Critical Analysis of Bladder Sparing with Trimodal Therapy in Muscle-invasive Bladder Cancer: A...
-
Upload
independent -
Category
Documents
-
view
1 -
download
0
Transcript of Critical Analysis of Bladder Sparing with Trimodal Therapy in Muscle-invasive Bladder Cancer: A...
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7
avai lable at www.sciencedirect .com
journal homepage: www.europeanurology.com
Collaborative Review – Bladder Cancer
Critical Analysis of Bladder Sparing with Trimodal Therapy in
Muscle-invasive Bladder Cancer: A Systematic Review
Guillaume Ploussard a,b, Siamak Daneshmand j, Jason A. Efstathiou c, Harry W. Herr d,Nicholas D. James h, Claus M. Rodel f, Shahrokh F. Shariat e, William U. Shipley c,Cora N. Sternberg g, George N. Thalmann i, Wassim Kassouf a,*
a Department of Surgery, Division of Urology, McGill University, Montreal, Quebec, Canada; b Department of Urology, Saint-Louis Hospital, Assistance
Publique Hopitaux de Paris, Paris, France; c Department of Radiation Oncology, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA;d Department of Urology, Memorial Sloan-Kettering Cancer Center, New York, NY, USA; e Department of Urology, Medical University of Vienna, Vienna,
Austria; f Department of Radiotherapy and Oncology, University of Frankfurt, Frankfurt, Germany; g Department of Medical Oncology, San Camillo Forlanini
Hospital, Rome, Italy; h University of Birmingham, School of Cancer Sciences, Edgbaston, Birmingham, UK; i Department of Urology, University of Berne,
Berne, Switzerland; j University of Southern California Institute of Urology, University of Southern California/Norris Comprehensive Cancer Center, Los
Angeles, CA, USA
Article info
Article history:
Accepted February 14, 2014Published online ahead ofprint on February 26, 2014
Keywords:
Urinary bladder neoplasms
Organ sparing treatments
Outcome assessment
Chemoradiotherapy
Chemotherapy
Radiotherapy
Cystectomy
Abstract
Context: Aims of bladder preservation in muscle-invasive bladder cancer (MIBC) are to offer aquality-of-life advantage and avoid potential morbidity or mortality of radical cystectomy (RC)without compromising oncologic outcomes. Because of the lack of a completed randomised con-trolled trial, oncologic equivalence of bladder preservation modality treatments compared with RCremains unknown.Objective: This systematic review sought to assess the modern bladder-preservation treatmentmodalities, focusing on trimodal therapy (TMT) in MIBC.Evidence acquisition: A systematic literature search in the PubMed and Cochrane databases wasperformed from 1980 to July 2013.Evidence synthesis: Optimal bladder-preservation treatment includes a safe transurethral resectionof the bladder tumour as complete as possible followed by radiation therapy (RT) with concurrentradiosensitising chemotherapy. A standard radiation schedule includes external-beam RT to thebladder and limited pelvic lymph nodes to an initial dose of 40 Gy, with a boost to the whole bladderto 54 Gy and a further tumour boost to a total dose of 64–65 Gy. Radiosensitising chemotherapy withphase 3 trial evidence in support exists for cisplatin and mitomycin C plus 5-fluorouracil. Acystoscopic assessment with systematic rebiopsy should be performed at TMT completion or earlyafter TMT induction. Thus, nonresponders are identified early to promptly offer salvage RC. The 5-yrcancer-specific survival and overall survival rates range from 50% to 82% and from 36% to 74%,respectively, with salvage cystectomy rates of 25–30%. There are no definitive data to support thebenefit of using of neoadjuvant or adjuvant chemotherapy. Critical to good outcomes is properpatient selection. The best cancers eligible for bladder preservation are those with low-volume T2disease without hydronephrosis or extensive carcinoma in situ.Conclusions: A growing body of accumulated data suggests that bladder preservation with TMTleads to acceptable outcomes and therefore may be considered a reasonable treatment option inwell-selected patients.Patient summary: Treatment based on a combination of resection, chemotherapy, and radiotherapyas bladder-sparing strategies may be considered as a reasonable treatment option in properly
pean Association of Urology. Published by Elsevier B.V. All rights reserved.
selected patients.
# 2014 Euro
* Corresponding author. Department of Surgery, Division of Urology, McGill University Health Center,1650 Cedar Avenue, Room L8-315, Montreal, Quebec H3G 1A4, Canada.Tel. +1 514 934 8246; Fax: +1 514 934 8297.E-mail address: [email protected] (W. Kassouf).
http://dx.doi.org/10.1016/j.eururo.2014.02.0380302-2838/# 2014 European Association of Urology. Published by Elsevier B.V. All rights reserved.
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7 121
1. Introduction
Radical cystectomy (RC) with pelvic lymph node dissection
remains widely accepted as the gold-standard treatment
for muscle-invasive bladder cancer (MIBC) supported by a
substantial body of evidence [1–3] with long-term follow-up.
Nevertheless, removal of the bladder may lead to significant
morbidity and affect patients’ comfort and quality of life
(QoL) [4,5]. Concerns about oncologic equivalence may in
part explain differences in local utilisation rates of bladder
preservation in eligible patients among different countries
[6–9].
Several bladder-preservation options exist, including
single-modality treatments such as transurethral resection
(TUR) alone, partial cystectomy, radiation therapy (RT), or
chemotherapy alone. Nevertheless, it is generally accepted
that single-modality treatments result in inferior outcomes
compared with RC. A trimodal therapy (TMT) approach,
including maximal TUR followed by concurrent radio-
sensitising chemotherapy and RT, is the most-studied
bladder-sparing strategy. The aim of this systematic review
was to assess the modern bladder-preservation treatment
modalities, focusing on TMT in MIBC.
2. Evidence acquisition
A systematic literature search in the PubMed and Cochrane
databases was performed to identify clinical and randomised
controlled trials (RCTs) published from 1980 to July 2013
[10]. Various algorithms, including the following terms,
were used: bladder cancer, bladder preservation, trimodality
treatment, radiotherapy, chemotherapy, chemoradiation, che-
moradiotherapy, organ-sparing, bladder-sparing, and salvage
cystectomy. Inclusion criteria used were published full
articles, clinical trials, retrospective series, and meta-
analyses written in English. The following exclusion criteria
were used: (1) articles reporting on bladder preservation only
in non-MIBC (NMIBC) and only in non–urothelial bladder
cancer (BCa) and (2) abstracts and congress communications.
Each identified article was analysed and classified.
Primary outcomes included oncologic results after bladder
preservation (response rates, cancer-specific survival [CSS],
overall survival [OS]). Secondary outcomes included safety
and tolerability, long-term bladder-preservation rate, QoL,
need for salvage treatment, type of TMT regimens, and
locoregional recurrence rate defined by recurrence in bladder
or pelvic nodes. Selection of articles is shown in a flow
diagram (Fig. 1). Original articles reporting clinical trials were
separated into three categories: TMT, neoadjuvant chemo-
therapy plus TMT, and TMT plus adjuvant therapy. TMT
articles were then separated between large- and small-
sample-size (<50 patients) trials. Large-sample-size TMT
trials were then separated into two categories: prospective
phase 3 trials and phase 2 or retrospective studies (Table 1).
3. Evidence analysis
Overall, five prospective TMT phase 3 trials have been
published, including two phase 3 RCTs. The remaining
articles included in this review were large retrospective
series (with heterogeneous treatment protocols) and phase
2 trials with small cohorts. Although use of conservative
management for MIBC has yielded promising results and
gained wider acceptance, most studies have small cohorts
or limited follow-up, providing few data on long-term
oncologic safety or late toxicity.
3.1. Description of optimal treatment courses
The basic strategy of TMT is to combine an aggressive but
safe TUR of the tumour followed by concurrent chemother-
apy and RT [11]. It also includes the need for prompt salvage
RC in patients who do not respond completely or who
develop invasive recurrence. Thus, the treatment is more an
attempt at bladder preservation than definitive bladder
preservation.
3.1.1. Split versus continuous course
Cystoscopic assessment with adequate biopsy of the
previous tumour site and voided urine cytology should
be performed at TMT completion (continuous course) and
may be performed early after TMT induction (split course;
Fig. 2). In case of incomplete response, patients are advised
to undergo immediate RC. To date, no prospective study has
compared both courses (continuous versus split) [12].
Induction therapy mainly consists of radiation to a dose of
40 Gy. Consolidation radiation is continued to a full dose
of approximately 65 Gy in most trials [13]. In the continuous-
course strategy, cystoscopic evaluation with biopsy is
deferred up to 1–3 mo after the end of TMT [14].
3.1.2. Radiation regimens
Several studies have assessed the impact of radiation
fractionation on oncologic outcomes in TMT trials. The
advantage of accelerated hypofractionation has been advo-
cated [15–17], but to date, radiation fractionation has not
been reported as a prognostic factor when comparing twice-
versus once-daily fractions [13,18]. The Radiation Therapy
Oncology Group (RTOG) 0712 protocol is currently under
assessment to evaluate a twice daily versus once daily
radiation regimen.
Inclusion of pelvic nodal packets in the target volume
varied among series [13,19]. One randomised trial that
included 230 patients has highlighted that targeting only
the bladder with 2-cm margins did not adversely affect
survival and could minimise side effects compared with a
whole-pelvis volume [20]. The BC2001 trial comparing RT
with or without chemotherapy by mitomycin C (MMC) and
5-fluorouracil (5-FU) had a planning target volume of
bladder plus 1.5 cm (2 cm around the visible tumour) but
nonetheless reported only a nodal recurrence rate of around
5% [14]. Nevertheless, most planned radiation regimens
included RT to a limited pelvic region (typically to the
mid-sacroiliac region, with an upper limit of the common
iliac artery bifurcation). The rationale for including a limited
pelvic field is that regional nodal involvement is not
uncommon in muscle-invasive disease; yet, by limiting the
nodal fields in size and dose (40–45 Gy), the treatments are
[(Fig._1)TD$FIG]
Records iden�fied through databasesearching(n = 1478)
Records screened(n = 973)
Records excluded(n = 542)
Full-text ar�cles assessedfor eligibility, first round
(n = 431)
Full-text ar�cles excluded, a�er rapid review, (n = 230)
Superficial cancers (n = 19)
Cystectomy series (n = 60)
Nonurothelial cancer (n = 19)
Upper urinary tract (n = 22)
Other cancers (n = 38)
Non-English (n = 43)
No link with outcomes (n = 35)
Full-text ar�cles excludeda�er complete reading*
(n = 118)
Full-text ar�cles assessed,second round
(n = 201)
Studies included insynthesis(n = 83)
* Did not meet criteria (phase 1 trials or editorials; n = 30), radia�on without concurrentchemotherapy series (n = 21), not relevant (n = 58), or duplicate data sets (n = 9).
Fig. 1 – Systematic review selection flow diagram.
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7122
designed to potentially conserve the small bowel for future
urinary diversions, if necessary [21]. In the BC2001 trial,
patients were also randomly assigned to undergo either
whole-bladder RT or modified-volume RT, in which the
volume of bladder receiving full-dose RT was reduced
[14,22]. The trial failed to show any side effect benefit from
reducing the dose, while the noninferiority of locoregional
control could not be concluded formally. There was,
however, a direct correlation between volume of bowel
irradiated and risk of grade 3 gastrointestinal (GI) toxicity.
