Caseload midwifery Evaluation 2011-2014
Transcript of Caseload midwifery Evaluation 2011-2014
Evaluation of the
Caseload
Midwifery
Model of Care July 2011 – June 2014
Blue Mountains District Anzac Memorial Hospital
Final Report
Mel Lewis
2
Table of Contents Index of Figures .............................................................................................................. 4
Index of tables ................................................................................................................ 5
Acknowledgements ........................................................................................................ 6
EXECUTIVE SUMMARY .................................................................................................... 7
RECOMMENDATIONS ..................................................................................................... 13
INTRODUCTION .............................................................................................................. 18 Background to the report .......................................................................................................................................... 18 Aims .................................................................................................................................................................................... 19
LOCAL HISTORY AND CONTEXT ...................................................................................... 21
DEFINING THE TERMS .................................................................................................... 24
POLICY AND EVIDENCE SUPPORTING THE MODEL .......................................................... 28 Establishment ................................................................................................................................................................ 29 Annualized salary agreement .................................................................................................................................. 29 The model ........................................................................................................................................................................ 31 Physical workspaces ................................................................................................................................................... 36 Women’s care journey ................................................................................................................................................ 37 Measures of birth continuity ................................................................................................................................... 42
WORK FLOW THROUGH THE MATERNITY UNIT .............................................................. 45 Booking into Blue Mountains hospital ................................................................................................................ 45 Who provides antenatal care? ................................................................................................................................ 45 Where do caseload women give Birth? ............................................................................................................... 46 All births at BMDAMH ................................................................................................................................................ 47
MATERNAL CHARACTERISTICS ........................................................................................ 48 Antenatal .......................................................................................................................................................................... 51 Admissions ........................................................................................................................................................................ 51 Plurality ............................................................................................................................................................................. 51
Labour ............................................................................................................................................................................... 51 Onset of labour ............................................................................................................................................................... 51 Induction ........................................................................................................................................................................... 52 Augmentation ................................................................................................................................................................. 53 Analgesia .......................................................................................................................................................................... 54
Birth .................................................................................................................................................................................... 54 Method of birth .............................................................................................................................................................. 54 Indications for caesareans-‐no labour (elective) .............................................................................................. 56 Perineal status after vaginal birth ........................................................................................................................ 57 Post-‐partum haemorrhage (PPH) ......................................................................................................................... 58
Babies ................................................................................................................................................................................ 58 Gestation ........................................................................................................................................................................... 58 Birth weight ..................................................................................................................................................................... 59 Live births ......................................................................................................................................................................... 59 Apgar score ...................................................................................................................................................................... 60 Admission to nursery ................................................................................................................................................... 61
Postnatal ........................................................................................................................................................................... 61 Breastfeeding .................................................................................................................................................................. 61 Length of stay after birth ........................................................................................................................................... 61 Home visits ....................................................................................................................................................................... 61
Attitudes to Professional Role (ATPR) ................................................................................................................ 62
3
Industrial Agreement Questionnaire (IQ) .......................................................................................................... 65 Work hours ...................................................................................................................................................................... 66 On call ................................................................................................................................................................................ 66 Yearly caseload .............................................................................................................................................................. 66 Caseload manageability ............................................................................................................................................. 67 Continuity of care .......................................................................................................................................................... 68 Professional supervision & Support ...................................................................................................................... 68 Midwives suggestions for change ........................................................................................................................... 69 Discussion ......................................................................................................................................................................... 71
WHAT THE WOMEN SAY – SURVEY RESPONSES ............................................................. 72 Methods ............................................................................................................................................................................ 72 Findings ............................................................................................................................................................................ 74 The women ....................................................................................................................................................................... 74 Model of care ................................................................................................................................................................... 75 Did women choose their model of care? .............................................................................................................. 75 Reasons for choice or allocation to a model of care. ..................................................................................... 76 Satisfaction with information -‐ Enabling informed choices ....................................................................... 77 Satisfaction with the information -‐ About the scope of services available at BMDAMH ............... 77 Were women’s wishes and needs respected and met by the service? ..................................................... 77 Did women attend parenting classes? ................................................................................................................. 77 Did women value antenatal information given by midwives or doctors? ............................................ 78 Caseload care – did women feel supported by their midwife? .................................................................. 79
The postnatal period ................................................................................................................................................... 82 Did women receive adequate information about the postnatal period? .............................................. 82 Did women feel confident about going home with a new baby? .............................................................. 82 What method of infant feeding did women choose? ...................................................................................... 82 Did women feel supported with, and informed about their choice of infant feeding? .................... 82 How long did women breastfeed for? ................................................................................................................... 83 Did women receive adequate information about community supports? ............................................. 83
Women have their say – Themes of importance ............................................................................................. 83
Appendix 2: Blue Mountains Hospital Obstetric Criteria ................................................. 93
Appendix 4: Industrial Agreement Questionnaire – Caseload Midwifery Model ............. 95
REFERENCES ................................................................................................................... 98
4
Index of Figures
Figure 1: Births per financial year trend, Koorana unit 22
Figure 2: Continuity of care models as reported in the literature 27
Figure 3: Proportion of birth attendance for primary midwife, Koorana unit 43
Figure 4: Proportion of births each primary midwife attended 44
Figure 5: Proportion of women per model of antenatal care, January 2011-June 2014 46
Figure 6: All Koorana unit births Jul 2011-Jun 2014 48
Figure 7: Age of Koorana mothers compared to NSW birth cohort 49
Figure 8: Proportion of ATSI women who birthed at Koorana unit 2011-2014 49
Figure 9: Parity group for mothers who gave birth in the caseload triennium 50
5
Index of tables
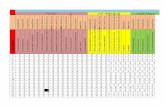
Table 1: Koorana caseload midwife staffing profile July 2011-June 2014 30
Table 2: Relational continuity between women and midwives at Koorana 41
Table 3: Booking-in visits at Koorana, according to intended maternity care provider 45
Table 4: No & proportion of women who received antenatal care, according to model 46
Table 5: Reasons why caseload women did not birth at Koorana, Jul 2011-Jun 2014 46
Table 6: Onset of labour type for all births, per caseload year 52
Table 7: Onset of labour profile for baseline and caseload triennium 52
Table 8: Method of labour induction 52
Table 9: List of indications for induction of labour 53
Table 10: Mode of birth for all mothers 54
Table 11: Comparison of mode of birth between mothers in baseline and caseload trienniums 55
Table 12: Indication for caesarean section –no labour 56
Table 13: Perineal status of vaginal births by instrumental and non-instrumental birth 57
Table 14: Blood loss at birth 58
Table 15: Blood loss at birth, vaginal v’s caesarean births 58
Table 16: Gestational age groupings 59
Table 17: Birth weight categories of infants 59
Table 18: Live birth and perinatal death rate 60
Table 19: Respondents according to parity, per birth year 74
Table 20: Respondents according to model of care, per birth year 75
Table 21: Caseload women, responses to feeling well supported per stage of maternity care 79
Table 22: Proportion of women who felt supported in labour & birth, according to primary midwife attending intra-partum care 79
Table 23: Numbers of positive and negative comments according to stage of maternity care 80
6
Acknowledgements I would like to thank all the caseload midwives at BMDAMH for their guidance in
completing this report; Robyn Carroll, Sally Whitson, Fiona Schonstein-Scott,
Barbara Rose, Jane Rutherford and Anne Couttes. To Peta Millard and Julie
Lahache (core staff) for assistance in folding and mailing out surveys to women. To
Ann Yates (District Nurse Manager of Midwifery Services) for review and addition of
some recommendations. To Juanita Taylor, (CMC Nepean) for assistance with file
audits and obstetriX reports. Therese Ross (NUM, BMDAMH) for your patience and
support, and supply of the design for the title page. To all the women who have
kindly taken the time to complete the surveys and leave valuable feedback, and all
those either directly or indirectly involved in the Caseload midwifery model at
BMDAMH.
*Corresponding author at: c/o Koorana Unit, BMDAMH, Woodlands Drive, Katoomba. E-mail address: [email protected] (Mel Lewis)
7
EXECUTIVE SUMMARY
Overveiw
The Blue Mountains District Anzac Memorial Hospital (BMDAMH) Caseload
midwifery model of care was established by the Nepean, Blue Mountains Local
Health District (NBMLHD), in July 2011. The caseload model was set up in
response to the Towards normal birth - NSW Health policy directive (2010)[1], and
sought to address long-standing issues with recruitment and retention of midwifery
staff, as well as community concerns about the continuation of maternity service
provision at the BMDAMH[2]. The aim of the caseload midwifery model was to
improve the quality of maternity care for women and babies at the Blue Mountains
Hospital, and to also improve the productivity and work experience of midwives
working in the service. The caseload midwifery model became fully staffed in June
2013, and data for this evaluation was collected from July 2011 to July 2014 (three
complete years of caseload operation).
Methods Quantitative data
Retrospective maternal and infant health outcome data for all BMDAMH (Koorana
Unit) births are reported on for the three years of caseload operation (July 2011-
June 2014 – Caseload triennium). The proportion of caseload clients in the
caseload triennium increased to over 95% by the end of the reporting period (table
4). However not ALL births reported on were caseload clients. This is because
caseload midwives are generally called on to provide intra-partum care for all
women birthing at the Koorana unit, irrespective of the model they are booked
under, and have undoubtedly influenced the standard of midwifery care across the
whole unit. For this reason, ALL BMDAMH birth data was used to report maternal
and infant health outcomes, to evaluate the effect that the caseload model has had
on the unit as a whole.
A further three years of retrospective birth data for BMDAMH (July 2008 – June
2011 – Baseline triennium), was used when available, to compare maternal and
infant health outcomes before and after the onset of the caseload model. When
8
baseline data was not available, comparisons were made in some cases with
published NSW perinatal data[3], to help contextualize quantitative findings.
Quantitative perinatal data was obtained through ObstetriX and reported in excel
format. The data was then cleaned and analyzed using IBM-SPSS© Statistical
software for Mac (version 22), with alpha significance levels set at 0.05 (95%
confidence) for all Chi2 tests performed on categorical perinatal variables.
Attitudes to the professional role of caseload and core midwives are measured with
a quantitative survey instrument (appendix 3).
Qualitative data
Data is collected from the patient quality satisfaction survey, and the industrial
questionnaire to caseload midwives. Responses were de-identified, coded and
analyzed for content and themes.
Findings The establishment of the midwifery caseload model of care represented a
significant change in service provision for women booking into the BMDAMH. The
service has only been fully staffed for the last year of the evaluation (June 2013-
June 2014), but has demonstrated considerable success towards the aims of
improving service provision and standard of care since commencement. The
caseload midwifery model delivers woman-centered, continuity of care for most
women who book into the Koorana Unit, and has improved the quality and safety of
maternity care provided at the BMDAMH. The findings from the quality survey
suggests that having a known midwife in pregnancy, birth and the postnatal period,
has enhanced the experience for women and families as users of the service.
Maternal and infant health outcomes
The following statistically significant improvements (p<0.05) were found when
comparing maternal and infant health outcome data from the caseload triennium, to
the baseline triennium:
• Increase of 9.5% in the proportion of women who labored spontaneously (from 59.3% to 68.8%).
• A 4% reduction in labour augmentation rate (from 10.9% to 6.9%)
9
• A 2% reduction in the epidural rate (from 18.1% to 16.1%)
• A 5.3% reduction in the total caesarean section rate (from 28.9% to 23.6%) • A 6.6% reduction in the elective caesarean rate (from 19.7% to 13.1%).
• A 23.9% increase in the proportion of babies born after 40 weeks gestation,
from 20.9% to 44.8%
• A 50% reduction in the proportion of babies born with low Apgar scores, five minute <7), from 2.2% to 1.1%
The following changes were also observed when comparing the caseload cohort
to the baseline cohort, but were not statistically significant (p>.05).
• A higher proportion of primiparous women birthed with caseload (38%)
compared to before (35.2%)
• A 2.9% reduction in the induction of labour rate from 21% to 18.1%
• A 5.1% increase in the normal vaginal birth rate from 63.4% to 68.5%.
• A 2.2% decrease in the episiotomy rate from 5.9% to 3.7%.
• A 0.7% decrease in the post-partum haemorrhage rate (>500mls) from 19.3% to 18.6% for all births (see page 58 for breakdown and discussion)
• A 1.7% increase in the proportion of babies born with a birth weight over 4000 grams from 15.3%-13.6%
• A reduction in the proportion of neonatal transfers to higher levels of care.
• A 0.9% increase in the proportion of third and forth degree tears, from 2% to
2.9%.
• A 0.4% decrease in the live birth rate, from 99.8% to 99.4%, although all 4 cases were associated with fetal anomalies in the caseload cohort, and neonatal deaths not related to labour (see page 59-60 for details).
What the midwives say
The attitudes to professional role (ATPR) questionnaire, highlighted:
• Caseload midwives experience higher levels of professional satisfaction than core midwife do in their respective roles, and feel that they have more opportunities to make decisions about care.
10
• Core midwives perceived a higher degree of professional independence than
caseload midwives within their scope and expectations of practice.
• Caseload and core midwives both affirmed strong support from their midwifery colleagues
• Core midwives perceived a higher level of support from obstetric colleagues than caseload midwives, but both groups felt that obstetricians were supportive in general.
• Both groups perceived a relative lack of managerial support.
• Core midwives felt that they have enough time to do their jobs properly,
whereas caseload midwives felt there is often not enough time.
• Both groups did not agree that their work is stressful.
• Both caseload and core midwives felt that they have enough opportunities to provide personalized care to women.
• Core midwives felt that they had more time to give to women than caseload
midwives.
• On the whole, both groups were satisfied in the domain of client interaction, with caseload midwives feeling more satisfied with the level of continuity they offer women.
• Caseload midwives felt that they had more opportunities for professional
development than core midwives, as well as the opportunities to develop midwifery skills in the course of their work.
• Both groups felt that they had sufficient midwifery skills for their work, with
caseload midwives feeling particularly confident in this area. The industrial questionnaire (IQ) of caseload midwives indicates:
• Caseload midwives were satisfied with the arrangements for covering each other’s caseload whilst on a day off and flexibility for having days off.
• Midwives who regularly come in to work on their days off to care for their own women had a higher level of satisfaction with the continuity they could offer. Midwives who do not regularly come in in their own time, were not satisfied with the continuity of care component of their work.
• Midwives receive good professional support from each other
• Midwives are satisfied with the degree of professional development they can
engage in.
• Midwives on the whole perceive a lack of management support.
11
• The biggest frustration for caseload midwives in the past, has been filling
shifts on the core roster, and short staffing. This has impacted on their capacity to provide continuity of care to women on many occasions over the past three years. Improved staffing levels in 2014 have mostly rectified this problem.
• Caseload midwives on the whole, would like to change the model’s working
configuration to two smaller groups, providing on-call care to a smaller group of women in the future.
What the women say – Survey responses
• 95% of caseload clients felt that their wishes and needs were respected by the service.
• 92% of women felt well supported in the antenatal period, 93% in labour and
birth, and 96% felt supported in the postnatal period at home.
• Having their primary midwife provide care in labour and birth increased women’s satisfaction levels to 95.7% (from 89.6% when the primary midwife could not be present for labour or birth).
• Women valued having their own midwife, and feedback was overwhelmingly
positive.
• The small number of criticisms centered on; problematic communication (via text messages or when women did not get a response from a midwife), perceiving that their choices were not respected in some way, and a lack of warmth and connection with the primary midwife.
• The most common criticisms of the postnatal period was conflicting
breastfeeding advice whilst in hospital, and feeling pressured to go home too early.
• Besides the major theme of appreciation for the hospital and caseload
service, the following sub-themes emerged:
! Continuity and connection with the primary midwife is important to women.
! ‘Please offer vaginal (normal) birth after caesarean section (VBAC’s
or NBAC’s)’
! Women want the opportunity to birth in water at the Koorana unit.
! Women do not want to be rushed into early discharge from hospital.
! General concerns about the staffing and working conditions of midwives.
12
Conclusion
The first evaluation of the safety and effectiveness of the caseload model finds that
the model has been able to meet the aims of improving maternity care provision for
mothers and babies at the Koorana unit at the BMDAMH, evidenced by significant
decreases in the caesarean section rate, augmentation rate, use of epidural
analgesia, and babies born with low Apgar-scores over the three year period of
operation. The evaluation supports the available evidence that being cared for by a
known midwife throughout pregnancy, birth and the postnatal period enhances the
women’s experience of birth. The new model has succeeded in improving the
retention, productivity and satisfaction of midwives in the Koorana unit, and
contributed to a relative lack of maternity service interruptions at BMDAMH since
2011. The following recommendations are provided to support the continued
provision of the caseload model to women in the Blue Mountains region.
RECOMMENDATIONS
Governance Recommendation 1: Formulate business rules for the operation of the caseload
model, and clarify the processes around the acceptance (booking-in) and ongoing
care of non-caseload as well as caseload women receiving care in the Koorana
unit. Include guidelines about how the caseload model will manage increased
demands for its services (i.e. an ‘overflow’ of bookings in certain months).
Rationale and discussion: pages 31-41& 70
Recommendation 2: Investigate and strengthen sources of managerial support for
the model. Rationale and discussion: pages 63, 69 & 71
Continuity of care Recommendation 3: Support full staffing levels for core and caseload midwives in
the Koorana unit, to enable to caseload model to provide enhanced continuity.
Rationale and discussion: pages 42, 67, 71, 87-88.
Recommendation 4: Support the re-configuration of caseload midwives on-call
arrangements, to enhance the continuity of labour and birth care by primary
midwives. This would most likely resemble two groups of three or four midwives
who care for a smaller pool of women, and would relinquish the need for monthly
‘meet and greet’ sessions for all midwives and clients in the practice.
Rationale and discussion: pages 26, 30-32, 41, 68, 70-71.
Recommendation 5: In consultation with consumers, revise the processes of
communication between caseload midwives and women. In particular, the use of
‘text’ messaging to relay clinical information.
Rationale and discussion: pages 35 & 81
Clinical service provision Recommendation 6: Normal birth after caesarean section (NBAC, otherwise
known as VBAC) be included in the obstetric criteria for birthing at the BMDAMH, in
line with the NSW Health Guidelines for teired-level three maternity services
14
(2014)[4] and draft Maternity and Neonatal Service Capability Framework[5]. Offering
VBAC options at BMDAMH will ensure compliance with the NSW Health guidelines,
increase birth numbers in the Koorana unit, reduce the need for local women to
labour and birth at Nepean Hospital, improve continuity of care for women booked
at Koorana, give more women the opportunity to persue a normal birth, and
enhance the patient experience. The most common reason for healthy pregnant
women to have their babies at Nepean hospital is because they want a VBAC,
there are many more women who elect a repeat caesarean section at BMDAMH
because they do not want to travel to Nepean hospital. Offering VBAC services at
the Koorana unit is consitant with the goals of the Towards Normal Birth–NSW
Policy Directive[1], will reduce the strain on maternity services at Nepean Hospital,
and will help reconcile the long-standing expectations of local birthing community.
