Case Scenario
Transcript of Case Scenario
Case Scenario: Anesthesia-related Cardiac Arrest in a Child withTimothy Syndrome
Aruna T. Nathan, M.B.B.S., F.R.C.A.*, Charles Antzelevitch, Ph.D.†, Lisa M. Montenegro,M.D.‡, and Victoria L. Vetter, M.D., M.P.H.§*Assistant Professor, Anesthesiology and Critical Care, Perelman School of Medicine, Universityof Pennsylvania, Philadelphia, Pennsylvania, and Division of Cardio-Thoracic Anesthesia, TheChildren’s Hospital of Philadelphia, Philadelphia, Pennsylvania‡Assistant Professor, Anesthesiology and Critical Care, Perelman School of Medicine, Universityof Pennsylvania, and The Children’s Hospital of Philadelphia§Professor, Pediatrics, Perelman School of Medicine, University of Pennsylvania, and Division ofCardiology, Department of Pediatrics, The Children’s Hospital of Philadelphia†Director of Research, Professor of Pharmacology, Masonic Medical Research Institute, Utica,New York
The long QT syndrome (LQTS) is characterized by prolonged ventricular repolarization, theelectrocardiographic appearance of long QT intervals, an atypical polymorphic ventriculartachycardia known as torsades de pointes (TdP), and an increased risk for sudden cardiacdeath.
Patients with LQTS can suffer severe cardiac events resulting in syncope, seizures, andsudden cardiac death during times of physical and emotional stress and when exposed tocertain pharmacological agents. The perioperative management of patients with LQTS hasbeen reviewed1,2; however, the individual risk posed by exposure to perioperative andanesthetic medications and interventions has not been quantified by prospective studies.
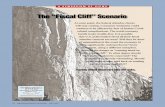
Case ReportsA 9-month-old male infant presented for placement of an epicardial pacemaker duringgeneral anesthesia. His medical history was significant for a suspected diagnosis of Timothysyndrome (LQT8) with prolongation of the QTc interval on his electrocardiogram, andsyndactyly of both hands. He was otherwise healthy. He was on oral 1.1 ml propranolol (4mg/ml) every 8 h. He had had two prior general anesthetics for repair of syndactyly of eitherhand. The first anesthetic was uneventful, and the second was notable for a short period ofinability to obtain noninvasive blood pressure measurements with release of the arterialtourniquet in the upper extremity. T wave alternans was noted on the surfaceelectrocardiogram (fig. 1). This adverse event prompted admission to the hospital, andfurther electrocardiographic telemetric monitoring revealed significant pauses lasting 3–4.7s. The patient was urgently scheduled for pacemaker placement. The anesthetic for thepacemaker placement involved general endotracheal anesthesia; premedication with
Copyright © 2012, the American Society of Anesthesiologists, Inc.
Address correspondence to Dr. Nathan: 12 NW 40, The Children’s Hospital of Philadelphia, 3400 Civic Center Boulevard,Philadelphia, Pennsylvania 19104. [email protected].
Information on purchasing reprints may be found at www.anesthesiology.org or on the masthead page at the beginning of this issue.Anesthesiology’s articles are made freely accessible to all readers, for personal use only, 6 months from the cover date of the issue.
NIH Public AccessAuthor ManuscriptAnesthesiology. Author manuscript; available in PMC 2013 November 01.
Published in final edited form as:Anesthesiology. 2012 November ; 117(5): 1117–1126. doi:10.1097/ALN.0b013e31826e73b1.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
midazolam; intravenous induction with thiopentone, fentanyl, and pancuronium; andmaintenance with sevoflurane in oxygen and nitrous oxide, with reversal of neuromuscularblockade with atropine and neostigmine. No adverse events (AE) were reported. The patientwas admitted 5 months later for an epicardial generator replacement and lead placementbecause of decreased sensitivity of the pacemaker lead.
Intravenous induction of anesthesia with 6 mg/kg thiopentone, 2 μg/kg fentanyl, and 0.1 mg/kg pancuronium, tracheal intubation, and transition to maintenance anesthesia with inhaledisoflurane in oxygen and nitrous oxide was uneventful. T wave alternans, noticed on thesurface electrocardiogram shortly after start of surgery, were treated with intravenous 1 mg/kg lidocaine and 25 mg/kg magnesium bolus with initial recovery of normal repolarization.Upon completion of the procedure, neuromuscular blockade was reversed with 0.02 mg/kgatropine and 0.07 mg/kg neostigmine, followed by local anesthetic infiltration of the woundwith 1 ml/kg plain bupivacaine, 0.25%. This was followed by sudden onset of bradycardia,with loss of pacemaker capture and blood pressure that could not be recorded. Successfulreturn of spontaneous circulation was achieved after 11 min of cardiopulmonaryresuscitation with external chest compressions, manual ventilation, and the administration ofintravenous 10 mEq/kg sodium bicarbonate in three divided doses, 250 mg calciumgluconate, and 6 mg dopamine.
DiscussionEpidemiology and Significance of LQTS
The current incidence of LQTS is considered to be 1 in 2,500 live births with variablepenetrance. To date, 13 LQTS genotypes have been described, with LQTS 1, 2, and 3comprising 90% of the cases that can be successfully genotyped (table 1).3 Arrhythmogenictriggers are genotype-specific and include adrenergic stimulation during exercise andemotional stress (LQT1, LQT2), loud noise or startle, or heightened emotional states; fear,fright, and exercise (LQT2); and a pause-dependent trigger mechanism during sleep orresting states (LQT3). Some patients with LQTS may develop prolongation of the QTc inresponse to certain drugs or electrolyte imbalances. Patients may have subclinical diseasethat becomes unmasked under certain conditions but returns to the subclinical state whenthese conditions are removed. LQT8 is especially associated with an increased risk ofmalignant arrhythmias during anesthesia, with case reports of arrhythmias occurring duringboth volatile and intravenous anesthesia. It results in a severe arrhythmia disorder caused bycardiac L-type calcium channel mutations.4
Pathophysiology of Long QT Syndrome 1, 2, 3, and Timothy SyndromeModels of the LQT1, LQT2, and LQT3 forms of the long QT syndrome have beendeveloped using the canine arterially perfused left ventricular wedge preparation. In thesethree forms of LQTS, preferential prolongation of the M cell action potential duration(APD) leads to an increase in the QT interval as well as an increase in transmural dispersionof repolarization (TDR), the latter providing the substrate for the development ofspontaneous as well as stimulation-induced TdP.