Daily soft-tissue computed tomography (CT)–guided setup
for RT has been shown to be superior to traditional
kilovoltage portal positioning based on skin or bony
alignment in BCa and to decrease the treatment-related
toxicity [23]. Proton beam therapy has also been assessed,
but reports remain preliminary [24].
To date, the current radiation protocol for bladder
preservation includes external-beam RT (either once daily
or twice daily) to the bladder and limited pelvic lymph nodes
to an initial dose of 40 Gy, with a boost to the whole bladder
to 54 Gy and a further tumour boost (which incorporates all
TUR and radiographic information) to a total dose of 64–
65 Gy [3].
3.1.3. Chemotherapy regimens
3.1.3.1. Cisplatin-based chemotherapy. Cisplatin is the most active
single agent for BCa in locally advanced and metastatic
settings [25]. Its radiosensitising properties are also attractive
for combined-modality therapies [26,27]. The addition of
cisplatin to preoperative or definitive RT has been shown to
improve local control in large retrospective series and in one
phase 3 RCT [28–31]. No impact on OS was prospectively
demonstrated, but this trial closed prematurely because of
slow accrual.
Different schedules of cisplatin administration did not
demonstrate any difference in terms of response rates
[13,15,20]. Intensification of chemotherapy has been
evaluated [16,29,32–34], but no definitive benefit has yet
been demonstrated.
Concurrent use of intra-arterial cisplatin-based chemo-
therapy has also been studied, but it may be associated with
higher toxicity [33,36,37]. The addition of regional deep
Table 1 – Published series of trimodal therapy for bladder preservation: homogeneous treatment regimens
Study Design and follow-up Stage No. ofpatients
Concomitantchemotherapy
RT CRrate
Salvagecystectomy rate
CSS OS
Large sample size (>50 patients) series
PROSPECTIVE PHASE 3 STUDIES
James et al., 2012z [14] Continuous
Phase 3
(second arm: RT alone)
69.9 mo
T2–T4a
N0
182 5-FU, MMC x2
(Neoadjuvant
chemotherapy: n = 57)
55 Gy or
64 Gy
– 11.4% (at 2 yr) – 5 yr: 48
Tunio et al., 2012 [20] Continuous
Phase 3
5 yr
T2–T4 N0/Nx 200 Cisplatin weekly 65 Gy
ST
93% – – 5 yr: 52
Shipley et al., 1998z [58] Split
Phase 3 (second arm:
chemotherapy-RT with
neoadjuvant
chemotherapy)
60.0 mo
T2–T4a N0/Nx 62 Cisplatin x3 64.8 Gy
ST
60% 25.8% – 5 yr: 49
Housset et al., 1993** [16] Split
Phase 3
27 mo
T2–T4 N0/N1: n = 4 54 Cisplatin + 5-FU x4 44 Gy
BID
74% N/A** 3 yr: 62 3 yr: 59
PHASE 2 OR RETROSPECTIVE STUDIES
Lagrange et al., 2011 [51] Split
Phase 2
8 yr
T2–T4a N0/Nx 51 Cisplatin + 5-FU x3 63 Gy
ST
– 33.3% – 8 yr: 36
Gogna et al., 2006 [56] Continuous
Phase 2
23 mo
T2–T4a
N0/Nx
<10 cm
T1
113 Cisplatin weekly 63–64 Gy
ST
70% 15% 5 yr: 50 –
Kragelj et al., 2005 [57] Continuous
Phase 2
10.3 yr
T2–T4a
N0/Nx
T1
84 Vinblastine weekly 63.8–64 Gy
ST
78% 8.3%
(***)
9 yr: 51 9 yr: 25
Weiss et al., 2007 [30] Continuous
Retrospective
27 mo
T2–T4a
N0/N1: n = 58
T1: n = 54
112 Cisplatin + 5-FU x2 55.8–59.4 Gy
ST
88% 17% 5 yr: 82
(for T2–4: 73)
5 yr: 74
(for T2–4: 63)
Small size (<50 patients) series
Zapatero et al., 2012 [59] Split
Retrospective
60 mo
T2–T4a
N0
39 Cisplatin weekly
(paclitaxel: n = 5)
64.8 Gy
ST
BID: n = 24
80% 33% 5 yr: 82 5 yr: 73
Choudhury et al., 2011 [19] Continuous
Phase 2
36 mo
T2–T3
N0/Nx
50 Gemcitabine weekly 52.5 Gy in 20 82%
(88%*)
14% 3 yr: 82
5 yr: 78
3 yr: 75
5 yr: 65
EU
RO
PE
AN
UR
OL
OG
Y6
6(
20
14
)1
20
–1
37
12
3
Table 1 (Continued )
Study Design and follow-up Stage No. ofpatients
Concomitantchemotherapy
RT CRrate
Salvagecystectomy rate
CSS OS
Aboziada et al., 2009 [60] Split
Retrospective
18 mo
T2–T3b N0 50 Cisplatin weekly 66 Gy
ST
60% 28% 1.5 yr: 84 1.5 yr: 100
Peyromaure et al., 2004 [61] Split
Retrospective
36.3 mo
T2N0/Nx 43 Cisplatin + 5-FU x2 24 Gy in 8
BID
74.4% 25.6% 3 yr: 75
5 yr: 60
–
Hussain et al., 2004 [39] Continuous
Phase 1/2
50.7 mo
T2–T4a N0/Nx 41 MMC + 5-FU x2 55 Gy in 20 71% 19.5% 2 yr: 68 2 yr: 49
5 yr: 36
Kaufman et al., 2000 [15] Split
Phase 1/2
29 mo
T2–T4a N0/Nx 34 Cisplatin + 5-FU x4 44 Gy
BID
67% 29.4% 3 yr: 83 –
Varveris et al., 1997 [62] Continuous
Phase 2
32 mo
T1–T4
N0/Nx
42 Cisplatin + docetaxel 68–74 Gy
ST
54.7% – – –
Tester et al., 1993 [63] Split
Phase 2
36 mo
T2–T4a
N0–N2/Nx
48 Cisplatin x3 64 Gy
ST
66% 20.8% – 3 yr: 64
Rotman et al., 1990 [64] Continuous
Phase 2
38 mo
T1–T4 N0/N1
M0/M1
20 5-FU
(+MMC in 5 patients)
60–65 Gy
ST
74% – – 5 yr: 54
Russell et al., 1990 [65] Split
Phase 2
18 mo
T1–T4 N0/N1 34 5-FU 60 Gy
ST
81% 29.4% – 4 yr: 64
5-FU = 5-fluorouracil; MMC = mitomycin C; BID = twice daily; CR = complete response; CSS = cancer-specific survival; OS = overall survival; N/A = not applicable; RC = radical cystectomy; RCT = randomised controlled trial;
RT = radiation therapy.* Defined by pT0, pTis, or pT1 after cystoscopic assessment.** 18 patients were treated by primary RC after complete response to induction treatment; only 22 patients received full chemotherapy-RT treatment.*** 17% of patients with indication for salvage cystectomy did not undergo surgery because of locally advanced, inoperable tumour and/or poor performance status.z Phase 3 RCT. CR is evaluated after induction (split course) or completion (continuous course) of chemotherapy-RT.
EU
RO
PE
AN
UR
OL
OG
Y6
6(
20
14
)1
20
–1
37
12
4
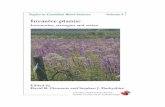
[(Fig._2)TD$FIG]
Maximal TUR
Induc�on radia�on to about 40 GyConcurrent chemotherapy
Con�nuous course Split course
Radia�on to full doseConcurrent chemotherapy
Cystoscopic assessmentwith biopsies
Cystoscopic assessmentwith biopsies
Completeresponse
Incompleteresponse
Incompleteresponse
Completeresponse
Salvage cystectomy
Surveillance
Consolida�on radia�on to fulldose
Concurrent chemotherapy
Surveillance
Fig. 2 – The two main courses of trimodal therapy (TMT): split and continuous course. The cystoscopic assessment is performed after TMT completion(continuous course) or after TMT induction and before consolidation (split course).TUR = transurethral resection.
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7 125
hyperthermia to current chemotherapy-RT has been
assessed by the University of Erlangen team with encourag-
ing results [38]. Preliminary findings in 45 patients showed
an impressive response rate of 96% with acceptable toxicity
(30% grade 3–4 toxicity).
To date, in most of protocols, chemotherapy with cisplatin
is the usual radiosensitising drug in those with adequate
renal function and remains a standard of care as no published
head-to-head phase 3 trial has examined noncisplatin
regimens versus cisplatin in BCa patients treated with TMT
with regard to efficacy and the safety profile.
3.1.3.2. Alternative chemotherapy regimens. A cisplatin-based
regimen is not acceptable for all BCa patients, because many
patients have impaired renal function caused by age,
comorbidities, or prolonged hydronephrosis. Other systemic
agents have shown efficacy as alternatives to cisplatin [35].
The regimen using MMC plus 5-FU has a proven radio-
sensitising effect with acceptable toxicity in patients unfit for
a platinum-based regimen [39].
Recently, the value of a concurrent MMC/5-FU–based
regimen in addition to RT has been supported by a
randomised phase 3 trial (BC2001), with benefits in terms
of locoregional control and relapse-free survival [14]. The
addition of this drug regimen was associated with a reduction
of 33% in the risk of locoregional recurrence and of almost
50% in the risk of invasive recurrence. However, no significant
improvement in OS was reported. Interestingly, there was a
nonsignificant trend towards higher rates of salvage RC in the
RT-only arm of the trial, suggesting whether early surgical
salvage may have prevented separation of the survival
curves. A similar effect was observed in the anal cancer trials
[40].
Low-dose gemcitabine has also been shown to be an active
and potent radiosensitiser in phase 1/2 BCa trials [19,41,42].
Twice-weekly low-dose gemcitabine is currently being
assessed with daily radiation in the phase 2 randomised
trial RTOG 0712. Other agents with evidence from a
randomised trial are tumour hypoxia–reducing drugs such
as carbogen and nicotinamide [43].
3.1.4. Contribution of each treatment modality within the trimodal
approach
Contribution of each modality to outcomes in multimodal
strategies is difficult to quantify. In properly selected
patients, acceptable outcomes can be achieved with various
bladder-preservation strategies (TUR with or without
chemotherapy, TMT, partial cystectomy).
3.1.4.1. Radiation therapy alone. For several decades, RT has
been used as bladder-sparing monotherapy for MIBC,
mainly in patients unfit for surgery. When used alone, RT
offers local control rates inferior to TMT [14,28,44]. All
available data suggest that concurrent chemotherapy-RT is
more effective than RT alone (level of evidence [LoE]: 1b).
3.1.4.2. Transurethral resection alone. It is generally recognised
that TUR alone provides inadequate cancer control and leads
to a high rate of BCa recurrence and progression. To date,
limited data exist reporting long-term outcomes after TUR as
monotherapy for MIBC [45–47]. In well-selected patients
with small muscle-invasive tumours, bladder-intact survival
rates ranged from 60% to 70%. The largest published
retrospective series assessed 151 patients after restaging
TUR [46] and a minimum follow-up >10 yr. Ninety-nine
patients were managed with active surveillance and had
Ta
ble
2–
Pu
bli
she
dse
rie
so
ftr
imo
da
lth
era
py
for
bla
dd
er
pre
serv
ati
on
:h
ete
rog
en
eo
us
coh
ort
sco
mp
ilin
gp
ati
en
tsre
ceiv
ing
va
rio
us
che
mo
the
rap
ya
nd
rad
iati
on
the
rap
yre
gim
en
s
Stu
dy
De
sig
na
nd
foll
ow
-up
Sta
ge
No
.o
fp
ati
en
tsN
eo
ad
juv
an
to
ra
dju
va
nt
che
mo
the
rap
y
Co
nco
mit
an
tch
em
oth
era
py
RT
CR
rate
Sa
lva
ge
cyst
ect
om
yra
te
CS
SO
S
Efs
tath
iou
et
al.
