toolkit including STOPLIGHT ZONE TOOLS
Decreasing Falls Amid COVID 19’s Increased Acuity: Development of a Fall-focused Communication Tool Engaging Patients and Care Teams Christine Inglisa MSN, RN, NEA-BC; Janelle Mirabeau MSN, RN, CPHQ; Kim Espinosa BSN, RN; LaKesha Braxton; Veronica Amaya MSHS, CPHQPatient Care Services and Patient Safety & Quality Improvement Department, Sibley Memorial Hospital | Washington, DC 20016 | Johns Hopkins Medicine
Background
Conclusion
Description & InterventionPlan: Implement intentional leadership rounding, reviewing all relevant information with care team and patient to mitigate any gaps in best practice interventions.
A fall-focused communication tool was created to develop a fall prevention plan that engaged staff and patient participation. This included:• Patients identified as high risk for fall by JHFRAT
score in addition to the clinician’s input.• Direct observations of nursing intervention(s)
present in patient room:o E.g., bed/chair alarm activated and functioning,
call light within reach and patient able to demonstrate use, safe footwear in place, and room free of clutter
• Conversation with patient/family about fall risk status and their perspective and perception of safety interventions.
Implications for PracticeAct: The first step in fall prevention is the nurse’s timely and accurate completion of the JHFRAT. • Assessment is completed at the bedside• Patient is actively participating in fall prevention plan • Implementation of evidence-based nursing
interventionsLessons Learned: • Engaging the patient as well as the care team with
targeted fall prevention questions, the care team was able to mitigate specific fall risks.
• Individualizing the patient’s toileting regimen was identified as an essential component for preventing falls.
Future considerations:• Integration of patient’s perceptions of fall prevention
into daily rounding practice of clinical staff.• Standardization of tool and integration into an
electronic platform for sustained use.• Expansion of use across nursing units to enhance
collaboration from clinical and non-clinical areas, e.g. Physical Therapy and Patient Transport.
For nearly two years, the COVID-19 pandemic has impacted the community, hospital operations, and care teams at Sibley Memorial Hospital.
• In FY21, inpatient falls increased across most adult inpatient units.
IntroductionDo: A fall-focused communication tool was initiated March 29 – June 30, 2021. • Environmental room assessments were conducted daily by
leadership and clinical staff for high fall risk patients to ensure nursing interventions were in place.
o Intervention gaps were corrected in real-time. o Patients shared their perceptions of what could
keep them safe.• Clinical staff shared their perceptions of potential safety
concerns for the next 24hrs.
Data Collection
ResultsStudy: Patient falls in the inpatient areas peaked in January 2021. As the fall-focused communication tool was developed, revised, and implemented with the medical-surgical unit, falls decreased over a three month period. The nursing unit achieved two consecutive months free of falls.
The aim of this QI project was to develop and evaluate the use of a fall-focused communication tool for patients assessed as “High Risk for Fall” on an adult medical-surgical unit using the Plan, Do, Study, Act quality improvement framework.
The total number of fall events (assisted and unassisted) and monthly patient days were captured to measure the monthly fall rate.
Project Aim
References1. Daniels, J. F. (2016). Purposeful and timely nursing rounds: a best practice
implementation project. JBI Evidence Synthesis, 14(1), 248-267.2. France, D., Slayton, J., Moore, S., Domenico, H., Matthews, J., Steaban, R. L.,
& Choma, N. (2017). A Multicomponent Fall Prevention Strategy Reduces Falls at an Academic Medical Center. Joint Commission journal on quality and patient safety, 43(9), 460–470.
3. Royal College of Physicians (2012). Implementing Fall Safe: Care bundles to reduce patient falls. London, UK: Royal College of Physicians.
4. Zhao, Y. L., Bott, M., He, J., Kim, H., Park, S. H., & Dunton, N. (2019). Evidence on fall and injurious fall prevention interventions in acute care hospitals. JONA: The Journal of Nursing Administration, 49(2), 86-92.
Patient Initials /Room Number
Ask the patient: What would you like us to know about you to keep you safe?
Nursing Staff: Are there any specific concerns you have regarding this patient as a high fall risk?
Nursing Staff: What additional information should be shared with the care team to protect this patient from falling in the next 24 hours?
Sample of Fall-focused Communication Tool
02468
101214161820
Jan-21 Feb-21 Mar-21 Apr-21 May-21 Jun-21
# Fa
ll Ev
ents
Inpatient/Med-Surg Unit Fall Events by Month Medical-Surgical Unit Falls All Inpatient Unit Falls
March 29th
Initiation of Fall-focused communication tool
TeamSTEPPS® In a Pediatric Operating RoomLisa Kerrick , DNP, MBA, RN, CNOR, NEA-BC, FACHE
Nursing Administration, Johns Hopkins All Children’s Hospital, St. Petersburg FL
Despite numerous patient safety and quality programs available and in use in the healthcare environment, adverse events in operating rooms continue to occur. Evidence suggests that teamwork training can improve patient safety in operating rooms.
To determine if the implementation of TeamSTEPPS® communication tools improves the perception of teamwork and efficiency in a pediatric operating room. There were two desired outcomes for this project:1. Improve the perception of teamwork 2. Improve efficiency metrics
Objective/Goal
Define: Background
InterventionA pre-intervention assessment, the TeamSTEPPS ® Teamwork Perception Questionnaire (T-TPQ) was administered to a multidisciplinary group. The T-TPQ is a validated tool, with 35 questions, that measures the perception of team work. TeamSTEPPS ® education modules were then introduced to the group by computer-based modules. Following the TeamSTEPPS ® education intervention, the T-TPQ post-assessment was repeated.
Implications for Practice & Lessons Learned
ReferencesKertesz, L., Walker, C., & Maliwat-Bandigan, B. (2019). Improving communication and teamwork in the operating room.
ACTA Scientific Paediatrics 2(2). 21-31.
Obenrader, C., Broome, M.E., Yap, T.L., & Jamison, F. (2019). Changing team member perceptions by implementing TeamSTEPPS in an emergency
department. Journal of Emergency Nursing 45(1). 31-37.
TeamSTEPPS® Teamwork Perceptions Questionnaire (T-TPQ) Manual. (2017). Agency for Healthcare Research and Quality, Rockville, MD.
Outcome Measures
Measure
There are five teamwork domains assessed by the T-TPQ: Team structure, Leadership, Situation Monitoring, Mutual Support, and Communication. Statistically significant results were demonstrated in two domains: Leadership and Situation Monitoring. The mean difference in efficiencies demonstrated that there was no improvement in efficiency metrics.
A paired sample t-test was used to compare the T-TPQ data gathered pre and post-intervention to determine if there were statistical differences between pre and post-TeamSTEPPS ® implementation on the perception of teamwork. A p-value determines statistical significance, and in this project data with a p-value of 0.05 or less was considered statistically significant. The OR efficiency metrics were calculated using a mean and the mean difference was calculated for two different but comparable time periods.
TEXT
Formal teamwork training can improve communication and collaboration in the operating room. Implications for practice include the need for continued team training, a plan for sustainability of TeamSTEPPS concepts, and a plan to address team dynamics when unexpected stress or change is introduced into the work environment.
This project adds to professional knowledge of TeamSTEPPS impact on the perception of teamwork in and efficiency in an operating room. There is an opportunity in nursing to continue teamwork projects to advance care and strive for optimal outcomes. The evidence suggests that unit-based teamwork improvements, can advance professional practice.
Implementation of a Nurse-Managed Bladder Management QI PilotLisa Klein, MSN, RN, AGCNS-BC, CNRN; Amelia Tenberg, MSN, AGNP-C; Hohyung Yi, BSN, RN, CNRN; Margie Burnett, MS, RN, CNRN;
John Probasco, MDDepartment of Neurosciences, Johns Hopkins Hospital, Baltimore, MD
Introduction• Monitoring and management of bladder
functioning following indwelling urinary catheter (IUC) removal and for urinary retention on the neurosciences units varies and is prescriber dependent.
• The aim of this quality improvement (QI) project was to ascertain: o whether nursing staff can use a bladder
management algorithm correctlyo whether bladder distention occurrences
are decreased using the bladder management algorithm
o any effect on IUC days (per 1000 IUC days) & urinary tract infection (UTI) rates.
Methods• A bladder management algorithm was
created following an evidence-based practice project on best practices to prevent UTIs following IUC removal and retention.
• The bladder management QI pilot was over six months (December 13, 2019-June 15, 2020) for patients on neurosciences services on two acute-care and two intermediate-care medical-surgical units.
• Based on bladder scan volumes, the algorithm and orders in the electronic medical record guided nursing staff to perform specific interventions and monitoring.
Results• 115 pilot patients were compared to 119
baseline patients (see Table 1).• Protocol use was associated with
(see Table 2): o improved nursing bladder management
compliance (e.g., timing of actions & intervention).
o improved rates of bladder management monitoring following IUC removal.
• Protocol use was not associated with:o length of stayo rates of fall during hospitalizationo decreased mobilityo rates of UTI
• More patients discharged with an IUC during the pilot period compared to baseline.
• Zero CAUTIs occurred during the pilot period compared to 4 during the baseline period.
Discussion• Implementation of a nurse-led bladder
management algorithm was successful and found to be safe for patients.
• Further study is warranted to:o adjust the bladder management algorithm
to ensure urinary volumes guiding intervention decisions and frequency of interventions have the greatest positive impact on patient outcomes.
o ascertain generalizability of the algorithm to a variety of patient populations.
Table 1
Table 2
The Operang room (OR) is a costly environment and it should be managed efficiently. Starng the first cases on me is crucial for maintaining an operang room’s schedule. However, for a myriad of reasons, first cases can be delayed, causing subsequent cases to be delayed, affecng OR efficiency and sasfacon of paents/families and the perioperave team. Across the Main OR, only 54% of cases on average started on me in 2018; and the naonal benchmark is 85%. In response, the Main OR First Case On-Time StStarts (FCOTS) team was formed under the Perioperave Joint Operang Council (JOC) to focus a shared effort on correcng the delays. The number one reason why the first cases started late was surgeons’ late arrival and other surgeon related issues; followed by paent related issues. Other common causes of delays were related to the following departments: anesthesia , OR , preop, sterile processing, breast health, registraon, laboratory, and facility (Figure 1). Delay reasons that were less than 5 were not included in the data.
Idenfy the root causes of first cases delays, including strategies to correct delays and achieve the benchmark of 85% FCOTS. This will improve OR efficiency and the sasfacon of paents/families and the perioperave team.
The goal to improve FCOTS to posively impact OR efficiency and paent/family sasfacon is a shared responsibility of the Department of Anesthesia, Surgery, and Perioperave Services. The success of the iniave has made the Perianesthesia team become more invested, movated, and commied to improve FCOTS and sustain improvements ulizing process improvement tools.
There is a substanal opportunity to enhance OR efficiency by improving FCOTS. The Perioperave JOC has engaged a muldisciplinary FCOTS team to apply the Lean process improvement methodology to increase OR efficiency: (1) A3 document and project charter were created. The current state and the future state were idenfied. The FCOTS team was focused on the metric and the FCOTS process was embedded in the pracce of the periop team; (2) Acon register with “just-do-it” items was generated (Figure 2) that contains the list of strategies that address the FCOTS delays; (3) Connuous measumeasurement, analysis, and evaluaon were demonstrated. (Figure 3). FCOTS delays report is sent to key FCOTS partners (Surgeon, Anesthesia, OR nurse manager, and Preop/PACU nurse manager to review report and address delays specific to their department. The FCOTS team analyzed the data and reported results to the Perioperave JOC monthly to summarize gains and barriers to success and sustainability. (4) Communicaon/reporng and disseminaon were iniated. FCOTS partners took ownership in disseminang FCOTS data and other FCOTS related informaon. (5) A Celebraon of success was put in place to reward the efforts of the periop team and to encourage them to sustain the gain.
Data has shown that in 2018, FCOTS ranges from 43% - 67%, with an average of 54% across service lines. In 2019, FCOTS ranges from 46%-84%, with an average of 73%. In 2020, due to the COVID 19 pandemic, FCOTS average has fallen to 64%, with ranges from 52%-82%, which are sll significantly higher than in 2018, the year when the iniave began. These results (Figure 3) demonstrate that the applicaon of Lean process improvement methodology, the presence of more credible data, enhanced communicaon processes, and most of all, the commitment of highly collaborave muldisciplinary teams can signifisignificantly improve FCOTS. This leads to a more efficient OR, higher sasfacon of paents/families and perioperave team, beer accountability, and improved provider and team morale.