LQT1—LQT1 is the most prevalent of the congenital long QT syndromes. It is caused by aloss of function of the slowly activating delayed rectifier (IKs). Inhibition of IKs usingchromanol 293B has been shown to lead to uniform prolongation of APD in all three celltypes in the wedge, causing little change in TDR. Although the QT interval is prolonged,TdP does not occur under these conditions, nor can it be induced. Addition of isoproterenolresults in abbreviation of epicardial and endocardial APD, but the APD of the M cell eitherprolongs or remains the same. The dramatic increase in TDR provides the substrate for the
Nathan et al. Page 2
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
development of spontaneous as well as stimulation-induced TdP. 5 These results support thethesis that the problem with the long QT syndrome is not the long QT interval, but rather theincrease in TDR that often accompanies the prolongation of the QT interval. These findingsprovide an understanding of the sensitivity of LQT1 patients, to sympathetic influences
LQT2—LQT2 is the second most prevalent form of congenital LQTS. It is because of lossof function of the rapidly activating delayed rectifier (IKr). IKr inhibition is also responsiblefor most cases of acquired LQTS. In the wedge, inhibition of IKr with d-sotalol produces apreferential prolongation of the M cells, resulting in accentuation of TDR and spontaneousas well as stimulation-induced TdP. When IKr block is combined with hypokalemia,bifurcated T waves develop in the wedge preparation, similar to those seen in patients withLQT2. Isoproterenol further exaggerates TDR and leads to an increased incidence of TdP inthis model, but only transiently.
LQT3—LQT3 has a much lower prevalence. It is encountered in approximately 10% ofgenotyped probands and is caused by a gain of function of late sodium current (late INa).Augmentation of late INa using the sea anemone toxin ATX-II produces a preferentialprolongation of the M cell action potential in the wedge, resulting in a marked increase inTDR and development of TdP. Because epicardial APD is also significantly prolonged,there is delay in the onset of the T wave in the wedge, as observed in the clinical syndrome.Under these conditions, β-adrenergic stimulation abbreviates APD of all cell types, reducingTDR and suppressing TdP. 6
In LQT1, isoproterenol produces an increase in TDR that is most prominent during the first2 min, but which persists, although to a lesser extent, during steady state. TdP incidence isenhanced during the initial period as well as during steady state. In LQT2, isoproterenolproduces only a transient increase in TDR that persists for less than 2 min. TdP incidence istherefore enhanced only for a brief period of time. These differences in time-course mayexplain the important differences in autonomic activity and other gene-specific triggers thatcontribute to events in patients with different LQTS genotypes.
Although β-blockers are considered first-line therapy in patients with LQT1, there arelimited data of their benefit in LQT3. Preliminary data suggest LQT3 patients might benefitfrom Na+ channel blockers, such as mexiletine, flecainide, and ranoalzine.7 Experimentaldata have shown that mexiletine reduces transmural dispersion and prevents TdP in LQT3 aswell as LQT1 and LQT2, suggesting that agents that block the late sodium current may beeffective in all forms of LQTS. The late INa blocker ranolazine is effective in significantlyabbreviating QTc in LQT3 patients.
LQT8—Timothy syndrome, also known as LQT8, is a multisystem disease caused bymutations in the calcium channel Cav1.2 encoded by the CACNA1C. Because the calciumchannel Cav1.2 is present in many tissues, patients with Timothy syndrome have manyclinical manifestations, including congenital heart disease, autism, syndactyly, and immunedeficiency. 4
Mutations in nine other genes have been associated with LQTS in recent years. Thesegenetic variations, which include structural proteins as well as other ion channel proteins,are relatively rare.
Gene-specific electrocardiographic patterns have been identified8 and triggers for cardiacevents have been shown to be gene-specific, but with considerable overlap. LQT1 patientsexperience most of the events during physical activity as opposed to LQT3 patients, whopresent the majority of cardiac events at rest or during sleep. Auditory stimuli and arousal
Nathan et al. Page 3
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
have been identified as relatively specific triggers for LQT2 patients, whereas swimming hasbeen identified as a predisposing setting for cardiac events in LQT1 patients.
The Electrocardioghic Phenotypes: Typical ST-T Wave Patterns in LQT1, LQT2, and LQT3Zhang8 identified typical ST-T wave patterns, four in LQT1, four in LQT2, and two inLQT3 patients in 88% of patients studied with a definite genotype. The QT interval rangedfrom borderline to definitely prolonged in all patients (figure 2).
Drug-induced QTc ProlongationDrug-induced QTc prolongation is because of prolongation of the IKr current via drug effecton the HERG (KCNH2 or LQT2 IKr) channel. Therefore, the electrocardiographicmanifestations of drug-induced QTc prolongation mimic the electrocardiographic findingsof LQT2.
Risk Stratification in LQTSA risk-stratification scheme based on genotype has been proposed by several authors.9 QTinterval, genotype, and gender were significantly associated with events. A QTc intervalmore than 500 ms in LQT2 or LQT3 forecasts a worse prognosis. The same authors reportedthat the response to β-blockers is also genotype-specific, with LQT1 patients showinggreater protection in response to β-blockers than LQT2 or LQT3 patients. A QTc duration ofmore than 500 ms and a prior history of syncope identify high risk of sudden cardiac deathin boys, and a prior history of syncope is the only significant risk factor in girls.10
Arrhythmogenic Mechanism in LQTSThe underlying condition predisposing to malignant arrhythmias is a defect in ventricularrepolarization (fig. 3). Accentuation of spatial dispersion of refractoriness within theventricular myocardium, secondary to exaggerated transmural or transseptal dispersion ofrepolarization, has been identified as the principal arrhythmogenic substrate in both acquiredand congenital LQTS.11 This exaggerated intrinsic heterogeneity together with early anddelayed afterdepolarization (EAD and DAD)-induced triggered activity, both caused byreduction in net repolarizing current, underlie the substrate and trigger for the developmentof TdP observed under LQTS conditions. Preferential prolongation of the M cell APD leadsto an increase in the QT interval as well as an increase in TDR (fig. 4), which contributes tothe development of spontaneous as well as stimulation-induced TdP. The spatial dispersionof repolarization is further exaggerated by sympathetic influences in LQT1 and LQT2,accounting for the great sensitivity of patients with these genotypes to adrenergic stimuli.Dispersion of repolarization is a quality that is difficult to quantify even by specialists, andmight be overly simplified as a concept. Electrophysiologists believe that there are microand macro environments locally that precipitate the reentrant arrhythmias. Our approach topatients with LQTS undergoing anesthesia is to discuss every patient with theelectrophysiologist caring for that patient and generate an individualized anesthesia careplan, which includes perioperative medications and infusions that are safe in LQTS or willbe necessary in the management of LQTS related arrhythmias.