,2
01
2y
[13
]S
pli
t
Re
tro
spe
ctiv
e
7.7
yr
T2
–T
4a
N0
/Nx
34
8V
ari
ou
sV
ari
ou
sV
ari
ou
s7
8%
29
%5
yr:
64
10
yr:
59
15
yr:
57
5y
r:5
2
10
yr:
35
15
yr:
22
Kra
use
et
al.
,2
01
1[8
4]
Sp
lit
Re
tro
spe
ctiv
e
71
.5m
o
T2
–T
4a
N0
/Nx
47
3N
oV
ari
ou
s
RT
alo
ne
:n
=1
42
Va
rio
us
70
.4%
––
5y
r:4
9
10
yr:
30
Ch
un
ge
ta
l.,
20
07
[31
]C
on
tin
uo
us
Re
tro
spe
ctiv
e
7.9
yr
T1
–T
4
N0
/N1
:
n=
44
34
0N
eo
ad
juv
an
t
che
mo
the
rap
y+
RT
:n
=5
7
Cis
pla
tin
RT
alo
ne
:n
=2
47
Va
rio
us
63
.5%
(79
%if
che
mo
the
rap
y-R
T)
17
.4%
10
yr:
35
10
yr:
19
Ro
de
le
ta
l.,
20
02yy
[29
]C
on
tin
uo
us
Re
tro
spe
ctiv
e
60
.0m
o
T1
:n
=8
9
T2
–T
4a
N0
/N1
:
n=
32
6
41
5N
oV
ari
ou
s
RT
alo
ne
:n
=1
26
Va
rio
us
Me
an
54
Gy
(45
–6
9.4
)
+4
5G
yp
ara
-ao
rtic
ifLN
I
72
%2
0%
5y
r:5
6
10
yr:
42
5y
r:5
1
10
yr:
31
BID
=tw
ice
da
ily
;C
R=
com
ple
tere
spo
nse
;C
SS
=ca
nce
r-sp
eci
fic
surv
iva
l;LN
I=
lym
ph
no
de
inv
olv
em
en
t;O
S=
ov
era
llsu
rviv
al;
RT
=ra
dia
tio
nth
era
py
.y
Up
da
teo
fS
hip
ley
et
al.
,2
00
2[6
6].
yyU
pd
ate
of
Sa
ue
re
ta
l.,
19
98
(su
bse
to
fK
rau
see
ta
l.,
20
11
[84
]).
CR
ise
va
lua
ted
aft
er
ind
uct
ion
(sp
lit
cou
rse
)o
rco
mp
leti
on
(co
nti
nu
ou
sco
urs
e)
of
che
mo
the
rap
y-R
T.
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7126
comparable outcomes to those reported in 52 patients
undergoing RC. Solsona et al. have prospectively reported
similar results in 133 patients [47]. The 10-yr disease-specific
survival and progression-free survival rates were 80% and
65%, respectively. Nevertheless, only 11–35% of patients
were eligible for surveillance after second TUR [45,46]. In one
series, 56% of active surveillance patients developed tumour
recurrence, leading to a 30% rate of salvage cystectomy after
short-term follow-up [45].
3.1.4.3. Transurethral resection plus chemotherapy. In retrospec-
tive series with a long-term follow-up, Herr looked at
oncologic outcomes in 63 patients who were planned for
RC and declined to undergo surgery after neoadjuvant
chemotherapy [48]. All patients had a complete response
(negative TUR) to chemotherapy. Two-thirds of patients
were alive after 5 yr, and 54% of them had an intact
bladder. In a more mature study, Solsona et al. reported
results from a phase 2 nonrandomised trial comparing
TUR plus cisplatin-based chemotherapy with RC [49].
Oncologic outcomes for 75 patients who chose to keep
their bladders were compared with those achieved in 71
patients undergoing RC. Limitations are sample size, long
recruitment time, various chemotherapy regimens, and
patient selection including only highly selected invasive
tumours.
3.2. Oncologic results
3.2.1. In medically inoperable patients
Bladder preservation has been assessed in different cohorts of
inoperable patients: patients with prohibitive medical
comorbidities contraindicating radical surgery and patients
with surgically unresectable disease (Tables 1 and 2) [50–53].
In studies including only patients who had surgically
unresectable disease, OS was poor and ranged from 30%
to 42% after 4-yr follow-up [27,52,53]. It is worth noting that
these patients should not be considered to have received
TMT with curative intent and are excluded from analyses
of TMT outcomes.
In the SWOG 9312 trial, Hussain et al. classified patients
into two categories (surgical vs medical reasons) and
highlighted that this factor was predictive for OS [50]. The
criterion ‘‘unfit for surgery,’’ defined by medical comorbid-
ities contraindicating general anaesthesia or surgery, has
been associated with poorer OS [50,51].
Given these different patient profiles, most phase 2/3
trials—specifically, the RTOG protocols—included patients
who were fit for surgery (no medical contraindications) and
had resectable disease but were motivated to pursue
bladder preservation.
3.2.2. In medically operable patients
3.2.2.1. Response rate. Overall mean response rate after TMT
was 73% (Tables 1 and 2). In most series, complete response
(CR) was defined by the absence of visible tumour, the
absence of persistent pathologically proven bladder tumour
on biopsy, and the absence of tumour cells in the urine
cytology. Patients who responded completely to treatment
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7 127
induction had significantly better (by one-third) survival
rates than those who failed to achieve a CR [13,29,54]. It is
unclear what the ‘‘real’’ pathologic response after TMT
induction is. It has been assessed in a small study from
Housset et al. as 45% of complete responders having elected
to be treated by RC and not by the completion of a TMT
protocol who were found to have pT0 disease at RC [16]. In
contrast, the Memorial Sloan-Kettering Cancer Center
experience demonstrated that 30% of patients following
chemotherapy alone have residual muscle-invasive disease
on cystectomy that was not detected on the preoperative
TUR [55].
3.2.2.2. Cancer-specific survival and overall survival. CSS rates
reported in the literature are shown in Tables 1 and 2
[14–16,19,20,30,39,51,56–65]. Overall, the 5-yr CSS ranged
from 50% to 82%. In a study pooling various protocols over
time, the 5-yr CSS rate was about 60–65% [13,66].
The 5-yr OS was approximately 50%, ranging from 36% to
74% in the literature (Table 1). Discrepancies in CSS and OS
may be explained by inclusion period, patient selection,
accurate staging, duration of follow-up, differences in
chemotherapy and radiation regimens, and use of neoad-
juvant or adjuvant chemotherapy.
3.2.2.2.1. Comparison with radical cystectomy. Any direct compar-
ison between bladder-preservation modalities and RC is
difficult because of the lack of RCTs. Nevertheless, in
appropriately selected patients, the data suggest that TMT
with prompt salvage cystectomy, if necessary, can achieve
5-yr OS rates of 48–60% [13,34,67]. However, when evalua-
ting the outcomes of cystectomy series from centres of
excellence, the OS rate reached 62–68% after 5-yr follow-up
[68]. Similarly, in a 1100-patient cohort, Hautmann et al.
recently reported long-term oncologic outcomes after RC,
showing a 10-yr CSS rate of 67%, including all pT stages [69].
In a recent study from the University of Texas MD Anderson
Cancer Center and the University of Southern California that
examined patients with MIBC (cT2) without high-risk
features (hydronephrosis, palpable mass, invasion into
adjacent organs, lymphovascular invasion [LVI]) who were
treated with RC alone, the outcomes were excellent, with a
5-yr CSS rate of 83.5% [70]. This outcome in cystectomy
series appears slightly higher when compared with that of
selected TMT series (Tables 1 and 2) [71]. Furthermore,
although one has to be careful when comparing the two
approaches in subset analyses, the recent update of the
Medical Research Council neoadjuvant trial, which ran-
domised patients to neoadjuvant chemotherapy or not
followed by either RC or radiation (alone or TMT), revealed
that the OS rate of patients in the cystectomy arm was
higher than the radiation arm [72]; however, the authors
recognised that the randomisation was for the neoadjuvant
chemotherapy and that there was selection bias in
subsequent local therapy choice.
Unfortunately, clinicopathologic stage discordance and
inclusion biases limit the validity of any comparisons
between the two procedures. Patients fit for surgery and
treated by bladder preservation are rigorously selected,
with exclusion criteria such as hydronephrosis, carcinoma
in situ (CIS), or inability to perform a maximally safe
TUR, and might not be comparable with all patients
undergoing primary RC. Conversely, potential discordance
between clinical and pathologic staging has also been
suggested to introduce an outcome bias favouring cystec-
tomy series when oncologic outcomes are stratified by
pathologic stage [73]. Nevertheless, it is worth noting that
the downstaging rate between TUR and cystectomy series
ranges from 17% to 30%, and presumed cT2 tumours treated
by chemotherapy-RT may persist as pT0/1 tumours after
TUR [70,73,74].
3.2.2.2.2. Predictors of good response. BCa constitutes a hetero-
geneous group of tumours. Thus, selection criteria in
determining ideal candidates for TMT are required. It would
be relevant to identify the subgroup of BCa types that would
not respond to TMT, as the 5-yr CSS rate was lower in
nonresponders (ranging from 20% to 40%) than in responders
[13,29–75].
Historical series of RT alone have suggested that flat
lesions such as CIS, incomplete resection, locally advanced-
stage disease (T4), and the presence of ureteral obstruction
were associated with poorer response to RT [76]. The impact
of several pretreatment variables on oncologic outcomes
has been assessed [13,17,29,31,52,58,59,61,77–86].
Hydronephrosis has also been suggested as a poor
prognostic factor and was an exclusion criterion from
participation in several studies [15,35,59,87–89]. In fact,
RTOG protocols after 1993 have excluded patients with
tumour-related hydronephrosis. Hydronephrosis that occur-
red in about 10–35% of eligible patients was significantly
linked to poorer outcomes, specifically in terms of response
rates. The response rate was improved by at least 1.5-fold in
the absence of ureteral obstruction [66,89].
Although multiplicity (defined in studies as more than
one tumour) has been identified as a predictive factor for
relapse in two studies [29,36], no significant association
was found between multiplicity and CR rate or survival.
However, studies did not include patients with diffuse
multifocal disease, and TMT is not advocated in this
subgroup of patients.
Maximal TUR before bladder preservation is a strong
predictive factor of oncologic control (Table 3). This advan-
tage may be explained by the extent of the tumour and by the
completeness of the resection. Complete TUR led to a 20%
improvement in CR and bladder preservation [13]. The role of
re-TUR would be to decrease residual tumour volume and to
optimise radiation treatment. The absence of complete TUR
was also an exclusion criterion in some TMT series [59,61,88].
Most series have significantly linked incomplete TUR to
poorer response rates and survival outcomes. Its indepen-
dent predictive impact requires further evaluation, as
incomplete TUR may be considered a surrogate for pT stage
[13]. Pathologic prognostic factors such as high clinical stage,
high tumour grade, lymph node involvement, and LVI bear
witness of aggressive disease and, as in RC series, have been
associated with poorer outcomes in patients treated with
TMT [90,91].
