Carbohydrate nutrition and development of adiposity during adolescence
Transcript of Carbohydrate nutrition and development of adiposity during adolescence
Reformatted author version Page 1
Carbohydrate Nutrition and Development of Adiposity During Adolescence
Bamini Gopinath1, Victoria M Flood2, Elena Rochtchina1, Louise A. Baur3,4, Jimmy Chun Yu Louie1,2,5, Wayne Smith6, Paul Mitchell1 1Centre for Vision Research, Department of Ophthalmology and Westmead Millennium Institute, University of Sydney, New South Wales, Australia. 2Faculty of Health and Behavioural Sciences, University of Wollongong, Sydney, New South Wales, Australia 3University of Sydney Clinical School, The Children’s Hospital at Westmead, Sydney, New South Wales, Australia 4School of Public Health, University of Sydney, Sydney, New South Wales, Australia 5Boden Institute of Obesity, Nutrition, Exercise and Eating Disorders, University of Sydney, Sydney, New South Wales, Australia 6School of Medicine and Public Health, University of Newcastle, Newcastle, New South Wales, Australia
Abstract
Objective: To examine the prospective association between glycemic index, glycemic load (GL) of diets and intakes of carbohydrates, sugars, fiber, and the main carbohydrate containing food groups (e.g., soft drinks) with changes in percent body fat, body mass index (BMI), and waist circumference among adolescents. Design and Methods: Students aged 12 at baseline (n = 856) were examined both in 2004-2005 and 2009-2011. A semiquantitative food frequency questionnaire was administered. Anthropometric parameters were measured and defined using standardized protocols. Results: After multivariable adjustment, in girls, each 1-SD increase in dietary GL was associated with concurrent 0.77 kg/m2 and 1.45 cm increase in BMI and waist circumference, respectively (both P = 0.01). Conversely, each 1-SD increase in dietary fiber intake was associated with a concurrent 0.44 kg/m2 decrease in mean BMI in girls (P = 0.02) and 1.45 cm decrease in waist circumference in boys (P = 0.002). Girls who consumed soft drinks once or more per day versus those who never/rarely consumed soft drinks, had a 4.45% increase in percent body fat after 5 years (Ptrend = 0.01). Conclusions: High-GL foods might adversely influence development of body composition, particularly in girls, whereas fiber-rich diets could limit excess weight during adolescence. Obesity 2013. [Epub ahead of print]. doi: 10.1002/oby.20405
Introduction
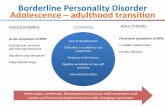
The tracking of adiposity in childhood and adolescence is quite strong (1), and many behaviors adopted in childhood and adolescence also track into adulthood. It is therefore important to assess the roles of modifiable behaviors (diet, physical inactivity) on adolescent adiposity (2). Carbohydrate nutrition, including dietary glycemic index (GI) and glycemic load (GL) of foods consumed, has been the recent focus of research to increase understanding of its impact on health outcomes.
Only the epidemiological study by Cheng et al. (3) investigated the association between dietary GI and GL intakes with change in percent body fat (%BF) and BMI among adolescents. In this German population-based study of 215 children aged nine at baseline who were subsequently followed over four years, dietary GI, GL, and fiber intakes were not associated with the development of %BF and BMI during puberty (3). Moreover, only three prospective studies in preadolescents and/or adolescents have examined the association of fiber and wholegrain intakes with the development of body composition (2–4).
Consumption of soft drinks has also increased dramatically in the recent decades, in parallel with increasing prevalence of overweight and obesity (5). Prior studies have provided evidence of a longitudinal relationship between intake of sugar-sweetened beverages and adiposity among children and adolescents (6-9). Further, a study of 196 non-obese girls showed that
consumption of sugar-sweetened beverages was associated with an increase in BMI z-score, but was not related to changes in %BF during adolescence (10). However, a recent quantitative meta-analysis and qualitative review by Forshee et al. (11), found that the association between sugar-sweetened beverages and BMI was near zero, based on the current body of scientific evidence. Additionally, analyses of 38,409 US adults aged 20-74 years showed that elevated BMI values or increased obesity rates were not observed in those frequently compared to those infrequently consuming soft drinks (12). Finally, a recent randomized control study of 103 adolescents (13) showed that decreasing soft drink consumption in the intervention group did not result in an appreciable decrease in BMI.
The authors used a large cohort of schoolchildren who were followed over 5 years to determine the following: 1) the association between baseline dietary intakes of carbohydrates, sugars, fiber, and the GI and GL of foods consumed, and their associations with temporal changes in BMI, %BF, and waist circumference; 2) the relationship between baseline consumption of soft drinks/ cordials and the principal carbohydrate containing food groups (e.g., cereals, potatoes, energy-dense nutrient poor sources of carbohydrates such as cookies) and development of adiposity; and 3) the association between change in dietary intakes of carbohydrate nutrition variables (e.g., carbohydrates, sugars, and soft drinks), and the GI and GL of foods consumed with concurrent changes in anthropometric measures during adolescence.