Figure 1 Figure 2
Figure 3
Figure 4
Improving AM-PAC and HLM Scores: An Educational Approach to Motivating Clinicians to help Patients Out of Their Beds and Out of The Hospital
Ni Lwin BSN, RN, CVRN & Katie Padgett BSN, RN, PCCNNelson 7, Department of Medicine, The Johns Hopkins Hospital, Baltimore, MD
ResultsBackgroundNelson 7 was not meeting the unit goal of helping 75% of patients achieve their Highest Level of Mobility (HLM) goal. After investigation, the cause was found to be staff’s misunderstanding of how to properly score the AM-PAC and its correlating HLM score, creating unrealistic mobility goals for the patients. Staff also were not updating the HLM after their first assessment, so the scores were not always reflecting the patient’s actual HLM. There was also a need for better collaboration between disciplines (RN, CT, PT/OT) to ensure actual HLM scores were being documented.
Aim of the ProjectTo improve nurse and tech understanding and documentation of patient mobility scores. Auditing, direct feedback, staff recognition and ongoing education will help staff understand the correlation between AM-PAC and HLM scores, resulting in increased compliance with documentation, improved patient mobility, and improved patient outcomes.
Interventions• Staff education on proper scoring of daily AMP and
appropriate HLM goal according to AM-PAC score (poster, staff recognition, huddle discussion, more visible scores)
• Recruitment of motivated and enthusiastic mobility champions.
• Added HLM goal to charge nurse checklist and discussed at mid-shift huddles. Charge nurses now follow up on patients who didn’t meet their goal by huddle.
• Collaboration with nurses, CTs, and PT/OT to make sure accurate HLM is documented.
Description of Data Collection and Analysis Implications for PracticeLiterature shows that decreased mobility of hospitalized patients is detrimental to patient outcomes, leading to increased morbidity and mortality (Jones, et al., 2019; Klein, et al., 2018; Schreiber, 2021). Poor mobility may result in functional decline, pressure injuries, falls, hospital-acquired pneumonia, venous thromboembolism, delirium, prolonged length of stay, and increased healthcare costs (Jones, et al., 2019; Klein et al., 2018). Unit-based initiatives to encourage nurse-led patient mobility will contribute to decreased patient harm and improved patient outcomes.
Lessons LearnedOngoing staff education and close follow-up by motivated mobility champions are necessary to encourage staff compliance with patient mobility and correct documentation of AM-PAC and HLM scores.
ReferencesJones, R. A., Merkle, S., Ruvalcaba, L., Ashton, P., Bailey, C., & Lopez, M. (2020). Nurse-Led Mobility Program: Driving a Culture of Early Mobilization in Medical-Surgical Nursing. Journal of Nursing Care Quality, 35(1), 20–26. https://doi.org/10.1097/NCQ.0000000000000404
Kappel, S. E., Larsen-Engelkes, T. J., Barnett, R. T., Alexander, J. W., Klinkhammer, N. L., Jones, M. J., Baustian, T. L., & Ye, P. (2018). Creating a Culture of Mobility: Using Real-Time Assessment to Drive Outcomes. AJN American Journal of Nursing, 118(12), 44–50.https://doi.org/10.1097/01.NAJ.0000549690.33457.bb
Klein, L. M., Young, D., Feng, D., Lavezza, A., Hiser, S., Daley, K. N., & Hoyer, E. H. (2018). Increasing patient mobility through an individualized goal-centered hospital mobility program: A quasi-experimental quality improvement project. Nursing Outlook, 66(3), 254–262. https://doi.org/10.1016/j.outlook.2018.02.006
Schreiber, M. L. (2021). Mobility: A Pathway to Recovery. MEDSURG Nursing, 30(4), 279–281.
Outcomes Measures or Results
*A=Audit*TDC=Total Doc Compliance*Unit's HLM Goal= 75% or >
Apr-21 A1 A2 A3 A4 % TDC
% AM-PAC (A/D) 100 100 100 100 100
% HLM compliance 90 80.48 98 95 90.87
% HLM goal achieved 36 40.4 33.8 35 36.3
May-21% AM-PAC (A/D) 99.25 100 99.5 94.25 98.25
% HLM Compliance 93 90 96.08 96.2 93.82
% HLM goal achieved 33 23.7 34 40.5 32.8
Jun-21AM-PAC (A/D) 100 100 100 100 100
% HLM compliance 96 92 94.7 93.02 93.93
# HLM goal achieved 41 25.8 36 50 38.2
Jul-21% AM-PAC (A/D) 100 100 100 100 100
% HLM compliance 97.02 97.2 96 98.7 97.23
% HLM goal achieved 62 55.6 68 74.8 65.1
Aug-21% AM-PAC (A/D) 100 100 100 100 100
% HLM compliance 97 93 95 93.4 94.6
% HLM goal achieved 70 72 78 70.8 72.7
21-Sep% AM-PAC (A/D) 99.7 99.8 99.8 100 99.8
% HLM compliance 97 93.2 93.4 95.2 94.7
% HLM goal achieved 72 68 61.6 70 67.9
* Data displays provided by Tableau ™
* Data display provided by Tableau™
Improving LGBTQ+ Knowledge and Practice of Sibley Hospital’s Rehabilitation DepartmentClare Madrigal, BSN, RN. (she/her) LGBTQ+ Resource Nurse
NICHE Department, Sibley Memorial Hospital, Washington, DC 20016Johns Hopkins Medicine
• Currently no standardized LGBTQ+ cultural competency training is required for rehabilitation specialists, including: physical, occupational, and speech therapists, nationally or at Sibley Memorial Hospital.
• In 2016, Washington D.C. instituted Law 21-95 requiring that all healthcare occupations have a minimum of 2 hours Continuing Education Credits specific to LGBTQ + cultural competency.
• This project aims to close the gaps of existing health inequities within the rehabilitation disciplines. After implementing these initiatives, this project will serve as a blueprint for all departments within Sibley Hospital to give LGBTQ+ education that is specific to the unit’s specialty.
• An educational program with the intention to promote inclusivity, knowledge, and improved attitudes surrounding the LGBTQ+ community was implemented April-September, 2021.
•
Objectives
Background Conclusion
Conclusion
References
Results
D.C. Law 21-95. LGBTQ Cultural Competency Continuing Education Amendment Act of 2016. Retrieved from https://code.dccouncil.us/dc/council/laws/21-95.html
Hill et all., (n.d.). Introduction to LGBTQ+ Competency Handbook for Physical Therapy. Retrieved from https://cdn.ymaws.com/www.aptahpa.org/resource/resmgr/csm_2019/csm_2019_handouts/Full_Handout_LGBTQIA-doc_1_1.pdf
Burch A. Health care providers' knowledge, attitudes, and self-efficacy for working with patients with spinal cord injury who have diverse sexual orientations. Phys Ther. 2008 Feb;88(2):191-8. doi: 10.2522/ptj.20060188. Epub 2007 Nov 20. PMID: 18029393.
Implementation● A one-group pre-/post-test design was conducted
for 90 staff comprised of therapists and supportive staff that work in settings that include acute care, outpatient and a sub-acute skilled unit.
● LGBTQ+ education was created specific to rehabilitation practices.
● Training included inclusive intake forms and SOGI (Sexual Orientation & Gender Identity) data collection training.
● Resource manual created for staff reference:○ Terminology○ Scripts for inclusive intake questions &
communication.○ Inclusive & gender neutral sexual positions for
post-op joint patients & partners● Pre-Post-survey was distributed to measure effect
of LGBTQ+ education
• LGBTQ+ education for rehabilitation staff contributes to comprehensive, inclusive care for LGBTQ+ patients.
• After department-specific training, rehabilitation health care providers felt an increase of confidence caring for Lesbian, Gay, Bisexual & Transgender patients.
• Easy access to resources, including terminology, communication scripts and gender-neutral inclusive sexual positions greatly increased the confidence of physical & occupational therapists discussing post-op sexual positions with their LGBTQ+ patients.
Wiping out CLABSIsHeidi MacDonald, RN, Cara Baldini, BSN, RN, Poopak Khorasani, BSN, RN, CV-BC, Cipriani Phillip, MSN, RN, CCRN, Raphael Oguariri, PhD, MSN, RN,
Rebecca Taff, BSN, RN, and Moira McCarthy, RN
Suburban Hospital | Johns Hopkins Medicine, Bethesda, MD
Results
Background• The Johns Hopkins Medicine goal for central line-
associated bloodstream infections (CLABSIs) is < 0.71/1,000 device days.
• In February 2021, the 12-month rolling rate at Suburban Hospital was 1.17/1,000 device days.
Aims of the Project1. To review the evidence to determine if chlorhexidine
(CHG) bathing should be implemented as a hospital-wide initiative to decrease the incidence of CLABSIs.
2. To demonstrate the value of an organizational nursing council approach to implementing an evidence-based practice to improve CLABSI rates.
Description of the Intervention• Using the nursing council structure at Suburban
Hospital, a referral to the Evidence-Based Practice and Research Council (EBP) was submitted to determine best practices for CLABSI prevention.
• EBP conducted a review of the published literature which supported recommending a practice change.
• Findings were forwarded to the Professional Practice Council and an agreement on the practice change was reached.
• A draft protocol for daily CHG bathing for patients with central lines was developed with input from the Nursing Quality, Safety and Service Council.
• Once finalized and approved, the Professional Development Council spearheaded the implementation in partnership with the nursing education team.
Description of Data Collection and Analysis
• Implementation of hospital-wide daily CHG bathing occurred during March 2021.
• Monthly data on central line device days and CLABSIs was collected and reviewed.
• No CLABSIs occurred for April thru September 2021. • The rolling 12-month rate as of August 15, 2021, is 0.
84/1,000 device days, representing a reduction of the 12-month rolling CLABSI rate by 0.33/1,000 device days.
Implications for Practice• Evidence supports that daily CHG bathing reduces
CLABSI rates. • By involving direct-care nurses who are active in the
nursing council structure, the translation of evidence into practice creates a shared mental model for improving quality outcomes.
Lessons Learned• Results are shared through the nursing council
structure and at the Hospital-Acquired Infection Steering Team meetings.
• Clear communication of council members’ responsibilities and follow up are essential for success.
• Collaboration between council chairs on a quarterly basis keeps priorities aligned.
ReferencesGorski, L. A., Hadaway, L., Hagle, M. E., Broadhurst, D., Clare, S., Kleidon, T., Meyer, B. M., Nickel, B., Rowley, S., Sharpe, E., & Alexander, M. (2021). Infusion therapy standards of practice, 8th edition. Journal of Infusion Nursing, 44 (1S), S1–S224. doi: 10.1097/NAN.0000000000000396
O’Grady, N. P., Alexander, M., Burns, L. A., Dellinger, E. P., Garland, J., Heard, S. O., Lipsett, P. A., Masur, H., Mermel, L. A., Pearson, M. L., Raad, I. I., Randolph, A. G., & Centers for Disease Control & Prevention, Healthcare Infection Control Practices Advisory Committee. (2017). Summary of recommendation: Guidelines for prevention of intravascular catheter-related infections. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America, 52(9), 1087–1099. doi: 10.1093/cid/cir138
Scheier, T., Saleschus, D., Dunic, M., Fröhlich, M. R., Schüpbach, R., Falk, C., Sax, H., Kuster, S. P., & Schreiber, P. W. (2021). Implementation of daily chlorhexidine bathing in intensive care units for reduction of central-line associated bloodstream infections. Journal of Hospital Infection, 110, 26–32. doi: 10.1016/j.jhin.2021.01.007
Results
After implementation of daily CHG bathing in March 2021, no CLABSIs occurred for April thru
September 2021.
*Implementation occurred in March 2021 (data not reported during this time)
High Risk Central Lines and CLABSI Prevention in the Pediatric Intensive Care UnitsStephanie Morgenstern, MSN, RN, Katie Thompson, DNP, APRN, Jessica Kitlas, BSN, RN, Laura Fleischmann, BSN, RN
Pediatric ICU and Pediatric Cardiac ICU, Johns Hopkins Children’s Center, Baltimore, Maryland
Results
Background• Central line associated
blood stream infections (CLABSIs) have a yearly incidence of roughly 250,000 in the United States (Savage et al., 2018)
• Despite several reported risk factors for CLABSIs in pediatric and neonatal patients, there is no published tool to assess a patient's overall risk for CLABSI.
Purpose and Aims
• Purpose: Implement a standardized algorithm to identify patients at increased risk for CLABSI
• Aims include decreasing CLABSI rates and central line days, and improving clinician maintenance of central lines
Intervention• Weekly screening of all central
vascular access devices using novel algorithm in the pediatric ICUs with report to medical team with risk mitigation recommendations.