Management of Patients with LQTSIn LQTS patients, the first line of therapy is β-blocker therapy,12 even though a number ofpatients will have an arrhythmia-related event or suffer sudden cardiac death despite thistherapy. Continuation of prescribed antiarrhythmics, especially β-blockers, is encouraged inpatients with LQTS unless contraindications exist. Additional management modalities aretypically based on LQTS genotype and clinical events, and might include class IB sodiumchannel blocker, e.g., mexiletine, other drugs, e.g., verapamil, nicorandil, potassium
Nathan et al. Page 4
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
supplementation, pacemakers, implantable cardioverter-defibrillators, or left cardiacsympathetic denervation (table 1).
Anesthesia Risk in LQTSThe myocardium is richly equipped with various ion channels, which are responsible forregulating the excitability and, secondarily, the contractility of the heart. The effect ofvolatile anesthetics on the cardiac ion channels and currents and the most important sideeffects have been summarized in a review by Huneke13 (table 2). Several studies confirmthese findings in cell and animal models of LQTS. In the heart, IK is important in initiatingrepolarization and therefore plays a key role in controlling the duration of is composed oftwo components: cardiac action potentials. IK a rapidly activating component, IKr, and aslowly activating component, IKs. Propofol is a selective blocker of IKs. Both IKr and IKsplay a crucial role in cardiac repolarization. Propofol inhibits both the ICa and IKs currents.The actual values of changes in APD would represent the sum of the inhibitory effects ofpropofol on ICa and IKs.14 Anesthetic drugs seem to be genotype-specific in terms of theeffects on QT prolongation in an animal model of impaired repolarization reserve. Drugsthat selectively block IKs prolong the QT interval only in an LQT2 rabbit model and not inLQT1 rabbits, which lack IKs. Drugs that block IK1 prolong the QT in both LQT1 and LQT2rabbits because of their reduced repolarization reserve. However, both LQT1 and LQT2models developed polymorphic ventricular tachycardia under isoflurane and propofol,indicating the heightened risk of arrhythmia when using IKs blockers in patients with areduced repolarization reserve because of decreased IKr currents.15 Therefore, genotyping ofLQT patients could allow genotype-specific anesthetic plans that would improveperioperative safety for patients. Interestingly, ketamine does not alter cardiac repolarizingcurrents or the QT interval in the LQT rabbit model. Although sevoflurane significantlyprolonged the QTc in normal children (American Society of Anesthesiologists I-II) incomparison with propofol, neither compound produced any change in the Tp-e interval orTDR.16 This was corroborated by a study on healthy children in whom propofol did notincrease TDR at clinically relevant doses.17 The use of volatile anesthesia in patients withLQTS is an unresolved clinical issue. 18–20 Among the barbiturates, thiopental sodiumprolongs QTc in healthy premedicated adults and children.21 Though QTc is prolonged bypentobarbital, TDR is reduced, reducing arrhythmogenicity.22 Of the benzodiazepines,midazolam has no effect on QTc.23,24
Succinylcholine and pancuronium are known to prolong the QTc, whereas vecuronium andatracurium do not.25 The use of anticholinesterase–anticholinergic combination to achievereversal of neuromuscular blockade might place patients at a higher risk of arrhythmias. Theanticholinergics prolong QTc in healthy volunteers and adults.26 Anticholinesterases bythemselves could induce bradycardia and pause dependent arrhythmias in susceptiblesubtypes.
Other factors that could affect the QTc interval could do so intrinsically, or by increasingsympathetic tone (e.g., hypoxia, hypercarbia, light anesthesia, tracheal intubation, oremergence phenomena). Hypothermia and hypothyrodism prolong QTc interval. Changes inelectrolyte balance such as hypokalemia, hypomagnesemia, and hypocalcemia couldprecipitate arrhythmias and should be aggressively treated. Agents or maneuvers thatproduce bradycardia should be avoided in LQT3 patients.
There is a positive correlation between the cardiotoxic potency of local anesthetics, lipidsolubility, and nerve-blocking potency.27,28 Local anesthetic agents exert their effects boththerapeutic and toxic through voltage-gated sodium channels in the myocardium andnervous system. Bupivacaine binds more rapidly and longer than lidocaine to cardiac NaVchannels. There is stereospecificity in the cardiotoxicity of local anesthetics with R-isomers
Nathan et al. Page 5
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
binding cardiac NaV channels more avidly than S-isomers (levobupivacaine andropivacaine).27 Local anesthetics inhibit cardiac conduction with the same rank order ofpotency as for nerve block (prilocaine ≤ lidocaine ≤ mepivacaine ≤ ropivacaine ≤levobupivacaine ≤ racemic bupivacaine ≤ R (+) bupivacaine = etidocaine = tetracaine) andproduce dose-dependent myocardial depression. Bupivacaine-induced tachyarrhythmiashave been concluded to be because of dispersion of conduction and dispersion ofrefractoriness of ventricular myocardium predisposing to reentrant ventricular arrhythmias.Hyperkalemia might enhance the cardiotoxicity of local anesthetics; whereas adenosinetriphosphate-sensitive potassium channel openers, β-adrenergic agonists, and Ca2+ channelblockers may have value in treating bupivacaine cardiotoxicity.