Rationale and discussion: pages 23, 47, 56, 85, 91-92.
Recommendation 7: Establish a working group to test and review occupational
health and safety concerns associated with conducting waterbirths in the Koorana
unit, in line with NBMLHD clinical and occupational health guidelines.
Rationale and discussion: pages 23, 85-86 & 92
Recommendation 8: That credentialled midwives perform well baby discharge
checks on neonates as per NBMLHD policy, to streamline and expediate the early
discharge process when clinically appropriate for mother and baby.
Rationale and discussion: page 40.
Recommendation 9: Ensure adequate discussion and preparation is provided to
women in the antenatal period, about the anticipated postnatal hospital stay and
home visiting supports available, in order to address consumer fears and
misconceptions about early discharge. Rationale and discussion: pages 86-87.
Recommendation 10: Investigate the feasability of enhanced primary caseload
care in the community, namely; antenatal visits, and early labour assesment and
support in the woman’s home. Rationale and discussion: pages 36-37 & 40
Recommendation 11: Conduct a clinical audit and review of all births resulting in
post-partum haemmorhage (PPH) and 3rd and 4th degree perineal tears at the
BMDAMH. Engage with midwives and obstetricians about ways to improve the
recording, reduce the proportion of births ending in PPH and anal sphincter injury,
and prioritise prospective monitoring and reporting of these outcomes.
Rationale and discussion: pages 57-58.
15
Recommendation 12: For periods of no obstetric or anaethetic cover to BMDAMH,
consider continuing birthing services by operating Koorana as a teired level-2
maternity unit as per Maternity and Neonatal Service Capability Framework[5], for
category-A[6], low-risk women rather than closing for all birthing services.
Recommendation 13: NBMLHD explore opportunities to engage with eligible
midwives by providing visiting rights for midwives to provide intrapartum services at
BMDAMH and the LHD.
Training and education Recommendation 14: Ensure caseload midwives have access to DAWN
(Discharge of the well neonate) training through the Nepean training program, and
are well supported by paediatric staff to establish and maintain competency in this
domain. Rationale and discussion: page 40. Recommendation 15: Support caseload midwives to complete a professional
credentialling process such as the Midwifery Practice Review (Australian College of
Midwives), and achieve NMBA ‘eligibility’. This would contribute to a culture of
professional reflection, and enhance the awareness of the ANMC Competency
Standards for the Midwife.
Recommendation 16: Maintain strong education and support linkages with
Nepean Hospital midwifery services, to ensure Koorana midwives have access to
the full range of professional support and education. Ensure that any rotations to
Nepean Hospital are planned well, to ensure women are prepared and informed
about their primary midwife being on away on rotation.
Rationale and discussion: pages 42, 80-81.
Recommendation 17: The Koorana unit consider acheiving BFHI (Baby Friendly
Health Inititative) accreditation, to improve the quality and consistency of
breastfeeding information given to women whilst in hospital.
Rationale and discussion: pages 82-83.
Resources Recommendation 18: Source additional laptops for use in the community for all
caseload midwives. Rationale and discussion: pages 36-37.
16
Recommendation 19: Authorise remote modum access for hospital laptops, in
order to access obstetriX and iPMs patient records during antenatal visits outside of
hospital grounds. Rationale and discussion: pages 36-37.
Recommendation 20: Antenatal clinic rooms to be booked in advance to avoid
overload in the unit. Rationale and discussion: page 36.
Feedback and information Recommendation 21: Continue to collect and report on all caseload clinical
outcomes. Ensure caseload midwives collect and maintain their own birth statistics.
Rationale and discussion: page 36.
Recommendation 22: Commence re-design of the quality satisfaction survey
instrument to simplify future analysis and reporting of consumer satisfaction.
Ensure all women who birth at the Koorana unit have the opportunity to provide
feedback on their experience of the service, and their individual caseload midwife.
Rationale and discussion: pages 72-73.
Community partnerships and cultural responsivness Recommendation 23: To support an enhanced focus on primary health care in the
community by forging partnerships with community facilities and services such as;
Women’s health and resource centre, Aboriginal resource centre and youth
centers. To explore options of antenatal care provision outside the hospital in such
venues, as appropriate to the woman (this is dependant on meeting
recommenndation 19). Rationale and discussion: page 37.
Recommendation 24: Foster partnerships with local Aboriginal women and
services to understand how the caseload midwifery model can better meet the
needs of Aboriginal and Torres Strait Islander birthing women in the region.
Rationale and discussion: pages 18 & 49.
Recommendation 25: Consider the development of a consumer reference group
for the Koorana unit, ensuring representation of socially disadvantaged or
marginalised members of the community. Rationale and discussion: pages 18 & 91.
Promotion of the caseload service Recommendation 26: That the BMDAMH engages midwives, local woman,
community stakeholders and GPs in publicising and showcasing the acheivments
17
of the caseload midwifery service at BMDAMH. Consider a Koorana caseload
service ‘page’ under the NBMLHD service directory, or multimedia promotion of
service. Rationale and discussion: pages 22-23 & 67.
Recommendation 27: Address community perceptions about the Koorana unit
being ‘closed’ by engaging local consumer groups and the media to promote the
service. This will help address the current unused capacity of the caseload model.
Rationale and discussion: pages 22-23 & 67.
18
INTRODUCTION
Background to the report In January 2014 I was approached by the Midwifery unit manager (MUM) to
undertake an evaluation of the caseload midwifery model at the Blue Mountains
District Anzac Memorial Hospital (BMDAMH). A submission made by a previous
MUM in July 2013, was successful in obtaining funding ($3,840) for the evaluation
(as part of the ‘Nurse Strategy Reserve Initiative’ (NSRI) funding process, stream
three; “Evidence-Based Patient Focused programs that develop midwifery practice
and knowledge”).
The initial NSRI proposal aims were to:
• Evaluate the resources available within the caseload midwifery model, with a
focus on the most efficient, and cost-effective patient journey through the
service.
• Review the collaboration and job satisfaction of core midwives as well as
caseload midwives.
• Identify current and future educational needs of caseload and core midwives.
• Identify ways to increase service provision to the community, particularly the
local indigenous community.
• Reporting on perinatal indicators; birth, breastfeeding, epidural and perineal
trauma rates.
• Report on the patient, demographical characteristics using the service.
• Highlight future innovations that could be adopted.
After resurrecting the document, amendments were made in consultation with the
Local Area District Midwifery Manager, current MUM, and caseload midwives, in
line with the current needs of the service. A concurrent initiative to specifically
identify, and provide, for the educational needs of midwives has since been
undertaken by the area district midwifery manager, and as a result has been
omitted from this evaluation. It was thought that a formal economic analysis would
best evaluate ‘cost-effectiveness’ of the caseload model, but unfortunately this was
beyond the scope and resources available for this report.
19
Extensive community forums (Appendix 1) were held with women in the Blue
Mountains local government area in 2008, as part of the proposal to reform
maternity services at BMDAMH[7]. Some community concerns have been
addressed over this time by the adoption of a caseload midwifery model of care, but
for this reason as well as time and resource limitations, we did not repeat
community consultations of 2008.
Aims The overarching aim of this evaluation is therefore to report on the clinical
effectiveness, quality and sustainability of the BMDAMH caseload model.
The specific objectives were to:
1. Undertake a process, impact and outcome evaluation of the Blue Mountains
Caseload Midwifery Model, using both quantitative and qualitative methods.
2. Describe the model of care, and the women’s journey through the service.
3. Evaluate protocols and guidelines used in the context of supporting
maternity services.
4. Identify significant emerging issues that may arise during the course of the
evaluation.
5. Outline and provide support to a clinical governance framework, to ensure
that all those involved in the model of care are accountable for ensuring high
standards. The goal being, to create an environment in which excellence in
clinical care will flourish.
The need for an evaluation is somewhat overdue, with the service being in
operation for over three years now. Perinatal outcomes under the caseload model
of care are reported over a three-year (triennium) period from July 2011 to June
2014. Data analysis therefore did not commence until after June 2014, to allow for
the availability of three full years (caseload triennium) of retrospective birth data.
20
Information sources
Consultations and information
Therese Ross, (Midwifery Unit Manager) Women and Children’s Unit, BMDAMH.
Anne Yates, (District Nurse Manager, Midwifery), Nepean.
Dr Anmar Mariud (Staff Specialist - Obstetrics), BMDAMH.
Dr Ruby Rashid (Registrar – O&G, BMDAMH)
Andrea Williams (General Manager), BMDAMH
Juanita Taylor (Clinical Midwifery Consultant), Nepean.
All caseload midwives, BMDAMH
All core midwives, BMDAMH.
Surveys
The Maternity unit quality satisfaction survey
Industrial questionnaire
Attitudes to professional role
Demographic data
Information management Group (IMU), NBMLHD
Blue Mountains City Council
Australian Bureau of Statistics
ObstetriX database reports
Perinatal data
ObstetriX database reports, raw in excel format
ObstetriX perinatal reports
NSW Government Health Stats
Bookings, transfers, model of care, and Continuity-of-care data
Caseload midwives diaries
Ward bookings diary
Patient medical records files.
Ward transfer register
ObsetriX reports.
21
Nursery admission register
Caseload midwives – participation and feedback
A participatory action research framework (PAR)[8] has guided the conduct of
information exchange with midwives for this evaluation. Interim reports have been
shared and discussed with midwives and management as they become available.
This enables verification of findings as well as affirming experience, and affecting
change collectively within the caseload group.
Other collateral outputs from this evaluation have included the supply of individual
birth databases and statistics to all caseload midwives in electronic format for use
in professional credentialing.
LOCAL HISTORY AND CONTEXT The Blue Mountains District ANZAC Memorial Hospital is situated within the Blue
Mountains Local Government area (LGA) comprising 26 townships[9]. The hospital
is within a five-kilometer radius of the Three Sisters rock formations, which forms
part of the Greater Blue Mountains World Heritage area, and attracts many tourists
each year. The Blue Mountains Aboriginal community is made up of many Gully
and non-Gully Darug and Gundungurra peoples[10]. Fertility rates for women who
reside in the Blue Mountains region remain above the national average, at 2.02
children per women, however the birth rate across the Blue Mountains LGA has
declined by almost 10% over the last decade[11].
In 2012, there were 810 women giving birth from the Blue Mountains LGA, with only
219 (27%) birthing at the Blue Mountain Hospital[11, 12]. Nepean hospital cares for
the majority of women who do not give birth at Blue Mountains hospital, and
Nepean Private hospital cares for another smaller proportion of Blue Mountains
women. The Blue Mountains LGA has a higher than average home-birth rate
(second highest in NSW)[13], and features a vibrant and politically engaged home
birth community, where several independent midwives provide maternity care to
women in the region.
22
A maternity unit was established at the Blue Mountains Hospital in 1945 and has
undergone two significant renovations and upgrades over this time. The original
maternity wing was known by the Indigenous name of ‘Koorana’ (to bring forth the
young). The name faded into obscurity for decades before being restored by the
hospital Aboriginal reconciliation committee in 2012. The Koorana unit now has
eight single maternity beds, two birthing suits, and one neonatal bed. The majority
of women who birth at Koorana come form the Upper Mountains area (66%), and
this declines to 18% from the mid Mountains, and 16% for the lower Mountains
area[12], which is geographically closer to Nepean hospital in Sydney.
A drop in the number of births at the BMDAMH since 2008 (see fig. 1), is evident
following intermittent maternity service disruptions in 2008 and 2009[14]. The
inability to attract specialist obstetric, anesthetic, and midwifery staff at BMDAMH
led to birthing service closures, resulting in women being transferred via ambulance
to Nepean hospital in labour. Whilst intra-partum transfer was considered to be the
safest option for women, media and parliamentary attention [15, 16], given to the
suspension of birthing services, has undoubtedly contributed to the perception that
women cannot give birth at BMDAMH anymore.
Figure 1: Births per financial year trend, Koorana unit.
The Koorana unit has struggled to recruit and retain midwifery staff in the years
leading up to commencement of the caseload model, owing to national shortages of
midwives and local birthing service interruptions. Nine out of nineteen midwifery
staff had resigned between 2008 and 2009, and ten more out of fifteen resigned in
2011[17]. This provided an impetus to change the way the BMDAMH utilised
0 50 100 150 200 250 300 Koorana unit -‐ Births per year
Ser
23
midwives to provide maternity care. Since the advent of the caseload midwifery
model in July 2011, recruitment into the caseload model has increased from four to
seven midwives over three years, and core staffing has remained stable. No
midwives have resigned since the commencement of caseload in July 2011.
The issue of where and how to birth in the Blue Mountains, has been represented
in the mainstream and social media[15]. Women’s voices opposing maternity service
interruptions have been captured in the mainstream press and television on several
occasions. Headlines such as; “Women in labor sent packing”[16] and “Blue
Mountains residents rally to save their maternity ward”[18] published in the Sydney
Morning Herald, are testimony to the strength and organizing abilities of the Blue
Mountains birthing community, in response to diminishing local birthing services.
Birthing numbers have not been restored to pre-2008 levels, and for this reason,
there is a need to engage with the local community once again to re-build trust, as
well as showcase the achievements of the caseload midwifery model of care at
BMDAMH.
Community forums were held in 2008, when women consistently voiced feeling like
they had ‘no choice’ when required to birth at Nepean hospital. Whilst appreciating
the role of Nepean hospital as a tertiary referral center, Mountains women wanted
to be assured they could birth closer to home when their pregnancy was low risk,
and they also wanted midwifery continuity of care by a known midwife. Next to
these issues, women wanted vaginal birth after caesarean section (VBAC) and
water-birth to be offered at BMDAMH[7]. Midwifery continuity of care has now largely
been realized for women who birth at the BMDAMH, however water-births and
VBACs have remained on the community agenda, as evidenced by consumer
surveys returned and reported on in this evaluation.
24
DEFINING THE TERMS
Continuity of care Over the last 10 years researchers have attempted to achieve consensus on a
definition of continuity of care [19-22]. In the midwifery literature the concept of
continuity has been variously described [23-28]. Midwifery continuity of care is defined
as “continuity over time that allows the development of a relationship in which the
woman and midwives may get to know each other and form a contract of
commitment” [28]p.29 Providing continuity of care allows a woman to establish a
relationship of trust with a named midwife, or small group of midwives throughout
her pregnancy, labour, birth and postnatal period.
Midwifery continuity of care models have demonstrated significant improvement in
maternal Infant outcomes when compared to standard care and address women’s
specific needs, preferences and expectations [24, 29]. Outcomes include:
• Reduced length of labour
• Reduced need for pharmacological pain relief
• Reduced need for intervention in labour, including operative vaginal births
and caesarean sections
• Lower rate of admission of babies to Neonatal Intensive Care Units (NICU)
• Increased satisfaction for the mother
• Reduced rates of postnatal depression
• Improved rates of successful breastfeeding
• Improved rates of attendance at antenatal classes
Caseload Midwifery Caseload midwives provide care to a number of women per year, organize their
time flexibly around their woman’s care needs, and do not work rostered shifts [28].
In this model, one midwife assumes the role of ‘primary’ midwife, providing
antenatal, birth and postnatal care to caseload of women. As well as being ‘primary’
midwife for an agreed number of women each midwife is also the backup midwife
for women who have another midwife as their primary carer. The primary midwife is
25
the woman’s coordinator of care, facilitating her access to more complex care
(often obstetricians), according to her needs. Also referred to as “continuity of carer
model” or “one-to-one” midwifery care. Privately practicing midwives generally
provide care in this model. The model established in BMDAMH in 2011, is basically
a caseload model, except midwives work ‘shifts’ with a ‘team’ style shift
arrangement for on-call birthing care.
Team midwifery Team midwifery is care provided throughout pregnancy, birth and postnatally for a
set number of women by a small team of midwives. These midwives are usually
employed in a maternity or birth unit, and are rostered to work shifts. The team
approach, limits opportunities for continuity of carer and the ability to establish
relationships with women, because care is provided by a team rather than a
primary midwife. The emphasis in these models is on continuity of ‘care’ rather than
continuity of ‘carer’ [28].
Team midwifery improves management and informational continuity for women and
families, and puts less emphasis on the relational dimension of continuity (i.e.
between a primary midwife and the women). In effect, the whole team carries a
caseload collectively, with the opportunity for the women to meet all the midwives
antenatally to provide some measure of intra-partum continuity. Caseload midwives
at BMDAMH, use an element of the ‘team’ approach with respect to birthing care,
by using a roster system to cover on-call with some flexibility for primary midwives
to attend their own women in labour if they choose to.
Caseload The actual number of women a caseload midwife provides care to in a year (i.e. her
workload). This is usually set at 35-42 women a year, depending on risk, complexity
and full or part-time status of midwives working in the model. [30]. The caseload is
40 women per full-time equivalent (FTE) midwife at BMDAMH.
Midwifery Group Practice A Midwifery Group Practice (MGP) is the organizational or management unit in
which caseload midwives usually work [28]. The MGP is organized to maximize
26
continuity of carer for individual women, while supporting and sustaining midwives
in their work. Continuity is usually achieved by midwives working in groups of two or
three, and negotiating backup arrangements for each midwife’s women. This
maximizes the women’s access to a known midwife at her birth, because the ‘pool’
of possible caregivers is small (2-3 midwives).
In larger MGPs (>3), women’s access to continuity of carer, particularly for intra-
partum care can be compromised[31]. Broadly distributed backup arrangements
(e.g. the whole group providing backup, such as the BMDAMH model), will tend to
provide only a small proportion of women with care from their named midwife in
labour and birth, unless individual midwives choose to come in for their women
when not rostered to work. Figure 2 provides an overview of continuity of care
models as reported in the literature.
Core midwives Core midwives are based in hospitals, usually work rostered shifts and provide
clinical support to the primary midwife. Core midwives provide the majority of
clinical care to women who are admitted to hospital.
POLICY AND EVIDENCE SUPPORTING THE MODEL In June 2010 the NSW Health Department introduced a policy directive for NSW
Maternity services; Towards Normal Birth [1]. The directive was partly a response to
the rising caesarean section rates that were published in The Mothers and Babies
report of 2006 [33], and a concern about the morbidity and mortality associated with
multiple caesarean sections in subsequent pregnancies (unexplained stillbirth,[34]
placenta accreta and percreta [35, 36], placental abruption, decreased fertility, ectopic
pregnancy, spontaneous abortion[37] and neonatal respiratory problems[38]).