Reformatted author version Page 2
Subjects and Methods
Study population
The Sydney Childhood Eye Study is a population-based survey of eye conditions in school children living within the Sydney Metropolitan Area, Australia. It was approved by the Human Research Ethics Committee, University of Sydney, the Department of Education and Training, and the Catholic Education Office, New South Wales, Australia (14). We obtained informed written consent from at least one parent of each child, as well as verbal assent from each child before the examinations. The study methods have been previously described (14). Briefly, students of mean age 12.7 years in a stratified random cluster sample of 21 high schools across Sydney were eligible to participate. Stratification was based on socioeconomic status data and led to a proportional mix of public, private, or religious high-schools. Of the 3144 eligible 12-year-old children, 2367 were given parental permission to participate and 2353 underwent examinations (74.9%). Data for the 12-year-old cohort were collected during 2004-2005 and then after 5 years during 2009-2011, when 1213 were re-examined (51.6% of baseline participants). Participants versus nonparticipants were more likely to have tertiary qualified parents and lower BMI, and have a higher consumption of fruits, but less likely to be older and Caucasian.
Dietary data
Dietary data were collected using a 120-item self-administered food frequency questionnaire (FFQ), designed for specific use in Australian children and adolescents (15). An allowance for seasonal variation of fruit and vegetables was made during analysis by weighting seasonal fruits and vegetables. The average daily intake of seasonal fruits and vegetables were calculated by adjusting the number of months per year the fruit was available. The validity of the FFQ has been previously reported in children (15). Briefly, Pearson correlation coefficients were calculated on the data after statistical adjustment (transformation, energy-adjustment, and de-attenuation). To adjust for within-person variation in the food records, de-attenuated correlation coefficients were calculated (16). Values were adjusted for energy by using the residual method (17). The de-attenuated, energy-adjusted Pearson correlation coefficient for carbohydrate and total sugars was 0.47 and 0.41, respectively, with 56% of carbohydrates and 58% of total sugars results ranked within one quintile when compared to weighed food records. Less than 5% of the results were grossly misclassified (i.e., ranked highest by FFQ method and lowest by weighed food records method, or vice-versa).
Corresponding food items from the nutrition composition database (NUTTAB2006) (18) were linked to the FFQ items, and the reported consumption frequencies were taken into account when translating the FFQ responses into actual food and nutrients intake using a purpose built query program in Microsoft Access 2007 based on the formula: (nutrient per 100 g � weight specified on FFQ question × frequency)/ 100. NUTTAB2006, however, does not provide the full range of nutrients of interest, for which we used values from other nutrient databases (19,20). GI values were assigned to individual food items in the FFQ based on previous published methods (21,22). The GL of each food item was calculated as the corresponding GI (as %) × amount (in grams) of available carbohydrates in a serve of that food. The daily dietary GL of each subject was calculated as the sum of GL from various food items, and the dietary GI was obtained by (dietary GL / total available carbohydrate intake in the day) × 100%. Analytical data on fructose were available for >90% of the foods used in the nutrient database. Fructose values were subjectively assigned to
the remaining foods based on their compositions, where recipes were used to determine the ingredients of foods wherever available.
We also extracted data on the fiber contribution from vegetables, fruit, and bread and cereals and on the consumption of main carbohydrate-containing food groups: vegetables, potatoes, fruit, bread, and cereals (comprising breakfast cereals, bread {white or other}, pasta, and rice), as well as foods high in refined sugars or refined starches (soft drinks, cordials, sweet biscuits, cakes, buns, scones, pastries, confectionary, sugar, honey, jams, and syrups), which we term as energy-dense, nutrient poor sources of carbohydrates. Data on the frequency of soft drink, cordial (a sweet flavored concentrated syrup that is mixed with water to taste), and fruit juice consumption, were also obtained from the FFQ.
Assessment of anthropometric measures
Data were collected during a pre-organized visit to each school. Each child’s weight and body fat percentage (utilizing leg--leg bioimpedance analysis) were measured using a Body Composition Analyser (Model TBF-300, Tanita, Tokyo, Japan). The mid-point between the lower rib border and iliac crest functioned as the standardized horizontal plane and was measured using a measuring tape to determine waist circumference in centimeters. Height was measured with shoes off using a freestanding SECA height rod (Model 220, Hamburg, Germany). Weight in kilograms was measured using a standard portable weighing machine, after removing any heavy clothing. BMI was calculated as weight divided by height squared (kg/m2).