• Data Collectiono Survey of clinical staff to
evaluate central line practices and perceptions
o Nursing CLABSI bundle compliance
o CLABSI rateso Central line days
Conclusions
• Significant indirect clinical time is needed to support this initiative
• Proactive identification of risk factors can reduce CLABSI rates
• Utilizing a novel screening algorithm for central lines improves provider awareness of CLABSI risk factors
Results
0
0.2
0.4
0.6
0.8
1
1.2
1.4
1.6
1.8
2
Pediatric ICUs CLABSI Rates (per 1000 line days)
2020 2021 (January - June)
0
0.1
0.2
0.3
0.4
0.5
0.6
0.7
0.8
2020 Q1 2020 Q2 2020 Q3 2020 Q4 2021 Q1 2021 Q2
Pediatric ICUs Central Line Utilization Ratio
• CLABSI rates decreased from 1.83 to 0.83 • Line days remained steady, ranging from 1372
to 1637• Qualitative survey themes
o Improved awareness of risk factorso Positive trends towards removalo Reduction in line entries
Minimizing SARS-CoV-2 (COVID-19) Hospitalizations by Offering Monoclonal Antibodies in the Outpatient setting
Jamie O’Connor, BSN, RN, OCNKatherine Evans, BSN, RN, OCN; Alice Catches, BSN, RN, OCN; Onyinye Mkparu, MSN, MBA, RN, OCN
Medical Oncology, Sibley Memorial Hospital, Washington DC
ResultsBackgroundThe Covid-Sars-19 outbreak has hit the widely populated area in the nation’s capitol with more force currently in 2021 than last year. Using technology developed over the past year with monoclonal antibodies, studies have shown that infusions given to patients during the first ten days of symptom onset have shortened the duration of illness and prevented further hospitalization in vulnerable populations of patients. Evidence of success of these medications has shown that by giving these medications in an outpatient setting it helps reduce care costs from emergency room operations and deflects care from the intensive care units.
Aim of the ProjectTo create a community clinic where providers can refer Covid positive patients for monoclonal antibody treatments and ensure safe, effective care without disrupting infusion care in a cancer center. Monoclonal antibodies are man-made proteins that act like human antibodies in the immune system and help fight infection.
Description of the InterventionJohn’s Hopkins protocols for infection control and the CDC recommendations were reviewed after the health department determined Sibley Memorial Hospital would be a good site for monoclonal antibody infusion delivery for the surrounding community. A multi-disciplinary team including physicians, pharmacy, administrative, infection control, nursing and security were consulted for input on how operations could be made for patient referrals and direct patient care. Utilization of a nursing team consisting of oncology nurses familiar with handling patients who are acutely ill and were intimately familiar with the administration of monoclonal therapies provided the right level of expert care that these patients deserved.
Discussion & EvaluationCollaborating with the team to ensure as little cross contamination as possible, our monoclonal antibody clinic has kept covid positive patients out of waiting rooms and other areas. The data and evidence in other similar clinics around the metropolitan area have shown success rates with monoclonal antibody infusions shortening the duration and severity of illness symptoms thus preventing further decline and hospitalization. This opens hospital beds up for patients who need other forms of high level care ideally keeping our nursing staff on the units where they should be instead of treating covid patients. By keeping our vulnerable population out of the ICU, we decrease the overall cost of covid care in general.
EvaluationOver the course of the last nine months, the amount of patients needing this therapy has increased and additional staff members have been brought in the help handle the growing numbers of infusions being given. Each patient who has been treated with the current therapy has been discharged ambulatory and stable and at this point have not needed any further healthcare interventions for covid related complications. Using a small model and having a dedicated nurse who is able to help the patient prior to infusion and after to check in on their status we are able to follow each patient at Sibley and ensure high quality care.
Lessons LearnedUsing a multidisciplinary approach has been key to the success of the clinic at Sibley. Most patients report symptoms from COVID resolved within 4-8 days of treatment, and no patient treated with the current Regeneron therapy has been admitted with covid related complications after treatment.
ReferencesChen, Nirula, Heller, Gottlieb, Boscia, Morris, Huhn, Cardona, Mocherla, Stosor, Shawa, Adams, et al., for the BLAZE-1 Investigators. SARS-CoV-2 Neutralizing Antibody LY-CoV555 in Outpatients with Covid-19 (2021). New England Journal Of Medicine. 384(3) 229-237. https://www.nejm.org/doi/full/10.1056/nejmoa2029849
James, M., Kayla W., Blind, F., Barbera, Bhisitkul, Hasara, Homa, Karp, Escowitz, Haber, DeGroot, Anderson, DeLeon, De Los Santos, J., Faviere, Fuell, Gillespie, R., Glueck, Reeber, Rhodes & Rodriguez. Impact of early versus late administration of bamlanivimab on readmissions in patients with high-risk COVID-19. (2020). The American Journal of Emergency Medicine 50, 437-441.
Marovich, M., Mascola, J. & Cohen, M., Monoclonal Antibodies for Prevention and Treatment of COVID-19 (2020). Journal of the American Medical Association (JAMA), 324(2): 131-132. (2p). DOI: 10.1001/jama.2020.10245
Outcomes Measures or ResultsClinical trial Symptom relief
https://www.nejm.org/doi/full/10.1056/nejmoa2029849
-Monoclonal antibodies are designed to block viral attachment and entry into human cells, thus neutralizing the virus.-Patients may still experience symptoms of the viral infection, but symptoms are usually milder and do not typically lead to severe
COVID-19, respiratory compromise or death.
Department of Medicine Telemetry to Intensive Care Bridge ProgramKeisha Perrin-Allen, MSN, RN; Tina Kim, BSN, RN; Kelly Alagna, BSN, RN; Ian Morris, MSN, RN;
Robin Lewis-Cherry, MSN, RN; Candice Zabko, MSN, RN; Cindy Rutledge, MSN, RN; Joy Rothwell, MSN, RNDepartment of Medicine, The Johns Hopkins Hospital, Baltimore, MD, USA
ResultsBackgroundNew graduate nurses in telemetry sought a structured pathway to move into critical care. Prior to this program, no mechanism existed to advance interested candidates.
Aim of the Project• Attract and retain nurses.• Improve hiring.• Maintain a flow of candidates to
the Department of Medicine (DOM).
• Provide a career pathway for new graduate nurses into intensive care units (ICUs).
Description of the Intervention
Data Collection and AnalysisA feedback form is completed by the ICU for all bridge candidates following each immersion shift.Bridge candidates are also asked to complete a Post-Bridge Qualtrics survey on their overall experience while in in the program.
Implications for PracticeThe hiring market is competitive, and by presenting a career pathway we were able to attract the attention of this market. The bridge program could improve nurse safety, knowledge, and resilience by allowing the nurse to develop a solid foundation in telemetry before transitioning to critical care.
Lessons LearnedWith more than 100 applicants per cohort, the demand for this program is great, which supports expanding it. The Post-Bridge Qualtrics survey reveals a steep learning curve and program candidates may need additional support in an ICU setting.
ReferencesMagtibay, D., Chesak, S., Coughlin, K., & Sood, A. (2017). Decreasing stress and burnout in nurses: Efficacy of
blended learning with stress management and resilience training program. The Journal of Nursing Administration, 47(78), 391-395.
Vanderspank-Wright, B., Lalonde, M., Smith, C., Wong, S., & Bentz, J. (2018). Exploring new graduate nurse transition into the intensive care unit (ICU). Canadian Journal of Critical Care Nursing, 29(2), 35.
Qian, S., Mengyao, J., Bei, Y., Yuxia, M., Yamei, Z., & Han, L. (2021). Effect of clinical teaching behaviours on transition shock in graduate nurses. Journal of Advanced Nursing, 77(20), 753-764. Doi: http://dx.doi.org/10.1111/jan.14635
Degrande, H., Fugin, L., Greene, P., & Stankus, J. (2018). The experiences of new graduate nurses hired and retained in adult intensive care units. Intensive and Critical Care Nursing, 49, 72-78. Doi: https://doi.org/10.1016/j.iccn.2018.08.005
Kim, S. and Kim, J. (2021). Association of work environment and resilience with transition shock in newly licensed nurses: A cross-sectional study. Journal of Critical Care Nursing, 30(8), 1037-1045. https://doi.org/10.1111/jocn.15649
ResultsCandidates felt the telemetry unit prepared them well for the ICU.Candidates rated ICU immersion shifts as beneficial.
Cohort # # RNs in Cohort
RNs Transferred to ICU of ChoiceMICU CCU
1 8 4 02 4 2 23 10 3 34 8 TBD TBD5 7 TBD TBD
Clarity Capsule: An Innovative Approach to Support Resiliency in the MICUAlphonsa Rahman, DNP, APRN-CNS, CCRN; Ian Morris, MSN, RN; Tina Kim, BSN, RN; Tracy Hopkins, BSN, RN
The Medical Intensive Care Unit, The Johns Hopkins Hospital, Baltimore, MD, USA
Results
BackgroundThe Medical Intensive Care Unit (MICU) is a highly stressed environment with increased staff turnover and burnout. Safety surveys showed high levels of exhaustion and burnout without the ability to promote resiliency.
Aim of the Project• Use Clarity Capsule to assist staff with
acclimating to a highly stressful environment. • Support the well being of staff by providing
an restorative space for decompression and self care.
• Decrease burnout, improve resiliency, and boost unit morale.
• Measure the effectiveness and usability of the area.
Methods Implications for Practice• Critical care nurses need support for selfcare
due to high stress environment.• Small spaces could be used in critical care units
as restorative space where space is an issue.• Meditation is one of the strategy that helps
with burnout and exhaustion.• Designated space helps in decreasing burnout
(87% agreed).• There is no evidence in the literature about the
use of a small space like the Clarity Capsule.• This was a QI project. A research study may be
helpful.
Lessons Learned• Staff required lots of encouragement and
education to use the space.• HEIC consulted during COVID-19 pandemic
and provided additional steps on how to use.• New nurses with less than one year
experience, (the most vulnerable group) used the space the least (only 8%).
• Need additional support and education for newer nurses.
Results
A Collaborative Approach for the Prevention of Perioperative Pressure Injuries in the Cardiac ORs
Mary Beth Riegel, MSN, RN, CNOR; Tim Madeira, DNP, CRNP, APRN-CNS
The Johns Hopkins Hospital – Cardiovascular Thoracic Operating Room
ResultsBackground
• HAPI prevention is an important patient quality measure and isconsidered a never event.
• With more complex patient populations that are older with morecomorbidities and longer surgeries, there is a greater risk of hospital-acquired pressure injuries (HAPI).
• The contributing factors can be intrinsic, extrinsic, or related tomedical devices.
• ICU patients are especially susceptible to PIs because of critical caredrugs, decreased consciousness, lack of mobility, hemodynamicinstability, poor nutritional status, and the use of multiple medicaldevices.
• Any PI discovered within 72 hours of surgery is classified as anintraoperatively acquired PI or a complication of the surgery.
Aim of the ProjectIn the Cardiovascular Surgical Intensive Care Unit (CVSICU) at The JohnsHopkins Hospital (JHH), the incidence of HAPIs was higher than anyother ICU in the hospital. Nurses from the CVSICU and the Cardiac ORmet in March 2020 to look at the current data and plan forimprovements that would result in fewer pressure injuries.
Description of the InterventionA review of the literature highlighted the following best practices for theprevention of HAPI in the OR:• Complete a preoperative assessment for PI risk using the Scott
Triggers Risk Assessment in EPIC• Perform a skin assessment when a patient arrives in the OR• Multidisciplinary collaboration in the OR while positioning the
patient and during surgery• Follow AORN positioning guidelines• Perform a post-operative skin assessment and communication with
the nurse receiving the patientA unit-based skin champion was appointed to help with education,implement changes, and help the staff take ownership of this patientsafety issue. Since the greatest incidence of these injuries occurred onthe sacrum, it was decided to use a larger sacral foam dressing thanwhat was currently being used. Education was provided using diagramsand videos since there were variations in placement. These dressingswere dated and timed so they could be replaced according to themanufacturer’s recommendations. A sterile Bair Hugger was used on allCABG patients to maintain their body temperature. Gel pads were usedinstead of foam to protect the elbows when securing the patient’s armsby their side and under the head. Education was provided to anesthesiaand nurses about medical device-related PIs, and there was a review ofany injuries caused by devices.
Description of Data Collection and Analysis
The CVSICU collects quarterly data related to HAPIs, which is reported at the CardiovascularThoracic (CVT) OR’s monthly CUSP meeting. The Clinical Nurse Specialist also communicates aboutany HAPIs within 72 hours of surgery through emails and HEROs (Hospital Event ReportingOnline).
Implications for Practice• AORN Guidelines for Perioperative Practice provides the best
evidence-based practices for positioning patients during surgery.
• Research has shown that the application of prophylactic dressings to
pressure areas has decreased the incidence of pressure injuries.
• The first step toward implementing a preventative care bundle to
decrease the incidence of HAPIs is the early identification of risk
factors.
• Ongoing education and an improved communication system during
handoff are critical components for pressure ulcer prevention
• Upgrading the OR support surfaces to pressure-reducing surfaces is
an important step in prevention.
• Patient positioning prior to surgery is the responsibility of the entire
OR team.
Lessons Learned
• The Scott Triggers Risk Assessment Tool showed that most cardiac
surgery patients were at high risk for PIs and was not helpful in
identifying the highest risk among these patients. There needs to be
a risk assessment tool specific for the cardiac surgery patient.