The Risk of Perioperative Adverse EventsIn an attempt to describe perioperative risk factors in patients with LQTS, a retrospectivecohort study of children with LQTS undergoing general anesthesia for noncardiac surgery ordevice was conducted at The Children’s Hospital of Philadelphia, Philadelphia,Pennsylvania. Seventy six patients with congenital LQTS were identified who had a total of114 anesthetic encounters. Of the 114 anesthetic encounters, there were three AE, twodefinite and one probable AE for an incidence of 2.6%. The events occurred in boys (aged11, 13, 15 yr), while undergoing noncardiac surgery during volatile general anesthesia. Allwere receiving β-blocker therapy preoperatively. The AE occurred in close proximity to theadministration of reversal agents (anticholinesterase–anticholinergic combinations) and theantiemetic ondansetron. The events occurred during emergence from anesthesia, andexclusively in the group who received both reversal agents and ondansetron. All weretreated successfully with short-term antiarrhythymic drug therapy and discharged thefollowing morning.29 We concluded that there is an increased risk of AE during periods ofenhanced sympathetic activity, especially emergence, which seems to be further enhanced ifagents that are known either to prolong the corrected QT interval (QTc) or the TDR orincrease the incidence of tachycardia are administered at this time. Restriction ofmedications that adversely affect ion channels, and intense vigilance and monitoring duringthis time and in the postoperative phase, might help prevent occurrence or progression ofAE. Our ongoing research involves genetic subtyping, monitoring of electrocardiographicchanges in response to exposure to commonly used drugs during anesthesia, and correlationof AE with specific anesthetic drugs and genetic subtypes in an effort to increaseunderstanding of anesthesia related risks in children with congenital LQTS.
The Risk of Adverse Events in Patients with LQTS in Relationship to PerioperativeMedications
Several commonly used drugs in the perioperative period have been shown to increase therisk of ventricular arrhythmias.30,31 Prolongation of the QT interval is the primary reason forwithdrawal or restriction of drugs during the past 10 yr. Of the perioperative medications,antibiotics, gastric prokinetics, antiemetics, neuromuscular blockers, and reversal agents,anticholinergics, are all associated with the potential to prolong the QTc interval.32 The risksare because of intrinsic blockade of K+ efflux (esp IKr), drug- drug interactions,coadministration of concomitant medications that prolong QTc or that inhibit metabolismresulting in toxic levels of drug, and medications that affect electrolyte balance especiallyextracellular potassium levels. Patient factors increase this risk in the presence of “cardiacion channelopathies” with reduced repolarization reserve, e.g., LQTS, female sex,electrolyte imbalance (hypokalemia/hypomagnesemia), bradycardia relative to age,symptomatic arrhythmias, renal/hepatic dysfunction, and structural heart disease.
QT prolongation has become a surrogate marker for arrhythmogenicity and is used inresearch and by regulatory authorities. Risk is associated with an absolute QTc of more than
Nathan et al. Page 6
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
500 ms, or change in QT of 30–60 ms.33 The FDA has issued guidance for industry for QTinterval prolongation and proarrhythmic potential of nonantiarrhythmic drugs. Agents thatprolong the mean QT/QTc in a study group by more than 5ms are considered to havesubstantial proarrhythmic potential per the “thorough QT/QTc study” protocol. It is not justthe prolongation of QTc interval but also the occurrence of morphologic T wave changesand increase in TDR that seem to predispose to arrhythmogenecity.
Of the antiemetics commonly used, all 5HT3 antagonists and all first-generation and somesecond-generation antihistaminics and the butyrophenone derivatives are associated withQTc prolongation at clinically used doses. In an in vitro electrophysiology model, the 5HT3antagonists cause blockage of Na2+ channels in the inactive state, especially with high heartrates or when depolarized or ischemic myocardium is present. Electrocardiographic changesoccur as a class effect in a dose-dependent phenomenon. Dolasetron is associated withprolongation of PR, QRS, and QTc, and ondansetron causes prolongation of the JT and QTcintervals.34 QTc prolongation is about 15 ms and occurs 0–4 h following drug, and isreversible in 24 h. Though not yet licensed for pediatric use, palonosetron might be theexception in not prolonging the QTc interval. Dexamethasone, dimenhydrinate, andmetoclopramide do not prolong the QTc and might be safe in children with LQTS. Theseobservations support the judicious and careful choice of antiemetics.
Knowledge GapCan we minimize anesthesia-related risk? There seems to be an increase in the observedincidence of AE during periods of enhanced sympathetic activity (LQT1), especiallyemergence from anesthesia conducted with volatile anesthetics in association with the use ofanticholinesterase–anticholinergic drug combinations and the antiemetic ondansetron inchildren with congenital LQTS. This risk seems to be further enhanced if agents that areknown to either prolong QTc or TDR or increase the incidence of tachycardia areadministered at times of sympathetic stimulation. Avoidance of offending pharmacologicagents and intense vigilance and monitoring during this time and in the postoperative phasecould help prevent occurrence or progression of AE. The anesthetic management of childrenwith LQTS has been reviewed excellently in an article by Booker et al. (table 3). A list ofdrugs that are known to prolong the QTc interval is available and regularly updated.||
Preoperative assessment should include assessment of medications used for the treatment ofLQTS/arrhythmias and other conditions, especially psychotropic medications. Druginteractions and cumulative toxicity should be considered in the formulation of a safeanesthetic plan.
The occurrence of TdP in children with LQTS often necessitates early use of magnesium ina slight modification of the ACLS protocol for the management of pulseless ventriculartachycardia or fibrillation.35 Also, the avoidance of bradycardia is judicious in patients withLQT2 and LQT3 related to pause-dependent arrhythmias. We speculate that geneticsubtyping of patients with LQTS could help formulate individualized anesthetic plans forthese high-risk patients. It is likely that patients with LQTS with lethal arrhythmias that canbe triggered by sympathetic stimuli, anxiety, fright, and loud noise could be at a higher riskof arrhythmias at the time of emergence when all these factors occur in concert. In addition,drugs that are commonly used during emergence may act in synergy with these triggers andfurther prolong the QTc to precipitate a ventricular arrhythmia. It is also important torecognize that some of the drugs use to treat ventricular arrhythmia, especially the type IIIantiarrhythmic amiodarone and the type I antiarrhythmic quinidine, further prolong the QTc
||www.qtdrugs.org. Accessed January 6, 2012.