Table 3 – Published series of neoadjuvant chemotherapy plus trimodal therapy
Study Design andfollow-up
Stage No. ofpatients
Neoadjuvantchemotherapy
Concomitantchemotherapy
RT CRrate
Salvagecystectomy rate
CSS OS
Lin et al., 2009 [88] Split
Retrospective
47 mo
T2–T4a
N0
23 Cisplatin + 5-FU +
paclitaxel
Cisplatin weekly
(or paclitaxel)
64.8 Gy
ST
73% – – 3 yr: 77
Sabaa et al., 2010 [83] Split
Retrospective
71 mo
T2–T3a N0/Nx 104 Gemcitabine +
cisplatin x3
Cisplatin x2 60–65 Gy
ST
78.8% 16.7% 5 yr: 76 5 yr: 68
Perdona et al., 2008 [82] Continuous
Retrospective
66 mo
T2–T4a N0/Nx 78 CMV x2 Cisplatin
(carboplatin: n = 25)
65 Gy
ST
85.7% 20.2% 5 yr: 79 5 yr: 72
Cobo et al., 2006 [95] Split
Retrospective
69.4 mo
T2–T3
N0/Nx
29 CMV x2 (n = 15)
Gemcitabine-
cisplatin (n = 14)
Cisplatin x2 64.8 Gy
ST
86% 24.1% – 6 yr: 72
Danesi et al., 2004 [80] Continuous
Retrospective
82.2 mo
T2–T4a N0/Nx 77 CMV x2 (n = 42) Cisplatin + 5-FU 69 Gy
ST
80.5% 22.1% 5 yr: 75
10 yr: 73
5 yr: 59
10 yr: 55
Arias et al., 2000 [81] Split
Retrospective
73 mo
T2–T4N0 50 M-VAC x2 Cisplatin x1 65 Gy
(45 Gy ST +20 Gy BID)
68% 26% – 5 yr: 48
Shipley et al., 1998z [58] Split
Phase 3 (second arm:
chemotherapy-RT
without neoadjuvant
chemotherapy)
60.0 mo
T2–T4a N0/Nx 61 CMV x2 Cisplatin x3 64.8 Gy
ST
72.5% 17% – 5 yr: 48
Kachnic et al., 1997y [89] Split
Retrospective
4.4 yr
T2–T4a N0/Nx 106 CMV x2 Cisplatin x3 64.8 Gy
ST
80% 21.7% 5 yr: 60 5 yr: 52
Fellin et al., 1997 [94] Split
Phase 2
46 mo
T2–T4
N0/Nx
56 CMV x2 Cisplatin 64 Gy
ST
50% 46.4% 5 yr: 59 5 yr: 54
Tester et al., 1996 [79] Spit
Phase 2
4.4 yr
T2–T4a
N0–N2/Nx
91 CMV x2 Cisplatin x3 64.8 Gy
ST
75% 39.5% – 4 yr: 62
RT = radiation therapy; CR = complete response; CSS = cancer-specific survival; OS = overall survival; 5-FU = fluorouracil; CMV = cisplatin, vinblastine, methotrexate; M-VAC = methotrexate, cisplatin, adriamycin,
vinblastine; BID = twice daily; RCT = randomised controlled trial.y Update of Kaufman et al., New England Journal of Medicine, 1993.z Phase 3 RCT. CR is evaluated after induction (split-course) or completion (continuous-course) of chemotherapy-RT.
EU
RO
PE
AN
UR
OL
OG
Y6
6(
20
14
)1
20
–1
37
12
8
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7 129
The presence of CIS has been correlated with higher local
recurrence rates in pure RT series [92], but the impact of CIS
on response rate after TMT has not been thoroughly studied.
Although CIS was often prognostic on univariable analysis,
the presence of CIS lost its significance on multivariable
analysis in other series [29,54,59]. The link between CIS and
response rate requires further evaluation.
Pooled together, all of these factors highlighted that a
limited number of patients with MIBC meet the criteria as
‘‘ideal patients for bladder preservation.’’ In a recent review of
the current literature, Smith et al. estimated that 10–15% of
medically operable patients were good candidates for
bladder preservation [93]. The recent International Consul-
tation on Urological Diseases–European Association of
Urology International Consultation on Bladder Cancer stated
that the best patients eligible for bladder preservation are
those with early-stage T2 disease and no hydronephrosis, no
extensive CIS, and no tumour invasion into the stroma of the
prostate [3]. Nevertheless, no strong LoE clearly identifies
ideal selection factors for TMT eligibility. Moreover, TMT
remains an alternative to RC in ‘‘not ideal’’ candidates if they
refuse surgery and plays a larger role in patients who are unfit
for surgery.
3.3. Role of neoadjuvant and adjuvant therapy in trimodal
therapy
3.3.1. Neoadjuvant therapy
The impact of neoadjuvant chemotherapy before RC in
MIBC is evident [71,74]. Meta-analysis of all randomised
prospective trials confirmed the 5% absolute improvement
in survival [93]. Although widely misquoted subgroup
analyses of the BA06 30894 trial suggest that neoadjuvant
chemotherapy had a greater impact on local recurrence-free
survival (RFS) before cystectomy (with a significant 26%
reduction in risk) than before RT (with a nonsignificant 9%
reduction in risk), a closer look revealed no evidence that
neoadjuvant cisplatin, methotrexate, and vinblastine (CMV)
chemotherapy had a greater or lesser effect in subgroups of
definitive treatments [72]. Hence, the benefit of neoadju-
vant chemotherapy appears mostly for distant disease,
which suggests that it may potentially have complementary
benefits for synchronous chemotherapy-RT, a conclusion
borne out by the BC2001 trial.
Efficacy of systemic neoadjuvant therapy in the context
of bladder preservation with TMT has been evaluated
(Table 3) [94,95]. The first large randomised trial (RTOG
89-03) comparing standard a TMT course with or without
two cycles of neoadjuvant CMV was prematurely closed
because of high rates of severe toxicities [57]. Only two-
thirds of included patients completed treatment as planned,
highlighting the poor tolerability. Moreover, no significant
difference in CR, metastasis-free survival, or OS was
reported between the two arms. Other teams have also
previously reported that the addition of neoadjuvant CMV
to cisplatin-based chemotherapy-RT was associated with a
greater incidence of mucositis, diarrhoea, and severe
leucopoenia [78,79,88,93]. Completion rates of neoadjuvant
chemotherapy plus TMT protocols ranged from 68% to 93%,
depending on the type of drug protocol [79,80,89,96].
In line with these series, when reviewing their institu-
tional experience, the Massachusetts General Hospital
(MGH) team did not find neoadjuvant chemotherapy to
be a predictor of better survival [13,66]. It is unclear why
neoadjuvant chemotherapy has been shown to improve
survival in patients treated with RC but not in patients
treated with TMT. Possible hypotheses include insufficient
chemotherapy having been given in some studies and
patients enrolling in clinical trials and treated with TMT
being more selected towards favourable pathology in which
neoadjuvant chemotherapy potentially has a lower survival
impact. Another possibility is that induction chemotherapy
before TMT may be associated with its own caveats, such as
selection of radioresistant clones, induction of accelerated
repopulation, and possibly reduced compliance with TMT
[97]. The lack of demonstrated benefit may be only
explained by inadequately powered studies using neoadju-
vant chemotherapy for adequate durations to answer this
question.
3.3.2. Adjuvant therapy
Series of adjuvant chemotherapy after TMT are listed in
Table 4. Completion of all adjuvant chemotherapy has
ranged from 45% to 70%, depending on the type of drug
protocol [17,35,98]. Grade 3–4 toxicity rates are higher
when adjuvant chemotherapy is used [17]. Moreover, the
completion rate for adjuvant chemotherapy was lower than
that reported for neoadjuvant treatment.
No survival outcomes from phase 3 trials evaluating
adjuvant chemotherapy following TMT have yet been
published. To date, no level 1 evidence exists to support
the use of either neoadjuvant or adjuvant chemotherapy
towards improving local control or survival in the setting of
TMT. However, in patients who can tolerate such therapy,
there may remain a clinical rationale for considering it, and
further studies are warranted.
3.4. Follow-up
Good responders with intact bladders have to be followed
closely by cystoscopy and CT or magnetic resonance
imaging (MRI) surveillance, with prompt salvage RC in
cases of invasive recurrence. Authors also suggest system-
atic tumour-site rebiopsy and bimanual examination under
general anaesthesia after completion of therapy, because on
rare occasions, patients may have a negative cystoscopy
but tumour growth underneath the TUR scar. Additional
biopsies are taken as seems appropriate. Although most
trials advocate and support rebiopsy following TMT, some
co-authors advocate a routine resection (rather than a cold-
cup biopsy) of the tumour scar at the first assessment
following TMT. Assuming that the biopsied tissue and
cytology do not show cancer (CR), the subsequent 2–3
cystoscopic evaluations over the next 9–12 mo may include
routine cold-cup biopsies. Nevertheless, no strong LoE
recommendation can be made concerning this follow-up
interval subsequent to the initial assessment. Voided urine
Table 4 – Published series of trimodal therapy plus adjuvant chemotherapy
Study Designand
follow-up
Stage No. ofpatients
Concomitantchemotherapy
RT(dose, fractionation)
Adjuvantchemotherapy
CR rate Salvagecystectomy
rate
CSS OS
Mitin et al., 2013 [34] Split
Phase 2
5 yr
T2–T4a N0/Nx 93 Arm 1: Cisplatin +
paclitaxel x3
Arm 2: Cisplatin +
5-FU x3
64.3 Gy
BID
Cisplatin +
gemcitabine +
paclitaxel
70%
85.5%**
5.4% – 5 yr: 73
Kaufman et al., 2009 [35] Split
Phase 1/2
49.4 mo
T2–T4a
N0
(biopsy or LN
dissection, if doubt)
80 Weekly cisplatin +
paclitaxel x5
64.3 Gy
BID
Cisplatin +
gemcitabine x4
81%* 12.5% 5 yr: 71 5 yr: 56
Hagan et al., 2003 [17] Split
Phase 1/2
26 mo
T2–T4a N0
(biopsy, if doubt)
47 Cisplatin weekly 64.8 Gy
BID
CMV x3 74%
(invasive: 19%)
25.5% – 3 yr: 61
Chen et al., 2003 [98] Continuous
Retrospective
36 mo
T3–T4 N0/N1 23 Cisplatin +
leucovorin +
5-FU x3
61.2 Gy
ST
Cisplatin +
leucovorin +
5-FU x3
86% – 3 yr: 69 3 yr: 65
Hussain et al., 2001 [50] Continuous
Phase 2
27.0 mo
T2–T4a N0/N1
Unresectable: 34%
56 Cisplatin +
5-FU x2
60 Gy
ST
Cisplatin +
5-FU x2
49% N/A – 5 yr: 45
Zietman et al., 1998 [87] Split
Phase 1/2
32 mo
T2–T4a N0/Nx 18 Cisplatin +
5-FU x4
55 Gy
BID
CMV x3 77.8% 14.3% – 3 yr: 83
5-FU = fluorouracil; BID = twice daily; CMV = cisplatin, methotrexate, vinblastine; CR = complete response; CSS = cancer-specific survival; LN = lymph node; N/A = not applicable; OS = overall survival; RT = radiation
therapy.* Defined by pT0, pTis, or pT1 after cystoscopic assessment.** Defined by pT0, pTis, or pTa after cystoscopic assessment. CR is evaluated after induction (split course) or completion (continuous course) of chemotherapy-RT.