• Greater communication and collaboration between nurses and
anesthesiologists across different areas can improve patient
outcomes by decreasing the incidence of HAPIs.
• This process involves many people, and there are multiple variables
with each patient with no quick fix.
• Improvement interventions need continual input from all caregivers
to see results.
References
Burlingame, B. (2017). Guideline implementation: Positioning thepatient. AORN Journal, 106(3), 227-237.
Conner, R. (Ed.). (2020). Guidelines for Perioperative Practice. Denver,CO: Association of Perioperative Registered Nurses (AORN).
Engels, D., Austin, M., McNichol, L., & Fencl, J. (2016). Pressure ulcers:Factors contributing to their development in the OR. AORNJournal, 103 (3), 271-281.
Pressure Injuries…Prevention across the acute-care continuum.(2018). American Nurse Today. Retrieved from http://www.americannursetoday.mydigitalpublication.com/publication/?m=41491&i=492685&p=1&ver=html5
Outcomes Measures or Results
As a result of this collaboration, the incidence of sacral pressure injuries has decreased in theCVSICU. There was also evidence that 95.6% of patients had a sacral dressing in place whenadmitted from the OR. In the last one and a half years, there has been an increase in the acuity ofthe CVSICU patients, with many on prolonged ECMO support due to COVID. There are also morePIs related to long-term medical devices that require innovation and monitoring. During thisQuality Improvement, there was only one lip pressure injury from an ET tube that occurred within72 hours of the OR. Consistent best practices continue being implemented in the Cardiac OR, withnursing and anesthesia taking ownership of the process. Greater communication has also beenobserved involving all disciplines within the Cardiac OR and CVSICU.
The CVSICU Bundle of Interventions:• Pre-op screening before surgery or admission to CVSICU• Use of air-fluidized specialty rental beds for “highest risk” patients• Pressure-point wound prevention using a standardized tool• Weekly wound rounds by wound champions with direct feedback given to staff• Education for CVSICU and CVOR nursing staff
5 5
3 3
2 2
1 1 1 1 1 1
Creating a Mentorship ProgramMadison Roth, BSN, RN, CCRN
Department of Medicine, The Johns Hopkins Hospital, Baltimore, MD
ResultsBackground
Mentorship is a two-way relationship in which a more experienced or more knowledgeable person helps to guide a less experienced or less knowledgeable person. It is important that the mentee have some input as to who their mentor is. It is imperative that the mentee and mentor have a good relationship that is based on trust, honesty, and availability. The mentee seeks out their mentor, who will provide guidance from personal experience to help develop clinical skills, aid professional growth, and provide emotional support. Mentorship programs are beneficial because novice nurses feel supported, experienced nurses feel rejuvenated, and nursing units have improved quality of care and engaged staff. 1
Aim of the ProjectOur goal was to implement designated nurse mentors and to improve the unit’s knowledge and view on mentorship. The aim of the project was to successfully create, implement, and improve a mentorship program on our unit.
Description of the Intervention▪ We defined our mentorship program and its components: Definition, Purpose, Importance, How it works, Goals, Expectations, Benefits, Confidentiality, and How to choose a mentor. ▪ A pre-survey was completed by our nurses. ▪ Our nursing staff was educated about the new mentorship program▪ Nurses filled out mentor request forms which included directions on how to choose a mentor. ▪ The mentees were matched to mentors, pending mentor acceptance. ▪ Mentorship Partnership Pacts were signed and filed. ▪ We implemented the program for our clin-techs. ▪ Climate checks were performed and nursing staff was re-surveyed. ▪ We intermittently reeducated and reinvigorated our nursing staff about the mentorship program via informational poster boards in the team room and flyers on the unit. ▪ As needed we re-assigned mentor-mentee matches, and matched mentors for our new staff.
Description of Data Collection and AnalysisWe performed an anonymous online pre-survey before initiation of the new mentorship program. We performed in-person climate checks and anonymous online post-surveys at both 6 months and 2 years after initiation of the new mentorship program. We utilized a PDSA template, and after each survey and climate check we studied how our nursing staff felt and brainstormed ways to improve our mentorship program. Example climate check question: “How has the mentorship program impacted you?”Example survey question: “I know what the expectations are of mentees and mentors”
Implications for PracticeImplementing a mentorship program has helped our nursing staff to feel more comfortable and be more likely to seek advice and guidance, knowing that they have a designated mentor that they can trust. We recommend that all nursing units consider implementing a mentorship program, as it has benefited both our novice and experienced nurses.
Lessons Learned▪ Let staff have a say in who their mentor is.▪ Do not ask for too many mentor choices.▪ Ask for the mentor’s approval before assigning a mentee to them.▪ Let the mentors decide how many mentees they are comfortable capping at.▪ The Mentorship Partnership Pact helps to reinforce the mentor-mentee relationship, as well as the programs expectations and flexibility. ▪ It is important to refresh and reeducate the nursing staff about the program▪ Have one designated point person to keep track of mentor requests, matching and pact signing.
References1. Dirks, J. L. (2021, February). Alternative approaches to mentoring. Critical Care Nurse, 41(1), e9-e16. doi:10.4037/ccn20217892. Nowell, L., White, D., Mrklas, K., & Norris, J. (2015). Mentorship in nursing academia: a systematic review protocol. BioMed Central, 4(16). doi:10.1186/s13643-015-0007-53. Saletnik, L. (2018, September). The importance of mentoring. AORN Journal, 108(4), 354-356. doi:10.1002/aorn.12386
Outcomes and ResultsPre-survey indicated lack of overall staff mentorship, sub-par mentor-mentee relationships, and a lack of knowledge about mentor-mentee expectations. Post-surveys showed significant improvement in mentor utilization, in quality of mentor-mentee relationships, and in staff knowledge. Climate checks indicated mostly positive feedback and identified areas for program improvement. Some staff utilized their mentors more than others, but most all were appreciative to have one. Example mentee response: “My mentor and I are always communicating back and forth. I like it. It gives people a reason to talk more”.Example mentor response: “My mentee comes to me with questions, but I don’t go to her and say let’s sit down and learn”.We found that by having designated mentors, newer nurses felt more supported and seasoned nurses felt renewed. We also discovered that having a mentorship program in place helps with staff engagement, clinical and professional development, and recruitment.
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
I know who my mentoris
I have a goodrelationship with my
mentor
I feel comfortable askingmy mentor questions
and discussing problemswith them
My mentor is availablewhen I need them
I know what theexpectation are for
mentees and mentors
My mentor gives mefeedback
My mentor helps medevelop my criticalthinking and clinical
skills
My mentor helpsfacilitate my
professional growth
Perc
enta
ge o
f “A
gree
” Re
spon
ses
Survey Questions
Survey Results
Pre-Survey Post-Survey #1 Post- Survey #2
Perianesthesia Orientation Redesign Phase I: Standardizing Minimal Documentation Across the PACUsPatricia L. Ryan, MSN, MHA, RN, CPAN (Lead); Liza Anicoche, MSN, RN, CPAN, CAPA, ACNS-BC; Peacemaker Mgboji, MSN, RN; Tricia Bulacan, BSN, CCRN; Tamara Garey ,BSN, RN, CPAN;
Rebecca Griffiths BSN, RN, CPAN; Danielle Crump BSN, RN, OCN; Melinda Walker, MSN, CPN; Kristi Wormack BSN, RN; Ashley Green, BSN, RN; Norren Cesar, BSN, RN, CAPA; MJ Monge, BSN, RN; Marifi Castillo, BSN, RN; Martha Conlon, BSN, RN, CPAN, CAPA; Patricia Guthrie, MSN,RN, CPAN; Myrna Mamaril, DNP, RN,CPAN, CAPA, FAAN, NEA-BC ; Katelynn Lee, BSN, RN, CPAN
Perioperative Services/Johns Hopkins Hospital, Baltimore, Maryland
IntroductionStandardizing orientation reduces confusion, increasing nursing safe practice. Nursing documentation remains the single largest area where differences exist and errors occur. Along with errors, issues with learning documentation accounts for increases in orientation cost due to extensions. It also accounts for a decrease in orientation satisfaction resulting in orientee and preceptor frustration. When surveyed, orientees reported their documentation differed daily based on which preceptor they were with. At times the variations orientees had to learn due to preceptor preference, lead to orientees either being extended for several weeks or failing orientation. Standardizing the documentation practices of both existing and new hire nurses showed an improvement in orientation outcomes.
ObjectivesStandardizing perianesthesia documentation’s aim was to :• Develop a consistent standardized method of charting essential
PACU data elements that reflected American Society of Perianesthesia Nursing (ASPAN) and the Joint Commission required documentation.
• Increase nurses’ satisfaction and efficiency of care. • Design training for new and existing RNs to the same standards so
all staff charts within comparable guidelines.• Reduce issues with orientees’ learning clinical documentation
requirements due to preceptor preferences.
Results• Data showed an approximate increase from 87% to 98% compliance with
ASPAN standards. • Areas being missed differed from unit to unit. In some cases items missed
were required but were not part of the unit’s routine. • Data demonstrated a need for re-education in those areas to harmonize
over all PACUs. • Areas for improvement were outpatient documentation, specialty
assessments, and hospital required documentation (ex: belonging documentation), however some standard items were missed in Prep and in PACU Phase I.
• Orientees stated the review and bedside reminder pages were helpful in making documentation easier.
• Preceptors reported orientees demonstrated increased documentation competency.
• Removing duplication and standardizing the intervals, resulting in more time for patient care was the greatest benefit RNs reported.
Implication for PracticeIn minimizing documentation, we systematically reduced issues with orientation and lowered stress on nurses keeping up with their workload and throughput. In maintaining a standardized documentation practice, we reduced confusion regarding what should be documented and when. This program sparked interest from other JHH Health System Prep/PACUs. The standardized design of this pilot can be readily used by other perianesthesia units to meet both ASPAN and Joint Commission requirements for Epic documentation.
Minimal Documentation Bed Side Guides
Implementation• Eight of the 11 PACUs at the East Baltimore Campus of The Johns
Hopkins Hospital worked together via committee to design documentation guidelines based on goals aimed at improving compliance and decreasing confusion.
• Minimal documentation standards were designed and approved to be applicable to many different Prep and PACUs.
• Units identified one champion to manage unit superusers.• In June, the superusers trained end-user groups. Nurses received
classes on the standards then practiced in Epic play environment. • New standards were piloted on nurses in orientation. • Preceptors held their orientees to documentation guidelines. • Audits were designed to track compliance of minimal
documentation standards. • Units were grouped based on their patient population. Each group
contained two units. (ambulatory, procedural only, surgical only & surgical/procedural mix)
• Baseline audits were performed from dates prior to onset of education.
• Unit champions and superusers performed the audits first on their assigned end-user groups to gauge effectiveness of training.
• By July 2021, the audit data began to be collected and disseminated bimonthly to superusers to give real time feedback to their end-user group members.
• By August, end-users started auditing their team members twice monthly to reinforce minimal documentation training.
• As survey numbers and compliance improved, end user audits were decreased to once per month.
Preop PACU Phase I PACU Phase II
Compliance Data Analysis
ReferencesDe Groot, K., De Veer, A. J., Paans, W., & Francke, A. L. (2020). Use of electronic health records and standardized terminologies: A nationwide survey of nursing staff experiences. International journal of nursing studies, 104, 103523.
Kusumaningsih, D., Hariyati, R. T. S., Hutahaean, S., Anggraini, N. V., & Nopriyanto, D. (2020, November). Efforts to Optimize the Orientation of New Nurses: Pilot Study. In International Conference of Health Development. Covid-19 and the Role of Healthcare Workers in the Industrial Era (ICHD 2020) (pp. 282-288). Atlantis Press.
Swietlik, M., & Sengstack, P. P. (2020). An Evaluation of Nursing Admission Assessment Documentation to Identify Opportunities for Burden Reduction. Journal of Informatics Nursing,5(3), 6-11
Tajabadi, A., Ahmadi, F., Sadooghi Asl, A., & Vaismoradi, M. (2020). Unsafe nursing documentation: A qualitative content analysis. Nursing ethics, 27(5), 1213-1224.
Lessons Learned• Collaboration within large groups proved at times to be challenging.• Population specific Prep/PACUs demonstrated that the standards did
not always apply to all areas. • Finding consensus and adding avenues to recognize each unit’s special
needs allowed the group to come together. • Piloting the program with nursing orientees proved beneficial in the
data and real time feedback it provided. • COVID caused a delay of 6 months in creating and implementing the
standards due to low staffing and higher patient census/acuity. • Adjustments in data collection needed to be made for appointment
based areas due to differences in Epic access.• Some RNs preferred to continue documenting more than needed. Will
continue to audit to see if this affects compliance over the long run.