Covariate assessment
Parents were asked to complete a comprehensive 193-item questionnaire. Socio-demographic information covering ethnicity, country of birth, education, occupation, and parental age was collected. Parents were also asked whether they or other people living in their home smoked inside the house. This defined the child’s exposure to current passive smoking.
The questions relating to physical activity comprised a list of nine common activities in which school-aged children participate such as athletics, swimming, soccer, etc. Children self-reported the usual number of hours per week they spent in each of these activities and whether the activity was performed outdoors or indoors (hall gym, classroom). The time spent in each activity was summated and the average hours per day spent were calculated separately for outdoor activities, indoor activities, and total activity time (i.e., sum of outdoor and indoor activities). Total screen time (hours/day) was calculated as the time reported that was spent on the following activities: watching TV, playing video games, and use of a computer for recreational and educational purposes.
Statistical analysis
Statistical analyses were performed using SAS (v9.1, SAS Institute, NC). We used mixed models and generalized estimating equations to appropriately model predictors of change in adiposity while accounting for variability attributable to the stratified randomized school-cluster design. The analysis focused on separate models for predicting three adiposity assessments: 1) change in BMI, 2) change in %BF, and 3) change in waist circumference. In each model the primary predictors of change were: carbohydrate nutrition assessments and the main carbohydrate containing food groups. Secondary predictors were the covariates: age, sex, ethnicity, parental education, exposure to passive smoking, change in height, screen viewing time, and time spent in physical activity. Dietary GI, GL, carbohydrates, sugar, and fiber variables were adjusted for total energy intake using the
Reformatted author version Page 3
residual method (17). Intakes of principal carbohydrate containing food groups (e.g., cereals) were energy adjusted by using the energy partition model, that is, consumption was adjusted for the energy intake from all other foods (17).
Linear regression models were used to estimate the slopes (magnitudes) of possible linear relationships between the dietary variables and anthropometric measures. These analyses generated two sets of regression coefficients representing the following: 1) prospective estimate – coefficients in models for predicting dietary variables at baseline on the change in BMI, %BF, and waist circumference at the 5-year follow-up; and 2) concurrent estimate – coefficients in models for predicting change in the dietary variables over the 5 years on the concurrent change in anthropometric measures. The change in dietary variables during the study period was calculated by
subtracting baseline intake from the intake recorded at the 5-year follow-up examination (17).
After multivariable adjustment, linear regression analyses indicated interactions between sex and the associations of soft drinks with %BF (Pinteraction = 0.02) and waist circumference (Pinteraction = 0.01), and potato consumption with BMI (Pinteraction = 0.04). Interactions were also observed between sex and the associations of fructose with BMI (Pinteraction = 0.02), waist circumference (Pinteraction = 0.02), and %BF (Pinteraction = 0.04). Finally, interactions were observed between sex and change in dietary GI and GL with concurrent change in waist circumference (Pinteraction = 0.01) and %BF (Pinteraction = 0.02), respectively. Subsequent analyses of all carbohydrate nutrition variables and the principal carbohydrate containing food groups were therefore stratified by sex.
Characteristics Girls (n = 421) Boys (n = 435) P value
Age, yr 12.7 (0.4) 12.8 (0.5) 0.06
Ethnicity, %
Caucasian 257 (61.1) 290 (66.7) 0.37
East Asian 82 (19.5) 70 (16.1)
Middle Eastern 17 (4.0) 14 (3.2)
Other 65 (15.4) 61 (14.0)
Parental educationa 212 (50.4) 237 (54.5) 0.23
Exposure to passive smoking 75 (17.8) 59 (13.6) 0.09
Height, cm 156.7 (7.1) 156.5 (8.1) 0.69
Weight, kg 49.4 (12.6) 48.8 911.4) 0.48
Body mass index, kg/m2 20.0 (4.1) 19.8 (3.6) 0.50
Waist circumference, cm 65.4 (8.3) 67.0 (7.8) 0.005
Percent body fat, % 23.9 (9.0) 15.8 (7.4) <0.0001
Time spent in screen viewing, h/d 2.50 (1.3) 2.82 (1.5) 0.001
Time spent in physical activity, h/d 0.70 (0.6) 0.99 (0.7) <0.0001
Dietary intake of
Carbohydrate, g/d 254.3 (97.7) 267.3 (99.3) 0.05
Total sugars, g/d 129.2 (55.1) 136.6 (56.9) 0.06
Total fibre, g/d 28.6 (12.9) 28.1 (12.2) 0.61
