California Surveillance for Pesticide-Related Illness and Injury
-
Upload
independent -
Category
Documents
-
view
0 -
download
0
Transcript of California Surveillance for Pesticide-Related Illness and Injury
This article was downloaded by: [University of California Davis]On: 19 February 2014, At: 12:15Publisher: Taylor & FrancisInforma Ltd Registered in England and Wales Registered Number: 1072954 Registered office: Mortimer House,37-41 Mortimer Street, London W1T 3JH, UK
Journal of AgromedicinePublication details, including instructions for authors and subscription information:http://www.tandfonline.com/loi/wagr20
California Surveillance for Pesticide-Related Illness andInjuryLouise N. Mehler MD, PhD a , Marc B. Schenker MD, MPH b , Patrick S. Romano MD, MPH c &Steven J. Samuels PhD da Department of Pesticide Regulation , California Environmental Protection Agency , USAb Department of Public Health Sciences , University of California Davis School of Medicine ,USAc Division of General Medicine and Center for Health Services Research in Primary Care ,University of California Davis School of Medicine , USAd Department of Epidemiology and Biostatistics , University at Albany, State University ofNew York , USAPublished online: 01 Oct 2008.
To cite this article: Louise N. Mehler MD, PhD , Marc B. Schenker MD, MPH , Patrick S. Romano MD, MPH & Steven J. SamuelsPhD (2006) California Surveillance for Pesticide-Related Illness and Injury, Journal of Agromedicine, 11:2, 67-79
To link to this article: http://dx.doi.org/10.1300/J096v11n02_10
PLEASE SCROLL DOWN FOR ARTICLE
Taylor & Francis makes every effort to ensure the accuracy of all the information (the “Content”) containedin the publications on our platform. However, Taylor & Francis, our agents, and our licensors make norepresentations or warranties whatsoever as to the accuracy, completeness, or suitability for any purpose of theContent. Any opinions and views expressed in this publication are the opinions and views of the authors, andare not the views of or endorsed by Taylor & Francis. The accuracy of the Content should not be relied upon andshould be independently verified with primary sources of information. Taylor and Francis shall not be liable forany losses, actions, claims, proceedings, demands, costs, expenses, damages, and other liabilities whatsoeveror howsoever caused arising directly or indirectly in connection with, in relation to or arising out of the use ofthe Content.
This article may be used for research, teaching, and private study purposes. Any substantial or systematicreproduction, redistribution, reselling, loan, sub-licensing, systematic supply, or distribution in anyform to anyone is expressly forbidden. Terms & Conditions of access and use can be found at http://www.tandfonline.com/page/terms-and-conditions
California Surveillancefor Pesticide-Related Illness and Injury:
Coverage, Bias, and Limitations
Louise N. Mehler, MD, PhDMarc B. Schenker, MD, MPHPatrick S. Romano, MD, MPH
Steven J. Samuels, PhD
ABSTRACT. The California Pesticide Illness Surveillance Program (PISP) is a major resourcefor pesticide illness epidemiology. This work attempts to improve characterization of pesticide ill-ness in California, evaluate case ascertainment of the PISP and identify PISP’s limitations and bi-ases for studying the incidence and epidemiology of pesticide-related illness. Abstractors collectedstandardized information from 1994-1996 PISP files, poison control logs, hospital records, anddeath certificates. Linkage produced a merged file of all records that documented consideration ofpesticide exposure as a cause of ill health. We identified 23 deaths and estimated 1,310 hospitaliza-tions attributable to pesticide exposure, corresponding to 0.024 fatalities and 1.38 hospitalizations(95% confidence interval [CI] = 1.01-1.74) per 100,000 California population person-years. Mostintoxications followed domestic exposures and were not reported to the surveillance program,which identified primarily occupational exposures. Excluding groups of five or more, we esti-mated 16% ascertainment (CI = 0.05-0.27) for non-agricultural occupational cases. Agriculturalconnections increased the probability of ascertainment to about 50%, cultural and economic barriersnotwithstanding. Surveillance records existed for all identified episodes in which five or more peoplewere exposed. California pesticide surveillance data appear complete for mass exposures, and adequateto characterize agricultural and occupational exposures. Work is needed to explore domestic expo-sures and occurrences beyond the reach of the health care system. doi:10.1300/J096v11n02_10 [Ar-ticle copies available for a fee from The Haworth Document Delivery Service: 1-800-HAWORTH. E-mail ad-dress: <[email protected]> Website: <http://www.HaworthPress.com> © 2006 by The HaworthPress, Inc. All rights reserved.]
KEYWORDS. California [epidemiology], pesticides [toxicity], poisoning, population surveil-lance, program evaluation
Louise N. Mehler is affiliated with the Department of Pesticide Regulation, California Environmental ProtectionAgency.
Marc B. Schenker is affiliated with the Department of Public Health Sciences, and Patrick S. Romano is affiliatedwith the Division of General Medicine and Center for Health Services Research in Primary Care, University of Cali-fornia Davis School of Medicine.
Steven J. Samuels is affiliated with the Department of Epidemiology and Biostatistics, University at Albany,State University of New York.
Address correspondence to: Louise N. Mehler, MD, PhD, Department of Pesticide Regulation, California Envi-ronmental Protection Agency, P.O. Box 4015, 1001 I Street, Sacramento, CA 95812-4015.
The work described in this paper was supported by the California Environmental Protection Agency’s Depart-ment of Pesticide Regulation, by the Agricultural Health and Safety Center of the University of California at Davis(funded by NIOSH Cooperative Agreement #U07/CCU906162), and by U.S. Environmental Protection Agency(U.S. EPA) contract 98-0249.
Journal of Agromedicine, Vol. 11(2) 2006Available online at http://ja.haworthpress.com
© 2006 by The Haworth Press, Inc. All rights reserved.doi:10.1300/J096v11n02_10 67
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
INTRODUCTION
California law (Health and Safety Code sec-tion 105200 [HSC 105200]) requires physi-cians to report suspected cases of pesticide-re-lated illness to local health officers. This lawdirects health officers to forward these reportsto county agricultural commissioners and tostate agencies, including the Department ofPesticide Regulation (DPR), which maintainsthe Pesticide Illness Surveillance Program(PISP). DPR supplements these reports throughan agreementwith the Departmentof IndustrialRelations and the Department of Health Ser-vices,underwhich theagenciescooperate in lo-cating evidence of pesticide effects in doctors’reports of care billed to workers’ compensa-tion. DPR has also arranged with county agri-cultural commissioners to investigate all re-ports of human health effects from pesticideexposure. DPR scientists evaluate the commis-sioners’ reports and abstract data from them.