The resultant 10-point action plan for normal birth, aims to decease the caesarean
section rate and increase the vaginal birth rate in NSW, as well as improving
women’s experience of birth, by ensuring access to continuity of midwifery care. The
Towards Normal Birth action plan runs parallel to the priorities and recommendations
contained in the National Maternity Services plan that recommends reforms
embracing improved access to models of care, collaboration and the expanded role
of the midwife[39].
The BMDAMH Caseload midwifery model fulfills steps three, four and nine of the
Towards normal Birth policy directive [1]. Namely; ‘To provide or facilitate access to
midwifery continuity of carer programs’ (step 3), ‘inform all pregnant women about
the benefits of normal birth and factors that promote normal birth’ (step 4), and
‘Provide one to one care to all women’ (step 9).
Midwife-led care has been consistently associated with higher rates of spontaneous
vaginal birth [24, 40, 41], and a reduction in caesarean section operation rates [42].
Furthermore, high-level evidence from randomized controlled trials indicate that
caseload midwifery is an ‘intervention’ that reduces obstetric intervention, (including
episiotomy and epidural analgesia rates) increases breastfeeding rates, and
provides high levels of satisfaction for women, with no measured detriment to
mothers or babies [43, 44]. In line with published evidence, it is anticipated that a
change to caseload midwifery model at the BMDAMH, has enhanced the quality of
maternity care in the region, without compromising the safety of women and babies.
29
DESCRIPTION OF THE MODEL OF CARE
Establishment There is a long history of consumer support for caseload midwifery care and birthing
in the Blue Mountains region. Plans were drafted in 2003 and 2008 for a caseload
model at BMDAMH that did not eventuate [2]. However, the current model did
commence at BMDAMH in July 2011, shortly after a similar model was established
at Nepean Hospital. The commencement directive came from the Local Area Health
Service in early 2011, and a caseload midwife from the Nepean program was
seconded to BMDAMH to support and mentor new caseload midwives in the
Koorana unit. The model was rolled-out in much the same way as the Nepean
model, with midwives being assigned a caseload of women each, but sharing on-call
birthing among the group. The new model that was established at Koorana did not
resemble earlier models proposed, with respect to the working configuration and on-
call arrangements of midwives (presumably because of the small number of
midwives recruited at commencement would have made it difficult to work in smaller
groups of twos or threes).
Annualized salary agreement Caseload midwives at BMDAMH are employed under an industrial agreement with
the Nepean Blue Mountains Local Health District, ratified by the NSW Nurses and
Midwives’ Association, and based on the Model NSW Department of Health MGP
annualized salary agreement[45], the agreement allows for flexible working
arrangements and self-management of midwives workload, deciding their own
working patterns and negotiating their own leave. This type of arrangement
empowers caseload midwives to be attentive to the needs of the women in their
care, rather than to the dictates of traditional shiftwork. Caseload midwives receive a
base salary in accordance with their year of service or clinical award, with a 29%
loading that replaces shift loadings and on-call allowances. Caseload midwives self-
roster, having nine days off a month (FTE), and are entitled to six weeks annual
leave per year. The agreement stipulates that midwives not work longer than 12
hours at a time, handing over care (usually of a woman in labour) to their caseload
30
colleague after the 12 hours has expired.
Table 1: Koorana Caseload midwife Profile July 2011 – June 2014
Date Team structure July-11 Recruitment 3 x fulltime midwives start + Aug-11 Working as one group of four 1 x fulltime midwife Nepean Sept-11 seconded as a mentor Oct-11 1 midwife leaves for 6 months Nov-11 1more fulltime midwife starts & Dec-11 Nepean mentor midwife Jan-12 leaves & is replaced Feb-12 Mar-12 1 X 0.7 FTE midwife starts Apr-12 Working a one group of five & Nepean midwife leaves May-12 1 fulltime midwife comes back
from 6 months leave June-12 (Caseload midwives care for 62.3% of all July-12 women who book into BMDAMH) Aug-12 Sept-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 Mar-13 Apr-13 May-13 June-13 Working as group of six 1x fulltime midwife starts July-13 Working as group of seven 1 x 0.5 FTE midwife starts Aug-13 (Caseload service care for 72.7% of all FULLY STAFFED Sept-13 women who book into BMDAMH) Oct-13 Nov-13 Dec-13 Jan-14 Working as group of six 1 x fulltime midwife Feb-14 Transferred to Nepean & 0.5 FTE
becomes 0.8 FTE Mar-14 (understaffed again) Apr-14 May-14 (Caseload midwives care for 95.6% of all June-14 women who book into BMDAMH)
31
The model Staffing for the model was taken from the existing complement of 12.53 full time
equivalent (FTE) midwives on the maternity ward. Six FTE caseload positions were
taken from the ward complement, and 6.53 FTE positions remained as ‘core staff’.
Each FTE midwife takes up to 40 women per year in her caseload (four women
booked per month, per midwife). The caseload practice started with a complement of
four midwives (one from Nepean), and only reached full capacity (6x FTE = 7x
midwives) in July 2013. For the duration of the model, the midwives have worked as
a whole group (of four, five, six and seven depending on stages of staffing capacity),
rather than in pairs, or groups of three (see table 1), and relieve each other for
annual holidays. (i.e. there is no holiday relief midwife position built into the model).
Midwives plan their holidays in advance and do not book women into their caseload
who are likely to birth whilst on leave.
Despite the annualized salary arrangement and associated assumptions for flexible
work arrangements, caseload midwives essentially work to a roster system at the
Koorana unit. Roster codes describe several types of shifts (J, K, M6 and M5) and
the duties expected of these shifts. Shift types were developed by management to
enable working hours to be entered into the ProAct hospital roster database.
Caseload shifts at the Koorana unit are described below:
1. J: 7am – 7pm on-call caseload midwife, who is called to care for women in
labour during these hours
2. K: 7pm-7am on-call midwife who cares for women in labour overnight, even if
these women are not allocated to caseload.
3. M6: 2nd on-call midwife during the day, however no specified start and finish
time. Midwife can schedule ante or postnatal visits on these days.
4. M5: Midwife works to own schedule, or can have this day off is she is has
worked too many hours. M5 days are only included in the roster when there is
close to a full complement of staff.
32
The shift system used in the model thus far, aims to give each caseload midwife time
to attend antenatal appointments for the women in her caseload, as well as visit
postnatal mothers and babies at home or on the ward. Intra-partum care is provided
in a rotating, on-call system where one caseload midwife in the group is on-call for
all birthing women in the practice after hours (shifts J and K). Thus each midwife
does a proportion of on-call shifts each month, where she only attends work if a
women presents in labour.
All caseload midwives divert their phone to the on-call midwife after hours, who is
the first port-of-call for all women’s phone calls to the practice, and cares for all
women in labour. A commonly occurring exception to this, is when the primary
midwife makes a arrangement with the on-call midwife ahead of time, that she will
come in and care for her women in labour should women present after hours, or
whilst the primary midwife is on a day-off. Provision for primary midwives to attend
their own women in labour when not rostered to work is built into the draft rules of
the model [46]. In effect, this means that a woman allocated to a primary midwife has
a one in six chance (or one in four, five or seven, depending on number of midwives
in the practice at the time) of having her primary midwife care for her at birth if all
midwives adhere to the roster. However, often the woman’s named midwife does
attends her birth on a day off, or when not rostered to be on-call, which improves the
chances for the woman, of her primary midwife attending her birth.
Despite the larger ‘pool’ of women for the on-call caseload midwife to potentially care
for in labour each shift, caseload midwives at Koorana on average still manage to be
present for over half of their own women’s births*, with an array of 44%† of their
women’s births, if midwives working in accordance with the roster, to up to 81% of
their women’s births, when midwives regularly attend women in labour outside of
roster hours. This is evidence that caseload midwives are flexible to varying extents,
and that frequent communication has boosted birth continuity outcomes within the
constraints of the rostering system that is in place.
The woman is given her primary midwives mobile phone number, and on-call
* Average Continuity at birth rate for all caseload midwives at BMDAMH between the period of July 2013 - June 2014. † Corrected, to exclude women who birthed at Nepean hospital, for the period July 2013 – June 2014.
33
arrangements are explained to all women on booking in to the service. Women have
the opportunity to meet the other caseload midwives (who they might otherwise meet
in labour) at monthly meet-and-greet sessions organized and hosted by Koorana
caseload midwives.*The purpose of meet-and-greet sessions is for women to meet
all of the caseload midwives, and make connections with other women.
Staffing and Support Management
The Nurse/Midwifery Unit Manager (NUM) of the combined Maternity and Children’s
ward (Women and Children’s Health) is responsible for leadership, management and
facilitation of communication relating to the Koorana caseload practice, and
processing of time sheets.
Administration
The ward clerk on the Maternity ward provides some administration support to the
caseload service by providing women with booking and administration forms to
complete. The ward clerk processes the completed paperwork that enables caseload
midwives to allocate women to a primary midwife.
Core midwives
Core midwives make up about half of the midwifery staffing component of the
maternity unit, and are employed on a rotating roster. They provide back up to the
caseload midwives after hours for intra-partum care, and care for the small
proportion of women (5%) who are not booked under caseload care (e.g. doctors
clinic or Nepean caesarean sections). Core-staff provide 24-hour care to all women
and babies who stay in hospital following the birth. Three core midwives are needed
to staff the unit in a 24-hour period (one per shift). Caseload midwives were often
called in to fill core staff roster gaps or sick leave in the preceding three years of the
evaluation.
Obstetric staff
Three part-time, specialist obstetricians and one part-time registrar provide the bulk
34
of obstetric support to the caseload model. All women wanting to book into the
caseload model of care, will be reviewed (or have her notes reviewed) by obstetric
staff at the Koorana unit soon after their initial booking visit. Collaboration occurs
between the caseload midwife and obstetric staff in the event of risks or
complications in any stage of the pregnancy, in accordance with the National
Midwifery Guidelines for Consultation and Referral [6] or at the wishes of the woman.
The woman consults again with the obstetrician at 40 weeks gestation to initiate a
post-dates induction of labour plan.
Specialist obstetricians, (and locums on occasions), provide 24-hour, on-call
obstetric support to caseload midwives who are the lead providers of intra-partum
care, as well as conducting elective Caesarean section theatre lists. The proportion
of women receiving obstetric-led care has diminished from 50% (2011) to less than
3% (2014) as a result of the introduction of the caseload model at BMDAMH (fig. 5).
This has considerably reduced the workload of specialists, and redirected their
efforts to clinically appropriate obstetric cases, and enhanced gynecological services
at BMDAMH.
Birthing services at BMDAMH were regularly suspended in 2008 and 2009 due to a
lack of either; obstetric, anesthetic and paediatric cover at BMDAMH. When there
are no specialists available to fill the roster, women in labour are re-directed to
Nepean hospital, 50 minutes drive away. It is likely that the unfolding of the caseload
model, as well as the appointment of a part-time obstetric registrar at BMDAMH has
contributed in a positive way to the retention of specialist obstetric staff in the unit,
resulting in a drastic reduction of maternity unit closures since the model
commenced.
Cars
Caseload midwives use their own private vehicles for visiting women and babies in
their homes, and claim these expenses back on personal tax. All midwives vehicles
carry baby scales, dopplers, and other equipment necessary to perform antenatal
and postnatal visits in women’s home.
Phones
Each caseload midwife is provided with a mobile phone to be used in accordance
35
with NDMLHD policy, and paid for by the health service. All midwives divert their
incoming calls on their phone to the midwife who is on-call from 7pm – 7am (K shift)
each night, and the day on-call midwife, (J shift), between the hours of 7am – 7pm.
When midwives are running clinics or doing home visits during the day, they may
also un-divert their phone to enable communication with women who have
appointments or need advice. Women, and other midwives communicate by ‘texting’
each other about appointments, or women in labour. A text message will register on
primary midwife’s phone, whereas a phone call will often be diverted to another
caseload midwife. In this way, the primary midwife can choose to check her work
phone messages and respond to text messages that women or colleagues leave on
her days off.
IT systems
Caseload midwives are required to enter all their antenatal appointments in the iPM
system as an occasion of service, as well as ObstetriX, an obstetric information
database for each client, based on the clinical perinatal dataset. Ward computer
terminals are used for data entry, as well as two laptops (whilst connected to hospital
Wi-Fi).
Clinical governance
Caseload midwives adhere to the National Guidelines for consultation and referral[6,
47].The guidelines ensure the appropriate referral and consultation pathways are
negotiated with the obstetric staff in the Koorana unit, and women significant risk
factors have their care transferred to Nepean hospital according to The Blue
Mountains Hospital Obstetric Criteria, last revised in 2009 (see appendix 2).
Midwives professional conduct and practice is guided by the Australian Nursing and
Midwifery Council’s National Competency Standards for the Midwife (ANMC 2008).
Critical incidents are reported using the Incident Information Management System
(IIMS) reporting framework [48].
Monthly maternity morbidity and mortality meetings (M&M meetings) are held
between all midwives on the unit, management and obstetric staff. These meetings
are an audit and quality assurance exercise, as well as an opportunity for the
professional development for all staff involved. It is recommended that caseload
36
midwives also keep individual monthly statistics of their activity and birth outcomes,
and submit these periodically to management. However this has largely not occurred
for various reasons, including the huge volume of other essential electronic and
paper-based documentation/reporting that is required of caseload midwives.
Physical workspaces The caseload practice operates out of the Koorana unit at BMDAMH. A beautiful unit
consisting of two birth suites, eight single maternity rooms, and one neonatal bed in
a level two nursery. A reception desk seats a ward clerk who greets women, families
and visitors on their way into both the maternity unit and Children’s ward. Directly
behind this, is an open ‘midwives work station’ with a computer. Outside the two
birthing suite rooms, there is a similar workspace, used by all clinicians in the
maternity unit.
The ‘caseload office’ serves the whole group of seven midwives and is a 2.4 x 3
meter space with a desk, computer and cabinets housing postnatal files, and
caseload documentation. The office serves as storage for all personal and
professional resources that are used by caseload midwives. Another small
consulting room provides the space for all antenatal consultations conducted by
midwives and obstetricians on the unit. During office hours the clinician demand for
this room is high, due to privacy and computer access, it enables contemporaneous
documentation in women’s electronic antenatal record whilst the consultation is in
progress. The problem with this however, is there is rarely only one caseload
midwife or doctor consulting with women at any one time. Caseload midwives keep
their own separate appointments diaries, often resulting in several caseload
midwives plus core staff in the workspaces at the same time, waiting for women to
arrive or for clinic space to become available.
The frustration of this scenario has been partly relieved with the introduction of two
laptops for the caseload service, which makes it possible for caseload midwives to
use an unoccupied maternity room with the laptop to complete an antenatal visit.
However, a lack additional laptops and remote access prevents midwives being able
to use a laptop outside the hospital environment. Caseload midwives could
37
potentially do antenatal visits in the woman’s own home, or a community venue such
as; Woman’s Health Centre, Aboriginal Resource Centre or a Youth center as
appropriate for each women.
Midwives at BMDAMH have historically conducted weekly antenatal clinics at the
Women’s Health and Resource center in nearby Katoomba. These community
clinics were well attended, and valued highly by women in the Blue Mountains area [7], and enjoyed by the midwives who conducted them. Such arrangements foster
linkages with community organisations, and provide women with convenient and
culturally safe places to access other than the hospital. For women with small
children, and limited transportation, antenatal visits in the home can reduce ‘no
shows’ and be a positive experience for the woman and the midwife. Midwives
currently have the equipment and transportation to conduct antenatal visits outside
the maternity unit, but lack remote computer access for laptops to connect with the
clinical databases required, which has proved to be a significant barrier to exploring
these options.
Women’s care journey Women usually attend their GP for pregnancy confirmation, antenatal screening
pathology and early ultrasounds. She is then advised to phone the maternity ward to
request a one page ‘booking in form’ that the W&CH ward clerk can mail or give to
her in person. The ‘booking in form’ is mailed or dropped back to the maternity unit
once the woman has completed it, along with a copy of any antenatal test results the
GP has initiated.
The women should receive a call from her newly appointed caseload midwife within
two weeks of sending in the form (after the midwife has reviewed her medical history
and any other requirements she has made explicit in the booking in form and GP
correspondence), this phone call is usually the woman’s first contact with her
caseload midwife, when they arrange a suitable time for a booking history visit at the
hospital. At this initial visit, a yellow pregnancy card is initiated (if not already by the
GP), and pregnancy record commenced on the ObstetriX electronic database. The
woman is introduced to the service, the philosophy of the model, and given her
38
primary caseload midwife’s phone number and guidelines for contacting her midwife.
The woman and her partner are also encouraged, and enrolled in parenting classes
conducted on the hospital grounds if they are interested in this. During the booking
visit, the woman is given a pamphlet pack pertaining to her pregnancy, and an
appointment is made for her to see the obstetric staff if there are medical or obstetric
concerns of consequence to the woman or midwife in the booking visit. The woman
in most cases attends the same venue to see an obstetrician. At this appointment
she can pursue specialist or allied health referrals as appropriate (e.g.
physiotherapy, psychology, psychiatry, medical, anesthetics), and be ‘cleared’ to
receive her care under the caseload midwifery model.
As Koorana is a low-risk, level three maternity unit, all women who meet the criteria
(appendix 2) for birthing at Koorana, are eligible to be cared for in the caseload
midwifery model. Even if the women should need to see an obstetrician periodically
throughout her pregnancy, the relationship with her caseload midwife is retained
throughout her pregnancy, birth and postnatal period. If a women's recommended
pregnancy care lies outside the Blue Mountains Obstetric guidelines (e.g. Vaginal
birth after caesarean section, VBAC), the woman is advised to also book in to
Nepean hospital for birth.
An average of seven (depending on gestation at booking) mutually convenient
antenatal appointments are arranged between the primary midwife and the women
to attend at the hospital in accordance with the antenatal visit schedule. The primary
midwife calls, or texts the woman if an appointment needs to be rescheduled due to
the midwife attending another woman in labour. The woman occasionally may see
another caseload midwife for an antenatal visit when her primary midwife is away on
annual leave. The primary midwife will arrange, and follow up any pathology or
ultrasounds and communicate results to the woman. The primary midwife also
liaises with obstetricians, allied health, and community agencies in consultation with
the woman if required. The woman is invited by her primary midwife to attend a
meet-and-greet evening sometime in her third trimester. Meet-and-greet sessions
allow the woman to make contact with the other five or six midwives in the caseload
practice in a friendly informal environment.