Glycemic index 54.3 (3.4) 54.3 (3.2) 0.86
Glycemic load 138.0 (53.3) 145.1 (54.2) 0.05
Consumption of
Vegetables, g/d 177.0 (128.5) 149.8 (111.0) 0.001
% contribution to GL (SD) 2.2 (2.1)
Fruits, g/d 249.8 (182.3) 228.9 (178.7) 0.09
% contribution to GL (SD) 11.4 (7.7)
Cereals, g/d 229.6 (121.4) 233.9 (125.3) 0.61
% contribution to GL (SD) 39.4 (14.8)
Energy dense, nutrient poor sources of carbohydrates, g/db 287.6 (245.7) 313.5 (221.0) 0.11
% contribution to GL (SD) 18.8 (9.4)
Soft drinks
Never or rarely 87 (20.7) 56 (12.9) 0.01
Up to once a week 201 (47.9) 212 (48.7)
2-6 times a week 97 (23.1) 126 (29.0)
Once or more a day 35 (8.3) 41 (9.4)
% contribution to GL (SD) 4.5 (5.6)
TABLE 1 Baseline characteristics of 12-year old children (n = 856), stratified by gender
Data are mean (SD) or proportions unless otherwise stated. aTertiary qualified mother and/or father. bIncludes soft drinks, cordials, cookies, cakes, buns, scones, pastries, confectionary, sugar, honey, jams, and syrups
Reformatted author version Page 4
Results
Baseline characteristics of study participants are shown in Table 1. Girls were more likely than boys to have smaller waist circumference and lower soft drink consumption but had higher consumption of vegetables, and spent less time in screen viewing and physical activity. Study characteristics of participants with (n = 856) and without (n = 360) complete data were also compared. Participants with, versus those without complete data were more likely to be Caucasian, older (significant difference in mean age at baseline) and have lower BMI.
Association between carbohydrate nutrition with adiposity among girls only
Nonsignificant associations were observed between baseline consumption of total carbohydrates, total sugars, fiber, and dietary GI and GL with temporal change in the three anthropometric measures (Table 2). Energy-dense nutrient poor sources of carbohydrates (e.g., cookies and cakes) and starch intake at baseline were also not associated with 5-year change in BMI among girls, β=0.06 (P = 0.63) and β=-0.03 (P = 0.77), respectively.
After controlling for all covariates, soft drink consumption remained significantly and positively associated with %BF among girls, that is, girls who consumed one or more soft drinks per day compared to those who never/ rarely drank soft drinks had significantly higher %BF, 3.79 versus -0.66% (Ptrend = 0.01). Although the trend was nonsignificant, girls who consumed one or more soft drinks per day compared to those who never/rarely consumed soft drinks at baseline had a significantly greater increase in BMI (3.20 versus 1.96 kg/m2, P = 0.01) and waist circumference (10.00 versus 6.46 cm, P = 0.004) after 5 years.
We analyzed the relationship between intake changes in dietary variables with concurrent change in BMI, %BF, and waist
circumference. For these particular analyses we had 513 (279 girls and 234 boys) participants with complete data on all covariates included in the multivariable model, as well as anthropometric and FFQ information at both the baseline and 5-year follow-up. Each 1-SD increase in dietary GL was concurrently associated with an increase in both mean BMI (β = 0.77, P = 0.01) and waist circumference (β = 1.45, P = 0.01) in girls over the study period (Table 3). Similarly, each SD increase in carbohydrates was associated with a 0.77 kg/m2 (P = 0.03) and 1.90 cm (P = 0.02) increase in BMI and waist circumference, respectively. In contrast, each 1-SD increase in fiber intake over the 5 years was associated with a concurrent decrease of 0.44 kg/m2 in mean BMI (P = 0.02; Table 3).
Association between carbohydrate nutrition with adiposity among boys only
There were no significant associations observed between most carbohydrate nutrition variables at baseline and anthropometric measures in boys. However, boys in the highest compared to those in the lowest tertile of baseline dietary intake of total sugars, had a lower decline in %BF over the 5 years (Ptrend = 0.02; Table 4). In boys, a marginally significant association was observed with fructose consumption, that is, each 1-SD (1-SD = 10.7) increase in fructose consumption at baseline was associated with 0.52% increase in %BF (P = 0.05) after 5 years. With respect to concurrent change, after multivariable adjustment, each 1-SD (1-SD = 11.8) increase in dietary fiber intake was associated with a concurrent 1.45-cm decrease in waist circumference in boys (P = 0.002). Also, a marginally significant association was observed with energy-dense, nutrient poor sources of carbohydrates, i.e., each 1-SD (1-SD = 215.1) increase in energy-dense, nutrient poor sources of carbohydrates was concurrently associated with a 0.54-cm increase in waist circumference (P = 0.05).