Nathan et al. Page 7
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
and worsen the existing arrhythmia. Onset of TdP in children with LQTS often necessitatesearly use of intravenous magnesium and electrical cardioversion/defibrillation.35
Management of TdPWith onset of TdP, magnesium should be administered intravenously at a bolus dose of 30mg/kg during 2 or 3 min, followed by an infusion of 2–4 mg/h. If initial dosing and infusiondo not suppress the episodes of TdP, the magnesium bolus should be repeated after 15 min.In the event of sustained TdP or TdP that degenerates into ventricular fibrillation, direct-current cardioversion or defibrillation will have to be performed. In some forms of LQTS,medical therapy includes lidocaine. Early use of 1 or 2 mg/kg boluses of lidocaine eitherbefore magnesium or with magnesium might prevent progression of the arrhythmia.Occasionally, the use of an isoproterenol infusion or transvenous pacing at 90–110 beat/minincreases the patient’s heart rate and prevents pause-induced TdP. 35 It is especiallyimportant to recognize that antiarrhythmics can prolong the QTc interval in patients withLQTS, and it is best to consult early with electrophysiologists during the management ofarrhythmias in this group of patients.
AcknowledgmentsThe authors thank David R. Jobes, M.D., Professor, Anesthesiology & Critical Care, Perelman School of Medicine,University of Pennsylvania, The Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania, for his efforts inreviewing and editing the manuscript.
References1. Kies SJ, Pabelick CM, Hurley HA, White RD, Ackerman MJ. Anesthesia for patients with
congenital long QT syndrome. Anesthesiology. 2005; 102:204–10. [PubMed: 15618804]
2. Booker PD, Whyte SD, Ladusans EJ. Long QT syndrome and anaesthesia. Br J Anaesth. 2003;90:349–66. [PubMed: 12594150]
3. Shimizu W. The long QT syndrome: Therapeutic implications of a genetic diagnosis. CardiovascRes. 2005; 67:347–56. [PubMed: 15979599]
4. Splawski I, Timothy KW, Decher N, Kumar P, Sachse FB, Beggs AH, Sanguinetti MC, KeatingMT. Severe arrhythmia desflurane disorder caused by cardiac L-type calcium channel mutations.Proc Natl Acad Sci U S A. 2005; 102:8089–96. [PubMed: 15863612]
5. Shimizu W, Antzelevitch C. Cellular basis for the ECG features of the LQT1 form of the long-QTsyndrome: Effects of β-adrenergic agonists and antagonists and sodium channel blockers ontransmural dispersion of repolarization and torsade de pointes. Circulation. 1998; 98:2314–22.[PubMed: 9826320]
6. Shimizu W, Antzelevitch C. Differential effects of β-adrenergic agonists and antagonists in LQT1,LQT2 and LQT3 models of the long QT syndrome. J Am Coll Cardiol. 2000; 35:778–86. [PubMed:10716483]
7. Roden DM. Pharmacogenetics and drug-induced arrhythmias. Cardiovasc Res. 2001; 50:224–31.[PubMed: 11334826]
8. Zhang L, Timothy KW, Vincent GM, Lehmann MH, Fox J, Giuli LC, Shen J, Splawski I, Priori SG,Compton SJ, Yanowitz F, Benhorin J, Moss AJ, Schwartz PJ, Robinson JL, Wang Q, Zareba W,Keating MT, Towbin JA, Napolitano C, Medina A. Spectrum of ST-T-wave patterns andrepolarization parameters in congenital long-QT syndrome: ECG findings identify genotypes.Circulation. 2000; 102:2849–55. [PubMed: 11104743]
9. Priori SG, Schwartz PJ, Napolitano C, Bloise R, Ronchetti E, Grillo M, Vicentini A, Spazzolini C,Nastoli J, Bottelli G, Folli R, Cappelletti D. Risk stratification. N Engl J Med. 2003; 348:1866–74.[PubMed: 12736279]
10. Goldenberg I, Moss AJ, Peterson DR, McNitt S, Zareba W, Andrews ML, Robinson JL, LocatiEH, Ackerman MJ, Benhorin J, Kaufman ES, Napolitano C, Priori SG, Qi M, Schwartz PJ,Towbin JA, Vincent GM, Zhang L. Risk factors for aborted cardiac arrest and sudden cardiac
Nathan et al. Page 8
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
death in children with congenital long-QT syndrome. Circulation. 2008; 117:2184–91. [PubMed:18427136]
11. Antzelevitch C. Heterogeneity and cardiac arrhythmias: An overview. Heart Rhythm. 2007; 4:964–72. [PubMed: 17599687]
12. Moss AJ, Zareba W, Hall WJ, Schwartz PJ, Crampton RS, Benhorin J, Vincent GM, Locati EH,Priori SG, Napolitano C, Medina A, Zhang L, Robinson JL, Timothy K, Towbin JA, AndrewsML. Effectiveness and limitations of β-blocker therapy in congenital long-QT syndrome.Circulation. 2000; 101:616–23. [PubMed: 10673253]
13. Hüneke R, Fassl J, Rossaint R, Lückhoff A. Effects of volatile anesthetics on cardiac ion channels.Acta Anaesthesiol Scand. 2004; 48:547–61. [PubMed: 15101848]
14. Hatakeyama N, Sakuraya F, Matsuda N, Kimura J, Kinoshita H, Kemmotsu O, Yamazaki M,Hattori Y. Pharmacological signifcance of the blocking action of the intravenous generalanesthetic propofol on the slow component of the cardiac delayed rectifier K+ current. JPharmacol Sci. 2009; 110:334–43. [PubMed: 19571462]
15. Odening KE, Hyder O, Chaves L, Schofield L, Brunner M, Kirk M, Zehender M, Peng X, KorenG. Pharmacogenomics of anesthetic drugs in transgenic LQT1 and LQT2 rabbits reveal genotype-specific differential effects on cardiac repolarization. Am J Physiol Heart Circ Physiol. 2008;295:H2264–72. [PubMed: 18835916]