EU
RO
PE
AN
UR
OL
OG
Y6
6(
20
14
)1
20
–1
37
13
0
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7 131
cytology is obtained before each evaluation. Ideally, the
same urologist should perform both the initial maximal TUR
of bladder tumour and the post-TMT evaluations. In
addition to the bladder, it is recommended that the
urologist perform risk-adapted surveillance for distant
metastasis and the upper tract.
Bladder-preservation studies that offer long-term follow-
up and address the risk of late metastatic or muscle-invasive
bladder failure suggested a decrease in cancer-specific events
and a flattening of the CSS curve beyond the first 5 yr after
TMT, similar to follow-up after cystectomy [13]. Other series
report that some patients may develop late recurrences
beyond the first 5 follow-up years [99–101]. Because of the
potential risk of delayed recurrences, it is recommended that
patients should be followed lifelong with cystoscopy.
3.5. Salvage therapy
Of the patients who experienced CR after induction TMT, the
rate of recurrent bladder tumours (both noninvasive and
muscle invasive) ranged from 24% to 43.1% [17,29,30,35,
56,68,89]. The median time to local recurrence was <2 yr in
general.
Of these recurrent tumours, the rate of muscle-invasive
recurrences ranged from 11% to 18.5% among patients
achieving CR [13,14,17,29,30,35,56,58,89]. RC is the
standard salvage treatment in medically operable patients
who have muscle-invasive recurrence. In their institutional
experience, Efstathiou et al. reported that cumulative 10-yr
rates of NMIBC and MIBC recurrences were 29% and 16%,
respectively [13]. James et al. reported 2-yr local RFS rates
of 67% [14]. Literature data (Table 1) suggest that the
average overall rate of salvage cystectomy, including
immediate cystectomy for nonresponders and delayed
cystectomy in cases of invasive recurrence, was approxi-
mately 25–30%, with many studies reporting data based on
<5-yr follow-up. Although difficult to determine, there
appears to be no significant diminution of survival related
to the delay in cystectomy in that setting. In the experience
from Erlangen, the CSS 5 yr after salvage RC for recurrent
muscle-invasive tumour approached 50% [29]. Better CSS
rates have been suggested in cases of delayed salvage
cystectomy for late recurrences compared with immediate
cystectomy for nonresponse [102]. Differences may be
explained by the fact that patients whose tumours did not
respond well to TMT are likely to have more aggressive
tumours than patients whose tumours respond well and
recur later.
In the past, cystectomy following radical RT has been
approached with concerns for increased morbidity. Although
the general experience among urologic surgeons is that
cystectomy following chemotherapy-RT is associated with a
higher risk of complications, contemporary series that use
conventionally fractionated regimens suggest potentially no
significant differences in perioperative mortality and major
complications rates after salvage RC compared with those
reported after primary cystectomy series [5,102,103].
Importantly, with regards to patient counselling, ortho-
topic neobladder reconstruction (although feasible) is not
advocated after pelvic radiation because of significantly
higher risk of functional complications. This risk is confirmed
within the published literature, as most patients who
underwent a cystectomy following TMT received an ileal
conduit diversion.
NMIBC recurrence can be managed conservatively with
TUR and subsequent intravesical therapies (bacillus Calm-
ette-Guerin [BCG], intravesical therapy) [99,100]. Never-
theless, these patients experiencing non–muscle-invasive
recurrence are at risk of requiring delayed cystectomy. Series
reported that 19–45% of recurrent non–muscle-invasive
tumours did not respond to conservative management and
needed to be treated by RC [19,30,58,66,80,100]. Although
non–muscle-invasive recurrence was associated with sig-
nificantly higher rates of salvage cystectomy, there was no
significant impact on CSS [30,100]. Finally, the effect of BCG
on QoL and bladder function in patients whose bladders were
treated with TMT previously requires evaluation.
3.6. Acute and late toxicity and effects on quality of life
3.6.1. Acute toxicity of trimodal therapy
Multimodal treatment for bladder preservation can be
offered to patients with an acceptable toxicity. The rates of
acute grade 3–4 toxicities and treatment completion rates
are listed in Table 5. Except in studies using neoadjuvant or
adjuvant chemotherapy, where toxicity seems higher, this
rate ranged from 10% to 36%, while the majority (80–90%) of
patients did complete the entire course of treatment. The
main toxicities are haematologic, GI, and genitourinary
(GU). Neuropathy may be reported in cases of cisplatin-
based concurrent chemotherapy. The BC2001 trial reported
neither an increase in grade 3–4 toxicity with concurrent
chemotherapy compared with RT alone nor a decrease in RT
completion rates caused by toxicity [14].
3.6.2. Late toxicity and quality of life
Bladder preservation must help to improve QoL if bladder
functions remain preserved after treatment, but systematic
assessment of toxicity beyond the 5-yr mark is presently
lacking. In the MGH experience and RTOG protocols, no
patient required cystectomy because of treatment-related
toxicity [13,66]. Overall, the rate of RC for late effects of RT
ranged from 0% to 2% [14,19]. Urodynamics studies on 32
patients reported reduced bladder compliance in about
one-quarter of patients but distressing symptoms in only
one-third of those patients [104]. Late grade 1–2 toxicity
rates ranged from 10% to 25% for GU and 5% to 6% for GI
toxicities [21,30,56]. The main low-grade toxicities were
urgency, nocturia, dysuria, diarrhoea, and proctitis. Hae-
morrhagic cystitis, ureteral or urethral strictures, proctitis,
and bladder compliance dysfunction may arise at varying
intervals after treatment. Late grade 3 urinary toxicity rates
ranged from 3% to 8% of cases [14,29,59]. Because many
toxicities were in physician-reported rather than patient-
reported assessments, it is unclear whether some were
underestimated.
Two prospective trials have confirmed good functional
results after TMT [51,105]. In the BC2001 trial, no differences
Table 5 – Reported rates of severe acute toxicity during trimodal therapy
Study Grade 3–4 toxicity Completion rate* Stop treatmentrelated to toxicity
Mitin et al., 2013 [34] 26.9% during induction
32% during consolidation
80.2% during adjuvant chemotherapy
58% 5.2% after TMT
29.8% after adjuvant chemotherapy
James et al., 2012 [14] 36%
GU: 21.3%
GI: 9.6%
80.2% –
Choudhury et al., 2011 [19] GI: 8% 92% 8%
Tunio et al., 2012 [20] 15%
Haematologic: 1%
GU: 6%
GI: 2%
Neuropathy: 2%
93.1% 7%
Lin et al., 2009 [88] Haematologic: 20%
GU: >10%
68% –
Kaufman et al., 2009 [35] 26% during induction
8% during consolidation
70% (including
adjuvant therapy)
–
Perdona et al., 2008 [82] Haematologic: 16.6%
GU: 11.5%
Diarrhoea: 14.1%
94.9% –
Weiss et al., 2007 [30] Haematologic: 14.4%
GU: 10%
Diarrhoea: 20.5%
87% 1.8%
Gogna et al., 2006 [56] 23%
Haematologic: 13.2%
GU: 3.5%
88.5% 0%
Kragelj et al., 2005 [57] 14% 64% –
Danesi et al., 2004 [80] Haematologic: 18.2%
GU: 16.9%
GI: 10.4%
93.5% 6.4%
Hussain et al., 2004 [39] Haematologic: 17%
Diarrhoea: 10%
Cystitis: 2%
85% –
Chen et al., 2003 [98] Haematologic: 4%
GI: 8%
GU: 4%
74% 0%
Rodel et al., 2002 [29] Haematologic: 22%
Diarrhoea: 5%
Cystitis: 5%
68% –
One death noted
Hussain et al., 2001 [50] 54.5%
Diarrhoea: 18.2%
Haematologic: 14.5%
Neuropathy: 7.2%
Other: 4–12%
57% 9%
Arias et al., 2000 [81] Haematologic: 20%
GU: 12%
GI: 16%
80% 0%
Kaufman et al., 2000 [15] Haematologic: 18%
GU: 9%
GI: 15%
87% 3%
Shipley et al., 1998 [58] Haematologic: 9.7%
Cystitis: 9.7%
GI disorders: 8.1%
Renal failure: 3.2%
Neuropathy: 3.2%
81% 6%
Kachnic et al., 1997 [89] – 80% 2% (one death)
Tester et al., 1996 [79] Haematologic: 15.4%
GU: 8%
GI: 3.3%
79% –
Tester et al., 1993 [63] Haematologic: 10.4%
GU: 8%
GI: 2%
– –
GI = gastrointestinal; GU = genitourinary; TMT = trimodal therapy.* Planned protocol or minor modifications because of toxicity. No grade 5 toxicity occurred.
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7132
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7 133
in late toxicity were reported with the addition of
chemotherapy to RT, where rates of grade 3–4 toxicity were
low (GI symptoms: 0.8%; GU symptoms: 7.4% in the
chemotherapy-RT arm) [14]. One small series retrospectively
compared QoL after RC with that after bladder preservation
[106]. QoL was suggested to be better after conservative
management, mainly because of better sexual activity. A
comparative cross-sectional study suggested that urinary
symptoms and sexual function may improve after RT [107],
but the retrospective design and interpretation biases
without accounting for surgical quality factors did not allow
drawing strong conclusions.
3.7. Limitations and perspectives
Although the use of conservative management for MIBC has
yielded promising results and gained wider acceptance,
most studies have limited follow-up, providing few data on
long-term oncologic safety or very late toxicity. Moreover,
several series included small cohorts. Thus, to date, most
bladder-preservation series have not reached the sample
size and follow-up of large published cystectomy series.
Although cancer control cannot be directly compared, the
similarity in survival after RC and TMT among properly
selected patients is likely in part because of a coherent
multidisciplinary effort among urologists, medical oncolo-
gists, radiation oncologists, pathologists, and motivated
patients, with prompt salvage therapy upon recurrence of
disease. TMT might induce an increased oncologic risk and
inferior survival if patients were not properly selected [108].
Large population-based studies consistently show that OS
was superior for patients who underwent RC compared with
those who underwent alternative treatments, including
chemotherapy and/or RT [109–111]. Although such compar-
ative retrospective studies are subject to significant selection
bias, with the reservation of chemotherapy and/or RT for
older patients who have significant comorbidities, they also
highlight the importance of proper patient selection and
coherent, coordinated multidisciplinary care.
Lymphadenectomy as well as the number of nodes
removed have been proven to be independent predictors of
survival after RC [112]. This therapeutic benefit may not be
fully addressed in the TMT approach, but no significant
difference in outcome has been shown between TMT series,
regardless of whether they include pelvic lymph nodes in
the targeted volume.
Many patients who have BCa have significant lower
urinary tract symptoms resulting from benign prostatic
obstruction, BCa, or repeated TURs with intravesical
therapies. In this subgroup of patients, the literature does
not adequately address whether these symptoms worsen or
improve after radiation. The use of TMT has not been
assessed in patients with nonurothelial histology.