Regulators, advocacy groups, industry, andprivatecitizens regularlyconsult thePISP data-baseforevidenceaboutadverseeffectsofpesti-cide exposure. A federal survey1 noted that“California had by far the most effective andwell-established monitoring system in place”and that the U.S. Environmental ProtectionAgency “relies heavily on the pesticide illnessdatacollectedbytheCaliforniamonitoringsys-tem.” Published reviews of pesticide illness2-7
regularly rely on PISP data. The accuracy andappropriate interpretation of these data remaincontroversial, however. One publication8 com-pared physician reports to farm worker self-re-ports in two surveys9,10 and arrived at a “guess”that “possibly no more than 1 or 2%” of fieldworker poisonings are reported. A poison con-trol study11 identified 41 occupational cases aseligible for reporting to PISP, of which onlyseven could be located in the program’srecords. We know of no other evidence on thePISP’s completeness.
The current study was undertaken to im-prove characterization of pesticide poisoningin California and to develop a context in whichto interpret surveillance results. We consideredpesticide poisoning or pesticide toxicity to in-clude any disturbance (illness or injury) in aperson’s usual state of health caused or exacer-bated by exposure to pesticide. Our approach
was to compare pesticide-related illnesses andinjuries reported to the PISP with pesticide-re-lated illnesses and injuries ascertained fromthreeothercomputerizeddata sets:deathcertif-icates, hospital discharge abstracts, and poisoncontrol center consultations. By linking re-cords across data sets, we also evaluated thecompleteness of the PISP and characterized thebiases caused by incomplete reporting.
MATERIALS AND METHODS
Code Identification
In consultation with analysts from the datasuppliers, we identified poison control, ICD-9,and ICD-9-CM codes that apply to pesticidetoxicity. We also identified ICD-9 and ICD-9-CM codes related to categories of substancesthat include pesticides or to types of pathologytypical of pesticide exposure. We designatedthese codes “general” codes, by contrast to the“specific” codes that explicitly reference pesti-cides. In selecting general codes, we attemptedto include all categories reviewed in previouswork on agrochemical toxicity.12-15 Adverseeffects of antimicrobials (sanitizers and disin-fectants) were included as pesticide-related,since federal law16 defines such products aspesticides (“any substance . . . intended for pre-venting, destroying, repelling, or mitigatingany pest . . .” [including microbes]). Appendi-ces A and B list the selected codes. It should benoted that poison control codes have since beenaugmented with codes specifically designed tofacilitate locating pesticide cases.
SAMPLE SELECTION
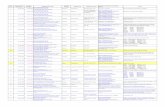
We planned the sample to maximize thenumber of pesticide-related cases from eachdata source, with a bias towards selecting se-vere cases that might appear in more than onesource. Secondarily, we incorporated collec-tion of evidence on the predictive value ofICD-9 and ICD-9-CM codes for identifyingpesticide-related cases. Figure 1 summarizesthe data collection process.
68 JOURNAL OF AGROMEDICINE
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
Sample Selection–Fatalities
We purchased 1994-1996 California multi-ple-cause-of-death tapes from the Vital Statis-tics Branch of the California Department ofHealthServices,andsearchedallentriesforanyof the codes of potential interest. We purchasedhard copies of all death certificates that listedspecific codes in any location, and a stratifiedrandom sample of those that listed general butnot specific codes. Preliminary review ex-cluded death certificates with a non-pesticidebasis for code assignment. We requested coro-ners’ reportsonallof theremainingfatalities.
Sample Selection–Hospitalization
Analysts at the California Office of State-wideHealthPlanningandDevelopmentsearched1994-1996 hospital discharge files for all re-cords that carried any ICD-9-CM code of inter-est in any location.These files containdata sup-plied by hospitals for each patient dischargedfrom their wards. As such, they provide infor-mation only about people admitted as inpa-tients.
After initial sample size and cost calcula-tions, we decided we could reasonably review1,000 charts from 100 hospitals. Based on stan-dard sampling theory,17 we over-sampled hos-pitals with larger numbers of specific pesti-cide-related codes. Specifically, we selected astratified cluster sample from the retrieved re-cords. Hospitals were the primary sampling
unit, and were divided into strata by type ornumber of codes. The first stratum consisted ofhospitals thathadassignedgeneralcodesbutnospecific codes. Hospitals with specific codeswere further stratified into three groups accord-ing to the number of cases with pesticide-spe-cific codes (1-3, 4-7, 8-28). We randomly se-lected 25 hospitals from each stratum. Werequested all charts with specific codes fromeach selected hospital, along with a stratifiedrandom sampleof charts with general codes butno specific codes. Trained professional ab-stractors reviewed each hospital chart forinformation related to pesticide exposure.
Sample Selection–Poison Control
We purchased extracts of electronic poisoncontrol logs from the CaliforniaPoison ControlSystem, consisting of all validated 1994-1996records that indicated referral to a health carefacility or evaluation by a health professional,and carried any of the codes identified as repre-senting pesticides. Since all of these cases wereevaluated at health facilities and had been iden-tified by poison control specialists as potentialcases of pesticide toxicity, all were subject tothe reporting requirement of HSC 105200.
The Central Valley Regional Poison ControlCenter (Fresno Center), which serves the mostheavily agricultural region of the state, col-lected validated data and case managementnotes throughout the period of interest. TheUniversity of California Davis Medical CenterRegional Poison Control Center (SacramentoCenter), which serves the northeast quadrant ofCalifornia, began collecting validated data andcase notes in September 1995. Four other poi-son control centers served coastal and southernCalifornia during the period of interest, buttheir data were considered unusable becausethey lacked any narrative description and hadnot been subject to standard edit and verifica-tion procedures. Among the poison control re-cords received, we reviewed all fatalities, allhospitalizations (both medical and psychiat-ric), and all cases evaluated as having majormedical outcomes. We reviewed a randomlyselected 20% sample of the remainder.