Nursing Satisfaction Survey Results
N= 42 responses
Response time was 2 weeks
RNs surveyed at month 4 of the pilot.
Acknowledgements:Nurses of Johns Hopkins Electrophysiology, Outpatient, Radiation Oncology, Smith Bendann, Weinberg, Weinberg Phase II, Zayed 3, and Zayed 5 Prep PACUs for participating in the design and pilot of the Minimum Documentation Standards QI project.
83.8
96
86
85.5
87.825
95.3
95
94.2
94
94.6
93.6
99
96.7
0
96.4
97.7
100
97.7
98
98.3
0 20 40 60 80 100 120
Ambulatory
Procedural only
Surgical Only
Surgery/Procedural Mix
Average All
Minimal Documentation Chart Audit Data
September August July Baseline
N= 244 audits
Just in Time: A Hybrid Learning Model for UAP Orientation Propelled during a Global PandemicMargo Preston Scott, MSN, NPD-BC, Stefanie Mann, MS, NPD-BC
Office of Nursing Professional Practice, The Johns Hopkins Hospital, Baltimore, MD
ResultsBackground
Aim of the Project
Description of the Intervention
Description of Data Collection & Analysis Implications for Practice
Lessons Learned
References
Outcomes Measures or Results
Onboarding of new staff is necessary in healthcare. With the increased demand for Unlicensed Assistive Personnel (UAPs) , lack of experience performing sterile skills, and lack of efficiency in classroom teaching time, educators were prompted to develop an innovative Hybrid Learning model for delivering orientation content. When the COVID-19 global pandemic began, NPD practitioners were well prepared to continue to meet the demands of onboarding new UAPs. The use of a hybrid learning model met CDC safety guidelines and increasing hospital demands for UAPs and patient care.
Survey completion rate was 75-95% depending on the segment evaluated. Although 78% of our new clinical technicians had prior experience with sterile gloving, only 20-40% had experience performing sterile skills. 99% of our learners enjoyed the gamification of content and found the access easy and met the learners’ needs. Finally, 100% of our learners found the refresher session useful and 96% felt confident in their skills performance after the session.
The hybrid learning model included three phases:1. Four online learning modules (concepts of sterile
technique, patient monitoring, patient safety, & wound care) with a review of skills videos, and a comprehensive assessment using formal and gamification methods
2. Instructor-lead skills refresher3. Final demonstration of skills
• New UAP hires were given four separate evaluation surveys that assessed skill readiness, the online platform, gamification of content and methods, and effectiveness of skills refresher.
• Each evaluation was converted to a QR code for ease of use and to increase the response rate.
• Confidence in skill performance and satisfaction in educational content were measured after each onboarding session.
• Data was collected for 13 months and included 73 UAPs.
The project aimed to develop an onboarding blended hybrid learning model for all types of UAPs learners that met the skill requirements for the Clinical Technician position, in an efficient, safe manner.
Testimonials“This was an awesome session. I am more confident for it”.“The refresher course was very helpful, definitely in areas where I haven’t practiced that skill in some time as well as the skills I’ve never utilized”.“I was very nervous coming in, but the instructors were very calm and helpful”.“I appreciate this class because it helped to gain knowledge of skills I never had to perform”.“Love this it should be given all the time”.
2.4 % Increase25% Time Reduction = $40/UAP or $4000/100 UAPs
• NPD practitioners will develop an innovative, interactive, orientation hybrid model, that meets learning needs for UAPs, using multiple enjoyable and applicable teaching methods, while increasing skill performance confidence.
• Improving efficiency while maintaining safe instruction prompted the NPD practitioners to seek out additional methods to streamline content while using interactive engaging methods that would serve varying levels of UAP experience.
• A 25% reduction of NPD practitioners’ time allows for further efficiency in training, less indirect time for direct care roles, less backfill of other clinical roles, and more time in scope of practice.
• Despite efforts to communicate the new format, there were challenges with UAPs completing modules before attending the in-person refresher courses.
• Multiple reminders were required for clinical department educators to register the UAPs for the sessions.
• UAPs are hands-on learners and prefer in-person sessions.
• Sessions were impacted by variability in skills.
McCrea, K. A., Leathers, B. N., Heitman, L. C., Hawkins, E. K., Abbott, T. M., & Opsahl, A. (2021). Transitioning Professional Development Classes to Virtual Instruction. The Journal of Continuing Education in Nursing, 52(9), 404–406. https://doi.org/10.3928/00220124-20210804-04
Noza Margallo, D., Billner-Garcia, R., & Bradley, K. (2021). The Show Must Go On: Using Technology for Rapid Onboarding and Orientation During COVID-19 and Beyond. The Journal of Continuing Education in Nursing, 52(3), 115–117. https://doi.org/10.3928/00220124-20210216-04
Improving the Safety of Medication Administration Using Dose Error Reduction SoftwareStacy Shilling MS, RN, Linda Fair MAS, RN, CCRN-CMC, Jedediah Gervacio BSN, RN, VA-BC, Rosemary Duncan, PharmD, BCPS, Ed Horvath, BS
The Johns Hopkins Hospital, Baltimore, MD
Introduction• Using Dose Error Reduction Software (DERS,
or the “drug library”) reduces smart pump programming errors. However, compliance with using DERS varies widely from 62% to 98% among 22 published studies.1
• The Institute for Safe Medication Practices recommends 95% compliance.
• Smart pump compliance at The Johns Hopkins Hospital (JHH) ranged from 35 - 47% in January - June 2020 revealing an opportunity for improvement.
Methods• Observations and interviews were conducted
over a four-week period on adult inpatient units and procedural areas. Nurses were asked to set up simulated infusions on a smart pump and trained observers watched for programming errors and method for using the Guardrails library.
• Nurses were then interviewed regarding barriers to use of the drug library. Reasons for not using the drug library were later categorized and analyzed for themes. Descriptive statistics were applied to determine frequency of themes.
• Updates were made to the Guardrails drug library based on the identified barriers. Following the drug library update, audits were conducted on active IV infusions in adult inpatient and procedure areas. Operative and perioperative areas were excluded, and patients on isolation precautions were excluded. Audits recorded the patient location, whether Guardrails Drug library, IV Fluid library, or Basic Infusion mode was being used, and names of medications/fluids infusing.
• The observations allowed us to determine compliance for individual units and conduct real-time education with bedside nurses.
Results
Discussion• This multifaceted approach increased drug
library usage by 38% in eight months. • Interviewing nurses about perceived
barriers was a valuable process that led to extensive changes to the drug library and improved ease of use.
• Despite more than doubling our compliance rate, we are not yet to the goal rate of 95% and more work remains to be done in this area.
Getting feedback from nurses helped us improve the Alaris Drug Library
navigation and now more nurses are using it!
Themes Number (%) Total N=116
No Barriers 20 (17.2%)
Medication being infused not available in library or cannot be located in library
37 (31.9%)
Significant time involved in programming 12 (10.3%)Drug or fluid specific concern 24 (20.7%)
Lack of education or use on library contents
14 (12.1%)
Other 9 (7.8%)
Johns Hopkins Hospital GuardrailsTM
Drug Library Usage
GuardrailsTM
Infusions (%)Basic Infusions
(%)
January 2020 35% 65%August 2021 73% 27%
Guard of Rail DrugsBy Margaret Chiumento
Meyer 3
Read more about our
project here!
A Novel Nursing Approach in Reducing Catheter-Associated Urinary Tract Infections in a Regional Burn Center
Lisa C. Smith, MSN, RN, Carrie A. Cox, MSN, RN, Rowena Orosco, BSN, RN, Carolina Flores, BSN, RN, Julie Caffrey, DO, MS, FACOS
Department of Plastic and Reconstructive Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, USA;Department of Nursing, Johns Hopkins Bayview Medical Center, Baltimore, MD, USA
Catheter-associated urinary tract infections (CAUTI) adversely affect more than 30% of patients in critical care hospital settings. Considered one of the most prevalent of nosocomial infections, CAUTI are linked to extended hospital stays, rising health care costs, as well as increased morbidity and mortality in patients. CAUTI are attributed to prolonged catheter use, contaminated catheter insertion, and improper care and maintenance of the catheter system. Adhering to infection control guidelines is essential in preventing CAUTI in healthcare institutions. To illustrate, nearly 380,000 CAUTIs could be prevented, and 9,000 lives saved, annually, with the prevention of CAUTI (Centers for Disease Control and Prevention, 2019).The National Healthcare Safety Network (NHSN) employs two measures for the surveillance of CAUTI, as well as other hospital-acquired infections. The first measure is the Standardized Infection Ratio (SIR), which can be calculated as the number of observed catheter-associated tract infections divided by the number of predicted infections. The second measure, the Standardized Utilization Ratio (SUR) is calculated by dividing the number of observed urinary catheter device days divided by the number of predicted device days (CDC, 2018; CDC, 2019).
Background Description of Data Collection and Analysis Results
Lessons Learned
From January 2019 to present, our burn team has been diligently working to reduce the catheter-associated urinary infection (CAUTI) SIR and SUR in the Regional Burn Center. Efforts to facilitate this reduction include the education of staff nurses, physicians and physician assistants using rounds and meetings as teaching platforms for appropriate indications for initial placement, replacement, and removal of indwelling urinary catheters. We also developed and assigned a PowerPoint presentation and post-assessment to staff members to educate and measure their understanding of the proper care for patients with urinary catheters in place. The hospital facility’s Indwelling Urinary Catheter Discontinuation Protocol was revised to reflect the specific needs and alternatives for urinary catheters in our burn patient population. The Indwelling Urinary Catheter Discontinuation Burn Nursing Protocol now serves as a guideline for the multidisciplinary team during daily rounds to reduce the risk of CAUTI in the burn center. Charge Nurses continue audits on patients with urinary catheters with real time re-education to strengthen the knowledge of staff nurses on the important aspects of catheter care and to empower nurses to reduce the risk of CAUTI in their patients.
The SIR benchmark for 2019 was 0.774. The SIR for the Burn Center at JHBMC in the 3rd quarter of 2019 was incalculable because the predicted number was less than 1 (two infections that quarter). The SIR for the 4th quarter of 2019 was 0.913 with 1 infection. The SUR benchmark for 2019 was 1. The SUR for the Burn Center in the 3rd and 4th quarters of 2019 were 1.035 and 1.150, respectively. This data indicated the need for a comprehensive plan for improvement.Following the implementation of our team’s comprehensive improvement plan, the SIR and number of infections for the 1st quarter of 2020 was 0, which is below the SIR benchmark 0.727 for 2020. The plan we instituted also reduced the SUR to 0.897 for the 1st quarter of 2020, compared to the benchmark of 1 for 2020. The SUR rate for the 2nd quarter was 1.118. We continue to dedicate our time and effort in driving and maintaining our SIR and SUR values below the national benchmarks.
Aim of Project
Employing national guidelines and evidence-based literature to enhance our knowledge and guide our practice can result in the reduction of the utilization of indwelling urinary catheters and the occurrence of CAUTI. This strategy empowers nurses to work collaboratively with the care team to improve patient outcomes.
References
Centers for Disease Control and Prevention. (2019). Guideline for Prevention of Catheter-Associated Urinary Tract Infections 2009.
Centers for Disease Control and Prevention. (2019). NHSN’s Guide to the SIR.
Centers for Disease Control and Prevention. (2018). NHSN’s Guide to the SUR.
• To reduce catheter-associated urinary tract infections in the Regional Burn Center by reducing the urinary catheter utilization rate and improving catheter care.
• To use evidence-based research to re-educate staff on best practices in catheter utilization and care.
0
0.2
0.4
0.6
0.8
1
1.2
1.4
SIR SURBenchmark 2019 2019 (4th Q)Benchmark 2020 2020 (1st Q)
References
Lorem Ipsum
In the tradional model, paent care in the hospital is delivered in silos by different care providers. This needs to be eradicated to deliver opmal paent care. Enhanced Recovery Aer Surgery (ERAS) pathway is a new standardized, muldisciplinary and collaborave, quality iniave that is evidence-based associated with beer outcomes for surgical paents.
With the With the connuous challenge posed by reimbursements, HCGH has a considerable interest in implemenng efficient and cost effecve iniave that improves paent care, paent and family sasfacon, and paent experience to support the Johns Hopkins Medicine Innovaon 2023 strategic plan – Improve the quality and affordability of health care; hence the birth of ERAS at HCGH: a muldisciplinary and collaborave iniave.
Develop and implement a standardized, paent centered protocol at Howard County General Hospital (HCGH) to facilitate opmal recovery of paents undergoing surgery or procedure which integrates the pre operave, intra operave, post operave, and post discharge phases of care to reduce hospital length of stay (LOS); and improve paent/family experience and sasfacon by ge ng the paent back to normal preoperave funcon.
The success of the iniave is dependent upon the proacve parcipaon of highly commied and collaborave muldisciplinary teams. HCGH colorectal cases data from NSQIP between 2015 to February 2017 has shown 1.3 days reducon in hospital length of stay (LOS) and 1 day earlier transion into oral pain medicaon due to more tolerable post operave pain (Diagram 1).