As highlighted previously, some patients who are candi-
dates for bladder preservation may not be eligible for
concurrent cisplatin-based chemotherapy because of im-
paired renal function. Although regimens using MMC plus 5-
FU or low-dose gemcitabine have shown radiosensitising
activity, these regimens have never been compared head to
head with cisplatin. Finally, another concern that has been
discussed is that limited data exist on whether a neobladder is
feasible after TMT. Most surgeons would not offer orthotopic
diversion because of the increased complication and inconti-
nence rates [113].
As evident from the studies above, it is noteworthy to
highlight that the importance of proper patient selection
yields acceptable outcomes in any of the bladder-preserva-
tion approaches, but to date, available data support TMT as
the primary bladder-preservation strategy of choice for MIBC
because it addresses not only the index tumour itself but also
the rest of the susceptible bladder urothelium as well as
limited pelvic lymph nodes. Ideal candidates for bladder
preservation should have the following criteria: adequate
renal function to allow cisplatin-based chemotherapy
(although alternative regimens such as 5-FU or MMC or
low-dose gemcitabine have shown good activity); adequate
bladder capacity and function; motivated patient without
history of pelvic radiation who is willing to forgo an ileal
neobladder upon recurrence; organ-confined tumour (cT2)
and small tumour size in the absence of a palpable mass; the
ability to safely perform a resection of all visible tumour with
TUR; the absence of tumour-associated hydronephrosis or
adenopathy; the absence of extensive CIS; and the absence of
diffuse, multifocal disease.
Inclusion of molecular markers predicting response to
TMT may improve patient selection and management. If
predictive markers could be identified and validated in
prospective trials, patients might be selected for the
treatment most likely to benefit them. Prognostic values of
markers appear to differ between the settings of bladder
preservation and cystectomy [114]. Several studies have
investigated the predictive role of MRI and of various
biomarkers such as MRE11 [115–122]. Nevertheless, their
usefulness in clinical practice has to be proven.
4. Conclusions
A growing body of accumulated data suggests that TMT
(with prompt cystectomy reserved for tumour recurrence
or nonresponders) leads to acceptable outcomes and may
therefore be considered a reasonable treatment option in
well-selected patients. TMT can be discussed not only in
patients unfit for surgery but also for those patients who
have MIBC and are not willing to undergo surgery.
Author contributions: Wassim Kassouf had full access to all the data in
the study and takes responsibility for the integrity of the data and the
accuracy of the data analysis.
Study concept and design: Ploussard, Kassouf.
Acquisition of data: Ploussard, Daneshmand, Efstathiou, Herr, James,
Rodel, Shariat, Shipley, Sternberg, Thalmann, Kassouf.
Analysis and interpretation of data: Ploussard, Daneshmand, Efstathiou,
Herr, James, Rodel, Shariat, Shipley, Sternberg, Thalmann, Kassouf.
Drafting of the manuscript: Ploussard, Daneshmand, Efstathiou, Herr,
James, Rodel, Shariat, Shipley, Sternberg, Thalmann, Kassouf.
Critical revision of the manuscript for important intellectual content:
Daneshmand, Efstathiou, Herr, James, Rodel, Shariat, Shipley, Sternberg,
Thalmann, Kassouf.
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7134
Statistical analysis: Kassouf.
Obtaining funding: None.
Administrative, technical, or material support: None.
Supervision: Kassouf.
Other (specify): None.
Financial disclosures: Wassim Kassouf certifies that all conflicts of
interest, including specific financial interests and relationships and
affiliations relevant to the subject matter or materials discussed in the
manuscript (eg, employment/affiliation, grants or funding, consultan-
cies, honoraria, stock ownership or options, expert testimony, royalties,
or patents filed, received, or pending), are the following: Dr Ploussard is
partially funded by the Association Francaise d’Urologie and Association
pour la Recherche sur le Cancer. Dr Kassouf is a recipient of a Research
Scholar Award from the Fonds de recherche Sante Quebec.
Funding/Support and role of the sponsor: None.
References
[1] Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer
J Clin 2012;62:10–29.
[2] Stenzl A, Cowan NC, De Santis M, et al. Treatment of muscle-
invasive and metastatic bladder cancer: update of the EAU guide-
lines. Eur Urol 2011;59:1009–18.
[3] Gakis G, Efstathiou J, Lerner SP, et al. ICUD-EAU International
Consultation on Bladder Cancer 2012: radical cystectomy and
bladder preservation for muscle-invasive urothelial carcinoma
of the bladder. Eur Urol 2013;63:45–57.
[4] Shabsigh A, Korets R, Vora KC, et al. Defining early morbidity of
radical cystectomy for patients with bladder cancer using a stan-
dardized reporting methodology. Eur Urol 2009;55:164–76.
[5] Donat SM, Shabsigh A, Savage C, et al. Potential impact of
postoperative early complications on the timing of adjuvant
chemotherapy in patients undergoing radical cystectomy: a
high-volume tertiary cancer center experience. Eur Urol 2009;
55:177–86.
[6] Gray PJ, Fedewa SA, Shipley WU, et al. Use of potentially curative
therapies for muscle-invasive bladder cancer in the United States:
results from the National Cancer Database. Eur Urol 2013;63:
823–9.
[7] Munro NP, Sundaram SK, Weston PM, et al. A 10-year retrospective
review of a nonrandomized cohort of 458 patients undergoing
radical radiotherapy or cystectomy in Yorkshire, UK. Int J Radiat
Oncol Biol Phys 2010;77:119–24.
[8] Huddart RA, Hall E, Lewis R, Birtle A, SPARE Trial Management
Group. Life and death of spare (selective bladder preservation
against radical excision): reflections on why the spare trial closed.
BJU Int 2010;106:753–5.
[9] Kozak KR, Hamidi M, Manning M, Moody JS. Bladder preservation
for localized muscle-invasive bladder cancer: the survival impact
of local utilization rates of definitive radiotherapy. Int J Radiat
Oncol Biol Phys 2012;83:197–204.
[10] Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Pre-
ferred reporting items for systematic reviews and meta-analyses:
the PRISMA statement. J Clin Epidemiol 2009;62:1006–12.
[11] Shipley WU, Kaufman DS, Tester WJ, Pilepich MV, Sandler HM,
Radiation Therapy Oncology Group. Overview of bladder cancer
trials in the Radiation Therapy Oncology Group. Cancer 2003;97:
2115–9.
[12] Moonen L, vd Voet H, de Nijs R, Hart AA, Horenblas S, Bartelink H.
Muscle-invasive bladder cancer treated with external beam ra-
diotherapy: pretreatment prognostic factors and the predictive
value of cystoscopic re-evaluation during treatment. Radiother
Oncol 1998;49:149–55.
[13] Efstathiou JA, Spiegel DY, Shipley WU, et al. Long-term outcomes of
selective bladder preservation by combined-modality therapy for
invasive bladder cancer: the MGH experience. Eur Urol 2012;61:
705–11.
[14] James ND, Hussain SA, Hall E, et al. Radiotherapy with or without
chemotherapy in muscle-invasive bladder cancer. N Engl J Med
2012;366:1477–88.
[15] Kaufman DS, Winter KA, Shipley WU, et al. The initial results in
muscle-invading bladder cancer of RTOG 95-06: phase I/II trial of
transurethral surgery plus radiation therapy with concurrent
cisplatin and 5-fluorouracil followed by selective bladder preser-
vation or cystectomy depending on the initial response. Oncolo-
gist 2000;5:471–6.
[16] Housset M, Maulard C, Chretien Y, et al. Combined radiation and
chemotherapy for invasive transitional-cell carcinoma of the
bladder: a prospective study. J Clin Oncol 1993;11:2150–7.
[17] Hagan MP, Winter KA, Kaufman DS, et al. RTOG 97-06: initial
report of a phase I–II trial of selective bladder conservation using
TURBT, twice-daily accelerated irradiation sensitized with cisplat-
in, and adjuvant MCV combination chemotherapy. Int J Radiat
Oncol Biol Phys 2003;57:665–72.
[18] Horwich A, Dearnaley D, Huddart R, et al. A randomised trial of
accelerated radiotherapy for localised invasive bladder cancer.
Radiother Oncol 2005;75:34–43.
[19] Choudhury A, Swindell R, Logue JP, et al. Phase II study of conformal
hypofractionated radiotherapy with concurrent gemcitabine in
muscle-invasive bladder cancer. J Clin Oncol 2011;29:733–8.
[20] Tunio MA, Hashmi A, Qayyum A, Mohsin R, Zaeem A. Whole-pelvis
or bladder-only chemoradiation for lymph node-negative invasive
bladder cancer: single-institution experience. Int J Radiat Oncol
Biol Phys 2012;82:457–62.
[21] Efstathiou JA, Bae K, Shipley WU, et al. Late pelvic toxicity
after bladder-sparing therapy in patients with invasive bladder
cancer: RTOG 89-03, 95-06, 97-06, 99-06. J Clin Oncol 2009;27:
4055–61.
[22] Huddart RA, Hall E, Hussain SA, et al. Randomized noninferiority
trial of reduced high-dose volume versus standard volume radia-
tion therapy for muscle-invasive bladder cancer: results of the
BC2001 trial (CRUK/01/004). Int J Radiat Oncol Biol Phys 2013;87:
261–9.
[23] Foroudi F, Pham D, Bressel M, et al. Bladder cancer radiotherapy
margins: a comparison of daily alignment using skin, bone or soft
tissue. Clin Oncol 2012;24:673–81.
[24] Hata M, Miyanaga N, Tokuuye K, et al. Proton beam therapy for
invasive bladder cancer: a prospective study of bladder-preserv-
ing therapy with combined radiotherapy and intra-arterial che-
motherapy. Int J Radiat Oncol Biol Phys 2006;64:1371–9.
[25] Loehrer Sr PJ, Einhorn LH, Elson PJ, et al. A randomized comparison
of cisplatin alone or in combination with methotrexate, vinblas-
tine, and doxorubicin in patients with metastatic urothelial carci-
noma: a cooperative group study. J Clin Oncol 1992;10:1066–73.
[26] Dunst J, Sauer R, Schrott KM, Kuhn R, Wittekind C, Altendorf-
Hofmann A. Organ-sparing treatment of advanced bladder cancer:
a 10-year experience. Int J Radiat Oncol Biol Phys 1994;30:261–6.
[27] Shipley WU, Prout Jr GR, Einstein AB, et al. Treatment of invasive
bladder cancer by cisplatin and radiation in patients unsuited for
surgery. JAMA 1987;258:931–5.
[28] Coppin CM, Gospodarowicz MK, James K, et al. Improved local
control of invasive bladder cancer by concurrent cisplatin and
preoperative or definitive radiation. The National Cancer Institute
of Canada Clinical Trials Group. J Clin Oncol 1996;14:2901–7.
[29] Rodel C, Grabenbauer GG, Kuhn R, et al. Combined-modality
treatment and selective organ preservation in invasive bladder
cancer: long-term results. J Clin Oncol 2002;20:3061–71.
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7 135
[30] Weiss C, Engehausen DG, Krause FS, et al. Radiochemotherapy with
cisplatin and 5-fluorouracil after transurethral surgery in patients
with bladder cancer. Int J Radiat Oncol Biol Phys 2007;68:1072–80.
[31] Chung PW, Bristow RG, Milosevic MF, et al. Long-term outcome of
radiation-based conservation therapy for invasive bladder cancer.
Urol Oncol 2007;25:303–9.
[32] Danesi DT, Arcangeli G, Cruciani E, et al. Combined treatment of
invasive bladder carcinoma with transurethral resection, induc-
tion chemotherapy, and radical radiotherapy plus concomitant
protracted infusion of cisplatin and 5-fluorouracil: a phase I study.