Special Features 69
Deathcertificates
Purchase and review:All with specific codes
Sample of general codes
Hospitaldischargerecords
Poisoncontrol
logs
Pesticideillness
surveillancedata
Stratify hospitalsby case counts;
sample fromeach stratum
Stratify byseverity;sample
less severe
Convertelectronicallyto database
format
Exclude deathsfrom obvious
non-pesticide cause
Stratify caseswithin hospitalby diagnosis,select sample
Abstract sampleand all severe
cases intodatabase
Request coroners’reports;
abstract intodatabase
Request charts;abstract into
database
Merge based onpatient and event
identifiers
FIGURE 1. Data Collection Flow Chart for HealthEvents Related to Pesticide Exposure in California,1994-1996.
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
Data Abstraction
Comparable data elements were abstractedfrom fatality, hospitalization, and poison con-trol records. We defined unintentional expo-sures as those that occurred when a pesticidewas used as intended or in the mistaken beliefthat the use was proper. Unintentional expo-sures also included self-exposure by childrenless than12 yearsoldor by adults compromisedby dementia, intoxication, or acute psychosis.Exposures were recorded as intentional onlywhen documentation indicated that they re-sulted from actions taken by a person 13 yearsold or older for the purpose of causing toxicity.Exposures were characterized as agricultural ifthe pesticide source was an agricultural enter-prise. Exposures were characterizedas occupa-tional if theyoccurredwhile theaffectedpeoplewere at work, whether or not their tasks in-volved pesticides.
Records were retained for analysis if the re-sponsiblehealthprofessionalsdocumentedanyconsideration that exposure to a federally de-fined pesticide product16 had contributed to thepatients’ ill health. The PISP collects onlyevents in which initial evaluation suggests pes-ticide exposure as a possible cause. PISP re-cords are maintained in an electronic databasethat represents all the data elements abstractedfor this project, but uses a somewhat differentcoding scheme. Therefore, all 6,079 PISP re-cords collected from 1994 through 1996 wereconverted electronically to the format of thisproject’s database, including 1,235 records(20.4%) initially identified as pesticide-relatedbut determined after investigation not to be re-lated.
Thefour filesweremerged inacomputer-as-sisted process. An investigator reviewed a dis-play of potential matches ordered by similaritybefore adding each case to the merged file. Theinvestigator decided whether to accept a poten-tial match or to add the case as a separate event.This produced a file in which one record repre-sented each known event of medical consulta-tion concerning possible health effects of pesti-cide exposure.
Rate Computation
Rates relative to California population werebased on intercensal estimates posted by the
California Department of Finance.18 Statewidefigures for deaths and hospitalizations werecomputed using the arithmetic mean of popula-tion estimates for 1994, 1995, and 1996. Ratesof poison control consultations were computedrelative to averaged estimates for the countiesthat comprised the catchment areas of the cen-ters that contributed data. For the SacramentoCenter, which contributed data only from Sep-tember 1995 through December 1996, annualpopulation estimates were weighted corre-spondingly. For comparison with earlier publi-cations,whichreportnumeratordataonly, rateswereapproximatedbyinterpolatingpopulationdata from the decennial censuses nearest to theperiod studied.
Data Analysis
Analyses were performed using Stata forWindows® statistical software, version 6.0,Stata Corporation, College Station, Texas. Caseweights were computed as the inverse of thestratum-specific sampling probability. For hos-pitalcases, thefinalweightwascomputedas theproductof thesamplingweights for thehospitaland for the case within the hospital; the hospitalwas identified as the primary sampling unit.We used survey commands,19 applying theseweights, to generate unbiased estimates ofprobabilities, total frequencies, and associatedstandard errors.
RESULTS
Fatalities
We identified a total of 23 deaths (including17 suicides) (Table 1) from pesticide toxicitythat occurred in California from 1994 through1996, for an estimated crude annual death rateof 0.024 per 100,000 person-years. Deathswere caused most frequently (Table 2) by in-secticides (six), rodenticides (six), and antimi-crobials (five). With the exception of one sui-cide by injection, all suicide victims ingestedthepesticides.Unintentional fatalities includedentries into structures under fumigation as wellas ingestions. Pesticide fatalities are fully de-scribed in a DPR report.20
70 JOURNAL OF AGROMEDICINE
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
Hospital Inpatients
Pesticide exposure was documented in 224of 313 hospital charts that carried pesticide-specificcodes, and in22 of 630 chartswithonlygeneral codes, corresponding to positive pre-dictive values of 0.81 (95% CI = 0.75-0.87) forspecific codes and 0.05 (95% CI = 0.02-0.08)for general codes identified as potentially re-flecting pesticide exposure or effects. A DPRreport21 summarizes our estimates of positivepredictive value for the selected codes.
For the three-year period, we estimated thatpesticide exposure was at least considered as apossible etiologic factor in 1,310 (95% CI =963-1656) hospital discharges correspondingto 1.38 (95% CI = 1.01-1.74) hospitalizationsper 100,000 persons per year.
Poison Control
We confirmed accurate representation of thesubstance of concern in all 741 poison controlrecords reviewed, but found that case notesdocumented a non-pesticide source in 190 re-cords. For example, the code for strychninerodenticide was assigned to a case in which acaller expressed concern that illicitdrugs mighthave been adulterated with strychnine. More
typically, non-pesticide cases involved expo-sure to pharmaceutical products, particularlypediculocides, which contain pesticidal ingre-dients but fall under the jurisdiction of the FoodandDrugAdministrationandfor that reasonarenot legallypesticides.Amongthe78apparentlypesticide-related poison control records thatmatched PISP investigations, investigatorsdocumented in eight cases that pesticides hadnot been involved (positive predictive value =0.89 [95% CI = 0.81-0.97]).
Suspicion of pesticide exposure led to an es-timated three-year total of 1,173 (95% CI =1063-1283) calls to the Fresno Center involv-ing patients who presented for medical evalua-tion or were referred for medical evaluation,and 843 (95% CI = 739-946) such calls to theSacramento Center during the 15 months forwhichdatawereavailable.All records thatdoc-umentedconsiderationofpesticideexposureasa possible etiologic factor were retained foranalysis.