HCGH is enrolled in the AHRQ Safety Program for Improving Surgical Care and Recovery (ISCR), a collaborave program launched by American College of Surgeons (ACS) and Johns Hopkins Medicine Armstrong Instute for Paent Safety and Quality to enhance the recovery of paents using the principles and methods from Comprehensive Unit-basaed Safety Program (CUSP). HCGH colorectal data from ISCR between 2018 to 2020 has shown >80% adherence in Mul-modal Pain Management, First Postop VTE Chemoprophylaxis Dose, and and Foley Removal. First Postop Mobilizaon has >80% adherence while First Postop Intake of Liquids has 70-80% adherence in 2020 (Diagram 2). Since the ERAS best pracces and the CUSP principles were ingrained, improvements were sustained despite the COVID 19 pandemic. The team is mindful about the work that needs to be done to impact the metrics that are <70% adherence.
ERAS at HCGH strongly promotes muldisciplinary collaboraon and the use of evidence-based pracces to deliver opmal care to surgical paents. Educaon of care providers and paents; connuous monitoring of compliance with the protocol, including barriers; and collecon of outcomes data are imperave to the success of the iniave. Improved outcomes, decreased LOS, and improved paent/family sasfacon have strongly encouraged perianesthesia nurses’ commitment and parcipaon.
Diagram 1
Diagram 2
On January 2016, a muldisciplinary ERAS Steering Commiee headed by a colorectal surgeon was developed. The commitee was tasked to create ERAS pre-op orderset and protocol, and ERAS resource booklet for paents and their family. The commiee also worked to get the buy in, disseminate informaon, and educate the different stakeholders about ERAS. On April 2016, ERAS was piloted with colorectal cases and later expanded to GYN and Orthopedic cases. On February 2019, ERAS was expanded to all surgical paents to promote and support “ERAS for ALL.” The NPO Guidelines for care prproviders were revised; the Adult Fasng Instrucons Before Surgery was created to promote carb loading 2 hours prior to surgery; and the Surgical posng sheet was revised.
Appointment with Surgeon-Surgery discussion begins•Preparaon for surgery••Recovery aer surgery
Paent educaon & Informaon disseminaon•Nutrion counseling•Smoking cessaon•”P•”Prehabilitaon”
-Paents are no longer NPO at midnight!-Drink Gatorade 2 hours before surgery-Pre-op area•Warming blanket-P-Pre-op meds for pain & nausea•Gabapenn•Acetaminophen•Celebrex•Scopolamine
Goals-Maintain normothermia-Minimize hypotension/hypoxia-Minimi-Minimize IVF with goal directed therapy-Minimize narcocs-PONV prophylaxis
Goals-Superior pain control - mul-modal analgesia-Minimize opioids--Early oral intake for GI funcon-Early mobilizaon-Early foley catheter removal-Minimize complicaons
Goals-Return to preoperave state-No readmission
New Pt CLinic Visit
Paent Educaon
PACU & Inpt Units
Pre-op OR Home
Maria Liza Anicoche, MSN, RN, ACNS-BC, CPAN, CAPA; Patricia Anne Bulacan, BSN, RN, CCRN; Kelly Webber, MSN, RN, MUS, MA-T. Integrated Music; Sylvia Urso, BSN, RN, Laura Kaiser, MSN, CPAN; Myrna Mamaril, DNP, RN, NEA-BC, CPAN, CAPA, FAAN, FASPAN
Perioperative Services, The Johns Hopkins Hospital, Baltimore, MD
ResultsIntroduction/Background
Patients undergoing major cancer surgery frequently expressincreased anxiety about how severe their pain will be and what willbe their oncology surgical outcomes. Laparoscopic radicalprostatectomy surgery patients have reported severe pain postoperatively and experienced psychological distress for potentialurinary incontinence and sexual dysfunction. Over this past year, painmanagement was also identified as the primary cause of patients’increased length of stay in post anesthesia care unit (PACU). ThePACU staff conducted a music listening evidence-based practice (EBP)project that recommended investigating complementary musiclistening methods.Null Hypothesis: There will be no difference in reported anxiety scores and pain scores between intervention groups
Purpose of the StudyTo compare two methods of music listening interventions on
anxiety, pain, heart rate, blood pressure, and oxygen saturationamong post anesthesia care unit (PACU) patients who are recoveringfrom laparoscopic radical prostatectomy surgeries:a) patient-preferred music listening via Spotify selections; andb) relaxation breathing narrative over minimalistic hypnotic music..
MethodologyProspective randomized comparative mixed method study of two
non-pharmacologic nursing music listening intervention groups explored effects of music on anxiety and pain management. Group I received patient-preferred music selection via Spotify consisting of assortment of artists. Group II received a narrative of relaxation/breathing exercises with minimalist, hypnotic music. Both groups listened to music before and after surgery.
A power analysis was calculated to have 80% power to detect between-group differences, with Type I error rate of 0.05.
Inclusion criteria:45-80 year old males; all ethnic backgroundsExclusion criteria: No visual, hearing, cognitive, psychiatric
deficitsStudy recruited 77 male participants who were randomly assigned
by a computerized table of random numbers to either the Spotify preferred music selection Group I (n=37) or relaxation breathing instructional narrative with hypnotic music Group II (n=40). Which were prepared in advance with coding placed on serially numbered envelopes containing the research consent, Spielberger STAI-Y questionnaire, and Baseline PACU Data Collection Tool.12 The envelopes were prepared by a person who was independent to the study and PACU nurses were blinded to the two interventions.
Ethical approval granted by JHMIRB eIRB00200771; Registered Clinical Trial NCT04596917.
Interventional Music Listening DevicesApple iPod Touch 32 GB devices were pre-programmed by the hospital IT Department staff to automatically log in to each email account and were set to the following:Group I was coded as ABA devices—set to Spotify Home screen to play patient’s preferred music choices from a search or featured album.Group II was coded as BAB devices—set to JHH Playlist with one instrumental minimalist track (relaxation and breathing exercises) downloaded on a loop playback.The pre-programmed iPods used the Maxell Solid2 Black Stereo over ear with noise-canceling Headphones with HygenX, Disposable Ear Covers. Spotify premium account created with x4 unique login emails for each iPod device.
DiscussionPain medication use did not differ between the two groups. Notably,three study participants did not require any pain medicationthroughout their entire PACU stay. Both interventions reduced STAIscores and pain scores to a similar degree; this reduction was clinicallyand statistically significant. These interventions should be importantcomplementary techniques for all surgical patients, especially in a busy,fast paced perianesthesia clinical setting.
Outcome Measures/ Results
Acknowledgements – Weinberg Prep PACU Staff
References1. Cho, SWC & Choi H. Effect of Music on Reducing Anxiety for Patients Undergoing Transrectal Ultrasound-Guided Prostate Biopsies: Randomized Prospective Trial. Urology Journal, 2016: 13(2), 2612-2614.2. Hole J, Hirsch M, Bell E, Meads C. Music as an aid for postoperative recovery in adults: A systematic review and meta-analysis. The Lancet, 2015: 386(10004), 1659-1671.3.Bojorquez G, Jackson K & Andrews A. Music therapy for surgical patients: Approach for managing pain and anxiety. Critical Care Nursing Quarterly, 2020:43,4.Kavak- Akelma, F, Altınso S, & Arslan M T. Effect of favorite music on postoperative anxiety and pain. Der Anaesthesist, 2020: 69, 198–204.5.Engwall M & Duppils G S. Music as a nursing intervention for postoperative pain: A systematic review. Journal of Perianesthesia Nursing, 2009: 24(6), 370-383.6.Spielberger CD, Gorsuch RC, Lushene RF. Manual of the State Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologist Press; 1970
Music Listening as a Postanesthesia Care Unit (PACU) Nursing Intervention for Laparoscopic Radical Prostatectomy Patients: A Randomized Comparative Clinical Trial
ConclusionStudy revealed both relaxation track and personally selected music can meaningfully improve patients’ anxiety and PACU pain scores.
Procedure/Description of Data Collection Procedure:: PACU co-investigators, using a preapproved research recruitment script, called the patients the day prior to their scheduled surgery to invite them to participate in the music listening study. • Day of surgery, principal investigator/co-investigators consented subjects in waiting room• Subjects completed Spielberger STAI-Y questionnaire in waiting room • Patients escorted to Prep Unit (changed into gowns, vital signs, pain scores were obtained)• Patients listened to assigned music interventions for 15 uninterrupted minutes of music,Data Collection: In PACU, patients listened to assigned interventions after emergence from anesthesia until transfer to inpatient unit. Once discharge criteria met, patients were asked about music listening experience.
Implications for PracticeListening to music is relatively easy to use in many different patient settings. Our findings suggest that music listening is safe, inexpensive, and effective intervention in postop setting. When comparing the cost of the two nursing listening interventions, the relaxation breathing exercises that were pre-recorded over minimalist hypnotic music were a one-time cost and proved to be less costly than the $15.00 per month or $180.00 annually
LimitationsSingle-center study limits generalization; Listening duration differencebetween 2 groups limits comparability of intervention; Study onlyincluded men and not generalizable to women.
Themes Quotes/Stories
Relaxation & Distraction
“It was very relaxing. It was very good. It helped me focus less on my surgery.”“It was relaxing. Postoperatively, I had some pain, and the music helped with the pain. Music was a distraction. It was very helpful.” Patient chose acoustic guitar at first. "Music helped me relax especially when I'm left by myself. Very calming. I like it.""The relaxation and breathing really helped me in the PREOP before my surgery and especially after surgery. This was very beneficial, as I was very anxious.""I feel relaxed, comfortable, and it helped provide distraction."
“I found it enjoyable and relaxing because it covered up some of the other noises around here.”“I like it. It's a pleasant distraction. I think it's helpful.”“I like it, and it helped me focus on the music and not the surgery.”
“Relaxing. It helped to clear my head.”“Perfect! Awesome! I listened to music! I wouldn't have made it for three hours without music before surgery. Moderately anxious before surgery.” There was a major OR delay > 3 hours. The patient’s wife states the patient was, “smiling into the OR.”
Relaxation & Comfort
"It made me feel relaxed and like I was dancing.""Relaxing." “I enjoyed the music listening.""Worked better for the pain & relaxation""Very good and very relaxing with the breathing meditation"
"Awesome! Very relaxing for me! I enjoyed it!""It was soothing.""It's very relaxing. I was listening for about 5 minutes and my wife can tell you my HR went down. I never had any pain medications after except my stomach became queasy after drinking water."
"The relaxation and breathing really helped me in the preop before my surgery and especially after surgery. This was very beneficial as I was very anxious. "It was hard to get the iPod working in prep but once he was in PACU he stated, "I loved it; very relaxing. I would recommend to all patients."
"Helped me a lot POSTOP. It made me relaxed.""Relaxing and very comfortable."“Very relaxing.”"I did not hear music, just the breathing techniques and relaxation. It was a good, relaxing experience."
Narratives on Music Listening Experience
Figure 2: Comparison of PACU pain score by group and visits
Figure 3: Comparison of S anxiety scores by group and visits
Quantitative Results Qualitative Inquiry Results
Correlation between Nursing Governance and Nurse-Related OutcomesEvidence-Based Practice and Nursing Research Council, Suburban Hospital | Johns Hopkins Medicine &
Chakra Budhathoki, PhD
Results
BackgroundThe Index of Professional Nursing Governance (IPNG) is an RN-focused tool that measures nurses’ perceptions of the governance structure of healthcare personnel in their facility. Professional governance is a continuum ranging from traditional governance dominated by managers and administrators to staff-led governance where nurses are allocated increasing control and influence over their professional practice.
This study examines where Suburban Hospital lies along the shared-governance spectrum and its relationship to nurse-sensitive indicators (NSIs), patient satisfaction, and RN satisfaction.
MethodsThis multicenter study was conducted at 20 hospitals in four countries. Of 492 RNs at Suburban Hospital invited to participate, results are presented for 226 RNs from 15 units (14 adult and 1 psychiatric inpatient units).
The survey consisted of demographics, RN satisfaction questions, and 50 IPNG questions.
Overall (total) IPNG scores and 6 subscale scores are reported:1. Personnel (who controls personnel and related structures),2. Information (who has access to information relevant to governance structures),3. Resources (who influences resources that support professional practice),4. Participation (who creates and participates in committee structures related to governance activities), 5. Practice (who controls professional practice), and 6. Goals (who sets goals and negotiates the resolution of conflict at various organizational levels).
IPNG Survey Results Outcomes
ReferencesConclusions
The overall (total) IPNG score and 6 subscale scores are summarized below for the 226 RNs from the 15 study units.