TABLE 2 Association between baseline dietary intakes of carbohydrate nutrition variables with change in mean BMI, percent body fat (%BF) and waist circumference from age 12 to 17 years old among girls (n = 420)
Change in mean BMIa Change in mean %BFa Change in mean waist circumferencea
Nutritional intake (per SD increase) β (SE) P β (SE) P β (SE) P
Glycemic index (1-SD = 3.3) -0.06 (0.06) 0.38 -0.25 (0.18) 0.17 0.22 (0.29) 0.45
Glycemic load (1-SD = 21.8) -0.11 (0.06) 0.08 -0.44 (0.24) 0.07 -0.006 (0.21) 0.98
Carbohydrates (1-SD = 31.7), g/day -0.08 (0.06) 0.23 -0.40 (0.25) 0.11 -0.04 (0.18) 0.83
Total sugars (1-SD = 29.5), g/day 0.06 (0.10) 0.57 0.01 (0.20) 0.96 0.17 (0.26) 0.51
Total fiber (1-SD = 7.1), g/day 0.09 (0.11) 0.38 -0.003 (0.28) 0.99 0.01 (0.24) 0.96
β-Coefficients refer to each SD increase in nutritional intake at baseline with a decrease/ increase in mean BMI, %BF, and waist circumference. aAdjusted for age, ethnicity, parental education, exposure to passive smoking, change in energy intake (residual method), change in height, screen viewing time, and time spent in physical activity
TABLE 3 Changes in dietary intake of carbohydrate nutrition variables with concurrent change in mean BMI, percent body fat (%BF), and waist circumference from age 12 to 17 years old among girls (n = 279)
Concurrent change in mean BMIa
Concurrent change in mean %BFa
Concurrent change mean waist
circumferencea
Nutritional intake (per SD increase) β (SE) P β (SE) P β (SE) P
Glycemic index (1-SD = 3.6) 0.28 (0.16) 0.09 0.61 (0.42) 0.15 0.40 (0.23) 0.08
Glycemic load (1-SD = 50.9) 0.77 (0.31) 0.01 1.10 (0.82) 0.18 1.45 (0.58) 0.01
Carbohydrates (1-SD = 92.7), g/day 0.77 (0.35) 0.03 1.07 (0.88) 0.23 1.90 (0.83) 0.02
Total sugars (1-SD = 14.2), g/day 0.29 (0.16) 0.07 0.46 (0.40) 0.25 1.18 (0.66) 0.08
Total fiber (1-SD = 11.8), g/day -0.44 (0.19) 0.02 -1.07 (0.62) 0.09 -0.19 (0.72) 0.80
β-Coefficients refer to each SD increase in nutritional intake at baseline with a decrease/ increase in mean BMI, %BF, and waist circumference. aAdjusted for age, ethnicity, parental education, exposure to passive smoking, change in energy intake (residual method), change in height, screen viewing time, and time spent in physical activity
Reformatted author version Page 5
Discussion
To our best knowledge, no prospective observational study has shown that both carbohydrate quantity and quality could be relevant to the development of adiposity among adolescents. In our study, increased dietary GL and carbohydrate intake was associated with concurrent development of adiposity in girls. Also, girls who consumed more servings of soft drinks per day at an age of 12 years had significantly higher %BF 5 years later during adolescence. Conversely, an increase in total dietary fiber consumption was associated with a concurrent decrease in mean BMI in girls and in waist circumference in boys during adolescence.
In contrast with some other prospective adolescent studies (3), we show that dietary GL and carbohydrate intake appear to be relevant to the development of body composition in girls. The inconsistent findings between our study and previously published reports could be at least partly explained by differences in study characteristics; dietary habits and lifestyles of the participants examined; the dietary assessment methods used; measures of adiposity applied; and potential confounding factors considered (23).
The significant linear association between carbohydrate intake and change in body composition among girls could explain the relationship with GL, since dietary GL is primarily determined by the intake of carbohydrates (24). High-GL diets have previously been shown to increase postprandial hyperinsulinemia, which favors fatty acid uptake, inhibits lipolysis and increases energy storage resulting in weight gain (25). Higher dietary GL intake could also result in other postprandial metabolic changes, including an increase in counter-regulatory hormones that could explain increased hunger and increased energy intake in the post-absorptive phase, possibly leading to weight gain over time (26,27). Indeed, some intervention studies in children have found an increase in satiety and a reduction in food consumption after lowering the GL of meals (28,29). It is unclear as to why only dietary GL, and not GI, was associated with concurrent changes in BMI and waist circumference, however, it suggests that both the quality and quantity of dietary carbohydrate rather than quality alone may be important predictors of development of body composition in adolescence. Additionally, the observed strengthening of the association with multiplying GI by the amount of available carbohydrates (i.e., GL), suggests that postprandial hyperglycemia and hyperinsulinemia are likely mediators of this weight gain during adolescence.