PISP
The PISP diverged strongly from other datasources with respect to population characteris-tics and exposure circumstances (Table 2). Pe-diatric and intentional exposures were practi-cally absent from the PISP, which recordedprimarily occupational exposures. Agricultur-ally related cases constituted a larger propor-tion of PISP records than of any other source.Insecticides and antimicrobials were promi-nent in all sources (Table 2), and only the PISPfailed to identify substantial numbers of rodenti-cide cases.
File Linkage
In all of these cases, physicians had reason tobelieve that their patients suffered from condi-tions caused by pesticides, so these casesshould have been reported to local health offi-cers in compliance with HSC 105200. They donot appear to have been reported, however, asDPR received reports on fewer than 15% of thecases ascertained from hospital or poison con-trol records (Figure 2).
Among the 23 fatalities, the PISP had re-cordsonsix (sensitivity=0.26), includingthreeof the17suicides.ThePISP had identifiednone
Special Features 71
TABLE 1. California Occurrences of Medically Eval-uated Health Events Related to Pesticide Expo-sure, 1994-1996
Events Rate per 100,000person-years
(95% confidenceinterval)
(95% confidenceinterval)
Deaths 23 0.024
Hospital Admissions 1310 (963-1656) 1.38 (1.01-1.74)
Poison ControlConsultations, CentralValley Regional PoisonControl Center (FresnoCenter)
1173 (1063-1283) 18.07 (16.38-19.77)
Poison ControlConsultations, Universityof California Davis MedicalCenter Regional PoisonControl Center(Sacramento Center),September 1995 throughDecember 1996
843 (739-946) 17.06 (14.95-19.14)
Reports to the CaliforniaPesticide IllnessSurveillance Program(PISP)
6709 7.05
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
72 JOURNAL OF AGROMEDICINE
TABLE 2. Demographic and Exposure Characteristics of Medically Evaluated Health Events Related toPesticide Exposure in California, 1994-1996
Estimated Poison Control Consultations withMedical Evaluation or Referral
Deaths Estimated Hospitaliztions Sacramento Center Fresno Center PISP
N % N (95% CI) % N (95% CI) % N (95% CI) % N %
Total 23 100 1310 (963-1656) 100 843 (739-946) 100 1,173 (1063-1283) 100 6,709 100
Age Range
0-4 years 1 4.3 277 (158-396) 21.1 277 (208-346) 32.9 348 (274-423) 29.7 22 0.3
5-14 years 0 0 39 (4-74) 3 79 (41-117) 9.4 120 (74-166) 10.2 142 2.1
15-64 years 11 47.8 859 (549-1169) 65.6 443 (361-524) 52.6 624 (532-716) 53.2 5980 89.1
64 + years 11 47.8 135 (66-203) 10.3 45 (16-73) 5.3 43 (17-70) 3.7 84 1.3
Unknown age 0 0 0 37 (13-62) 3.2 481 7.2
Male 15 65.2 822 (512-1133) 62.7 546 (456-636) 64.8 673 (578-768) 57.4 4021 59.9
Female 8 34.8 487 (327-648) 37.2 297 (227-366) 35.2 494 (409-580) 42.1 2633 39.2
Unknown Sex 0 0 0 6 (0-16) 0.5 55 0.8
Intentional 17 73.9 352 (257-446) 26.9 74 (43-105) 8.8 106 (68-144) 9 50 0.7
Unintentional 6 26.1 958 (618-1298) 73.1 769 (668-871) 91.2 1067 (959-1176) 91 6659 99.3
Agricultural
Occupational 0 0 37 (0-88) 2.8 21 (1-41) 2.5 198 (142-255) 16.9 2381 35.5
Non-Occupational 2 8.7 21 (0-47) 1.6 5 (0-15) 0.6 68 (33-102) 5.8 265 3.9
Non-Agricultural
Occupational 0 0 162† (0-432) 12.4 100 (58-143) 11.9 107 (64-150) 9.1 3470 51.7
Non-Occupational 21 91.3 1089 (826-1353) 83.1 716 (617-815) 84.9 800 (700-900) 68.2 593 8.8
Pesticide Class
CholinesteraseInhibitingInsecticides
3 13 358 (80-636) 27.3 112 (69-156) 13.3 282 (216-349) 24 840 12.5
OtherInsecticides
3 13 172 (97-247) 13.1 167 (113-222) 19.8 228 (167-289) 19.4 1,076 16
Herbicides 1 4.3 57 (14-99) 4.4 75 (38-112) 8.9 118 (73-164) 10.1 310 4.6
Fungicides 1 4.3 3 (0-8) 0.2 11 (0-25) 1.3 10 (0-21) 0.9 332 4.9
Fumigants 2 8.7 29 (0-62) 2.2 0 42 (14-70) 3.6 283 4.2
AnticoagulantRodenticides
1 4.3 113 (73-153) 8.6 173 (118-228) 20.5 193 (135-250) 16.5 5 0.1
OtherRodenticides
5 21.7 95 (44-146) 7.3 26 (4-49) 3.1 2 (0-5) 0.2 4 0.1
Antimicrobials 5 21.7 420 (196-644) 32.1 195 (136-253) 23.1 227 (167-287) 19.4 1,787 26.6
Miscellaneous 0 0 2 (0-5) 0.2 15 (0-32) 1.8 13 (0-28) 1.1 79 1.2
Combinations 1 4.3 23 (0-48) 1.8 31 (9-54) 3.7 24 (4-45) 2 406 6.1
Unknown 1 4.3 39 (5-73) 3 36 (10-63) 4.3 34 (10-59) 2.9 352 5.2
None 0 0 0 0 0 1,235 18.4
Total 23 100 1310 (963-1656) 100 843 (739-946) 100 1,173 (1063-1283) 100 6,709 100
a. Columns may not add to total because of rounding.b. Confidence interval bounds below 0 are represented as 0.c. Based on seven sampled cases, one of which accounted for 135 estimated cases.
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
of the deaths attributed to antimicrobial orrodenticide exposure. The 11 hospital chartsthat matched PISP records were estimated torepresent 70 (95% CI = 12-127) of the 1,310 es-timated hospitalized cases (sensitivity = 0.05[95% CI = 0.008-0.098]). The 78 matched poi-son control records were estimated to represent294 (95% CI = 225-363) of the 2,016 estimatedpoison control consultations (sensitivity = 0.15[95% CI = 0.11-0.18]). Only one case, a home-owner who got sick after spraying an organo-phosphate insecticide in his yard, was identi-fied in all three data sets (poison control,hospital, and PISP records).