Governance Type*Traditional=RedShared=Green
IPNG Average Scale Score (SD)
Overall IPNG Score[Scale range: trad=50-100; shared=101-200; self=201-250]
106.3 (24.47)
Six Subscale IPNG Scores1. Personnel[trad=12-24; shared=25-48; self=49-60]
16.8 (7.05)
2. Information[trad=9-18; shared=19-36; self=37-45]
20.0 (5.63)
3. Resources[trad=9-18; shared=19-36; self=37-45]
24.5 (6.27)
4. Participation[trad=8-16; shared=17-32; self=33-40]
17.7 (5.12)
5. Practice[trad=7-14; shared=15-28; self=29-35]
15.8 (4.43)
6. Goals[trad=5-9; shared=10-20; self=21-25]
11.6 (3.44)
*Traditional governance (lowest) = management/administration onlyShared governance = combination of staff and management/administrationSelf-governance (highest) = staff only [Note: there were no self-governance scores]
1. Hess, R.G. (2017). The measurement of professional governance: Scoring guidelines and benchmarks. Hobe Sound, FL: Forum for Shared Governance.
2. Speroni, K.G., Wisner, K., Stafford, A., Haines, F., AL-Ruzzieh, M.A., Walters, C., & Budhathoki, C. (2021). Effect of shared governance on nurse-sensitive indicator and satisfaction outcomes: An international comparison. Journal of Nursing Administration, 51(5): 287-296.
3. Speroni, K.G., Wisner, K., Ober, M., Haines, F., Walters, C., & Budhathoki, C. (2021). Effect of shared governance on nurse-sensitive indicator and satisfaction outcomes by Magnet recognition status. Journal of Nursing Administration, 51(7/8): 379-388.
For the 15 study units at Suburban Hospital, a shared-governance structure correlated with outcomes above benchmark in all domains—NSIs, patient satisfaction, and RN satisfaction.
Study site Co-PI: Raphael Oguariri, PhD, MSN, RN ([email protected])
All 15 units scored shared governance based on overall IPNG score, as well as on 5 of 6 subscales (except Personnel). NSI, patient satisfaction, and RN satisfaction data are summarized below.
NSI: # of quarters above benchmark Mean (SD)
Falls with injury 2.6 (1.24)Hospital-acquired pressure injury stages >2 2.9 (1.07)Central line-associated blood stream infection 3.6 (0.79)
Catheter-associated urinary tract infection 3.0 (0.63)
Pt. Satisfaction: # of quarters above benchmark
Courtesy and respect 2.9 (0.94)Careful listening 2.7 (1.53)Patient education 3.5 (0.76)Responsiveness 3.0 (1.00)Care coordination 3.1 (1.07)Pain 3.0 (0.89)Patient engagement 3.0 (1.41)Safety 2.7 (1.53)RN Satisfaction: % units reporting above
benchmark (%)
Autonomy 73.3%RN-to-RN teamwork 66.7%Leadership and responsiveness 100%Professional development 73.3%
Impact of Virtual Reality Training on Healthcare Providers’ Empathy Towards Older Adults with Sensory ImpairmentSuzanne Dutton DNP, GNP-BC, RNNICHE Department, Sibley Memorial Hospital | Washington, DC 20016 | Johns Hopkins Medicine
Background
Conclusion
MethodsDesign: One-group pre/post-test Sample & Setting: 129 direct healthcare providers in a mid-Atlantic community hospitalSurvey: Empathy was measured using a 5-point, validated Kiersma-Chen Empathy Scale (KCES) and participants self-reported changes in knowledge and future behaviorAnalysis: Paired t-test, ∆ mean, effect sizesData Collection: IRB-approved, Qualtrics survey
ResultsAlmost all participants agreed or strongly agreed that
VR improved their knowledge related to the pathophysiology of sensory impairments (Fig. 1).
ConclusionEvidence suggests VR is an effective intervention to
increase empathy and positively change behavior to support persons with sensory impairment.
Studies show that the human brain remembers 20% of what is heard, 30% of what is seen, and 80% of what is experienced. Virtual Reality (VR) learning methods are more effective than text or video-based learning because VR synchronously engages multiple learning systems in the brain.
Macular Degeneration (MD) is present in nearly 30% of people over age 60 and in the U.S. 11 million people have MD. Hearing Impairment is the 3rd most common reported chronic problem over the age of 65 and is present in 75% of people over 70 years.
IntroductionParticipants wore an Oculus Rift VR Headset and watched a
7-minute VR scenario by Embodied Labs from the viewpoint of “Alfred”, a 74-year-old with macular degeneration and high frequency hearing loss.
VR Tools & Scenario
Survey Results9 of 14 items (64.3%) had significant increases in empathy from .15-.66 points (Avg∆ Mean= .41) and effect sizes from .25-.68. The total score increased by .22 points, t(df=128) = -6.01, p <.01, Cohen’s d = .08.
This study evaluated the effect of VR-assisted sensory impairments on direct care health providers’ empathy and knowledge towards older adults with macular degeneration and high frequency hearing impairment.
Purpose of the Study
References1. Mendez, K.J., Piasecki, R.J., Hudson, K., Renda, S., Mollenkopf, N., Nettles, B.S., &
Han, H.R. (2020). Virtual and augmented reality: Implications for the future of nursing education. Nurse Education Today, 93, 104531-104531.
2. Ventura, S., Badenes -Ribera, L., Herrero, R., Cebolla, A., Galiana, L., & Banos, r. (2020). Virtual reality as a medium to elicit empathy: a meta-analysis. Cyberpsychology, Behavior, and Social Networking, 23(10, 667-676.
3. Wiederhold, B.K. (2020). Forging stronger bonds through technology: how virtual reality can instill empathy.
Table 1. Statistically Significant Items (p <.01) on the KCES Empathy Survey
Pre-M(SD)
Post M(SD)
∆Mean
2. I’m able to express my understanding of someone's feelings 6.12(.92) 6.47(.75) .35
3. I’m able to comprehend someone else's experiences 5.77(.97) 6.43(.67) .66
4. I will not allow myself to be influenced by someone's feelings when determining the best treatment
3.6(1.88) 4.08(2.10) .48
8. I'm able to view the world from another person's perspective 5.77(.99) 6.36(.8) .59
9. Considering someone's feelings is not necessary to provide patient-centered care 5.78(1.67) 5.29(2.22) -.49
10. I’m able to value someone else's point of view 6.47(.57) 6.62(.66) .1512. To build a strong relationship with patients, it is essential for a health care practitioner to be caring 6.53(.94) 6.77(.70) .24
13. It is necessary for a health care practitioner to identify with someone else's feelings 6.16(1.08) 6.56(.82) .4
14. It is necessary for a health care practitioner to be able to view the world from another person's perspective
6.32(.84) 6.69(.53) .37
009
4376
11
845
73
0 20 40 60 80
Disagree
Somewhat agree
Agree Strongly
Number of participants
Figure 1. VR improved my knowledge on the pathophysiology of…
High frequencyhearing lossMaculardegeneration
Over 97% of participants agreed or strongly agreed that they would utilize the information learned in their work with patients (Fig. 2). Mostly to better understand how lost patients feel (34%), utilize hearing/vision support devices (17%), change how they communicate/position themselves (15%), and check for impairments (13%)
123
103
020406080
100120
Neitheragree ordisagree
Agree AgreeStrongly
Figure 2. Utilize information in my practice
There are between 1.4-3.8 million lesbian, gay, bisexual, transgender, and queer (LGBTQ) Americans over the age of 65.1 A 2010 study found that more than half of lesbian, gay, and bisexual respondents and 70% of transgender (LGBTQ) respondents had experienced discrimination by healthcare providers.2 Older LGBTQ adults face additional impediments to healthcare because of solitude, fewer family supports, and a lack of social and support services.2
Nurses receive limited education on LGBTQ health issues and even less information specifically about LGBTQ older adults.
The purpose of this study was to evaluate the change in nurses’ knowledge and attitudes of LGBTQ patients after watching a 60-minute documentary video called Gen Silent, which depicts the lives of six LGBTQ older adults who experience homophobia and discrimination in the long-term health care system.3
Objectives
Background Qualitative Results
Conclusion
References
MethodsDesign: One-group pretest/posttest studySample & Setting: A total of 397 nurses attending a Nurse Residency Program across one academic and four community-based hospitals in the JHCRNSurvey: 16-item, 5-point Likert survey on LGBTQ Health Care Knowledge & Attitudes4 and an open-ended question. Analysis: Paired t-test, mean change, effect sizesData Collection: IRB-approved, anonymous survey administered Nov 2017 – Jun 2019
Survey ResultsOverall, nurses demonstrated statistically significant increases in 9
of 16 items. The total absolute change of the significant items was 1.76 (Avg. Δmean = .19, SD = .23)
When implementing evidence-based practices for patient centered care, it is imperative to include sensitivity training specifically on the LGBTQ community. It is a priority for healthcare systems to create an environment where LGBTQ
1. Fredriksen-Goldsen, K. I., & Muraco, A. (2010). Aging and sexual orientation: A 25-year review of the literature. Research on Aging, 32(3), 372-413.2. American Geriatrics Society, American Geriatrics Society Care of Lesbian, Gay, Bisexual, and Transgender Older Adults Position Statement, JAGS, 2015.3. Maddux, S. (Ed.). (2011). Gen silent. Novato, CA: Interrobang Productions.4. Kelley, L., Chou, C., Dibble, S. & Robertson, P. (2008) A Critical Intervention in Lesbian, Gay, Bisexual, and Transgender Health: Knowledge and Attitude Outcomes Among Second-year Medical Students, Teaching and Learning in Medicine, 20:3, 248-253.5. Witten, T.M., & Eyler, A.E. (Eds.). (2012). Gay, lesbian, bisexual and transgender aging: Challenges in research practice and policy. Baltimore, MD: Johns Hopkins University Press.
Our project hypothesized that participants would increase their knowledge of LGBTQ health care disparities and increase positive attitudes towards LGBTQ issues after watching the documentary video.
Conclusion
A total of 173 participants responded to the question, “What is the one thing you would do to change your interaction with LGBTQ patients?”
The top three most common themes were to ‘ask patients their pronouns’, followed by ‘increase my own understanding of LGBTQ issues’ and finally, ‘be more comfortable treating LGBTQ patients’.
Statistically Significant Items Pre-test M(SD)
Post-test M(SD)
∆Mean
1. LGBT populations have unique health risks and health needs.
2.06 (.90) 1.93 (.95) -.13**
2. Access to health care is the same for LGBT persons as for other members of the population.
2.87(1.14) 3.65(1.16) .79**
3. I regularly encounter LGBT individuals in my daily life.
2.53(1.12) 2.43(1.03) -.10**
8. Gender reassignment surgery is easily available and is covered by most insurance policies.
4.02 (.78) 4.19 (.79) .17**
9. I believe that homosexuality is immoral. 4.28 (.95) 4.37 (.93) .08**
10. LGBT people are less likely than heterosexual people to be in long-term monogamous relationships.
4.03 (.85) 4.18 (.86) .15**
11. I feel comfortable around people whose gender presentation is ambiguous.
2.24 (.93) 2.12 (.94) -.11**
12. As a hospital employee, I feel it is important for me to know about my patients' sexual orientation, sexual practices and gender identity.