Our study presents some potentially important implications for clinical practice and public health guidelines. Specifically, the finding that girls may be more sensitive to high GL foods is an important message given the prevalence of obesity in adolescents and the role of foods contributing to high GL in current dietary behavior in younger generations (30). Decrements of 1-SD in dietary GL and carbohydrates were previously shown to be achievable in practice in young adults (31). Therefore, reducing dietary GL and carbohydrate intake could be a feasible component of the nutritional advice for a healthy lifestyle in adolescents (30).
The positive association found between soft drink consumption and %BF in girls confirms data from other adolescent populations demonstrating a link between sweetened beverage consumption and BMI (7,9,10,32), and with waist circumference and %BF (6). Although, we caution that not all studies have confirmed an association between soft drink consumption and adolescent weight gain (13,33).
It has been speculated that soft drinks increase hunger, decrease satiety, or simply calibrate individuals to a high level of sweetness that generalizes to preferences in other foods (34), which could lead to an increase in %BF during adolescence. We also caution that frequent soft drink consumption could be a marker of other unhealthy dietary and lifestyle patterns, which could be driving the observed associations with %BF in girls.
Interpreting the sex-specific differences observed in the current study is complex. Vartanian et al. (34) in their meta-analysis of soft drink consumption and body weight observed significantly larger effect sizes among women, which concurs with our finding. Also, Sieri et al. (35) demonstrated that dietary GL intake increased the overall risk of coronary heart disease in women but not men. Given that girls are intrinsically more insulin resistant than boys during puberty (36,37), increased consumption of high-GL foods among girls could lead to magnification of postprandial hyperglycemia, which in turn causes the observed weight gain in girls but not boys. Thus, we speculate that differing actions of estrogen and testosterone could have contributed to the sex-specific associations observed in our study. Further prospective studies are required to both confirm and clarify the existence of this sex-specific difference during adolescence.
We document an independent, inverse association between consumption of total dietary fiber with subsequent development of body composition in both boys and girls. Contradictory results have been reported by other adolescent population-based
TABLE 4 Association between baseline consumption of carbohydrate nutrition variables with change in BMI, percent body fat (%BF), and waist circumference from age 12 to 17 years among boys (n 5 435), presented as adjusted means (95% confidence interval, CI)
Carbohydrate nutrition intake at baseline (range)
n Change in mean BMI (95% CI)a
Change in mean %BF (95% CI)a
Change in mean waist circumference (95% CI)a
Total sugars, g/day
First tertile (≤120.91) 141 2.81 (2.32-3.30) -3.60 (-4.61-2.58) 11.73 (10.35-13.10)
Second tertile (121.1–143.7) 142 2.84 (2.45-3.24) -3.61 (-4.80-2.41) 11.45 (9.93-13.0)
Third tertile (≥143.8) 152 3.06 (2.67-3.45) -2.21 (-3.19-1.23) 12.08 (10.85-13.30)
P for trend 0.09 0.02 0.49
Fructose, g/day
First tertile (≤26.10) 161 2.86 (2.31-3.40) -3.96 (-5.28-2.65) 11.60 (10.15-13.04)
Second tertile (26.2–34.6) 141 2.86 (2.49-3.22) -2.85 (-4.22-1.47) 11.57 (10.55-12.59)
Third tertile (≥34.7) 133 3.03 (2.64-3.41) -2.85 (-4.22-1.47) 12.16 (10.25-14.07)
P for trend 0.45 0.05 0.32
a Adjusted for age, ethnicity, parental education, exposure to passive smoking, energy intake (residual method), change in height, screen viewing time, and time spent in physical activity
Reformatted author version Page 6
studies (2,3). However, prior experimental studies conducted in adults have demonstrated a modest long-term beneficial effect of higher consumption of fiber-rich foods on body composition (38,39). Dietary fiber could facilitate body-weight control through several mechanisms including: 1) high-fiber diets are more satiating and can lead to lower energy intake; 2) fiber can limit the access of other nutrients to digestive enzymes; and 3) increasing fiber intake can improve insulin sensitivity and stimulate fat oxidation (38). All these aspects benefit weight control (39). We caution, however, that the finding related to fiber intake could reflect a dietary pattern rather than fiber consumption per se, so that the possibility of confounding by unmeasured or imprecisely measured factors contributing to this association cannot be excluded (40).