Sampled poison control records includedthose of 37 people involved in nine episodesidentified by the PISP as involving more thanfour exposed individuals (range = 6-243). Nounmatched poison control case indicated oc-currence as part of an episode of comparablesize. Only one hospital chart identifieda personaffected in a group episode; this concerned anon-agricultural occupational exposure andwas recorded in thePISP, althoughultimately itproved not to involve any pesticide.
When episodes involving five or more peo-plewereexcluded,weestimatedroughlya50%probability that exposures to agricultural pesti-cides (based on either hospitalization or poisoncontrol data) appear in the PISP. Occupationalexposure did not affect this percentage signifi-cantly. Non-agricultural exposures showed ahigher probability of recognition by the PISP iftheyoccurredatwork (Table3).Severity (as re-
flected by hospital admission or poison controlevaluation of outcome) did not affect theprobability of ascertainment significantly.
DISCUSSION
Context
Pesticide toxicity is a rare diagnosis in Cali-fornia as in other developed economies.22-24
We estimated rates of 0.024 deaths and 1.38hospitalizations per 100,000 person-years. Ex-cluding antimicrobials, which previous publi-cations have not addressed, reduced these esti-mates to 0.019 deaths and 0.92 (95% CI =0.64-1.20) hospitalizations per 100,000 per-son-years. These latter estimates are similar toratescalculatedfrompreviouslypublishedcasecounts: North Carolina25 reported 0.045 deathsand 0.98 hospitalizations per 100,000 per-son-years, and South Carolina26 reported 0.61hospitalizations. A review of national statisti-cal extracts22 indicated 0.023 deaths and 1.7hospitalizations per 100,000 person-years. Weconclude that our estimates of the occurrencerates of medically evaluated health events re-lated to pesticide exposure, based on multipledata sources in California, are similar toestimates from other states.
We identified only six unintentional pesti-cide deaths, including two related to antimicro-bial pesticides. The four non-antimicrobial ac-cidental deaths correspond to a rate of 0.004/100,000 person-years. This low rate continuesthe declining trend identified by Hayes and col-laborators,12-14 who did not investigate sui-
Special Features 73
Hospital(sample)
PoisonControl
(sample)Excluding groups of 5 or more
affected individuals
OccupationalAgricultural
Non-OccupationalAgricultural
Overall
Groups of 5 or moreaffected individuals
(number of individuals)Occupational
Non-Agricultural
Non-Occupational
Non-Agricultural
1(1) 91
(1648)
9(36)
(1)6
44
83018
209
4
151
369
38211
PISP
220
10
15
177
6621
458
3
31490
1822 2
2
9
496
FIGURE 2. Overlap of Health Events Related toPesticide Exposure in California, 1994-1996, Iden-tified Through Hospital, Poison Control, and Pesti-cide Illness Surveillance Program (PISP) Records
TABLE 3. Probability of PISP Recognition of Pesti-cide-Related California Health Events InvolvingFewer Than Five People, 1994-1996
Exposure Hospitalizations Poison Control Consultations
(95% CI) (95% CI)
Agricultural
Occupational 0.53* (0.42-0.64) 0.52 (0.34-0.69)
Non-Occupational 0.38* (0-0.91) 0.43 (0.10-0.77)
Non-Agricultural
Occupational 0* 0.16 (0.05-0.27)
Non-Occupational 0.035 (0-0.081) 0.024 (0.008-0.041)
* Based on six sampled cases or fewer; see Figure 1
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
cides, but found unintentional deaths droppingfrom 0.065/100,000 in 1961 to 0.043 in 1969and 0.027 in 1973-1974. This trend reflectschanges in pesticide use patterns. Earlier workidentified arsenic, phosphorus, and strychnine(all rodenticides) as common causes of fatalpesticide poisoning. Phosphorus is no longeravailable as a pesticide, and access to arsenicand strychnine has decreased as less toxic alter-natives (primarily anticoagulants) have displacedthem. Table 2 illustrates this phenomenon,showing the preponderance of anticoagulantsamong rodenticide exposure reports to poisoncontrol, while rodenticides containing strych-nine and arsenic continue to cause rare suicidalfatalities. The one anticoagulant rodenticidedeathwas thatofadisturbedyoungwomanwhoingested thematerialpersistently.She had beenhospitalized and treated at least three times be-fore her final presentation, when she sufferedan intracranial hemorrhage and died.
Program Evaluation
California’s Pesticide Illness SurveillanceProgram identified every episode we encoun-tered inwhichfiveormore individualswereex-posed, while its ascertainment rates for occupa-tional and agricultural exposures were withinthe range of “6% to 90%” estimated for surveil-lance in the United States of America.27 Expo-sures in socially sensitive contexts, such as sui-cide or through carelessness at home, were sorarely captured as to limit the applicability ofPISP data to these situations. Relying on thePISP alone would yield seriously biased esti-matesof theoveralldistributionofpesticide-re-lated injury in the population.
DPR hasattemptedtoaddress this shortcom-ing by developing cooperation with poisoncontrol centers. Under contracts funded by theU.S. Environmental Protection Agency, poi-son control specialists offered to fulfill the re-porting requirement on behalf of physicianswho consulted them. This effort produced en-couraging results, but the state’s fiscal crisisprevented continuation of the contract whenfederal funding ended. When resources becomeavailable, DPR plans to pursue funding for acontinuing contractual relationship with theCalifornia Poison Control System.
The PISP’s success in identifying agricul-tural and group episodes probably results fromthe involvement of agricultural commissionersand their staffs in every California county.Since the1970s, these localofficershave inves-tigated every case in which pesticide exposurewas identified as causing or contributing to ad-verse effects on human health. Their vigilanceprovides coverage far superior to passive col-lection of reports of this notifiable condition,and substantiallybetter than even active reviewof workers’ compensation documents.