39
The woman will be transferred to Nepean hospital by ambulance if she presents to
the Koorana unit with threatened premature labour at less than 36 weeks gestation,
or if another significant risk factor emerges such as pre-eclampsia. If the woman
requires additional ultrasounds in her pregnancy, she can attend a private ultrasound
service in Katoomba, or the Feto-Maternal Assessment Unit (FMAU) facility at
Nepean hospital. The woman will also be advised to present at the FMAU - post-
dates clinic if she is still pregnant at 41 weeks gestation.
The women calls her primary midwife in the event of her labour starting, waters
breaking, vaginal bleeding, or reduced fetal movements (or any other concern). In
most cases she will encounter the caseload midwife on call on the other end of the
phone (unless her primary midwife’s phone is un-diverted), who will advise the
woman accordingly. The woman may also text her primary midwife if the concern is
not urgent. The on-call caseload midwife (or primary midwife) will advise the woman
if a hospital presentation is necessary, and in which case the woman will be
assessed and cared for by the on-call caseload midwife (or the primary midwife if
she already on duty, or able to come in). Ideally, the woman has met the on-call
caseload midwife at a previous meet-and-greet session. The woman will also
encounter a core staff midwife at this time, acting in a support role for the caseload
midwife after-hours.
The on-call caseload, or core midwife may care for the woman in early labour to
enable her primary midwife to take over for labour and birth care at a later time. If the
woman needs to birth at Nepean hospital (e.g. VBAC), the woman’s caseload
midwife can accompany her to Nepean hospital to provide intra-partum care there if
caseload-staffing levels permit. This has only been possible since June 2013, due to
improved staffing levels at the Koorana unit.
If the woman’s primary midwife was not present for her labour or birth, she will visit
the woman and new baby in hospital on her next working day. The women will be
transferred to a postnatal room in the maternity unit a few hours after giving birth,
and if everything is normal she may have early discharge home after four hours
(however this is rarely taken up by women in the Koorana unit). Core midwives will
care for the woman in hospital, with the primary, or on-call birth midwife providing
40
input and additional support with breastfeeding and postnatal care. The core, or
caseload midwife will initiate hospital discharge for the woman and her baby, which
includes arranging a hearing screen appointment for the baby within the next week,
and liaising with the paediatrician to attend to a well-baby check before the mother
and baby leave the hospital, sometime delaying discharge for several hours, or until
the next day. The woman is visited by a community health nurse usually before she
leaves the hospital, and given a pamphlet and contact details of the community
health center.
Once the woman is home with her baby, her primary midwife visits her there for two
weeks. The schedule of home visits is determined in accordance with the needs of
the woman and her baby. In the event that the primary midwife is unable to attend a
visit on a day when one is required, another caseload midwife may visit the woman
at home. The woman is formally discharged from the service around two weeks
postpartum, after appropriate community support and referrals have been made.
A note about ‘early labour’, assessment and support
Due to the twelve hour, on-call shift arrangements in place, the caseload midwife on-
call will always be relieved at 7am or 7pm if the woman has not birthed in that time
frame, so there is no pressure on the caseload midwives time (unless she has
appointments the next day). This can result in women admitted to hospital overnight
for comfort measures (e.g. warm water immersion, panadeine forte, heat packs and
sleep) in early labour, often to be discharged in the morning when the ‘contractions’
have ceased. If the primary midwife remains on-call for more of her women, this
scenario becomes problematic, as her own hours are consumed by caring for
woman (in hospital) who are not in active labour, and she may be more inclined to
encourage women to stay home for longer. Under most caseload low-risk models,
early labour assessments (including cervical assessment if necessary), and
reassurance are performed in the comfort of the woman’s home to avoid an
unnecessary, and early admissions[30] and is something that should be discussed
with women in the antenatal period.
41
Table 2: Relational continuity between woman and midwives at Koorana A
nten
atal
car
e
• Primary midwife conducts 85-100% of the antenatal visits for each woman (notes audit 2014, excluding obst. visits).
• Woman sees a backup caseload midwife only when her primary midwife is on leave.
• Primary midwife will reschedule appointments with the woman if held up at a birth.
Labo
ur a
nd b
irth
care
• After-hours, primary midwife phone diverted to midwife on-call.
• As labour is unpredictable, woman will not know which midwife is on-call.
• Midwife on-call (1 of 7), will care for her in labour & birth.
• Primary midwife can come in to care for woman if the midwife on-call or woman informs her by text message.
• The woman is likely to meet a core staff midwife in labour and birth.
• Model had a an average 52% continuity at birth rate (see fig.3)
Post
nata
l car
e - H
ospi
tal
• Core midwives in hospital care for woman & baby.
• The woman will meet 3 core midwives/ 24hrs.
• The primary midwife or her backup (usually the birth midwife) will visit her in hospital for additional support.
• The woman & baby stay in hospital for 4-48 hours.
• Caseload or core midwife will initiate discharge arrangements.
Post
nata
l car
e - H
ome
• Primary midwife sees the woman at home usually for 2 weeks.
• A backup midwife may visit if the visit is urgent and the primary midwife cannot attend.
• Home visit continuity rate 70-100% for primary midwives (notes audit 2014).
• Primary midwife ensures community referrals are made, and postnatal support is adequate.
1 backup midwife (pre-‐arranged)
Primary midwife Woman
Woman & baby Primary
midwife
Core midwives
(or backup midwife)
backup midwife
Woman & baby Primary midwife
Core midwife
42
Measures of birth continuity
There are limited benchmarks or indicators for birth continuity in the literature on
caseload midwifery models. In the past few years, the public maternity sector has
been flooded with discourses describing and promoting midwifery continuity of care
models[28, 30]. The literature, guides and toolkits available, describe all aspects of
caseload operation, including sample roster templates and self-care strategies. The
literature is not as explicit however, in defining benchmarks for primary midwife
continuity at birth, and existing caseload practices rarely publish data on the matter.
One study describes a 94.5% primary midwife-birth continuity rate, in a caseload
practice where midwives work in pairs[49]. Unpublished data describing primary
midwife-birth continuity rates from two interstate caseload practices, ranged from
57% (when working in three’s, with annual-leave midwife substitution), to 98% (when
working in two’s, with no fixed days off). Two other caseload practices in Sydney
report continuity at birth rates of between 70%-80%[50].
Primary midwife-birth continuity is typically compromised by roster arrangements
that limit on-call availability of the primary midwife for her women, or when women
birth whilst midwives are on leave. This former of these is certainly a factor impacting
birth continuity at the Koorana unit. Another factor is the stability of the unit as a
whole, as caseload midwives are required to regularly fill “core” shifts when the unit
is under staffed, (evident in 2011-2012, when the unit endured unstable
management and low core staffing levels for over twelve months). On occasions
being unable to attend to their women in labour, having just filled a “core” shift or
acting in management positions during the day. (see figure 3). The continuity rate
improved from 2011 by 80%, (from 28.5% - 51.5%) once the unit had stable
management and all positions were filled. The last twelve months of data (continuity
rate of 51.5%), is thought to be more indicative of the how the model design can truly
accommodate continuity of intra-partum care in its current form (see figure 3).
43
Figure 3: Proportion of birth attendance for primary midwife, & reasons. (Attendance at birth does not necessarily = accoucher.)
44
In an attempt to separate factors intrinsic to the model’s design, from factors relating
to the wider unit’s operation and the need for referrals to higher levels of care,
reasons for primary midwife not attending her births are expanded by explanations
(such as; No- acting NUM role, exceeded 12 hours, or birthed at Nepean). Although
there is a provision for the primary midwife to travel to Nepean to attend her women
in labour, this represents an obstacle of time and distance, that is not a
compromising factor in the continuity of care of larger metropolitan units.
The trend towards improved birth continuity in the past twelve months is evident
again in figure 4. With cases affected by babies born before arrival to hospital
(BBA’s), Nepean births and ward staffing removed, there is still a wide variation of
continuity between individual midwives (44.4% -80.6%), not necessarily related to
full-time employment in the practice. The apparent variation between midwives
reflects a degree of flexibility within the model, as midwives juggle the demands of
on-call work and life commitments.
Figure 4: Proportion of births each primary midwife attended (cases excluded that were extraneous to operation of model, such as BBA, birth at another institution, exceeded hours).*
* Midwives # 3, 4, 7, 8 & 9 employed for part of the three-year duration of caseload.
31.4
43.3
54.5
26.3 31.2
44.4 42.9
0 0
25.0
0 0
33.3
50.0
73.7
46.3 43.8
66.7
0.0
30.8
50.0
0.0
66.7
80.6
0 0
76.5
29.3
44.3
63.8
0.0
10.0
20.0
30.0
40.0
50.0
60.0
70.0
80.0
90.0
2011-‐2012 2012-‐2013 2013-‐2014
% of own caseload births
attended
Caseload year of operation
MW 1
MW 2
MW 3
MW 4
MW 5
MW 6
MW 7
MW 8
MW 9
Average
45
WORK FLOW THROUGH THE MATERNITY UNIT
Booking into Blue Mountains hospital More women book into the BMDAMH maternity unit, than intend to continue
antenatal care there. Since the commencement of caseload in 2011, booking-in
visits are predominantly attended by caseload midwives, irrespective of intended
antenatal care provider or place.
Table 3: Booking-in visits at Koorana according to intended maternity provider, July 2011-June2014 Intended maternity provider & birth place at booking N %
BMDAMH 737 94.9
Nepean hospital 23 3.0%
Independent midwife* 8 1.0%
Unknown 9 1.2%
Total 777 100.0
There is an attrition rate of 18.3% between booking in visits and number of women
who end up birthing at the BMDAMH; the antenatal pathways for these women are
shown in table 3.
Who provides antenatal care? Caseload midwives overwhelmingly provide the majority of antenatal care at
Koorana, as at June 2014. Obstetricians (obstetric-led), core midwives and GP
shared-care, also provide antenatal care in small numbers (see figure 5).
Introduction of the midwifery caseload model in 2011 has resulted in a diminished
demand for obstetric-led care.
* Woman planning a homebirth with an independent midwife are required to attend a booking-in visit at hospital in the event the women should need an intra-partum transfer from home.
46
Table 4: Number and proportion of women who received antenatal care at Koorana according to model of care
Caseload n (%)
Obstetric led n (%)
Standard midwife (core) n (%)
GP Shared care n (%)
Jan-Jun 2011 0 48 (50%) 46 (47.9%) 2 (2.%1) Jul11-Jun12 162 (62.3%) 71 (27.3%) 24 (9.2%) 3 (1.2%) Jul12-Jun13 183 (72.7%) 47 (18.6%) 19 (7.5%) 3 (1.2%) Jul13-Jun14 239( 95.6%) 7 (2.8%) 3 (1.2%) 1 (0.4%)
Figure 5: Proportion of women per model of antenatal care, Jan 2011 – June 2014
Where do caseload women give Birth? As the Koorana unit is a level three, low risk maternity unit, women transfer care
between BMDAMH, and other institutions due to emerging risk factors or relocation.
From the women receiving caseload antenatal care at Koorana from July 2011-June
2014, 83.2% had their babies at the BMDAMH, and 16.8% had their babies
elsewhere*. Table 5 below, gives a breakdown of the reasons why caseload women
have their babies elsewhere (usually Nepean hospital).
Table 5: Reasons why caseload model women did not birth at Koorana July 2011-June 2014.
Trimester Reason for birthing elsewhere Number of women Second trimester (13w-27w) Gestational diabetes 7 Premature rupture membranes 1 Third Trimester Wanted a VBAC 15 Premature rupture membranes 7 Pregnancy induced hypertension 4 Moved out of area 4 Heart arrhythmia of mother of baby 3 Intrauterine growth restriction 3 Post-dates (>42w) induction 3 Threatened premature labour 3 No obstetric or anesthetic services at BMDAMH 3
* 18% of all women (irrespective of model of care) had their babies elsewhere.
0
20
40
60
80
100
120
Jan-‐Jun 2011 Jul11-‐Jun12 Jul12-‐Jun13 Jul13-‐Jun14
Proportion of w
omen
Caseload
Obstetric led
Standard midwife (core) GP Shared care
47
Born before arrival to hospital (BBA) 2* Deep vein thrombosis 1 Wanted a water-birth 1 TOTAL 84 Women seeking a vaginal birth after caesarean section (VBAC) is the most common
reason for caseload women to have their babies at Nepean hospital (n=15, 17.8%).
As the Koorana unit does not offer VBACs, women are forced to seek this option
elsewhere. In addition to this, there are a number of women who choose an elective
caesarean section at BMDAMH for their subsequent birth, because they do not want
to travel to Nepean to have their baby. These women would have otherwise chosen
a VBAC if it were offered at the Koorana unit. Three women were transferred to
Nepean due to lack of obstetric or anesthetic cover.
All births at BMDAMH In January 2014, BMDAMH started performing elective caesarean sections on a
small number of women who were previously booked at Nepean hospital, in order to
redistribute births between the hospitals, and enhance activity-based funding for
BMDAMH. These births (“Nepean booked CS” n=23) represented in figure 6, have
been excluded from all other reporting and analysis of maternal characteristics and
outcomes for this evaluation (as BMDAMH was not involved in the antenatal care, or
clinical decision making process for these women).
79% (501) of all the women who gave birth at BMDAMH over three years were
cared for in the caseload model of care (figure 6). The proportion of women cared for
by caseload midwives increased over the three years, in accordance with the
increasing capacity of the model over that time period.
* There were three BBA’s in total, two were caseload care, and one was obstetric care.
48
Figure 6: All Koorana unit births July 2011-June 2014, by antenatal care provider.
MATERNAL CHARACTERISTICS
Maternal age
From 1st of July 2011 until 30th June 2014, the average age of mothers giving birth at
the Koorana unit was 30.5 [SD 6.0] years, ranging from 15.9 to 48.2 years of age,
and this did not significantly change over the three years. Age groupings displayed in
figure 7 below, show that there is a slightly higher proportion of teenage mothers and
mothers aged 35 and older in the Koorana cohort when compared to mothers across
NSW[51]. Younger and older mothers have an increased risk of medical
complications of pregnancy such as hypertension (high blood pressure) and their
babies are more likely to be low birth weight, premature or to be stillborn [51].
49
Figure 7: Age of Koorana mothers compared with NSW state birth cohort
Indigenous status
There were 25 (4%) women who identified as being Aboriginal or Torres Strait
Islander, in the three years of caseload (caseload triennium). This is higher than the
proportion of Aboriginal residents living in the Blue Mountains Local government
area (2.7%)[11]. Maternal and infant health outcomes for this population are
considerably worse when compared to their non-indigenous counterparts. Continuity
of midwifery care (caseload) for these women has been shown to considerably
improve maternal and infant health outcomes[52].
Figure 8: Proportion of ATSI women who birthed at the Koorana unit, July 2011-June 2014
Parity
There were 241 (38%) primiparous women (having their first baby), and 387 (61%)
multiparous women having their second or subsequent baby in in the three-year
period of the evaluation. Another 10 (1%) women had had their fifth or more baby
(grand multip) during this time in the Koorana unit*.
* Includes characteristics of three mothers who gave birth shortly before arrival (BBA) to BMDAMH
<20 years 20-‐34 years >34 years Blue Mountains Hopsital 4.0% 68.6% 27.4% Rest of NSW comparison 3.2% 73.1% 23.7%
0.0% 20.0% 40.0% 60.0% 80.0%
Axis Title
Age group of mother (in years)
96%
4% ATSI women
Non-‐ATSI
ATSI women
50
The proportion of primiparous to multiparous women was slightly higher in the
caseload cohort (38%, n=635), compared to before caseload (35.2%, n=643),
however this was not statistically significant*
Figure 9: Parity group for mothers who gave birth in the caseload triennium.
Smoking in pregnancy
11% of women who birthed at Koorana smoked in pregnancy, this did not differ for
women booked into the caseload model of care, and was on par with the NSW rate
of tobacco smoking in pregnancy (11.2%)[3]
Body mass index (BMI)
The majority of women (97.5%) who birthed at Koorana had a healthy BMI. The
average BMI was 24.5 [SD 4.7], which ranged from 16kg/m2 to 41.5kg/m2. Twenty-
two women (3.4%) were underweight, † and only 18 women were considered
overweight (2.8%).‡ Due to increased risks, midwives who care for women who are
under or overweight, are likely to consult with an obstetrician more frequently during
the course of the pregnancy[6].
Mental health and wellbeing
A huge proportion of women who birthed at Koorana reported experiencing mental
illness and trauma, with more than a third reporting anxiety and depression (n=221, * Chi2 test (p>0.05) † BMI < 18 ‡ BMI > 35
38%
61%
1%
Parity
Primiparous
Multiparous
Grand multiparous (5+)
51
34.8%). History of childhood abuse was subsequently reported by 13.6% (n=85) of
women. Overall, psychosocial issues were identified in 83.5% (n=533) of cases,
necessitating the initiation of support and referrals.
MATERNAL AND INFANT HEALTH OUTCOMES*
Antenatal Admissions 41 (6.4%) women were admitted to hospital at least once during pregnancy†. The
most common diagnoses for antenatal admission over the three-year period were
threatened premature labour (n=11, 2.7%), followed by vaginal bleeding (n=6, 1.5%),
and hyperemesis gravidarum (n=5, 1.2%).
Plurality 634 women had singleton pregnancies, and 1 woman had a twin pregnancy over the
caseload triennium.
Labour
Onset of labour Labour onset is categorized as ‘spontaneous’, ‘induced’ or ‘no-labour’, i.e., where
caesarean sections were performed before labour had started. Despite the apparent
increase in induction rate in the third year of caseload, the overall average induction
rate at Koorana has decreased from 21.0% in the baseline triennium to 18.1% in the
caseload triennium, however this reduction was not statistically significant at α<.05
‡.
* Outcomes are only for all births at BMDAMH, and do not include 3 x BBA’s † Not including 2 occasions of care for external cephalic version (ECV), performed at Nepean, otherwise recorded as admissions. ‡ Chi2 p<0.194
52
Table 6: Onset on labour type for all births, per year of caseload operation.
Onset labour 2011-2012 2012-2013 2013-2014 Total – Caseload triennium
N % N % N % N %
Spontaneous 144 68.3 154 72.0 139 66.2 437 68.8
Induced 33 15.6 36 16.8 46 21.9 115 18.1
No labour (elective
CS)
34 16.1 24 11.2 25 11.9 83 13.1
Total 211 100 214 100 210 100 635 100
Table 7: Onset of labour profile, for baseline and caseload trienniums
Onset labour Baseline triennium 2008-2011
Caseload Triennium 2011-2014
N % N %
Spontaneous 381 59.3 437 68.8
Induced 135 21.0 115 18.1
No labour 127 19.8 83 13.1
Total 643* 100 635 100
Induction A combination of artificial rupture of membranes (ARM) and oxytocins, accounted for
the highest proportion (35.7%) of induction method used over the three years of
caseload. Oxytocins (syntocinon) were used in 52.2% of all labour inductions in this
time period.