The key strengths of our study are its longitudinal design, random cluster sample of a relatively large number of school children, and use of standardized protocols to measure adiposity. Additionally, dietary information was collected twice, which afforded us the opportunity to investigate the concurrent associations between changes in carbohydrate nutrition variables and changes in anthropometric measures. Limitations of our study include that we did not have information available on pubertal stage and thus cannot discount that our findings could be confounded by the different pubertal stages of our participants. Also, while the validity of the long FFQ tool has been previously reported (15), and performs moderately well for carbohydrate, its validity for GI has not been investigated. It is, however, encouraging that we see consistent results between energy dense, nutrient poor foods with carbohydrate and the GI data from the long FFQ. Finally, we cannot discount the possibility of residual confounding from unmeasured confounders (e.g., parental BMI), which could have influenced findings.
In summary, we show that increased dietary intake of carbohydrates and GL are independent risk factors for the development of body composition among girls. We demonstrate a potential salutary role of fiber-rich diets in the prevention of adiposity development during puberty. Future research should include randomized controlled trials aimed at reducing the intakes of carbohydrates and high-GL foods, and increasing the consumption of dietary fiber, these studies could contribute to the development of potentially effective strategies to limit excess weight gain in adolescents.
Funding agencies: The Sydney Myopia Study (Sydney Childhood Eye Study) was supported by the Australian National Health & Medical Research Council (grant no. 253732); the Westmead Millennium Institute, University of Sydney; the Vision Co-operative Research Centre, University of New South Wales, Sydney; and the National Heart Foundation of Australia (grant no. G11S 6106), Melbourne, Australia.
Author’s contributions: Study concept and design: BG and PM, Acquisition of data: PM; Analysis and interpretation of data: BG, VF, JCYL, ER, PM; Drafting of the manuscript: BG and PM; Critical revision of the manuscript: BG, VF, ER, LAB, JCYL, WS, PM
References
1. Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997;337: 869-873.
2. Berkey CS, Rockett HR, Field AE, et al. Activity, dietary intake, and weight changes in a longitudinal study of preadolescent and adolescent boys and girls. Pediatrics 2000;105:E56.
3. Cheng G, Karaolis-Danckert N, Libuda L, Bolzenius K, Remer T, Buyken AE. Relation of dietary glycemic index, glycemic load, and fiber and whole-grain intakes during puberty to the concurrent development of percent body fat and body mass index. Am J Epidemiol 2009;169:667-677.
4. Steffen LM, Jacobs DR, Jr., Murtaugh MA, et al. Whole grain intake is associated with lower body mass and greater insulin sensitivity among adolescents. Am J Epidemiol 2003;158:243-250.
5. Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 2006;84:274-288.
6. Fiorito LM, Marini M, Francis LA, Smiciklas-Wright H, Birch LL. Beverage intake of girls at age 5 y predicts adiposity and weight status in childhood and adolescence. Am J Clin Nutr 2009;90:935-942.
7. Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet 2001;357:505-508.
8. Kral TV, Stunkard AJ, Berkowitz RI, Stallings VA, Moore RH, Faith MS. Beverage consumption patterns of children born at different risk of obesity. Obesity (Silver Spring) 2008;16:1802-1808.
9. Tam CS, Garnett SP, Cowell CT, Campbell K, Cabrera G, Baur LA. Soft drink consumption and excess weight gain in Australian school students: results from the Nepean study. Int J Obes (Lond) 2006;30:1091-1093.
10. Phillips SM, Bandini LG, Naumova EN, et al. Energy-dense snack food intake in adolescence: longitudinal relationship to weight and fatness. Obes Res 2004;12:461-472.
11. Forshee RA, Anderson PA, Storey ML. Sugar-sweetened beverages and body mass index in children and adolescents: a meta-analysis. Am J Clin Nutr 2008;87:1662-1671.
12. Sun SZ, Empie MW. Lack of findings for the association between obesity risk and usual sugar-sweetened beverage consumption in adults – a primary analysis of databases of CSFII-1989-1991, CSFII-1994-1998, NHANES III, and combined NHANES 1999–2002. Food Chem Toxicol 2007;45:1523-1536.
13. Ebbeling CB, Feldman HA, Osganian SK, Chomitz VR, Ellenbogen SJ, Ludwig DS. Effects of decreasing sugar-sweetened beverage consumption on body weight in adolescents: a randomized, controlled pilot study. Pediatrics 2006;117:673-680.
14. Ojaimi E, Rose KA, Smith W, Morgan IG, Martin FJ, Mitchell P. Methods for a population-based study of myopia and other eye conditions in school children: the Sydney Myopia Study. Ophthalmic Epidemiol 2005;12:59-69.