2.46(1.15) 2.37(1.14) -.08*
15. My experiences with LGBT individuals have positively altered my beliefs about sexuality and gender identity.
2.31 (.90) 2.16 (.88) -.15**
*p <.05; **p < .01
patients feel welcomed and safe. That includes educating employees to understand what LGBTQ patient specific needs are and how we can best support them throughout the healthcare system.5
LGBTQ+ Awareness Training for Nurse Residency Program Participants: Evaluation of Knowledge and Attitude
Suzanne Dutton DNP, RN; Andrea N. Cimino PhD, MSW; MaryJo Lombardo DNP, RN; Periwinkle Mackay MSN, RN; Jessica Borthwick MSN, RN; Nia Wright MSN, RN; Melissa Gerstenhaber MSN, RN
Johns Hopkins Clinical Research Network (JHCRN)
Nurse-Led Gratitude Intervention and the Patient ExperienceCathy Lindauer DNP, RN, CEN; Karen Gabel Speroni, PhD, RN, BSN, MHSA Kim Godinez BSN, RN;
Taylor Lurz BSN, RN; Rossana Oakley MSN, RN, CMSRN; April Zakes BSN, RN
Department of Medicine, Johns Hopkins Bayview Medical Center, Baltimore, MD
Introduction / AimGratitude, that feeling of thankfulness and appreciation, is a helpful form of self-care. Study aims were: • Evaluate effect of a nurse-
led, multidisciplinary focused gratitude intervention on the patient experience
• Evaluate if by asking gratitude related questions, nurses are able to identify actionable items for nurses and / or multidisciplinary team members to improve the patient experience
Methods• After medical, adult patients
were consented they completed gratitude surveys twice a day for up to 6 shifts and a study discharge form documenting gratitude intervention perceptions
• RNs documented actions taken for six 12-hour shifts per patient responses from twice daily surveys, and intervention perceptions
ResultsDemographics: 80 patients completed the study; most were female (57.5%), average age was 56.1 years, and length of stay was 8 days Intervention Helpfulness: •Mean 4.1: How helpful it was to share what was working well regarding
hospitalization (1=Very unhelpful; 2=Somewhat unhelpful; 3=Neutral; 4=Somewhat helpful; 5=Very helpful)
•Mean 4.3: How often a nurse we able to improve hospitalization experience (1=Never; 2=Seldom; 3=Somewhat often; 4=Very often; 5=Always)
Actions Taken: RNs took actions for 50% of patient responses, including collaborating with multidisciplinary teams (30.6%), assistance with care (13.3%), and addressing noise (8.7%)
Conclusions•Patients ranked the nurse-led gratitude
intervention as helpful. and that nurses were able to improve their hospitalization experience
•Gratitude interventions for patients require RN action 50% of the time
•Nurses had positive perceptions regarding providing the intervention
•Nursing leaders can innovate and test nurse-led and multidisciplinary team focused gratitude interventions and their effect on patient experience
Quantitative GRATITUDE INTERVENTIONS WERE HELPFUL FOR PATIENTS
QualitativeGRATITUDE INTERVENTIONS WERE POSITIVE FOR NURSES • Provide more mindful personalized care• Provide best possible care• Thankful for being able to help / be helpful“it validated that the staff was meeting the patient’s expectations”
• Publication: Lindauer, C, Speroni, KG, Godinez, K, Lurz, T, Oakley, R, & Zakes, A. (2021). Effect of A Nurse-Led, Patient-Centered, Gratitude Intervention on Patient Hospitalization Experience. Journal of Nursing Administration. 51(4): 1920199. https://pubmed.ncbi.nlm.nih.gov/33734178/
• Grant: Funding was received from the Armstrong Institute
• Contact: Cathy Lindauer, DNP, RN, CEN [email protected]
Nursing Practice SpecialistJohns Hopkins Bayview Medical CenterAlpha Commons Room 290Baltimore, MD 21224
Publication, Grant & Contact
What worked well each shift:
treatments / medications, nurses and their
professionalism, being thankful for all staff
What can be done to improve patient
experience: continue good patient care,
communication and rapport
Gratitude intervention in general: Patients were grateful, thankful and
appreciative of staff, and thinking of their own care
differently
Qualitative Analysis Patient Themes
Temporal Artery (TA) thermometry has become increasingly popular in the past decade, but no study to date directly compares its accuracy to that of axillary and oral thermometry in pediatric immunocompromised patients. Due to the high risk of immunosuppressed patients for sepsis,
accurate temperature readings are imperative. This study examined a sample of immunocompromised pediatric
patients in order to describe decisive thermometer performance on a specialized population.
The aim of this study was to evaluate whether TA temperature readings have comparable accuracy to oral and/or axillary measurements in the immunocompromised patient population.
DiscussionIntroduction
Methods
Results
48x36 Poster Template: 96 ptAuthors: 60 ptAffiliations: 50 pt
This was a descriptive correlational research study. PED patients 6 months to 22 years with any
immunosuppressive condition were enrolled. Staff were instructed on study criteria, including verbal
consent at time of temperature measurements and proper use of the Exergen TA thermometer.
Clinical decision algorithms in this subset of patients were based on whether the patient had a fever of at least 38 degrees and checked using TA along with a traditional oral or axillary route of measurement.
154 children participated in the study, contributing to 313 measurements. Each sex had equal representation in the sample (77 male and female patients). Most patients were between the ages of 2-11.
TA thermometry has shown variability in different physiologic conditions. This can also be true for both axillary and oral routes.
For low grade fevers, TA is at a different defined range as shown in literature which would need more quantification.
TA thermometry has been referenced as core temperature, however, secondary to the sensitivity and vast movement/fluctuations reported during fevers, it has shown wide variations. These wide variations show TA thermometer’s ability to quickly detect a change in body temperature.
Reynolds et al. (2014) compared TA thermometry to axillary which showed bias and precision values favoring the TA thermometer. In 52 pediatric ED children < 4 years old, “The percentage of temporal artery and axillary temperatures that were >± 1.0°C and/or >± 1.5°C above or below the clinical reference temperature 15% and 6%, respectively, for the temporal artery thermometer and 39% and 14%, respectively, for the axillary thermometer.”
In children, the oral route is not always appropriate. Kiekkas et al. (2019) mentioned TA thermometry accuracy and precision in children were much higher compared to adults with a mean difference of -0.17 degrees C (32. F) or 95% LOA (-1.14 to 0.79 degrees C (34.0-33.4 F).
Barnason et.al. (2011) concluded oral and TA thermometers were highly recommended for use in children three to 18 years of age febrile or not, whereas axillary thermometers were not recommended in febrile patients and only moderately recommended in non-febrile patients.
Temporal Artery (TA) Thermometry; is it as Effective as Axillary or Oral in Detecting Fever in Immunocompromised Children?
Ann Schaeffer BSN, RN
References
TA measurements, compared to axillary and oral trend slightly higher (expected >0.03°C more) when body temperature is near 36°C, essentially the same when body temperatures were between 37°C
and 38°C, and lower (up to an expected difference of nearly 0.5°C) at
highertemperatures.
The Bland-Altman analyses estimated a maximum expected difference of less than 1°C between TA and other measurements, even at extremely high levels of fever.
There was higher sensitivity with TA and axillary and higher specificity with TA and oral.
There were wider limits of agreement (LOA) between TA and axillary vs
TA and oral measurements. There was a higher bias when compared oral to TA (0.38) versus
axillary to TA (-0.503). Two temperatures (38.0 C and 38.5 C) were used to define fever.
Temperatures correlated better with temperatures >38 5 C There
Difference Between Oral and Temporal ArteryTemperature Reading
Difference Between Axillary and Temporal ArteryTemperature Reading
Temp > 38.0
Temporal vs Axillary
Temporalvs Oral
Prevalence 19% (13, 26.9%) 40% (33, 48%)
Agreeance 99/135 (73.3%) 139/178 (78.1%)
Sensitivity 92.3% 66.7%
Specificity 68.8% 85.8%
TA thermometer should be considered as a first choice over oral or axillary for temperature measurement in immunocompromised pediatric patients.
When checking temperatures with a TA, oral or axillary thermometer, consider rechecking another temperature site if there are concerns for fever.
Displaying and analyzing higher temperature comparisons would be valuable to clearly document when overestimations or quick decline in fevers occur.
Future studies may be needed to further validate its use in immunocompromised pediatric patients.
Limitations to this study include wide age group categories. There were also relatively few temperatures in 38.0-degree range recorded in this study, yet they were most influential describing the TA measurement discrepancy.
Conclusion
References available upon request at [email protected].
Temp >38.5
Temporal vs Axillary
Temporalvs Oral
Prevalence 9.6% (5.2, 15.9%) 22% (16, 27.7%)
Agreeance 117/135 (86.7%) 150/178 (84.3%)
Sensitivity 76.9% 56.4%
Specificity 87.7% 92.1%
Absolute Bias & Limits of Agreement (LOA) Axillary Oral
Diff (X-Y): Bias -0.503 0.038
Lower LOA -1.917 -1.421Upper LOA 0.912 1.497
www.postersession.com
Background/Objectives• While professional nursing governance exists in nursing
professional practice structures, effects of governance levels on nurse related-outcomes [i.e., nurse sensitive indicators (NSI), and patient and nursing satisfaction] has not been well studied. This is one of the first studies to measure associations between levels of governance and nurse-related outcomes. The Index for Professional Nursing Governance (IPNG) 50-item survey, version 3.0, measures professional nursing governance continuum levels from traditional to shared to self governance.1
• Study objectives: Quantify associations between IPNG governance scores to nurse-related outcomes by Magnet status (Magnet versus non-Magnet) and by location (US versus International), for both overall IPNG scores and the 6 IPNG subscale scores.
• Hypothesis: Study units with IPNG shared governance scores will have statistically significant associations with nurse-related outcomes outperforming unit level benchmarks.
Results US Versus International2
VEffect of Professional Nursing Governance on Nurse-Related Outcomes
Karen Gabel Speroni, PhD, MHSA, BSN, RN and Cindy Walters, DNP, RN, NE-BC
Study Methods• This multicenter study was conducted at 20 hospitals in 4
countries (US=17; Saudi Arabia=1; United Arab Emirates=1; Jordan=1).2,3 From these hospitals, 205 study units met eligibility criteria. For analysis reporting, study units were categorized as adult inpatient, pediatric inpatient, rehabilitation inpatient, psychiatric inpatient, ambulatory care, emergency services, or perioperative services.
• The Institutional view Board (IRB) deemed the study exempt. Informed consent was obtained.
• IPNG Survey Research: RNs (both study units and hospital-wide) completed a 58-item survey (demographics=7; nurse satisfaction=1; IPNG=50) electronically after consenting. Traveler / agency RNs were excluded. A total of 2170 RNs from the 205 study units completed the IPNG survey.
• Outcome Measures (NSI, patient and RN satisfaction): For each study unit, nurse researchers provided the number of 4 quarters (range=0-4) that NSI and patient satisfaction outperformed unit benchmarks, and if RN satisfaction outperformed unit benchmarks for the last survey. One nurse satisfaction question was also asked.
References/Acknowledgments1. Hess, R.G. (2017). The Measurement of Professional Governance: Scoring Guidelines And Benchmarks. Hobe Sound, FL: Forum for Shared Governance.2. Speroni, K.G., Wisner, K., Stafford, A., Haines, F., AL-Ruzzieh, M.A., Walters, C., & Budhathoki, C. (2021). Effect of Shared Governance on Nurse Sensitive Indicator and Satisfaction Outcomes: An International Comparison. Journal of Nursing Administration, 51(5): 287-296.3. Speroni, K.G., Wisner, K., Ober, M., Haines, F., Walters, C., & Budhathoki, C. (2021) Effect of Shared Governance on Nurse Sensitive Indicator and Satisfaction Outcomes by Magnet Recognition Status. Journal of Nursing Administration.
• IPNG scores: International hospitals had significantly higher average IPNG scores than US hospitals• Average score=shared governance: International=113.5, US=100.6 (p<.001)
• Nurse-related outcomes significantly outperforming unit benchmarks:• International: 6 of 15 (40.0%)• US: 2 of 15 (13.3%)
• Nurse-related outcomes by governance type:• Shared governance significantly outperformed traditional governance for 5 of 20
(25.0%) US outcomes (patient satisfaction=1; RN satisfaction=4); and for 3 of 11 (27.3%) International outcomes (patient satisfaction=1; RN satisfaction= 2)
• Internationally, self-governance significantly outperformed traditional governance and shared governance for 5 of 12 (41.7%) outcomes (NSI=2; patient satisfaction=3)
Study Contact: Dr. Cindy Walters [email protected]
Results Magnet Versus Non-Magnet3• IPNG scores: Magnet hospitals had significantly higher average IPNG governance
scores than non-Magnet hospitals• Average score=shared governance: Magnet=106.7, Non-Magnet=101.3 (p<.001)
• Nurse-related outcomes significantly outperforming unit benchmarks:• Magnet: 3 of 20 (15.0%)• Non-Magnet: 5 of 20 (40.0%)
• Nurse-related outcomes by governance type:• Shared governance units significantly outperformed traditional governance
• Magnet: 9 of 19 (47.4%) outcomes (NSI=2; patient satisfaction=3; RN satisfaction=4)
• Non-Magnet 1 of 15 (6.7%) outcomes (patient satisfaction)• Self-governance outperformed shared governance
• Magnet: 8 of 15 (53.3%) outcomes (NSI=2; patient satisfaction=6; RN satisfaction=0)
International analysis: • Facilitating achievement of shared governance or self-
governance is a strategy that nurse leaders can utilize to improve select nurse-related outcomes in both the US and International organizations
• Both International and US units that scored as shared governance versus traditional governance on the IPNG survey significantly outperformed benchmarks for about a quarter of measured outcomes (US=5 of 20, 25.0%; International=3 of 11, 27.3%)
Magnet analysis:• Units scoring as shared governance significantly outperformed
units with traditional governance for about half of the outcomes (47.4%)
• As the continuum of professional nursing governance improved from traditional to self-governance, the percentage increased (66.7%), as it did from shared to self-governance (53.3%)
• Units scoring as traditional governance outperformed for only 1 outcome (CLABSI) in Magnet hospitals, and 0 outcomes in non-Magnet hospitals
• Facilitate evaluation of professional nursing governance structures and processes in your organization, noting differences by unit types
• Focus on achieving and enculturating shared and self-governance as a strategy to facilitate improvement in select nurse-related outcomes
Conclusions
Implications for Practice
Self-governance
Shared governance
Traditional governance
Improve governance
levelImprove
outcomes