Table 8: Method of labour induction
Method of induction used N %
ARM only 10 8.7
ARM+Oxy 41 35.7
Prostaglandin only 9 7.8
Prostaglandin+ARM 3 2.6
Prostaglandin +ARM+Oxy 12 10.4
Prostaglandin +Oxy 7 6.1
Oxy only 32 27.8
Not recorded 1 .9
* Unknown labour details for 2 women in baseline cohort
53
Total 115 100.0 Table 9: List of indications for induction of labour.
Indication for induction N %
Chorioamnionitis Diabetes Elective/social Fetal demise Fetal growth restriction Hypertensive disease No pre-labour intervention/s Non-reassuring fetal status Other Pre-labour rupture membranes Pre-labour rupture membranes & non-reassuring fetal status Pre-labour rupture membranes & other reason Prolonged pregnancy >=41 weeks Prolonged pregnancy >=41 weeks & hypertensive disease Prolonged pregnancy >=41 weeks & other reason Prolonged pregnancy >=41 weeks & pre-labour rupture membranes Total
1 .9
1 .9
2 1.7
3 2.6
4 3.5
2 1.7
1 .9
1 .9
17 14.8
27 23.5
1 .9
5 4.3
44 38.3
1 .9
3 2.6
2 1.7
115 100.0
The main reasons for induction at Koorana were prolonged pregnancy (>41 weeks) with hypertensive disease (38.3%), followed by pre-labour rupture of membranes
with a non-reassuring fetal status (23.5%). Post-dates inductions (prolonged pregnancy >=41 weeks), collectively accounted for 46.1% of inductions at Koorana over the triennium of caseload.
Augmentation Labour was augmented for 44 women (6.9% of all pregnancies), which translates to
10.0% of all spontaneous labours in the caseload cohort. This compares favorably to
the baseline cohort augmentation rate (10.9%, n=70 of all pregnancies),
representing a significant reduction of 4% (p<.013)* since the commencement of
caseload.
* Pearson’s Chi-square test for independence, (value 6.158, df=1, p<.013)
54
Analgesia About 60.1% of caseload women with spontaneous or induced labour had some
form of pharmacological analgesia administered. This is lower than the NSW state
average in 2011[3] of 76.2%.
Women in the caseload triennium also had a significantly lower epidural rate (16.1%)
compared to the baseline group (18.1%), (p<.013), a reduction of 4%*, that is
almost half that of the 2011 NSW state average of (30.1%)[3]. In addition to this, 64
(12.4%) caseload women used warm water immersion at BMDAMH as a non-
pharmacological means of pain relief. Use of warm water immersion was not known
about in the baseline cohort.
Birth
Method of birth The total proportion of mothers who had a non-instrumental (normal) vaginal birth
between July 2011 and June 2014 was 68.5%, and 76.4% of mothers had a vaginal
birth. Furthermore, the caesareans section - no labour (elective caesarean section)
rate has declined over the three years of caseload from 16.1% to 10.6%. The
caesarean-labour (emergency caesarean section) rate has remained relatively
constant over three years.
Table 10: Mode of birth for all mothers
Method of birth
2011-2012 2012-2013 2013-2014 Total caseload triennium
N % N % N % N %
Non-instrumental vaginal birth† 132 62.6 155 72.4 148 70.5 435 68.5
Forceps 2 0.9 1 0.5 0 0.0 3 0.5
Vacuum extraction 21 10.0 9 4.2 17 8.1 47 7.4
ALL VAGINAL BIRTHS 155 73.5 165 77.1 165 78.6 485 76.4
Caesarean - no labour 34 16.1 24 11.2 25 11.9 83 13.1
Caesarean - Labour 22 10.4 25 11.7 20 9.5 67 10.6
ALL CS BIRTHS 56 26. 49 22.9 45 21.4 150 23.6
Total 211 100 214 100 210 100 635 100
* Pearson’s Chi-square test for independence, (value 6.236, df=1, p<.013) † This includes non-instrumental vaginal breech births
55
There was a higher proportion of women who had non-instrumental vaginal births
(normal births) since caseload commenced (68.5%), compared to the baseline three
years (63.4%), however this did not reach statistical significance at α<.05 *. There
was however an overall significant increase in the proportion of women having
vaginal births (normal + instrumental vaginal births) after caseload commenced
(76.4%) compared with before (71%)†.
Likewise, a significant reduction was seen in the rate of elective caesarean sections
from the caseload triennium (13.1%), compared to the baseline triennium (19.7%),
p<.001‡. This represents a reduction in the elective caesarean section rate of 6.6%.
There is a non-significant increase in the caesarean section rate after labour started
(emergency caesareans), from 9.1% in the baseline group compared with 10.6% in
the caseload group § . The overall caesarean section rate at BMDAMH has
significantly decreased from the baseline rate of 28.9% to 23.6% since the caseload
model has commenced (p<.034)**.
Table 11: Comparison of mode of birth between mothers in baseline and caseload triennium
Method of birth Total in caseload triennium Total in baseline triennium
N % N %
Non-instrumental vaginal birth 435 68.5 409 63.4
Forceps 3 0.5 8 1.2
Vacuum extraction 47 7.4 42 6.5
ALL VAGINAL BIRTHS 485 76.4 459 71.0
CS- no labour 83 13.1 127 19.7
CS labour 67 10.6 59 9.1
ALL CS BIRTHS 150 23.6 186 28.9
Total 635 100 645 100
It must be reiterated at this point, that the small number of imported Nepean
caesarean sections (23) in the first half of 2014 have not been included in the
analysis of this report. Published perinatal data will reflect a higher elective
caesarean section rate for BMDAMH in the years to come due to this arrangement.
* p=0.055 † Pearson’s Chi-square test for independence (value 4.758, df=1, p<0.029) ‡ Pearson’s Chi-square test for independence (value 10.222, df=1, p<0.001) § p>0.399 ** Pearson’s Chi-squared test for independence (value 4.495, df=1, p<0.034)
56
Importing elective caesarean sections from another hospital, whilst attracting
additional funding for BMDAMH, will inflate the caesarean section rate at BMDAMH,
and detract from any favorable birth rates achieved after January 2014.
Indications for caesareans-no labour (elective) Previous caesarean section/s was the most common indication for caesarean
section, when no labour occurred. Women with a history of 1 x previous caesarean
made up the largest proportion (37.3%) of all elective caesarean sections at
Koorana, followed by 2 x previous caesareans (21.7%), and breech presentations
(10.8%).
Unfortunately, BMDAMH does not offer vaginal birth after caesarean section (VBAC
after 1 x previous caesarean), which has likely contributed to the large proportion of
elective caesarean sections for previous one previous caesarean birth.
Table 12: Indication for caesarean section-no labour.
Indication N %
1 previous caesarean 31 37.3%
2 previous caesareans 18 21.7%
3 previous caesareans 5 6.0%
Failed induction (cervix < 3cm) 2 2.4%
High presenting part 4 4.8%
Breech presentation 9 10.8%
Intrauterine growth restriction 2 2.4%
Macrosomia 5 6.0%
Oblique/transverse lie 3 3.6%
Uterine anomaly 1 1.2%
Previous anal sphincter injury 2 2.4%
Reason not ascertainable 1 1.2%
Total 83 100%
57
Perineal status after vaginal birth The overall episiotomy rate was 3.7%; most of these were done during instrumental
births (76%). Anal sphincter injury* occurred in 2.9% (n=14) of all vaginal births, and
half of these occurred during instrumental births (50%, n=7).
Table 13: Perinatal status of vaginal births, by instrumental & non-instrumental births
Perineal status non-instrumental vaginal births N %
No injury 82 18.9%
Intact/graze 84 19.3%
Episiotomy 5 1.1%
1st degree tear 70 16.1%
2nd degree tear 142 32.6%
3rd degree tear 7 1.6%
4th degree tear 0 0.0%
Other trauma (incl. vaginal wall, cervical & labial tears) 45 10.3%
Total 435 100%
Perineal status of instrumental births N %
Intact, graze, 1st & 2nd * tears 32 64.0%
3rd degree tear (without epis) 5 10.0%
4th degree tear (without epis) 0 0.0%
Episiotomy, no tear extension 11 22.0%
Episiotomy & tear extended 3th* 1 2.0%
Episiotomy & tear extended 4th* 1 2.0%
Total 50 100%
There has been an increase in anal sphincter injury (third and fourth degree tears) in
the caseload triennium (2.9%), compared with the baseline triennium (2.0%) that did
not reach statistical significance†. A slightly higher rate of instrumental births in the
caseload triennium may account for this difference. There was also a non-
significant‡ decrease in the proportion of episiotomies performed in the caseload
triennium (3.7%), compared to the baseline triennium (5.9%).
* Defined by the presence of a 3rd or 4th degree perineal tear, with or without episiotomy. † p>0.356 ‡ p>0.118
58
Post-partum haemorrhage (PPH) The total PPH rate (blood loss >=500mls) was marginally lower in the caseload
triennium (18.6%) compared to the baseline triennium (19.3%), but not significantly
so* . Both cohorts have a much higher rate of PPH compared to comparable
Australian PPH rates (NSW state; 14.3%[3], Ryde caseload midwifery model;
10%[53]).
Table 14: Blood loss at birth
Blood loss at birth N %
Blood loss < 500mls (normal) 517 81.4%
Blood loss 500 to <1000mls 97 15.3%
Blood loss1000 – 1500mls 14 2.2%
Blood loss > 1500mls 7 1.1%
Aggregated PPH (>=500mls) 118 18.6%
An estimation of blood loss > 500mls occurred in 44.7% of all caesarean births, and
10.6% of all vaginal births.
Table 15: Blood loss at birth, vaginal v’s caesarean births
Blood loss at birth All Vaginal births All Caesarean births
N % N %
<500Ml 432 89.4 83 55.3
>=500<1000Ml 39 8.1 58 48.7
>=1000Ml<=1500Ml 8 1.7 6 4.0
>1500Ml 4 0.8 3 2.0
Total 483 100.0 150 100.0
AggregatedPPH(>=500mls) 51 10.6 67 44.7
Babies
Gestation The proportion of babies born after 40 weeks gestation increased by almost 25%
since the caseload model commenced. Babies born over 40 weeks gestation
significantly increased from 20.9% in the baseline group, to 44.8% in the caseload
* p>0.716
59
group (p<.001)*. A small drop in the induction rate for women in the caseload
triennium can only partially account for this; as women are not being induced as
readily before 40 weeks gestation throughout the caseload triennium, resulting in a
higher proportion of babies being born after 40 weeks. The proportion of pre-term
births (2.6%-3.1%) has not changed significantly over time.
Table 16: Gestational age groupings
Gestational age
group
Baseline triennium Caseload triennium
N % N %
20-29 weeks 1 0.2 2 0.3
30-36 weeks 19 2.9 14 2.2
37-40 weeks 491 76.0 330 51.9
> 40 weeks 135 20.9 285 44.8
Not known 0 0.0 5 0.8
Total 646 100 636 100
Birth weight There was little difference in the birth weights of babies across both trienniums. The
proportion of babies weighing over 4000 grams was higher in the caseload group
(15.3%), than the baseline group (13.6%), however not significantly so†. Categorical
birth weight groupings are used for comparison, because individual weight data as a
continuous variable was not available for birth weights of babies in the baseline
cohort.
Table 17: Birth weight categories of infants Birth weight categories Baseline triennium Caseload triennium
N % N % < 2499 grams 13 2.0 13 2.0 2500-3999 grams 545 84.4 526 82.7 > 4000 grams 88 13.6 97 15.3 Total 646 100 636 100
Live births There were four stillbirths in the caseload triennium compared to one stillbirth in the
baseline group. Three stillbirths were associated with fetal and chromosomal * Pearson’s Chi-square test for independence (value 83.197, df=1, p<0.001) † Chi2 p>0.407
60
anomalies (one of these was a Cervagem termination at 20.4 weeks), and one
stillbirth was associated with fetal demise in second trimester (at 26 weeks). There
were no stillbirths or perinatal deaths attributable to labour in the caseload triennium.
Reason for the one stillbirth in the baseline triennium is not known. The difference in
stillbirth rates between groups was not statistically significant*
Table 18: Live birth and perinatal death rate
Perinatal deaths Baseline triennium Caseload triennium
N % N %
Live born
surviving
645 99.8 632 99.4
Stillbirth 1 0.2 4† 0.6
Neonatal death 0 0.0 0 0.0
Total 646 100 636 100
Apgar score Apgar scores are an indication of a baby’s condition shortly after birth, an apgar
score of less than 7 at 5 minutes after birth is considered to be an indicator of
complications and compromise for the baby.
There were half as many infants born with a low 5 minute apgar score in the
caseload triennium (n=7, 1.1%), compared to the baseline triennium (n=14, 2.2%),
After controlling for fetal demise prior to the onset of labour (these 5 minute apgar
scores are recorded as ‘0’), there was a significant improvement in the 5 minute
scores of babies born in the caseload triennium, compared to the baseline
triennium‡. One baby with a low apgar score in 2013, died > 28 days, and is
therefore not recorded as a perinatal death, this case was followed up in a root
cause analysis (RCA).
* p>0.173 † 1 stillbirth in June 2013, 20.4 week termination for severe cardiac defect. 1 fetal demise prior to labour, stillbirth Apr 2012 at 36.6 weeks, with birth defect. 1 fetal demise prior to labour (lack of fetal movements felt on admission), stillbirth Nov 2012 at 26 weeks, no birth defect. 1 fetal demise prior to labour, stillbirth Sep 2013 at 37.4 weeks with chromosomal abnormality. ‡ Chi2 value 6.157, df=1, p<0.013
61
Admission to nursery There were 40 (6.3% of babies) nursery admissions in the caseload triennium; four
of these were NETS transfers. General nursery admission data is not available for
the baseline cohort, however there were 21 (3.2%) neonatal transfers out of the unit
in the baseline triennium. This represents a reduction in the proportion of babies
requiring transfer to other hospitals in the caseload triennium.
Postnatal
Breastfeeding In the caseload triennium, 92.1% of infants were receiving breast milk on discharge
from hospital, this includes 3.4% of women who were mixing breast milk and
formula. 84.7% of the caseload triennium babies were exclusively breastfeeding, and
only 7.1% of infants who were exclusively formula fed on discharge. Similar data
was not available for comparison with the baseline group, however the caseload
group compares favorably to NSW state exclusive breastfeeding rate of 82.1% in
2012[51].
Length of stay after birth The average length of postnatal stay for women in the caseload triennium was 2.2
days [SD 1.7], ranging from 0 to 13 days.
Home visits The average number of days that caseload women* remained in caseload care
following discharge from hospital was 11 [SD 5.2], ranging from 1 to 37 days. This
average is just less than two weeks of continuity usually by their primary midwife
following discharge.
* “Caseload women” are a proportion of the caseload triennium cohort, caseload clients make up approximately 76% of the caseload triennium.
62
WHAT THE MIDWIVES SAY
Attitudes to Professional Role (ATPR)
Caseload and core midwives satisfaction with their roles, was assesses through the
administration of an ‘Attitudes to Professional Role’ (ATPR) questionnaire (Appendix
3). Six caseload, and six core midwives (permanent staff) completed questionnaires
in September 2014. The questionnaire was developed by Turnbull et al (1995), and
is comprised of 20 questions measuring four domains of satisfaction; professional
satisfaction; professional support; client interaction and professional development.
The questions are presented as completed statements across a five point Likert
scale. The available responses range from ‘strongly agree’ (mean scale score of =
2), to ‘strongly disagree’ (mean scale score = -2). These are graphically represented
in the figures below.
Professional satisfaction
Caseload midwives consistently affirmed a degree of satisfaction with their work,
whereas core midwives on average, indicated less satisfaction with their role by
agreeing with the statements about feeling frustrated with their role, and feeling ‘in a
rut’, despite on the whole agreeing with the statement about role satisfaction.
63
Caseload midwives feel they have more opportunities to make decisions about care
than core midwives, however core midwives scored slightly higher in perceiving a
degree of professional independence. This could be a result of job expectations (i.e.
a caseload midwife may be more likely to expect more professional independence
than core midwives as a function of their role.) Both groups generally agreed they
had enough opportunities to make decisions about the care they provide women.
Professional support
Caseload and core midwives had similar responses in the support domain, reporting
the highest level of support from other midwives. Core midwives were slightly more
likely to feel more support from obstetric colleagues than the caseload group. Both
groups felt a small deficit in managerial support. There was a marked difference
between caseload and core midwives perception of ‘enough time to do my job
properly’, with core midwives feeling they have enough time for their work. Both
groups disagree with the statement about their work being stressful.
64
Client interaction
Both groups scored similarly with being able to provide women with a choice about
care, interestingly core midwives scored slightly higher on this measure. Both groups
felt they had enough opportunities to give personalized care to women, which is
probably reflective of the size and pace of the unit, resulting in less time pressures
for midwives as a whole. Likewise, both groups felt they had enough time to give to
women, with core midwives indicating this to a stronger degree. Caseload midwives
agreed strongly with feeling they could plan care with women. As expected, there
was a large discrepancy in the way groups perceived ‘opportunities to provide
continuity of care to women’, in accordance with being in a continuity of care role
(caseload) or not. On the whole, both groups of midwives were satisfied in the
domain of client interaction.
65
Professional development
Caseload midwives felt they had more opportunities for professional development
than did their core midwife counterparts, as well as the opportunity to develop
midwifery skills in the course of their work. Both groups were confident they had the
midwifery skills for their current role, with caseload midwives being highly confident
of their skills in this domain.
Industrial Agreement Questionnaire (IQ) Caseload midwives (n=6) completed an Industrial Questionnaire (IQ) (Appendix 4)
which was based on an Australian Nursing Federation (ANF) IQ used in the
evaluation of the Midwifery Group Practice (MGP) at the Women’s and Children’s
Hospital in Adelaide. The IQ asked about hours worked, being on call, the
manageability of caseload, days off, and professional supervision and support. The
document was circulated to Koorana unit caseload midwives in September 2014.
Freestanding quotes derived from text have been de-identified, and are presented in
italics, verbatim.
The results and key themes emerging from the IQ are discussed in this report.
Where available and appropriate, caseload quantitative evaluation data reported on
in the last section is used to contextualize and support themes emerging from this
questionnaire.
66
Work hours Half (3/6) of the caseload midwives reported routinely, working over and above the
required hours. Reported hours accrued, ranged from ten to fifty in addition to their
full-time equivalent (FTE). One midwife commented that it had not been possible to
claim back her hours over several months.
On call There was a variation in the number of days on-call reported by midwives, from three
to six days a week. The average number of days OFF-call was 3.7, meaning that
caseload midwives report being on-call for about half of their working week.