15. Watson JF, Collins CE, Sibbritt DW, Dibley MJ, Garg ML. Reproducibility and comparative validity of a food frequency questionnaire for Australian children and adolescents. Int J Behav Nutr Phys Act 2009;6:62.
16. Willett W. Correction for the effects of measurement error. In: Willett W, ed. Nutritional Epidemiology. New York: Oxford University Press, 1998.
17. Hu FB, Stampfer MJ, Rimm E, et al. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements [see comments]. Am J Epidemiol 1999;149:531-540.
18. Food Standards Australia New Zealand. NUTTAB 2006. Canberra, Australia: FSANZ, 2007. 2011. 2011.
19. Food Standards Australia New Zealand. NUTTAB 2010. Canberra, Australia: FSANZ, 2010.
20. Food Standards Australia New Zealand. AUSNUT 2007. Canberra, Australia: FSANZ, 2007.
21. Louie JC, Flood V, Turner N, Everingham C, Gwynn J. Methodology for adding glycemic index values to 24-hour recalls. Nutrition, in press.
22. Flood A, Subar AF, Hull SG, Zimmerman TP, Jenkins DJ, Schatzkin A. Methodology for adding glycemic load values to the National Cancer Institute Diet History Questionnaire database. J Am Diet Assoc 2006;106:393-402.
23. Murakami K, Miyake Y, Sasaki S, Tanaka K, Arakawa M. Dietary glycemic index and glycemic load in relation to risk of overweight in Japanese children and adolescents: the Ryukyus Child Health Study. Int J Obes (Lond) 2011;35:925-936.
24. Davis JN, Alexander KE, Ventura EE, et al. Associations of dietary sugar and glycemic index with adiposity and insulin dynamics in overweight Latino youth. Am J Clin Nutr 2007;86:1331-1338.
25. Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA 2002;287:2414-2423.
26. Ludwig DS, Majzoub JA, Al Zahrani A, Dallal GE, Blanco I, Roberts SB. High glycemic index foods, overeating, and obesity. Pediatrics 1999;103:E26.
27. Pittas AG, Das SK, Hajduk CL, et al. A low-glycemic load diet facilitates greater weight loss in overweight adults with high insulin secretion but not in overweight adults with low insulin secretion in the CALERIE Trial. Diabetes Care 2005;28: 2939-2941.
28. Warren JM, Henry CJ, Simonite V. Low glycemic index breakfasts and reduced food intake in preadolescent children. Pediatrics 2003;112:e414.
29. Spieth LE, Harnish JD, Lenders CM, et al. A low-glycemic index diet in the treatment of pediatric obesity. Arch Pediatr Adolesc Med 2000;154:947-951.
Reformatted author version Page 7
30. Burger KNJ, Beulens JWJ, Boer JMA, Spijkerman AMW, van der A DL. Dietary glycemic load and glycemic index and risk of coronary heart disease and stroke in Dutch men and women: The EPIC-MORGEN Study. PLoS ONE 2011;6:e25955.
31. Ebbeling CB, Leidig MM, Feldman HA, Lovesky MM, Ludwig DS. Effects of a low-glycemic load vs low-fat diet in obese young adults: a randomized trial. JAMA 2007;297:2092-2102.
32. Berkey CS, Rockett HR, Field AE, Gillman MW, Colditz GA. Sugar-added beverages and adolescent weight change. Obes Res 2004;12:778-788.
33. Vanselow MS, Pereira MA, Neumark-Sztainer D, Raatz SK. Adolescent beverage habits and changes in weight over time: findings from Project EAT. Am J Clin Nutr 2009;90:1489-1495.
34. Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health 2007;97:667-675.
35. Sieri S, Krogh V, Berrino F, et al. Dietary glycemic load and index and risk of coronary heart disease in a large italian cohort: the EPICOR study. Arch Intern Med 2010;170:640-647.
36. Shields BM, Knight B, Hopper H, et al. Measurement of cord insulin and insulinrelated peptides suggests that girls are more insulin resistant than boys at birth. Diabetes Care 2007;30:2661-2666.
37. Moran A, Jacobs DR, Jr., Steinberger J, et al. Insulin resistance during puberty: results from clamp studies in 357 children. Diabetes 1999;48:2039-2044.
38. Pereira MA, Ludwig DS. Dietary fiber and body-weight regulation. Observations and mechanisms. Pediatr Clin North Am 2001;48:969-980.
39. Du H, van der AD, Boshuizen HC, et al. Dietary fiber and subsequent changes in body weight and waist circumference in European men and women. Am J Clin Nutr 2010;91:329-336.
40. van Dam RM, Seidell JC. Carbohydrate intake and obesity. Eur J Clin Nutr 2007; 61:S75-S99.