Limitations
This work includes only events evaluated byhealth care providers. This approach allows di-rect comparison to the PISP, which relies pri-marily on reports submitted by physicians,through either local health officers or workers’compensation. It also takesadvantageof theex-pertise of health care providers to limit atten-tion to cases with a high probability of relationto pesticide exposure. In excluding any pesti-cide exposure that did not lead to medical con-sultation, however, this approach biases find-ings towards people with access to health careand ability to use social resources such as poi-son control centers. Agricultural workers maywell be under-represented in hospital and poi-son control samples. The California HealthInterview Survey28 found that agriculturalworkers consulted physicians less often thanworkers in any other industrial sector, althoughmore than half of agricultural workers visited adoctor at least once in the course of a year.
Hospital and poison control records do notsystematically identify group episodes, so wecould not sample on that basis or develop esti-mates of the total number of such events. Thisproblem qualifies confidence about the PISP’scompleteness in identifying group exposures.Hospital and poison control case notes did,however, describe mass exposures in all caseslinkedtoPISPgroupepisodesandinnoothers.
The 72% hospital participation rate was dis-appointing compared to rates in excess of 90%achieved in Nebraska,15 North Carolina,25 andSouth Carolina26 surveys. Our data probablyunder-represent suicide attempts, as six non-participating hospitals cited special protectionfor confidentiality of psychiatric records. Par-
74 JOURNAL OF AGROMEDICINE
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
ticipating hospitals appeared representative interms of size and geographic distribution. Hos-pital records reviewed were found to resemblethe full dataset closely with respect to distribu-tions by age, sex, severity, length of hospitalstay, and disposition upon discharge.
Data from poison control requires cautiousinterpretation because it reflects only the infor-mation specialists glean from telephone con-versations while providing clinical consulta-tion. This investigation used only data that hadpassed edits for internal consistency, so record-ing errors were probably minimized. No mech-anism, however, verified that callers providedaccurate information to poison control special-ists. On the contrary, in eight of the 78 poisoncontrol entries that matched PISP cases, wefound that on-site investigations documented afundamental misunderstanding: Those eightcases did not involve any pesticide exposure.This suggests that similar misunderstandingsmay distort some of the 473 case reports frompoison control that did not match PISP data.
Because the PISP captures information on apopulation very different from that reflected inother information sources, overlap was limitedand did not support detailed analysis or estima-tion of the number of events that escaped de-tection by all sources.29-31 Scanty exposure in-formation and large number of implicatedproducts restricted analyses by pesticide iden-tity toonlyafewgeneralcategoriesofproducts.
CONCLUSIONS
The Pesticide Illness Surveillance Programprovides a valuable resource to anyone con-cerned about health effects of pesticide expo-sure. Exposures to agricultural-use pesticidesare particularly well represented. The PISP da-tabase supports a variety of parametric and keyword searches of tens of thousands of records,accumulated over decades, each representingan on-site investigation that documented expo-sure circumstances and health conditions. Datausers risk misleading themselves and others,however, if they overlook the biases inherent inthe program’s structure. Domestic exposuresareseriouslyunder-represented in theprogram.Consequently, DPR can respond promptly toemergingproblemsinagriculture,butmust rely
on surrogate information, models and assump-tions to evaluate pesticide products for homeuse.
Future research should be directed towardsevaluating the validity of ICD-10 and ICD-10-CM codes that indicate pesticide toxicity andtowards identifying informationsources on do-mestic exposures. Broader investigations areneeded to resolve the discrepancy betweenmedical sources, in which pesticide toxicityrarely appears, and the perceptions of agricul-tural workers,8-10,32 who report much more fre-quent episodes of pesticide toxicity in surveyresearch.Finally,our findingshighlight that thetrue distribution of pesticide-related healthevents in the population differs markedly fromthe distribution that would be expected basedupon existing pesticide injury surveillance pro-grams,suchas thePISP. Inparticular,morevig-orous prevention efforts should be directed tonon-occupational, non-agricultural settings.
REFERENCES
1. U.S. General Accounting Office. Pesticides onFarms: Limited capability exists to monitor occupa-tional illnesses and injuries; 1993. Report to the Chair-man, Committee on Agriculture, Nutrition, and Forestry,U.S. Senate GAO/PEMD-94-6.
2. Centers for Disease Control and prevention Noso-comial Poisoning Associated With Emergency Depart-ment Treatment of Organophosphate Toxicity–Georgia.Morb Mortal Wkly Rep. 2000;49(51):1156.
3. Centers for Disease Control and Prevention Pes-ticide-related illnesses associated with the use of a plantgrowth regulator–Italy. Morb Mortal Wkly Rep. 2001;50(39): 845-7.
4. Goldstein DA, Acquavella JF, Mannion RM,Farmer DR. An analysis of glyphosate data from theCalifornia Environmental Protection Agency PesticideIllness Surveillance Program. J Toxicol Clin Toxicol.2002;40(7):885-92.
5. Calvert GM, Mehler LN, Rosales R, Baum L,Thomsen C, Male D, Shafey O, Das R, Lackovic M,Arvizu E. Acute pesticide-related illnesses among work-ing youths, 1988-1999. Am J Public Health. 2003 Apr;93(4):605-10.
6. Centers for Disease Control and Prevention. Sur-veillance for acute insecticide-related illness associatedwith mosquito-control efforts–nine states, 1999-2002.Morb Mortal Wkly Rep. 2003;52(27):629-34.
7. Reeves M, Schafer KS. Greater risks, fewer rights:U.S. farmworkers and pesticides. Int J Occup EnvironHealth. 2003 Jan-Mar;9(1):30-9.
Special Features 75
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
8. Kahn E. Pesticide related illness in Californiafarm workers. J Occup Med. 1976 Oct;18(10):693-6.
9. Howitt, RE. Pesticide externality policy, an opti-mal control approach [dissertation]. University of Cali-fornia at Davis; 1975.
10. U.S. Public Health Service. 1970. California De-partment of Health Contract Report No. 19, CaliforniaCommunity Studies on Pesticides, Jan 1-Dec 15, 1969.
11. Blanc PD, Rempel D, Maizlish N, Hiatt P, OlsonKR. Occupational illness: case detection by poison con-trol surveillance. Ann Intern Med. 1989 Aug 1;111(3):238-44.
12. Hayes WJ. Mortality in 1969 from pesticides, in-cluding aerosols. Arch Environ Health. 1976 Mar-Apr;31(2):61-72.
13. Hayes WJ Jr., Pirkle CI. Mortality from pesti-cides in 1961. Arch Environ Health. 1966 Jan;12(1):43-55.
14. Hayes WJ Jr., Vaughn WK. Mortality from pesti-cides in the United States in 1973 and 1974. ToxicolAppl Pharmacol. 1977 Nov;42(2):235-52.