Midwives, who reported being on-call for more of the week, were more likely to be
present for the births of their women.
Four midwives (4/6), responded to the question about being called or texted after
hours to give considered advice. The number of calls/texts received ranged from
two-ten per day (after hours), and the number of times midwives are typically woken
up on average a week ranged from one-five times.
Yearly caseload The annual caseload was reported to be between three and four women a month,
depending on part, or full time work. Taking into account the annual leave of six
weeks per year, plus two additional weeks when midwives would not be booking in
women before and after leave, annual caseloads are as follows:
• Full time midwives take 4 women a month for 10 months a year = 40 women
a year.
• 0.8 FTE midwives take 3.5 women a month (4 women one month & 3 the
next) for 10 months of the year = 35 women a year.
• 0.7 FTE midwives take 3 women month for 10 months = 30 women a year.
For the final twelve months of the evaluation, there were five full time midwives (one
only for six months of the year) and 2 part-time midwives (1 x 0.7 & 1 x 0.8 FTE).
Therefore the capacity of the Blue Mountains caseload service, based on staffing
throughout the 2013-2014 year is calculated to be:
40 + 40 + 40 + 40 + 20 (fulltime midwife for 6/12 effectively) + 35 + 30
67
= 245 women
The number of women booked, and cared for by the service in 2013-2014 was 239,
which represents a gap of only 6 women. Any shortfall in workload this might
represent, has been taken up by the additional non-caseload births and bookings
that caseload midwives provide, and filling gaps in the core midwives roster. 16%
(n=39 women), of all caseload women did not birth at Blue Mountains hospital, due
to risk or other factors.
Caseload manageability Most caseload midwives (5/6) felt that their caseload was not always manageable
throughout the year. In particular, unmanageability was a characteristic of work in
the following circumstances:
• Unplanned & unexpected absences of other caseload midwives (described by
5/6 caseload midwives)
• Core midwife shortages & sick leave, covering ward (described by 5/6
midwives)
• Other caseload midwives annual leave (described by 3/6 midwives).
Midwives generally book women in for antenatal appointments on a day they are
working. If women birth whilst their primary midwife is on a day off or on leave, the
on-call midwife attends this birth, as well as any antenatal or postnatal visits that the
primary midwife cannot attend to. The use of core staff to do antenatal appointments
was also cited by one midwife, as an alternative arrangement to the on-call caseload
midwife.
Five out of six caseload midwives said they were satisfied with this arrangement.
Most midwives felt they were able to request days off as desired, and would let their
colleagues know if they were available to attend the care of their woman in labour,
whilst on a day off. One midwife says:
“I mostly respond to the needs of the women, I do my best to get a day off”.
68
Implying a sacrificing of the midwife’s personal time, to meet the needs of the
women in labour. All of the midwives indicated that they were satisfied with the way
they structured their workload to get days off.
Continuity of care 50% (3/6) of caseload midwives said they were satisfied with the level of continuity
they could offer women, and 50% (3/6) were not satisfied with this aspect of care.
Continuity of care satisfaction by midwives was associated with their individual birth
continuity statistics. All midwives who had a continuity of care at birth rate < 60%
reflected their dissatisfaction with the response to this question. Whereas, the other
half of midwives (with birth continuity rates > 60%) said they were satisfied with the
continuity they could offer.
Comments given in relation to reduced continuity were:
“Staff shortages diminish the flexibility to attend births.”
“Using our time to meet the needs of core women, and women not on my
caseload means I cannot be with my women during their labour and birth (my
time has been used up already!)”
“I would like to offer more continuity, however the demands of the role often
lead to long work-hours, and days off are essential!”
Comments given in relation to higher continuity:
“I choose to, & am able to come in for a birth when not rostered on”
Professional supervision & Support In regard to professional supervision and support, the midwives were asked to
comment on management, peer and other support, as well as professional
development. The comments are summarized below.
69
Management: 2/6 midwives perceived management as a source of support.
Peer Support: 5/6 midwives felt supported by other midwives,
“I have learnt most of my skills from my fellow midwives, ad hoc, asking
questions and observation of their practice”
Other support: 2/6 midwives mentioned clinical supervision, and self-directed
support and learning.
Professional Development: All midwives listed external conferences and courses,
they had attended over the past year, as well as midwifery mandatory training
(K2MS, FONT). 2 /6 listed ‘M & M meetings’. Staff in-services were mentioned once
as an avenue for professional development.
Midwives suggestions for change Most midwives (4/6) volunteered additional comments about their working conditions
and aspirations for change, these centered on issues of staff shortages, and the
configuration of the midwives as a group. Caseload midwives consistently describe a
compromising effect on continuity of care, by filling core-staff roster shortages.
“I feel that meeting the needs of women in a continuity of care model is
hampered when we are on call so much, and have to fill gaps in the ward roster.”
Larger metropolitan hospitals typically use casual midwifery pool, and agency staff
for this purpose, and the regional location and size of BMDAMH, poses staffing
challenges in specialist areas such as midwifery. These appear to have been
managed over the past three years of the report, by using the caseload midwives as
a quasi-casual workforce for the maternity services in the Koorana unit.
The benefit of this has been the absence of service interruptions due to midwifery
shortages since caseload commenced. Prior to the caseload model, the Koorana
unit was “closed” during midwifery staff shortages, resulting in women being
70
transferred to Nepean hospital at short notice, or birthing in the emergency
department of BMDAMH with no midwife in attendance. Disruptions to continuity of
birth-care, has been the cost of using caseload midwives to cover the ward. This
essentially erodes the purpose and integrity of the model over time.
Another issue that crystalized from the comments of the questionnaire is how the
model itself is organized to provide continuity of care to women.
“We are not offering true caseload, except when the caseload midwife comes in
in her own time to be with her women (& then accrues too many hours on
timesheets)”
Some midwives state a preference for working in smaller ‘teams’, to concentrate
continuity of care between a few midwives, and a general dissatisfaction with the
structure of the current model.
“I feel the model of care we are offering with a caseload of 6 midwives is
becoming cumbersome, better to offer 2 small MGP's in 3 mw's, which would
enable the women and midwives to know each other better, so there are no
surprises when a women goes into labour & meets a new midwife”.
And…
“Would like 2 teams, to meet all women in teams & achieve continuity as a group”
And…
“I would like to work in a smaller team, be on-call more to increase [continuity of
care] with a smaller group of women.”
It is interesting to note that working in smaller groups, is how the model was initially
envisaged and proposed by stakeholders[2].
Reasons for the current configuration of six to seven midwives who provide on-call
care for all women are not known. Anecdotally, the reasons seem to be related to a
long lag-time between initial proposal and implementation of the service (two years),
71
followed by a hasty set up, without adequate staffing or a local project manager in
2011. The conditions affecting the set up and configuration of the service in 2011
have likely stabilized over time, however organization of the model, have persisted
into 2014.
Four of the six midwives expressed a desire to change the configuration of the
group, to improve continuity outcomes.
“I'm keen for a working party to discuss change in the team structure of caseload,
i.e.; smaller teams & hearing midwives experience working in different models of
[caseload] care”
Discussion Midwives indicated they were satisfied with various aspects of working in the current
caseload model such as; arrangements for covering other midwives work whilst on
days off, and having the flexibility for desired days off. Half of the midwives were
satisfied with the level of continuity they could offer women, and half were not, and
this reflected the ability to attend to women’s births on their days off. Midwives who
could attend births on days off-call, were generally more satisfied with the continuity
component of their work.
Midwives receive the highest amount of professional support from each other, and
are satisfied with the degree of professional development they can engage in. The
IQ has highlighted some areas of dissatisfaction and opportunities for further
engagement, namely; lack of management support (although what this means is
unclear), filling gaps in the core staff roster, and the configuration of the caseload
model itself.
72
WHAT THE WOMEN SAY – SURVEY RESPONSES
Methods Aims
To report on the ‘patient satisfaction survey’ responses returned from women who
received care at the Koorana maternity unit between January 2012 and June 2014.
To describe the aspects of care that women liked, as well as what they were
dissatisfied with, particularly in regard to their experience of caseload midwifery care.
Survey
The Women and Children’s Health Unit satisfaction survey instrument was designed
to elicit feedback from women about the quality of maternity services offered at
BMDAMH. The survey was designed by Koorana unit staff in 2012, however little is
known about the rationale used in the design of the questions, but it is thought to be
modeled on an earlier, pre-caseload survey instrument in the unit that was rarely
used. Most questions in the survey relate to the women’s experience of maternity
care as a whole, and not particularly to caseload or midwifery care.
The survey is essentially comprised of 22 dichotomous questions (yes/no response),
with 14 short comment segments (see appendix 4). It asks about model of care, (and
if this was a choice), information received though pregnancy birth and postnatal
period, information received about the scope of services at the hospital, value of
education provided in parenting classes (both at the hospital and privately), quality of
education form midwives and doctors, confidence going home, caseload midwifery
support throughout the woman’s journey, breastfeeding support and information, and
other external sources of support.
Questions are weighted towards the woman’s satisfaction with the ‘information’ she
was given on her journey through the service, rather than the satisfaction with the
‘care’ she received. Despite this, most women made valuable and specific
comments pertaining to care they received from midwives, but often the word ‘staff’
was used by respondents, making it difficult to distinguish whether they meant
caseload midwives, core midwives, doctors, management or administration staff in
73
some cases. There was only one question in the survey that asked specifically about
satisfaction with caseload midwifery care, which most women responded to
extensively in comparison to other questions asked.
Another limitation with the survey design is the inappropriate response options for
complex and multifaceted questions, such as: “Did you receive the information you needed to make informed choices in relation to your pregnancy, labour and birth and postnatal care?” YES/NO
Many women answered, “YES” and “NO” to questions like this, which raises many
more questions about their experience, but renders the response invalid when
quantifying satisfaction according to dichotomous response criteria.
A section of the survey focuses on parenting classes, and education sources for
women that are largely external to the unit. Responses to these questions were
scant, but are included here nonetheless in summary form. The questions relating to
infant feeding were problematic, without a reference date for when the survey was
returned; “…are you still breastfeeding your baby? YES/NO”, is meaningless for the
purpose it was intended for without a reference to when the form was completed in
relation to the baby’s birth.
The structure of the survey invites women to express their satisfaction via ‘yes’
responses to the dichotomous questions, and reserve the comments section for
criticisms, which are sometimes aimed at a specific issues or staff members rather
than the service at as whole. A wide array of critical comments can be useful, and
indicate that a degree of appreciation bias has been avoided inadvertently in the
design of the study.
Data collection
The survey was posted to an unknown number of women at the end of 2012, and
returned 48 completed responses. These were stored in an office in the maternity
unit for 18 months until plans for an evaluation of the service were commenced. It
was thought that the 48 returned surveys were not representative of all women’s
satisfaction with the service (the caseload model was not fully staffed in 2012, and
unstable management affected the unit’s operations, which was reflected in women’s
74
comments). In order to report on women’s satisfaction with the service running at full
capacity (2013-2014), another mail-out of 336 surveys (with an accompanying cover
letter) followed in June 2014 for all women booked into the maternity unit between
January 2013 and June 2014. This returned another 71 completed surveys, a
response rate of 21% for the years 2013 and 2014. Many surveys were returned
unopened due to women relocating in the time between the birth and when the
survey was sent out. The responses in 119 returned surveys are therefore reported
on in this section of the report.
Ethical considerations
Return of a completed survey was taken as consent. Confidentiality was maintained
throughout the evaluation process, and demographic data collected in the survey
was separated from responses. No responses have been linked to particular
individuals.
Findings
The women 34% of all respondents were having their first baby at the time they completed the
survey, which is similar to the proportion of primiparous women who birthed at
BMDAMH in this time (38%). The majority of respondents (86.6%) had received
caseload care, followed by a smaller proportion receiving obstetric care (10%), and
only two respondents received core midwifery care (1.7%). Two responses came
from women in 2012, who received midwifery antenatal care at Nepean, but were
obviously also cared for at the BMDAMH. There were four respondents who also
circled GP Shared care in conjunction with either caseload, obstetrician or hospital-
based midwifery care, and these responses were absorbed into the primary care
category.
Table 19: Respondents according to parity, per birth year.
Parity 2012
(12 months)
2013
(12 months)
2014
(6 months)
Total
Primiparous 16 (33%) 19 (35%) 5 (31%) 40 (34%)
75
Multiparous 32 (66%) 36 (65%) 11 (69%) 79 (66%)
Total 48 (100%) 55 (100%) 16 (100%) 119 (100%)
Model of care
Respondents (particularly in 2012) often circled multiple options for “Which model of
care did you receive during your pregnancy?” making classification problematic.
Respondent’s names and baby’s birth dates were cross-checked with the
quantitative birth data, to ensure respondents were categorized properly in this
respect. Respondents receiving caseload model care were more likely to know they
were caseload clients by the second half of 2013 and into 2014. Some women may
have thought that they were recipients of “Hospital Based Midwifery Care” when in
fact they were “Caseload Midwifery Care” clients, due to the ambiguous wording in
the question (caseload care is also provided by midwives in hospital). It is possible
that fluxuating-staffing levels in 2012 may have contributed to confusion about who
the lead maternity carer was for women. It is also possible that the distinguishing
features of the caseload model of care were not made explicit to women until 2013-
2014.
Table 20: Respondents according to model of care, per birth year.
Model of care 2012
(12 months)
2013
(12 months)
2014
(6 months)
Total
Caseload model 37 (77%) 50 (90.9%) 16 (100%) 103 (86.6%)
Obstetrician model 9 (18.8%) 3 (5.5%) 0 12 (10%)
Hospital based midwifery 0 (0%) 2 (3.6%) 0 2 (1.7%)
Antenatal care at Nepean 2 (4.2%) 0 (0%) 0 2 (1.7%)
Total 48 (100%) 55 (100%) 16 (100%) 119 (100%)
Did women choose their model of care?
When asked; “Was the model of care you received chosen by yourself or were you
allocated care?” 50% of caseload clients indicated that they choose that model of
care, and 50% said they were allocated into caseload. Out of the 12 women
receiving obstetric care, 4 (33%) indicated they chose that model, and 8 (67%) were
76
allocated. All four women in hospital base midwifery (core staff at BMDAMH and two
at Nepean), indicated that they choose their model of care. The proportion of women
choosing caseload care for themselves increased from 46% in 2012 to 69% in 2014.
Reasons for choice or allocation to a model of care.
41 (34%) Respondents commented on the reasons given for their allocated model of
care. For obstetric care, women referred to themselves as being ‘high risk’, and
having had previous caesarean sections as being the main reason they were
receiving obstetric-led care:
“I previously had two emergency c-sections so I was told that I had to have a planned c-section and see the doctor every time”. (Obstetric care 2012)
One respondent chose obstetric care because she did not want a postnatal early
discharge (often associated with caseload midwifery care):
“I chose obstetric care as I could stay in hospital after birth” (Obstetric care 2012).
On occasions, convenience was a factor for women, depending on how the clinics
were organised .
“We booked too late so no caseload option was available. Also, visiting my doctor was easier than time slots for hospital visits due to working 5 days/week prior to birth” (Hospital midwife care, & GP Shared care, 2013)
Caseload clients generally indicated that; “Caseload was standard at this point in
time” (Caseload, 2012). Other women responded with similar comments that reflect
the change in service provision at the Koorana unit:
“Hospital was changing the model of how midwifery care was being provided” (caseload, 2012)
“Was allocated caseload, not upset by it though. It was wonderful” (caseload 2013)
There were also two women who indicated that they chose BMDAMH due to the
availability the caseload service:
“We changed to Katoomba from Nepean to receive better care and a caseload midwife” (caseload, 2013)
77
Satisfaction with information - Enabling informed choices
94% of caseload clients indicated they received enough information to make
informed choices in relation to pregnancy, labour and birth care. Women were
generally very satisfied, and the majority of comments reflected satisfaction:
“All the midwives were very knowledgeable and more than happy to give me all the information I needed” (caseload, 2013)
The few negative comments centred on a perceived lack of information on specific
aspects of care that women felt unprepared for, such as:
“Everything was great but I was uninformed with enough time to know the possible outcomes of a failed induction.”
All Obstetric care clients indicated that they had received enough information, and
none commented further on this aspect.
Satisfaction with the information - About the scope of services available at BMDAMH
86% of caseload clients and 64% of obstetric clients indicated that they were given
information about the scope of services available at BMDAMH and there were no
comments related to this.
Were women’s wishes and needs respected and met by the service? Caseload: 95% (89) of women who responded to being asked if their wishes and
needs were respected and met by the service agreed, and 5% (7) women did not.
Obstetric: 73% (8) of women who responded to this question agreed that their
wishes and needs were respected.
Hospital based midwife: 3 out of 4 women agreed with this question.
Specific comments made by women who did not feel satisfied in this regard are
incorporated into main comments themes below.
Did women attend parenting classes? 27 (23%) of caseload clients indicated that they had attended some form of
parenting classes, as well as one obstetric care, and one hospital midwife care
client. All comments relating to the BMDAMH parenting classes were positive.
78
Calmbirth© classes were the most commonly cited private birth preparation method
used by women (6 women), who did not attend hospital birth classes. 100% positive
comments were expressed in relation to this.
Did women value antenatal information given by midwives or doctors? This question was categorized along with the value of hospital based and private
education. It asked respondents to comment on the value of education they received
from their midwife or doctor, and 38 (32%) of women made comments. 32 (84%) of
these comments were very positive. The minority of criticisms that were made,
centred around a lack of, or conflicting information given:
“The midwife gave me contrary information to the hospital doctor. I was left confused up to the last minute which I was very unhappy about” (Caseload, 2012)
AND
“Unless you knew the questions to ask, info wasn't freely given” (Caseload, 2012)
There were also three critical comments about communication from doctors:
“I found ALL doctors bar one to be very poor listeners and communicators” (Obstetric care 2012).
The responses to this question generally became more positive over time, with no
critical responses to the question after April 2013. Women usually expressed
accolades for their own midwives after this time, naming their primary midwife and
expressing gratitude for information given in the majority of cases:
“My midwife [X] was great. Always made my partner & I feel we could ask her anything and call or text her anytime. She gave us lots of info and answered all out questions in depth” (Caseload, 2013).
“[Y] was perfect, even supplied books and DVD and information sheet on acupressure” (Caseload, 2013) “[Z] was full of knowledge & discussed all our questions in depth” (Caseload, 2014)
79
Caseload care – did women feel supported by their midwife? This question asked women to indicate if they felt well supported by their caseload
midwife during the antenatal period, labour and birth, and at home. Separate yes/no
answers were linked to the three categories, which are reported in table form below.