Cancer 1997;80:1464–71.
[33] Nichols Jr RC, Sweetser MG, Mahmood SK, et al. Radiation therapy
and concomitant paclitaxel/carboplatin chemotherapy for muscle
invasive transitional cell carcinoma of the bladder: a well-tolerated
combination. Int J Cancer 2000;90:281–6.
[34] Mitin T, Hunt D, Shipley WU, et al. Transurethral surgery and
twice-daily radiation plus paclitaxel-cisplatin or fluorouracil-
cisplatin with selective bladder preservation and adjuvant chemo-
therapy for patients with muscle invasive bladder cancer (RTOG
0233): a randomised multicentre phase 2 trial. Lancet Oncol 2013;
14:863–72.
[35] Kaufman DS, Winter KA, Shipley WU, et al. Phase I–II RTOG study
(99–06) of patients with muscle-invasive bladder cancer under-
going transurethral surgery, paclitaxel, cisplatin, and twice-daily
radiotherapy followed by selective bladder preservation or radical
cystectomy and adjuvant chemotherapy. Urology 2009;73:833–7.
[36] Onozawa M, Miyanaga N, Hinotsu S, et al. Analysis of intravesical
recurrence after bladder-preserving therapy for muscle-invasive
bladder cancer. Jpn J Clin Oncol 2012;42:825–30.
[37] Eapen L, Stewart D, Collins J, Peterson R. Effective bladder sparing
therapy with intra-arterial cisplatin and radiotherapy for localized
bladder cancer. J Urol 2004;172:1276–80.
[38] Wittlinger M, Rodel CM, Weiss C, et al. Quadrimodal treatment of
high-risk T1 and T2 bladder cancer: transurethral tumor resection
followed by concurrent radiochemotherapy and regional deep
hyperthermia. Radiother Oncol 2009;93:358–63.
[39] Hussain SA, Stocken DD, Peake DR, et al. Long-term results of a
phase II study of synchronous chemoradiotherapy in advanced
muscle invasive bladder cancer. Br J Cancer 2004;90:2106–11.
[40] Epidermoid anal cancer: results from the UKCCCR randomised trial
of radiotherapy alone versus radiotherapy, 5-fluorouracil, and mi-
tomycin. UKCCCR Anal Cancer Trial Working Party. UK Co-ordinat-
ing Committee on Cancer Research. Lancet 1996;348:1049–54.
[41] Caffo O, Fellin G, Graffer U, et al. Phase I study of gemcitabine and
radiotherapy plus cisplatin after transurethral resection as con-
servative treatment for infiltrating bladder cancer. Int J Radiat
Oncol Biol Phys 2003;57:1310–6.
[42] Oh KS, Soto DE, Smith DC, Montie JE, Lee CT, Sandler HM. Com-
bined-modality therapy with gemcitabine and radiation therapy
as a bladder preservation strategy: long-term results of a phase I
trial. Int J Radiat Oncol Biol Phys 2009;74:511–7.
[43] Hoskin PJ, Rojas AM, Bentzen SM, Saunders MI. Radiotherapy with
concurrent carbogen and nicotinamide in bladder carcinoma.
J Clin Oncol 2010;28:4912–8.
[44] Pollack A, Zagars GK, Swanson DA. Muscle-invasive bladder cancer
treated with external beam radiotherapy: prognostic factors. Int J
Radiat Oncol Biol Phys 1994;30:267–77.
[45] Leibovici D, Kassouf W, Pisters LL, et al. Organ preservation for
muscle-invasive bladder cancer by transurethral resection. Urol-
ogy 2007;70:473–6.
[46] Herr HW. Transurethral resection of muscle-invasive bladder
cancer: 10-year outcome. J Clin Oncol 2001;19:89–93.
[47] Solsona E, Iborra I, Collado A, Rubio-Briones J, Casanova J,
Calatrava A. Feasibility of radical transurethral resection as
monotherapy for selected patients with muscle invasive bladder
cancer. J Urol 2010;184:475–80.
[48] Herr HW. Outcome of patients who refuse cystectomy after re-
ceiving neoadjuvant chemotherapy for muscle-invasive bladder
cancer. Eur Urol 2008;54:126–32.
[49] Solsona E, Climent MA, Iborra I, et al. Bladder preservation in
selected patients with muscle-invasive bladder cancer by complete
transurethral resection of the bladder plus systemic chemotherapy:
long-term follow-up of a phase 2 nonrandomized comparative trial
with radical cystectomy. Eur Urol 2009;55:911–21.
[50] Hussain MH, Glass TR, Forman J, et al. Combination cisplatin,
5-fluorouracil and radiation therapy for locally advanced unre-
sectable or medically unfit bladder cancer cases: a Southwest
Oncology Group Study. J Urol 2001;165:56–60.
[51] Lagrange JL, Bascoul-Mollevi C, Geoffrois L, et al. Quality of life
assessment after concurrent chemoradiation for invasive bladder
cancer: results of a multicenter prospective study (GETUG 97-015).
Int J Radiat Oncol Biol Phys 2011;79:172–8.
[52] Chauvet B, Brewer Y, Felix-Faure C, Davin JL, Choquenet C, Reboul
F. Concurrent cisplatin and radiotherapy for patients with muscle
invasive bladder cancer who are not candidates for radical cystec-
tomy. J Urol 1996;156:1258–62.
[53] Einstein Jr AB, Wolf M, Halliday KR, et al. Combination transurethral
resection, systemic chemotherapy, and pelvic radiotherapy for
invasive (T2-T4) bladder cancer unsuitable for cystectomy: a phase
I/II Southwestern Oncology Group study. Urology 1996;47:652–7.
[54] Koga F, Numao N, Saito K, et al. Sensitivity to chemoradiation
predicts development of metastasis in muscle-invasive bladder
cancer patients. Urol Oncol 2013;37:1270–5.
[55] Donat SM, Herr HW, Bajorin DF, et al. Methotrexate, vinblastine,
doxorubicin and cisplatin chemotherapy and cystectomy for unre-
sectable bladder cancer. J Urol 1996;156:368–71.
[56] Gogna NK, Matthews JH, Turner SL, et al. Efficacy and tolerability
of concurrent weekly low dose cisplatin during radiation treat-
ment of localised muscle invasive bladder transitional cell carci-
noma: a report of two sequential phase II studies from the Trans
Tasman Radiation Oncology Group. Radiother Oncol 2006;81:9–
17.
[57] Kragelj B, Zaletel-Kragelj L, Sedmak B, Cufer T, Cervek J. Phase II
study of radiochemotherapy with vinblastine in invasive bladder
cancer. Radiother Oncol 2005;75:44–7.
[58] Shipley WU, Winter KA, Kaufman DS, et al. Phase III trial of
neoadjuvant chemotherapy in patients with invasive bladder
cancer treated with selective bladder preservation by combined
radiation therapy and chemotherapy: initial results of Radiation
Therapy Oncology Group 89-03. J Clin Oncol 1998;16:3576–83.
[59] Zapatero A, Martin De Vidales C, Arellano R, et al. Long-term results
of two prospective bladder-sparing trimodality approaches for
invasive bladder cancer: neoadjuvant chemotherapy and concur-
rent radio-chemotherapy. Urology 2012;80:1056–62.
[60] Aboziada MA, Hamza HM, Abdlrahem AM. Initial results of bladder
preserving approach by chemo-radiotherapy in patients with
muscle invading transitional cell carcinoma. J Egypt Natl Canc
Inst 2009;21:167–74.
[61] Peyromaure M, Slama J, Beuzeboc P, Ponvert D, Debre B, Zerbib M.
Concurrent chemoradiotherapy for clinical stage T2 bladder can-
cer: report of a single institution. Urology 2004;63:73–7.
[62] Varveris H, Delakas D, Anezinis P, et al. Concurrent platinum and
docetaxel chemotherapy and external radical radiotherapy in
patients with invasive transitional cell bladder carcinoma. A pre-
liminary report of tolerance and local control. Anticancer Res
1997;17:4771–80.
[63] Tester W, Porter A, Asbell S, et al. Combined modality program
with possible organ preservation for invasive bladder carcinoma:
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7136
results of RTOG protocol 85-12. Int J Radiat Oncol Biol Phys
1993;25:783–90.
[64] Rotman M, Aziz H, Porrazzo M, et al. Treatment of advanced
transitional cell carcinoma of the bladder with irradiation and
concomitant 5-fluorouracil infusion. Int J Radiat Oncol Biol Phys
1990;18:1131–7.
[65] Russell KJ, Boileau MA, Higano C, et al. Combined 5-fluorouracil
and irradiation for transitional cell carcinoma of the urinary
bladder. Int J Radiat Oncol Biol Phys 1990;19:693–9.
[66] Shipley WU, Kaufman DS, Zehr E, et al. Selective bladder preser-
vation by combined modality protocol treatment: long-term out-
comes of 190 patients with invasive bladder cancer. Urology 2002;
60:62–7.
[67] Kotwal S, Choudhury A, Johnston C, Paul AB, Whelan P, Kiltie AE.
Similar treatment outcomes for radical cystectomy and radical
radiotherapy in invasive bladder cancer treated at a United King-
dom specialist treatment center. Int J Radiat Oncol Biol Phys 2008;
70:456–63.
[68] Madersbacher S, Hochreiter W, Burkhard F, et al. Radical cystec-
tomy for bladder cancer today—a homogeneous series without
neoadjuvant therapy. J Clin Oncol 2003;21:690–6.
[69] Hautmann RE, de Petriconi RC, Pfeiffer C, Volkmer BG. Radical
cystectomy for urothelial carcinoma of the bladder without
neoadjuvant or adjuvant therapy: long-term results in 1100
patients. Eur Urol 2012;61:1039–47.
[70] Culp SH, Dickstein RJ, Grossman HB, et al. Refining patient selec-
tion for neoadjuvant chemotherapy before radical cystectomy.
J Urol 2014;191:40–7.
[71] Bekelman JE, Handorf EA, Guzzo T, et al. Radical cystectomy versus
bladder-preserving therapy for muscle-invasive urothelial carcino-
ma: examining confounding and misclassification bias in cancer
observational comparative effectiveness research. Value Health
2013;16:610–8.
[72] Griffiths G, Hall R, Sylvester R, Raghavan D, Parmar MK. Interna-
tional phase III trial assessing neoadjuvant cisplatin, methotrex-
ate, and vinblastine chemotherapy for muscle-invasive bladder
cancer: long-term results of the BA06 30894 trial. J Clin Oncol
2011;29:2171–7.
[73] Svatek RS, Shariat SF, Novara G, et al. Discrepancy between clinical
and pathological stage: external validation of the impact on
prognosis in an international radical cystectomy cohort. BJU Int
2011;107:898–904.
[74] Yafi FA, Aprikian AG, Chin JL, et al. Contemporary outcomes of
2287 patients with bladder cancer who were treated with radical
cystectomy: a Canadian multicentre experience. BJU Int 2011;108:
539–45.
[75] Grossman HB, Natale RB, Tangen CM, et al. Neoadjuvant chemo-
therapy plus cystectomy compared with cystectomy alone for
locally advanced bladder cancer. N Engl J Med 2003;349:859–66.