15. Rettig BA, Klein DK, Sniezek JE. The incidenceof hospitalizations and emergency room visits resultingfrom exposure to chemicals used in agriculture. NebrMed J. 1987 Jul;72(7):215-9.
16. United States Code. 1972. Federal Insecticide,Fungicide, and Rodenticide Act (FIFRA), Title 7 UnitedStates Code, sections 135 et seq.
17. Kish L. Survey Sampling; 1965. New York: JWWiley and Sons, Inc.
18. State of California, Department of Finance, Pop-ulation of California. State and Counties, July 1,1990-1999, with 1990 and 2000 Census Counts; 2004[cited 2006 May 10]. Available from: http://www.dof.ca.gov/HTML/DEMOGRAP/I90-00.HTM.
19. Sribney WM. Two-way contingency tables forsurvey or clustered data. Stata Technical Bulletin. 1998;45:33-49.
20. Mehler L, Romano P, Samuels S, Schenker M.Pesticide Deaths in California, 1990-1996. CaliforniaEnvironmental Protection Agency, Department of Pes-ticide Regulation, Worker Health and Safety Branch;2001b. Report: HS-1821.
21. Mehler L, Romano P, Samuels S, Schenker M.Using routinely Collected Codes to Identify MedicalConsultations About Pesticide Health Effects in Califor-nia. California Environmental Protection Agency, De-
partment of Pesticide Regulation, Worker Health andSafety Branch; 2001a. Report: HS-1820.
22. Klein-Schwartz W, Smith GS. Agricultural andhorticultural chemical poisonings: mortality and mor-bidity in the United States. Ann Emerg Med. 1997Feb;29(2):232-8.
23. Lamminpää A, and Riihimäki V. Pesticide-re-lated incidents treated in Finnish hospitals–a review ofcases registered over a 5-year period. Hum Exp Toxicol.1992 Nov;11(6), 473-9.
24. Persson H, Palmborg M, Irestedt B, Westberg U.Pesticide poisoning in Sweden–actual situation andchanges over a 10 year period. Przegl Lek. 1997;54(10):657-61.
25. Swinker M, Smith CG, Shy C, Storm J. Pesticidepoisoning cases in North Carolina, 1990-1993. A retro-spective review. N C Med J. 1999 Mar-Apr;60(2): 77-82.
26. Caldwell ST, Barker M, Schuman SH, SimpsonWM Jr. Hospitalized pesticide poisonings decline inSouth Carolina, 1992-1996. J S C Med Assoc. 1997Dec;93(12):448-52.
27. Teutsch SM, Churchill RE, editors. Principlesand Practice of Public Health Surveillance. Oxford: Ox-ford University Press; 1994, p. 36.
28. UCLA Center for Health Policy Research. Cali-fornia Health Interview Survey, Findings from CHIS2001; 2002 [cited 2006 May 10]. Available from: http://www.chis.ucla.edu/.
29. Hook EB, Regal RR. The value of capture-recap-ture methods even for apparent exhaustive surveys. AmJ Epidemiol. 1992 May 1;135(9):1060-7.
30. International Working Group for Disease Moni-toring and Forecasting. Capture-recapture and multi-ple-record systems estimation I: history and theoreticaldevelopment. Am J Epidemiol. 1995;142(10):1047-58.
31. Keifer M, McConnell R, Pacheco AF, Daniel W,Rosenstock L. Estimating Underreported Pesticide Poi-sonings in Nicaragua. Am J Ind Med. 1996 Aug;30:195-201.
32. Osorio AM, Beckman J, Geiser CR, Husting EL,Inai A, Summerill KF. California Farm Survey of Occu-pational Injuries and Hazards. J Agric Saf Health. 1998;(1) (special issue):99-108.
RECEIVED: 11/02/2005REVISED: 02/27/2006
ACCEPTED: 03/29/2006
doi:10.1300/J096v11n02_10
76 JOURNAL OF AGROMEDICINE
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
APPENDIX A. ICD-9-CM Codes Selected for Review
Code Description
Specific to Pesticides9891 Toxic effects of strychnine and its salts9892 Toxic effects of chlorinated hydrocarbons, excluding chlorinated hydrocarbon solvents9893 Toxic effects of organophosphates and carbamates9894 Toxic effects of other pesticides and mixtures, not elsewhere classifiedE8614 Accidental poisoning by household and other disinfectants not ordinarily used on the personE8630 Accidental poisoning by insecticides of organochlorine compoundsE8631 Accidental poisoning by insecticides of organophosphorus compoundsE8632 Accidental poisoning by carbamatesE8633 Accidental poisoning by mixtures of insecticidesE8634 Accidental poisoning by other and unspecified insecticidesE8635 Accidental poisoning by herbicidesE8636 Accidental poisoning by fungicidesE8637 Accidental poisoning by rodenticidesE8638 Accidental poisoning by fumigantsE8639 Accidental poisoning by other and unspecified pesticidesE9506 Suicide and self-inflicted poisoning by agricultural and horticultural chemical and
pharmaceutical preparations other than plant foods and fertilizersE9807 Poisoning by agricultural and horticultural chemical and pharmaceutical preparations other
than plant foods and fertilizers, undetermined whether accidentally or purposely inflicted
Metals9840 Toxic effect of inorganic lead compounds9841 Toxic effect of organic lead compounds9848 Toxic effect of other lead compounds9849 Toxic effect of unspecified lead compounds9850 Toxic effect of mercury and its compounds9851 Toxic effect of arsenic and its compounds9854 Toxic effect of antimony and its compounds9859 Toxic effect of unspecified metalE8615 Accidental poisoning by lead paintsE8660 Accidental poisoning by lead and its compounds and fumesE8661 Accidental poisoning by mercury and its compounds and fumesE8662 Accidental poisoning by antimony and its compounds and fumesE8663 Accidental poisoning by arsenic and its compounds and fumesE8664 Accidental poisoning by other metals and their compounds and fumesE9508 Suicide and self-inflicted poisoning by arsenic and its compoundsE9808 Poisoning by arsenic and its compounds, undetermined whether accidentally or purposely
inflicted
Cleaners9896 Toxic effect of soaps and detergentsE8610 Accidental poisoning by synthetic detergents and shampoosE8611 Accidental poisoning by soap productsE8612 Accidental poisoning by polishesE8613 Accidental poisoning by other cleansing and polishing agentsE8619 Accidental poisoning by unspecified cleansing and polishing agents