Table 21: Caseload women responses to feeling well supported by caseload midwife, per stage of
maternity care
Caseload clients Felt well
supported Did not feel
supported
Did not
respond
Total
caseload
clients
Antenatal period
92 (89%)
92%*
8 (8%) 3 (3%) 103 (100%)
Labour and birth
93 (90%)
93%*
7 (5%) 3 (6%) 103 (100%)
At home
96 (93%)
96%*
4 (4%) 3 (3%) 103 (100%)
The proportion of women who felt supported by their caseload midwife was high
(>90%), especially once the women got home (96% felt supported). Survey
response data was linked with continuity of the primary midwife at birth data, to see if
the presence of the women’s primary midwife at birth had an effect on her
satisfaction in labour and birth (see table 22).
Table 22: Proportion of women who felt supported in labour and birth, according to whether their primary midwife attended intra-partum care. Felt well
supported in
labour & birth
Did not feel
supported in
labour & birth
Did not
respond
Total†
Primary midwife present at
birth
44 (89.8%)
95.7%*
2 (4.1%) 3 (6.1%) 49 (100%)
Primary midwife NOT present
at birth
43 (89.6%)
89.6%*
5 (10.4%) 0 (0%) 48 (100%)
* Amended proportion, excluding non-responses to the question. † Continuity at birth (of primary midwife) was known for 97 out of 103 caseload clients who returned surveys
80
Having the woman’s primary midwife care for her in labour and/or birth had a small
positive effect on women’s perception of support in labour and birth. Women who did
not have continuity of care (by their primary midwife) at birth still felt supported in
89.6% of cases, and this increased to 95.7% when the primary midwife was able to
attend.
68 (66%) of women made additional comments specific to the support they received
or did not receive from caseload midwives. The comments are incorporated into
themes in the next section, however the frequency of positive and negative
comments in relation to each each stage of maternity care are presented in table 23.
Table 23: Numbers of positive and negative comments according to stage of caseload maternity care.
Antenatal
care
Labour & birth
care
Postnatal care at
home
Not specific to
any stage
Total
Number positive
comments
15 20 23 20 78
Number of criticisms 9 8 4 0 21
Women had the most praise for postnatal care at home, which is consistent with
postnatal satisfaction levels expressed in table 20. Women on the whole were highly
appreciative of this aspect of the service:
“Unlike my first experience with home visits post-delivery, I felt very comfortable with [X] visiting once we were home from the hospital. She was relaxed and diligent and managed to ease my anxiety regarding my new baby. The whole experience was very positive” (Caseload, 2013)
Comments that were critical of postnatal home care described a relative lack of it:
“We didn't have any major problems with our baby once returning home however we really noticed the lack of visits compared to our other child. We had a visit on the 2nd day home then didn't get another visit for a week. Thankfully everything went fine, it appears from the outside that the caseload midwife program is a little understaffed?” (Caseload, 2014).
Women responded with a majority of positive comments about labour and birth
support. Comments relating to this aspect of care were largely around the availability
of midwives, both the woman’s primary midwife, as well as the on-call midwife:
“It was good that I could see the same midwife at every visit at the hospital and made a special connection to her. At the labour, even though she was
81
not on duty, she came for my birth. I felt relieved when I saw her, thinking this pain would be over soon and could see my baby soon” (Caseload 2013). I loved my caseload midwife - however she was not there for my inductions and it was emotionally hard having strangers coming in. She was present for the birth and gave excellent antenatal & postnatal care. Worth her weight in gold!! (Caseload, 2013)
“When I was in labour I was instructed to ring my midwife mobile. Which we discovered later was turned off and in a draw, because I hadn't been told that my midwife's leave had ended or given a new number to ring. I was VERY UPSET when I GOT IN TROUBLE for ringing the landline number to contact the midwives when they failed to ring me back after leaving messages all day during labour”. (Caseload, 2012)
Antenatal care attracted slightly less praise and more criticisms from women than
other stages of maternity care. Positive comments related to information shared by
specific midwives (the woman’s primary midwife), and a perceived respect of
choices made by the woman.
“I found caseload midwifery to be a really positive experience. You were able to get to known your assigned midwife and they knew you and your needs / wants. It is really nice not to have to relay information over and over to different people” (Caseload, 2013).
“My midwife, [X] gave me the most thorough and sensitive care. She fully supported my choices and was able to inform me about anything I was unsure or concerned about” (Caseload, 2014)
Criticisms made about caseload antenatal care varied in nature. Women’s
comments centered around not perceiving that her choices were respected in the
antenatal period, and antenatal visits being disorganized and inconvenient for
women. As in labour and birth care, women were critical of the means of
communicating with midwives, when they did not get a response.
“….the method of contact i.e. text only, was absurd and resulted in days between requesting appointments and a getting response”. (Caseload, 2013) “The caseload midwife was terribly unorganised never had the right paperwork or left it behind whilst fetching something else. This was frustrating as I had my toddler and very busy husband at the appointment”. (Caseload, 2012)
82
“I left all my midwife appointments being made to feel bad or inadequate for feeling the need for an epidural after 2 previous births and experiencing both. I feel my opinions were constantly brushed over”. (Caseload, 2013)
Other comments made were incorporated into main themes, and reported on below.
The postnatal period
Did women receive adequate information about the postnatal period? 94% of caseload clients and 75% of obstetric clients indicated satisfaction with the
information given about the postnatal period. 24 women made mostly positive
comments in relation to this question, and any criticisms centered around conflicting
breastfeeding advice: “Very conflicting and confusing advice on breastfeeding while in hospital.” (Caseload, 2012)
Did women feel confident about going home with a new baby? 96 (93%) of caseload clients and 11 (92%) of obstetric clients answered ‘yes’ to the
question about feeling confident to go home with their new baby. 40 women made
comments about this aspect, 18 (45%) of women made comments that were critical
of early discharge arrangements, such as: “I did not receive enough support in the hospital, I was just shipped out” (Caseload, 2012).
What method of infant feeding did women choose? 95% (96) of caseload clients indicated that they choose to exclusively breastfeed
their baby, another 3% (3), chose to combine breastfeeding and bottle-feeding, and
only 2% (2) women choose to only bottle-feed their baby.
Did women feel supported with, and informed about their choice of infant feeding? All women (100%) regardless of the model of care received answered ‘yes’ to the
question; ‘Were you supported with and given enough information to support you
choice [infant feeding]?’ Despite this, several comments were made about
breastfeeding advice in hospital: “All midwives had a different 'styles' & were rather forceful with the first days of learning to breastfeed”. (Caseload, 2013)” “The very first midwife I saw who took all my details told me because I had a boob job I wouldn't be able to breast feed. SO NOT TRUE!!” (Hospital-based
83
midwife 2012) “Each midwife that came in gave different advice - this was often quite upsetting for a first time mum”. (Caseload, 2014) “Of course! This [breastfeeding] was advocated to no end!” (Caseload, 2012)
Conflicting breastfeeding advice was a common theme for women who made
comments about their experience of the postnatal period in hospital.
How long did women breastfeed for? 67 (56%) of all women indicated they they were still breastfeeding, but unfortunately
there is no reference date for many returned surveys, so this is difficult to interpret.
However 34 women indicated how old their baby was when weaned from
breastfeeding, which averaged 10 months, and ranged from 1 to 15 months in
duration.
Did women receive adequate information about community supports? 100 (84%) of all women indicated that they did receive relevant information about
community supports. Women specifically mentioned the ‘community nurse’, ‘local
parenting groups’, ‘face-book parenting group’ and ‘group from hospital antenatal
classes’. There were no criticisms in relation to this question.
Women have their say – Themes of importance Comments that were made in response to being asked; “Please feel free to add any
comments about your experience” and “Do you have any suggestions to help us
improve our service?” are organized here into common themes. Respondents also
made qualitative comments throughout the survey in relation to other questions that
have been incorporated into the themes below. Comments have been organized
mostly into in vivo themes that were derived from the most frequent and consistent
comments made, these are: Continuity and connection, offer VBACs, it was much
easier birthing in water, don’t rush to kick mums out of the ward, and the staff need
to be cared for.
84
Continuity and connection
This theme relates to women’s experiences of the connection (or disconnection) with
their primary midwife, and encompasses many eclectic views and experiences in
relation to continuity. Women’s appreciation for the caseload midwifery service was
expressed again and again (comments provided in ‘bubbles’, next section). This
theme relates to other, less positive dimensions of the continuity of care experience,
such as when the woman does not connect with her primary midwife: “I didn't feel I connected with my midwife, I didn't feel I could ask to change as I was a public patient…. I’m glad I had another wonderful midwife when I went into labour” (Caseload, 2013) “I was happy with my midwife caseload care, but would like to suggest that sometimes women my wish to swap midwives if they don't 'connect' with the midwife”.
“The midwife I was allocated often seemed distracted and made comments that she did not wish to be working, I felt this was unprofessional. As a result I was glad to have other midwives care for me through labour and the postnatal period”. (Caseload, 2014) “The caseload service is wonderful in theory but only works where the patient and midwife can form a positive relationship. This required commitment and professionalism on the part of all midwives involved in the program.” (Caseload, 2014)
Women also wanted a degree of connection and familiarity with the midwife who
would be caring for them in labour: “Even though it was nice to have a caseload midwife and see only one person it would have been good to get to know the other midwives better as well. My midwife who I saw throughout my pregnancy couldn't be there at the end due to unforeseen circumstances so I had another midwife who I wasn't that familiar with. Maybe if I could have seen some of the other midwives and gotten the chance to know them a little better it would have been a bit better” (Caseload, 2013) “I think the old service was better. I think it's more isolating having one midwife. With the old system you had a better chance of meeting the midwife who will attend your birth”.(Caseload 2012)
Women valued for the most part, having their primary midwife care for them in labour, and perceived that this improved their birth outcomes:
85
“I would have preferred to have my midwife during labour but she was managing the ward. I think having 2 midwives that I had not met before slowed my labour.”(Caseload, 2012) “Caseload midwife did not attend start of labour. First midwife was not as experience and labour was prolonged. The next shift the caseload midwife attended and improved the labour. If it is a true caseload midwife ideal if they are called for the labour / birth.” (Caseload, 2013)
Women emphasized the value of a having a good ‘connection’ with their primary
midwife, and being able to change midwives if a friendly connection was not
established. Women value someone who is known to them in labour, and this
continuity can be tied into perceptions of clinical outcomes for the woman.
Offer VBAC’s
The frequency and consistency of comments about vaginal birth after caesarean
section (VBAC), necessitated including it as a separate theme. Women who have
had a previous caesarean section, explicitly desire the opportunity to try for a vaginal
birth at BMDAMH next time. At the moment this option is not offered at BMDAMH,
and women are required to travel to Nepean hospital to try for a VBAC birth: “Offer VBACs - when I gave birth last year I was advised I wouldn't be able to have my next baby at Katoomba which is very disappointing - has this changed? Or is the option available to participate in caseload at Katoomba, birth at Nepean and then transfer” (Caseload, 2013) “Allow women to attempt VBAC! PLEASE! I loved my midwife care and would dearly like to birth there again.” (Caseload, 2014)
Although not captured in survey quotes, it is evident from many conversations with
midwives and women on the unit that an unknown proportion of women choose
repeat elective caesarean sections in order to have their babies in BMDAMH, and
avoid travelling to Nepean.
It was much easier birthing in water
Women also frequently made suggestions for water-birth to be made available at
BMDAMH: “Offer water birth option -There was a marked difference in the reduction of pain and how much easier it was birthing in the water” (Caseload, 2013)
86
“PLEASE put a water birth policy in place!!” (Caseload, 2013)
As with women’s requests to have VBACs at BMDAMH, there was not much
variation to the content, the suggestions were unambiguously direct.
Don’t rush to kick mums out of the ward
This theme describes women’s resistance to the notion of early discharge. There is
clearly an expectation and preference to stay in hospital for a few days after the
baby is born. As previously mentioned, one respondent elected the obstetric care
model because she thought she would be able to stay in hospital for longer. This
contrasts to the popularity that women have also expressed for caseload home visits
and conflicted breastfeeding advice in hospital. Women who have a vaginal birth are
recommended to stay in hospital for a maximum of 24-48 hours, and early discharge
from birthing suite is also suggested in the caseload model for women and babies
with no complications, who can have midwifery follow up at home. The average
postnatal hospital stay for women at BMDAMH is 2.2 days (2011-2014), which is
probably longer than busier hospitals. Many women describe their fear and
disappointment with not being able to stay in hospital for longer. “I was not informed that the intention was that I should leave within 24 hours. I found this out from a friend who had recently had a baby. This was very concerning and contrasted with the wonderful are in 2010” (Caseload, 2013) “Did not receive enough support in the hospital, I was just shipped out!” (Caseload, 2012) “Don't rush to kick out mums from the ward. Appreciate cost-cutting but would have liked more time to discuss bubs inability to attach.” (Caseload, 2012) “Baby was not attaching when I was discharged and I had to syringe feed him. I was discharged within 5 hours of birth, despite this.” (Caseload, 2103) “My only reservation with childbirth under the new system is the length of stay in hospital after Midwife Caseload care. I feel all mothers should have a choice to stay or go home. You don't know how you'll feel after giving birth and to know that you HAVE to leave can be quite daunting.” (Caseload, 2012) “Caseload midwifery is a brilliant model, WITHOUT the assumption of going home within the first day.” (Caseload, 2014) “But wasn't up to it physically - I had no choice they told me no one was on shift to look after me” (Caseload, 2012)
87
“I would have been happy to go with Caseload Midwifery Care but I didn't want to be sent home within hours of birth.” (Obstetric care, 2012) “I was unaware that I would not be able to stay in hospital with the new baby until a few weeks before delivery - If I had known this, I may have chosen to use private medical cover to enable me to stay at Nepean Private - with 2 kids already at home, I didn't like being required to leave so soon after giving birth Allow women to stay longer after the birth.” (Caseload, 2013)
The dissatisfaction with early discharge (or any discharge before the woman feels
ready), is accentuated by the woman not knowing about this, being surprised, being
informed after she has given birth, and feeling ‘kicked out’ of a place that she
perceives should be taking care of her and the baby in their most vulnerable period.
However, women have also overwhelmingly expressed their gratitude for home
visits, confirming this as a superior postnatal care option. Women who are well
prepared for hospital discharge and length of stay in the antenatal period, and
reassured about continuity of care in the home can be more satisfied in this respect.
“I felt very ready and wasn't rushed out” (Caseload, 2014)
“We were made to feel as if we could stay in hospital as long as needed and liked that our caseload midwife visited us at home”. (Caseload, 2013)
Concerns about staffing
This theme relates to how women perceive the workload of midwives who care for
them. Concerns of this nature were expressed frequently in 2012 and the early part
of 2013, and may reflect actual staff shortages affecting service provision over this
time:
The staff really need to be cared for as they do a fantastic job caring for us. I fear the workload will burn many out …look after the staff. You have a wonderful facility which is an excellent resource for the community.” (Caseload, 2012) “Caseload midwives roster scheduled somehow to promote better rested [midwives].” (Caseload, 2013)
“The midwifery caseload program was excellent, however I felt that the postnatal period was difficult as the nurses seemed very busy and rushed. Perhaps more staff or a better roster system would help...?” (Caseload, 2012)
88
“Only problem I had was all the paperwork the poor midwife had, let them focus on mums, not paperwork. Give them staff for paperwork! Not their job!!!” (Caseload, 2013)
Observations of this nature may indicate an underlying concern about the
sustainability of maternity service provision at BMDAMH. Caseload midwives
particularly form close therapeutic relationships with women, and therefore women
are more likely to feel ‘reciprocity of concern’ for their caregiver. It is clear that
women have noticed staffing and workload pressures, and the flow-on effect this has
on their own care.
The Goodies – Positive comments from women
89
“FANTASTIC experience and care. Happy,
HEALTHY BABY Couldn't be more APPRECIATIVE!
Keep using CASELOAD
model.”
“Everyone DESERVES a
good EXPERIENCE like I had! Midwife caseload model is FANTASTIC!!”
CASELOADS ARE MARVELLOUS.
Midwifery care was excellent from
BEGINNING TO END.”
“The staff and DOCTORS at
BMDAMH were fantastic, very CARING and SUPPORTIVE post birth”
“My MIDWIFE was AMAZING! She RESPECTED MY CHOICES but supported me with all the
information and CARE throughout my ENTIRE
experience. I couldn't SING HER PRAISES LOUDLY
enough! Thank you very much for a FANTASTIC BIRTH
experience.
“I had my 1st at
Nepean and KATOOMBA was 100% better and
FREINDLIER”
LOVED our
midwife!
“The midwives do an amazing job and I am GREATFUL for the chance to
BIRTH LOCALLY.”
“We felt very SUPPORTIVE
during our stay at Katoomba
Hospital following our
child’s BIRTH!”
“EXTREMELY HAPPY with caseload service and care received at
Blue Mountains Hospital. Had two
other children at RPA and was good but not
as good as Blue Mountains.”
“My MIDWIFE gave me the most thorough and
SENSITIVE CARE. She fully supported my choices and was able to inform me about anything I
was unsure or concerned about”
“I was pleased with the way
MY CASELOAD MIDWIFE
handled my case.”
“Very positive
experience”
“Amazing!! I had my first baby at a private hospital under the care
of a private doctor. EXPERIENCE at BMDAMH with caseload midwifery care was by
FAR BETTER EXPERIENCE for me. Along the way I felt respected,
EMPOWERED informed and cared for. My midwife was
wonderful and every member of staff we had dealings with caring PROFESSIONAL. If I had my time over gain I would have had
both my babies at BMDAMH! THANK YOU”
“The midwives
were FABULOUS
“After the birth I was taken care of very thoroughly. I
DEEPLY APPRECIATE
everyone’s
LOVE and CARE”
“This is a very VALUABLE
resource for the COMMUNITY.
I had such a POSITIVE
EXPERIENCE “
“FANTASTIC hospital,
made us feel like HUMANS
not
numbers.”
90
“During LABOUR I appreciated the concern
and attention of the midwives and staff. I felt supported in all my
choices, Appreciated my husband being able to
spend the night with us when we were a NEW
FAMILY”
“My caseload midwife was very
supportive and
respectful of my wishes. She was
100% available and
made me feel very confident.”
“OUR MIDWIFE was wonderful! It was
great seeing her every time we had an
appointment. We both felt very comfortable
with the whole EXPERERIENCE! Thank
you!”
“I am OVERWHELMED by the SUPPORT
from my midwife, she was
excellent.”
“I really enjoyed my experience with the
caseload model. I was always met with a FAMILIAR FACE and received the best care possible. If I had more
children I would use it again.”
“I could not RECOMMEND any higher a service as
having a
caseload midwife. I
hope it continues for years to come.”
LOVE the caseload model!