16. Whyte SD, Booker PD, Buckley DG. The effects of propofol and sevoflurane on the QT intervaland transmural dispersion of repolarization in children. Anesth Analg. 2005; 100:71–7. [PubMed:15616054]
17. Hume-Smith HV, Sanatani S, Lim J, Chau A, Whyte SD. The effect of propofol concentration ondispersion of myocardial repolarization in children. Anesth Analg. 2008; 107:806–10. [PubMed:18713888]
18. Güler N, Kati I, Demirel CB, Bilge M, Eryonucu B, Topal C. The effects of volatile anesthetics onthe Q-Tc interval. J Cardiothorac Vasc Anesth. 2001; 15:188–91. [PubMed: 11312477]
19. Kang J, Reynolds WP, Chen XL, Ji J, Wang H, Rampe DE. Mechanisms underlying the QTinterval-prolonging effects of sevoflurane and its interactions with other QT-drugs.Anesthesiology. 2006; 104:1015–22. [PubMed: 16645454]
20. Yildirim H, Adanir T, Atay A, Katircioğlu K, Savaci S. The on QT effects of sevoflurane,isoflurane and interval of the ECG. Eur J Anaesthesiol. 2004; 21:566–70. [PubMed: 15318470]
21. McConachie I, Keaveny JP, Healy TE, Vohra S, Million L. Effect of anaesthesia on the QTinterval. Br J Anaesth. 1989; 63:558–60. [PubMed: 2605073]
22. Antzelevitch C, Fish J. Electrical heterogeneity within the ventricular wall. Basic Res Cardiol.2001; 96:517–27. [PubMed: 11770069]
23. Michaloudis DG, Kanakoudis FS, Petrou AM, Konstantinidou AS, Pollard BJ. The effects ofmidazolam or propofol followed by suxamethonium on the QT interval in humans. Eur JAnaesthesiol. 1996; 13:364–8. [PubMed: 8842657]
24. Michaloudis DG, Kanakoudis FS, Xatzikraniotis A, Bischiniotis TS. The effects of midazolamfollowed by administration of either vecuronium or atracurium on the QT interval in humans. EurJ Anaesthesiol. 1995; 12:577–83. [PubMed: 8665880]
25. Saarnivaara L, Klemola UM, Lindgren L. QT interval of the ECG, heart rate and arterial pressureusing five non-depolarizing muscle relaxants for intubation. Acta Anaesthesiol Scand. 1988;32:623–8. [PubMed: 2905566]
26. Saarnivaara L, Simola M. Effects of four anticholinesterase-anticholinergic combinations andtracheal extubation on in the long-QT syndrome. QTc interval of the ECG, heart rate and arterialpressure. Acta Anaesthesiol Scand. 1998; 42:460–3. [PubMed: 9563867]
27. Butterworth JF. 4th: Models and mechanisms of local anesthetic cardiac toxicity: A review. RegAnesth Pain Med. 2010; 35:167–76. [PubMed: 20301823]
28. Heavner JE. Cardiac toxicity of local anesthetics in the intact isolated heart model: A review. RegAnesth Pain Med. 2002; 27:545–55. [PubMed: 12430103]
29. Nathan AT, Berkowitz DH, Montenegro LM, Nicolson SC, Vetter VL, Jobes DR. Implications ofanesthesia in children with long QT syndrome. Anesth Analg. 2011; 112:1163–8. [PubMed:21346158]
Nathan et al. Page 9
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
30. Charbit B, Alvarez JC, Dasque E, Abe E, Démolis JL, Funck-Brentano C. Droperidol andondansetron-induced QT interval prolongation: A clinical drug interaction study. Anesthesiology.2008; 109:206–12. [PubMed: 18648229]
31. Charbit B, Albaladejo P, Funck-Brentano C, Legrand M, Samain E, Marty J. Prolongation of QTcinterval after postoperative nausea and vomiting treatment by droperidol or ondansetron.Anesthesiology. 2005; 102:1094–100. [PubMed: 15915019]
32. Kao LW, Furbee RB. Drug induced q-T prolongation. Med Clin N Am. 2005; 89:1125–44.[PubMed: 16227057]
33. De Ponti F, Poluzzi E, Cavalli A, Recanatini M, Montanaro N. Safety of non-antiarrhythmic drugsthat prolong the QT interval or induce torsades de pointes: An overview. Drug Saf. 2002; 25:263–86. [PubMed: 11994029]
34. Navari RM, Koeller JM. Electrocardiographic and cardiovascular effects of the 5-hydroxytryptamine3 receptor antagonists. Ann Pharmacother. 2003; 37:1276–86. [PubMed:12921512]
35. Homme JH, White RD, Ackerman MJ. Management of ventricular fibrillation or unstableventricular tachycardia in patients with congenital long-QT syndrome: A suggested modificationto ACLS guidelines. Resuscitation. 2003; 59:111–5. [PubMed: 14580741]
Nathan et al. Page 10
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig. 1.Baseline electrocardiogram (ECG) and T wave alternans in a patient with Timothysyndrome.
Nathan et al. Page 11
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig. 2.Subtype-specific ST-T wave morphology in the long QT syndrome genotypes. Reproducedwith permission: Zhang L, Timothy KW, Vincent GM, Lehmann MH, Fox J, Giuli LC, ShenJ, Splawski I, Priori SG, Compton SJ, Yanowitz F, Benhorin J, Moss AJ, Schwartz PJ,Robinson JL, Wang Q, Zareba W, Keating MT, Towbin JA, Napolitano C, Medina A:Spectrum of ST-T-wave patterns and repolarization parameters in congenital long-QTsyndrome: ECG findings identify genotypes. Circulation 2000; 102:2849–55.
Nathan et al. Page 12
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig. 3.Cellular ionic currents and action potentials in long QT syndrome. IKs = delayed rectifier;INa = sodium current.
Nathan et al. Page 13
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Fig. 4.Heterogeneity of repolarization. AV node = atrio ventricular node; SA node = sino atrialnode.