Miscellaneous Toxicants9821 Toxic effect of carbon tetrachloride9822 Toxic effect of carbon disulfide9873 Toxic effect of sulfur dioxide9875 Toxic effect of lacrimogenic gas9876 Toxic effect of chlorine gas9877 Toxic effect of hydrocyanic acid gas
Special Features 77
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
Miscellaneous Toxicants (continued)9890 Toxic effect of hydrocyanic acid and cyanides98984 Toxic effect of tobaccoE8624 Accidental poisoning by other specified solventsE8665 Accidental poisoning by plant foods and fertilizers, excluding mixtures with herbicidesE8691 Accidental poisoning by sulfur dioxideE8693 Accidental poisoning by lacrimogenic gas
Caustics and Corrosives9830 Toxic effect of corrosive aromatics9831 Toxic effect of acids9839 Toxic effect of unspecified causticE8640 Accidental poisoning by corrosive aromaticsE8641 Accidental poisoning by acidsE8643 Accidental poisoning by other specified corrosives and causticsE8644 Accidental poisoning by unspecified corrosives and causticsE9507 Suicide and self-inflicted poisoning by corrosive and caustic substancesE9806 Poisoning by corrosive and caustic substances, undetermined whether accidentally or
purposely inflicted
Alcohols9800 Toxic effect of ethyl alcohol9801 Toxic effect of methyl alcohol9802 Toxic effect of isopropyl alcohol9808 Toxic effect of other specified alcohol9809 Toxic effect of unspecified alcoholE8601 Accidental poisoning by ethyl alcoholE8602 Accidental poisoning by methyl alcoholE8603 Accidental poisoning by isopropyl alcoholE8608 Accidental poisoning by other specified alcoholsE8609 Accidental poisoning by unspecified alcohol
Irritant Effects5060 Bronchitis and pneumonitis due to fumes and vapors5061 Acute pulmonary edema due to fumes and vapors5062 Upper respiratory inflamation due to fumes and vapors5063 Other acute and subacute respiratory conditions due to fumes and vapors5064 Chronic respiratory conditions due to fumes and vapors5069 Unspecified respiratory conditions due to fumes and vapors6924 Contact dermatitis due to chemical products other than detergents, oils, greases, and
solvents9400 Chemical burn of eyelids and periocular area947 Burn of internal organs9470 Burn of mouth and pharynx9471 Burn of larynx, trachea, and lung9472 Burn of esophagus9473 Burn of gastrointestinal tract
Other/Unspecified Toxicants9878 Toxic effect of other specified gases, fumes, or vapors9879 Toxic effect of unspecified gases, fumes, or vapors9898 Toxic effect of other substances, chiefly nonmedicinal as to source9899 Toxic effect of unspecified substance, chiefly nonmedicinal as to sourceE8629 Accidental poisoning by unspecified solventE8668 Accidental poisoning by other specified solid or liquid substancesE8669 Accidental poisoning by unspecified solid or liquid substanceE8698 Accidental poisoning by other specified gases and vapors
78 JOURNAL OF AGROMEDICINE
APPENDIX A (continued)
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014
E8699 Accidental poisoning by unspecified gases and vaporsE9292 Late effects of accidental poisoningE9509 Suicide and self-inflicted poisoning by other and unspecified solid and liquid substancesE9528 Suicide and self-inflicted poisoning by other specified gases and vaporsE9621 Assault by poisoning with other solid and liquid substancesE9622 Assault by poisoning with other gases and vaporsE9629 Assault by unspecifed poisoningE9809 Poisoning by other and unspecified solid and liquid substances, undetermined whether
accidentally or purposely inflictedE9828 Poisoning by other specified gases and vapors, undetermined whether accidentally or
purposely inflictedE9829 Poisoning by unspecified gases and vapors, undetermined whether accidentally or purposely
inflicted
APPENDIX B. Poison Control Generic Substance Codes Selected for Review
Code Description
4562 Pesticidal arsenic9000 Carbon tetrachloride12563 Cyanide rodenticide17000 2,4-D; 2,4,5-T33000 Naphthalene mothballs38000 Organophosphates38560 OP-carbamate combination38561 OP-organochlorine combination38562 OP-other pesticide combination39282 Pine oil40280 Phenolic disinfectant42280 Bleach42280 Hypochlorites42281 Hypochlorites, non-bleach43000 Strychnine rodenticide48563 Anticoagulant rodenticide48564 Long-acting anticoagulant rodenticide49000 Paraquat49561 Paraquat/diquat49562 Diquat50000 Organochlorine50430 p-DCB mothballs50560 Organochlorine + other62562 Pesticidal borates70000 Carbamates70560 Carbamate + other77121 Plant hormones77286 Other/unknown disinfectant77360 Essential oils77430 Unknown mothball77431 Other mothball
77439 Other aquarium/swimming pool products77561 Other herbicide77562 Other insecticide/pesticide77563 Other rodenticide77564 Mercurial fungicide77565 Non-mercurial fungicide77566 Other/unknown fungicide77567 Unknown herbicide77568 Veterinary pesticide77569 Unknown insecticide/pesticide77577 Unknown rodenticide115441 Muriatic acid116400 Gas generated by acid + hypochlorite116401 Chlorine gas144000 Pyrethrin/piperonyl butoxide144001 Pyrethrin145000 Rotenone149000 Formaldehyde/formalin162000 Monofluoroacetate (1080)174000 Antu176000 Piperonyl butoxide197000 Vacor/pnu213000 Triazine herbicide215000 Urea herbicide217000 Thallium218000 Insect repellant243561 Carbamate herbicide243566 Carbamate fungicide244577 Barium carbonate rodenticide253000 Phthalimide fungicide254370 Anti-algal paint254371 Wood preservative
Special Features 79
Dow
nloa
ded
by [
Uni
vers
ity o
f C
alif
orni
a D
avis
] at
12:
15 1
9 Fe
brua
ry 2
014