[76] Shipley WU, Rose MA, Perrone TL, Mannix CM, Heney NM, Prout Jr
GR. Full-dose irradiation for patients with invasive bladder carci-
noma: clinical and histological factors prognostic of improved
survival. J Urol 1985;134:679–83.
[77] Coen JJ, Paly JJ, Niemierko A, et al. Nomograms predicting response
to therapy and outcomes after bladder-preserving trimodality
therapy for muscle-invasive bladder cancer. Int J Radiat Oncol
Biol Phys 2013;86:311–6.
[78] Fung CY, Shipley WU, Young RH, et al. Prognostic factors in invasive
bladder carcinoma in a prospective trial of preoperative adjuvant
chemotherapy and radiotherapy. J Clin Oncol 1991;9:1533–42.
[79] Tester W, Caplan R, Heaney J, et al. Neoadjuvant combined mo-
dality program with selective organ preservation for invasive
bladder cancer: results of Radiation Therapy Oncology Group
phase II trial 8802. J Clin Oncol 1996;14:119–26.
[80] Danesi DT, Arcangeli G, Cruciani E, et al. Conservative treatment of
invasive bladder carcinoma by transurethral resection, protracted
intravenous infusion chemotherapy, and hyperfractionated radio-
therapy: long term results. Cancer 2004;101:2540–8.
[81] Arias F, Domınguez MA, Martınez E, et al. Chemoradiotherapy for
muscle invading bladder carcinoma. Final report of a single insti-
tutional organ-sparing program. Int J Radiat Oncol Biol Phys 2000;
47:373–8.
[82] Perdona S, Autorino R, Damiano R, et al. Bladder-sparing, combined-
modality approach for muscle-invasive bladder cancer: a multi-
institutional, long-term experience. Cancer 2008;112:75–83.
[83] Sabaa MA, El-Gamal OM, Abo-Elenen M, Khanam A. Combined
modality treatment with bladder preservation for muscle invasive
bladder cancer. Urol Oncol 2010;28:14–20.
[84] Krause FS, Walter B, Ott OJ, et al. 15-year survival rates after
transurethral resection and radiochemotherapy or radiation in
bladder cancer treatment. Anticancer Res 2011;31:985–90.
[85] May M, Bastian PJ, Brookman-May S, et al. Gender-specific differ-
ences in cancer-specific survival after radical cystectomy for
patients with urothelial carcinoma of the urinary bladder in
pathologic tumor stage T4a. Urol Oncol 2013;31:1141–7.
[86] Keck B, Ott OJ, Haberle L, et al. Female sex is an independent risk
factor for reduced overall survival in bladder cancer patients
treated by transurethral resection and radio- or radiochemother-
apy. World J Urol 2013;31:1023–8.
[87] Zietman AL, Shipley WU, Kaufman DS, et al. A phase I/II trial
of transurethral surgery combined with concurrent cisplatin,
5-fluorouracil and twice daily radiation followed by selective
bladder preservation in operable patients with muscle invading
bladder cancer. J Urol 1998;160:1673–7.
[88] Lin CC, Hsu CH, Cheng JC, et al. Induction cisplatin and fluorouracil-
based chemotherapy followed by concurrent chemoradiation for
muscle-invasive bladder cancer. Int J Radiat Oncol Biol Phys 2009;
75:442–8.
[89] Kachnic LA, Kaufman DS, Heney NM, et al. Bladder preservation by
combined modality therapy for invasive bladder cancer. J Clin
Oncol 1997;15:1022–9.
[90] Tilki D, Shariat SF, Lotan Y, et al. Lymphovascular invasion is
independently associated with bladder cancer recurrence and
survival in patients with final stage T1 disease and negative lymph
nodes after radical cystectomy. BJU Int 2013;111:1215–21.
[91] Watts KL, Ristau BT, Yamase HT, Taylor 3rd JA. Prognostic
implications of lymph node involvement in bladder cancer:
are we understaging using current methods? BJU Int 2011;108:
484–92.
[92] Gospodarowicz MK, Hawkins NV, Rawlings GA, et al. Radical
radiotherapy for muscle invasive transitional cell carcinoma of
the bladder: failure analysis. J Urol 1989;142:1448–53.
[93] Smith ZL, Christodouleas JP, Keefe SM, Malkowicz SB, Guzzo TJ.
Bladder preservation in the treatment of muscle-invasive bladder
cancer (MIBC): a review of the literature and a practical approach
to therapy. BJU Int 2013;112:13–25.
[94] Fellin G, Graffer U, Bolner A, Ambrosini G, Caffo O, Luciani L.
Combined chemotherapy and radiation with selective organ
preservation for muscle-invasive bladder carcinoma. A single-
institution phase II study. Br J Urol 1997;80:44–9.
[95] Cobo M, Delgado R, Gil S, et al. Conservative treatment with
transurethral resection, neoadjuvant chemotherapy followed by
radiochemotherapy in stage T2–3 transitional bladder cancer. Clin
Transl Oncol 2006;8:903–11.
[96] Advanced Bladder Cancer (ABC) Meta-analysis Collaboration.
Neoadjuvant chemotherapy in invasive bladder cancer: update
of a systematic review and meta-analysis of individual patient
data. Eur Urol 2005;48:202–6.
E U R O P E A N U R O L O G Y 6 6 ( 2 0 1 4 ) 1 2 0 – 1 3 7 137
[97] Glynne-Jones R, Hoskin P. Neoadjuvant cisplatin chemotherapy
before chemoradiation: a flawed paradigm? J Clin Oncol 2007;
25:5281–6.
[98] Chen WC, Liaw CC, Chuang CK, et al. Concurrent cisplatin, 5-
fluorouracil, leucovorin, and radiotherapy for invasive bladder
cancer. Int J Radiat Oncol Biol Phys 2003;56:726–33.
[99] Weiss C, Wittlinger M, Engehausen DG, et al. Management of
superficial recurrences in an irradiated bladder after combined-
modality organ-preserving therapy. Int J Radiat Oncol Biol Phys
2008;70:1502–6.
[100] Zietman AL, Grocela J, Zehr E, et al. Selective bladder conservation
using transurethral resection, chemotherapy, and radiation: man-
agement and consequences of Ta, T1, and Tis recurrence within
the retained bladder. Urology 2001;58:380–5.
[101] Herr HW. Tumour progression and survival in patients with T1G3
bladder tumours: 15-year outcome. Br J Urol 1997;80:762–5.
[102] Eswara JR, Efstathiou JA, Heney NM, et al. Complications and long-
term results of salvage cystectomy after failed bladder sparing
therapy for muscle invasive bladder cancer. J Urol 2012;187:
463–8.
[103] Iwai A, Koga F, Fujii Y, et al. Perioperative complications of radical
cystectomy after induction chemoradiotherapy in bladder-
sparing protocol against muscle-invasive bladder cancer: a single
institutional retrospective comparative study with primary radi-
cal cystectomy. Jpn J Clin Oncol 2011;41:1373–9.
[104] Zietman AL, Sacco D, Skowronski U, et al. Organ conservation in
invasive bladder cancer by transurethral resection, chemotherapy
and radiation: results of a urodynamic and quality of life study on
long-term survivors. J Urol 2003;170:1772–6.
[105] Herman JM, Smith DC, Montie J, et al. Prospective quality-of-life
assessment in patients receiving concurrent gemcitabine and radio-
therapy as a bladder preservation strategy. Urology 2004;64:69–73.
[106] Caffo O, Fellin G, Graffer U, Luciani L. Assessment of quality of life
after cystectomy or conservative therapy for patients with infil-
trating bladder carcinoma. A survey by a self-administered ques-
tionnaire. Cancer 1996;78:1089–97.
[107] Henningsohn L, Wijkstrom H, Dickman PW, Bergmark K, Steineck
G. Distressful symptoms after radical radiotherapy for urinary
bladder cancer. Radiother Oncol 2002;62:215–25.
[108] Tran E, Souhami L, Tanguay S, Rajan R. Bladder conservation treat-
ment in the elderly population: results and prognostic factors of
muscle-invasive bladder cancer. Am J Clin Oncol 2009;32:333–7.
[109] Chamie K, Hu B, Devere White RW, Ellison LM. Cystectomy in the
elderly: does the survival benefit in younger patients translate to
the octogenarians? BJU Int 2008;102:284–90.
[110] Gore JL, Litwin MS, Lai J, et al. Use of radical cystectomy for
patients with invasive bladder cancer. J Natl Cancer Inst 2010;
102:802–11.
[111] Hollenbeck BK, Miller DC, Taub D, et al. Aggressive treatment for
bladder cancer is associated with improved overall survival
among patients 80 years old or older. Urology 2004;64:292–7.
[112] Svatek R, Zehnder P. Role and extent of lymphadenectomy during
radical cystectomy for invasive bladder cancer. Curr Urol Rep 2012;
13:115–21.
[113] Eisenberg MS, Dorin RP, Bartsch G, Cai J, Miranda G, Skinner EC.
Early complications of cystectomy after high dose pelvic radiation.
J Urol 2010;184:2264–9.
[114] Choudhury A, Nelson LD, Teo MT, et al. MRE11 expression is
predictive of cause-specific survival following radical radiotherapy
for muscle-invasive bladder cancer. Cancer Res 2010;70:7017–26.
[115] Chakravarti A, Winter K, Wu CL, et al. Expression of the epidermal
growth factor receptor and Her-2 are predictors of favorable out-
come and reduced complete response rates, respectively, in patients
with muscle-invading bladder cancers treated by concurrent
radiation and cisplatin-based chemotherapy: a report from the
Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys
2005;62:309–17.
[116] Lautenschlaeger T, George A, Klimowicz AC, et al. Bladder preserva-
tion therapy for muscle-invading bladder cancers on Radiation
Therapy Oncology Group trials 8802, 8903, 9506, and 9706: vascular
endothelial growth factor B overexpression predicts for increased
distant metastasis and shorter survival. Oncologist 2013;18:685–6.
[117] Laurberg JR, Brems-Eskildsen AS, Nordentoft I, et al. Expression of
TIP60 (tat-interactive protein) and MRE11 (meiotic recombina-
tion 11 homolog) predict treatment-specific outcome of localised
invasive bladder cancer. BJU Int 2012;110:1228–36.
[118] Agerbaek M, Alsner J, Marcussen N, Lundbeck F, von der Maase H.
Retinoblastoma protein expression is an independent predictor of
both radiation response and survival in muscle-invasive bladder
cancer. Br J Cancer 2003;89:298–304.
[119] Garcia del Muro X, Condom E, Vigues F, et al. p53 and p21
expression levels predict organ preservation and survival in
invasive bladder carcinoma treated with a combined-modality
approach. Cancer 2004;100:1859–67.
[120] Moonen L, Ong F, Gallee M, et al. Apoptosis, proliferation and p53,
cyclin D1, and retinoblastoma gene expression in relation to
radiation response in transitional cell carcinoma of the bladder.
Int J Radiat Oncol Biol Phys 2001;49:1305–10.
[121] Koga F, Yoshida S, Tatokoro M, et al. ErbB2 and NFkB overexpres-
sion as predictors of chemoradiation resistance and putative
targets to overcome resistance in muscle-invasive bladder cancer.
PLoS One 2011;6:27616.
[122] Yoshida S, Koga F, Kobayashi S, et al. Role of diffusion-weighted
magnetic resonance imaging in predicting sensitivity to chemor-
adiotherapy in muscle-invasive bladder cancer. Int J Radiat Oncol
Biol Phys 2012;83:21–7.