Nathan et al. Page 14
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Nathan et al. Page 15
Tabl
e 1
Ioni
c C
urre
nts,
Pro
tein
s, a
nd G
enes
Ass
ocia
ted
with
LQ
TS;
Ass
ocia
ted
Tri
gger
s an
d Po
ssib
le T
hera
pies
LQ
TS
Typ
eP
rote
inP
rote
in T
ype
Gen
eC
urre
nt
Pre
vale
nce
ofG
enot
yped
Cas
es*
Tri
gger
sP
ossi
ble
The
rapi
es
LQ
T1
Kv7
.1K
+ c
hann
el (
I Ks)
sub
unit
KC
NQ
1↓
I Ks
50–6
0%E
xerc
ise
β-bl
ocke
rs
Swim
min
gC
lass
IB
sod
ium
cha
nnel
bloc
ker,
mex
iletin
e
Sym
path
etic
stim
ulat
ion
Pace
mak
ers
—Im
plan
tabl
e ca
rdio
vert
er-
defi
brill
ator
(IC
D)
—L
eft c
ardi
ac s
ympa
thet
icde
nerv
atio
n
LQ
T2
Kv1
1.1
K+ c
hann
el (
I Kr)
sub
unit
KC
NH
2↓
I Kr
30–4
0%St
artle
β-bl
ocke
rs +
con
junc
tive
ther
apy
Aud
itory
stim
ulus
Pota
ssiu
m a
dmin
istr
atio
n
Post
part
umPa
cem
aker
s
—IC
D
—L
eft c
ardi
ac s
ympa
thet
icde
nerv
atio
n
LQ
T3
Na v
1.5
Na
2+ c
hann
el (
I Na)
sub
unit
SCN
5A↑
I Na
5–10
%Sl
eep
Cla
ss I
B s
odiu
m c
hann
elbl
ocke
r, m
exile
tine,
inco
njun
ctio
n w
ith β
-blo
cker
sor
IC
D
Res
tPa
cem
aker
s
—IC
D
—L
eft c
ardi
ac s
ympa
thet
icde
nerv
atio
n
LQ
T4
Ank
yrin
-BM
embr
ane
anch
orin
g/ad
apte
r pr
otei
nA
NK
2L
oss
of f
unct
ion
<1%
Exe
rcis
eβ-
bloc
kers
Men
tal s
tres
sIC
D
LQ
T5
min
KK
+ c
hann
el (
I Ks)
βsu
buni
tK
CN
E1
↓ I K
sA
ppro
xim
atel
y 1%
—β-
bloc
kers
Cla
ss I
B s
odiu
m c
hann
elbl
ocke
r, m
exile
tine
Oth
er d
rugs
: ver
apam
il(I
Ca-
L);
nic
oran
dil (
I K-A
TP)
Pace
mak
ers
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Nathan et al. Page 16
LQ
TS
Typ
eP
rote
inP
rote
in T
ype
Gen
eC
urre
nt
Pre
vale
nce
ofG
enot
yped
Cas
es*
Tri
gger
sP
ossi
ble
The
rapi
es
Lef
t car
diac
sym
path
etic
dene
rvat
ion
ICD
LQ
T6
miR
P1K
+ c
hann
el (
I Kr)
βsu
buni
tK
CN
E2
↓ I K
r<
1%—
β-bl
ocke
rs +
con
junc
tive
ther
apy
with
IB s
odiu
mch
anne
l blo
cker
,m
exile
tine,
or
I Ca-
L c
hann
elbl
ocke
r, v
erap
amil
Pota
ssiu
m a
dmin
istr
atio
n
Age
nts
that
blo
ck I K
r
curr
ent
Pace
mak
ers
ICD
And
erse
n-T
awil
synd
rom
e
L
QT
7 (A
TS1
)K
ir2.
1K
+ c
hann
el (
I K1)
sub
units
KC
NJ2
↓ I K
150
% o
f A
nder
sen-
Taw
il ca
ses
Hyp
okal
emia
Pota
ssiu
m S
uppl
emen
tatio
n
β-bl
ocke
rs
I Ca-
L c
hann
el b
lock
er,
vera
pam
il
Lef
t car
diac
sym
path
etic
dene
rvat
ion
ICD
Tim
othy
syn
drom
e
L
QT
8C
av1.
2L
type
Ca2+
cha
nnel
(I C
a, L
) su
buni
tC
AC
NA
1C↑
I Ca-
L<
1% o
f T
imot
hysy
ndro
me
case
s—
β-bl
ocke
rs
I Ca-
L c
hann
el b
lock
er,
vera
pam
il
ICD
L
QT
9C
aveo
lin-3
Cav
eola
e co
at p
rote
inC
AV
3↑
I Na
<1%
——
L
QT
10N
a Vβ4
Na
2+ c
hann
el β
sub
unit
SCN
4B↑
I Na
Rar
e—
—
L
QT
11Y
otia
oA
-kin
ase
anch
or p
rote
in 9
/ada
pter
prot
ein
AK
AP9
Los
s of
fun
ctio
nR
are
——
L
QT
12α
-1-s
yntr
ophi
nM
embr
ane
scaf
fold
SNT
A1
↑ I N
aR
are
——
Jerv
ell a
nd L
ange
-Nie
lsen
synd
rom
e
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Nathan et al. Page 17
LQ
TS
Typ
eP
rote
inP
rote
in T
ype
Gen
eC
urre
nt
Pre
vale
nce
ofG
enot
yped
Cas
es*
Tri
gger
sP
ossi
ble
The
rapi
es
JL
N1
Kv7
.1K
+ s
ubun
it ch
anne
l (I K
s)K
CN
Q1
↓ I K
s80
% o
f Je
rvel
l and
Lan
ge-N
iels
enca
ses
——
JL
N2
Min
KK
+ s
ubun
it ch
anne
l (I K
s)K
CN
E1
↓ I K
s20
%—
—
Arr
ows
in C
urre
nt c
olum
n in
dica
te in
crea
sed/
gain
of
func
tion
(up
arro
w)
or d
ecre
ased
/loss
of
func
tion
(dow
n ar
row
) cu
rren
t rel
ativ
e to
nor
mal
fun
ctio
n.
* For
LQ
T1–
LQ
T6,
pre
vale
nce
valu
es a
re r
elat
ive
to a
ll L
QT
S ca
ses
that
can
be
geno
type
d; f
or n
amed
sub
type
s, p
reva
lenc
e va
lues
are
rel
ativ
e to
all
case
s w
ithin
that
sub
type
.