“I tell all of my Sydney friends about the
EXCELLENT CARE I received by my midwife
and BM hospital and they are jealous! I tell
them they need to move up here just to have
their baby, you don't just feel
like a number”.
“Katoomba maternity is by far
a private hospital experience. The
midwives are SUPPORTIVE and
warm. Both my children were born here and both times I
received exceptional care. CASELOAD IS AWESOME!”
“I was very happy with the midwives while I was there.
They were all caring and SUPPORTIVE I
would choose Katoomba again in a
HEARTBEAT over Nepean (1st
child born there).”
“Thank you very much for all the midwives and doctors to make my PREGNANCY and birth happy and help
me meet my BEAUTIFUL BABY I was very lucky to
have my baby at
Katoomba”.
“MY MIDWIFE was very GOOD AT HER JOB and if I was to have a
baby again I would be very happy to have
her again.”
“I had the best experience with the caseload care. I would
go again if I was
guaranteed the same midwife as I felt really COMFORTABLE
with her”.
91
Appendix 1: Feedback from consumer consultations Blue
Mountains LGA, October 2008
Facilitator – Hannah Dahlen Description - Katoomba Woman's Health Centre - 38 women - Lawson Community Centre - 10 women under 25 years of age Why Katoomba should remain open - Beautiful unit, nice and small - Closer to family support - No travel for partner and children "When the unit is shut we have to go to Lithgow, 40 minutes travel. This is difficult due to having other children at home. Don' know the staff and we are strangers to the unit." - The staffs have more time - Midwives have better attitude / approach - Midwives support lower / less intervention - Even if you see different midwives you still bond with the unit - Travel / much closer; hard for family ; single room ; more peaceful postnatal in Katoomba - Weather meant had to give birth in Katoomba (snow!). Felt safe and cared for Why Nepean is not an option - Birth too quickly for some women (one woman spent labour in hotel while waiting to birth then eventually birthed at Blue Mountains Hospital) - Midwives and staff too busy - not enough time - Unit too busy - "I felt just like a number" - Could not visit delivery suite before hand - More intervention at Nepean District Hospital - Nepean good place for higher intervention births though - Nepean has been good but prefer to birth closer to home - Hard in the postnatal period. Family had to travel. - Negative experiences (attitudes / judgemental / negative towards home birth). Needs to be easier / smoother transfer to Nepean from home birth. - Distance to neonatal ward and emergency - No options at Nepean District Hospital - felt no choices - too high risk - Continuous monitoring - told have 'no choice' Transfer issues - Blue mountains unit unpredictable - not sure if it is open or closed - Had to go to Nepean by ambulance with midwife but she had to go back tot the mountains - No partner with her - Ended up with caesarean - was this impacted by transfer? - Would have been improved if same midwife? - Follow-up care - in the unit and at home - I nearly gave birth in the car VBAC issues - Informed consent - lack of information re: risks
92
- No information about benefits - VBAC - told she had to have an epidural - Felt need to speak up for herself to withstand pressure to have an epidural - Please allow VBAC in Blue Mountains as women choose home birth because they feel they have no option - How can women make a decision without all the information - Personal story - first birth, 2nd baby, no risk factors but told would need a caesarean, felt pressured, no continuity of care How can we improve services - VBAC at Katoomba - Midwifery led care backed by obstetrics - Continuity of care provided by midwives (one option for this was to go to Blacktown) - Continuity of care not just for low risk women - Concerned about midwives - how are thy feeling with all of this What do we want? - Continuity - Advocacy - Water Birth - VBAC - A policy to cover women who refuse interventions - Right of refusal - If transferred can midwife stay with woman at Nepean - It no anaesthetist cover - no problem we have enough other staff - Respect and dignity - Acknowledgement - Need to be able to trust - is all this intervention necessary - Acknowledgement of grief and loss Summary - Want birth at Katoomba - Want assurances unit will remain open all the time - Want continuity of midwifery care - Want consistent information - Want more choices around VBAC, IOL, fetal monitoring etc. - Want water birth - Less medicalization of birth - More personal touch - Respect, choice and control
94
Appendix 3: Attitudes to Professional Role (ATPR) – Questionnaire Circle one number for each question which best describes your feeling towards the statement.
Strongly agree
Agree Not sure
Disagree
Strongly disagree
1. Generally speaking, I am satisfied with my current role as a midwife.
1 2 3 4 5
2. I have enough professional independence 1 2 3 4 5 3. I have limited opportunities to provide continuity 1 2 3 4 5 4. I am confident that I have the skills for my current role 1 2 3 4 5 5. I have few opportunities to develop my skills as a midwife 1 2 3 4 5 6. I feel I am in a rut 1 2 3 4 5 7. I have enough opportunities to make decisions about care 1 2 3 4 5 8. My current role is very stressful 1 2 3 4 5 9. I lack professional support from my managers 1 2 3 4 5
10. I have plenty of opportunities to further my professional education
1 2 3 4 5
11. My current role allows me to provide women with choice about their care
1 2 3 4 5
12. My current role allows me to plan care with women 1 2 3 4 5 13. There is not enough time to do my job properly 1 2 3 4 5 14. I have enough time to give women the care they need 1 2 3 4 5 15. I get professional support from my midwife colleagues 1 2 3 4 5 16. I have limited opportunities for professional development 1 2 3 4 5 17. I get enough support from obstetric colleagues 1 2 3 4 5 18. I need greater scope to provide women with information
about their care 1 2 3 4 5
19. I feel frustrated with my current role 1 2 3 4 5 20. I have limited opportunities to provide women with
personalized care 1 2 3 4 5
95
Appendix 4: Industrial Agreement Questionnaire – Caseload Midwifery Model
1. HOURS
1.1 Are the hours you are working routinely over and above your FTE? YES/NO 1.2 If YES, how many hours/week are you working on average over & above your FTE? _______p/wk
2. ON CALL
2.1 How many days in a week period are you not on call? _____ d/wk 2.2 How many times per week, on average, are you rang out of office hours whilst on call? ____x/wk 2.3 How many times in a week are you woken to give considered telephone advice? _____x/wk
3. CASELOAD
3.1 What is your current caseload? ___________________________ 3.2 Do you feel this caseload is manageable at all times? YES/NO 3.3 If NO, during which period is it not manageable? (Please tick)
a. During others annual leave
b. During unplanned & unexpected absences of other caseload midwives
c. All the time
d. Other
3.4 What arrangements do you have to cover your colleague’s caseload? __________________________________________________________________________________ 3.5 Are you satisfied with this arrangement? YES/NO
4. DAYS OFF
4.1 How do you currently structure your workload to get days off? __________________________________________________________________________________ -‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐-‐ -‐ 4.2 Are you satisfied with this arrangement? YES/NO
5. PROFESSIONAL SUPERVISION & SUPPORT
5.1 What arrangements are there in place to provide you with professional support? Choose one or more of the following –
• Clinical supervision
• Management support
• Peer support
• Other support
5.2 What professional development activities have you been able to attend in the last 12 months? 5.3 Are there any more comments you would like to make on your working conditions? YES/NO (Please make any comments below)
96
Appendix 5: Satisfaction survey
Wom
en and Children’s
Health U
nit B
lue Mountains D
istrict A
nzac Mem
orial Hospital
Katoom
ba
Quality S
urvey C
ontact: N
urse Unit M
anager Ph: 47846572
Baby’s D
ate of Birth: …
……
……
Was this your first baby? Y
es / No
Which M
odel(s) of Care did you
receive during your pregnancy?
Hospital B
ased Midw
ifery Care
�
C
aseload Midw
ifery Care
�
O
bstetrician Care
�
G
P shared care
�
O
ther (please describe)
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
Was the m
odel of care you received chosen by yourself or w
ere you allocated care? C
hoice:�
A
llocated:�
If you were allocated care or the
model of care w
as changed during your pregnancy w
ere you given a reason?
C
omm
ent:……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
…
Did you receive the inform
ation
Were you given inform
ation about the scope of services available at B
MD
AM
H?
Yes:
�
N
o: �
Were your w
ishes and needs respected and m
eet by the service (w
ithin the scope of the services available at B
MD
AM
H)?
Yes:
�
N
o: �
Com
ment:…
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
…
Did you attend Parenting C
lasses? Y
es: �
No:
�
Please comm
ent on the value of education you received: H
ospital B
ased:……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
…
Private:
(Type)……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
…
From your m
idwife or
Doctor:…
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
97
Did you receive adequate inform
ation in relation to the postnatal period?
Yes:
�
N
o: �
Comment:…
…………………………………………………………
……………………………………………………………………………
……………………………………………………………………………
……………………………………………………………………………
……………………………………………………………………………
……………………………………………………………………………
…………………………………………………………………………….
Did you feel confident about going
home w
ith your new baby?
Y
es: �
No:
�
Com
ment:…
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
If you received C
aseload Midw
ifery C
are, were you w
ell supported during:
•the antenatal period:
Yes/ N
o •
your labour and birth : Yes / N
o •
at home?
Yes / N
o C
omm
ent:……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
…
What M
ethod did you choose for feeding your baby?
•B
reastfeeding
☐
•B
ottle Feeding
☐
•B
reast and Bottle Feeding
☐ W
ere you supported with and given
enough information to support this
choice? Yes:
No:
Comm
ent:……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
If you chose to breastfeed are you still breastfeeding your baby? Y
es: �
No:
�
If you are no longer breastfeeding your baby, how
old was your baby
when you w
eaned? …
……
……
……
…W
eeks/Months
Were you given relevant inform
ation about the available com
munity
supports for mothers and babies?
Y
es: �
No:
�
Com
ment:…
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
…..
What other sources of inform
ation did you use to prepare for the birth of your baby?
•Friends:
☐
•Fam
ily:
☐ •
Books: (e.g.)
☐
•M
agazines: (e.g.) ☐
•Internet: (e.g.)
☐
•O
ther:
☐
Com
ment on the m
ost valuable source of inform
ation:……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
……
Have your say:
(Please feel free to add any com
ments about
your experience) D
o you have any suggestions to help us im
prove our service? Thank you, Your com
ments and suggestions w
ill help us provide a better service. If you w
ould like us to contact you with
regard to your comm
ents please com
plete the details below:
98
REFERENCES
1. Health, M.o., Maternity -‐ Towards Normal Birth in NSW, Policy Directive PD2010_045, N.G. Health, Editor. 2010, NSW Health: North Sydney, NSW.
2. Dahlen, H. and S. Tracey, Proposal for Three Sisters Midwifery Group Practice at BMDAMH. 2008, University of Western Sydney,
University of Technology. 3. Li, Z., et al., Australia's mothers and babies 2011, in Perinatal statistics series no
28. 2013, AIHW National Perinatal Epidemiology and Statistics unit.: Canberra. 4. NSWGovernmentHealth, Maternity-‐Supporting WOmen in their Next Birth after
Caesarean Section (NBAC). GL2014_004, N.K.a. Families, Editor. 2014, NSW Government: North Sydney.
5. NSWKids+Families, Guideline-‐Maternity and Neonatal Service Capability Framework (Draft), NSWHealth, Editor. 2014, NSW Health: North Sydney.
6. Midwives, A.C.o., National Midwifery Guidelines for Consultation and Referral. 3rd Edition. 2013: ACM.
7. LGA, P.o.C.F.-‐B.M., Feedback from consumer consultations, Blue Mountains, H. Dahlen and S. Van Opdorp, Editors. 2008, (Unpublished).
8. Baum, F., C. MacDougall, and D. Smith, Participatory action research. J Epidemiology Community Health, 2006. 60(10): p. 854-‐857.
9. Council, B.M.C. Overview of local government area. BMCC Website 2014. 10. Council, B.M.C. Aboriginal Blue Mountains 2014; Available from:
http://aboriginalbluemountains.com.au/community/the-‐aboriginal-‐community. 11. ABS, Fertility Rates, Australia, in Births, Australia. 2012, Australian Bureau of
Statistics. 12. ObstetriX, ObstetriX Report, in All variables. 2011-‐2014. 13. Health, N.M.o., Place of birth by local health district and year. 2012. 14. NSWLegislativeAssembly, Blue Mountains Hospital Maternity Unit, Hansard,
Editor. 2009, Parliament of New South Wales. 15. O'Keeffe, R., Throwing the lies out with the birth water,
http://janetfraser.id.au/blog/2010/08/10/throwing-‐out-‐the-‐lies-‐with-‐the-‐birth-‐water-‐sydney-‐screening/, Editor. 2010.
16. Wallace, N., Women in labour sent packing, in Sydney Morning Herald. 2008, SMH: Sydney.
17. communications, P., Staffing of midwives 2008-‐2011, Maternity unit, M. Lewis, Editor. 2014.
18. Benson, K., Blue Mountains residents rally to save their maternity ward, in The Sydney Morning Herald. 2009, SMH: Sydney.
19. Freeman, G., et al., Report of a scoping exercise for the National Coordinating Centre for NHS Service Delivery and Organisation R & D NCCSDO, Editor. 2001, NCCSDO.
20. Freeman, G., et al., Continuity of Care 2006: What have we learned since 2000, and what are policy imperatives now?, NCCSDO, Editor. 2007, NCCSDO.
21. Reid, R. and J. Haggerty, Defusing the confusion concepts and Measures of Continuity of Health Care, C.H.S.R. Foundation, Editor. 2002, Canadian Health Services Research Foundation.
22. Saultz, J., Defining and measuring Interpersonal Continuity of Care. Annals of Family Medicine, 2003. 1(3): p. 134-‐143.
99
23. Green, J.M., M.J. Renfrew, and P.A. Curtis, Continuity of carer: what matters to women? A review of the evidence. Midwifery, 2000. 16(3): p. 186-‐96.
24. Hatem, M., et al., Midwife-‐led verses other models of care for childbearing women (Review). Cochrane Database of Systematic Reviews, 2008. Oct 8(4).
25. Hundley, V., et al., Satisfaction and Continuity of care: Staff views of care in a midwife-‐managed delivery unit. Midwifery, 1995. 11(4): p. 163-‐173.
26. McCourt, C., et al., Evaluation of one-‐to-‐one midwifery:Women's responses to care. Birth, 1998. Jun;25(2): p. 73-‐80.
27. Sandall, J., et al., Discussions of findings from a Cochrane review of midwife-‐led versus other models of care for childbearing women: continuity, normality and safety. Midwifery, 2009. 25: p. 8-‐13.
28. Homer, C., P. Brodie, and N. Leap, Midwifery continuity of care: A Practical guide, ed. C. Homer, P. Brodie, and N. Leap. 2008, Chatswood: Churchill Livingstone.
29. Hodnett, E., et al., Continuous support for women during childbirth. Cochrane Database Syst Rev., 2011. 16(2).
30. Health, N.M.O., Midwifery Continuity of Carer Model Tool-‐kit, N. Health, Editor. 2012, NSW Ministry Of Health: North Sydney, NSW.
31. Queensland and Health, Delivering contiuity of midwifery care to Queensland women, A guide to implementation. 2012, Queensland Health: Brisbane, QLD.
32. Henderson, J., J. Hornbuckle, and D. Doherty, Models of Maternity Care: A reveiw of the evidence. 2007, Women's and Infants Research Foundation.: Perth.
33. Research, C.f.E.a., New South Wales Mothers and Babies 2006, N.D.o. Health, Editor. 2007, NSW Public Health Bull: North Sydney, NSW.
34. Smith, G., J. Pell, and R. Dobbie, Caesarean section and risk of unexplained stillbirth in subsequent pregnancy. Lancet, 2003. 362: p. 1779-‐84.
35. Boutikou, T. and A. Malamitsi-‐Puchner, Caesarean section: impact on mother and child. Acta Paediatr, 2011. 100(15): p. 18-‐22.
36. Kennare, R., et al., Risks of adverse outcomes in the next birth after a first cesarean delivery. Obstet Gynecol, 2007. 109: p. 270-‐6.
37. Hemminki, E. and J. Merilainen, Long-‐term effects of cesarean sections: ectopic pregnancies and placental problems. American Journal Obstet Gynecol, 1996. 174: p. 1061-‐74.
38. Gerten, K., et al., Cesarean delivery and respiratory distress sydrome: Does labor make a difference? American Journal Obstet Gynecol, 2005. 193: p. 1061-‐4.
39. Department of Health, A., National Maternity Services Plan, D.o. Health, Editor. 2008: Canberra.
40. Johnson, M., et al., A Comparison of the outcomes of partnership caseload midwifery and standard hospital care in low risk mothers. Australian journal of Advanced Nursing, 2005. 22(3): p. 21-‐27.
41. Turnbull, D., et al., An evaluation of Midwifery Group Practice. Part I: clinical effectiveness. Women Birth, 2009. 22(1): p. 3-‐9.
42. Homer, C., et al., Collaboration in Maternity care: a randomised controlled trail comparing continuity of care with standard hospital care. BJOG, 2001. 108(1): p. 16-‐22.
43. McLachlan, H.L., et al., Effects of continuity of care by a primary midwife (caseload midwifery) on caesarean section rates in women of low obstetric risk: the COSMOS randomised controlled trial. BJOG, 2012. 119(12): p. 1483-‐92.
44. Research, N.S.C.C., A randomised study of midwifery caseload care and traditional shared-‐care. Midwifery, 2000. 16(4): p. 295-‐302.
100
45. NSWHealth, 2007 Pilot Model agreement for Midwifery Caseload Practice Anualised Salary Agreement, N. Health, Editor. 2007, Document number r IB2014_050: Sydney.
46. Taylor, J.C., Business Rules for Caseload Midwifery at Blue Mountains Hospital. 2012, Nepean Blue Mountains Local Health District (policy).
47. NSWHealth, Maternity-‐National Midwifery Guidelines for Consultation and Referral. Policy Directive, N. Health, Editor. 2010, NSW Health: North Sydney.
48. NSWHealth, Incident Management Policy. PD2014_004. 2014, NSW Health: North Sydney.
49. Williams, K., et al., Mothers' views of caseload midwifery and the value of continuity of care at an Australian regional hospital. Midwifery, 2010. 26(6): p. 615-‐21.
50. Members, M.G.P.F.p., Facebook Midwifery Group Practice discussion page. 2014: Facebook Midwifery Group Practice discussion page.
51. NSWGovernment, Total births by maternal age, trends. 2012: http://www.healthstats.nsw.gov.au/Indicator/mum_bthage.
52. Gao, Y., et al., A cost-‐consequences analysis of a Midwifery Group Practice for Aboriginal mothers and infants in the Top End of the Northern Territory, Australia. Midwifery, 2014. 30(4): p. 447-‐455.
53. Tracey, S. and D. Hartz, The Quality Review of Ryde Midwifery Group Practice, September 20144 to October 2005. Final Report, N.S.a.C.C. Health, Editor. 2006: Sydney.