ICD
= im
plan
tabl
e ca
rdio
vert
er d
efib
rilla
tor;
LQ
TS
= lo
ng Q
T s
yndr
ome.
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Nathan et al. Page 18
Table 2
Summary of the Actions of Volatile Anesthetics on Various Ion Currents in the Heart and the Most ImportantSide Effects of the Drugs
Target Effect Anesthetic Agent Cardiac Side Effects
L-type Ca2+ current Inhibition Halothane, sevoflurane, isoflurane Reduced contractility
Shortened APD and refractory time
β-adrenergic regulation of the L-typeCa2+ current
Complex interference Halothane Enhanced proarrhythmicity
Voltage-dependent transient outwardK+ current
Inhibition Halothane, isoflurane Shortened APD, APD mismatch withinthe heart
Voltage-dependent sustainedoutward K+ current
Inhibition Halothane, isoflurane, sevoflurane Delayed repolarization, mismatch ofAPD
ATP-dependent K+ current Enhancement Isoflurane, sevoflurane Myocardial preconditioning
Fast Na+ current Inhibition Halothane, isoflurane, sevoflurane Slowed conduction
Induction of tachyarrhythmias
Reproduced with permission: Hüneke R, Fassl J, Rossaint R, Lückhoff A: Effects of volatile anesthetics on cardiac ion channels. Acta AnaesthesiolScand. 2004; 48:547–61.
APD = action-potential duration; ATP = adenosine triphosphate.
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Nathan et al. Page 19
Table 3
Anesthetic Management of Patients with LQTS
PerioperativeManagement:GuidingPrinciples
1 Preoperative Assessment
i. 12-lead ECG; Calculation of QTc at baseline
ii. Adequacy of electrophysiology/antiarrhythmic therapy, e.g., adequate heart rate control on β-blockade in LQT1
iii. Device: Pacemaker/ICD interrogation to determine settings and function
iv. Electrophysiology (EP) consult, especially in patients with:
History of aborted sudden cardiac death
History of syncope
Recently diagnosed LQTS
Significant pauses on the ECG (might require pacing)
Emergent surgery
Recommendations for prophylaxis or emergent treatment of LQTS related arrhythmias.
v. Maintenance of normal acid-base and electrolyte balance, especially K+ and Mg+
vi. Review of agents that prolong the QTc*
2 Premedication/Preoperative Management
i. Continue therapy, especially b-blockers
ii. Electrophysiology recommendation for drug therapy if patient is newly diagnosed and not on therapy
iii. Perioperative anxiolysis, e.g., midazolam probably safe
iv. Maintain adequate preoperative hydration
3 Considerations of Anesthesia Care
Monitoring
i. Standard ASA monitoring prior to induction of anesthesia (minimum of 3-lead ECG)
ii. Consideration for invasive vascular monitoring in case of extensive surgery, fluid and electrolyteshifts, or variations of autonomic tone (arterial ± central venous monitoring)
iii. Extreme vigilance at critical time-points of enhanced stress or changes in autonomic tone, e.g.,induction, intubation, emergence, and during surgical stimulation irrespective of type of anestheticused
Minimization of sympathetic stimulation, and avoidance of autonomic imbalance
i. Consider topical local anesthetic (lidocaine) to vocal cords, esmolol bolus for laryngoscopy/endotracheal intubation if heart rate is poorly controlled
ii. Ensure adequate analgesia perioperatively
iii. Regional anesthesia when appropriate (avoid epinephrine in local anesthetic solutions)
iv. Extubation under deep anesthesia or with esmolol prophylaxis if possible
v. Maintenance of normal homeostasis: normothermia, normoxia, normocapnia, normoglycemia
vi. Avoidance of bradycardia in pause-induced states of TdP, e.g., LQT3 patients
Induction/maintenance of anesthesia
i. Anesthetic agents: Caution with use of volatile anesthesia or total intravenous anesthesia
ii. Intravenous induction with thiopental or propofol probably safe, consider total intravenousanesthesia if appropriate
Neuromuscular blockade
i. Vecuronium/Cis atracurium probably safe if necessary for surgery
ii. Avoidance of reversal of neuromuscular blockade, i.e.., anticholinesterase/anticholinergic agents ifpossible.
Anesthesiology. Author manuscript; available in PMC 2013 November 01.
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
NIH
-PA Author Manuscript
Nathan et al. Page 20
Ventilation strategy
i. Maintain normocapnia and normal acid base status (be aware of the effect of hyperventilation onserum K+ concentration)
ii. Avoid Valsalva maneuvers/sustained high intrathoracic pressures, because these increase the QTc
iii. Optimize ventilation strategy, i.e., avoid high peak and end expiratory pressures, prolongedinspiratory times/pauses, and low or reversed I:E ratios.
Prophylaxis and treatment of postoperative nausea and vomiting
i. Avoidance of conditions that increase PONV: ensure adequate hydration, regional/nerve blocktechniques to minimize narcotics, avoid hypotension, propofol-based TIVA in patients at high risk ofPONV
ii. Choice of agents that have minimal effect on QT interval for PONV prophylaxis: of note, all agentsof the 5HT3 antagonist class can prolong QTc, as do antihistaminics and butyrophenones.
Cautious use of such agents and avoidance of using two agents that can prolong QTc is important.Dexamethasone does not prolong QTc, and could be a safe antiemetic.
Recovery
i Continuous ECG monitoring/telemetry in a high-dependency area during recovery from anesthesia
ii Recovery in a quiet environment
iv Continue adequate β-blockade/genotype directed therapy postoperatively
v Gradual mobilization as tolerated by patient
Modified and adapted from Booker PD, Whyte SD, Ladusans EJ: Long QT syndrome and anaesthesia. Br J Anaesth 2003; 90:349–66.
*http://www.azcert.org/medical-pros/drug-lists/drug-lists.cfm. Accessed September 21, 2012.
ASA = American Society of Anesthesiologists; ECG = electrocardiogram; I:E ratio = ratio of the duration of inspiration to the duration ofexpiration; ICD = implantable cardioverter defibrillator; LQTS = long QT syndrome; PONV = postoperative nausea and vomiting; QTc = correctedQT interval; TdP = torsades de pointes.
Anesthesiology. Author manuscript; available in PMC 2013 November 01.